Background:
Functional ankle instability (FAI) is defined as the subjective sensation of instability or “giving way” after an ankle sprain and occurs in approximately 40% of patients with lateral ankle instability. As an ankle joint rehabilitation intervention, heel raising exercises, toe jumping exercises, ankle joint proprioceptive exercises, as well as orthosis and taping are commonly applied to prevent the recurrence of an ankle joint injury. So this study was evaluated effect of quarter heel raising exercise (QHR) on balance and peroneus longus muscle strength in FAI subjects.
Methods:
Among 26 FAI subjects, 13 with FAI were assigned to the QHR group, and 13 with FAI were assigned to the control group which was no intervention. All of 30 subjects were evaluated Teskscan included static balance ability, Y balance test included dynamic balance ability with three directions which is anterior, posterolateral, posteromedial direction. Commander muscle testing included eversion/inversion strength ratio at pre- and post-intervention.
Results:
There was a significant interaction between group and time in static, dynamic balance, and strength. In QHR group, there was simple effect on static, dynamic balance, and strength. But control group showed no simple effect on static, dynamic balance, and strength. In the pre- and post-intervention differences between the groups. There was a significant difference in pre-intervention condition between the groups, but no significant difference between the groups in post-intervention in all conditions.
Conclusions:
QHR exercise is useful for improving the balance ability and muscle strength of the peroneus longus muscle in FAI subjects.
Keywords: balance, functional ankle instability, peroneus longus, quarter heel raising exercise, strength
1. Introduction
Ankle sprains are a common injury resulting from physical activity.[1] Repetitive ankle sprains lead to chronic instability of the ankle joint.[2,3] Functional ankle instability (FAI) is defined as the subjective sensation of instability or “giving way” after an ankle sprain and occurs in approximately 40% of patients with lateral ankle instability.[4,5] FAI causes various symptoms such as swelling, pain, and neuromuscular deficits.[6–10]
In addition, FAI is often accompanied by postural control deficit or weakness of the peroneus longus muscle. Docherty et al[11] identified deficiencies in the postural control ability of FAI subjects compared to uninjured subjects using the balance error scoring system. Santos and Liu[12] also reported that people with FAI have poorer balance control ability than their unaffected side lower limb. Meanwhile, the peroneus longus and brevis muscles act as major muscles during concentric eversion, and maximum activation occurs when the bodyweight is shifted to the forefoot during walking; that is, midstance with single limb support.[9,13] Thus, the peroneus longus muscle plays a critical role in lateral perturbation during walking, so FAI subjects might fail to maintain proper ankle positioning during landing due to functional deficits in the peroneal muscle.[14]
As an ankle joint rehabilitation intervention, heel raising exercises, toe jumping exercises, ankle joint proprioceptive exercises, as well as orthosis and taping, are commonly applied to prevent the recurrence of an ankle joint injury.[6,15] Especially, heel raising exercises are used to improve muscle strength and muscular sensation control function and are recommended as an exercise for the equal weight distribution of both limbs.[16,17] Meanwhile, the quarter heel raising exercise (QHR) is a modification of the general ankle eversion exercise in consideration of the biomechanical role of the peroneus longus muscle. Bellew et al[18] reported that the muscle activity of the peroneus longus muscle during QHRs was higher than that during traditional ankle eversion. However, few studies have been conducted on the effect of QHRs on the functional recovery of patients with FAI.
Therefore, the present study was conducted to investigate the effect of QHRs on balance and muscle strength in FAI subjects.
2. Materials and Methods
2.1. Subjects and setting
This study included 26 healthy subjects, divided into the QHR group (3 men, 10 women; mean age = 21.23 ± 1.96 years) and control group (5 men, 8 women; mean age, 20.62 ± 1.98 years) according to FAI (Table 1). Subjects were included in the QHR group if they had a FAI of less than 24 points on the Cumberland Ankle Instability Tool Questionnaire and had experienced an ankle sprain at least once, a person without congenital anomalies or diseases of the feet, ankles, knees, pelvis or spine, and person without a pacemaker. FAI subjects and no history of ankle sprains were included in the control group. Subjects were excluded from either group if they had congenital feet, ankle, knees, pelvis and spine deformities, and ankle pain, or a history of ankle surgery or fracture, person who had a pacemaker, and had never experienced an ankle sprain at least once.
