Background:
This study aimed to identify whether early postoperative shoulder stiffness is associated with improved healing following rotator cuff repair, and if so, how this factor might interact with other factors known to affect rotator cuff repair integrity.
Methods:
We conducted a retrospective analysis of prospectively collected data from 1,526 primary arthroscopic rotator cuff repairs. Six-week range of motion was assessed to determine shoulder stiffness, and repair integrity was evaluated at 6 months by ultrasound. Multiple logistic regression analysis was used to identify variables that affected retear, and receiver operating characteristic (ROC) curve analysis was used to evaluate predictive thresholds for retear.
Results:
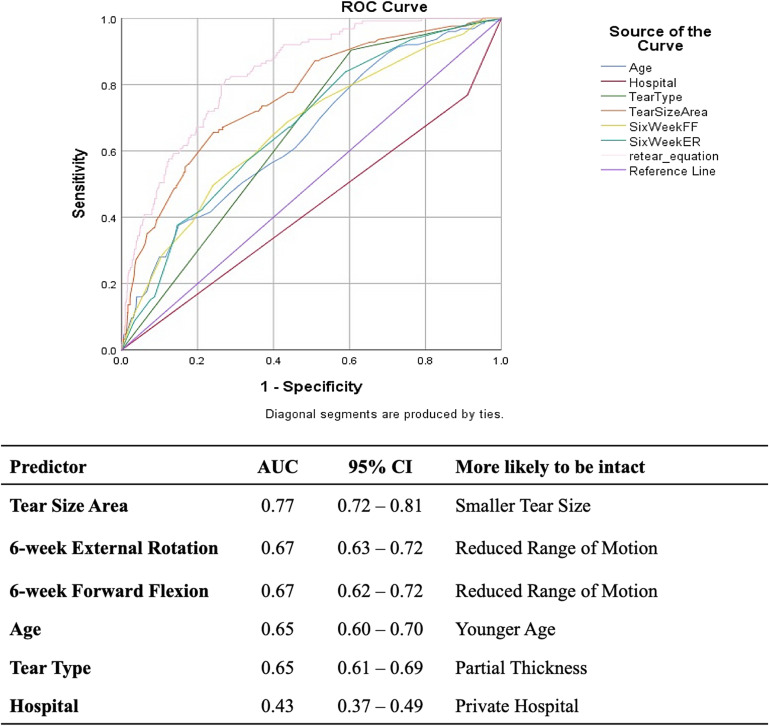
Tear-size area was the most accurate predictor of retear (area under the curve [AUC] = 0.77; 95% confidence interval [CI] = 0.72 to 0.81), followed by 6-week passive external rotation (AUC = 0.67; 95% CI = 0.63 to 0.72), 6-week passive forward flexion (AUC = 0.67; 95% CI = 0.62 to 0.72), age (AUC = 0.65; 95% CI = 0.60 to 0.70), tear type (partial-thickness versus full-thickness) (AUC = 0.65; 95% CI = 0.61 to 0.69), and hospital type (public versus private) (AUC = 0.43; 95% CI = 0.37 to 0.49). Patients with smaller tears, reduced 6-week passive external rotation, reduced 6-week passive forward flexion, younger age, partial-thickness tears, and operations performed in a private day surgery or hospital setting were more likely to have an intact rotator cuff repair at 6 months. The AUC of this curve was 0.84 (95% CI = 0.80 to 0.87), which indicates that this combination of factors can accurately predict 84% of retears. Reduced range of motion at 6 weeks was associated with improved repair integrity for patients with tears of >1 to 6 cm2; however, this effect was less pronounced in tears of ≤1 cm2 or >6 cm2.
Conclusions:
Early postoperative stiffness following arthroscopic single-row, inverted-mattress rotator cuff repair at 6 weeks was associated with an intact repair at 6 months. The protective effects of postoperative stiffness and tear size were additive. The chance of retear in patients with a tear of ≤1 cm2 and external rotation of ≤27° at 6 weeks was 1%, while those with tears of >6 cm2 and external rotation of >27° had a 40% chance.
Level of Evidence:
Prognostic Level III. See Instructions for Authors for a complete description of levels of evidence.
Retear remains the most common complication of a rotator cuff repair1. Previous studies have identified several factors as independent predictors of retear, specifically, larger tear size, patient age, less surgeon experience, public hospital type, and full-thickness tears2-7.
A reduction in shoulder range of motion following surgery, particularly at 6 weeks, is the second-most-common complication of rotator cuff repair surgery8 and coincides with increasing pain, which is often interpreted by patients as a failure of the repair9. Some surgeons recommend secondary capsular release surgery and/or manipulation under anesthesia to treat postoperative stiffness10. Others apply more aggressive rehabilitation protocols or corticosteroid injections. However, this reduction in shoulder range of motion typically resolves by 6 months postoperatively with or without treatment11.
