Abstract
Medical uninsurance (MU) is associated with cancer disparities, particularly among underprivileged and minority sections of the United States. In this cross-sectional study of National Health and Nutritional Examination Survey (NHANES) data from 2013 to 2018, we evaluated sociodemographic attributes of MU disparity in the US cancer population. Those aged ≥20 years with a history of cancer and disclosed MU status were included. We calculated the descriptive statistics of the population stratified by insurance type and performed bivariate and multivariate logistic regression models to assess the association of sociodemographic attributes and MU and reported unadjusted (UOR) and adjusted odds ratios (AOR). Among the 1681 participants (US estimated, 25,982,352), 4.3% ± 0.62 were uninsured. Uninsured individuals were 13.5-year younger, largely female, less educated, and non-US born compared to insured individuals. Age (UOR: 0.94, 95% CI: 0.93–0.96), female sex (UOR: 3.53, 95% CI: 1.73–7.19), Hispanics (UOR: 4.30, 95% CI: 2.45–7.54), <high school education (UOR: 7.41, 95% CI: 2.51–21.86), and non-US born with <20-years-stay in US (UOR: 7.69, 95% CI: 3.32–17.82) were associated with MU. In the multivariate model, age (AOR: 0.95, 95% CI: 0.93–0.96), female sex (AOR: 2.88, 95% CI: 1.25–6.62), <high school education (AOR: 4.02, 95% CI: 1.24–13.00), and non-US-born status with <20-years stay (AOR: 3.42, 95% CI: 1.44–8.11) were independent predictors of MU. Income was not a predictor of MU. The US cancer population has unique determinants of MU. Ethnicity alone is not a predictor of MU, whereas income is not correlated with MU. Public health interventions focusing on the attributes of MU are needed.
Keywords: cancer disparities, medical uninsurance, NHANES, public health interventions, United States
1. Introduction
Health disparities in the United States continue to be a major public health problem despite legislation such as the Affordable Care Act (ACA).[1] These disparities are deeply rooted in conditions around birth, development, education, employment, culture, and healthcare access.[2] These conditions, known as social determinants of health[2] determine the trajectory of our illnesses and influence our life paths; whether someone would receive preventive care or seek medical attention when a disease is disabling would depend on the factors mentioned above. Cancer disparities, therefore, are due to disparate exposures to carcinogens, socioeconomic statuses, health behaviors, and racial/ethnic differences.[1] Educational attainment is an essential predictor of socioeconomic well-being, and its lack adds to increased mortality across all racial/ethnic groups.[3] Interestingly, the difference in cancer survival across racial/ethnic strata in the US gets diluted when socioeconomic imbalances resolve.[1] Affluent Americans are at a lower risk of death from cancer as they benefit from advanced preventive, diagnostic, and therapeutic services compared to their poor contemporaries.[4] Contrarily, those Americans who live in deprived areas, have limited education, or low income are at increased risk of all-cancer mortality. Socioeconomically disadvantaged Americans are at enhanced risk of mortality caused by lung, colorectal, stomach, liver, and cervical cancers.[4] All-cancer mortality in the US has declined dramatically from 1950 to 2014. Still, deprived Americans remained with a 22% higher cancer-related mortality compared to the most well-off Americans in 2010 to 2014.[4] Between 2003 and 2011, men with less than a high school education had about 68% greater cancer-related mortality when compared to college graduates.[4] All-cancer mortality is worst for African Americans than for White Americans. Poor and disadvantaged neighborhoods with scarce resources also play a role in cancer mortality. According to a study of National Health Interview Survey data from 1998, Hispanics, Asian Americans, and Pacific Islanders were less likely to undergo cancer-related screening procedures than Whites.[5] On the other hand, ethnic minorities were as likely to experience screening procedures as their White counterparts when adjusted for foreign birth. So foreign birth could potentially contribute to cancer disparities, and this could be partly explained by poor access to healthcare among foreign-born individuals.[5] According to a population-based cohort of 577,716 patients, medical insurance provides cancer-specific mortality benefits consistently across all racial groups.[6] In this study, we evaluated the National Health and Nutrition Examination Survey (NHANES) data for the years 2013 to 2018[7] among cancer patients and determined the association of medical coverage with social determinants of health so that public health interventions could focus on those factors to improve medical coverage.