Table 1.
General characteristics of the subjects.
| QHR group | Control group | t | |
|---|---|---|---|
| Mean ± SD | Mean ± SD | ||
| Sex (M/F) | 3/10 | 5/8 | −0.83 |
| FAI score | 19.54 ± 3.80 | 29.39 ± 0.87 | −9.11 * |
| Age | 21.23 ± 1.96 | 20.62 ± 1.98 | 0.80 |
| Height | 165.88 ± 9.43 | 165.46 ± 6.08 | 0.13 |
| Weight | 59.62 ± 11.18 | 62.00 ± 11.64 | −0.53 |
FAI = functional ankle instability, QHR = quarter heel raising, SD = standard deviation.
P < .05
Sample size was calculated using G*power 3.1.9.7 (Franz Faul, Kiel, Germany) based on our previous published data.[2] A required total sample size of 18 was determined by calculating an estimated effect size of 0.72, α level of 0.05, and power of 0.80. Consequently, a total of 26 individuals (13 in each group) were recruited.
This study was approved by the Daegu Haany University Hospital Institutional Review Committee (DHUMC-D19014-PRO-02). Informed consent was obtained from all subjects.
All subjects understood the experimental procedures and provided informed consent prior to the study.
2.2. Static balance
To measure the static balance ability, we used the MatScan VersaTek System (TekScan Inc., South Boston, MA). The subjects stood with a single limb in the center of the force plate, crossed their arms in front of their chest, lifted the uninvolved limb to about 30° of hip flexion and 45º of knee flexion, and stood as still as possible for the 10-second trial. We collected data for 30 frames/s to measure postural sway. Research foot ver. 7.0 (TekScan Inc.) and the Sway Analysis Module (SAM™; TekScan Inc.) were used to measure and analyze the center of force (CoF) movement including the area and distance.
2.3. Dynamic balance
To measure dynamic balance ability, we used the Y Balance Test. The subjects stood on the involved leg while reaching as far as possible with the uninvolved leg in three separate directions, to the anterior (A), posterolateral (PL), and posteromedial (PM) sides. To minimize errors caused by shoes, measurements were taken barefoot, and the average value of three measurements was used.
2.4. Muscle strength
Ankle inversion and eversion muscle strength were measured by the Commander Muscle Tester (JTECH MEDICAL, Midvale, UT). To measure the ankle evertor muscle strength, the subjects were seated with their ankle in the neutral position. The investigator held just above the subject’s malleolus with one hand to stabilize the ankle and placed the console on the forefoot and lateral edges of the foot to apply resistance in the direction of inversion and dorsiflexion. To measure ankle invertor muscle strength, the subject was seated with the ankle in slight dorsiflexion. The investigator held just above the subject’s malleolus with one hand to stabilize the ankle as well, and resistance was applied by placing the console in the inner part of the metatarsal head and eversion was applied with plantar flexion.[19] Each foot was measured three times, and the ratio of the ankle invertor to the evertor muscle was used.