The association between postoperative stiffness and retear remains controversial. Collin et al.12 and Parsons et al.13 found no significant association between postoperative stiffness and retear following rotator cuff repair in cohorts of 288 and 43 patients, respectively, whereas in a cohort of 999 patients, our group reported a significantly lower retear rate among patients with external rotation of ≤20° compared with >20° at 6 and 12 weeks postoperatively11.
Therefore, the aims of the current study were to identify whether or not reduced range of motion at 6 weeks is associated with improved healing following rotator cuff repair, and if so, by how much, as well as how this factor might interact with other factors known to affect rotator cuff repair integrity. We hypothesized that reduced range of motion at 6 weeks was associated with postoperative repair integrity.
Materials and Methods
Study Design
This was a retrospective analysis, performed using prospectively collected data. We evaluated the effects of 6-week shoulder range of motion on rotator cuff repair integrity at 6 months. This study received ethics approval from the South Eastern Sydney Local Health District Human Research Ethics Committee (11/STG/37).
Inclusion and Exclusion Criteria
Included patients underwent primary arthroscopic rotator cuff repair by the senior author and returned for 6-week clinical follow-up and 6-month follow-up ultrasonography. A primary repair was defined as repair of a rotator cuff without previous surgical treatment. Concurrent arthroscopic biceps procedures or subacromial decompression were included. Exclusion criteria included repairs with an interpositional polytetrafluoroethylene patch; isolated subscapularis tears; concurrent procedures including capsular release, stabilization, calcific tendinitis debridement, or fracture reduction; irreparable or partially repaired tendons; or failure to return for 6-week follow-up.
Range of Motion
Physical therapy providers measured passive shoulder range of motion via visual estimation and strength of shoulder external rotation, internal rotation, abduction in the scapular plane, lift-off, and adduction using a handheld dynamometer. Previously validated protocols have demonstrated that the inter- and intrarater reliability using this method are comparable with the reliability of other methods, including the use of a goniometer14.
Operative Procedure
All rotator cuff repairs were performed arthroscopically with patients in the upright beach-chair position, under an interscalene block15. Partial-thickness tears were converted into full-thickness tears using an 11-blade scalpel. The indication for conversion of a partial-thickness rotator cuff tear to a full-thickness tear was a symptomatic tear of >50% thickness. The torn rotator cuff tendon was reattached to the greater tuberosity using a single row of suture anchors (Opus Magnum; Smith & Nephew) in a knotless, inverted-mattress configuration. Undersurface repairs were visualized from within the glenohumeral joint15. Bursal repairs were visualized from within the subacromial bursa. Some repairs were conducted via both approaches15.
Anteroposterior and mediolateral tear-size measurements were obtained through comparison with the known diameter of the arthroscopic shaver (4.0 or 5.5 mm) and were multiplied to obtain tear-size area. Tear thickness was visually estimated by assessing the bare portion of the tendon. Tissue quality, tendon mobility, and repair quality were scored from 1 to 4, as previously detailed15. Glenohumeral joint osteoarthritis was graded visually on a 5-point scale, from none to severe16.
Rehabilitation
Patients followed a 6-month postoperative rehabilitation protocol under physical therapist guidance. Earlier in the study period, rehabilitation was more intensive; passive range-of-motion exercises were commenced immediately postoperatively, and active range-of-motion exercises began at day 8. Active exercises increased at 6 weeks, and active resistance was introduced at 3 months. Gradual modification of postoperative rehabilitation occurred over the study course, including initial immobilization during the day for 6 weeks using a sling with a small abduction pillow. Range-of-motion exercises began at postoperative day 8. Isometric strengthening exercises began at 6 weeks, and resistance exercises, at 3 months. Lifting and overhead restrictions were adjusted at 6-week and 3-month physical therapist consultations. Both protocols permitted return to normal activity at 6 months.
Assessment of Rotator Cuff Integrity
Patients underwent shoulder ultrasonography at 6 months, performed by a single experienced musculoskeletal sonographer using a Siemens ACUSON S2000 ultrasound system, to assess the presence of rotator cuff retear or nonhealing17.
Statistical Analysis
Bivariate Spearman tests for correlation were conducted to generate a correlation matrix to identify relationships between variables and to identify multicollinearity between the parameters of tear size and parameters for passive range of motion. Multiple logistic regression analysis was performed to identify variables that independently affected retear. Receiver operating characteristic (ROC) curve analysis and the Youden J statistic (sensitivity [%] + specificity [%] – 100), for assessing the accuracy of the predictors, were used to evaluate predictive thresholds for retear. The value generated from the ROC curve was used to allocated patients to a “stiff” or “non-stiff” group. Significance was set at p < 0.05 for all analyses.
