Abstract
Background
Multi‐strategic community wide interventions for physical activity are increasingly popular but their ability to achieve population level improvements is unknown.
Objectives
To evaluate the effects of community wide, multi‐strategic interventions upon population levels of physical activity.
Search methods
We searched the Cochrane Public Health Group Segment of the Cochrane Register of Studies,The Cochrane Library, MEDLINE, MEDLINE in Process, EMBASE, CINAHL, LILACS, PsycINFO, ASSIA, the British Nursing Index, Chinese CNKI databases, EPPI Centre (DoPHER, TRoPHI), ERIC, HMIC, Sociological Abstracts, SPORTDiscus, Transport Database and Web of Science (Science Citation Index, Social Sciences Citation Index, Conference Proceedings Citation Index). We also scanned websites of the EU Platform on Diet, Physical Activity and Health; Health‐Evidence.org; the International Union for Health Promotion and Education; the NIHR Coordinating Centre for Health Technology (NCCHTA); the US Centre for Disease Control and Prevention (CDC) and NICE and SIGN guidelines. Reference lists of all relevant systematic reviews, guidelines and primary studies were searched and we contacted experts in the field. The searches were updated to 16 January 2014, unrestricted by language or publication status.
Selection criteria
Cluster randomised controlled trials, randomised controlled trials, quasi‐experimental designs which used a control population for comparison, interrupted time‐series studies, and prospective controlled cohort studies were included. Only studies with a minimum six‐month follow up from the start of the intervention to measurement of outcomes were included. Community wide interventions had to comprise at least two broad strategies aimed at physical activity for the whole population. Studies which randomised individuals from the same community were excluded.
Data collection and analysis
At least two review authors independently extracted the data and assessed the risk of bias. Each study was assessed for the setting, the number of included components and their intensity. The primary outcome measures were grouped according to whether they were dichotomous (per cent physically active, per cent physically active during leisure time, and per cent physically inactive) or continuous (leisure time physical activity time (time spent)), walking (time spent), energy expenditure (as metabolic equivalents or METS)). For dichotomous measures we calculated the unadjusted and adjusted risk difference, and the unadjusted and adjusted relative risk. For continuous measures we calculated percentage change from baseline, unadjusted and adjusted.
Main results
After the selection process had been completed, 33 studies were included. A total of 267 communities were included in the review (populations between 500 and 1.9 million). Of the included studies, 25 were set in high income countries and eight were in low income countries. The interventions varied by the number of strategies included and their intensity. Almost all of the interventions included a component of building partnerships with local governments or non‐governmental organisations (NGOs) (29 studies). None of the studies provided results by socio‐economic disadvantage or other markers of equity. However, of those included studies undertaken in high income countries, 14 studies were described as being provided to deprived, disadvantaged or low socio‐economic communities. Nineteen studies were identified as having a high risk of bias, 10 studies were unclear, and four studies had a low risk of bias. Selection bias was a major concern with these studies, with only five studies using randomisation to allocate communities. Four studies were judged as being at low risk of selection bias although 19 studies were considered to have an unclear risk of bias. Twelve studies had a high risk of detection bias, 13 an unclear risk and four a low risk of bias. Generally, the better designed studies showed no improvement in the primary outcome measure of physical activity at a population level.
All four of the newly included, and judged to be at low risk of bias, studies (conducted in Japan, United Kingdom and USA) used randomisation to allocate the intervention to the communities. Three studies used a cluster randomised design and one study used a stepped wedge design. The approach to measuring the primary outcome of physical activity was better in these four studies than in many of the earlier studies. One study obtained objective population representative measurements of physical activity by accelerometers, while the remaining three low‐risk studies used validated self‐reported measures. The study using accelerometry, conducted in low income, high crime communities of USA, emphasised social marketing, partnership with police and environmental improvements. No change in the seven‐day average daily minutes of moderate to vigorous physical activity was observed during the two years of operation. Some program level effect was observed with more people walking in the intervention community, however this result was not evident in the whole community. Similarly, the two studies conducted in the United Kingdom (one in rural villages and the other in urban London; both using communication, partnership and environmental strategies) found no improvement in the mean levels of energy expenditure per person per week, measured from one to four years from baseline. None of the three low risk studies reporting a dichotomous outcome of physical activity found improvements associated with the intervention.
Overall, there was a noticeable absence of reporting of benefit in physical activity for community wide interventions in the included studies. However, as a group, the interventions undertaken in China appeared to have the greatest possibility of success with high participation rates reported. Reporting bias was evident with two studies failing to report physical activity measured at follow up. No adverse events were reported.The data pertaining to cost and sustainability of the interventions were limited and varied.
Authors' conclusions
Although numerous studies have been undertaken, there is a noticeable inconsistency of the findings in the available studies and this is confounded by serious methodological issues within the included studies. The body of evidence in this review does not support the hypothesis that the multi‐component community wide interventions studied effectively increased physical activity for the population, although some studies with environmental components observed more people walking.
Plain language summary
Community wide interventions for increasing physical activity
Not having enough physical activity leads to poorer health. Regular physical activity can reduce the risk of chronic disease and improve one's health and wellbeing. The lack of physical activity is a common and in some cases a growing health problem. To address this, 33 studies have used improvement activities directed at communities, using more than one approach in a single program. When we first looked at the available research in 2011 we observed that there was a lack of good studies which could show whether this approach was beneficial or not. Some studies claimed that community wide programs improved physical activities and other studies did not. In this update we found four new studies that were of good quality; however none of these four studies increased physical activity levels for the population. Some studies reported program level effects such as observing more people walking, however the population level of physical activity had not increased. This review found that community wide interventions are very difficult to undertake, and it appears that they usually fail to provide a measurable benefit in physical activity for a population. It is apparent that many of the interventions failed to reach a substantial portion of the community, and we speculate that some single strategies included in the combination may lack individual effectiveness.
Summary of findings
for the main comparison.
| Community wide interventions for promoting physical activity | |||
|
Patient or population: whole communities (adults, adolescents and children) Settings: community based Intervention: multi‐component of at least two physical activity interventions targeting the whole community Comparison: existing programmes and infrastructure | |||
| Outcomes [duration of follow up] | Summary of effects | Number of communities (studies) | Quality of the evidence (GRADE) |
|
Physical activity % Physically active Intervention compared to control adjusted pre/post cross‐sectional sampling (end of intervention to 6 years) |
Typically no evidence of benefit | 25 (10) | ⊕⊕OO1 Low |
|
Physical activity % physically active Intervention compared to control adjusted pre‐post cross‐sectional sampling (end of intervention to 3 years, 4 months) |
Typically no evidence of benefit | 160 (3) | ⊕⊕⊕⊕ High |
|
Energy expenditure METS/week score, adjusted mean difference (follow up; end of intervention to 4 years) |
Typically no evidence of effect Range: ‐241 to +176 |
156 (5) | ⊕⊕OO1 Low |
|
Physical activity Average daily minutes of moderate to vigorous (24 months) |
No evidence of effect from the baseline of 36 minutes per day | 2 (1) | ⊕⊕⊕O2 Moderate |
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect. Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate. Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate. Very low quality: We are very uncertain about the estimate. | |||
1Substantial heterogeneity between trials regarding type of interventions and measured outcomes; wide and overlapping range of effects
2Findings based on a single study in only two communities
Background
Physical activity is recognised as being important for reducing the overall burden of disease (WHO 2009). Very strong scientific evidence based on a wide range of well‐conducted studies shows that physically active people have higher levels of health‐related fitness, a lower risk profile for developing a number of disabling medical conditions and lower rates of various chronic diseases than do people who are inactive (US Physical Activity Guidelines 2008).
Despite the positive health effects associated with regular physical activity, physical inactivity remains a common public health problem in high, middle and low income countries (Heath 2012). The prevalence of physical inactivity remains high, and in some cases has even increased in recent years (Bauman 2009; Guthold 2008). In addition, low income and ethnic minority adults have the highest rates of physical inactivity, people at the top of the socio‐economic scale appear to perform more leisure‐time activity than those at the bottom of the scale, and participation is patterned by age and gender (Belanger 2011; Crespo 2000; Crespo 2001; Gidlow 2006).
The lack of physical activity cannot be attributed solely to personal motivation and so countries that are tackling this complex issue are increasingly electing to employ multi‐component approaches (that is informational, behavioural, and environmental) in increasing a population's physical activity (Heath 2012; Kahn 2002; WHO 2004).
Description of the intervention
Community wide interventions are attractive in that they aim to improve the health risk factors (especially low physical activity) of a whole population. These strategies generally involve investment in visible infrastructure and planning initiatives with the aim of producing long‐lasting benefits for the community. They differ from singular community based strategies which may target only a particular subset of the population. Community wide interventions offer a number of advantages over offering only one approach to a population. They operate at a series of levels to impact on behaviour. These levels reflect social‐ecological models of health and include changes to policies and environments, and involve mass media and individually focused activities (for example primary healthcare screening).
One systematic review has categorised these interventions into four types (Cavill and Foster 2004). These are (1) comprehensive integrated community approaches, where physical activity is part of an overall risk factor reduction programme (for example the Minnesota Heart Health Project (Luepker et al 1994)); (2) community wide ‘campaigns’ using mass media (Renger 2002)); (3) community based approaches using person focused techniques; and (4) community approaches to environmental change. The third category includes programmes that use methods and strategies such as one‐to‐one counselling, classroom instruction, and cognitive‐behavioural strategies but in community facilities and settings such as church halls or community centres (Sharpe 2003). The final category includes programmes that use some form of community action, often including a coalition or advocacy group, to make positive changes to the physical environment (King 1994). These interventions are often delivered to communities in combinations.
How the intervention might work
We developed a logic model to capture the broad range of different approaches found in community interventions (Figure 1). This framework divides the actions into two phases, a community strategy development phase and an implementation phase, as there is some evidence to suggest community wide approaches appear more sustainable in the longer term (Foster 2000). The community strategy development phase describes the construction phase of a community intervention. Actions include identification of target groups, populations, the setting for delivery, stakeholders and intervention options. The implementation phase describes the delivery of actions to encourage physical activity behaviour change. Actions might include mass media campaigns, community participation or educational events, advocacy and environmental changes. The outputs of both phases might be measured in a range of variables as short to long‐term outcomes. For example, intermediate outcomes could include knowledge of the benefits of an active lifestyle or improved access to physical activity. Examples of long‐term outcomes could be a reduction in morbidity and mortality related to physical activity behaviour. Changes in the proximal and intermediate variables, such as knowledge or attitudes, are likely to be more amenable to change through communication campaigns (Cavill and Bauman 2004).
1.
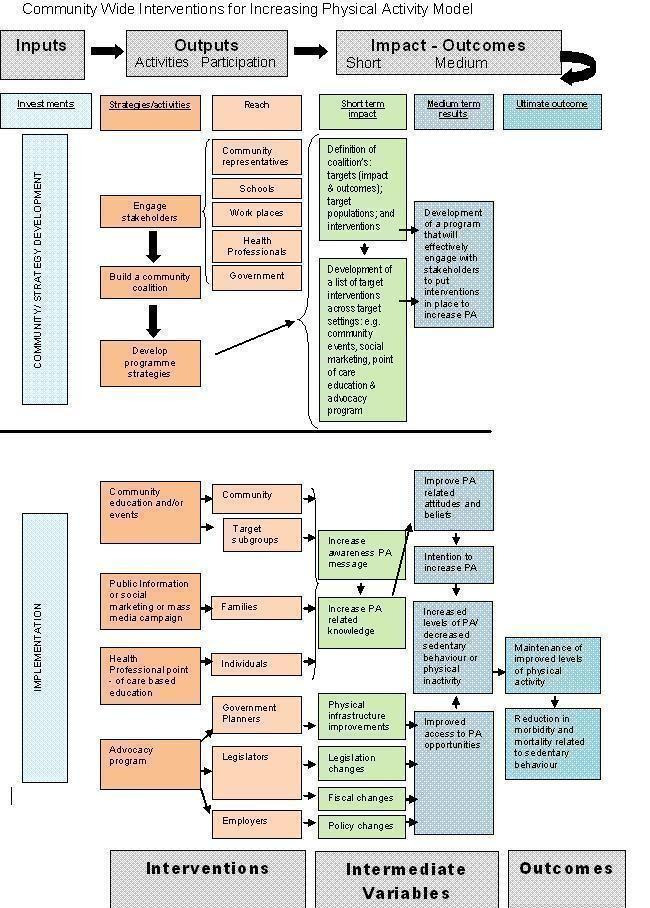
Logic Model for Community Wide Interventions for Increasing Physical Activity.
Why it is important to do this review
Many studies of community wide interventions have been undertaken but, prior to our earlier review, few have published evaluations of their process or impact. Although the popularity of these interventions is increasing, there was a need to combine all the global evidence currently available in an up‐to‐date systematic review. We believed a review would enable a more in‐depth exploration of the effectiveness of the interventions as well as investigating equity and inclusiveness issues. Earlier reviews (for example Kahn 2002) do not contain the more recent studies and newer health promotion strategies built upon more recent research and health promotion theory. It is hoped that this update of the Cochrane review will be particularly useful to those decision makers with the responsibility of selecting and implementing community wide investments. The application of the logic model for this review illustrates the belief that community wide interventions should be understood more broadly than as being just the sum of several interventions that have been implemented in a community.
Objectives
Primary research objective
We sought to determine the effects of community wide, multi‐strategic interventions upon community levels of physical activity.
Secondary research objectives
We addressed the following predetermined research objectives.
To explore whether any effects of the intervention are different within and between populations, and whether these differences form an equity gradient.
To describe other health (e.g. cardiovascular disease morbidity) and behavioural effects (e.g. diet) where appropriate outcomes are available.
To explore the influence of context in the design, delivery and outcomes of the interventions.
To explore the relationship between the number of components, duration and effects of the interventions. As an addition to the published protocol, we sought to understand more explicitly whether the intensity of the community wide intervention could explain differences of effects between studies.
To highlight implications for further research and research methods to improve knowledge of the interventions in relation to the primary research objective.
Methods
Criteria for considering studies for this review
Types of studies
It is recognised that public health and health promotion interventions are evaluated using a wide variety of approaches and designs. We permitted the inclusion of cluster randomised controlled trials, randomised controlled trials (RCTs), quasi‐experimental designs which used a control population for comparison, interrupted time‐series (ITS) studies, and prospective controlled cohort studies (PCCS). Only studies with a minimum six‐month follow up from the start of the intervention to measurement of outcomes were included. The six‐month period was considered as the minimal time frame as physical activity behaviour changes, as understood by the Prochaska and DiClemente model (Prochaska 1992), are established in the action stage, which is when the individual actively engages in the new behaviour. For physical activity, the highest likelihood for relapse occurs within the first six months of starting a regular program (Dishman 1994).
Types of participants
The term community wide generally refers to either: 1) an intervention directed at a geographic area, such as a city or a town defined by geographical boundaries; or 2) an intervention directed toward groups of people who share at least one common social or cultural characteristic.
As the focus of the review was whole‐of‐community interventions, we defined participants in the included studies as comprising those persons of any age residing in a geographically defined community, such as urban, peri‐urban, village, town, or city. We excluded interventions which were whole of state or country. Although some of the strategies targeted individuals with chronic disease, collectively the participants included in the studies needed to be representative of the whole community and not restricted to a particular geographic subregion (for example a park) or subgroups (for example only elderly people). To be included, a strategy must have shown intent to be comprehensive in reaching the targeted community. Participants must have been free living and not part of any institutionalised community, such as those who were mentally ill, the frail or bedridden elderly population, or those incarcerated in prison.
Types of interventions
It is recognised that to achieve a whole of community approach requires more than a singular strategy, as changing behaviour is a difficult task (Mummery 2009). Although little is known about how to reach the most disadvantaged groups in the community (Mummery 2009), we defined a community wide approach as one which should include strategies that have, within their scope, outreach to many disadvantaged groups. For this review, we defined a community wide intervention as one which has at least two of the following six broad strategies aimed at physical activity. The list categories of suitable strategies, which would be components of an integrated community wide intervention, are consistent with the logic model.
1. Social marketing through local mass media (e.g. television (TV), radio, newspapers).
2. Other communication strategies (e.g. posters, flyers, information booklets, websites, maps) to raise awareness of the project and provide specific information to individuals in the community.
3. Individual counselling by health professionals (both publicly and privately funded), such as the use of physical activity prescriptions.
4. Working with voluntary, government and non‐government organisations, including sporting clubs, to encourage participation in walking, other activities and events.
5. Working within specific settings such as schools, workplaces, aged care centres, community centres, homeless shelters, and shopping malls. This may include settings that provide an opportunity to reach disadvantaged persons.
6. Environmental change strategies such as creation of walking trails and infrastructure with legislative, fiscal or policy requirements, and planning (having ecological validity) for the broader population.
Studies that were community based but did not include at least two of the six stated strategies were excluded. We recognised that single strategy interventions (for example mass media only) are likely to be topics of other reviews and they were beyond the scope of this review.
Types of outcome measures
Primary outcomes
Whilst it is desirable to focus on a small range of outcome measures, the context for research in this area of health is that measures of physical activity at a population level are complex (both the measures and the methods) and international consensus on gold standards has not been reached.
To be included in this review, studies needed to measure physical activity in the study population. Physical activity could be quantified using a variety of measurements, for example percentage of people active or inactive, frequency of physical activity, percentage meeting recommendations, percentage undertaking active travel; and other objective (for example accelerometers, pedometers) or subjective methods (for example self‐reported questionnaires, diaries) (Bassett et al 2008).
Secondary outcomes
Data on other related measures of health were extracted.
1. Measures of health outcomes and risk factor status (e.g. cardiovascular disease, body mass index (BMI), energy expenditure).
2. Measures of other health behaviours (e.g. sedentary behaviour, dietary patterns, or smoking).
3. Intermediate outcomes (e.g. knowledge of and attitudes toward the benefit of physical activity).
4. Any adverse outcomes that were reported (e.g. unintended changes in other risk factors, opportunity cost, and injuries).
Process measures
Measures relating to the process of implementing an intervention were also extracted.
Search methods for identification of studies
Electronic searches
We searched the following databases:
Cochrane Public Health Group Specialised Register in the Cochrane Register of Studies (CRS);
The Cochrane Library;
MEDLINE, MEDLINE In‐Process;
EMBASE;
CINAHL;
PsycINFO ;
LILACS;
ASSIA;
British Nursing Index (BNI);
Database: CAJ, CCND, CPCD, CJSS, CMFD, CDFD, Chinese CNKI databases (http://www.global.cnki.net/grid20/index.htm);
EPPI Centre;
DoPHER;
TRoPHI;
ERIC;
Health Management Information Consortium (HMIC) (grey literature);
Sociological Abstracts;
SPORTDiscus;
Transport Database TRIS;
Web of Science
Science Citation Index, Social Sciences Citation Index and Conference Proceedings Citation Index,
Science Citation Index, Social Sciences Citation Index and Conference Proceedings Citation Index.
We searched the following websites for relevant publications, including grey literature:
EU Platform on Diet, Physical Activity and Health;
Health Evidence (http://healthevidence.org);
IUHPE (International Union for Health Promotion and Education);
NCCHTA (National Coordinating Centre for Health Technology Assessment) (http://www.ncchta.org);
NICE guidelines (http://www.nice.org.uk);
SIGN guidelines (http://www.sign.ac.uk);
US Centres for Disease Control and Prevention (http://www.cdc.gov/);
World Health Organization (http://www.who.int/en/).
Searches were carried out for studies published from January 1995 to January 2014. The search strategies and details of the search dates can be found in Appendix 1 . The MEDLINE search was developed for precision and sensitivity with advice from the Public Health Group's Trials Search Co‐ordinator and tested against a set of 38 relevant studies from across the globe. The search was then adapted to the remaining databases using database‐specific subject headings, where available.
Searching other resources
In addition, reference lists of all relevant systematic reviews, guidelines and included primary studies were searched.
For the original review, the following experts in the field were contacted to ask if they were aware of any recently published, in press or unpublished studies: Dr Harry Rutter (National Obesity Observatory, Oxford), Dr Nick Cavill (Oxford University), Mr Glenn Austin (GP Links Wide‐Bay), Mr Jiandong Sun (Queensland University of Technology), Professor Kerry Mummery (University of Central Queensland), Professor Gregory W Heath (University of Tennessee College of Medicine) and Professor Ross C Brownson (Washington University in St Louis). Subsequent to the original review we had studies brought to our attention by experts and researchers.
The past 12 months of the six journals that contained two or more studies (completed or in progress) meeting the review inclusion criteria were handsearched in the original review, however for the update this was determined as unnecessary and was not repeated. The journals were:
American Journal of Public Health;
Australia Health Promotion;
BMC Public Health;
Norsk Epidemiologi;
Preventive Medicine;
Scandinavian Journal of Public Health.
Through various methods, including contact with authors, the review team obtained a full text PDF or an abstract containing sufficient details to determine eligibility of all potentially relevant studies. Non‐English study reports were all examined by readers with appropriate language skills to determine whether they were to be excluded or included.
Data collection and analysis
Selection of studies
The initial search strategy produced a listing of nearly 26,000 citations across the original review and this update. An initial screening of titles and abstracts was undertaken to remove those which were obviously outside the scope of the review. Authors were overly inclusive at this stage and, if in doubt, a paper was left in. The full text was obtained for the papers potentially meeting the inclusion criteria (based on the title and abstract only) and multiple publications and reports on the same study were linked together. All the full text papers obtained were then screened by two review authors (PB and shared between DF, JS, and CF) who compared the description of the intervention with the logic model (Figure 1) to assess whether the required components of a community wide intervention and permissible study designs were fully met. Where there was a persisting difference of opinion, a third review author was asked to review the paper in question and a consensus was reached between the three review authors.
Data extraction and management
Data were extracted for all the studies that met the inclusion criteria. For each study, two review authors (PB and shared between DF, JS, and CF) independently completed data extraction forms, which were tailored to the requirements of this review. Quality criteria questions for RCTs, controlled clinical trials (CCTs), controlled before and after (CBA) studies and ITS study designs were incorporated into the data extraction form. A checklist was used to ensure inclusion of data relevant for health equity (Ueffing 2009). In addition, multiple reports and publications of the same study were assembled and compared for completeness and possible contradictions. Data were extracted from companion studies that reported findings on the process evaluation of the intervention. The specific components present in the primary paper and companion publications were reviewed using the logic model (Figure 1) to assist in the categorisation of studies and interpretation of results where heterogeneity was present.
Numerical data for analysis were extracted from the included studies and managed in an Excel spreadsheet.
The data extraction form was first piloted by three review authors (PB, DF, and JS) to assess its ability to capture study data and inform assessment of study quality. Problems in the use of the form that were identified were resolved through discussion and the form was revised as required.
Where studies reported more than one endpoint per outcome, the primary endpoint identified by the authors was extracted. Where no primary endpoint was identified by the authors, the measures were ranked by effect size and we extracted the median measure (Curran 2007). Measures of physical activity or sedentary behaviour that were based upon meeting a national standard were noted and the potential for unequal comparisons identified. We collected information on how physical activity was reported, that is whether it was through self‐report in a telephone survey or devices such as pedometers. Data extracted independently by the review authors were compared and any differences were resolved through discussion.
Assessment of risk of bias in included studies
Only studies that met the inclusion criteria were assessed and reported in a risk of bias table as per the recommendation of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008).
Two review authors (PB and one other author) assessed the risk of bias for each study. Analysis of non‐randomised controlled trials followed the recommendations in Chapter 13 of the Cochrane Handbook for Systematic Reviews of Interventions. Where there was disagreement between review authors in risk of bias assessment, this was resolved by discussion and consensus.
Studies were assessed for the five general domains of bias: selection, performance, attrition, detection, and reporting, as well as for an additional category to capture any other concerns pertaining to the study quality that did not fit distinctly into either of the five domains. For example, this additional category included instances where the statistical analyses presented in the included study were problematic and failed to adjust for baseline differences between the control and intervention groups, or failed to address what appeared to be regression to the mean. This category was also applicable if there appeared to be a 'head‐start' or other advantage for the intervention community. Each was assessed with answers of 'Yes' indicating low risk of bias, 'No' indicating high risk of bias, and 'Unclear' indicating either lack of information or uncertainty over the potential for bias. Studies were judged overall as at 'low', 'unclear' or 'high' risk of bias after consideration of the study design and size, and the potential impact of the identified weaknesses noted in the table for each study.
Specifically, assessment of performance bias included identification of explicit statements of measures undertaken to avoid contamination (that can occur when the control group also receives the intervention) such as spatial separation, non‐delivery of the program to the control communities, and minimisation of wide‐reaching mass media. We also considered measurement of the community's awareness of the message obtained through community surveys, both of the intervention and control communities. Additionally, integrity of the intervention was considered and performance bias was assessed as being present when the study's process evaluation (perhaps an additional publication) described instances where the program was not delivered as planned.
Studies were assessed as at high risk of detection bias when incomplete data were inadequately defined or, particularly in cross‐sectional sampling, where the characteristics of the follow‐up groups varied significantly from the baseline groups.
Detection bias was assessed to be at low risk where measurement tools were used in their entirety, the outcome assessment was blind (if deemed appropriate), the outcome measure metrics were valid, the measure was of sufficient quality (for example assessed over the period > one day) and the sample was representative (for example random sampling of the community).
Reporting bias was assessed as being at low risk if the reports appeared to be free from selective reporting and the measures reported were complete and matched the aims of the studies. Studies where follow‐up measurement was absent, or appeared to be deliberately withheld, were assessed as at high risk of reporting bias.
The review authors determined a priori that the best evidence (both contextually relevant and representing the purpose of the intervention) was likely to come from cluster RCTs and CBA studies. Although this differs from the usual evidence hierarchy (NHMRC 1999) (which emphasises RCTs for assessment of interventions), it is considered a better approach than the problematic application of the usual criteria when appraising the evidence for social and public health interventions (Petticrew 2003).
Measures of intervention effect
The effect sizes for dichotomous outcomes were expressed as relative risk (RR) and risk difference (RD) in the first instance. For comparability across studies, given the important baseline differences between intervention (I) and control (C) groups, we calculated from the authors' data an adjusted estimate of effect based on the differences at baseline. Therefore, for dichotomous outcomes we calculated the following.
1. Net percentage change from baseline = ((Ipost ‐ Ipre)/Ipre) ‐ ((Cpost ‐ Cpre)/Cpre) x 100.
2. Adjusted risk difference = (Ipost ‐ Ipre) ‐ (Cpost ‐ Cpre).
3. Adjusted relative risk = (Ipost / Cpost)/(Ipre/Cpre).
Confidence intervals (95%) were calculated using the Wald test.
For continuous outcomes we calculated the following from the authors' data.
1. Post mean differences (PMD) = Imeanpost ‐ Cmeanpost
2. Adjusted mean difference = [(Imeanpost ‐ Cmeanpost) ‐ (Imeanpre ‐ Cmeanpre)]
3. Adjusted percentage change relative to the control group = [((Imeanpost ‐ Cmeanpost) ‐ (Imeanpre ‐ Cmeanpre))/Cmeanpost] x 100.
The 95% confidence intervals could not be calculated using this approach.
Unit of analysis issues
Studies allocated by clusters that did not account for clustering during analysis were not re‐analysed. This was because these studies were not randomised and there was only a small number of clusters, and so clustering would have a minimal effect.
Dealing with missing data
Protocols and baseline publications for the studies were used to identify outcome data that were expected to be present in the follow‐up report which presented the outcomes. Incomplete data (that is less than 40% of data) were assessed during the risk of bias assessment. Data that appeared to be completely absent were noted as reporting bias. Missing data were also captured in the data extraction form and reported in the risk of bias table. The authors were contacted to try and acquire missing data for inclusion. In some instances this included the use of a Chinese speaking epidemiologist.
Assessment of heterogeneity
Due to heterogeneity in the study designs employed, the populations in which the interventions were conducted, and the interventions themselves no meta‐analysis was conducted.
Assessment of reporting biases
We considered plotting trial effect against standard error and presenting this in a funnel plot (Higgins 2008) to determine whether asymmetry could be caused by a relationship between effect size and sample size or by publication bias (Egger 1998). However, we decided against doing this given the high risks of bias in the data and the poor quality of measurement undertaken in the studies.
Intensity of intervention
We categorised the intensity of the community wide intervention to assess whether intensity could account for differences that existed in the outcomes between studies. The intensity of the intervention was categorised based on the following six characteristics and attributes that we hypothesised would be important in understanding differences in the effectiveness of the community wide intervention; two review authors (PB and DF) independently assessed each characteristic as 'more intensive', 'less intensive' or 'unclear':
development of community partnerships and coalition (first level of the logic model ‘Community/Strategy Development’), showing evidence of engaging stakeholders and building a community coalition;
levels of intervention (second level of the logic model ‘Implementation’), intervening at the individual (personal), social (interpersonal) and environmental (physical and legislative) levels;
reach of the strategies (second level of the logic model), the intervention reaches the whole of the community, multiple sectors of the community, targets subgroups, with awareness > 85%;
magnitude of the intervention, the extent of continuous provision of the intervention through the intervention period (volume of the intervention): frequency and duration of strategies, with high intensity typified as sustained integration of the intervention;
description of cost, where stated the cost per person for the intervention (excluding the evaluation) in the context of the year and the location, presumably indicating the magnitude of the intervention;
statement of intensity by the authors, descriptors found within the studies where the investigators themselves used descriptors such as 'high impact' or 'significant cost'.
We categorised the overall assessment of intensity for each study as 'high', 'medium', 'low', or 'unclear'. Given that the six categories we assessed on were not distinct, and the sufficiency of detail varied between the studies, each review author independently made the overall assessment using subjective informed determination rather than a predefined algorithm. Discrepancies were resolved by discussion.
Data synthesis
Continuous outcomes were reported on the original scale. where possible. We predetermined we would undertake a meta‐analysis only when data were clinically homogeneous. We followed Chapter 9: 'Analysing data and undertaking meta‐analyses' of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2008). As data were not available that were sufficiently similar and of sufficient quality, a meta‐analysis was not performed. We predetermined that evidence from differing study designs and outcome types was not to be combined in a forest plot from standard meta‐analysis (Christinsen 2009). However, to identify trends and provide summary statements, simple forest plots were generated for three dichotomous outcomes (% physically active, % physically active during leisure time and % physically inactive).
Subgroup analysis
We predetermined that, where sufficient data were available, we would perform additional subgroup analyses to compare outcomes by: types of study designs; group effects for people who shared a common social, cultural, or health status characteristic (for example age, gender, ethnicity); reach of intervention and intensity of intervention (derived from use of the logic model and process evaluations). We had intended that a subgroup analysis would be used to explore whether there was likely to be a relationship of effect to disadvantage and whether an equity gradient was present. Given the limitations of the data, both in their quality and the absence of subgroup reporting, no further subgroup analysis could be undertaken.
Sensitivity analysis
The studies with low risk of bias have been grouped in the forest plots.
Summary of findings
We had intended to undertake a summary of findings table for the primary outcomes related to physical activity and sedentary behaviour using GRADE profiler (Cochrane IMS 2009). This was to be created using the measures for the primary outcomes identified as being most reliable and which predominated. Given that very few studies had reliable measures of physical activity and sedentary behaviour, and much of the data were incomplete, a modified approach was required in which we split the presentation of findings according to the risk of bias. We considered the primary challenge that all the community wide interventions were different and all of the communities unique and thus caution was required in potentially homogenising very different approaches. As conducting meta‐analyses was deemed inappropriate, a summary table has been prepared using narrative analysis of the included studies.
Results
Description of studies
See Characteristics of included studies; Characteristics of excluded studies
Results of the search
Electronic searches from 1995 to November 2009, in the original review, yielded 17,538 hits following removal of duplicates (Figure 2), of which 207 were considered potentially eligible and were assessed in full text. The update search, to January 2014, identified an additional 9551 hits following removal of duplicates (Figure 2), of which 62 were considered potentially eligible and assessed in full text. The results of the searches of the electronic databases and websites are found in Table 2 and Table 3, respectively. The full search strategies, dates, and number of hits are given in Appendix 1. Twenty‐five studies were included in the original review (Brown 2006; Brownson 2004; Brownson 2005; De Cocker 2007; Eaton 1999; Goodman 1995; Gu 2006; Guo 2006; Jenum 2006; Jiang 2008; Kloek 2006; Kumpusalo 1996; Luepker 1994; Lupton 2003; Nafziger 2001; Nishtar 2007; NSW Health 2002; O'Loughlin 1999; Osler 1993; Reger‐Nash 2005; Sarrafzadegan 2009; Simon 2008; Wendel‐Vos 2009; Young 1996; Zhang 2003). Eight additional studies were identified in the update search (Gao 2013; Kamada 2013; Mead 2013; Nguyen 2012; Phillips 2014; Rissel 2010; Solomon 2014; Wilson 2014) resulting in a total of 33 included studies. We identified one study for which there is no published conclusion and have identified it as 'ongoing' (Davey 2011).
2.
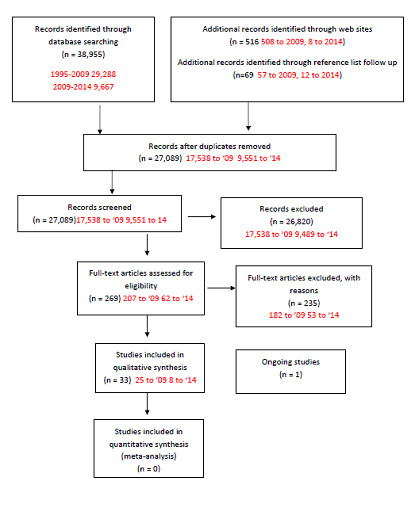
PRISMA diagram based upon Moher 2009.
1. Search results for electronic databases.
| Database | Number of hits |
| ASSIA | 1144 |
| British Nursing Index (BNI) | 105 |
| CINAHL | 2881 |
| Chinese atabase:CAJ,CCND,CPCD,CJSS,CMFD,CDFD, http://www.global.cnki.net/grid20/index.htm | 124 |
| Cochrane Library | 1841 |
| Cochrane Public Health Group Specialized Register | 31 |
| EMBASE | 4941 |
EPPI Centre
|
38 200 |
| ERIC | 416 |
| Health Management Information Consortium (HMIC) | 308 |
| LILACS | 416 |
| MEDLINE & MEDLINE In‐Process | 5691 |
| PsycINFO | 1315 |
| Sociological Abstracts | 874 |
| SPORTDiscus | 365 |
| Transport Database TRIS | 49 |
| Web of Science Science Citation Index, Social Sciences Citation Index and Conference Proceedings Citation Index |
9108 |
2. Search results for websites.
| Web sites | Hits |
| EU Platform on Diet, Physical Activity and Health | 0 |
| http://health‐evidence.ca | 5 |
| IUHPE (International Union for Health Promotion and Education) | 0 |
| NCCHTA http://www.ncchta.org | 1 |
| NICE guidelines http://www.nice.org.uk | 4 |
| SIGN guidelines http://www.sign.ac.uk | 0 |
| US Centres for Disease Control and Prevention http://www.cdc.gov/ | 0 |
| World Health Organisation http://www.who.int/en/ | 1 |
Included studies
Communities in the included studies
Twenty‐five of the included studies were set in high income countries (using the World Bank economic classification). Of these, 11 studies were conducted in North America (Brownson 2004; Brownson 2005; Eaton 1999; Goodman 1995; Luepker 1994; Mead 2013; Nafziger 2001; O'Loughlin 1999; Reger‐Nash 2005; Wilson 2014; Young 1996), three in Australia (Brown 2006; NSW Health 2002; Rissel 2010), one in Japan (Kamada 2013) and 10 in Europe (De Cocker 2007; Jenum 2006; Kloek 2006; Kumpusalo 1996; Lupton 2003; Osler 1993; Phillips 2014; Simon 2008; Solomon 2014; Wendel‐Vos 2009). Of the remaining eight studies, two were set in lower middle income countries: one in Pakistan (Nishtar 2007) and one in Vietnam (Nguyen 2012); and six were set in upper middle income countries: five in China (Gao 2013; Gu 2006; Guo 2006; Jiang 2008; Zhang 2003) and one in Iran (Sarrafzadegan 2009).
A total of 267 communities were included in the review. The size of the community in which the intervention took place varied greatly, from two small villages with a total population of less than 1000 inhabitants (Kumpusalo 1996) and clusters of villages greater than 500 (Solomon 2014) to a large region with a population of 1,895,856 (Sarrafzadegan 2009). Similarly, the location of the communities varied with 12 studies taking place in what could be considered rural or remote settings and the remaining 21 studies located in urban centres or cities.
Interventions in included studies
When assessed against the six categories, we found substantial differences in the combinations of interventions used in the included studies. Almost all of the interventions included a component of building partnerships with local governments or non‐government organisations (NGOs) (29 studies). Other strategies used in the interventions included some form of individual counselling by health professionals (20 studies), mass media campaigns (23 studies) or other communication strategies (26 studies). Some studies were delivered in specific settings (18 studies) and used environmental change strategies (14 studies).
Only four interventions that were investigated by the included studies contained elements of all six of the components described in the inclusion criteria (Brown 2006; Gao 2013; Goodman 1995; Luepker 1994) (see Methods section). Three interventions were comprised of five components, 10 of four components, seven of three components and two of two components (Table 4).
3. Categories of strategies included in interventions.
| Study | Mass Media | Other communication | Individual | Partnerships | Settings | Environmental | Total |
| Brown 2006 | X | X | X | X | X | X | 6 |
| Brownson 2004 | X | X | X | X | 4 | ||
| Brownson 2005 | X | X | X | X | 4 | ||
| De Cocker 2007 | X | X | X | X | X | 5 | |
| Eaton 1999 | X | X | X | X | 4 | ||
| Gao 2013 | X | X | X | X | X | X | 6 |
| Goodman 1995 | X | X | X | X | X | X | 6 |
| Gu 2006 | X | X | 2 | ||||
| Guo 2006 | X | X | X | 3 | |||
| Jenum 2006 | X | X | X | X | X | 5 | |
| Jiang 2008 | X | X | X | 3 | |||
| Kamada 2013 | X | X | X | X | 4 | ||
| Kloek 2006 | X | X | X | X | 4 | ||
| Kumpusalo 1996 | X | X | X | X | 4 | ||
| Luepker 1994 | X | X | X | X | X | X | 6 |
| Lupton 2003 | X | X | X | X | 4 | ||
| Mead 2013 | X | X | X | 3 | |||
| Nafziger 2001 | X | X | X | X | 4 | ||
| Nguyen 2012 | X | X | X | X | 4 | ||
| Nishtar 2007 | X | X | X | 3 | |||
| NSW Health 2002 | X | X | X | X | 4 | ||
| O'Loughlin 1999 | X | X | X | X | 4 | ||
| Osler 1993 | X | X | X | 3 | |||
| Phillips 2014 | X | X | X | 3 | |||
| Reger‐Nash 2005 | X | X | X | X | X | 5 | |
| Rissel 2010 | X | X | X | 3 | |||
| Sarrafzadegan 2009 | X | X | X | 3 | |||
| Simon 2008 | X | X | X | 3 | |||
| Solomon 2014 | X | X | X | X | X | 5 | |
| Wendel‐Vos 2009 | X | X | X | X | 4 | ||
| Wilson 2014 | X | X | X | X | 4 | ||
| Young 1996 | X | X | X | 3 | |||
| Zhang 2003 | X | X | 2 | ||||
| Total | 23 | 26 | 20 | 29 | 18 | 14 |
2 components ‐2 studies; 3 components ‐ 10 studies; 4 components ‐ 13 studies; 5 components ‐ 4 studies; 6 components ‐ 4 studies.
See Types of interventions for examples of suitable strategies which would be components of an integrated community wide strategy
Theoretical perspectives
Interventions were developed from a variety of theoretical perspectives, although many studies did not identify any such perspective in their papers. Nine of the studies sought to increase physical activity in a community by developing an intervention based on an ecological approach (Brown 2006; Brownson 2004; Brownson 2005; De Cocker 2007; Gao 2013; Jenum 2006; Mead 2013; Simon 2008; Wilson 2014). Six studies developed interventions with the stages of change model as their guiding framework (Kamada 2013; Kloek 2006; Luepker 1994; Phillips 2014; Reger‐Nash 2005; Rissel 2010) while four studies used the social learning model (Eaton 1999; Luepker 1994; O'Loughlin 1999; Osler 1993). Two studies used the community empowerment model for developing their interventions (Jenum 2006; Lupton 2003). Other theoretical approaches used included behaviour change of self‐efficacy (O'Loughlin 1999), persuasive communications theory (Luepker 1994), social cognitive theory (Mead 2013), active friendly environments (Solomon 2014), social marketing (Rissel 2010; Wilson 2014) and community organisation principles (Kloek 2006; Osler 1993). Of note, a number of studies described basing their interventions or components of interventions on multiple models. However, 11 did not explicitly state a theoretical model (Goodman 1995; Gu 2006; Guo 2006; Jiang 2008; Nafziger 2001; Nishtar 2007; NSW Health 2002; Sarrafzadegan 2009; Solomon 2014; Young 1996; Zhang 2003).
Intensity of Interventions
A subjective assessment of the intensity of each intervention was conducted based on the consideration of six criteria, as described in the methods section. Ten studies were judged to be high intensity, 14 of medium intensity and nine of low intensity (Table 5). The categorisation of high intensity was typically assigned to an intervention which acted on multiple levels within a community via multiple strategies as understood by the logic model (Figure 1). For example, the Brown 2006 study used mass media as well as other forms of communication to increase awareness of physical activity. The study also promoted self monitoring and goal setting using a website and provided access for individuals to pedometers and logbooks. Counselling by health professionals was another mode of intervention and a number of setting‐specific initiatives were conducted. The investigators also collaborated with the local government in improving the environment for physical activity by repairing walking tracks and creating signage and maps. Importantly, this intervention had the express intent of increasing the physical activity of the whole population, whereas some interventions included in this review targeted a range of behaviours other than physical activity. O'Loughlin 1999 was one such study which, with quite a modest budget (when compared to some of the larger interventions), employed multiple strategies in targeting smoking and diet along with physical activity. Given these factors it was considered to be of moderate intensity.
4. Assessment of intensity of the interventions.
| Study | High | Medium | Low | Unclear |
| Brown 2006 | X | |||
| Brownson 2004 | X | |||
| Brownson 2005 | X | |||
| De Cocker 2007 | X | |||
| Eaton 1999 | X | |||
| Gao 2013 | X | |||
| Goodman 1995 | X | |||
| Gu 2006 | X | |||
| Guo 2006 | X | |||
| Jenum 2006 | X | |||
| Jiang 2008 | X | |||
| Kamada 2013 | X | |||
| Kloek 2006 | X | |||
| Kumpusalo 1996 | X | |||
| Luepker 1994 | X | |||
| Lupton 2003 | X | |||
| Mead 2013 | X | |||
| Nafziger 2001 | X | |||
| Nguyen 2012 | X | |||
| Nishtar 2007 | X | |||
| NSW Health 2002 | X | |||
| O'Loughlin 1999 | X | |||
| Osler 1993 | X | |||
| Phillips 2014 | X | |||
| Rissel 2010 | X | |||
| Reger‐Nash 2005 | X | |||
| Sarrafzadegan 2009 | X | |||
| Simon 2008 | X | |||
| Solomon 2014 | X | |||
| Wendel‐Vos 2009 | X | |||
| Wilson 2014 | X | |||
| Young 1996 | X | |||
| Zhang 2003 | X | |||
| Total | 10 | 14 | 9 | 0 |
Intensity was assessed subjectively and independently based upon six characteristics as described in Data collection and analysis
The interventions studied by Gu 2006, Jiang 2008 and Zhang 2003 reached every individual in their target communities through quite substantial contacts such as repeated door‐to‐door visitation and health screening. The extensive reach of the intervention, combined with what was a potentially significant dose, led to their classification as high intensity interventions despite them being very different to Brown 2006. Conversely, most of the interventions judged as being of low level intensity had a much poorer reach into the communities. Indeed, several of the studies judged as being of low intensity were described by their authors as being of low intensity or low cost (Osler 1993; Simon 2008). In the case of Osler 1993, the low cost of the intervention was demonstrated in the limited amount of activity that took place compared to the more intense interventions. Similarly, Simon 2008 was judged as a low intensity intervention as, while it aimed to reach the whole community, the vast majority of its activities were targeted at one section of the community (in this case adolescents attending school). Overall, some studies appeared to have good reach (Gao 2013) whilst others (Solomon 2014) identified that very few residents were even aware of, and participated in, the intervention. Several of the studies provided descriptions of people participating in the components.
Outcome measures
To be included in the review, the study had to include a measurement of physical activity. A variety of dichotomous and continuous outcomes were used in these studies. Thirteen studies reported the proportion of participants attaining a certain level of physical activity (Brown 2006; Gao 2013; Jiang 2008; Kamada 2013; Kloek 2006; Lupton 2003; NSW Health 2002; Phillips 2014; Reger‐Nash 2005; Rissel 2010; Sarrafzadegan 2009; Solomon 2014; Wendel‐Vos 2009). The inverse of these outcomes was the reporting of the proportion of participants who were physically inactive, that is failing to attain a defined level of physical activity (Eaton 1999; Gao 2013; Goodman 1995; Jenum 2006; Nafziger 2001; Nguyen 2012; Osler 1993). Three other studies also reported the percentage of participants attaining a certain level of physical activity but prescribed that this had to have taken place during leisure time (Kumpusalo 1996; Luepker 1994; Nishtar 2007).
Time spent being physically active during leisure time (for example as hours per week) was also reported as a continuous outcome in three studies (De Cocker 2007; Simon 2008; Wendel‐Vos 2009). Other continuous outcomes of physical activity reported in the included studies included walking (Brownson 2004; Brownson 2005; De Cocker 2007; Wendel‐Vos 2009), energy expenditure (Kloek 2006; Phillips 2014; Sarrafzadegan 2009; Solomon 2014) and minutes in moderate‐vigorous physical activity each day (Wilson 2014).
Most of the included studies also measured other behaviours and health outcomes related to chronic disease. Behaviours measured included smoking, alcohol consumption, fruit and vegetable intake, fat and junk food intake and BMI. Other studies included speciality activity measures such as percentage of persons cycling. Knowledge and attitudes towards physical activity and health knowledge were reported in some studies. Health outcomes measured included chronic disease such as diabetes and hypertension, obesity and laboratory measures such as vitamin C, plasma and cholesterol levels. Reviewing the findings of these measures was not the objective of this review and so they have not been explored here.
Excluded studies
The Excluded studies table lists the studies that were excluded and the determined reasons. In several cases the studies were excluded for more than one reason. The predominant reasons for studies being excluded at this stage of the selection process were the study design (n = 84) or the intervention (n = 83) not meeting the inclusion criteria. In 42 cases the study was not designed in a way which could target the entire community, and in 28 cases the population sampled was not inclusive. In one case the study described the intervention without providing any results, in one case the report was inadequate and in five the measurement of physical activity was absent (deemed not likely to be the result of selective reporting of outcomes bias).
Risk of bias in included studies
The update has noted the increased use of randomisation in the allocation procedure and a significant improvement in the study design methodology from earlier studies. Earlier, all of the included studies were described as controlled before and after studies with the exception of one controlled ITS study (Luepker 1994) and one cluster cohort study (O'Loughlin 1999). Although the original review contained only one cluster RCT (Simon 2008), the updated review now includes an additional four RCTs: three cluster randomised studies (Kamada 2013; Phillips 2014; Wilson 2014) and one stepped wedge cluster randomised trial (Solomon 2014). This should be clearly understood as a change in the methodological approach of evaluation of community wide interventions. Each of these studies used a random selection of participants (representative sample) from the communities to participate in the measurement of outcomes.
All included studies were assessed for their risk of bias. Graphical presentation of the results of the risk of bias assessments of the individual studies and of the overall body of evidence are found in Figure 3 and Figure 4. In the earlier review no studies were identified as low risk of bias, however in this update four of the eight studies have been identified as low risk (Kamada 2013; Phillips 2014; Solomon 2014; Wilson 2014). Overall, 19 studies were identified as being at a high risk of bias (Brown 2006; Brownson 2004; De Cocker 2007; Gao 2013; Gu 2006; Guo 2006; Jenum 2006; Kumpusalo 1996; Lupton 2003; Mead 2013; Nguyen 2012; NSW Health 2002; O'Loughlin 1999; Osler 1993; Reger‐Nash 2005; Simon 2008; Wendel‐Vos 2009; Young 1996; Zhang 2003). Ten studies were found to have an unclear risk of bias (Brownson 2005; Eaton 1999; Goodman 1995; Jiang 2008; Kloek 2006; Luepker 1994; Nafziger 2001; Nishtar 2007; Rissel 2010; Sarrafzadegan 2009). Of those studies judged as at either high or unclear risk of bias only one of the studies was randomised, thus selection bias was a major risk for these studies. This was exacerbated as many of these studies only included one measurement point pre‐intervention and one post‐intervention, and in a number of the studies there were differences in important baseline characteristics between the study groups. We observed minor methodological deviations such as a change in the method of application of the survey questions from baseline to follow‐up (for example Phillips 2014). Where a singular minor methodological issue occurred which was deemed unlikely to change interpretation of the findings, we determined that an overall downgrading of the study to high risk was unwarranted.
3.
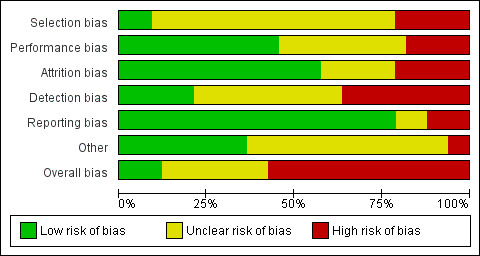
Risk of bias graph: review authors' judgements about each risk of bias item presented as percentages across all included studies.
4.
