Abstract
Background
Neck pain is common, disabling and costly. Exercise is one treatment approach.
Objectives
To assess the effectiveness of exercises to improve pain, disability, function, patient satisfaction, quality of life and global perceived effect in adults with neck pain.
Search methods
We searched MEDLINE, MANTIS, ClinicalTrials.gov and three other computerized databases up to between January and May 2014 plus additional sources (reference checking, citation searching, contact with authors).
Selection criteria
We included randomized controlled trials (RCTs) comparing single therapeutic exercise with a control for adults suffering from neck pain with or without cervicogenic headache or radiculopathy.
Data collection and analysis
Two review authors independently conducted trial selection, data extraction, 'Risk of bias' assessment and clinical relevance. The quality of the evidence was assessed using GRADE. Meta‐analyses were performed for relative risk and standardized mean differences (SMD) with 95% confidence intervals (CIs) after judging clinical and statistical heterogeneity.
Main results
Twenty‐seven trials (2485 analyzed /3005 randomized participants) met our inclusion criteria.
For acute neck pain only, no evidence was found.
For chronic neck pain, moderate quality evidence supports 1) cervico‐scapulothoracic and upper extremity strength training to improve pain of a moderate to large amount immediately post treatment [pooled SMD (SMDp) ‐0.71 (95% CI: ‐1.33 to ‐0.10)] and at short‐term follow‐up; 2) scapulothoracic and upper extremity endurance training for slight beneficial effect on pain at immediate post treatment and short‐term follow‐up; 3) combined cervical, shoulder and scapulothoracic strengthening and stretching exercises varied from a small to large magnitude of beneficial effect on pain at immediate post treatment [SMDp ‐0.33 (95% CI: ‐0.55 to ‐0.10)] and up to long‐term follow‐up and a medium magnitude of effect improving function at both immediate post treatment and at short‐term follow‐up [SMDp ‐0.45 (95%CI: ‐0.72 to ‐0.18)]; 4) cervico‐scapulothoracic strengthening/stabilization exercises to improve pain and function at intermediate term [SMDp ‐14.90 (95% CI:‐22.40 to ‐7.39)]; 5) Mindfulness exercises (Qigong) minimally improved function but not global perceived effect at short term. Low evidence suggests 1) breathing exercises; 2) general fitness training; 3) stretching alone; and 4) feedback exercises combined with pattern synchronization may not change pain or function at immediate post treatment to short‐term follow‐up. Very low evidence suggests neuromuscular eye‐neck co‐ordination/proprioceptive exercises may improve pain and function at short‐term follow‐up.
For chronic cervicogenic headache, moderate quality evidence supports static‐dynamic cervico‐scapulothoracic strengthening/endurance exercises including pressure biofeedback immediate post treatment and probably improves pain, function and global perceived effect at long‐term follow‐up. Low grade evidence supports sustained natural apophyseal glides (SNAG) exercises.
For acute radiculopathy, low quality evidence suggests a small benefit for pain reduction at immediate post treatment with cervical stretch/strengthening/stabilization exercises.
Authors' conclusions
No high quality evidence was found, indicating that there is still uncertainty about the effectiveness of exercise for neck pain. Using specific strengthening exercises as a part of routine practice for chronic neck pain, cervicogenic headache and radiculopathy may be beneficial. Research showed the use of strengthening and endurance exercises for the cervico‐scapulothoracic and shoulder may be beneficial in reducing pain and improving function. However, when only stretching exercises were used no beneficial effects may be expected. Future research should explore optimal dosage.
Keywords: Adult; Female; Humans; Male; Physical Therapy Modalities; Acute Pain; Acute Pain/therapy; Chronic Pain; Chronic Pain/therapy; Headache; Headache/etiology; Headache/therapy; Manipulation, Chiropractic; Manipulation, Chiropractic/methods; Neck; Neck Pain; Neck Pain/etiology; Neck Pain/therapy; Pain Management; Pain Management/methods; Radiculopathy; Radiculopathy/therapy; Randomized Controlled Trials as Topic
Plain language summary
Exercise for Neck Pain
Review question
We reviewed the evidence about the effect of exercise therapy on pain, disability, patient satisfaction, and quality of life among people with neck pain.
Background
Neck pain is common; it can limit a person's ability to participate in normal activities and is costly. Exercise therapy is a widely used treatment for neck pain. This review includes active exercises (including specific neck and shoulder exercises, stretching, strengthening, postural, breathing, cognitive, functional, eye‐fixation and proprioception exercises) prescribed or performed in the treatment of neck pain. Studies in which exercise therapy was given as part of a multidisciplinary treatment, multimodal treatment (along with other treatments such as manipulation or ultrasound), or exercises requiring application by a trained individual (such as hold‐relax techniques, rhythmic stabilization, and passive techniques) were excluded.
Study characteristics
The evidence is current to May 2014. We found 27 trials (with a total of 2485 participants) examining whether exercise can help reduce neck pain and disability; improve function, global perceived effect, patient satisfaction and/or quality of life. In these trials, exercise was compared to either a placebo treatment, or no treatment (waiting list), or exercise combined with another intervention was compared with that same intervention (which could include manipulation, education/advice, acupuncture, massage, heat or medications). Twenty‐four of 27 trials evaluating neck pain reported on the duration of the disorder: 1 acute; 1 acute to chronic; 1 subacute; 4 subacute/chronic; and 16 chronic. One study reported on neck disorder with acute radiculopathy; two trials investigated subacute to chronic cervicogenic headache.
Key results
Results showed that exercise is safe, with temporary and benign side effects, although more than half of the trials did not report on adverse effects. An exercise classification system was used to ensure similarity between protocols when looking at the effects of different types of exercises. Some types of exercise did show an advantage over the other comparison groups. There appears to be a role for strengthening exercises in the treatment of chronic neck pain, cervicogenic headache and cervical radiculopathy if these exercises are focused on the neck, shoulder and shoulder blade region. Furthermore, the use of strengthening exercises, combined with endurance or stretching exercises has also been shown to be beneficial. There is some evidence to suggest the beneficial effects of specific exercises (e.g. sustained natural apophyseal glides) with cervicogenic headaches and mindfulness exercises (e.g. Qigong) for chronic mechanical neck pain. There appears to be minimal effect on neck pain and function when only stretching or endurance type exercises are used for the neck, shoulder and shoulder blade region.
Quality of the evidence
No high quality evidence was found, indicating that there is still uncertainty about the effectiveness of exercise for neck pain. Future research is likely to have an important impact on the effect estimate.There were a number of challenges with this review; for example, the number of participants in most trials was small, more than half of the included studies were either of low or very low quality and there was limited evidence on optimum dosage requirements.
Summary of findings
Summary of findings for the main comparison. Chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION compared to THAT SAME INTERVENTION.
| Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION compared to THAT SAME INTERVENTION for chronic mechanical neck disorders | |||
| Patient or population: patients with mechanical neck disorders Settings: ambulatory care clinic Intervention: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION Comparison: THAT SAME INTERVENTION | |||
| Outcomes | Effects | No of Participants (studies) | Quality of the evidence (GRADE) |
|
Pain Intensity: VAS 0 no pain to 10 worst pain (follow‐up: 6 months) |
Three trials showed a small reduction in pain. Pooled scores estimated using a mean difference of ‐0.67 (‐1.32 to ‐0.02) |
241 (3 studies: Bronfort 2011, Chiu 2005, Franca 2008) | ⊕⊕⊕⊝ moderate1 |
| Function: NDI 0 no disability to 50 maximum disability (follow‐up: 6 months) | Three trials showed a small to moderate improvement in function. Pooled scores estimated using a mean difference of ‐2.80 (‐6.36 to 0.76) |
241 (3 studies: Bronfort 2011, Chiu 2005, Franca 2008) | ⊕⊕⊕⊝ moderate1 |
|
Quality of Life: SF‐36 (physical component) 0 worse to 100 better, SF‐12. (follow‐up: Immediate post treatment) |
Two trials showed no significant difference Pooled scores estimated using a standard mean difference of ‐0.18 (‐0.48 to 0.13) |
165 (2 studies: Bronfort 2001, Martel 2011) |
⊕⊕⊝⊝ low1 |
|
Patient Satisfaction: 1 to 7; completely satisfied to completely dissatisfied (follow‐up: 24 months) |
One trial showed moderate improvement in satisfaction Scores estimated using a standard mean difference of ‐0.93 (‐1.35 to ‐0.52) |
101 (1 study: Bronfort 2001) |
⊕⊕⊕⊝ moderate |
|
Global Perceived Effect: Patient‐ Rated Improvement 1 more improvement to 9 less improvement (follow‐up: 24 months) |
One trial showed a small to moderate improvement in global perceived effect Scores estimated using a standard mean difference of ‐0.42 (‐0.81 to ‐0.03) |
101 (1 study: Bronfort 2001) |
⊕⊕⊕⊝ moderate |
| Adverse Effects | One study reported increased neck or headache pain: Intervention group (n = 8), comparison group (n = 6); increased radicular pain intervention group (n = 1); severe thoracic pain comparison group (n = 1); all cases self‐limiting and no permanent injuries (Bronfort 2001). 3 trials reported no complications or serious adverse events (Chiu 2005, Franca 2008, Martel 2011) | ||
| Moderate quality evidence: (4 trials, 341 participants, Bronfort 2001; Chiu 2005; Franca 2008; Martel 2011) shows moderate pain relief and improved function up to long‐term follow‐up for combined cervical, scapulothoracic stretching and strengthening for chronic neck pain. A clinician may need to treat 6 to18 people to achieve this type of pain relief and 4 to 13 to achieve this functional benefit. Moderate quality evidence (one trial, 101 participants; Bronfort 2001) demonstrates patients are very satisfied with their care. Changes in quality of life are suggestive of benefit but not conclusive. Changes in global perceived effect measures indicate a difference immediately post treatment and at long‐term follow‐up. | |||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||
1 Two of the pooled studies had high risk of bias scores (Franca 4/12 and Martel 5/12). That is, the studies met fewer than 6 of the 12 criteria, indicating high risk of bias.
Summary of findings 2. Chronic MND: Cervical Stretch/ROM Exercises + Cervical/Scapulothoracic Strengthening + Static/Dynamic Cervical/Shoulder Stabilization compared to WAIT LIST.
| Cervical Stretch/ROM Exercises + Cervical/Scapulothoracic Strengthening + Static/Dynamic Cervical/Shoulder Stabilization compared to WAIT LIST for mechanical neck disorders | |||
| Patient or population: patients with chronic mechanical neck disorders Settings: residential community Intervention: Cervical Stretch/ROM Exercises + Cervical/Scapulothoracic Strengthening + Static/Dynamic Cervical/Shoulder Stabilization Comparison: WAIT LIST | |||
| Outcomes | Effects | No of Participants (studies) | Quality of the evidence (GRADE) |
|
Pain Intensity: VAS 0 no pain to 100 worst pain; (follow‐up: immediate post treatment) a. 12 weeks of treatment b. 24 weeks of treatment or 12 weeks of treatment+ 12 weeks follow‐up |
Two trials showed a medium reduction in pain. a. Pooled mean difference ‐14.90 (‐22.40 to ‐7.39) b. Pooled mean difference ‐10.94 (‐18.81 to ‐3.08) |
147 (2 studies: Rendant 2011, von Trott 2009) | ⊕⊕⊕⊝ moderate1,2 |
|
Function: NPDI or NDI 0 no disability to 100 maximum disability; (follow‐up: immediate post treatment)
a. 12 weeks of treatment b. 24 weeks of treatment or 12 weeks treatment + 12 weeks follow‐up |
Two trials showed a medium improvement in function. a. Pooled SMD ‐0.50 (‐1.04 to 0.03) b. Pooled SMD ‐0.40 (‐0.74 to ‐0.06) |
147 (2 studies: Rendant 2011, von Trott 2009) | ⊕⊕⊕⊝ moderate1,2 |
|
Quality of Life: SF‐36 (physical component) 0 worse to 100 better; (follow‐up: immediate post treatment) a. 12 weeks of treatment b. 24 weeks of treatment or 12 weeks treatment + 12 weeks follow‐up |
Two trials showed no significant difference in quality of life scores a. Pooled mean difference ‐2.22 (‐5.17 to 0.72) b. Pooled mean difference 0.06 (‐4.06 to 4.17) |
143 (2 studies: Rendant 2011, von Trott 2009) | ⊕⊕⊕⊝ moderate1,2 |
|
Global Perceived Effect: General Health Perception 0 worse to 100 better (follow‐up: immediate post treatment) a. 12 weeks of treatment b. 24 weeks of treatment |
One trial showed no significant difference in GPE. | 70 (1 study: von Trott 2009) |
⊕⊕⊕⊝ moderate2 |
| Adverse Effects | Reported by 18 patients in exercise group: muscle soreness (n = 15), myogelosis (n = 11), headaches (n = 5), vertigo (n = 2), change in mood (n = 1), worsening of neck pain (n = 1), worsening of tinnitus (n = 1) , nausea (n = 1), muscle tensions (n = 2) | ||
| Moderate quality evidence (two trials, 147 participants, von Trott 2009; Rendant 2011) shows cervical stretch/ROM exercises + cervical/scapulothoracic strengthening + static/dynamic cervical/shoulder stabilization probably has moderate benefit for pain and function, but not GPE and QoL at immediate post treatment and short‐term follow‐up. A clinician may need to treat four people to achieve moderate degree of pain relief and five to achieve moderate functional benefit in one patient. | |||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||
1 One of the studies (Rendant 2011) scored 6/12 on 'Risk of bias' assessment.That is, the study met 6 or fewer than 6 of the 12 criteria, indicating high risk of bias. 2 Small studies
Summary of findings 3. Chronic MND: Qigong Stretch/ROM + Endurance Training + Dynamic Stabilization + Cognitive (mindfulness & emotional balance) compared to WAIT LIST.
| Stretch/ROM + Endurance Training + Dynamic Stabilization + Cognitive (mindfulness & emotional balance) compared to WAIT LIST for mechanical neck disorders | |||
| Patient or population: patients with chronic mechanical neck disorders Settings: residential community Intervention: Stretch/ROM + Endurance Training + Dynamic Stabilization + Cognitive (mindfulness & emotional balance) Comparison: WAIT LIST | |||
| Outcomes | Effects | No of Participants (studies) | Quality of the evidence (GRADE) |
|
Pain Intensity: VAS 0 no pain to 100 worst pain (follow‐up: immediate post treatment) a. 12 weeks of treatment b. 24 weeks of treatment or 12 treatments + 12 weeks follow‐up |
Two trials showed a moderate reduction in pain Pooled scores estimated using a a. Mean difference of ‐13.28 (‐20.98 to ‐5.58) b. Mean difference of ‐7.82 (‐14.57 to ‐1.07) |
148 (2 studies: Rendant 2011, von Trott 2009) | ⊕⊕⊕⊝ moderate1 |
|
Function: NPDI 0 no disability to 100 maximum disability (follow‐up: immediate post treatment) a. 12 weeks of treatment b. 24 weeks of treatment or 12 weeks treatment + 12 weeks follow‐up |
Two trials showed a small improvement in function Pooled scores estimated using a a. Standard mean difference of ‐0.36 (‐0.68 to ‐0.03) b. Standard mean difference of ‐0.28 (‐0.68 to 0.11) |
148 (2 studies: Rendant 2011, von Trott 2009) | ⊕⊕⊕⊝ moderate1 |
|
Quality of Life: SF‐36 (physical component) 0 worse to 100 better (follow‐up: immediate post treatment) a. 12 weeks of treatment b. 24 weeks of treatment or 12 weeks treatment + 12 weeks follow‐up |
Two trials showed little to no difference in quality of life Pooled scores estimated using a a. Mean difference of ‐2.72 (‐5.42 to ‐0.01) b. Mean difference of ‐1.88 (‐5.80 to 2.04) |
148 (2 studies: Rendant 2011, von Trott 2009) | ⊕⊕⊕⊝1 moderate |
| Global Perceived Effect: General Health Perception 0 worse to 100 better (follow‐up immediate post treatment and short‐term) | One trial showed no significant difference in GPE. | 70 (1 study: von Trott 2009) |
⊕⊕⊕⊝ moderate1,2 |
| Adverse Effects | Reported by 23 patients in qigong group including: muscle soreness (n = 17), myogelosis (n = 12), vertigo (n = 10), other pain (n = 4), headache (n = 3), thirst (n = 1), engorged hands (n = 1), twinge in the neck (n = 1), urinary urgency (n = 1), bursitis of left shoulder (n = 1), nausea (n = 2), muscle tension (n = 1) | ||
| Moderate quality evidence: (2 trials, 148 participants, Rendant 2011; von Trott 2009) shows Qigong exercises (Dantian Qigong) may improve pain and function slightly when compared with a wait list control at immediate and short‐term follow‐up. It may have little or no benefit at immediate and short‐term follow‐up on quality of life and global perceived effect. A clinician may need to treat four to six people to achieve this type of pain relief, five to eight people to achieve this functional benefit, and seven to 10 people for this improvement in quality of life. | |||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||
1 One included study (Rendant 2011) scored 6/12 on risk of bias assessment.That is, the study met 6 or fewer than 6 of the 12 criteria, indicating high risk of bias. 2 Small studies.
Summary of findings 4. Acute Radiculopathy: Cervical Stretch/ROM + Cervical/Scapulothoracic/UE Strengthening + Static/Dynamic Cervical Stabilization vs WAIT LIST.
| Cervical Stretch/ROM + Cervical/Scapulothoracic/UE Strengthening + Static/Dynamic Cervical Stabilization compared with wait list for acute radiculopathy | |||
|
Patient or population: patients with acute radiculopathy Settings: Three hospitals in Netherlands Intervention: Cervical Stretch/ROM + Cervical/Scapulothoracic/UE Strengthening + Static/Dynamic Cervical Stabilization Comparison: Wait list | |||
| Outcomes | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) |
|
Pain Intensity: VAS 0 no pain to 10 worst pain (follow‐up: immediate post treatment) a. 6 weeks of treatment (follow‐up period after treatment) b. 6 months |
One trial showed a small reduction in pain immediately post treatment and no benefit at 6 months follow‐up. a. Standard mean difference are ‐0.47 (‐0.81 to ‐0.12) post intervention b. Standard mean difference are 0.16 (‐0.19 to 0.51) at 6 months follow‐up. |
133 participants (1 study: Kuijper 2009) | ⊕⊕⊝⊝1,2 low |
|
Function: NDI 0 no disability to 50 maximum disability (follow‐up: immediate post treatment) a. 6 weeks of treatment (follow‐up period after treatment) b. 6 months |
One trial showed a small reduction in functional disability immediately post treatment and no benefit at 6 months follow‐up. a. Standard mean difference are ‐0.11 (‐0.45 to 0.23) post intervention. b. Standard mean difference are 0.06 (‐0.29 to 0.40) at 6 month follow‐up. |
133 participants (1 study: Kuijper 2009) | ⊕⊕⊝⊝1,2 low |
|
Patient Satisfaction: 5‐point scale, 1 to 5; very satisfied to unsatisfied (follow‐up: immediate post treatment) a. 6 weeks of treatment |
a. One trial showed no difference in patient satisfaction immediately post treatment. relative risk ratio are 0.92 (0.62 to 1.37) post intervention. | 129 participants (1 study: Kuijper 2009) | ⊕⊕⊝⊝1,2 low |
| Adverse Effects | Not reported | ||
| Low quality evidence: (one trial, 133 participants, Kuijper 2009) Cervical Stretch/ROM + Cervical/Scapulothoracic/UE Strengthening + Static/Dynamic Cervical Stabilization may improve pain slightly, but may make no difference in function and patient satisfaction when compared immediately post treatment with a control for acute cervical radiculopathy. However, there may be no difference in pain and functional improvement at intermediate‐term follow‐up. | |||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||
1 One included study (Kuijper 2009) scored 4/12 on risk of bias assessment.That is, the study met 6 or fewer than 6 of the 12 criteria, indicating high risk of bias. 2 Small study.
Summary of findings 5. Acute to subacute CGH: Cervical stretch/ROM vs SHAM.
| Cervical stretch/ROM vs SHAM compared with SHAM intervention for subAcute CGH | |||
|
Patient or population: patients with subAcute cervicogenic headache (CGH) Settings: Physiotherapy Private Practice Intervention: Cervical stretch/ROM Comparison: SHAM INTERVENTION | |||
| Outcomes | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) |
|
Pain Intensity: VAS 0 no pain to 100 worst pain (follow‐up: immediate post treatment ) a. 4 weeks of treatment (follow‐up period after treatment) b. 12 months |
One trial showed a small reduction in pain a. Standard mean difference are ‐1.58 (‐2.38 to ‐0.77) at 4 weeks b. Standard mean difference are ‐1.74 (‐2.57 to ‐0.91) at 12 months. |
32 (1 study: Hall 2007) |
⊕⊕⊝⊝ low1,2 |
| Adverse effects | Not reported | ||
| Low quality evidence: (one trial, 32 participants, Hall 2007 ) shows Cervical stretch/ROM may improve a large amount for pain reduction at short‐ and long‐term follow‐up with the use of C1 to C2 self‐SNAG exercises when compared with a sham for (sub)acute cervicogenic headache. A clinician may need to treat three people to achieve this type of long‐term pain relief. | |||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||
1 Percision: Small study (n=16 per arm).
2 Reporting bias: due to trial size and single outcome, future research is likely to influence the direction of reported effect. Replication in a second trial is needed.
Summary of findings 6. Chronic CGH: Cervical/Scapulothoracic Strengthening with Endurance Training + Craniocervical Pressure Biofeedback + Dynamic Cervical Stabilization vs NO INTERVENTION.
| Cervical/Scapulothoracic Strengthening with Endurance Training + Craniocervical Pressure Biofeedback + Dynamic Cervical Stabilization compared with NO INTERVENTION for Chronic CGH | |||
|
Patient or population: patients with chronic CGH Settings: multiple trial centres Intervention: Cervical/Scapulothoracic Strengthening with Endurance Training + Craniocervical Pressure Biofeedback + Dynamic Cervical Stabilization Comparison: NO INTERVENTION | |||
| Outcomes | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) |
|
Pain Intensity: VAS 0 no pain to 10 worst pain (follow‐up: immediate post treatment) a. 6 weeks (follow‐up period after treatment) b. 12 months |
One trial showed a large reduction in pain at 6 weeks and 12 months follow up. a. Standard mean difference are ‐0.75 (‐1.16 to ‐0.34) at 6 weeks b. Standard mean difference are ‐0.59 (‐1.00 to ‐0.18) at 12 months follow‐up. |
97 (1 study: Jull 2002) |
⊕⊕⊕⊝ moderate1 |
|
Function: NPNPQ 0% no disability to 100% maximum disability (follow‐up: immediate post treatment) a. 6 weeks (follow‐up period after treatment) b. 12 months |
One trial showed a moderate reduction in functional disability a. Standard mean difference are ‐0.56 (‐0.96 to ‐0.15) at 6 weeks b. Standard mean difference are ‐0.70 (‐1.11 to 0.29) at 12 months follow‐up. |
97 (1 study: Jull 2002) |
⊕⊕⊕⊝ moderate1 |
|
Global Perceived Effect: VAS 0 to 100 (follow‐up: immediate post treatment) a. 6 weeks (follow‐up period after treatment) b. 12 months |
One trial showed a large benefit in global perceived effect a. Standard mean difference are ‐2.96 (‐3.55 to ‐2.38) at 6 weeks. b. Standard mean difference are ‐2.51 (‐3.05 to ‐1.97) at 12 months follow‐up. |
97 (1 study: Jull 2002) |
⊕⊕⊕⊝ moderate1 |
| Adverse effects | Minor and temporary adverse effects were noted: 6.7% of headaches were provoked by treatment | ||
| Moderate quality evidence: (one trial, 97 participants, Jull 2002) shows cervicoscapular strengthening and endurance exercises including pressure biofeedback probably improves pain, function and global perceived effect for chronic cervicogenic headaches at long term follow‐up when compared to no treatment. A clinician may need to treat six people to achieve this type of pain relief and functional benefit in one patient. | |||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||
1 Percision: Although small study, consistent findings are noted across multiple outcomes at long term follow‐up.
Summary of findings 7. Chronic CGH: Cervical/Scapulothoracic Strengthening with Endurance Training + Craniocervical Pressure Biofeedback + Dynamic Cervical Stabilization + Manual Therapy vs Manual Therapy.
| Cervical/Scapulothoracic Strengthening with Endurance Training + Craniocervical Pressure Biofeedback + Dynamic Cervical Stabilization + Manual Therapy compared with Manual Therapy for Chronic CGH | |||
|
Patient or population: patients with Chronic CGH Settings: multiple trial centres Intervention: Cervical/Scapulothoracic Strengthening with Endurance Training + Craniocervical Pressure Biofeedback + Dynamic Cervical Stabilization + Manual Therapy Comparison: MANUAL THERAPY | |||
| Outcomes | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) |
|
Pain Intensity: 6 weeks treatment VAS 0 no pain to 10 worst pain (follow‐up: immediate post treatment) a. 6 weeks (follow‐up period after treatment) b. 12 months |
One trial showed a small reduction in pain a. Standard mean difference are ‐0.11 (‐0.50 to 0.29) at 6 weeks b. Standard mean difference are ‐0.17 (‐0.57 to 0.23) at 12 months follow‐up. |
96 (1 study: Jull 2002) |
⊕⊕⊕⊝ moderate1 |
|
Function: NPNPQ 0% no disability to 100% maximum disability (follow‐up: immediate post treatment) a. 6 weeks of treatment (follow‐up period after treatment) b. 12 months |
One trial showed a small reduction in functional disability a. Standard mean difference are ‐0.11 (‐0.51 to 0.28) at 6 weeks b. Standard mean difference are ‐0.23 (‐0.63 to 0.17) at 12 months follow‐up. |
96 (1 study: Jull 2002) |
⊕⊕⊕⊝ moderate1 |
|
Global Perceived Effect: VAS 0 to 100 (follow‐up: immediate post treatment) a. 6 weeks of treatment (follow‐up period after treatment) b. 12 months |
One trial showed a small benefit in global perceived effect a. Standard mean difference are ‐0.29 (‐0.68 to 0.11) at 6 weeks b. Standard mean difference ‐0.30 (‐0.70 to 0.10) at 12 months follow‐up. |
96 (1 study: Jull 2002) |
⊕⊕⊕⊝ moderate1 |
| Adverse effects | Minor and temporary adverse effects were noted: 6.7% of headaches were provoked by treatment | ||
| Moderate quality evidence (one trial, 96 participants, Jull 2002) shows when exercise combined with manual therapy contrasted with manual therapy alone there is probably no difference in pain, function and global perceived effect for chronic cervicogenic headaches at long‐term follow‐up. | |||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||
1 Percision: Although small study, consistent findings are noted across multiple outcomes at long term follow‐up.
Summary of findings 8. Chronic MND: Cervical/UE Stretch/ROM Exercise + Cervical/UE Strengthening + Dynamic Cervical Stabilization vs PLACEBO or SHAM.
| Cervical/UE Stretch/ROM Exercise + Cervical/UE Strengthening + Dynamic Cervical Stabilization compared with PLACEBO or SHAM for Chronic MND | |||
|
Patient or population: patients with chronic MND Settings: Primary care physical therapy and private physical therapy practices Intervention: Cervical/UE Stretch/ROM Exercise + Cervical/UE Strengthening + Dynamic Cervical Stabilization Comparison: PLACEBO or SHAM | |||
| Outcomes | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) |
|
Pain Intensity: VAS 0 no pain to 100 worst pain (follow‐up: immediate post treatment) a. 2 months of treatment (follow‐up period after treatment) b. 6 months c. 12 months |
One trial showed no difference in pain immediately post intervention and at 6 and 12 months follow‐up. a. Standard mean difference 0.26 (‐0.33 to 0.85) immediately 2 months post intervention. b. Standard mean difference ‐0.16 (‐0.75 to 0.43) at 6 months follow‐up. c. Standard mean difference ‐0.19 (‐0.40 to 0.78) at 12 months follow‐up. |
77 (1 study: Kjellman 2002) |
⊕⊕⊝⊝ low1,2 |
|
Function: 2 months treatment NDI 0 no disability to 50 maximum disability (follow‐up: immediate post treatment) a. 2 months of treatment (follow‐up period after treatment ) b. 6 months c. 12 months |
One trial showed no difference in function immediately post intervention and at 6 and 12 months follow‐up. a. Standard mean difference are 0.14 (‐0.45 to 0.73) immediately post 2 months intervention. b. Standard mean difference ‐0.06 (‐0.66 to 0.53) at 6 months follow‐up. c. Standard mean difference 0.12 (‐0.47 to 0.72) at 12 months follow‐up. |
77 (1 study: Kjellman 2002) |
⊕⊕⊝⊝ low1,2 |
| Adverse effects | Not reported | ||
| Low quality evidence: (One trial, 77 participants, Kjellman 2002) No difference for pain relief and function immediately post intervention, at 6 and 12 months follow‐up using Cervical/UE Stretch/ROM Exercise + Cervical/UE Strengthening + Dynamic Cervical Stabilization for chronic MND. | |||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||
1 One of the studies (Kjellman 2002)) scored 5/12 on 'Risk of bias' assessment.That is, the study met 6 or fewer than 6 of the 12 criteria, indicating high risk of bias. 2 Small studies
Summary of findings 9. Chronic MND: Cervical Stretch/ROM Exercises + Dynamic Cervical Stabilization vs SHAM.
| Cervical Stretch/ROM Exercise + Dynamic Cervical Stabilization compared with SHAM for Chronic MND | |||
|
Patient or population: patients with chronic MND Settings: Primary care physical therapy and private physical therapy practices Intervention: Cervical/UE Stretch/ROM Exercise + Cervical/UE Strengthening + Dynamic Cervical Stabilization Comparison: PLACEBO or SHAM | |||
| Outcomes | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) |
|
Pain Intensity: VAS 0 no pain to 100 worst pain (follow‐up: immediate post treatment) a. 2 months of treatment (follow‐up period after treatment) b. 6 months c. 12 months |
One trial showed no difference in pain immediately post intervention and at 6 and 12 months follow‐up. a. Standard mean difference are ‐0.10 (‐0.66 to 0.45) immediately post 2 months intervention. b. Standard mean difference ‐0.29 (‐0.85 to 0.27) at 6 months follow‐up. c. Standard mean difference 0.04 (‐0.51 to 0.60) at 12 months follow‐up. |
50 (1 study: Kjellman 2002) |
⊕⊕⊝⊝ low1,2 |
|
Function: NDI 0 no disability to 50 maximum disability (follow‐up: immediate post treatment) a. 2 months of treatment (follow‐up period after treatment ) b. 6 months c. 12 months |
One trial showed no difference in function immediately post intervention and at 6 and 12 months follow‐up. a. Standard mean difference are ‐0.24 (‐0.79 to 0.32) immediately post 2 month intervention. b. Standard mean difference ‐0.22 (‐0.79 to 0.36) at 6 months follow‐up c. Standard mean difference 0.14 (‐0.44 to 0.71) at 12 months follow‐up. |
50 (1 study: Kjellman 2002) |
⊕⊕⊝⊝ low1,2 |
| Adverse effects | Not reported | ||
| Low quality evidence: (One trial, 50 participants, Kjellman 2002) No difference for pain relief and function immediately post intervention, at 6 and 12 month follow‐up using Cervical Stretch/ROM Exercise + Dynamic Cervical Stabilization for chronic MND. | |||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||
1 One of the studies (Kjellman 2002) scored 5/12 on 'Risk of bias' assessment.That is, the study met 6 or fewer than 6 of the 12 criteria, indicating high risk of bias. 2 Small studies
Summary of findings 10. Chronic MND: Cervical/Scapulothoracic/UE Stretch + UE Endurance Training vs NO INTERVENTION or WAIT LIST.
| Chronic MND: Cervical/Scapulothoracic/UE Stretch + UE Endurance Training compared with NO INTERVENTION or WAIT LIST for chronic MND | ||||
|
Patient or population: patients with chronic MND Settings: office workers Intervention: Cervical/Scapulothoracic/UE Stretch + UE Endurance Training Comparison: NO INTERVENTION or WAIT LIST |
||||
| Outcomes | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) | |
|
Pain Intensity: VAS 0 no pain to 100 worst pain (follow‐up: immediate post treatment) a. 12 weeks of treatment (follow‐up period after treatment) b. 3 months c. 9 months |
One trial showed no difference in pain immediately post intervention and at 3 and 9 months follow‐up. a. Standard mean difference are 0.08 (‐0.16 to 0.32) immediately post 12 weeks intervention. b. Standard mean difference 0.00 (‐0.24 to 0.24) at 3 months follow‐up. c. Standard mean difference ‐0.04 (‐0.28 to 0.20) at 9 months follow‐up. |
393 (1 study: Viljanen 2003) |
⊕⊕⊕⊝ moderate1 | |
|
Function: NDI 0 no disability to 50 maximum disability (follow‐up: immediate post treatment) a. 12 weeks of treatment (follow‐up period after treatment) b. 3 months c. 9 months |
One trial showed no difference in function immediately post intervention and at 3 and 9 months follow up. a. Standard mean difference 0.07 (‐0.17 to 0.31) immediately post 12 weeks intervention. b. Standard mean difference 0.07 (‐0.17 to 0.31) at 3 months follow‐up. c. Standard mean difference 0.14 (‐0.11 to 0.38) at 9 months follow‐up. |
393 (1 study: Viljanen 2003) |
⊕⊕⊕⊝ moderate1 | |
| Adverse effects | Not reported | |||
| Moderate quality evidence: (one trial, 393 participants, Viljanen 2003) Little to no difference for pain relief and function immediately post intervention, at 3 and 9 months follow‐up using Cervical/Scapulothoracic/UE Stretch + UE Endurance Training for chronic MND. | ||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | ||||
1 Percision: high drop out rate (14%); reason for dropout not described.
Summary of findings 11. Acute to Chronic MND: Scapulothoracic/UE Endurance Training vs CONTROL.
| Scapulothoracic/UE Endurance Training compared with CONTROL for (sub)Acute/Chroninc MND | |||
|
Patient or population: patients with Acute to Chronic MND Settings: two large withe collar organizations Intervention: Scapulothoracic/UE Endurance Training Comparison: CONTROL | |||
| Outcomes | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) |
|
Pain Intensity: VAS 0 no pain to 10 worst pain (follow‐up: immediate post 10 weeks treatment) a. 2‐minute training group b. 12‐minute training group |
One trial showed moderate pain relief immediately post intervention. a. Standard mean difference for the 2 minute training group ‐0.66 (‐1.02 to ‐0.30). b. Standard mean difference for the 12 minute training group ‐0.59 (‐0.94 to ‐0.23). |
198 (1 study: Andersen 2011) |
⊕⊕⊕⊝ moderate1 |
| Adverse effects | Reported worsening of neck muscle tension during and/or in the days after training (2‐minute n = 1, 12‐minute n = 4), shoulder joint pain during training (2‐minute n = 1, 12‐minute n = 4), pain in the upper arm during training (2‐minute n = 1, 12‐minute n = 1), pain of the forearm/wrist during training (12‐minute n = 2), worsening of headache after training (2‐minute n = 1, 12‐minute n = 1). No long‐lasting or major complications resulted from the training program. | ||
| Moderate quality evidence: (one trial, 198 participants, Andersen 2011) Moderate benefit for pain relief immediately post intervention using Scapulothoracic/UE Endurance Training for (sub)Acute/Chronic MND. A clinician may need to treat four people to achieve this type of pain relief. | |||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||
1 Percision: small sample (n = 63 or 64 per Arm) measured at Immediate post treatment.
Summary of findings 12. Subacute to Chronic WAD: Trunk/Extremity Stretch/ROM + Trunk/Extremity Strengthening + Trunk/Extremity Endurance Training + Pattern/Synchronization: Coordination + Cardiovascular/Aerobic + Cognitive (CBT) + ANOTHER TREATMENT vs THAT SAME OTHER TREATMENT.
| Trunk/Extremity Stretch/ROM + Trunk/Extremity Strengthening + Trunk/Extremity Endurance Training + Pattern/Synchronization: Coordination + Cardiovascular/Aerobic + Cognitive (CBT) + ANOTHER TREATMENT compared with THAT SAME OTHER TREATMENT for Subacute/chronic WAD | |||
|
Patient or population: patients with subacute/chronic WAD Settings: two physiotherapy clinics Intervention: Trunk/Extremity Stretch/ROM + Trunk/Extremity Strengthening + Trunk/Extremity Endurance Training + Pattern/Synchronization: Coordination + Cardiovascular/Aerobic + Cognitive (CBT) + ANOTHER TREATMENT Comparison: THAT SAME OTHER TREATMENT | |||
| Outcomes | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) |
|
Pain Intensity: VAS 0 no pain to 10 worst pain (follow‐up: immediate post treatment) a. 6 weeks of treatment (follow‐up period after treatment) b. 12 months |
One trial showed small pain relief immediately post intervention and no difference at 12 months follow‐up. a. Standard mean difference ‐0.46 (‐0.81 to ‐0.12) immediately post 6 weeks intervention. b. Standard mean difference ‐0.12 (‐0.47 to 0.23) at 12 months follow‐up. |
132 (1 study: Stewart 2007) |
⊕⊕⊝⊝ low1,2 |
|
Function: NDI 0 no disability to 50 maximum disability (follow‐up: immediate post treatment) a. 6 weeks of treatment (follow‐up period after treatment) b. 12 months |
One trial showed small benefit in function immediately post intervention and at 12 months follow‐up. a. Standard mean difference ‐0.50 (‐0.85 to ‐0.15) immediately post 6 weeks intervention. b. Standard mean difference ‐0.39 (‐0.74 to ‐0.03) at 12 months follow‐up. |
132 (1 study: Stewart 2007) |
⊕⊕⊝⊝ low1,2 |
|
Global perceived effect: ‐5 to 5 scale; vastly worse to completely recovered (follow‐up: immediate post treatment) a. 6 weeks of treatment (follow‐up after treatment) b. 12 months |
One trial showed small benefit in global perceived effect immediately post intervention and no difference at 12 months follow‐up. a. Standard mean difference ‐0.46 (‐0.80 to ‐0.11) immediately post 6 weeks intervention. b. Standard mean difference ‐0.18 (‐0.54 to 0.17) at 12 months follow‐up. |
132 (1 study: Stewart 2007) |
⊕⊕⊝⊝ low1,2 |
|
Quality of Life: SF‐36 0 high disability to 100 no disability (follow‐up: immediate post treatment) a. 6 weeks of treatment (follow‐up after treatment) b. 12 months |
One trial showed small benefit in global perceived effect immediately post intervention and no difference at 12 month follow‐up. a. Standard mean difference ‐0.35 (‐0.69 to ‐0.01) immediately post 6 weeks intervention. b. Standard mean difference ‐0.15 (‐0.50 to 0.20) at 12 month follow‐up. |
132 (1 study: Stewart 2007) |
⊕⊕⊝⊝ low1,2 |
| Adverse effects | Reported; The main complaint in this group was muscle pain with exercise (3) followed by knee pain (2) and lumbar spine pain (2). | ||
| Low quality evidence: (one trial, 132 participants, Stewart 2007) Small benefit for pain relief, function, global perceived effect and quality of life immediately post treatment and small benefit at 12 month follow up for function using Trunk/Extremity Stretch/ROM + Trunk/Extremity Strengthening + Trunk/Extremity Endurance Training + Pattern/Synchronization: Coordination + Cardiovascular/Aerobic + Cognitive (CBT) + ANOTHER TREATMENT for Subacute/chronic WAD. | |||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||
1 One of the studies (Stewart 2007) scored 6/12 on 'Risk of bias' assessment.That is, the study met 6 or fewer than 6 of the 12 criteria, indicating high risk of bias. 2 Small studies
Summary of findings 13. Acute to Chronic MND: Scapulothoracic + UE Strengthening vs CONTROL.
| Scapulothoracic + UE Strengthening compared with CONTROL for (sub)Acute/Chronic MND | |||
|
Patient or population: patients with Acute to Chronic MND Settings: Seven workplaces Intervention: Scapulothoracic + UE Strengthening Comparison: CONTROL | |||
| Outcomes | Relative effect (95% CI) | No of Participants (studies) | Quality of the evidence (GRADE) |
| Pain Intensity: VAS 0 no pain to 100 worst pain (follow‐up: immediate post 10 to 20 weeks of treatment) | Three trials showed a moderate reduction in pain. Pooled scores estimated using a standard mean difference ‐0.71 (‐1.33 to ‐0.10). | 157 (3 studies: Andesen 2008, Andersen CH 2012, Dellve 2011) |
⊕⊕⊕⊝ moderate |
|
Pain Intensity: VAS 0 no pain to 100 worst pain (follow‐up: immediate post 20 weeks of treatment) a. 1 weekly session b. 9 weekly sessions |
One trial (two comparisons) showed no difference in pain relief immediately post intervention. a. One weekly session of 60 minutes, scores using a standard mean difference ‐0.20 (‐0.63 to 0.22). b. Nine weekly sessions of seven minutes, scores using a standard mean difference ‐0.13 (‐0.61 to 0.34). |
163 (1 study: three groups, Andersen CH 2012) |
⊝⊝⊝⊝ very low1 |
| Pain Intensity: VAS 0 no pain to 100 worst pain (follow‐up: immediate post 10 weeks of treatment) | One trial showed moderate reduction in pain 10 weeks post intervention. Scores using a standard mean difference ‐0.89 (‐1.76 to ‐0.01) at 10 week follow‐up. | 26 (1 study: Andersen 2008) |
⊕⊕⊝⊝ low |
|
Function: DASH 20% no difficulty to 100% fully unable (follow‐up: immediate post 20 weeks of treatment). a. 1 weekly session b. 9 weekly sessions |
One trial showed no difference in function immediately post intervention. a. Standard mean difference ‐0.17 (‐0.58 to 0.24) immediately post intervention for one weekly session of 60 minutes b. Standard mean difference ‐0.06 (‐0.53 to 0.41) for nine weekly sessions of seven minutes. |
163 (1 study: Andersen CH 2012) |
⊝⊝⊝⊝ very low1 |
| Work ability index: 7 poor ability to 49 excellent ability treatment (follow‐up: immediate post 20 weeks treatment) | One trial showed a small improvement in work ability immediately post intervention. Standard mean difference ‐0.23 (‐0.66 to 0.19) immediately post 20 weeks intervention. | 88 (1 study: Dellve 2011) |
⊕⊕⊝⊝ low |
| Adverse effects | Not reported | ||
| Moderate quality evidence: (3 trials, 157 participants, Andersen 2008, Andersen Ch 2012, Dellve 2011) that scapulothoracic and upper extremity strength training probably improves pain. It probably functional outcomes when compared to control for chronic mechanical neck pain immediately post treatment (10 or 20 week interventions). However low quality evidence suggests that scapulothoracic and upper extremity strength training may improve pain slightly. | |||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||
1 Design: 0, Limitations: ‐1, Inconsistency: 0, Indirectness: 0, Imprecision: ‐1, Other: ‐1 subgroup analysis.
Background
Description of the condition
Neck disorders are common (Hogg‐Johnson 2008; Hoy 2014), painful, and limit function in the general population (Carroll 2008a, Haldeman 2010,), workers (Côté 2008) and people with whiplash associated disorders (WAD) (Carroll 2008b; Buitenhuis 2009). The global point prevalence of neck pain was estimated to be 4.9% in 2010 (Hoy 2014). In the United States, 15.1% of adults state having had neck pain within the previous three months (NCHS 2013).
In 2005, the mean medical expenditure amongst Americans with spine problems was estimated to be $6096USD per individual annually compared with $3516USD amongst those without spine problems (Martin 2008). Côté 2008 reported 3% to 11% of claimants in the work force were sufficiently disabled to lose time from work each year. Direct and indirect costs are substantive (Martin 2008).
Description of the intervention
We adopted the Therapeutic Exercise Intervention Model to sub‐classify exercise (Sahrmann 2002). This model is based on the elements of movement system. Sahrmann 2002 originally described movement as a system made up of five elements. Hall 2005 further developed this concept into a three dimensional model. The elements of movement system intersect with two other axes ‐ activity and dosage. After determining which element of the movement system needs to be addressed to restore function, the activity or technique to achieve the functional goal is chosen. The dosage parameters are modified according to the tissues involved and the principles of tissue healing. A brief description of each element follows.
1.Support Element: An exercise categorized under this element would affect the functional status of the cardiac, pulmonary and metabolic systems (e.g. aerobic endurance activities).
2. Base Element: Exercises categorized under base element would affect the functional status of the muscular and skeletal systems and is commonly linked to the biomechanical element. This element provides the basis for movement as follows:
extensibility/stiffness properties of muscle, fascia and periarticular tissues for range of motion and stretching exercises,
mobility of neuromeningeal tissue for neural mobilization exercises,
force or torque capability of muscles and the related muscle length‐tension properties for strengthening exercises, and
endurance of muscle also involved in strengthening for endurance‐strength training.
3.Modulator Element: Exercises under this element relate to motor control for neuromuscular reeducation as follows:
patterns and synchronization of muscle recruitment, and
feed‐forward or feedback systems using verbal, visual, tactile and other proprioceptive input to the patient.
4. Biomechanical Element: This element is an interface between the motor control associated with the modulator element and musculoskeletal function associated with the base element. Components of the biomechanical element include:
static stabilization forces involved in alignment and muscle recruitment, and
dynamic stabilization forces involved in arthrokinetics, osteokinetics and kinematics.
5. Cognitive or Affective Element: Exercises in this category affect the functional status of the psychological system as it is related to movement as follows:
the cognitive ability to learn,
patient and caregiver compliance,
motivation, and
emotional status.
How the intervention might work
Exercise has both physical and mental benefits through its effects on numerous systems such as the cardiovascular system; immune system; brain function; sleep; mood; and the musculoskeletal system (Abernethy 2013). Exercise can result in the following.
Increase flexibility and mobility of structures; improve muscle strength and endurance; increase tensile strength of ligaments and capsule; amplify strength and prevent injury of tendons and cartilage; and is also important for repair of these tissues.
Improve cardiovascular function resulting in less chance of developing heart conditions, strokes, or high blood pressure.
Relieve stress, anxiety and depression; improve mood; and increase self‐esteem and weight management by producing positive biochemical changes in the body and brain. Endorphins released post exercise act as a natural pain reliever and antidepressant in the body.
Reduce the risk of premature mortality; improve functional capacity and help older adults maintain independence. Exercise increases circulation throughout the spine and supporting structures, which is crucial to promote healing.
Improve quality and duration of sleep and help sleep disorders such as insomnia.
Enhance cognitive function in older adults through physical activity and aerobic exercise.
Positively benefit the human immune system if done in moderation.
Central to these benefits are the stages of change, encompassing the health belief and cognitive behavior models, used to help patients make the lifestyle changes necessary for successful adherence to exercise, maintain new behaviours over time and address anticipated relapses (Zimmerman 2000). Helping patients change behavior is an important role for all clinicians.
Why it is important to do this review
In our last update on exercise therapy, we found low to moderate quality evidence of pain relief benefit for combined cervical, scapulothoracic stretching and strengthening for chronic neck pain in the short and long term. The relative benefit of other types of exercise was not clear (Kay 2012). Since then, five other reviews have found primarily very low to low grade evidence as follows: 1) Stretching and strengthening for chronic neck pain (Bertozzi 2013; Southerst 2014; Vincent 2013), 2) Strengthening, endurance and modular element (Bronfort 2009; Racicki 2012) for chronic cervicogenic headache, 3) Neuromuscular exercises (proprioception/eye‐neck co‐ordination) (Leaver 2010; Teasell 2010a) for subacute and chronic WAD, 4) Stretching and range of motion (ROM) exercises (Leaver 2010) for non‐specific neck pain, 5) Stretching, strengthening, endurance training, balance/co‐ordination, cardio and cognitive/affective elements (Leaver 2010; Lee 2009; Salt 2011; Southerst 2014; Teasell 2010c) for chronic neck pain, 6) Qigong exercises (; Lee 2009; Southerst 2014) for chronic neck pain, 7) Supervised exercise (Teasell 2010c) for chronic WAD, and 8) Strengthening neck exercises (Bertozzi 2013; Southerst 2014) for chronic neck pain.
In contrast, reviews found low grade evidence for no beneficial effect on pain as follows: 1) Stretching and strengthening (Salt 2011; Southerst 2014) for radiculopathy, 2) General fitness training (Bertozzi 2013; Kay 2012) for acute to chronic neck pain, and 3) Stretching and endurance training in chronic neck pain (Bertozzi 2013; Kay 2012). There may be more than one way to summarize the results but few used the grade system. The GRADE approach considers a number of additional factors (adverse events, costs, temporality, plausibility, dose response, strength of association, and clinical applicability) to place the results into a larger context (Guyatt 2006).
Many previous reviews looked at multimodal approaches such as manual therapy and exercise (Bronfort 2009; Clar 2014; Miller 2010; Schroeder 2013) but our focus is on exercise alone.
A number of these reviews included studies that were not clearly categorized; they also included studies that were not single intervention trials. The results limited our ability to understand the comparative effectiveness of exercise interventions for the management of neck pain. Therefore, the true impact of exercise alone could not be determined with strong evidence. Although there was some evidence of benefit as noted above, it became clear that categorizing exercises into a classification system according to their elements was essential in differentiating the intended effect that different types of exercises may have had. Exploring the dosage and mode of delivery of recommended exercises is essential in future reviews.
In the current update, our objective was to adapt a therapeutic model for exercise and sub‐classify the different exercises. This allowed us to link the specific aims of the exercise activity to its anatomical rationale. As a result, we gained a better perspective on the intended aim of the specific exercise, which allowed us to clarify some of the reporting variances and the variance in exercise types that may have been affecting the estimates of effect size. We wanted to determine the more accurate effect of exercises, which have clinical implications in patients with neck pain.
Objectives
This systematic review assessed the short‐ to long‐term effect of exercise therapy on pain, function, patient satisfaction, quality of life, and global perceived effect in adults experiencing mechanical neck pain with or without cervicogenic headache or radiculopathy. Where appropriate, the influence of risk of bias, duration of the disorder and subtypes of neck disorder on the treatment effect was assessed.
Methods
Criteria for considering studies for this review
Types of studies
We included any published or unpublished randomized controlled trials (RCTs) in any language. We excluded quasi‐RCTs and clinical controlled trials (CCTs).
Types of participants
Participants included in the review were adults (males or females aged 18 years or older) with acute (less than 30 days), subacute (30 days to 90 days) or chronic (greater than 90 days) neck disorders categorized as:
mechanical neck disorders (MND), which included whiplash associated disorders (WAD) category I and II (Spitzer 1987; Spitzer 1995), myofascial neck pain, and degenerative changes that encompassed osteoarthritis and cervical spondylosis (Schumacher 1993),
cervicogenic headache (CGH) (Olesen 1988; Olesen 1997; Sjaastad 1990; Sjaastad 1998; Sjaastad 2008), and
neck disorders with radicular findings (NDR) (Spitzer 1987; Spitzer 1995).
We excluded studies if they investigated neck disorders with definitive or possible long tract signs (e.g. myelopathies); neck pain caused by other pathological entities (Schumacher 1993); headache associated with the neck, but not of cervical origin; co‐existing headache, when either neck pain was not dominant or the headache was not provoked by neck movements or sustained neck postures; and 'mixed' headache.
Types of interventions
We included studies that used one or more type of exercise therapy specified in the Therapeutic Exercise Intervention Model to sub‐classify exercise (Sahrmann 2002) prescribed or performed in the treatment of neck pain. For the purposes of this review, we excluded studies in which exercise therapy was given as part of a multidisciplinary treatment, multimodal treatment (e.g. manual therapy plus exercise), or exercises that required manual therapy techniques by a trained individual (such as hold‐relax techniques, rhythmic stabilization, and passive techniques).
Types of comparisons
We contrasted interventions against the following comparisons:
sham or placebo,
no treatment or wait list, and
exercise plus another intervention versus that same intervention (for example, exercise plus manual therapy versus manual therapy).
We excluded all other comparisons.
Types of outcome measures
A study was included if it used at least one of the four primary outcome measures of interest:
pain,
measures of function/disability (including, but not limited to, neck disability index, activities of daily living, return to work, and sick leave),
patient satisfaction, and
global perceived effect/quality of life.
We extracted information on adverse events and costs of care when available.
We defined the duration of follow‐up as:
immediately post treatment (≤ one day),
short‐term follow‐up (one day to three months),
intermediate‐term follow‐up (three months up to, but not including, one year), and
long‐term follow‐up (one year or longer).
Search methods for identification of studies
A research librarian searched computerized bibliographic databases, without language restrictions, for medical, chiropractic and allied health literature. Subject headings (MeSH) and key words included anatomical terms, disorder or syndrome terms, treatment terms and methodological terms.
Electronic searches
We searched the following databases from their inception up to between January and May 2014:
Cochrane Central Register of Controlled Trials (CENTRAL, which includes the CBRG Trials Register; Ovid, 21 May 2014),
MEDLINE(Ovid, 1950 to April 2014 week 4),
Embase (Ovid, 1980 to April 21, 2014),
Manual Alternative and Natural Therapy (MANTIS; Ovid, 1980 to May 2014),
Cumulative Index to Nursing and Allied Health Literature (CINAHL; EBSCO, 1982 to March 2014),
Index to Chiropractic literature (ICL; Jan 2014), and
ClinicalTrials.gov (May 2014).
See Appendix 1 for the search strategies used for CENTRAL, MEDLINE, Embase, MANTIS, CINAHL, and ICL.
Searching other resources
We also screened references of all retrieved full‐text articles, identified content experts and searched conference proceedings from the World Confederation of Physical Therapist (WCPT 2007; WCPT 2011, International Federation of Orthopaedic and Manipulative Therapists IFOMPT 2012; IFOMPT 2008 ‐ hardcopy used), World Federation of Chiropractic (WFC 2013 ‐ CD copy used), and searched personal files up to May 2014 for grey literature.
Data collection and analysis
For continuous data, standardized mean differences (SMD) with 95% confidence intervals (CI) were calculated using a random‐effects model. Standard mean difference was selected over mean difference (WMD) because different types of exercises were assessed and most interventions used different outcome measures that used different scales.
Selection of studies
Two review authors with expertise in medicine, physiotherapy, chiropractic, massage therapy, statistics, or clinical epidemiology independently conducted citation identification and study selection using pre‐piloted forms. The assembled group did not author any of the primary trials. We assessed agreement for study selection using the quadratic weighted Kappa statistic (Kw), Cicchetti weights (Cicchetti 1976). We resolved disagreements through consensus and consultation with a third party if required.
Data extraction and management
Two review authors independently conducted data abstraction on pre‐piloted forms. We resolved disagreements through consensus. We consulted a neutral third party if consensus was not reached. We contacted study authors for missing information and data clarification. We extracted data on design (RCT, number analyzed/number randomized, intention‐to‐treat analysis, power analysis), participants (disorder subtype, duration of disorder), intervention (treatment characteristics for the treatment and comparison group, dosage/treatment parameters, co‐intervention, treatment schedule, duration of follow‐up), and outcomes (baseline mean, end of study mean, absolute benefit, reported results, point estimate with 95% CI, power, side effects, cost of care, and adverse events). These factors are noted in the Characteristics of included studies table.