Source of Funding
This study had no external sources of funding.
Results
Cohort
During the study period of January 2005 to December 2020, a single surgeon performed 3,669 consecutive arthroscopic rotator cuff repairs. Of these, 260 were excluded for revision repair; 131 for patch repair; 1,025 for concurrent procedures (stabilizations, capsular release, or calcific tendinitis); 7 for incomplete 6-month ultrasound data; and 720 for incomplete 6-week range-of-motion data. This left 1,526 cases, which formed the cohort of our study.
Demographics
There were 863 male and 663 female patients. The mean patient age at surgery (and standard deviation [SD]) was 59 ± 11 years. There were 918 right shoulders and 608 left shoulders.
Intraoperatively, 851 full-thickness and 538 partial-thickness tears were identified. The mean tear-size area was 3.3 ± 4.3 cm2. The repair technique was bursal-sided for 145 patients and undersurface for 1,013, while both techniques were used for 296 patients. The mean operative time was 18 ± 11 minutes, and the mean number of suture anchors was 2 ± 1. There were 1,218 repairs performed in a private day surgery or private hospital setting, while 149 were performed in a public hospital.
Factors Associated with Retear
At the 6-month follow-up, 1,381 rotator cuff repairs were intact, while 145 repairs had retorn or not healed. This corresponded to an overall retear rate of 9.5%. Patients with retear at 6 months were more likely to be older, to have presented with full-thickness tears, and to have had tears with a larger area. Operative times for the patients with retear at 6 months were greater, more suture anchors were utilized, and the patients were more likely to have undergone surgery in the public hospital setting (Table I).
TABLE I.
Demographic Comparison of Patients with Intact Repairs and Those with Retear at 6 Months Postoperatively*
| Variables | Intact | Retear | P Value† |
|---|---|---|---|
| No. of patients | 1,381 | 145 | |
| Sex (no. [%]) | NS | ||
| Male | 771 (54%) | 92 (63%) | |
| Female | 610 (44%) | 53 (37%) | |
| Age‡ (yr) | 58 ± 11 | 65 ± 11 | <0.0001 |
| Affected shoulder (no. [%]) | NS | ||
| Right | 829 (60%) | 89 (61%) | |
| Left | 552 (40%) | 56 (39%) | |
| Tear type (no. [%]) | <0.0001 | ||
| Full-thickness | 728 (58%) | 123 (90%) | |
| Partial-thickness | 524 (42%) | 14 (10%) | |
| Tear-size area‡ (mm2) | 287 ± 367 | 705 ± 723 | <0.0001 |
| Operative time‡ (min) | 18 ± 11 | 24 ± 12 | <0.0001 |
| Number of anchors‡ | 1.9 ± 1 | 2.7 ± 1.2 | <0.0001 |
| Hospital type (no. [%]) | <0.0001 | ||
| Private | 1,114 (90%) | 104 (77%) | |
| Public | 118 (10%) | 31 (23%) |
Not all patients had available data for some variables.
Statistical analysis performed using chi-square analysis and Student t test. NS = not significant.
The values are given as the mean and standard deviation.