2.5. Intervention
2.5.1. Quarter heel raising exercises.
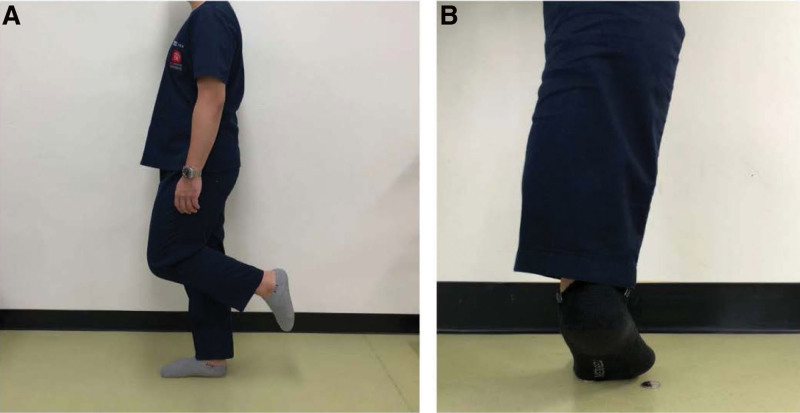
The subjects in the QHR group performed QHRs 4 times a week for 5 weeks. The quarter heel raising is a movement that takes into account the biomechanical role of the peroneus longus muscles.[18] To induce contraction of the peroneus longus muscle with ankle eversion as well as plantar flexion during the heel raising exercise, a coin was placed under the 1st metatarsal bone head where the peroneus longus muscle stops and the fifth metatarsal bone head, and then pressed the coin with the 1st metatarsal bone head but the 5th metatarsal bone head was not pressed the coin.[18] The subjects were instructed to fully raise and maintain the tip position for 4 seconds and minimal support was provided if the subjects needed it. One set of 15 repetitions were performed in each leg, for a total of 5 sets. To prevent muscle fatigue, the exercise was performed alternately by changing legs (Fig. 1).
Figure 1.
QHR: induce contraction of the peroneus longus muscle with ankle eversion as well as plantar flexion during the heel raise exercise, place a coin under the 1st metatarsal bone head where the peroneus longus muscle stops and the fifth metatarsal bone head, and then press the coin with 1st metatarsal bone head but not the fifth metatarsal bone head (A: starting position, B: end of QHR). QHR = quarter heel raising exercise.
In the control group, the intervention was not applied, and only pre- and post-tests were performed. The subjects were asked to avoid any ankle strength exercises during the 5 weeks between the pretest and post-test. However, they were allowed to continue their regular activities to maintain their pre-participation activity levels.
2.6. Statistical analysis
SPSS version 25 for Windows (IBM Corporation, New York) was used for analyzing the results. We used the Shapiro–Wilk test to test for normality. To investigate the interaction of group and time, two-way repeated-measures ANOVA was conducted. In addition, an independent t test was used to determine the pre- and post-intervention difference between the groups. The significant level was set at P < .05.
3. Results
3.1. Static balance
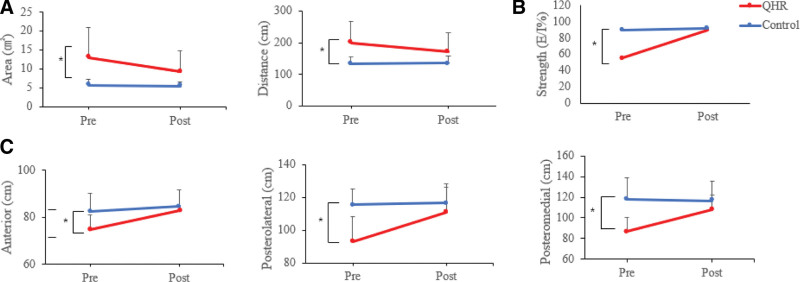
There was a significant interaction between group and time in the COF movement distance (F(1,24) = 26.475, P = .000) and COF movement area (F(1,24) = 6.961, P = .14). In the QHR group, there were simple effects of the intervention on distance (F(1,12) = 11.353, P = .002) and area (F(1,12) = 8.441, P = .013). In the control group, there was no simple effect of the intervention on distance (F(1,12) = 0.303, P = .353) and area (F(1,12) = 8.441, P = .592). In the pre- and post-intervention differences between the groups, there was a significant difference pre-intervention between the groups (P < .05), but there was no significant difference post-intervention (P > .05) (Table 2; Fig. 2).