Assessment of risk of bias in included studies
Two review authors independently conducted assessment of risk of bias in included studies using pre‐piloted forms. Disagreements were resolved through consensus (Graham 2011). The Cervical Overview Group used a calibrated team of assessors and at least two assessors independently assessed the risk of bias. 'Risk of bias' tables were presented and discussed by the broader validity assessment team to maximize inter‐rater reliability (Graham 2011), and consensus was reached on final 'Risk of bias' assessments. We did not exclude studies from this review on the basis of the 'Risk of bias' assessment results. The following biases were assessed: selection bias (random sequence generation, allocation concealment, groups similarity at baseline); performance bias (blinding of personnel/care providers, co‐intervention, and compliance); detection bias (blinding of outcome assessor); attrition bias (incomplete outcome data); reporting bias (selective reporting) (see Appendix 2 for the 'Risk of bias' criteria recommended by the Cochrane Back Review Group (Furlan 2009)). We rated each 'Risk of bias' item as low, high, or unclear and entered it into the 'Risk of bias' table for each included study.
Measures of treatment effect
We used primarily SMD with 95% CIs for continuous data. There are two summary statistics used for meta‐analysis of continuous data, the mean difference (MD) and the standard mean difference (SMD). The selection of the summary statistic was determined by whether all studies in a homogenous meta‐analysis group reported an outcome using the same scale (pooled MD) or using a different scale (pooled SMD). The estimation of minimal clinically important difference (MCID) for pain, function and disability were in accordance with the Cochrane Back Group recommendations (Furlan 2009). For the purpose of the review, the MCID for pain was 10 on a 100‐point pain intensity scale (Farrar 2001; Felson 1995; Goldsmith 1993). To assign some descriptors on the size of the difference between the treatment group and control groups, we considered the effect to be small when it was less than 10% of the visual analogue scale (VAS) scale, medium when it was between 10% and 20% of the VAS scale, and large when it was 20% to 30% of the VAS scale. For the neck disability index (NDI), we used a MCID of 7/50 neck disability index units (MacDermid 2009). It is noted that the minimal detectable change varies from 5/50 for non‐complicated neck pain to 10/50 for cervical radiculopathy (MacDermid 2009). For other outcomes (i.e. global perceived effect and quality of life), where there was an absence of clear guidance on the size of clinically important effect sizes, we used the common hierarchy of Cohen 1988: small (0.20), medium (0.50) or large (0.80). Risk ratios (RR) were calculated for dichotomous outcomes. When neither continuous nor dichotomous data were available, we extracted the findings and the statistical significance as reported by the author(s) in the original study.
Dealing with missing data
Where data were not extractable, we contacted the primary authors. For continuous outcomes reported as medians, we calculated effect sizes (Kendal 1963; p 237).
Assessment of heterogeneity
Prior to calculation of a pooled effect measure, the reasonableness of pooling was assessed, based on clinical judgement. Using a random‐effects model, statistical heterogeneity was tested using the Chi2 method between the studies. In the absence of heterogeneity (P > 0.10), we calculated a pooled SMD, MD or RR.
Assessment of reporting biases
We planned to assess reporting bias using sensitivity analysis but this was not possible due to a paucity of trials in any one category. Assessment of publication bias included use of the graphical aide funnel plot.
Data synthesis
We assessed the quality of the body of the evidence using the GRADE approach (Guyatt 2006). Domains that may have decreased the quality of the evidence are: 1) study design, 2) risk of bias, 3) inconsistency of results, 4) indirectness (not generalizable), 5) imprecision (insufficient data), other factors (e.g. reporting bias) (Higgins 2009). The quality of the evidence was adjusted by a level based on the performance of the studies against the five domains. All plausible confounding factors were considered, as were their effects on the demonstrated treatment effects and their impact on the dose‐response gradient (Atkins 2004).
Levels of evidence were defined as follows.
High quality evidence: Further research is very unlikely to change our confidence in the estimate of effect. There are consistent findings among 75% of RCTs, with low risk of bias, that generalize to the population in question. There are sufficient data, with narrow confidence intervals. There are no known or suspected reporting biases (all of the domains are met).
Moderate quality evidence: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate (one of the domains is not met).
Low quality evidence: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate (two of the domains are not met).
Very low quality evidence: We are very uncertain about the estimate (three of the domains are not met).
No evidence: No RCTs were identified that measured this outcome.
We used the Cochrane GRADE approach and considered a number of additional factors (adverse events, costs, temporality, plausibility, dose response, strength of association, and clinical applicability) to place the results into a larger context. The number needed to treat to benefit (NNTB) and treatment advantages were calculated to communicate the magnitude of effect for main findings (Gross 2002).
Subgroup analysis and investigation of heterogeneity
Not conducted due to lack of data.
Sensitivity analysis
Sensitivity analysis or meta‐regression for the factors: symptom duration, methodological quality and subtype of neck disorder were planned but were not carried out because we did not have enough data in any one category.
Results
Description of studies
Results of the search
Considering all sources, we identified 5614 records through database searches and we found 44 records from other sources searched from start up to November 2013. Following screening of 201 full text articles, 192 were assessed for eligibility, (agreement on selection showed weighted kappa 0.94, SE 0.02). After further application of the eligibility criteria, we found 27 trials that used exercise treatment for non‐specific subacute and chronic neck pain, and selected them for this review; Figure 1 describes the flow of included, excluded, and ongoing, as well as those awaiting classification.
1.
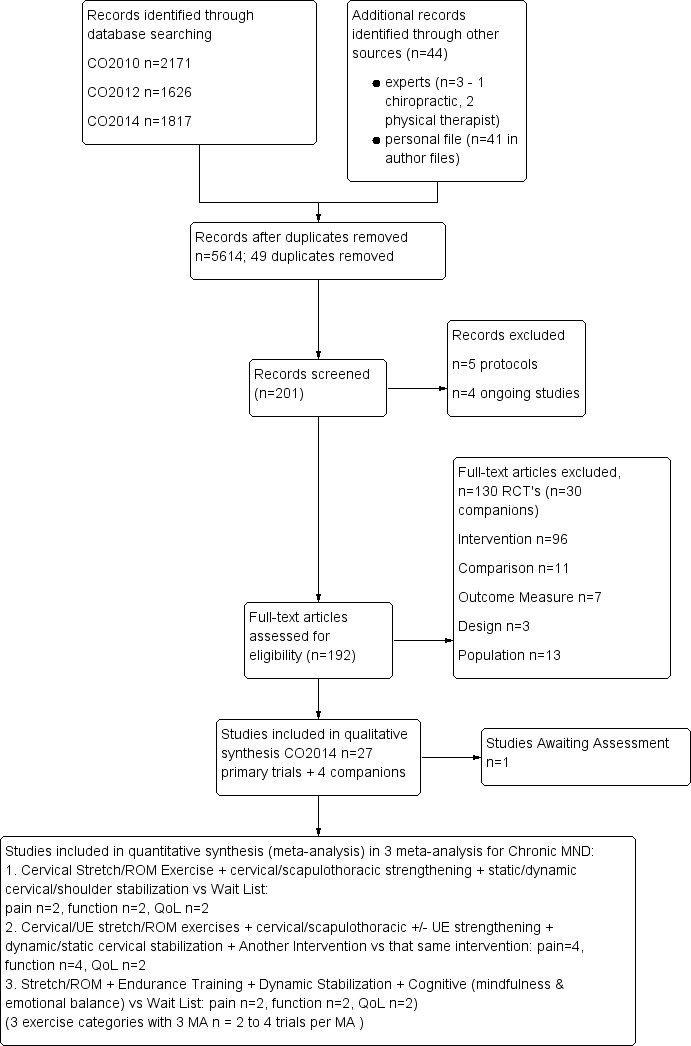
Study flow diagram (PRISMA).
Included studies
Twenty‐seven trials [(2485/3005) analyzed at end of study /randomized participants] were selected for this review.
Three studies described different aspects of the same study population under additional publications: Andersen 2008 ‐ one trial, two publications; Bronfort 2001 ‐ one trial, four publications; Stewart 2007 ‐ one trial, three publications.
Twenty‐four trials evaluated neck pain: one evaluated acute neck pain (Lange 2013); one evaluated acute/subacute/chronic neck pain (Kjellman 2002); one evaluated subacute neck pain (Chiu 2005); four evaluated subacute/chronic neck pain (Andersen 2008; Andersen 2011; Andersen Ch 2012; Stewart 2007); 16 trials evaluated chronic neck pain (Allan 2003; Ang 2009; Beer 2012; Bronfort 2001; Dellve 2011; Franca 2008; Hansson 2013; Helewa 2007; Humphreys 2002; Lundblad 1999; Hallman 2011; Martel 2011; Rendant 2011; Revel 1994; Viljanen 2003; von Trott 2009); and one trial did not specify the duration of neck pain (Takala 1994).
One study reported on neck disorder with radicular signs and symptoms (Kuijper 2009) and 14 studies did not specify if radicular signs and symptoms were present (Andersen 2011; Andersen Ch 2012; Beer 2012; Dellve 2011; Hall 2007; Hallman 2011; Hansson 2013; Helewa 2007; Humphreys 2002; Lange 2013; Lundblad 1999; Rendant 2011; Viljanen 2003; von Trott 2009).
Two trials investigated cervicogenic headache, one subacute (Hall 2007) and the other chronic (Jull 2002).
One trial investigated acute radiculopathy (Kuijper 2009).
Studies varied in sample size from 16 to 340 (n analyzed), and 27 of 28 trials were considered small (less than 70 participants per intervention arm).
Excluded studies
Studies (n=130 primary papers and 30 companion paper) were excluded for the following reasons: two used a quasi‐RCT design, one used a prospective observational design, 12 examined a different type of participant (e.g. chronic tension headache, cervical dystonia), one reported on a subgroup of the included population, 96 tested a different intervention (e.g. not active exercise, the exercise was the same in all groups, or the exercise group could not be separated out from a multimodal intervention), 11 used a comparison group and seven did not measure any of the identified primary outcomes. See Characteristics of excluded studies tables for more details.
Risk of bias in included studies
We used the quadratic weighted Kappa (Kw) statistic to assess agreement on a per question basis (Kw 0.23 to 1.00). Each 'Risk of Bias' item is presented as a percentage across all included studies Figure 2. Common methodological weaknesses included each of the criteria listed below (see 'Risk of Bias' tables). Methodological quality did not appear to influence the end results of the reviews; both high and low quality studies had similar outcome directions. Albeit, limited data were available to analyze for publication bias; Figure 3 suggests that we cannot rule out publication bias. This relationship between risk of bias and end results of the review was not formally tested using sensitivity analysis or meta‐regression, as there were not enough trials in any one meta‐analysis.
2.
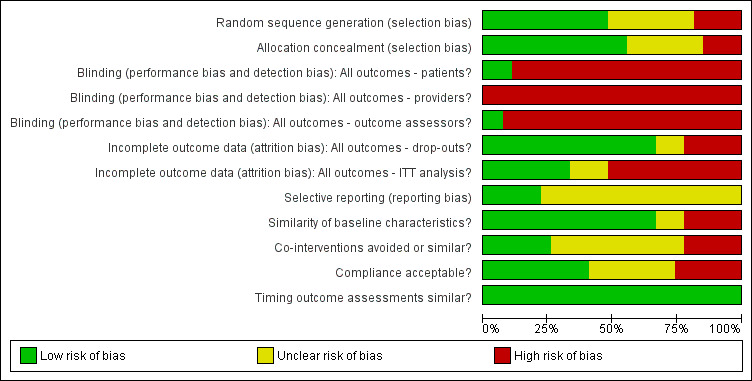
'Risk of bias' graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
3.
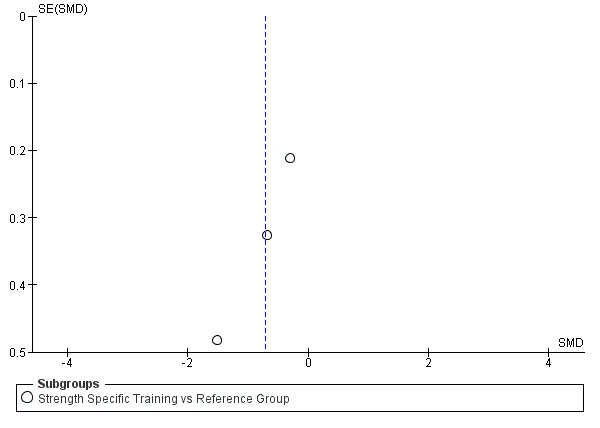
Funnel plot of comparison: 7 Acute to Chronic MND: Scapulothoracic + UE Strengthening vs CONTROL, outcome: 7.2 Pain Intensity: 10 to 20 weeks of treatment.
Allocation
There was failure to describe or use appropriate concealment of allocation in 42.9% of studies.
Blinding
There was a lack of effective "blinding" procedures in 92.9% of trials ‐ the minimum expectation being blinding of the outcome assessor.
Incomplete outcome data
There were incomplete outcome data provided by 28.6% of the trials.
Selective reporting
There was selective reporting bias with 78.6% of the trials.
Other potential sources of bias
Compliance was monitored and acceptable in only 42.9% of trials, and co‐intervention was either not avoided or not described in 71.4% of trials. The funnel plot (Figure 3) has the classic small negative trial missing that may suggest publication bias (language bias); we did not search non‐English databases. Alternatively, it could reflect the poor methodological quality leading to inflated effects in smaller trials.
Effects of interventions
See: Table 1; Table 2; Table 3; Table 4; Table 5; Table 6; Table 7; Table 8; Table 9; Table 10; Table 11; Table 12; Table 13
Chronic Mechanical Neck Pain
1. Support Element
a) Breathing Exercises
Diaphragmatic Breathing Exercises versus Control
One trial Hallman 2011 compared diaphragmatic breathing with a no treatment control. This latter group took part in the breathing protocol in sessions 1 and 10, without any prescribed treatment in between.
Pain Intensity outcomes
No difference in pain between groups immediately post treatment (Figure 4).
4.
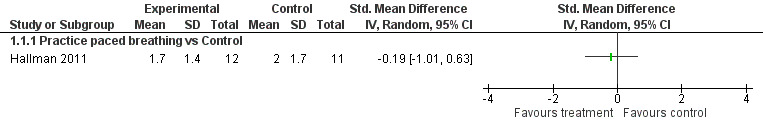
Forest plot of comparison: 1 Chronic MND: Breathing Patterns vs CONTROL, outcome: 1.1 Pain Intensity (Borg 0 to 10): 10 weeks of treatment vs Control.
Function outcomes
No difference in function between groups immediately post treatment.
Quality of Life outcomes
No difference in quality of life between groups immediately post treatment.
Conclusion: There is low quality evidence (one trial, 24 participants, Hallman 2011) that diaphragmatic breathing may have no effect on pain, function and quality of life when compared to a no treatment control for chronic mechanical neck pain immediately post treatment (50 sessions over 10 weeks).
b) Cardiovascular/Aerobic Training
General Fitness Training versus Control
One trial with two publications (Andersen 2008) compared a general exercise program with a no treatment control (general health information) intervention.
Pain Intensity Outcomes
No difference in pain between both (see above: general exercise versus control) groups immediately post treatment (Figure 5).
5.
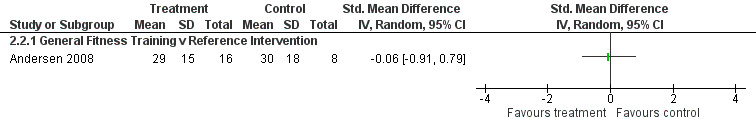
Forest plot of comparison: 2 Acute to Chronic MND: General Fitness Training vs CONTROL, outcome: 2.2 Pain Intensity (VAS): 10 weeks of treatment + 10 weeks follow‐up.
Conclusion: There is low quality evidence (one trial with two publications, 24 participants, Andersen 2008) that general fitness training exercises may have no difference in pain when compared with a reference intervention for (sub)acute/chronic neck pain immediately post treatment.
2. Base Element
a) Stretching
Cervical Stretch/range of motion (ROM) Exercises + Another Intervention versus That Same Intervention
One trial (Allan 2003) evaluated neck stretching either before or after manipulation compared with manipulation alone.
Pain Intensity Outcomes
No difference in pain between all groups immediately post treatment.
Function Outcomes
No difference in function between all groups immediately post treatment.
Conclusion: There is low quality evidence (one trial, 16 participants, Allan 2003) that stretching exercises, either before or after a manipulation, made no difference on pain and function when compared with that same manipulation for chronic neck pain immediately post treatment. Manipulation was the control group in both arms of the trial and therefore, the contribution of the base element of stretching could be factored out.
Cervical Stretch/ROM Exercises + Dynamic Cervical Stabilization versus Sham
One trial (Kjellman 2002) compared cervical movement exercises (McKenzie protocol) with sham ultrasound.
Pain Intensity Outcomes
There is no evidence of benefit on pain immediately post treatment, at intermediate‐term or long‐term follow‐up (Figure 6).
6.
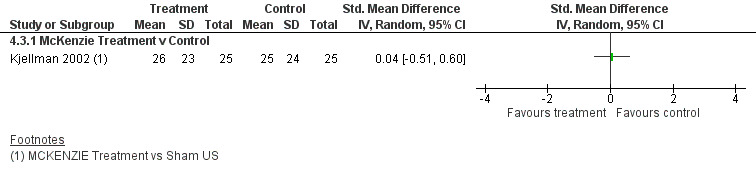
Forest plot of comparison: 4 Chronic MND: Cervical Stretch/ROM Exercises + Dynamic Cervical Stabilization vs SHAM, outcome: 4.3 Pain Intensity (VAS): 8 weeks of treatment + 12 months follow‐up.
Function Outcomes
There was no evidence of benefit on function immediately post treatment, at intermediate‐term or long‐term follow‐up.
Conclusion: Low quality evidence (one trial, 50 participants, Kjellman 2002) shows no difference for pain relief and function immediately post intervention, at six‐ and 12‐month follow‐up using Cervical Stretch/ROM Exercise + Dynamic Cervical Stabilization for chronic MND.
b) Strengthening
Static Cervical Strengthening + Static Stabilization versus No Intervention or Wait List
One trials (two comparisons) studying chronic neck pain compared either manually (1) resisted isometric neck exercise plus postural training with mirror feedback to a control, or (2) these same isometric neck exercises and the use of an orthopaedic pillow were compared with the use of an orthopaedic pillow (Helewa 2007).
Pain Intensity Outcomes
Of the two comparisons, one showed no evidence of benefit (exercise versus control) while the other showed evidence of benefit (exercise + an intervention versus that same intervention) on function immediately post treatment and at short‐term follow‐up. (Helewa 2007).
Function Outcomes
Of the two comparisons, one showed no evidence of benefit (exercise versus control) while the other showed evidence of benefit (exercise + an intervention versus that same intervention) on function immediately post treatment and at short‐term follow‐up. (Helewa 2007).
Quality of Life
In two comparisons (exercise versus control, exercise + an intervention versus that same intervention), there was no evidence of benefit immediately post treatment and at short‐term follow‐up on quality of life (Helewa 2007), albeit there may be a clinically important effect favouring exercise + pillow versus pillow alone.
Conclusion : Evidence exists from two trials (three comparisons) where data are not combinable. Low quality evidence from one trial (two independent comparisons, 50 participants, Helewa 2007) gives varying results. Evidence of benefit showed people may improve slightly when exercise was added to a pillow versus a pillow alone (NNTB = 9). However, this was not observed when isometric exercise alone was evaluated for function and quality of life, from immediately post treatment to short‐term follow‐up.
Postural Exercise versus Control
One trial Beer 2012 compared sitting postural exercises versus control.
Pain Intensity Outcomes:
No difference in pain between groups immediately post treatment.
Physical Function outcomes
No difference in physical function between groups immediately post treatment.
Conclusion: We are uncertain whether postural exercises improve pain or function. There is very low quality evidence (one trial, 20 participants, Beer 2012) that postural exercises have no difference on pain and function when compared to control for chronic mechanical neck pain immediately post treatment (two‐week intervention).
Scapulothoracic + Upper Extremity (UE) Strengthening versus Control
Three trials (Andersen 2008; Andersen Ch 2012; Dellve 2011), each with different dosages compared specific strength training of the scapulothoracic region and upper extremity with a reference intervention.
Pain Intensity Outcomes
No difference in pain at four weeks of treatment. There is a moderate to large difference in pain reduction between groups at 10 to 20 weeks of treatment, [SMD pooled ‐0.71 (95%CI:‐1.33 to ‐0.10); Figure 7]. Additionally one and nine weekly sessions were no different when contrasted with the reference group.
7.
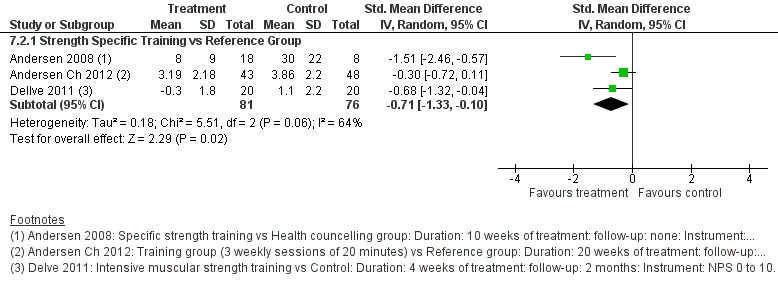
Forest plot of comparison for (sub)Acute/Chronic MND: Scapulothoracic + UE Strengthening vs CONTROL, outcome: Pain Intensity: 10 to 20 weeks of treatment.
Physical Function Outcomes
No statistical difference in physical function between groups immediately post treatment, but may achieve a minimal clinically important difference at short‐term follow‐up.
Conclusion: There is moderate quality evidence (three trials, 157 participants, Andersen 2008; Andersen Ch 2012; Dellve 2011) that scapulothoracic and UE strength training probably improves pain a moderate to large amount immediately post treatment and at short‐term follow‐up. It may improve functional outcomes when compared to control at short‐term follow‐up (10 to 20 weeks of intervention).
c) Stretch and Strengthening
Cervical/UE Stretch/ROM Exercise + Cervical/UE Strengthening + Dynamic Cervical Stabilization versus Placebo or Sham
One trial (Kjellman 2002) compared general exercises including neck and shoulder ROM, active neck endurance and strength exercises with sham ultrasound.
Pain Intensity Outcomes
There was no evidence of benefit immediately post treatment, at intermediate‐term and long‐term follow‐up.
Physical Function Outcomes
There was no evidence of benefit immediately post treatment, at intermediate‐term and long‐term follow‐up.
Conclusion: Low quality evidence (one trial, 50 participants, Kjellman 2002) shows no difference for pain relief and function immediately post intervention, at six and 12 months follow‐up using Cervical/UE Stretch/ROM Exercise + Cervical/UE Strengthening + Dynamic Cervical Stabilization for chronic MND.
Cervical Stretch/ROM Exercises + Cervical/Scapulothoracic Strengthening + Static/Dynamic Cervical/Shoulder Stabilization versus Wait List
Two trials (Rendant 2011; von Trott 2009) compared a standardized exercise program for neck pain including repeated active cervical rotations, strength and flexibility exercises to a wait list. The two trials appeared clinically similar and were pooled.
Pain Intensity Outcomes
When two studies (Rendant 2011; von Trott 2009) were pooled, there was a significant difference, moderate clinically important 15‐point change post treatment [Heterogeneity: Chi² = 0.74, df = 1 (P = 0.39); I² = 0% MD pooled ‐14.90 (CI 95% ‐22.40 to ‐7.39), NNTB =4]. This reduced to a small difference of [pooled MD ‐10.94 (CI 95% ‐18.81 to ‐3.08)] at short‐term follow‐up (Figure 8).
8.
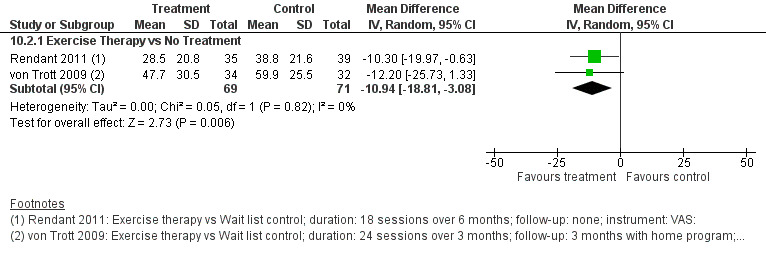
Forest plot of comparison for Chronic MND: Cervical Stretch/ROM Exercises + Cervical/Scapulothoracic Strengthening + Static/Dynamic Cervical/Shoulder Stabilization vs WAIT LIST, outcome: Pain Intensity (VAS): 24 weeks of treatment.
Function Outcomes
One trial (Rendant 2011), showed evidence of benefit for function post treatment. One trial (von Trott 2009) showed no significant difference immediately post treatment and at short‐term follow‐up. When the two studies were pooled, there was a significantly different, clinically important, moderate change in function. [Heterogeneity: Tau² = 0.09; Chi² = 2.63, df = 1 (P = 0.10); I² = 62% SMD pooled:‐0.50 (CI 95% ‐1.04 to 0.03), NNTB = 5 (Analysis 10.3)]. At short‐term follow‐up (24 weeks of treatment), pooled SMD: ‐0.40 (CI 95% ‐0.74 to ‐0.06) (Analysis 10.4).
10.3. Analysis.
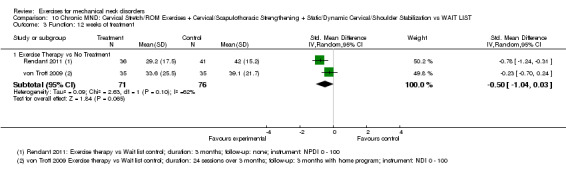
Comparison 10 Chronic MND: Cervical Stretch/ROM Exercises + Cervical/Scapulothoracic Strengthening + Static/Dynamic Cervical/Shoulder Stabilization vs WAIT LIST, Outcome 3 Function: 12 weeks of treatment.
10.4. Analysis.
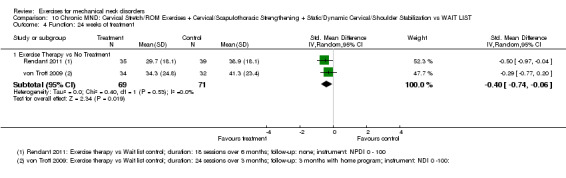
Comparison 10 Chronic MND: Cervical Stretch/ROM Exercises + Cervical/Scapulothoracic Strengthening + Static/Dynamic Cervical/Shoulder Stabilization vs WAIT LIST, Outcome 4 Function: 24 weeks of treatment.
Global Perceived Effect
No significant difference in global perceived effect was found at any time points.
Quality of Life
When the two trials were pooled, no significant difference in quality of life was found at any time point. [Heterogeneity: Tau² = 0.00; Chi² = 0.95, df = 1 (P = 0.33); I² = 0% MD pooled at 12 weeks ‐2.22 (CI 95% ‐5.17 to 0.72) (Analysis 10.7), at short‐term follow‐up pooled MD 0.01 (CI 95% ‐0.47 to 0.49) (Analysis 10.8)].
10.7. Analysis.
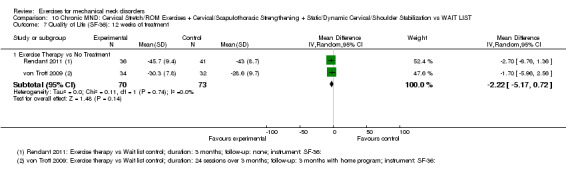
Comparison 10 Chronic MND: Cervical Stretch/ROM Exercises + Cervical/Scapulothoracic Strengthening + Static/Dynamic Cervical/Shoulder Stabilization vs WAIT LIST, Outcome 7 Quality of Life (SF‐36): 12 weeks of treatment.
10.8. Analysis.
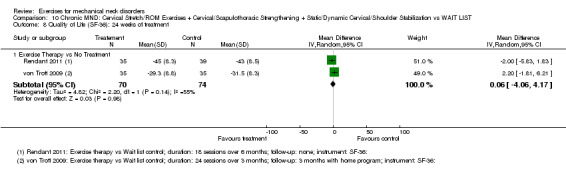
Comparison 10 Chronic MND: Cervical Stretch/ROM Exercises + Cervical/Scapulothoracic Strengthening + Static/Dynamic Cervical/Shoulder Stabilization vs WAIT LIST, Outcome 8 Quality of Life (SF‐36): 24 weeks of treatment.
Conclusion : Moderate quality evidence (two trials, 147 participants, Rendant 2011; von Trott 2009) shows cervical stretch/ROM exercises + cervical/scapulothoracic strengthening + static/dynamic cervical/shoulder stabilization probably has moderate benefit for pain and function, but not global perceived effect and quality of life immediately post treatment and at short‐term follow‐up. A clinician may need to treat four people to achieve a moderate degree of pain relief and five to achieve moderate functional benefit in one patient.
Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic +/‐UE Strengthening + Dynamic/Static Cervical Stabilization + Another Intervention versus That Same Intervention
Four trials studying chronic neck pain compared the following exercise interventions with a control group:
deep neck flexor retraining with pressure biofeedback and resisted neck flexion/extension strengthening using multicervical rehabilitation unit (Chiu 2005);
low technology exercise including progressive resisted neck and upper body strengthening using dumbells and pulley systems, light stretching and a short aerobic warm‐up program (Bronfort 2001);
muscle stretching and strengthening exercises of the neck and upper limb regions including strengthening of the deep cervical flexor muscles (Franca 2008); and
a home exercise program of ROM, stretching/mobilization and strengthening exercises of the cervical and upper thoracic spine (Martel 2011).
Both treatment arms of all groups received another intervention and were compared with that same intervention combined with exercise. We considered the exercise protocols to be clinically similar; that is, they all contained an exercise component, which applied a resistance force directly to the cervicoscapular region. Other similar clinical elements included the dosage and duration of care. We judged these exercise trials to be both clinically and statistically homogeneous (P = 0.67, I2= 0%).
Pain Intensity Outcomes
When data were pooled into a summary estimate, we found consistent evidence of reduced pain from immediately post treatment pooled SMD ‐0.33 (95% CI:‐0.55 to ‐0.10) (Analysis 9.1; Bronfort 2001; Chiu 2005; Franca 2008; Martel 2011) to intermediate‐term (Analysis 9.3) and long‐term follow‐up (Bronfort 2001). This suggests an initial small‐ to longer‐term large treatment benefit. The number needed to treat for one patient to benefit varies from six to 18.
9.1. Analysis.
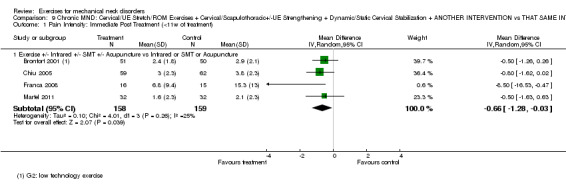
Comparison 9 Chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION vs THAT SAME INTERVENTION, Outcome 1 Pain Intensity: Immediate Post Treatment (<11w of treatment).
9.3. Analysis.
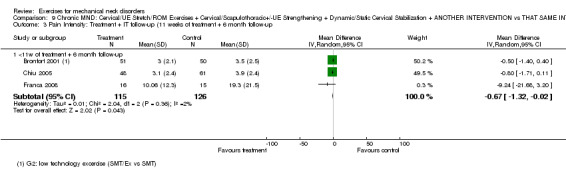
Comparison 9 Chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION vs THAT SAME INTERVENTION, Outcome 3 Pain Intensity: Treatment + IT follow‐up (11 weeks of treatment + 6 month follow‐up.
Function Outcomes
There was evidence of benefit in function immediately post treatment pooled SMD ‐0.25 (95% CI: ‐0.48 to ‐0.01), intermediate‐term pooled SMD ‐0.45 (95% CI: ‐0.72, to ‐0.18) (Figure 9; Bronfort 2001; Chiu 2005; Franca 2008) and long‐term follow‐up (Bronfort 2001). The latter represents the largest improvement. The number needed to treat for one patient to benefit varies from four to 13.
9.
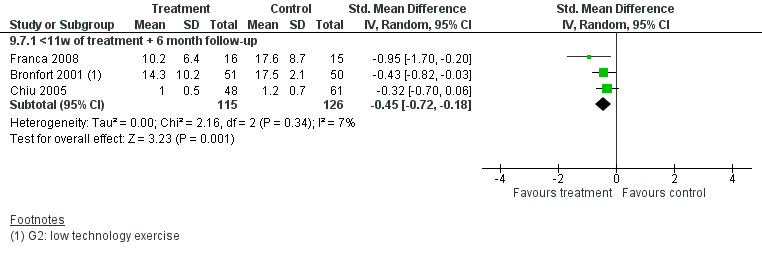
Forest plot of comparison for chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION vs THAT SAME INTERVENTION in the outcome Function at intermediate term follow‐up.
Global Perceived Effect and Quality of Life
There was a statistically important difference in global perceived effect noted immediately post treatment (Analysis 9.9) and at long‐term follow‐up (Bronfort 2001; Martel 2011).
9.9. Analysis.
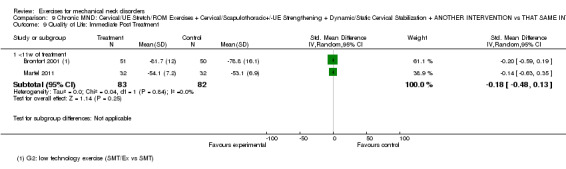
Comparison 9 Chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION vs THAT SAME INTERVENTION, Outcome 9 Quality of Life: Immediate Post Treatment.
Patient Satisfaction
There were statistically and clinically important differences for patient satisfaction noted at all time points (Bronfort 2001).
Conclusion : Moderate quality evidence (four trials, 341 participants, Bronfort 2001; Chiu 2005; Franca 2008; Martel 2011) shows moderate pain relief and improved function up to long‐term follow‐up for combined cervical, scapulothoracic stretching and strengthening for chronic neck pain. A clinician may need to treat six to 18 people to achieve this type of pain relief and four to 13 to achieve this functional benefit. Moderate quality evidence (one trial, 101 participants) demonstrates patients are very satisfied with their care. Changes in quality of life are suggestive of benefit but not conclusive. Changes in global perceived effect measures indicate a difference immediately post treatment and at long‐term follow‐up.
d) Stretching and Endurance Training
Cervical/Scapulothoracic/UE Stretch + UE Endurance Training versus No Intervention
One trial (Viljanen 2003) compared dynamic muscle training with free weights with ordinary activity.
Pain Intensity Outcomes
There was no significant pain relief immediately post treatment and at short‐term or long‐term follow‐up.
Function Outcomes
There was no significant change in function at the same three time points.
Conclusion: Moderate quality evidence (one trial, 393 participants, Viljanen 2003), shows little to no difference for UE stretching and endurance training for chronic neck pain and function immediately post treatment, at short‐term and long‐term follow‐up.
e) Strengthening and Endurance Training
Cervical/Scapulothoracic Strengthening + Endurance Training versus Control
One trial (Ang 2009) compared non‐postural and postural strengthening exercises and endurance‐strength exercises versus a control group.
Pain Prevalence Outcomes
There was no significant decrease in pain prevalence immediately post treatment or at long‐term follow‐up.
Conclusion: Very low quality evidence (one trial, 68 participants, Ang 2009) shows we are uncertain whether cervical/scapulothoracic strengthening and endurance‐strength exercises improves the prevalence of neck pain in chronic neck pain at immediately post treatment and at long‐term follow‐up.
Pattern synchronization and Cervical/Scapulothoracic Strengthening and Scapulothoracic Endurance versus Control
One trial Lange 2013 compared deep neck flexor recruitment combined with upper extremity strengthening/endurance exercises versus control.
Pain Intensity Outcomes
There was evidence of a very small change in pain intensity immediately post treatment (24 weeks of treatment).
Conclusion: Low quality evidence due to floor effect (one trial, 55 participants, Lange 2013) shows deep neck flexor recruitment combined with UE strengthening/endurance exercises may have little difference in pain immediately post treatment.
f) Endurance Training
Scapulothoracic/UE Endurance Training versus Control
One trial (Andersen 2011) with two comparisons compared shoulder abduction endurance training for two minutes or 12 minutes with a control group.
Pain Intensity Outcomes
There was evidence of benefit immediately post treatment for pain for both the two‐minute and 12‐minute training programs.
Conclusion: Moderate quality evidence (one trial, 198 participants, Andersen 2011) shows moderate benefit for pain relief immediately post intervention using scapulothoracic/UE endurance training for (sub)acute/chronic MND. A clinician may need to treat four people to achieve this type of pain relief.
3. Modulator Elements
Neuromuscular Exercise (eye‐neck co‐ordination/proprioception) + Another Intervention versus That Same Intervention
One trial (Revel 1994) compared eye‐neck co‐ordination exercises and analgesic/anti‐inflammatory medication with that same medication only for chronic neck pain.
Pain Intensity
There was evidence of benefit on pain at short‐term follow‐up. The number needed to treat for one patient to benefit is four.
Function
There was evidence of benefit on function at short‐term follow‐up. The number needed to treat for one patient to benefit is three.
Conclusion: We are uncertain whether eye‐neck co‐ordination exercises improve pain or function. Very low quality evidence (one trial, 60 participants, Revel 1994) shows a moderate reduction in pain and improved function in chronic neck pain in the short term for eye‐neck co‐ordination exercises. A clinician may need to treat four people to achieve this type of pain relief and three to achieve this functional benefit in one person.
Patterns synchronization + Feedforward/feedback exercises for co‐ordinating the neck, eyes and upper limbs versus No Intervention
One trial (Humphreys 2002) compared eye‐neck‐upper limb co‐ordination exercises versus no intervention in patients with chronic neck pain.
Pain Intensity
No difference in pain between groups immediately post treatment. Conclusion : Low quality evidence (one trial, 56 participants, Humphreys 2002) shows eye‐neck‐upper limb exercises show little or no difference in pain immediately post treatment.
Patterns synchronization + Feedforward/feedback: vestibular rehabilitation (balance on unstable surfaces and walking with head movements and eyes closed) vs No Intervention
One trial (Hansson 2013) compared vestibular rehabilitation program vs no intervention in patients with chronic neck pain.
Pain Intensity
No difference in pain between groups immediately post treatment or at short‐term follow‐up.
Conclusion: Low quality evidence (one trial, 29 participants, Hansson 2013) shows vestibular rehabilitation type exercises may have little or no difference in neck pain both immediately post treatment and at short‐term follow‐up.
4. Base + Modulator Elements + Support
Trunk and Extremity Stretch + Pattern/Synchronization: Balance Co‐ordination + Cardiovascular/Aerobic versus No Intervention
One trial (Takala 1994) with unspecified duration of neck pain at baseline, compared a group of whole body exercise program, which included aerobic training and shoulder/thoracic exercises, with no treatment.
Pain Intensity
There was no evidence of benefit for pain reduction immediately post treatment.
Conclusion: Low quality evidence (one trial, 44 participants,Takala 1994) shows little to no difference for pain reduction immediately post treatment in patients with neck pain of unspecified duration when treated with group exercise that combined extensibility and co‐ordination exercises with cardiovascular training.
General Endurance Training + Dynamic/Static Lowback/pelvic Stabilization + General Stretching + Neuromuscular/body Mechanics Movement Training versus No Intervention
One trial (Lundblad 1999) compared lumbopelvic stabilization, ergonomic exercises, endurance, general strengthening, and co‐ordination exercises with no treatment.
Pain Intensity
There was no evidence of benefit for pain reduction at short‐term follow‐up.
Conclusion: Low quality evidence (one trial, 38 participants, Lundblad 1999) shows little to no difference for pain reduction with a combined exercise approach of stabilization of the low back and pelvis, posture awareness, ergonomic training, and strength, co‐ordination, endurance, flexibility/smoothness and rhythm exercises when compared to no intervention or a wait list control in chronic neck pain at short‐term follow‐up.
5. Base + Cognitive/Affective Element
Stretch/ROM + Endurance Training + Dynamic Stabilization + Cognitive (mindfulness & emotional balance) versus Wait List
Two trials (Rendant 2011; von Trott 2009) compared a program of Qigong exercises (Dantian Qigong) including relaxation of mind and body, conscious breathing and movement exercises of the hip, legs, shoulders, arms and head with a wait list.
Pain Intensity
When data were pooled into a summary estimate, there was evidence of reduced pain post treatment at 12 weeks [pooled MD ‐13.28 (‐20.98 to ‐5.58)] (Analysis 18.1) and 24 weeks [pooled MD ‐7.82 (‐14.57, ‐1.07)] (Analysis 18.2) of treatment (Rendant 2011; von Trott 2009).
18.1. Analysis.
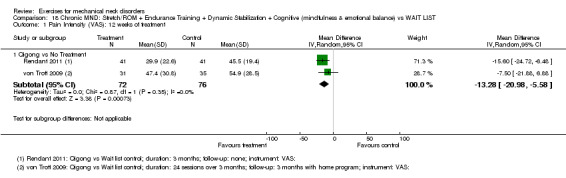
Comparison 18 Chronic MND: Stretch/ROM + Endurance Training + Dynamic Stabilization + Cognitive (mindfulness & emotional balance) vs WAIT LIST, Outcome 1 Pain Intensity (VAS): 12 weeks of treatment.
18.2. Analysis.
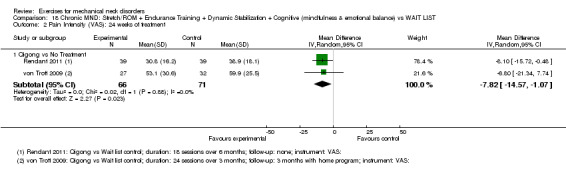
Comparison 18 Chronic MND: Stretch/ROM + Endurance Training + Dynamic Stabilization + Cognitive (mindfulness & emotional balance) vs WAIT LIST, Outcome 2 Pain Intensity (VAS): 24 weeks of treatment.
Function
When data were pooled into a summary estimate, there was evidence of reduced function post treatment at 12 weeks [pooled SMD ‐0.36 (‐0.68 to ‐0.03); Analysis 18.3] and 24 weeks [pooled SMD ‐0.28 (‐0.68 to 0.11); Analysis 18.4] of treatment (Rendant 2011; von Trott 2009)
18.3. Analysis.
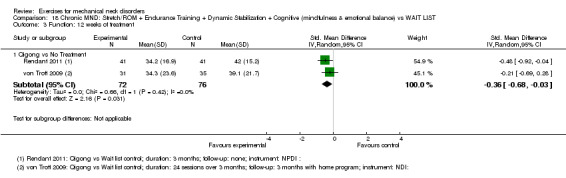
Comparison 18 Chronic MND: Stretch/ROM + Endurance Training + Dynamic Stabilization + Cognitive (mindfulness & emotional balance) vs WAIT LIST, Outcome 3 Function: 12 weeks of treatment.
18.4. Analysis.
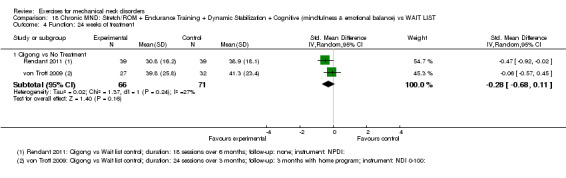
Comparison 18 Chronic MND: Stretch/ROM + Endurance Training + Dynamic Stabilization + Cognitive (mindfulness & emotional balance) vs WAIT LIST, Outcome 4 Function: 24 weeks of treatment.
Global Perceived Effect
There was no evidence of benefit for global perceived effect immediately post treatment and at short‐term follow‐up.
Quality of Life
There was evidence of benefit for SF36 physical component immediately post 12 weeks of treatment [pooled MD ‐2.72 (95% CI: ‐5.42 to ‐0.01); Analysis 18.7]; but not at short‐term follow‐up of 24 weeks [pooled MD ‐1.88 (95%CI: ‐5.80 to 2.04); Analysis 18.8] (Rendant 2011; von Trott 2009).
18.7. Analysis.
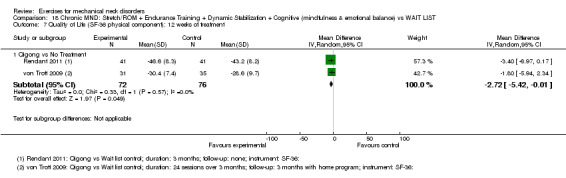
Comparison 18 Chronic MND: Stretch/ROM + Endurance Training + Dynamic Stabilization + Cognitive (mindfulness & emotional balance) vs WAIT LIST, Outcome 7 Quality of Life (SF‐36 physical component): 12 weeks of treatment.
18.8. Analysis.
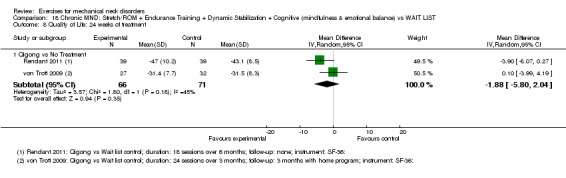
Comparison 18 Chronic MND: Stretch/ROM + Endurance Training + Dynamic Stabilization + Cognitive (mindfulness & emotional balance) vs WAIT LIST, Outcome 8 Quality of Life: 24 weeks of treatment.
Conclusion: Moderate quality evidence (two trials, 191 participants, Rendant 2011; von Trott 2009) shows Qigong exercises (Dantian Qigong) may improve pain and function slightly when compared with a wait list control at immediate‐ and short‐term follow‐up. It may have little or no benefit at immediate and short‐term follow‐up on quality of life and global perceived effect. A clinician may need to treat four to six people to achieve this type of pain relief, five to eight people to achieve this functional benefit, and seven to 10 people for this improvement in quality of life.
6. Base + Modular + Cognitive Affective + Support
Stretch/ROM + Strength and Endurance Training (trunk and limb) + Pattern/Synchronization: Balance Co‐ordination + Cardiovascular/Aerobic + Cognitive (Coaching + Motivational) versus that Same Intervention
One trial (Stewart 2007) compared an individualized, progressive submaximal program, which included aerobic training, trunk and limb exercises and advice compared with advice alone.
Pain Intensity
There was evidence of small benefit on pain post treatment but not at long‐term follow‐up.
Function
There was evidence of small benefit on function post treatment and at long‐term follow‐up.
Global Perceived Effect
There was evidence of small benefit on global perceived effect post treatment but not at long‐term follow‐up.
Quality of Life
There was evidence of small benefit on quality of life post treatment but not at long‐term follow‐up.
Conclusion: Low quality evidence (one trial, 132 participants, Stewart 2007) shows small benefits for pain relief, function,global perceived effect and quality of life immediately post treatment and small benefit at 12‐month follow‐up for function using Trunk/Extremity Stretch/ROM + Trunk/Extremity Strengthening + Trunk/Extremity Endurance Training + Pattern/Synchronization: Co‐ordination + Cardiovascular/Aerobic + Cognitive (CBT) + another treatment for Subacute/chronic WAD.
Cervicogenic Headache
1. Base Element
Stretch/ROM exercises versus Sham
One trial (Hall 2007) investigated patients with subacute cervicogenic headache; this trial compared C1‐C2 self‐sustained natural apophyseal glide (SNAG) exercises with a sham mobilization.
Pain Intensity Outcomes
There was pain reduction at both short‐ and long‐term follow‐up. The number needed to treat for one patient to benefit is three.
Conclusion: Low quality evidence (one trial, 32 participants, Hall 2007) shows people may improve a large amount for pain reduction at short‐ and long‐term follow‐up with the use of C1‐C2 self‐SNAG exercises when compared with a sham for (sub)acute cervicogenic headache. A clinician may need to treat three people to achieve this type of long‐term pain relief.
2. Base and Modular Element
Cervical/Scapulothoracic Strengthening with Endurance Training + Craniocervical Pressure Biofeedback + Dynamic Cervical Stabilization versus No Intervention
One trial (Jull 2002) studied chronic cervicogenic headache and compared endurance exercises including pressure biofeedback for the cervicoscapular region with no treatment.
Pain Intensity
When compared with no treatment, there was evidence of a large benefit post treatment and a moderate size benefit at long‐term follow‐up ( Analysis 21.2) for pain relief. The number needed to treat for one patient to benefit is six.
21.2. Analysis.
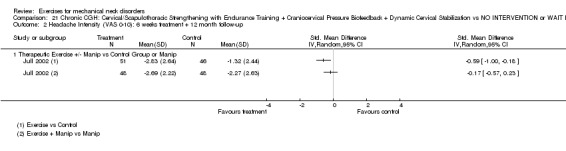
Comparison 21 Chronic CGH: Cervical/Scapulothoracic Strengthening with Endurance Training + Craniocervical Pressure Biofeedback + Dynamic Cervical Stabilization vs NO INTERVENTION or WAIT LIST, Outcome 2 Headache Intensity (VAS 0‐10): 6 weeks treatment + 12 month follow‐up.
Function
When compared with no treatment, there was evidence of a moderate degree of benefit at post treatment and at long‐term follow‐up (Analysis 21.4) on function. The number needed to treat for one patient to benefit is six.
21.4. Analysis.
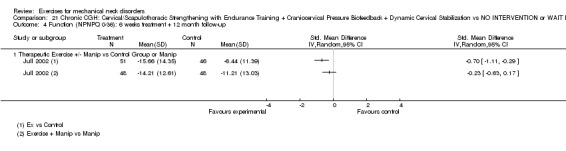
Comparison 21 Chronic CGH: Cervical/Scapulothoracic Strengthening with Endurance Training + Craniocervical Pressure Biofeedback + Dynamic Cervical Stabilization vs NO INTERVENTION or WAIT LIST, Outcome 4 Function (NPNPQ 0‐36): 6 weeks treatment + 12 month follow‐up.
Global Perceived Effect
When compared with no treatment, there was evidence of a large benefit post treatment and at long‐term follow‐up ( Analysis 21.6) on global perceived effect.
21.6. Analysis.
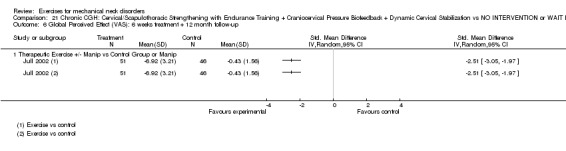
Comparison 21 Chronic CGH: Cervical/Scapulothoracic Strengthening with Endurance Training + Craniocervical Pressure Biofeedback + Dynamic Cervical Stabilization vs NO INTERVENTION or WAIT LIST, Outcome 6 Global Perceived Effect (VAS): 6 weeks treatment + 12 month follow‐up.
Conclusion : Moderate quality evidence (one trial, 97 participants, Jull 2002) shows cervicoscapular strengthening and endurance exercises including pressure biofeedback probably improve pain, function and global perceived effect for chronic cervicogenic headaches at long‐term follow‐up when compared to no treatment. A clinician may need to treat six people to achieve this type (medium to large amount) of pain relief and functional benefit in one patient.
Cervical/Scapulothoracic Strengthening with Endurance Training + Craniocervical Pressure Biofeedback + Dynamic Cervical Stabilization + Manual Therapy versus Manual Therapy
One trial (Jull 2002) studied chronic cervicogenic headache and compared endurance exercises including pressure biofeedback plus manual therapy for the cervicoscapular region with manual therapy.
Pain Intensity
When compared with manual therapy, there was evidence of no difference post treatment and at long‐term follow‐up for pain relief.
Function
When compared with manual therapy, there was evidence of no difference post treatment and at long‐term follow‐up on function.
Global Perceived Effect
When compared with manual therapy, there was evidence of no difference post treatment and at long‐term follow‐up on global perceived effect. However, we believe there may be a clinically important but not statistical difference at long‐term follow‐up.
Conclusion : Moderate quality evidence (one trial, 96 participants, Jull 2002) shows when exercise combined with manual therapy contrasted with manual therapy alone there is probably no difference in pain, function and global perceived effect for chronic cervicogenic headaches at long‐term follow‐up.
Acute Radiculopathy
1. Base Element
a) Stretching and Strengthening
Cervical Stretch/ROM + Cervical/Scapulothoracic/UE Strengthening + Static/Dynamic Cervical Stabilization versus Wait List
One trial (Kuijper 2009) studying acute cervical radiculopathy compared cervical mobilizing and stabilizing exercises with a wait list control.
Pain Intensity
There was a significant difference in reduction of pain immediately post treatment but no difference at intermediate‐term follow‐up.
Function
There was no statistical significant difference in improved function immediately post treatment and at intermediate‐term follow‐up.
Patient Satisfaction
There was no difference between groups in patient satisfaction at immediate post treatment follow‐up.
Conclusion : There is low quality evidence (one trial, 133 participants, Kuijper 2009) showing cervical mobilization and stabilization exercises may improve pain slightly, but may make no difference in function and patient satisfaction when compared immediately post treatment with a control for acute cervical radiculopathy. However, there may be no difference in pain and functional improvement at intermediate‐term follow‐up.
Adverse Events
Fifteen of the 27 trials did not report on adverse events (Andersen 2008; Andersen Ch 2012; Ang 2009; Beer 2012; Dellve 2011; Hall 2007; Hallman 2011; Hansson 2013; Humphreys 2002; Kjellman 2002; Kuijper 2009; Lundblad 1999; Revel 1994; Takala 1994; Viljanen 2003); six trials found patients did not report any adverse events (Allan 2003; Chiu 2005; Franca 2008; Helewa 2007; Lange 2013; Martel 2011; six studies reported self‐limiting side effects such as headache, neck, shoulder or thoracic pain or worsening of symptoms (Andersen 2011; Bronfort 2001; Jull 2002; Rendant 2011; Stewart 2007; von Trott 2009).
Discussion
Summary of main results
Limiting the eligible trials to those with single interventions that compared exercise with a control or comparative group maximized the opportunity to evaluate the treatment effect of exercise interventions. Moreover, having selected a priori an exercise classification system allowed us to use a clinical rationale for selecting studies with similar interventions for interpretation and inclusion within meta‐analyses, particularly for the outcomes of pain and function. Although there were only 28 studies eligible for this systematic review, these two new strategies provided greater clarity in our conclusions about the effectiveness of exercise therapy. In summary, for moderate quality evidence there is still uncertainty about the effectiveness of exercise for neck pain. Further research is likely to have an important impact on the effect estimate. Furthermore, for low quality evidence further research is very likely to have an important impact on the effect estimate. The reader should take these limitations into account when interpreting the following evidence statements.
Moderate to low quality evidence suggests there can be small to large beneficial effects on chronic mechanical neck pain when combining the use of cervical, shoulder/scapulothoracic strengthening and stretching exercises immediately post treatment and at short‐ and long‐term follow‐up. There may also be a small to moderate beneficial effect on function when combining the use of cervical, shoulder/scapulothoracic strengthening and stretching exercises immediately post treatment and at short‐ to long‐term follow‐up.
Moderate grade evidence suggests there may be a slight beneficial effect on chronic mechanical neck pain with the use of scapulothoracic and upper extremity endurance training immediately post treatment.
Moderate quality evidence suggests there may be a slight improvement in chronic mechanical neck pain and function with the use of Qigong (stretch, endurance, dynamic stabilization exercises combined with cognitive exercises emphasizing mindfulness and emotion) immediately post treatment and at short‐term follow‐up. There may be little to no difference in quality of life and general perceived effect measures with the use of qigong exercises.
Low quality evidence suggests there may be a large beneficial effect in cervicogenic headaches with the use of craniovertebral stretch and range of motion exercises (C1‐C2 Self‐SNAG) both at short‐ and long‐term follow‐up.