2. Materials and Methods
2.1. Study population
We performed a cross-sectional study using the NHANES data for the years 2013 to 2018[7] to evaluate the predictors or sociodemographic correlates of medical uninsurance (MU) in the US cancer population. The NHANES collects data via interviews and medical examinations on medical conditions, sociodemographic factors, and healthcare access patterns in nationally representative noninstitutionalized civilians. The data are published in every 2-year survey cycle and are available online at https://wwwn.cdc.gov/nchs/nhanes/default.aspx. The National Center for Health Statistics (NCHS) in the Centers for Disease Control and Prevention (CDC) is responsible for these nutritional and health assessment surveys through authorization by National Health Survey Act 1956. The NHANES uses a complex, multistage sampling design and incorporates probability sampling, which oversamples certain populations to increase the reliability of the sample. In this study, we combined data from 3 consecutive survey cycles: 2013 to 2014, 2015 to 2016, and 2017 to 2018. These cycles were selected being the most recent ones at the time of the study. Data collection for the cycle 2019 to 2020 was interrupted amid the COVID-19 pandemic and is therefore not US representative; it became available in May 2021. To incorporate the fact that data spanned over 6 years and 3 cycles, we divided the total weighted sample by 3. The NCHS Research Ethics Review Board approved the surveys in the NHANES protocol for 2011 to 2017. All the participants provided informed consent. We extracted data on cancer, health insurance coverage, and selective sociodemographic correlates such as age, sex, and race/ethnicity. We chose education, annual household income and US birth and US length of stay in the context of their significance as social determinants of health and previous literature.[4]
2.2. Inclusion/exclusion criteria and sociodemographic attributes
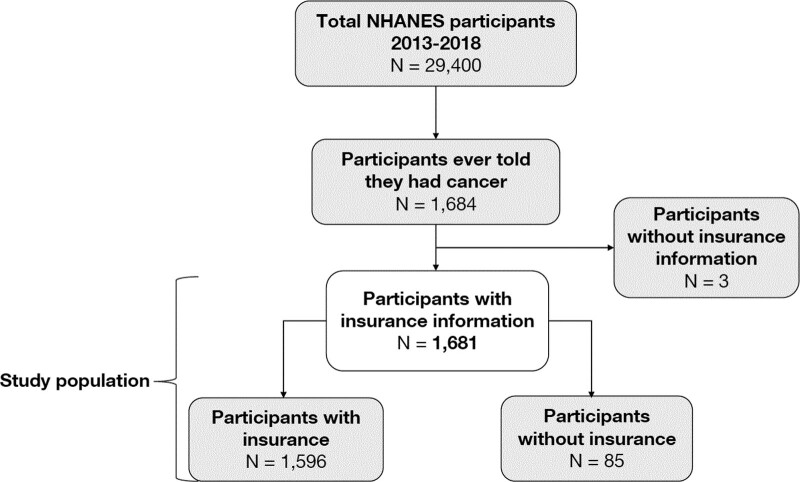
Those participants (aged 20 years and above) who reported any previous or current history of cancer (ever told you had cancer or malignancy of any kind) met the inclusion criteria. The outcome of interest was medical uninsurance (are you covered by health insurance or some other kind of health care plan, irrespective of the type of coverage). We excluded participants who did not disclose medical insurance information (yes vs no). We evaluated the association of sociodemographic correlates, such as age, sex, education, race/ethnicity, annual household income, and US birth/length status, with MU. NHANES asked about race/ethnicity using 6 categories: Mexican American, other Hispanic, non-Hispanic White, non-Hispanic Black, non-Hispanic Asian and other races, including multiracial individuals. We combined Mexican American and other Hispanic group as a single Hispanic group as both groups were relatively small. We combined non-Hispanic Asian and other race including multiracial individuals groups for the same reason. A flow diagram of the study population selection process is shown in Figure 1.
Figure 1.
Flow diagram showing the selection process of study population.
For the US birth/length status, we combined 2 NHANES questions. In the first question, participants were asked if they were born in the United States. In the second question, those who were not born in the United States were asked about their length of stay in the United States. Answers to these 2 questions were combined to create a unified variable for US birth/length status.