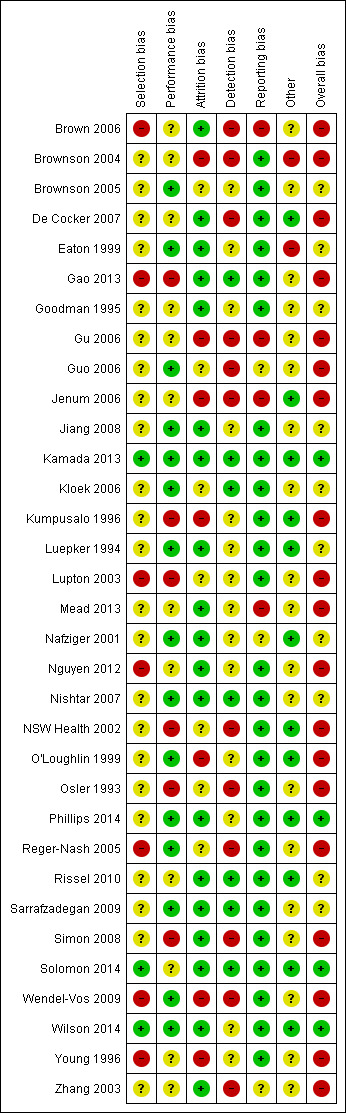
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
For the studies deemed to be low risk, allocation to the intervention and control occurred by randomisation (for example cluster RCT) rather than by purposeful allocation of the intervention community to communities which had the capacity to undertake the intervention rather than those which did not, such as Gao 2013. Non‐randomised controlled trials could also have been assessed as lower risk if the measurement was repeated pre and post‐intervention (to determine whether the changes were a result of trends toward the mean or the result of imprecision of the outcome measures). Low risk studies used measurement metrics that were both valid and reliable for population level interventions, avoided subjective self‐report assessment, and typically made over more than one day. Further, the individuals sampled should be representative of the population and include those difficult to reach. Studies at low risk of bias should, in the publication of results, include all of the measures stated in the study protocol and all of those reported in the initial publication of the study.
Selection bias
Selection bias was a major concern in the earlier review as only one study used randomisation to allocate communities (Simon 2008). Previously, no studies were judged as being at low risk of selection bias, although 19 studies were considered to have an unclear risk of bias (if the groups were comparable at baseline for important potential confounders; and if the assessors judged that if the communities were reversed it was likely that the same outcome would be achieved) (Brownson 2004; Brownson 2005; De Cocker 2007; Eaton 1999; Goodman 1995; Gu 2006; Guo 2006; Jenum 2006; Jiang 2008; Kloek 2006; Luepker 1994; Nafziger 2001; Nishtar 2007; NSW Health 2002; O'Loughlin 1999; Osler 1993; Sarrafzadegan 2009; Simon 2008; Zhang 2003). In this update, two of the new studies were identified as being at high risk of selection bias (Gao 2013; Nguyen 2012) and three unclear (Mead 2013; Phillips 2014; Rissel 2010). Four new randomised studies were considered to be at low risk of selection bias (Kamada 2013; Solomon 2014; Wilson 2014).
Performance bias
Collectively, 15 studies were judged as having a low risk of performance bias (Brownson 2005; Eaton 1999; Guo 2006; Jiang 2008; Kamada 2013; Kloek 2006; Luepker 1994; Nafziger 2001; Nishtar 2007; O'Loughlin 1999; Phillips 2014; Reger‐Nash 2005; Sarrafzadegan 2009; Wendel‐Vos 2009; Wilson 2014). While information on the blinding of communities was rare, these studies were judged as being at low risk of contamination and provided evidence of good integrity in the delivery of the intervention even though in some circumstances the intervention was clearly weak.
Attrition bias
Nineteen studies were assessed as being at low risk of attrition bias (Brown 2006; De Cocker 2007; Eaton 1999; Gao 2013; Goodman 1995; Jiang 2008; Kamada 2013; Luepker 1994; Mead 2013; Nafziger 2001; Nguyen 2012; Nishtar 2007; Phillips 2014; Rissel 2010; Sarrafzadegan 2009; Simon 2008; Solomon 2014; Wilson 2014; Zhang 2003). Potential for attrition bias was often not applicable through the cross‐sectional sampling of different individuals as representatives of the same population rather than following specific individuals through time. Some cohort studies had very high completion rates possibly related to recruitment intention of being resident in the community for the duration of the study (Mead 2013; Rissel 2010). There were no cases of communities withdrawing from the studies.
Detection bias
Twelve studies had a high risk of detection bias, 14 an unclear risk and 7 were low risk (Gao 2013; Kamada 2013; Kloek 2006; Nishtar 2007; Rissel 2010; Sarrafzadegan 2009; Solomon 2014). Assessment of detection bias included an assessment of the validity of the measurement tools and the quality of the outcome measures. In this update, one study used accelerometers to objectively measure physical activity.
Reporting bias
Four studies had a high risk of reporting bias (Brown 2006; Gu 2006; Jenum 2006; Mead 2013), with three assessed as being unclear (Guo 2006; Nafziger 2001; Zhang 2003) and 26 as low risk of bias. In the studies judged as having a high risk of reporting bias, there was evidence to indicate that outcomes important to the study were collected but not reported (as confirmed through communication with the authors). Ideally, access to study protocols would help with the process of accessing reporting bias, however in most cases this was not possible. Some studies did publish papers describing the intervention and evaluation methods prior to the final evaluation of the study thus enabling some scrutiny of reporting bias. Some studies with negative findings provided limited reporting of the outcomes and a preference towards the higher quality measurement instruments (for example Phillips 2014; Wilson 2014); however, with no likely impact upon the conclusions we determined them low risk for reporting bias.
Other bias
One study was judged as being at high risk of other bias (Brownson 2004), having had a 'head‐start' with several years of preparation in the intervention community prior to the program start, which was deemed to provide it with an advantage. The effect of this bias was unpredictable as it could have resulted in a null effect or been an effect modifier.
Effects of interventions
See: Table 1
Physical activity, dichotomous outcomes
Twenty‐seven studies reported physical activity as some form of dichotomous measure.
Fourteen studies reported physical activity measured as the attainment of a predefined amount of physical activity (Brown 2006; Brownson 2005; Gao 2013; Jiang 2008; Kamada 2013; Kloek 2006; Lupton 2003; NSW Health 2002; Phillips 2014; Reger‐Nash 2005; Rissel 2010; Sarrafzadegan 2009; Solomon 2014; Wendel‐Vos 2009) (Table 6; Figure 5). Only two of these studies, both based in China, found the intervention to be collectively effective across the whole population, in an intense intervention in urban Beijing (Jiang 2008) and Hangzhou China (Gao 2013). Lupton 2003 and Brown 2006 found the interventions to be effective in the male and female populations of the targeted communities respectively. The remaining studies found no evidence of effect.
5. Dichotomous outcomes ‐ physical activity.
| Study | Overall bias | Measure | Definition | Net % change | Unadjusted RD | Adjusted RD (95% CI) | Unadjusted RR (95% CI) | Adjusted RR (95% CI) | Baseline |
| Brown 2006 | High risk of bias | % physically active | 150 minutes of activity in at least 5 separate sessions in the last week | 15.40 | 0.9 | 7.33 (‐23.48 ‐ 38.13) | 1.02 | 1.18 (0.60 ‐ 2.35) | 41.9 |
| Gao 2013 | High risk of bias | % Moderate or high physically active | Categories on IPAQ | 3.34 | 7.4 | 2.50 (1.17 ‐ 3.83) | 1.10 | 1.03 (1.01 ‐ 1.05) | 70.5 |
| Jiang 2008 | Unclear risk of bias | Regular physical activity | Not provided | 18.12 | 6.38 | 10.75 (5.23 ‐ 16.27) | 1.24 | 1.20 (1.09 ‐ 1.31) | 60.39 |
| Kamada 2013 | Low risk of bias | % physically active | Engaging in 150mins/week or more of walking, engaging in daily flexibility or engaging in 2 or more days a week of in muscle strengthening activities (All groups vs. control) |
‐0.17 | ‐1.6 | 0.00 (0.0‐0.0) | 0.973 | 1.00 (0.99‐1.00) | 63.0 |
| Low risk of bias | % physically active | Engaging in 150mins/week or more of walking, engaging in daily flexibility or engaging in 2 or more days a week of in muscle strengthening activities (Aerobic exercise group vs. control) |
‐2.80 | 0.000 | ‐2.0 | 1.00 | 0.97 | 66.6 | |
| Low risk of bias | % physically active | Engaging in 150mins/week or more of walking, engaging in daily flexibility or engaging in 2 or more days a week of in muscle strengthening activities (Aerobic exercise and strengthening group vs. control) |
0.41 | ‐0.3 | 0.30 (‐4.56 ‐ 5.16) | 1.00 | 1.00 (0.94 ‐ 1.08) | 64.0 | |
| Kloek 2006 | Unclear risk of bias | % physically active | At least 30 minutes of moderate‐intensity physical activity on at least 5 days a week | ‐7.36 | ‐1 | ‐3.97 (5.02 ‐ ‐12.95) | 1.04 | 0.93 (0.79 ‐1.10) | 59.0 |
| Lupton 2003 | High risk of bias | % physically active | Minimum of four hours of weekly moderate PA during the last year | 9.84 | 8.3 | 6.87 (‐13.04 ‐ 26.78) | 0.98 | 1.10 (0.84 ‐ 1.43) | 72.5 |
| NSW Health 2002 | High risk of bias | % physically active | Engaged in at least 150 minutes and five sessions of moderate activity or three sessions of vigorous activity per week | 7.14 | ‐0.2 | 3.39 (‐0.29 ‐ 7.08) | 1.14 | 1.08 (0.99 ‐ 1.17) | 49.2 |
| Phillips 2014 | Low risk of bias | % meeting | Physical activity: 5x30 minutes per week | 7.89 | 1.9 | 5.00 (‐2.879 ‐ 12.879) | 1.029 | 1.079 (0.957 ‐ 1.216) | 63.4 |
| Reger‐Nash 2005 | High risk of bias | % physically active | Moderate activity at least 30 minutes for at least 5 days per week or vigorous activity at least 20 minutes for at least 3 days per week | 0.36 | 1.2 | 0.38 (‐0.06 ‐ 0.82) | 1.15 | 1.01 (0.10 ‐ 1.01) | 46.9 |
| Rissel 2010 | Unclear risk of bias | % physically active | undertaking 150 min/week | ‐5.55 | ‐5.0 | ‐2.8(‐6.47 ‐ 0.873) | 0.907 | 0.951 ( 0.891 ‐1.015) | 44.9 |
| Sarrafzadegan 2009 | Unclear risk of bias | % physically active | Individuals with >= 30 minutes/day of moderate or vigorous activity | 4.17 | 2.1 | 1.89 (‐0.23 ‐ 4.02) | 1.07 | 1.06 (1.00 ‐ 1.14) | 47.0 |
| Solomon 2014 | Low risk of bias | % physically active | Did sufficient physical activity to meet the current United Kingdom physical activity guidelines (at least 150 minutes of moderate‐intensity activity per week in bouts of 10 minutes or more, or at least 75 minutes of vigorous intensity activity per week | 1.03 | NA | NA | NA | 1.02 (0.88 ‐ 1.17)† | 66.9 |
| Wendel‐Vos 2009 | High risk of bias | % physically active | 150 min/week and at least 5 sessions per week, and physically active at least 30 min/day at least 5 days a week | ‐3.50 | ‐0.7 | ‐1.60 (‐0.10 ‐ ‐3.10) | 0.86 | 0.97 (0.93 ‐ 1.00) | 42.8 |
RD = Risk difference
RR = Relative Risk
† Data as presented by the study authors. Odds ratio of adjusted comparison (Intervention minus control in stepped wedge cluster randomised controlled design, p‐value = 0.80, ICC 0.008. Baseline represents baseline for all..
5.
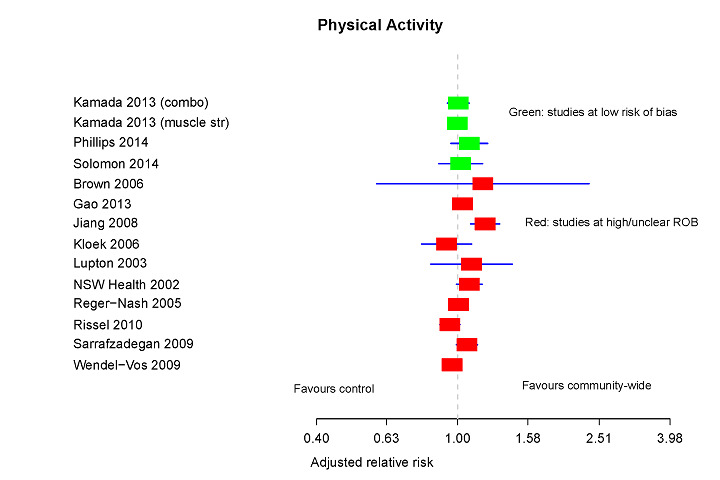
Forest plot of dichotomous outcomes of meeting a criteria of being physically active ‐ mixed measures and study designs by risk of bias.
Jiang 2008 reported an increase in regular physical activity (we calculated an adjusted RR 1.20, 95% CI 1.09 to 1.31) for an intervention involving intensive contact with individuals in urban communities in Beijing. The intervention had very substantial penetration into the community with quarterly door‐to‐door distribution of handouts, counselling by health practitioners, and the identification of those within the community with high risk factors through an intensive individual screening campaign in which 73% of the community participated. Gao 2013 also reported a small but statistically significant increase (adjusted RR 1.03, 95% CI 1.01 to 1.05). This intervention was a multi‐component high intensity intervention and the study was at high risk of bias as the authors allocated communities to the control arm which did not have the capacity to support the intervention.
The Finnmark Intervention study (Lupton 2003) aimed at improving cardiovascular health in a small arctic community in Norway, and reported a significant increase (P = 0.047) in males being physically active, as defined as accruing a minimum of four hours of moderate physical activity over a week during the last year. This was measured six years after the initial baseline measurement and commencement of an intervention which involved the engagement of the community largely through activities run by sporting clubs and associations. Unfortunately, no significant change was found in the female population (P = 0.151) as reported by the authors and the calculated adjusted RR for the entire population was non‐significant (RR 1.10, 95% CI 0.84 to 1.43).
Conversely, the Rockhampton 10,000 Steps Project conducted in a regional Australian community found an increase in the proportion of physically active females (achieving 150 minutes of activity in at least five separate sessions over the last week) but not males (Brown 2006). The interpretation of these findings was complicated as the control community was significantly more active than the comparison community at baseline (OR 0.77, 95% CI 0.65 to 0.93). At follow‐up, two years later, there was no longer a significant difference with the percentage of the comparison community categorised as being active decreasing by 6.4% while the intervention community increased 0.9%. Combined, there was once again no difference between the two populations (adjusted RR 1.18, 95% CI 0.60 to 2.35).
No evidence of effectiveness was found in the three studies at low risk of bias. Phillips 2014 found no increase in the percentage of people meeting the target of 5 x 30 minutes per week (adjusted RR 1.03, 95% CI 0.96 to 1.22) and, similarly, Solomon 2014 did not find an increase in the percentage meeting the UK recommendation of at least 150 minutes of moderate‐intensity activity per week in bouts of 10 minutes or more, or at least 75 minutes of vigorous‐intensity activity per week (RR 1.02, 95% CI 0.88 to 1.17). Further, in Japan Kamada 2013 in three comparisons, controlled versus muscle strengthening versus aerobic activity versus combined, found no statistical increases in either arm of the intervention analysed (adjusted RR 1.00, 95% CI 0.99 to 1.00; RR 0.97 (confidence interval could not be calculated); RR 1.00 95% CI 0.94 to 1.10).
The Isfahan Healthy Heart program aimed to improve the health of a large population (> two million) through a multi‐strategic, large scale intervention (Sarrafzadegan 2009). The adjusted RR of 1.06 (95% CI 0.99 to 1.14) suggested a small increase in the percentage of the population with greater than, or equal to, 30 minutes per day of moderate or vigorous activity, although this was not found to be statistically significant. This result needs to be understood in the context of a decreasing trend in physical activity in both the intervention and comparison groups. Further, for the continuous outcome energy expenditure, a decrease was observed.
Wendel‐Vos 2009 reported no effect on the percentage of participants meeting the study's target of 150 minutes per week and at least five sessions per week in the Maastricht region of the Netherlands, following a large five‐year project aiming to improve individuals' chronic disease risk factors (adjusted RR 0.97, 95% CI 0.93 to 1.0). Also, targeting several health‐related behaviours, Kloek 2006 reported on an intervention targeting socioeconomically deprived neighbourhoods in Eindhoven, the Netherlands. No effect was found on the proportion of the population attaining at least 30 minutes of moderate‐intensity physical activity on at least five days in a week (adjusted RR 0.93, 95% CI 0.79 to 1.10).
In investigating a mass media dominated intervention aimed at increasing walking behaviour, Reger‐Nash 2005 found no effect on moderate activity of at least 30 minutes for at least five days per week or on vigorous activity for at least 20 minutes on at least three days per week (adjusted RR 1.00, 95% CI 1.00 to 1.01).
NSW Health 2002 reported no statistically significant effects on physical activity, defined as those individuals engaged in at least 150 minutes and five sessions of moderate activity or three sessions of vigorous activity per week, for a short intervention aimed at increasing the use of parks and walking. The calculated adjusted RR was 1.08 (95% CI 0.99 to 1.17) with the interpretation of this finding complicated by a decrease in physical activity attainment in both the intervention and the comparison communities. This was demonstrated with the risk difference (RD) for the intervention being ‐0.2. Similarly, Rissel 2010, with an emphasis on cycling, used the same outcome measures and found no increase (adjusted RR 0.95, 95% CI 0.89 to 1.02).
A further study did report on the number of people involved in physical exercise, however we could not obtain a definition of physical exercise (Guo 2006). Given this, interpretation of the results of this study conducted in rural villages in China was difficult (and this study was not included in Table 6). This was further complicated as the villages were not comparable at baseline for the number of people undertaking physical activity (34.6%, 95% CI 29.7 to 40.2; 6.2%, 95% CI 12.2 to 20.8). The study did conclude there was a significant difference in the number of people undertaking physical exercise between the intervention and control villages over the period of the study (change of 27%; P value not found).
Three studies reported the measure of leisure time physical activity (Kumpusalo 1996; Luepker 1994; Nishtar 2007) (Table 7; Figure 6). Two studies, one set across a large region in Pakistan (Nishtar 2007) and the other in Finnish villages (Kumpusalo 1996), found no evidence of effect. One of these studies, the Minnesota Heart Health Program, found some evidence of effectiveness although this was not consistent across the different sampling methods used in the study nor over the time span of data collection (Luepker 1994).
6. Dichotomous outcomes ‐ physical activity during leisure time.
| Study | Overall bias | Measure | Definition | Net % change | Unadjusted RD | Adjusted RD (95% CI) | Unadjusted RR | Adjusted RR (95% CI) | Baseline |
| Luepker 1994 | Unclear risk of bias | PA during leisure time | Regularly active during leisure time | a11.26 | 8.5 | 5.35 (‐3.32 ‐ 14.02) | 1.08 | 1.11 (0.94 ‐ 1.30) | 48.6 |
| b9.4 | 4.3 | 4.70 (‐1.64 ‐ 11.04) | 1.09 | 1.08 (0.97 ‐ 1.20) | 49.4 | ||||
| Kumpusalo 1996 | High risk of bias | PA during leisure time | Undertaking physical activity during leisure time > 3 times weekly | ‐1.76 | 0.6 | ‐0.64 (‐8.24 ‐ 6.96) | 1.02 | 0.98 (0.80 ‐ 1.21) | 39.0 |
| Nishtar 2007 | Unclear risk of bias | PA during leisure time | Not provided | ‐25.58 | 2.5 | 0.52 (‐0.04 ‐ 1.08) | 2.41 | 0.88 (0.77 ‐ 1.02) | 3.0 |
adata from independent surveys
bdata from cohort surveys
RD = Risk difference
RR = Relative Risk
6.
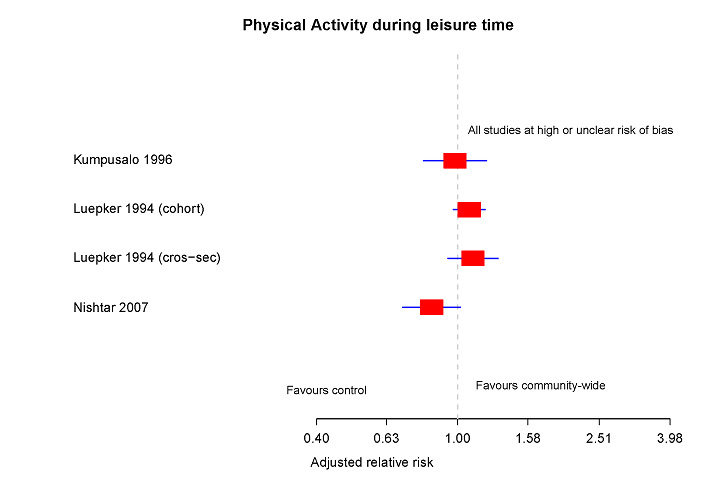
Forest plot of dichotomous outcomes of meeting a criteria of being physically active during leisure time ‐ mixed measures and study designs.
Luepker 1994 reported the findings of a large scale, high intensity, long‐term cardiovascular disease prevention intervention called the Minnesota Heart Health Program. In this study, six communities were matched, with one community of each pair non‐randomly selected to receive this large scale, five to six‐year intervention. Independent cross‐sectional samples of 300 to 500 randomly selected adults were surveyed periodically, including multiple measurements during the 16‐month baseline period and then at one, three, five and six years post‐implementation. Concurrently, a cohort randomly selected from the pre‐intervention cross‐sectional surveys (n = 7097) were re‐surveyed at baseline, two, four and seven years post‐intervention (end of study follow‐up 67.1%), although alternate halves of the cohort group were surveyed at two and four years. The authors presented the pooled data at the various measurement points adjusted for age, gender and education. They reported that the cross‐sectional surveys found the intervention communities to have a significantly greater proportion of the population being physically active during leisure time at one and three years; at five and six years there was no longer a statistically significant difference despite trending higher (P values not provided). The cohort data found no significant differences at two and four years, however there was a statistically significant difference at seven years post‐intervention (P values not provided). The adjusted RR calculated using data extracted from year zero and the final year of measurement was 1.11 (95% CI 0.94 to 1.30) for the cross‐sectional data and 1.08 (95% CI 0.97 to 1.20) for the cohort data, respectively.
Nishtar 2007 reported on the Heartfile Lodhran CVD project aimed at cardiovascular disease prevention in Pakistan. The authors reported no change in leisure time physical activity (adjusted RR 0.84, 95% CI 0.70 to 1.02).
In a study set in Finnish villages (Finnish Healthy Village Study), Kumpusalo 1996 found that the intervention was not associated with improvements in the physical activity patterns of people living in rural villages. The adjusted RR was 0.98 (95% CI 0.80 to 1.21).
An additional study reported on the effectiveness of an intense community intervention in Shandong, China for the similar outcome of non‐occupational physical activity (Zhang 2003). This study found no difference in the relative proportion of the intervention community found to be physically active pre and post‐measurement (P > 0.05), although over the same time the authors reported a significant reduction in the proportion of the control community who were physically active (P < 0.05).
Seven studies reported a dichotomous measure of physical inactivity, that is the proportion of people who failed to attain a defined level of activity (Eaton 1999; Gao 2013; Goodman 1995; Jenum 2006; Nafziger 2001; Nguyen 2012; Osler 1993) (Table 8; Figure 7). Of the remaining studies, the Romsas in motion study showed some evidence that the three‐year, multi‐strategic intervention was effective at decreasing the proportion of a population in a low socio‐economic district in Oslo, Norway not engaging in heavy physical activity (Jenum 2006). Eaton 1999, Nafziger 2001, Osler 1993 and Goodman 1995 all found the community wide interventions that they investigated not to be effective.
7. Dichotomous outcomes ‐ physically inactive or sedentary.
| Study | Overall bias | Measure | Definition | Net % change | Unadjusted RD | Adjusted RD (95% CI) | Unadjusted RR | Adjusted RR (95% CI) | Baseline |
| Eaton 1999 | High risk of bias | Physically inactive (%) | used different criteria for physical inactivity combined questions XS1, XS2 (exercise <1 times per week on average), XS5 & XS6 (=0 days of sweat related physical activity) (not validated measures). Men <=35 yo |
1.77 | ‐20.3 | 0 | 1.08 | 1.03 | 50.2 |
| Men >35 | 0.09 | 1.9 | 0 | 0.98 | 1.00 | 53.6 | |||
| Women <=35 yo | ‐0.18 | ‐8.2 | 0 | 0.99 | 1.00 | 56.2 | |||
| Women >35 yo | ‐0.09 | ‐6.1 | 0 | 0.99 | 1.00 | 62.6 | |||
| Gao 2013 | High risk of bias | Low physical activity (%) | IPAQ category | ‐8.76 | ‐7.3 | ‐2.30 (‐3.39 ‐ ‐1.01)) | 0.77 | 0.91 (0.86 ‐0.95) | 29.4 |
| Goodman 1995 | Unclear risk of bias | Physically inactive (%) | Physically inactive was defined as engaging in no physical activity or exercise during the last month | ‐1.82 | ‐1.7 | ‐1.02 (‐3.03 ‐ 0.99) | 0.97 | 0.99 (0.96 ‐ 1.01) | 44.6 |
| Jenum 2006 | High risk of bias | Physically inactive | No heavy physical activity in leisure time or commuting (%) | 20.04 | 12.9 | 8.13 (5.25 ‐ 10.99) | 1.36 | 1.20 (1.12 ‐1.28) | 40.5 |
| Nafziger 2001 | Unclear risk of bias | Physically inactive (%) | Described as self‐reported sedentary life‐style unless they were involved in a physical activity strenuous enough to work up a sweat <3 times/week | ‐15.85 | ‐7.8 | ‐11.43 (‐23.06 ‐ 0.21) | 0.89 | 0.84 (0.71 ‐ 1.00) | 72.5 |
| Nguyen 2012 | High risk of bias | Physically inactive (%) | Total physical activity less than 3,000 MET‐minutes per week (all) | 71.26 | 4.9 | 5.63 (2.64 ‐ 8.62) | 1.51 | 1.65 (1.26 ‐ 2.16) | 8.0 |
| Total physical activity less than 3,000 MET‐minutes per week (men) | 45.24 | 5.8 | 4.82 (0.99 ‐ 8.65) | 1.50 | 1.35 (1.06 ‐ 1.72) | 10.0 | |||
| Total physical activity less than 3,000 MET‐minutes per week (women) | 93.44 | 4.44 | 6.43 (1.85 ‐ 11.02) | 1.52 | 1.98 (1.21 ‐ 3.24) | 6.8 | |||
| Osler 1993 | High risk of bias | Physically inactive (%) | No details provided | 20.51 | 0.1 | 2.07 (‐125.30 ‐ 129.45) | 1.00 | 1.16 (extreme 95% CI crossing 1)a | 13.0 |
This table contains data where % inactive, not undertaking sufficient PA, or classed as achieving a level of PA defined as low or inactive.
Eaton 1999 did not provide a sufficient breakdown of the respective sample sizes to calculate 95% CI. Author was contacted for further details, no reply was provided.
RD ‐ Risk difference
RR ‐ Relative Risk
a Due to small numbers, the confidence interval for the adjusted 95% using Wald‐test yields extreme values.
7.
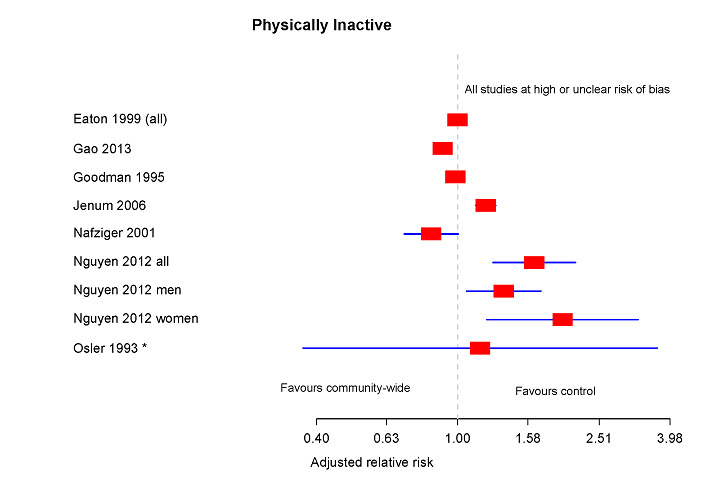
Forest plot of dichotomous outcomes of meeting a criteria of being physically inactive ‐ mixed measures and study.
The Romsas in motion study was a controlled before and after study with a cohort follow‐up panel (Jenum 2006). After a three‐year follow‐up it reported that the percentage of respondents not achieving heavy physical activity sufficient to make them sweat and feel out of breath was significantly smaller in the intervention population, with a pre‐post reduction during the study period in the intervention district of 8.1% (95% CI 2.4 to 13.8; P = 0.005). However, the calculated adjusted RR for the whole study was 0.8 (95% CI 0.59 to 1.08). As has been the case with other studies, these findings were complicated by the differences between the two communities at baseline. In this situation, the intervention community had a 5% higher baseline inactivity proportion as compared to the control community.
The Ostego‐Schoharie health heart program targeted the prevention of cardiovascular disease in rural USA through a hospital based intervention. This study collected both cross‐sectional data and cohort data at baseline and at five‐year follow‐up (Nafziger 2001). The cross‐sectional data were reported as a non‐significant reduction in self‐reported physically inactive lifestyle in the intervention population. Our analysis of the extracted results found an adjusted RR of 0.84 (95% CI 0.71 to 1.00). The cohort data also reported no evidence of effect with both the intervention and control communities decreasing in the proportion found to be inactive (P > 0.05).
The Osler 1993 study reported an increase in physical inactivity in both the intervention and control communities of rural municipalities in Denmark. The calculated adjusted RR of 1.16 (having an extreme 95% CI crossing 1), which suggested the intervention group was more physically inactive after the intervention as compared to the control group, was not statistically significant. Nguyen 2012, in rural Vietnam, found a significant failure of the intervention at a population level (adjusted RR 1.65, 95% CI 1.16 to 2.16), less so for men (adjusted RR 1.35, 95% 1.06 to 1.72) and most detrimental for females (adjusted RR 1.98, 95% CI 1.21 to 3.24), from relatively low levels of physical activity. The intervention fared worse than the control in advancement of inactivity within the community.
Goodman 1995 also found no difference between the intervention and control groups for physical inactivity in a chronic disease prevention project in an urban US setting (adjusted RR 0.99, 95% CI 0.96 to 1.01).
Three studies reported leisure time physical activity (Kumpusalo 1996; Nishtar 2007; O'Loughlin 1999). None demonstrated evidence of effectiveness.
Nishtar 2007 investigated an intervention aimed at increasing the physical activity levels in a large regional population in Pakistan. The investigators found no difference between the intervention and comparison populations in recreation or leisure time physical inactivity (P values not reported). Similarly, Kumpusalo 1996 reported no difference in leisure time physical inactivity in the Finnish Healthy Village study (P > 0.05) and O'Loughlin 1999 found no difference in an intervention targeting a low income, inner city neighbourhood in Montreal, Canada (P = 0.063).
Two studies reported the attainment of vigorous activity (NSW Health 2002; Young 1996).
The Stanford five‐city project, based in California, found inconsistent and limited intervention effects between intervention cities and control cities for behavioural measures of physical activity (Young 1996). In this study, independent cross‐sectional surveys were conducted at baseline, 25, 51 and 73 months (n = 1800 to 2500 participants). Those who participated at baseline also comprised a cohort who were sampled at 17, 39 and 60 months (n = 907). The percentage of men who regularly engaged in at least one vigorous activity did significantly differ over time between the treatment and control cities (P < 0.004), although this increase was not found in the cohort sample (P = 0.068) nor in an independent (P = 0.237) or cohort sample of women (P = 0.842).
The NSW Health study also reported the percentage of people engaging in physical activity and found no difference between the intervention and treatment groups (P = 0.077) (NSW Health 2002).
Physical activity, continuous outcomes
Eleven of the included studies reported continuous measures of physical activity.
Three studies reported leisure time physical activity measured by time (De Cocker 2007; Simon 2008; Wendel‐Vos 2009) (Table 9) with each of the three studies showing some evidence of effectiveness, however only Simon 2008 reported an increase in physical activity levels.
8. Continuous outcomes ‐ leisure time physical activity.
| Study | Measure | Subgroup | Post mean difference | Adjusted mean difference | Adjusted % change relative to the control mean | Baseline value | Timeline |
| De Cocker 2007 | Leisure time PA (hours/week) | No subgroup‡ | 0 | 0.53 | 25.60 | 2.33 | 1 year |
| Simon 2008 | Supervised leisure time physical activity (hours/week) | Measured only in children† | 0.9 | 1.1 | 43.14 | 2.5 | 4 years |
| Wendel‐Vos 2009 | Leisure time PA (hours/week) | Men (NS) | ‐0.2 | ‐0.4 | ‐2.06 | 19.8 | 5 years |
| Women‡ | ‐4.4 | 2.2 | 14.01 | 11.7 |
† authors reported a statistically significant increase (P < 0.05) in favour of the community
‡authors reported a statistically significant difference ( P < 0.05), however there was no observed increase in PA
NS ‐ no statistically significant difference
Wendel‐Vos 2009 reported on a regional cardiovascular disease prevention program in Limburg, Netherlands. Total leisure time physical activity was reported for both males and females. Both groups decreased their leisure time physical activity between baseline and follow‐up at five years, with no difference between the intervention and control groups for men. In women, however, the reduction in leisure time physical activity in the intervention group was significantly less then in the control group (P < 0.05).
Leisure time physical activity also decreased from baseline to follow‐up in both the intervention and control communities in the Ghent 10,000 steps study (De Cocker 2007). Importantly, this reduction was significantly greater in the control group than the intervention group (P ≤ 0.05) with the adjusted percentage change calculated as 25.60%. The authors reported that in addition to leisure time physical activity there were significant intervention effects for a range of physical activity outcomes including moderate physical activity (minutes per week) and work‐related physical activity (minutes per week) but not vigorous physical activity, transport‐related physical activity and household physical activity.
Simon 2008 reported the results of a cluster RCT of an intervention based predominantly in a school setting. It reported an adjusted change in supervised leisure time physical activity of 43% in adolescents and an adjusted mean difference of 1.1 hour per week (95% CI 0.56 to 1.63) in leisure time physical activity at four years post‐baseline. This was a statistically significant difference between the intervention and control groups (P < 0.0001).
Four studies reported a continuous measure of walking (Brownson 2004; Brownson 2005; De Cocker 2008; Wendel‐Vos 2009) (Table 10). Two of the studies (De Cocker 2007; Wendel‐Vos 2009) reported some evidence of effectiveness although two that were conducted in the same population in Missouri, USA found no evidence of increased time spent walking (Brownson 2004; Brownson 2005).
9. Continuous outcomes ‐ walking.
| Study | Measure | Sub group | Post mean difference | Adjusted mean difference | Adjusted % change relative to the control mean | Baseline value | Timeline |
| Brownson 2004 | 7 day total walking (mean min/week) (NS) | N/A | ‐5.3 | ‐1.4 | ‐1.38 | 97.2 | 2 years |
| 7 day walking for exercise (mean min/week) (NS) | N/A | ‐0.1 | ‐5.6 | ‐17.61 | 37.3 | ||
| Brownson 2005 | Walking (mean min/week) (NS) | N/A | ‐0.8 | 5.2 | 4.75 | 97 | 1 year |
| De Cocker 2007 | Pedometer‐determined (steps/day)† | N/A | 957 | 1030 | 10.80 | 9597 | 1 year |
| Walking (min/week)† | N/A | 34 | 47 | 17.34 | 288 | ||
| Wendel‐Vos 2009 | Walking (hours/week)‡ | Male (NS) | ‐0.4 | ‐1.1 | ‐12.09 | 8.5 | 5 years |
| Women | 2.4 | 2.6 | 38.24 | 8.9 |
NS ‐ authors reported no statistically significant difference
† authors reported a statistically significant increase (P < 0.001) in favour of the intervention community
‡ authors reported as a statistically significant difference ( P < 0.05), however there was no observed increase in PA for the intervention community
In an evaluation of a large, expensive five‐year intervention in a region in the Netherlands, Wendel‐Vos 2009 reported a small decrease in walking time per week in males in the intervention group compared to the comparison group (adjusted change ‐12.09%), however this was not found to be statistically significant (P > 0.05). Despite a reduction in walking hours per week in women from both groups, there was a larger reduction in the control community than the intervention community (adjusted change 29.41%) with the intervention group found to be statistically significantly different (or having less of a reduction) than the control community (P ≤ 0.05).
The Ghent 10,000 steps study reported a statistically significant increase in walking measured with a pedometer (steps per day) (P < 0.01) and self‐reported walking (minutes per week) (P < 0.01). The adjusted changes were 10.8% and 17.34%, respectively (De Cocker 2007).
Two studies conducted in a rural area of Missouri reported measures of walking. Brownson 2004 found no difference between the communities in seven‐day total walking (P = 0.91) and seven‐day walking for exercise (P = 0.37). A later study reported on the mean rates of walking per week and found that the intervention and control communities were not statistically significantly different (P value not reported) (Brownson 2005).
Five studies reported continuous measures of energy expenditure (Gao 2013; Kloek 2006; Phillips 2014; Sarrafzadegan 2009; Solomon 2014) (Table 11).
10. Continuous outcomes ‐ energy expenditure.
| Study | Measure | Post mean difference | Adjusted mean difference | Adjusted % change relative to the control mean | Baseline value | Timeline |
| Gao 2013 | Physical activity MET ‐ min/week† | 462 | 176 | 38.09 | 1204 | 2 years |
| Kloek 2006 | METs/week (NS) | 81 | ‐241 | ‐3.54 | 7253 | 2 years |
| Phillips 2014 | METS/week score (NS) | 4.2 | ‐113 (95% CI ‐ 847‐ 621)* | n/a | 2626 (95% CI 1978 to 3279) | 3‐4 years |
| Sarrafzadegan 2009 | Total daily PA (MET‐m/week ± SD) (P<0.01)b | ‐65 | ‐51 | ‐8.46 | 606 | 3 years |
| Leisure time PA (MET‐min/week) (P<0.01)b | ‐2 | ‐3 | ‐2.83 | 85 | 3 years | |
| Solomon 2014 | METs/week (NS) | 155 | 171 (95%CI: ‐16 ‐ 358) p=0.07a | n/a | 2561 (SD=2977) | Stepped wedge design ˜ 12 months follow up |
*Adjusted analysis adjusted for age, gender, ethnicity, education, employment, appropriate baseline values
a Adjusted analysis adjusted for period, gender, age and area as reported by the authors
b When compared to the control, the authors reported a statistically significant decrease in physical activity for the intervention group.
† authors reported a statistically significant increase (P < 0.05) in favour of the intervention
MET‐ metabolic equivalent of task
The Isfahan Healthy Heart program aimed to improve the health of a large population (> two million) through a multi‐strategic, large‐scale intervention (Sarrafzadegan 2009). This study reported total daily physical activity as well as leisure time physical activity, expressed as metabolic equivalent of task (MET), in minutes per week. The MET is commonly used as a means of expressing the energy cost of physical activity as the ratio of the metabolic rate of any activity to the metabolic rate at rest. The total daily physical activity (MET) decreased in both the intervention and comparison areas over the three years of evaluation. This decrease was significantly greater in the comparison area then the intervention area (‐114 versus ‐68 MET minutes per week; P < 0.05). The intervention and control areas did increase for leisure time physical activity (MET) with the difference at the final evaluation being significantly different (P < 0.01) with an adjusted change of 12.26%.
Kloek 2006 reported on an intervention targeting deprived neighbourhoods in Eindhoven, Netherlands. The study found no evidence of an increase in energy expenditure in the intervention group as compared to the comparison groups at two years post‐baseline (P = 0.95). In the UK, both Phillips 2014, using an intervention targeting socio‐economically disadvantaged neighbourhoods of London, and Solomon 2014, in rural villages of Devon, found no evidence of an effect. However, Gao 2013 using a two‐year intervention in China with communities selected on the basis of their capacity to support the intervention against a control with no capacity found an adjusted mean difference of 176 MET minutes/week.
One study (Wilson 2014) reported the average daily minutes of moderate to vigorous physical activity (MVPA) (Table 12). As a study at low risk of bias, Wilson 2014 reported on an intervention which focused primarily upon an environmental intervention with social marketing emphasising walking and access to walking trails in underserved African American communities. The study measured the average daily minutes of moderate to vigorous physical activity using two methods: with accelerometry, and four‐month recall. Data on the individual level accelerometry, noted by the authors as representing the program effects upon individuals who were representative of the community, were analysed with a mixed model ANCOVA. They examined potential differences between the community estimates that differed across the communities. The analysis revealed no significant differences by communities from baseline, months 12, 18 and 24 for MVPA, indicating that the intervention did not have a broader effect at a population level. However, the authors did observe a more immediate intervention or program level impact of the walking programs using attendance and stationary observations of walking. The multi‐strategy community increased from 40 to 400 walkers per month by 9 months, and the intervention program level effects were sustained with over 200 walkers per month on average. The two samples analysed were not linked.
11. Continuous outcomes ‐ physical activity.
| Study | Measure | Estimate of effect for full intervention | Baseline value | Timeline |
| Wilson 2014 | Average daily minutes of moderate to vigorous PA Measured by acceleratory (7‐day estimates) (NS) |
0.69 (SE 0.39); 95% CI: ‐0.14 ‐ 1.39) | 35.96 (SE 4.17) | Measured 6, 12 & 24 months |
| Wilson 2014 | Average daily minutes of moderate to vigorous PA self‐reported 4 month recall |
data unavailable, only more robust measurement of PA reported |
SE ‐ standard error
NS ‐ authors reported no statistically significant difference
Average daily minutes of MVPA is on the square root scale. Analysis as reported by the author using a mixed model ANCOVA implemented to examine difference between communities in accelerometer‐assessed MVPA, random effects for individuals over time.
We noted that the self‐reported measures of MVPA were not included in the published reports. It seems the authors opted to publish only the more valid accelerometry measures, which were neither clinically meaningful nor statistically significant.
More intense studies
Ten of the studies included in the review were classified as being of high intensity based upon the subjective assessment described in the methods section (Brown 2006; Eaton 1999; Gu 2006; Jiang 2008; Luepker 1994; Lupton 2003; Nafziger 2001; Wendel‐Vos 2009; Wilson 2014; Zhang 2003).
Several of these studies reported some improved physical activity outcomes (Brown 2006; Jiang 2008; Luepker 1994; Lupton 2003; Zhang 2003) however this finding was inconsistent, with several studies finding no effect (Eaton 1999; Nafziger 2001; Wendel‐Vos 2009; Wilson 2014) and one study selectively not reporting the study outcome of physical activity (Gu 2006).
Higher quality studies
Four newly published studies were deemed to be high quality studies (Kamada 2013; Phillips 2014; Solomon 2014; Wilson 2014), however none reported evidence of effect upon community levels of physical activity. Wilson 2014 reported an immediate program level effect of more walking.
Eleven studies were assessed as having unclear risk of bias (Brownson 2005; Eaton 1999; Goodman 1995; Jiang 2008; Kloek 2006; Luepker 1994; Nafziger 2001; Nishtar 2007; Rissel 2010; Sarrafzadegan 2009; Simon 2008). Of the 11 studies with unclear risk of bias, only three studies reported some evidence of effect (Jiang 2008; Luepker 1994; Simon 2008).
Equity pointers
In the data extraction we sought to identify studies which had conducted analyses of outcome measures by subgroups of socio‐economic disadvantage such as income, education, occupation, ethnicity and other proxy measures of economic status. Brownson 2004 presented results stratified by whether respondents had a high school certificate or less, whether they had household incomes ≤ USD 20,000 or were African American respondents. In no instance was the net intervention effect statistically significant within these strata for the two outcomes measured in the study (seven‐day total walking, seven‐day walking for exercise). Wendel‐Vos 2009 reported the outcomes of time spent in leisure time physical activity and walking (adjusted for age) for communities stratified into low educational level (intermediate secondary education or less) and moderate or high educational level (higher secondary educational, and higher vocational education or university). In this analysis differences between the intervention and comparison communities were not significant except in walking hours per week in males where the intervention community stayed constant while the control community significantly decreased (P ≤ 0.05) over the period of the study (P ≤ 0.05) as reported by the authors. No other studies had analyses by socio‐economic subgroups that we could identify, although a number of interventions were set or were targeted at areas of deprivation, disadvantage or low socio‐economic status (Brownson 2004; Brownson 2005; Eaton 1999; Jenum 2006; Kloek 2006; Kumpusalo 1996; Lupton 2003; Nafziger 2001; Mead 2013; O'Loughlin 1999; Phillips 2014; Reger‐Nash 2005; Wendel‐Vos 2009; Wilson 2014). Eight of the included studies were also undertaken in low middle or high middle income countries (Gao 2013; Gu 2006; Guo 2006; Jiang 2008; Nishtar 2007; Nguyen 2012; Sarrafzadegan 2009; Zhang 2003).
Several studies did provide results analysed by gender (Brown 2006; Eaton 1999; Kumpusalo 1996; Lupton 2003; Wendel‐Vos 2009; Young 1996). Eaton 1999 presented results grouped by age (< 35 and > 35 years, categories described by the authors) and by sex, with significant differences between age (P = 0.001) and sex (P = 0.001) being identified for physical inactivity. Over the course of the study, men under the age of 35 years decreased physical activity significantly more than men over 35 years and women (both age groups), although there was no difference between the intervention and comparison cities. As already outlined above, time spent in leisure time physical activity and walking (adjusted for age and educational level) as reported by Wendel‐Vos 2009 decreased in both the control and intervention communities over the period of the study, however there was significantly less reduction in the intervention community compared to the control community in females (P ≤ 0.05) than in males (P ≥ 0.05). Brown 2006 provided data on the proportion of the population of the intervention and control communities being physically active, for males and females. The investigators concluded that there was a different pattern between the sexes with the proportion of males in the intervention community categorised as being physically active decreasing by 4.2% (95% CI ‐10.1 to 1.7) compared to females where the proportion increased by 5% (95% CI ‐0.6 to 10.6). In a fishing village in Northern Norway, Lupton 2003 investigated the efficacy of an intervention aimed at improving the risk factor profile of the population. The proportion of males and females in the intervention group increased over the three‐year study as compared to the control population, however this was only statistically significant in the male population (P = 0.047). In the Stanford Five City Project, Young 1996 presented the results of each of the intervention and control cities by men and women. Intervention effects of behavioural improvement were limited and not always consistent between intervention cities, however the percentage of men who regularly engaged in vigorous activity was significantly different over time between the intervention and comparison cities (P < 0.004) in the independent sample (there was also a cohort sample). Kumpusalo 1996 provided results analysed by male and female and for the participating villages. No significant differences were found in any group between the baseline and follow‐up measurements (P > 0.05).
Reach
To be an included study (see Types of participants) each intervention was required to show an intent to be comprehensive in reaching the targeted community. Although intent of reach was required, it was hypothesised using the logic model (Figure 1) that reach (both intended and actual) would differ between the studies and could affect the outcome. There is evidence from some process evaluations that in many community wide interventions not everyone was able to be reached. Goodman 1995 found that African Americans perceived the intervention explored in their study as 'upper class'. Further, there was evidence in the Brown 2006 study, based in Rockhampton Australia, that the intervention was less attractive to men, or that “It didn't speak to men”, a finding that was borne out in the gender differential in the outcomes. Similar findings were also present in Wendel‐Vos 2009. The approach of Simon 2008 was extremely limited in reach as it used 12‐year olds as the target of the intervention and therefore was unlikely to penetrate much beyond the school community. Very few studies described how they recruited participants to events or the intervention strategies. Solomon 2014 found that very few residents were even aware of and participated in the intervention and, not surprisingly, no evidence of an increased prevalence of activity was observed. These studies have accordingly described community levels of physical activity by drawing an evaluation sample using a sampling frame from the community, rather than the actual participants in the events, unlike traditional RCTs.
The absence of reporting by subgroups and process evaluation made the assessment of reach difficult for most studies. Furthermore, as reach is also a component of the assessment of intensity, it was not possible to undertake further interpretation due to the inconsistency of findings when overall intensity was assessed.
Adverse events
None of the included studies reported the occurrence of adverse events.
Discussion
Summary of main results
We updated our previous review with eight new studies, an increase of one‐third in total. Four new studies were at low risk of bias in that the allocation of the intervention was randomly assigned. None of these four low risk studies reported an increase in population levels of physical activity for the community wide intervention. Overall, we still found no consistent evidence to support the effectiveness of multi‐component community wide interventions to increase population levels of physical activity, with the weight of the evidence indicating no increase in physical activity levels. There was still considerable heterogeneity between intervention approaches, intensity of actions delivered, the outcomes assessed and the comparison communities. The overall quality of the remaining studies was poor with the majority assessed as having a high risk of bias. The high risk of bias was largely due to studies with no randomisation to control and comparator groups, the selection and retention of participants, and the use of non‐validated outcome measures. Even amongst the studies at high risk of bias we consistently did not observe positive results. As a group, the interventions undertaken in China appeared to have the greatest possibility of success through high participation rates and may indicate that culturally China retains the potential to increase population levels of physical activity through community interventions, However, in Vietnam where advances in technology and urbanisation are leading to decreased physical activity, the one included study (Nguyen 2012) (at high risk of bias) found the community wide intervention to be problematic, having reported a statistically significant decline for the intervention group. Some of the studies such as Wilson 2014 and Rissel 2010 found a measurable increase in the use of trails and pathways indicating that some people were reached by the program, however increased trail use did not translate into increased population levels of physical activity. Wilson 2014 provides some evidence that social marketing and environmental enhancements together lead to an increase trail usage. Selective outcome reporting bias, identified in Mead 2013 and Gu 2006, may lead to an understatement of the evidence of ineffectiveness or of potential harm of some community wide approaches.
Overall completeness and applicability of evidence
Our review was able to draw upon the best available evidence from studies across the globe, conducted in high and low and high middle income countries. We were also able to successfully obtain additional information and data from study authors. The review shows that the hypothesis that multi‐component community wide interventions effectively increase population levels of physical activity continues to be unsupported by current evidence. Although we found differences in the mix of intervention components deployed by the included studies, one common approach was applicable across most studies. Almost all of the interventions included a component of building partnerships with local governments or NGOs (29 studies). Many also employed some form of individual counselling by health professionals (18 studies), mass media (15 studies) or other forms of communication (18 studies). Fewer studies worked in specific settings (11 studies) or used environmental change strategies (seven studies). Despite some common principles and approaches, of the 10 studies assessed as being of unclear risk of bias only three studies reported some evidence of effect. This finding is also consistent with the finding of no effect in all four low risk of bias studies. There is the potential that selective outcome reporting bias exists in this body of research as two authors appear not to have published all of the outcomes available from the measurement tools they used when the primary finding was negative, and that this co‐exists with publication bias of other studies.