Moderate quality evidence suggests there is a large beneficial effect on pain in cervicogenic headaches when combining the use of static and dynamic cervical, scapulothoracic strengthening and endurance exercises including pressure biofeedback immediately post treatment and probably improves pain moderately in cervicogenic headaches at long‐term follow‐up. There was also a moderate beneficial effect on function immediately post treatment and at long‐term follow‐up.
Low quality evidence suggest that there is a slight beneficial effect on pain with acute cervical radiculopathy when combining the use of static and dynamic cervical, scapulothoracic and upper extremity stretching and strengthening immediately post treatment but not at intermediate‐term follow‐up. There was little to no difference in function.
Low grade evidence suggests there is little to no difference in chronic mechanical neck pain and function with respect to the use of breathing exercises or general fitness training
Low grade evidence suggests there is little to no difference in chronic mechanical neck pain and function with respect to the use of cervical spine stretches and range of motion exercises.
Moderate grade evidence suggests there is little to no difference in chronic neck pain and function with the use of cervical, scapulothoracic and upper extremity stretching and endurance training both immediately post treatment as well as short‐ and long‐term follow‐up.
Low quality evidence suggests that there is little to no difference in chronic mechanical neck pain when combining the use of trunk and upper extremity stretching, balance exercises and aerobic training immediately post treatment.
Low quality evidence suggests that there is little to no difference in chronic mechanical neck pain when combining the use of endurance, general stretching, body mechanics and lumbar stabilization exercises at short‐term follow‐up.
Knowledge of key multimodal approaches like exercise and manual therapy is still needed as this model of combined care is commonly used in clinical practice.
Overall completeness and applicability of evidence
Our group looked at the clinical applicability of 28 trials associated with neck disorders versus control: 25 studies were interested in neck pain, two in cervicogenic headache and one in cervical radiculopathy. The level of evidence ranged from low to moderate. Most studies adequately described the study population. Three studies did not specify the duration of neck pain. Radicular signs and symptoms were present in 14% of the studies, absent in 29% and not specified in 57%. Of the 28 studies in this update, 36% provided sufficient details for the treatment protocol to be replicated and 18 studies omitted important details about the treatment administration or included insufficient description of the qualifications of the treatment provider.
The outcomes were as follow: 96% of the studies reported pain, 64% reported function and 36% reported quality of life or patient satisfaction. Of the ones that reported pain, function and quality of life, benefit was shown in respectively 81%, 89% and 80%, but no study reached the minimal clinically important difference for any outcome. These results can be applied to an adult population suffering from acute, subacute and chronic mechanical neck pain.
Follow‐up was reported at immediate or short term in 54% of the studies and the remaining trials (46%) had intermediate‐ or long‐term measurement timing. Minor and short lasting adverse events were reported in 25% of the studies, their occurrence was not specified in 57%, and no adverse events happened in the remaining studies (18%). Drop‐outs occurred in 68% of the studies and none evaluated the cost of care. To better understand the direct and indirect costs of the different treatments and make decisions regarding the most effective and efficient type of care, attempts to evaluate and report cost‐related outcomes are required.
The clinical applicability was evaluated in 28 studies contrasting the use of exercise for neck pain compared with a control group. Sample population was adequately described in 82% of the trials. Treatment protocol was adequately described in 36% of the trials; the remaining studies omitted information about treatment providers and exercise dosage, which hinders reproducibility. The magnitude of effect and clinical applicability showed benefits that outweigh any transient and minor side effects. The level of evidence of these studies varied from low to moderate; thus clinicians should not underestimate their clinical judgement in the choice of optimal treatment modality for client needs.
The stage of the pathology, commonly described as acute, subacute and chronic, can certainly affect the effect size of an intervention such as exercise. For instance, in regards to pain, none of the included trials reached the minimal clinically important difference of 2.0 points (NPRS) or 20 mm (VAS); this could be related to the low to moderate pain levels experienced by the chronic neck pain population with lesser room for improvement compared to an acute neck pain population with high initial levels of pain. Thus, according to the stage of the pathology, it could respectively under or overestimate the size effect of a specific exercise.
To date, there is no standardized definition of mechanical neck pain even if it has evolved over the last three decades. Spitzer 1987 defined mechanical neck pain as complaints of pain, stiffness, and tenderness with or without referral to proximal extremity. Merskey 1994 proposed the following definition: “pain perceived as arising from anywhere within the region bounded superiorly by the superior nuchal line through the tip of the first thoracic spinous process, and laterally by the sagittal plane tangential to the lateral borders of the neck.” More recently, other authors suggested different definitions such as generalized neck and/or shoulder pain with mechanical characteristics including: symptoms provoked by maintained neck postures or by movement, or by palpation of the cervical muscles (Fernandez‐de‐las‐Penas 2007). Thus, considering that mechanical neck pain is a heterogeneous group, subgrouping based on diagnosis, treatment or prognosis system classification would be useful to increase homogeneity for research and clinical applicability.
Exercise classification is also of utmost importance when interested in the nature of the intervention. The model implemented in this review, proposed by Sahrmann 2002, reveals the interaction between dosage, elements of movement system and activity by describing the physiological effect of exercise on the body rather than describing the types of activity used to produce that effect. Using this kind of model would allow practitioners and researchers to classify exercises into a specific category by recognizing their mechanisms of actions. It also allows placement of similar exercise interventions from different trials into more homogeneous subgroups enabling meta‐analyses. Thus, by a better understanding and classification of the physical impairments, exercise interventions and stage or type of pathology, accuracy in the clinical applicability of results could be improved.
In general, there is also limited evidence on optimal dosage requirements (Bronfort 2001; Jull 2002) for exercise therapies, and other modalities used to treat neck disorders. To address questions regarding the dose of therapies used to treat the neck, researchers (Gross 2007) have recommended using factorial designs and studying only single interventions (Carroll 2008b; Helewa 2007). Subsequently, dosage comparisons of similar types of exercises (or exercises that address the same element) can be made; these comparisons can be used to evaluate the impact of dosage variation of the exercise element on the magnitude of treatment outcomes. Specific dosage information is clinically relevant and specific therapeutic recommendations can be drawn from such clinical trials.
Different control interventions have been used in the reference group, but were absent in the experimental group in eight trials of this review. A study design comparing exercise and another intervention with the same intervention was used in four trials. No intervention or wait list as a control intervention was used in the remaining 12 studies. Using different control interventions could lead to underestimation of the effect of exercise if that intervention also shows beneficial effects. Using the same intervention in both exercise and control group may provide a better idea of adding exercise to a treatment plan, but an interaction of effect is also possible and could lead to overestimation of the effect of exercise.
Self‐reported outcome measures of function are popular in the literature to evaluate the effectiveness of treatment in a patient’s everyday life. The Neck Disability Index (NDI) is well accepted in the current literature and is one of the most used tools to assess patient’s functional capacities. However, the NDI recently showed an insufficient unidimensionality ( Ailliet 2013;Hung 2014 ; van der Velde 2009) and a very large floor effect. Its use in research in regards to construct validity is now questioned.
The use of only self‐reported outcome measures may bias the effect estimate. More objective and performance‐based measures of functional tasks should be used in conjunction with subjective measures and questionnaires to establish a complete picture of the results. Such tools need to be developed and integrated into future research.
The timing of outcome measurement has been well reported in all trials. However, most studies did not specify if participants continued their exercises program at home after the end of the intervention period. Knowing the instructions given for the continuation or cessation of the exercise before follow‐up would improve the accuracy of their effectiveness according to how long they were performed. This information could lead to conclusions about carry‐over effect of the exercise program.
Quality of the evidence
One of the major methodological difficulties inherent to studies evaluating exercise interventions is blinding of therapists and patients. None of the trials in this review blinded the care provider, as this is not possible in an exercise trial. Patient blinding can minimize expectation bias by ensuring the treatments are equally credible and acceptable to patients; patients have limited experience or expectations for either the index treatment or control intervention. However, the nature of exercise interventions makes it difficult to blind the patient and care provider. Therefore, it is very important to control for measurement bias by blinding the outcome assessor and the data analyst. A caveat to this is that the use of self‐reported outcome measures de facto makes the patient the outcome assessor and blinding cannot be achieved easily. Two of the 28 trials did blind the outcome assessor and therefore, blinding can be obtained for certain outcomes.
Other issues that are important in studies evaluating exercise therapy are that of compliance (reducing the treatment effect), co‐intervention (increasing the treatment effect and reducing the magnitude of effect if it occurs in the control group) and contamination (reducing the magnitude of effect). The intervention requires patient motivation and therefore strategies to support behavior changes (Teixeira 2012). Twelve of the 28 studies had acceptable compliance, and eight of 28 studies monitored co‐interventions. This provides greater confidence that the outcome is due to the exercise intervention and that the dosage is consistent between individual participants and treatment groups.
Adequate randomization is a crucial component for a randomized controlled trial. However, adequate sequence generation was evident in only 46% (13/28) of the trials included in this review. Greater care should be taken to ensure the method of randomization is adequate and clearly reported.
Ninety‐six per cent (27/28) of the clinical trials contained small sample sizes (<70 per arm analyzed). Risk of random error will of course be reduced with increased precision or increased sample size. Request for larger trials is a challenge on a per site basis. A co‐ordinated multi‐centre trial is one answer but recruiting and retaining is the challenge. For this it is helpful to identify the motivation factors for participation. First, motivation for clinical study participation has been linked to types of personal benefit, including financial and therapeutic (Nappo 2013). Although financial incentives are important in recruiting healthy volunteers, their motivations are not limited to financial gains (Stunkel 2011). It has been proposed that altruism should be the main reason for a person's decision to participate in a research study (Grady 2001). Ideally, the volunteer is capable of making decisions based on the information provided about the proposed study, and understands the purpose, risks, benefits, alternatives and requirements of the study. After receiving this information, the volunteer is able to decide to participate, free from coercion or improper influences (Grady 2001). Second, clinician recruitment may be difficult. Technology has the potential to facilitate this task. With the emerging presence of electronic medical charting, data sharing has become a point of interest. By training clinicians around the world, patients could be screened on a global scale. A standardized protocol could then be applied in a standardized setting to those who meet the inclusion criteria. As a result, valid and reliable objective measures with low risk of bias could be gathered and accessed by researchers internationally. Finally, it is imperative for investigators to clearly articulate the relevance of the study to the appropriate stakeholders: the neck pain patients who will allocate a significant amount of time to the trial and the clinicians who will contribute patients to the study and, in the process, upset their usual routine and suffer some financial loss. The relevance of the study needs to emphasize the possible benefits to present and future patients, to the healthcare system and to society in general.
This being said, the overarching feature to low precision resides in the subclassification of control trials and restriction of their use. What first must be done is to establish a firm foundation of the effect of (x type of) exercise in clinical control trials and not include head‐to‐head exercise comparison trials. We believe once sound evidence has been formed, the next step is to do comparison trials to establish the superiority of different variations of similar exercises.
Potential biases in the review process
The validity of any systematic review is dependent on the selection of all relevant studies. Although studies published in any language were accepted, many scientific journals in non‐English languages are not indexed in MEDLINE and Embase. We did not search non‐English databases, which may have introduced 'language bias' in the review. Studies without a control or comparative group were excluded so that exercise treatment effectiveness and efficacy could be properly ascertained (Carroll 2008b). This review contains only published studies therefore 'publication bias' was not guarded against.
Agreements and disagreements with other studies or reviews
This review has provided more detailed informations with respect to the degree of evidence and the types of exercise that have an impact on neck pain.
There were no new trials added to our update with respect to acute whiplash associated disorders (WAD) that compared exercise with a control.
For chronic neck pain, Leaver 2010 showed evidence supporting stretching/range of motion (ROM) exercises for pain relief immediately post treatment but no change in the intermediate and long term for pain and function. Our review disagreed with these findings while using the same evidence. We found low quality evidence that neck stretching or ROM had no benefit relative to a control treatment for chronic neck pain and function from immediately post treatment up to long‐term follow‐up.
Three reviews included Qigong (an approach encompassing stretching, strengthening, endurance training, balance/co‐ordination, cardiovascular and cognitive/affective elements). Lee 2009 showed no evidence of benefit in the short term while Southerst 2014 and Teasell 2010c found Qigong exercise effective on pain in the short term for chronic WAD. Although our review supported the latter findings, there was only a very small magnitude of effect on pain and function, but not on global perceived effect and quality of life immediately post treatment. Additionally, a non‐significant effect of a three‐point change on NDI (zero to 50 scale) for function was noted at long‐term follow‐up. For cervico‐scapulothoracic and upper extremity stretching and strengthening,Bertozzi 2013, similarly to our data, suggested that it may improve pain immediately post treatment and at short‐term follow‐up. A meta‐analysis of four studies (Bronfort 2001; Chiu 2005; Franca 2008; Martel 2011) of moderate quality evidence showed medium pain relief and function improvement at immediately post treatment and long‐term follow‐up. Changes in global perceived effect measures indicated a difference immediately post treatment and at long‐term follow‐up. Finally, for stretching and strengthening, two new reviews (Bertozzi 2013; Southerst 2014) showed evidence of benefit on pain and function in long‐term follow‐up. Our review concurred with these reviews. The studies showed moderate quality evidence and two trials (Rendant 2011; von Trott 2009) showed cervico‐scapulothoracic and shoulder stretching, strengthening and stabilization exercises probably have medium benefit for pain and function, but not global perceived effect and quality of life at immediately post treatment and at short‐term follow‐up.
Neuromuscular exercises (Leaver 2010; Teasell 2010b) showed evidence of benefit for subacute/chronic neck pain with or without WAD in the short term for pain and function. This review found very low quality evidence (Revel 1994) for a moderate reduction in pain and function improvement in the short term for eye‐neck co‐ordination exercises.
Salt 2011 found a multimodal exercise approach favoured exercise in acute radiculopathy. There was inconclusive evidence for the effect of non‐invasive management. We found low quality evidence (Kuijper 2009) showing cervical mobilization and specific stabilization exercises may improve pain slightly, but may make no difference in function and patient satisfaction when compared immediately post treatment with a control. There may be no difference in pain and functional improvement at intermediate‐term follow‐up. The challenge in acute radiculopathy is to determine the utility of exercises that provide immediate relief but not longer‐term benefit.
Our review is in agreement with 1) The reports by Racicki 2012, Bronfort 2009, and Hurwitz 2008, suggesting evidence of benefit for exercise in subacute/chronic cervicogenic headache and 2) Bertozzi 2013 about cardiovascular/aerobic training. There is low quality evidence (Andersen 2008) that 3) general fitness training may have no difference in pain when compared with a reference intervention for (sub)acute/chronic neck pain immediately post treatment.
Authors' conclusions
Implications for practice.
This review shows that there is still no high quality evidence and uncertainty about the effectiveness of exercise for neck pain. Further research is likely and in some cases very likely to have an important impact on the effect estimate. Moderate quality evidence supports the use specific strengthening exercises as a part of routine practice for chronic neck pain, cervicogenic headache and radiculopathy. Specifically the use of strengthening exercises for the cervical spine, scapulothoracic and shoulders may be beneficial in reducing pain and improving function when used for the treatment of chronic mechanical neck pain, cervicogenic headache and cervical radiculopathy. Moderate quality evidence supports the use of strengthening exercises, combined with endurance or stretching exercises may also yield similar beneficial results. However, low quality evidence notes when only stretching or only endurance type exercises were used for the cervical, scapulothoracic and shoulders regions, there may be minimal beneficial effects for both neck pain and function. There is moderate quality evidence to suggest beneficial effects of a specific type exercises (e.g. sustained natural apophyseal glides) for cervicogenic headache.
Implications for research.
This update shows some positive findings for using exercise for neck pain, but further research is warranted because it is (very) likely to have an important impact on the effect estimate. Ongoing research to increase sample size and to pool similar data is required to further validate these findings, particularly in the area of cervicogenic headache and cervical radiculopathy.
Neck pain continues to be a somewhat heterogeneous classification. Use of prognostic and treatment classification variables may aid in distilling, which subgroups will most benefit from what specific exercise. An international standardization of a ‘core outcome measure set’ is needed to improve reporting of effects and to aid in the systematic review process. The length of follow‐up in many studies is limited and adherence to exercise not monitored. Adequate recording of the types and exact dosage of the exercise programs is also important to assist in translation of its use into practice as well as for the pooling of data to improve in directness of the outcomes.
What's new
| Date | Event | Description |
|---|---|---|
| 27 June 2014 | New citation required and conclusions have changed | Based on 28 trials, five subclasses of exercise were identified to show moderate quality evidence of be beneficial versus two in our 2012 update. Four subclasses of exercise were identified showing low quality evidence of no benefit in this update compared to three in our 2012 update. |
| 22 May 2014 | New search has been performed | Eligible trials were added that compared exercise with a control group. Twenty‐eight trials have been incorporated resulting in a report of 25 evidence‐based findings. |
History
Protocol first published: Issue 2, 2003 Review first published: Issue 3, 2005
| Date | Event | Description |
|---|---|---|
| 8 November 2013 | New citation required but conclusions have not changed | Eligible trials were limited to those with single interventions that compared exercise with a control or comparative group. Conclusions similar. |
| 8 November 2013 | New search has been performed | Updated literature search November 08 2013 |
| 18 June 2008 | Amended | Converted to new review format. |
| 4 May 2008 | New citation required and conclusions have changed | Substantive amendment |
| 1 June 2005 | Amended | June 2005 ‐‐ we reduced the length of the abstract; made some edits to the text for clarification; corrected the format in some of the references. |
Acknowledgements
We thank the Cervical Overview Group, Bruce Craven, for their contribution to this document. Dr. Craven was instrumental in directing us to the exercise classification framework that was used as our foundation within this review.
Appendices
Appendix 1. Computerised search strategies
MEDLINE‐ OVID
1. Neck Pain/
2. exp Brachial Plexus Neuropathies/
3. exp neck injuries/ or exp whiplash injuries/
4. cervical pain.mp.
5. neckache.mp.
6. whiplash.mp.
7. cervicodynia.mp.
8. cervicalgia.mp.
9. brachialgia.mp.
10. brachial neuritis.mp.
11. brachial neuralgia.mp.
12. neck pain.mp.
13. neck injur*.mp.
14. brachial plexus neuropath*.mp.
15. brachial plexus neuritis.mp.
16. thoracic outlet syndrome/ or cervical rib syndrome/
17. Torticollis/
18. exp brachial plexus neuropathies/ or exp brachial plexus neuritis/
19. cervico brachial neuralgia.ti,ab.
20. cervicobrachial neuralgia.ti,ab.
21. (monoradicul* or monoradicl*).tw.
22. or/1‐21
23. exp headache/ and cervic*.tw.
24. exp genital diseases, female/
25. genital disease*.mp.
26. or/24‐25
27. 23 not 26
28. 22 or 27
29. neck/
30. neck muscles/
31. exp cervical plexus/
32. exp cervical vertebrae/
33. atlanto‐axial joint/
34. atlanto‐occipital joint/
35. Cervical Atlas/
36. spinal nerve roots/
37. exp brachial plexus/
38. (odontoid* or cervical or occip* or atlant*).tw.
39. axis/ or odontoid process/
40. Thoracic Vertebrae/
41. cervical vertebrae.mp.
42. cervical plexus.mp.
43. cervical spine.mp.
44. (neck adj3 muscles).mp.
45. (brachial adj3 plexus).mp.
46. (thoracic adj3 vertebrae).mp.
47. neck.mp.
48. (thoracic adj3 spine).mp.
49. (thoracic adj3 outlet).mp.
50. trapezius.mp.
51. cervical.mp.
52. cervico*.mp.
53. 51 or 52
54. exp genital diseases, female/
55. genital disease*.mp.
56. exp *Uterus/
57. 54 or 55 or 56
58. 53 not 57
59. 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 58
60. exp pain/
61. exp injuries/
62. pain.mp.
63. ache.mp.
64. sore.mp.
65. stiff.mp.
66. discomfort.mp.
67. injur*.mp.
68. neuropath*.mp.
69. or/60‐68
70. 59 and 69
71. Radiculopathy/
72. exp temporomandibular joint disorders/ or exp temporomandibular joint dysfunction syndrome/
73. myofascial pain syndromes/
74. exp "Sprains and Strains"/
75. exp Spinal Osteophytosis/
76. exp Neuritis/
77. Polyradiculopathy/
78. exp Arthritis/
79. Fibromyalgia/
80. spondylitis/ or discitis/
81. spondylosis/ or spondylolysis/ or spondylolisthesis/
82. radiculopathy.mp.
83. radiculitis.mp.
84. temporomandibular.mp.
85. myofascial pain syndrome*.mp.
86. thoracic outlet syndrome*.mp.
87. spinal osteophytosis.mp.
88. neuritis.mp.
89. spondylosis.mp.
90. spondylitis.mp.
91. spondylolisthesis.mp.
92. or/71‐91
93. 59 and 92
94. exp neck/
95. exp cervical vertebrae/
96. Thoracic Vertebrae/
97. neck.mp.
98. (thoracic adj3 vertebrae).mp.
99. cervical.mp.
100. cervico*.mp.
101. 99 or 100
102. exp genital diseases, female/
103. genital disease*.mp.
104. exp *Uterus/
105. or/102‐104
106. 101 not 105
107. (thoracic adj3 spine).mp.
108. cervical spine.mp.
109. 94 or 95 or 96 or 97 or 98 or 106 or 107 or 108
110. Intervertebral Disk/
111. (disc or discs).mp.
112. (disk or disks).mp.
113. 110 or 111 or 112
114. 109 and 113
115. herniat*.mp.
116. slipped.mp.
117. prolapse*.mp.
118. displace*.mp.
119. degenerat*.mp.
120. (bulge or bulged or bulging).mp.
121. 115 or 116 or 117 or 118 or 119 or 120
122. 114 and 121
123. intervertebral disk degeneration/ or intervertebral disk displacement/
124. intervertebral disk displacement.mp.
125. intervertebral disc displacement.mp.
126. intervertebral disk degeneration.mp.
127. intervertebral disc degeneration.mp.
128. 123 or 124 or 125 or 126 or 127
129. 109 and 128
130. 28 or 70 or 93 or 122 or 129
131. animals/ not (animals/ and humans/)
132. 130 not 131
133. exp *neoplasms/
134. exp *wounds, penetrating/
135. 133 or 134
136. 132 not 135
137. Neck Pain/rh [Rehabilitation]
138. exp Brachial Plexus Neuropathies/rh
139. exp neck injuries/rh or exp whiplash injuries/rh
140. thoracic outlet syndrome/rh or cervical rib syndrome/rh
141. Torticollis/rh
142. exp brachial plexus neuropathies/rh or exp brachial plexus neuritis/rh
143. 137 or 138 or 139 or 140 or 141 or 142
144. Radiculopathy/rh
145. exp temporomandibular joint disorders/rh or exp temporomandibular joint dysfunction syndrome/rh
146. myofascial pain syndromes/rh
147. exp "Sprains and Strains"/rh
148. exp Spinal Osteophytosis/rh
149. exp Neuritis/rh
150. Polyradiculopathy/rh
151. exp Arthritis/rh
152. Fibromyalgia/rh
153. spondylitis/rh or discitis/rh
154. spondylosis/rh or spondylolysis/rh or spondylolisthesis/rh
155. or/144‐154
156. 59 and 155
157. exp Combined Modality Therapy/
158. Exercise/
159. Physical Exertion/
160. exp Exercise Therapy/
161. exp Electric Stimulation Therapy/
162. exp Rehabilitation/
163. exp Physical Therapy Modalities/
164. Hydrotherapy/
165. postur* correction.mp.
166. Feldenkrais.mp.
167. (alexander adj (technique or method)).tw.
168. Relaxation Therapy/
169. Biofeedback, Psychology/
170. or/157‐169
171. 136 and 170
172. 143 or 156 or 171
173. animals/ not (animals/ and humans/)
174. 172 not 173
175. exp randomised controlled trials as topic/
176. randomised controlled trial.pt.
177. controlled clinical trial.pt.
178. (random* or sham or placebo*).tw.
179. placebos/
180. random allocation/
181. single blind method/
182. double blind method/
183. ((singl* or doubl* or trebl* or tripl*) adj25 (blind* or dumm* or mask*)).ti,ab.
184. (rct or rcts).tw.
185. (control* adj2 (study or studies or trial*)).tw.
186. or/175‐185
187. 174 and 186
188. limit 187 to yr="2006 ‐Current"
189. limit 187 to yr="1902 ‐ 2005"
190. guidelines as topic/
191. practice guidelines as topic/
192. guideline.pt.
193. practice guideline.pt.
194. (guideline? or guidance or recommendations).ti.
195. consensus.ti.
196. or/190‐195
197. 174 and 196
198. 136 and 196
199. 197 or 198
200. limit 199 to yr="2006 ‐Current"
201. limit 199 to yr="1902 ‐ 2005"
202. meta‐analysis/
203. exp meta‐analysis as topic/
204. (meta analy* or metaanaly* or met analy* or metanaly*).tw.
205. review literature as topic/
206. (collaborative research or collaborative review* or collaborative overview*).tw.
207. (integrative research or integrative review* or intergrative overview*).tw.
208. (quantitative adj3 (research or review* or overview*)).tw.
209. (research integration or research overview*).tw.
210. (systematic* adj3 (review* or overview*)).tw.
211. (methodologic* adj3 (review* or overview*)).tw.
212. exp technology assessment biomedical/
213. (hta or thas or technology assessment*).tw.
214. ((hand adj2 search*) or (manual* adj search*)).tw.
215. ((electronic adj database*) or (bibliographic* adj database*)).tw.
216. ((data adj2 abstract*) or (data adj2 extract*)).tw.
217. (analys* adj3 (pool or pooled or pooling)).tw.
218. mantel haenszel.tw.
219. (cohrane or pubmed or pub med or medline or embase or psycinfo or psyclit or psychinfo or psychlit or cinahl or science citation index).ab.
220. or/202‐219
221. 174 and 220
222. limit 221 to yr="2006 ‐Current"
223. limit 221 to yr="1902 ‐ 2005"
224. (ae or to or po or co).fs.
225. (safe or safety or unsafe).tw.
226. (side effect* or side event*).tw.
227. ((adverse or undesirable or harm* or injurious or serious or toxic) adj3 (effect* or event* or reaction* or incident* or outcome*)).tw.
228. (abnormalit* or toxicit* or complication* or consequence* or noxious or tolerabilit*).tw.
229. or/224‐228
230. 174 and 229
231. limit 230 to yr="2006 ‐Current"
232. limit 230 to yr="1902 ‐ 2005"
233. limit 187 to ed=20100701‐20120313
234. limit 199 to ed=20100701‐20120313
235. limit 221 to ed=20100701‐20120313
236. limit 230 to ed=20100701‐20120313
237. limit 189 to ed=20120313‐20131108
Embase‐OVID
1. neck pain/
2. brachial plexus neuropathy/
3. neck injury/ or whiplash injury/
4. cervical pain.mp.
5. neckache.mp.
6. whiplash.mp.
7. cervicodynia.mp.
8. cervicalgia.mp.
9. brachialgia/
10. brachialgia.mp.
11. brachial neuritis.mp.
12. brachial neuralgia.mp.
13. neck pain.mp.
14. neck injur*.mp.
15. brachial plexus neuropath*.mp.
16. brachial plexus neuritis.mp.
17. thorax outlet syndrome/
18. torticollis/
19. cervico brachial neuralgia.ti,ab.
20. cervicobrachial neuralgia.ti,ab.
21. (monoradicul* or monoradicl*).tw.
22. or/1‐21
23. exp headache/ and cervic*.tw.
24. exp gynecologic disease/
25. genital disease*.mp.
26. exp *uterine cervix/
27. or/24‐26
28. 23 not 27
29. 22 or 28
30. neck/ or neck muscle/
31. cervical plexus/
32. cervical spine/
33. atlantoaxial joint/
34. atlantooccipital joint/
35. atlas/
36. "spinal root"/
37. brachial plexus/
38. (odontoid* or cervical or occip* or atlant*).tw.
39. odontoid process/
40. cervical vertebra.mp.
41. cervical vertebrae.mp.
42. cervical plexus.mp.
43. cervical spine.mp.
44. (neck adj3 muscles).mp.
45. (brachial adj3 plexus).mp.
46. (thoracic adj3 vertebra?).mp.
47. neck.mp.
48. (thoracic adj3 spine).mp.
49. (thoracic adj3 outlet).mp.
50. trapezius.mp.
51. cervical.mp.
52. cervico*.mp.
53. 51 or 52
54. exp gynecologic disease/
55. genital disease*.mp.
56. exp *uterine cervix/
57. 54 or 55 or 56
58. 53 not 57
59. 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 58
60. exp pain/
61. exp injury/
62. pain.mp.
63. ache.mp.
64. sore.mp.
65. stiff.mp.
66. discomfort.mp.
67. injur*.mp.
68. neuropath*.mp.
69. or/60‐68
70. radiculopathy/
71. temporomandibular joint disorder/
72. myofascial pain/
73. spondylosis/ or cervical spondylosis/
74. neuritis/
75. exp arthritis/
76. fibromyalgia/
77. exp spondylitis/
78. diskitis/
79. spondylolisthesis/
80. radiculopathy.mp.
81. radiculitis.mp.
82. temporomandibular.mp.
83. myofascial pain syndrome*.mp.
84. spinal osteophytosis.mp.
85. neuritis.mp.
86. spondylosis.mp.
87. spondylitis.mp.
88. spondylolisthesis.mp.
89. or/70‐88
90. 59 and 89
91. neck/
92. cervical spine/
93. neck.mp.
94. (thoracic adj3 vertebra?).mp.
95. cervical.mp.
96. cervico*.mp.
97. exp gynecologic disease/
98. genital disease*.mp.
99. exp *uterine cervix/
100. or/97‐99
101. 95 or 96
102. 101 not 100
103. (thoracic adj3 spine).mp.
104. cervical spine.mp.
105. 91 or 92 or 93 or 94 or 102 or 103 or 104
106. intervertebral disk/
107. (disc or discs).mp.
108. (disk or disks).mp.
109. 106 or 107 or 108
110. 105 and 109
111. herniat*.mp.
112. slipped.mp.
113. prolapse*.mp.
114. displace*.mp.
115. degenerat*.mp.
116. (bulge or bulged or bulging).mp.
117. 110 or 111 or 112 or 113 or 114 or 115 or 116
118. 110 and 117
119. intervertebral disk hernia/
120. intervertebral disk degeneration/
121. intervertebral disc degeneration.mp.
122. intervertebral disk degeneration.mp.
123. intervertebral disc displacement.mp.
124. intervertebral disk displacement.mp.
125. 119 or 120 or 121 or 122 or 123 or 124
126. 105 and 125
127. 59 and 69
128. 29 or 90 or 118 or 126 or 127
129. exp *neoplasm/
130. exp *penetrating trauma/
131. 129 or 130
132. 128 not 131
133. neck pain/rh [Rehabilitation]
134. brachial plexus neuropathy/rh
135. neck injury/rh or whiplash injury/rh
136. brachialgia/rh
137. thorax outlet syndrome/rh
138. Torticollis/rh
139. 133 or 134 or 135 or 136 or 137 or 138
140. radiculopathy/rh
141. temporomandibular joint disorder/rh
142. myofascial pain/rh
143. spondylosis/rh or cervical spondylosis/rh
144. neuritis/rh
145. exp arthritis/rh
146. fibromyalgia/rh
147. exp spondylitis/rh
148. diskitis/rh
149. spondylolisthesis/rh
150. or/140‐149
151. 59 and 150
152. exp exercise/
153. exp kinesiotherapy/
154. physical medicine/
155. feedback system/
156. biofeedback.tw.
157. relaxation training/
158. bodywork/ or alexander technique/ or feldenkrais method/
159. postur* correction.mp.
160. or/152‐159
161. 132 and 160
162. 139 or 151 or 161
163. human/
164. nonhuman/
165. animal/
166. animal experiment/
167. or/164‐166
168. 167 not (163 and 167)
169. 162 not 169
170. randomized controlled trial/
171. controlled clinical trial/
172. (random* or sham or placebo*).tw.
173. placebo/
174. randomization/
175. single blind procedure/
176. double blind procedure/
177. ((singl* or doubl* or trebl* or tripl*) adj5 (blind* or dumm*or mask*)).ti,ab.
178. (rct or rcts).tw.
179. (control* adj2 (study or studies or tiral*)).tw.
180. or/170‐179
181. human/
182. nonhuman/
183. animal/
184. animal experiment/
185. or/182‐184
186. 185 not (185 and 181)
187. 180 not 186
188. 169 and 187
189. limit 219 to yr="2006 ‐Current"
190. limit 219 to yr="1928 ‐ 2005"
191. guidelines as topic/
192. practice guidelines as topic/
193. (guideline? or guidance or recommendations).ti.
194. consensus.ti.
195. or/191‐194
196. 169 and 195
197. limit 196 to yr="2006 ‐Current"
198. limit 196 to yr="1928 ‐ 2005"
199. meta analysis/
200. systematic review/
201. (meta analy* or metaanaly* or met analy* or metanaly*).tw.
202. (collaborative research or collaborative review* or collaborative overview*).tw.
203. (integrative research or integrative review* or intergrative overview*).tw.
204. (quantitative adj3 (research or review* or overview*)).tw.
205. (research integration or research overview*).tw.
206. (systematic* adj3 (review* or overview*)).tw.
207. (methodologic* adj3 (review* or overview*)).tw.
208. biomedical technology assessment/
209. (hta or thas or technology assessment*).tw.
210. ((hand adj2 search*) or (manual* adj search*)).tw.
211. ((electronic adj database*) or (bibliographic* adj database*)).tw.
212. ((data adj2 abstract*) or (data adj2 extract*)).tw.
213. (data adj3 (pooled or pool or pooling)).tw.
214. (analys* adj3 (pool or pooled or pooling)).tw.
215. mantel haenszel.tw.
216. (cochrane or Pubmed or pub med or medline or embase or psycinfo or psyclit or psychinfo or psychlit or cinahl or science citation index).ab.
217. or/199‐216
218. 169 and 217
219. limit 218 to yr="2006 ‐Current"
220. limit 218 to yr="1928 ‐ 2005"
221. (ae or co or si or to).fs.
222. (safe or safety or unsafe).tw.
223. (side effect* or side event*).tw.
224. ((adverse or undesirable or harm* or injurious or serious or toxic) adj3 (effect* or event* or reaction* or incident* or outcome*)).tw.
225. (abnormalit* or toxicit* or complication* or consequence* or noxious or tolerabilit*).tw.
226. or/221‐225
227. 169 and 226
228. limit 227 to yr="2006 ‐Current"
229. limit 227 to yr="1928 ‐ 2005"
230. limit 188 to em=201027‐201210
231. limit 196 to em=201027‐201210
232. limit 218 to em=201027‐201210
233. limit 227 to em=201027‐201210
CENTRAL‐OVID
1. Neck Pain/
2. exp Brachial Plexus Neuropathies/
3. exp neck injuries/ or exp whiplash injuries/
4. cervical pain.mp.
5. neckache.mp.
6. whiplash.mp.
7. cervicodynia.mp.
8. cervicalgia.mp.
9. brachialgia.mp.
10. brachial neuritis.mp.
11. brachial neuralgia.mp.
12. neck pain.mp.
13. neck injur*.mp.
14. brachial plexus neuropath*.mp.
15. brachial plexus neuritis.mp.
16. thoracic outlet syndrome/ or cervical rib syndrome/
17. Torticollis/
18. exp brachial plexus neuropathies/ or exp brachial plexus neuritis/
19. cervico brachial neuralgia.ti,ab.
20. cervicobrachial neuralgia.ti,ab.
21. (monoradicul* or monoradicl*).tw.
22. or/1‐21
23. exp headache/ and cervic*.tw.
24. exp genital diseases, female/
25. genital disease*.mp.
26. or/24‐25
27. 23 not 26
28. 22 or 27
29. neck/
30. neck muscles/
31. exp cervical plexus/
32. exp cervical vertebrae/
33. atlanto‐axial joint/
34. atlanto‐occipital joint/
35. Cervical Atlas/
36. spinal nerve roots/
37. exp brachial plexus/
38. (odontoid* or cervical or occip* or atlant*).tw.
39. axis/ or odontoid process/
40. Thoracic Vertebrae/
41. cervical vertebrae.mp.
42. cervical plexus.mp.
43. cervical spine.mp.
44. (neck adj3 muscles).mp.
45. (brachial adj3 plexus).mp.
46. (thoracic adj3 vertebrae).mp.
47. neck.mp.
48. (thoracic adj3 spine).mp.
49. (thoracic adj3 outlet).mp.
50. trapezius.mp.
51. cervical.mp.
52. cervico*.mp.
53. 51 or 52
54. exp genital diseases, female/
55. genital disease*.mp.
56. exp *Uterus/
57. 54 or 55 or 56
58. 53 not 57
59. 29 or 30 or 31 or 32 or 33 or 34 or 35 or 36 or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 46 or 47 or 48 or 49 or 50 or 58
60. exp pain/
61. exp injuries/
62. pain.mp.
63. ache.mp.
64. sore.mp.
65. stiff.mp.
66. discomfort.mp.
67. injur*.mp.
68. neuropath*.mp.
69. or/60‐68
70. 59 and 69
71. Radiculopathy/
72. exp temporomandibular joint disorders/ or exp temporomandibular joint dysfunction syndrome/
73. myofascial pain syndromes/
74. exp "Sprains and Strains"/
75. exp Spinal Osteophytosis/
76. exp Neuritis/
77. Polyradiculopathy/
78. exp Arthritis/
79. Fibromyalgia/
80. spondylitis/ or discitis/
81. spondylosis/ or spondylolysis/ or spondylolisthesis/
82. radiculopathy.mp.
83. radiculitis.mp.
84. temporomandibular.mp.
85. myofascial pain syndrome*.mp.
86. thoracic outlet syndrome*.mp.
87. spinal osteophytosis.mp.
88. neuritis.mp.
89. spondylosis.mp.
90. spondylitis.mp.
91. spondylolisthesis.mp.
92. or/71‐91
93. 59 and 92
94. exp neck/
95. exp cervical vertebrae/
96. Thoracic Vertebrae/
97. neck.mp.
98. (thoracic adj3 vertebrae).mp.
99. cervical.mp.
100. cervico*.mp.
101. 99 or 100
102. exp genital diseases, female/
103. genital disease*.mp.
104. exp *Uterus/
105. or/102‐104
106. 101 not 105
107. (thoracic adj3 spine).mp.
108. cervical spine.mp.
109. 94 or 95 or 96 or 97 or 98 or 106 or 107 or 108
110. Intervertebral Disk/
111. (disc or discs).mp.
112. (disk or disks).mp.
113. 110 or 111 or 112
114. 109 and 113
115. herniat*.mp.
116. slipped.mp.
117. prolapse*.mp.
118. displace*.mp.
119. degenerat*.mp.
120. (bulge or bulged or bulging).mp.
121. 115 or 116 or 117 or 118 or 119 or 120
122. 114 and 121
123. intervertebral disk degeneration/ or intervertebral disk displacement/
124. intervertebral disk displacement.mp.
125. intervertebral disc displacement.mp.
126. intervertebral disk degeneration.mp.
127. intervertebral disc degeneration.mp.
128. 123 or 124 or 125 or 126 or 127
129. 109 and 128
130. 28 or 70 or 93 or 122 or 129
131. animals/ not (animals/ and humans/)
132. 130 not 131
133. exp *neoplasms/
134. exp *wounds, penetrating/
135. 133 or 134
136. 132 not 135
137. Neck Pain/rh [Rehabilitation]
138. exp Brachial Plexus Neuropathies/rh
139. exp neck injuries/rh or exp whiplash injuries/rh
140. thoracic outlet syndrome/rh or cervical rib syndrome/rh
141. Torticollis/rh
142. exp brachial plexus neuropathies/rh or exp brachial plexus neuritis/rh
143. 137 or 138 or 139 or 140 or 141 or 142
144. Radiculopathy/rh
145. exp temporomandibular joint disorders/rh or exp temporomandibular joint dysfunction syndrome/rh
146. myofascial pain syndromes/rh
147. exp "Sprains and Strains"/rh
148. exp Spinal Osteophytosis/rh
149. exp Neuritis/rh
150. Polyradiculopathy/rh
151. exp Arthritis/rh
152. Fibromyalgia/rh
153. spondylitis/rh or discitis/rh
154. spondylosis/rh or spondylolysis/rh or spondylolisthesis/rh
155. or/144‐154
156. 59 and 155
157. exp Combined Modality Therapy/
158. Exercise/
159. Physical Exertion/
160. exp Exercise Therapy/
161. exp Rehabilitation/
162. exp Physical Therapy Modalities/
162. Hydrotherapy/
163. postur* correction.mp.
164. Feldenkrais.mp.
165. (alexander adj (technique or method)).tw.
166. Relaxation Therapy/
167. Biofeedback, Psychology/
168. or/157‐167
169. 136 and 168
170. 143 or 156 or 169
171. limit 170 to yr="2006 ‐Current"
172. limit 170 to yr="1888 ‐ 2005"
173. limit 170 to yr="2010 ‐Current"
CINAHL‐EBSCO for Physical Medicine
S151 S90 or S104 or S150
S150 S82 and S149
S149 S105 or S106 or S107 or S108 or S109 or S110 or S111 or S112 or S113 or S114 or S115 or S116 or S117 or S118 or S119 or S120 or S121 or S122 or S123 or S124 or S125 or S126 or S127 or S128 or S129 or S130 or S131 or S132 or S133 or S134 or S135 or S136 or S137 or S138 or S139 or S140 or S141 or S142 or S143 or S144 or S145 or S146 or S147 or S148
S148 TX faradic
S147 MH biofeedback
S146 TX Relaxation Therapy
S145 MH Relaxation Therapy
S144 TX alexander N3 technique OR TX alexander N3 method
S143 TX Feldenkrais
S142 TX postur* correction
S141 MH ice
S140 TX Cryoanesthesia
S139 MH Cryoanesthesia
S138 TX vapocoolant spray
S137 (MH "Hyperthermia, Induced")
S136 MH Hydrotherapy
S135 MH cryotherapy
S134 TX repetitive magnetic stimulation
S133 (MH "Physical Therapy+")
S132 (MH "Physical Therapy Modalities+")
S131 MH lasers
S130 (MH "Phototherapy+")
S129 MH Ultrasonic Therapy
S128 (MH "Rehabilitation+")
S127 TX Laser Therapy
S126 (MH "Laser Therapy")
S125 TX traction
S124 MH traction
S123 TX pillow* OR TX collar*
S122 "Occlusal Splints"
S121 TX oral splints
S120 (MH "Periodontal Splints")
S119 TX taping
S118 TX kinesiotaping
S117 (MH "Orthoses")
S116 (MH "Electric Stimulation")
S115 (MH "Magnet Therapy")
S114 MH electromagnetics
S113 (MH "Electromagnetic Fields")
S112 "pulsed electromagnetic field"
S111 TX pulsed electro magnetic field
S110 (MH "Electrical Stimulation, Functional") OR (MH "Electrical Stimulation, Neuromuscular")
S109 (MH "Therapeutic Exercise+")
S108 (MH "Exertion")
S107 (MH "Exercise+")
S106 (MH "Exercise+")
S105 (MH "Combined Modality Therapy+")
S104 S34 and S103
S103 S91 or S92 or S93 or S94 or S95 or S96 or S97 or S98 or S99 or S100 or S101 or S102
S102 (MH "Spondylolisthesis/RH")
S101 (MH "Spondylolysis/RH") OR (MH "Spondylosis/RH")
S100 (MH "Spondylitis, Ankylosing/RH")
S99 (MH "Fibromyalgia/RH")
S98 (MH "Arthritis+/RH")
S97 (MH "Polyradiculopathy/RH")
S96 (MH "Neuritis/RH")
S95 (MH "Spinal Osteophytosis/RH")
S94 (MH "Sprains and Strains/RH")
S93 (MH "Myofascial Pain Syndromes/RH")
S92 (MH "Temporomandibular Joint Syndrome/RH") OR (MH "Temporomandibular Joint Diseases/RH")
S91 (MH "Radiculopathy/RH")
S90 S83 or S84 or S85 or S86 or S87 or S88 or S89
S89 (MH "Brachial Plexus Neuritis/RH")
S88 (MH "Torticollis/RH")
S87 (MH "Thoracic Outlet Syndrome/RH")
S86 (MH "Whiplash Injuries/RH")
S85 (MH "Neck Injuries/RH")
S84 (MH "Brachial Plexus Neuropathies/RH")
S83 (MH "Neck Pain/RH")
S82 S78 NOT S81
S81 S79 or S80
S80 (MM "Pregnancy+")
S79 (MM "Abortion, Induced+")
S78 S74 NOT S77
S77 S75 or S76
S76 (MM "Wounds, Penetrating+")
S75 (MM "Neoplasms+")
S74 S16 or S41 or S56 or S69 or S73
S73 S63 and S72
S72 S70 or S71
S71 TX intervertebral disk displacement or TX intervertebral disc displacement or TX intervertebral disk degeneration or TX intervertebral disc degeneration
S70 (MH "Intervertebral Disk Displacement")
S69 S67 and S68
S68 TX herniat* or TX slipped or TX prolapse* or TX displace* or TX degenerat* or TX ( bulged OR bulge OR bulging )
S67 S63 and S66
S66 S64 or S65
S65 TX disc or TX discs or TX disk or TX disks
S64 (MH "Intervertebral Disk")
S63 S61 NOT S62
S62 (MM "Genital Diseases, Female+") or ( (MM "Cervix") or (MM "Cervix Diseases") )
S61 S57 or S58 or S59 or S60
S60 TX thoracic N3 spine or TX cervical spine or TX cervico*
S59 TX neck or TX thoracic N3 vertebr*
S58 (MH "Thoracic Vertebrae")
S57 (MH "Neck")
S56 S34 and S55
S55 S42 or S43 or S44 or S45 or S46 or S47 or S48 or S49 or S50 or S51 or S52 or S53 or S54
S54 TX neuritis or TX spondylosis or TX spondylitis or TX spondylolisthesis
S53 TX myofascial pain syndome* or TX thoracic outlet syndrome* or TX spinalosteophytosis
S52 TX radiculopathy or TX radiculitis or TX temporomandibular
S51 (MH "Spondylolysis") or (MH "Spondylolisthesis+")
S50 (MH "Fibromyalgia")
S49 (MH "Arthritis+")
S48 (MH "Polyradiculopathy")
S47 (MH "Neuritis+")
S46 (MH "Spinal Osteophytosis")
S45 (MH "Sprains and Strains+")
S44 (MH "Myofascial Pain Syndromes+")
S43 (MH "Temporomandibular Joint Diseases+") or (MH "Temporomandibular Joint Syndrome")
S42 (MH "Radiculopathy")
S41 S34 and S40
S40 S35 or S36 or S37 or S38 or S39
S39 (MH "Neuralgia")
S38 TX stiff or TX discomfort or TX injur* or TX neuropath*
S37 TX pain or TX ache* or TX sore
S36 (MH "Wounds and Injuries+")
S35 (MH "Pain+")
S34 S33 NOT S32
S33 S17 or S18 or S19 or S20 or S21 or S22 or S23 or S24 or S25 or S26 or S27 or S28 or S29 or S30 or S31
S32 (MM "Genital Diseases, Female+") or ( (MM "Cervix") or (MM "Cervix Diseases") )
S31 TX trapezius or TX cervico*
S30 TX thoracic N3 spine or TX thoracic N3 outlet
S29 TX neck
S28 TX thoracic N3 verteb*
S27 TX brachial N3 plexus
S26 TX neck n3 muscles
S25 (MH "Thoracic Vertebrae")
S24 TX ondontoid* or TX cervical or TX occip* or TX atlant*
S23 (MH "Brachial Plexus+")
S22 (MH "Spinal Nerve Roots+")
S21 (MH "Atlanto‐Axial Joint") or (MH "Atlanto‐Occipital Joint")
S20 (MH "Cervical Vertebrae+") or (MH "Cervical Atlas")
S19 (MH "Cervical Plexus+")
S18 (MH "Neck")
S17 (MH "Neck Muscles+")
S16 S10 or S15
S15 S11 NOT S14
S14 S12 or S13
S13 (MM "Cervix") or (MM "Cervix Diseases")
S12 (MM "Genital Diseases, Female+")
S11 (MH "Headache+") and TX cervic*
S10 S1 or S2 or S3 or S4 or S5 or S6 or S7 or S8 or S9
S9 (MH "Brachial Plexus Neuritis")
S8 TX cervical brachial neuralgia
S7 TX cervical rib sydrome* or TX cervico brachial neuralgia or TX cervicobrachial neuralgia or TX monoradicul* or TX monoradicl*
S6 (MH "Thoracic Outlet Syndrome") or (MH "Torticollis")
S5 TX brachial neuralgia or TX neck pain or TX neck injur* or TX brachial plexus neuropath* or TX brachial plexus neuralgia or TX brachial plexus neuritis
S4 TX cervicalgia or TX brachialgia or TX brachial neuritis
S3 TX cervical pain or TX neckache or TX neck ache or TX whiplash or TX cervicodynia
S2 (MH "Neck Injuries+")
S1 (MH "Neck Pain") or (MH "Brachial Plexus Neuropathies") or (MH "Brachial Plexus Neuritis")
ICL Search
S1 Subject:"Neck Pain" OR Subject:"Brachial Plexus Neuritis" OR All Fields:"brachial plexus neuropathies"
S2 All Fields:brachial plexus neuropathy
S4 Subject:"Neck Injuries" OR Subject:"Whiplash Injuries" OR Subject:"Cervical Vertebrae / abnormalities
S5 All Fields:"cervical pain" OR All Fields:neckache OR All Fields:whiplash
S6 All Fields:cervicodynia OR All Fields:cervicalgia OR All Fields:brachialgia
S7 All Fields:"brachial neuritis" OR All Fields:"brachial neuralgia" OR All Fields:"neck pain"
S8 Subject:"Thoracic Outlet Syndrome" OR Subject:"Torticollis" OR All Fields:cervical rib syndrom*
S11 All Fields:cerv* AND All Fields:headache*
S12 All Fields:monoradicul* OR All Fields:monoradicl*
S13 S1 OR S2 OR S4 OR S5 OR S6 OR S7 OR S8 OR S11 OR S12
S14 Subject:"Neck" OR Subject:"Neck Muscles" OR Subject:"Cervical Vertebrae"
S16 Subject:"Cervical Atlas" OR Subject:"Atlanto‐Axial Joint" OR Subject:"Atlanto‐Occipital Joint" S17 Subject:"Atlas" OR Subject:"Spinal Nerve Roots" OR All Fields:"brachial plexus"
S18 All Fields:ondontoid* OR All Fields:occip* OR All Fields:atlant*
S20 Subject:"Odontoid Process" OR Subject:"Thoracic Vertebrae" OR All Fields:"cervical vertebrae"
S21 All Fields:"cervical spine" OR All Fields:trapezius OR All Fields:cervico*
S22 S14 OR S16 OR S17 OR S18 OR S20 OR S21
S23 Subject:"Pain" OR All Fields:sore OR All Fields:stiff
S24 All Fields:ache OR All Fields:pain OR All Fields:discomfort
S25 All Fields:injur* OR All Fields:neuropath*
S26 S23 OR S24 OR S25
S27 S22 AND S26
S28 Subject:"Radiculopathy" OR Subject:"Temporomandibular Joint Disorders" OR Subject:"Temporomandibular Joint Dysfunction Syndrome"
S30 Subject:"Myofascial Pain Syndromes" OR Subject:"Sprains and Strains" OR Subject:"Spinal Osteophytosis"
S31 Subject:"Neuritis" OR Subject:"Polyradiculoneuritis" OR Subject:"Arthritis"
S32 Subject:"Fibromyalgia" OR Subject:"Discitis" OR Subject:"Spondylitis"
S33 Subject:"Spondylolisthesis" OR Subject:"Spondylolysis" OR Subject:"Spondylosis"
S34 S28 OR S30 OR S31 OR S32 OR S33
S35 S22 AND S34
S36 Subject:"Neck" OR Subject:"Cervical Vertebrae" OR Subject:"Thoracic Vertebrae"
S37 All Fields:"thoracic spine" OR All Fields:"cervical spine" OR All Fields:cervico*
S38 S36 OR S37
S39 All Fields:herniat* OR All Fields:slipped OR All Fields:prolapse*
S40 All Fields:displace* OR All Fields:degenerat*
S41 All Fields:bulge OR All Fields:bulged OR All Fields:bulging
S42 S39 OR S40 OR S41
S43 S38 AND S42
S44 Subject:"Intervertebral Disk Displacement" OR All Fields:"intervertebral disk degeneration" OR All Fields:"intervertebral disc degeneration"
S45 All Fields:"Intervertebral Disk Displacement" OR All Fields:"intervertebral disc displacement"
S46 S44 OR S45
S47 S38 AND S46
S48 S13 OR S27 OR S35 OR S43 OR S47
S49 Subject:"Exercise" OR Subject:"Exercise Therapy" OR Subject:"Electric Stimulation therapy"
S50 Subject:"Physical Medicine" OR Subject:"Physical Therapy" OR Subject:"Physical Stimulation"
S51 Subject:"Physical Therapy Techniques" OR Subject:"Cryotherapy" OR Subject:"Hydrotherapy"
S52 Subject:"Hyperthermia, Induced" OR Subject:"Ice" OR Subject:"Biofeedback (Psychology)"
S53 Subject:"Relaxation Techniques" OR Subject:"Postural Balance" OR All Fields:feldenkrais
S54 S49 OR S50 OR S51 OR S52 OR S53
S55 S48 AND S54
S56 Subject:"Randomized Controlled Trials as Topic" OR Subject:"Controlled Clinical Trials" OR Subject:"Placebos"
S57 All Fields:random* OR All Fields:sham OR All Fields:placebo*
S58 All Fields:clinical trial* OR All Fields:"controlled study" OR All Fields:"controlled studies"
S59 All Fields:RCT OR All Fields:RCTs
S60 S56 OR S57 OR S58 OR S59
S61 S55 AND S60
S62 Year: from 2006 to 2014
S63 S61 AND S62
MANTIS‐OVID
1 neck pain.mp. [mp=title, abstract, descriptors] (2538)
2 brachial plexus neuropathies.mp. [mp=title, abstract, descriptors]
(58)
3 neck injuries.mp. [mp=title, abstract, descriptors] (201)
4 cervical pain.mp. [mp=title, abstract, descriptors] (196)
5 neckache.mp. [mp=title, abstract, descriptors] (3)
6 whiplash.mp. [mp=title, abstract, descriptors] (1165)
7 cervicodynia.mp. [mp=title, abstract, descriptors] (1)
8 cervicalgia.mp. [mp=title, abstract, descriptors] (20)
9 brachialgia.mp. [mp=title, abstract, descriptors] (25)
10 brachial neuritis.mp. [mp=title, abstract, descriptors] (15)
11 brachial neuralgia.mp. [mp=title, abstract, descriptors] (64)
12 brachial plexus neuropath*.mp. [mp=title, abstract, descriptors]
(70)
13 brachial plexus neuritis.mp. [mp=title, abstract, descriptors]
(65)
14 (thoracic outlet syndrome or cervical rib syndrome).mp.