2.3. Statistical analyses
We divided the cancer population with insurance information into 2 groups: medically insured and uninsured. We used Chi-square and t-test procedures to check the distribution of categorical and continuous variables in insured and uninsured groups, respectively. To describe categorical variables, we used counts and percentages. For the distribution of continuous variables, we used mean and standard errors. A 2-sided P value of < 0.05 was considered significant for a difference among groups. We performed a bivariate logistic regression model to evaluate the association of individual sociodemographic attributes and MU and calculated the unadjusted odds ratios (UOR) of uninsurance. Finally, we performed a multivariate logistic regression model, evaluated the association of the same sociodemographic attributes (when considered together) and MU, and calculated the adjusted odds ratio (AOR). Proc survey procedures were used to perform data analysis to incorporate the survey design features. We used interview weights (WTINT2YR/3), strata (SDMVSTRA), and cluster (SDMVPSU) variables during survey procedures. For subgroup or subset analyses, we used table statement in the surveyfreq procedure, whereas domain statement in the survey means procedure. Missing values were dealt with in the NOMCAR statement, as recommended by the NHANES. Data analysis was performed using SAS/STAT software, version 9.4, Copyright (c) 2016 by SAS Institute Inc., Cary, NC, USA.
3. Results
The total sampled US cancer population was 1681 participants (weighted US population: 25,982,352), with 4.3% ± 0.62 being uninsured (weighted US population of 1,129,421). Among the insured, 64.8% of the total (weighted estimate of 16,840,800) had private insurance, 52.7% (weighted estimate of 13,685,905) had Medicare, and 7.8% had Medicaid (weighted estimate of 2,037,202). The sociodemographic attributes of the population stratified by insurance status are presented in Table 1. Uninsured individuals were about 13.5-year younger than the insured individuals, P < .0001. The proportion of women was much larger in the uninsured category than in the insured category (81.2% ± 5.1 vs 55.0% ± 1.7, P = .0002). Among uninsured, those with less than high school education were 18.6% ± 5.1, whereas this proportion was 8.4% ± 0.6 among insured ones. The percentage of Hispanics in the uninsured group was 18.7% ± 4.0, compared to 5.2% ± 0.7 in the insured group. In the uninsured category, the proportions of non-Hispanic Blacks and other racial group were slightly higher than in the insured category. Among the insured individuals, the proportions of individuals with higher annual household incomes were larger than that of uninsured individuals, but the result insignificant. Those participants with an annual household income greater than $100K were 27.6 ± −2.1 in the insured category compared to 10.0% ± 6.5 in the uninsured category. About 18.2% ± 4.4 of participants in the uninsured category were non-US-born compared to 7.8% ± 0.95 in the insured category (P < .0001). Among uninsured, those who were not US born, 9.7% ± −3.1 of the total had lived in the US for <20 years. This proportion was exceedingly small, up to 1.4% ± 0.3 among the insured.
Table 1.
Sociodemographic attributes of the US cancer population stratified by insurance status using NHANES data 2013–2018.
| Variable | Total | Insured | Uninsured | P | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| n* = 1681 | n = 1596 | n = 85 | ||||||||
| N† = 25,982,352 | N = 24,852,930 | N = 1129,421 | ||||||||
| n | N | % ± SE | n | N | % ± SE | n | N | % ± SE | ||
| Age, mean ± SE | 63.4 ± 0.49 | 64.0 ± 0.49 | 50.5 ± 1.51 | <.0001 | ||||||
| Sex | .0002 | |||||||||
| Male | 780 | 11,391,983 | 43.8 ± 1.6 | 759 | 11,179,409 | 45.0 ± 1.7 | 21 | 212,573 | 18.8 ± 5.1 | |
| Female | 901 | 14,590,369 | 56.2 ± 1.6 | 837 | 13,673,521 | 55.0 ± 1.7 | 64 | 916,848 | 81.2 ± 5.1 | |
| Education | 0.0010 | |||||||||