Quality of the evidence
The overall quality of the studies has improved in the past three years, with four assessed as having a low risk of bias by virtue of improved design. All of the designs of the studies were controlled before and after studies with the exception of one controlled interrupted time series (Luepker 1994), one cluster cohort study (O'Loughlin 1999), and four cluster randomised controlled trials (Kamada 2013; Phillips 2014; Simon 2008; Wilson 2014). More sophisticated study designs emerged, including the stepped wedge cluster randomised trial, to accommodate the complexity of the intervention delivery undertaken (Solomon 2014). Selection bias was a main concern as only five studies were randomised. Many studies only had one measurement point pre‐intervention and one post‐intervention, and a number of the control groups had different baseline characteristics compared to the intervention groups. The other common problem related to detection bias as few studies reported the validity of their measurement tools. Validity of the measurement tools is particularly important given the small differences in physical activity reported by some studies. Many studies also relied on self‐reported physical activity measures as these are the most feasible way of collecting data from a large population. However, improvements are underway as in one recent study (Wilson 2014) individual accelerometer estimates were undertaken at baseline, 12, 18 and 24 months. Collectively the newer studies provide evidence that a more robust approach to health promoting interventions is possible. However, some studies failed to report primary outcomes measured post‐intervention.
Potential biases in the review process
One limitation of this review remains, potential publication bias. Other studies may exist but have not been submitted or accepted for publication and therefore were not identified through our searching efforts. The likelihood of this is difficult to judge. Through the new stricter requirements by journals and broader definitions for trial registration, we found evidence of an increasing registration of trials as we were able to use trial registries to determine whether a study had been completed but not published.
Our inclusion criteria required studies to have at least two intervention strategies and this excluded a number of large‐scale mass media interventions. It is possible that these mass media only studies may have included other strategies as part of their approaches but have not reported these activities formally. However, our objective to examine the effects of community interventions that deployed multiple strategies rather than a single strategy approach meant that without evidence of multiple strategies studies were excluded from our review.
Agreements and disagreements with other studies or reviews
The recent Lancet series on physical activity, published in London in 2012, also examined review level evidence for a range of global physical activity interventions in studies published between 2000 and 2011 (Heath 2012) but came to a slightly different conclusion on effectiveness. This review adopted a more mixed approach to typologies of interventions and concluded that the evidence of effectiveness of community interventions was "inconsistent, especially in communities in countries of low to middle income". Heath 2012 presented a reason for the inconsistent interpretation of effectiveness, because they found that more rigorous reviews (including the earlier version of this review) had not included in their reviews "observational studies or investigations with insufficient evidence (not necessarily ineffective)". This observation is indeed correct as design biases (such as an absence of a suitable comparison) would drive more inconstant results and fail to provide substantial evidence for causality as defined by GRADE (Schünemann 2011) and also by the Bradford‐Hill criteria for causality. Our findings differ as we included only studies with an element of controlled design and not those with pre‐post measures only. Our decision to maintain a higher design quality for included studies could be justified not only on the grounds of genuine assessment of impact but also it may in part have contributed to improvements since our last review in the design quality of newly published studies. This has been seen in other Cochrane physical activity reviews where recommendations on study quality are reflected in subsequent generations of studies, for example with longer follow‐up (Foster 2005). Brand 2014, a narrative overview of systematic reviews, found community interventions to be inconclusive in their ability to increase physical activity.
An earlier review by Yang 2010 examined the effectiveness of abroad range of interventions to promote cycling. This review found small positive effects to promote cycling in two city level community intervention studies (Yang 2010). For example, The English Cycle Demonstration Towns programme reported increases in cycling across six towns between 2005 and 2008. Towns opted for different strategies to promote cycling, ranging from mass media campaigns, travel planning, cycle training services and improvements to local cycling infrastructures. Yang 2010 mirrored our findings in the conclusions of their review, as they were also limited by the quality of study design, measures and data analysis. This is a consistent finding with systematic reviews of physical activity interventions; that the limitations of study design and measures probably mask any possible effects of such interventions (Foster 2005; NICE 2008; Ogilvie 2007; Richards 2013). Some of the measures may be useful for surveillance but may not be sensitive to change in intervention studies.
Often cited is Kahn 2002, a systematic review conducted on the effectiveness of a range of interventions intended to increase physical activity, including community wide campaigns. This review found that there was strong evidence that community wide campaigns are likely to be effective in increasing physical activity in the population, assuming that they are modified to target the populations in which they are implemented (Kahn 2002). The systematic review upon which these conclusions were based does not, however, include the latest studies (studies published since the year 2000) and six of the 10 studies that were included in the Kahn 2002 review (Jason 1991; Malmgren 1986; Meyer 1980; Owen 1987; Tudor‐Smith 1998; Wimbush 1998) were excluded from our systematic review for reasons outlined in the excluded studies table (Characteristics of excluded studies). Twelve years later, this Cochrane review presents evidence from recently published and in press studies at low risk of bias, previously unincorporated into any other systematic review. Collectively, the newer studies have trended towards more robust design and also conclusions of an absence of effectiveness for community wide interventions.
The absence of an effect from the most recently published suite of higher quality studies could be explained by the attributes of the intervention, their design, measures and reach. The apparent failure or potential reach of studies and their penetration into their target communities has also been described in a number of recent reviews on recruitment and potential impact of studies on inequalities. The lack of reporting of recruitment and marketing approaches in our studies were also highlighted by Foster et al's reviews of walking interventions (Foster 2011). More worrisome is the lack of data exploring the potential impacts of these community interventions upon specific subgroups, particularly those groups whose physical activity participation is socially patterned (Humphreys 2013). In theory, any potential impact in one group might be masked by a decline in another, and there might be the potential for differential effects of such interventions. In the absence of adequate reporting the impact of population level physical activity interventions on social inequality effects will remain unknown (Humphreys 2013).
Authors' conclusions
Implications for practice.
Although numerous studies of community wide interventions have been undertaken, there is a noticeable absence of studies reporting any benefits. The body of evidence in this review does not support the hypothesis that multi‐component community wide interventions effectively increase population levels of physical activity. It could be postulated that, given the conflicting findings and the evidence from new high quality studies, that community wide interventions lack efficacy. We suggest caution in making such a broad conclusion as many of the authors of the included studies identified the reason for failure, as the program being unable to achieve penetration, being too short and poor measures were used to detect an effect, or the study was otherwise under‐resourced. It is unclear whether effectiveness may be achieved if further resources or other improvements were made to these interventions. Historically, the tools used to measure physical activity were generally weak, inhibiting the ability to interpret the results and draw conclusions. However, with newer approaches such as accelerometry, the accurate measurement of physical activity appears possible. Accelerometers may not be used in poorly funded studies, nor their use prioritised when physical activity is only one component of the intervention. Some interventions might alter the choices which people make resulting in greater use of the environmental enhancements; these changes fail to result in measurable increases in population physical activity levels. An example of this is Wilson 2014 (an environmental intervention promoting walking combined with social marketing), which showed promising sustained participation in the program over 24 months but no program effects measured in individuals representative of the population.
It is also worth considering the significant challenges of implementing multi‐strategic community wide interventions in an attempt to reach the whole community. Some studies found gender differences in the effectiveness of the intervention. For example, Brownson 2004 found that men did not relate to the key message and as such the intervention failed to reach them. Conversely, other studies suggested greater effectiveness in the male population than the female population (Lupton 2003). These issues should be considered in the design and implementation of any community wide intervention, particularly in recruitment and marketing messages.
Policy makers and health professionals need to consider the options they advocate for and the programs they fund because this review has not found evidence of effectiveness at a population level. Community wide interventions to promote physical activity could in principle be effective, however in practice their effects may remain undetected unless the current research improves design, implementation and evaluation of these interventions.
Implications for research.
The central question of this research is whether it is worthwhile to develop and undertake multi‐component interventions to increase population levels of physical activity. Neither of the four studies at low risk of bias provided evidence of an effect, however on their own they are inadequate to capture the breadth of the community wide approach, which is a global phenomenon. Based on the lack of robust studies achieving adequate penetration and duration, further exploration of combined community interventions may be merited if practical and likely to achieve penetration. The design of interventions may benefit from assessing the evidence from systematic reviews of individual strategies to guide which strategies should be included or excluded from the suite. An overview of systematic reviews of public health interventions to increase physical activity is warranted (Baker 2014). There may also be scope for further studies focusing on outcomes by population characteristics such as social, gender or cultural groups; or targeting programmes at high risk groups. Many of the interventions were attempted in disadvantage communities. This could indicate that the intervention may not have been adequately designed for the intervention to meet the needs of those in the communities. A recent study showed that mass media health promotion campaigns for chronic disease prevention (for example to increase physical activity) may not reach lower socio‐economic groups as they do high socio‐economic groups, and the net result could be a widening of the gaps in health inequality (Armstrong 2014). Focusing only on higher socio‐economic status communities that have the capacity to support physical activity and respond to the intervention may lead to increases in health inequalities.
One clear message is that any new studies should be rigorously designed and analysed, ensuring that the measures are reliable and sensitive to change at a population level. Design issues of particular importance in this field include the quality of the measurement of physical activity. Alternatives for self‐report telephone surveys should be considered. It is disappointing that several of the included studies were intensive but relied on a singular low quality, unvalidated outcome measure rather than a validated measure such as the International Physical Activity Questionnaires (IPAQ) or accelerometry.
This update shows that robust evaluation is possible. The assignment of communities as comparison or control communities should, where ever possible, be through randomisation. Assignment to control for communities which have a lower level of capability to implement the intervention should be avoided, although our update shows that this practice continues. It would be advantageous to measure physical activity at multiple time points, prior to, during and after the intervention, to consider the effect of the intervention against trends and regression to the mean.
To minimise risks of biases by which all studies are assessed, those planning future studies should consider that the sample size calculation should take account of clustering, completeness and duration of follow‐up, and that analysis accounts for clustering and for attrition. Studies should be registered in accordance with the Declaration of Helsinki (World Medical Association 2013). Researchers are also encouraged to conduct and publish process evaluations, which provide valuable information on potential facilitators and barriers, and give an indication of how successfully an intervention has been implemented. Given the large investment in community wide interventions, assessments of resource consumption and economic evaluations are also warranted in future evaluations.
What's new
| Date | Event | Description |
|---|---|---|
| 9 January 2015 | Amended | 'Assessed as up to date' date has been corrected to reflect when search was last conducted |
History
Protocol first published: Issue 2, 2010 Review first published: Issue 4, 2011
| Date | Event | Description |
|---|---|---|
| 27 August 2014 | New citation required and conclusions have changed | The original review has been updated with eight additional studies, increasing the study base by one‐third. Four of the eight new studies are at low risk of bias, whereas earlier there were no studies at low risk of bias upon which conclusions could be drawn. The addition of the eight new studies provides a more complete view of an absence of benefit from the approaches to community wide interventions studied to date. |
Acknowledgements
The authors would like to thank the review advisory group (Darren Hauser, Greg Heath, Dheeraj Bansal), Carolyn Lang (assistance with the logic model) and the Public Health Group Trials Search Coordinator (Ruth Turley) for their contributions, and Jaindong Sun for assistance with searching, translating and assessing the Chinese literature, Peter Kopittke for study retrieval, Robin Christensen and Jo McKenzies for statistical support and Rebekah Clowes for text editing. We especially thank Yolanda Lovie‐Toon for her support with the update through the Queensland University of Technology VRES Scholarship.
The authors also acknowledge, with thanks, help from the following experts in the field: Jiandong Sun (Queensland University of Technology), who identified Zhung 2003, indicated knowledge of further Chinese studies, and undertook searches of Chinese databases. Harry Rutter (National Obesity Observatory, Oxford), Nick Cavill, (Oxford University), Glen Austin (Queensland Health), Kerry Mummery (University of Central Queensland), Gregory W Heath (University of Tennessee College of Medicine) and Ross C Brownson (Washington University in St. Louis) were contacted for advice on additional published and unpublished studies. Dawn Wilson, Gemma Phillips, Emma Solomon and Masamitsu Kamada provided additional information and informed us of the progress of their studies.
The original review published in 2011 and this update both received clearance from Centers for Disease Control and Prevention USA. The comments received through this process were helpful for providing greater clarity for public health decision makers.
Appendices
Appendix 1. Search strategies
The searches were based on the following strategy, developed in Medline and adapted as appropriate to the specifications of each database and web site. The strategy was deliberately designed to capture a broad range of references and the 'explode' feature was used wherever this was applicable to the database. There were no language restrictions.
All information sources were searched most recently in January 2014 for publications from January 1995 onwards.
ASSIA (Proquest) January 1995 to 12 November 2009 [1144 hits]; November 2009 to 16 January 2014 [163 hits]; Total = 1307 hits
(su("Communities" OR "health promotion" OR "mass media" OR "communications" OR "Social marketing") OR ti("state wide" OR "nation wide" OR "nationwide" OR "community wide" OR "land use" OR "urban renewal" OR "transportation policy" OR "travel policy" OR "neighbourhood regeneration" OR "mass media" OR advertising OR radio OR television OR newspaper* OR poster* OR flyer* OR social marketing OR "point of decision" OR legislation OR legislative OR policy) OR ab("state wide" OR "nation wide" OR "nationwide" OR "community wide" OR "land use" OR "urban renewal" OR "transportation policy" OR "travel policy" OR "neighbourhood regeneration" OR "mass media" OR advertising OR radio OR television OR newspaper* OR poster* OR flyer* OR social marketing OR "point of decision" OR legislation OR legislative OR policy)) AND (su(exercise OR "physical fitness" OR sports) OR ti(fitness OR aerobic capacity OR activ* OR walk* OR yoga OR sedentary OR deskbound OR inactiv* OR running OR jogging OR pilates OR yoga OR cycle OR cycling OR bicycl* OR bike* OR biking OR swim* OR swimming OR rollerblading OR rollerskating OR skating OR exertion* OR "stair use" OR "active transport*") OR ab(fitness OR aerobic capacity OR activ* OR walk* OR yoga OR sedentary OR deskbound OR inactiv* OR running OR jogging OR pilates OR yoga OR cycle OR cycling OR bicycl* OR bike* OR biking OR swim* OR swimming OR rollerblading OR rollerskating OR skating OR exertion* OR "stair use" OR "active transport*")) AND (su(trials) OR ti(randomized OR randomised OR placebo OR randomly OR trial OR "quasi‐experiment*" OR "pre test" OR pretest OR posttest OR "post test" OR "time series" OR "controlled stud*" OR "before and after" OR "controlled before") OR ab(randomized OR randomised OR placebo OR randomly OR trial OR "quasi‐experiment*" OR "pre test" OR pretest OR posttest OR "post test" OR "time series" OR "controlled stud*" OR "before and after" OR "controlled before"))Limits applied
British Nursing Index (BNI) (Proquest) January 1995 to 9 November 2009 [105 hits]; November 2009 to 16 January 2014 [262 hits]; Total = 367 hits
((SU.EXACT.EXPLODE("Health Promotion") OR SU.EXACT.EXPLODE("Community Health Services") OR SU.EXACT.EXPLODE("Mass Media") OR SU.EXACT.EXPLODE("Health Education") OR SU.EXACT.EXPLODE("Social Marketing") OR SU.EXACT.EXPLODE("Marketing") OR SU.EXACT.EXPLODE("Public Relations")) OR ti("state wide" OR "nation wide" OR "nationwide" OR "community wide" OR "land use" OR "urban renewal" OR "transportation policy" OR "travel policy" OR "neighbourhood regeneration" OR "mass media" OR advertising OR radio OR television OR newspaper* OR poster* OR flyer* OR social marketing OR "point of decision" OR legislation OR legislative OR policy) OR ab("state wide" OR "nation wide" OR "nationwide" OR "community wide" OR "land use" OR "urban renewal" OR "transportation policy" OR "travel policy" OR "neighbourhood regeneration" OR "mass media" OR advertising OR radio OR television OR newspaper* OR poster* OR flyer* OR social marketing OR "point of decision" OR legislation OR legislative OR policy)) AND ((SU.EXACT.EXPLODE("Physical Fitness") OR SU.EXACT.EXPLODE("Leisure")) OR ti(fitness OR aerobic capacity OR activ* OR walk* OR yoga OR sedentary OR deskbound OR inactiv* OR running OR jogging OR pilates OR yoga OR cycle OR cycling OR bicycl* OR bike* OR biking OR swim* OR swimming OR rollerblading OR rollerskating OR skating OR exertion* OR "stair use" OR "active transport*") OR ab(fitness OR aerobic capacity OR activ* OR walk* OR yoga OR sedentary OR deskbound OR inactiv* OR running OR jogging OR pilates OR yoga OR cycle OR cycling OR bicycl* OR bike* OR biking OR swim* OR swimming OR rollerblading OR rollerskating OR skating OR exertion* OR "stair use" OR "active transport*")) AND (ti(randomized OR randomised OR placebo OR randomly OR trial OR "quasi‐experiment*" OR "pre test" OR pretest OR posttest OR "post test" OR "time series" OR "controlled stud*" OR "before and after" OR "controlled before") OR ab(randomized OR randomised OR placebo OR randomly OR trial OR "quasi‐experiment*" OR "pre test" OR pretest OR posttest OR "post test" OR "time series" OR "controlled stud*" OR "before and after" OR "controlled before")) AND date limits applied. ‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐‐
CINAHL (EBSCOhost) January 1995 to 13 November 2009 [2881 hits]; November 2009 to 16 January 2014 [796 hits]; Total = 3677 hits
| S14 | S4 AND S8 AND S12 | |
| S13 | S4 AND S8 AND S12 | |
| S12 | S9 OR S10 OR S11 | |
| S11 | AB (randomized or randomised or placebo or randomly or trial or “quasi‐experiment*” or pre test or pretest or posttest or “post test” or “time series” or “controlled stud*” or "before and after" or “controlled before”) | |
| S10 | TI (randomized or randomised or placebo or randomly or trial or “quasi‐experiment*” or pre test or pretest or posttest or “post test” or “time series” or “controlled stud*” or "before and after" or “controlled before”) | |
| S9 | (MH "experimental studies+") | |
| S8 | S5 OR S6 OR S7 | |
| S7 | AB (fitness or aerobic capacity or activ* or walk* or yoga or sedentary or deskbound or inactiv* or running or jogging or pilates or yoga or cycle or cycling or bicycl* or bike* or biking or swim* or swimming or rollerblading or rollerskating or skating or exertion* or "stair use" or "active transport*") | |
| S6 | TI (fitness or aerobic capacity or activ* or walk* or yoga or sedentary or deskbound or inactiv* or running or jogging or pilates or yoga or cycle or cycling or bicycl* or bike* or biking or swim* or swimming or rollerblading or rollerskating or skating or exertion* or "stair use" or "active transport*") | |
| S5 | (MH "Exercise+") or (MH "physical fitness+") or (MH "Sports+") | |
| S4 | S1 OR S2 OR S3 | |
| S3 | AB ("state wide" or “nation* wide” or “community wide” or "land use" or “urban renewal” or “transportation policy” or "travel policy" or “neighbourhood regeneration” or “mass media” or advertising or radio or television or newspaper* or poster* or flyer* or social marketing or "point of decision" * or legislation or legislative or policy) | |
| S2 | TI ("state wide" or “nation* wide” or “community wide” or "land use" or “urban renewal” or “transportation policy” or "travel policy" or “neighbourhood regeneration” or “mass media” or advertising or radio or television or newspaper* or poster* or flyer* or social marketing or "point of decision" * or legislation or legislative or policy) | |
| S1 | (MH "Communities+") or (MH "health promotion+") or (MH "Communications media") or (MH "Social marketing") |
Limit to dates
Chinese databases: CAJ,CCND,CPCD,CJSS,CMFD,CDFD. January 1995 to 20 November 2009 [124 hits]; November 2009 ‐ January 2014 [1 hit]; Total = 125 hits
http://www.global.cnki.net/grid20/index.htm
Search Condition:((题名=community intervention))(Precise);时间排序;不排重 Cross‐database Search(初级检索)
OR
Search Condition:((题名="health+education" And 题名=intervention))and (全文=Physical+activity" 或者 全文=physical+exercise))(Precise);时间排序;不排重 Cross‐database Search(高级检索)
OR
Search Condition:((题名=community And 题名=intervention))and (全文="physical+activity" 或者全文="Physical+exercise"))(Precise);时间排序;不排重 Cross‐database Search(高级检索)
The Cochrane Library (Wiley) January 1995 to 9 November 2009 [1841 hits]; November 2009 to 16 January 2014 [166 hits]; Total = 2007 hits
| ID | Search |
| #1 | MeSH descriptor residence characteristics |
| #2 | MeSH descriptor community health planning |
| #3 | MeSH descriptor health promotion |
| #4 | MeSH descriptor community health services |
| #5 | (national next (policy or policies or strateg* or program*)):ti,ab |
| #6 | MeSH descriptor mass media |
| #7 | MeSH descriptor community networks |
| #8 | MeSH descriptor community health centers |
| #9 | MeSH descriptor "marketing of health services" |
| #10 | MeSH descriptor cities |
| #11 | MeSH descriptor rural population or MeSH descriptor rural health |
| #12 | MeSH descriptor urban population |
| #13 | MeSH descriptor community‐institutional relations |
| #14 | MeSH descriptor environment design |
| #15 | MeSH descriptor city planning |
| #16 | environmental planning:ti,ab |
| #17 | MeSH descriptor social environment |
| #18 | MeSH descriptor urban health |
| #19 | MeSH descriptor "health education" |
| #20 | MeSH descriptor social marketing |
| #21 | ((state or county or town or city or village or nation*) next (wide or whole or communit*)):ti,ab |
| #22 | ((combined* or multiple or multi or multifactorial or partner*) next (program* or strateg* or intervention* or organi*ation*)):ti,ab |
| #23 | (media intervention* or whole community or community intervention* or community organsai*ation*):ti,ab |
| #24 | (community near (design or action or program* or partner*)):ti,ab |
| #25 | ((health or community or environment*) next (policy or policies)):ti,ab |
| #26 | (urban design or "land use policies" or "land use policy"):ti,ab |
| #27 | ((transportation or travel) next (policy or policies)):ti,ab |
| #28 | health planning:ti,ab |
| #29 | ((neighbo*rhood* or city or cities or community) near (development or regeneration or renewal or design* or plan* or polic*)):ti,ab |
| #30 | (community wide or community setting* or community group* or organi*ation* level*):ti,ab |
| #31 | (Communit* near base*):ti,ab |
| #32 | ((built environment* or urban environment* or environmental) next (change* or intervention*)):ti,ab |
| #33 | (environment* near infrastructure):ti,ab |
| #34 | (urban near (regeneration or renewal or plan* or design* or policy or policies or strateg* or program*)):ti,ab |
| #35 | (media or advertising or radio or television or newspaper* or poster* or flyer* or information booklet*) near (information or education or campaign or intervention or strateg* or program* or policy or policies):ti,ab |
| #36 | social marketing:ti,ab |
| #37 | ("point of decision" near (stair* or travel*)):ti,ab |
| #38 | (health counsel* or individual counsel*):ti,ab |
| #39 | (community near (collaborati* or coalition)):ti,ab |
| #40 | ((school* or work*place* or employer* or classroom or college) near (strateg* or program* or policy or policies)):ti,ab |
| #41 | ((public or community) near (information or education or campaign or intervention or strateg* or program* or policy or policies)):ti,ab |
| #42 | (policy change* or fiscal change*):ti,ab |
| #43 | (policy near (intervene* or change or introduce* or modif* or alter*)):ti,ab |
| #44 | physical infrastructure:ti,ab |
| #45 | ((road or land) next us*):ti,ab |
| #46 | (Legislation or legislative):ti,ab |
| #47 | ((Voluntary or volunteer or charities or charity or non‐government or government or "not for profit") next (group* or organisation* or department* or club*)):ti,ab |
| #48 | (#1 OR #2 OR #3 OR #4 OR #5 OR #6 OR #7 OR #8 OR #9 OR #10 OR #11 OR #12 OR #13 OR #14 OR #15 OR #16 OR #17 OR #18 OR #19 OR #20 OR #21 OR #22 OR #23 OR #24 OR #25 OR #26 OR #27 OR #28 OR #29 OR #30 OR #31 OR #32 OR #33 OR #34 OR #35 OR #36 OR #37 OR #38 OR #39 OR #40 OR #41 OR #42 OR #43 OR #44 OR #45 OR #46 OR #47) |
| #49 | MeSH descriptor exercise |
| #50 | MeSH descriptor running |
| #51 | MeSH descriptor walking |
| #52 | MeSH descriptor physical fitness |
| #53 | MeSH descriptor swimming |
| #54 | (fitness adj class*):ti,ab |
| #55 | MeSH descriptor gardening |
| #56 | MeSH descriptor "physical education and training" |
| #57 | MeSH descriptor dancing |
| #58 | MeSH descriptor sports |
| #59 | MeSH descriptor sport |
| #60 | MeSH descriptor yoga |
| #61 | MeSH descriptor fitness centers |
| #62 | MeSH descriptor recreation |
| #63 | MeSH descriptor "play and playthings" |
| #64 | MeSH descriptor motor activity |
| #65 | (fitness next (regime* or program*)):ti,ab |
| #66 | cardiorespiratory fitness:ti,ab |
| #67 | aerobic capacity:ti,ab |
| #68 | ((moderate or vigorous*) next activ*):ti,ab |
| #69 | (led walk* or health walk*):ti,ab |
| #70 | (physical next (fit* or train* or activ* or endur*)):ti,ab |
| #71 | (exercis* near (fit* or train* or activ* or endur*)):ti,ab |
| #72 | ((leisure or fitness) near (centre* or center* or facilit*)):ti,ab |
| #73 | ((promot* or uptak* or encourag* or increas* or start* or adher* or sustain* or maintain*) near gym*):ti,ab |
| #74 | ((promot* or uptak* or encourag* or increas* or start* or adher* or sustain* or maintain*) near physical activ*):ti,ab |
| #75 | ((promot* or uptak* or encourag* or increas* or start* or adher* or sustain* or maintain*) near (circuit* or aqua*)):ti,ab |
| #76 | (promot* or uptak* or encourag* or increas* or start* or adher* or sustain* or maintain*) near (exercis* or exertion or keep fit or fitness class or yoga or aerobic*):ti,ab |
| #77 | ((decreas* or reduc* or discourag*) near (sedentary or deskbound or "physical* inactiv*")):ti,ab |
| #78 | sport*:ti,ab |
| #79 | walk*:ti,ab |
| #80 | Running:ti,ab |
| #81 | Jogging:ti,ab |
| #82 | Pilates:ti,ab |
| #83 | Yoga:ti,ab |
| #84 | ((cycle or cycling) near (school* or work or workplace or commut* or travel* or equipment or facility* or rack* or store* or storing or park* or friendly or infrastructure)):ti,ab |
| #85 | bicycl*:ti,ab |
| #86 | (bike* or biking):ti,ab |
| #87 | (swim* or swimming):ti,ab |
| #88 | (exercis* near aerobic*):ti,ab |
| #89 | Rollerblading:ti,ab |
| #90 | Rollerskating:ti,ab |
| #91 | Skating:ti,ab |
| #92 | exertion*:ti,ab |
| #93 | strength training:ti,ab |
| #94 | resilience training:ti,ab |
| #95 | weight lifting:ti,ab |
| #96 | travel mode*:ti,ab |
| #97 | (active next (travel* or transport* or commut*)):ti,ab |
| #98 | (multimodal transportation or alternative transport* or alternative travel*):ti,ab |
| #99 | recreation*:ti,ab |
| #100 | ("use" near stair*):ti,ab |
| #101 | (pedestrianis* or pedestrianiz*):ti,ab |
| #102 | (#49 OR #50 OR #51 OR #52 OR #53 OR #54 OR #55 OR #56 OR #57 OR #58 OR #59 OR #60 OR #61 OR #62 OR #63 OR #64 OR #65 OR #66 OR #67 OR #68 OR #69 OR #70 OR #71 OR #72 OR #73 OR #74 OR #75 OR #76 OR #77 OR #78 OR #79 OR #80 OR #81 OR #82 OR #83 OR #84 OR #85 OR #86 OR #87 OR #88 OR #89 OR #90 OR #91 OR #92 OR #93 OR #94 OR #95 OR #96 OR #97 OR #98 OR #99 OR #100 OR #101) |
| #103 | randomized controlled trial:pt |
| #104 | controlled clinical trial:pt |
| #105 | (randomized or randomised or placebo or randomly or trial|):ab |
| #106 | MeSH descriptor Random allocation or MeSH descriptor clinical trial or MeSH descriptor single‐blind method or MeSH descriptor double‐blind method or MeSH descriptor control groups |
| #107 | MeSH descriptor Intervention studies |
| #108 | MeSH descriptor evaluation studies |
| #109 | MeSH descriptor program evaluation |
| #110 | Comparative study:pt |
| #111 | quasi‐experiment*:ti,ab |
| #112 | (pre test or pretest or (posttest or post test)):ti,ab |
| #113 | Trial:ti |
| #114 | (time next series):ti,ab |
| #115 | (pre test or pretest or (posttest or post test)):ti,ab |
| #116 | ((evaluat* or intervention or interventional) near (control or controlled or study or program* or comparison or "before and after" or comparative)):ti,ab |
| #117 | ((intervention or interventional) near (effect* or evaluat* or outcome*)):ti,ab |
| #118 | ((process or program*) near (effect* or evaluat*)):ti,ab |
| #119 | (controlled before or "before and after stud*" or follow up assessment):ti,ab |
| #120 | (#103 OR #104 OR #105 OR #106 OR #107 OR #108 OR #109 OR #110 OR #111 OR #112 OR #113 OR #114 OR #115 OR #116 OR #117 OR #118 OR #119) |
| #121 | MeSH descriptor animals not (MeSH descriptor humans and MeSH descriptor animals) |
| #122 | (#120 AND NOT #121) |
Limit by dates
Cochrane Public Health Group segment of the Cochrane Register of Studies (CRS) January 1995 to 19 November 2009 [31 hits]; November 2009 to 21 January 2014 [1 hit]; Total = 32 hits
Community wide interventions
Characteristics of the intervention: Physical activity
EMBASE (Ovid) January 1995 to 6 November 2009 [4941 hits]; November 2009 to 17 January 2014 [2215 hits]; Total = 7156 hits ‐‐‐‐‐‐‐‐
| # | Searches |
| 1 | health promotion/ |
| 2 | community program/ |
| 3 | (national adj (policy or policies or strateg$ or program$)).ti,ab. |
| 4 | mass medium/ |
| 5 | social network/ |
| 6 | health center/ |
| 7 | marketing/ |
| 8 | city/ |
| 9 | rural population/ |
| 10 | urban population/ |
| 11 | public relations/ |
| 12 | exp environment/ |
| 13 | city planning/ |
| 14 | environmental planning.ti,ab. |
| 15 | exp social environment/ |
| 16 | school health education/ |
| 17 | social marketing/ |
| 18 | ((state or county or town or city or village or nation*) adj2 (wide or whole or communit*)).ti,ab. |
| 19 | ((combined$ or multiple or multi or multifactorial or partner$) adj2 (program$ or strateg$ or intervention$ or organi?ation$)).ti,ab. |
| 20 | (media intervention* or whole community or community intervention* or community organsai?ation$1).ti,ab. |
| 21 | (community adj2 (design or action or program* or partner$)).ti,ab. |
| 22 | ((health or community or environment*) adj (policy or policies)).ti,ab. |
| 23 | (urban design or "land use policies" or "land use policy").ti,ab. |
| 24 | ((transportation or travel) adj (policy or policies)).ti,ab. |
| 25 | health planning.ti,ab. |
| 26 | ((neighbo?rhood* or city or cities or community) adj2 (development or regeneration or renewal or design* or plan* or polic*)).ti,ab. |
| 27 | (community wide or community setting$ or community group$ or organi?ation$ level$1).ti,ab. |
| 28 | (Communit$ adj2 base$).ti,ab. |
| 29 | ((built environment* or urban environment* or environmental) adj (change* or intervention*)).ti,ab. |
| 30 | (environment$ adj2 infrastructure).ti,ab. |
| 31 | (urban adj2 (regeneration or renewal or plan* or design* or policy or policies or strateg* or program$)).ti,ab. |
| 32 | (urban adj2 (regeneration or renewal or plan* or design* or policy or policies or strateg* or program$)).ti,ab. |
| 33 | social marketing.ti,ab. |
| 34 | ("point of decision" adj3 (stair* or travel*)).ti,ab. |
| 35 | (health counsel* or individual counsel*).ti,ab. |
| 36 | (community adj3 (collaborati* or coalition)).ti,ab. |
| 37 | ((school* or work?place* or employer* or classroom or college) adj2 (strateg$ or program$ or policy or policies)).ti,ab. |
| 38 | ((public or community) adj2 (information or education or campaign or intervention or strateg$ or program$ or policy or policies)).ti,ab. |
| 39 | (policy change* or fiscal change*).ti,ab. |
| 40 | (policy adj3 (interven$ or change or introduce$ or modif$ or alter$)).ti,ab. |
| 41 | physical infrastructure.ti,ab. |
| 42 | ((road or land) adj us*).ti,ab. |
| 43 | (Legislation or legislative).ti,ab. |
| 44 | ((Voluntary or volunteer or charities or charity or non‐government or government or "not for profit") adj2 (group$1 or organisation$ or department$1 or club$1)).ti,ab. |
| 45 | or/1‐44 |
| 46 | exp exercise/ |
| 47 | exp physical activity/ |
| 48 | walking/ |
| 49 | fitness/ |
| 50 | swimming/ |
| 51 | (fitness adj class*).ti,ab. |
| 52 | gardening/ |
| 53 | physical education/ |
| 54 | dancing/ |
| 55 | exp sport/ |
| 56 | exp kinesiotherapy/ |
| 57 | (fitness adj (regime* or program*)).ti,ab. |
| 58 | cardiorespiratory fitness.ti,ab. |
| 59 | aerobic capacity.ti,ab. |
| 60 | ((moderate or vigorous*) adj activ*).ti,ab. |
| 61 | (led walk* or health walk*).ti,ab. |
| 62 | (physical adj5 (fit* or train* or activ* or endur*)).ti,ab. |
| 63 | (exercis* adj5 (fit* or train* or activ* or endur*)).ti,ab. |
| 64 | ((leisure or fitness) adj5 (centre* or center* or facilit*)).ti,ab. |
| 65 | ((promot* or uptak* or encourag* or increas* or start* or adher* or sustain* or maintain*) adj5 gym*).ti,ab. |
| 66 | ((promot* or uptak* or encourag* or increas* or start* or adher* or sustain* or maintain*) adj5 physical activ*).ti,ab. |
| 67 | ((promot* or uptak* or encourag* or increas* or start* or adher* or sustain* or maintain*) adj5 (circuit* or aqua*)).ti,ab. |
| 68 | ((promot* or uptak* or encourag* or increas* or start* or adher* or sustain* or maintain*) adj5 (exercis* or exertion or keep fit or fitness class or yoga or aerobic*)).ti,ab. |
| 69 | ((decreas* or reduc* or discourag*) adj5 (sedentary or deskbound or "physical* inactiv*")).ti,ab. |
| 70 | sport*3.ti,ab. |
| 71 | walk*3.ti,ab. |
| 72 | running.ti,ab. |
| 73 | jogging.ti,ab. |
| 74 | pilates.ti,ab. |
| 75 | yoga.ti,ab. |
| 76 | ((cycle or cycling) adj5 (school$ or work or workplace or commut$ or travel$ or equipment or facilit$ or rack$1 or store$1 or storing or park$ or friendly or infrastructure)).ti,ab. |
| 77 | bicycl*.ti,ab. |
| 78 | (bike*1 or biking).ti,ab. |
| 79 | (swim*1 or swimming).ti,ab. |
| 80 | (exercis*3 adj5 aerobic*).ti,ab. |
| 81 | rollerblading.ti,ab. |
| 82 | rollerskating.ti,ab. |
| 83 | skating.ti,ab. |
| 84 | exertion*1.ti,ab. |
| 85 | strength training.ti,ab. |
| 86 | resilience training.ti,ab. |
| 87 | weight lifting.tw. |
| 88 | travel mode*1.tw. |
| 89 | (active adj (travel*4 or transportation or commut$)).tw. |
| 90 | (multimodal transportation or alternative transport* or alternative travel*).ti,ab. |
| 91 | recreation*1.ti,ab. |
| 92 | ("use" adj3 stair*).ti,ab. |
| 93 | (pedestrianis* or pedestrianiz*).ti,ab. |
| 94 | or/46‐93 |
| 95 | randomized controlled trial/ |
| 96 | controlled clinical trial/ |
| 97 | (randomized or randomised or placebo or randomly or trial).ab. |
| 98 | exp controlled study/ |
| 99 | Intervention study/ |
| 100 | evaluation research/ |
| 101 | evaluation/ |
| 102 | Comparative study/ |
| 103 | quasi‐experiment$.ti,ab. |
| 104 | (pre test or pretest or (posttest or post test)).ti,ab. |
| 105 | trial.ti. |
| 106 | (time adj series).ti,ab. |
| 107 | (pre test or pretest or (posttest or post test)).ti,ab. |
| 108 | ((evaluat$ or intervention or interventional) adj8 (control or controlled or study or program$ or comparison or "before and after" or comparative)).ti,ab. |
| 109 | ((intervention or interventional) adj8 (effect* or evaluat* or outcome*)).ti,ab. |
| 110 | ((process or program*) adj3 (effect* or evaluat*)).ti,ab. |
| 111 | (controlled before or "before and after stud$" or follow up assessment).ti,ab. |
| 112 | or/95‐111 |
| 113 | 45 and 94 and 112 |
| 114 | animals/ not (humans/ and animals/) |
| 115 | 113 not 114 |
| 116 | limit 115 to (exclude medline journals and yr="2011 ‐ 2014") |
EPPI Centre DoPHER January 1995 to 24 November 2009 [38 hits]; November 2009 to 20 January 2014 [0 hits]; Total = 38 hits
Focus of the Report = Physical Activity
AND
What type of study does this report describe = Intervention
Then screened for potentially relevant studies.
EPPI Centre TRoPHI January 1995 to 24 November 2009 [200 hits]; November 2009 to 20 January 2014 [12 hits]; Total = 212 hits
Focus of the report = Physical activity
AND
Intervention site(s): community site OR educational institution OR home OR mass media OR outreach OR preschool OR primary education OR secondary education OR tertiary education OR workplace site OR intervention site unspecified
AND
Type(s) of intervention: activity OR environmental modification OR incentives OR legislation OR regulation OR resource access OR service access OR social support OR intervention type unspecified
AND
What type of study does this report describe?: RCT OR trial
Then manually selected potentially relevant studies (using dates in free text search)
ERIC (Proquest) January 1995 to 13 November 2009 [416 hits]; November 2009 to 16 January 2014 [102 hits]; Total = 518 hits
((SU.EXACT.EXPLODE("Mass Media") OR SU.EXACT.EXPLODE(""Community Action"") OR SU.EXACT.EXPLODE("Health Education") OR SU.EXACT.EXPLODE("Marketing") OR SU.EXACT.EXPLODE("Public Relations")) OR ti("state wide" OR "nation wide" OR "nationwide" OR "community wide" OR "land use" OR "urban renewal" OR "transportation policy" OR "travel policy" OR "neighbourhood regeneration" OR "mass media" OR advertising OR radio OR television OR newspaper* OR poster* OR flyer* OR social marketing OR "point of decision" OR legislation OR legislative OR policy) OR ab("state wide" OR "nation wide" OR "nationwide" OR "community wide" OR "land use" OR "urban renewal" OR "transportation policy" OR "travel policy" OR "neighbourhood regeneration" OR "mass media" OR advertising OR radio OR television OR newspaper* OR poster* OR flyer* OR social marketing OR "point of decision" OR legislation OR legislative OR policy)) AND ((SU.EXACT.EXPLODE("Physical Activity Level") OR SU.EXACT.EXPLODE("Physical Fitness") OR SU.EXACT.EXPLODE("Leisure Time")) OR ti(fitness OR aerobic capacity OR activ* OR walk* OR yoga OR sedentary OR deskbound OR inactiv* OR running OR jogging OR pilates OR yoga OR cycle OR cycling OR bicycl* OR bike* OR biking OR swim* OR swimming OR rollerblading OR rollerskating OR skating OR exertion* OR "stair use" OR "active transport*") OR ab(fitness OR aerobic capacity OR activ* OR walk* OR yoga OR sedentary OR deskbound OR inactiv* OR running OR jogging OR pilates OR yoga OR cycle OR cycling OR bicycl* OR bike* OR biking OR swim* OR swimming OR rollerblading OR rollerskating OR skating OR exertion* OR "stair use" OR "active transport*")) AND (ti(randomized OR randomised OR placebo OR randomly OR trial OR "quasi‐experiment*" OR "pre test" OR pretest OR posttest OR "post test" OR "time series" OR "controlled stud*" OR "before and after" OR "controlled before") OR ab(randomized OR randomised OR placebo OR randomly OR trial OR "quasi‐experiment*" OR "pre test" OR pretest OR posttest OR "post test" OR "time series" OR "controlled stud*" OR "before and after" OR "controlled before"))
Limit by dates.
EU Platform on Diet, Physical Activity and Health 23 November 2009 [0 hits]; 17 January 2014 [0 hits]; Total = 0 hits
http://www.eufic.org/page/en/health‐and‐lifestyle/physical‐activity/
health‐evidence.org 25 November 2009 [5 hits] ; 20 January 2014 [47 hits]; Total = 52 hits
(physical activity) and (city or cities or regional or community or public) and (systematic review)
Articles added to the registry since [date], then manually adjust returns by date.
HMIC Health Management Information Consortium [OVID] January 1995 to 9 November 2009 [308 records]; November 2009 to 20 January 2014 [65 hits]; Total = 373 hits
| # | Searches |
| 1 | exp health promotion/ |
| 2 | exp community health services/ |
| 3 | (national adj (poliy or policies or strateg$ or program$)).ti,ab. |
| 4 | exp mass media/ |
| 5 | cities/ |
| 6 | rural population/ or rural health/ |
| 7 | environmental planning.ti,ab. |
| 8 | social environment/ or social network/ or marketing/ or public relations/ |
| 9 | urban health/ |
| 10 | "health education"/ |
| 11 | ((state or county or town or city or village or nation*) adj2 (wide or whole or communit*)).ti,ab. |
| 12 | ((combined$ or multiple or multi or multifactorial or partner$) adj2 (program$ or strateg$ or intervention$ or organi?ation$)).ti,ab. |
| 13 | (media intervention* or whole community or community intervention* or community organsai?ation$1).ti,ab. |
| 14 | (community adj2 (design or action or program* or partner$)).ti,ab. |
| 15 | ((health or community or environment*) adj (policy or policies)).ti,ab. |
| 16 | (urban design or "land use policies" or "land use policy").ti,ab. |
| 17 | ((transportation or travel) adj (policy or policies)).ti,ab. |
| 18 | health planning.ti,ab. |
| 19 | ((neighbo?rhood* or city or cities or community) adj2 (development or regeneration or renewal or design* or plan* or polic*)).ti,ab. |
| 20 | (community wide or community setting$ or community group$ or organi?ation$ level$1).ti,ab. |
| 21 | (Communit$ adj2 base$).ti,ab. |
| 22 | ((built environment* or urban environment* or environmental) adj (change* or intervention*)).ti,ab. |
| 23 | (environment$ adj2 infrastructure).ti,ab. |
| 24 | (urban adj2 (regeneration or renewal or plan* or design* or policy or policies or strateg* or program$)).ti,ab. |
| 25 | ((media or advertising or radio or television or newspaper* or poster* or flyer* or "information booklet*") adj3 (information or education or campaign or intervention or strateg$ or program$ or policy or policies)).ti,ab. |
| 26 | social marketing.ti,ab. |
| 27 | ("point of decision" adj3 (stair* or travel*)).ti,ab. |
| 28 | (health counsel* or individual counsel*).ti,ab. |
| 29 | (community adj3 (collaborati* or coalition)).ti,ab. |
| 30 | ((school* or work?place* or employer* or classroom or college) adj2 (strateg$ or program$ or policy or policies)).ti,ab. |
| 31 | ((public or community) adj2 (information or education or campaign or intervention or strateg$ or program$ or policy or policies)).ti,ab. |
| 32 | (policy change* or fiscal change*).ti,ab. |
| 33 | (policy adj3 (interven$ or change or introduce$ or modif$ or alter$)).ti,ab. |
| 34 | physical infrastructure.ti,ab. |
| 35 | ((road or land) adj us*).ti,ab. |
| 36 | (Legislation or legislative).ti,ab. |
| 37 | ((Voluntary or volunteer or charities or charity or non‐government or government or "not for profit") adj2 (group$1 or organisation$ or department$1 or club$1)).ti,ab. |
| 38 | or/1‐37 |
| 39 | exp exercise/ or exp physical activity/ or fitness/ or physical education/ |
| 40 | running/ |
| 41 | walking/ |
| 42 | swimming/ |
| 43 | (fitness adj class*).ti,ab. |
| 44 | gardening/ |
| 45 | exp dancing/ |
| 46 | exp sport/ |
| 47 | exp yoga/ |
| 48 | recreation/ |
| 49 | (fitness adj (regime* or program*)).ti,ab. |
| 50 | cardiorespiratory fitness.ti,ab. |
| 51 | aerobic capacity.ti,ab. |
| 52 | ((moderate or vigorous*) adj activ*).ti,ab. |
| 53 | (led walk* or health walk*).ti,ab. |
| 54 | (physical adj5 (fit* or train* or activ* or endur*)).ti,ab. |
| 55 | (exercis* adj5 (fit* or train* or activ* or endur*)).ti,ab. |
| 56 | ((leisure or fitness) adj5 (centre* or center* or facilit*)).ti,ab. |
| 57 | ((promot* or uptak* or encourag* or increas* or start* or adher* or sustain* or maintain*) adj5 gym*).ti,ab. |
| 58 | ((promot* or uptak* or encourag* or increas* or start* or adher* or sustain* or maintain*) adj5 physical activ*).ti,ab. |
| 59 | ((promot* or uptak* or encourag* or increas* or start* or adher* or sustain* or maintain*) adj5 (circuit* or aqua*)).ti,ab. |
| 60 | ((promot* or uptak* or encourag* or increas* or start* or adher* or sustain* or maintain*) adj5 (exercis* or exertion or keep fit or fitness class or yoga or aerobic*)).ti,ab. |
| 61 | ((decreas* or reduc* or discourag*) adj5 (sedentary or deskbound or "physical* inactiv*")).ti,ab. |
| 62 | sport*3.ti,ab. |
| 63 | walk*3.ti,ab. |
| 64 | running.ti,ab. |
| 65 | jogging.ti,ab. |
| 66 | pilates.ti,ab. |
| 67 | yoga.ti,ab. |
| 68 | ((cycle or cycling) adj5 (school$ or work or workplace or commut$ or travel$ or equipment or facilit$ or rack$1 or store$1 or storing or park$ or friendly or infrastructure)).ti,ab. |
| 69 | bicycl*.ti,ab. |
| 70 | (bike*1 or biking).ti,ab. |
| 71 | (swim*1 or swimming).ti,ab. |
| 72 | (exercis*3 adj5 aerobic*).ti,ab. |
| 73 | rollerblading.ti,ab. |
| 74 | rollerskating.ti,ab. |
| 75 | skating.ti,ab. |
| 76 | exertion*1.ti,ab. |
| 77 | strength training.ti,ab. |
| 78 | resilience training.ti,ab. |
| 79 | weight lifting.tw. |
| 80 | travel mode*1.tw. |
| 81 | (active adj (travel*4 or transport* or commut$)).tw. |
| 82 | (multimodal transportation or alternative transport* or alternative travel*).ti,ab. |
| 83 | recreation*1.ti,ab. |
| 84 | ("use" adj3 stair*).ti,ab. |
| 85 | (pedestrianis* or pedestrianiz*).ti,ab. |
| 86 | or/39‐85 |
| 87 | (randomized or randomised or placebo or randomly or trial).ab. |
| 88 | Random allocation/ or clinical trial/ or single‐blind method/ or double‐blind method/ or control groups/ or evaluation/ |
| 89 | quasi‐experiment$.ti,ab. |
| 90 | (pre test or pretest or (posttest or post test)).ti,ab. |
| 91 | trial.ti. |
| 92 | (time adj series).ti,ab. |
| 93 | (pre test or pretest or (posttest or post test)).ti,ab. |
| 94 | ((evaluat$ or intervention or interventional) adj8 (control or controlled or study or program$ or comparison or "before and after" or comparative)).ti,ab. |
| 95 | ((intervention or interventional) adj8 (effect* or evaluat* or outcome*)).ti,ab. |
| 96 | ((process or program*) adj3 (effect* or evaluat*)).ti,ab. |
| 97 | (controlled before or "before and after stud$" or follow up assessment).ti,ab. |
| 98 | or/87‐97 |
| 99 | 38 and 86 and 98 |
| 100 | animals/ not (humans/ and animals/) |
| 101 | 99 not 100 |
Limit by date
IUHPE (International Union for Health Promotion and Education)http://www.iuhpe.org 23 November 2009 [0 hits]; 20 January 2014 [0 hits]; Total = 0 hits
Browse
LILACS http://lilacs.bvsalud.org/en/ January 1995 to 13 November 2009 [416 hits]; November 2009 to 17 January 2014 [2 hits]; Total = 428 hits
(Small cities or mass media or cities or health promotion) and (Physical activity or physical fitness or exercise)
MEDLINE (Ovid) January 1995 to 9 November 2009 [Medline/Medline in Process 5691 hits]; November 2009 to 17 January 2014 [3370 hits]; Total = 9061 hits
| # | Searches |
| 1 | exp health promotion/ or residence characteristics/ |
| 2 | community health planning/ or exp community health services/ |
| 3 | (national adj (policy or policies or strateg$ or program$)).ti,ab. |
| 4 | exp mass media/ |
| 5 | community networks/ |
| 6 | community health centers/ |
| 7 | "marketing of health services"/ |
| 8 | cities/ |
| 9 | rural population/ or rural health/ |
| 10 | urban population/ |
| 11 | community‐institutional relations/ |
| 12 | exp environment design/ |
| 13 | city planning/ |
| 14 | environmental planning.ti,ab. |
| 15 | social environment/ |
| 16 | urban health/ |
| 17 | social marketing/ or "health education"/ |
| 18 | ((state or county or town or city or village or nation*) adj2 (wide or whole or communit*)).ti,ab. |
| 19 | ((combined$ or multiple or multi or multifactorial or partner$) adj2 (program$ or strateg$ or intervention$ or organi?ation$)).ti,ab. |
| 20 | (media intervention* or whole community or community intervention* or community organsai?ation$1).ti,ab. |
| 21 | (community adj2 (design or action or program* or partner$)).ti,ab. |
| 22 | ((health or community or environment*) adj (policy or policies)).ti,ab. |
| 23 | (urban design or "land use policies" or "land use policy").ti,ab. |
| 24 | ((transportation or travel) adj (policy or policies)).ti,ab. |
| 25 | health planning.ti,ab. |
| 26 | ((neighbo?rhood* or city or cities or community) adj2 (development or regeneration or renewal or design* or plan* or polic*)).ti,ab. |
| 27 | (community wide or community setting$ or community group$ or organi?ation$ level$1).ti,ab. |
| 28 | (Communit$ adj2 base$).ti,ab. |
| 29 | ((built environment* or urban environment* or environmental) adj (change* or intervention*)).ti,ab. |
| 30 | (environment$ adj2 infrastructure).ti,ab. |
| 31 | (urban adj2 (regeneration or renewal or plan* or design* or policy or policies or strateg* or program$)).ti,ab. |
| 32 | (urban adj2 (regeneration or renewal or plan* or design* or policy or policies or strateg* or program$)).ti,ab. |
| 33 | social marketing.ti,ab. |
| 34 | ("point of decision" adj3 (stair* or travel*)).ti,ab. |
| 35 | (health counsel* or individual counsel*).ti,ab. |
| 36 | (community adj3 (collaborati* or coalition)).ti,ab. |
| 37 | ((school* or work?place* or employer* or classroom or college) adj2 (strateg$ or program$ or policy or policies)).ti,ab. |
| 38 | ((public or community) adj2 (information or education or campaign or intervention or strateg$ or program$ or policy or policies)).ti,ab. |
| 39 | (policy change* or fiscal change*).ti,ab. |
| 40 | (policy adj3 (interven$ or change or introduce$ or modif$ or alter$)).ti,ab. |
| 41 | physical infrastructure.ti,ab. |
| 42 | ((road or land) adj us*).ti,ab. |
| 43 | (Legislation or legislative).ti,ab. |
| 44 | ((Voluntary or volunteer or charities or charity or non‐government or government or "not for profit") adj2 (group$1 or organisation$ or department$1 or club$1)).ti,ab. |
| 45 | or/1‐44 |
| 46 | exp exercise/ |
| 47 | running/ |
| 48 | walking/ |
| 49 | physical fitness/ |
| 50 | swimming/ |
| 51 | (fitness adj class*).ti,ab. |
| 52 | gardening/ |
| 53 | exp "physical education and training"/ |
| 54 | exp dancing/ |
| 55 | exp sports/ |
| 56 | exp yoga/ or exp fitness centers/ or recreation/ or "play and playthings"/ or exp motor activity/ |
| 57 | (fitness adj (regime* or program*)).ti,ab. |
| 58 | cardiorespiratory fitness.ti,ab. |
| 59 | aerobic capacity.ti,ab. |
| 60 | ((moderate or vigorous*) adj activ*).ti,ab. |
| 61 | (led walk* or health walk*).ti,ab. |
| 62 | (physical adj5 (fit* or train* or activ* or endur*)).ti,ab. |
| 63 | (exercis* adj5 (fit* or train* or activ* or endur*)).ti,ab. |
| 64 | ((leisure or fitness) adj5 (centre* or center* or facilit*)).ti,ab. |
| 65 | ((promot* or uptak* or encourag* or increas* or start* or adher* or sustain* or maintain*) adj5 gym*).ti,ab. |
| 66 | ((promot* or uptak* or encourag* or increas* or start* or adher* or sustain* or maintain*) adj5 physical activ*).ti,ab. |
| 67 | ((promot* or uptak* or encourag* or increas* or start* or adher* or sustain* or maintain*) adj5 (circuit* or aqua*)).ti,ab. |
| 68 | ((promot* or uptak* or encourag* or increas* or start* or adher* or sustain* or maintain*) adj5 (exercis* or exertion or keep fit or fitness class or yoga or aerobic*)).ti,ab. |
| 69 | ((decreas* or reduc* or discourag*) adj5 (sedentary or deskbound or "physical* inactiv*")).ti,ab. |
| 70 | sport*3.ti,ab. |
| 71 | walk*3.ti,ab. |
| 72 | running.ti,ab. |
| 73 | jogging.ti,ab. |
| 74 | pilates.ti,ab. |
| 75 | yoga.ti,ab. |
| 76 | ((cycle or cycling) adj5 (school$ or work or workplace or commut$ or travel$ or equipment or facilit$ or rack$1 or store$1 or storing or park$ or friendly or infrastructure)).ti,ab. |
| 77 | bicycl*.ti,ab. |
| 78 | (bike*1 or biking).ti,ab. |
| 79 | (swim*1 or swimming).ti,ab. |
| 80 | (exercis*3 adj5 aerobic*).ti,ab. |
| 81 | rollerblading.ti,ab. |
| 82 | rollerskating.ti,ab. |
| 83 | skating.ti,ab. |
| 84 | exertion*1.ti,ab. |
| 85 | strength training.ti,ab. |
| 86 | resilience training.ti,ab. |
| 87 | weight lifting.tw. |
| 88 | travel mode*1.tw. |
| 89 | (active adj (travel*4 or transportation or commut$)).tw. |
| 90 | (multimodal transportation or alternative transport* or alternative travel*).ti,ab. |
| 91 | recreation*1.ti,ab. |
| 92 | ("use" adj3 stair*).ti,ab. |
| 93 | (pedestrianis* or pedestrianiz*).ti,ab. |
| 94 | or/46‐93 |
| 95 | randomized controlled trial.pt. |
| 96 | controlled clinical trial.pt. |
| 97 | (randomized or randomised or placebo or randomly or trial).ab. |
| 98 | random allocation/ or clinical trial/ or single‐blind method/ or double‐blind method/ or control groups/ |
| 99 | Intervention studies/ |
| 100 | evaluation studies/ |
| 101 | program evaluation/ |
| 102 | Comparative study.pt. |
| 103 | quasi‐experiment$.ti,ab. |
| 104 | (pre test or pretest or (posttest or post test)).ti,ab. |
| 105 | trial.ti. |
| 106 | (time adj series).ti,ab. |
| 107 | (pre test or pretest or (posttest or post test)).ti,ab. |
| 108 | ((evaluat$ or intervention or interventional) adj8 (control or controlled or study or program$ or comparison or "before and after" or comparative)).ti,ab. |
| 109 | ((intervention or interventional) adj8 (effect* or evaluat* or outcome*)).ti,ab. |
| 110 | ((process or program*) adj3 (effect* or evaluat*)).ti,ab. |
| 111 | (controlled before or "before and after stud$" or follow up assessment).ti,ab. |
| 112 | or/95‐111 |
| 113 | 45 and 94 and 112 |
| 114 | animals/ not (humans/ and animals/) |
| 115 | 113 not 114 |
Limit by year
MEDLINE In‐process
As above
NCCHTAhttp://www.ncchta.org 23 November 2009 [1 hit]; 20 January 2014 [3 hits]; Total = 4 hits
Browsed publications for ‘project complete’ and ‘generic health relevance’ in date range
NICEhttp://www.nice.org.uk. 23 November 2009 [4 hits]; 20 January 2014 [2 hits]; Total = 6 hits
Reference lists of physical activity guidance browsed for all included references with a multi‐component intervention.