Stiffness and Retear
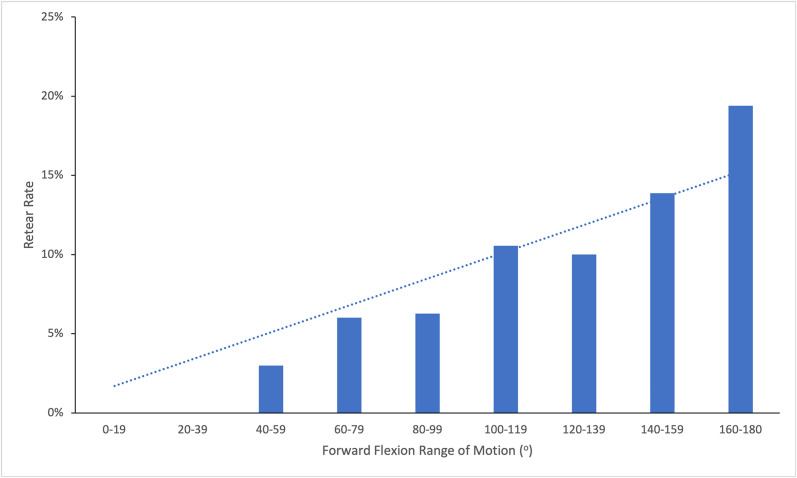
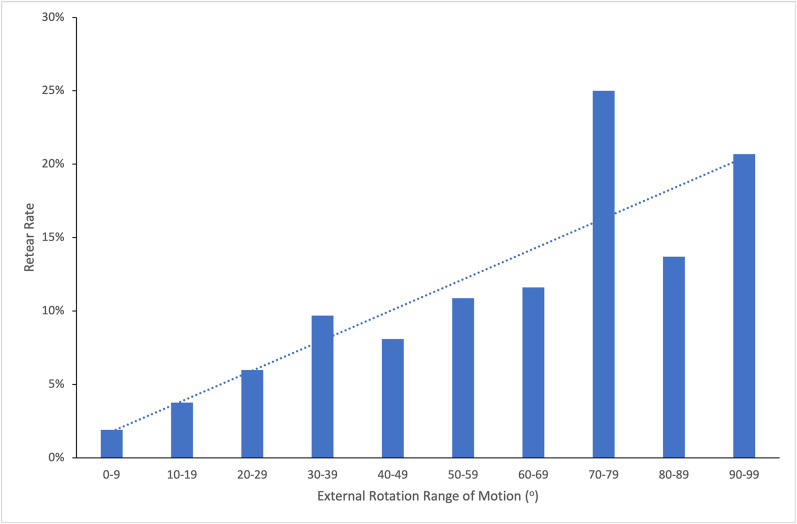
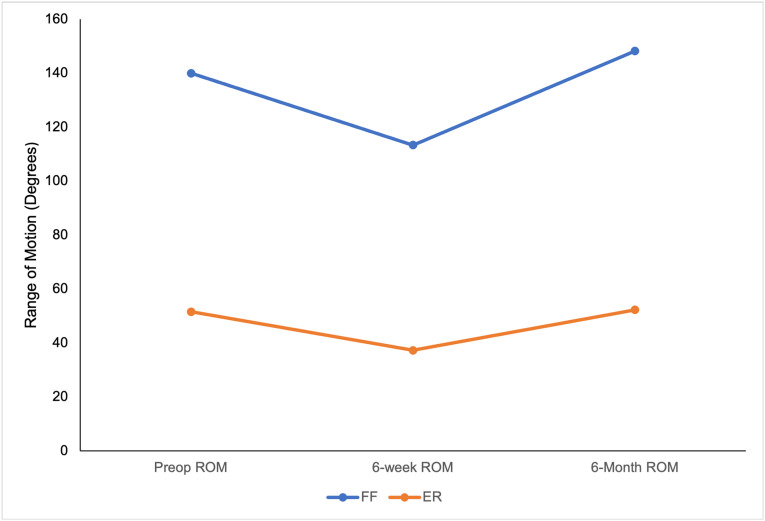
Patients with retear at 6 months, on average, were observed to have more passive range of motion at 6 weeks than those with intact repairs at 6 months. This association was strongest for external rotation and forward flexion (Figs. 1-A and 1-B). On average, patients returned to preoperative range of motion by 6 months of follow-up (Fig. 2).
Figs. 1-A and 1-B The effect of passive range of motion at 6 weeks on rotator cuff retear rate.
Fig. 1-A.
Fig. 1-B.
Fig. 2.
Passive range of motion (ROM) preoperatively and at 6 weeks and 6 months postoperatively. FF = forward flexion, and ER = external rotation.
Multivariate Analysis
Multiple logistic regression analysis was performed to identify independent predictors of retear at 6 months. Preoperative, intraoperative, and postoperative variables found to have significant univariate associations (case number, age, hospital type, tear type, tear thickness, tear-size area, number of anchors, surgeon-ranked tissue quality, surgeon-ranked tissue mobility, surgeon-ranked repair quality, operative time, 6-week forward flexion, 6-week abduction, 6-week external rotation, 6-week internal rotation, 6-week internal rotation strength, and 6-week lift-off strength) with repair integrity at 6 months were assessed. Multivariate analysis identified increased tear-size area, surgeries in a public hospital setting, greater 6-week forward flexion, full-thickness tears, greater 6-week external rotation, and advanced patient age at surgery as independent predictors of rotator cuff retear at 6 months. A predictive equation for cuff retear was developed using the identified predictors (where FF = forward flexion and ER = external rotation):
Logit (p) = 0.030 × Patient Age at Surgery − 1.346 × Hospital Type + 1.193 × Tear Type + 0.001 × Tear Size Area + 0.016 × 6-Week FF + 0.016 × 6-Week ER.
ROC Curve Analysis
The above predictive regression equation was used to generate an ROC curve, and the area under the curve (AUC) was calculated to assess the accuracy of this equation in predicting retears. The AUC of this curve was 0.84 (95% confidence interval [CI] = 0.80 to 0.87), which indicates that this equation can accurately predict 84% of retears.