Table 2.
Pre- and post-intervention comparison of balance and muscle strength.
| QHR group | Control group | Time × group interaction (F) | ||||
|---|---|---|---|---|---|---|
| Mean ± SD | Mean ± SD | |||||
| Balance | Static | Distance | Pre | 200.22 ± 66.98 | 133.96 ± 20.53‡ | 26.48* |
| Post | 171.73 ± 60.26† | 134.99 ± 22.99 | ||||
| Area | Pre | 13.04 ± 7.93 | 5.69 ± 1.62‡ | 6.96* | ||
| Post | 9.27 ± 5.46† | 5.48 ± 1.12 | ||||
| Dynamic | A | Pre | 74.89 ± 6.09 | 82.68 ± 7.52‡ | 11.94* | |
| Post | 82.98 ± 6.42† | 84.67 ± 6.95 | ||||
| PL | Pre | 93.00 ± 15.42 | 115.47 ± 9.71‡ | 18.26* | ||
| Post | 110.93 ± 15.22† | 116.75 ± 11.62 | ||||
| PM | Pre | 86.84 ± 13.25 | 117.68 ± 20.78‡ | 66.78* | ||
| Post | 107.64 ± 14.68† | 116.56 ± 19.14 | ||||
| Strength | Pre | 55.59 ± 17.31 | 89.67 ± 10.37‡ | 26.80* | ||
| Post | 89.33 ± 11.51† | 92.07 ± 10.29 | ||||
A = anterior direction, PL = posterolateral direction, PM = posteromedial direction, QHR = quarter heel raising, SD = standard deviation.
Interaction between time and group (P < .05).
Simple effect of the intervention on the interaction between time and group (P < .05).
Significant difference between groups by the independent t test (P < .05).
Figure 2.
(A) Comparison of pre- and post-intervention differences in static balance between the QHR group and the control group. (B) Comparison of pre- and post-intervention differences in the strength between the QHR group and the control group. (C) Comparison of pre- and post-intervention differences in the dynamic balance between the QHR group and the control group. QHR = quarter heel raising exercise.
3.2. Dynamic balance
A significant interaction between group and time was seen in all three directions (A, F(1,24) = 11.943, P = .002; PL, F(1,24) = 18.264, P = .000; and PM, F(1,24) = 66.780, P = .000). The QHR group showed the simple effect of the intervention in all conditions (A, F(1,12) = 32.788, P = .000; PL, F(1,12) = 27.171, P = .000; and PM, F(1,12) = 65.490, P = .000). The control group did not show the simple effect of the intervention in any of the three conditions (A, F(1,24) = 3.530, P = .085; PL, F(1,12) = 0.490, P = .497; and PM, F(1,12) = 2.128, P = .170). In the pre- and post-intervention differences between the groups, there was a significant difference pre-intervention between the groups (P < .05), but there was no significant difference post-intervention between the groups in the three conditions of A, PL, and PM (P > .05) (Table 2; Fig. 2).
3.3. Muscle strength
There was a significant interaction between group and time in muscle strength (F(1,24) = 26.795, P = .000). In the QHR group, there was a simple effect of intervention on muscle strength (F(1,12) = 33.385, P = .000). The control group did not show a simple effect of the intervention (F(1,12) = 2.248, P = .160). In the pre- and post-intervention differences between the groups, there was a significant pre-intervention difference (P < .000), but there was no significant difference between the groups post-intervention (P > .05) (Table 2; Fig. 2).
4. Discussion
This present study examined the effect of QHRs on balance and muscle strength in FAI subjects. The QHR group showed significant improvements in static and dynamic balance ability and muscle strength after QHRs. In the comparison between the groups, there were significant differences in static and dynamic balance and muscle strength before intervention. However, there were no significant differences in any conditions post-intervention. The results suggested that QHRs might be effective in improving balance ability and muscle strength in FAI subjects.