PsycINFO (Ovid) January 2005 to 9 November 2009 [1315 hits]; November 2009 to 20 January 2014 [876 hits]; Total = 2191 hits
| # | Searches |
| 1 | exp health promotion/ |
| 2 | (national adj (policy or policies or strateg$ or program$)).ti,ab. |
| 3 | exp mass media/ |
| 4 | cities/ |
| 5 | environmental planning.ti,ab. |
| 6 | exp social environment/ or social network/ |
| 7 | "health education"/ |
| 8 | social marketing/ or marketing/ or public relations/ |
| 9 | ((state or county or town or city or village or nation*) adj2 (wide or whole or communit*)).ti,ab. |
| 10 | ((combined$ or multiple or multi or multifactorial or partner$) adj2 (program$ or strateg$ or intervention$ or organi?ation$)).ti,ab. |
| 11 | (media intervention* or whole community or community intervention* or community organsai?ation$1).ti,ab. |
| 12 | (community adj2 (design or action or program* or partner$)).ti,ab. |
| 13 | ((health or community or environment*) adj (policy or policies)).ti,ab. |
| 14 | (urban design or "land use policies" or "land use policy").ti,ab. |
| 15 | ((transportation or travel) adj (policy or policies)).ti,ab. |
| 16 | health planning.ti,ab. |
| 17 | ((neighbo?rhood* or city or cities or community) adj2 (development or regeneration or renewal or design* or plan* or polic*)).ti,ab. |
| 18 | (community wide or community setting$ or community group$ or organi?ation$ level$1).ti,ab. |
| 19 | (Communit$ adj2 base$).ti,ab. |
| 20 | ((built environment* or urban environment* or environmental) adj (change* or intervention*)).ti,ab. |
| 21 | (environment$ adj2 infrastructure).ti,ab. |
| 22 | (urban adj2 (regeneration or renewal or plan* or design* or policy or policies or strateg* or program$)).ti,ab. |
| 23 | ((media or advertising or radio or television or newspaper* or poster* or flyer* or "information booklet*") adj3 (information or education or campaign or intervention or strateg$ or program$ or policy or policies)).ti,ab. |
| 24 | social marketing.ti,ab. |
| 25 | ("point of decision" adj3 (stair* or travel*)).ti,ab. |
| 26 | (health counsel* or individual counsel*).ti,ab. |
| 27 | (community adj3 (collaborati* or coalition)).ti,ab. |
| 28 | ((school* or work?place* or employer* or classroom or college) adj2 (strateg$ or program$ or policy or policies)).ti,ab. |
| 29 | ((public or community) adj2 (information or education or campaign or intervention or strateg$ or program$ or policy or policies)).ti,ab. |
| 30 | (policy change* or fiscal change*).ti,ab. |
| 31 | (policy adj3 (interven$ or change or introduce$ or modif$ or alter$)).ti,ab. |
| 32 | physical infrastructure.ti,ab. |
| 33 | ((road or land) adj us*).ti,ab. |
| 34 | (Legislation or legislative).ti,ab. |
| 35 | ((Voluntary or volunteer or charities or charity or non‐government or government or "not for profit") adj2 (group$1 or organisation$ or department$1 or club$1)).ti,ab. |
| 36 | or/1‐35 |
| 37 | exp exercise/ or exp physical activity/ |
| 38 | running/ |
| 39 | walking/ |
| 40 | physical fitness/ |
| 41 | swimming/ |
| 42 | (fitness adj class*).ti,ab. |
| 43 | gardening/ |
| 44 | exp sports/ |
| 45 | exp yoga/ |
| 46 | recreation/ |
| 47 | (fitness adj (regime* or program*)).ti,ab. |
| 48 | cardiorespiratory fitness.ti,ab. |
| 49 | aerobic capacity.ti,ab. |
| 50 | ((moderate or vigorous*) adj activ*).ti,ab. |
| 51 | (led walk* or health walk*).ti,ab. |
| 52 | (physical adj5 (fit* or train* or activ* or endur*)).ti,ab. |
| 53 | (exercis* adj5 (fit* or train* or activ* or endur*)).ti,ab. |
| 54 | ((leisure or fitness) adj5 (centre* or center* or facilit*)).ti,ab. |
| 55 | ((promot* or uptak* or encourag* or increas* or start* or adher* or sustain* or maintain*) adj5 gym*).ti,ab. |
| 56 | ((promot* or uptak* or encourag* or increas* or start* or adher* or sustain* or maintain*) adj5 physical activ*).ti,ab. |
| 57 | ((promot* or uptak* or encourag* or increas* or start* or adher* or sustain* or maintain*) adj5 (circuit* or aqua*)).ti,ab. |
| 58 | ((promot* or uptak* or encourag* or increas* or start* or adher* or sustain* or maintain*) adj5 (exercis* or exertion or keep fit or fitness class or yoga or aerobic*)).ti,ab. |
| 59 | ((decreas* or reduc* or discourag*) adj5 (sedentary or deskbound or "physical* inactiv*")).ti,ab. |
| 60 | sport*3.ti,ab. |
| 61 | walk*3.ti,ab. |
| 62 | running.ti,ab. |
| 63 | jogging.ti,ab. |
| 64 | pilates.ti,ab. |
| 65 | yoga.ti,ab. |
| 66 | ((cycle or cycling) adj5 (school$ or work or workplace or commut$ or travel$ or equipment or facilit$ or rack$1 or store$1 or storing or park$ or friendly or infrastructure)).ti,ab. |
| 67 | bicycl*.ti,ab. |
| 68 | (bike*1 or biking).ti,ab. |
| 69 | (swim*1 or swimming).ti,ab. |
| 70 | (exercis*3 adj5 aerobic*).ti,ab. |
| 71 | rollerblading.ti,ab. |
| 72 | rollerskating.ti,ab. |
| 73 | skating.ti,ab. |
| 74 | exertion*1.ti,ab. |
| 75 | strength training.ti,ab. |
| 76 | resilience training.ti,ab. |
| 77 | weight lifting.tw. |
| 78 | travel mode*1.tw. |
| 79 | (active adj (travel*4 or transport* or commut$)).tw. |
| 80 | (multimodal transportation or alternative transport* or alternative travel*).ti,ab. |
| 81 | recreation*1.ti,ab. |
| 82 | ("use" adj3 stair*).ti,ab. |
| 83 | (pedestrianis* or pedestrianiz*).ti,ab. |
| 84 | or/37‐83 |
| 85 | (randomized or randomised or placebo or randomly or trial).ab. |
| 86 | Random allocation/ or clinical trial/ or single‐blind method/ or double‐blind method/ or control groups/ |
| 87 | program evaluation/ or evaluation/ |
| 88 | quasi‐experiment$.ti,ab. |
| 89 | (pre test or pretest or (posttest or post test)).ti,ab. |
| 90 | trial.ti. |
| 91 | (time adj series).ti,ab. |
| 92 | (pre test or pretest or (posttest or post test)).ti,ab. |
| 93 | ((evaluat$ or intervention or interventional) adj8 (control or controlled or study or program$ or comparison or "before and after" or comparative)).ti,ab. |
| 94 | ((intervention or interventional) adj8 (effect* or evaluat* or outcome*)).ti,ab. |
| 95 | ((process or program*) adj3 (effect* or evaluat*)).ti,ab. |
| 96 | (controlled before or "before and after stud$" or follow up assessment).ti,ab. |
| 97 | or/85‐96 |
| 98 | 36 and 84 and 97 |
| 99 | animals/ not (humans/ and animals/) |
| 100 | 98 not 99 |
Limit by date
SIGNhttp://www.sign.ac.uk 25 November 2009 [0 hits]; 20 January 2014 [0 hits]; Total = 0 hits
Browse
Sociological Abstracts (Proquest) January 1995 to 13 November 2009 [874 hits]; November 2009 to 17 January 2014 [120 hits]; Total = 994 hits
(SU.EXACT.EXPLODE("Boom Towns" OR "Central Cities" OR "Cities" OR "Communities" OR "Ethnic Neighborhoods" OR "Fishing Communities" OR "Ghettos" OR "Global Cities" OR "Neighborhoods" OR "New Towns" OR "Retirement Communities" OR "Rural Communities" OR "Suburbs" OR "Towns" OR "Villages") OR SU.EXACT.EXPLODE("Health Promotion") OR SU.EXACT.EXPLODE("Editorials" OR "Mass Media" OR "News Media") OR SU.EXACT.EXPLODE("Health Education") OR SU.EXACT.EXPLODE("Marketing") OR SU.EXACT.EXPLODE("Public Relations") OR ti("state wide" OR "nation wide" OR "nationwide" OR "community wide" OR "land use" OR "urban renewal" OR "transportation policy" OR "travel policy" OR "neighbourhood regeneration" OR "mass media" OR advertising OR radio OR television OR newspaper* OR poster* OR flyer* OR social marketing OR "point of decision" OR legislation OR legislative OR policy) OR ab("state wide" OR "nation wide" OR "nationwide" OR "community wide" OR "land use" OR "urban renewal" OR "transportation policy" OR "travel policy" OR "neighbourhood regeneration" OR "mass media" OR advertising OR radio OR television OR newspaper* OR poster* OR flyer* OR social marketing OR "point of decision" OR legislation OR legislative OR policy)) AND ((SU.EXACT.EXPLODE("Physical Fitness") OR SU.EXACT.EXPLODE("Leisure") OR ti(fitness OR aerobic capacity OR activ* OR walk* OR yoga OR sedentary OR deskbound OR inactiv* OR running OR jogging OR pilates OR yoga OR cycle OR cycling OR bicycl* OR bike* OR biking OR swim* OR swimming OR rollerblading OR rollerskating OR skating OR exertion* OR "stair use" OR "active transport*") OR ab(fitness OR aerobic capacity OR activ* OR walk* OR yoga OR sedentary OR deskbound OR inactiv* OR running OR jogging OR pilates OR yoga OR cycle OR cycling OR bicycl* OR bike* OR biking OR swim* OR swimming OR rollerblading OR rollerskating OR skating OR exertion* OR "stair use" OR "active transport*")) AND (ti(randomized OR randomised OR placebo OR randomly OR trial OR "quasi‐experiment*" OR "pre test" OR pretest OR posttest OR "post test" OR "time series" OR "controlled stud*" OR "before and after" OR "controlled before") OR ab(randomized OR randomised OR placebo OR randomly OR trial OR "quasi‐experiment*" OR "pre test" OR pretest OR posttest OR "post test" OR "time series" OR "controlled stud*" OR "before and after" OR "controlled before"))
Limit by year
SPORTDiscus (EBSCOhost) January 1995 to 23 November 2009 [365 hits]; November 2009 to 4 February 2014 [157 hits]; Total = 522 hits
| S1 | TI ("state wide" or “nation* wide” or “community wide” or "land use" or “urban renewal” or “transportation policy” or "travel policy" or “neighbourhood regeneration” or “mass media” or advertising or radio or television or newspaper* or poster* or flyer* or social marketing or "point of decision" * or legislation or legislative or policy) |
| S2 | AB ("state wide" or “nation* wide” or “community wide” or "land use" or “urban renewal” or “transportation policy” or "travel policy" or “neighbourhood regeneration” or “mass media” or advertising or radio or television or newspaper* or poster* or flyer* or social marketing or "point of decision" * or legislation or legislative or policy) |
| S3 | (SU “sports & state") or (SU “community recreation programs (Government)”) |
| S4 | S1 OR S2 OR S3 |
| S5 | TI (fitness or aerobic capacity or activ* or walk* or yoga or sedentary or deskbound or inactiv* or running or jogging or pilates or yoga or cycle or cycling or bicycl* or bike* or biking or swim* or swimming or rollerblading or rollerskating or skating or exertion* or "stair use" or "active transport*") |
| S6 | AB (fitness or aerobic capacity or activ* or walk* or yoga or sedentary or deskbound or inactiv* or running or jogging or pilates or yoga or cycle or cycling or bicycl* or bike* or biking or swim* or swimming or rollerblading or rollerskating or skating or exertion* or "stair use" or "active transport*") |
| S7 | (SU “swimming pools") or (SU “aquatic sports facilities”) or (SU "recreation centers") |
| S8 | S5 OR S6 OR S7 |
| S9 | TI (randomized or randomised or placebo or randomly or trial or “quasi‐experiment*” or pre test or pretest or posttest or “post test” or “time series” or “controlled stud*” or "before and after" or “controlled before”) |
| S10 | AB (randomized or randomised or placebo or randomly or trial or “quasi‐experiment*” or pre test or pretest or posttest or “post test” or “time series” or “controlled stud*” or "before and after" or “controlled before”) |
| S11 | S9 OR S10 |
| S12 | S4 AND S8 AND S11 |
Limit by year
TRID, formerly Tris Online [ http://trid.trb.org/ ] January 1995 to 23 November 2009 [13 hits]; November 2009 to 20 January 2014 [146 hits]; Total = 159 hits
((journey* OR travel* OR transport*) AND (community*) AND (trial* OR intervention* OR experiment*))
Web of Science: Science Citation Index & Social Science Citation Index & Conference Proceedings Citation Index
January 1995 to 13 November 2009 [9,108 hits]; November 2009 to 10 January 2014 [3770 hits]; Total = 12,878 hits
| Set | [Amend limit by year] |
| # 46 | #45 AND #44 AND #25 Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 45 | TS=(randomized controlled trial* OR randomised controlled trial* OR RCT OR controlled trial* OR interrupted time series OR controlled before) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 44 | #43 OR #42 OR #41 OR #40 OR #39 OR #38 OR #37 OR #36 OR #35 OR #34 OR #33 OR #32 OR #31 OR #30 OR #29 OR #28 OR #27 OR #26 Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 43 | TS=(use AND stair*) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 42 | TS=(multimodal transportation OR alternative transport* OR alternative travel* OR recreation* OR pedestrianis* OR pedestrianiz*) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 41 | TS=(bicycl* OR bike* OR biking OR swim* OR swimming OR aerobic* exercise* OR rollerblading OR rollerskating OR skating OR exertion* OR "strength training" OR "resilience training" OR "weight lifting" OR travel mode*) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 40 | TS=((cycle OR cycling) AND (school* OR work OR workplace OR commut* OR travel* OR equipment OR facilit* OR rack* OR store* OR storing OR park* OR friendly OR infrastructure)) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 39 | TS=(sport* OR walk* OR running OR jogging OR pilates OR yoga) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 38 | TS=((decreas* OR reduc* OR discourag*) AND (sedentary OR deskbound OR "physical* inactiv*")) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 37 | TS=((promot* OR uptak* OR encourag* OR increas* OR start* OR adher* OR sustain* OR maintain*) AND (exercis* OR exertion OR keep fit OR fitness class OR yoga OR aerobic*)) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 36 | TS=((promot* OR uptak* OR encourag* OR increas* OR start* OR adher* OR sustain* OR maintain*) AND (circuit* OR aqua*)) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 35 | TS=((promot* OR uptak* OR encourag* OR increas* OR start* OR adher* OR sustain* OR maintain*) AND physical activ*) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 34 | TS=((promot* OR uptak* OR encourag* OR increas* OR start* OR adher* OR sustain* OR maintain*) AND gym*) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 33 | TS=((leisure OR fitness) AND (centre* OR center* OR facilit*)) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 32 | TS=(exercis* AND (fit* OR train* OR activ* OR endur*)) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 31 | TS=(physical AND (fit* OR train* OR activ* OR endur*)) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 30 | TS=(led walk* OR health walk*) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 29 | TS=((moderate OR vigorous*) AND activ*) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 28 | TS=(cardiorespiratory fitness OR aerobic capacity) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 27 | TS=(fitness AND (regime* OR program*)) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 26 | TS=(exercise OR physical fitness OR sport* OR fitness class*) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 25 | #24 OR #23 OR #22 OR #21 OR #20 OR #19 OR #18 OR #17 OR #16 OR #15 OR #14 OR #13 OR #12 OR #11 OR #10 OR #9 OR #8 OR #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1 Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 24 | TS=((Voluntary OR volunteer OR charities OR charity OR non‐government OR government OR "not for profit") AND (group* OR organisation* OR department* OR club*)) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 23 | TS=(Legislation OR legislative) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 22 | TS=((road OR land) AND (use or usage)) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 21 | TS=(physical infrastructure) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 20 | TS=(policy AND (interven* OR change OR introduce* OR modif* OR alter*)) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 19 | TS=(policy change* OR fiscal change*) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 18 | TS=((public OR community) AND (information OR education OR campaign OR intervention OR strateg* OR program* OR policy OR policies)) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 17 | TS=((school* OR work?place* OR employer* OR classroom OR college) AND (strateg* OR program* OR policy OR policies)) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 16 | TS=(community AND (collaborati* OR coalition)) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 15 | TS=(health counsel* OR individual counsel*) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 14 | TS=("point of decision" and (stair* OR travel*)) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 13 | TS=social marketing Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 12 | TS=((media OR advertising OR radio OR television OR newspaper* OR poster* OR flyer* OR "information booklet*") AND (information OR education OR campaign OR intervention OR strateg* OR program* OR policy OR policies)) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 11 | TS=(urban AND (regeneration OR renewal OR plan* OR design* OR policy OR policies OR strateg* OR program*)) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 10 | TS=environment* infrastructure Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 9 | TS=((built environment* OR urban environment* OR environmental) AND (change* OR intervention*)) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 8 | TS=(community wide OR community setting* OR community group* OR organi?ation* level* OR Communit* base*) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 7 | TS=((neighbo?rhood* OR city OR cities OR community) AND (development OR regeneration OR renewal OR design* OR plan* OR polic*)) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 6 | TS=(health planning) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 5 | TS=((urban design OR "land use policies" OR "land use policy" OR transportation OR travel) AND (policy OR policies)) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 4 | TS=((health OR community OR environment*) AND (policy OR policies)) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 3 | TS=(community AND (design OR action OR program* OR partner*)) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 2 | TS=(media intervention* OR whole community OR community intervention* OR community organisation*) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
| # 1 | TS=((state or county or town or city or village or nation*) AND (wide or whole or communit*)) Databases=SCI‐EXPANDED, SSCI, CPCI‐S, CPCI‐SSH Timespan=2011‐2013 |
US Centres for Disease Control and Preventionhttp://www.cdc.gov/ 25 November 2009 [0 hits]; 20 January 2014 [3 hits]; Total = 3 hits
Browsed under nutrition and physical activity sections. In addition one author (JS) provided reference lists for relevant studies included in CDC Community Guide updates.
World Health Organizationhttp://www.who.int/en/ 25 November 2009 [1 hit]; 20 January 2014 [0 hits]; Total = 1 hit
Browse
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Brown 2006.
| Methods |
Study design: Controlled before and after study (independent samples) Sampling frame: Electronic database of telephone numbers Sampling method: Random Collection method: Computer assisted telephone interview Ethics and informed consent: Ethics approved, informed consent limited to the participation in the survey |
|
| Participants |
Communities: Regional cities Country: Australia Ages included in the assessment: 18 ‐ 60 years Reason provided for selection of the intervention community: none stated, presumably location of the study centre and pre‐existing partnerships Intervention community: City of Rockhampton (60,000) Comparison community: City of Mackay (75,000) |
|
| Interventions |
Name of the intervention: 10,000 steps Rockhampton Theory: Social ecologic framework Aim: Evaluation of a whole community approach to improving population levels of physical activity Community strategy development phase: Yes Description of costs and resources: Provided (see below) Components of the intervention as per the inclusion criteria: #1 Social marketing ‐ media campaign; #2 Other communication strategies ‐ including pedometers & logbooks, website advertising, local pharmacies, libraries, posters dog walking; #3 Individual counselling ‐ promotion by health professionals (21 of 23 GP practices); #4 Partnering ‐ specific settings, local activity task force with community organisations, government sport & recreation, business and media organisations; #5 Specific settings ‐ workplaces and shopping malls; #6 Environmental change ‐ "working with the city council to improve local environment, creating repairing key footpaths, "10,000 steps" signage & maps Emphasis of intervention: Promotion physical activity Information given on intensity: Grant scheme of AUD 100,000, plus in kind support. AUD 20,000 spent on paid advertising and event marketing, AUD 50,000 provided through in kind marketing contributions Assessment of intensity: High Start date: August 2001 Duration: 18 months |
|
| Outcomes |
Outcomes and Measures: 1. Active (%). Measurement tool: Active Australia questionnaire Time points: Baseline 2001 and follow‐up 2003 |
|
| Notes | Brown 2006; indicates that the "10,000 steps a day" did not appeal to men. Men were less likely than women to have used a pedometer (thus not appealing to middle‐aged men) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | High risk | Not randomised. Levels of PA different at beginning |
| Performance bias | Unclear risk | One third of control community had heard about the project. Intervention appears to have good integrity, however, one paper suggest that the message was not well received by males "it doesn't speak to me" |
| Attrition bias | Low risk | No cohort study done ‐ so no attrition |
| Detection bias | High risk | Low response rates. Samples not representative, 46.4% in 2001% survey; 47.3% in the 2003 survey (plus persons who could not be contacted because of no telephone) |
| Reporting bias | High risk | Not all of the measures are reported in the completed study that are presented in the Brown 2003 paper (e.g. METs). Summary only reported |
| Other | Unclear risk | Results are difficult to interpret and appear to be a regression to the mean of the state in which the intervention was undertaken. No sample size provided Intervention community is a university town |
| Overall bias | High risk | High Risk. 3 high risk categories |
Brownson 2004.
| Methods |
Study design: Controlled before and after study (independent samples) Sampling frame: Electronic telephone registry Sampling method: Random digit dialling Collection method: Telephone interviews Ethics and informed consent: Unclear |
|
| Participants |
Communities: Rural communities Country: United States Ages included in the assessment: Adults Reason provided for selection of the intervention community: unclear Intervention community: 6 communities in Missouri Comparison community: 6 communities in Arkansas |
|
| Interventions |
Name of the intervention: Bootheel heart health project Theory: Social ecological framework Aim: Increase physical activity / walking Community strategy development phase: Yes Description of costs and resources: none stated Components of the intervention as per the inclusion criteria: #2 Other communication ‐ computer tailored newsletters and cards; #3 Individual counselling (unclear); #4 Partnering ‐ working with volunteers (delivered by community volunteers via organised coalition); #6 Environmental change ‐ walking trails, recognised lack of places to walk Emphasis of intervention: working with community organisations Information given on intensity: "moderate intervention" Assessment of intensity: Medium Start date: December 2000 Duration: 2.5 years |
|
| Outcomes |
Outcomes and measures 1. 7 day total walking for exercise per week 2. 7 day walking for exercise per week Time points: Baseline (December 2000 to May 2001) and follow‐up (June to August 2002) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | Not randomised, no details of allocation. Unclear whether the communities where comparable at baseline (stated communities matched, but no details how "matched according to size, proportion of population African American, poverty levels"). Baseline comparison do not have statistical testing. The intervention community had 25 years of earlier work. It is difficult to ascertain which parts belong in the present intervention and thus it is impossible to determine the effect if the communities were reversed. |
| Performance bias | Unclear risk | No statement of blinding of the communities. There is no statement pertaining to the avoidance of contamination; however the control communities are in a different state and there does not appear to be a mass‐media component that could reach the control communities. The intervention was delivered to the targeted communities and no evidence of delivery to the control. The integrity of the intervention is unclear. |
| Attrition bias | High risk | The outcomes are inconsistent. The follow‐up included a higher percentage of African Americans (38.9% post versus 31.5% baseline) suggesting the sampling is unstable |
| Detection bias | High risk | Assumed to use the measurement tool as intended and in entirety (BRFSS sampling method with self reported measure of walking and physical activity and trail use). No details of blinding. It is unclear whether the outcome measures are reliable as they are self report with face validity only. Used report of physical activity over a week. The samples are not representative with significantly lower representation of males. No data is provided of the response rate. Selection was by random digit dialling. |
| Reporting bias | Low risk | The reports of the study appear to be free of selective outcome reporting as all the results shown are negative findings. The reporting is complete as the reporting is consistent with the ails of reducing the lack of physical activity |
| Other | High risk | Allocation is by community (cluster) and the analysis is aggregated with no adjustment. No sample size provided. There appears to be a "head start" with early work in the intervention community |
| Overall bias | High risk | High risk of bias. 3 high risk categories. Note that with the high risks which could positively influence the results, the findings are negative |
Brownson 2005.
| Methods |
Study design: Controlled before and after study (independent samples) Sampling frame: non‐institutionalised individuals with a telephone Sampling method: random digit dialling Collection method: computer assisted telephone interviews Ethics and informed consent: no information |
|
| Participants |
Communities: Rural communities in Missouri, Tennesee, Kansas USA. Compared to the rest of Missouri and the USA, this region had significantly more poverty, medically underserved, lower education levels. Death rates from chronic diseases (i.e. heart rate, stroke, cancer, diabetes) were significantly higher in the 5‐county intervention area Country: United States Ages included in the assessment: adults Reason provided for selection of the intervention community: Both communities selected because of their demographic comparability Intervention community: 6 communities 6 in the intervention Missouri Ozark Region. Comparison community: 4 control in Tennessee and 2 Arkansas |
|
| Interventions |
Name of the intervention: Theory: Ecological approach Aim: Increase physical activity Community strategy development phase: Yes Description of costs and resources: none stated Components of the intervention as per the inclusion criteria: #1 Social marketing ‐ newspaper articles and media events; #2 Other communication strategies ‐ enrolling people; #3 Individual counselling; #4 Partnering ‐ based on community input ‐ walking clubs, events, trail events Emphasis of intervention: Promoting walking, achieving moderate physical activity Information given on intensity: none stated Assessment of intensity: medium Start date: 2003 Duration: 1 year |
|
| Outcomes |
Outcomes and measures 1. Meeting recommendation for walking (%). Measurement tool: Behavioural risk factor surveillance system 2. Meeting recommendation for moderate PA (%). Measurement tool: Behavioural risk factor surveillance system 3. Mean rates of walking (min). Measurement tool: Behavioural risk factor surveillance system Time points: Baseline and follow‐up (12 months) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | Not randomised. No details of allocation as to why the intervention communities were chosen. Comparison and intervention communities were matched according to size, race, ethnicity and proportion of the population living below the poverty level. However the intervention community had higher education than the control. Required participants to be living near a trail and may not be representative of the community. If the communities were reversed it is unclear what the effects would be as this project was an outgrowth of an earlier project. |
| Performance bias | Low risk | Communities were not blind. Measures were taken to prevent the control communities (unnamed) against contamination as they are in different states. The control communities were not provided with the intervention. There is no evidence to suggest that there are problems with the integrity of the intervention which is substantially described in a wide range of activities. |
| Attrition bias | Unclear risk | Not possible to determine as no description whether the follow‐up survey was undertaken as a cohort or as independent samples |
| Detection bias | Unclear risk | Measurement tools appeared to be applied as intended. No description whether the outcome assessment was blind. Physical activity questions were validated and reliable. Outcome measures quality acceptable as physical activity was measured for a period of a week. Sampling undertaken using random digit dialling. The baseline response rate = 65.2%; no details given for follow‐up methods (independent or cohort) if the follow‐up is n = 1531, 62.0% net response rate of completers is 40.4%. Uncertain of the effect of requiring proximity to a trail. "Eligible households were within a two‐mile radius around an existing trail, which for most communities encompassed the entire town" |
| Reporting bias | Low risk | No evidence of selective outcome reporting. Measures reported upon reflect the aims of the intervention |
| Other | Unclear risk | No issues of statistical quality. However claims of the presence of an effect are made by the authors which are not statistically significant. No details of a sample size calculation provided |
| Overall bias | Unclear risk | 4 unclear categories |
De Cocker 2007.
| Methods |
Study design: Controlled before and after study (cohort follow‐up) Sampling frame: Population registries Sampling method: Random sample, 2500 from each city Collection method: Telephone survey and pedometer Ethics and informed consent: informed consent obtained for data collection |
|
| Participants |
Communities: Urban population (cities) Country: Belgium Ages included in the assessment: 25 to 75 years Reason provided for selection of the intervention community: both cities selected because of their demographic comparability Intervention community: Ghent, capital city of East Flanders (22,800) Comparison community: Asalt, a city located 35km from Ghent (77,000) |
|
| Interventions |
Name of the intervention: 10,000 steps Ghent Theory: Social ecologic approach Aim: Promotion of physical activity to adult population Community strategy development phase: Yes Description of costs and resources: none stated Components of the intervention as per the inclusion criteria: #1 Social marketing ‐ mass media "Physical activity aimed at all adults"; #2 Other communication strategies ‐ website; #4 Partnering ‐ partnerships; #5 Specific settings ‐ workplaces, #6 Environmental changes ‐ signage. "This whole community intervention was designed to intervene at the individual (e.g. pedometer sale), social and environmental level." Emphasis of intervention: Multi‐strategy Information given on intensity: none stated Assessment of intensity: medium Start date: May 2005 Duration: 1 year |
|
| Outcomes |
Outcomes and measures 1. Steps per day. Measurement tool: Pedometer 2. Walking minutes per week. Measurement tool: International Physical Activity Questionnaire 3. Moderate physical activity minutes per week. Measurement tool: International Physical Activity Questionnaire 4. Vigorous physical activity minutes per week. Measurement tool: International Physical Activity Questionnaire 5. Work‐related physical activity minutes per week. Measurement tool: International Physical Activity Questionnaire 6. Transport‐related physical activity minutes per week. Measurement tool: International Physical Activity Questionnaire 7. Household physical activity minutes per week. Measurement tool: International Physical Activity Questionnaire 8. Leisure time physical activity minutes per week. Measurement tool: International Physical Activity Questionnaire Time points: baseline and follow‐up (12 months) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | Not randomised therefore not low. Reasonable comparability of the groups therefore not high. Unclear what the effect would be if the intervention and control communities were reversed |
| Performance bias | Unclear risk | No information of blinding of communities. No evidence of contamination. Not delivered in the control communities. Only 10% of the comparison community had heard of the intervention (compared to a much higher rate in Rockhampton 10,000 steps) |
| Attrition bias | Low risk | Attrition reasonable: Ghent = 24%; Aalst = 22% Incomplete data adequately addressed |
| Detection bias | High risk | The status of blinding is unclear. Measurement tools applied as intended using validated IPAQ. Quantity of physical activity = 1 week. Low response rate. Population: n = 2,500 randomly selected. Response rate in Ghent = 42%. Response rate Aalst = 41% ‐ telephone and postal survey. Completed the follow‐up survey Ghent 76%, Aalst 78%) |
| Reporting bias | Low risk | No evidence of selective outcomes reporting or incompleteness of reporting |
| Other | Low risk | No sample size calculation provided |
| Overall bias | High risk | High risk of bias. High risk category in 1 and unclear in 2 |
Eaton 1999.
| Methods |
Study design: Controlled before and after study (independent samples) Sampling frame: Whole community Sampling method: Cross‐sectional surveys of one person aged 18 to 64 years from randomly selected households Collection method: examination Ethics and informed consent: Unclear |
|
| Participants |
Communities: City Country: United States Ages included in the assessment: 18‐64 Reason provided for selection of the intervention community: unclear Intervention community: City of Pawtucket (population 7529) Comparison community: Name of comparison city withheld (population 7732) |
|
| Interventions |
Name of the intervention: Pawtucket Heart Health Program Theory: Social learning theory Aim: To reduce cardiovascular disease risk factors Community strategy development phase: Yes Description of costs and resources: none provided Components of the intervention as per the inclusion criteria: #2 Other communication strategies ‐ self help materials; #4 Partnering ‐ community organisations, walking club; #5 Specific settings ‐ 27 public and private schools; #6 Environment change ‐ fitness trails, lighted walking tracks Emphasis of intervention: Chronic disease risk factor reduction Information given on intensity: described as "intensive" Assessment of intensity: High Start date: 1982 Duration: 7 years |
|
| Outcomes |
Outcomes and measures: 1. Sedentary (%). Measurement tool: Unnamed questionnaire 2. Knowledge that Physical activity prevents CVD (%). Measurement tool: Unnamed questionnaire 3. Attempted to increase physical activity (%). Measurement tool: Unnamed questionnaire Time points: Baseline (1982 and 1984), Peak intervention (1987 and 1991), Post intervention (1992 and 1993) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | Non‐randomised. Groups appear comparable at baseline although there is no statistical testing. Participants likely to be representative of the communities aimed at whole of community. >1000 participants for both intervention and comparison group for each survey. Response rates Intervention 70%, 67%, 68%, 65%, 68% Control 70%, 68%, 68%, 67%, 64%, 70% |
| Performance bias | Low risk | Communities unblinded. Little risk of contamination given the community based emphasis of the intervention. No mass media component |
| Attrition bias | Low risk | Independent samples, not applicable |
| Detection bias | Unclear risk | Physical activity question used in XS1 and XS2 not validated. Physical activity question used in XS4, XS5 and XS6 has been validated against measures of maximum oxygen consumption (r = 0.6), and has a test‐retest reliability of r = 0.7. Measured over period of the week |
| Reporting bias | Low risk | No indication of missing data in the reporting |
| Other | High risk | No sample size calculation provided |
| Overall bias | Unclear risk | 2 unclear, 3 low risk |
Gao 2013.
| Methods |
Study design: Controlled before and after study (non random allocation with independent cross‐sectional sampling) Sampling frame: Lists of community households of three districts. Sampling method: Population level through community as sampling framework with random sampling, comparisons not at the same time. One of the eligible persons in the sampled households identified with the Kish method Collection method: In‐person Questionnaire applied by trained interviewers Ethics and informed consent: Approved by ethics review board. Informed consent ensuring privacy and confidentiality |
|
| Participants |
Communities: City districts (2 intervention, 1 control) Country: China Ages included in the assessment: Adults, residents aged 18–64 years who had lived in the local district for at least 1 year Reason provided for selection of the intervention community: The authors stated the control communities lacked capacity for the intervention Intervention community: 2 districts of Hangzhou China ‐ Xia Cheng District and Gongshu District Comparison community: 1 district of Hangzhou China ‐ Xihu district |
|
| Interventions |
Name of the intervention: Check the Community Interventions for Health (CHI) Theory: Social‐ecological approach Aim: Increase physical activity (reduce physical inactivity) and change knowledge, attitudes and behaviour with respect to three major lifestyle (smoking, physical activity and diet) Community strategy development phase: unclear Description of costs and resources: none stated Components of the intervention as per the inclusion criteria: #1 Social marketing ‐ mass media; #2 Other communication strategies ‐ poster campaigns; #3 Individual counselling including fitness tests and free disease screening and risk assessment for cardiovascular disease; #4 Partnering ‐ based on community input ‐ walking clubs, events, trail events. #5 settings of neighbourhoods, schools, workplaces and community health centres settings; #6 Environmental component with signage for encouraging walking, places for walking, walking distances, health theme parks for exercising Emphasis of intervention: Physical activity, whole of community Information given on intensity: Authors stated that they did not pursue highest intervention intensity Assessment of intensity: Medium Start date: 2009 Duration: 2 years |
|
| Outcomes |
Outcomes and Measures: 1. METS/week measured with IPAQ 2. % of people physically active at specified level (High level physical activity) Secondary measures 3. Recognise PA is good for your body: Cognition score of the advantages of physical activity Time points: Baseline and follow up (2 years) Baseline Oct 2008 to Aug 2009; follow up June 2011 to Feb 2012 |
|
| Notes | Gao 2013 was identified as the primary paper published first in Chinese with the physical activity only reported Lv 2014 is a duplicate publication | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | High risk | Non‐randomised. Comparison appears to be purposefully unfair: "Two intervention areas have better bases to comply with the design and implement intervention activities." Considerable differences between the comparison communities: 1) Relative to the individuals in the comparison area, the individuals in the intervention areas demonstrated a higher mean age at baseline, a lower education level and a lower socioeconomic status; in addition, in the intervention areas there was a lower proportion of household‐owned cars than in the comparison area. 2) Considering the outcome of interest the intervention area at baseline had higher proportion of individuals in moderate and higher IPAQ categories (70.5%) than in the comparison area (65.6%) |
| Performance bias | High risk | No measures undertaken to protect against contamination although More people in the intervention area (87.8%) than in the control (78.6%) saw or participated in the mentioned events or activities. Unblinded |
| Attrition bias | Low risk | They used the same number of participants in both surveys (pre and post) |
| Detection bias | Low risk | Used IPAQ |
| Reporting bias | Low risk | The IPAQ assessed PA undertaken across a comprehensive set of domains including (1) leisure time PA; (2) domestic and gardening activities; (3) work‐related PA; (4) transport‐related PA, and reported as median (IQR) of MET ‐ minutes per week. Percentage of participants in each of the IPAQ categories |
| Other | Unclear risk | No details of sample size calculation provided. The authors identified the control community did not have the capacity to undertake the intervention |
| Overall bias | High risk | |
Goodman 1995.
| Methods |
Study design: Controlled before and after study (cohort follow‐up) Sampling frame: Telephone directory and city directory for households Sampling method: Random Collection method: Questionnaire: telephone and non‐telephone Ethics and informed consent: No information given regarding ethical approval. Consent obtained for physical measurements |
|
| Participants |
Communities: Urban city Country: United States Ages included in the assessment: > 18 years of age Reason provided for selection of the intervention community: "selected first" Intervention community: City of Florence (population 56,240) Comparison community: City of Anderson (population 51,014) |
|
| Interventions |
Name of the intervention: Heart to Heart Project Theory: Not explicitly stated Aim: Chronic disease prevention Community strategy development phase: Unclear Description of costs and resources: Received 2.2 million dollars over 5 years run by local public health staff members in consultation from state health department and the CDC Components of the intervention as per the inclusion criteria: #1 Social marketing ‐ through mass media; #2 Other communication strategies ‐ development of health promotion programs; #3 Individual counselling ‐ through health providers; #4 Partnerships ‐ working with other organisations; #5 Specific settings ‐ churches, and with work places ‐ "development of health promotion programs distributed to local work sites"; #6 Environmental changes ‐ the development of walking trails throughout Florence Emphasis of intervention: Chronic disease prevention Information given on intensity: Not described Assessment of intensity: Low Start date: 1987 Duration: 5 years |
|
| Outcomes |
Outcomes and measures 1. Physical inactivity (%) Measurement tool: unnamed questionnaire Time points: Baseline (1987) and follow up (1991) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | Non‐randomised, controlled before and after cohort with a matched community. Allocation unclear. The groups appeared to be comparable at baseline. Intervention community matched for population size and race, income, education and vital statistics, and by economic indicators. No statistical tests undertaken to determine if differences were significant. No reason to believe that the communities couldn't be reversed |
| Performance bias | Unclear risk | Blinding of the communities unknown. Measures were undertaken to protect against contamination. The two communities had different media markets (were as far apart in South Carolina as possible) and the intervention not delivered to the control. Potential problems with the integrity of the intervention as it appears not to be delivered as planned: “The evaluation showed that some of the items of the design did not match the actual projects delivered” |
| Attrition bias | Low risk | Attrition rate for cohort from baseline to follow‐up (5 years) was 29.3% |
| Detection bias | Unclear risk | No reason to believe measurement tools were not applied as intended. No indication that outcome assessor was blinded. Outcome measure metrics were validated "each survey question was evaluated as the rationale, reliability, consistency and validity". Physically inactive was defined as engaging in no physical activity or exercise during the last month. Individuals sampled are likely to be representative. Samples were randomly drawn through random digit dialling. The response rates in 1987 were 83% with telephone and 94% without telephone. No difference between communities |
| Reporting bias | Low risk | No evidence of selective outcome reporting or incompleteness of reporting. Measures reported match the aims |
| Other | Unclear risk | No other issues. Statistical quality acceptable. No sample size calculation for physical activity. No appearance of "head‐start" advantage |
| Overall bias | Unclear risk | Unclear risk of bias (> 3 unclear) |
Gu 2006.
| Methods |
Study design: Controlled before and after study (cohort follow up) Sampling frame: Regular residents Sampling method: Cross‐section surveys of all residents Collection method: Questionnaire survey, physical examination and laboratory tests Ethics and informed consent: not stated |
|
| Participants |
Communities: Rural villages Country: China Ages included in the assessment: 25 to 74 years Reason provided for selection of the intervention community: The two intervention villages were chosen for convenience Intervention community: Two villages in Jiaxing, Shejian Province (total population 2404) Comparison community: Control village. Not clear |
|
| Interventions |
Name of the intervention: None provided Theory: None reported Aim: Risk factors for CVD including physical activity Community strategy development phase: Yes Description of costs and resources: None provided Components of the intervention as per the inclusion criteria: #2 Other communication strategies ‐ using various kinds of media brochures, classes and information board; #3 Individual counselling ‐ health professionals Emphasis of intervention: several strategies, but appears to involve individual counselling by health professionals. Also emphasis on mass media "propagandism" Information given on intensity: no information Assessment of intensity: high Start date: 1998 Duration: 5 years |
|
| Outcomes |
Outcomes and measures 1. Non‐occupational physical activity Measurement tool: unnamed questionnaire Time points: Baseline and follow up (5 years) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | Non‐randomised. No details for reason of allocation. The author stated that there was no significant difference in demographic characters without reporting detailed information. However, the prevalence of hypertension in intervention group was significantly higher at baseline |
| Performance bias | Unclear risk | No details of blinding. The control community was in a different village in a different town, assume using local knowledge there would be reasonable distance for no overlap |
| Attrition bias | High risk | Stated that the two surveys were conducted with the same sample before and after intervention (5 years). The sample size in the second survey was about 30% smaller than at baseline. The authors did not report reasons and effects of this attrition |
| Detection bias | High risk | The tool to measure physical activity was a set of questions. No detailed information about validity and reliability. Questions pertain to a weeks period. Participants were all adults in a village. Not possible to determine whether the persons selected were representative of the population. Measured persons ages 25 to 74 years |
| Reporting bias | High risk | Results on physical activity were not reported although stated in the methods of the thesis. Personal communication confirmed the measurement both pre and post‐intervention. The reason provided for not reporting was that "PA was not considered to be the main outcome of this intervention." It is highly probable that the results for PA were of no difference or were lowered by the intervention |
| Other | Unclear risk | No results about the intervention effects on physical activity were reported though measured. No mention of a sample size calculation. Further communication via email and telephone was rejected by the author |
| Overall bias | High risk | High risk of bias. 3 high risk categories |
Guo 2006.