[mp=title,
abstract, descriptors] (245)
15 torticollis.mp. [mp=title, abstract, descriptors] (227)
16 cervico brachial neuralgia.mp. [mp=title, abstract, descriptors]
(64)
17 (monoradicul* or monoradicl*).tw. (26)
18 or/1‐17 (4232)
19 headache.mp. and cervic*.tw. [mp=title, abstract, descriptors]
(796)
20 genital diseases, female.mp. [mp=title, abstract, descriptors]
(9)
21 genital disease*.mp. [mp=title, abstract, descriptors] (12)
22 or/20‐21 (12)
23 19 not 22 (796)
24 18 or 23 (4759)
25 neck.mp. [mp=title, abstract, descriptors] (8069)
26 neck muscles.mp. [mp=title, abstract, descriptors] (260)
27 cervical plexus.mp. [mp=title, abstract, descriptors] (15)
28 cervical vertebrae.mp. [mp=title, abstract, descriptors] (3569)
29 atlanto‐axial joint.mp. [mp=title, abstract, descriptors] (217)
30 atlanto‐occipital joint.mp. [mp=title, abstract, descriptors]
(132)
31 cervical atlas.mp. [mp=title, abstract, descriptors] (2)
32 spinal nerve roots.mp. [mp=title, abstract, descriptors] (754)
33 brachial plexus.mp. [mp=title, abstract, descriptors] (744)
34 (odontoid* or cervical or occip* or atlant*).tw. (11621)
35 (axis or odontoid process).mp. [mp=title, abstract, descriptors]
(3007)
36 thoracic vertebrae.mp. [mp=title, abstract, descriptors] (920)
37 cervical vertebrae.mp. [mp=title, abstract, descriptors] (3569)
38 cervical plexus.mp. [mp=title, abstract, descriptors] (15)
39 cervical spine.mp. [mp=title, abstract, descriptors] (4032)
40 (neck adj3 muscles).mp. [mp=title, abstract, descriptors] (590)
41 (brachial adj3 plexus).mp. [mp=title, abstract, descriptors]
(749)
42 (thoracic adj3 vertebrae).mp. [mp=title, abstract, descriptors]
(974)
43 (thoracic adj3 spine).mp. [mp=title, abstract, descriptors]
(1422)
44 (thoracic adj3 outlet).mp. [mp=title, abstract, descriptors]
(266)
45 trapezius.mp. [mp=title, abstract, descriptors] (696)
46 cervical.mp. [mp=title, abstract, descriptors] (11164)
47 cervico*.mp. [mp=title, abstract, descriptors] (915)
48 46 or 47 (11552)
49 genital diseases, female.mp. [mp=title, abstract, descriptors]
(9)
50 genital disease*.mp. [mp=title, abstract, descriptors] (12)
51 uterus.mp. [mp=title, abstract, descriptors] (484)
52 49 or 50 or 51 (495)
53 48 not 52 (11533)
54 25 or 26 or 27 or 28 or 29 or 30 or 31 or 32 or 33 or 34 or 35 or
36
or 37 or 38 or 39 or 40 or 41 or 42 or 43 or 44 or 45 or 53 (23259)
55 pain.mp. [mp=title, abstract, descriptors] (52530)
56 injuries.mp. [mp=title, abstract, descriptors] (29006)
57 ache.mp. [mp=title, abstract, descriptors] (303)
58 sore.mp. [mp=title, abstract, descriptors] (239)
59 stiff.mp. [mp=title, abstract, descriptors] (480)
60 discomfort.mp. [mp=title, abstract, descriptors] (1911)
61 injur*.mp. [mp=title, abstract, descriptors] (39409)
62 neuropath*.mp. [mp=title, abstract, descriptors] (5362)
63 or/55‐62 (88035)
64 54 and 63 (10588)
65 radiculopathy.mp. [mp=title, abstract, descriptors] (1323)
66 (temporomandibular joint disorders or temporomandibular joint
dysfunction syndrome).mp. [mp=title, abstract, descriptors] (409)
67 myofascial pain syndromes.mp. [mp=title, abstract, descriptors]
(692)
68 "sprains and strains".mp. [mp=title, abstract, descriptors]
(3593)
69 spinal osteophytosis.mp. [mp=title, abstract, descriptors] (492)
70 neuritis.mp. [mp=title, abstract, descriptors] (273)
71 polyradiculopathy.mp. [mp=title, abstract, descriptors] (76)
72 arthritis.mp. [mp=title, abstract, descriptors] (8230)
73 fibromyalgia.mp. [mp=title, abstract, descriptors] (1439)
74 (spondylitis or discitis).mp. [mp=title, abstract, descriptors]
(1048)
75 (spondylosis or spondylolysis or spondylolisthesis).mp.
[mp=title,
abstract, descriptors] (1674)
76 radiculitis.mp. [mp=title, abstract, descriptors] (246)
77 tempomandibular.mp. [mp=title, abstract, descriptors] (2)
78 myofascial pain syndrome*.mp. [mp=title, abstract, descriptors]
(755)
79 thoracic outlet syndrome*.mp. [mp=title, abstract, descriptors]
(247)
80 spinal osteophytosis.mp. [mp=title, abstract, descriptors] (492)
81 neuritis.mp. [mp=title, abstract, descriptors] (273)
82 spondylosis.mp. [mp=title, abstract, descriptors] (472)
83 spondylitis.mp. [mp=title, abstract, descriptors] (881)
84 spondylolisthesis.mp. [mp=title, abstract, descriptors] (1068)
85 or/65‐84 (18580)
86 54 and 85 (2910)
87 neck.mp. [mp=title, abstract, descriptors] (8069)
88 cervical vertebrae.mp. [mp=title, abstract, descriptors] (3569)
89 thoracic vertebrae.mp. [mp=title, abstract, descriptors] (920)
90 (thoracic adj3 vertebrae).mp. [mp=title, abstract, descriptors]
(974)
91 cervical.mp. [mp=title, abstract, descriptors] (11164)
92 cervico*.mp. [mp=title, abstract, descriptors] (915)
93 91 or 92 (11552)
94 genital diseases, female.mp. [mp=title, abstract, descriptors]
(9)
95 genital disease*.mp. [mp=title, abstract, descriptors] (12)
96 uterus.mp. [mp=title, abstract, descriptors] (484)
97 or/94‐96 (495)
98 93 not 97 (11533)
99 (thoracic adj3 spine).mp. [mp=title, abstract, descriptors]
(1422)
100 cervical spine.mp. [mp=title, abstract, descriptors] (4032)
101 87 or 88 or 89 or 90 or 98 or 99 or 100 (18115)
102 intervertebral disk.mp. [mp=title, abstract, descriptors] (2894)
103 (disc or discs).mp. [mp=title, abstract, descriptors] (6484)
104 (disk or disks).mp. [mp=title, abstract, descriptors] (3754)
105 102 or 103 or 104 (8015)
106 101 and 105 (1423)
107 herniat*.mp. [mp=title, abstract, descriptors] (2358)
108 slipped.mp. [mp=title, abstract, descriptors] (205)
109 prolapse*.mp. [mp=title, abstract, descriptors] (434)
110 displace*.mp. [mp=title, abstract, descriptors] (6285)
111 degenerat*.mp. [mp=title, abstract, descriptors] (6917)
112 (bulge or bulged or bulging).mp. [mp=title, abstract,
descriptors]
(323)
113 107 or 108 or 109 or 110 or 111 or 112 (14641)
114 106 and 113 (881)
115 intervertebral disk displacement.mp. [mp=title, abstract,
descriptors] (1455)
116 intervertebral disc displacement.mp. [mp=title, abstract,
descriptors] (9)
117 intervertebral disk degeneration.mp. [mp=title, abstract,
descriptors] (12)
118 intervertebral disc degeneration.mp. [mp=title, abstract,
descriptors] (179)
119 115 or 116 or 117 or 118 (1632)
120 101 and 119 (279)
121 24 or 64 or 86 or 106 or 114 or 120 (13027)
122 (animals not (animals and humans)).mp. [mp=title, abstract,
descriptors] (8422)
123 121 not 122 (12814)
124 neoplasms.mp. [mp=title, abstract, descriptors] (12262)
125 wounds, penetrating.mp. [mp=title, abstract, descriptors] (12)
126 124 or 125 (12274)
127 123 not 126 (12532)
128 rehabilitation.mp. [mp=title, abstract, descriptors] (14485)
129 therapy.mp. [mp=title, abstract, descriptors] (44097)
130 128 or 129 (55359)
131 (neck pain or brachial plexus neuropathies or neck injuries or
whiplash or thoracic outlet syndrome or cervical rib syndrome or torticollis or brachial plexus neuritis).mp. [mp=title, abstract, descriptors]
(4034)
132 (temporomandibular joint disorder or temporomandibular joint
dysfunction syndrome).mp. [mp=title, abstract, descriptors] (181)
133 (myofascial pain syndromes or "sprains and strains").mp.
[mp=title,
abstract, descriptors] (4274)
134 (radiculopathy or osteophytosis or neuritis or polyradiculopathy
or
arthritis or fibromyalgia or spondylitis or spondylosis or spondylolysis or spondylolisthesis).mp. [mp=title, abstract, descriptors] (13607)
135 131 or 132 or 133 or 134 (21290)
136 130 and 135 (4916)
137 54 and 136 (1655)
138 (acupuncture or chiropractic).mp. [mp=title, abstract,
descriptors]
(29544)
139 musculoskeletal manipulation*.mp. [mp=title, abstract,
descriptors]
(179)
140 massage.mp. [mp=title, abstract, descriptors] (1649)
141 mobili?ation.mp. [mp=title, abstract, descriptors] (1966)
142 acupuncture therapy.mp. [mp=title, abstract, descriptors] (936)
143 (acupuncture or acu‐puncture or needling or acupressure or
mox?bustion).mp. [mp=title, abstract, descriptors] (8413)
144 ((neck or spine or spinal or cervical or chiropractic* or
musculoskeletal*) adj3 (adjust* or manipulat* or mobiliz* or mobilis*)).mp.
[mp=title, abstract, descriptors] (6218)
145 (manual adj therap*).mp. [mp=title, abstract, descriptors] (824)
146 (manipulati* adj (therap* or medicine)).mp. [mp=title, abstract,
descriptors] (998)
147 (massag* or reflexolog* or rolfing or zone therap*).mp.
[mp=title,
abstract, descriptors] (1720)
148 Nimmo.mp. [mp=title, abstract, descriptors] (14)
149 vibration therapy.mp. [mp=title, abstract, descriptors] (11)
150 (vibration adj5 (therap* or treatment*)).mp. [mp=title,
abstract,
descriptors] (61)
151 (ChihYa or Shiatsu or Shiatzu or ZhiYa).mp. [mp=title, abstract,
descriptors] (65)
152 (flexion adj2 distraction*).mp. [mp=title, abstract,
descriptors]
(157)
153 (myofascial adj3 (release or therap*)).mp. [mp=title, abstract,
descriptors] (221)
154 muscle energy technique*.mp. [mp=title, abstract, descriptors]
(59)
155 trigger point.mp. [mp=title, abstract, descriptors] (359)
156 proprioceptive neuromuscular facilitation*.mp. [mp=title,
abstract,
descriptors] (94)
157 cyriax friction.mp. [mp=title, abstract, descriptors] (0)
158 (lomilomi or lomi‐lomi or trager).mp. [mp=title, abstract,
descriptors] (13)
159 aston patterning.mp. [mp=title, abstract, descriptors] (1)
160 (strain adj counterstrain).mp. [mp=title, abstract, descriptors]
(22)
161 (craniosacraltherap* or cranio‐sacral therap* or craniosacral
therap*).mp. [mp=title, abstract, descriptors] (45)
162 (amma or ammo or effleuurage or effleurage or petrissage or
hacking
or tapotment).mp. [mp=title, abstract, descriptors] (30)
163 complementary therapies.mp. [mp=title, abstract, descriptors]
(4070)
164 ((complement* or alternat* or osteopathic*) adj (therap* or
medicine)).mp. [mp=title, abstract, descriptors] (13440)
165 (Tui Na or Tuina).mp. [mp=title, abstract, descriptors] (56)
166 or/138‐165 (45999)
167 127 and 166 (3028)
168 136 or 137 or 167 (6966)
169 (animals not (animals and humans)).mp. [mp=title, abstract,
descriptors] (8422)
170 168 not 169 (6925)
171 randomized controlled trial*.mp. [mp=title, abstract,
descriptors]
(4411)
172 controlled clinical trial*.mp. [mp=title, abstract, descriptors]
(1187)
173 (random* or sham or placebo*).mp. [mp=title, abstract,
descriptors]
(31492)
174 placebos.mp. [mp=title, abstract, descriptors] (447)
175 random allocation.mp. [mp=title, abstract, descriptors] (103)
176 single blind method.mp. [mp=title, abstract, descriptors] (30)
177 double blind method.mp. [mp=title, abstract, descriptors] (339)
178 ((singl* or doubl* or trebl* or tripl*) adj25 (blind* or dumm*
or
mask*)).mp. [mp=title, abstract, descriptors] (5989)
179 (rct or rcts).mp. [mp=title, abstract, descriptors] (844)
180 (control* adj2 (study or studies or trial*)).mp. [mp=title,
abstract, descriptors] (14625)
181 or/171‐180 (37245)
182 170 and 181 (1292)
183 (guideline* or practice guideline*).mp. [mp=title, abstract,
descriptors] (7859)
184 (guideline* or guidance* or recommendation*).ti. (2163)
185 consensus.ti. (308)
186 183 or 184 or 185 (8394)
187 170 and 186 (196)
188 meta‐analysis.mp. [mp=title, abstract, descriptors] (1159)
189 (metaanaly* or meta analy* or met analy* or metanaly*).mp.
[mp=title, abstract, descriptors] (1479)
190 (collaborative research or collaborative review* or
collaborative
overview*).mp. [mp=title, abstract, descriptors] (61)
191 (integrative research or integrative review* or integrative
overview*).mp. [mp=title, abstract, descriptors] (42)
192 (quantitative adj3 (research or review* or overview*)).mp.
[mp=title, abstract, descriptors] (280)
193 (research integration or research overview*).mp. [mp=title,
abstract, descriptors] (18)
194 (systematic* adj3 (review* or overview*)).mp. [mp=title,
abstract,
descriptors] (2712)
195 (methodologic* adj3 (review* or overview*)).mp. [mp=title,
abstract,
descriptors] (234)
196 technology assessment biomedical.mp. [mp=title, abstract,
descriptors] (33)
197 (hta or thas or technology assessment*).mp. [mp=title, abstract,
descriptors] (212)
198 ((hand adj2 search*) or (manual* adj search*)).mp. [mp=title,
abstract, descriptors] (312)
199 ((electronic adj database*) or (bibliographic* adj
database*)).mp.
[mp=title, abstract, descriptors] (450)
200 ((data adj2 abstract*) or (data adj2 extract*)).mp. [mp=title,
abstract, descriptors] (1077)
201 (analys* adj3 (pool or pooled or pooling)).mp. [mp=title,
abstract,
descriptors] (199)
202 mantel haenszel.mp. [mp=title, abstract, descriptors] (62)
203 (cochrane or pubmed or pub med or medline or embase or psycinfo
or
psyclit or psychinfo or psychlit or cinahl or science citation index).ab.
(2730)
204 or/188‐203 (6435)
205 170 and 204 (273)
206 182 or 187 or 205 (1529)
207 limit 206 to yr="2009 ‐Current" (190)
Appendix 2. Criteria for 'Risk of Bias' Assessment
Random sequence generation (selection bias)
Selection bias (biased allocation to interventions) due to inadequate generation of a randomized sequence
There is a low risk of selection bias if the investigators describe a random component in the sequence generation process such as: referring to a random number table, using a computer random number generator, coin tossing, shuffling cards or envelopes, throwing dice, drawing of lots, minimization (minimization may be implemented without a random element, and this is considered to be equivalent to being random).
There is a high risk of selection bias if the investigators describe a non‐random component in the sequence generation process, such as: sequence generated by odd or even date of birth, date (or day) of admission, hospital or clinic record number; or allocation by judgement of the clinician, preference of the participant, results of a laboratory test or a series of tests, or availability of the intervention.
Allocation concealment (selection bias)
Selection bias (biased allocation to interventions) due to inadequate concealment of allocations prior to assignment
There is a low risk of selection bias if the participants and investigators enrolling participants could not foresee assignment because one of the following, or an equivalent method, was used to conceal allocation: central allocation (including telephone, web‐based and pharmacy‐controlled randomization); sequentially numbered drug containers of identical appearance; or sequentially numbered, opaque, sealed envelopes.
There is a high risk of bias if participants or investigators enrolling participants could possibly foresee assignments and thus introduce selection bias, such as allocation based on: using an open random allocation schedule (e.g. a list of random numbers); assignment envelopes were used without appropriate safeguards (e.g. if envelopes were unsealed or non‐opaque or not sequentially numbered); alternation or rotation; date of birth; case record number; or other explicitly unconcealed procedures.
Blinding of participants
Performance bias due to knowledge of the allocated interventions by participants during the study
There is a low risk of performance bias if blinding of participants was ensured and it was unlikely that the blinding could have been broken; or if there was no blinding or incomplete blinding, but the review authors judge that the outcome is not likely to be influenced by lack of blinding.
Blinding of personnel/ care providers (performance bias)
Performance bias due to knowledge of the allocated interventions by personnel/care providers during the study
There is a low risk of performance bias if blinding of personnel was ensured and it was unlikely that the blinding could have been broken; or if there was no blinding or incomplete blinding, but the review authors judge that the outcome is not likely to be influenced by lack of blinding.
Blinding of outcome assessor (detection bias)
Detection bias due to knowledge of the allocated interventions by outcome assessors
There is low risk of detection bias if the blinding of the outcome assessment was ensured and it was unlikely that the blinding could have been broken; or if there was no blinding or incomplete blinding, but the review authors judge that the outcome is not likely to be influenced by lack of blinding, or:
for patient‐reported outcomes in which the patient was the outcome assessor (e.g. pain, disability): there is a low risk of bias for outcome assessors if there is a low risk of bias for participant blinding (Boutron 2005)
for outcome criteria that are clinical or therapeutic events that will be determined by the interaction between patients and care providers (e.g. co‐interventions, length of hospitalization, treatment failure), in which the care provider is the outcome assessor: there is a low risk of bias for outcome assessors if there is a low risk of bias for care providers (Boutron 2005)
for outcome criteria that are assessed from data from medical forms: there is a low risk of bias if the treatment or adverse effects of the treatment could not be noticed in the extracted data (Boutron 2005)
Incomplete outcome data (attrition bias)
Attrition bias due to amount, nature or handling of incomplete outcome data
There is a low risk of attrition bias if there were no missing outcome data; reasons for missing outcome data were unlikely to be related to the true outcome (for survival data, censoring unlikely to be introducing bias); missing outcome data were balanced in numbers, with similar reasons for missing data across groups; for dichotomous outcome data, the proportion of missing outcomes compared with the observed event risk was not enough to have a clinically relevant impact on the intervention effect estimate; for continuous outcome data, the plausible effect size (difference in means or standardized difference in means) among missing outcomes was not enough to have a clinically relevant impact on observed effect size, or missing data were imputed using appropriate methods (if drop‐outs are very large, imputation using even "acceptable" methods may still suggest a high risk of bias) (Van Tulder 2003). The percentage of withdrawals and drop‐outs should not exceed 20% for short‐term follow‐up and 30% for long‐term follow‐up and should not lead to substantial bias (these percentages are commonly used but arbitrary, not supported by literature) (Van Tulder 2003.
Selective Reporting (reporting bias)
Reporting bias due to selective outcome reporting
There is low risk of reporting bias if the study protocol is available and all of the study's pre‐specified (primary and secondary) outcomes that are of interest in the review have been reported in the pre‐specified way, or if the study protocol is not available but it is clear that the published reports include all expected outcomes, including those that were pre‐specified (convincing text of this nature may be uncommon).
There is a high risk of reporting bias if not all of the study's pre‐specified primary outcomes have been reported; one or more primary outcomes is reported using measurements, analysis methods or subsets of the data (e.g. subscales) that were not pre‐specified; one or more reported primary outcomes were not pre‐specified (unless clear justification for their reporting is provided, such as an unexpected adverse effect); one or more outcomes of interest in the review are reported incompletely so that they cannot be entered in a meta‐analysis; the study report fails to include results for a key outcome that would be expected to have been reported for such a study.
Group similarity at baseline (selection bias)
Bias due to dissimilarity at baseline for the most important prognostic indicators
There is low risk of bias if groups are similar at baseline for demographic factors, value of main outcome measure(s), and important prognostic factors (examples in the field of back and neck pain are duration and severity of complaints, vocational status, percentage of patients with neurological symptoms) (Van Tulder 2003).
Co‐interventions (performance bias)
Bias because co‐interventions were different across groups
There is low risk of bias if there were no co‐interventions or they were similar between the index and control groups (Van Tulder 2003).
Compliance (performance bias)
Bias due to inappropriate compliance with interventions across groups
There is low risk of bias if compliance with the interventions was acceptable, based on the reported intensity/dosage, duration, number and frequency for both the index and control intervention(s). For single‐session interventions (e.g. surgery), this item is irrelevant (Van Tulder 2003).
Intention‐to‐treat‐analysis
There is low risk of bias if all randomized patients were reported/analyzed in the group to which they were allocated by randomization.
Timing of outcome assessments (detection bias)
Bias because important outcomes were not measured at the same time across groups
There is low risk of bias if all important outcome assessments for all intervention groups were measured at the same time (Van Tulder 2003).
Other bias
Bias due to problems not covered elsewhere in the table
There is a low risk of bias if the study appears to be free of other sources of bias not addressed elsewhere (e.g. study funding).
Data and analyses
Comparison 1. Chronic MND: Breathing Patterns vs CONTROL.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain Intensity (Borg 0 to 10): 10 weeks of treatment vs Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Practice paced breathing vs Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Function (NDI 0 to 100): 10 weeks of treatment vs Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Practice paced breathing vs Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 SF‐36 (physical function): 10 weeks of treatment vs Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected |
1.1. Analysis.
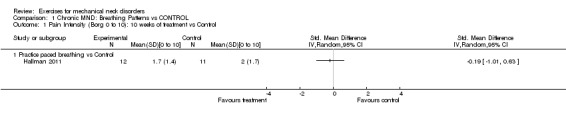
Comparison 1 Chronic MND: Breathing Patterns vs CONTROL, Outcome 1 Pain Intensity (Borg 0 to 10): 10 weeks of treatment vs Control.
1.2. Analysis.
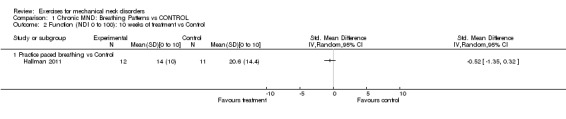
Comparison 1 Chronic MND: Breathing Patterns vs CONTROL, Outcome 2 Function (NDI 0 to 100): 10 weeks of treatment vs Control.
1.3. Analysis.
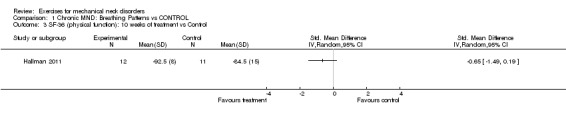
Comparison 1 Chronic MND: Breathing Patterns vs CONTROL, Outcome 3 SF‐36 (physical function): 10 weeks of treatment vs Control.
Comparison 2. Acute to Chronic MND: General Fitness Training vs CONTROL.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain Intensity (VAS): 10 weeks of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 General Fitness Training v Reference Intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Pain Intensity (VAS): 10 weeks of treatment + 10 weeks follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 General Fitness Training v Reference Intervention | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
2.1. Analysis.
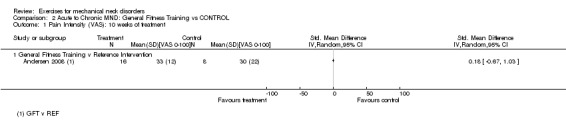
Comparison 2 Acute to Chronic MND: General Fitness Training vs CONTROL, Outcome 1 Pain Intensity (VAS): 10 weeks of treatment.
2.2. Analysis.
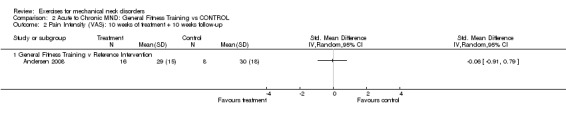
Comparison 2 Acute to Chronic MND: General Fitness Training vs CONTROL, Outcome 2 Pain Intensity (VAS): 10 weeks of treatment + 10 weeks follow‐up.
Comparison 3. Chronic MND: Cervical Stretch/ROM Exercises + ANOTHER INTERVENTION vs THAT SAME INTERVENTION.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain Intensity (NRS‐101): 4 weeks of treatment | Other data | No numeric data | ||
| 1.1 Stretch before Manip v Manip alone | Other data | No numeric data | ||
| 1.2 Stretch after Manip v Manip alone | Other data | No numeric data | ||
| 2 Function (NDI): 4 weeks of treatment | Other data | No numeric data | ||
| 2.1 Stretch before Manip v Manip alone | Other data | No numeric data | ||
| 2.2 Stretch after Manip v Manip alone | Other data | No numeric data |
3.1. Analysis.
Comparison 3 Chronic MND: Cervical Stretch/ROM Exercises + ANOTHER INTERVENTION vs THAT SAME INTERVENTION, Outcome 1 Pain Intensity (NRS‐101): 4 weeks of treatment.
| Pain Intensity (NRS‐101): 4 weeks of treatment | |
|---|---|
| Study | |
| Stretch before Manip v Manip alone | |
| Allan 2003 | Although the stretch before manipulation group had 30% (n = 2) greater decrease in intra‐group pain by the end of the study than those who received maniplation alone, inter‐group analysis using the Kruskal‐Wallis test found no statistical signifance between the groups (X2 = 2.447, d.f. = 2, P = 0.294) There was no statistically significant difference in pain between the stretch before manipulation group and the control group of manipulation alone There was no statistically significant difference between the stretch before manipulation vs stretch after manipulation |
| Stretch after Manip v Manip alone | |
| Allan 2003 | Although the manipulation then stretch group had 26% (n = 2) greater decrease in intra‐group pain by the end of the study than those who received maniplation alone, inter‐group analysis using the Kruskal‐Wallis test found no statistical signifance between the groups (X2 = 2.447, d.f. = 2, P = 0.294). There was no statistically significant difference in pain between the stretch after manipulation group from the control group of manipulation alone There was no statistically significant difference between the stretch before manipulation vs stretch after manipulation |
3.2. Analysis.
Comparison 3 Chronic MND: Cervical Stretch/ROM Exercises + ANOTHER INTERVENTION vs THAT SAME INTERVENTION, Outcome 2 Function (NDI): 4 weeks of treatment.
| Function (NDI): 4 weeks of treatment | |
|---|---|
| Study | |
| Stretch before Manip v Manip alone | |
| Allan 2003 | There was no statistically significant difference in function between the stretch before manipulation and the control group of manipulation alone There was no statistically significant difference in function between stretch before manipulation vs stretch after manipulation |
| Stretch after Manip v Manip alone | |
| Allan 2003 | no statistically significant difference in function between stretch after manipulation groups from control group of manipulation alone no statistically significant difference in function between stretch before manipulation vs stretch after manipulation |
Comparison 4. Chronic MND: Cervical Stretch/ROM Exercises + Dynamic Cervical Stabilization vs SHAM.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain Intensity (VAS): 8 weeks of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 McKenzie Treatment v Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Pain Intensity (VAS): 8 weeks of treatment + 6 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 McKenzie Treatment v Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Pain Intensity (VAS): 8 weeks of treatment + 12 months follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 McKenzie Treatment v Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Function (NDI): 8 weeks of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 McKenzie Treatment v Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Function (NDI): 8 weeks of treatment + 6 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 McKenzie Treatment v Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Function (NDI): 8 weeks of treatment + 12 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 McKenzie Treatment v Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
4.1. Analysis.
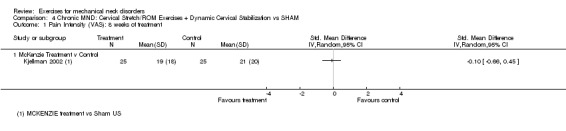
Comparison 4 Chronic MND: Cervical Stretch/ROM Exercises + Dynamic Cervical Stabilization vs SHAM, Outcome 1 Pain Intensity (VAS): 8 weeks of treatment.
4.2. Analysis.
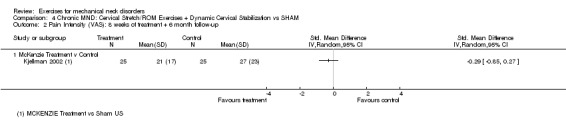
Comparison 4 Chronic MND: Cervical Stretch/ROM Exercises + Dynamic Cervical Stabilization vs SHAM, Outcome 2 Pain Intensity (VAS): 8 weeks of treatment + 6 month follow‐up.
4.3. Analysis.
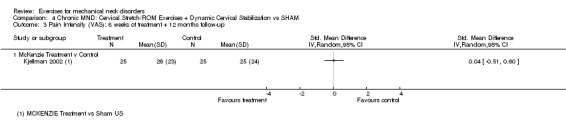
Comparison 4 Chronic MND: Cervical Stretch/ROM Exercises + Dynamic Cervical Stabilization vs SHAM, Outcome 3 Pain Intensity (VAS): 8 weeks of treatment + 12 months follow‐up.
4.4. Analysis.
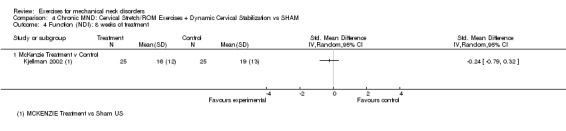
Comparison 4 Chronic MND: Cervical Stretch/ROM Exercises + Dynamic Cervical Stabilization vs SHAM, Outcome 4 Function (NDI): 8 weeks of treatment.
4.5. Analysis.
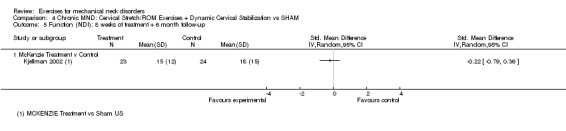
Comparison 4 Chronic MND: Cervical Stretch/ROM Exercises + Dynamic Cervical Stabilization vs SHAM, Outcome 5 Function (NDI): 8 weeks of treatment + 6 month follow‐up.
4.6. Analysis.
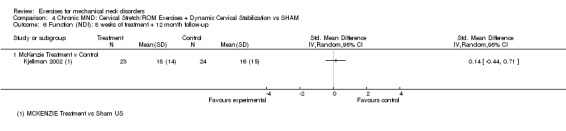
Comparison 4 Chronic MND: Cervical Stretch/ROM Exercises + Dynamic Cervical Stabilization vs SHAM, Outcome 6 Function (NDI): 8 weeks of treatment + 12 month follow‐up.
Comparison 5. Chronic MND: Static Cervical Strengthening + Static Stabilization vs NO INTERVENTION OR WAIT LIST.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain Intensity (VAS): 6 weeks of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Isometric neck exercises +/‐ pillow vs control or pillow | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Pain Intensity (VAS): 6 weeks of treatment + 6 weeks follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Isometric neck exercises +/‐ pillow vs pillow or placebo | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Function (NPQ): 6 weeks of treatment | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Isometric neck exercises +/‐ pillow vs pillow or placebo | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Function (NPQ): 6 weeks of treatment + 6 weeks follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Isometric neck exercises +/‐ pillow vs pillow or placebo | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Global Perceived Effect Treatment (patients assessment): 3 weeks of treatment | 0 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.1 Isometric exercises vs no intervention | 0 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Quality of Life (SF‐36): 6 weeks of treatment + 6 w follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Isometric neck exercises +/‐ pillow vs pillow or placebo | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
5.1. Analysis.
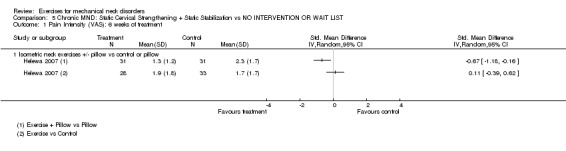
Comparison 5 Chronic MND: Static Cervical Strengthening + Static Stabilization vs NO INTERVENTION OR WAIT LIST, Outcome 1 Pain Intensity (VAS): 6 weeks of treatment.
5.2. Analysis.
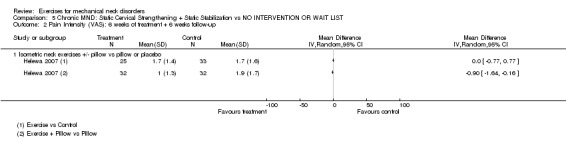
Comparison 5 Chronic MND: Static Cervical Strengthening + Static Stabilization vs NO INTERVENTION OR WAIT LIST, Outcome 2 Pain Intensity (VAS): 6 weeks of treatment + 6 weeks follow‐up.
5.3. Analysis.
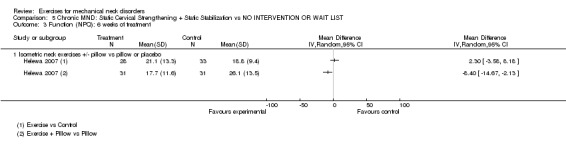
Comparison 5 Chronic MND: Static Cervical Strengthening + Static Stabilization vs NO INTERVENTION OR WAIT LIST, Outcome 3 Function (NPQ): 6 weeks of treatment.
5.4. Analysis.
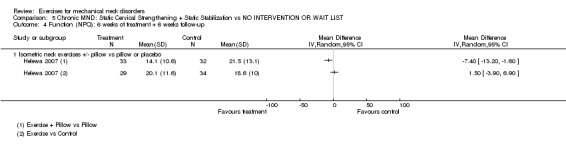
Comparison 5 Chronic MND: Static Cervical Strengthening + Static Stabilization vs NO INTERVENTION OR WAIT LIST, Outcome 4 Function (NPQ): 6 weeks of treatment + 6 weeks follow‐up.
5.6. Analysis.
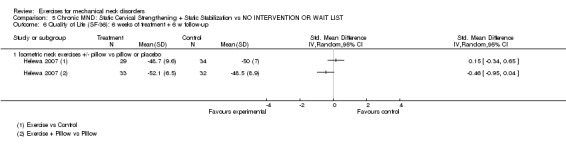
Comparison 5 Chronic MND: Static Cervical Strengthening + Static Stabilization vs NO INTERVENTION OR WAIT LIST, Outcome 6 Quality of Life (SF‐36): 6 weeks of treatment + 6 w follow‐up.
Comparison 6. Chronic MND: Pattern synchronization (sitting posture) vs CONTROL.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain intensity (VAS) 2 weeks of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Postural Exercise vs Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Function (NDI): 2 weeks of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Postural Exercise vs Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
6.1. Analysis.
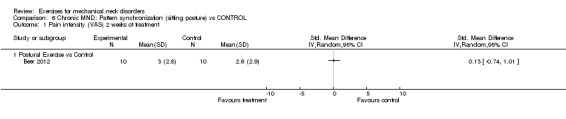
Comparison 6 Chronic MND: Pattern synchronization (sitting posture) vs CONTROL, Outcome 1 Pain intensity (VAS) 2 weeks of treatment.
6.2. Analysis.
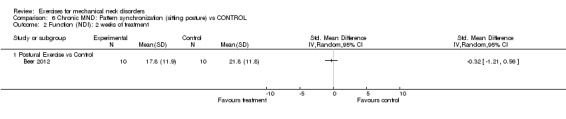
Comparison 6 Chronic MND: Pattern synchronization (sitting posture) vs CONTROL, Outcome 2 Function (NDI): 2 weeks of treatment.
Comparison 7. Acute to Chronic MND: Scapulothoracic + UE Strengthening vs CONTROL.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain Intensity (NPS): 4 weeks of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Muscle strength training vs CONTROL | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Pain Intensity: 10 to 20 weeks of treatment | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Strength Specific Training vs Reference Group | 3 | 157 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.71 [‐1.33, ‐0.10] |
| 3 Pain Intensity: 20 weeks of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Strength Specific Training vs Reference Group | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Pain Intensity (VAS): 10 weeks of treatment + 10 weeks follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Strength Specific Training vs Reference Group | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Function: 4 weeks of treatment | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Intensive muscular strength training vs CONTROL | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Function: 20 weeks of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Specific strength training vs Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Function: 12 to 20 weeks of treatment/follow‐up | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Muscle strength training vs CONTROL | 2 | 128 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.63, 0.07] |
7.1. Analysis.
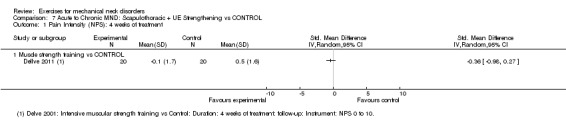
Comparison 7 Acute to Chronic MND: Scapulothoracic + UE Strengthening vs CONTROL, Outcome 1 Pain Intensity (NPS): 4 weeks of treatment.
7.2. Analysis.
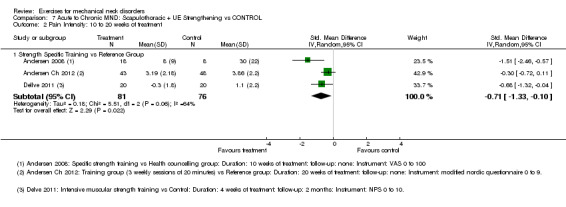
Comparison 7 Acute to Chronic MND: Scapulothoracic + UE Strengthening vs CONTROL, Outcome 2 Pain Intensity: 10 to 20 weeks of treatment.
7.3. Analysis.
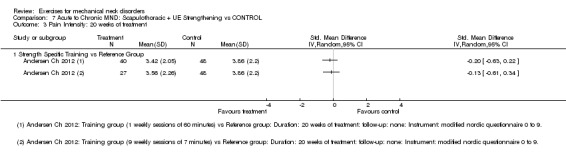
Comparison 7 Acute to Chronic MND: Scapulothoracic + UE Strengthening vs CONTROL, Outcome 3 Pain Intensity: 20 weeks of treatment.
7.4. Analysis.
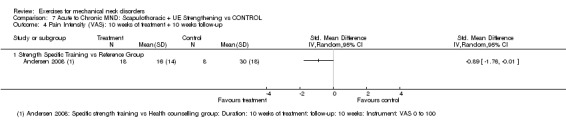
Comparison 7 Acute to Chronic MND: Scapulothoracic + UE Strengthening vs CONTROL, Outcome 4 Pain Intensity (VAS): 10 weeks of treatment + 10 weeks follow‐up.
7.5. Analysis.
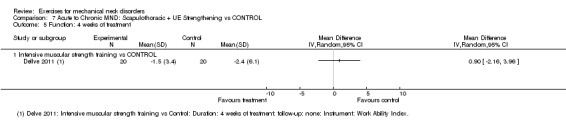
Comparison 7 Acute to Chronic MND: Scapulothoracic + UE Strengthening vs CONTROL, Outcome 5 Function: 4 weeks of treatment.
7.6. Analysis.
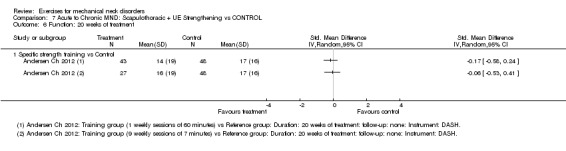
Comparison 7 Acute to Chronic MND: Scapulothoracic + UE Strengthening vs CONTROL, Outcome 6 Function: 20 weeks of treatment.
7.7. Analysis.
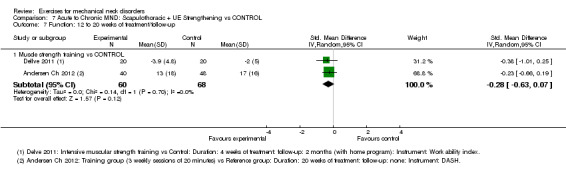
Comparison 7 Acute to Chronic MND: Scapulothoracic + UE Strengthening vs CONTROL, Outcome 7 Function: 12 to 20 weeks of treatment/follow‐up.
Comparison 8. Chronic MND: Cervical/UE Stretch/ROM Exercise + Cervical/UE Strengthening + Dynamic Cervical Stabilization vs PLACEBO or SHAM.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain Intensity (VAS): 8 weeks of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 General Exercise vs Sham US | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Pain Intensity (VAS): 8 weeks of treatment + 6 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 General Exercise vs Sham US | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Pain Intensity (VAS): 8 weeks of treatment + 12 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 General Exercise vs Sham US | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Function (NDI): 8 weeks of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 General Exercise vs Sham US | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Function (NDI): 8 weeks of treatment + 6 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 General Exercise vs Sham US | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Function (NDI): 8 weeks treatment + 12 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 General Exercise vs Sham US | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
8.1. Analysis.
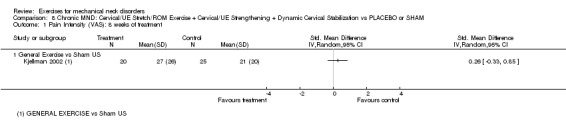
Comparison 8 Chronic MND: Cervical/UE Stretch/ROM Exercise + Cervical/UE Strengthening + Dynamic Cervical Stabilization vs PLACEBO or SHAM, Outcome 1 Pain Intensity (VAS): 8 weeks of treatment.
8.2. Analysis.
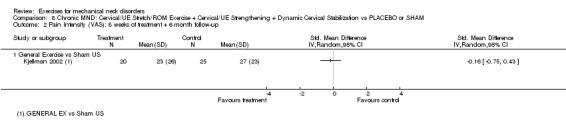
Comparison 8 Chronic MND: Cervical/UE Stretch/ROM Exercise + Cervical/UE Strengthening + Dynamic Cervical Stabilization vs PLACEBO or SHAM, Outcome 2 Pain Intensity (VAS): 8 weeks of treatment + 6 month follow‐up.
8.3. Analysis.
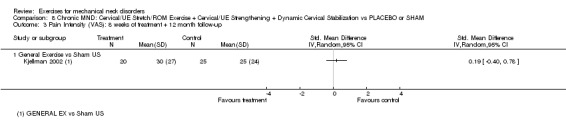
Comparison 8 Chronic MND: Cervical/UE Stretch/ROM Exercise + Cervical/UE Strengthening + Dynamic Cervical Stabilization vs PLACEBO or SHAM, Outcome 3 Pain Intensity (VAS): 8 weeks of treatment + 12 month follow‐up.
8.4. Analysis.
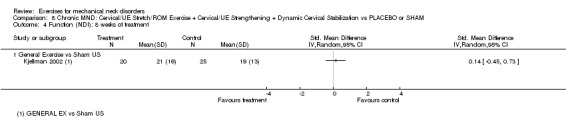
Comparison 8 Chronic MND: Cervical/UE Stretch/ROM Exercise + Cervical/UE Strengthening + Dynamic Cervical Stabilization vs PLACEBO or SHAM, Outcome 4 Function (NDI): 8 weeks of treatment.
8.5. Analysis.
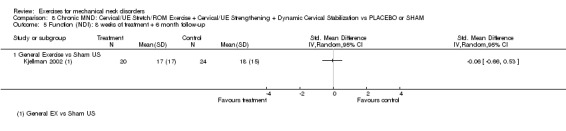
Comparison 8 Chronic MND: Cervical/UE Stretch/ROM Exercise + Cervical/UE Strengthening + Dynamic Cervical Stabilization vs PLACEBO or SHAM, Outcome 5 Function (NDI): 8 weeks of treatment + 6 month follow‐up.
8.6. Analysis.
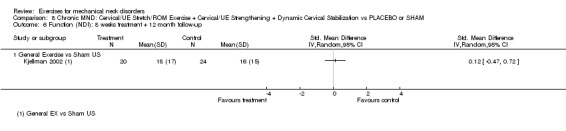
Comparison 8 Chronic MND: Cervical/UE Stretch/ROM Exercise + Cervical/UE Strengthening + Dynamic Cervical Stabilization vs PLACEBO or SHAM, Outcome 6 Function (NDI): 8 weeks treatment + 12 month follow‐up.
Comparison 9. Chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION vs THAT SAME INTERVENTION.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain Intensity: Immediate Post Treatment (<11w of treatment) | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Exercise +/‐ Infrared +/‐ SMT +/‐ Acupuncture vs Infrared or SMT or Acupuncture | 4 | 317 | Mean Difference (IV, Random, 95% CI) | ‐0.66 [‐1.28, ‐0.03] |
| 2 Pain Intensity: 11 w of treatment + 3 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 SMT + Rehab Exercises vs SMT | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Pain Intensity: Treatment + IT follow‐up (11 weeks of treatment + 6 month follow‐up | 3 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 <11w of treatment + 6 month follow‐up | 3 | 241 | Mean Difference (IV, Random, 95% CI) | ‐0.67 [‐1.32, ‐0.02] |
| 4 Pain Intensity: Treatment + LT follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 <11w of treatment + 24 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Function: Immediate Post treatment | 4 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 5.1 <11w of treatment | 4 | 317 | Mean Difference (IV, Random, 95% CI) | ‐1.91 [‐4.65, 0.83] |
| 6 Function: Treatment + ST follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 <11w of treatment + 3 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Function: Treatment + IT follow‐up | 3 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 <11w of treatment + 6 month follow‐up | 3 | 241 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.45 [‐0.72, ‐0.18] |
| 8 Function: Treatment + LT follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.1 <11w of treatment + 24 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 9 Quality of Life: Immediate Post Treatment | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 9.1 <11w of treatment | 2 | 165 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.18 [‐0.48, 0.13] |
| 10 Quality of Life: Treatment + ST follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 10.1 11w of treatment + 3 month follow‐up | 1 | Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 11 Quality of Life: Treatment + IT follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 11.1 11w of treatment + 6 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 12 Quality of Life: Treatment + LT follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 12.1 11w of treatment + 24 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 13 Patient Satisfaction: Immediate Post Treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 13.1 11>w of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 14 Patient Satisfaction: Treatment + ST follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 14.1 11w of treatment + 3 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 15 Patient Satisfaction: Treatment + IT follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 15.1 11w of treatment + 6 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 16 Patient Satisfaction: Treatment + LT follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 16.1 11w of treatment + 24 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 17 Global Perceived Effect: Immediate Post Treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 17.1 11w of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 18 Global Perceived Effect: Treatment + ST follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 18.1 11w of treatment + 3 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 19 Global Perceived Effect: Treatment + IT follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 19.1 11w of treatment + 6 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 20 Global Perceived Effect: Treatment + LT follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 20.1 11w of treatment + 24 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
9.2. Analysis.
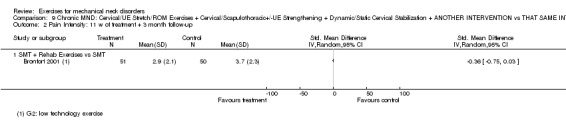
Comparison 9 Chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION vs THAT SAME INTERVENTION, Outcome 2 Pain Intensity: 11 w of treatment + 3 month follow‐up.
9.4. Analysis.
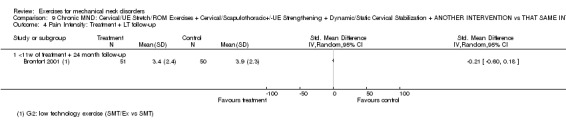
Comparison 9 Chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION vs THAT SAME INTERVENTION, Outcome 4 Pain Intensity: Treatment + LT follow‐up.
9.5. Analysis.
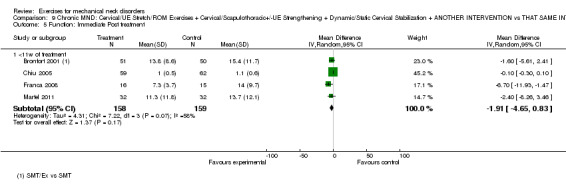
Comparison 9 Chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION vs THAT SAME INTERVENTION, Outcome 5 Function: Immediate Post treatment.
9.6. Analysis.
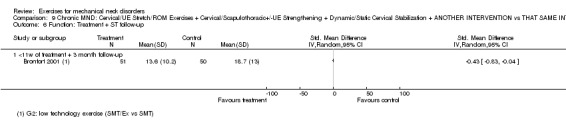
Comparison 9 Chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION vs THAT SAME INTERVENTION, Outcome 6 Function: Treatment + ST follow‐up.
9.7. Analysis.
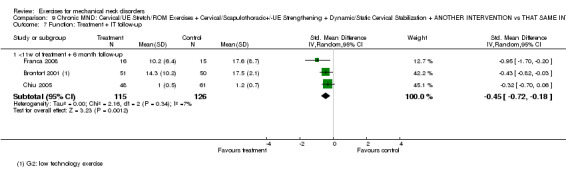
Comparison 9 Chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION vs THAT SAME INTERVENTION, Outcome 7 Function: Treatment + IT follow‐up.
9.8. Analysis.
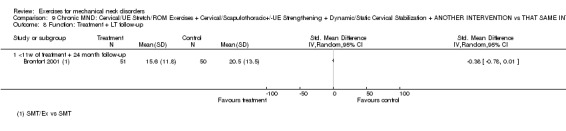
Comparison 9 Chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION vs THAT SAME INTERVENTION, Outcome 8 Function: Treatment + LT follow‐up.
9.10. Analysis.
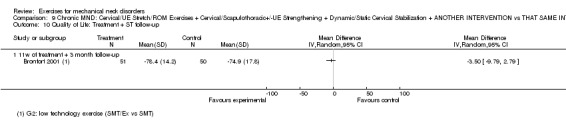
Comparison 9 Chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION vs THAT SAME INTERVENTION, Outcome 10 Quality of Life: Treatment + ST follow‐up.
9.11. Analysis.
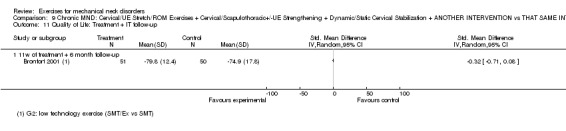
Comparison 9 Chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION vs THAT SAME INTERVENTION, Outcome 11 Quality of Life: Treatment + IT follow‐up.
9.12. Analysis.
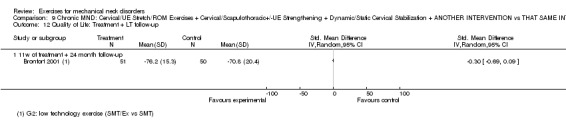
Comparison 9 Chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION vs THAT SAME INTERVENTION, Outcome 12 Quality of Life: Treatment + LT follow‐up.
9.13. Analysis.
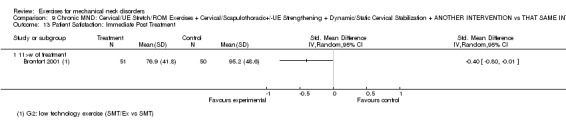
Comparison 9 Chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION vs THAT SAME INTERVENTION, Outcome 13 Patient Satisfaction: Immediate Post Treatment.
9.14. Analysis.
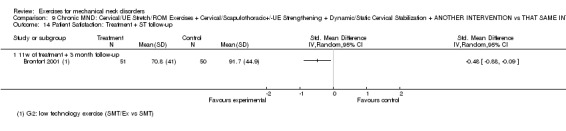
Comparison 9 Chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION vs THAT SAME INTERVENTION, Outcome 14 Patient Satisfaction: Treatment + ST follow‐up.
9.15. Analysis.
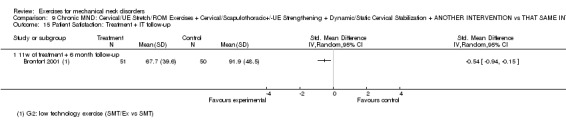
Comparison 9 Chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION vs THAT SAME INTERVENTION, Outcome 15 Patient Satisfaction: Treatment + IT follow‐up.
9.16. Analysis.
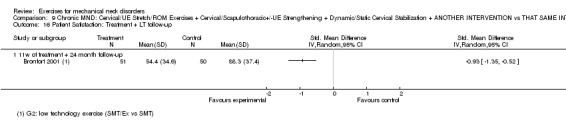
Comparison 9 Chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION vs THAT SAME INTERVENTION, Outcome 16 Patient Satisfaction: Treatment + LT follow‐up.
9.17. Analysis.
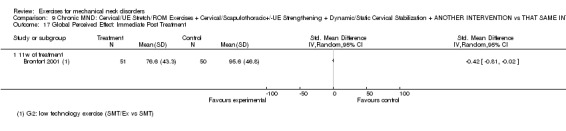
Comparison 9 Chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION vs THAT SAME INTERVENTION, Outcome 17 Global Perceived Effect: Immediate Post Treatment.
9.18. Analysis.
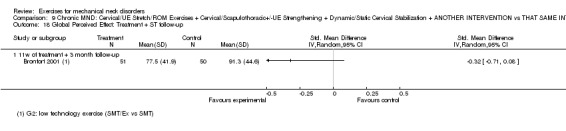
Comparison 9 Chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION vs THAT SAME INTERVENTION, Outcome 18 Global Perceived Effect: Treatment + ST follow‐up.
9.19. Analysis.
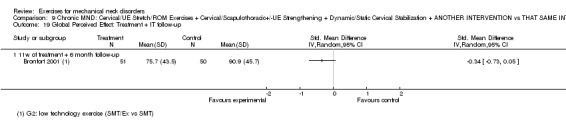
Comparison 9 Chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION vs THAT SAME INTERVENTION, Outcome 19 Global Perceived Effect: Treatment + IT follow‐up.
9.20. Analysis.
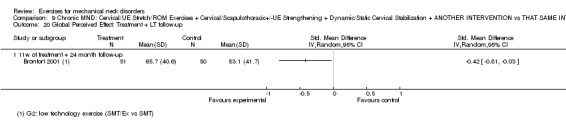
Comparison 9 Chronic MND: Cervical/UE Stretch/ROM Exercises + Cervical/Scapulothoracic+/‐UE Strengthening + Dynamic/Static Cervical Stabilization + ANOTHER INTERVENTION vs THAT SAME INTERVENTION, Outcome 20 Global Perceived Effect: Treatment + LT follow‐up.
Comparison 10. Chronic MND: Cervical Stretch/ROM Exercises + Cervical/Scapulothoracic Strengthening + Static/Dynamic Cervical/Shoulder Stabilization vs WAIT LIST.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain Intensity (VAS): 12 weeks of treatment | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Exercise Therapy vs No Treatment | 2 | 147 | Mean Difference (IV, Random, 95% CI) | ‐14.90 [‐22.40, ‐7.39] |
| 2 Pain Intensity (VAS): 24 weeks of treatment | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Exercise Therapy vs No Treatment | 2 | 140 | Mean Difference (IV, Random, 95% CI) | ‐10.94 [‐18.81, ‐3.08] |
| 3 Function: 12 weeks of treatment | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Exercise Therapy vs No Treatment | 2 | 147 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.50 [‐1.04, 0.03] |
| 4 Function: 24 weeks of treatment | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Exercise Therapy vs No Treatment | 2 | 140 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.40 [‐0.74, ‐0.06] |
| 5 Global Perceived Effect (General Health Perception): 12 weeks of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Exercise Therapy vs No Treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Global Perceived Effect (General Health Perception): 12 weeks of treatment + 12 weeks follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Exercise Therapy vs No Treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Quality of Life (SF‐36): 12 weeks of treatment | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Exercise Therapy vs No Treatment | 2 | 143 | Mean Difference (IV, Random, 95% CI) | ‐2.22 [‐5.17, 0.72] |
| 8 Quality of Life (SF‐36): 24 weeks of treatment | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 8.1 Exercise Therapy vs No Treatment | 2 | 144 | Mean Difference (IV, Random, 95% CI) | 0.06 [‐4.06, 4.17] |
10.1. Analysis.
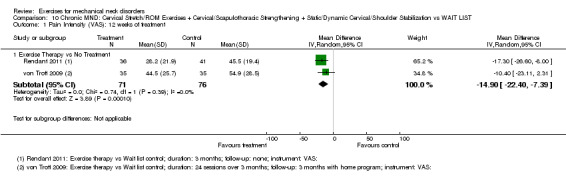
Comparison 10 Chronic MND: Cervical Stretch/ROM Exercises + Cervical/Scapulothoracic Strengthening + Static/Dynamic Cervical/Shoulder Stabilization vs WAIT LIST, Outcome 1 Pain Intensity (VAS): 12 weeks of treatment.