Individuals with FAI often complain of weakness in lateral ankle joint components, which affects the balance ability and muscle strength of the ankle joint.[19] Palmieri-Smith et al[10] reported that FAI subjects easily experienced muscle fatigue, ankle pain, and a low level of peroneus longus muscle activation. One possible theory to peroneal muscle deactivation is interference by gamma motor neuron system, and altered peripheral proprioception(afferent) affects the gamma loop, essential for employing type 2 motor units.[10] Dysfunction of gamma loops negatively influences mechanical receptors located in the ligaments, reducing muscle function.[10] These can lead that person with FAI prefer using hip strategy than using ankle strategy when they are in dynamic situation.[10,20] In this study, a significant pretest difference in balance and strength was seen between the QHR group and the control group.
Several previous studies have reported on improving balance through various exercises in ankle instability subjects. Youssef et al[22] divided chronic ankle instability subjects in two groups and applied weight-bearing for better balance exercises program and unilateral balance exercises to women with chronic ankle instability in each two groups. On an unstable support surface, both weight-bearing for better balance and unilateral balance exercise group showed a positive effect on balance of the lower limbs with chronic ankle instability.[22] Ha et al[23] reported that the application of ankle joint strengthening training on an unstable support surface to FAI subjects showed positive effects on proprioceptive ability and static balance ability.[23] In addition, the peroneal muscle is known to play an important role in maintaining balance as the main dynamic lateral stabilizer in the ankle.[24] In this study, we thought that a positive effect on balance ability through QHR exercise that improves muscle function of peroneal muscle.
The peroneus longus muscle originates at the peroneal bone head and ends at the 1st metatarsal bone head, and its biomechanical movement is defined as plantar flexion and eversion. Bellew et al[18] described the biomechanical movement of these peroneal muscles and examined the muscle activation that occurred during closed chain exercises, where the peroneus longus muscle was activated more than by open chain exercises. In this study, the QHR suggested by Bellew et al,[18] was applied to improve the activation of the peroneus longus muscle. This study showed that there was no significant difference in muscle strength between the control group and the FAI group after the intervention. The peroneus longus muscle supports lateral ankle stability in the stance phase during the gait cycle. Many previous studies reported that peak peroneus longus muscle activity occurred during the stance phase when the bodyweight is over the forefoot without any support and at high walking speeds.[25,26] To induce more excitability peroneus longus activation, we conducted QHRs at a single limb position with the heel raised.
Similar to the results of this study, previous studies reported improvements in muscle strength through specific interventions in FAI subjects. Smith et al[27] reported that a 6-week gradual strength training program using a Thera-band and a multiaxial ankle exerciser applied to FAI subjects showed a significant improvement in both inversion and eversion of the ankle joint. Hall et al[28] reported that there was a significant increase in ankle joint inversion and eversion muscle strength before and post-intervention in both the resistance band group and the proprioceptive neuromuscular facilitation group.
In conclusion, this study investigated the effect of QHRs on balance and muscle strength in FAI subjects. The QHR group showed the effect of the intervention on balance and strength compared to the control group. The results of the study indicated that the QHR was useful for improving the balance ability and muscle strength of the peroneus longus muscle in the ankle joint rehabilitation of FAI subjects in clinical practice. Considering the results of this study, quarter heel raise exercise had a positive effect on the improvement in strength and balance ability. If this quarter heel raise exercise is applied to the general public, it is thought that the incidence of musculoskeletal disease can be decreased by preventing an ankle sprain from progressing to a chronic ankle instability. In addition, in the case of professional athletes, the increase in strength and balance ability through quarter heel raise exercise can free them from ankle injuries during competitions or training, which is thought to have a direct effect on performance improvement. The limitation of the current study was that the results cannot be generalized to all ages because the study targeted adults in their twenties and FAI subjects exhibiting mild symptoms. Therefore, it is necessary to confirm the effect of QHRs on patients with FAI with various degrees of injury in various age groups in future studies.