Effect of Independent Predictors
The AUC of the ROC curves for the independent predictors of retear was used to determine the accuracy of each individual predictor. Tear-size area was the most accurate predictor of retear (AUC = 0.77; 95% CI = 0.72 to 0.81), followed by 6-week passive external rotation (AUC = 0.67; 95% CI = 0.63 to 0.72), 6-week passive forward flexion (AUC = 0.67; 95% CI = 0.62 to 0.72), age (AUC = 0.65; 95% CI = 0.60 to 0.70), tear type (partial-thickness versus full-thickness) (AUC = 0.65; 95% CI = 0.61 to 0.69), and hospital type (public versus private) (AUC = 0.43; 95% CI = 0.37 to 0.49) (Fig. 3). Thus, patients with smaller initial tears, reduced 6-week passive external rotation and forward flexion, younger age at the time of surgery, partial-thickness tears, and operations performed in a private day surgery or private hospital setting were more likely to have an intact rotator cuff repair at 6 months.
Fig. 3.
Receiver operating characteristic (ROC) curve and area under the curve (AUC) data for the independent predictors of retear at 6 months following arthroscopic rotator cuff repair, ranked in order of predictive value. FF = forward flexion, and ER = external rotation.
Predictive Thresholds
The ROC curves were used to identify a predictive threshold value (based on the highest Youden J statistic) at which rotator cuffs were more likely to retear at 6 months for each predictor. The threshold value for tear-size area was 4 cm2 (J = 0.41). The threshold value was 27° (J = 0.25) for 6-week postoperative external rotation and was 145° for 6-week postoperative forward flexion (J = 0.26) (Table II).
TABLE II.
Predictive Threshold Values for Predictors Identified from the ROC Curve
| Predictor | Threshold Value | Youden J Statistic |
|---|---|---|
| Tear-size area | 4 cm2 | 0.41 |
| 6-wk postop. passive external rotation | 27.5°* | 0.25 |
| 6-wk postop. passive forward flexion | 145° | 0.26 |
Value given to 1 decimal point.
Effect of Predictor Interactions on Retear
A post-hoc subgroup analysis was performed by allocating patients with ≤27° of external rotation at 6 weeks to a “stiff” group and patients with >27° to a “non-stiff” group, in accordance with the threshold value identified. Similarly, patients were also allocated to “stiff” or “non-stiff” groups on the basis of the threshold value identified for forward flexion (145°).
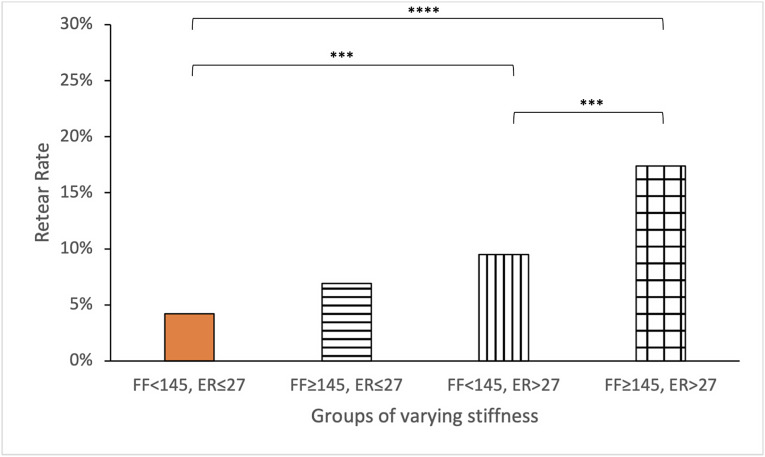
The overall retear rate for patients with stiffer shoulders (≤27° of external rotation and <145° of forward flexion) at 6 weeks (4%) was significantly lower than that of patients with non-stiff shoulders (>27° of external rotation and ≥145° of forward flexion) (17%) (p < 0.0001). Compared with 6-week forward flexion stiffness, 6-week external rotation stiffness had a stronger association with an intact repair at 6 months (Fig. 4).
Fig. 4.
The relationship between passive range of motion at 6 weeks (measured in degrees) and rotator cuff repair integrity at 6 months. FF = forward flexion, and ER = external rotation. ***P < 0.001 and ****p < 0.0001 using chi-square analysis.