10.2. Analysis.
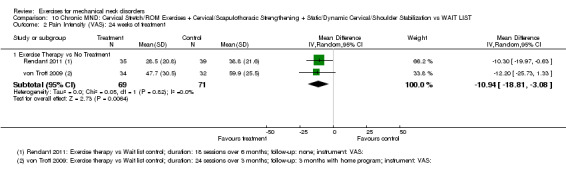
Comparison 10 Chronic MND: Cervical Stretch/ROM Exercises + Cervical/Scapulothoracic Strengthening + Static/Dynamic Cervical/Shoulder Stabilization vs WAIT LIST, Outcome 2 Pain Intensity (VAS): 24 weeks of treatment.
10.5. Analysis.
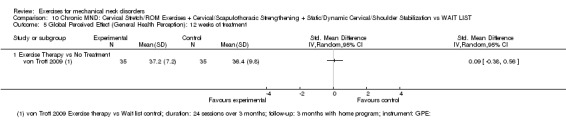
Comparison 10 Chronic MND: Cervical Stretch/ROM Exercises + Cervical/Scapulothoracic Strengthening + Static/Dynamic Cervical/Shoulder Stabilization vs WAIT LIST, Outcome 5 Global Perceived Effect (General Health Perception): 12 weeks of treatment.
10.6. Analysis.
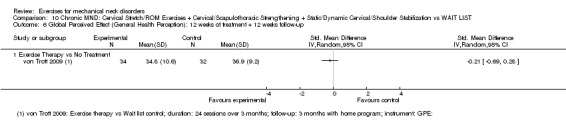
Comparison 10 Chronic MND: Cervical Stretch/ROM Exercises + Cervical/Scapulothoracic Strengthening + Static/Dynamic Cervical/Shoulder Stabilization vs WAIT LIST, Outcome 6 Global Perceived Effect (General Health Perception): 12 weeks of treatment + 12 weeks follow‐up.
Comparison 11. Chronic MND: Cervical/Scapulothoracic/UE Stretch + UE Endurance Training vs NO INTERVENTION or WAIT LIST.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain Intensity (VAS): 12 weeks of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Dynamic muscle training vs control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Pain Intensity (VAS): 12 weeks of treatment + 3 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Dynamic muscle training vs control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Pain Intensity (VAS): 12 weeks of treatment + 9 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Dynamic muscle training vs control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Function (Neck Disability 0‐80): 12 weeks of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Dynamic muscle training vs control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Function (Neck Disability 0‐80): 12 weeks of treatment + 3 month follow‐up | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | Totals not selected | |
| 5.1 Dynamic muscle training vs control | 1 | Std. Mean Difference (IV, Fixed, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Function (Neck Disability 0‐80): 12 weeks of treatment + 9 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Dynamic muscle training vs control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
11.1. Analysis.
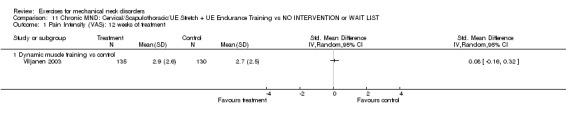
Comparison 11 Chronic MND: Cervical/Scapulothoracic/UE Stretch + UE Endurance Training vs NO INTERVENTION or WAIT LIST, Outcome 1 Pain Intensity (VAS): 12 weeks of treatment.
11.2. Analysis.
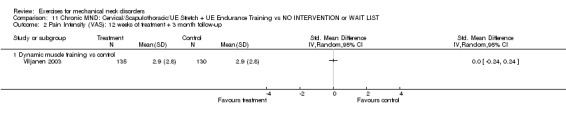
Comparison 11 Chronic MND: Cervical/Scapulothoracic/UE Stretch + UE Endurance Training vs NO INTERVENTION or WAIT LIST, Outcome 2 Pain Intensity (VAS): 12 weeks of treatment + 3 month follow‐up.
11.3. Analysis.
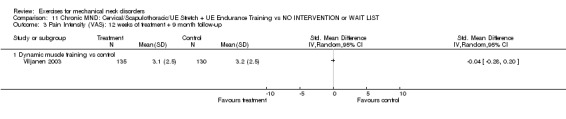
Comparison 11 Chronic MND: Cervical/Scapulothoracic/UE Stretch + UE Endurance Training vs NO INTERVENTION or WAIT LIST, Outcome 3 Pain Intensity (VAS): 12 weeks of treatment + 9 month follow‐up.
11.4. Analysis.
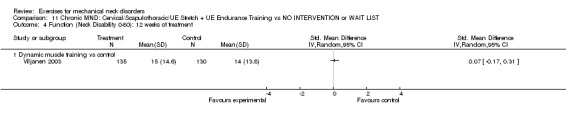
Comparison 11 Chronic MND: Cervical/Scapulothoracic/UE Stretch + UE Endurance Training vs NO INTERVENTION or WAIT LIST, Outcome 4 Function (Neck Disability 0‐80): 12 weeks of treatment.
11.5. Analysis.
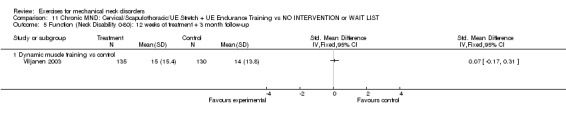
Comparison 11 Chronic MND: Cervical/Scapulothoracic/UE Stretch + UE Endurance Training vs NO INTERVENTION or WAIT LIST, Outcome 5 Function (Neck Disability 0‐80): 12 weeks of treatment + 3 month follow‐up.
11.6. Analysis.
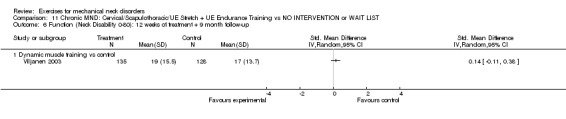
Comparison 11 Chronic MND: Cervical/Scapulothoracic/UE Stretch + UE Endurance Training vs NO INTERVENTION or WAIT LIST, Outcome 6 Function (Neck Disability 0‐80): 12 weeks of treatment + 9 month follow‐up.
Comparison 12. Acute to Chronic MND: Pattern synchronization + cervical/scapulothoracic strengthening + scapulothoracic endurance vs NO INTERVENTION.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain Intensity (VAS 0 to 10): 24 weeks of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Training group vs control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
12.1. Analysis.
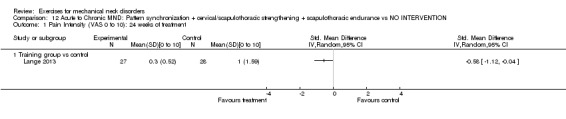
Comparison 12 Acute to Chronic MND: Pattern synchronization + cervical/scapulothoracic strengthening + scapulothoracic endurance vs NO INTERVENTION, Outcome 1 Pain Intensity (VAS 0 to 10): 24 weeks of treatment.
Comparison 13. Chronic MND: Cervical/Scapulothoracic Strengthening + Cervical/Scapulothoracic Endurance Training.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain Prevelance during previous week: 6 weeks of treatment + 46 weeks follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 1.1 Exercise Regimen vs control group | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
13.1. Analysis.
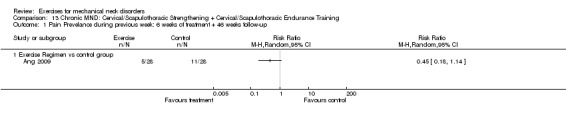
Comparison 13 Chronic MND: Cervical/Scapulothoracic Strengthening + Cervical/Scapulothoracic Endurance Training, Outcome 1 Pain Prevelance during previous week: 6 weeks of treatment + 46 weeks follow‐up.
Comparison 14. Acute to Chronic MND: Scapulothoracic/UE Endurance Training vs CONTROL.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain Intensity (VAS): 10 weeks treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 2 minute training group vs Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 1.2 12 minute training group vs Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
14.1. Analysis.
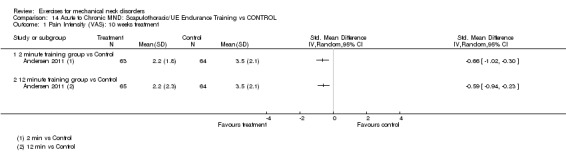
Comparison 14 Acute to Chronic MND: Scapulothoracic/UE Endurance Training vs CONTROL, Outcome 1 Pain Intensity (VAS): 10 weeks treatment.
Comparison 15. Chronic MND: Neuromuscular Education (eye neck coordination/proprioception) + ANOTHER INTERVENTION VS THAT SAME INTERVENTION.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain Intensity (VAS): 8 weeks treatment + 10 weeks follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Rehabilitation Group vs Control Group | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Function (pt's assessment of functional improvement): 8 weeks treatment + 10 weeks follow‐up | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 2.1 Rehabilitation Group vs Control Group | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
15.1. Analysis.
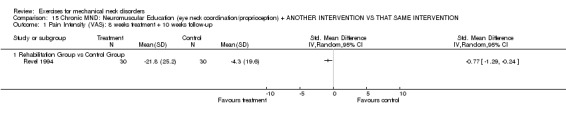
Comparison 15 Chronic MND: Neuromuscular Education (eye neck coordination/proprioception) + ANOTHER INTERVENTION VS THAT SAME INTERVENTION, Outcome 1 Pain Intensity (VAS): 8 weeks treatment + 10 weeks follow‐up.
15.2. Analysis.
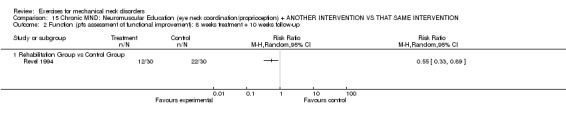
Comparison 15 Chronic MND: Neuromuscular Education (eye neck coordination/proprioception) + ANOTHER INTERVENTION VS THAT SAME INTERVENTION, Outcome 2 Function (pt's assessment of functional improvement): 8 weeks treatment + 10 weeks follow‐up.
Comparison 16. Chronic MND:Trunk/Extremity Stretch + Pattern/Synchronization: Balance and Coordination + Cardiovascular/Aerobic vs NO TREATMENT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain Intensity (VAS): 10 weeks of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Group Gymnastics vs Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
16.1. Analysis.
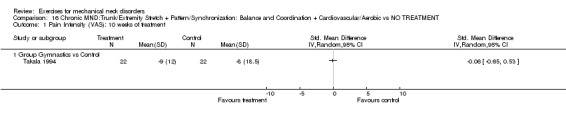
Comparison 16 Chronic MND:Trunk/Extremity Stretch + Pattern/Synchronization: Balance and Coordination + Cardiovascular/Aerobic vs NO TREATMENT, Outcome 1 Pain Intensity (VAS): 10 weeks of treatment.
Comparison 17. Chronic MND:General Endurance Training + Dynamic/Static Lowback/pelvic Stabilization + General Stretching + Neuromuscular/body Mechanics Movement Training vs NO INTERVENTION OR WAIT LIST.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain Intensity (VAS): 16 weeks treatment + 6 weeks follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Physiotherapy Group vs Control Group | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
17.1. Analysis.
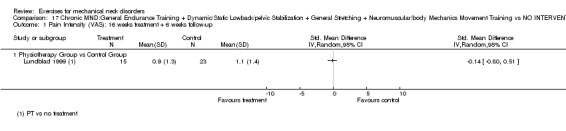
Comparison 17 Chronic MND:General Endurance Training + Dynamic/Static Lowback/pelvic Stabilization + General Stretching + Neuromuscular/body Mechanics Movement Training vs NO INTERVENTION OR WAIT LIST, Outcome 1 Pain Intensity (VAS): 16 weeks treatment + 6 weeks follow‐up.
Comparison 18. Chronic MND: Stretch/ROM + Endurance Training + Dynamic Stabilization + Cognitive (mindfulness & emotional balance) vs WAIT LIST.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain Intensity (VAS): 12 weeks of treatment | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 1.1 Qigong vs No Treatment | 2 | 148 | Mean Difference (IV, Random, 95% CI) | ‐13.28 [‐20.98, ‐5.58] |
| 2 Pain Intensity (VAS): 24 weeks of treatment | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Qigong vs No Treatment | 2 | 137 | Mean Difference (IV, Random, 95% CI) | ‐7.82 [‐14.57, ‐1.07] |
| 3 Function: 12 weeks of treatment | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 3.1 Qigong vs No Treatment | 2 | 148 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.36 [‐0.68, ‐0.03] |
| 4 Function: 24 weeks of treatment | 2 | Std. Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 4.1 Qigong vs No Treatment | 2 | 137 | Std. Mean Difference (IV, Random, 95% CI) | ‐0.28 [‐0.68, 0.11] |
| 5 Global Perceived Effect (General Health Perception): 12 weeks of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Qigong vs No Treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Global Perceived Effect (General Health Perception): 12 weeks of treatment + 12 weeks Follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Qigong vs No Treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Quality of Life (SF‐36 physical component): 12 weeks of treatment | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 7.1 Qigong vs No Treatment | 2 | 148 | Mean Difference (IV, Random, 95% CI) | ‐2.72 [‐5.42, ‐0.01] |
| 8 Quality of Life: 24 weeks of treatment | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 8.1 Qigong vs No Treatment | 2 | 137 | Mean Difference (IV, Random, 95% CI) | ‐1.88 [‐5.80, 2.04] |
18.5. Analysis.
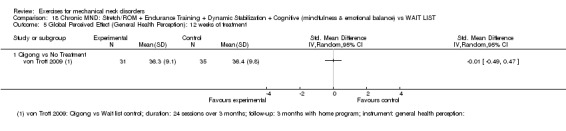
Comparison 18 Chronic MND: Stretch/ROM + Endurance Training + Dynamic Stabilization + Cognitive (mindfulness & emotional balance) vs WAIT LIST, Outcome 5 Global Perceived Effect (General Health Perception): 12 weeks of treatment.
18.6. Analysis.
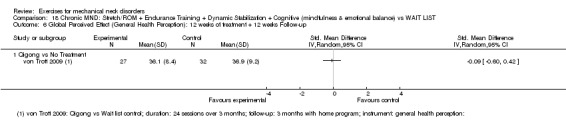
Comparison 18 Chronic MND: Stretch/ROM + Endurance Training + Dynamic Stabilization + Cognitive (mindfulness & emotional balance) vs WAIT LIST, Outcome 6 Global Perceived Effect (General Health Perception): 12 weeks of treatment + 12 weeks Follow‐up.
Comparison 19. Subacute to chronic WAD: Trunk/Extremity Stretch/ROM + Trunk/Extremity Strengthening + Trunk/Extremity Endurance Training + Pattern/Synchronization: Coordination + Cardiovascular/Aerobic + Cognitive (CBT) + ANOTHER TREATMENT vs THAT SAME OTHER TREATMENT.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain Intensity: (0‐10 box scale): 6 weeks of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Exercise + Advice vs Advice | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Pain Intensity (0‐10 box scale): 6 weeks treatment + 12 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Exercise + Advice vs Advice | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Function (NDI): 6 weeks of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Exercise + Advice vs Advice | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Function (NDI): 6 weeks of treatment + 12 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Exercise + Advice vs Advice | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Global Perceived Effect (‐5 to 5 scale): 6 weeks of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Exercise + Advice vs Advice | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Global Perceived Effect (‐5 to 5 scale): 6 weeks of treatment + 12 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Exercise + Advice vs Advice | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 7 Quality of Life (SF‐36): 6 weeks of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 7.1 Exercise + Advice vs Advice | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 8 Quality of Life (SF‐36): 6 weeks of treatment + 12 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 8.1 Exercise + Advice vs Advice | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
19.1. Analysis.
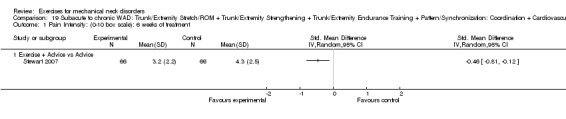
Comparison 19 Subacute to chronic WAD: Trunk/Extremity Stretch/ROM + Trunk/Extremity Strengthening + Trunk/Extremity Endurance Training + Pattern/Synchronization: Coordination + Cardiovascular/Aerobic + Cognitive (CBT) + ANOTHER TREATMENT vs THAT SAME OTHER TREATMENT, Outcome 1 Pain Intensity: (0‐10 box scale): 6 weeks of treatment.
19.2. Analysis.
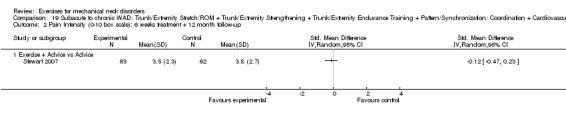
Comparison 19 Subacute to chronic WAD: Trunk/Extremity Stretch/ROM + Trunk/Extremity Strengthening + Trunk/Extremity Endurance Training + Pattern/Synchronization: Coordination + Cardiovascular/Aerobic + Cognitive (CBT) + ANOTHER TREATMENT vs THAT SAME OTHER TREATMENT, Outcome 2 Pain Intensity (0‐10 box scale): 6 weeks treatment + 12 month follow‐up.
19.3. Analysis.
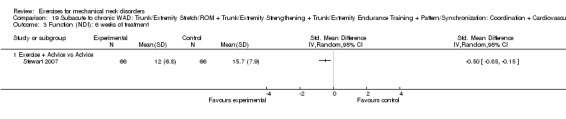
Comparison 19 Subacute to chronic WAD: Trunk/Extremity Stretch/ROM + Trunk/Extremity Strengthening + Trunk/Extremity Endurance Training + Pattern/Synchronization: Coordination + Cardiovascular/Aerobic + Cognitive (CBT) + ANOTHER TREATMENT vs THAT SAME OTHER TREATMENT, Outcome 3 Function (NDI): 6 weeks of treatment.
19.4. Analysis.
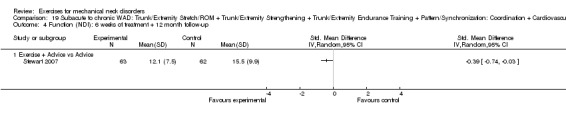
Comparison 19 Subacute to chronic WAD: Trunk/Extremity Stretch/ROM + Trunk/Extremity Strengthening + Trunk/Extremity Endurance Training + Pattern/Synchronization: Coordination + Cardiovascular/Aerobic + Cognitive (CBT) + ANOTHER TREATMENT vs THAT SAME OTHER TREATMENT, Outcome 4 Function (NDI): 6 weeks of treatment + 12 month follow‐up.
19.5. Analysis.
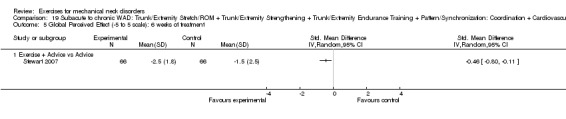
Comparison 19 Subacute to chronic WAD: Trunk/Extremity Stretch/ROM + Trunk/Extremity Strengthening + Trunk/Extremity Endurance Training + Pattern/Synchronization: Coordination + Cardiovascular/Aerobic + Cognitive (CBT) + ANOTHER TREATMENT vs THAT SAME OTHER TREATMENT, Outcome 5 Global Perceived Effect (‐5 to 5 scale): 6 weeks of treatment.
19.6. Analysis.
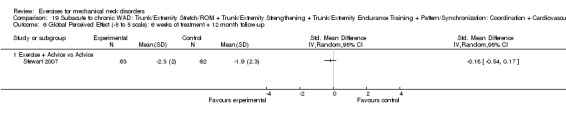
Comparison 19 Subacute to chronic WAD: Trunk/Extremity Stretch/ROM + Trunk/Extremity Strengthening + Trunk/Extremity Endurance Training + Pattern/Synchronization: Coordination + Cardiovascular/Aerobic + Cognitive (CBT) + ANOTHER TREATMENT vs THAT SAME OTHER TREATMENT, Outcome 6 Global Perceived Effect (‐5 to 5 scale): 6 weeks of treatment + 12 month follow‐up.
19.7. Analysis.
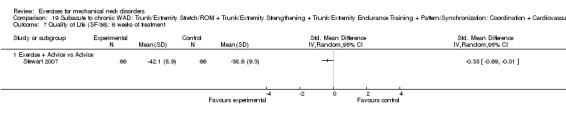
Comparison 19 Subacute to chronic WAD: Trunk/Extremity Stretch/ROM + Trunk/Extremity Strengthening + Trunk/Extremity Endurance Training + Pattern/Synchronization: Coordination + Cardiovascular/Aerobic + Cognitive (CBT) + ANOTHER TREATMENT vs THAT SAME OTHER TREATMENT, Outcome 7 Quality of Life (SF‐36): 6 weeks of treatment.
19.8. Analysis.
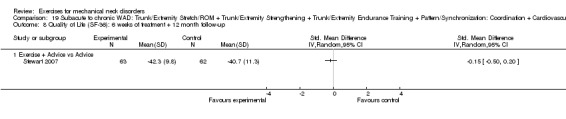
Comparison 19 Subacute to chronic WAD: Trunk/Extremity Stretch/ROM + Trunk/Extremity Strengthening + Trunk/Extremity Endurance Training + Pattern/Synchronization: Coordination + Cardiovascular/Aerobic + Cognitive (CBT) + ANOTHER TREATMENT vs THAT SAME OTHER TREATMENT, Outcome 8 Quality of Life (SF‐36): 6 weeks of treatment + 12 month follow‐up.
Comparison 20. Acute to Subacute CGH: Cervical Stretch/ROM vs SHAM.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain Intensity (Headache Questionnaire): Treatment + 4 weeks follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 C1‐C2 Self Snag vs Placebo Group | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Pain Intensity (Headache Questionnaire): Treatment + 12 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 C1‐C2 Self Snag vs Placebo Group | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
20.1. Analysis.
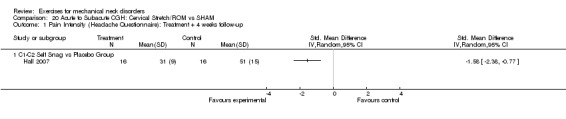
Comparison 20 Acute to Subacute CGH: Cervical Stretch/ROM vs SHAM, Outcome 1 Pain Intensity (Headache Questionnaire): Treatment + 4 weeks follow‐up.
20.2. Analysis.
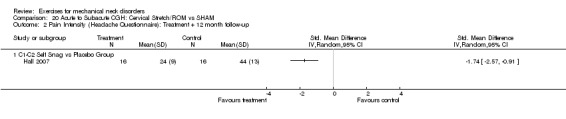
Comparison 20 Acute to Subacute CGH: Cervical Stretch/ROM vs SHAM, Outcome 2 Pain Intensity (Headache Questionnaire): Treatment + 12 month follow‐up.
Comparison 21. Chronic CGH: Cervical/Scapulothoracic Strengthening with Endurance Training + Craniocervical Pressure Biofeedback + Dynamic Cervical Stabilization vs NO INTERVENTION or WAIT LIST.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Headache Intensity (VAS 0‐10): 6 weeks of treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Therapeutic Exercise +/‐ Manip vs Control Group or Manip | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Headache Intensity (VAS 0‐10): 6 weeks treatment + 12 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Therapeutic Exercise +/‐ Manip vs Control Group or Manip | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Function (NPNPQ 0‐36): 6 weeks treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Therapeutic Exercise +/‐ Manip vs Control Group or Manip | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Function (NPNPQ 0‐36): 6 weeks treatment + 12 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Therapeutic Exercise +/‐ Manip vs Control Group or Manip | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Global Perceived Effect (VAS): 6 weeks treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 5.1 Therapeutic Exercise +/‐ Manip vs Control Group or Manip | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 6 Global Perceived Effect (VAS): 6 weeks treatment + 12 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 6.1 Therapeutic Exercise +/‐ Manip vs Control Group or Manip | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] |
21.1. Analysis.
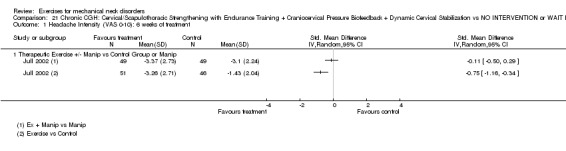
Comparison 21 Chronic CGH: Cervical/Scapulothoracic Strengthening with Endurance Training + Craniocervical Pressure Biofeedback + Dynamic Cervical Stabilization vs NO INTERVENTION or WAIT LIST, Outcome 1 Headache Intensity (VAS 0‐10): 6 weeks of treatment.
21.3. Analysis.
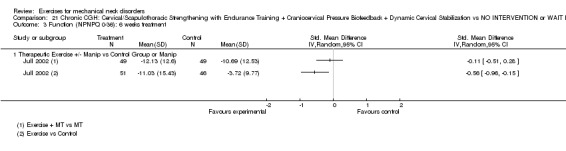
Comparison 21 Chronic CGH: Cervical/Scapulothoracic Strengthening with Endurance Training + Craniocervical Pressure Biofeedback + Dynamic Cervical Stabilization vs NO INTERVENTION or WAIT LIST, Outcome 3 Function (NPNPQ 0‐36): 6 weeks treatment.
21.5. Analysis.
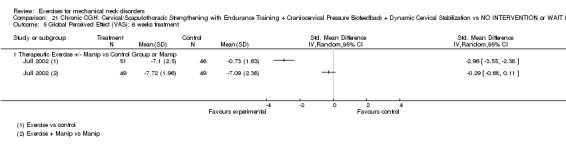
Comparison 21 Chronic CGH: Cervical/Scapulothoracic Strengthening with Endurance Training + Craniocervical Pressure Biofeedback + Dynamic Cervical Stabilization vs NO INTERVENTION or WAIT LIST, Outcome 5 Global Perceived Effect (VAS): 6 weeks treatment.
Comparison 22. Acute Radiculopathy (NDR): Cervical Stretch/ROM + Cervical/Scapulothoracic/UE Strengthening + Static/Dynamic Cervical Stabilization vs WAIT LIST.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain Intensity (VAS): 6 weeks treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 1.1 Physiotherapy vs Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 2 Pain Intensity (VAS): 6 weeks treatment + 6 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2.1 Physiotherapy vs Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 3 Function (NDI): 6 weeks treatment | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 3.1 Physiotherapy vs Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 4 Function (NDI): 6 weeks treatment + 6 month follow‐up | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 4.1 Physiotherapy vs Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | 0.0 [0.0, 0.0] | |
| 5 Satisfaction (5 point scale): 6 weeks treatment | 1 | Risk Ratio (M‐H, Random, 95% CI) | Totals not selected | |
| 5.1 Physiotherapy vs Control | 1 | Risk Ratio (M‐H, Random, 95% CI) | 0.0 [0.0, 0.0] |
22.1. Analysis.
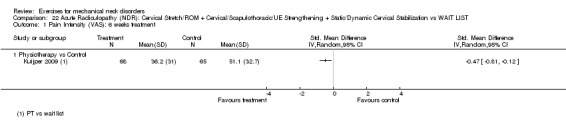
Comparison 22 Acute Radiculopathy (NDR): Cervical Stretch/ROM + Cervical/Scapulothoracic/UE Strengthening + Static/Dynamic Cervical Stabilization vs WAIT LIST, Outcome 1 Pain Intensity (VAS): 6 weeks treatment.
22.2. Analysis.
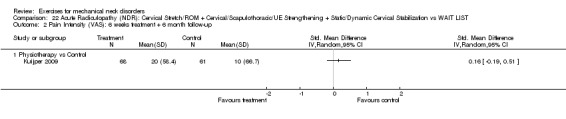
Comparison 22 Acute Radiculopathy (NDR): Cervical Stretch/ROM + Cervical/Scapulothoracic/UE Strengthening + Static/Dynamic Cervical Stabilization vs WAIT LIST, Outcome 2 Pain Intensity (VAS): 6 weeks treatment + 6 month follow‐up.
22.3. Analysis.
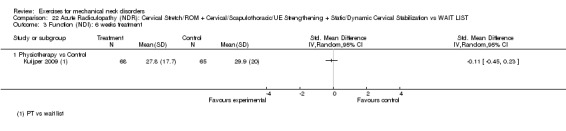
Comparison 22 Acute Radiculopathy (NDR): Cervical Stretch/ROM + Cervical/Scapulothoracic/UE Strengthening + Static/Dynamic Cervical Stabilization vs WAIT LIST, Outcome 3 Function (NDI): 6 weeks treatment.
22.4. Analysis.
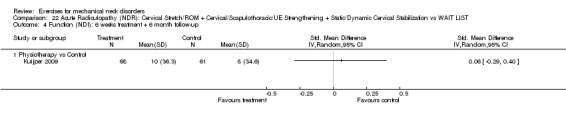
Comparison 22 Acute Radiculopathy (NDR): Cervical Stretch/ROM + Cervical/Scapulothoracic/UE Strengthening + Static/Dynamic Cervical Stabilization vs WAIT LIST, Outcome 4 Function (NDI): 6 weeks treatment + 6 month follow‐up.
22.5. Analysis.
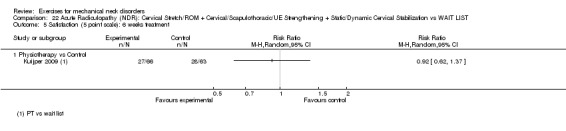
Comparison 22 Acute Radiculopathy (NDR): Cervical Stretch/ROM + Cervical/Scapulothoracic/UE Strengthening + Static/Dynamic Cervical Stabilization vs WAIT LIST, Outcome 5 Satisfaction (5 point scale): 6 weeks treatment.
Comparison 23. Chronic MND: Patterns synchronization + Feedforward/feedback: vestibular rehabilitation (balance on unstable surfaces and walking with head movements and eyes closed) vs NO INTERVENTION.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain Intensity (VAS) 6 weeks vs Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected | |
| 2 Pain Intensity (VAS) 3 months vs control | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected |
23.1. Analysis.
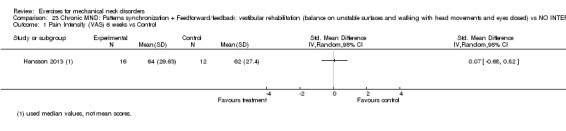
Comparison 23 Chronic MND: Patterns synchronization + Feedforward/feedback: vestibular rehabilitation (balance on unstable surfaces and walking with head movements and eyes closed) vs NO INTERVENTION, Outcome 1 Pain Intensity (VAS) 6 weeks vs Control.
23.2. Analysis.
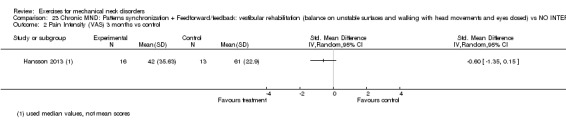
Comparison 23 Chronic MND: Patterns synchronization + Feedforward/feedback: vestibular rehabilitation (balance on unstable surfaces and walking with head movements and eyes closed) vs NO INTERVENTION, Outcome 2 Pain Intensity (VAS) 3 months vs control.
Comparison 24. Chronic MND: Patterns synchronization + Feedforward/feedback: exercises for coordinating the neck, eyes and upper limbs vs NO INTERVENTION.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Pain intensity (VAS) 4 weeks vs Control | 1 | Std. Mean Difference (IV, Random, 95% CI) | Totals not selected |
24.1. Analysis.
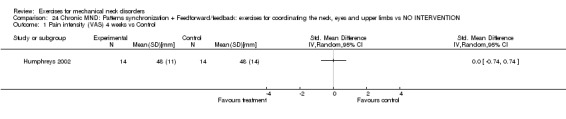
Comparison 24 Chronic MND: Patterns synchronization + Feedforward/feedback: exercises for coordinating the neck, eyes and upper limbs vs NO INTERVENTION, Outcome 1 Pain intensity (VAS) 4 weeks vs Control.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Allan 2003.
| Methods | Type of Trial: RCT Number Analyzed/Randomized: 16/16 Intention‐to‐treat Analysis: N/A Power Analysis: NR | |
| Participants | Chronic MND (Myofascial Pain Syndrome) Radicular signs/symptoms: Absent Setting: Outpatient university teaching clinic Country: UK | |
| Interventions |
INDEX TREATMENT
Arm 1‐ a. Stretch before Manipulation: Activity‐ Static passive stretches into Movement ‐ lateral flexion and rotation on both sides of neck, held for 15 seconds, Mode‐ administered by chiropractor with patient in supine position, immediately followed by cervical manipulation given in accordance with the motion palpation findings. Manipulation was administered with patient in supine position and the chiropractor making an index‐finger contact on the affected cervical segment(s); Dosage‐ 8 sessions over 4 weeks, b. Cervical manipulation given in accordance with the motion palpation findings. Maipulation was administered with patient in supine position and the chiropractor making an index‐finger contact on the affected cervical segment(s) immediately followed by static passive stretches in lateral flexion and rotation on both sides of neck, held for 15 seconds, administered by chiropractor with patient in seated position; Arm 2‐ a. Stretch after Manipulation: Stretches as in Arm 1 was administered after manipulation treatment. b. Cervical manipulation administered as in Arm 1. Treatment Schedule: 8 sessions over 4 weeks COMPARISON TREATMENT Arm 3‐ Manipulation: Cervical manipulation given in accordance with the motion palpation findings. Maipulation was administered with patient in supine position and the chiropractor making an index‐finger contact on the affected cervical segment(s); 8 sessions over 4 weeks. Treatment Schedule: 4 weeks, 20 sessions Duration of Follow‐up: none CO‐INTERVENTION: avoided in trial design |
|
| Outcomes |
PAIN NRS, 0 to 100 Baseline Mean: Manip 30, Stretch before 58, Stretch After 63 Reported Results: no significant difference between groups FUNCTION NDI, 0 to 50 Baseline Mean: Manip 5, Stretch before 16, Stretch After 11 Reported Results: no significant difference between groups REASON FOR DROP‐OUTS: N/A SIDE EFFECTS: none COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | No description |
| Allocation concealment (selection bias) | Unclear risk | No description given |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Not possible due to design |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible due to design |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Not possible due to design |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | See abstract |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | No drop‐outs |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Similarity of baseline characteristics? | High risk | ROM different between groups |
| Co‐interventions avoided or similar? | Unclear risk | No mention |
| Compliance acceptable? | Low risk | See abstract |
| Timing outcome assessments similar? | Low risk | Tables 1 and 2 |
Andersen 2008.
| Methods | Type of Trial: RCT Number Analyzed/Randomized: 42/48 Intention‐to‐treat Analysis: NR Power Analysis: NR | |
| Participants | (sub) Acute/Chronic MND (Trapezius Myalgia) Radicular signs/symptoms: Absent Setting: Seven workplaces Country: Denmark | |
| Interventions |
INDEX TREATMENT Arm 1‐ Specific Strength Training (SST) or General Fitness Training (GFT): Activity‐ (SST): high intensity specific strength training locally for neck and shoulder muscles. (GFT): Cycling high‐intensity general fitness training with legs only, upright position without holding onto the handlebars (relaxing shoulders during training), Mode‐ (SST): 5 dumbbell exercises. (GFT): Monark bicycle ergometer, Movement‐ (SST): single arm row, shoulder abduction, shoulder elevation, reverse flies, and upright row).Training program progressively increased using the principles of periodization and progressive overload from 12 repetitions maximum (˜70% of maximal intensity) at beginning to 8 repetitions maximum (˜80% of maximal intensity) later. (GFT): high‐intensity cycling, Dosage‐ (SST): performed using consecutive concentric and eccentric muscle contractions (raising and lowering pair of dumbbells) in a controlled manner without pause, each set lasting 25‐35 seconds. 30 of 5 different exercises with 3 sets per exercise were performed during each training session in an alternating manner (shoulder elevation was performed during each session). Doubled training load by end of 10 weeks. 20 minutes, 3x/week for 10 weeks of intervention for an average of 26 ± 3.6 sessions (GFT): 20 min at a relative workloads of 50% (initial training level) to 70% (increased during following weeks and maintained) of maximal oxygen uptake (V02 max). Heart rate monitor (Polar Sport Tester, Polar, Kempele, Finland) used to adjust workload to meet the intended relative level. Treatment schedule: (SST): Doubled training load by end of 10 weeks. 20 minutes 3 times/week for 10 weeks of intervention for an average of 25 ± 4.8 sessions. (GFT): 20 minutes 3 times/week for 10 weeks. COMPARISON TREATMENT Arm 2‐ Health Counseling Group: Lectures with information on activities promoting general health and individual: workplace ergonomics, diet, health, relaxation, and stress management. 1 hour per week for 10 weeks for an average of average 27 ± 2.8 sessions Treatment Schedule: 10 weeks, 20 sessions Duration of Follow‐up: 10 weeks CO‐INTERVENTION: Not avoided COMPARISON TREATMENT Reference intervention without physical activity (REF): Activity‐the participants received health counselling on group and individual levels regarding workplace ergonomics, diet, health, relaxation, and stress management, frequency: 3x per week. Dosage‐ 20‐minutes sessions Treatment Schedule: 30 sessions over 10 weeks Duration of Follow‐up: none CO‐INTERVENTION: Not specified |
|
| Outcomes |
PAIN in trapezius muscle VAS, 0 to 100 Baseline Mean: SST 44, GFT 50, REF 43 Reported Results: no significant difference between groups SMD immediate post: 0.18 (‐0.67 to 1.03) SMD ST: ‐0.06 (95% CI: ‐0.91 to 0.79) REASON FOR DROP‐OUTS: 6 in Reference group, reason not specified SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | No description of concealment |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Not possible due to intervention |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible due to intervention |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Not possible due to study design |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Unclear risk | 9% drop‐out acceptable, but reason for drop‐outs not described. Furthermore, it is unclear which groups' data were missing (see Sogaard 2012) |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Unclear risk | p 90 ‐ 6 drop‐outs in the REF group ‐ not analyzed |
| Selective reporting (reporting bias) | Low risk | Trial registration adequate. International Standard Randomized Controlled Trial Number Register: ISRCTN87055459. (see Sogaard 2012) |
| Similarity of baseline characteristics? | Unclear risk | Table 1 p 88 |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | High risk | p 87 |
| Timing outcome assessments similar? | Low risk | P175, right column, 2nd paragraph (Sogaard 2012) |
Andersen 2011.
| Methods | Type of Trial: RCT Number Analyzed/Randomized: 192/198 Intention‐to‐treat Analysis: calculated Power Analysis: 95% | |
| Participants | (sub) Acute/Chronic MND (Myofascial Pain Syndrome/Cervicogenic headache/tension type headache?) Radicular signs/symptoms: Not specified Setting: two large white collar organizations Country: Denmark | |
| Interventions |
INDEX TREATMENT
Arm 1‐ 2 minute training (2‐minutes):Activity‐ Progressive resistance training with theraband. Mode‐Shoulder Movement‐ abduction‐ lateral raise. Dosage: 2 minutes, 5 times/week for 10 weeks of intervention for an average of 26 ± 3.6 sessions Arm 2‐ 12‐minute training: Activity‐ Progressive resistance training with theraband. Mode‐Shoulder, Movement‐ abduction‐ lateral raise. Dosage‐ 12 minutes 5 times/week for 10 weeks of intervention for an average of 25 ± 4.8 sessions COMPARISON TREATMENT Arm 3‐ Control Group: Weekly e‐mailed information on various aspects of general health and internet links with additional relevant information Treatment Schedule:10 weeks, 20 sessions Duration of Follow‐up: 10 weeks CO‐INTERVENTION: Not avoided |
|
| Outcomes |
PAIN VAS, 0 to 10 Baseline Mean: 2 minutes 3.5, 12 minutes 3.9, Control 3.5 Reported Results: ANOVA showed a strong group‐by‐time effect for neck/shoulder pain intensity (P < 0.0001). Compared with the control group, pain intensity decreased in both training groups. This change was not significantly different between the 2 training groups. SMD (2 min): ‐0.66 (95% CI: ‐1.02 to ‐0.30) SMD (12 min): ‐0.59 (95% CI: ‐0.94 to ‐0.23) REASON FOR DROP‐OUTS: 3 in 2 minutes group, 1 in 12 minutes group, 2 in Control group, reasons reported SIDE EFFECTS: Reported worsening of neck muscle tension during and/or in the days after training (2‐minute n = 1, 12‐minute n = 4), shoulder joint pain during training (2‐minute n = 1, 12‐minute n = 4), pain in the upper arm during training (2‐minute n = 1, 12‐minute n = 1), pain of the forearm/wrist during training (12‐minute n = 2), worsening of headache after training (2‐minute n = 1, 12‐minute n = 1). No long‐lasting or major complications resulted from the training program. COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | pg 444 second column/ pg 442 first column |
| Allocation concealment (selection bias) | Low risk | Described pg 444 |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Not possible due to intervention |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible due to intervention |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Not possible self‐ assessment evaluation NPRS |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | p 443 second column |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | Figure 1 p 441 ‐ not all participants randomized were analyzed |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | Low risk | Co‐interventions similar p 443 section 2.5 |
| Compliance acceptable? | Low risk | p 443 second column |
| Timing outcome assessments similar? | Low risk | p 443 top of 1st/p 441 under methods |
Andersen Ch 2012.
| Methods |
Type of trial: RCT Number Analyzed/Randomized: 158/449 Intention‐to‐treat analysis: calculated Power Analysis: 95% |
|
| Participants | Non specific neck pain Radicular signs/symptoms: NR Setting: NR Country: Denmark |
|
| Interventions |
INDEX TREATMENT Arm 1‐ Training groups (WS): Activity‐ Upper extremity strength training Mode‐ Weights. Movement‐ Dumbbell exercises front raise, lateral raise, reverse flies shrugs and wrist extension.Dosage‐ Type of contraction (dynamic); Intensity (20 repetition maximum at baseline to 8 repetition maximum at later phase); Speed (NR); Duration/Frequency (1‐weekly session WS = 1hour/week, 3WS = 20 minutes at 3 sessions/week, 9 WS = 7 minutes at 9 sessions/week; Sequence (NR); Environment (NR); Feedback (experienced instructor supervised every other training session). Treatment Schedule: 20 weeks. COMPARISON TREATMENT Arm 2‐ Reference group: No treatment Treatment Schedule: 20 weeks Duration of Follow‐up: NR CO‐INTERVENTION: NR |
|
| Outcomes |
PAIN Modified Nordic Questionnaire (MNQ), 0 to 9 Baseline Mean: 1WS (4.83), 3WS (4.96), 9WS (4.71), REF (4.83) Reported Results: no significant difference between groups SMD (1WS vs control): ‐0.44 (95% CI: ‐1.31 to 0.43); SMD (3WS vs control): ‐0.67 (95% CI: ‐1.59 to 0.25); SMD (9WS vs control): ‐0.30 (95% CI: ‐1.36 to 0.76) FUNCTION Disability of the arm, shoulder and hand (DASH), 0 to100 Baseline Mean: 1WS (16), 3WS (18), 9WS (15), REF (16) Reported Results: no significant difference between groups SMD (1WS vs control): ‐0.17 (95% CI: ‐0.58 to 0.24); SMD (3WS vs control): ‐0.23 (95% CI: ‐0.66 to 0.19); SMD (9WS vs control): ‐0.06 (95% CI: ‐0.53 to 0.41) REASON FOR DROP‐OUTS: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described in this paper, but Anderson 2010 is referenced to have details |
| Allocation concealment (selection bias) | Unclear risk | Not described in this paper, but Anderson 2010 is referenced to have details |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Perceptible difference between groups |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Perceptible difference between groups |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Patient is the assessor |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | High risk | 38% drop‐out rate |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Unclear risk | Minimum supervision group not described (Figure 1); P1007Lp |
| Selective reporting (reporting bias) | Low risk | See trial registration |
| Similarity of baseline characteristics? | Low risk | Table 2 ‐ gave yes, but some hesitation because of higher proportion of males in 3WS group |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | High risk | P1007Lp1; 56% did more than 20 minutes exercise per week ‐ 60min/week was planned |
| Timing outcome assessments similar? | Low risk | Baseline, 20 weeks |
Ang 2009.
| Methods | Type of Trial: RCT Number Analyzed/Randomized: 56/68 Intention‐to‐treat Analysis: Calculated Power Analysis: Calculated | |
| Participants | Chronic MND (Mechanical Neck Pain & Myofascial Pain Syndrome) Radicular signs/symptoms: Absent Setting: 2 air force helicopter bases Country: Sweden | |
| Interventions |
INDEX TREATMENT
Arm 1‐ Exercise Group: Activity‐ Patterns and synchronization of muscle recruitment, Endurance‐Strengthening exercises, Mode‐ Progression from non postural (supine, prone) low‐load active craniocervical flexion at 5 pressure levels (22 to 30 mmHg), seated postural exercises with active craniocervical flexion and active scapular retraction. Seated and standing elastic resistance, Movement‐ supine craniocervical flexion exercises, prone isometric shoulder/scapular, seated active craniocervical flexion with cervical rotation to end range and simultaneous scapular retraction to mid motion range, sitting controlled dynamic shoulder retraction following a rowing exercise movement, dynamic scapular retraction with weight load over long movement arms in "rowing"exercises in regular pulls, emphasizing shoulder retraction in the initial concentric phase and upright trunk postures in the inner range, Dynamic neck rotation exercises in upright posture against moderate resistance using elastic bands, Dosage‐ Non postural exercises‐held isometrically (low load) for 10 seconds, repeated 10 times. Postural (seated, isometric held at 5 pressure levels like supine, holding 10 seconds, repeated 10 times, neck rotation to end range 3 sets repeated 10 to 15 times on each side. Endurance‐strength exercises 3 sets of 15 repetitions (elastic bands were used to replicate the exercises at home). Feedback The supervising physiotherapist monitored potential surface flexor activity visually, with palpation if necessary. Treatment schedule: Assigned exercises (2 to 4) were to be completed 2 times/day lasting 10 to 15 minutes, supervised weekly by a physiotherapist providing instruction and manual guidance. COMPARISON TREATMENT Arm 2‐ Control: No exercise, encouraged to continue with ordinary exercise activity Treatment Schedule: 6 weeks, instructed to do 2 to 4 exercises 2 times/day, for 10 to 15 minutes, supervised by physiotherapist weekly. Duration of Follow‐up: 12 months CO‐INTERVENTION: Not specified |
|
| Outcomes |
PAIN Prevelance during previous week Baseline Mean (SD): Exercise 13 (38), Control 11 (32) Reported Results: In the exercise group, the prevalence of cases for the previous week and the previous 3 months decreased from 38% to 15% and 76% to 44% respectively, whereas in controls it was unchanged. RR (exercise group vs control): 0.45 (95% CI: 0.18 to 1.14). Between‐group regression analyses revealed that the members of the exercising group had a 3.2 times greater chance (odds ratio) than the control group of having been pain‐free during the previous 7 days and a 1.9 times great chance (odds ratio) of having been pain‐free during the previous 3 months, P = 0.01. REASON FOR DROP‐OUTS: 6 in Exercise Group, 6 in Control Group, reasons reported SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization technique not adequately described |
| Allocation concealment (selection bias) | Unclear risk | Not adequately described |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Patient is assessor |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | Described in Figure 2 |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | Figure 2; P 457Lp3 |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | See Tables 1‐3 |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Unsure of long‐term compliance in exercise group; unsure what compliance data refer to |
| Timing outcome assessments similar? | Low risk | Baseline, 6 weeks, 1 year |
Beer 2012.
| Methods | Type of Trial: RCT Number Analyzed/Randomized: 20/20 Intention‐to‐treat Analysis: Not calculated Power Analysis: Not calculated | |
| Participants | Persistent neck pain Radicular signs/symptoms: Not specified Setting: Local university and newsletter, sedentary office workers Country: Australia | |
| Interventions |
INDEX TREATMENT Arm 1‐ Exercise group: Activity‐ Functional postural exercise. Mode‐ Sitting. Movement‐ Assumes an upright posture in a neutral lumbo‐pelvic position and then gently lengthens the cervical spine by imagining they are lifting the base of their skull from the top of their neck. Dosage‐ concentric‐isometric hold with postural awareness, low intensity,10 second hold every 15 to 20 minutes throughout the day for a total of 2 weeks,all sorts of environment throughout their waking day, feedback was taught initially but not reviewed during the 2 weeks Treatment schedule: 2 weeks COMPARISON TREATMENT Arm 2‐ Control group: Did not undertake any exercise intervention during the study. Treatment schedule: 2 weeks Duration of Follow‐up: NR CO‐INTERVENTION: participants in control group were requested not to seek other treatment for their neck pain for the 2 weeks. |
|
| Outcomes |
PAIN VAS, 0 to 10 Baseline mean: treatment 3.0 control 2.6 Reported results: no significant SMD (exercise vs control): 0.13 (95% CI: ‐0.74 to 1.01) FUNCTION NDI, 0 to100 Baseline mean: treatment 18.1 control 20.6 Reported results: no significant SMD (exercise vs control): ‐0.32 (95% CI: ‐1.21 to 0.56) REASONS FOR DROP‐OUTS: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Randomization technique not adequately described (p.221‐ left column) |
| Allocation concealment (selection bias) | Unclear risk | Not described. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Not possible. Required active patient participation (exercise/posture). |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible. Required active provider participation (exercise prescription/posture education). |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Patient is the outcome assessor. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Unclear risk | Not described. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Unclear risk | Not described. |
| Selective reporting (reporting bias) | Unclear risk | No protocol. |
| Similarity of baseline characteristics? | Low risk | p.222‐ Table 1 |
| Co‐interventions avoided or similar? | Unclear risk | Not measured |
| Compliance acceptable? | Unclear risk | Study group was supposed to do exercise every 15‐20 minutes; see p.222/right column/paragraph 1 for vast range. |
| Timing outcome assessments similar? | Low risk | Baseline and 2 weeks |
Bronfort 2001.
| Methods | Type of Trial: RCT Number Analyzed/Randomized: 158 to 160/191 Intention‐to‐treat analysis: NR Power Analysis: NR | |
| Participants | Chronic MND Radicular signs/symptoms: Absent Setting: University Centre for Clinical Studies and the Physician's Neck and Back Clinic Country: USA, Canada |
|
| Interventions |
INDEX TREATMENT Arm 1‐ MedX Exercise (MedX): Activity‐ High technology exercise, Mode/Movement‐ medically supervised rehabilitative exercise. Dosage‐ 20 sessions over 3 months Arm 2‐ Manipulation and low tech Exercise (SMT/Ex):Activity‐ Chiropractic manipulation, supervised low technology rehabilitative exercise, Mode‐ progressive strengthening exercises for the neck and upper body proceeded by a short aerobic warm up of the upper body and light stretching, Movement‐ the upper body strengthening exercises included push ups and dumbbell shoulder exercises as described by Dyrssen et al 1989. Dosage‐ 45 minutes total, 2 sets of 15 to 30 repetitions, weight 2 to 10 lbs; cervical progressive resisted strengthening exercises where performed while lying on a therapy table with wearing head gear with variable weights from 1.25 lb to 10 lbs guided by a simple pulley system attached to the table Treatment Schedule: 20 sessions over 3 months COMPARISON TREATMENT Arm 3‐ Spinal Manipulative (SMT): Chiropractic manipulation, 20 sessions over 3 months Treatment Schedule: 11 weeks, 20 session Duration of Follow‐up: 12 months CO‐INTERVENTION: NR |
|
| Outcomes |
CUMULATIVE ADVANTAGE for six patient‐oriented outcomes Reported Results: favours SMT/Ex over SMT; MONOVA value yielded a significant group difference (Wilk's Lambda = 0.85, F(12,302) = 2.2, P < 0.01) PAIN VAS, 0 to 10 Baseline Mean: SMT 56.6, MedX 57.1, SMT/Ex 56.0 Reported Results: group difference in patient‐rated pain ANOVA F(2,156) = 4.2, P = 0.02 favours the two exercise groups SMD (SMT/Ex vs SMT) at LT follow‐up: ‐0.21 (95% CI: ‐0.60 to 0.18); power 28%, NNTB 10; treatment advantage 15% FUNCTION NDI, 0 to 50 Reported Results: no significant group differences were found ANOVA: F(2, 156) = 2.04, P = 0.13 SMD (SMT/Ex vs SMT) at LT follow‐up: ‐0.38 (95% CI: ‐0.78 to 0.01), power 28%, NNTB 11, treatment advantage 11% HEALTH‐RELATED QUALITY OF LIFE SF‐36, 0 to 100 Baseline mean: SMT 69.1, MedX 69.0, SMT/Ex 71.7 Reported Results: SMD at LT follow‐up: ‐0.30 (95% CI: ‐0.69 to 0.09) PATIENT SATISFACTION scale 1 to 7 completely satisfied to completely dissatisfied Reported Results: A clinically worthwhile cumulative advantage was reported favouring manipulation/exercise (low tech) group over exercise (high tech) and manipulation alone ANOVA: F(2, 158) = 6.7, P = 0.002 SMD (SMT/Ex vs SMT) at LT follow‐up:‐0.93 (95% CI: ‐1.35 to ‐0.52) PATIENT‐RATED IMPROVEMENT scale 1 to 9 Reported Results: substantial improvement over time, ANOVA: F(2, 174) = 1.7, P = 0.18 SMD (SMT/Ex vs SMT) at LT follow‐up: ‐0.42 (95% CI: ‐0.81 to 0.03); power 44% REASONS FOR DROP‐OUTS: Reported SIDE EFFECTS: increase neck or headache pain 8 SMT/Ex, 9 MedX, 6 SMT; increased radicular pain 1 SMT/Ex; severe thoracic pain 1 SMT; all cases self‐limiting and no permanent injuries; RR(SMT/Ex vs MedX): 0.81 (95% CI: 0.23 to 1.55) RR(SMT vs MedX): 0.61 (95% CI: 0.23 to 1.55) COST OF CARE: NR |
|
| Notes | Final data since there was small difference in reporting data between Bronfort 2001 and Evans 2002, we elected to abstract Evans 2002 data for the data and analyses table. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Sequentially numbered, opaque envelopes, prepared using a computer‐generated list prior to start of study p2384. |
| Allocation concealment (selection bias) | Low risk | Study staff, investigators, clinicians, and patients were masked to upcoming treatment assignments p2384. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Not possible due to self‐report measures |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible due to study design |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Not possible due to study design. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | High risk | 93% at 11 weeks, 76% overall, but not described. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | Only 145 out of 178 participants were analyzed according to Table 2. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Similarity of baseline characteristics? | Low risk | Comparable on measured clinical and demographic characteristics, see Table 1. |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported with respect to exercise |
| Timing outcome assessments similar? | Low risk | 5, 11 weeks of treatment, 3, 6, 12 months |
Chiu 2005.
| Methods | Type of Trial: RCT cross‐over design Number Analyzed/Ransomized: 109/145 Intention‐to‐treat Analysis: Calculated Power Analysis: 90% | |
| Participants | Subacute MND (Cervical Brachial Pain Syndrome) Radicular signs/symptoms: Absent Setting: Physiotherapy Outpatient Department Country: Hong Kong |
|
| Interventions |
INDEX TREATMENT
Arm 1‐ Craniocervical Flexion and isometric neck strengthening (CCF): Activity‐ deep neck flexor strengthening, Infrared irradiation Mode‐ ‐using pressure sensor @20mmhg x10 minutes (10 seconds on/15 seconds off) Strengthening using a Multi Cervical Rehabilitation Unit (MCRU). Movement/Dosage‐ 15 repetitions of flexion, extension at 20% of Peak Isometric Strength (PIS) as warm‐up. Then dynamic flexion and extension with variable resistance x 0 to 12 repetitions.