| <High school graduate | 285 | 2289,136 | 8.8 ± 0.6 | 259 | 2083,022 | 8.4 ± 0.6 | 26 | 206,114 | 18.6 ± 5.1 | |
| High school graduate | 361 | 5345,715 | 20.6 ± 1.4 | 344 | 5143,771 | 20.7 ± 1.4 | 17 | 201,944 | 18.2 ± 5.0 | |
| Some college or associate degree | 577 | 8743,648 | 33.7 ± 1.6 | 546 | 8168,070 | 33.0 ± 1.6 | 31 | 575,578 | 51.9 ± 10.0 | |
| College grad or more | 455 | 9579,661 | 36.9 ± 2.1 | 445 | 9453,419 | 38.0 ± 2.1 | 10 | 126,242 | 11.4 ± 5.5 | |
| Race/Ethnicity | <.0001 | |||||||||
| Hispanic | 253 | 1510,057 | 5.8 ± 0.8 | 223 | 1299,221 | 5.2 ± 0.7 | 30 | 210,836 | 18.7 ± 4.0 | |
| Non-Hispanic White | 1051 | 21,870,023 | 84.2 ± 1.4 | 1012 | 21,074,633 | 84.8 ± 1.5 | 39 | 795,390 | 70.4 ± 5.1 | |
| Non-Hispanic Black | 240 | 1326,909 | 5.1 ± 0.7 | 230 | 1268,307 | 5.1 ± 0.7 | 10 | 58,603 | 5.2 ± 1.6 | |
| Other | 137 | 1275,363 | 4.9 ± 0.8 | 131 | 1210,770 | 4.9 ± 0.9 | 6 | 64,593 | 5.7 ± 2.8 | |
| Annual Household Income | 0.0822 | |||||||||
| <$20K | 348 | 3168,850 | 12.9 ± 1.1 | 328 | 2993,801 | 12.7 ± 1.1 | 20 | 175,049 | 17.6 ± 5.5 | |
| $20K-$44,999 | 526 | 6847,272 | 27.9 ± 1.7 | 489 | 6383,214 | 27.1 ± 1.7 | 37 | 464,059 | 46.7 ± 8.5 | |
| $45K-$74,999 | 301 | 5351,490 | 21.8 ± 1.8 | 291 | 5179,606 | 22.0 ± 1.8 | 10 | 171,884 | 17.3 ± 7.3 | |
| $75K-$99,999 | 123 | 2549,658 | 10.4 ± 1.2 | 117 | 2467,480 | 10.5 ± 1.3 | 6 | 82,178 | 8.3 ± 4.7 | |
| >$100K | 279 | 6594,498 | 26.9 ± 2.1 | 276 | 6494,872 | 27.6 ± 2.1 | 3 | 99,626 | 10.0 ± 6.5 | |
| US Birth/Length Status | <.0001 | |||||||||
| US born | 1400 | 23,843,474 | 92.0 +/1.0 | 1345 | 22,919,859 | 92.4 ± 0.9 | 55 | 923,615 | 83.1 ± 4.0 | |
| Non-US born with LOS < 20 yrs | 56 | 456,615 | 1.8 ± 0.3 | 41 | 348,630 | 1.4 ± 0.3 | 15 | 107,984 | 9.7 ± 3.1 | |
| Non-US born with LOS 20–39 yrs | 98 | 674,839 | 2.6 ± 0.5 | 87 | 621,686 | 2.5 ± 0.5 | 11 | 53,153 | 4.8 ± 1.7 | |
| Non-US born with LOS ≥ 40 yrs | 117 | 938,330 | 3.6 ± 0.5 | 114 | 912,165 | 3.7 ± 0.5 | 3 | 26,165 | 2.4 ± 1.1 | |
All the bold values are significant.
K = thousands, LOS = length of stay in US, n = actual individual observed in the sample, N = estimated weighted frequency of the individuals with similar observation in the population, SE = standard error.
*acute individual observed in the sample.
†estimated weighted frequency of the individuals with similar observation in the population.
Missing values: Education = 3, Annual Household Income = 104, US Birth/Length Status = 10.
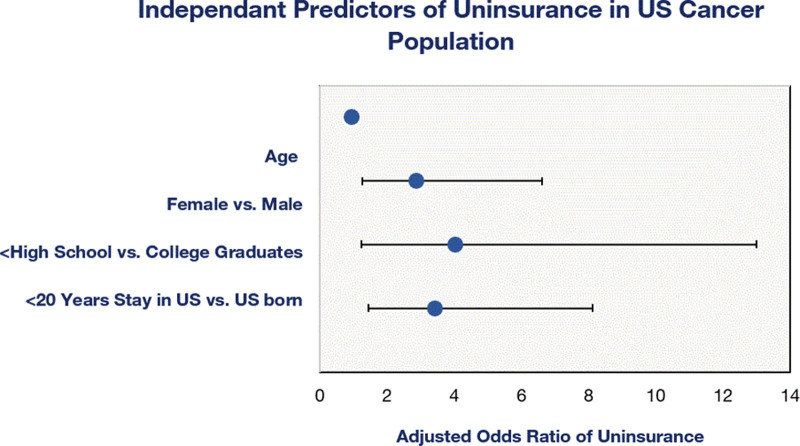
Using bivariate logistic regression models (Table 2), we determined the association between sociodemographic factors as predictors and MU as outcome and found that the odds of being uninsured were 6% lower in 1-year older participants (UOR: 0.94, 95% CI: 0.93–0.96). The female sex had 3.53-fold higher odds (95% CI: 1.73–7.19) of MU compared to males. Hispanics had 4.30-fold higher odds (95% CI: 2.45–7.54) of being uninsured than non-Hispanic Whites. When referencing college graduates, those with less than high school education, and with some college or associated degree had 7.41 times (95% CI: 2.51–21.86) and 5.28 times (95% CI: 1.43–19.46) higher odds of MU. Compared to the US natives, those who were not born in the US and lived in the US for <20 years had 7.69-fold (95% CI: 3.32–17.82) higher odds of MU. Referencing the individuals who earned an annual household income less than $20K, the odds of MU increased for those with an annual household income of 20K–$44,999 but then decreased for those with earnings greater than $45K; the results, however, were not significant. In the multivariate logistic regression (Table 3), age (AOR: 0.95, 95% CI: 0.93–0.96), female sex (AOR: 2.88, 95% CI: 1.25–6.62), <high school education (AOR: 4.02, 95% CI: 1.24–13.00), and non-US birth with <20 years of stay (AOR: 3.42, 95% CI: 1.44–8.11) in the US were independent predictors of MU (Fig. 2). Race/ethnicity (including Hispanics) and annual household income were not significant predictors of MU in multivariate analysis.