| Methods |
Study design: Controlled before and after study (independent samples) Sampling frame: all residents > 35 years old Sampling method: Convenience sample Collection method: questionnaire survey (face to face interview) plus physical examination Ethics and informed consent: Ethics and informed consent unclear |
|
| Participants |
Communities: Rural Villages Country: China Ages included in the assessment: 35 years and older Reason provided for selection of the intervention community: none stated Intervention community: Tam Mu Gang (unknown population) Comparison community: Nan Guan Cum (unknown population) |
|
| Interventions |
Aim: To enhance public awareness regarding hypertension and to change unhealthy lifestyles and behaviours Community strategy development phase: Yes Description of costs and resources: none provided Components of the intervention as per the inclusion criteria: Primarily health education to enhance awareness of hypertension health life style and behaviours. #1 Social marketing ‐ mass media, including information boards for the whole community; #2 Other communication strategies ‐ one brochure per household about healthy lifestyle; #3 Individual counselling ‐ classes and seminars by health professionals (settings unspecified), Individual consultation to persons at high risk and to patients Emphasis of intervention: multiple strategies Information given on intensity: not given Assessment of intensity: Medium Start date: October 2004 Duration: 1 year |
|
| Outcomes |
Outcomes and measures: 1. Number of people involved in physical exercises. Measurement tool: Unnamed questionnaire Time points: Baseline and follow up (1 year) |
|
| Notes | Intervention increased knowledge and awareness of hypertension treatment. Very brief reporting | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | Not randomised and no details of the reasons for allocation. Stated that the two communities were comparable in terms of demographic characters, and prevalence of hypertension. The two communities were not adjacent. Comparisons were done after intervention with samples from these communities. However, it was not clear about the characters of populations and the methods to determine the samples. Unclear what the effects would be of reversing the communities |
| Performance bias | Low risk | No special measures were taken to prevent contamination. The control community was in a different village but it is unclear whether they were the same town, assume using local knowledge, they stated that there would be reasonable distance for no overlap. No interventions in control |
| Attrition bias | Unclear risk | Independent samples ‐ attrition not applicable |
| Detection bias | High risk | Physical activity was measured using survey questions. No information about the source and validity. Representativeness unclear because no information about the populations and methods to draw the samples |
| Reporting bias | Unclear risk | Very brief reporting. Can not determine which measures were undertaken and which were reported |
| Other | Unclear risk | Data on PA were numbers only. No indication a sample size calculation was undertaken |
| Overall bias | High risk | High risk of bias. 2 high risk categories |
Jenum 2006.
| Methods |
Study design: Controlled before and after study (cohort follow up) Sampling frame: Whole community Sampling method: All individuals invited by letter Collection method: Survey Ethics and informed consent: Ethical review and informed consent obtained |
|
| Participants |
Communities: Districts of Oslo Country: Norway Ages included in the assessment: 30 to 67 years Reason provided for selection of the intervention community: Highest mortality rates and most disadvantaged Intervention community: Romsas, a district of Oslo (population 6700) Comparison community: Furuset, a neighbouring district in Oslo |
|
| Interventions |
Name of the intervention: Romsas in motion Theory: Based on social‐psychological and ecological models and perspectives of empowerment and participatory approaches Aim: Promoting physical activity Community strategy development phase: Yes Description of costs and resources: "low cost" Components of the intervention as per the inclusion criteria: 4 main strategies of 10 intervention components. #1 Social marketing ‐ mass media communication to communicate information about physical activity & promote physical activity programs of the project; #2 Other communication strategies ‐ various; #3 Individual counselling ‐GPs prescribed physical activity programs; #4 Partnering ‐ participatory approaches of local health & welfare workers, incorporated in strategic plans of the community; #6 Environmental change ‐ environmental approaches Emphasis of intervention: Difficult to tell: but appears to have an emphasis on #4 working with organisations Information given on intensity: none stated Assessment of intensity: Medium Start date: 2000 Duration: 3 years |
|
| Outcomes |
Outcomes and measures: 1. Physically inactive (%). Measurement tool: Unnamed questionnaire 2. Change in physical activity (hours per week). Measurement tool: Unnamed questionnaire 3. Physically inactive (stages of change). Measurement tool: Unnamed questionnaire Time points: Baseline and follow up (3 years) |
|
| Notes | Participation in physical activity groups were more strongly related to forward transition in stages of changes in physical activity than others. Exposure and participation rates in the various interventions components varied greatly (1.5% to 92.7%) | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | The communities were not randomised. There is evidence that the groups are not comparable although not statistically significant (Intervention community, 12% less had full time work, 8% more were on disability pension, 5% more smoked, 4% more physically inactive). The Intervention community is the most disadvantaged in Oslo |
| Performance bias | Unclear risk | No indication of blinding. Some possibility of contamination with neighbouring district (e.g. mass media etc) |
| Attrition bias | High risk | Incomplete data not adequately addressed. Attrition from intervention 33.4% and control was 33% |
| Detection bias | High risk | Unclear whether the measurement tools were used as intended and in their entirety. No details of blinding of outcome assessors. Used "a specially designed questionnaire concerning physical activity". A summary document identifies the measure as the IPAQ a validated questionnaire reporting for 1 week. Of the 6140 invited subjects 2950 (48%) completed the survey; reporting outcomes only for those persons 30 to 67 years |
| Reporting bias | High risk | Likely, the baseline publication provides data of METS min per week for leisure time, however this is absent in the follow‐up results with no explanation |
| Other | Low risk | No sample size calculation undertaken, but whole of community sample |
| Overall bias | High risk | High risk of bias. Three high risk categories |
Jiang 2008.
| Methods |
Study design: Controlled before and after study (independent samples) Sampling frame: Community aged 35 to 74 years Sampling method: Randomised cluster sampling Collection method: Face to face questionnaire survey and physical examination Ethics and informed consent: not stated |
|
| Participants |
Communities: Urban communities in Beijing (2 communities) Country: China Ages included in the assessment: 35 to 74 years Reason provided for selection of the intervention community: Intervention community: Chongwen community in Beijeng (population about 50,000) Comparison community: Xicheng community in Beijeng (population about 50,000) |
|
| Interventions |
Name of the intervention: Theory: none stated Aim: Prevention and control of hypertension Community strategy development phase: Yes Description of costs and resources: none provided Components of the intervention as per the inclusion criteria: #2 Other communication strategies ‐ handouts were distributed 4 times a year going house to house, community information board 4X a year; #3 Individual counselling ‐ Individual screening everyone (73% participation) and then counselling by health professionals for high risk factors; #4 Partnering ‐ involved community councils comprising of primary health education and health promotion about healthy diet, increasing physical activity and less drinking Emphasis of intervention: Individual counselling Information given on intensity: not described Assessment of intensity: High Start date: 1997 Duration: 3 years |
|
| Outcomes |
Measures: Regular exercise (singular simple question) Time points: Baseline (1997) and follow up (2000) |
|
| Notes | Improvements observed in health knowledge, care about health. No change in other health outcomes measured | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | Not randomised. Not details of reasons for allocation. Stated that the two communities were comparable in terms of population, economics and culture. The samples from these communities were comparable in terms of age and gender. There is nothing to suggest that the communities couldn't be reversed |
| Performance bias | Low risk | Communities not blinded. No special measures were taken to prevent contamination. The control community was in a different district and no interventions were provided to the control. Considering the communities were chosen from two districts of Beijing and the nature of the interventions (mass media, workshops, patient management etc.) and of the city of Beijing, it is unlikely contamination of the control group occurred. The integrity of the intervention is unclear |
| Attrition bias | Low risk | Independent samples ‐ Attrition not applicable. The post‐intervention surveys were conducted in different samples from baseline but within the studied communities |
| Detection bias | Unclear risk | It is likely the tools were applied as intended and in their entirety. Physical activity was measured using individual questions without detailed information on their source and validity. No details of duration of PA. Representativeness is unclear. The two studied communities had 50,000 residents each. Surveys were done with randomised samples (839 to 962) from the communities before and after intervention |
| Reporting bias | Low risk | Both positive and negative results were reported. The measures reported are the same as those described in the aims of the intervention |
| Other | Unclear risk | Allocation and analyses were done by community. The net changes after intervention were calculated and tested. No description of a sample size calculation |
| Overall bias | Unclear risk | Unclear risk of bias |
Kamada 2013.
| Methods |
Study design: Cluster randomised controlled trial Sample frame: Computer based resident registry system Collection method: Postal questionnaire with 74% response rate, participants blinded to the study design and hypothesis Ethics and informed consent: Ethical review and informed consent obtained. |
|
| Participants |
Communities: whole of communities (12) within Unnan (population 45,364, rural mountainous region of Shimane) Country: Japan Ages included in the assessment: residents aged 40 to 79 years (middle‐aged and elderly people) Reason provided for selection of the intervention community: Randomised, not otherwise specified, assumed risk of need to increase PA to middle‐age elderly people, particularly aerobic, flexibility and muscle strengthening activities Intervention community: 3 arms of intervention comprising of 3 communities (neighbourhood populations not specified) Comparison community: 3 matched neighbourhoods |
|
| Interventions |
Name of the intervention:COMMUNICATE (COMMUNIty‐wide Campaign To promote Exercise) (CWC) Theory: Stages of change model Aim: Promoting physical activity in middle‐aged and elderly people Community strategy development phase: Unclear Description of costs and resources: none provided Components of the intervention as per the inclusion criteria: #1 audio broadcasts delivered to households in the intervention communities via cable network. #2 flyers, leaflets, community newsletters, posters, banners delivered to households directly, #4 and #5 cooperative relationships developed with education and sports organizations, regional development departments of Unnan City Hall, Unnan police department, community self‐administered organizations, Senior citizens club, schools and clinics. also includes community events, provision of pedometers and reflective material, DVD’s, call centre but no environmental component Three arms of the intervention: Group FM ‐ Flexibility ‐ focus on mainly stretching exercises, Group A ‐ Activity ‐ mainly walking, and Group AFM ‐ combination of promotion of mainly walking and stretches Group A, the walking behaviour was promoted for aerobic activity. It also included information, education, and support delivery, according to a social marketing process Authors identify a social marketing campaign implementation program: Situational analysis. Market segmentation and targeting. Used theTARPARE model to determine the primary communication target segment. Setting objectives and marketing strategy development. A CWC follows the “4 Ps” concept of marketing mix (i.e. making sure the right Product is available at the right Price, in the right Place and is well‐Promoted) Information given on intensity: not described, used existing infrastructure. Supplies and costs for producing new materials (leaflets etc.) and kept to a minimum. Assessment of intensity: Low, specifically targeted some segments of the population Start date: November 2009 Duration: 1 years |
|
| Outcomes |
Outcomes and Measures: Per cent of people engaged in regular physical activity comprising of: 1. engaging in 150 mins/week or more of walking a number of days per week and mean number of minutes walked per day was recorded (walking time for recreation and transport was included) 2. engaging in daily flexibility activity – assessed categorically (daily, not daily but occasionally, not at all) 3. engaging in muscle‐strengthening activities two or more days a week Study also reports on low back and knee pain ‐ self reported; awareness, knowledge, belief and intention of the intervention or physical activity Time points: Baseline and 1 year |
|
| Notes | Authors conclude: 1. The CWC did not promote physical activity in 1 year. 2. Did not increase walking time Significant differences were observed in awareness and knowledge between intervention and control groups as short‐term impacts of the campaign |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Low risk | Cluster randomised controlled trial with a community as the unit of randomisation, randomly allocated nine communities to the intervention groups and three to the control group Cluster randomised controlled, superiority trial, stratified by high, moderate and low population density, with imbalanced randomisation (three interventions; one control) Randomization of the clusters was done using a computer‐generated list of random numbers by a clerical staff member of Unnan City Hall, blind to the name and identity of the clusters. Another staff member had a list of all cluster names and the relevant numbers and assigned the clusters. Neither staff member was involved in the intervention, evaluation, and analysis of this study |
| Performance bias | Low risk | Residents blinded to (not informed about) the study design and hypothesis (i.e. the existence of the control group and cluster allocation). Because the local audio broadcast system was established all over Unnan using a network of cables it could be controlled to broadcast campaign messages limited to specific relevant communities in order to avoid contamination of the intervention. All three components of the CWC were implemented in all intervention communities, although some components were weakly or not implemented in some communities because of the lack of resources and/or the feature (e.g. low population) of the relevant community |
| Attrition bias | Low risk | No attrition |
| Detection bias | Low risk | Both participants and data collectors randomly‐sampled residents. Japan IPAQ, validated. Applied as intended. The 1‐week test‐retest reliability of the walking questionnaire was acceptable (Spearman’s P = 0.79) The criterion‐related validity of this self‐administered walking questionnaire compared with average daily step counts recorded by uniaxial accelerometer (Lifecorder, Suzuken Co., Ltd., Nagoya, Japan was also found to be acceptable (Spearman’s P = 0.38) in 95 elderly subjects (40 men and 55 women) aged 74.9 ± 4.5 (range 62 to 85) years living in the city of Unnan |
| Reporting bias | Low risk | IPAQ reported. Each arm reported. METS not reported. Authors conclusions of negative findings, thus reporting bias unlikely to be applicable |
| Other | Low risk | Statistical methods acceptable. Detailed ample size calculation in the protocol (supplied). Trial registered: UMIN‐CTR, UMIN000002683 |
| Overall bias | Low risk | |
Kloek 2006.
| Methods |
Study design: Controlled cluster before and after study (cohort follow up) Sampling frame: Not identified Sampling method: Random sample Collection method: postal questionnaire Ethics and informed consent: Medical ethical committee of Catharina Hospital. Informed consent unclear |
|
| Participants |
Communities: Neighbourhoods in Eindhovern (3 intervention, 3 control) Numbers range from 1800 to 6700) |
|
| Interventions |
Name of the intervention: Program "Wijkegezondheidswek" Theory: Transtheoretical model stages of change, attitude social influence ‐ efficacy model Aim: Improve health related behaviour outcomes Community strategy development phase: Yes Description of costs and resources: none stated Components of the intervention as per the inclusion criteria: #1 Social marketing ‐ mass media; #3 Individual counselling ‐ provided face to face; #4 Partnering ‐ working with coalitions ‐ community; #5 Specific settings ‐ special events held in schools Emphasis of intervention: Multiple strategies Information given on intensity: none given Assessment of intensity: Low Start date: 2000 and 2001 Duration: 2 years |
|
| Outcomes |
Outcomes and measures: 1. Enough physical activity (%). Measurement tool: Short Questionnaire to Assess Health Enhancing Physical Activity (SQUASH) 2. Physical activity (METs/wk). Measurement tool: Short Questionnaire to Assess Health Enhancing Physical Activity (SQUASH) 3. Physical activity stages of change. Measurement tool: Unnamed questionnaire 4. Physical activity attitude score. Measurement tool: Unnamed questionnaire 5. Physical activity efficacy score. Measurement tool: Unnamed questionnaire Time points: Baseline (2000) and follow up (2002) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | Non‐randomised. Groups appear to be comparable at baseline. Participants likely to be representative of the community. Both intervention and control equally deprived |
| Performance bias | Low risk | Not much mass media, most intervention based on community, neighbourhoods, schools etc. |
| Attrition bias | Unclear risk | Cohort ‐ attrition rate 31% |
| Detection bias | Low risk | Validated questionnaire used. Unkown if assessors blinded. Participants likely to be representative of the community as random sample with response rate of 60% |
| Reporting bias | Low risk | No evidence of reporting bias |
| Other | Unclear risk | No statement of sample size calculation |
| Overall bias | Unclear risk | Unclear risk of bias. 3 Unclear and 3 low risk categories |
Kumpusalo 1996.
| Methods |
Study design: Controlled cluster before and after study (independent) Sampling frame: All residents of villages Sampling method: census Collection method: No information Ethics and informed consent: None described |
|
| Participants |
Communities: Rural Villages Country: Finland Ages included in the assessment: 20 to 64 years Reason provided for selection of the intervention community: unclear Intervention community: 4 villages, although only 2 qualify with both pre and post measurement. (populations between 220 and 490 inhabitants) Comparison community: 2 comparison communities |
|
| Interventions |
Name of the intervention: Finnish Healthy Village Study Theory: standard health promotion principles of inter‐sectorial collaboration Aim: Improve healthy lifestyles Community strategy development phase: No Description of costs and resources: described as "low cost" Components of the intervention as per the inclusion criteria: #2 Other communication strategies ‐ booklets sent to every household, Village seminars once a month during Autumn and Spring terms; #3 Individual counselling ‐ "intensive advice given by local health nurses"; #4 Partnering ‐ clubs, Red Cross, hunting clubs etc, study group, sports groups, walking campaigns; #5 Specific settings ‐ local adult education centres Emphasis of intervention: none identified Information given on intensity: none given Assessment of intensity: Medium Start date: 1986 Duration: 3 years |
|
| Outcomes |
Outcomes and measures: 1. Physically active during leisure time (%). Measurement tool: unnamed questionnaire 2. Physical inactive during leisure time (%). Measurement tool: unnamed questionnaire Time points: Baseline and follow up (3 years) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | No description of reasons for allocation. Non randomised ‐ quasi experimental. Can't tell if the communities are comparable at baseline as there is inadequate demographic data and inadequate statistical testing. Aims to be inclusive of the community. Difficult to tell what the effects might be if the control and community communities were reversed |
| Performance bias | High risk | No details of blinding of communities. Limited measures taken to protect against contamination as villages are quite close. Possibly some contamination as some of the intervention was delivered to the control "Due to ethical imperatives and the relatively short distances between the villages, some extra activities, such as walking tests, health seminars and personal feedback of the results of individual health examinations, were also organized in the control villages." Efforts made to ensure intervention integrity "During the program, a careful process evaluation was made.." |
| Attrition bias | High risk | Communities with both baseline data and follow‐up data are included in the analysis in accordance to the inclusion criteria (those with outcome only data excluded). Attrition 34% not adequately addressed |
| Detection bias | Unclear risk | Nothing otherwise to indicate that the measurement tools weren't used in their entirety. No indication of blinding. Questionnaires assessed for internal consistency and reliability only. No indication of any assessment of validity. Physical activity measured over one week (adequate duration). Representative, aimed for whole of village inclusion with response rates ranging from 88% to 55% |
| Reporting bias | Low risk | No evidence of selective outcome reporting as outcomes in baseline publication are consistent with outcome publication. Measures reported are the same as those described in the aims of the intervention |
| Other | Low risk | No statement of sample size calculation |
| Overall bias | High risk | 2 high risk of bias, 3 unclear |
Luepker 1994.
| Methods |
Study design: Controlled before and after study (cohort follow‐up and independent samples) Sampling frame: census blocks Sampling method: random selection of census blocks. Geographically adjacent groups of 5 households were randomly selected within those blocks Collection method: in‐person measurement Ethics and informed consent: No details of informed consent or ethical approval |
|
| Participants |
Communities: Towns in the upper mid‐west, Minnesota Country: United States Ages included in the assessment: 25 to 74 years Reason provided for selection of the intervention community: unclear Intervention community: The towns of Mankato (population 37,812), Fargo‐Moorhead (population 111,579) and Bloomington (population 81,831) Comparison community: The towns of Winona (population 25,075), Sioux Falls (81,831) and Roseville (population 74,731). These towns were matched for size of community, type of community, and distance from the Twin Cities |
|
| Interventions |
Name of the intervention: Minnesota Heart Health Program Theory: Social learning theory; Persuasive communications theory and models for involvement of community leaders and institutions Aim: Cardiovascular disease prevention Community strategy development phase: Unclear Description of costs and resources: None described Components of the intervention as per the inclusion criteria: #1 Social marketing ‐ through mass media; #2 Other communication strategies; 3) Individual counselling; 4) Partnering ‐ working with sporting clubs etc; #5 Specific settings ‐ in workplace; 6) Environmental change. Emphasis of intervention: Multi‐level high intensity media campaign Information given on intensity: described as high intensity Assessment of intensity: High Start date: Baseline measurement for 16 months. Intervention commenced 1981 Duration: 5 to 6 years |
|
| Outcomes |
Outcomes and measures: 1. Leisure time physical activity (%). Unnamed questionnaire 2. Physical activity score kcal/day. Home interview Time points: Baseline (for 3 years) and post‐intervention (years 1, 3, 5 and 6 (pooled comparison)) |
|
| Notes | Smoking was measured and decreased in females only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | Non‐randomised. Significant but small differences in groups for multiple characteristics. No suggestion that reversal of intervention and control communities would alter results |
| Performance bias | Low risk | No indication communities were blinded. Paper suggests intervention delivered as intended. No evidence of contamination through as the communities were a significant distance apart |
| Attrition bias | Low risk | Cohort study suffered acceptable attrition |
| Detection bias | Unclear risk | Blinding status of outcome assessors unknown. Leisure time physical activity was assessed as the percentage of participants who answered "yes" to the question "Are you regularly active in your leisure time?" Leupker cites two questionnaires for physical activity, however the validity of the work‐time physical activity measure is not established. It seems unlikely this was used in full. Representativeness good. Cross sectional study had > 100 participants in each survey, 300 to 500 randomly selected adults sampled periodically (cross‐sectional). A baseline cohort was also followed. Response rates were high (> 60%) |
| Reporting bias | Low risk | Reports of the study appear to be free of selective reporting. Measures reported same as expected and match aims of the intervention |
| Other | Low risk | Sample size calculation undertaken, but not described |
| Overall bias | Unclear risk | Unclear risk of bias. This study used a better study design than most trials |
Lupton 2003.
| Methods |
Study design: Controlled before and after study (cohort follow up) Sampling frame: All residents aged 20 to 62 years Sampling method: A complete cohort of resident aged 40 to 62 years was included, and a random sample of those aged 20 to 39 years Collection method: Questionnaires and physical examination Ethics and informed consent: Ethical approval obtained. Informed consent unclear |
|
| Participants |
Communities: Regional villages in the county of Finnmark (located in the Arctic region of Norway) Country: Norway Ages included in the assessment: 20 to 62 years Reason provided for selection of the intervention community: "local initiative" Intervention community: The village of Batsfjord (population 2500) Comparison community: The villages of Loppa, Gamvik and Maoy (total population 5000) |
|
| Interventions |
Name of the intervention: Finnmark Intervention Study Theory: community empowerment Aim: Change cardiovascular risk factors Community strategy development phase: Yes Description of costs and resources: none Components of the intervention as per the inclusion criteria: "Health and well being", Based on community empowerment. #1 Social marketing ‐ through mass media; #3 Individual counselling ‐ e.g. activity scripts; #4 Partnering ‐ working with organisations; #5 Specific settings ‐ various Emphasis of intervention: Not stated however there appears to be an emphasis working with community organisations Information given on intensity: none provided Assessment of intensity: High Start date: 1987 Duration: 3 years |
|
| Outcomes |
Outcomes and measures: 1. Physically active (%). Measures reported: unnamed questionnaire Time points: Baseline (1987) and follow up (1993) |
|
| Notes | Changes in blood pressure and BMI observed | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | High risk | Non‐randomised, groups comparable at baseline but communities chosen based on local initiative |
| Performance bias | High risk | The local newspaper was distributed to one of the control communities. The radio station also covered the control communities so some contamination of multimedia component of intervention likely |
| Attrition bias | Unclear risk | Attrition unclear, limited data on dropouts |
| Detection bias | Unclear risk | Unclear of whether physical activity measurement was validated Participants likely to be representative of the community. In 1987 survey all residents aged 40 to 62 years; and a 15% random sample of residents aged 20 to 39 years invited: 2435 total in the four communities; In 1993, 1957 residents still alive were re‐invited: follow up of 68%, 1324 total persons |
| Reporting bias | Low risk | No evidence of selective outcomes reporting or incompleteness of reporting |
| Other | Unclear risk | Head‐start: community instigated intervention. Unclear if study was adequately powered |
| Overall bias | High risk | High risk of bias. 2 high risk categories |
Mead 2013.
| Methods |
Study design: Controlled before and after study (independent samples), quasi‐experimental contemporaneous data collection, non‐randomised Sampling frame: all households using government housing maps Sampling method: Random sampling cohort. One Inuit or Inuvialuit adults (19 yrs. or older) per household was selected if he or she was a main food shopper or preparer in the household, was not pregnant or breastfeeding, had lived in the community for at least 6 months and intended to remain in the community for at least another year Collection method: questionnaire survey, short form IPAQ Ethics and informed consent: Ethical approval and licensed by the Aurora Research Institute in the NWT and the Nunavut Research Institute. All respondents signed written consent forms (in English or the local language) and were compensated with a gift card for CAD 25 to a local store |
|
| Participants |
Communities: Two remote communities in Nunavut received the intervention from October 2008 to November 2009, and one semi‐remote and one remote community in the North West Territories received it from May 2008 to August 2009. One remote community in each territory served as the comparison (“delayed intervention”). Geographical Canadian Artic and indigenous people: Inuvialuit and Inuit Country: Canada Ages included in the assessment: 19 years +. Mean age 42.4 years women (SD 13.1) and 42.3 men (SD 12.8) Reason provided for selection of the intervention community: Intervention based upon need and health inequality (increasing rates of obesity and physical inactivity, high chronic disease profile), but the reasons for allocating the intervention to specific communities not stated Intervention community: Participating communities not specifically named but ranged in size from 800 ‐ 3,500 residents. Comparison community: Reference communities (delayed intervention) not specifically named had populations of 400 and 1000 |
|
| Interventions |
Name of the intervention: Healthy Food Network Theory: Social cognitive theory and social ecological model Aim: Increase healthy eating knowledge, self‐efficacy, and intentions to engage in both healthy food‐related behaviours and physical activity through the media and participation in intervention activities Community strategy development phase: Yes, messages identified in community workshops Description of costs and resources: None provided Components of the intervention as per the inclusion criteria: #1 Social marketing mass media of radio and TV. #4 & #5 activities in recreational centres, health and wellness centres, worksites, schools. other venues. Walking clubs with pedometer challenges. Worked with local food stores, retailers and other partners to increase availability and accessibility of healthier food options and opportunities for engaging in PA. comprised of 7 phases Emphasis of intervention: “HFN’s primary aims were to improve dietary adequacy, increase physical activity and reduce risk of chronic disease among Inuit and Nunavut and Inuvialuit in the NWT.” Information given on intensity: no information Assessment of intensity: Medium Start date: Baseline data 4 months in 2008 Nunavut, 9 months 2007 to 2008 in Northwest Territory Duration: 12 months each community |
|
| Outcomes |
Outcomes and measures: Physical activity (IPAQ) measured pre‐post. No outcome data provided in the papers not upon request |
|
| Notes |
Study protocol (Sharma, 2010) describes using the following measurements: Quantitative Food Frequency Questionnaire, 24hr food recall, Adult Impact Questionnaire (socioeconomic and psychosocial factors), International Physical Activity Questionnaire Results paper (Mead, 2012) describes measuring: psychosocial constructs (healthy eating knowledge, self‐efficacy and behavioural intentions), frequency of healthy/unhealthy food acquisition, healthiness of commonly used food preparation methods and body mass index. Several papers of the study have been published by the author team. The results paper fails to describe PA measurements. However, correspondence with authors have confirmed that PA was measured pre and post intervention, but there are no currently existing publications reporting PA outcomes The published studies describe positive effects of the strategy for healthy eating, but are silent on the effects of physical activity |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | Not randomised. “Communities were assigned to the intervention or comparison arm based on a range of population sizes, percentages of the population who were Inuit or Inuvialuit, percentages of the population engaged in the wage economy and percentages of the population engaged in traditional hunting and fishing practices”. Communities did not differ in their baseline values of healthy eating knowledge and self‐efficacy, healthy and unhealthy food acquisition, and food preparation scores, though comparison respondents had greater intentions to engage in healthier food‐related behaviours than intervention respondents at baseline (mean score 22.02 versus 20.58, P = 0.0027) |
| Performance bias | Unclear risk | Good evidence of engagement with partners. No details of potential contamination as mass media was used, although the communities were remote. No evidence of blinding |
| Attrition bias | Low risk | Minimal attrition: 91.5% of the 494 baseline respondents participated in the follow up (same sample follow up) |
| Detection bias | Unclear risk | For culturally appropriateness, the IPAQ was modified to include relevant examples such as hunting and fishing. May not be representative of the broader community, and may in fact be more active |
| Reporting bias | High risk | High risk of bias. Increasing physical activity was identified clearly as an intention of the study. Confirmed by the authors pre and post, but absence in Table 1 |
| Other | Unclear risk | Sample size was calculated using a two‐sided paired t test, a significance level of 5%, and a power of 80%, which showed that a sample size of 50 per community was required. Post‐intervention data collection occurred from October to December 2009, starting 1 month after intervention completion. Unclear if PA included in the sample size |
| Overall bias | High risk | Outcome data are unavailable for this unique study in Canada's Arctic |
Nafziger 2001.
| Methods |
Study design: Controlled before and after study (cohort follow up and independent samples) Sampling frame: All inhabitants Sampling method: 3 stage cluster sample Collection method: telephone and clinic surveys Ethics and informed consent: yes |
|
| Participants |
Communities: Counties, Northern New York State Country: United States Ages included in the assessment: 20 to 69 years Reason provided for selection of the intervention community: unclear Intervention community: Otesgo and Scholarie counties Comparison community: Herkimer county |
|
| Interventions |
Name of the intervention: Ostego‐Schoharie Healthy Heart Program Theory: none stated Aim: Provide health education to isolated villages and populations. to increase physical activity, decrease smoking and improve nutrition and identify hypercholestaeremia and hypertension Community strategy development phase: Yes Description of costs and resources: 6 staff Components of the intervention as per the inclusion criteria: #1 Social marketing ‐ through mass media; #2 Other communication; #4 Partnering ‐ working with organisations; #5 Specific settings Emphasis of intervention: Health education with a strong mass media emphasis Information given on intensity: "small staff", extensive volunteers" Assessment of intensity: High Start date: 1989 Duration: 5 years |
|
| Outcomes |
Outcomes and measures: 1. Sedentary % (self report). Measurement tool: CDC Behavioural Risk factor Survey Time points: Baseline (1989) and follow up (1995) |
|
| Notes | Smoking decreased in the intervention group | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | Non‐randomised, but no significant difference between reference and intervention counties. The reason for allocation is unclear. Nothing to indicate the communities couldn't be reversed |
| Performance bias | Low risk | Comparison community is geographically and culturally isolated with different sources of newspaper, radio and television information. Little risk of contamination. No evidence of any issues with integrity of the intervention |
| Attrition bias | Low risk | Attrition in cohort 16.2%, acceptable |
| Detection bias | Unclear risk | Measurement tools were likely to be applied as intended. Questionnaire not validated (single question). Sedentary activity was measured over 1 week. Representativeness: Baseline response rate = 61.8%, 5‐year panel = 83.8%, 5‐year cross‐sectional = 45% |
| Reporting bias | Unclear risk | No evidence of selective outcome reporting or incompleteness of reporting |
| Other | Low risk | None |
| Overall bias | Unclear risk | Unclear risk of bias. 3 unclear categories |
Nguyen 2012.
| Methods |
Study design: Controlled, non‐randomised, before and after study (cohort follow up), quasi‐experimental Sampling frame: A list of persons resident in the commune Sampling method: randomised cross‐sectional surveys of year cohort Collection method: two random cross‐sectional sample surveys of the general population at baseline and 3 years. Method of application not specified Ethics and informed consent: Ethical approval obtained. “All human subjects in the of study were asked for their written consent before the collection of the data, and after full explanation of the goals and protocols of the study” |
|
| Participants |
Communities: Two "typical" rural communes of Ba‐Vi district, 60 km to the west of Hanoi. (average populations 5000 to 10,000) Country: Vietnam Ages included in the assessment: adults (25+ years) inhabiting in the intervention and reference communes – included healthy adults and hypertensive adults Reason provided for selection of the intervention community: Reason not provided, “the choice of reference and intervention communes was made before any screening surveys or preparation activities were undertaken” Intervention community: Phu‐Cuong commune (size not specified) Comparison community: Phu‐Phuong commune |
|
| Interventions |
Name of the intervention: generically stated as "healthy lifestyle promotion" Theory: The community‐based model (health education) Aim: hypertension and behavioural cardiovascular risk factors in a rural Vietnamese population Community strategy development phase: Yes, includes implementation phase. A cross‐sectional survey on 1180 randomly selected adults at Phu‐Cuong, which found 469 (39.8%) people with hypertension. Among hypertensive persons, 37.3% previously knew about their BP, 68.7% did not have any treatment and 0.6% had well‐controlled BP Description of costs and resources: none stated Components of the intervention as per the inclusion criteria: #1 broadcasting of healthy lifestyle promotion campaigns, #2 leaflets, #3 monthly check‐ups for persons with hypertension, #5 working with local teams trained and supervised my ministry of health doctors. No environmental components Emphasis of intervention: Multiple strategies CVD risk factors includes physical activity Information given on intensity: authors suggest, in view of their negative findings a need for higher intensity health education interventions Assessment of intensity: Medium Start date: December 2006 Duration: 3 years |
|
| Outcomes |
Outcomes and measures: 1.Physical inactivity presented as a proportion of the population, defined at less than 3000 MET minutes per week Measures other CVD risk factors of smoking status, salt intake. Blood pressure Time points: Baseline (2006) and follow up (2009) |
|
| Notes | The authors noted physical activity and obesity increased over time in the intervention commune, there was a significant reduction in systolic and diastolic BP (3.3 and 4.7 mmHg in women, versus 3.0 and 4.6 in men). Impact upon salty diets, not no impact on daily smoking or heavy alcohol consumption | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | High risk | Not randomised, before and after with reference. No formal justification for approach, other than the decision to allocate the commune to the intervention was undertaken prior to screening. Some baseline differences between the 2 groups were observed Education, occupation (reference lower); salty diet, diastolic BP. Awareness among hypertensive persons, presence of hypertension (34% among reference 46.7% among intervention); Physical inactivity slightly higher among the reference community |
| Performance bias | Unclear risk | No evidence the communities were blinded. Potential for contamination not identified, both communities in low lands and unclear if broadcasts reached the reference population |
| Attrition bias | Low risk | Both communities remained in the study. A total of 1131 and 1189 adults from Phu‐Phuong commune and 1176 and 1192 people from Phu‐Cuong commune participated in the baseline and evaluation surveys respectively, amounting to an overall response rate of 97.7% |
| Detection bias | Unclear risk | Participants surveyed 1200 adults (> 25 years old), representative, randomly selected from the whole list of local inhabitants in both communes with randomly invited. 97.7% response rate. Energy requirement in metabolic equivalents (METs) for each individual was estimated based on details of duration and type of all self‐reported physical activities in a typical week, following the WHO’s STEP approach. Method of application not described |
| Reporting bias | Low risk | No evidence of selective reporting |
| Other | Unclear risk | No sample size provided |
| Overall bias | High risk | |
Nishtar 2007.
| Methods |
Study design: Controlled before and after study (independent samples) Sampling frame: Entire populations of the districts Sampling method: Multi‐stage clustering sampling Collection method: Survey Ethics and informed consent: Ethics unknown. Informed consent obtained from the respondent before each interview |
|
| Participants |
Communities: Districts Country: Pakistan Ages included in the assessment: 18 to 65 years Reason provided for selection of the intervention community: None stated Intervention community: Lodhran (population 1.17 million) Comparison community: Rahin Yar Khan (population similar to Lodhran) |
|
| Interventions |
Name of the intervention: The Heartfile Lodhran CVD prevention project Theory: None stated Aim: Cardiovascular disease preventions Community strategy development phase: No Implementation phase: Unclear Description of costs and resources: none provided Components of the intervention as per the inclusion criteria: #1 Social marketing ‐ mass media Message of CVD prevention ‐ risk factors; #3 Individual counselling ‐ training of health professionals; #4 Partnering ‐ community health education Emphasis of intervention: unclear ‐ health knowledge Information given on intensity: none provided Assessment of intensity: Low Start date: 2000 Duration: 3 years |
|
| Outcomes |
Outcomes and measures: 1. Physical activity work domain (3 categories). Measurement tool: Global Physical Activity Questionnaire instrument 2. Physical activity during transportation. Measurement tool: Global Physical Activity Questionnaire instrument 3. Physical activity during recreation/leisure. Measurement tool: Global Physical Activity Questionnaire instrument 4. Opinion about regular physical activity. Measurement tool: BRFSS questionnaire and Heartfile methodology Time points: Baseline (2000) and follow up (2003) |
|
| Notes | Some improvement observed for consumption of vegetables only | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | Non‐randomised. No details of allocation. Unclear whether comparable at baseline as Control group had a greater number of those with the lowest monthly income. Difficult to tell whether outcomes would be the same if the Intervention and Control communities were reversed |
| Performance bias | Low risk | Blinding of participants unknown. No evidence of contamination, comparator 160 km away. Adequate description of delivery implementation |
| Attrition bias | Low risk | No evidence of incomplete data adequately addressed, cross‐sectional independent samples |
| Detection bias | Low risk | Questionnaire used GPAQ STEPS module to measure physical activity. Measurement tools applied as intended. Blinding status of outcome assessors unknown. Validated measure used. Adequate representativeness of samples of the communities through multistage cluster sampling. First stage random sampling. Second stage "systematic sampling" to select households. Response rate to the baseline survey was 100% in the control, and similar in the intervention group |
| Reporting bias | Low risk | Report seems free of selective outcome reporting and match the aims of the intervention. No evidence of incomplete reporting |
| Other | Unclear risk | Statistical methods acceptable. Nothing apparently distinctive of the intervention community to explain outcome |
| Overall bias | Unclear risk | Unclear risk of bias attributed to uncertainty of selection bias |
NSW Health 2002.
| Methods |
Study design: Controlled before and after study (independent) Sampling frame: Electronic telephone registry (white pages) Sampling method: Random selection Collection method: Computer assisted telephone interview Ethics and informed consent: Not stated |
|
| Participants |
Communities: Urban Suburbs (wards) Country: Australia Ages included in the assessment: 25 to 65 years Reason provided for selection of the intervention community: unclear Intervention community: Lachlan Macquarie ward Comparison community: Caroline Chisholm ward |
|
| Interventions |
Name of the intervention: Walk It: Active Parks Theory: not stated Aim: To increase physical activity in moderate physical activity in adults aged 25 to 65 years Community strategy development phase: No Description of costs and resources: Components of the intervention as per the inclusion criteria: #1 Social marketing ‐ through mass media; #2 Other communication strategies ‐ various; #4 Partnering ‐ working with voluntary groups; #6 Environmental changes ‐ working with the council for local park improvement Emphasis of intervention: Environmental interventions Information given on intensity: No details Assessment of intensity: Low Start date: 1997 Duration: 1 year |
|
| Outcomes |
Measures: 1. Walking (any, for exercise or recreation, other reasons) (%). Measurement tool: Questionnaire 2. Vigorous exercise (%). Measurement tool: Questionnaire 3. Light to moderate physical activity (%). Measurement tool: Questionnaire 4. Adequate activity (%). Measurement tool: Questionnaire 5. Awareness. Measurement tool: Questionnaire Time points: Baseline and follow up (12months) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | No details of allocation sequence. Not randomised. No details of allocation concealment. The publications fails to provide the details of the demographics of the populations to make comparisons "Caroline Chisholm ward selected as the control as it matched closely to the intervention." Can't tell what the effects would be if the control and intervention communities were reversed |
| Performance bias | High risk | No details of blinding. Some efforts to protect against contamination. "Two other wards separated the study wards, creating a spatial barrier". The control ward was exposed to some of the promotion campaign, and park modifications were not completed as planned. One control park received a major improvement during the program, low response rate to the survey ‐ no definite conclusions can be drawn. The intervention lacks integrity. “Due to problems in the implementation of the study interventions it was not possible to evaluate their effectiveness in increasing participation in physical activity (objective 1).” |
| Attrition bias | Unclear risk | Uncertain whether incomplete data was adequately addressed. State independent samples, but unclear whether cross‐sectional, some of the questions incomplete |
| Detection bias | High risk | Measures were used in their entirety. Unclear whether outcome assessment was blind. Unclear of the validity of the outcome metrics. No description of validated survey, just used previous survey questions. Period of outcome measurement adequate comprising of participation in physical activity in the past 2 weeks: (1) Walking for exercise / recreation, (2) Walking for other reasons, (3) vigorous exercise, (4) light to moderate physical activity. Results not representative: No: response rate is 20%. Significant risk of bias |
| Reporting bias | Low risk | Reports are free from selective reporting (survey was attached to the published report). The reporting does not seem complete, outcome measures do not report on the message of 30 minutes of walking most days |
| Other | Low risk | None. Sample size calculation undertaken |
| Overall bias | High risk | High risk of bias. 2 high risk of bias categories |
O'Loughlin 1999.
| Methods |
Study design: Controlled before and after study (cohort follow up and independent samples) Sampling frame: Electronic telephone registry Sampling method: Random sample, or neighbourhood cluster design random selection Collection method: Telephone survey Ethics and informed consent: None stated |
|
| Participants |
Communities: Inner‐city neighbourhoods of Montreal Country: Canada Ages included in the assessment: 18 to 65 years Reason provided for selection of the intervention community: Disadvantaged, but unclear Intervention community: Neighbourhood of St Henri (population 25,000) Comparison community: Neighbourhood of Centre‐Sud |
|
| Interventions |
Name of the intervention: Coeur en Santé St‐Henri Theory: Bandura social learning theory and behavioural change theory of self‐efficacy Aim: Heart disease prevention, risk factors including physical activity Community strategy development phase: Yes Description of costs and resources: 5 year budget of CAD 775,000 Components of the intervention as per the inclusion criteria: #1 Social marketing ‐ minimal, through mass media (Column in local press); #2 Other communication strategies ‐ direct mailing of print education 12,789 household directly mailed, Video cassette; #3 Individual counselling ‐ screening for CV risk factors and advice through heart health fairs; #4 Partnering ‐ walking clubs; #6 Environmental changes ‐ minimal environmental changes applicable to physical activity Emphasis of intervention: not identified Information given on intensity: "did not have a large budget" Assessment of intensity: Medium Start date: 1992 Duration: 5 years |
|
| Outcomes |
Outcomes and measures: 1. Leisure time physical activity infrequency (%). Measurement tools: Canadian heart health survey 2. Self‐rated physical activity (%). Measurement tools: Canadian heart health survey Time points: Baseline (1992) and follow up (1997) |
|
| Notes | No changes observed in health behaviours or health status measures | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | Non‐randomised before and after (independent 3‐year, and cohort 5‐year). Allocation not described. Some differences in characteristics of population but unclear of impact. Aimed at adults. Nothing to suggest reversal of control and interventions communities to have an impact upon outcomes both disadvantaged communities in Montreal |
| Performance bias | Low risk | Blinding of participants unknown. Measures taken to avoid contamination as non adjoining. Minimal contamination evident and intervention only delivered to the one community. 13.1% of control community had heard of program, but only 0.9% had participated in 1 or more of its activities. Nothing to suggest the intervention wasn't delivered as planned |
| Attrition bias | High risk | Attrition for the cohort study was 50% |
| Detection bias | Unclear risk | Measures appeared to be applied as intended. No evidence of blinding. The validity and reliability of the instruments unclear. Representativeness possible as random sampling from telephone directory, however there is concern because the intervention and control communities are disadvantaged with 85% to 90% of coverage and 10% to 15% of persons with confidential telephone numbers. 79.3% and 77.8% completed the interview |
| Reporting bias | Low risk | No suggestion of selective outcome reported. The measures reported appear the same as the aims of the intervention although details are limited |
| Other | Low risk | No issues of statistical quality. No details of a sample size calculation undertaken |
| Overall bias | High risk | High risk of bias. 1 significant high risk category |
Osler 1993.
| Methods |
Study design: Controlled before and after study (independent samples) Sampling frame: Central persons registry Sampling method: Random sample Collection method: Postal survey Ethics and informed consent: Unclear |
|
| Participants |
Communities: Rural municipalities Country: Denmark Ages included in the assessment: 20 to 65 years Reason provided for selection of the intervention community: Unclear Intervention community: Slangerup (population 8000) Comparison community: Helsinge (population comparable) |
|
| Interventions |
Name of the intervention: Slangerup ‐ a heart‐healthy town Theory: Social learning theory; Persuasion model Aim: Prevention of cardiovascular disease Community strategy development phase: Unclear Description of costs and resources: USD 50,000 (USD 6 per person) Components of the intervention as per the inclusion criteria: #1 Social marketing ‐ mass media; #3 Individual counselling; #4 Partnering ‐ working with voluntary organisations (community organisation) with education. General statement of the intervention: "the project almost ended up being a pure mass‐media campaign, which experience shows may increase awareness, but as experience shows has little effect on adaption of new behaviour" Emphasis of intervention: Intention for the emphasis to be mass media, as well as involvement of the local population, however it ended up being purely mass media Information given on intensity: "Low cost" Assessment of intensity: Low Start date: 1989 Duration: 1 year |
|
| Outcomes |
Outcomes and measures: 1. Physically inactive (%). Measurement tool: unnamed questionnaire 2. Stages of change ‐ considered doing more exercise. Measurement tool: unnamed questionnaire Time points: Baseline (October 1989) and follow up (October 1990) |
|
| Notes | No changes in smoking and fat consumption measures | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | Not randomisation, but reported characteristics similar |
| Performance bias | High risk | Lack of blinding, absence of detail to protect contamination |
| Attrition bias | Unclear risk | Independent samples, but response rates vary by ages |
| Detection bias | High risk | No details of the measurement tool, very low response rate |
| Reporting bias | Low risk | Limited description |
| Other | Unclear risk | No details of sample size calculation undertaken |
| Overall bias | High risk | High risk of bias. 2 high risk categories |
Phillips 2014.
| Methods |
Study design: Cluster randomised controlled trial Sampling frame: Post office address File Sampling method: Randomly selected 16 years and older Collection method: Paper questionnaires were used at baseline and computer assisted personal interviewing at follow up Ethics and informed consent: Ethics approved. Informed consent described in Wall 2009 |
|
| Participants |
Communities: 20 matched pairs of neighbourhoods in London were randomised to intervention/ control condition Country: England Ages included in the assessment: Adults, aged 16 + Reason provided for selection of the intervention community: 1. All 4765 LSOAs in London were ranked by the English Indices of Multiple Deprivation (IMD) 2004 2. The 20 London boroughs containing the most deprived 11% of LSOAs were identified; 3. Within each of these 20 boroughs, the four most deprived LSOAs (based on the IMD) were identified 4. Local authorities and health professionals were asked to select two LSOAs, which were not geographically contiguous, from the four identified in their borough; 5. Random allocation was used to assign one of the LSOAs to the intervention and the other became the control site Intervention community: 10 London boroughs as described above Comparison community: 10 London boroughs as described above |
|
| Interventions |
Name of the intervention: Well London Theory: Theory of change model Aim: 1) Increase levels of physical activity by focusing on the most sedentary individuals, promoting incorporation of physical activity into daily routines and improving the ability of communities to organize and run activities that provide opportunities to take part in physical activity; 2)· Improve mental well being by increasing user‐involvement in the design and running of projects, developing preventative approaches for common mental health problems, tackle stigma to change community perspectives of mental health and positively promote mental health; and 3) Increase levels of healthy eating by increasing access to healthy foods and increasing knowledge of healthy foods and improving food skills Community strategy development phase: Yes, The Well London Alliance Description of costs and resources: Components of the intervention as per the inclusion criteria: #2. Project “Active Living Maps”: maps of facilities and opportunities for healthy activities/lifestyle made for each LSOA and delivered in paper format to all residents. #4 ProjectActivate London ‐ work with Central YMCA ( leading UK health charity) to provide a range of activities for young people and adults to engage in physical activity, and #6. Project ‐ “Healthy Spaces”: improve physical environments through development of community gardens and allotments and re‐development of green‐spaces and greenery Emphasis of intervention: wellbeing, physical activity and healthy eating Specific emphasis of approach not stated. Base estimated risk for healthy physical activity 18% Information given on intensity: none provided. No description of cost as it relied on local investment Assessment of intensity: Medium Start date: October 2007 Duration: 3 years and 5 months |
|
| Outcomes |
Measures: Primary 1. Taking 5 x 30 min moderate‐intensity physical activity per week Secondary 2. Meeting 7 x 60 moderate‐intensity physical activity per week 3· Doing 150 minutes of moderate‐intensity physical activity per week 4· Mean MET minutes per week 5· Mental wellbeing (based on GHQ 12 score) 6· Healthy eating – meeting five a day (fruit and vegetable portions) 7· Unhealthy eating (number of portions of fruit and vegetables per day 8· Mental wellbeing (based on GHQ 12 score) Time points: Baseline and follow up |
|
| Notes | The study authors highlight the inherent tensions in the use of cluster‐randomised trials to measure the effects of ‘community’‐level interventions since clusters are geographically defined, whereas natural communities may not be. Greater investment in refining such programmes before implementation and trialling will be desirable in the future. Authors suggest there is a need to develop new methods to understand, longitudinally different pathways residents take through such interventions and their outcomes, and new theories of change that apply to each pathway | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | Random allocation was used to assign one of the LSOAs to the intervention and the other became the control site. Method not stated to determine randomisation or by whom it was performed. Intervention and control groups comparable at baseline |
| Performance bias | Low risk | No statement on blinding of the communities The authors addressed “Resident turnover and contamination”, the control communities are in a different area of London. Participants could have used services outside their area |
| Attrition bias | Low risk | Data appear complet |
| Detection bias | Unclear risk | Households were randomly selected in each intervention and control neighbourhood, using the Post Office Address File as a sampling frame. Quota sample approach used to get random sample at household level sample. Used IPAQ, however, paper questionnaires were used at baseline and computer assisted personal interviewing at follow up |
| Reporting bias | Low risk | The reports of the study appear to be free of selective outcome reporting as all the results shown are negative findings. The reporting is complete as the reporting is consistent with the study failing to detect any change in physical activity but had a very unusual high baseline per cent meeting recommendations |
| Other | Low risk | Statistical methods appropriate: Effect‐estimates were calculated by comparing intervention and control neighbourhoods at follow‐up. Crude and adjusted effect‐estimates were calculated for all health and social outcomes. Means and proportions for the outcomes and socio‐demographic characteristics are presented. The paired t test was used to test for differences between control and intervention neighbourhoods (mean differences for continuous and log (risk ratios) for binary outcomes) and corresponding. 95% CIs were calculated using the t distribution. Sample size calculation |
| Overall bias | Low risk | Only minor methodological deviations observed which were considered insufficient to downgrade from low risk of bais this well designed study |
Reger‐Nash 2005.