Treatment Schedule: 35 minutes of exercise per session COMPARISON TREATMENT: Arm 2‐ Transcutaneous Electrical Nerve Stimulation (TENS): 30 minutes of dual channel portable TENS unit (ITO model 1302). Continuous trains of 150ms square pulse at 80Hz. 4 Electrodes (4x4cm). Arm 3‐ Control Group: Infrared Irradiation (IR): place on Ex 21, GB21, LI 11, intensity 2 to 3 times of participants sensory threshold education on neck care Treatment schedule: 20 minutes per session, 6 weeks, 2 sessions/wk Duration of Follow‐up: 6 months CO‐INTERVENTION: NS |
|
| Outcomes |
PAIN VAS, 0 to 10 Baseline Mean: CCF 4.61, TENS 4.69, IR 4.26 Reported Results: NS SMD (CCF vs IR): ‐0.34 (95% CI: ‐0.72 to 0.04); NNTB 6, treatment advantage 24% FUNCTION Northwick Park Questionnaire (NPQ) ‐ Chinese version, 0 to 4 Baseline Mean: CCF 1.39, TENS 1.55, IR 1.36 Reported Results: CCF vs IR was significant (P = 0.02) SMD (CCF vs IR): ‐0.33 (95% CI: ‐0.71 to 0.05); NNTB 6, treatment advantage 16% REASON FOR DROP‐OUTS: Reported SIDE EFFECTS: No complications occurred. COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Computer‐generated minimization method |
| Allocation concealment (selection bias) | Low risk | Computer‐based randomization |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Not possible due to study design |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible due to study design |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Not possible due to study design |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | |
| Selective reporting (reporting bias) | Low risk | |
| Similarity of baseline characteristics? | Low risk | See Table 1 |
| Co‐interventions avoided or similar? | Low risk | |
| Compliance acceptable? | Low risk | |
| Timing outcome assessments similar? | Low risk | See Table 2 |
Dellve 2011.
| Methods |
Type of trial: RCT Number Analyzed/Randomized: 60/73 Intention‐to‐treat Analysis: NR Power Analysis: Not calculated |
|
| Participants | Chronic cervical neck pain or cervicobrachial pain syndrome Radicular signs/symptoms: NR Setting: University Hospital Clinic Country: Sweden |
|
| Interventions |
INDEX TREATMENT Arm 1‐ Myofeedback Training (MT): Activity‐ activities of daily living; Mode‐ wearing a myofeedback device; Movement‐ ergonomic adjustments; Dosage‐ Duration/Frequency (minimum of 8 hours per week, typically 2 hours per day and 4 days per week); ; Environment (various); Feedback (discussion with ergonomist once per week). Arm 2‐ Intensive Muscular Strength Training (IMST): Activity‐ Upper extremity strength training Mode‐ resistance bands Movement‐ Exercises for strengthening and co‐ordinating the upper extremities. Dosage‐ Type of contraction (NR); Intensity (NR); Speed (NR); Duration/Frequency (2 times per day, 6 days per week for 4 weeks); Sequence (warm‐up movements followed by strengthening exercises then ending with breathing and slow down movements); Environment (participant's home); Feedback (ergonomist coaching). Treatment Schedule: 4 weeks COMPARISON TREATMENT Arm 3‐ Control Group: Diary entries to record activities, discomfort, pain and sleeping disturbances Treatment Schedule: 4 weeks Duration of Follow‐up: 2 months CO‐INTERVENTION: not avoided |
|
| Outcomes |
PAIN Numeric Pain Scale, 0 to 10 Baseline Mean: MT (6.0), IMST (6.3), Control (6.2) Reported Results: no significant difference between groups SMD (IMST vs control) at immediate post‐treatment: ‐0.30 (95% CI: ‐0.92 to 0.33); SMD (IMST vs control) at 2 months follow‐up: ‐0.63 (95% CI: ‐1.27 to 0.00) FUNCTION Work Ability Index, 7 to 49 Baseline Mean: MT (19.3), IMST (19.0), Control (19.0) Reported Results: no significant difference between groups SMD (IMST vs control) at immediate post‐treatment: ‐0.18 (95% CI: ‐0.80 to 0.44); SMD (IMST vs control) at 2 months follow‐up: 0.38 (95% CI: ‐0.25 to 1.01) REASON FOR DROP‐OUTS: 5 in MT Group, 7 in IMST Group, 1 in Control Group, reasons reported SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Not possible due to design |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible due to design |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Not possible due to design |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Unclear risk | High drop‐out rate in second group; reasons for drop‐outs not described |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | Figure 1 ‐ only 20 analyzed per group |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Low risk | Table 1 |
| Co‐interventions avoided or similar? | Unclear risk | Not reported by group |
| Compliance acceptable? | Unclear risk | Not reported |
| Timing outcome assessments similar? | Low risk | Baseline, 1 month, 3 months |
Franca 2008.
| Methods | Type of Trial: RCT Number Analyzed/Randomized: 46/49 Intention‐to‐treat Analysis: Not specified Power Analysis: Not calculated | |
| Participants | Chronic MND (Myofascial Pain Syndrome) Radicular signs/symptoms: Absent Setting: University Research and Rehabilitation Department Country: Brazil | |
| Interventions |
INDEX TREATMENT
Arm 1‐ Physiotherapy protocol performed according to Hall and Brody consisting of Activity‐stretching, strengthening Mode‐ muscle stretching of neck and upper limbs regions; recruitment exercise of Deep Cervical Flexion Muscles; Movement‐ strengthening exercise of Deep Cervical Flexion Muscles and upper limbs. Duration of treatment 20 minutes, 1 to 2 times/week for 10 weeks. Arm 2‐ Acupuncture combined with Physiotherapy (G1) Activity‐ Stage 1: acupuncture therapy based on the TCM theory of biao‐li (symptom/root) treatment. Mode‐ Chinese acupuncture, as the root treatment, was performed with a selection of body points by means of the diagnostic of syndromes of TCM. Movement‐ Disposable stainless steel needles (0.25 mm x 30 mm) with guide‐tubes (Dong‐bang Acupuncture Needle, Korea) inserted bilaterally into the body points to a depth of 10 to 15 mm. YNSA was carried out as the symptom treatment with a selection of the kinetic and ypsilon points as the main scalp points to treat TNS. The kinetic points were stimulated bilaterally with needle measuring 0.25 mm x 5 to 15 mm (Dongbang Acupuncture Needle, Korea) to a depth of 1 to 2 mm, whereas the selection of the ypsilon points were ipsilateral of the scalp to the diagnosed side of the neck. All acupoints (body and scalp points) were stimulated in an uneven manner every 10 minutes to maintain the needling sensation. Chinese acupuncture was performed in 20 minutes and YNSA was maintained until 40 minutes. Stage 2: Physiotherapy given simultaneously with YNSA. COMPARISON TREATMENTS: Arm 3‐ Acupuncture (G2): Same protocol of acupuncture therapy as described in the first stage of G1 for 20 minutes. Arm 4‐ Physiotherapy (G3): Same protocol of physiotherapy as described in the second stage of G1 for 20 minutes. Treatment Schedule: 10 weeks, 20 sessions Duration of Follow‐up: 6 months follow‐up CO‐INTERVENTION: avoided in trial |
|
| Outcomes |
PAIN VAS, 0 to 100 Baseline Mean: PT+Acup 85.0, Acup 80.0, PT 70.0 Reported Results: According to KWT (Kruskal‐Wallis test), the statistical analysis of the inter‐groups demonstrated significant (P < 0.05) differences among the groups. The DMCT (Dunn's Multiple Comparison test) showed that G1 was superior to G3 in pain improvement (P < 0.05) SMD (PT+ Acup vs Acup) at immediate post treatment: ‐0.73 (95% CI: ‐1.46 to ‐0.00), treatment advantage 11% FUNCTION NDI ‐ Brazilian/Portuguese version Baseline Mean: PT+Acup 24.0, Acup 30.0, PT 28.0 Reported Results: The DMCT (Dunn's Multiple Comparison test) showed that G1 was superior to G3 in reducing functional disability (P < 0.0001) SMD (PT + Acup vs Acup) at IT follow‐up: ‐0.95 (95% CI: ‐1.70 to ‐0.20), NNTB13, treatment advantage 13%. REASONS FOR DROP‐OUTS: Reported (3 drop‐outs, 1 in each group) SIDE EFFECTS: Reported; no record of serious complication of acupuncture or physiotherapy occurred during treatments or during the follow‐up period after any of the treatments that could harm the patients during the assessment all stages of the trial COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | |
| Allocation concealment (selection bias) | Low risk | |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Not possible due to study design |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible due to study design |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Not possible due to study design |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | 1 per group |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | No ITT performed |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Similarity of baseline characteristics? | High risk | VAS scores were significantly different between groups |
| Co‐interventions avoided or similar? | Unclear risk | Not clear |
| Compliance acceptable? | Unclear risk | Not clear |
| Timing outcome assessments similar? | Low risk | 10 weeks and 6 months |
Hall 2007.
| Methods | Type of Trial: RCT Number Analyzed/Randomized: 32/32 Intention‐to‐treat Analysis: NR Power Analysis: NR | |
| Participants | (sub)acute Cervicogenic headache (CGH) Radicular symptoms/signs: NS Setting: Physiotherapy Private Practice Country: USA, Canada | |
| Interventions |
INDEX TREATMENT
Arm 1‐ C1‐2 self SNAG (SSng): Activity‐Belt was used as per Mulligans detailed techniques. Mode‐ The participant was instructed by the PT on the proper positioning and technique of mobilization belt on 3 trials to familiarize themselves. The participant was instructed to perform technique without producing pain. Movement‐ (supplemental video available on line) Treatment schedule: 1 day COMPARISON TREATMENT Arm 2‐ Control group (Mock): Sham mobilizations with same belt. This group did not receive instruction to rotate head towards restriction. Treatment Schedule: 1 day Duration of Follow‐up: 4 weeks and 12 months CO‐INTERVENTION: Not avoided |
|
| Outcomes |
PAIN Headache intensity change score (VAS), 0 to 100 Baseline Mean: SSng 52 Mock 51 Reported Results: group difference in patient‐rated pain favours the SSng exercise group SMD(SSng vs Mock) at ST follow‐up: ‐1.58 (95% CI: ‐2.38 to ‐0.77); power 100%, NNTB 2, Treatment advantage 40% SMD(SSng vs Mock) at LT follow‐up: ‐1.74 (95% CI:‐2.57 to ‐0.91);power 100%, NNTB 3, treatment advantage 40% REASONS FOR DROP‐OUTS: N/A SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Participans were allocated to treatment group using lottery ticket randomization chosen from a concealed container. |
| Allocation concealment (selection bias) | High risk | |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | Low risk | |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible due to study design |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Low risk | |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | No drop‐outs |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Similarity of baseline characteristics? | Low risk | No significant differences were detected between the 2 groups in terms of age, headache history, FRT range, and headache severity index score. Gender distribution was similar. See Table 2 |
| Co‐interventions avoided or similar? | High risk | Not addressed |
| Compliance acceptable? | Low risk | Compliance investigated |
| Timing outcome assessments similar? | Low risk | 4 weeks postintervention and 12 months postintervention |
Hallman 2011.
| Methods | Type of Trial: RCT Number Analyzed/Randomized: 23/24 Intention‐to‐treat Analysis: Not calculated Power Analysis: Not calculated | |
| Participants | Stress‐related chronic neck‐shoulder pain Radicular signs/symptoms: NR Setting: NR Country: Sweden | |
| Interventions |
INDEX TREATMENT Arm 1‐ Practice paced breathing: Activity‐ breathing exercises;Mode‐ resonance heart rate variability (HRV) biofeedback (BF) training and paced breathing; Movement‐ respiration.Dosage‐ Type of contraction (concentric diaphragm concentrically contracts with this breathing exercise), intensity (low as was breathing exercises), On‐site sessions: speed (Sessions 1 and 10: between 4.5 to 6.5 breaths per minute to determine speed with highest HRV. Sessions 2 to 9: performed at speed of highest HRV.), duration (Sessions 1 and 10: 2‐minutes of paced breathing for 2‐minutes of free, non‐paced breathing. Sessions 2 to 9: 4 times 5‐minutes of resonant HRV BF with 2‐minutes breaks), frequency (1time/week), environment in which exercise is performed (morning or afternoon is standardized in a comfortable semi‐reclined chair semi‐reclined, 23 Celsius, dim light, relaxing atmosphere), feedback (psychologist weekly session). Home exercise‐program: at least 15‐minutes of paced breathing with watch or easy air pacer software, 5 times/week Treatment schedule: 10 weeks COMPARISON TREATMENT Arm 2‐ Control Group: This group took part in the breathing protocol in sessions 1 and 10, without any prescribed treatment in between. Treatment schedule: week 1 and 10 Duration of Follow‐up: Directly after 10 weeks CO‐INTERVENTION: Not specified |
|
| Outcomes |
PAIN Borg Scale, 0 to 10 Baseline Mean : Treatment 2.6, Control 2.5 Reported Results: no significant difference between groups SMD (treatment vs control): ‐0.19 (95% CI: ‐1.01 to 0.63) FUNCTION NDI, 0 to 100 Baseline Mean: Treatment 21.3, Control 25.6 Reported Results: no significant difference between groups SMD (treatment vs control): ‐0.52 (95% CI: ‐1.35 to 0.32) QUALITY OF LIFE SF‐36 (physical function subscale) Baseline mean: Treatment 89.6, Control 77.5 Reported Results: no significant difference between groups SMD (treatment vs control): 0.65 (95% CI: ‐0.19 to 1.49) REASONS FOR DROP‐OUTS: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | Author contacted but no response | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method not described |
| Allocation concealment (selection bias) | Unclear risk | Method not described |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Not possible due to design |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible due to design |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Patient is outcome assessor |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | P.74, right column |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | 1 drop‐out not included in analysis ‐ Table 1 |
| Selective reporting (reporting bias) | Unclear risk | No protocol |
| Similarity of baseline characteristics? | Unclear risk | See Table 2 ‐ differences in physical function, vitality, social function, depression |
| Co‐interventions avoided or similar? | Unclear risk | Not reported |
| Compliance acceptable? | Unclear risk | Not reported |
| Timing outcome assessments similar? | Low risk | Baseline and 10 weeks |
Hansson 2013.
| Methods | Type of Trial: RCT Number Analyzed/Randomized: 29/29 Intention‐to‐treat Analysis: calculated Power Analysis: calculated | |
| Participants | WAD Radicular signs/symptoms: Not specified Setting: Physiotherapy centre Country: Sweden | |
| Interventions |
INDEX TREATMENT Arm 1‐ Vestibular rehabilitation program: Activity‐ circuit training of six balance exercises with warm‐up and recovery phases;Mode‐ static and dynamic balance exercises with neck movements, eyes opened and closed; Movement‐ Warm‐up phase‐ walking around the room and changing direction as well as turning the head from side to side. Exercises in standing, including training of co‐ordination of movements. Circuit training‐ Standing up and sitting down on a chair while turning the head from side to side. Eyes closed if possible. Standing on a trampoline, eyes closed and slightly flexing the knees and turning the head from side to side simultaneously. Standing on a 10 cm foam with eyes closed and turning the head from side to side. Standing on a sport mat, walking on the spot and turning the head from side to side. Eyes closed if possible. Sitting on a ball, feet on foam, eyes closed and bouncing slightly while turning the head from side to side. Walking forward and backward while turning the head from side to side. Recovery phase‐ Soft, relaxing movements. Stretch of the muscles in the upper cervical region. Dosage‐ Warm‐up duration‐ 10‐minutes. Circuit training duration‐ 2‐ minutes per exercise, 2 laps. Recovery phase duration‐ 5‐minutes. Frequency (2 times/week), environment in which exercise is performed (physical therapy centre), feedback (supervised group sessions). Treatment Schedule: 6 weeks, 12 sessions COMPARISON TREATMENT Arm 2‐ Control Group: no intervention Treatment Schedule: 6 weeks Duration of Follow‐up: 6 weeks and 3 months CO‐INTERVENTION: reported and not avoided |
|
| Outcomes |
PAIN VAS, 0 to 100 Baseline Median : Intervention 60, Control 60 Reported Results: no significant difference between groups, SMD (6 weeks vs control) 6 weeks 0.07 (95% CI: ‐0.68 to 0.82); SMD (3 months vs control) ‐0.60 (95% CI: ‐1.35 to 0.15) REASONS FOR DROP‐OUTS: reported SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | We utilized median values (SD) rather than mean scores (SMD) to calculate SMD. | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | p.907 L bottom column: Random number table |
| Allocation concealment (selection bias) | High risk | p. 907 L bottom column: The same independent person also carried out the intervention |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Not possible due to design |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible due to design |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Not possible since pt is outcome assessor for VAS. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | High risk | Drop‐ out rate too high: 17/29 dropped out (figure 1) |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | Table 3‐ 6 weeks control (N = 12) |
| Selective reporting (reporting bias) | Unclear risk | Unable to find registration online (reg. number lu 702‐01) |
| Similarity of baseline characteristics? | Low risk | Table 2 |
| Co‐interventions avoided or similar? | High risk | P907 Lp1 – 5 patients underwent other types of physio during the study |
| Compliance acceptable? | Unclear risk | Not reported |
| Timing outcome assessments similar? | Low risk | p.907 bottom right column: the control group was tested at the same intervals as the intervention group |
Helewa 2007.
| Methods | Type of Trial: RCT Number Analyzed/Randomized: 128/151 Intention‐to‐treat Analysis: Calculated Power Analysis: Calculated: For factorial effects (not differences between treatment groups) and based on a change on the Northwick Park Questionnaire. | |
| Participants | Chronic MND Radicular signs/symptoms: NS Setting: University School of Physical Therapy Country: Canada | |
| Interventions |
INDEX TREATMENT
Arm 1‐ Exercise: Activity‐Standard Pillow + Exercise + Active Control Treatment Group: Standard (regular) pillow is assumed to be used by this group. Mode‐ Exercise including: Posture, Relaxation, Active Movement‐ 1‐Postural correction in sitting, standing or during work and leisure activities emphasizing chin in retracted position with cervical spine elongations not beyond normal curves of cervical spine practised with mirror feedback first, then freely using other prompts to become habitual), 2‐Relaxation Exercise Techniques designed to interrupt cycle of pain and muscle spasm (hold‐relax approach repeated up to 5 times and/or rhythmic stabilization applied manually by the PT and taught to the patient), 3‐Free Active Exercise (following relaxation techniques patients freely move head and neck according to normal patterns of movement, may initially be helped by the physiotherapists, patterns are diagonal and involve head flexion and rotation to the right followed by head extension and rotation to the left, diagonal patterns are then repeated to the contralateral sides), and 4‐ Strengthening Exercises (to strengthen the anterior neck muscles using manual resistance (within the limit of pain) with a combination of isometric and isotonic movements, the principle involving reversing movements of flexion and extension, using the principles of successive induction (Sherrington 1961)). Dosage‐ 13 sessions over 10 weeks, as well as home exercises and Active Control treatment (massage and thermal modality) were administered to this group isometric rehabilitative exercise. Arm 2‐ Neck Support (Pillow): Activity‐ Orthopaedic Pillow(s) + Active Control Treatment Group: Mode‐ Neck Support Pillows Movement‐ could be one of two designs: Shape of Sleep pillow (Manutex Products, Mississauga, ON, Canada) or the Sissel Design AB pillow (Sissel Design AB, Svedala, Sweden). The two types of pillows were randomly assigned equally in each arm. The pillows did not differ in shape but in the firmness of the foam. The pillow use was combined with the Active Control treatment (massage and thermal modality). COMPARISON TREATMENT Arm 3‐ Neck Support and Exercise (Exercise + Pillow): Orthopaedic Pillow(s) + Exercise + Active Control Treatment: Orthopaedic pillows were used and were of two types: Shape of Sleep pillow (Manutex Products, Mississauga, ON, Canada) or the SIssel Design AB pillow (Sissel Design AB, Svedala, Sweden). The two types of pillows were randomly assigned equally in each arm. The pillows did not differ in shape but in the firmness of the foam. Pillow use, plus Exercise plus Active control treatment (massage and thermal modality) were administered in this group. Arm 4‐ Massage Therapy and thermal modality (Control): Standard (regular) Pillow + Active Control Group: The Standard (regular) pillow is assumed to be used by this group. Active Control treatment that included massage and thermal modality, Efflurage type massage for 10 sessions in 10 weeks. Visits were 2 sessions/week for 3 weeks, then 1 visit/week for 3 weeks, then 1 visit in 10th week. Arm 5‐ Thermal modality: 20 minutes of moist heat or ice. Treatment Schedule: 6 weeks (assume that the use of the pillow was constrained to these 6 weeks) Duration of Follow‐up: 6 weeks CO‐INTERVENTION: avoided in trial design |
|
| Outcomes |
PAIN VAS, 0 to 10 Baseline Mean: Exercise 2.9, Pillow 3.6, Exercise + Pillow 2.3, Control 2.5 Reported Results: Not significant at all points SMD (Exercise v Control): SMD ‐0.00 (95% CI: ‐0.52 to 0.52) SMD (Exercise + Pillow v Pillow): SMD ‐0.59 (95% CI: ‐1.09 to ‐0.09); power 50.69% FUNCTION Northwick Park Neck Pain Questionnaire (NPQ), 0 to 100 Baseline Mean: Exercise 32.3, Pillow 35.01, Exercise + Pillow 29.9, Control 27.4 Reported Results: Interaction of pillow and exercises are statistically significant and clinically important SMD (Exercise vs Control): 0.00 (‐0.52 to 0.52); power 100% SMD (Exercise + Pillow vs Pillow): ‐0.61 (‐1.11 to ‐0.12); power 100% QUALITY OF LIFE SF 36, 0 to 100 Baseline Mean: Exercise 42.8, Pillow 41.1, Exercise + Pillow 43.7, Control 43.8 Reported Results: no significant difference between groups SMD (Exercise vs Control): 0.15 (95% CI: ‐0.34 to 0.65); power 100% SMD (Exercise + Pillow vs Pillow): ‐0.46 (95% CI: ‐0.95, to 0.04); power 100% REASON FOR DROP‐OUTS: Reported SIDE EFFECTS: None present COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 2x2 balanced factorial design, balanced treatment‐group allocation was done using randomly selected randomly ordered blocks. |
| Allocation concealment (selection bias) | Low risk | |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Not possible due to study design |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible due to study design |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Not possible due to study design |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Similarity of baseline characteristics? | Low risk | See Table 1 |
| Co‐interventions avoided or similar? | Low risk | Reminder to participants at 12 weeks |
| Compliance acceptable? | Low risk | |
| Timing outcome assessments similar? | Low risk | Post treatment, 6 weeks treatment + 6 weeks follow‐up, 6 weeks treatment + 18 weeks follow‐up, 6 weeks treatment + 46 weeks follow‐up |
Humphreys 2002.
| Methods | Type of trial: RCT Number Analyzed/Randomized: 56/56 Intention‐to‐treat Analysis: Not specified Power Analysis: NR | |
| Participants | Chronic neck pain Radicular Signs/Symptoms: Not specified Setting: Students attending a chiropractic college Country: United Kingdom |
|
| Interventions |
INDEX TREATMENT Arm 1‐ Symptomatic exercise group (SEG): Activity‐ One eye‐head‐neck co‐ordination and one eye‐head‐neck‐upper limb co‐ordination. Mode‐ sitting. Movement‐ Exercise one: participants were required to fix their eyes on a target in front of them and move their head maximally in a slow and carefully controlled movement in one direction while keeping their eyes fixed on the target straight ahead. Exercise two: participants were required to hold up both arms in front of them with their thumb extended upwards and to keep their eyes fixed on one thumb as the ipsilateral arm went through the sequential movements of the left and right rotation, flexion and extension, with the eyes and head followed the movement in a slow and co‐ordinated fashion. Dosage‐ Speed (slow and co‐ordinated movement), Duration/Frequency (4 weeks, 2 times/day), Feedback (one training session given by the author and an instruction sheet), Monitoring (exercise compliance form), Environment (home exercise program). Dose (NR). Treatment Schedule: 4 weeks, 2 daily sessions. COMPARISON TREATMENT Arm 2‐ Control group: Symptomatic non‐exercise group (SNEG). Treatment Schedule: 4 weeks Duration of Follow‐up: none CO‐INTERVENTION: NR |
|
| Outcomes |
PAIN VAS, 0 to 100 Baseline Mean: SEG 55, SNEG 49 Reported Results: no significant difference between groups SMD (SEG vs SNEG): 0.00 (95% CI: ‐0.74 to 0.74) REASON FOR DROP‐OUTS: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Not described |
| Allocation concealment (selection bias) | Unclear risk | Not described |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Patient is the assessor |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | p.105, Results: 56/63 |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Unclear risk | Not described |
| Selective reporting (reporting bias) | Unclear risk | No registration or protocol |
| Similarity of baseline characteristics? | Unclear risk | Inadequate information provided |
| Co‐interventions avoided or similar? | Unclear risk | Not described |
| Compliance acceptable? | Low risk | p.107‐108 Exercise Compliance: 95% & 89% compliance per group |
| Timing outcome assessments similar? | Low risk | Baseline, 2 weeks & 4 weeks |
Jull 2002.
| Methods | Type of Trial: RCT Number Analyzed/Randomized: 193/200 Intention‐to‐treat Analysis: calculated Power Analysis: NR | |
| Participants | Chronic CGH Radicular signs/symptoms: NR Setting: Multiple trial centres Country: Australia |
|
| Interventions |
INDEX TREATMENT
Arm 1‐ Exercise Therapy (CCF/ISO) Activity‐ therapeutic low load exercise to cervical‐scapular region Mode‐ craniocervical flexor training with pressure biofeedback, scapular muscle training, postural correction, Movement‐ exercise performed throughout the day, isometric strengthening with co‐contraction of neck flexion and extension, stretching as needed. Treatment Schedule: 30‐minute session duration, 2 sessions/weeks, 8 to 12 sessions total Arm 2‐ Combined Therapy (MT/ET): Activity‐ manipulation, mobilization & exercise Treatment Schedule: 30‐minute session duration, two sessions/weeks, 8 to 12 sessions total COMPARISON TREATMENT Arm 3‐ Manipulative Therapy (SMT): manipulation: high velocity, low‐amplitude manipulation described by Maitland; mobilization (low velocity), 30‐minute session duration. Dosage: 2 sessions/week, 8 to 12 sessions total Arm 4‐ Control Group (NT): no treatment Treatment Schedule: 6 weeks, 8 to 12 sessions Duration of Follow‐up: 52 weeks CO‐INTERVENTION: NR |
|
| Outcomes |
PAIN Headache intensity change score (VAS), 0 to 10 Baseline Mean: SMT 4.8, CCF 5.4, MT/ET 5.1, NT 5.3 Reported Results: significant favouring SMT and CCF SMD (CCF v NT) at LT follow‐up:‐0.59 (95% CI:‐1.00 to ‐0.18), NNTB 6, treatment advantage 28% FUNCTION Northwick Park Neck Pain Questionnaire (NPQ) change score, 0 to 36 Baseline Mean: SMT 27.5, CCF 29.6, MT/ET 29.7, NT 30.7 Reported Results: significant favouring MT or MT/ET over control; no significant difference between MT, ET and MT/ET comparisons SMD (CCF vs NT) at LT follow‐up:‐0.59 (95% CI:‐1.00 to ‐0.18), NNTB 6, treatment advantage 32% GLOBAL PERCEIVED EFFECT Participant perceived effect (VAS 0 to 100) Reported Results: significant favouring SMT and MT/ET over NT, not significant for SMT or MT/ET when compared to CCF SMD (CCF vs NT):‐2.51 (95% CI:‐3.05 to ‐1.97) REASONS FOR DROP‐OUTS: reported SIDE EFFECT: minor and temporary, 6.7% of headaches were provoked by treatment COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | 2x2 factorial design, randomized permuted block design was used with stratification for length of headache history and city of residence |
| Allocation concealment (selection bias) | Low risk | An independent body implemented randomization by telephone contact with each trial centre |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Not possible due to study design |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible due to study design |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | Low risk | |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | ITT analysis performed |
| Selective reporting (reporting bias) | Unclear risk | No protocol provided |
| Similarity of baseline characteristics? | Low risk | Baseline characteristics across the four treatment groups were similar (See Table 1). The only exception was the distribution of females across treatment groups, subsequently included as a covariate in the analysis |
| Co‐interventions avoided or similar? | High risk | Present |
| Compliance acceptable? | Low risk | Reported |
| Timing outcome assessments similar? | Low risk | 6 weeks treatment + 1 week, 3 months, 6 months and 12 months follow‐up |
Kjellman 2002.
| Methods | Type of Trial: RCT Number Analyzed/Randomized: 70/77 Intention‐to‐treat Analysis: Calculated Power Analysis: NR | |
| Participants | (sub)Acute to Chronic MND with or without radiation Radicular signs/symptoms: Present Setting: Primary care physical therapy and private physical therapy practices Country: Sweden |
|
| Interventions |
INDEX TREATMENT
Arm 1‐ General Exercise (ET): Activity‐stretching, strengthening, Mode‐ neck and shoulder, Movement‐ ROM, active neck endurance and strength exercises, 16 sessions over 2 months Arm 2‐ McKenzie Exercise (McK): Specific McKenzie protocol. Sessions over 2 months. Number not specified COMPARISON TREATMENT Arm 3‐ Sham Ultrasound (SUS): Set at lowest setting for 7 minutes. Applied over the superior portion of the trapezius Treatment Schedule: 4 weeks of treatment Duration of Follow‐up: 6 and 12 months CO‐INTERVENTION: Comparable between index and control groups. |
|
| Outcomes |
PAIN VAS, 0 to 100 Baseline Mean: ET 27.0, McK 19, SUS 21 Reported Results: no significant difference between groups SMD (ET vs SUS) at LT follow‐up: ‐0.19 (95% CI: ‐0.41 to 0.80) SMD (McK vs SUS) at LT follow‐up: 0.04 (95% CI: ‐0.51 to 0.60) FUNCTION NDI, 0 to 50 Baseline Mean: ET 27.0, McK 19, US 21 Reported Results: no significant difference between groups SMD (ET vs SUS) at LT follow‐up: ‐0.19 (95% CI: ‐0.41 to 0.80) SMD (McK vs SUS) at LT follow‐up: 0.04 (95% CI: ‐0.51 to 0.60) REASONS FOR DROP‐OUTS: reported SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization by drawing sealed envelopes out of a box |
| Allocation concealment (selection bias) | High risk | Not reported |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Not possible due to study design |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible due to study design |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Not possible due to study design |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | Drop‐outs noted |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | Not reported |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Similarity of baseline characteristics? | High risk | Reported Table 1; no analysis |
| Co‐interventions avoided or similar? | High risk | Table 5, higher use by control group |
| Compliance acceptable? | Low risk | |
| Timing outcome assessments similar? | Low risk | Post treatment, 8 weeks treatment + 6 months, 8 weeks treatment + 52 weeks follow‐up |
Kuijper 2009.
| Methods | Type of Trial: RCT Number Analyzed/Randomized: 200/205 at 6 weeks, 192/205 at 6‐month follow‐up Intention‐to‐treat Analysis: Calculated; sample size based on 90% power and to detect a 10mm difference in the VAS (primary outcome) for arm pain (not neck pain). Power Analysis: calculated | |
| Participants | Acute NDR Radicular signs/symptoms: Present Setting: Three Hospitals Country: Netherlands | |
| Interventions |
INDEX TREATMENT
Arm 1‐ Physiotherapy Group (PG): Activity‐Therapy was focused on mobilizing and stabilizing the neck and was characterized as "hands off". Mode‐ The sessions were standardized provided by a certified Physiotherapist, the patient was instructed on graded exercise activities to strengthen the superficial and deep muscle of the neck. The patients were also instructed in a home exercise program. Movement‐ Patients were advised to practice the exercises daily and asked to record the duration of their exercise daily. Dosage: 2 times/week for 6 weeks COMPARISON TREATMENT Arm 2‐ Wait and see list Group (WLG): Patients in the control group were advised to continue their daily activities as much as possible. As well they were asked to note in their diaries the parts of the day where they were unable to continue their normal activities. Patients were asked to contact the investigators if they had any questions. Arm 3‐ Collar Group (CG): Semi‐hard collar (Cerviflex S, Bauerfeind and available in 6 sizes), The best size (to fit snugly) was selected for each patient. Patients advised to wear the pillow during the day for 3 weeks. Over the next 3 weeks patients were weaned off the collar. After 6 weeks they were asked to no longer wear the collar. Treatment Schedule: 6 weeks, 12 sessions Duration of Follow‐up: 6 months CO‐INTERVENTION: Comparable between index and control groups. Patients were asked to take paracetamol (usually) either with or without a non‐steriodal antiinflammatory. If necessary opioids were prescribed. |
|
| Outcomes |
PAIN VAS, 0 to100 Baseline Mean: Cervical Collar 57.4, Physiotherapy 61.7, WLG 55.6 Reported Results: At 6 weeks there was a significant decrease in neck pain in the collar group 2.8 mm/week (17 mm in 6 weeks) and 2.4 mm/week in the physiotherapy group (14 mm in 6 weeks), while the control group showed only 0.9 mm reduction in pain over the 6 weeks. After 6 months the pain scores in the two treatment groups did not differ from those of the control patients. SMD (PT vs WLG) at Immediate post treatment: ‐0.47 (95% CI: ‐0.81 to ‐0.12); NNTB 4, treatment advantage 33% FUNCTION NDI, 0 to 100 Baseline Mean: Cervical Collar 41.0, Physiotherapy 45.1, WLG 39.8 Reported Results: The collar group showed a significant difference in rate of improvement compared with the control group, the weekly change in the physiotherapy group was not significantly different from that of the control patients. SMD (PT vs WLC) at immediate post treatment: ‐0.11 (95% CI: ‐0.45 to 0.23) PATIENT SATISFACTION scale 0 to 5 Reported Results: NR RR (PT vs WLC) at immediate post treatment: 0.92 (95% CI: 0.62 to 1.37) REASONS FOR DROP‐OUTS: NR SIDE EFFECT: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | |
| Allocation concealment (selection bias) | Low risk | Sealed envelopes prepared by an employee who had no other involvement with the study. The investigator assigned patients to specific groups. |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Stated within text page 2 |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Stated within text page 2 |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Patient self‐report so not blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | High risk | There were 5 participants who were not available for follow‐up at 6 weeks;similarly there were 13 participants lost to follow‐up at 6 months. Figure one details this. |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | Not all those randomized were included in the analysis ( those without follow‐up data were excluded). However this was a very small number and unlikely to affect the estimates. They undertook a LOCF analysis but did not state an ITT analysis within the report. |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Similarity of baseline characteristics? | High risk | Greater arm pain in the collar group. Also the control group had the smallest evidence for root compression based on MRI . |
| Co‐interventions avoided or similar? | Unclear risk | All groups were allowed to take analgesics and anitinflammatories.All patients received the same information about the natural course of the disease. |
| Compliance acceptable? | Low risk | Compliance was monitored for both collar use and physiotherapy. A total of 6 patients (almost 10%) did not wear the collar at all during the first 3 weeks. |
| Timing outcome assessments similar? | Low risk | 6 weeks of treatment + 6 months and 12 months follow‐up |
Lange 2013.
| Methods | Type of trial: RCT Number Analyzed/Randomized: 55/55 Intention‐to‐treat Analysis: calculated Power Analysis: NR | |
| Participants | Acute to chronic non‐specific neck and shoulder pain Radicular Signs/Symptoms: Not specified Setting: Air force base‐ Fighter Wing Skrydstrup Country: Denmark |
|
| Interventions |
INDEX TREATMENT Arm 1‐ Training group: Activity‐ Patterns and synchronization of muscle recruitment, Strengthening exercises, Endurance exercises Mode‐ Patterns and synchronization ‐Standing supine and gentle rotation stood erect, Strenthening‐the whole spine was held in an anatomic neutral position during pull exercises, shrugs standing erect holding the dumbbells in their hands on both sides and sitting position leaning the upper body 45 degrees forward with a straight back for reverse flies. Endurance‐holding the bodyblade with both hands, and with shoulders 90% flexed and elbows 5% flexed Movement‐ Patterns and synchronization‐3 conditioning exercises focusing on activation of the deep cervical flexors, Strengthening‐Static pull in 8 directions, shrugs, reverse flys, Endurance‐Small shoulder extensions and flexions were performed to make the bodyblade oscillate Dosage‐ Patterns and synchronization‐Type of contraction (concentric), Speed (slow and controlled movement), Duration/Frequency (5 reps, 3x week), Sequence (sequence warm‐up then strengthening then endurance), Feedback (the pilots had access to help from educated trainers at the base and at Tactical Air Command Karup), Strengthening‐Type of contraction (concentric), Intensity (equivalent to 70% to 85% of 1 repetition maximum), Duration/Frequency (8‐15 reps, 3x week), Shrugs and static neck pull were performed during every session and reverse flies were performed every second session), Sequence (after warm‐up), Feedback (the pilots had access to help from educated trainers at the base and at Tactical Air Command Karup), Endurance‐Type of contraction (dynamic), Intensity (equivalent to 70% to 85% of 1 repetition maximum), Speed (as the participants became more accustomed to the bodyblade exercise, they attempted to make it oscillate increasingly more rapidly) Duration/Frequency (up to 60 seconds, performed every second session, 3x week), Sequence (after strengthening), Feedback (the pilots had access to help from educated trainers at the base and at Tactical Air Command Karup). Dosage‐ 3 sessions a week, 20 minutes of training session for 24 weeks COMPARISON TREATMENT Arm 2‐ Control group: No intervention but offered the training after the study. Encouraged to continue their physical activity as usual. Treatment Schedule: 24 weeks Duration of Follow‐up: none CO‐INTERVENTION: comparable between index and control groups |
|
| Outcomes |
PAIN VAS, 0 to 10 Baseline Mean:Training group 1 and control 1.2 Reported Results: no significant difference between groups SMD (training vs control): ‐0.58 (95% CI: ‐1.12 to ‐0.04) REASON FOR DROP‐OUTS: Reported SIDE EFFECTS: Reported COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | P.51, right column, 1st paragraph: method of randomization very unconventional. |
| Allocation concealment (selection bias) | Low risk | p.51, top R column |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Not possible due to design. |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible due to design |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Not possible due to design |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | P53, left column: 1 drop‐out per group |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | P53, left column, paragraph 6 |
| Selective reporting (reporting bias) | Low risk | Consistent with registration |
| Similarity of baseline characteristics? | Low risk | Table 1, Table 3, Table 4 |
| Co‐interventions avoided or similar? | Unclear risk | Not monitored |
| Compliance acceptable? | High risk | P54, right column, Figure 3: 58% compliance |
| Timing outcome assessments similar? | Low risk | Baseline and 24 weeks |
Lundblad 1999.
| Methods | Type of Trial: RCT Number Analyzed/Randomized: 58/97 Intention‐to‐treat Analysis: NR Power Analysis: NR | |
| Participants | Chronic MND Radicular signs/symptoms: NS Setting: Factory Country: Sweden |
|
| Interventions |
INDEX TREATMENT
Arm 1‐ Feldenkrais Intervention (F): Activity‐Education Mode‐ Individualized (functional integration) teacher guides through movement sequences; Group (awareness through movement) verbally guided through exercises for Movement‐ neck‐shoulder complaints, home exercises, frequency (individually 4 times and in group (7 to 8 participants) 12 times; required 50% participation in both segments of program). Dosage‐ 50 minutes per week Arm 2‐ Physiotherapy Intervention (MmPT): Activity‐ Stabilization exercises for low back and pelvis, isolated and relaxed shoulder movements Mode‐ Education use of body emphasizing self‐directed control and responsibility for body, ability to cope with pain, muscle tension, and complaints. Awareness of body posture. Movement‐ Practice work‐related lift and movement techniques. Exercise program of strength, co‐ordination, endurance, flexibility/smoothness and rhythm, Home exercises. Dosage‐ 50 minutes; 2 times/week for 16 weeks in group of 5 to 8 participants; Required 50% participation in the exercises COMPARISON GROUP Arm 3‐ Control Regimen (NT): no treatment Treatment Schedule: 16 weeks, 32 sessions Duration of Follow‐up: 52 weeks CO‐INTERVENTION: NR |
|
| Outcomes |
PAIN VAS, 0 to 10 Baseline Mean: VAS ‐ usually MmPT 1.2, F 1.5, NT 2.0, VAS ‐ worst MmPT 4.1, F 4.4, NT 5.5 Reported Results: no significant differences SMD (PT vs no treatment) at LT follow‐up: ‐0.14 (95% CI: ‐0.80 to 0.51) DISABILITY Work and leisure, 0 to 4; Sick leave, days and % Baseline Mean: Disability ‐ work MmPT 1.3, F 1.2, NT 1.3, Disability ‐ leisure MmPT 0.6, F 0.9, NT 0.6 Sick leave (days) MmPT 12.7, F 12.0, NT 11.5, Sick leave (%) MmPT 6.5, F 5.8, NT 5.9 Reported Results: no significant differences REASON FOR DROP‐OUTS: Reported SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomization not described |
| Allocation concealment (selection bias) | High risk | Concealment not described |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Not possible due to study design |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible due to study design |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Not possible due to study design |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | High risk | Not reported |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | No ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Similarity of baseline characteristics? | Low risk | Table 3 no significant difference |
| Co‐interventions avoided or similar? | Low risk | Avoided in trial design |
| Compliance acceptable? | Low risk | |
| Timing outcome assessments similar? | Low risk | 16 weeks of treatment + 6 weeks follow‐up |
Martel 2011.
| Methods | Type of Trial: RCT Number Analyzed/Randomized: 64/69 Intention‐to‐treat Analysis: Calculated Power Analysis: NR | |
| Participants | Chronic MND with or without referral/radiation to the head, trunk or limbs Radicular signs/symptoms: Present Setting: Chiropractic Clinic and Human Research Laboratory of the Department of Chiropractice at the Universite du Quebec Country: Canada |
|
| Interventions |
INDEX TREATMENT
Arm 1‐ SMT Group: Activity‐ Spinal Manipulation Mode‐ Maximum 4 spinal manipulations Movement‐ cervical and upper thoracic areas. Dosage‐ One treatment per month, lasted 10 to 15 minutes Arm 2‐ SMT + Exercise Group:Activity‐ Spinal Manipulation + Home Exercise Program, range of motion, stretching, strengthening Mode‐ Maximum 4 spinal manipulations. Advised to perform a home exercise program Movement‐ manipulation‐ cervical and upper thoracic areas (down to T4). home exercise program‐ range of motion exercises, followed by 4 stretching/ mobilization, and 4 strengthening exercises (concentric and isometric contractions) of the cervical and upper thoracic spine (primarily flexion, extension, lateral flexion and rotation of the cervical spine). Dosage‐ manipulation‐ one treatment per month, lasted 10 to15 minutes. Home exercise program 3x/week. Three series of each exercises with a 30 to 60 second rest between series were performed during each training session. A training session lasted 20 to 30 minutes All participants were instructed in the same routine, exercise volume was tailored to each participant's strength, flexibility and ability to complete the routine with minimal neck pain. Each patient received a written copy of the program. Exercise checked every 2 months by a kinesiologist. COMPARISON TREATMENT Arm 3‐ Control Group: Attention‐control, No treatment, attended clinic once every 2 months, visited lasted 20 to 30 minutes for data collection. Treatment Schedule: 10 months, 10 sessions Duration of Follow‐up: none CO‐INTERVENTION: NR |
|
| Outcomes |
PAIN VAS, 0 to 10 Baseline Mean: SMT 3.1, SMT + Ex 3.8 Reported Results: no significant differences FUNCTION NDI, 0 to 50 Baseline Mean: SMT 21.4, SMT + Ex 22.2 Reported Results: no significant differences HEALTH‐RELATED QUALITY OF LIFE SF‐12, 0 to 100 Baseline Mean Physical Scale: SMT 48.7, SMT + Ex 50.0, Mental Scale: SMT 45.3, SMT + Ex 44.8 Reported Results: no significant differences REASON FOR DROP‐OUTS: Reported SIDE EFFECTS: Reported: No serious adverse events were reported during RCT COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | |
| Allocation concealment (selection bias) | Low risk | Sealed, opaque envelopes |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Not possible due to study design |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible due to study design |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Not possible due to study design |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | No ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Similarity of baseline characteristics? | Low risk | Table 1 |
| Co‐interventions avoided or similar? | High risk | |
| Compliance acceptable? | High risk | Not Reported |
| Timing outcome assessments similar? | Low risk | 10 months of treatment |
Rendant 2011.
| Methods | Type of Trial: RCT Number Analyzed/Randomized: 113/122 Intention‐to‐treat Analysis: calculated Power Analysis: calculated | |
| Participants | Chronic MND Radicular signs/symptoms: NS Setting: Community Country: Germany |
|
| Interventions |
INDEX TREATMENT
Arm 1‐ Qigong: Activity‐12 neck exercises, 9 shoulder exercises Mode/Movement‐ ROM/mobility, imagery, breathing and moving exercise (Figure 1) home exercise with a manual; Qigong qualified teacher was certified by German Qigong Society Dosage‐18 sessions, 90 minute sessions over 6 months Arm 2‐ Exercise: Activity‐ ROM, stretching, strengthening Mode/Movement‐ Warm‐up included neck ROM, use of soft ball, strengthening using a theraband; flexibility exercise, home exercise with a manual, individual pain level was not exceeded;Dosage‐ 18 sessions over 6 months; exercise is monitored by a qualified physiotherapist COMPARISON TREATMENT Arm 3‐ Control: no intervention Treatment Schedule: 24 weeks treatment, 18 sessions Duration Follow‐up: none CO‐INTERVENTION: not avoided |
|
| Outcomes |
PAIN VAS, 0 to 100 Baseline Mean: Qigong 57.7, E 57.5, NT 53.4 Reported Results: significant differences Qigong vs no treatment; MD (Qigong vs no treatment) at 12 weeks treatment: ‐15.60 (‐24.72 to ‐6.48) MD (Qigong vs no treatment) at 24 weeks treatment: ‐8.10 (‐15.72 to ‐0.48) MD (Exercise vs no treatment) at 12 weeks treatment:‐17.30 (95%CI: ‐26.60 to ‐8.00) MD (Exercise vs no treatment) at 24 weeks treatment:‐10.30 (95%CI: ‐19.97 to ‐0.63) No significant difference Qigong vs exercise FUNCTION NPDI, 0 to 100 Baseline Mean: Qigong 44.0, E 39.5, NT 43.2 Reported Results: significant differences Qigong vs no treatment; SMD (Qigong vs no treatment) at 12 weeks treatment: ‐0.48 (95%CI: ‐0.92 to ‐0.04) SMD (Qigong vs no treatment) at 24 weeks treatment: ‐0.47 (95%CI: ‐0.92 to ‐0.02) SMD (Exercise vs no treatment) at 12 weeks treatment: ‐0.78 (95%CI: ‐1.24 to ‐0.31) SMD (Exercise vs no treatment) at 24 weeks treatment: ‐0.50 (95%CI: ‐0.97 to ‐0.04) No difference Qigong vs exercise QUALITY of LIFE SF 36, physical component Baseline Mean: Qigong 43.1, E 43.7, NT 43.3 Reported Results: significant differences qigong vs no treatment; MD (Qigong vs no treatment) at 12 weeks treatment: ‐3.40 (95% CI: ‐6.97 to 0.17) MD (Qigong vs no treatment) at 24 weeks treatment: ‐3.90 (95%CI: ‐8.07 to 0.27) MD (Exercise vs no treatment) at 12 weeks treatment:‐2.70 (95%CI: ‐6.76 to 1.36) MD (Exercise vs no treatment) at 24 weeks treatment:‐2.00 (95%CI: ‐5.83 to 1.83) No difference qigong vs exercise REASON FOR DROP‐OUTS: detailed SIDE EFFECTS: Reported by 19 patients in qigong group including: muscle soreness (n = 15), myogelosis (n = 12), vertigo (n = 10), other pain (n = 4), headache (n = 3), thirst (n = 1), engorged hands (n = 1), twinge in the neck (n = 1), urinary urgency (n = 1), bursitis of left shoulder (n = 1). Reported by 16 patients muscle soreness (n = 14), myogelosis (n = 11), headaches (n = 5), vertigo (n = 2), change in mood (n = 1), worsening of neck pain (n = 1), worsening of tinnitus (n = 1). COST OF CARE: NR |
|
| Notes | Additional unpublished data received from author * attrition bias may exist as ITT analysis are not presented in this overviews; ITT was performed in the RCT report |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | page 420 |
| Allocation concealment (selection bias) | Low risk | page 420 |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Not possible due to study design |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible due to study design |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | The outcome assessor was the patient (i.e. VAS) therefore not blind to previous answer. |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | Quigong 39/42 – acceptable; exercise 35/39 acceptable ; Wait list 39/41 |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | ITT was stated |
| Selective reporting (reporting bias) | Unclear risk | No study protocol |
| Similarity of baseline characteristics? | Low risk | Table 1, Overall no difference noted between most variables albeit perceived effectiveness has some differences |
| Co‐interventions avoided or similar? | Unclear risk | Not noted |
| Compliance acceptable? | Unclear risk | Not reported |
| Timing outcome assessments similar? | Low risk | Baseline, 3 months and 6 months |
Revel 1994.
| Methods | Type of Trial: RCT Number Analyzed/Randomized: 60/60 Intention‐to‐treat: NA Power analysis: NR | |
| Participants | Chronic MND (osteoarthritic changes 27 of 30) Radicular signs/symptoms: Absent Setting: Outpatient Rheumatology Department Country: France |
|
| Interventions |
INDEX TREATMENT
Arm 1‐ Proprioception Rehabilitation Group (RG) Activity‐ Proprioceptive rehabilitation program: purpose to improve neck proprioception; Mode‐ 15 minute individualized exercise session, exercises were mainly concerned with eye‐neck co‐ordination including; Movement‐ a) slow passive motions of the head with gaze on a fixed target, b) active movements of the head, automatic movements of the neck with passive trunk movements and head position relocation exercises, c) exercises in a wide range of motion with free eye‐head coupling (author description well detailed in Rehabilitation Procedure page 896). Dosage‐ 2 times per week; 30 to 40 minute sessions COMPARISON TREATMENT Arm 2‐ Control Group (CG): Medication: analgesic, antiinflammatory typical dosage was indomethacin 100mg; aspirin, 3000 mg; diclofenac, 150 mg; naproxen, 1000 mg Treatment Schedule: 8 weeks Duration of Follow‐up: 2 weeks CO‐INTERVENTION: NR |
|
| Outcomes |
PAIN VAS, 0 to 100 Baseline Mean: RG 50.5, CG 45.9 Reported Results: significant favouring RG SMD at ST follow‐up: ‐0.77 (95% CI: ‐1.29 to ‐0.24), NNTB 4, treatment advantage 34% DAILY INTAKE OF NSAID / ANALGESICS Baseline Mean: RG 2.0/1.8, CG 2.3/1.6 Reported Results: not significant FUNCTIONAL IMPROVEMENT SELF‐ ASSESSED scale 0 to 5 Reported Results: significant favouring RG SMD at ST follow‐up: 0.55 (95% CI: 0.33 to 0.89), NNTB 3, treatment advantage NA REASON FOR DROP‐OUTS: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomization not described |
| Allocation concealment (selection bias) | Low risk | |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | Low risk | |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible due to intervention |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Patient self‐report so not blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | No ITT analysis |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Similarity of baseline characteristics? | High risk | |
| Co‐interventions avoided or similar? | Low risk | |
| Compliance acceptable? | High risk | Not reported |
| Timing outcome assessments similar? | Low risk | 8 weeks of treatment + 10 weeks follow‐up |
Stewart 2007.
| Methods | Type of Trial: RCT Number Analyzed/Randomized: 16/16 Intention‐to‐treat Analysis: NA Power Analysis: NR | |
| Participants | Subacute and Chronic WAD with or without radiation Radicular signs/symptoms: Present Setting: Two physiotherapy clinics Country: Australia | |
| Interventions |
INDEX TREATMENT
Arm 1‐ Exercise and Advice: Activity‐ Exercise, Mode‐ aerobic exercise, stretches, functional activities, activities to build speed, endurance and co‐ordination, trunk and limb strengthening, CBT (setting goals of progressively increasing difficulty, shaping, encouraging self‐monitoring of progress, self‐reinforcement), home exercise program (individual specified), Movement‐ graded exercise program supervised by a physiotherapist, Dosage‐ duration (1 hour of exercise per session), feedback (supervised for 30 minutes) Individualized, progressive, intensity (submaximal program) designed to improve participants ability to complete functional activities specified by the participant as being difficult because of whiplash. Regular evaluation by a physiotherapist. Encouraged to continue home exercises even after intervention was completed. Dosage‐ 6 weeks, 12 sessions COMPARISON TREATMENT Arm 2‐ Advice Alone: Standardised education, reassurance and encouragement to resume light activity alone. One consultation and 2 follow‐up phone contacts. Favorable prognosis of whiplash, addressed common inaccurate beliefs about whiplash, exploration of fear‐avoidance beliefs. Participants given a written report of main points of advice session. Standardized advice reinforced at 2 weeks and 4 weeks Treatment Schedule: 6 weeks, 12 sessions Duration of Follow‐up: 42 weeks CO‐INTERVENTION: avoided in trial design |
|
| Outcomes |
PAIN VAS, 0 to 10 Baseline Mean: Exercise + Advice 5.2, Advice Alone 5.3 Reported Results: Groups were similar at baseline. SMD post: ‐0.46 (95% CI: ‐0.81 to ‐0.12) SMD 12 month: ‐0.12 (95% CI: ‐0.47 to 0.23) FUNCTION NDI, 0 to 50 Baseline Mean: Exercise + Advice 18.2, Advice Alone 19.7 Reported Results: Groups were similar at baseline. SMD post: ‐0.50 (95% CI: ‐0.85 to ‐0.15) SMD 12 month: ‐0.39 (95% CI: ‐0.74 to ‐0.03) GLOBAL PERCEIVED EFFECT scale ‐5 to 5 Baseline Mean: Exercise + Advice 0.6, Advice Alone 0.3 Reported Results: Groups were similar at baseline. SMD post: ‐0.46 (95% CI: ‐0.80 to ‐0.11), SMD 12 month: ‐0.18 (95% CI: ‐0.54 to 0.17) QUALITY OF LIFE SF‐36 Physical, 0 to 100 Baseline Mean: Exercise + Advice 36.4, Advice Alone 36.8 Reported Results: Groups were similar at baseline SMD post: ‐0.35 (95% CI: ‐0.69 to ‐0.01), SMD 12 month: ‐0.15 (95% CI: ‐0.50 to 0.20) REASON FOR DROP‐OUTS: Reported but not specified SIDE EFFECTS: Reported; The main complaint in this group was muscle pain with exercise (3) followed by knee pain (2) and lumbar spine pain (2). COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Randomized method is not described |
| Allocation concealment (selection bias) | Low risk | Reported p 60 |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Not described |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | pg 61, self‐report scales therefore patient is assessor even though author reports scales being administered and scored by staff blind to group assignment |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | Although descriptions of drop‐outs were not given, due to the low number of drop‐outs we feel this is acceptable |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | |
| Selective reporting (reporting bias) | Low risk | pg 61, referenced protocol |
| Similarity of baseline characteristics? | Low risk | Table 1 |
| Co‐interventions avoided or similar? | High risk | Not similar at 12 months |
| Compliance acceptable? | Low risk | Section 3.3 |
| Timing outcome assessments similar? | Low risk | 6 weeks and 12 months |
Takala 1994.