4.1. Limitation
The limitation of the current study was that there were all normal subjects with mild FAI so that we cannot used randomized controlled trail in this study. And the results cannot be generalized to all ages because the study targeted adults in their twenties and FAI subjects exhibiting mild symptoms.
Acknowledgments
The authors are grateful to all volunteer participants for their co-operation and participation in this study.
Author contributions
Conceptualization: Joon Ho Seo, Mi Young Lee.
Data curation: Joon Ho Seo.
Funding acquisition: Mi Young Lee.
Investigation: Joon Ho Seo.
Methodology: Joon Ho Seo.
Project administration: Joon Ho Seo.
Supervision: Mi Young Lee.
Writing – original draft: Joon Ho Seo.
Writing – review & editing: Mi Young Lee.
Abbreviations:
- A =
- anterior
- CoF =
- center of force
- FAI =
- functional ankle instability
- PL =
- posterolateral
- PM =
- posteromedial
- QHR =
- quarter heel raise
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (no. 2021R1F1A1062308).
This study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Institutional Review Board of Daegu Haany University Hospital Institutional Review Committee (DHUMC-D19014-PRO-02) and informed consent was obtained from all subjects involved in the study and
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
How to cite this article: Seo JH, Lee MY. Effects of quarter heel raising exercise on balance and ankle strength in functional ankle instability subjects. Medicine 2022;101:38(e30672).
References
- [1].Cho BK, Park JK. Correlation between joint-position sense, peroneal strength, postural control, and functional performance ability in patients with chronic lateral ankle instability. Foot Ankle Int. 2019;40:961–8. [DOI] [PubMed] [Google Scholar]
- [2].Kaminski TW, Buckley BD, Powers ME, Hubbard TJ, Ortiz C. Effect of strength and proprioception training on eversion to inversion strength ratios in subjects with unilateral functional ankle instability. Br J Sports Med. 2003;37:410–5; discussion 415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Park SH. Effects of neuromuscular training on muscle activity and balance ability in badminton club members with chronic ankle instability. J Kor Phys Ther. 2016;28:243–8. [Google Scholar]
- [4].Freeman MAR, Dean MRE, Hanham IWF. The etiology and prevention of functional instability of the foot. J Bone Joint Surg Am. 1965;47:678–85. [PubMed] [Google Scholar]
- [5].Arnold BL, Linens SW, De La Motte SJ, Ross SE. Concentric evertor strength differences and functional ankle instability: a meta-analysis. J Athl Train. 2009;44:653–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Kannus P, Renstrom P. Current concepts review: treatment for acute tears of the lateral ligaments of the ankle. J Bone Joint Surg Am. 1991;73:305–12. [PubMed] [Google Scholar]
- [7].Hertel J. Functional anatomy, pathomechanics, and pathophysiology of lateral ankle instability. J Athl Train. 2002;37:364–75. [PMC free article] [PubMed] [Google Scholar]
- [8].Tropp H. Commentary: functional ankle instability revisited. J Athl Train. 2002;37:512–5. [PMC free article] [PubMed] [Google Scholar]
- [9].Hertel J. Functional instability following lateral ankle sprain. Sports Med. 2000;29:361–71. [DOI] [PubMed] [Google Scholar]
- [10].Palmieri-Smith RM, Ty Hopkins J, Brown TN. Peroneal activation deficits in persons with functional ankle instability. Am J Sports Med. 2009;37:982–8. [DOI] [PubMed] [Google Scholar]
- [11].Docherty CL, McLeod TCV, Shultz SJ. Postural control deficits in participants with functional ankle instability as measured by the balance error scoring system. Clin J Sport Med. 2006;16:203–8. [DOI] [PubMed] [Google Scholar]
- [12].Santos MJ, Liu W. Possible factors related to functional ankle instability. J Orthop Sports Phys Ther. 2008;38:150–7. [DOI] [PubMed] [Google Scholar]