Table 2.
Bivariate logistic regression analysis for predictors of medical uninsurance in the US cancer population from NHANES data 2013–2018.
| Predictor | UOR (95% CI) of uninsurance vs insurance |
|---|---|
| Age | 0.94 (0.93–0.96) |
| Gender | |
| Male | REF |
| Female | 3.53 (1.73–7.19) |
| Race/Ethnicity | |
| Non-Hispanic White | REF |
| Non-Hispanic Black | 1.22 (0.64–2.35) |
| Non-Hispanic other races | 1.41 (0.44–4.53) |
| Hispanics | 4.30 (2.45–7.54) |
| Education | |
| College graduates | REF |
| <High school | 7.41 (2.51–21.86) |
| High school/GED | 2.94 (0.92–9.43) |
| Some college/associate degree | 5.28 (1.43–19.46) |
| US birth/length status | |
| US born | REF |
| Non-US born with LOS < 20 yrs | 7.69 (3.32–17.82) |
| Non-US born with LOS 20–39 yrs | 2.12 (0.87–5.17) |
| Non-US born with LOS ≥ 40 yrs | 0.71 (0.27–1.90) |
| Annual household income | |
| <$20K | REF |
| $20K–$44,999 | 1.24 (0.59–2.65) |
| $45K–$74,999 | 0.57 (0.19–1.73) |
| $75K–$99,999 | 0.57 (0.13–2.45) |
| ≥$100K | 0.26 (0.05–1.40) |
CI = confidence interval, GED = graduate equivalency degree, K = thousands, LOS = length of stay in US, REF = reference, UOR = unadjusted odds ratio.
Table 3.
Multivariate logistic regression analysis for the predictors of medical uninsurance in the US cancer population from NHANES data 2013–2018.
| Predictor | AOR (95% CI) of uninsurance vs insurance |
|---|---|
| Age | 0.95 (0.93–0.96) |
| Gender | |
| Male | REF |
| Female | 2.88 (1.25–6.62) |
| Race/Ethnicity | |
| Non-Hispanic White | REF |
| Non-Hispanic Black | 1.06 (0.46–2.44) |
| Non-Hispanic other races | 0.97 (0.28–3.40) |
| Hispanics | 1.02 (0.44–2.34) |
| Education | |
| College graduates | REF |
| <High school | 4.02 (1.24–13.00) |
| High school/GED | 2.12 (0.64–7.11) |
| Some college/associate degree | 3.15 (0.76–13.09) |
| US birth/length status | |
| US born | REF |
| Non-US born with LOS < 20 yrs | 3.42 (1.44–8.11) |
| Non-US born with LOS 20–39 yrs | 1.57 (0.56–4.37) |
| Non-US born with LOS ≥ 40 yrs | 0.44 (0.09–2.24) |
| Annual household income | |
| <$20K | REF |
| $20K–$44,999 | 1.88 (0.90–3.91) |
| $45K–$74,999 | 1.12 (0.32–3.90) |
| $75K–$99,999 | 0.86 (0.19–3.83) |
| ≥$100K | 0.56 (0.10–3.30) |
AOR = adjusted odds ratio, CI = confidence interval, GED = graduate equivalency degree, K = thousands, LOS = length of stay, REF = reference.
Figure 2.