| Methods |
Study design: Controlled before and after study (cohort follow up) Sampling frame: electronic telephone registry Sampling method: Random digit dialling Collection method: Telephone survey Ethics and informed consent: Ethics approval, but unclear if consent obtained |
|
| Participants |
Communities: Cities in West Virginia Country: United States Ages included in the assessment: 50 to 65 years Reason provided for selection of the intervention community: proximity to the university Intervention community: Wheeling, West Virginia (population 31,240) Comparison community: Parkersburg, West Virginia |
|
| Interventions |
Name of the intervention: Wheeling walks Theory: Theory of Planned Behaviour and Transtheoretical model Aim: Increase physical activity Community strategy development phase: Yes Description of costs and resources: 12 weeks of participatory planning. Purchase of 5,104 television gross points and 3,461 radio gross rating points, local TV adds, 14 quarter newspaper adds media relations with 170 stories. Plus booster of 521 TV points, 370 radio points, 2 quarter page newspaper. Details of staffing not provided. Paid advertising about USD 300,000. Components of the intervention as per the inclusion criteria: #1 Social marketing ‐paid mass media; #2 Other communication strategies ‐ public relations activities, campaign website, #3 Individual counselling ‐ physicians "prescriptions for walking"; #4 Partnering ‐ working with organisations; #5 Specific settings ‐ work places Emphasis of intervention: Mass media intensive ("a community campaign using paid media to encourage walking among sedentary older adults") Information given on intensity: none provided Assessment of intensity: Low Start date: April 2002 Duration: 12 months |
|
| Outcomes |
Measures: 1. Sufficiently active (moderate or vigorous). Measurement tool: BRFSS questions 2. Sufficiently active walker (%). Measurement tool: BRFSS questions 3. Change in minutes. Measurement tool: BRFSS questions 4, Change in walking per day. Measurement tool: BRFSS questions 5. Change in walking minutes per week. Measurement tool: BRFSS questions 6. Change in minutes of mod to vigorous physical activity per week. Measurement tool: BRFSS questions Time points: Baseline and follow up (3 months; 6 months; 12 months) |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | High risk | Not randomised. Intervention community chosen based on proximity to university. Baseline characteristics of intervention and control group mostly comparable however full time employed much higher in wheeling. Wheeling is a university town so may be an effect modifier |
| Performance bias | Low risk | No evidence of blinding; No evidence of contamination. Mass media of control community unknown. Appears to have adequate distance between the town. No issues identified in the integrity of the intervention |
| Attrition bias | Unclear risk | Attrition rate > 30% for Waves 3 and 4 |
| Detection bias | High risk | Unclear whether the measurement tools applied as intended and in their entirety. Unclear whether assessment blinded. Quality of physical activity > 1 day. Sample only included 50 to 65 year olds randomly recruited; response rate not given |
| Reporting bias | Low risk | No evidence of selective outcome reporting |
| Other | Unclear risk | Sample size calculation was undertaken |
| Overall bias | High risk | High risk of bias. 2 high risk categories |
Rissel 2010.
| Methods |
Study design: Controlled before and after study (follow‐up), non‐randomised allocation Sampling frame: Post‐codes within 2 km of bike paths followed by Electronic White Page Directory (EWPD) of these postal codes Sampling method: three‐stage clustering, random sample. 1450 interviews at baseline with follow up Collection method: Telephone interviews of those who spoke English Ethics and informed consent: Ethical approval not stated. Informed written consent obtained for interview |
|
| Participants |
Communities: Cities Country: Australia Ages included in the assessment: 18 years and older Reason provided for selection of the intervention community: None stated, selected as having bicycle initiative and low SES. Intervention community: Liverpool (population approximately 180,000 ) and Fairfield (population approximately 200,000) NSW Comparison community: Bankstown (population approximately 195,000) |
|
| Interventions |
Name of the intervention: Cycling Connecting Communities Theory: Social marketing and behaviour change theories including trans‐theoretical model and stages of change Aim: increase cycling on newly completed off‐road cycle paths Community strategy development phase: Unclear Description of costs and resources: Yes, $300,00 AUS for 3 years including evaluation 1/3 of budget $0.35 per person per year. Described as "low budget" Components of the intervention as per the inclusion criteria: #2 other communication such as booklets and maps, #4 working with organisation such as work day event, community rides, free cycling skills course #5 Specific setting such as 1 hour presentation in community and workplaces. Also included other approaches such as water bottles and slap bands Emphasis of intervention: social marketing of cycling Information given on intensity: "low budget" Assessment of intensity: Low Start date: May to June 2007 Duration: 2 years |
|
| Outcomes |
Measures: 1. Physical activity (PA) behaviour‐ Sufficiently active: sufficient to confer health benefit if total time is greater or at least 150 minutes (using the Active Australia questionnaire) 2. Frequency of cycling 2. Total time cycling per week: estimated time spent on cycling in the past week Other measures Bike count monitoring (separate study) of trail use Time points: Baseline, and follow up (2 years) |
|
| Notes | The study used 2 data sources. telephone surveys and observations of usage. The project appears to have increased awareness of the project, increased use of bicycle paths, increased cycling among novice or beginner riders, and increased the mean number of minutes cycled in the past week among participants riding at both baseline and follow‐ up. However, there was no overall increase in the population frequency of cycling, or overall increase in physical activity levels. Increased use of paths and among riders did not translate to population increases in physical activity levels | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | No random allocation. No description of reasons for allocation. There however appears to be good comparability at baseline |
| Performance bias | Unclear risk | Authors appear to state they were without sufficient resources. Authors raise concerns about the value of limited local social marketing, however the intervention appears to be carried out as planned. No details of approaches to prevent contamination. Recall awareness of the CCC project (73.7%) compared with the comparison area (23.5%) (P = 0.004) |
| Attrition bias | Low risk | No attrition, 90% follow‐up rate |
| Detection bias | Low risk | Random cross‐sectional sampling of the community in the first survey and voluntary participation in the follow‐up interview. A total of 1450 interviews were completed, with a response rate of 64.7% the authors considered response rate "excellent" and a strength of the study.No details of blinding of outcome assessors. |
| Reporting bias | Low risk | Other outcomes of Active Australia such as minutes are not reported. Negative findings provided, however outcomes could be worse than described |
| Other | Low risk | Appropriate methodology employed |
| Overall bias | Unclear risk | Re‐analysis of data shows a statistical decrease in physical activity in the intervention group |
Sarrafzadegan 2009.
| Methods |
Study design: Controlled before and after study (independent samples) Sampling frame: whole population Sampling method: multi‐stage clustering Collection method: not stated Ethics and informed consent: Ethical approval obtained. Informed written consent provided by each participant in the assessment |
|
| Participants |
Communities: Cities (2 cities) Country: Republic of Iran Ages included in the assessment: Stated as "adults" Reason provided for selection of the intervention community: None stated Intervention community: Isfahan (population 1,895,856) and Najaf‐Abad (275,084) Comparison community: Arak (population 668,531) |
|
| Interventions |
Name of the intervention: Isfahan Healthy Heart Program Theory: not stated Aim: Cardiovascular disease prevention and control of non‐communicable disease Community strategy development phase: Yes Description of costs and resources: Insufficient details Components of the intervention as per the inclusion criteria: #1 Social marketing ‐ "public education throughout the mass media; #3 Individual counselling; #4 Partnering ‐ working with special organisations Emphasis of intervention: community engagement Information given on intensity: "comprehensive, integrated" Assessment of intensity: Medium Start date: 2000 Duration: 4 years |
|
| Outcomes |
Measures: 1. Individuals with greater than or equal to 30 minutes per day of moderate or vigorous activity (%). Measurement tool: STEPwise approach to chronic disease risk factor surveillance (STEPS) 2. Leisure time physical activity (MET‐m/week). Measurement tool: STEPwise approach to chronic disease risk factor surveillance (STEPS) 3. Total daily physical activity (MET‐m.week). Measurement tool: STEPwise approach to chronic disease risk factor surveillance (STEPS) Time points: Baseline and follow up (1 year, 2 year, 3 year, 4 year) |
|
| Notes | Improvements in the outcomes of smoking and diet | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | Quasi experimental controlled before and after study not randomised. The 2 intervention communities resembled the control community in its socioeconomic, demographic and health profile except control group had a much higher percentage of rural living people. Nothing to suggest the outcomes would be different if the communities were reversed |
| Performance bias | Low risk | Comparison community did not receive intervention ‐ unlikely risk of contamination |
| Attrition bias | Low risk | Status of incomplete data unknown. Attrition not applicable as sampling independent samples |
| Detection bias | Low risk | Physical activity measured using validated Baecke questionnaire of regular physical activity. Assumed to use questionnaire in the entirety. Time period not specified. Sampling likely to be representative. A random sample of adults selected yearly by multi‐stage cluster sampling. Response rate very high (98% to 100%) |
| Reporting bias | Low risk | No evidence of selective reporting bias or incompleteness of reporting |
| Other | Unclear risk | None. Sample size calculation undertaken, but no details provided |
| Overall bias | Unclear risk | Unclear risk of bias. No high risk category, 2 unclear categories |
Simon 2008.
| Methods |
Study design: Cluster randomised controlled trial Sampling frame: 12 year adolescents (first level in public middle schools) Sampling method: All of the sampling frame were included Collection method: Survey Ethics and informed consent: Ethical approval obtained and informed consent obtained at 3 levels |
|
| Participants |
Communities: Schools in four school catchment defined communities in Bas‐Rhin of Eastern France Country: France Ages included in the assessment: 11/12 year olds (at baseline) Reason provided for selection of the intervention community: not applicable ‐ random assignment Intervention community: Public middle schools Comparison community: Public middle schools |
|
| Interventions |
Name of the intervention: Intervention centred on adolescents' physical activity and sedentary behaviour Theory: ecological models Aim: Prevention of overweight through physical activity Community strategy development phase: No Description of costs and resources: Costs concerned mainly the coordination of the different partners by the ICAPS team and the supervision of the activities provided Components of the intervention as per the inclusion criteria: #4 Partnering ‐ home, community/neighbourhood/recreation fitness / sports facilities; #5 Specific settings ‐ schools; #6 Environmental changes ‐ various. Emphasis of intervention: Working in schools setting (with reach to homes) with some environmental strategies Information given on intensity: not stated Assessment of intensity: Low Start date: 2002 Duration: 4 years |
|
| Outcomes |
Measures: 1. Supervised leisure physical activity (hrs/wk). Measurement tool: modifiable activity questionnaire for adolescents 2. Active commuting between home and school (minutes/day). Measurement tool: modifiable activity questionnaire for adolescents 3. Intention towards physical activity score. Measurement tool: modifiable activity questionnaire for adolescents Time points: Baseline, and follow up (1‐year, 2‐year, 3‐year, 4‐year) |
|
| Notes | Improvement in BMI only for those children initially non‐overweight | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | Cluster randomisation, method of randomisation is not described |
| Performance bias | High risk | Implementation. The intervention delivered primarily from middle schools with to those in the first year. Schools are public, unknown what percentage of the community children are in private schools |
| Attrition bias | Low risk | No evidence of attrition bias |
| Detection bias | High risk | The sampling uses the children in sixth grade of public schools exclusively for the outcomes. The outcomes of other children and residents in the community are unknown |
| Reporting bias | Low risk | No evidence of reporting bias |
| Other | Unclear risk | Missing some relevant detail |
| Overall bias | High risk | High risk. 2 high risk categories |
Solomon 2014.
| Methods |
Study design: Stepped wedge cluster randomised trial (with control comparison) Sampling frame: Addresses of all households purchased from a private company Sampling method: Stratified random sample of adult, resident Collection method: Postal questionnaire, prepaid envelope Ethics and informed consent: ethics committee, implied consent when participants returned a completed questionnaire |
|
| Participants |
Communities: Rural village, 128 villages, population ranging 500 to 2,000 in seven rural regions of Devon Country: England Ages included in the assessment: 18 years and older, included up to 102 years Reason provided for selection of the intervention community: Rural communities required enhancement of sporting opportunities for physical activity. "large enough to have local facilities suitable for physical activity, but limited in the amount of activity opportunities they could offer". Allocated through randomisation to intervention or waiting Intervention community: Villages in Devon where not previously involved in the program, however these were later crossed over to the intervention Comparison community: Waiting for intervention in step for the intervention |
|
| Interventions |
Name of the intervention: Active VIllages Devon Theory: None stated but appears to be based upon creating more ‘activity‐friendly’ environments holds promise for improving population‐wide physical activity (King and Sallis); whole of community intervention Partnership, Focus on sport Aim: disease burden associated with physical inactivity as a public health imperative. Increasing physical activity Community strategy development phase: Yes, 12 weeks prior to implementation Description of costs and resources: Total program costs of the program with evaluation was GBP 1 million with very low reach Components of the intervention as per the inclusion criteria: #1 mass media via newspapers, #2 other communication strategies of websites, posters, leaflets, village newsletters. #4 working with local district authority sports development team, charitable organisations, physical activity sessions, with each village receiving at least three different types of activities. Supported by coaches. #5 settings of after school club aimed at primary school children, #6 environmental components including purchase of equipment and support facilities Emphasis of intervention: none stated, but appears to be activity‐friendly environments through community engagement. "many of the intervention activities were targeted at a specific group within the community (i.e. basketball for primary school children, or armchair aerobics for older adults) Information given on intensity: The authors indicate that the intervention failed to achieve penetration. 1 million Pounds was spent on the intervention. Authors describe the intervention as "low reach". Evaluation highlighted very few residents were even aware of and participated in the intervention although GBP one million was spent Assessment of intensity: Low Start date: April 2011 Duration: 12 weeks intervention plus 12 months supported follow up |
|
| Outcomes | Physical activity was measured using the self‐administered, short version of the International Physical Activity Questionnaire (IPAQ‐SV) 1. Categorised according to whether they did sufficient physical activity to meet the current United Kingdom physical activity guidelines (at least 150 minutes of moderate‐intensity activity per week in bouts of 10 minutes or more, or at least 75 minutes of vigorous intensity activity per week 2. Physical activity level was also analysed using metabolic equivalent (MET) values to calculate participants’ total MET‐minutes per week of moderate intensity walking, moderate intensity physical activity, and vigorous intensity physical activity, using the IPAQ‐SV scoring methods for calculating physical activity levels |
|
| Notes | Showed no evidence that the intervention increased the prevalence of physical activity within the villages, and only weak evidence of an increase in physical activity level. The intervention did lead to an increase in physical activity habits. The evaluation highlighted that very few residents were even aware of and participated in the intervention | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Low risk | Characteristics were similar between the intervention and 309 control mode participants, with comparable responses being reported for gender, age, 310 education leaving age, and car ownership |
| Performance bias | Unclear risk | Unclear whether contamination occurred. However there appeared to be generally low penetration into the community so any contamination is likely to be minimal |
| Attrition bias | Low risk | Independent samples |
| Detection bias | Low risk | Physical activity was measured using the validated self‐administered, short version of the International Physical Activity Questionnaire (IPAQ‐SV) Response rate 37.7% in initial survey and lower in the follow‐up“. This raises concerns that those who consented may not represent the wider population (non‐response bias)” |
| Reporting bias | Low risk | Verified outcomes against published protocol and details in the thesis |
| Other | Low risk | Statistical methods appropriate. Power calculation |
| Overall bias | Low risk | Only concerns pertain to possible contamination and possibility of non‐response bias |
Wendel‐Vos 2009.
| Methods |
Study design: Controlled before and after study (independent samples and cohort follow up) Sampling frame: Population registries Sampling method: Stratified random sample Collection method: Questionnaire and physical examination Ethics and informed consent: Dutch medical ethics committee TNO provided approval. All participant gave informed consent |
|
| Participants |
Communities: Cities Country: Netherlands Ages included in the assessment: 14 years and older Reason provided for selection of the intervention community: Unclear, seems likely related to study centre location Intervention community: Maastricht (population 185,000) Comparison community: Doestiche (population comparable to Maastricht) |
|
| Interventions |
Name of the intervention: Hartslag Limburg Theory: Multi‐stage conceptual framework Aim: Improvement of lifestyle factors: (energy intake, fat intake, time spent on leisure‐time physical activity (of walking, bicycling and sports), and smoking Community strategy development phase: Yes Description of costs and resources: Total program costs of the program was 809,650 Euro; of which 555148 Euro was spent on exercise. Total cost of 5 year was 900,000 Euro, 86,000E start‐up costs Components of the intervention as per the inclusion criteria: #1 Social marketing ‐ mass media; #2 Other communication strategies ‐ printed guides showing walking and cycling routes including schedule; #4 Partnering ‐ working with organisations to encourage walking; #5 Specific settings ‐ schools Emphasis of intervention: Community participation Information given on intensity: 790 interventions over 4 years Assessment of intensity: High Start date: 1999 Duration: 4 years |
|
| Outcomes |
Measures: 1. Physical activity level (%). Measurement tool: unnamed questionnaire 2. Walking (hours/week). Measurement tool: Unnamed questionnaire 3. Bicycling (hrs/wk). Measurement tool: unnamed questionnaire 4. Leisure time physical activity (hours/week). Measurement tool: unnamed questionnaire Time points: Baseline and follow up (2 years and 3 years) |
|
| Notes | Some gender specific changes observed in other measures | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | High risk | Not randomised. Basis of allocation is unclear, but presumably related to Maastrich being the same location as the study centre. Groups were comparable with respect to the incidence and prevalence of CVD, number of inhabitants, number of municipalities and degree of urbanisation. Differences in % of males and females. Poor response rate to sample survey ‐ 55.5% and 57.5%. The effect of the study centre location within the intervention community is unknown |
| Performance bias | Low risk | Unclear on whether communities were blinded. No evidence of contamination. Indeed contamination doubtful ‐ 200 km apart. Evaluation study does not identify issues of the interventions integrity |
| Attrition bias | High risk | Attrition from baseline to post‐test was 37.3% |
| Detection bias | High risk | Outcome measure metric appropriate ‐ validated short version. Assumed to be applied as intended. Assessors were blinded to pre‐intervention measurement. Quality of the physical activity assessed acceptable ‐ over the period of one week. Poor response rate to sample (57.5% in Maastricht and 52.9% in control region). Based on population registries and would miss people not on registries. |
| Reporting bias | Low risk | No evidence of selective outcome reporting or incomplete reporting. Measures reported match the aims |
| Other | Unclear risk | The outcome analysis did adjust for baseline physical activity levels. Sample size calculation was undertaken |
| Overall bias | High risk | High risk of bias. 3 high risk categories |
Wilson 2014.
| Methods |
Study design: Cluster randomised controlled trial of communities Sampling frame: Lists of households phone numbers in the census tracts provided a survey lab and sampling group complimented with open through recruitment flyers, posters, banners in the community (schools, churches, local businesses) Sampling method: random sampling for community level measurement effects of the program Collection method: survey and direct collection through accelerometer Ethics and informed consent: Ethics approval and signed informed consent |
|
| Participants |
Communities: “underserved” (low income, high crime) communities located in the southeastern region of the United States, trial registration lists communities as Florence South Carolina (estimated population 47,000); Orangeburg South Carolina (estimated population 14,000) and Sumter South Carolina (estimated population 41,000). The assignment to the arms of the intervention is not specified Country: United States Ages included in the assessment (population level effects): 18 years and older, residents with no plans to move in the next 2 years Reason provided for selection of the intervention community: identified as matched on crime rates, poverty rates, PA levels and per cent minorities, then randomised Intervention community 1 (full intervention): not stated, described as underserved Intervention community 2 (walking only): not stated, described as underserved Comparison community (general population health information only): not stated, described as underserved |
|
| Interventions |
Name of the intervention: Positive Action for Today's Health (PATH) Theory: Ecological framework, social marketing Aim: Increase walking in low income, minority communities Components: Intervention #1: Police patrolled and social marketing strategy ‐ full intervention. #2 other communication ‐ calendars, door hangers & other incentives message objective developed community members and leader #4 working with police officers and #6 Environmental creating walking paths. "Identify walking route, hire walking leaders and police support, maintain route and monitor stray dogs PLUS grass‐roots social marketing campaign to promote walking on the route" Intervention #2 (partial): Police patrolled walking program Identify walking route, hire walking leaders and police support, maintain route and monitor stray dogs Community strategy development phase: Yes Description of costs and resources: None described Components of the intervention as per the inclusion criteria: #1 Social marketing ‐ mass media print materials, newspaper column, evening news; #4 Partnering ‐talks seminars by health. Described as an integrated community wide multi‐factorial risk factor education program Emphasis of intervention: walking trails Information given on intensity: The level of intensity of the intervention was not described by the authors, although multiple components and strategies are described. Process evaluation describes that an adequate dose was achieved Assessment of intensity: High Start date: July 2007, recruitment fall 2008. Duration: 2 years, final data collection July 2011 (obtained from Clinical Trials.gov) NCT01025726 |
|
| Outcomes | Community‐level impact of the program (measurement in individuals representing the community): undertaken at baseline, 6, 12 18 and 24 months 1. include 7‐day accelerometry estimates of PA: Actical. min MVPA/day. MET‐weighr min MVP/day Secondary (some publications state 7‐day whilst others state 8‐day) 2. four week PA recall pencil/paper survey min MPVPA/day, self reported plus other measures including blood pressure, BMI. waist circumference Measurement was undertaken at individual level including health screenings and measurements including the accelerometry PA data and a 4‐week PA recall. Data are analysed with a mixed model ANCOVA implemented within the community sample to examine intervention differences between communities Intervention, program‐level impact (describing a more immediate impact of the walking program): Direct stationary walking observations, trail users, scheduled walk participation |
|
| Notes | The individual level accelerometer estimates of PA showed no significant differences, however the community observations showed a greater number of community walkers on the trail. Intervention appears to have resulted in an increased trail use but not an overall increase in PA. Three communities were randomised, the community with the multi‐component intervention (full‐intervention) was deemed the intervention community.The authors state "Importantly the two samples are linked for the analysis reported here". The community of origin of these participants is unknown | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Low risk | Computer generated randomised allocation sequence with adequate allocation concealment |
| Performance bias | Low risk | Formative process evaluation provides evidence of program fidelity and adequate dose |
| Attrition bias | Low risk | Relatively low loss to follow adequate reporting using consort flow diagram |
| Detection bias | Unclear risk | The measure for physical activity through accelerometer is at low risk of bias. It is unclear whether the sample is representative of the population as 581 of 1216 reached through the household sampling frame declined and then of the 635, only 231 enrolled. The remaining 46% of the participants in the survey were those who self selected through advertisements rather than being a chance determination for their participation. Participants received financial incentives for their participation in the data collection in all arms of the study. Only those persons of African‐American, > 18 years ad older ad no plans to move in 2 years were included. Although the impact of the sampling is unknown |
| Reporting bias | Low risk | Primary outcomes reported from accelerometer were found to be negative. Self‐reported measures for the same primary outcome were not reported,by the authors, however we did not deem this discrepancy as reporting bias as the self‐report measure is at higher risk of bias than the accelerometer recorded data |
| Other | Low risk | Power for this trial to detect differences in outcomes 1 year into the trial and the maintenance of outcomes from month 12 to 24 were calculated. Analyses assume that to have a clinically meaningful effect the patrolled walking plus social marketing community should have an increase of 8 min/day of MVPA over either of the other communities, this translates into an effect size of 0.35 standard deviation units assuming a standard deviation of 23 which is in the range of what was observed in the Behavioral Risk Factor Surveillance Survey (BRFSS) validation study |
| Overall bias | Low risk | Appropriate statistical analyses were undertaken |
Young 1996.
| Methods |
Study design: Controlled before and after study (cohort and independent) Sampling frame: no detail Sampling method: no detail Collection method: survey Ethics and informed consent: no detail |
|
| Participants |
Communities: Cities of California, USA ‐ California, four cities: two intervention and two control (a fifth city, Santa Aria had only cardiovascular morbidity and mortality surveillance) Country: United States Ages included in the assessment: 12 ‐ 74 years age Reason provided for selection of the intervention community: limited resources and overlap of media markets Intervention community: Monterey and Salinas Comparison community: Modesto and San Luis |
|
| Interventions |
Name of the intervention: Stanford five city project Theory: Not explicitly stated Aim: Risk reduction educational program Components: 6 year integrated community wide multifactorial risk factor education program #1: mass media print materials, newspaper column, evening news; #4 talks seminars by health : April 1980 to July 1996 Community strategy development phase: No Description of costs and resources: None described Components of the intervention as per the inclusion criteria: #1 Social marketing ‐ mass media print materials, newspaper column, evening news; #4 Partnering‐talks seminars by health. Described as an integrated community wide multifactorial risk factor education program Emphasis of intervention: unclear Information given on intensity: described as "relatively weak intervention effort" Assessment of intensity: Medium Start date: 1980 Duration: 5 years |
|
| Outcomes |
Measures: 1. % in vigorous activities. Measurement tool: Questionnaire 2. Sum of usual activities (maximum value =5); Questionnaire 3. Daily expenditure (kcal kg‐1 day‐1); Measurement tool: Stanford 7‐day physical activity recall 4. Exercise knowledge. Measurement tool: Questionnaire (5 questions) Time points: Baseline (I1) and 3 other independent surveys (I2 to 4) and 3 other cohort surveys (C2 to C4) which cover the first 6 years of the project. Surveys were conducted every 2 years |
|
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | High risk | Not randomised. Allocation not concealed. There were significant baseline differences between treatment and control cities for most demographic variables. Control cities were more likely to be white, non‐Hispanic and were more highly educated, less likely to smoke and have lower BMI ’s. The men in the control cities were significantly younger than the men in the treatment cities |
| Performance bias | Unclear risk | No evidence of blinding. No evidence of contamination although possible (although likely low) risk given that mass media was used, and all communities were in northern California |
| Attrition bias | High risk | High attrition 61% ‐ due largely to emigration |
| Detection bias | Unclear risk | Physical activity measurement shown previously to be valid and reliable. Physical activity measured over period of 7 days. Stated that participants we "Identified from randomly selected households", however there are no details as per the sampling frame nor the method of randomisation to determine appropriateness and whether truly representative. Response rates were 65%, 70%, 65% and 56% and thus reasonably representative |
| Reporting bias | Low risk | No evidence of reporting bias |
| Other | Unclear risk | None identified. No sample size calculation for physical activity |
| Overall bias | High risk | High risk of bias. 2 high risk categories |
Zhang 2003.
| Methods |
Study design: Controlled before and after study (independent) Sampling frame: Whole community Sampling method: Independent random samples using simple cluster plus systematic randomisation Collection method: Questionnaire survey and physical examination and blood tests Ethics and informed consent: not stated |
|
| Participants |
Communities: Community in Shandong, China Country: China Ages included in the assessment: 25 to 75 years Reason provided for selection of the intervention community: Intervention community: Intervention community (population 50,000) Comparison community: Control village |
|
| Interventions |
Duration: 4 years Name of the intervention: not stated Theory: none stated Aim: reduction of risk factors for diabetes Community strategy development phase: yes Description of costs and resources: no description Components of the intervention as per the inclusion criteria: #2 Other communication strategies ‐ to all residents of the city, going regularly from house to house to personally distribute handouts primarily info booklets. Local health officer providing health education and lectures. Exercise included as a risk factor targeted for modification; #3 Individual counselling ‐ high risks and diabetes identified by primary care clinicians and tested and individual counselling (every 6 months high risk, 3 months diabetes). Primary intervention was health education of the risk factors for diabetes to ordinary people Emphasis of intervention: emphasis on individual counselling and screening with the provision of advise on risk factors. (#3) Information given on intensity: none provided Assessment of intensity: high Start date: 1997 Duration: 4 years |
|
| Outcomes |
Measures: 1. Non‐occupational physical activity (times/wk) Measurement tool: unnamed questionnaire Time points: Baseline and follow‐up |
|
| Notes | Effects on measures of BMI and overweight | |
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Selection bias | Unclear risk | Not randomised and no details provided for allocation of communities. The studied communities had 50,000 population each. No information about the geographic, economic and culture characters. Comparisons were made with small samples (around 200) randomly chosen from the two communities. At baseline, two groups were comparable in terms of gender and age. Unclear what the effects of reversing communities would be |
| Performance bias | Unclear risk | No interventions in control group. There is no description of special measures to prevent contamination. Unlikely to have contamination because they were two cities. The integrity of the intervention is unclear |
| Attrition bias | Low risk | Independent samples ‐ Attrition n/a |
| Detection bias | High risk | Physical activity was measured using survey questions and likely to have been applied as intended. No detailed information about the source and validity of the measures. Representativeness of the samples unclear. The samples were relatively small (around 200). It is hard to say that they can represent the whole communities |
| Reporting bias | Unclear risk | Reporting bias is possible given the brevity of reporting |
| Other | Unclear risk | None |
| Overall bias | High risk | High risk of bias. 2 high risk categories |
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Aadahl 2009 | Not community wide |
| Ackermann 2003 | Population not inclusive |
| Alcalay 1999 | Wrong study design |
| Alfonso 2011 | Wrong study design, same community |
| Aranceta 2013 | Inadequate description |
| Austin 2006 | Wrong study design, not community wide (8 participants only) |
| Baker 2008 | Not community wide |
| Balagopal 2008 | Wrong study design, singular intervention without control |
| Battram 2011 | Not community wide, lack of focus on physical activity |
| Bauman 2001 | State level mass‐media intervention rather than community level |
| Baxter 1997a | Intervention not eligible, does not address physical activity behaviour directly |
| Baxter 1997b | Intervention not eligible, does not address physical activity behaviour directly |
| Beets 2013 | School based primary focused, not community |
| Bennett 2006 | Wrong study design |
| Berkowitz 2008 | Population not inclusive |
| Berry 2013 | Not community physical activity, weight management in schools |
| Bickmore 2013 | Not community wide intervention, randomised individuals not communities |
| Bjaras 2001 | Intervention not eligible |
| Blake 1987 | Wrong study design, no control population |
| Blunt 2009 | Intervention not eligible |
| Bopp 2008 | Wrong study design |
| Brown 1996 | Not community wide |
| Bryant 2010 | Wrong study design (VERB) |
| Bull 2006 | Wrong study design, baseline data of an RCT in one community |
| Caballero 1998 | Intervention not eligible |
| Castro 2013 | Wrong study design, uncontrolled pilot study of obesity |
| Chan 2008 | Not community wide, pedometer evaluation |
| Cheadle 2000 | Wrong study design |
| Cheadle 2011 | Wrong study design |
| Cheadle 2012 | Wrong study design |
| Chen 2005 | Wrong study design |
| Chen 2008 | Wrong study design, no control group before intervention |
| Cheng 1998 | Intervention not eligible |
| Cheng 2009 | Not community wide, not inclusive |
| Chomitz 2010 | Primary weight management, wrong study design |
| Cochrane 2008 | Wrong study design, outcome assessment is retrospective |
| Cohen 2013 | Park intervention, not community wide PA intervention |
| Coitinho 2002 | Wrong study design |
| Craig 2006 | Wrong study design, primarily a national campaign with pedometers |
| Croker 2012 | Primarily school based, not community wide PA |
| Currie 2001 | Wrong study design, intervention not eligible |
| Davis 2003 | Intervention not eligible |
| De Bourdeaudhuij, 2011 | Wrong study design, school based rather than community wide |
| De Cocker 2008 | Intervention does not meet criteria, not part of an included study |
| DeBar 2009 | Population not inclusive |
| DeBate 2009 | Wrong study design, post‐test only |
| Dishman 2005 | Intervention not eligible |
| Dollahite 1998 | Intervention not eligible, physical activity not measured |
| Dowse 1995 | Wrong study design, no control |
| Draper 2009 | Intervention not eligible, study design retrospective qualitative process evaluation |
| Dubuy 2013 | Wrong study desgin lacking baseline data for intervention group, statewide intervention |
| Economos 2007 | Population not inclusive (school children in years 1 to 3), no intent to be community wide |
| Economos 2013 | Not focused on PA, wrong study design |
| Egawa 2007 | Intervention not eligible, not inclusive of community |
| Eisenmann 2008 | Primarily a school based intervention, not community wide |
| Eliah 2008 | Intervention not eligible, eye care only |
| Englert 2004 | Wrong study design, pilot only |
| Estabrooks 2008 | Wrong study design, community based but not community wide |
| Fang 2003 | Intervention not eligible, no physical activity |
| Fisher 2004 | Population not inclusive |
| Fotu 2011 | PA not primary outcome, focus is obesity |
| Fotu 2011a | PA not primary focus, focus is obesity |
| Frew 2014 | Wrong study design, no contemporary control ‐ modelling only |
| Futterman 2004 | Intervention not eligible, insufficient |
| Gao 2008 | Wrong study design, no control, only before and after comparison of intervention |
| Gesell 2013 | Small not community‐wide sample |
| Gorely 2009 | Intervention not eligible, insufficient components, primary school based |
| Grydeland 2013 | School based, not community wide |
| Guo 2007 | Wrong study design |
| Guo 2008 | Not community wide |
| Han 2003 | Intervention not eligible, not aimed at physical activity |
| Herbert 2013 | School based, not community wide |
| Hillsdon 1995 | Wrong study design, review only |
| Huhman 2007 | Wrong study design, no contemporary control, primarily mass media, specific community components and effects not identified |
| Jason 1991 | Intervention not eligible, less than 6 months, wrong study design |
| Kamieneski 2000 | Intervention not eligible, too short, lack of physical activity |
| Kandula 2013 | Trial registration only, trial of heart disease intervention targeting individuals |
| Kelder 1995 | Intervention not eligible, focus is on healthy eating rather than physical activity |
| Kimura 2013 | Intervention delivered at community centres, not defined geographically |
| King 1995 | Wrong study design |
| King 1998 | Wrong study design |
| Kiyu 2006 | Wrong study design, no control group, limited physical activity intervention |
| Kogan 2013 | Not community wide, and enrolled intervention |
| Kremer 2011 | Empahsis on obesity rather than PA, no valid measure of PA |
| Krishnan 2011 | Wrong study design, uncontrolled before and after of 2 intervention communities |
| Larkin 2003 | Wrong study design |
| Lawlor 2003 | Intervention not eligible, singular strategy |
| Lee 2004 | Intervention not eligible, only 3 months duration |
| Lee 2007 | Not community wide, participants from the same community |
| Lee 2008a | Intervention not eligible, focus is substance misuse |
| Lee 2008b | Not community wide, participants from the same community |
| Li 2002 | Wrong study design |
| Li 2008 | Intervention not eligible, patients with impaired glucose tolerance recruited from 35 clinics |
| Lindstrom 2003 | Intervention not eligible, high risk groups identified and then randomised to intervention |
| Lyle 2008 | Wrong study design, lacks a control, only 12 weeks duration |
| Maddock 2005 | Wrong study design, lacks a control |
| Madsen 2013 | Not community wide |
| Malmgren 1986 | Wrong study design, also lacks relevancy |
| Marshall 2004 | Wrong study design, inadequate intervention |
| Matsudo 2002 | Wrong study design |
| Matsudo 2003 | Wrong study design, no results |
| McDermott 2010 | Wrong study design, no baseline comparison |
| Merom 2005 | Wrong study design, intervention not eligible (too short) |
| Meyer 1980 | Intervention not eligible: primarily mass media, but the additional component not available to whole of community only selected individuals |
| Millar 2011 | Physical activity not the primary outcome, obesity |
| Millar 2013 | Physical activity not primary outcome, obesity |
| Mohan 2006 | Wrong study design |
| Muntoni 1999 | Intervention not eligible, wrong study design ‐ no control |
| Napolitano 2006 | Wrong study design, work sites rather than community, duration too short |
| Nickelson 2011 | Wrong study design, drawn from same community |
| Niederer 2009 | Intervention not eligible, primarily school‐based |
| Ogilvie 2014 | Project description only. Wrong study design, not community wide intervention for PA |
| Owen 1987 | Intervention not eligible, not to whole of community |
| Pabayo 2010 | Wrong study design, no control or intervention |
| Pekmezi 2009 | Not community wide |
| Phelan 2002 | Intervention not eligible |
| Plescia 2008 | Wrong study design, comparison against historic reference data |
| Pucher 2003 | Intervention not eligible, describes injuries |
| Puoane 2006 | Intervention not eligible, not aimed at whole of community |
| Quan 2006 | Wrong study design |
| Reger 2002 | Intervention not eligible, intervention only 8 weeks, 1 month post‐follow up |
| Reger‐Nash 2006 | Intervention not eligible, intervention only 8 weeks |
| Renger 2002 | Wrong study design, uncontrolled, primarily mass media |
| Rhoades 2001 | Intervention not eligible |
| Rodrigues 2006 | Wrong study design, analysis of enviromental factors |
| Roman 2008 | Intervention not eligible |
| Ronda 2004 | Intervention not eligible, organisational only, physical activity not measured |
| Ronda 2004a | Intervention not eligible |
| Ronda 2005 | Intervention not eligible |
| Rooney 2008 | Wrong study design, uncontrolled, limited intervention |
| Ross 2009 | No results, only a listing of interventions |
| Roux 2008 | Wrong study design, cost‐effectiveness synthesis |
| Sallis 2003 | Intervention not eligible, primarily school based |
| Salmon 2011 | Protocol description. Primarily school based intervention |
| Sarrafzadegan 2013 | Outcomes of cardio‐metabolic risk factors only |
| Sayers 2012 | Although ITS, does not have a valid measure of population PA levels, lack of clarity whether intervention is community wide |
| Sevick 2000 | Intervention not eligible |
| Sevick 2007 | Not community wide, groups defined by randomisation not community |
| Shea 1996 | Intervention not eligible, inadequate physical activity focus |
| Shen 2007 | Intervention not eligible, no physical activity |
| Simmons 1998 | Population not inclusive |
| Simmons 2004 | Not community wide, primarily only one strategy |
| Simmons 2008 | Intervention not eligable, no outcomes of physical activity |
| Simoes 2009 | Wrong study design |
| Simons‐Morton 1998 | Wrong study design |
| Sinclair 2007 | Wrong study design |
| Singh 2006 | Population not inclusive, school strategy only, no community involvement |
| Singh 2009 | Population not inclusive |
| Slootmaker 2005 | Intervention not eligible, no results |
| Smith 2000 | Wrong study design |
| Smith 2002 | Wrong study design |
| Smith 2004 | Wrong study design |
| Smolander 2000 | Not community wide |
| Sorensen 2005 | Wrong study design |
| Sorensen 2006 | Wrong study design, systematic review |
| Speck 2007 | Intervention not eligible, one site, minimal environmental, women only |
| Spink 2008 | Population not inclusive, one strategy only |
| Spittaels 2007 | Intervention not eligible, web‐based and no attempt to reach broader community |
| Spruijt‐Metz 2008 | Population not inclusive |
| Stamm 2001 | Wrong study design |
| Stanton 1997 | Intervention not eligible |
| Staten 2004 | Not community wide |
| Staten 2005 | Wrong study design, no control |
| Staunton 2003 | Wrong study design, process evaluation |
| Steckler 2003 | Wrong study design, school based only |
| Steele 2007 | Not community wide, not inclusive |
| Steptoe 1999 | Not community wide |
| Steptoe 2000 | Not community wide, GP practices only |
| Steptoe 2001 | Not community wide, GP practices only |
| Sternberg 2006 | Not community wide |
| Sternfeld 2009 | Not community wide |
| Stevens 1998 | Intervention not eligible |
| Stevens 1999 | Wrong study design |
| Stevens 2005 | Not community wide |
| Stewart 2001 | Not community wide |
| Stewart 2004 | Wrong study design |
| Stewart 2006 | Intervention not eligible, school based |
| Stock 2007 | Intervention not eligible |
| Stone 1996 | Not community wide, process evaluation of school based intervention |
| Stone 1998 | Wrong study design, review of school and community interventions |
| Strachan 2007 | Wrong study design, no control |
| Stubbs 2002 | Intervention not eligible |
| Sugden 2008 | Not community wide |
| Suminski 2009 | No measure of physical activity |
| Sun 2007 | Wrong study design |
| Swinburn 2011 | Umbrella description of study addressing obesity, individual studies excluded |
| Tan 2006 | Population not inclusive, randomised in same community, one strategy |
| TenBrink 2009 | Wrong study design |
| Thomas 2009 | Same as Sayers 2012. Does not have valid measures of physical activity at a population level |
| Timperio 2004 | Wrong study design |
| Toftager 2011 | Primarily school based. Inadequate community wide component |
| Togami 2008 | Intervention not eligible |
| Tsai 2009 | Intervention not eligible |
| Tsorbatzoudis 2005 | Internvention not eligible, primarily school based |
| Tudor‐Smith 1998 | Intervention not eligible, physical activity not the focus |
| Tully 2007 | Intervention not eligible, inadequate strategies |
| Two Feathers 2005 | Population not inclusive, geography undefined |
| Utter 2010 | School based, not community wide |
| Utter 2011 | School based, not community wide |
| van Stralen 2009 | Not community wide |
| van Stralen 2011 | No community wide |
| Voyle 1999 | Wrong study design, formative evaluation |
| Walker 2009 | Intervention not eligible, population reach weak |
| Wallace 1998 | Intervention not eligible, intervention and control participants from the same community |
| Wallmann 2011 | Not community wide, wrong study design |
| Wallmann 2012 | Not community wide, wrong study design |
| Wang 2009 | Population not inclusive |
| Warden 1999 | Wrong study design |
| Wardle 2001 | Intervention not eligible, mass media |
| Warren 1999 | Wrong study design |
| Wellman 2007 | Not community wide, limited to one setting |
| Wen 2002 | Not community wide in focus |
| Whaley 2008 | Intervention not eligible |
| Wheat 1996 | Not community wide |
| Wiesemann 1997 | Not community wide |
| Wilcox 2006 | Population not inclusive, persons recruited at sites, non‐participants not exposed |
| Wilcox 2007 | Not community wide, restricted setting |
| Wilcox 2009 | Intervention not eligible, not community inclusive |
| Williams 2007 | Not community wide, restricted to one employment sector |
| Wimbush 1998 | Intervention not eligible, primarily mass media, wrong study design |
| Withall 2012 | No outcomes of physical activity. Description of recruitment into programs. Wrong study design |
| Wu 2004 | Wrong study design, pre and post only |
| Wyatt 2008 | Not community wide, recruited using mass media |
| Xu 2000 | Intervention not eligible |
| Xu 2001 | Intervention not eligible, does not include physical activity |
| Xu 2012 | Solely based in the school environment, not community wide |
| Yancey 2001 | Population not inclusive |
| Yancey 2003 | Wrong study design, before and after only, uncontrolled |
| Yang 2012 | Trial registration only. Not community wide intervention |
| Yin 2012 | Physical activity not primary outcomes. Intervention characteristics not community wide |
| Zhu 2008 | Population not inclusive |
| Zivkovic 1998 | Intervention not eligible |
| Zoellner 2011 | Intervention does not appear to aim to have comprehensive community wide reach, thus not community wide |
| Zoellner 2012 | Process evaluation of an excluded study. Unclear if measured physical activity, not control |
Characteristics of ongoing studies [ordered by study ID]
Davey 2011.
| Trial name or title | My Health Matters |
| Methods | Community interventions, pre & post, control ‐ but the identification of the control is undescribed "Analysis plan describes chi‐squared analysis to test for differences in the distributions of PA categories in the intervention and control areas." |
| Participants | most deprived electoral wards in Stoke‐on‐Trent, UK |
| Interventions | Community‐lend interventions (working with the community and multiple agencies) 4 overlapping phases over 3 years |
| Outcomes | % of population physically active (taking part on at least 3 days/week in moderate intensity sport and active leisure) by 10% more (after 2 years of intervention) |
| Starting date | July 2009; no completion date identified |
| Contact information | None available; rachel.davey@canberra.edu.au |
| Notes | This study is identified as a past project on http://www.staffs.ac.uk/schools/sciences/geography/links/IESR/projects.shtml website. Rachel Davey is no longer in the UK. The trial does not appear to be registered |
Differences between protocol and review
In the review, we did not specifically list 'historically controlled studies' as an included study design, given that these studies would be included already as interrupted time‐series. Otherwise, all studies were required to have a contemporary control. Planned analyses which were not required or appropriate are described in the methods section.
In the protocol we had not envisaged the important differences in baseline between intervention and control group for a number of studies. Given these differences we calculated several additional effect measures as discussed in the methods section, in consultation with statisticians.
Contributions of authors
PB and DF were responsible for the primary conceptualisation of the review. The draft of the protocol and the completed review were written in accordance with a project plan by all authors (Baker 2010). PB led the development of the writing of the protocol and both PB and DF the review.
PB assessed risk of bias, extracted data for all studies meeting the inclusion criteria. DF, JS and CF shared independent completion of risk of bias assessment and data extraction forms.
PB and DF developed the criteria and independently assessed the intensity of intervention. They shared the management and analysis of the numerical data. CF and JS also contributed to the analysis of the data.
ALW contributed to the design of the protocol, developed the search strategy, ran the majority of electronic database searches and de‐duplicated the results, unpicked systematic reviews and guidelines for relevant primary studies, and commented on the review.
All authors contributed to the conduct and writing of the update.
Disclaimer
The findings and conclusions of this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention, Queensland University of Technology, Queensland Health or other institutions of affiliation of the authors.
Sources of support
Internal sources
-
Health Practitioner Research Scheme 2009 ‐ 2010: Queensland Health, Australia.
$29,000 Australian was provide as a research fellowship supporting the reviewers PB and DF.
-
Vacation Research Expereince Scheme 2013/2014: Queensland University of Technology, Australia.
$2,000 Scholarship was provided to under‐graduate student Ms Yolanda Lovie‐Toon who supported the update.
External sources
-
National Institute for Health Research, Cochrane Review Incentive Scheme, UK.
5000 pounds sterling for publication of the review by a set deadline (4 February 2011)
Declarations of interest
The authors have no conflicts of interest pertaining to this research.
Edited (no change to conclusions)
References
References to studies included in this review
Brown 2006 {published data only}
- Austin G, Mummery K, Schofield G. The 10,000 Steps Rockhampton project: Using a community grant scheme to build community capacity for health related physical activity in Rockhampton. 2004 Australian Conference of Science and Medicine in Sport Hot topics from the Red Centre 2004:43.
- Brown W, Eakin E, Mummery K, Trost S. 10,000 Steps Rockhampton: Establishing a multi‐strategy physical activity promotion project in a community. Health Promotion Journal of Australia 2003;14(2):96‐101. [Google Scholar]
- Brown WJ, Mummery K, Eakin E, Schofield G. 10,000 Steps Rockhampton: Evaluation of a whole community approach to improving population levels of physical activity. Journal of Physical Activity and Health 2006;1:1‐14. [Google Scholar]
- Burton NW, Walsh A, Brown WJ. It just doesn't speak to me: mid‐aged men's reactions to '10,000 Steps a Day'. Health Promotion Journal of Australia 2008;19(1):52‐9. [DOI] [PubMed] [Google Scholar]
- Mummery K, Brown W, Schofield G, Caperchione C, Austin G, Steele R. Multi‐strategy approaches to the promotion of health‐related physical activity at the community level: examples from 10,000 Steps Rockhampton (Abstract). Journal of Science and Medicine in Sport 2004;7(4 Suppl):42. [Google Scholar]
- Mummery WK, Brown WJ. Whole of community physical activity interventions: easier said than done. British Journal of Sports Medicine 2009;43(1):39‐43. [DOI] [PubMed] [Google Scholar]
- Schofield G, Steele R, Mummery K, Brown. Engaging a local council to promote physical activity: the case of dog walking in the 10,000 Steps Rockhampton project. Health Promotion Journal of Australia 2004;15:78‐81. [Google Scholar]
Brownson 2004 {published data only}
- Brownson RC, Baker EA, Boyd RL, Caito NM, Duggan K, Housemann RA, et al. A community‐based approach to promoting walking in rural areas. American Journal of Preventive Medicine 2004;27(1):28‐34. [DOI] [PubMed] [Google Scholar]
- Brownson RC, Smith CA, Pratt M, Mack NE, Jackson‐Thompson J, Dean CG, et al. Preventing cardiovascular disease through community‐based risk reduction: The Bootheel Heart Project. American Journal of Public Health 1996;86(2):206‐13. [DOI] [PMC free article] [PubMed] [Google Scholar]
Brownson 2005 {published data only}
- Brownson RC, Hagood L, Lovegreen SL, Britton B, Caito NM, Elliott MB, et al. A multilevel ecological approach to promoting walking in rural communities. Preventive Medicine 2005;41(5‐6):837‐42. [DOI] [PubMed] [Google Scholar]
De Cocker 2007 {published data only}
- Cocker KA, Bourdeaudhuij IM, Brown WJ, Cardon GM. Effects of "10,000 steps Ghent": a whole‐community intervention. American Journal of Preventive Medicine 2007;33(6):455‐63. [DOI] [PubMed] [Google Scholar]
- Cocker KA, Bourdeaudhuij IM, Brown WJ, Cardon GM. Four‐year follow‐up of the community intervention '10 000 steps Ghent'. Health Education Research 2011;26(2):372‐80. [DOI] [PubMed] [Google Scholar]
- Cocker KA, Bourdeaudhuij IM, Brown WJ, Cardon GM. The effect of a pedometer‐based physical activity intervention on sitting time. Preventive Medicine 2008;47(2):179‐81. [DOI] [PubMed] [Google Scholar]
Eaton 1999 {published data only}
- Carleton RA, Lasater TM, Assaf AR, Feldman HA, McKinlay S. The Pawtucket Heart Health Program: community changes in cardiovascular risk factors and projected disease risk. American Journal of Public Health 1995;85(6):777‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton CB, Lapane KL, Garber CE, Gans KM, Lasater TM, Carleton RA. Effects of a community‐based intervention on physical activity: the Pawtucket Heart Health Program. American Journal of Public Health 1999;89(11):1741‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGraw SA, McKinlay SM, McClements L, Lasater TM, Assaf A, Carleton RA. Methods in program evaluation: The process evaluation system of the Pawtucket Heart Health Program. Evaluation Review 1989;13(5):459‐83. [Google Scholar]
Gao 2013 {published data only}
- Gao F, Liu Q M, Ren Y J, He P P, Lv J, Li L M. [Assessment on the short‐term impact regarding the community‐based interventions to improve physical activities in three urban areas of Hangzhou city]. [Chinese]. Chung‐Hua Liu Hsing Ping Hsueh Tsa Chih Chinese Journal of Epidemiology 2013;34:582‐5. [PubMed] [Google Scholar]
- Lv J, Liu QM, Ren YJ, He PP, Wang SF, Gao F, et al. A community‐based multilevel intervention for smoking, physical activity and diet: short‐term findings from the Community Interventions for Health programme in Hangzhou, China. Journal of Epidemiology and Community Health 2014;68:333‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Goodman 1995 {published data only}
- Goodman RM, Wheeler FC, Lee PR. Evaluation of the Heart to Heart Project: lessons from a community‐based chronic disease project. American Journal of Health Promotion 1995;9(6):443‐55. [DOI] [PubMed] [Google Scholar]
- Wheeler FC, Lackland DT, Mace ML, Reddick A, Hogelin G, Remington PL. Evaluating South Carolina's community cardiovascular disease prevention project. Public Health Reports 1991;196(5):536‐43. [PMC free article] [PubMed] [Google Scholar]
Gu 2006 {published data only}
- Gu W. Study on the risk factors of hypertension and the evaluation of the comprehensive intervention in the rural community of Jiaxing. Master thesis of Zhejiang University, School of Public Health 2006.