Stiffness and Tear Size
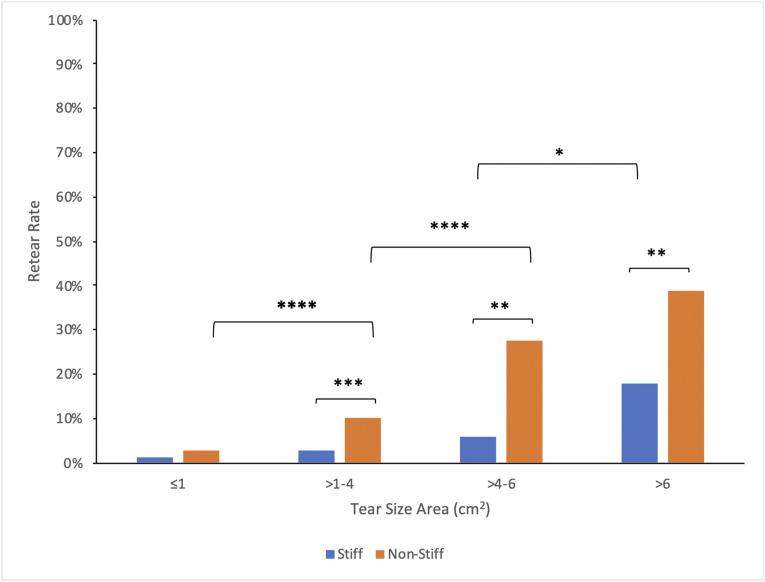
To examine the interactive effect of the strongest predictors of retear, 6-week stiffness and tear size, patients were separated into 4 groups according to tear-size area: ≤1 cm2, >1 to 4 cm2, >4 to 6 cm2, and >6 cm2. The 4-cm2 cutoff value was chosen in concordance with the identified threshold value from the ROC curve.
For all tear sizes, patients with 6-week postoperative shoulder stiffness had lower retear rates compared with patients with non-stiff shoulders. The effects of 6-week stiffness and tear-size area were additive: the rate of retear was 1% in patients with a tear of ≤1 cm2 and 6-week shoulder stiffness, while for those with tears of >6 cm2 and a non-stiff shoulder, it was 40%. The data suggest that early postoperative stiffness was protective against retear for patients with tears of >1 to 6 cm2. However, the protective effect of stiffness was less pronounced for tears of ≤1 cm2 and tears of >6 cm2, where the detrimental tear-size effects began to overwhelm the protective effect of stiffness (Fig. 5). This protective effect for small to medium tears was seen in shoulders that were stiff on the basis of external rotation and those that were stiff on the basis of forward flexion.
Fig. 5.
Comparison of retear rates by tear-size area between patients who were stiff (≤27° of external rotation) versus non-stiff (>27° of external rotation) at 6 weeks postoperatively. *P < 0.05, **p < 0.01, ***p < 0.001, and ****p < 0.0001 using chi-square analysis.
Discussion
The major findings of this study were that patients with 6-week postoperative stiffness in external rotation and forward flexion following arthroscopic rotator cuff repair were less likely to experience retear at 6 months. The beneficial effect of stiffness at 6 weeks was not as important as smaller initial tear size, but was of greater importance than younger patient age, surgery in a private hospital, and partial-thickness tear type. A post-hoc subgroup analysis demonstrated an additive effect of tear size and 6-week stiffness on retear.
It is unclear whether early postoperative stiffness following rotator cuff repair is a treatment complication or a protective factor against retear. Several studies have identified stiffness at different time points as a complication following rotator cuff repair13,18. Furthermore, there is a general agreement among surgeons that stiffness is a negative postoperative outcome, and that measures (e.g., delaying surgery in patients with “capsulitis”) should be taken to avoid this complication. In contrast, our study demonstrated that shoulder stiffness at 6 weeks is protective against retear.
The predictors of retear have been the focus of several large cohort studies. The majority of studies support the hypothesis that tear size is the most important predictor of retear2-7,19-21, followed by advanced age5,7,22. Other suggested factors include case number (a proxy measure for surgeon experience), tear thickness, and hospital type5,22. However, all of the aforementioned studies failed to include examiner-assessed postoperative range of motion as a variable for analysis. Our study found a reduction in passive range of motion at 6 weeks to be the second-most-powerful predictor of retear.