- [13].Zdolšek A, Strojnik V, Dolenec A. Peroneal muscle activity during different types of walking. J Foot Ankle Res. 2018;11:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Kunugi S, Masunari A, Yoshida N, Miyakawa S. Postural stability and lower leg muscle activity during a diagonal single-leg landing differs in male collegiate soccer players with and without functional ankle instability. J Phys Fitness Sports Med. 2017;6:257–65. [Google Scholar]
- [15].Dabadghav R. Rehabilitation of Lateral Ankle Sprains in Sports. Essential in Hip and Ankle. Carlos SA, Anell OM, Arie MR, eds. London, UK: IntechOpen; 2019:101–110. [Google Scholar]
- [16].Uchida MC, Nishida MM, Sampaio RAC, Moritani T, Arai H. Thera-band® elastic band tension: reference values for physical activity. J Phys Ther Sci. 2016;28:1266–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Revak A, Diers K, Kernozek TW, Gheidi N, Olbrantz C. Achilles tendon loading during heel-raising and-lowering exercises. J Athl Train. 2017;52:89–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Bellew JW, Frilot CF, Busch SC, Lamothe TV, Ozane CJ. Facilitating activation of the peroneus longus: electromyographic analysis of exercises consistent with biomechanical function. J Strength Cond Res. 2010;24:442–6. [DOI] [PubMed] [Google Scholar]
- [19].Helen HJ, Avers D, Brown M. Daniels Worthingham’s Muscle Testing: Techniques of Manual Examination and Performance Testing. 9th ed. St Lousi, MO: Saunders; 2014:257–67. [Google Scholar]
- [20].Kalantariyan M, Minoonejad H, Rajabi R, Seidi F. Effects of functional ankle instability on balance recovery strategy in athletes. Phys Treat. 2018;8:99–106. [Google Scholar]
- [21].Pintsaar A, Brynhildsen J, Tropp H. Postural corrections after standardised perturbations of single limb stance: effect of training and orthotic devices in patients with ankle instability. Br J Sports Med. 1996;30:151–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Youssef NM, Abdelmohsen AM, Ashour AA, Elhafez NM, Elhafez SM. Effect of different balance training programs on postural control in chronic ankle instability: a randomized controlled trial. Acta Bioeng Biomech. 2018;20:159–69. [PubMed] [Google Scholar]
- [23].Ha SY, Han JH, Sung YH. Effects of ankle strengthening exercise program on an unstable supporting surface on proprioception and balance in adults with functional ankle instability. J Exerc Rehabil. 2018;14:301–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Cho BK, Park JK, Choi SM, SooHoo NF. The effect of peroneal muscle strength on functional outcomes after the modified Broström procedure for chronic ankle instability. Foot Ankle Int. 2018;39:105–12. [DOI] [PubMed] [Google Scholar]
- [25].Jonsson B, Rundgren A. The peroneus longus and brevis muscles. A roentgenologic and electromyographic study. Electromyography. 1971;11:93–103. [PubMed] [Google Scholar]
- [26].Louwerens JWK, Linge BV, de Klerk LW, Mulder PG, Snijders CJ. Peroneus longus and tibialis anterior muscle activity in the stance phase: a quantified electromyographic study of 10 controls and 25 patients with chronic ankle instability. Acta Orthop Scand. 1995;66:517–23. [DOI] [PubMed] [Google Scholar]
- [27].Smith BI, Docherty CL, Simon J, Klossner J, Schrader J. Ankle strength and force sense after a progressive, 6-week strength-training program in people with functional ankle instability. J Athl Train. 2012;47:282–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Hall EA, Docherty CL, Simon J, Kingma JJ, Klossner JC. Strength-training protocols to improve deficits in participants with chronic ankle instability: a randomized controlled trial. J Athl Train. 2015;50:36–44. [DOI] [PMC free article] [PubMed] [Google Scholar]