Independent predictors of medical uninsurance in US cancer population with associated adjusted odds ratios (blue circles show odds ratios and horizonal error bars show 95% confidence intervals. Error bar for age is not visible as confidence interval for age is very narrow, 0.93–0.96).
4. Discussion
Medical insurance plays a significant role in more accessible access to healthcare, which is especially important in providing uninterrupted and standard care to patients with chronic diseases such as cancer. Cancer is one of the most expensive conditions in the United States, and even those who have insurance end up paying 20% to 30% of the treatment cost out of their pocket and suffer medical financial hardships.[8] Therefore, one could deduce that the out-of-pocket payment would be 100% when uninsured with cancer and may result in potential forgoing or delaying lifesaving care.[8] According to the US Census Bureau report, approximately 27.5 million (8.5%) Americans in 2018 were uninsured. Moreover, there was an increase of roughly 2 million more uninsured individuals in 2018 than in 2017. Private insurance accounted for 67.3% of the insured population, whereas 34.4% had public insurance.[9] In this study, we reviewed NHANES data in the cancer population in association with medical coverage and factors that might impact it across different groups. Our study showed that younger patients with cancer had higher MU rates than older patients. Previous studies have reported a similar association between younger age and MU and found an association between medical noncoverage and adverse cancer outcomes such as metastatic presentation, undertreatment, and higher mortality.[10] Though ACA ensures some protection for young adults (<26 years), prohibitively higher premiums for those below 40 years may compel them to opt out of the insurance, given the lack of affordability. According to the Center for Medicare and Medicaid Services (CMS), young adults have the highest MU rates, with only 30% being insured. They also have lower access to employer-based insurance compared to older employees due to entry level and early career jobs. One in 6 young adults has chronic illnesses, for example, cancer or diabetes. Therefore, the notion that young adults do not need medical insurance is a myth.[11]
In our study, women had higher odds (AOR: 2.88, 95% CI: 1.25–6.62) of MU than men. It is no wonder that uninsured women would have lower rates of pap smears, mammograms, and colorectal cancer screenings.[12] MU is also attributed to a late breast cancer diagnosis and higher mortality even when adjusted for confounders.[13,14] A review of population-based state cancer registries showed that MU is associated with nonstandard chemotherapy and maintenance regimens.[15] Uninsurance is associated with poor outcomes among women with invasive cervical cancer.[16] Education level affected insurance coverage in our study, with individuals with less than high school education having a higher MU rate than college graduates, AOR: 4.02, 95% CI: 1.24–13.00. Similar findings were noted in the 2015 National Health Interview survey data, in which individuals who did not have high school diplomas had higher uninsurance rates, irrespective of employment. The MU rate was 2 to 3 times higher for individuals with no high school diploma than for those with at least a high school degree.[17]
Hispanics in our analysis had higher odds of MU when compared with Whites in the unadjusted model (UOR: 4.30, 95% CI: 2.45–7.54) but when adjusted for age, sex, education, US birth/length status, and annual household income, these results became insignificant (AOR: 1.02, 95% CI: 0.44–2.34) pointing to the fact that race/ethnicity does not contribute independently to medical noncoverage. Previous studies have shown that people of color have a longstanding disparity in accessing healthcare and receiving standard of care compared to whites.[4] The etiology of poor and disparate disease outcomes in people of color is multifactorial; one of the factors is uninsurance, apart from many other socio-cultural barriers. Colored minorities, such as Hispanics, were more likely to be uninsured before ACA. After ACA, a decline in the uninsured rate among people of color, mainly Hispanics (32.6–19.1%), was reported between 2010 and 2016. Despite this, the MU disparity between people of color and their white counterparts never disappeared. Following 2017, uninsurance rates increased across the board because of federal policy changes. As of 2019, nonelderly Hispanics (26%), American Indians/Alaskan Natives (25%), and Blacks (14%) were more likely to be uninsured than Whites (9%). A more considerable disparity in MU among people of color existed among those aged 19 to 64, given their lower private insurance rates, that is, 48% for Hispanics and 52% for Blacks compared to 74% for Whites. States without Medicaid expansion programs also have twice MU rates in people of color compared to the states with ACA Medicaid expansion programs.[18] Although ACA attempted to narrow the medical coverage gap for disadvantaged communities, other factors still drive the disparities and effect outcomes specifically related to cancer care in affected communities.[19] US birth/length status is one of the health determinants that may influence medical coverage. Those who were not born in the US but lived in the US for <20 years were more likely to be uninsured compared to US citizens in our study, even when adjusted for other factors (AOR: 3.42, 95% CI: 1.44–8.11). The annual household incomes greater than $75K were protective against uninsurance in the adjusted model, but the results were not significant.