| Methods | Type of Trial: RCT Number Analyzed/Randomized: 44/45 Intention‐to‐treat: NR Power Analysis: NR | |
| Participants | MND, disorder duration NR Radicular signs/symptoms: Absent Setting: Printing Company Country: Finland |
|
| Interventions |
INDEX TREATMENT
Arm 1‐ Exercise treatment (ET): Activity‐ Group gymnastic, instructional type (group), Mode‐ setting (work); treatment characteristics (exercise planned to train whole body), Movement‐ aerobic dynamic exercise (10 minutes walking or stepping), relaxation, stretching of muscles of the trunk and extremities and dynamic exercises (10 minutes), Dosage‐ sequence (10 minutes walking/stepping, 10 minutes stretch/dynamic exercises, 5 minutes walking/stepping, 10 minutes dynamic and co‐ordination exercises, 10 minutes stretch and relaxation); duration of session (45 minutes);1 time/week COMPARISON TREATMENT Arm 2‐ No treatment (NT) Treatment Schedule: 10 weeks, 10 sessions of treatment in the spring session (cross‐over of placebo group occurred in autumn, the groups were reversed) Duration of Follow‐up: none CO‐INTERVENTION: NR |
|
| Outcomes |
PAIN VAS, 0 to 100 Baseline Median: ET 40, NT 50 Reported Results: no significant difference PRESSURE PAIN SENSITIVITY Algometer (pressure pain threshold (PPT) on upper trapezius, levator scapulae, rhomboid, infraspinatus) mean score of 8 measures Baseline Mean: ET 45.2, NT 44.8 Reported Results: no significant difference SMD at immediate post treatment: ‐0.06 (95% CI: ‐0.65 to 0.53) REASON FOR DROP‐OUTS: NR SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | High risk | Matching then random allocation not described |
| Allocation concealment (selection bias) | Low risk | The rater was blinded with respect to the group status (treatment or control) of the participant |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | Low risk | |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Patient self‐report so not blinded |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | High risk | ITT not performed |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Similarity of baseline characteristics? | High risk | |
| Co‐interventions avoided or similar? | Low risk | Similar in all groups |
| Compliance acceptable? | High risk | Not monitored |
| Timing outcome assessments similar? | Low risk | 10 weeks of treatment |
Viljanen 2003.
| Methods | Type of Trial: RCT Number Analyzed/Randomized: 340/393 Intention‐to‐treat Analysis: Calculated Power Analysis: Calculated | |
| Participants | Chronic MND (NDR, NDH, WAD) Radicular signs/symptoms: NR Setting: Office workers Country: USA, Canada | |
| Interventions |
INDEX TREATMENT
Arm 1‐ Exercise: Activity‐ muscle training; Mode‐ activating large muscle groups in neck and shoulders Movement‐ dumbbells with weight of 1 to 3 kg; Dosage‐ Dynamic muscle training, Sequence (stretching followed each exercise); progression in weeks 5 and 9. Arm 2‐ Relax: Activity‐ Relaxation training; Mode/Movement‐ progressive relaxation, autogenic training, functional relaxation, systematic desensitization. COMPARISON TREATMENT Arm 3‐ Control: No treatment Treatment Schedule: 12 weeks plus 1 week reinforcement, Arm 1‐13.6 sessions; Arm 2‐ 14.6 sessions Duration of Follow‐up: 3 and 9 months CO‐INTERVENTION: Comparable between groups |
|
| Outcomes |
PAIN VAS, 0 to 10 Baseline Mean: Exercise 4.8, Relax 4.8, Cntl 4.1 Reported Results: no group difference SMD (Exercise v Cntl): ‐0.04 (95% CI: ‐0.28 to 0.20) FUNCTION NDI, 0 to 50 Baseline Mean: Exercise 29, Relax 2 29, Cntl 26 Reported Results: no significant group differences were found SMD (Exercise vs Cntl): ‐0.11 (95% CI: ‐0.11 to 0.38) REASON FOR DROP‐OUTS: Noted but no difference between groups SIDE EFFECTS: NR COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | Randomization according to a random numbers table |
| Allocation concealment (selection bias) | Low risk | Treatment allocation was concealed in a numbered opaque envelope, which was opened by the physician after baseline measurements had been taken |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Not possible due to study design |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible due to study design |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Not possible due to study design |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | High risk | Reasons for drop‐outs not described |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | |
| Selective reporting (reporting bias) | Unclear risk | No protocol available |
| Similarity of baseline characteristics? | Low risk | |
| Co‐interventions avoided or similar? | Low risk | Comparable between groups |
| Compliance acceptable? | High risk | |
| Timing outcome assessments similar? | Low risk | 12 weeks of treatment + 3 and 9 month follow‐up |
von Trott 2009.
| Methods | Type of Trial: RCT Number Analyzed/Randomized: 93/117 Intention‐to‐treat Analysis: Calculated Power Analysis: Calculated | |
| Participants | Chronic MND in elderly adults Radicular signs/symptoms: NR Setting: Residents of residential homes for elderly people Country: Germany |
|
| Interventions |
INDEX TREATMENT
Arm 1‐ Qigong: Activity‐ Qigong, Mode‐ lessons, Movement‐ started with about 10 minutes of typical Qigong "opening" exercises, continued with up to 4 exercises of Dantian Qigong, and finished with about 10 minutes of "closing" exercises. Dosage‐ Qigong was provided by 5 approved Qigong therapists; 24 sessions (45 minutes) over 3 months (2 sessions/week). Arm 2‐ Exercise: Activity‐ Exercise therapy Mode‐ was based on a standardized program for computer and workplace related neck pain Movement‐ including repeated active cervical rotations, strength and flexibility exercises. A detailed description is provided in Weidmann 2008. Dosage‐ 24 sessions (45 minutes) over 3 months (2 sessions/week). Participants were asked to continue exercising on their own for the next 3 months. COMPARISON TREATMENT Arm 3‐ Wait List Control: Patients were free to treat their neck pain with the treatment or therapies they were using prior to randomization. Patients did not received Qigong or exercise therapy. After 6 months they were offered an intervention of their choice. Treatment Schedule: 12 weeks, 24 sessions Duration of Follow‐up: 12 weeks follow‐up CO‐INTERVENTION: Comparable between index and control groups |
|
| Outcomes |
PAIN VAS, 0 to100 Baseline Mean : Qigong 56.4, Exercise 47.1, Wait List Control 49.9 Reported Results: After 3 months there was not significant difference for the average neck pain between the Qigong and the wait list group ‐11.0 mm (95% CI: ‐24.0 to 2.1; P = 0.99, ANCOVA), and no significant difference between the Qigong and the exercise therapy group the group difference being ‐2.5 mm (95% CI: ‐15.4 to 10.3, P = 0.68). MD (Qigong vs control) at 12 weeks treatment: ‐7.50 (95% CI: ‐21.88 to 6.88) MD (Qigong vs control) at 12 weeks treatment + 12 weeks follow‐up: ‐6.80 (95% CI: ‐21.34 to 7.74) MD (Exercise vs control) at 12 weeks treatment: ‐10.40 (95%CI: ‐23.11 to 2.31) MD (Exercise vs control) at 12 weeks treatment + 12 weeks follow‐up: ‐12.20 (95%CI: ‐25.73 to 1.33) FUNCTION NDI, 0 to100 Baseline Mean: Qigong 38.5, Exercise 41.8, Wait List Control 36.1 Reported Results: No significant difference was found between the groups after 3 and 6 months. SMD (Qigong vs control) at 12 weeks treatment: ‐0.21 (95% CI: ‐0.69 to 0.28) SMD (Qigong vs control) at 12 weeks treatment + 12 weeks follow‐up: ‐0.06 (95% CI:‐0.57 to 0.45) SMD (Exercise vs control) at 12 weeks treatment: ‐0.23 (95%CI: ‐0.70 to 0.24) SMD (Exercise vs control) at 12 weeks treatment + 12 weeks follow‐up: ‐0.29 (95%CI: ‐0.77 to 0.20) GLOBAL PERCEIVED EFFECT SMD (Qigong vs control) at 12 weeks treatment: ‐0.01 (95% CI: ‐0.49 to 0.47) SMD (Qigong vs control) at 12 weeks treatment + 12 weeks follow‐up: ‐0.09 (95% CI: ‐0.60 to 0.42) SMD (Exercise vs control) at 12 weeks treatment: 0.09 (95%CI: ‐0.38 to 0.56) SMD (Exercise vs control) at 12 weeks treatment + 12 weeks follow‐up: ‐0.21 (95% CI: ‐0.69 to 0.28) QUALITY OF LIFE SF‐36 physical component, 0 to 100 Baseline Mean: Qigong 30.4, Exercise 28.7, Wait List Control 30.6 Reported Results: No significant difference was found between the groups after 3 and 6 months. MD (Qigong vs control) at 12 weeks treatment: ‐1.80 (95% CI: ‐5.94 to 2.34) MD (Qigong vs control) at 12 weeks treatment + 12 weeks follow‐up: 0.10 (95% CI: ‐3.99 to 4.19) MD (Exercise vs control) at 12 weeks treatment: ‐1.70 (95%CI: ‐5.96 to 2.56) MD (Exercise vs control) at 12 weeks treatment + 12 weeks follow‐up: 2.20 (95%CI: ‐1.81 to 6.21) REASON FOR DROP‐OUTS: Reported SIDE EFFECTS: Reported; 5 side‐effects were reported by 4 patients in the Qigong group (2 nausea, 2 aching muscles, 1 muscle tension) and 4 side effects by 2 patients in the exercise therapy group (2 muscle tensions, 1 acing muscles, 1 nausea) COST OF CARE: NR |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Low risk | |
| Allocation concealment (selection bias) | Low risk | |
| Blinding (performance bias and detection bias) All outcomes ‐ patients? | High risk | Perceptibly different interventions between groups |
| Blinding (performance bias and detection bias) All outcomes ‐ providers? | High risk | Not possible due to intervention |
| Blinding (performance bias and detection bias) All outcomes ‐ outcome assessors? | High risk | Patient is assessor |
| Incomplete outcome data (attrition bias) All outcomes ‐ drop‐outs? | Low risk | |
| Incomplete outcome data (attrition bias) All outcomes ‐ ITT analysis? | Low risk | |
| Selective reporting (reporting bias) | Low risk | Wiedmann 2008 |
| Similarity of baseline characteristics? | Low risk | Table 1 |
| Co‐interventions avoided or similar? | Unclear risk | Unclear about the wait list group |
| Compliance acceptable? | Unclear risk | Compliance of home based exercises was not measured |
| Timing outcome assessments similar? | Low risk | 3 months, 6 months |
1.0 Definitions of terms 1.1 duration of disorder:
Acute = <30 days (1 month, 4 weeks) Subacute = 30 days (1 month, 4 weeks) to 90 days (3 months, 12 weeks) Chronic = > 90 days (3 months, 12 weeks)
1.2 duration of follow‐up
immediate post (IP) treatment ≤ one day short‐term (ST) follow‐up = one day to three months intermediate‐term (IT) follow‐up = three months up to, but not including, one year long‐term (LT) follow‐up = one year or longer
2.0 Short forms commonly used in text and tables: 2.1 Clinical terms CBT = Cognitive Behavioral Therapy CCF = Craniocervical Flexion CGH = Cervicogenic ED = Education ET = Exercise Therapy F = Feldenkrais GFT = General Fitness Training IR = Infrared Radiation ISO = Isometric Neck Exercise ISOSh = Isometric Shoulder Exercise ISOShEn = Isometric Shoulder Endurance ISOShST = Isometric Shoulder Strength McK = McKenzie MmPT = Multimodal Phyical Therapy MND = mechanical neck disorders Mock = Mock therapy MT = manual therapy NDR = neck disorders with radicular findings NoEG = No Exercise Group NeuT = Neural Mobilizations NT = No treatment Pil = Pillow REL = Relaxation ROM = range of motion SFT = Specific Strength Training SMP = Self Management Prog SMT = Manipulation SMT/ET = Manipulation and exercise SpvT = supervised training of CSP/Scap SSng =Self Snag StEx = Standard exercise SUS = Sham Ultra Sound TENS = transcutaneous electrical nerve stimulation US = ultrasound WAD = whiplash‐associated disorders
2.2 Outcome measures WHYMPI = West Haven‐Yale Multidimensional Pain Inventory [sub scale pain severity] SF‐36 = short‐form 36 [short‐form with 36 questions yielding an 8‐scale health profile] NDI = neck disability index VAS = visual analogue scale NRS‐101 = numeric rating scale 101 [0 to 100 point scale] PPT = pain pressure threshold [measured by algometer] BORG = Borg pain scale MNQ = Modified Nordic Pain Questionnaire NPS = Numeric Pain Scale NPQ = Northwick Park Questionnaire DASH = Disability of the Arm, Shoulder and Hand WAI = Work Ability Index NPDI = Neck Pain Driving Index SF‐36 = Short Form 36 SF‐12 = Short Form 12
2.3 Other vs = versus w = weeks m = months y = years CI = Confidence Interval ITT = Intention‐To‐Treat NA = Not Applicable NR = Not Reported NNTB = Number‐Needed‐to‐Treat‐to‐Benefit RCT = Randomized Controlled Trial Q‐RCT ‐ Quasi‐randomized Controlled Trial RR = Risk Ratio SD = Standard Deviation SMD = Standardized Mean Difference
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Acar 2012 | Intervention: exercise in all arms. |
| Ahlgren 2001 | Intervention: exercise in all arms. |
| Allison 2002 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Andersen 2008a | Comparison: Comparison group received equal attention by forming groups which should improve workplace ergonomics, stress management, etc. |
| Andersen 2010 | Comparison: Comparison group received equal attention by forming groups which should improve workplace ergonomics, stress management, etc. |
| Arami 2012 | Intervention: exercise in all arms. |
| Ardic 2002 | Intervention: exercise in all arms. |
| Bernaards 2007 | Intervention: Multimodal including exercise and cognitive behavioral training (companion paper to Bernaards 2008 and Bernaards 2012. |
| Bernaards 2008 | Intervention: Multimodal including cognitive behavioral training (companion paper to Bernaards 2007 and Bernaards 2012). |
| Bernaards 2012 | Intervention: Multimodal including exercise and cognitive behavioral training (companion to Bernaards 2007 and Bernaards 2008). |
| Bissett 1985 | Intervention: EMG biofeedback mediated muscle relaxation not active exercise. |
| Blangsted 2008 | Comparison: Comparison group received equal attention by forming groups which should improve workplace etc (companion paper to Andersen 2008). |
| Bonk 2000 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Bosmans 2011 | Intervention: Multimodal approach with intervention groups without ability to differentiate each treatment techniques contribution. |
| Boyce 2012 | Population: cervical dystonia. |
| Brewerton 1966 | Intervention: Instruction on posture is not considered an exercise. There was no exercise group outside "instruction on posture". |
| Brodin 1985 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Bronfort 2012 | Comparison: No control group. |
| Burketorp 2006 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Carlsson 1990 | Population: Chronic tension headache (either occipital, temporal and/or frontal). |
| Cleland 2010 | Intervention: Both treatment and control received same exercise intervention. |
| Cramer 2013 | Intervention: exercise in all arms, no control group. |
| Cunha 2008 | Intervention: Multimodal ‐ manual therapy and exercise. |
| Cuzdan 2013 | Intervention: exercise in all arms. |
| Dusunceli 2009 | Intervention: Multimodal ‐ exercise and PT agents. |
| Ehrenborg 2010 | Intevention: exercise in all arms. |
| Escortell‐Mayor 2008 | Intervention: Both treatment and control received same exercise intervention. |
| Escortell‐Mayor 2011 | Intevention: Both treatment and control received same exercise intervention. |
| Evans 2002 | Intervention: manual therapy, medication and education. |
| Falla 2006 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Fitz‐Ritson 1995 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Foley‐Nolan 1992 | Intervention: Not exercise. |
| Friedrich 1996 | Intervention: Education comparison, exercise is the same in all 3 groups. |
| Gam 1998 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Giebel 1997 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Goldie 1970 | Design: Q‐RCT |
| Gustavsson 2006 | Intervention: The control treatment was individualized care (acupuncture, massage, mobs, hot pack, TENS, US, exercise) and we were not able to elucidate the exact treatment mix for the treat as usual group. |
| Guzel 2006 | Intervention: Both groups received the same exercise intervention. |
| Hagberg 2000 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Hamberg‐van Reenen 2009 | Population: Convenience sample of 22 healthy workers. |
| Hansson 2006 | Population: dizziness not neck pain as main complain. |
| Hanten 1997 | Outcome Measures: Did not use any of the identified outcome measures (only pain pressure threshold as a proxy for pain). |
| Hanten 2000 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Henning 1997 | Population: Preventional trial, although participants rated neck and shoulder discomfort this subpopulation was never identified, nor was discomfort ratings in neck and shoulders reported. |
| Hoving 2002 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Hoving 2006 | Intervention: manual therapy versus exercise versus continued care (medication and education). |
| Huber 2013 | Intervention: exercise in all arms, no control group. |
| Hudson 2010 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Hurwitz 2002 | Intervention: No active exercise. |
| Hurwitz 2005 | Intervention: Exercise was same in all groups. |
| Häkkinen 2008 | Intervention: exercise in all arms. |
| Jay 2013 | Outcome: no patient important outcome. |
| Jensen 2001 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Jensen 2005 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Jordan 1998 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Jull 2007 JOR | Intervention: All groups received exercise. |
| Jull 2007 Pain | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Jull 2009 | Intervention: All groups received exercise. |
| Jull 2013 | Intervention: multimodal therapy versus usual care. |
| Kamwendo 1991 | Intervention: Exercises not specified. |
| Karlberg 1996 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Karlsson 2011 | Comparison: comparison was another active exercise treatment. |
| Kietrys 2007 | Comparison: Comparison was activities. |
| Koes 1991 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Kogstad 1978 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Lamb 2013 | Intervention: multimodal treatment. |
| Lansinger 2007 | Intevention: Both treatment and control received same exercise intervention. |
| Lansinger 2013 | Intervention: one exercise vs another exercise type. |
| Lee 2013 | Intervention: Exercise within a multimodal care approach specifically MT + Ex + PT vs that same PT. |
| Levoska 1993 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Linton 2001a | Intervention: Unable to separate exercise group within treatment as usual comparison group. |
| Lluch 2014 | Comparison: mobilization versus exercise. |
| Ma 2011 | Intervention: No control group, comparison group received education. |
| Madson 2010 | Intevention: Both treatment and control received same exercise intervention. |
| Maiers 2013 | Intervention: exercise in all arms. |
| Manca 2006 | Intervention: Exercise prescription was not a significant component of the study (less than 10%). |
| Marangoni 2010 | Population: less than 80% of the population have neck pain (72%). |
| McKinney 1989 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Mealy 1986 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Michalsen 2012 | Comparison: exercise in all arms. |
| Moffet 2006 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Mongini 2012 | Population: all types of headaches included. |
| Murphy 2010 | Intervention: Both treatment and control received same exercise intervention. |
| Nielsen 2010 | Outcome: no patient important outcome. |
| Nordemar 1981 | Intervention: Passive exercise. |
| O'Leary 2007 | Outcome Measures: The reported outcomes are not outcomes of interest to this review. |
| O'Leary 2007 JoPain | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Pato 2010 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Pedersen 2013 | Study design: prospective observational study. |
| Pennie 1990 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Persson 1994 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Pool 2006 | Intervention: Protocol only, multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution (Ex+graded activity+MT). |
| Provinciali 1996 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Ragonese 2009 | Comparison: Exercise vs. Manual Therapy. |
| Randlov 1998 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Rosenfeld 2000 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Rosenfeld 2003 | Intervention: Both groups received exercise. |
| Rundcrantz 1991 | Design: This was a quasi‐RCT, treatment was individualized and unable to specify exercise. |
| Ryan 2001 | Intervention: Both groups received exercise (strength vs endurance). |
| Salmon 2013 | Population: participants did not have neck pain prior to start of trial. |
| Schnabel 2004 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Scholten‐Peeters 2006 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Sharan 2011 | Intervention: multimodal treatment in all arms. |
| Skargren 1997 | Intervention: Unable to separate data for exercise group (unclear if McKenzie treatment mobilization or exercise). |
| Skillgate 2007 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Skoglund 2011 | Outcome: no baseline data. |
| Soderlund 2000 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Soderlund 2001 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Song 2012 Abstract | Outcome/Publication: Insufficient information. Further data were sought but not found. No full publication could be source. |
| Taimela 2000 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Telci 2012 | Intervention: Multimodal treatment with exercise VS multimodal treatment VS medicines. |
| Tsauo 2004 | Population: Prevention trial, between than 14.3 ‐58.5 % of participants had neck pain at baseline. |
| van den Heuvel 2003 | Population: Prevention trial, greater proportion of participants non‐symptomatic in past week at baseline. |
| van Ettekoven 2006 | Population: The primary diagnosis was tension type headaches. |
| Vasseljen 1995 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Vikne 2007 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Voerman 2007 | Intervention: Relaxation therapy using myofeedback versus ergonomic intervention, no active component. |
| von Piekartz 2011 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Waling 2002 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Wani 2013 | Comparison: exercise in all arms. |
| Wei 2007 | Outcome Measure: not our primary outcomes of interest in this review. |
| Yang 2013 | Intervention: multimodal treatment compared with acupuncture. |
| Ylinen 2003 | Comparison: Control group included exercise. |
| Ylinen 2006b | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Ylinen 2007b | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Ylinen 2010 | Intervention: Both treatment and control received same exercise intervention. |
| Yogitha 2012 | Intervention: Yoga but deep relaxation only. |
| Youseff 2013 | Intervention: mobs + exercises vs massage + exercises. |
| Zaproudina 2007 | Intervention: Multimodal approach within intervention groups without ability to differentiate each treatment techniques contribution. |
| Zebis 2011 | Population: Is for the greater part a prevention trial (2/3 of N without neck pain). |
EMG: electromyography Ex: exercise therapy MT: manual therapy PT: physiotherapy RCT: randomized controlled trial TENS: transcutaneous electrical nerve stimulation US: ultrasound
Characteristics of studies awaiting assessment [ordered by year of study]
Falla 2013.
| Methods | RCT |
| Participants | Chronic neck pain |
| Interventions | 8‐week exercise program |
| Outcomes | NDI, pain, EMG |
| Notes | Awaiting data extraction |
EMG: electromyographic NDI: neck disability index RCT: randomized controlled trial
Characteristics of ongoing studies [ordered by study ID]
Andersen 2010a (Protocol).
| Trial name or title | Protocol for work place adjusted intelligent physical exercise reducing musculoskeletal pain in shoulder and neck (VIMS): a cluster randomized controlled trial |
| Methods | |
| Participants | |
| Interventions | Specific strength training with supervision vs specific strength training with minimal supervision vs reference groups without training |
| Outcomes | Pain |
| Starting date | |
| Contact information | National Research Centre for the Working Environment, Copenhagen O, Denmark |
| Notes |
Andersen 2011a (Protocol).
| Trial name or title | Protocol for shoulder function training reducing musculoskeletal pain in shoulder and neck: A randomized controlled trial |
| Methods | |
| Participants | Neck pain |
| Interventions | Shoulder function training with supervision vs reference group receiving advice to stay physically active |
| Outcomes | Pain intensity, strength, work disability |
| Starting date | |
| Contact information | National Research Centre for the Working Environment, Copenhagen O, Denmark |
| Notes | Protocol |
Guerriero 1997.
| Trial name or title | Comparative effects of manipulation and physical therapy on motion in the cervical spine |
| Methods | |
| Participants | Chronic neck pain |
| Interventions | Cervical spine manipulation vs sham treatment vs cervical spine manipulation, ischaemic compression of myofascial trigger points, PNF, interferential therapy |
| Outcomes | Cervical ROM |
| Starting date | |
| Contact information | Palmer Institute of Graduate Studies and Research, Davenport, Iowa. |
| Notes |
Gurumoorthy 2000.
| Trial name or title | A prospective study of acute whiplash injury and its clinical management |
| Methods | |
| Participants | Acute neck injury (WAD) |
| Interventions | Early immobilization vs early active mobilization |
| Outcomes | Pain, cervical ROM, neck muscle strength, time to return to normal duties |
| Starting date | |
| Contact information | Curtin University of Technology, Perth, Australia |
| Notes |
Hansen 2011 (Protocol).
| Trial name or title | Neck exercises, physical and cognitive behavioral‐graded activity as a treatment for adult whiplash patients with chronic neck pain: Design of a randomized controlled trial |
| Methods | |
| Participants | Chronic neck pain (WAD) |
| Interventions | Pain management (control) group vs combined pain management and training (intervention) group |
| Outcomes | Pain, function, disability, quality of life |
| Starting date | |
| Contact information | Research Unit for Musculoskeletal Function and Physiotherapy, Institute of Sports Science and Clinical Biomechanics, University of Southern Denmark, Odense M, Denmark |
| Notes |
Michaleff 2009 (Protocol).
| Trial name or title | A randomized clinical trial of a comprehensive exercise program for chronic whiplash: trial protocol |
| Methods | |
| Participants | Chronic neck pain (WAD I & II) |
| Interventions | Education Booklet + Comprehensive Exercise Program vs Education Booklet + Advice |
| Outcomes | Pain intensity, disability, health‐related quality of life and health service utilization |
| Starting date | |
| Contact information | The George Institute for International Health, The University of Sydney, George Street, Sydney, 2000, Australia |
| Notes |
Reginiussen 2000.
| Trial name or title | Efficiency of manual therapy on patients with cervicogenic headache. A randomized single‐blinded controlled trial |
| Methods | |
| Participants | Cervicogenic headache |
| Interventions | Manual therapy (soft tissue methods, stretching/massage, mobilizing and thrust techniques) vs standardized physiotherapy treatment consisting of SWD, exercises and stretching |
| Outcomes | Headache, neck pain, function, use of drugs, patient satisfaction |
| Starting date | |
| Contact information | Institut of Manual Therapy, Alta, Norway |
| Notes |
Stokke 1995.
| Trial name or title | A randomized comparison of chiropractic and physiotherapy treatment for neck pain of functional (mechanical) origins. A controlled clinical trial |
| Methods | |
| Participants | Neck pain, neck and head pain, neck and shoulder pain |
| Interventions | Chiropractic spinal manipulation vs physiotherapy vs medication |
| Outcomes | NDI, pain intensity VAS |
| Starting date | |
| Contact information | Institute of Community Medicine, School of Medicine, Uniersity of Tramso, 9037 Tromso, Norway. |
| Notes |
Williamson 2009 (Protocol.
| Trial name or title | Development and delivery of a physiotherapy intervention for the early management of whiplash injuries: The Managing Injuries of Neck Trial (MINT) Intervention |
| Methods | |
| Participants | WAD I, II, & III |
| Interventions | Manual therapy, exercise, and psychological strategies and self‐management advice |
| Outcomes | |
| Starting date | |
| Contact information | Clinical Trials Unit, Medical School Building, Gibbet Hill Campus, University of Warwick, Coventry CV4 7AL, UK |
| Notes |
NDI: neck disability index PNF: Proprioceptive neuromuscular facilitation ROM: range of motion SWD: short‐wave diathermy vs: versus VAS: visual analogue scale WAD: whiplash associated disorders
Contributions of authors
This is one review of a series conducted by the Cervical Overview Group: Gross A, Goldsmith C, Graham N, Santaguida PL, Burnie S, Miller J, Peloso P, Kay T, Kroeling P, Trinh K, Langevin P, Santaguida PL, Patel K, Haines T, Haraldsson B, Radylovick Z, Forget M, Szeto G, LeBlanc F, Ezzo J, Morien A, Rice M, Perry L, Fraser M, Cameron I, Wang Z, Lilge L, White R, Bronfort G, Hoving J, Gelley G Empey B, Lalonde P
Primary review authors ‐ Kay T, Gross A , Goldsmith C, Graham N, Blanchette S, Paquin JP, Dupont G, Christie T, Lalonde P, Hoving J, Bronfort G, Burnie S, Forget M, Empey B Statistician ‐ Goldsmith C Methodological Quality Assessment ‐ Burnie S, Forget M, Goldsmith C, LeBlanc F, Empey B, Szeto G, Gelley G, Lalonde P Study Identification and Selection ‐ Graham N, Brunarski D, Haines T, Gross A Research Librarian ‐ Rice M Data Abstraction, Synthesis, Manuscript Preparation, Public Responsibility, Grants, Administration ‐ Dupont G, Christie T, Lalonde P, Paquin JP, Blanchette S, MacDermid J Final Synthesis ‐ Dupont G, Paquin JP, Blanchette S, Lalonde P, Christie T, Gross A
Sources of support
Internal sources
Centric and LifeMark Health, Canada.
McMaster University, Department of Clinical Epidemiology and Biostatistics, School of Rehabilitation Science, Occupational Health Program, Canada.
University of Toronto, Department of Rehabilitation Medicine, Canada.
External sources
CIHR Knowledge Synthesis Grant 2010, Canada.
National Institutes of Health, Consortial Center for Chiropractic Research, Bethesda, MD (2002), USA.
Hamilton Hospital Assessment Centre (2002), Canada.
Hamilton District Research Grant (2000), Canada.
Hamilton Health Sciences Corporation, Chedoke‐McMaster Foundation (1997), Canada.
University of Saskatchewan, Clinical Teaching and Research Award (1997), Canada.
Declarations of interest
Dr. Gert Bronfort is the first author of one of the trials included in this systematic review. He was not involved in the selection of studies, quality assessment, or data extraction for the study for which he was author.
New search for studies and content updated (conclusions changed)
References
References to studies included in this review
Allan 2003 {published data only}
- Allan M, Brantingham JW, Menezes A. Stretching as an adjunct to chiropractic manipulation of chronic neck pain ‐ before, after or not at all? A prospective randomized controlled clinical trial. European Journal of Chiropractic 2003;50:41‐52. [Google Scholar]
Andersen 2008 {published data only}
- Andersen L, Kjaer M, Sogaard K, Hansen L, Kryger A, Sjogaard G. Effect of two contrasting types of physical exercise on chronic neck muscle pain. Arthritis and Rheumatism 2008;59(1):84‐91. [DOI] [PubMed] [Google Scholar]
- Sogaard K, Blangsted AK, Nielsen PK, Hansen L, Andersen LL, Vedsted P, Sjogaard G. Changed activation, oxygenation, and pain response of chronically painful muscles to repetitive work after training interventions:a randomized controlled trial.. European Journal of Applied Physiology 2012;112:173‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Andersen 2011 {published data only}
- Andersen LL. Influence of psychosocial work environment on adherence to workplace exercise. Journal of Occupational & Enfironmental Medicine 2011;53:182‐4. [DOI] [PubMed] [Google Scholar]
- Andersen LL, Mortensen OS, Zebis MK, Jensen Rh, Poulsen OM. Effect of brief daily exercise on headache among adults‐‐secondary analysis of a randomised controlled trial. Scandinavian Journal of Work, Environment & Health 2011;37:547‐50. [DOI] [PubMed] [Google Scholar]
- Andersen LL, Saervoll CA, Mortensen OS, Poulsen OM, Hannerz H, Zebis MK. Effectiveness of small daily amounts of progressive resistance training for frequent neck/shoulder pain: randomised controlled trial. Pain 2011;152:440‐6. [DOI] [PubMed] [Google Scholar]
Andersen Ch 2012 {published data only}
- Andersen CH, Andersen LL, Gram B, Pedersen MT, Mortensen OS, Zebis MK, et al. Influence of frequency and duration of strength training for effective management of neck and shoulder pain: a randomised controlled trial. British Journal of Sports Medicine 2012;46:1004–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ang 2009 {published data only}
- Ang BO, Monnier A, Harms‐Ringdahl K. Neck/shoulder exercise for neck pain in air force helicopter pilots: a randomized controlled trial. Spine 2009;34(16):E544‐E551. [DOI] [PubMed] [Google Scholar]
Beer 2012 {published data only}
- Beer A, Treleaven J, Jull G. Can a functional postural exercise improve performance in the cranio‐cervical flexion test?‐ A preliminary study. Manual Therapy 2012;17:219‐24. [DOI] [PubMed] [Google Scholar]
Bronfort 2001 {published data only}
- Bronfort G, Aker PD, Evans R, Goldsmith CH, Nelson B, Vernon H. A randomized controlled clinical trial of rehabilitative exercise and chiropractic spinal manipulation for chronic neck pain. Spine 2001;26(7):788‐99. [DOI] [PubMed] [Google Scholar]
- Bronfort G, Evan R, Nelson B. Aker PD, Goldsmith CH, Vernon H. A randomized controlled clinical trial of spinal manipulation and exercise for chronic neck pain: A report on neck performance outcomes after 11 weeks and long‐term effects on patient‐rated outcomes. Proceedings of the Scientific symposium, 1997 World Chiropractic Congress. 1998:62‐8. [{CO97:65}]
- Bronfort G, Evans R, Nelson B, Aker PD, Goldsmith CH, Vernon H. A randomized controlled clinical trial of rehabilitative exercise and spinal manipulation for chronic neck pain. Effects on neck pain and disability, functional health status, biomechanical neck dysfunction, and somato‐visceral symptoms. Proceedings of the 1998 International Conference of Spinal Manipulation. 1998:67‐70. [{CO97:310}]
- Evans R, Bronfort G, Nelson B, Goldsmith C. Two‐year follow‐up of a randomized clinical trial of spinal manipulation and two types of exercise for patients with chronic neck pain. Spine 2002;27:2383‐9. [CO2002] [DOI] [PubMed] [Google Scholar]
Chiu 2005 {published data only}
- Chiu T, Huiu‐Chan C, Cheing G. A randomized clinical trial of TENS and exercise for patients with chronic neck pain. Clinical Rehabilitation 2005;19:850‐60. [DOI] [PubMed] [Google Scholar]
Dellve 2011 {published data only}
- Dellve L, Ahlstrom L, Johsson A, Sandsjo L, Forsman M, Lindegard A, et al. Myofeedback training and intensive muscular strength training to decrease pain and improve work ability among female workers on long‐term sick leave with neck pain: a randomized controlled trial. International Archives of Occupational & Environmental Health 2011;84:335‐46. [DOI] [PMC free article] [PubMed] [Google Scholar]
Franca 2008 {published data only}
- Franca DLM, Senna‐Fernades V, Martins Cortez C, Jackson MN, Bernardo‐Filho M, Guimaraes MAM. Tension neck syndrome treated by acupuncture combined with physiotherapy: A comparative clinical trial (pilot study). Complementary Therapies in Medicine 2008;16:268‐77. [DOI] [PubMed] [Google Scholar]
Hall 2007 {published data only}
- Hall T, Chan H, Christensen L, Odenthal B, Wells C, Robinson K. Efficacy of a C1‐C2 self‐sustained natural apophyseal glide (SNAG) in the management of cervicogenic headache. Journal of Orthopaedic and Sports Physical Therapy 2007;37(3):100‐7. [DOI] [PubMed] [Google Scholar]
Hallman 2011 {published data only}
- Hallman D, Olsson E, Schéele B, Melin L, Lyskov E. Effects of heart rate variability biofeedback in subjects with stress‐related chronic neck pain: a pilot study. Applied Psychophysiology and Biofeedback 2011;36(2):71‐80. [DOI] [PubMed] [Google Scholar]
Hansson 2013 {published data only}
- Hansson EE, Persson L, Malmström EM. Influence of vestibular rehabilitation on neck pain and cervical range of motion among patients with whiplash associated disorders: a randomized controlled trial. Journal of Rehabilitation Medicine 2013;45(9):906–10. [DOI] [PubMed] [Google Scholar]
Helewa 2007 {published data only}
- Helewa A, Goldsmith C, Smythe H, Lee P, Obright K. Effect of therapeutic exercise and sleeping neck support on patients with chronic neck pain: a randomized clinical trial. Journal of Rheumatology 2007;34(1):151‐8. [PubMed] [Google Scholar]
Humphreys 2002 {published data only}
- Humphreys BK, Irgens PM. The effect of a rehabilitation exercise program on head repositioning accuracy and reported levels of pain in chronic neck pain subjects. Journal of Whiplash & Related Disorders 2002;1(1):99‐112. [Google Scholar]
Jull 2002 {published data only}
- Jull G, Trott P, Potter H, Zito G, Niere K, Shirley D, et al. A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache. Spine 2002;27(17):1835‐43. [CO2002] [DOI] [PubMed] [Google Scholar]
Kjellman 2002 {published data only}
- Kjellman G, Oberg B. A randomized clinical trial comparing general exercise, McKenzie treatment and a control group in patients with neck pain. Journal of Rehabilitation Medicine 2002;34:183‐90. [DOI] [PubMed] [Google Scholar]
Kuijper 2009 {published data only}
- Kuijper B, Tans JT, Beelen A, Nollet F, Visser M. Cervical collar or physiotherapy versus wait and see policy for recent onset cervical radiculopathy: randomised trial. BMJ 2009;339:b3883. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lange 2013 {published data only}
- Lange B, Toft P, Myburgh C, Sjogaard G. Effect of targeted strength, endurance, and coordination exercise on neck and shoulder pain among fighter pilots: a randomized controlled trial. Clinical Journal of Pain 2013;29(1):50‐9. [DOI] [PubMed] [Google Scholar]
Lundblad 1999 {published data only}
- Lundblad I, Elert J, Gerdle B. Randomized controlled trial of physiotherapy and Feldenkrais interventions in female workers with neck‐shoulder complaints. Journal of Occupational Rehabilitation 1999;9(3):179‐94. [Google Scholar]
Martel 2011 {published data only}
- Martel J, Dugas C, Dubois JD, Descarreaux M. A randomised controlled trial of preventive spinal manipulation with and without a home exercise program for patients with chronic neck pain. BMC Musculoskeletal Disorders 2011;12:41‐54. [DOI] [PMC free article] [PubMed] [Google Scholar]
Rendant 2011 {published and unpublished data}
- Rendant D, Pach D, Ludtke R, Reishauer A, Mietzner A, Willich SN, et al. Qigong versus exercise versus no therapy for patients with chronic neck pain. Spine 2011;36(6):419‐29. [DOI] [PubMed] [Google Scholar]
Revel 1994 {published data only}
- Revel M, Minguet M, Gergoy P, Vaillant J, Manuel JL. Changes in cervicocephalic kinesthesia after a proprioceptive rehabilitation program in patients with neck pain: a randomized controlled study. Archives of Physical Medicine Rehabilitation 1994;75:895‐9. [DOI] [PubMed] [Google Scholar]
Stewart 2007 {published data only}
- Stewart MJ, Maher CG, Refshauge KM, Herbert RD, Bogduk N, Nicholas M. Randomized controlled trial of exercise for chronic whiplash‐associated disorders. Pain 2007;128:59‐68. [DOI] [PubMed] [Google Scholar]
- Stewart MJ, Maher CG, Refshauge KM, Herbert RD, Bogduk N, Nicholas N. Advice or exercise for chronic whiplash disorders? Design of a randomized controlled trial. BMC Musculoskeletal Disorders 2003;4:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart MJ, Maher CG, Refshauge KM, Herbert RD, Nicholas MK. Patient and clinician treatment preferences do not moderate the effect of exercise treatment in chronic whiplash‐associated disorders. European Journal of Pain 2008;12:879‐85. [DOI] [PubMed] [Google Scholar]
Takala 1994 {published data only}
- Takala EP, Viikari‐Juntura E, Tynkkynen EM. Does group gymnastics at the workplace help in neck pain? A controlled study. Scandinavian Journal of Rehabilitation Medicine 1994;26:17‐20. [PubMed] [Google Scholar]
Viljanen 2003 {published data only}
- Viljanen M, Malmivaara A, Uitti J, Rinne M, Palmroos P, Laippala P. Effectiveness of dynamic muscle training, relaxation training, or ordinary activity for chronic neck pain: randomised controlled trial. BMJ 2003;327(7413):475‐80. [DOI] [PMC free article] [PubMed] [Google Scholar]
von Trott 2009 {published data only}
- Trott P, Wiedemann A, Ludtke R, Reibhauer A, Willich ST, Witt CM. Qigong and exercise therapy for elderly patients with chronic neck pain (QIBANE): A randomized controlled study. Journal of Pain 2009;10(5):501‐8. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Acar 2012 {published data only}
- Acar B, Yilmaz OT. Effects of different physiotherapy applications on pain and mobility of connective tissue in patients with myofascial pain syndrome. Journal of Back and Musculoskeletal Rehabilitation 2012;25(4):261‐7. [DOI] [PubMed] [Google Scholar]
Ahlgren 2001 {published data only}
- Ahlgren C, Waling K, Kadi F, Djupsjöbacka M, Thornell LE, Sundelin G. Effects on physical performance and pain from three dynamic training programs for women with work‐related trapezius myalgia. Journal of Rehabilitation Medicine 2001;33(4):162‐9. [PubMed] [Google Scholar]
Allison 2002 {published data only}
- Allison GT, Nagy BM, Hall T. A randomized clinical trial of manual therapy for cervico‐brachial pain syndrome ‐ a pilot study. Manual Therapy 2002;7(2):95‐102. [DOI] [PubMed] [Google Scholar]
Andersen 2008a {published data only}
- Andersen LL, Andersen CH, Zebis MK, Nielsen PK, Sogaard K, Sjogaard G. Effect of physical training on function of chronically painful muscles: a randomized controlled trial. Journal of Applied Physiology 2008b;105:1796‐801. [DOI] [PubMed] [Google Scholar]
- Andersen LL, Andersen JL, Suetta C, Kjaer M, Sogaard K, Sjogaard G. Effect of contrasting physical exercise interventions on rapid force capacity of chronically painful muscles. Journal of Applied Physiology 2009;107:1413‐19. [DOI] [PubMed] [Google Scholar]
- Andersen LL, Jorgensen MB, Blangsted AK, Pedersen MT, Hansen EA, Sjogaard G. A randomized controlled intervention trial to relieve and prevent neck/shoulder pain. Medicine & Science in Sports & Exercise 2008a;40(6):983‐90. [DOI] [PubMed] [Google Scholar]
Andersen 2010 {published data only}
- Andersen LL, Christensen KB, Holtermann A, Poulsen OM, Sjogaard G, Pedersen MT, et al. Effect of physical exercise interventions on musculoskeletal pain in all body regions among office workers: A one‐year randomized controlled trial. Manual Therapy 2010;15:100‐4. [DOI] [PubMed] [Google Scholar]
Arami 2012 {published data only}
- Arami J, Rezasoltani A, Khalkhali Zaavich M, Rahnama L. The effect of two exercise therapy programs (proprioceptive and endurance training) to treat patients with chronic non‐specific neck pain. Journal of Babol University Medical Sciences 2012;14(1):78‐84. [Google Scholar]
Ardic 2002 {published data only}
- Ardic F, Sarhus M, Topuz O. Comparison of two different techniques of electrotherapy on myofascial pain. Journal of Back and Musculoskeletal Rehabilitation 2012;16(1):11‐6. [DOI] [PubMed] [Google Scholar]
Bernaards 2007 {published data only}
- Bernaards CM, Ariens GAM, Knol DL, Hildebrandt VH. The effectiveness of a work style intervention and a lifestyle physical activity intervention on the recovery from neck and upper limb symptoms in computer workers. Pain 2007;132:142‐53. [DOI] [PubMed] [Google Scholar]
Bernaards 2008 {published data only}
- Bernaards CM, Ariens GAM, Simons M, Knol DL, Hildebrandt VH. Improving work style behavior in computer workers with neck and upper limb symptoms. Journal of Occupational Rehabilitation 2008;18(1):87‐101. [DOI] [PubMed] [Google Scholar]
Bernaards 2012 {published data only}
- Bernaards CM, Ariens GAM, Knold DL, Hildebrandt VH. The effectiveness of a work style intervention and a lifestyle physical activity intervention on the recovery from neck and upper limb symptoms in computer workers. Pain 2007;132:142‐53. [DOI] [PubMed] [Google Scholar]
Bissett 1985 {published data only}
- Bissett A, Mitchell KR, Major G. The cervico‐brachial pain syndrome: Muscle activity and pain relief. Behaviour Change 1985;2(2):129‐35. [Google Scholar]
Blangsted 2008 {published data only}
- Blangsted AK, Sogaard K, Hansen EA, Hannerz H, Sjogaard G. One‐year randomized controlled trial with different physical‐activity programs to reduce musculoskeletal symptoms in the neck and shoulder among office workers. Scandinavian Journal of Work, Environment & Health 2008;34(1):55‐65. [DOI] [PubMed] [Google Scholar]
Bonk 2000 {published data only}
- Bonk AD, Ferrari R, Giebel GD, Edelmann M, Huser R. Prospective randomized controlled study of activity versus collar and the natural history for whiplash injury in Germany. Journal of Musculoskeletal Pain 2000;8:123‐32. [Google Scholar]
Bosmans 2011 {published data only}
- Bosmans J, Pool J, Vet H, Tulder M, Ostelo R. Is behavioral graded activity cost‐effective in comparison with manual therapy for patients with subacute neck pain. Spine 2011;36(18):E1179‐E1186. [DOI] [PubMed] [Google Scholar]
Boyce 2012 {published data only}
- Boyce MJ, Canning CG, Mahant N, Morris J, Latimer J, Fung VS. Active exercise for individuals with cervical dystonia: a pilot randomized controlled trial. Clinical Rehabilitation 2012;27(3):226‐35. [DOI] [PubMed] [Google Scholar]
Brewerton 1966 {published data only}
- Brewerton DA. Pain in the neck and arm: a multicentre trial of the effects of physiotherapy, arranged by the British Association of Physical Medicine. BMJ 1966;1(5482):253‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brodin 1985 {published data only}
- Brodin H. Cervical pain and mobilization. International Journal of Rehabilitation Research 1984;7(2):190‐1. [DOI] [PubMed] [Google Scholar]
- Brodin H. Cervical pain and mobilization. Manual Medicine 1985;2:18‐22. [Google Scholar]
Bronfort 2012 {published data only}
- Bronfort G, Evans R, Anderson AV, Svendsen KH, Bracha Y, Grimm RH. Spinal manipulation, medication, or home exercise with advice for acute and subacute neck pain: a randomized trial. Annals of Internal Medicine 2012;159:1‐10. [DOI] [PubMed] [Google Scholar]
Burketorp 2006 {published data only}
- Burketorp L. Psychological determinants of quality of life in patients with whiplash associated disorders ‐ a prospective study. Disability and Rehabilitation 2009;31(3):227‐36. [DOI] [PubMed] [Google Scholar]
- Burketorp L, Lindh M, Carlsson J, Stener‐Victorin E. The effectiveness of a supervised physical training model tailored to the individual needs of patients with whiplash‐associated disorders‐ a randomized controlled trial. Clinical Rehabilitation 2006;20:201‐17. [DOI] [PubMed] [Google Scholar]
- Burketorp L, Lindh M, Carlsson J, Stener‐Victorin E. The perception of pain and pain‐related cognitions in subacute whiplash‐associated disorders; Its influence on prolonged disability. Disability and Rehabilitation 2006;28(5):271‐9. [DOI] [PubMed] [Google Scholar]
Carlsson 1990 {published data only}
- Carlsson J, Fahlcrantz A, Augustinsson L. Muscle tenderness in tension headache treated with acupuncture or physiotherapy. Cephalgia 1990;10(3):131‐41. [DOI] [PubMed] [Google Scholar]
Cleland 2010 {published data only}
- Cleland J, Childs JD, Glynn PE, Mintken P, Carpenter K, Whitman J. Thoracic spine manipulation and exercise versus exercise alone in the management of mechanical neck pain: Preliminary analysis of a randomized clinical trial. Journal of Orthopaedic & Sports Physical Therapy 2010;40:A23. [Google Scholar]
- Cleland JA, Mintken PE, Carpenter K, Fritz JM, Glynn P, Whitman J. Examination of a clinical prediction rule to identify patients with neck pain likely to benefit from thoracic spine thrust manipulation and a general cervical range of motion exercise: multi‐center randomized clinical trial. Physical therapy 2010;90:1239‐50. [DOI] [PubMed] [Google Scholar]
Cramer 2013 {published data only}
- Cramer H, Lauche R, Hohmann C, Langhorst J, Dobos G. Yoga for chronic neck pain: a 12‐month follow‐up. Pain Medicine 2013;14(4):541–8. [DOI] [PubMed] [Google Scholar]
Cunha 2008 {published data only}
- Cunha ACV, Burke TN, Rendovato FJ, Marques AP. Effect of global posture reeducation and of static stretching on pain, range of motion and quality of life in women with chronic neck pain: A randomized clinical trial. Clinics 2008;63(6):763‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cuzdan 2013 {published data only}
- Cuzdan N, Koldas SK, Evcik D, Ay S. The effectiveness of portable audio biofeedback device in myofascial pain syndrome in neck and upper trapezius muscles. Journal of Musculoskeletal Pain 2013;21(3):217‐23. [Google Scholar]
Dusunceli 2009 {published data only}
- Dusunceli Y, Ozturk C, Atamaz F, Hepguler S, Durmaz B. Efficacy of neck stabilization exercise for neck pain: A randomized controlled study. Journal of Rehabilitation Medicine 2009;41:626‐31. [DOI] [PubMed] [Google Scholar]
Ehrenborg 2010 {published data only}
- Ehrenborg C, Archenholtz B. Is surface EMG biofeedback an effective training method for persons with neck and shoulder complaints after whiplash‐associated disorders concerning activities of daily living and pain‐‐a randomized controlled trial. Clinical Rehabilitation 2010;24:715‐26. [DOI] [PubMed] [Google Scholar]
Escortell‐Mayor 2008 {published data only}
- Escortell‐Mayor E, Lebrijo‐Perez G, Perez‐Martin Y, Asunsolo‐del Barco A, Riesgo‐Fuertes R, Saa‐Requejo C, TEMA‐TENS Group. Randomised clinical trial for primary care patients with neck pain: manual therapy versus electrical stimulation [Ensayo clinico aleatorizado en pacientes con cervicalgia mecanica en atencion primaria: terapia manual frente a elctroestimulacion nerviosa transcutanea]. Aten Primaria 2008;40(7):337‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Escortell‐Mayor 2011 {published data only}
- Escortell‐Mayor E, Riesgo‐Fuertes R, Garrido‐Elustondo S, Asunsolo‐del Barco A, Diaz‐Pulido B, Blanco‐Diaz M, et al. TEMA‐TENS Group. Primary care randomized clinical trial: Manual therapy effectiveness in comparison with TENS in patients with neck pain. Manual Therapy 2011;16:66‐73. [DOI] [PubMed] [Google Scholar]
Evans 2002 {published data only}
- Evans R, Bronfort G, Bittell S, Anderson AV. A pilot study for a randomized clinical trial assessing chiropractic care, medical care, and self‐care education for acute and subacute neck pain patients. Journal of Manipulative and Physiological Therapeutics September 2003;26:403‐11. [DOI] [PubMed] [Google Scholar]
Falla 2006 {published data only}
- Falla D, Jull G, Russel T, Vincenzino B, Hodges P. Effect of neck exercise on sitting posture in patients with chronic neck pain. Physical Therapy 2007;87:408‐17. [DOI] [PubMed] [Google Scholar]
- Falla D, Jull G, Vincenzino B, Hodges P. An endurance‐strength training regime is effective in reducing myoelectric manifestations of cervical flexor muscle fatigue in females with chronic neck pain. Clinical Neurophysiology 2006;117:828‐37. [DOI] [PubMed] [Google Scholar]
Fitz‐Ritson 1995 {published data only}
- Fitz‐Ritson D. Phasic exercises for cervical rehabilitation after "whiplash" trauma. Journal of Manipulative and Physiological Therapeutics 1995;18(1):21‐4. [PubMed] [Google Scholar]
Foley‐Nolan 1992 {published data only}
- Foley‐Nolan D, Moore K, Codd M, Barry C, O'Connor P, Coughlan RJ. Low energy high frequency pulsed electromagnetic therapy for acute whiplash injuries: A double blind randomized controlled study. Scandinavian Journal of Rehabilitation Medicine 1992;24:51‐9. [CO97;61] [PubMed] [Google Scholar]
Friedrich 1996 {published data only}
- Friedrich M, Cermak T, Maderbacher P. The effect of brochure use versus therapist teaching on patients performing therapeutic exercise and on changes in impairment status. Physical Therapy 1996;76(10):1082‐8. [DOI] [PubMed] [Google Scholar]
Gam 1998 {published data only}
- Gam AN, Warming S, Larsen LH, Jensen B, Hoydalsmo O, Allon I, et al. Treatment of myofascial trigger‐points with ultrasound combined with massage and exercise ‐ a randomised controlled trial. Pain 1998;77:73‐9. [CO2002] [DOI] [PubMed] [Google Scholar]
Giebel 1997 {published data only}
- Giebel GD, Edelmann M, Huser R. Die distorsion der halswirbelsaule: Fruhfunktionalle vs. ruhigstellende behandlung. Zentralblatt für Chirurgie 1997;122:517‐21. [PubMed] [Google Scholar]
Goldie 1970 {published data only}
- Goldie I, Landquist A. Evaluation of the effects of different forms of physiotherapy in cervical pain. Scandinavian Journal of Rehabilitation Medicine 1970;2‐3:117‐21. [PubMed] [Google Scholar]
Gustavsson 2006 {published data only}
- Gustavsson C, Koch L. Applied relaxation in the treatment of long‐lasting neck pain: a randomized controlled pilot study. Journal of Rehabilitation Medicine 2006;38:100‐7. [DOI] [PubMed] [Google Scholar]
Guzel 2006 {published data only}
- Guzel R, Akkoca H, Seydaoglu G, Uguz S, Kozanoglu E, Sarpel T. Efficacy of local anesthetic injection versus dry needling in myofascial pain syndrome treatment [Miyofasiyal agri sendromunun tedavisinde lokal anestezik enjeksiyonu ve kuru lgneleme yontemlerinin etkinliginin karsilastirilmasi]. Turkish Journal of Physical and Medical Rehabilitation 2006;52(1):22‐7. [Google Scholar]
Hagberg 2000 {published data only}
- Hagberg M, Harms‐Ringdahl K, Nisell R, Hjelm EW. Rehabilitation of neck‐shoulder pain in women industrial workers: A randomized trial comparing isometric shoulder endurance training with isometric shoulder strength training. Archives of Physical Medicine and Rehabilitation 2000;81:1051‐8. [DOI] [PubMed] [Google Scholar]
Häkkinen 2008 {published data only}
- Häkkinen A, Kautiainen H, Hannonen P, Ylinen J. Strength training and streching versus stretching only in the treatment of patients with chronic neck pain: a randomized one‐year follow‐up study. Clinical Rehabilitation 2008;22(7):592‐600. [DOI] [PubMed] [Google Scholar]
Hamberg‐van Reenen 2009 {published data only}
- Hamberg‐van Reenen HH, Visser B, Beek AJ, Blatter BM, Dieen JH, Mechelen W. The effect of a resistance‐training program on muscle strength, physical workload, muscle fatigue and musculoskeletal discomfort: An experiment. Applied Ergonomics 2009;40:396‐403. [DOI] [PubMed] [Google Scholar]
Hansson 2006 {published data only}
- Hansson EE, Mansson N, Ringsberg KAM, Hakansson A. Dizziness among patients with whiplash‐associated disorder: A randomized controlled trial. Journal of Rehabilitation Medicine 2006;38:387‐90. [DOI] [PubMed] [Google Scholar]
Hanten 1997 {published data only}
- Hanten WP, Barrett M, Gillespie‐Plesko M, Jump KA, Olson SL. Effects of active head retraction with retraction/extension and occipital release on the pressure pain threshold of cervical and scapular trigger points. Physiotherapy Theory and Practice 1997;13:285‐91. [CO2002] [Google Scholar]
Hanten 2000 {published data only}
- Hanten WP, Olson SL, Butts NL, Nowicki AL. Effectiveness of a home program of ischemic pressure followed by sustained stretch for treatment of myofascial trigger points. Physical Therapy 2000;80(10):997‐1003. [PubMed] [Google Scholar]
Henning 1997 {published data only}
- Henning RA, Jacques P, Kissel GV, Sullivan AB, Alter as‐Webb SM. Frequent short rest breaks from computer work: effects on productivity and well‐being at two field sites. Ergonomics 1997;40(1):78‐91. [DOI] [PubMed] [Google Scholar]
Hoving 2002 {published data only}
- Hoving JL, Koes BW, Vet HCW, Windt DAWM, Assendelft WJJ, Mameren H, et al. Manual therapy, physical therapy, or continued care by a general practitioner for patients with neck pain. Annals of Internal Medicine 2002;136(10):713‐59. [CO2002] [DOI] [PubMed] [Google Scholar]
- Hoving JL, Vet HCW, Koes BW, Mameren H, Deville WJLM, Windt DAWM, et al. Manual therapy, physical therapy, or continued care by the general practitioner for patients with neck pain: long‐term results from a pragmatic randomized trial. In: Hoving JL editor(s). Neck pain in primary care. 1st Edition. Wageningen: Pons & Looijen bv, 2001:59‐73. [CO97] [Google Scholar]
- Korthals‐de Bos IBC, Hoving JL, Tulder MW, Rutten‐van Molken MPMH, Ader HJ, Vet HCW, et al. Manual therapy is more cost‐effective than physical therapy and GP care for patients with neck pain. In: Hoving JL editor(s). Neck pain in primary care. 1st Edition. Wageningen: Pons & Looijen bv, 2001:75‐90. [CO97] [Google Scholar]
Hoving 2006 {published data only}
- Hoving JL, Vet HC, Koes BW, Mameren H, Devillé WL, Windt DA, et al. Manual therapy, physical therapy, or continued care by the general practitioner for patients with neck pain long‐term results from a pragmatic randomized clinical trial. Clinical Journal of Pain May 2006;22(4):370‐7. [DOI] [PubMed] [Google Scholar]
Huber 2013 {published data only}
- Huber J, Lisinski P, Polowczyk A. Reinvestigation of the dysfunction in neck and shoulder girdle muscles as the reason of cervicogenic headache among office workers. Disability and Rehabilitation 2013;35(10):793‐802. [DOI] [PubMed] [Google Scholar]
Hudson 2010 {published data only}
- Hudson JS, Ryan CG. Multimodal group rehabilitation compared to usual care for patients with chronic neck pain: a pilot study. Manual Therapy 2010;15:552‐6. [DOI] [PubMed] [Google Scholar]
Hurwitz 2002 {published data only}
- Hurwitz EL, Morgenstern H, Harber P, Kominski GF, Yu F, Adams AH. A randomized trial of chiropractic manipulation and mobilization for patients with neck pain: clinical outcomes from the UCLA neck‐pain study.. Research and Practice 2002;92(10):1634‐41. [CO2002:] [DOI] [PMC free article] [PubMed] [Google Scholar]
Hurwitz 2005 {published data only}
- Hurwitz E, Morganstern H, Vassilki M, Chiang LM. Frequency and clinical predictors of adverse reactions to chiropractic care in the UCLA neck pain study. Spine 2005;30:1477‐84. [DOI] [PubMed] [Google Scholar]
Jay 2013 {published data only}
- Jay K, Schraefel M, Andersen CH, Ebbesen FS, Christiansen DH, Skotte J, et al. Effect of brief daily resistance training on rapid force development in painful neck and shoulder muscles: randomized controllled trial. Clinical Physiology and Functional Imaging 2013;33(5):386‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jensen 2001 {published data only}
- Jensen IB, Bergstrom G, Ljungquist T, Bodin L, Nygren AL. A randomized controlled component analysis of a behavioral medicine rehabilitation program for chronic spinal pain: Are the effects dependent on gender?. Pain 2001;91:65‐78. [DOI] [PubMed] [Google Scholar]
Jensen 2005 {published data only}
- Jensen I, Bergstrom G, Ljungquist T, Bodin L. A 3‐year follow‐up of a multidisciplinary rehabilitation programme for back and neck pain. Pain 2005;115:273‐83. [DOI] [PubMed] [Google Scholar]
Jordan 1998 {published data only}
- Jordan A, Bendix T, Nielsen H, Hansen FR, Host D, Winkel A. Intensive training, physiotherapy, or manipulation for patients with chronic neck pain. A prospective single‐blind randomized clinical trial. Proceedings of the 1996 International conference on spinal manipulation. 1996.