Our study findings are consistent with our earlier work, in which our group identified that “stiff” patients, defined as having 6-week postoperative external rotation of ≤20°, had lower retear rates compared with their “non-stiff” counterparts, defined as having external rotation of >20°. The current study has a larger cohort (1,526 versus 999 patients11) and assessed the relationships between shoulder range of motion and other factors associated with impaired rotator cuff repair integrity. We found that the protective effect of stiffness at 6 weeks was most evident in patients with medium-sized (>1 to 6 cm2) rotator cuff tears. Patients in the non-stiff group demonstrated a fourfold increase in retear rates when crossing the predictive threshold for tear size area (4 cm2) compared with a twofold increase in retear rates for patients in the stiff group. The protective effect of 6-week stiffness was reduced for tear-size extremes, i.e., less protective for patients with tears of ≤1 cm2 or >6 cm2. This suggests that, while tear size still has the greatest effect on retear overall, stiffness is particularly important for repair integrity in the smaller-to-medium distribution of tear sizes. These data support the hypothesis that small and medium tears heal more exuberantly (and hence, get stiffer at 6 weeks), while larger tears heal less vigorously, and the race to healing is overwhelmed in patients with large tears. Interestingly, the ROC curve value for the range of motion at which retears became more likely (27° of external rotation) was similar to that arbitrarily determined by McNamara et al.11 (20° of external rotation).
A major strength of this study lies in the large sample size. The data were collected prospectively in a standardized, systematic fashion. Retear was assessed by a single experienced ultrasonographer, 6-week range of motion was assessed using a validated protocol by experienced physical therapy providers, and all operations were performed by a single surgeon.
There were several limitations to this study. These results may not be reproducible by other surgeons and centers that use different techniques or rehabilitation protocols. Furthermore, some factors that were assessed, such as cuff tissue quality, tendon mobility, and repair quality, are qualitative and subjective. Some changes were made to the rehabilitation protocol throughout the course of data collection, which may have influenced tendon healing. The study was retrospective, and so some patients were lost to follow-up. An exclusion criterion was concurrent capsular release. It is likely the protective effects of stiffness would have been enhanced if these patients were included, as we have demonstrated that patient undergoing concurrent capsular release (for stiffness) and rotator cuff repair have almost no retears at 6 months23.
In summary, this study demonstrated that, following arthroscopic rotator cuff repair using a single-row, inverted-mattress configuration, postoperative stiffness at 6 weeks was a powerful, independent predictor of rotator cuff integrity at 6 months. This predictor (6-week postoperative stiffness) was nearly as powerful as reduced tear size, and more powerful than younger age, private versus public hospital, and partial-thickness versus full-thickness tear type in predicting a healed tendon at 6 months. Patients with tears of ≤1 cm2 and stiffer shoulders at 6 weeks had a retear rate of 1%, while those with tears of >6 cm2 and good range of motion (external rotation of >27°/forward flexion of ≥145°) at 6 weeks had a retear rate of 40%. Stiffness provided a significant protective effect against retear for patients with small to medium tear sizes; however, this effect was less pronounced at the extremes (≤1 and >6 cm2) of tear size. The findings support the hypothesis that early postoperative stiffness should not be considered a postoperative complication but rather an indicator of a more robust recovery following rotator cuff repair.
Footnotes
Investigation performed at the Orthopaedic Research Institute, St George Hospital Campus, University of New South Wales, Sydney, New South Wales, Australia
Disclosure: The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A419).
References
- 1.Randelli P, Spennacchio P, Ragone V, Arrigoni P, Casella A, Cabitza P. Complications associated with arthroscopic rotator cuff repair: a literature review. Musculoskelet Surg. 2012. Jun;96(1):9-16. [DOI] [PubMed] [Google Scholar]
- 2.Kwon J, Lee YH, Kim SH, Ko JH, Park BK, Oh JH. Delamination does not affect outcomes after arthroscopic rotator cuff repair as compared with nondelaminated rotator cuff tears: a study of 1043 consecutive cases. Am J Sports Med. 2019. Mar;47(3):674-81. [DOI] [PubMed] [Google Scholar]