This study highlights various social determinants of health that might be associated with MU disparity among cancer survivors, such as young age, female sex, lower education, and non-US birth status with <20 years of stay in the country. The influence of race/ethnicity was eliminated when we incorporated the impact of the aforementioned factors, which are more prevalent in Hispanics. To improve community health and cancer-related outcomes, underprivileged societies continue to demand a special attention. Cancer financial support programs that target high-risk populations and ensure they do not lose medical coverage can help reduce disparities in health outcomes between insured and uninsured individuals. Providing healthcare coverage is the first step toward improving outcomes in high-risk individuals diagnosed with cancer. This step should pair with easy access to healthcare facilities, the availability of well-structured community organizations, and healthcare agencies in disadvantaged areas.[20] To devise better public health interventions, it is critical to look at various factors contributing to MU, especially among cancer patients. We recommend a proactive and systematic screening of such factors during patients’ first encounter in their cancer care with the help of social workers and cancer navigators. Social workers and cancer navigators’ workforce should be culturally competent or have sufficient resources to deal with minority groups such as Hispanics and non-US-born individuals. Individuals with the potential of having MU in the future should be followed beyond their cancer treatment and remission and should be screened for MU periodically when they are lost to follow-up.
This study had several limitations associated with the data collected from the NHANES data registry. MU and its association with social determinants are complex. MU data vary across states owing to differences in population structures and policies across state lines. The data included in the analysis were obtained from states with variable insurance and ACA coverage guidelines. The information on insurance status from the available data may not be the true representative of insurance status, as seen in other studies, the possibility of uninsured patients with a new diagnosis of cancer enrolling in Medicaid shortly after the diagnosis. Last but not least, the proportion of those without insurance was much smaller than those who were insured. Therefore, comparison of these groups may give unstable estimates and will need to be interpretated with caution. In logistic regression models, sample sizes further dropped and gave wider confidence intervals due to smaller subgroups. Unmeasured confounding is still possible, as in any observational study, and this analysis does not account for all possible exposures or variables. Future research should focus on a better understanding of the effects of insurance coverage, along with the complex socioeconomic dynamics related to diagnosis, treatment, and outcomes in various cancers.
Author contributions
AW formulated the research question and performed data analysis and final editing of the article. He also wrote the methods section. BA helped with the literature review and collection of NHANES data. AM and MK wrote the Introduction and Results sections, respectively. BKJ and the UK helped with part of the discussion, figures, and tables. HE has been involved in research appraisal, discussion, and final editing.
Abbreviations:
- ACA =
- affordable care act
- AOR =
- adjusted odds ratio
- CDC =
- centers for disease control and prevention
- CI =
- confidence interval
- MU =
- medical uninsurance
- NCHS =
- National Center for Health Statistics
- NHANES =
- National Health and Nutritional Examination Survey
- UOR =
- unadjusted odds ratio
- US =
- United States
The datasets generated during and/or analyzed during the current study are publicly available.
The authors have no funding and conflicts of interest to disclose.
How to cite this article: Wahab A, Abdelazeem B, Masood A, Khakwani M, Kumar Jakka B, Koduru U, Ehsan H. Association of medical uninsurance with sociodemographic attributes in US cancer population: A cross-sectional study of NHANES data 2013 to 2018. Medicine 2022;101:38(e30539).
Contributor Information
Basel Abdelazeem, Email: baselelramly@gmail.com.
Adeel Masood, Email: adeelmasood100@gmail.com.
Maria Khakwani, Email: Mkhakwani03@gmail.com.
Bharath Kumar Jakka, Email: drbharath.j@gmail.com.
Ujwala Koduru, Email: sunshineujwal255@gmail.com.
Hamid Ehsan, Email: Hamidehsan173@gmail.com.