- Zhou A, Gu W, Wang J, Cao J, Li R, Li X. Evalaution of the comprehensive intervention of hypertension in the rural community of Jiaxing. Prevention and Treatment of Cardio‐Cerebral‐Vascular Disease 2005;5(6):52‐4. [Google Scholar]
Guo 2006 {published data only}
- Guo Y, Wang H, Yan H, Zhang F, Gao C, Xiang N, et al. Evaluation on the effect of hypertension health education in country community. Chinese Journal of Health Education 2006;22(10):770‐2. [Google Scholar]
Jenum 2006 {published data only}
- Jenum AK, Anderssen SA, Birkeland KI, Holme I, Graff‐Iversen S, Lorentzen C, et al. Promoting physical activity in a low‐income multiethnic district: effects of a community intervention study to reduce risk factors for type 2 diabetes and cardiovascular disease: a community intervention reducing inactivity. Diabetes Care 2006;29(7):1605‐12. [DOI] [PubMed] [Google Scholar]
- Jenum AK, Lorentzen C, Anderssen SA, Birkeland KrI, Holme I, Lund‐Larsen PG, et al. Promoting physical activity in a multi‐ethnic district: methods and baseline results of a pseudo‐experimental intervention study. European Journal of Cardiovascular Prevention and Rehabilitation 2003;10(5):387‐96. [DOI] [PubMed] [Google Scholar]
- Jenum AK, Lorentzen C, Graff‐Iversen S, Anderssen S, Ødegaard AK, Holme I, et al. Can area‐based public health strategies reduce the social gradient in health? The “Romsås in Motion” Study – background, main results and lessons learnt [Kan lokalbaserte strategier bidra til å redusere sosiale helseforskjeller?]. Norsk Epidemiologi 2007;17(1):49‐57. [Google Scholar]
- Jenum AK, Lorentzen C, Ommundsen Y. Targeting physical activity in a low socioeconomic status population: observations from the Norwegian "Romsas in Motion" study. British Journal of Sports Medicine 2009;43(1):64‐9. [DOI] [PubMed] [Google Scholar]
- Lorentzen C, Ommundsen Y, Jenum AK, Holme I. The "Romsas in Motion" community intervention: mediating effects of psychosocial factors on forward transition in the stages of change in physical activity. Health Education and Behavior 2009;36(2):348‐65. [DOI] [PubMed] [Google Scholar]
- Lorentzen C, Ommundsen Y, Jenum AK, Holme I. The "Romsas in Motion" community intervention: program exposure and psychosocial mediated relationships to change in stages of change in physical activity. International Journal of Behavioral Nutrition and Physical Activity 2007;4:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Jiang 2008 {published data only}
- Jiang B, Wang W, Wu S. The effects of community intervention measures on prevention and control of hypertension. Chinese Journal of Prevention and Control of Chronic Non‐communicable Disease 2008;16(6):254‐7. [Google Scholar]
- Wang WZ, Fang XH, Wu Sp, Li SZ, Du XL, Bao SG, et al. Methods and evaluation on community health education in Beijing. Zhong Guo Man Xing Bing Yu Fang Yu Kong Zhi 1997;5(6):268‐71. [Google Scholar]
Kamada 2013 {published data only}
- Kamada M, Kitayuguchi J, Inoue S, Ishikawa Y, Nishiuchi H, Okada S, et al. A community‐wide campaign to promote physical activity in middle‐aged and elderly people: a cluster randomized controlled trial. International Journal of Behavioral Nutrition and Physical Activity 2013;10:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kloek 2006 {published data only}
- Kloek GC, Lenthe FJ, Nierop PWM, Koelen MA, Mackenbach JP. Impact evaluation of a Dutch community intervention to improve health‐related behaviour in deprived neighbourhoods. Health & Place 2006;12(4):665‐77. [DOI] [PubMed] [Google Scholar]
Kumpusalo 1996 {published data only}
- Kumpusalo E, Neittaanmaki L, Halonen P, Pekkarinen H. Finnish Healthy Village Study: impact and outcomes of a low‐cost local health promotion programme. Health Promotion International 1996;11(2):15. [Google Scholar]
- Kumpusalo E, Neittaanmaki L, Pekkarinen H, Hanninen O, Parviainen M, Penttila I, et al. Finnish Healthy Village Study: health profile analysis for local health promotion. Health Promotion International 1991;6(1):3‐12. [Google Scholar]
Luepker 1994 {published data only}
- Jacobs DR, Luepker RV, Mittelmark MB, Folsom AR, Pirie PL, Mascioli SR, et al. Community‐wide prevention strategies: evaluation design of the Minnesota Heart Health Program. Journal of Chronic Diseases 1986;39(10):775‐88. [DOI] [PubMed] [Google Scholar]
- Luepker RV, Murray DM, Jacobs DR, Mittelmark MB, Bracht N, Carlaw R, et al. Community education for cardiovascular disease prevention: risk factor changes in the Minnesota Heart Health Program. American Journal of Public Health 1994;84(9):1383‐92. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lupton 2003 {published data only}
- Lupton BS, Fonnebo V, Sogaard AJ. The Finnmark Intervention Study: Is it possible to change CVD risk factors by community‐based intervention in an Arctic village in crisis?. Scandinavian Journal of Public Health 2003;31(3):178‐86. [DOI] [PubMed] [Google Scholar]
- Lupton BS, Fonnebo V, Sogaard AJ, Fylkesnes K. The Finnmark Intervention Study: do community‐based intervention programmes threaten self‐rated health and well‐being? Experiences from Batsfjord, a fishing village in North Norway. European Journal of Public Health 2005;15(1):91‐6. [DOI] [PubMed] [Google Scholar]
- Lupton BS, Fonnebo V, Wilsegaard T, Sogaard AJ. The Finnmark Intervention Study: Does community intervention work? Trends in CVD risk factors in Arctic Norway. Norsk Epidemiologi 2003;13(1):65‐72. [Google Scholar]
Mead 2013 {published data only}
- Erber E, Beck L, Hopping BN, Sheehy T, Roose E, Sharma S. Food patterns and socioeconomic indicators of food consumption amongst Inuvialuit in the Canadian Arctic. Journal of Human Nutrition and Dietetics 2010;23:59‐66. [DOI] [PubMed] [Google Scholar]
- Hopping BN, Erber E, Mead E, Roache C, Sharma S. High levels of physical activity and obesity co‐exist amongst Inuit adults in Arctic Canada. Journal of Human Nutrition and Dietetics 2010;23:110‐4. [DOI] [PubMed] [Google Scholar]
- Hopping BN, Mead E, Erber E, Sheehy C, Roache C, Sharma S. Dietary adequacy of Inuit in the Canadian Arctic. Journal of Human Nutrition and Dietetics 2010;23:27‐34. [DOI] [PubMed] [Google Scholar]
- Mead EL, Gittelsohn J, Roache C, Corriveau A, Sharma S. A community‐based, environmental chronic disease prevention intervention to improve healthy eating psychosocial factors and behaviors in indigenous populations in the Canadian Arctic. Health Education & Behavior 2013;40:592‐602. [DOI] [PubMed] [Google Scholar]
- Sharma S. Assessing diet and lifestyle in the Canadian Arctic Inuit and Inuvialuit to inform a nutrition and physical activity intervention programme. Journal of Human Nutrition and Dietetics 2010;23:5‐17. [DOI] [PubMed] [Google Scholar]
- Sharma S, Gittelsohn J, Rosol R, Beck L. Addressing the public health burden caused by the nutrition transition through the Healthy Foods North nutrition and lifestyle intervention programme. Journal of Human Nutrition and Dietetics 2010;23:120‐7. [DOI] [PubMed] [Google Scholar]
Nafziger 2001 {published data only}
- Nafziger AN, Erb TA, Jenkins PL, Lewis C, Pearson TA. The Otsego‐Schoharie healthy heart program: prevention of cardiovascular disease in the rural US. Scandinavian Journal of Public Health Supplement 2001;56:21‐32. [PubMed] [Google Scholar]
Nguyen 2012 {published data only}
- Nguyen QN, Pham ST, Nguyen VL, Wall S, Weinehall L, Bonita R, et al. Implementing a hypertension management programme in a rural area: local approaches and experiences from Ba‐Vi district, Vietnam. BMC Public Health 2011;11:325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen QN, Pham ST, Nguyen VL, Weinehall L, Wall S, Bonita R, et al. Effectiveness of community‐based comprehensive healthy lifestyle promotion on cardiovascular disease risk factors in a rural Vietnamese population: a quasi‐experimental study. BMC Cardiovascular Disorders 2012;12:56. [DOI] [PMC free article] [PubMed] [Google Scholar]
Nishtar 2007 {published data only}
- Nishtar S, Badar A, Kamal MU, Iqbal A, Bajwa R, Shah T, et al. The Heartfile Lodhran CVD prevention project‐‐end of project evaluation. Promotion & Education 2007;14(1):17‐27. [PubMed] [Google Scholar]
NSW Health 2002 {published data only}
- NSW Health Department. 'Walk It: Active Local Parks' Summary Report. NSW Health Department April 2002:36.
O'Loughlin 1999 {published data only}
- O'Loughlin J, Paradis G, Kishchuk N, Gray‐Donald K, Renaud L, Fines P, et al. Coeur en sante St‐Henri‐‐a heart health promotion programme in Montreal, Canada: design and methods for evaluation. Journal of Epidemiology and Community Health 1995;49(5):495‐502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Loughlin JL, Paradis G, Gray‐Donald K, Renaud L. The impact of a community‐based heart disease prevention program in a low‐income, inner‐city neighbourhood. American Journal of Public Health 1999; Vol. 89, issue 12:1819‐26. [DOI] [PMC free article] [PubMed]
- Paradis G, O'Loughlin J, Elliott M, Masson P, Renaud L, Sacks‐Silver G, et al. Coeur en sante St‐Henri‐‐a heart health promotion programme in a low income, low education neighbourhood in Montreal, Canada: theoretical model and early field experience. Journal of Epidemiology and Community Health 1995;49(5):503‐12. [DOI] [PMC free article] [PubMed] [Google Scholar]
Osler 1993 {published data only}
- Osler M, Jespersen NB. The effect of a community‐based cardiovascular disease prevention project in a Danish municipality. Danish Medical Bulletin 1993;40:485‐9. [PubMed] [Google Scholar]
Phillips 2014 {published data only}
- Phillips G, Bottomley C, Schmidt E, Tobi P, Lais S, Yu G, et al. Measures of exposure to the Well London Phase‐1 intervention and their association with health well‐being and social outcomes. Journal of Epidemiology and Community Health 2014;68:597‐605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips G, Bottomley C, Schmidt E, Tobi P, Lais S, Yu G, et al. Well London Phase‐1: results among adults of a cluster‐randomised trial of a community engagement approach to improving health behaviours and mental well‐being in deprived inner‐city neighbourhoods. Journal of Epidemiology and Community Health 2014;68:606‐24. [DOI: 10.1136/jech-2013-202505] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips G, Renton A, Moore DG, Bottomley C, Schmidt E, Lais S, et al. The Well London program‐a cluster randomized trial of community engagement for improving health behaviors and mental wellbeing: baseline survey results. Trials 2012;13:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wall M, Hayes R, Moore D, Petticrew M, Clow A, Schmidt E, et al. Evaluation of community level interventions to address social and structural determinants of health: a cluster randomised controlled trial. BMC Public Health 2009;9:207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wall M, Hayes R, Moore D, Petticrew M, Clow A, Schmidt E, et al. Evaluation of community level interventions to address social and structural determinants of health: a cluster randomised controlled trial. BMC Public Health 2009;9:207. [DOI] [PMC free article] [PubMed] [Google Scholar]
Reger‐Nash 2005 {published data only}
- Gebel K, Bauman A, Reger‐Nash B, Leyden K. Does the environment moderate the impact of a mass media campaign to promote walking?. American Journal of Health Promotion 2011;26(1):45‐8. [DOI] [PubMed] [Google Scholar]
- Reger B, Cooper L, Booth‐Butterfield S, Smith H, Bauman A, Wootan M, et al. Wheeling walks: a community campaign using paid media to encourage walking among sedentary older adults. Preventive Medicine 2002;35(3):285‐92. [DOI] [PubMed] [Google Scholar]
- Reger‐Nash B, Bauman A, Booth‐Butterfield S, Cooper L, Smith H, Chey T, et al. Wheeling walks: evaluation of a media‐based community intervention. Family & Community Health 2005;28(1):64‐78. [DOI] [PubMed] [Google Scholar]
- Reger‐Nash B, Bauman A, Cooper L, Chey T, Simon KJ. Evaluating community wide walking interventions. Evaluation and Program Planning 2006;29(3):251‐9. [Google Scholar]
Rissel 2010 {published data only}
- Rissel CE, New C, Wen LM, Merom D, Bauman AE, Garrard J. The effectiveness of community‐based cycling promotion: findings from the Cycling Connecting Communities project in Sydney, Australia. International Journal of Behavioral Nutrition and Physical Activity 2010;7:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sarrafzadegan 2009 {published data only}
- Kelishadi R, Sarrafzadegan N, Sadri G, Pashmi R, Mohammadifard N, Tavasoli A, et al. Short‐term results of a community‐based program on promoting healthy lifestyle for prevention and control of chronic diseases in a developing country setting: Isfahan Healthy Heart Program. Asia‐Pacific Journal of Public Health 2011;23(4):518‐33. [DOI] [PubMed] [Google Scholar]
- Rabiei K, Kelishadi R, Sarrafzadegan N, Ali Abedi H, Alavi M, Heidari K, et al. Process evaluation of a community‐based program for prevention and control of non‐communicable disease in a developing country: The Isfahan Healthy Heart Program, Iran. BMC Public Health 2009;9:57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarraf‐Zadegan N, Sadri G, Malek Afzali H, Baghaei M, Mohammadi Fard N, Shahrokhi S, et al. Isfahan Healthy Heart Programme: a comprehensive integrated community‐based programme for cardiovascular disease prevention and control. Design, methods and initial experience. Acta Cardiologica 2003;58(4):309‐20. [DOI] [PubMed] [Google Scholar]
- Sarrafzadegan N, Kelishadi R, Esmaillzadeh A, Mohammadifard N, Rabiei K, Roohafza H, et al. Do lifestyle interventions work in developing countries? Findings from the Isfahan Healthy Heart Program in the Islamic Republic of Iran. Bulletin of the World Health Organization 2009;87(1):39‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarrafzadegan N, Kelishadi R, Sadri G, Malekafzali H, Pourmoghadas M, Heidari K, et al. Outcomes of a comprehensive healthy lifestyle program on cardiometabolc risk factors in a developing country: The Isfahan Healthy Heart Program. Archives of Iranian Medicine 2013;16(1):4‐11. [PubMed] [Google Scholar]
Simon 2008 {published data only}
- Simon C, Schweitzer B, Oujaa M, Wagner A, Arveiler D, Triby E, et al. Successful overweight prevention in adolescents by increasing physical activity: a 4‐year randomized controlled intervention [erratum appears in International Journal of Obesity 2008;32:1606]. International Journal of Obesity 2008;32(10):1489‐98. [DOI] [PubMed] [Google Scholar]
- Simon C, Wagner A, Platat C, Arveiler D, Schweitzer B, Schlienger JL, et al. ICAPS: a multilevel program to improve physical activity in adolescents. Diabetes & Metabolism 2006;32(1):41‐9. [DOI] [PubMed] [Google Scholar]
Solomon 2014 {published data only}
- ISRCTN. Understanding the impact upon physical activity of the ‘Devon Active Villages’ intervention. http://www.controlled‐trials.com/ISRCTN37321160 9/1/2013. [DOI: 10.1186/ISRCTN37321160; ISRCTN37321160] [DOI]
- Solomon E, Rees T, Ukoumunne O C, Metcalf B, Hillsdon M. The Devon Active Villages Evaluation (DAVE) trial of a community‐level physical activity intervention in rural south‐west England: a stepped wedge cluster randomised controlled trial. International Journal of Behavioral Nutrition and Physical Activity 2014;11(94). [DOI: 10.1186/s12966-014-0094-z] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon E, Rees T, Ukoumunne OC, Hillsdon M. The Devon Active Villages Evaluation (DAVE) trial: Study protocol of a stepped wedge cluster randomised trial of a community‐level physical activity intervention in rural southwest England. BMC Public Health 2012;12(581):1‐7. [DOI: 10.1186/1471-2458-12-581] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon E, Rees T, Ukoumunne OC, Metcalf B, Hillsdon M. Personal, social, and environmental correlates of physical activity in adults living in rural south‐west England: a cross‐sectional analysis. International Journal of Behavioral Nutrition and Physical Activity 2013;10:129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Solomon EL. The Devon Active Villages Evaluation (DAVE) Trial of a Community‐level Physical Activity Intervention in Rural South‐West England: A Stepped Wedge Cluster Randomised Controlled Trial: submitted as a thesis for the degree of Doctor of Philosophy in Sport and Health Sciences. 2014: The University of Exter, 2014:1‐456. [DOI] [PMC free article] [PubMed]
Wendel‐Vos 2009 {published data only}
- Ronckers ET, Groot W, Steenbakkers M, Ruland E, Ament A. Costs of the 'Hartslag Limburg' community heart health intervention. BMC Public Health 2006;6(51):1‐10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ronda G, Assema P, Candel M, Ruland E, Steenbakkers M, Ree J, et al. The Dutch Heart Health community intervention 'Hartslag Limburg': results of an effect study at individual level. Health Promotion International 2004;19(1):21‐31. [DOI] [PubMed] [Google Scholar]
- Ronda G, Assema P, Ruland E, Steenbakkers M, Ree J, Brug J. The Dutch heart health community intervention 'Hartslag Limburg': results of an effect study at organizational level. Public Health 2005;119(5):353‐60. [DOI] [PubMed] [Google Scholar]
- Ronda G, van AP, Ruland E, Steenbakkers M, Brug J. The Dutch Heart Health Community Intervention 'Hartslag Limburg': Design and results of a process study. Health Education Research 2004;19(5):596‐607. [DOI] [PubMed] [Google Scholar]
- Schuit AJ, Wendel‐Vos GCW, Verschuren WMM, Roncker ET, Ament A, Assema P, et al. Effect of 5‐year community intervention Harstlag Limburg on cardiovascular risk factors. American Journal of Preventive Medicine 2006;30(2):237‐42. [DOI] [PubMed] [Google Scholar]
- Verkleij SPJ, Adriaanse MC, Verschuren WMM, Ruland E, Wendel‐Vos GCW, Schuit AJ. Five‐year effect of community‐based intervention Hartslag Limburg on quality of life: A longitudinal cohort study. Health and Quality of Life Outcomes 2011;9(1):11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wendel‐Vos GCW, Dutman AE, Verschuren WMM, Ronckers ET, Ament A, Assema P, et al. Lifestyle factors of a five‐year community‐intervention program: the Hartslag Limburg intervention. American Journal of Preventive Medicine 2009;37(1):50‐6. [DOI] [PubMed] [Google Scholar]
Wilson 2014 {published data only}
- Coulon S, Wilson D, Griffin S, George SM, Alia KA, Trumpeter NN, et al. Formative process evaluation for implementing a social marketing intervention to increase walking among African Americans in the Positive Action for Today's Health Trial. American Journal of Public Health 2012;102:2315‐21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- University of South Carolina. Positive Action for Today's Health (PATH). http://clinicaltrials.gov/show/NCT01025726. [NCT01025726]
- Wilson DK, George SM, Trumpeter NN, Coulon SM, Griffin SF, Wandersman A, et al. Qualitative developmental research among low income African American adults to inform a social marketing campaign for walking. International Journal of Behavioral Nutrition and Physical Activity 2013;10:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson DK, Trumpeter NN, George SM, Coulon SM, Griffin S, Lee Van Horn M, et al. An overview of the “Positive Action for Today's Health”(PATH) trial for increasing walking in low income, ethnic minority communities. Contemporary Clinical Trials 2010;31:624‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson DK, Horn ML, Siceloff ER, Alia KA, George SM, Lawman HG, et al. The results of the “Positive Action for Today’s Health” (PATH) trial for increasing walking and physical activity in underserved African American communities. Annals of Behavioral Medicine 2014:1‐13. [DOI: 10.1007/s12160-014-9664-1] [DOI] [PMC free article] [PubMed] [Google Scholar]
Young 1996 {published data only}
- Farquhar JW, Fortmann SP, Maccoby N, Haskell WL, Williams PT, Flora JA, et al. The Stanford Five‐City Project: Design and methods. American Journal of Epidemiology 1985;122(2):323‐34. [DOI] [PubMed] [Google Scholar]
- Young DR, Haskell WL, Taylor CB, Fortmann SP. Effect of community health education on physical activity knowledge, attitudes, and behavior. The Stanford Five‐City Project. American Journal of Epidemiology 1996;144(3):264‐74. [DOI] [PubMed] [Google Scholar]
Zhang 2003 {published data only}
- Zhang Y, Zhao ZT, Hao FR, Jia CX, Wang SM, Feng YQ. Effectiveness of diabetes mellitus community intervention on urban population’s obesity and related factors. Chinese Journal of Public Health 2003;19(11):1396‐8. [Google Scholar]
- Zhang Y, Zhao ZT, Li GR, Hao FR, Wang SM, Pan YZ, et al. Effectiveness of community intervention on population's diabetes mellitus knowledge and its influencing factors. Chinese Journal of Public Health 2003;19(7):888‐9. [Google Scholar]
References to studies excluded from this review
Aadahl 2009 {published data only}
- Aadahl M, Huth Smith L, Toft U, Pisinger C, Jorgensen T. Does a population‐based multi‐factorial lifestyle intervention increase social inequality in physical activity? The Inter99 study. British Journal of Sports Medicine 2011;45(3):209‐15. [DOI] [PubMed] [Google Scholar]
Ackermann 2003 {published data only}
- Ackermann RT, Cheadle A, Sandhu N, Madsen L, Wagner EH, LoGerfo JP. Community exercise program use and changes in healthcare costs for older adults. American Journal of Preventive Medicine 2003;25(3):232‐7. [DOI] [PubMed] [Google Scholar]
Alcalay 1999 {published data only}
- Alcalay R, Alvarado M, Balcazar H, Newman E, Ortiz G. Evaluation of a community‐based Latino heart disease prevention program in metropolitan Washington D.C. International Quarterly of Community Health Education 1999;19(3):191‐204. [Google Scholar]
Alfonso 2011 {published data only}
- Alfonso ML, McDermott RJ, Thompson Z, Bryant CA, Courtney AH, Jones JA, et al. Vigorous physical activity among tweens, VERB Summer Scorecard program, Lexington, Kentucky, 2004‐2007. Preventing Chronic Disease 2011;8:A104. [PMC free article] [PubMed] [Google Scholar]
Aranceta 2013 {published data only}
- Aranceta Bartrina J, Perez Rodrigo C, Campos Amado J, Calderon Pascual V, Garcia Cuadra A, Gavidia Catalan V, et al. PERSEO project: Design and methods of the evaluation study. [Spanish]. Revista Espanola de Nutricion Comunitaria 2013;19(June):1‐10. [Google Scholar]
Austin 2006 {published data only}
- Austin EN, Johnston YA, Morgan LL. Community gardening in a senior center: a therapeutic intervention to improve the health of older adults. Therapeutic Recreation Journal 2006;40(1):48‐56. [Google Scholar]
Baker 2008 {published data only}
- Baker G, Gray SR, Wright A, Fitzsimons C, Nimmo M, Lowry R, et al. The effect of a pedometer‐based community walking intervention "Walking for Wellbeing in the West" on physical activity levels and health outcomes: A 12‐week randomized controlled trial. International Journal of Behavioral Nutrition and Physical Activity 2008;5:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
Balagopal 2008 {published data only}
- Balagopal P, Kamalamma N, Patel TG, Misra R. A community‐based diabetes prevention and management education program in a rural village in India. Diabetes Care 2008;31(6):1097‐104. [DOI] [PubMed] [Google Scholar]
Battram 2011 {published data only}
- Battram DS, Harvey B, Harris SB, Mandich G, Beynon C, He Brescia M. Families in action: A culturally and linguistically sensitive community‐based obesity prevention program for Latin‐Canadian children and their families. Canadian Journal of Diabetes.Conference: 2nd National Obesity Summit Montreal, QC Canada.Conference Start: 20110428 Conference End: 20110501.Conference Publication: (var.pagings) 2011;35:May. [Google Scholar]
Bauman 2001 {published data only}
- Bauman AE, Bellew B, Owen N, Vita P. Impact of an Australian mass media campaign targeting physical activity in 1998. American Journal of Preventive Medicine 2001;21(1):41‐7. [DOI] [PubMed] [Google Scholar]
Baxter 1997a {published data only}
- Baxter T, Milner P, Wilson K, Leaf M, Nicholl J, Freeman J, Cooper N. A cost effective, community based heart health promotion project in England: prospective comparative study. BMJ 1997;315(7108):582‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Baxter 1997b {published data only}
- Baxter AP, Milner PC, Hawkins S, Leaf S, Simpson C, Wilson KV, et al. The impact of heart health promotion on coronary heart disease lifestyle risk factors in schoolchildren: lessons learnt from a community‐based project. Public Health 1997;111:231‐7. [PubMed] [Google Scholar]
Beets 2013 {published data only}
- Beets MW, Huberty J, Beighle A. Systematic observation of physical activity in afterschool programs: preliminary findings from Movin' Afterschool intervention. Journal of Physical Activity & Health 2013;10:974‐81. [DOI] [PubMed] [Google Scholar]
Bennett 2006 {published data only}
- Bennett JA, Winters‐Stone K, Nail LM, Scherer J. Definitions of sedentary in physical‐activity‐intervention trials: A summary of the literature. Journal of Aging and Physical Activity 2006;14(4):456‐77. [DOI] [PubMed] [Google Scholar]
Berkowitz 2008 {published data only}
- Berkowitz JM, Huhman M, Nolin MJ. Did augmenting the VERB campaign advertising in select communities have an effect on awareness, attitudes, and physical activity?. American Journal of Preventive Medicine 2008;34(6 Suppl):257‐66. [DOI] [PubMed] [Google Scholar]
Berry 2013 {published data only}
- Berry DC, Neal M, Hall EG, McMurray RG, Schwartz TA, Skelly AH, et al. Recruitment and retention strategies for a community‐based weight management study for multi‐ethnic elementary school children and their parents. Public Health Nursing 2013;30:80‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bickmore 2013 {published data only}
- Bickmore TW, Schulman D, Sidner C. Automated interventions for multiple health behaviors using conversational agents. Patient Education and Counseling 2013;92:142‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bjaras 2001 {published data only}
- Bjaras G, Harberg LK, Sydhoff J, Ostenson CG. Walking campaign: a model for developing participation in physical activity? Experiences from three campaign periods of the Stockholm Diabetes Prevention Program (SDPP). Patient Education and Counseling 2001;42(1):9‐14. [DOI] [PubMed] [Google Scholar]
Blake 1987 {published data only}
- Blake SM, Caspersen CJ, Fruetel JR, Ringhofer KR, Pirie PL, Crow RS, et al. Process evaluation of a community‐based physical activity campaign: the Minnesota Heart Health Program experience. Health Education Research 1987;2(2):115‐21. [Google Scholar]
Blunt 2009 {published data only}
- Blunt GH, Magner MA. First steps in designing a community based physical activity program. Kentucky Newsletter for Health, Physical Education, Recreation & Dance 2009;45(1):12‐5. [Google Scholar]
Bopp 2008 {published data only}
- Bopp M, Fallon E. Community‐based interventions to promote increased physical activity: a primer. Applied Health Economics and Health Policy 2008;6(4):173‐87. [DOI] [PubMed] [Google Scholar]
Brown 1996 {published data only}
- Brown WJ, Lee C, Oyomopito R. Effectiveness of a bilingual heart health program for Greek‐Australian women. Health Promotion International 1996;11(2):117‐25. [Google Scholar]
Bryant 2010 {published data only}
- Bryant CA, Courtney AH, McDermott RJ, Alfonso ML, Baldwin JA, Nickelson J, et al. Promoting physical activity among youth through community‐based prevention marketing. Journal of School Health 2010;80:214‐24. [DOI] [PubMed] [Google Scholar]
Bull 2006 {published data only}
- Bull S, Eakin E, Reeves M, Kimberly R. Multi‐level support for physical activity and healthy eating. Journal of Advanced Nursing 2006;54(5):585‐93. [DOI] [PubMed] [Google Scholar]
Caballero 1998 {published data only}
- Caballero B, Davis S, Davis CE, Ethelbah B, Evans M, Lohman T, et al. Pathways: A school‐based program for the primary prevention of obesity in American Indian children. Journal of Nutritional Biochemistry 1998;9(9):535‐43. [DOI] [PMC free article] [PubMed] [Google Scholar]
Castro 2013 {published data only}
- Castro DC, Samuels M, Harman AE. Growing healthy kids: a community garden‐based obesity prevention program. American Journal of Preventive Medicine 2013;44 Suppl:9. [DOI] [PubMed] [Google Scholar]
Chan 2008 {published data only}
- Chan CB, Tudor‐Locke C. Real‐world evaluation of a community‐based pedometer intervention. Journal of Physical Activity and Health 2008;5(5):648‐64. [DOI] [PubMed] [Google Scholar]
Cheadle 2000 {published data only}
- Cheadle A, Sterling TD, Schmid TL, Fawcett SB. Promising community‐level indicators for evaluating cardiovascular health‐promotion programs. Health Education Research 2000;15(1):109‐16. [DOI] [PubMed] [Google Scholar]
Cheadle 2011 {published data only}
- Cheadle A, Bourcier E, Krieger J, Beery W, Smyser M, Vinh DV, et al. The impact of a community‐based chronic disease prevention initiative: evaluation findings from Steps to Health King County. Health Education & Behavior 2011;38:222‐30. [DOI] [PubMed] [Google Scholar]
Cheadle 2012 {published data only}
- Cheadle A, Rauzon S, Spring R, Schwartz PM, Gee S, Gonzalez E, et al. Kaiser Permanente's Community Health Initiative in Northern California: evaluation findings and lessons learned. American Journal of Health Promotion 2012;27:e59‐68. [DOI] [PubMed] [Google Scholar]
Chen 2005 {published data only}
- Chen W‐L, Cai C‐H, Huang T‐B, Yan Z‐S, Li B‐H, Li X‐G, et al. Evaluation of community intervention on cardiocerebrovascular disease in Guzhan town, Zhongshan city, Guangdong province. Chinese Journal of Clinical Rehabilitation 2005;9(37):124‐6. [Google Scholar]
Chen 2008 {published data only}
- Chen J‐E, Zhang L‐N, Zhang T, Cui J. Evaluation of effect of community intervention on chronic diseases. Chinese Journal of Natural Medicines 2008;10(3):179‐82. [Google Scholar]
Cheng 1998 {published data only}
- Cheng M, Qian L, Zhou N, Wang H, Chen S. Evaluation of effectiveness on health education intervention on health behaviors in rural population. Medicine and Society 1998;11:4. [Google Scholar]
Cheng 2009 {published data only}
- Cheng SP, Tsai TI, Lii YK, Yu S, Chou CL, Chen IJ. The effects of a 12‐week walking program on community‐dwelling older adults. Research Quarterly for Exercise and Sport 2009;80(3):524‐32. [DOI] [PubMed] [Google Scholar]
Chomitz 2010 {published data only}
- Chomitz VR, McGowan RJ, Wendel JM, Williams SA, Cabral HJ, King SE, et al. Healthy Living Cambridge Kids: a community‐based participatory effort to promote healthy weight and fitness. Obesity (Silver Spring) 2010;18 Suppl 1:S45‐53. [DOI] [PubMed] [Google Scholar]
Cochrane 2008 {published data only}
- Cochrane T, Davey RC. Increasing uptake of physical activity: a social ecological approach. Journal of the Royal Society of Health 2008;128(1):31‐40. [DOI] [PubMed] [Google Scholar]
Cohen 2013 {published data only}
- Cohen DA, Han B, Derose KP, Williamson S, Marsh T, McKenzie TL. Physical Activity in Parks: A randomized controlled trial using community engagement. American Journal of Preventive Medicine 2013;45:590‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Coitinho 2002 {published data only}
- Coitinho D, Monteiro CA, Popkin BM. What Brazil is doing to promote healthy diets and active lifestyles. Public Health Nutrition 2002;5(1A):263‐7. [DOI] [PubMed] [Google Scholar]
Craig 2006 {published data only}
- Craig CL, Tudor‐Locke C, Bauman A. Twelve‐month effects of Canada on the Move: a population‐wide campaign to promote pedometer use and walking. Health Education Research 2006;22(3):406‐13. [DOI] [PubMed] [Google Scholar]
Croker 2012 {published data only}
- Croker H, Lucas R, Wardle J. Cluster‐randomised trial to evaluate the 'Change for Life' mass media/ social marketing campaign in the UK. BMC Public Health 2012;12:404. [DOI] [PMC free article] [PubMed] [Google Scholar]
Currie 2001 {published data only}
- Currie JL, Develin ED. The Strollers Pramwalking Program: a community intervention aimed at increasing the physical activity level of mothers with young children. Health Promotion Journal of Australia 2000;10(1):57‐9. [Google Scholar]
Davis 2003 {published data only}
- Davis SM, Clay T, Smyth M, Gittelsohn J, Arviso V, Flint‐Wagner H, et al. Pathways curriculum and family interventions to promote healthful eating and physical activity in American Indian schoolchildren. Preventive Medicine 2003;37(6 Pt 2):24‐34. [DOI] [PMC free article] [PubMed] [Google Scholar]
DeBar 2009 {published data only}
- DeBar LL, Dickerson J, Clarke G, Stevens VJ, Ritenbaugh C, Aickin M. Using a website to build community and enhance outcomes in a group, multi‐component intervention promoting healthy diet and exercise in adolescents. Journal of Pediatric Psychology 2009;34(5):539‐50. [DOI] [PMC free article] [PubMed] [Google Scholar]
DeBate 2009 {published data only}
- DeBate RD, Baldwin JA, Thompson Z, Nickelson J, Alfonso ML, Bryant CA, et al. VERB™ Summer Scorecard: Findings from a multi‐level community‐based physical activity intervention for tweens. American Journal of Community Psychology 2009;44:363‐73. [DOI] [PubMed] [Google Scholar]
De Bourdeaudhuij, 2011 {published data only}
- Bourdeaudhuij SC, Simon C, Meester F, Lenthe F, Spittaels H, Lien N, et al. Are physical activity interventions equally effective in adolescents of low and high socio‐economic status (SES): results from the European Teenage project. Health Education Research 2011;26:119‐30. [DOI] [PubMed] [Google Scholar]
De Cocker 2008 {published data only}
- Cocker KA, Bourdeaudhuij IM, Cardon GM. The effect of pedometer use in combination with cognitive and behavioral support materials to promote physical activity. Patient Education and Counseling 2008;70(2):209‐14. [DOI] [PubMed] [Google Scholar]
Dishman 2005 {published data only}
- Dishman RK, Motl RW, Saunders R, Felton G, Ward DS, Dowda M, et al. Enjoyment mediates effects of a school‐based physical‐activity intervention. Medicine & Science in Sports & Exercise 2005;37(3):478‐87. [DOI] [PubMed] [Google Scholar]
Dollahite 1998 {published data only}
- Dollahite J, Hosig KW, White KA, Rodibaugh R, Holmes TM. Impact of a school‐based community intervention program on nutrition knowledge and food choices in elementary school children in the rural Arkansas Delta. Journal of Nutrition Education 1998;30(5):289‐301. [Google Scholar]
Dowse 1995 {published data only}
- Dowse GK, Gareeboo H, Alberti KG, Zimmet P, Tuomilehto J, Purran A, et al. Changes in population cholesterol concentrations and other cardiovascular risk factor levels after five years of the non‐communicable disease intervention programme in Mauritius. Mauritius Non‐communicable Disease Study Group.[see comment]. BMJ 1995;311(7015):1255‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Draper 2009 {published data only}
- Draper CE, Kolbe‐Alexander TL, Lambert EV. A retrospective evaluation of a community‐based physical activity health promotion program. Journal of Physical Activity and Health 2009;6(5):578‐88. [DOI] [PubMed] [Google Scholar]
Dubuy 2013 {published data only}
- Dubuy V, Cocker KA, Bourdeaudhuij IM, Maes L, Metsu P, Acker R, et al. '10 000 Steps Flanders': evaluation of the state‐wide dissemination of a physical activity intervention in Flanders. Health Educucation Research 2013;28:546‐51. [DOI] [PubMed] [Google Scholar]
Economos 2007 {published data only}
- Economos CD, Hyatt RR, Goldberg JP, Must A, Naumova EN, Collins JJ, et al. A community intervention reduces BMI z‐score in children: Shape Up Somerville first year results. Obesity 2007;15(5):1325‐36. [DOI] [PubMed] [Google Scholar]
Economos 2013 {published data only}
- Economos CD, Hyatt RR, Must A, Goldberg JP, Kuder J, Naumova EN, et al. Shape Up Somerville two‐year results: A community‐based environmental change intervention sustains weight reduction in children. Preventive Medicine 2013;57:322‐7. [DOI] [PubMed] [Google Scholar]
Egawa 2007 {published data only}
- Egawa Ki, Oida Y, Arao T, Matsuzuki H, Shirako M, Kasai W. [Efficacy of a community‐based weight reduction program to improve exercise and diet behavior in overweight adults]. Nippon Koshu Eisei Zasshi ‐ Japanese Journal of Public Health 2007;54(12):847‐56. [PubMed] [Google Scholar]
Eisenmann 2008 {published data only}
- Eisenmann JC, Gentile DA, Welk GJ, Callahan R, Strickland S, Walsh M, et al. SWITCH: rationale, design, and implementation of a community, school, and family‐based intervention to modify behaviors related to childhood obesity. BMC Public Health 2008;8:223. [DOI] [PMC free article] [PubMed] [Google Scholar]
Eliah 2008 {published data only}
- Eliah E, Shayo A, Gendo C, Courtright P, Theraney M, Lewallen S. Can VISION 2020 be implemented in rural government settings? Findings from two programmes in Tanzania. Tropical Medicine & International Health 2008;13(10):1284‐7. [DOI] [PubMed] [Google Scholar]
Englert 2004 {published data only}
- Englert HS, Diehl HA, Greenlaw RL. Rationale and design of the Rockford CHIP, a community‐based coronary risk reduction program: results of a pilot phase. Preventive Medicine 2004;38(4):432‐41. [DOI] [PubMed] [Google Scholar]
Estabrooks 2008 {published data only}
- Estabrooks PA, Bradshaw M, Dzewaltowski DA, Smith‐Ray RL. Determining the impact of Walk Kansas: applying a team‐building approach to community physical activity promotion. Annals of Behavioral Medicine 2008;36:1‐12. [DOI] [PubMed] [Google Scholar]
Fang 2003 {published data only}
- Fang XH, Wang WZ, Wu Sp, Li SZ, Cheng XM, Du XL, et al. Community intervention on hypertension and stroke. Chinese Journal of Epidemiology 2003;24(7):538‐41. [PubMed] [Google Scholar]
Fisher 2004 {published data only}
- Fisher KJ, Li F. A community‐based walking trial to improve neighborhood quality of life in older adults: a multilevel analysis. Annals of Behavioral Medicine 2004;28(3):186‐94. [DOI] [PubMed] [Google Scholar]
Fotu 2011 {published data only}
- Fotu KF, Millar L, Mavoa H, Kremer P, Moodie M, Snowdon W, et al. Outcome results for the Ma'alahi Youth Project, a Tongan community‐based obesity prevention programme for adolescents. Obesity Reviews 2011;12:41‐50. [DOI] [PubMed] [Google Scholar]
Fotu 2011a {published data only}
- Fotu KF, Moodie MM, Mavoa HM, Pomana S, Schultz JT, Swinburn BA. Process evaluation of a community‐based adolescent obesity prevention project in Tonga. BMC Public Health 2011;11:284‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
Frew 2014 {published data only}
- Frew EJ, Bhatti M, Win K, Sitch A, Lyon A, Pallan M, et al. Cost‐effectiveness of a community‐based physical activity programme for adults (Be Active) in the UK: an economic analysis within a natural experiment. British Journal of Sports Medicine 2014;48:207‐12. [DOI] [PubMed] [Google Scholar]
Futterman 2004 {published data only}
- Futterman R. Evaluation of a community‐based intervention to promote physical activity in youth: lessons from active winners. (Review). American Journal of Health Promotion 2004;19(2):148‐9. [DOI] [PubMed] [Google Scholar]
Gao 2008 {published data only}
- Gao Y, Griffiths S, Chan EYY. Community‐based interventions to reduce overweight and obesity in China: a systematic review of the Chinese and English literature. Journal of Public Health 2008;30(4):436‐48. [DOI] [PubMed] [Google Scholar]
Gesell 2013 {published data only}
- Gesell SB, Sommer EC, Lambert EW, Vides de Andrade AR, Whitaker L, Davis L, et al. Comparative effectiveness of after‐school programs to increase physical activity. Journal of Obesity 2013;2013:576821. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gorely 2009 {published data only}
- Gorely T, Nevill ME, Morris JG, Stensel DJ, Nevill A. Effect of a school‐based intervention to promote healthy lifestyles in 7‐11 year old children. International Journal of Behavioral Nutrition and Physical Activity 2009;6:5‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Grydeland 2013 {published data only}
- Grydeland M, Bergh I, Bjelland M, Lien N, Andersen L, Ommundsen Y, et al. Intervention effects on physical activity: the HEIA study ‐‐ a cluster randomized controlled trial. International Journal of Behavioral Nutrition and Physical Activity 2013;10:17‐29. [DOI] [PMC free article] [PubMed] [Google Scholar]
Guo 2007 {published data only}
- Guo SX, Sun F, XU SZ, Guo H, Niu Q, Zhang JY, et al. Effect evaluation of community‐based health education on patients with hypertension in Shihezi. Modern Preventive Medicine 2007;34(8):3530‐1. [Google Scholar]
Guo 2008 {published data only}
- Guo X‐Y, Guo Y‐H. An investigation on intervening physical exercise behavior of community inhabitants in Sichuan Province. Ruan Ke Xue 2008;22(5):86‐9. [Google Scholar]
Han 2003 {published data only}
- Han X, Wang M, Hou B. Study on efficacy of adult obesity after intervention in community in Anyang. Journal of Hygiene Research 2003;32(4):369‐71. [PubMed] [Google Scholar]
Herbert 2013 {published data only}
- Herbert PC, Lohrmann DK, Seo DC, Stright AD, Kolbe LJ. Effectiveness of the energize elementary school program to improve diet and exercise. Journal of School Health 2013;83:780‐6. [DOI] [PubMed] [Google Scholar]
Hillsdon 1995 {published data only}
- Hillsdon M, Thorogood M, Anstiss T, Morris J. Randomised controlled trials of physical activity promotion in free living populations: a review. Journal of Epidemiology and Community Health 1995;49(5):448‐53. [DOI] [PMC free article] [PubMed] [Google Scholar]
Huhman 2007 {published data only}
- Huhman ME, Potter LD, Duke JC, Judkins DR, Heitzler CD, Wong FL. Evaluation of a national physical activity intervention for children: VERM Campaign, 2002‐2004. American Journal of Preventive Medicine 2007;32(1):38‐43. [DOI] [PubMed] [Google Scholar]
Jason 1991 {published data only}
- Jason LA, Greiner BJ, Naylor K, Johnson SP, Egeren LV. A large‐scale, short‐term, media‐based weight loss program. American Journal of Health Promotion 1991;5(6):432‐7. [DOI] [PubMed] [Google Scholar]
Kamieneski 2000 {published data only}
- Kamieneski R, Brown CM, Mitchell C, Perrin KM, Dindial K. Health benefits achieved through the Seventh‐Day Adventist Wellness Challenge program. Alternative Therapies in Health and Medicine 2000;6(6):65‐9. [PubMed] [Google Scholar]
Kandula 2013 {published data only}
- Kandula, N. Translating a heart disease lifestyle intervention into the community. Ethnicity & Disease 2013;23:385‐6. [PubMed] [Google Scholar]
Kelder 1995 {published data only}
- Kelder SH, Perry CL, Lytle LA, Klepp KI. Community‐wide youth nutrition education: long‐term outcomes of the Minneota Heart Health Program. Health Education Research 1995;10(2):119‐31. [DOI] [PubMed] [Google Scholar]
Kimura 2013 {published data only}
- Kimura M, Moriyasu A, Kumagai S, Furuna T, Akita S, Kimura S, et al. Community‐based intervention to improve dietary habits and promote physical activity among older adults: a cluster randomized trial. BMC Geriatrics 2013;13:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
King 1995 {published data only}
- King AC, Haskell WL, Young DR, Oka RK, Stefanick ML. Long‐term effects of varying intensities and formats of physical activity on participation rates, fitness, and lipoproteins in men and women aged 50 to 65 years. Circulation 1995;91(10):2596‐604. [DOI] [PubMed] [Google Scholar]
King 1998 {published data only}
- King AC. How to promote physical activity in a community: research experiences from the US highlighting different community approaches. Patient Education and Counseling 1998;33(1 Suppl):3‐12. [DOI] [PubMed] [Google Scholar]
Kiyu 2006 {published data only}
- Kiyu A, Steinkuehler AA, Hashim J, Hall J, Lee PFS, Taylor R. Evaluation of the Healthy Village Program in Kapit District, Sarawak, Malaysia. Health Promotion International 2006;21(1):13‐8. [DOI] [PubMed] [Google Scholar]
Kogan 2013 {published data only}
- Kogan AC, Gonzalez J, Hart B, Halloran S, Thomason B, Levine M, et al. Be well: Results of a nutrition, exercise, and weight management intervention among at‐risk older adults. Journal of Applied Gerontology 2013;32(7):889‐901. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kremer 2011 {published data only}
- Kremer P, Waqa G, Vanualailai N, Schultz JT, Roberts G, Moodie M, et al. Reducing unhealthy weight gain in Fijian adolescents: results of the Healthy Youth Healthy Communities study. Obesity Reviews 2011;12:29‐40. [DOI] [PubMed] [Google Scholar]
Krishnan 2011 {published data only}
- Krishnan A, Ekowati R, Baridalyne N, Kusumawardani N, Suhardi, Kapoor SK, et al. Evaluation of community‐based interventions for non‐communicable diseases: experiences from India and Indonesia. Health Promotion International 2011;26:276‐89. [DOI] [PubMed] [Google Scholar]
Larkin 2003 {published data only}
- Larkin M. Can cities be designed to fight obesity? Urban planners and health experts work to get people up and about. Lancet 2003;362(9389):1046‐7. [DOI] [PubMed] [Google Scholar]
Lawlor 2003 {published data only}
- Lawlor DA, Ness AR, Cope AM, Davis A, Insall P, Riddoch C. The challenges of evaluating environmental interventions to increase population levels of physical activity: the case of the UK National Cycle Network. Journal of Epidemiology and Community Health 2003;57(2):96‐101. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lee 2004 {published data only}
- Lee SW, Mancuso CA, Charlson ME. Prospective study of new participants in a community‐based mind‐body training program. Journal of General Internal Medicine 2004;19(7):760‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Lee 2007 {published data only}
- Lee L‐L, Arthur A, Avis M. Evaluating a community‐based walking intervention for hypertensive older people in Taiwan: a randomized controlled trial.[see comment]. Preventive Medicine 2007;44(2):160‐6. [DOI] [PubMed] [Google Scholar]
Lee 2008a {published data only}
- Lee KSK, Conigrave KM, Clough AR, Wallace C, Silins E, Rawles J. Evaluation of a community‐driven preventive youth initiative in Arnhem Land, Northern Territory, Australia. Drug & Alcohol Review 2008;27(1):75‐82. [DOI] [PubMed] [Google Scholar]
Lee 2008b {published data only}
- Lee LL, Arthur A, Avis M. Effect of a community walking intervention on exercise self‐efficacy among older people: A randomized controlled trial. Journal of Aging and Physical Activity 2008;16:S18. [Google Scholar]
Li 2002 {published data only}
- Li LM, Hu YH, Cao WH, Zhan ST, Li J, Wu T, et al. The community‐based comprehensive prevention and control for hypertention in China. Journal of Peking University (Health Science) 2002;34(5):519‐24. [Google Scholar]
Li 2008 {published data only}
- Li G, Zhang P, Wang J, Gregg EW, Yang W, Gong Q, et al. The long‐term effect of lifestyle interventions to prevent diabetes in the China Da Qing Diabetes Prevention Study: a 20‐year follow‐up study [see comment]. Lancet 2008;371(9626):1783‐9. [DOI] [PubMed] [Google Scholar]
Lindstrom 2003 {published data only}
- Lindstrom J, Louheranta A, Mannelin M, Rastas M, Salminen V, Eriksson J, et al. The Finnish Diabetes Prevention Study (DPS): Lifestyle intervention and 3‐year results on diet and physical activity. Diabetes Care 2003;26(12):3230‐6. [DOI] [PubMed] [Google Scholar]
Lyle 2008 {published data only}
- Lyle D, Hobba J, Lloyd K, Bennett D, George T, Giddings N, et al. Mobilising a rural community to lose weight: Impact evaluation of the WellingTonne Challenge. Australian Journal of Rural Health 2008;16:80‐5. [DOI] [PubMed] [Google Scholar]
Maddock 2005 {published data only}
- Maddock J, Takeuchi L, Nett B, Tanaka C, Irvin L, Matsuoka C, Wood B. Evaluation of a statewide program to reduce chronic disease: The Healthy Hawaii Initiative, 2000‐2004. Evaluation and Program Planning 2006;29(3):293‐300. [Google Scholar]
Madsen 2013 {published data only}
- Madsen K, Thompson H, Adkins A, Crawford Y. School‐community partnerships: a cluster‐randomized trial of an after‐school soccer program. JAMA Pediatrics 2013;167:321‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Malmgren 1986 {published data only}
- Malmgren S, Andersson G. Who were reached by and participated in a one year newspaper health information campaign. Scandinavian Journal of Social Medicine 1986;14:133‐40. [DOI] [PubMed] [Google Scholar]
Marshall 2004 {published data only}
- Marshall AL, Bauman AE, Owen N, Booth ML, Crawford D, Marcus BH. Reaching out to promote physical activity in Australia: a statewide randomized controlled trial of a stage‐targeted intervention. American Journal of Health Promotion 2004;18(4):283‐7. [DOI] [PubMed] [Google Scholar]
Matsudo 2002 {published data only}
- Matsudo V, Matsudo S, Andrade D, Araujo T, Andrade E, Oliveira LC, et al. Promotion of physical activity in a developing country: the Agita Sao Paulo experience. Public Health Nutrition 2002;5(1A):253‐61. [DOI] [PubMed] [Google Scholar]
Matsudo 2003 {published data only}
- Matsudo SM, Matsudo VR, Araujo TL, Andrade DR, Andrade EL, Oliveira LC, et al. The Agita Sao Paulo Program as a model for using physical activity to promote health. Pan American Journal of Public Health 2003;14(4):265‐72. [DOI] [PubMed] [Google Scholar]
McDermott 2010 {published data only}
- McDermott RJ, Davis JL, Bryant CA, Courtney AH, Alfonso ML. Increasing physical activity in children 8 to 12 years old: experiences with VERB Summer Scorecard. Perceptual & Motor Skills 2010;111:240‐8. [DOI] [PubMed] [Google Scholar]
Merom 2005 {published data only}
- Merom D, Miller Y, Lymer S, Bauman A. Effect of Australia's Walk to Work Day Campaign on adults' active community and physical activity behavior. American Journal of Health Promotion 2005;19(3):159‐62. [DOI] [PubMed] [Google Scholar]
Meyer 1980 {published data only}
- Meyer AJ, Nash JD, McAlister AC, Maccoby N, Farquhar JW. Skills training in a cardiovascular health education campaign. Journal of Consulting and Clinical Psychology 1980;48:129‐42. [DOI] [PubMed] [Google Scholar]
Millar 2011 {published data only}
- Millar L, Kremer P, Silva‐Sanigorski A, McCabe MP, Mavoa H, Moodie M, et al. Reduction in overweight and obesity from a 3‐year community‐based intervention in Australia: the 'It's Your Move!' project. Obesity Reviews 2011;12 Suppl:8. [DOI] [PubMed] [Google Scholar]
Millar 2013 {published data only}
- Millar L, Robertson N, Allender S, Nichols M, Bennett C, Swinburn B. Increasing community capacity and decreasing prevalence of overweight and obesity in a community based intervention among Australian adolescents. Preventive Medicine 2013;56:379‐84. [DOI] [PubMed] [Google Scholar]
Mohan 2006 {published data only}
- Mohan V, Shanthirani CS, Deepa M, Datta M, Williams OD, Deepa R. Community empowerment‐‐a successful model for prevention of non‐communicable diseases in India‐‐the Chennai Urban Population Study (CUPS‐17). Journal of the Association of Physicians of India 2006;54:858‐62. [PubMed] [Google Scholar]
Muntoni 1999 {published data only}
- Muntoni S, Stabilini L, Stabilini M, Muntoni S. Results of a five‐year community‐based programme for cardiovascular disease prevention: The ATS‐Sardegna Campaign. European Journal of Epidemiology 1999;15(1):29‐34. [DOI] [PubMed] [Google Scholar]
Napolitano 2006 {published data only}
- Napolitano MA, Lerch H, Papandonatos G, Marcus BH. Worksite and communications‐based promotion of a local walking path. Journal of Community Health 2006;31(4):326‐42. [DOI] [PubMed] [Google Scholar]
Nickelson 2011 {published data only}
- Nickelson J, Alfonso ML, McDermott RJ, Bumpus EC, Bryant CA, Baldwin JA. Characteristics of 'tween' participants and non‐participants in the VERB summer scorecard physical activity promotion program. Health Education Research 2011;26:225‐38. [DOI] [PubMed] [Google Scholar]
Niederer 2009 {published data only}
- Niederer I, Kriemler S, Zahner L, Bürgi F, Ebenegger V, Hartmann T, et al. Influence of a lifestyle intervention in preschool children on physiological and psychological parameters (Ballabeina): study design of a cluster randomized controlled trial. BMC Public Health 2009;9:94‐104. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ogilvie 2014 {published data only}
- Ogilivie D. Health impacts of the Cambridgeshire Guided Busway: in progress. http://www.nets.nihr.ac.uk/projects/phr/09300106 2014. [PubMed]
Owen 1987 {published data only}
- Owen N, Lee C, Naccarella L, Haag K. Exercise by mail: a mediated behavior‐change program for aerobic exercise. Journal of Sport Psychology 1987;9:346‐57. [Google Scholar]
Pabayo 2010 {published data only}
- Pabayo R, Gauvin L, Barnett TA, Nikiéma B, Séguin L. Sustained active transportation is associated with a favorable body mass index trajectory across the early school years: Findings from the Quebec Longitudinal Study of Child Development birth cohort. Preventive Medicine 2010;50 Suppl 1:59‐64. [DOI] [PubMed] [Google Scholar]
Pekmezi 2009 {published data only}
- Pekmezi DW, Neighbors CJ, Lee CS, Gans KM, Bock BC, Morrow KM, et al. A culturally adapted physical activity intervention for Latinas: A randomized controlled trial. American Journal of Preventive Medicine 2009;37(6):495‐500. [DOI] [PMC free article] [PubMed] [Google Scholar]
Phelan 2002 {published data only}
- Phelan EA, Williams B, Leveille S, Snyder S, Wagner EH, LoGerfo JP. Outcomes of a community‐based dissemination of the health enhancement program. Journal of the American Geriatrics Society 2002;50(9):1519‐24. [DOI] [PubMed] [Google Scholar]
Plescia 2008 {published data only}
- Plescia M, Herrick H, Chavis L. Improving health behaviors in an African American community: the Charlotte Racial and Ethnic Approaches to Community Health Project. American Journal of Public Health 2008;98(9):1678‐84. [DOI] [PMC free article] [PubMed] [Google Scholar]
Pucher 2003 {published data only}
- Pucher J, Dijkstra L. Promoting safe walking and cycling to improve public health: lessons from The Netherlands and Germany. American Journal of Public Health 2003;93(9):1509‐16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Puoane 2006 {published data only}
- Puoane T, Bradley H, Hughes G. Community intervention for the emerging epidemic of non‐communicable diseases. South African Journal of Clinical Nutrition 2006;19(2):56‐62. [Google Scholar]
Quan 2006 {published data only}
- Quan SC, Wang SF, Chen RX, Pan JY. The community comprehensive prevention and control on hypertension risk factors in Songtal community of Wenzhou. Journal of Medical Research 2006;35(10):59‐61. [Google Scholar]
Reger 2002 {published data only}
- Reger B, Cooper L, Booth‐Butterfield S, Smith H, Bauman A, Wootan M, et al. Wheeling Walks: a community campaign using paid media to encourage walking among sedentary older adults. Preventive Medicine 2002;35(3):285‐92. [DOI] [PubMed] [Google Scholar]
Reger‐Nash 2006 {published data only}
- Reger‐Nash B, Fell P, Spicer D, Fisher BD, Cooper L, Chey T, et al. BC Walks: replication of a communitywide physical activity campaign. Preventing Chronic Disease 2006;3(3):A90. [PMC free article] [PubMed] [Google Scholar]
Renger 2002 {published data only}
- Renger R, Steinfelt V, Lazarus S. Assessing the effectiveness of a community‐based media campaign targeting physical inactivity. Family & Community Health 2002;25(3):18‐30. [DOI] [PubMed] [Google Scholar]
Rhoades 2001 {published data only}
- Rhoades R, Beebe L, Jones W. Physicians' campaign for a healthier Oklahoma. Evaluation of the schools for healthy lifestyles: program overview and baseline results. Journal ‐ Oklahoma State Medical Association 2001;94(9):412‐8. [PubMed] [Google Scholar]
Rodrigues 2006 {published data only}
- Rodrigues AN, Moyses MR, Bissoli NS, Pires JGP, Abreu GR. Cardiovascular risk factors in a population of Brazilian schoolchildren. Brazilian Journal of Medical & Biological Research 2006;39(12):1637‐42. [DOI] [PubMed] [Google Scholar]
Roman 2008 {published data only}
- Roman CG, Chalfin A. Fear of walking outdoors. A multilevel ecologic analysis of crime and disorder. American Journal of Preventive Medicine 2008;34(4):306‐12. [DOI] [PubMed] [Google Scholar]
Ronda 2004 {published data only}
- Ronda G, Assema P, Candel M, Ruland E, Steenbakkers M, Ree J, et al. The Dutch Heart Health community intervention 'Hartslag Limburg': results of an effect study at individual level. Health Promotion International 2004;19(1):21‐31. [DOI] [PubMed] [Google Scholar]
Ronda 2004a {published data only}
- Ronda G, van AP, Ruland E, Steenbakkers M, Brug J. The Dutch Heart Health Community Intervention 'Hartslag Limburg': Design and results of a process study. Health Education Research 2004;19(5):596‐607. [DOI] [PubMed] [Google Scholar]
Ronda 2005 {published data only}
- Ronda G, Assema P, Ruland E, Steenbakkers M, Ree J, Brug J. The Dutch heart health community intervention 'Hartslag Limburg': results of an effect study at organizational level. Public Health 2005;119(5):353‐60. [DOI] [PubMed] [Google Scholar]
Rooney 2008 {published data only}
- Rooney B, Hooks T, Baciak K, Havens S, Gilles H. Minutes in motion: motivating a community to move. WMJ 2008;107(3):118‐23. [PubMed] [Google Scholar]
Ross 2009 {published data only}
- Ross J. Promoting active lifestle in New Zealand. www.icsspe.org/portalindex.php?w=1&z=5 (acccesed 2/11/2009).