- 3.Kwon J, Kim SH, Lee YH, Kim TI, Oh JH. The rotator cuff healing index: a new scoring system to predict rotator cuff healing after surgical repair. Am J Sports Med. 2019. Jan;47(1):173-80. [DOI] [PubMed] [Google Scholar]
- 4.Lee YS, Jeong JY, Park CD, Kang SG, Yoo JC. Evaluation of the risk factors for a rotator cuff retear after repair surgery. Am J Sports Med. 2017. Jul;45(8):1755-61. [DOI] [PubMed] [Google Scholar]
- 5.Duong JKH, Lam PH, Murrell GAC. Anteroposterior tear size, age, hospital, and case number are important predictors of repair integrity: an analysis of 1962 consecutive arthroscopic single-row rotator cuff repairs. J Shoulder Elbow Surg. 2021. Aug;30(8):1907-14. [DOI] [PubMed] [Google Scholar]
- 6.Le BT, Wu XL, Lam PH, Murrell GA. Factors predicting rotator cuff retears: an analysis of 1000 consecutive rotator cuff repairs. Am J Sports Med. 2014. May;42(5):1134-42. [DOI] [PubMed] [Google Scholar]
- 7.Wu XL, Briggs L, Murrell GA. Intraoperative determinants of rotator cuff repair integrity: an analysis of 500 consecutive repairs. Am J Sports Med. 2012. Dec;40(12):2771-6. [DOI] [PubMed] [Google Scholar]
- 8.Vastamäki H, Vastamäki M. Postoperative stiff shoulder after open rotator cuff repair: a 3- to 20-year follow-up study. Scand J Surg. 2014. Dec;103(4):263-70. [DOI] [PubMed] [Google Scholar]
- 9.Rizvi SMT, Bishop M, Lam PH, Murrell GAC. Factors predicting frequency and severity of postoperative pain after arthroscopic rotator cuff repair surgery. Am J Sports Med. 2021. Jan;49(1):146-53. [DOI] [PubMed] [Google Scholar]
- 10.Huberty DP, Schoolfield JD, Brady PC, Vadala AP, Arrigoni P, Burkhart SS. Incidence and treatment of postoperative stiffness following arthroscopic rotator cuff repair. Arthroscopy. 2009. Aug;25(8):880-90. [DOI] [PubMed] [Google Scholar]
- 11.McNamara WJ, Lam PH, Murrell GAC. The relationship between shoulder stiffness and rotator cuff healing: a study of 1,533 consecutive arthroscopic rotator cuff repairs. J Bone Joint Surg Am. 2016. Nov 16;98(22):1879-89. [DOI] [PubMed] [Google Scholar]
- 12.Collin P, Kempf JF, Molé D, Meyer N, Agout C, Saffarini M, Godenèche A; Société Française de Chirurgie Orthopédique et Traumatologique (SoFCOT). Ten-year multicenter clinical and MRI evaluation of isolated supraspinatus repairs. J Bone Joint Surg Am. 2017. Aug 16;99(16):1355-64. [DOI] [PubMed] [Google Scholar]
- 13.Parsons BO, Gruson KI, Chen DD, Harrison AK, Gladstone J, Flatow EL. Does slower rehabilitation after arthroscopic rotator cuff repair lead to long-term stiffness? J Shoulder Elbow Surg. 2010. Oct;19(7):1034-9. [DOI] [PubMed] [Google Scholar]
- 14.Ronquillo JC, Szomor Z, Murrell GAC. Examination of the Shoulder. Tech Shoulder Elbow Surg. 2011;12:116-25. [Google Scholar]
- 15.Wu XL, Baldwick C, Briggs L, Murrell GAC. Arthroscopic Undersurface Rotator Cuff Repair. Tech Shoulder Elbow Surg. 2009;10:112-8. [Google Scholar]
- 16.Slattery C, Kweon CY. Classifications in Brief: Outerbridge Classification of Chondral Lesions. Clin Orthop Relat Res. 2018. Oct;476(10):2101-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Briggs L, Murrell GAC. Diagnostic Ultrasound: Examination of the Shoulder. Tech Shoulder Elbow Surg. 2011;(12)4:101-107. [Google Scholar]
- 18.Chung SW, Huong CB, Kim SH, Oh JH. Shoulder stiffness after rotator cuff repair: risk factors and influence on outcome. Arthroscopy. 2013. Feb;29(2):290-300. [DOI] [PubMed] [Google Scholar]
- 19.Kim IB, Jung DW. A rotator cuff tear concomitant with shoulder stiffness is associated with a lower retear rate after 1-stage arthroscopic surgery. Am J Sports Med. 2018. Jul;46(8):1909-18. [DOI] [PubMed] [Google Scholar]
- 20.Tan M, Lam PH, Le BTN, Murrell GAC. Trauma versus no trauma: an analysis of the effect of tear mechanism on tendon healing in 1300 consecutive patients after arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2016. Jan;25(1):12-21. [DOI] [PubMed] [Google Scholar]
- 21.Park JS, Park HJ, Kim SH, Oh JH. Prognostic factors affecting rotator cuff healing after arthroscopic repair in small to medium-sized tears. Am J Sports Med. 2015. Oct;43(10):2386-92. [DOI] [PubMed] [Google Scholar]
- 22.Diebold G, Lam P, Walton J, Murrell GAC. Relationship between age and rotator cuff retear: a study of 1,600 consecutive rotator cuff repairs. J Bone Joint Surg Am. 2017. Jul 19;99(14):1198-205. [DOI] [PubMed] [Google Scholar]
- 23.McGrath JP, Lam PH, Tan MT, Murrell GA. The effect of concomitant glenohumeral joint capsule release during rotator cuff repair—a comparative study. J Shoulder Elbow Surg. 2016. May;25(5):714-22. [DOI] [PubMed] [Google Scholar]