References
- [1].Minas TZ, Kiely M, Ajao A, Ambs S. An overview of cancer health disparities: new approaches and insights and why they matter. Carcinogenesis. 2021;42:2–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. 2011;32:381–98. [DOI] [PubMed] [Google Scholar]
- [3].Jemal A, Thun MJ, Ward EE, Henley SJ, Cokkinides VE, Murray TE. Mortality from leading causes by education and race in the United States, 2001. Am J Prev Med. 2008;34:1–8. [DOI] [PubMed] [Google Scholar]
- [4].Singh GK, Jemal A. Socioeconomic and racial/ethnic disparities in cancer mortality, incidence, and survival in the United States, 1950-2014: over six decades of changing patterns and widening inequalities. J Environ Public Health. 2017;2017:2819372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Goel MS, Wee CC, McCarthy EP, Davis RB, Ngo-Metzger Q, Phillips RS. Racial and ethnic disparities in cancer screening: the importance of foreign birth as a barrier to care. J Gen Intern Med. 2003;18:1028–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Pan HY, Walker GV, Grant SR, et al. Insurance status and racial disparities in cancer-specific mortality in the United States: a population-based analysis. Cancer Epidemiol Biomarkers Prev. 2017;26:869–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Centers for Disease Control and Prevention (CDC). National Center for Health Statistics (NCHS). National Health and Nutrition Examination Survey Data. Hyattsville MUSDoH. Hyattsville, MD: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention. 2020. Available at: https://wwwn.cdc.gov/nchs/nhanes/default.aspx. [Access date December 2, 2021]. [Google Scholar]
- [8].Yabroff KR, Gansler T, Wender RC, Cullen KJ, Brawley OW. Minimizing the burden of cancer in the United States: goals for a high-performing health care system. CA Cancer J Clin. 2019;69:166–83. [DOI] [PubMed] [Google Scholar]
- [9].Berchick ER, Hood E, Barnett JC. Health insurance coverage in the United States: 2018. Washington, DC: U.S. Department of Commerce, U.S. CENSUS BUREAU. U.S. Government Printing Office. 2019. Available at: https://www.census.gov/content/dam/Census/library/publications/2019/demo/p60-267.pdf [access date December 2, 2021]. [Google Scholar]
- [10].Aizer AA, Falit B, Mendu ML, et al. Cancer-specific outcomes among young adults without health insurance. J Clin Oncol. 2014;32:2025–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Centers for Medicare and Medicaid Services. Young adults and the affordable care act: protecting young adults and eliminating burdens on families and businesses. CMS. 2010. Available at: https://www.cms.gov/CCIIO/Resources/Files/adult_child_fact_sheet. [Access date December 2, 2021]. [Google Scholar]
- [12].Shi L, Lebrun LA, Zhu J, Tsai J. Cancer screening among racial/ethnic and insurance groups in the United States: a comparison of disparities in 2000 and 2008. J Health Care Poor Underserved. 2011;22:945–61. [DOI] [PubMed] [Google Scholar]
- [13].Ko NY, Hong S, Winn RA, Calip GS. Association of insurance status and racial disparities with the detection of early-stage breast cancer. JAMA Oncol. 2020;6:385–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Ayanian JZ, Kohler BA, Abe T, Epstein AM. The relation between health insurance coverage and clinical outcomes among women with breast cancer. N Engl J Med. 1993;329:326–31. [DOI] [PubMed] [Google Scholar]
- [15].Wu XC, Lund MJ, Kimmick GG, et al. Influence of race, insurance, socioeconomic status, and hospital type on receipt of guideline-concordant adjuvant systemic therapy for locoregional breast cancers. J Clin Oncol. 2012;30:142–50. [DOI] [PubMed] [Google Scholar]
- [16].Churilla T, Egleston B, Dong Y, et al. Disparities in the management and outcome of cervical cancer in the United States according to health insurance status. Gynecol Oncol. 2016;141:516–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Cohen RA, Martinez ME, Zammitti EP. Health insurance coverage: early release of estimates from the National Health Interview Survey, 2015. 2016. Available at: https://www.cdc.gov/nchs/data/nhis/earlyrelease/insur201508.pdf [access date December 2, 2021].
- [18].Artiga S, Hill L, Orgera K, Damico A. Health coverage by race and Ethnicity, 2010–2019. 2021. Available at: https://www.kff.org/racial-equity-and-health-policy/issue-brief/health-coverage-by-race-and-ethnicity/ [access date December 2, 2021].
- [19].Abdelsattar ZM, Hendren S, Wong SL. The impact of health insurance on cancer care in disadvantaged communities. Cancer. 2017;123:1219–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Marlow NM, Pavluck AL, Bian J, Ward EM, Halpern MT. The relationship between insurance coverage and cancer care: a literature synthesis. 2009. Available at: https://www.ncbi.nlm.nih.gov/books/NBK542737/pdf/Bookshelf_NBK542737.pdf. [Access date December 02, 2021]. [PubMed]