Roux 2008 {published data only}
- Roux L, Pratt M, Tengs TO, Yore MM, Yanagawa TL, Bos J, et al. Cost effectiveness of community‐based physical activity interventions. American Journal of Preventive Medicine 2008;35(6):578‐88. [DOI] [PubMed] [Google Scholar]
Sallis 2003 {published data only}
- Sallis JF, McKenzie TL, Conway TL, Elder JP, Prochaska JJ, Brown M, et al. Environmental interventions for eating and physical activity: a randomized controlled trial in middle schools. American Journal of Preventive Medicine 2003;24(3):209‐17. [DOI] [PubMed] [Google Scholar]
Salmon 2011 {published data only}
- Salmon J, Arundell L, Hume C, Brown H, Hesketh K, Dunstan D, et al. A cluster‐randomized controlled trial to reduce sedentary behavior and promote physical activity and health of 8‐9 year olds: The Transform‐Us! Study. BMC Public Health 2011;11:759. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sarrafzadegan 2013 {published data only}
- Sarrafzadegan N, Kelishadi R, Sadri G, Malekafzali H, Pourmoghaddas M, Heidari K, et al. Outcomes of a comprehensive healthy lifestyle program on cardiometabolic risk factors in a developing country: the Isfahan Healthy Heart Program. Archives of Iranian Medicine 2013;16:4‐11. [PubMed] [Google Scholar]
Sayers 2012 {published data only}
- Sayers SP, LeMaster JW, Thomas IM, Petroski GF, Ge B. Bike, walk, and wheel: a way of life in Columbia, Missouri, revisited. American Journal of Preventive Medicine 2012;43 Suppl:83. [DOI] [PubMed] [Google Scholar]
Sevick 2000 {published data only}
- Sevick MA, Bradham DD, Muender M, Chen GJ, Enarson C, Dailey M, et al. Cost‐effectiveness of aerobic and resistance exercise in seniors with knee osteoarthritis. Medicine & Science in Sports & Exercise 2000;32(9):1534‐40. [DOI] [PubMed] [Google Scholar]
Sevick 2007 {published data only}
- Sevick MA, Napolitano MA, Papandonatos GD, Gordon AJ, Reiser LM, Marcus BH. Cost‐effectiveness of alternative approaches for motivating activity in sedentary adults: results of Project STRIDE. Preventive Medicine 2007;45(1):54‐61. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shea 1996 {published data only}
- Shea S, Basch CE, Wechsler H, Lantigua R. The Washington Heights‐Inwood Healthy Heart Program: a 6‐year report from a disadvantaged urban setting. American Journal of Public Health 1996;86(2):166‐71. [DOI] [PMC free article] [PubMed] [Google Scholar]
Shen 2007 {published data only}
- Shen Y, Yu S, Cui M, Shen Q, Qi X. Health education and health promotion affecting farmers' health in rural communities. Chinese Rural Health Service Administration 2007;27(8):603‐6. [Google Scholar]
Simmons 1998 {published data only}
- Simmons D, Fleming C, Voyle J, Fou F, Feo S, Gatland B. A pilot urban church‐based programme to reduce risk factors for diabetes among Western Samoans in New Zealand. Diabetic Medicine 1998;15(2):136‐42. [DOI] [PubMed] [Google Scholar]
Simmons 2004 {published data only}
- Simmons D, Voyle JA, Fou F, Feo S, Leakehe L. Tale of two churches: differential impact of a church‐based diabetes control programme among Pacific Islands people in New Zealand. Diabetic Medicine 2004;21(2):122‐8. [DOI] [PubMed] [Google Scholar]
Simmons 2008 {published data only}
- Simmons D, Rush E, Crook N, Wai o Rona: Diabetes Prevention Strategy T. Development and piloting of a community health worker‐based intervention for the prevention of diabetes among New Zealand Maori in Te Wai o Rona: Diabetes Prevention Strategy. Public Health Nutrition 2008;11(12):1318‐25. [DOI] [PubMed] [Google Scholar]
Simoes 2009 {published data only}
- Simoes EJ, Hallal P, Pratt M, Ramos L, Munk M, Damascena W, et al. Effects of a community‐based, professionally supervised intervention on physical activity levels among residents of Recife, Brazil. American Journal of Public Health 2009;99(1):68‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
Simons‐Morton 1998 {published data only}
- Simons‐Morton DG, Calfas KJ, Oldenburg B, Burton NW. Effects of interventions in health care settings on physical activity or cardiorespiratory fitness. American Journal of Preventive Medicine 1998;15(4):413‐30. [DOI] [PubMed] [Google Scholar]
Sinclair 2007 {published data only}
- Sinclair KM, Hamlin MJ. Self‐reported health benefits in patients recruited into New Zealand's 'Green Prescription' primary health care program. Southeast Asian Journal of Tropical Medicine & Public Health 2007;38(6):1158‐67. [PubMed] [Google Scholar]
Singh 2006 {published data only}
- Singh AS, Chin A Paw MJM, Kremers SPJ, Visscher TLS, Brug J, Mechelen W. Design of the Dutch Obesity Intervention in Teenagers (NRG‐DOiT): systematic development, implementation and evaluation of a school‐based intervention aimed at the prevention of excessive weight gain in adolescents. BMC Public Health 2006;6:304. [DOI] [PMC free article] [PubMed] [Google Scholar]
Singh 2009 {published data only}
- Singh AS, Chin A Paw MJM, Brug J, Mechelen W. Dutch obesity intervention in teenagers: effectiveness of a school‐based program on body composition and behavior [see comment]. Archives of Pediatrics & Adolescent Medicine 2009;163(4):309‐17. [DOI] [PubMed] [Google Scholar]
Slootmaker 2005 {published data only}
- Slootmaker SM, Chin A Paw MJM, Schuit AJ, Seidell JC, Mechelen W. Promoting physical activity using an activity monitor and a tailored web‐based advice: design of a randomized controlled trial [ISRCTN93896459]. BMC Public Health 2005;5:134. [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2000 {published data only}
- Smith BJ, Bauman AE, Bull FC, Booth ML, Harris MF. Promoting physical activity in general practice: a controlled trial of written advice and information materials. British Journal of Sports Medicine 2000;34(4):262‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Smith 2002 {published data only}
- Smith CE, Ross EM. PACE: evaluating its use in the primary care setting. Nutrition in Clinical Care 2002;5(3):133‐5. [DOI] [PubMed] [Google Scholar]
Smith 2004 {published data only}
- Smith BJ. Promotion of physical activity in primary health care: update of the evidence on interventions. Journal of Science and Medicine in Sport 2004;7(1 Suppl):67‐73. [DOI] [PubMed] [Google Scholar]
Smolander 2000 {published data only}
- Smolander J, Blair SN, Kohl HW 3rd. Work ability, physical activity, and cardiorespiratory fitness: 2‐year results from Project Active. Journal of Occupational and Environmental Medicine 2000;42(9):906‐10. [DOI] [PubMed] [Google Scholar]
Sorensen 2005 {published data only}
- Sorensen G, Barbeau E, Stoddard AM, Hunt MK, Kaphingst K, Wallace L. Promoting behavior change among working‐class, multiethnic workers: results of the healthy directions‐‐small business study. American Journal of Public Health 2005;95(8):1389‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sorensen 2006 {published data only}
- Sorensen JB, Skovgaard T, Puggaard L. Exercise on prescription in general practice: a systematic review. Scandinavian Journal of Primary Health Care 2006;24(2):69‐74. [DOI] [PubMed] [Google Scholar]
Speck 2007 {published data only}
- Speck BJ, Hines‐Martin V, Stetson BA, Looney SW. An environmental intervention aimed at increasing physical activity levels in low‐income women. Journal of Cardiovascular Nursing 2007;22(4):263‐71. [DOI] [PubMed] [Google Scholar]
Spink 2008 {published data only}
- Spink KS, Reeder B, Chad K, Wilson K, Nickel D. Examining physician counselling to promote the adoption of physical activity. Canadian Journal of Public Health Revue Canadienne de Sante Publique 2008;99(1):26‐30. [DOI] [PMC free article] [PubMed] [Google Scholar]
Spittaels 2007 {published data only}
- Spittaels H, Bourdeaudhuij I, Vandelanotte C. Evaluation of a website‐delivered computer‐tailored intervention for increasing physical activity in the general population. Preventive Medicine 2007;44(3):209‐17. [DOI] [PubMed] [Google Scholar]
Spruijt‐Metz 2008 {published data only}
- Spruijt‐Metz D, Nguyen‐Michel ST, Goran MI, Chou C‐P, Huang TTK. Reducing sedentary behavior in minority girls via a theory‐based, tailored classroom media intervention. International Journal of Pediatric Obesity 2008;3(4):240‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stamm 2001 {published data only}
- Stamm H, Lamprecht M, Somaini B, Peters M. "Getting Switzerland to move": evaluation of a new "Sport for All" programme. Sozial‐ und Praventivmedizin 2001;46(1):20‐8. [DOI] [PubMed] [Google Scholar]
Stanton 1997 {published data only}
- Stanton B, Fang X, Li X, Feigelman S, Galbraith J, Ricardo I. Evolution of risk behaviors over 2 years among a cohort of urban African American adolescents. Archives of Pediatrics & Adolescent Medicine 1997;151(4):398‐406. [DOI] [PubMed] [Google Scholar]
Staten 2004 {published data only}
- Staten LK, Gregory‐Mercado KY, Ranger‐Moore J, Will JC, Giuliano AR, Ford ES, et al. Provider counseling, health education, and community health workers: the Arizona WISEWOMAN project. Journal of Women's Health 2004;13(5):547‐56. [DOI] [PubMed] [Google Scholar]
Staten 2005 {published data only}
- Staten LK, Scheu LL, Bronson D, Pena V, Elenes J. Pasos Adelante: the effectiveness of a community‐based chronic disease prevention program. Preventing Chronic Disease 2005;2(1):A18. [PMC free article] [PubMed] [Google Scholar]
Staunton 2003 {published data only}
- Staunton CE, Hubsmith D, Kallins W. Promoting safe walking and biking to school: the Marin County success story. American Journal of Public Health 2003;93(9):1431‐4. [DOI] [PMC free article] [PubMed] [Google Scholar]
Steckler 2003 {published data only}
- Steckler A, Ethelbah B, Martin CJ, Stewart D, Pardilla M, Gittelsohn J, et al. Pathways process evaluation results: a school‐based prevention trial to promote healthful diet and physical activity in American Indian third, fourth, and fifth grade students. Preventive Medicine 2003;37(6 Pt 2):S80‐90. [DOI] [PubMed] [Google Scholar]
Steele 2007 {published data only}
- Steele R, Mummery WK, Dwyer T. Using the Internet to promote physical activity: a randomized trial of intervention delivery modes. Journal of Physical Activity and Health 2007;4(3):245‐60. [DOI] [PubMed] [Google Scholar]
Steptoe 1999 {published data only}
- Steptoe A, Doherty S, Rink E, Kerry S, Kendrick T, Hilton S. Behavioural counselling in general practice for the promotion of healthy behaviour among adults at increased risk of coronary heart disease: randomised trial.[see comment]. BMJ 1999;319(7215):943‐7; discussion 947‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Steptoe 2000 {published data only}
- Steptoe A, Rink E, Kerry S. Psychosocial predictors of changes in physical activity in overweight sedentary adults following counseling in primary care. Preventive Medicine 2000;31(2 Pt 1):183‐94. [DOI] [PubMed] [Google Scholar]
Steptoe 2001 {published data only}
- Steptoe A, Kerry S, Rink E, Hilton S. The impact of behavioral counseling on stage of change in fat intake, physical activity, and cigarette smoking in adults at increased risk of coronary heart disease. American Journal of Public Health 2001;91(2):265‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Sternberg 2006 {published data only}
- Sternberg A, Muzumdar H, Dinkevich E, Quintos JB, Austin‐Leon G, Owens T, et al. The Downstart Program: a hospital‐based pediatric healthy lifestyle program for obese and morbidly obese minority youth. Pediatric Endocrinology Reviews 2006;3 Suppl 4:584‐9. [PubMed] [Google Scholar]
Sternfeld 2009 {published data only}
- Sternfeld B, Block C, Quesenberry CP Jr, Block TJ, Husson G, Norris JC, et al. Improving diet and physical activity with ALIVE: a worksite randomized trial. American Journal of Preventive Medicine 2009;36(6):475‐83. [DOI] [PubMed] [Google Scholar]
Stevens 1998 {published data only}
- Stevens W, Hillsdon M, Thorogood M, McArdle D. Cost‐effectiveness of a primary care based physical activity intervention in 45‐74 year old men and women: a randomised controlled trial.[see comment]. British Journal of Sports Medicine 1998;32(3):236‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stevens 1999 {published data only}
- Stevens M, Bult P, Greef MH, Lemmink KA, Rispens P. Groningen Active Living Model (GALM): stimulating physical activity in sedentary older adults. Preventive Medicine 1999;29(4):267‐76. [DOI] [PubMed] [Google Scholar]
Stevens 2005 {published data only}
- Stevens J, Murray DM, Catellier DJ, Hannan PJ, Lytle LA, Elder JP, et al. Design of the Trial of Activity in Adolescent Girls (TAAG). Contemporary Clinical Trials 2005;26(2):223‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stewart 2001 {published data only}
- Stewart AL, Verboncoeur CJ, McLellan BY, Gillis DE, Rush S, Mills KM, et al. Physical activity outcomes of CHAMPS II: a physical activity promotion program for older adults. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 2001;56(8):M465‐70. [DOI] [PMC free article] [PubMed] [Google Scholar]
Stewart 2004 {published data only}
- Stewart JA, Dennison DA, Kohl HW, Doyle JA. Exercise level and energy expenditure in the TAKE 10! in‐class physical activity program. Journal of School Health 2004;74(10):397‐400. [DOI] [PubMed] [Google Scholar]
Stewart 2006 {published data only}
- Stewart AL, Gillis D, Grossman M, Castrillo M, Pruitt L, McLellan B, et al. Diffusing a research‐based physical activity promotion program for seniors into diverse communities: CHAMPS III. Preventing Chronic Disease 2006;3(2):A51. [PMC free article] [PubMed] [Google Scholar]
Stock 2007 {published data only}
- Stock S, Miranda C, Evans S, Plessis S, Ridley J, Yeh S, et al. Healthy Buddies: a novel, peer‐led health promotion program for the prevention of obesity and eating disorders in children in elementary school. Pediatrics 2007;120(4):e1059‐68. [DOI] [PubMed] [Google Scholar]
Stone 1996 {published data only}
- Stone EJ, Osganian SK, McKinlay SM, Wu MC, Webber LS, Luepker RV, et al. Operational design and quality control in the CATCH multicenter Trial. Preventive Medicine 1996;25(4):384‐99. [DOI] [PubMed] [Google Scholar]
Stone 1998 {published data only}
- Stone EJ, McKenzie TL, Welk GJ, Booth ML. Effects of physical activity interventions in youth. Review and synthesis. American Journal of Preventive Medicine 1998;15(4):298‐315. [DOI] [PubMed] [Google Scholar]
Strachan 2007 {published data only}
- Strachan G, Wright G, Hancock E. An evaluation of a community health intervention programme aimed at improving health and wellbeing. Health Education Journal 2007;66(5):277‐85. [Google Scholar]
Stubbs 2002 {published data only}
- Stubbs J, Giles‐Corti B, Engelhard S, Milat AJ. Promoting participation in physical activity in a community intervention study. Health Promotion Journal of Australia 2002;13(3):205‐10. [Google Scholar]
Sugden 2008 {published data only}
- Sugden JA, Sniehotta FF, Donnan PT, Boyle P, Johnston DW, McMurdo MET. The feasibility of using pedometers and brief advice to increase activity in sedentary older women‐‐a pilot study. BMC Health Services Research 2008;8:169. [DOI] [PMC free article] [PubMed] [Google Scholar]
Suminski 2009 {published data only}
- Suminski RR, Petosa RL, Jones L, Hall L, Poston CW. Neighborhoods on the move: a community‐based participatory research approach to promoting physical activity. Progress in community health partnerships : research, education, and action 2009;3:19‐29. [DOI] [PubMed] [Google Scholar]
Sun 2007 {published data only}
- Sun F, Guo SX, Zhang JY, Niu Q, Guo H, XU SZ, et al. Evaluation of the effects of intervention of knowledge, attitudes and behaviors about hypertension in communities of Shihezi. Modern Preventive Medicine 2007;34(19):3717‐9. [Google Scholar]
Swinburn 2011 {published data only}
- Swinburn BA, Millar L, Utter J, Kremer P, Moodie M, Mavoa H, et al. The Pacific Obesity Prevention in Communities project: project overview and methods. Obes Rev 2011;12 Suppl 2:3‐11. [DOI] [PubMed] [Google Scholar]
Tan 2006 {published data only}
- Tan EJ, Xue Q‐L, Li T, Carlson MC, Fried LP. Volunteering: a physical activity intervention for older adults‐‐The Experience Corps program in Baltimore. Journal of Urban Health 2006;83(5):954‐69. [DOI] [PMC free article] [PubMed] [Google Scholar]
TenBrink 2009 {published data only}
- TenBrink DS, McMunn R, Panken S. Project U‐Turn: Increasing Active Transportation in Jackson, Michigan. American Journal of Preventive Medicine 2009;37(6 Suppl 2):329‐35. [DOI] [PubMed] [Google Scholar]
Thomas 2009 {published data only}
- Thomas IM, Sayers SP, Godon JL, Reilly SR. Bike, walk, and wheel: a way of life in Columbia, Missouri. American Journal of Preventive Medicine 2009;37:S322‐8. [DOI] [PubMed] [Google Scholar]
Timperio 2004 {published data only}
- Timperio A, Salmon J, Ball K. Evidence‐based strategies to promote physical activity among children, adolescents and young adults: review and update. Journal of Science and Medicine in Sport 2004;7(1 Suppl):20‐9. [DOI] [PubMed] [Google Scholar]
Toftager 2011 {published data only}
- Toftager M, Christiansen L, Kristensen P, Troelsen J. SPACE for physical activity ‐ a multicomponent intervention study: study design and baseline findings from a cluster randomized controlled trial. BMC Public Health 2011;11:777. [DOI] [PMC free article] [PubMed] [Google Scholar]
Togami 2008 {published data only}
- Togami T. Interventions in local communities and work sites through physical activity and nutrition programme. Obesity Reviews 2008;9 Suppl 1:127‐9. [DOI] [PubMed] [Google Scholar]
Tsai 2009 {published data only}
- Tsai P‐Y, Boonpleng W, McElmurry BJ, Park CG, McCreary L. Lessons learned in using TAKE 10! with Hispanic children. Journal of School Nursing 2009;25(2):163‐72. [DOI] [PubMed] [Google Scholar]
Tsorbatzoudis 2005 {published data only}
- Tsorbatzoudis H. Evaluation of a school‐based intervention programme to promote physical activity: an application of the theory of planned behavior. Perceptual and Motor Skills 2005;101(3):787‐802. [DOI] [PubMed] [Google Scholar]
Tudor‐Smith 1998 {published data only}
- Tudor‐Smith C, Nutbeam D, Moore L, Catford J. Effects of the Heartbeat Wales programme over five years on behavioural risks for cardiovascular disease: quasi‐experimental comparison of results from Wales and a matched reference area [see comment]. BMJ 1998;316(7134):818‐22. [DOI] [PMC free article] [PubMed] [Google Scholar]
Tully 2007 {published data only}
- Tully MA, Cupples ME, Young IS. Evaluating a community‐based walking intervention for hypertensive older people in Taiwan: a randomized controlled trial [comment]. Preventive Medicine 2007;44(5):466. [DOI] [PubMed] [Google Scholar]
Two Feathers 2005 {published data only}
- Two Feathers J, Kieffer EC, Palmisano G, Anderson M, Sinco B, Janz N, et al. Racial and Ethnic Approaches to Community Health (REACH) Detroit partnership: improving diabetes‐related outcomes among African American and Latino adults. American Journal of Public Health 2005;95(9):1552‐60. [DOI] [PMC free article] [PubMed] [Google Scholar]
Utter 2010 {published data only}
- Utter J, Warbrick J, Scragg R, Denny S, Schaaf D. Design, development, and achievements of a youth‐led nutrition and physical activity intervention in a Pacific community in New Zealand. Journal of the American Dietetic Association 2010;110:1634‐7. [DOI] [PubMed] [Google Scholar]
Utter 2011 {published data only}
- Utter J, Scragg R, Robinson E, Warbrick J, Faeamani G, Foroughian S, et al. Evaluation of the Living 4 Life project: a youth‐led, school‐based obesity prevention study. Obesity Reviews 2011;12:51‐60. [DOI] [PubMed] [Google Scholar]
van Stralen 2009 {published data only}
- Stralen MM, Vries H, Mudde AN, Bolman C, Lechner L. Efficacy of two tailored interventions promoting physical activity in older adults. American Journal of Preventive Medicine 2009;37(5):405‐17. [DOI] [PubMed] [Google Scholar]
van Stralen 2011 {published data only}
- Stralen MM, Vries H, Mudde AN, Bolman C, Lechner L. The long‐term efficacy of two computer‐tailored physical activity interventions for older adults: main effects and mediators. Health Psychology 2011;30:442‐52. [DOI] [PubMed] [Google Scholar]
Voyle 1999 {published data only}
- Voyle JA, Simmons D. Community development through partnership: promoting health in an urban indigenous community in New Zealand. Social Science & Medicine 1999;49(8):1035‐50. [DOI] [PubMed] [Google Scholar]
Walker 2009 {published data only}
- Walker DG, Aedo C, Albala C, Allen E, Dangour AD, Elbourne D, et al. Methods for economic evaluation of a factorial‐design cluster randomised controlled trial of a nutrition supplement and an exercise programme among healthy older people living in Santiago, Chile: the CENEX study. BMC Health Services Research 2009;9:85. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wallace 1998 {published data only}
- Wallace JI, Buchner DM, Grothaus L, Leveille S, Tyll L, LaCroix AZ, et al. Implementation and effectiveness of a community‐based health promotion program for older adults. Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 1998;53(4):M301‐6. [DOI] [PubMed] [Google Scholar]
Wallmann 2011 {published data only}
- Wallmann B, Froboese I. [Intervention effects of 3000 steps more per day]. [German]. Wiener Klinische Wochenschrift 2011;123:369‐77. [DOI] [PubMed] [Google Scholar]
Wallmann 2012 {published data only}
- Wallmann B, Spittaels H, Bourdeaudhuij I, Froboese I. The perception of the neighborhood environment changes after participation in a pedometer based community intervention. International Journal of Behavioral Nutrition and Physical Activity 2012;9:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wang 2009 {published data only}
- Wang Z, Zhou L, Wang H, Zhang J, Lu H, Zhuang X, et al. Effectiveness of health education for management of hypertension of rural community in Zhangpu town. Jiangsu Journal of Preventive Medicine 2009;20(1):1‐3. [Google Scholar]
Warden 1999 {published data only}
- Warden SJ, Wajswelner H, Bennell KL. Comparison of Abshaper and conventionally performed abdominal exercises using surface electromyography. Medicine & Science in Sports & Exercise 1999;31(11):1656‐64. [DOI] [PubMed] [Google Scholar]
Wardle 2001 {published data only}
- Wardle J, Rapoport L, Miles A, Afuape T, Duman M. Mass education for obesity prevention: the penetration of the BBC's 'Fighting Fat, Fighting Fit' campaign. Health Education Research 2001;16(3):343‐55. [DOI] [PubMed] [Google Scholar]
Warren 1999 {published data only}
- Warren C, Brown P, Freudenberg N. Evaluation of the New York City Beacons. Phase I Findings. Report. Academy for Educational Development, Inc., New York, NY., 1999:83.
Wellman 2007 {published data only}
- Wellman NS, Kamp B, Kirk‐Sanchez NJ, Johnson PM. Eat better & move more: a community‐based program designed to improve diets and increase physical activity among older Americans. American Journal of Public Health 2007;97(4):710‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wen 2002 {published data only}
- Wen LM, Thomas M, Jones H, Orr N, Moreton R, King L, et al. Promoting physical activity in women: evaluation of a 2‐year community‐based intervention in Sydney, Australia. Health Promotion International 2002;17(2):127‐37. [DOI] [PubMed] [Google Scholar]
Whaley 2008 {published data only}
- Whaley DE, Haley PP. Creating community, assessing need: Preparing for a community physical activity intervention. Research Quarterly for Exercise and Sport 2008;79(2):245‐55. [DOI] [PubMed] [Google Scholar]
Wheat 1996 {published data only}
- Wheat G, Carter A, McAfee T, Thompson RS, Gayman J, Meuchel K. Addressing a neglected coronary heart disease risk factor in an HMO: exercise counseling and fitness testing at group health cooperative. HMO Practice 1996;10(3):131‐6. [PubMed] [Google Scholar]
Wiesemann 1997 {published data only}
- Wiesemann A, Metz J, Nuessel E, Scheidt R, Scheuermann W. Four years of practice‐based and exercise‐supported behavioural medicine in one community of the German CINDI area. Countrywide Integrated Non‐Communicable Diseases Intervention. International Journal of Sports Medicine 1997;18(4):308‐15. [DOI] [PubMed] [Google Scholar]
Wilcox 2006 {published data only}
- Wilcox S, Dowda M, Griffin SF, Rheaume C, Ory MG, Leviton L, et al. Results of the first year of active for life: translation of 2 evidence‐based physical activity programs for older adults into community settings [erratum appears in American Journal of Public Health 2006 96:1901]. American Journal of Public Health 2006;96(7):1201‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wilcox 2007 {published data only}
- Wilcox S, Laken M, Bopp M, Gethers O, Huang P, McClorin L, et al. Increasing physical activity among church members: community‐based participatory research. American Journal of Preventive Medicine 2007;32(2):131‐8. [DOI] [PubMed] [Google Scholar]
Wilcox 2009 {published data only}
- Wilcox S, Dowda M, Dunn A, Ory MG, Rheaume C, King AC. Predictors of increased physical activity in the Active for Life program. Preventing Chronic Disease 2009;6(1):A25. [PMC free article] [PubMed] [Google Scholar]
Williams 2007 {published data only}
- Williams NH, Hendry M, France B, Lewis R, Wilkinson C. Effectiveness of exercise‐referral schemes to promote physical activity in adults: systematic review. British Journal of General Practice 2007;57(545):979‐86. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wimbush 1998 {published data only}
- Wimbush W, MacGregor A, Fraser E. Impacts of a mass media campaign on walking in Scotland. Health Promotion International 1998;13:45‐53. [Google Scholar]
Withall 2012 {published data only}
- Withall J, Jago R, Fox K. The effect a of community‐based social marketing campaign on recruitment and retention of low‐income groups into physical activity programmes ‐ a controlled before‐and‐after study. BMC Public Health 2012;12:836. [DOI] [PMC free article] [PubMed] [Google Scholar]
Wu 2004 {published data only}
- Wu S‐P, Wang W‐Z, Du X‐L, Bao Q‐J, Zhao D‐H. Follow‐up study in stroke after community intervention in urban Beijing. Chinese Journal of Prevention and Control of Chronic Non‐communicable Diseases 2004;12(6):253‐5. [Google Scholar]
Wyatt 2008 {published data only}
- Wyatt HR, Jortberg BT, Babbel C, Garner S, Dong F, Grunwald GK, et al. Weight loss in a community initiative that promotes decreased energy intake and increased physical activity and dairy consumption: Calcium Weighs‐In. Journal of Physical Activity and Health 2008;5(1):28‐44. [DOI] [PubMed] [Google Scholar]
Xu 2000 {published data only}
- Xu X, Huang G, Gan W, Gao S, Xie B, Zhao J, et al. Assessment of health education on knowledge, attitude and behavior of cardiovascular disease in Fangshan farmers, Beijing. Chinese Journal of Behavioral Medical Science 2000;9(4):246‐8. [Google Scholar]
Xu 2001 {published data only}
- Xu HW, Yang QD, Liu YH, Zhou YH, Xie YQ, Xiao JF, et al. Evaluation on community intervention on risk factors of cerebrovascular disorders. Modern Rehabilitation 2001;5(8):36‐7. [Google Scholar]
Xu 2012 {published data only}
- Xu F, Ware R, Tse L, Wang Z, Hong X, Song A, et al. A school‐based comprehensive lifestyle intervention among chinese kids against obesity (CLICK‐Obesity): rationale, design and methodology of a randomized controlled trial in Nanjing city, China. BMC Public Health 2012;12:316. [DOI] [PMC free article] [PubMed] [Google Scholar]
Yancey 2001 {published data only}
- Yancey AK, Miles OL, McCarthy WJ, Sandoval G, Hill J, Leslie JJ, et al. Differential response to targeted recruitment strategies to fitness promotion research by African‐American women of varying body mass index. Ethnicity & Disease 2001;11(1):115‐23. [PubMed] [Google Scholar]
Yancey 2003 {published data only}
- Yancey AK, Jordan A, Bradford J, Voas J, Eller TJ, Buzzard M, et al. Engaging high‐risk populations in community‐level fitness promotion: ROCK! Richmond. Health Promotion Practice 2003;4(2):180‐8. [DOI] [PubMed] [Google Scholar]
Yang 2012 {published data only}
- Yang Y. Encouraging Active School Travel by Making it "Cool" A Quasi‐experimental Study using Boltage, Phase II. http://otrec.us/project/550 2012.
Yin 2012 {published data only}
- Yin Z, Parra‐Medina D, Cordova A, He M, Trummer V, Sosa E, et al. Miranos! Look at us, we are healthy! An environmental approach to early childhood obesity prevention. Childhood Obesity 2012;8:429‐39. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zhu 2008 {published data only}
- Zhu Y. Appraisal to community intervention on hypertension. Journal of Zhejiang University of Traditional Chinese 2008;32(2):43‐4. [Google Scholar]
Zivkovic 1998 {published data only}
- Zivkovic M, Bjegovic V, Vukovic D, Marinkovic J. [Evaluation of the effect of the health education intervention project "Healthy School"]. Srpski Arhiv Za Celokupno Lekarstvo 1998;126(5‐6):164‐70. [PubMed] [Google Scholar]
Zoellner 2011 {published data only}
- Zoellner J, Connell C, Madson M, Wang B, Reed V, Molaison E, et al. H.U.B city steps: methods and early findings from a community‐based participatory research trial to reduce blood pressure among African Americans. International Journal of Behavioral Nutrition and Physical Activity 2011;8:12p. [DOI] [PMC free article] [PubMed] [Google Scholar]
Zoellner 2012 {published data only}
- Zoellner J, Motley M, Wilkinson ME, Jackman B, Barlow ML, Hill JL. Engaging the Dan River Region to reduce obesity: application of the Comprehensive Participatory Planning and Evaluation process. Family & Community Health 2012;35:44‐56. [DOI] [PubMed] [Google Scholar]
References to ongoing studies
Davey 2011 {published data only}
- Davey RC, Hurst GL, Smith GR, Grogan SC, Kurth J. The impact and process of a community‐led intervention on reducing environmental inequalities related to physical activity and healthy eating ‐ a pilot study. BMC Public Health 2011;11:697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurst GL, Davey RC, Smith GR, Kurth J. Qualitative findings from a community‐led intervention aimed. Journal of Science and Medicine in Sport 2012;15:S310. [Google Scholar]
- Hurst GL, Smith GR, Davey RC. Final Report: “My Health Matters” A community‐led intervention aimed at reducing health inequalities related to physical activity and healthy eating. http://www.staffs.ac.uk/schools/sciences/geography/links/IESR/projects_myhealthmatters.shtml 2012:383. [DOI] [PMC free article] [PubMed]
Additional references
Armstrong 2014
- Armstrong, R. Socioeconomic position and mass media campaigns to prevent chronic illness. http://eprints.qut.edu.au/69375/ 2014, issue Thesis:410 pages.
Baker 2010
- Baker PRA, Francis DP, Hall BJ, Doyle J, Armstrong R. Managing the production of a Cochrane systematic review. Journal of Public Health 2010;32:448‐50. [DOI: 10.1093/pubmed/fdq058] [DOI] [PubMed] [Google Scholar]
Baker 2014
- Baker PRA, Costello JT, Dobbins M, Waters EB. The benefits and challenges of conducting an overview of systematic reviews in public health: a focus on physical activity. Journal of Public Health 2014;Advance access:1‐5. [DOI: 10.1093/pubmed/fdu050] [DOI] [PubMed] [Google Scholar]
Bassett et al 2008
- Bassett D, Mahar M, Rowe D, Morrow J. Walking and measurement. Medicine & Science in Sports & Exercise 2008;40(7 Suppl):529‐36. [DOI] [PubMed] [Google Scholar]
Bauman 2009
- Bauman A, Bull F, Chey T, Craig CL, Ainsworth BE, Sallis JF, et al. The IPS Group. The international prevalence study on physical activity: results from 20 countries. International Journal of Behavioral Nutrition and Physical Activity 2009;6(1):21. [DOI] [PMC free article] [PubMed] [Google Scholar]
Belanger 2011
- Bélanger M, Townsend N, Foster C. Age‐related differences in physical activity profiles of English adults. Preventive Medicine 2011;52:247‐49. [DOI] [PubMed] [Google Scholar]
Brand 2014
- Brand T, Pischke CR, Steenbock B, Schoenbach J, Poettgen S, Samkange‐Zeeb F, et al. What works in community‐based interventions promoting physical activity and healthy eating? A review of reviews. International Journal of Environmental Research and Public Health 2014;11:5866‐88. [DOI] [PMC free article] [PubMed] [Google Scholar]
Cavill and Bauman 2004
- Cavill N, Bauman A. Changing the way people think about health‐enhancing physical activity: do mass media campaigns have a role?. Journal of Sports Sciences 2004;22(8):771‐90. [DOI] [PubMed] [Google Scholar]
Cavill and Foster 2004
- Cavill N, Foster C. How to promote health enhancing physical activity: Community interventions. Health Enhancing Physical Activity. Perspectives Vol. 6. London: Meyer & Meyer Sport, 2004. [Google Scholar]
Christinsen 2009
- Christensen R, Nair S. Statistical method guidelines for Cochrane Public Health reviews (draft, 1st edit). CPHG Report May, 2009:16.
Cochrane IMS 2009 [Computer program]
- GRADE Working Group. GRADEprofiler. Version 3.2. Cochrane, 2009.
Crespo 2000
- Crespo CJ, Smit E, Anderson RE, Carter‐Pokras O, Ainsworth BE. Race/ethnicity, social class, and their relation to physical inactivity during leisure time: Results from the Third National Health and Nutrition Examination Survey, 1988‐1984. American Journal of Preventive Medicine 2000;18:46‐53. [DOI] [PubMed] [Google Scholar]
Crespo 2001
- Crespo CJ, Smit E, Carter‐Pokras O, Andersen R. Acculturation and leisure‐time physical inactivity in Mexican‐American adults: Results from NHANES III, 1988‐1994. American Journal of Public Health 2001;91:1254‐7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Curran 2007
- Curran JA, Dartnell J, Magee K, Sinclair D, McGrath PJ. Organisational and professional interventions to promote the uptake of evidence in emergency care: Effects on professional practice and health outcomes. Cochrane Database of Systematic Reviews 2007, Issue 2. [DOI: 10.1002/14651858.CD006557] [DOI] [Google Scholar]
Dishman 1994
- Dishman RK. Advances in exercise adherence. Champaign, IL: Human Kinetics, 1994. [Google Scholar]
Egger 1998
- Egger M, Smith GD. Meta‐analysis bias in location and selection of studies. BMJ (Clinical Research Ed.) 1998 Jan 3;316(7124):61‐6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Foster 2000
- Foster C. Guidelines for Health Enhancing Physical Activity Programmes. Tampere: UKK, 2000. [Google Scholar]
Foster 2005
- Foster C, Hillsdon M, Thorogood M. Interventions for promoting physical activity. Cochrane Database of Systematic Reviews 2005, Issue Issue 1. Art. No.: CD003180. [DOI: 10.1002/14651858.CD003180.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Foster 2011
- Foster C, Brennan G, Matthews A, McAdam C, Fitzsimons C, Mutrie N. Recruiting participants to walking intervention studies: a systematic review. International Journal of Behavioral Nutrition and Physical Activity 2011;8:137. [DOI] [PMC free article] [PubMed] [Google Scholar]
Gidlow 2006
- Gidlow C, Johnston HL, Crone D, Ellis N, James D. A systematic review of the relationship between socio‐economic position and physical activity. Health Education Journal 2006;65(4):338‐67. [Google Scholar]
Guthold 2008
- Guthold R, Ono T, Strong KL, Chatterji S, Morabia A. Worldwide variability in physical inactivity. A 51‐country survey. American Journal of Preventive Medicine 2008;34(6):486‐94. [DOI] [PubMed] [Google Scholar]
Heath 2012
- Heath G, Parra D. Evidence‐based intervention in physical activity: lessons from around the world. Lancet 2012;380:272‐81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Higgins 2008
- Higgins JPT, Altman DG on behalf of the Cochrane Statistical Methods Group and the Cochrane Bias Methods Group. Chapter 8: Assessing risk of bias in included studies. In: Higgins JPT, Green S editor(s). Cochrane Handbook for Systematic Reviews of Interventions. Chichester: Wiley‐Blackwell, 2008. [Google Scholar]
Humphreys 2013
- Humphreys D, Ogilvie D. Synthesising evidence for equity impacts of population‐based physical activity interventions:a pilot study. International Journal of Behavioral Nutrition and Physical Activity 2013;10:76. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kahn 2002
- Kahn EB, Ramsey LT, Brownson RC, Heath GW, Howze EH, Powell KP, et al. Task Force on Community Preventive Services. The effectiveness of interventions to increase physical activity: A systematic review. American Journal of Preventive Medicine 2002;22:73‐107. [DOI] [PubMed] [Google Scholar]
King 1994
- King AC. Community and public health approaches to the promotion of physical activity. Medicine & Science in Sports & Medicine 1994;26(11):1405‐12. [PubMed] [Google Scholar]
Luepker et al 1994
- Luepker RV, Murray DM, Jacobs DR Jr, Mittelmark MB, Bracht N, Carlaw R, et al. Community education for cardiovascular disease prevention: risk factor changes in the Minnesota Heart Health Program. American Journal of Public Health 1994;84(9):1383‐93. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group. referred Reporting Items for Systematic Reviews and Meta‐Analyses: The PRISMA Statement. PLoS Medicine 2009;6(6)::e1000097. doi:10.1371/journal.pmed1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
Mummery 2009
- Mummery WK, Brown WJ. Whole of community physical activity interventions: easier said than done. British Journal of Sports Medicine 2009;43(1):39‐43. [DOI] [PubMed] [Google Scholar]
NHMRC 1999
- NHMRC. A guide to the development, implementation and evaluation of clinical practice guidelines. Canberra: NHMRC, 1999. [Google Scholar]
NICE 2008
- National Institute for Health and Clinical Excellence. Physical activity and the environment: guidance on the promotion and creation of physical environments that support increased levels of physical activity. National Institute for Health and Clinical Excellence 2008.
Ogilvie 2007
- Ogilvie D, Foster C, Rothnie H, Cavill N, Hamilton V, Fitzsimons CF, Mutrie N. Scottish Physical Activity Research Collaboration. Interventions to promote walking: systematic review. BMJ 2007;334:1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
Petticrew 2003
- Petticrew M, Roberts H. Evidence, hierachies, and typologies: horses for courses. Journal of Epidemiology and Community Health 2003;57:527‐9. [DOI] [PMC free article] [PubMed] [Google Scholar]
Prochaska 1992
- Prochaska JO, DiClemente CC. Stages of change in the modification of problem behaviors. Progress in Behavior Modification 1992;28:183‐218. [PubMed] [Google Scholar]
Renger 2002
- Renger R, Steinfelt V, Lazarus S. Assessing the effectiveness of a community‐based media campaign targeting phsyical inactivity. Family & Community Health 2002;25(3):18‐30. [DOI] [PubMed] [Google Scholar]
Richards 2013
- Richards J, Thorogood M, Hillsdon M, Foster C. Face‐to‐face interventions for promoting physical activity. Cochrane Database of Systematic Reviews 2013, Issue 9. [DOI: 10.1002/14651858.CD010392.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]
Schünemann 2011
- Schünemann H, Hill S, Guyatt G, Akl EA, Ahmed F. The GRADE approach and Bradford Hill's criteria for causation. Journal of Epidemiology and Community Health 2011;65:392‐5. [DOI] [PubMed] [Google Scholar]
Sharpe 2003
- Sharpe P. Community‐based physical activity intervention. Arthritis and Rheumatism 2003;49(3):455‐62. [DOI] [PubMed] [Google Scholar]
Ueffing 2009
- Ueffing E, Tugwell P, Welch V, Petticrew M, Kristjansson E for the Cochrane Health Equity Field. C1, C2 Equity Checklist for Systematic Review Authors ‐ 2009‐05‐28. http://equity.cochrane.org/sites/equity.cochrane.org/files/uploads/equitychecklist.pdf on 28, August 2009.
US Physical Activity Guidelines 2008
WHO 2004
- World Health Organization. Global Strategy on Diet, Physical Activity and Health. 57th World Health Assembly 2004:41‐55.
WHO 2009
- WHO. Global health risks: mortality and burden of disease attributable to selected major risks. World Health Organization, 2009. [Google Scholar]
World Medical Association 2013
- World Medical. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 2013;310:2191. [DOI] [PubMed] [Google Scholar]
Yang 2010
- Yang L, Sahlqvist S, McMinn A, Griffin SJ, Ogilvie D. Interventions to promote cycling: systematic review. BMJ 2010;341:5293. [DOI] [PMC free article] [PubMed] [Google Scholar]