- Jordan A, Bendix T, Nielsen H, Hansen FR, Host D, Winkel A. Intensive training, physiotherapy, or manipulation for patients with chronic neck pain: A prospective single‐blind randomized clinical trial. Spine 1998;23(3):311‐9. [DOI] [PubMed] [Google Scholar]
Jull 2007 JOR {published data only}
- Jull G, Falla D, Treleaven J, Hodges P, Vicenzino B. Retraining cervical joint position sense: the effect of two exercise regimes. Journal of Orthopaedic Research 2007;25:404‐12. [DOI] [PubMed] [Google Scholar]
Jull 2007 Pain {published data only}
- Jull G, Sterling M, Kenardy J, Beller E. Does the presence of sensory hypersensitivity influence outcomes of physical rehabilitation for chronic whiplash?‐ A preliminary RCT. Pain 2007;129:28‐34. [DOI] [PubMed] [Google Scholar]
Jull 2009 {published data only}
- Jull GA, Falla D, Vcenzino B, Hodges PW. The effect of therapeutic exercise on activation of the deep cervical flexor muscles in people with chronic neck pain. Manual Therapy 2009;14:696‐701. [DOI] [PubMed] [Google Scholar]
Jull 2013 {published data only}
- Jull G, Kenardi J, Hendrik J, Cohen M, Sterling M. Management of acute whiplash: a randomized controlled trial of multidisciplinary stratified treatments. PAIN 2013;154:1798‐806. [DOI] [PubMed] [Google Scholar]
Kamwendo 1991 {published data only}
- Kamwendo K, Linton SJ. A controlled study of the effect of neck school in medical secretaries. Scandinavian Journal of Rehabilitation Medicine 1991;23:143‐52. [CO97;119] [PubMed] [Google Scholar]
Karlberg 1996 {published data only}
- Karlberg M, Magnusson M, Malmström EM, Melander A, Moritz U. Postural and symptomatic improvement after physiotherapy in patients with dizziness of suspected cervical origin. Archives of Physical Medicine and Rehabilitation 1996;77(9):874‐82. [{CO97:262}] [DOI] [PubMed] [Google Scholar]
Karlsson 2011 {published data only}
- Karlsson L, Takala E‐P, Ghafouri N, Frumerie A, Gerdle B, Larsson B. The effects of two different home‐exercise programmes on women suffering long‐term neck muscle pain.. European Journal of Pain Supplements 2011 2011;5:285. [Google Scholar]
Kietrys 2007 {published data only}
- Kietrkys DM, Galper JS, Verno V. Effects of at‐work exercises on computer operators. Work 2007;28:67‐75. [PubMed] [Google Scholar]
Koes 1991 {published data only}
- Koes B, Bouter LM, Knipshild PG. The effectiveness of manual therapy, physiotherapy and continued treatment by general practitioner for chronic nonspecific back and neck complaints. Journal of Manipulative and Physiological Therapeutics 1991;14:498‐502. [{C097:3285}] [PubMed] [Google Scholar]
- Koes BW. Efficacy of manual therapy and physiotherapy for back and neck complaints (Thesis). den Haag: Cip‐Gegevens Koninklijke Bibliotheek, 1992a. [{CO97:124}] [Google Scholar]
- Koes BW, Bouter LM, Mameren H, Esser AH, Verstegen GH, Hofhuizen DM, et al. Randomized clinical trial of manual therapy and physiotherapy for persistent back and neck complaints. Manual Therapy in the Netherlands 1992d;1:7‐12. [{CO97:128}] [Google Scholar]
- Koes BW, Bouter LM, Mameren H, Esser AH, Verstegen GM, Hofhuizen DM, et al. A blind randomized clinical trial of manual therapy and physiotherapy for chronic back and neck complaints: Physical outcome measures. Journal of Manipulative and Physiological Therapeutics 1992e;15(1):16‐23. [{CO97:126}] [PubMed] [Google Scholar]
- Koes BW, Bouter LM, Mameren H, Esser AH, Verstegen GM, Hofhuizen DM, et al. Randomized clinical trial of manipulative therapy and physiotherapy for persistent back and neck complaints: results of one year follow up. BMJ 1992b;304:601‐5. [{CO97:127}] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koes BW, Bouter LM, Mameren H, Essers AH, Verstegen GM, Hofhuizen DM, et al. The effectiveness of manual therapy, physiotherapy, and treatment by the general practitioner for nonspecific back and neck complaints. Spine 1992c;17(1):28‐35. [{CO97:129}] [DOI] [PubMed] [Google Scholar]
- Koes BW, Bouter LM, Mameren H, Essers AH, Verstegen GJ, Hofhuizen DM, et al. A randomized clinical trial of manual therapy and physiotherapy for persistent back and neck complaints: subgroup analysis and relationship between outcomes measure. Journal of Manipulative and Physiological Therapeutics 1993;16(4):211‐9. [{CO97:2320}] [PubMed] [Google Scholar]
Kogstad 1978 {published data only}
- Kogstad OA, Karterud S, Gudmundsen J. Cervicobrachialgia. A controlled trial with conventional treatment and manipulation. Tidiskr Nor Loegeforen 1978;98(16):845‐8. [PubMed] [Google Scholar]
Lamb 2013 {published data only}
- Lamb SE, Gates S, Williams MA, Williamson EM, Mt‐Isa S, Withers EJ, et al. Managing Injuries of the Neck Trial (MINT) Study Team. Emergency department treatments and physiotherapy for acute whiplash: a pragmatic, two‐step, randomised controlled trial. Lancet 2013;381(9866):546‐56. [DOI] [PubMed] [Google Scholar]
Lansinger 2007 {published data only}
- Lansinger B, Larsson E, Persson LC, Carlsson JY. Qigong and exercise therapy in patients with long‐term neck pain: A prospective randomized trial. Spine 2007;32(22):2415‐22. [DOI] [PubMed] [Google Scholar]
Lansinger 2013 {published data only}
- Lansinger B, Carlesson JY, Kreuter M, Taft C. Health‐related quality of life in persons with long‐term neck pain after treatment with qigong and exercise therapy respectively. European Journal of Physiotherapy 2013;15:111–7. [Google Scholar]
Lee 2013 {published data only}
- Lee JH, Park SJ, Na SS. The effect of proprioceptive neuromuscular facilitation therapy on pain and function. Journal of Physical Therapy Science 2013;25(6):713–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Levoska 1993 {published data only}
- Levoska S, Keinanen‐Kiukaanneimi S. Active or passive physiotherapy for occupational cervicobrachial disorders? A comparison of two treatment methods with a 1‐year follow‐up. Archives of Physical Medicine and Rehabilitation 1993;74:425‐30. [PubMed] [Google Scholar]
Linton 2001a {published data only}
- Linton SJ, Ryberg M. A cognitive‐behavioral group intervention as prevention for persistent neck and back pain in a non‐patient population: A randomized controlled trial. Pain 2001;90:83‐90. [DOI] [PubMed] [Google Scholar]
Lluch 2014 {published data only}
- Lluch E, Schomacher J, Gizzi L, Petzke F, Seegar D, Falla D. Immediate effects of active cranio‐cervical flexion exercise versus passive mobilisation of the upper cervical spine on pain and performance on the cranio‐cervical flexion test. Manual Therapy 2014;19(1):25‐31. [DOI] [PubMed] [Google Scholar]
Ma 2011 {published data only}
- Ma C, Szeto GP, YanT, Wu S, Lin C, Li L. Comparing biofeedback with active exercise and passive treatment for the management of work‐related neck and shoulder pain: a randomized controlled trial. Archives of Physical Medicine and Rehabilitation 2011;92:849‐58. [DOI] [PubMed] [Google Scholar]
Madson 2010 {published data only}
- Madson TJ, Cieslak KR, Gay RE. Joint mobilization vs massage for chronic mechanical neck pain: A pilot study to assess recruitment strategies and estimate outcome measure variability. Journal of Manipulative and Physiological Therapeutics 2010;33:644‐51. [DOI] [PubMed] [Google Scholar]
Maiers 2013 {published data only}
- Maiers M, Bronfort G, Evans R, Hartvigsen J, Svendsen K, Bracha Y, et al. Spinal manipulative therapy and exercise for seniors with chronic neck pain. Spine Journal 2013;14(9):1879‐89. [DOI] [PubMed] [Google Scholar]
Manca 2006 {published data only}
- Manca A, Epstein, Torgerson D, Moffet J, Coulton S, Farrin A, et al. Randomized trial of a brief physiotherapy intervention compared with usual physiotherapy of neck pain patients: Cost effectiveness analysis. International Journal of Technology Assessment in Health Care 2006;22:1:67‐75. [DOI] [PubMed] [Google Scholar]
Marangoni 2010 {published data only}
- Marangoni AH. Effects of intermittent stretching exercises at work on musculoskeletal pain associated with the use of a personal computer and the influence of media on outcomes. Work 2010;36:27‐37. [DOI] [PubMed] [Google Scholar]
McKinney 1989 {published data only}
- McKinney LA. Early mobilization and outcome in acute sprain of the neck. BMJ 1989b;299:1006‐8. [{CO97:154}] [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinney LA, Dornan JO, Ryan M. The role of physiotherapy in the management of acute neck sprains following road traffic accidents. Archives of Emergency Medicine 1989a;6(1):27‐33. [{CO97:155}] [DOI] [PMC free article] [PubMed] [Google Scholar]
Mealy 1986 {published data only}
- Mealy K, Brennan H, Fenelon GC. Early mobilisation of acute whiplash injuries. British Medical Journal 1986;92:656‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Michalsen 2012 {published data only}
- Michalsen A, Traitteur H, Lüdtke R, Brunnhuber S, Meier L, Jeitler M, et al. Yoga for chronic neck pain: a pilot randomized controlled clinical trial. Journal of Pain 2012;13(11):1122‐30. [DOI] [PubMed] [Google Scholar]
Moffet 2006 {published data only}
- Moffett J, McLean ST. The role of physiotherapy in the management of non‐specific back pain and neck pain. Rheumatology (Oxford) 2006;45(4):371‐8. [DOI] [PubMed] [Google Scholar]
Mongini 2012 {published data only}
- Mongini F, Evangelista A, Milani C, Ferrero L, Ciccone G, Ugolini A, et al. An educational and physical program to reduce headache, neck/shoulder pain in a working community: a cluster‐randomized controlled trial. PLoS ONE 2012;7(1):1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Murphy 2010 {published data only}
- Murphy B, Taylor HH, Marshall P. The effect of spinal manipulation on the efficacy of a rehabilitation protocol for patients with chronic neck pain: A pilot study. Journal of Manipulative and Physiological Therapeutics 2010;33:168‐77. [DOI] [PubMed] [Google Scholar]
Nielsen 2010 {published data only}
- Nielsen PK, Andersen LL, Olsen HB, Rosendal L, Sjøgaard G, Søgaard K. Effect of physical training on pain sensitivity and trapezius muscle morphology. Muscle and Nerve 2010;41:836‐44. [DOI] [PubMed] [Google Scholar]
Nordemar 1981 {published data only}
- Nordemar R, Thorner C. Treatment of acute cervical pain ‐ a comparative group study. Pain 1981;10:93‐101. [DOI] [PubMed] [Google Scholar]
O'Leary 2007 {published data only}
- O'Leary S, Jull G, Kim M, Vincenzino B. Specificity in retraining craniocervical flexor muscle performance. Journal of Orthopaedic and Sports Physical Therapy 2007;37:3‐9. [DOI] [PubMed] [Google Scholar]
O'Leary 2007 JoPain {published data only}
- O’Leary S, Falla D, Hodges P, Jull G, Vicenzino B. Specific therapeutic exercise of the neck induces immediate local hypoalgesia. Journal of Pain 2007;8(11):832‐9. [DOI] [PubMed] [Google Scholar]
Pato 2010 {published data only}
- Pato U, DiStefano G, Fravi N, Arnold M, Curatolo M, Fadanov BP, et al. Comparison of randomized treatment for late whiplash. Neurology 2010;74:1223‐30. [DOI] [PubMed] [Google Scholar]
Pedersen 2013 {published data only}
- Pedersen MM, Zebis MK, Langberg H, Poulsen OM, Mortensen OS, Jensen JN, er al. Influence of self‐efficacy on compliance to workplace exercise. International Journal of Behavioral Medicine 2013;20(3):365‐370. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pennie 1990 {published data only}
- Pennie B, Agambar L. Whiplash injuries. A trial of early management. Journal of Bone & Joint Surgery 1990;72(2):277‐9. [{CO97:178}] [DOI] [PubMed] [Google Scholar]
Persson 1994 {published data only}
- Persson L, Karlberg M, Magnusson M. Effects of different treatments on postural performance in patients with cervical root compression. A randomized prospective study assessing the importance of the neck in postural control. Journal of Vestibular Research 1996;6(6):439‐53. [CO2002] [PubMed] [Google Scholar]
- Persson LCG, Carlsson CA, Carlsson JY. Long‐lasting cervical radicular pain managed with surgery, physiotherapy, or a cervical collar. A prospective, randomized study. Spine 1997;22(7):751‐8. [CO97: 324] [DOI] [PubMed] [Google Scholar]
- Persson LCG, Lilja A. Pain, coping, emotional state and physical function in patients with chronic radicular neck pain. A comparison between patients treated with surgery, physiotherapy or neck collar ‐ a blinded, prospective randomized study. Disability and Rehabilitation 2001;23(8):325‐35. [CO2002:2809] [DOI] [PubMed] [Google Scholar]
- Persson LCG, Moritz U, Brandt L, Carlsson CA. Cervical radiculopathy: pain, muscle weakness and sensory loss in patients with cervical radiculopathy treated with surgery, physiotherapy or cervical collar. A prospective, controlled study. European Spine Journal 1994;6(4):256‐66. [CO97: 1493] [DOI] [PMC free article] [PubMed] [Google Scholar]
Pool 2006 {published data only}
- Bosmans JE, Pool JJM, DeVet HC, VanTulder MW, Ostelo RWJG. Is behavioral graded activity cost‐effective in comparison with manual therapy for patients with subacute neck pain. Spine 2011;36(18):1179‐86. [DOI] [PubMed] [Google Scholar]
- Pool JJM, Ostelo RWJG, Knol DL, Vlaeyen JWS, Bouter LM, DeVet HCW. Is a behavioral graded activity program more effective than manual therapy in patients with subacute neck pain. Spine 2010;35(10):1017‐24. [DOI] [PubMed] [Google Scholar]
- Pool JJM, Ostelo RWJG, Koke AJ, BouterLM, DeVet HCW. Comparison of the effectiveness of a behavioural graded activity program and manual therapy in patients with sub‐acute neck pain: Design of a randomized clinical trial. Manual Therapy 2006;11:297‐305. [DOI] [PubMed] [Google Scholar]
Provinciali 1996 {published data only}
- Provinciali L, Baroni M, Illuminati L, Ceravolo MG. Multimodal treatment to prevent the late whiplash syndrome. Scandinavian Journal of Rehabilitation Medicine 1996;28:105‐11. [PubMed] [Google Scholar]
Ragonese 2009 {published data only}
- Ragonese J. A randomized trial comparing manual physical therapy to therapeutic exercises, to a combination of therapies, for the treatment of cervical radiculopathy. Orthopaedic Practice 2009;21(3):71‐7. [Google Scholar]
Randlov 1998 {published data only}
- Randlov A, Ostergaard M, Manniche C, Kryger P, Jordan A, Heegaard S, et al. Intensive dynamic training for females with chronic neck/shoulder pain. A randomized controlled trial. Clinical Rehabilitation 1998;12(3):200‐10. [DOI] [PubMed] [Google Scholar]
Rosenfeld 2000 {published data only}
- Rosenfeld M, Gunnarsson R, Borenstein P. Early intervention in whiplash‐associated disorders. Spine 2000;25(14):1782‐7. [CO2002] [DOI] [PubMed] [Google Scholar]
Rosenfeld 2003 {published data only}
- Rosenfeld M, Seferiadis A, Carlsson J, Gunnarsson R. Active intervention in patients with whiplash‐associated disorders improves long‐term prognosis: A randomized controlled clinical trial. Spine 2003;28(22):2491‐8. [DOI] [PubMed] [Google Scholar]
- Rosenfeld M, Seferiadis A, Gunnarsson R. Active involvement and intervention in patients exposed to whiplash trauma in automobile crashes reduces costs: A randomized, controlled clinical trial and health economic evaluation. Spine 2006;31(16):1799‐804. [DOI] [PubMed] [Google Scholar]
Rundcrantz 1991 {published data only}
- Rundcrantz B, Johnsson B, Moritz U, Roxendal G. Cervico‐brachial disorders in dentists: A comparison between two kinds of physiotherapeutic interventions. Scandinavian Journal of Rehabilitation Medicine 1991;23:11‐7. [PubMed] [Google Scholar]
Ryan 2001 {published data only}
- Ryan JM. Reducing pain and disability for for patients with chronic neck pain: A double‐blind randomised controlled trial. Thesis. Canberra: Australian National University, 2001. [Google Scholar]
Salmon 2013 {published data only}
- Salmon DM, Harrison MF, Sharpe D, Candow D, Albert WJ, Neary PJ. Exercise therapy for improved neck muscle function in helicopter aircrew. Aviation, Space, and Environmental Medicine 2013;84(10):1046‐54. [DOI] [PubMed] [Google Scholar]
Schnabel 2004 {published data only}
- Schnabel M, Ferrari R, Vassiliou T, Kaluza G. Randomised, controlled outcome study of active mobilisation compared with collar therapy for whiplash injury. Emergency Medicine Journal 2004;21:306‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
Scholten‐Peeters 2006 {published data only}
- Scholten‐Peeters GM, Neeleman‐van der Steen CWM, Windt DAWM, Hendriks EJM, Verhagen AP, Oostendorp RAB. Education by general practitioners or education and exercises by physiotherapists for patients with whiplash‐associated disorders? A randomized clinical trial. Spine 2006;31(7):723‐31. [DOI] [PubMed] [Google Scholar]
Sharan 2011 {published data only}
- Sharan D, Jacob BN, Ajeesh PS, Bookout JB, Barathur RR. The effect cetylated fatty esters and physical therapy on myofascial pain syndrome of the neck. Journal of Bodywork and Movement Therapies 2011;15(3):363‐74. [DOI] [PubMed] [Google Scholar]
Skargren 1997 {published data only}
- Skargren EI, Carlsson PG, Oberg BE. One‐year follow‐up comparison of the cost and effectiveness of chiropractic and physiotherapy as primary management for back pain. Spine 1998;23(17):1875‐84. [DOI] [PubMed] [Google Scholar]
- Skargren EI, Oberg BE, Carlsson PG, Gade M. Cost and effectiveness analysis of chiropractic and physiotherapy treatment for low back and neck pain: Six‐month follow‐up. Spine 1997;22(18):2167‐71. [DOI] [PubMed] [Google Scholar]
Skillgate 2007 {published data only}
- Skillgate E, Vingard E, Alfredsson L. Naprapathic manual therapy or evidence‐based care for back and neck pain: a randomized, controlled trial. Clinical Journal of Pain 2007;23(5):431‐9. [DOI] [PubMed] [Google Scholar]
Skoglund 2011 {published data only}
- Skoglund L, Josephson M, Wahlstedt K, Lampa E, Norbäck D. Qigong training and effects on stress, neck‐shoulder pain and life quality ina computerised office environment. Complementary Therapies in Clinical Practice 2011;17:54‐7. [DOI] [PubMed] [Google Scholar]
Soderlund 2000 {published data only}
- Soderlund A, Olerud C, Lindberg P. Acute whiplash‐associated disorders (WAD): the effects of early mobilization and prognostic factors in long‐term symptomatology. Clinical Rehabilitation 2000;14:457‐67. [CO2002] [DOI] [PubMed] [Google Scholar]
Soderlund 2001 {published data only}
- Soderlund A, Lindberg P. Cognitive behavioural components in physiotherapy management of chronic whiplash associated disorders (WAD)‐‐a randomised group study. Physiotherapy Theory and Practice 2001;17:229‐38. [PubMed] [Google Scholar]
Song 2012 Abstract {unpublished data only}
- Song CH, Jang HJ, Lee K J, Lee YW. Active exercise program in patient with nonspecific chronic neck pain: A randomised controlled trial. 6th World Congress ‐ World Institute of Pain. Miami Beach, Florida, USA, February 2012; Vol. 12:1‐199.
Taimela 2000 {published data only}
- Taimela S, Takala EP, Asklof T, Seppala K, Parviainen S. Active treatment of chronic neck pain. Spine 2000;25(8):1021‐7. [DOI] [PubMed] [Google Scholar]
Telci 2012 {published data only}
- Aslan Telci E, Karaduman A. Effects of three different conservative treatments on pain, disability, quality of life, and mood in patients with cervical spondylosis. Rheumatology International 2012;32(4):1033‐40. [DOI] [PubMed] [Google Scholar]
Tsauo 2004 {published data only}
- Tsauo JY, Lee HY, Hsu JH, Chen CY, Chen CJ. Physical exercise and health education for neck and shoulder complaints among sedentary workers. Journal of Rehabilitation Medicine 2004;36:253‐7. [DOI] [PubMed] [Google Scholar]
van den Heuvel 2003 {published data only}
- Heuvel SG, Looze MP, Hildebrandt VH, The KH. Effects of software programs stimulating regular breaks and exercises on work‐related neck and upper‐limb disorders. Scandinavian Journal of Work, Environment & Health 2003;29(2):106‐16. [DOI] [PubMed] [Google Scholar]
van Ettekoven 2006 {published data only}
- Ettekoven H, Lucas C. Efficacy of physiotherapy including a craniocervical training programme for tension‐type headache; a randomized clinical trial. Cephalagia 2006;26(8):983–91. [DOI] [PubMed] [Google Scholar]
Vasseljen 1995 {published data only}
- Vasseljen O, Johansen BM, Westgaard RH. The effect of pain reduction on perceived tension and EMG‐recoded trapezius muscle activity in workers with shoulder and neck pain. 1995; 27:243‐252. Scandinavian Journal of Rehabilitation Medicine 1995;27:243‐52. [PubMed] [Google Scholar]
Vikne 2007 {published data only}
- Vikne J, Oedegaard A, Laerum E, Ihlebaek C, Kirkesola G. A randomized study of new sling exercise treatment vs traditional physiotherapy for patients with chronic whiplash‐associated disorders with unsettled compensation claims. Journal of Rehabilitation Medicine 2007;39(3):252‐9. [DOI] [PubMed] [Google Scholar]
Voerman 2007 {published data only}
- Voerman G, Sandsjo L, Vollenbroek‐Hutten M, Larsman P, Kadefors R, Hermans H. Changes in cognitive‐behavioral factors and muscle activation patterns after interventions for work‐related neck‐shoulder complaints: Relations with discomfort and disability. Journal of Occupational Rehabilitation 2007;17:593‐609. [DOI] [PubMed] [Google Scholar]
- Voerman GE, Sandsjo L, Vollenbroek‐Hullen MMR, Larsman P, Kadefors R, Hermens HJ. Effects of ambulant myofeedback training and ergonomic counselling in female computer workers with work‐related neck‐shoulder complaints: a randomized controlled trial. Journal of Occupational Rehabilitation 2007;17:137‐52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Voerman GE, Vollenbrock‐Hutten MMR, Sandsjo L, Kadefors R, Hermens HJ. Prognostic factors for the effects of two interventions for work‐related neck‐shoulder complaints: Myofeedback training and ergonomic counselling. Applied Ergonomics 2008;39:743‐53. [DOI] [PubMed] [Google Scholar]
von Piekartz 2011 {published data only}
- Piekartz H, Ludtke K. Effect of treatment of temporomandibular disorders (TMD) in patients with cervicogenic headache: A single‐blind, randomized controlled study. Journal of Craniomandibular Practice 2011;29(1):1‐14. [DOI] [PubMed] [Google Scholar]
Waling 2002 {published data only}
- Waling K, Jarvholm B, Sundelin G. Effects of training on female trapezius myalgia. Spine 2002;27(8):789‐96. [DOI] [PubMed] [Google Scholar]
- Waling K, Sundelin G, Ahlgren C, Jarvholm B. Perceived pain before and after three exercise programs‐‐a controlled clinical trial of women with work‐related trapezius myalgia. Pain 2000;85:201‐7. [DOI] [PubMed] [Google Scholar]
Wani 2013 {unpublished data only}
- Wani SK, Raka N, Jethwa J. Comparative efficacy of cervical retraction exercises (McKenzie) with and without using pressure biofeedback in cervical spondylosis. International Journal of Therapy and Rehabilitation 2013;20(10):501.. [Google Scholar]
Wei 2007 {published data only}
- Wei FA, Jiang J, Zhang SF. Preventative and curative effect of initiative motion on cervical headache. Zhongguo Zuzhi Gongcheng Yanjlu yu Linchuang Kangfu 2007;11(39):8012‐4. [Google Scholar]
Yang 2013 {published data only}
- Yang Jun‐xiong, Zhang Jian‐ping, Yu Jian‐chun, Han Jing‐xian. Treatment of cervical spondylosis by spinal balancing combined with intervention of pathway of qi: a randomized controlled study. Chinese Acupuncture and Moxibustion Jul. 2013;33(7):582‐6. [PubMed] [Google Scholar]
Ylinen 2003 {published data only}
- Ylinen J, Hakkinen A, Nykanen M, Kautiainen HJ, Takala P. Neck muscle training in the treatment of chronic neck pain: a three year follow‐up study. Europa Medicophysica 2007;43(2):161‐9. [PubMed] [Google Scholar]
- Ylinen J, Takala EP, Kautiainen H, Nykanen M, Hakkinen A, Phojolainen T, et al. Effect of long‐term neck muscle training on pressure pain threshold: a randomized controlled trial. European Journal of Pain 2005;9:673‐81. [DOI] [PubMed] [Google Scholar]
- Ylinen J, Takala EP, Nykanen M, Hakkinen A, Malkia E, Pohjolainen T, et al. Active neck muscle training in the treatment of chronic neck pain in women: a randomized controlled trial. JAMA 2003;289(19):2509‐16. [DOI] [PubMed] [Google Scholar]
- Ylinen JJ, Hakkinen AH, Takala EP, Nykanen MJ, Kautiainen HJ, Malkia EA, et al. Effects of neck muscle training in women with chronic neck pain: one‐year follow‐up study. Journal of Strength and Conditioning Research 2006;20(1):6‐13. [DOI] [PubMed] [Google Scholar]
Ylinen 2006b {published data only}
- Ylinen JJ, Takala EP, Nykanen MJ, Kautiainen HJ, Hakkinen AH, Airaksinen OVP. Effects of twelve‐month stretching exercise in treatment of chronic neck pain. Journal of Strength and Conditioning Research 2006;20(2):304‐8. [DOI] [PubMed] [Google Scholar]
Ylinen 2007b {published data only}
- Ylinen J, Kautiainen H, Wirén K, Häkkinen A. Stretching exercises vs manual therapy in treatment of chronic neck pain: a randomized, controlled cross‐over trial. Journal of Rehabilitation Medicine 2007;39:126–32. [DOI] [PubMed] [Google Scholar]
Ylinen 2010 {published data only}
- Ylinen J, Nikander R, Nukanen M, Kautiainen H, Hakkinen A. Effect of neck exercises on cervicogenic headache: A randomized controlled trial. Journal of Rehabilitation Medicine 2010;42:344‐9. [DOI] [PubMed] [Google Scholar]
Yogitha 2012 {published data only}
- Yogitha B, Ebnezar J. Efficacy of mind sound resonance technique in common neck pain. International Journal of Research in Ayurveda & Pharmacy 2012;3(2):227‐32. [Google Scholar]
Youseff 2013 {published data only}
- Youssef EF, Shanb AS A. Mobilization versus massage therapy in the treatment of cervicogenic headache: A clinical study. Journal of Back and Musculoskeletal Rehabilitation 2013;26:17–24. [DOI] [PubMed] [Google Scholar]
Zaproudina 2007 {published data only}
- Zaproudina N, Hanninen O, Airaksinen O. Effectiveness of traditional bone setting in chronic neck pain: randomized clinical trial. Journal of Manipulative and Physiological Therapuetics July/August;30(6):432‐7. [DOI] [PubMed] [Google Scholar]
Zebis 2011 {published data only}
- Zebis M, Andersen L, Pedersen M, Mortensen P, Andersen C, Pedersen M, et al. Implementation of neck/shoulder exercises for pain relief among industrial workers: A randomized controlled trial. BMC Musculoskeletal Disorders 2011;12(205):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
References to studies awaiting assessment
Falla 2013 {published data only}
- Falla D, Lindstrom R, Rechter L, Boudreau S, Petzke F. Effectiveness of an 8‐week exercise programme on pain and specificity of neck muscle activity in patients with chronic neck pain: A randomized controlled study. European Journal of Pain 2013;17:1517‐28. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
Andersen 2010a (Protocol) {published data only}
- Andersen LL, Zebis MK, Pedersen MT, Roessler KK, Andersen CH, Pedersen MM, et al. Protocol for work place adjusted intelligent physical exercise reducing musculoskeletal pain in shoulder and (VMS): A cluster randomized controlled. BMC Musculoskeletal Disorders 2010;11:173. [DOI] [PMC free article] [PubMed] [Google Scholar]
Andersen 2011a (Protocol) {published data only}
- Andersen Ch, Andersen LL, Mortensen OS, Zebis MK, Sjogaard G. Protocol for shoulder function training reducing musculoskeletal pain in shoulder and neck: A randomized controlled trial. BMC Musculoskeletal Disorders 2011;12:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guerriero 1997 {published data only}
- Guerriero D. Comparative effects of manipulation and physical therapy on motion in the cervical spine. Proceedings of the International Conference on Spinal Manipulation. 1991.
Gurumoorthy 2000 {published data only}
- Gurumoorthy D, Twomey LT, Batalin NJ. A prospective study of acute whiplash injury and its clinical management. Internation Federation of Manipulation Therapy, 7th Scientific Conference. November 2000:Abstract 78. [CO2002]
Hansen 2011 (Protocol) {published data only}
- Hansen I, Sogaard K, Christensen R, Thomsen B, Manniche C, Juul‐Kristensen B. Neck exercises, physical and cognitive behavioural‐graded activity as a treatment for adult whiplash patients with chronic neck pain: Design of a randomised controlled trial. BMC Musculoskeletal Disorders 2011;12:274. [DOI] [PMC free article] [PubMed] [Google Scholar]
Michaleff 2009 (Protocol) {published data only}
- Michaleff ZA, Maher CG, Jull G, Latimer J, Connelly LB, Lin CWC, et al. A randomised clinical trial of a comprehensive exercise program for chronic whiplash: trial protocol. BMC Musculoskeletal Disorders 2009;10:149. [doi:10.1186/1471‐2474‐10‐149] [DOI] [PMC free article] [PubMed] [Google Scholar]
Reginiussen 2000 {published data only}
- Reginiussen T, Johnsen R, Torstensen TA. Efficiency of manual therapy on patients with cervicogenic headache. A randomized single blinded controlled trial. Internation Federation of Manipulation Therapy, 7th Scientific Conference. November 2000:Abstract 105.
Stokke 1995 {published data only}
- Stokke O. A randomized comparison of chiropractic and physiotherapy treatment of neck pain of functional (mechanical) origins: A controlled clinical trial. Conference Proceedings of the Chiropractic Centennial Foundation. 1995:372‐3.
Williamson 2009 (Protocol {published data only}
- Williamson E, Williams M, Hansen Z, Joseph S, Lamb SE. Development and delivery of a physiotherapy intervention for the early management of whiplash injuries: The managing injuries of neck trial (MINT) intervention. Physiotherapy 2009;95:1523. [DOI] [PubMed] [Google Scholar]
Additional references
Abernethy 2013
- Abernethy B, Kippers V, Hanrahan SJ, Paddy MG, McManus AM, MacKinnon L. Biophysical Foundations of Human Movement. 3rd Edition. Champaign: Sheridan Books, 2013. [Google Scholar]
Ailliet 2013
- Ailliet L, Knol DL, Rubinstein SM, Vet HCW, Tulder MW, Terwee CB. Definition of the construct to be measured in a prerequisite for the assessment of validity. The Neck Disability Index as an example. Journal of Clinical Epidemiology 2013;66:775‐82. [DOI] [PubMed] [Google Scholar]
Atkins 2004
- Atkins D, Best D, Briss PA, Eccles M, Falck‐Ytter Y, Flottorp S, et al. Grade Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004;328(7454):1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bertozzi 2013
- Bertozzi L, Gardenghi I, Turoni F, Villafane JH, Capra F, Guccione AA, Pillastrini P. Effect of therapeutic exercise on pain and disability in the management of chronic Nonspecific neck pain: Systematic review and meta‐analysis of randomized trials. Physical Therapy 2013;93(8):1026‐36. [DOI] [PubMed] [Google Scholar]
Boutron 2005
- Boutron I, Moher D, Tugwell P, Giraudeau B, Poiraudeau S, Nizard R, et al. A checklist to evaluate a report of a non pharmacological trial (CLEAR NPT) was developed using consensus. Journal of Clinical Epidemiology 2005;58:1233‐40. [DOI] [PubMed] [Google Scholar]
Bronfort 2009
- Brønfort G, Nilsson N, Haas M, Evans RL, Goldsmith CH, Assendelft WJJ, et al. Non‐invasive physical treatments for chronic/recurrent headache (Review). Cochrane Database of Systematic Reviews 2004, Issue 3. [DOI: 10.1002/14651858.CD001878.pub2] [DOI] [PubMed] [Google Scholar]
Buitenhuis 2009
- Buitenhuis J, Jong PJ, Jaspers JP, Groothoff JW. Work disability after whiplash: A prospective cohort study. Spine 2009;34:262‐7. [DOI] [PubMed] [Google Scholar]
Carroll 2008a
- Carroll LJ, Hogg‐Johnson S, Velde G, Haldeman S, Holm LW, Carragee EJ, et al. Course and prognostic factors for neck pain in the general population: results of the Bone and Joint Decade 2000‐2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008;22(4S):S75‐82. [DOI] [PubMed] [Google Scholar]
Carroll 2008b
- Carroll L, Holm L, Hogg‐Johnson S, Cote P, Cassidy J, Haldeman S, et al. Course and prognostic factors for neck pain in whiplash‐associated disorders (WAD). Spine 2008;33(4S):S83‐92. [DOI] [PubMed] [Google Scholar]
Cicchetti 1976
- Cicchetti DV. Assessing inter‐rater reliability for rating scales: resolving some basic issues. British Journal of Psychiatry 1976;129:452‐6. [DOI] [PubMed] [Google Scholar]
Clar 2014
- Clar C, Tsertsvadze A, Court R, Hundt GL, Clarke A, Sutcliffe P. Clinical effectiveness of manual therapy for the management of musculoskeletal and non‐musculoskeletal conditions: systematic review and update of UK evidence report. Chiropractic & Manual Therapies 2014;22(12):1‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cohen 1988
- Cohen J. Statistical Power Analysis for the Behavioural Sciences. 2nd Edition. Hilldale, NJ: Lawance Erlbaum, 1988. [Google Scholar]
Côté 2008
- Côté P, Velde G, Cassidy D, Carroll LJ, Hogg‐Johnson S, Holm LW, et al. The burden and determinants of neck pain in workers: Results of the Bone and Joint Decade 2000‐2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008;33(4S):S60‐74. [DOI] [PubMed] [Google Scholar]
Farrar 2001
- Farrar JT, Young JP Jr, LaMoreaux L, Werth JL, Poole RM. Clinical importance of changes in chronic pain intensity measured on an 11‐point numerical pain rating scale. Pain 2001;94(2):149‐58. [DOI] [PubMed] [Google Scholar]
Felson 1995
- Felson DT, Anderson JJ, Boers M, Bombardier C, Furst D, Goldsmith C, et al. Preliminary definition of improvement in rheumatoid arthritis. Arthritis and Rheumatism 1995;Jun;38(6):727‐35. [DOI] [PubMed] [Google Scholar]
Fernandez‐de‐las‐Penas 2007
- Fernandez‐de‐las‐Penas C, Simons DG, Cuadrado ML, Pareja JA. The role of myofascial trigger points in musculoskeletal pain syndromes of the head and neck. Current Pain and Headache Reports 2007;11(5):365‐72. [DOI] [PubMed] [Google Scholar]
Furlan 2009
- Furlan AD, Pennick V, Bombardier C, Tulder M, Editorial Board, Cochrane Back Review Group. Updated method guidelines for systematic reviews in the Cochrane Back Review Group. Spine (Phila Pa 1976) 2009 Aug 15;34(18):1929‐41. [DOI] [PubMed] [Google Scholar]
Goldsmith 1993
- Goldsmith CH, Boers M, Bombardier C, Tugwell P. Criteria for clinically important changes in outcomes. Development, scoring and evaluation of rheumatoid arthritis patients and rial profiles. Journal of Rheumatology 1993;20(3):561‐5. [PubMed] [Google Scholar]
Grady 2001
- Grady C. Money for Research Participation: Does it jeopardize informed consent?. American Journal of Bioethics 2001;2:40‐4. [DOI] [PubMed] [Google Scholar]
Graham 2011
- Graham N, Haines T, Goldsmith CG, Gross A, Burnie S, Shahzad U, et al. Reliability of 3 assessment tools used to evaluate randomized controlled trials for treatment of neck pain.. Spine 2012;37(6):515‐22. [DOI] [PubMed] [Google Scholar]
Gross 2002
- Gross AR, Kay T, Hondras M, Goldsmith C, Haines T, Peloso P, et al. Manual therapy for mechanical neck disorders: a systematic review. Manual Therapy 2002;7(3):131‐49. [DOI] [PubMed] [Google Scholar]
Gross 2007
- Gross AR, Goldsmith C, Hoving JL, Haines T, Peloso P, Aker P, et al and the Cervical Overview Group. Conservative Management of Mechanical NeckDisorders: A Systematic Review. Journal of Rheumatology 2007;34:1083‐102. [PubMed] [Google Scholar]
Guyatt 2006
- Guyatt G, Gutterman D, Baumann MH, Addrizzo‐Harris D, Hylek EM, Phillips B, et al. Grading strength of recommendations and quality of evidence in clinical guidelines:Report fom an American College of Chest Physicians task force. Chest 2006;129:174‐81. [DOI] [PubMed] [Google Scholar]
Haldeman 2010
- Haldeman S, Carroll L, Cassidy JD. Findings from the bone and joint decade 2000 to 2010 task force on neck pain and its associated disorders. Journal of Occupational and Environmental Medicine 2010;52:424‐7. [DOI] [PubMed] [Google Scholar]
Hall 2005
- Hall CM, Brody L. Therapeutic Exercise: Moving Toward Function. 1st Edition. Baltimore, MD: Lippincott Williams & Wilkins, 2005. [Google Scholar]
Higgins 2009
- Higgins JPT, Green S (editors). Cochrane Handbookfor Systematic Reviews of Interventions 5.0.2. www.cochrane‐handbook.org. [updated September 2009]. Chichester: John Wiley& Sons, Ltd, 2008. [Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane Collaboration, 2011. Available from www.cochrane‐handbook.org.] [Google Scholar]
Hogg‐Johnson 2008
- Hogg‐Johnson S, Velde G, Carroll LJ, Holm LW, Cassidy JD, Guzman J, et al. The burden and determinants of neck pain in the general population: results of the Bone and Joint Decade 2000‐2010 Task Force on Neck Pain and Its Associated Disorders. Spine 2008;33((4 Suppl)):S39‐51. [DOI] [PubMed] [Google Scholar]
Hoy 2014
- Hoy D, March L, Woolf A, Blyth F, Brooks P, Smith E, et al. The global burden of neck pain: estimates from the Global Burden of Disease 2010 study. Annals of Rheumaric Diseases 2014;73(7):1309‐15. [doi:10.1136/ annrheumdis‐2013‐204431] [DOI] [PubMed] [Google Scholar]
Hung 2014
Hurwitz 2008
- Hurwitz EL, Carragee JEJ, Velde G, Carroll LJ, Nordin M, Guzman J, et al. Treatment of neck pain: Noninvasive interventions: Results of the bone and joint decade 2000‐2010 Task Force on Neck Pain and its associated disorders. Spine 2008;33(4S):S123‐52. [DOI] [PubMed] [Google Scholar]
Kendal 1963
- Kendal MG, Stuart A. The Advanced Theory of Statistics: Distribution Theory. 2nd Edition. New York: Hofner Publishing Co, 1963. [Google Scholar]
Leaver 2010
- Leaver AM, Refshauge KM, Maher CG, McAuley JH. Conservative interventions provide short‐term relief for non‐specific neck pain: a systematic review. Journal of Physiotherapy 2010;56(2):73‐85. [DOI] [PubMed] [Google Scholar]
Lee 2009
- Lee MS, Pittler MH, Ernst E. Internal qigong for pain conditions: a systematic review. Journal of Pain 2009;10(11):1121‐7. [DOI] [PubMed] [Google Scholar]
MacDermid 2009
- MacDermid JC, Walton DM, Avery S, Blanchard A, Etruw E, McAlpine C, et al. Measurement properties of the neck disability index: a systematic review. Journal of Orthopaedic & Sports Physical Therapy 2009;39(5):400‐17. [DOI] [PubMed] [Google Scholar]
Martin 2008
- Martin BI, Deyo RA, Mirza SK, Turner JA, Comstock BA, Hollingworth W, et al. Expenditures and health status among adults with back and neck problems. JAMA 2008;299(6):656‐64. [DOI] [PubMed] [Google Scholar]
Merskey 1994
- Merskey H, Bogduk N. Classification of Chronic Pain: Descriptions of Chronic Pain Syndromes and Definition of Pain Terms, second edition. International Association for the Study of Pain 1994.
Miller 2010
- Miller J, Gross A, D'Sylva J, Burnie SJ, Goldsmith CH, Graham N, et al. Manual therapy and exercise for neck pain: A systematic review. Manual Therapy 2010;15:334‐54. [PubMed] [Google Scholar]
Nappo 2013
- Nappo S, Lafrate G, Sanchez Z. Motives for participating in a clinical research trial: a pilot study in Brazil. BMC Public Health 2013;13(19):1‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
NCHS 2013
- National Center for Health Statistics. Health, United States, 2012: With Special Feature on Emergency Care. Available from http://www.cdc.gov/nchs/ (accessed 17 March 2014). Hyattsville, MD. [PubMed]
Olesen 1988
- Olesen J. Classification and diagnostic criteria for headache disorders, cranial neuralgias and facial pain. Cephalgia 1988;8(7):61‐2. [PubMed] [Google Scholar]
Olesen 1997
- Olesen J, Gobel H. ICD‐10 Guide for Headaches. Guide to the classification, diagnosis and assessment of headaches in accordance with the tenth revision of the International classification of diseases and related health problems and its application to neurology. Cephalalgia 1997;17 Suppl 19:29‐30. [Google Scholar]
Racicki 2012
- Racicki S, Gerwin S, DiClaudio S, Reinmann S, Donaldson M. Conservative physical therapy management for the treatment of cervicogenic headache: a systematic review. Journal of Manual and Manipulative Therapy. 2013;21(2):113‐24. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sahrmann 2002
- Sahrmann SA. Diagnosis and Treatment of Movement Impairment Syndromes. St.Louis:Mosby, Inc, 2002.. Diagnosis and Treatment of Movement Impairment Syndromes. 1. St.Louis: Mosby Inc, 2002. [Google Scholar]
Salt 2011
- Salt E, Wright C, Kelly S, Dean A. A systematic literature review on the effectiveness of non‐invasive therapy for cervicobrachial pain. Manual Therapy 2011;16:53‐65. [DOI] [PubMed] [Google Scholar]
Schroeder 2013
- Schroeder J, Kaplan L, Fischer DJ, Skelly AC. The outcomes of manipulation or mobilization therapy compared with physical therapy or exercise for neck pain: a systematic review. Evidence‐Based Spine‐Care Journal 2013;4(1):30‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Schumacher 1993
- Schumacher HR, Klippel JH, Koopman WJ (eds). Primer on the Rheumatic Diseases. 10th Edition. Atlanta: Arthritis Foundation, 1993. [Google Scholar]
Sherrington 1961
- Sherrington C. The Integrative Action of the Nervous System. New Haven: Yale University Press, 1961:340. [Google Scholar]
Sjaastad 1990
- Sjaastad O, Fredriksen TA, Pfaffenrath V. Cervicogenic headache: diagnostic criteria. Headache 1990;30:723‐6. [DOI] [PubMed] [Google Scholar]
Sjaastad 1998
- Sjaastad O, Fredriksen TA, Pfaffenrath V. Cervicogenic headache: diagnostic criteria. Headache 1998;38:442‐5. [DOI] [PubMed] [Google Scholar]
Sjaastad 2008
- Sjaastad O. Cervicogenic headache: Comparison with migraine without aura; vaga study. Cephalgia 2008;28(S1):18‐20. [DOI] [PubMed] [Google Scholar]
Southerst 2014
- Southerst D, Nordin M, Côté P, Shearer H, Varatharajan S, Yu H, et al. Is exercise effective for the management of neck pain and associated disorders or whiplash‐associated disorders? A systematic review by the Ontario Protocolfor Traffic Injury Management (OPTIMa) Collaboration. Spine Journal 2014;Available on line(15 Feb):1‐70. [DOI] [PubMed] [Google Scholar]
Spitzer 1987
- Spitzer WO, Leblanc FE, Dupuis M. Scientific approach to the assessment and managment of activity related spinal disorders. Spine 1987;suppl 7:S1‐S59. [PubMed] [Google Scholar]
Spitzer 1995
- Spitzer WO, Skovron M L, Salmi L R, Cassidy JD, Duranceau J, Suissa S, et al. Scientific monograph of the Quebec Task Force on Whiplash‐Associated Disorders: redefining "whiplash" and its management. Spine 1995;20:1S‐73S. [PubMed] [Google Scholar]
Stunkel 2011
- Stunkel L, Grady C. More than the money: A review of the literature examining healthy volunteer motivations. Contemporary Clinical Trials 2011;32(3):342–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
Teasell 2010a
- Teasell RW, McClure JA, Walton D, Pretty J, Salter K, Meyer M, et al. A research synthesis of therapeutic interventions for whiplash associated disorder (WAD) Part 2 ‐ interventions for acute WAD. Pain Research & Management 2010a;15(5):295‐304. [DOI] [PMC free article] [PubMed] [Google Scholar]
Teasell 2010b
- Teasell RW, McClure AJ, Walton D, Pretty J, Salter K, Meyer M, et al. A research synthesis of therapeutic interventions for whiplash‐associated disorder (WAD): Part 3 ‐ interventions for subacute WAD. Pain Research & Management 2010;15(5):305‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Teasell 2010c
- Teasell RW, McClure JA, Walton D, Pretty J, Salter K, Meyer M, et al. A research synthesis of therapeutic interventions for whiplash‐associated disorder (WAD): Part 4 ‐ interventions for chronic WAD. Pain Research & Management 2010;15(5):313‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Teixeira 2012
- Teixeira P, Carraça E, Markland D, Silva M, Ryan R. Exercise, physical activity, and self‐determination theory: A systematic review. International Journal of Behavioral Nutrition and Physical Activity 2012;9(78):1‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
van der Velde 2009
- Velde G, Beaten D, Hogg‐Johnston S, Hurwitz E, Tennant A. Rasch analysis provides new insights into the measurement properties of the neck disability index. Arthritis and Rheumatism 2009;61(4):544‐51. [DOI] [PubMed] [Google Scholar]
Van Tulder 2003
- Tulder M, Furlan A, Bombardier C, Bouter L, Editorial Board of the Cochrane Collaboration Back Review Group. Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine 2003;28(12):1290‐9. [DOI] [PubMed] [Google Scholar]
Vincent 2013
- Vincent K, Maigne JV, Fischhoff C, Lanlo O, Dagenais S. Systematic review of manual therapies for non specific neck pain. Joint Bone Spine. 2013;80(5):508‐15. [DOI] [PubMed] [Google Scholar]
Zimmerman 2000
- Zimmerman GL, Olsen CG, Bosworth MF. A ’stages of change’ approach to helping patients change behavior. American Family Physician 2000;61(5):1409‐16. [PubMed] [Google Scholar]
References to other published versions of this review
Aker 1996
- Aker P, Gross AR, Goldsmith CH, Peloso P. Conservative management of neck pain: systematic overview and meta‐analysis. BMJ 1996;313:1291‐6. [PMC free article] [PubMed] [Google Scholar]
Gross 1996
- Gross AR, Aker PD, Goldsmith CH, Peloso P. Conservative management of mechanical neck disorders: A meta‐analysis. Online Journal of Current Clinical Trials 1996 July 30;5:Doc No 200‐1. [PubMed] [Google Scholar]
Kay 2005
- Kay TM, Gross A, Goldsmith CH, Hoving JL, Brønfort G. Exercises for mechanical neck disorders. Cochrane Database of Systematic Reviews 2005, Issue 3. [DOI: 10.1002/14651858.CD004250.pub3] [DOI] [PubMed] [Google Scholar]
Kay 2012
- Kay TM, Gross A, Goldsmith CH, Rutherford S, Voth S, Hoving JL, et al. Exercises for mechanical neck disorders. Cochrane Database of Systematic Reviews 2012, Issue 8. [DOI: 10.1002/14651858.CD004250.pub4] [DOI] [PubMed] [Google Scholar]


