Abstract
Background:
Adults experiencing homelessness have much higher rates of alcohol misuse than housed individuals. This study describes the development and preliminary effectiveness of a smartphone-based, just-in-time adaptive intervention (JITAI) to reduce alcohol use among adults experiencing homelessness.
Methods:
We conducted a pilot trial (N = 41; mean age [SD] = 45.2 [11.5]; 19.5% women) of the Smart-T Alcohol JITAI where participants completed brief ecological momentary assessments (EMAs) each day, received personalized treatment messages following each EMA, and accessed on-demand intervention content for 4 weeks. The prediction algorithm and treatment messages were developed based on an independent but similar sample as part of the trial. We examined three drinking outcomes: daily drinking (yes/no), drinks per day, and heavy episodic drinking, controlling for scores on the Alcohol Use Disorders Identification Test (AUDIT) at baseline, age, and sex using quadratic growth curve models.
Results:
Over the 4-week period, participants showed a decline in all alcohol use outcomes. Participants also reported high levels of satisfaction with the JITAI.
Conclusions:
Use of the Smart-T Alcohol JITAI was well received and provided encouraging evidence that it may reduce any drinking, drinks per day, and heavy episodic drinking among adults experiencing homelessness.
Keywords: alcohol, ecological momentary assessment, homeless, just-in-time adaptive intervention, treatment
INTRODUCTION
In 2020, more than 580,000 people in the United States experienced homelessness on a given night (United States Department of Housing and Urban Development, 2021). The 2020 statistics on homelessness show a fourth consecutive year of increase in the number of people experiencing homelessness, including a substantial increase in the number of people who are chronically homeless. People experiencing homelessness are more likely to be men, African American, and have an average life expectancy that is substantially shorter than domiciled adults (Morrison, 2009; United States Department of Housing and Urban Development, 2021). One primary contributor to the increased morbidity and mortality is the elevated rates of alcohol use: Adults experiencing homelessness are up to eight times more likely than adults in the general population to have an alcohol use disorder (AUD; Hasin et al., 2007; Fazel et al., 2008). In addition to exacerbating health risks, alcohol use contributes to the onset and chronicity of homelessness by inhibiting progress toward employment, housing, and a better quality of life (North et al., 1998; United States Conference of Mayors, 2008).
People experiencing homelessness face several barriers to engaging in AUD treatment, including lack of stable housing (Wenzel et al., 2001), fractured social networks (Kertesz et al., 2006), and high rates of co-occurring disorders (Gonzalez & Rosenheck, 2002; Neisler et al., 2019; Reitzel et al., 2020). In fact, many of the barriers to access alcohol treatment in the general population are exacerbated for people experiencing homelessness, including lengthy waitlists, cost, and transportation problems (Brubaker et al., 2013; Upshur et al., 2018). At the same time, key factors that would ordinarily predict success in AUD treatment (e.g., good health status, higher socioeconomic status, and no co-occurring disorders) are less prevalent among people experiencing homelessness (Moos & Moos, 2007). Moreover, AUDs tend to be highly dynamic, with multiple individual and contextual factors influencing alcohol use (Maisto et al., 2014; Morgenstern et al., 2014). This may be especially true for people experiencing homelessness, whose environments tend to be less structured and whose social networks are often saturated with people who drink heavily (Rhoades et al., 2011; Wenzel et al., 2009).
Smartphone-based interventions offer numerous advantages over traditional service delivery methods for this population, including portability, personalization, and easy access in real-world contexts (Ali et al., 2016; Carreiro et al., 2020; Kazemi et al., 2017; Marcolino et al., 2018). A majority of people experiencing homelessness already own mobile phones, with rates approaching 80% in some studies (Heaslip et al., 2021), and charging stations widely available in locations such as homeless shelters and libraries. Moreover, this number is expected to increase with US government programs now providing free smartphones and data plans to eligible low-income adults (https://www.safelinkwireless.com/). People who are homeless report the value of having a smartphone in terms of maintaining social connections, the ability to reach healthcare providers, and the ability to obtain help when needed (Heaslip et al., 2021). Thus, smartphone interventions have the potential for significant public health impact in this group given the majority access to smartphones, reduced access to traditional interventions, and high need.
Despite the proliferation of mHealth interventions, relatively few studies have examined the effectiveness of smartphone-based apps for adults with alcohol misuse, and none, to our knowledge, have been tested specifically among adults experiencing homelessness. A 2020 review identified 19 unique smartphone apps designed to reduce alcohol use that had been evaluated for effectiveness (Colbert et al., 2020). Of the seven apps designed for adults with AUD, only three were evaluated in randomized clinical trials (Colbert et al., 2020). One app that focused on individuals entering residential alcohol treatment, the Addiction-Comprehensive Health Enhancement Support System (A-CHESS), reduced heavy drinking days across the intervention window and at follow-up, relative to usual care (Gustafson et al., 2014). The A-CHESS app included advice, motivational messages, on-demand resources, a GPS alert when approaching high-risk locations, and the ability to alert key people if relapse was imminent. We are not aware of any smartphone-based interventions that have been designed specifically for adults with alcohol misuse who are experiencing homelessness.
This paper reports on the development and preliminary effectiveness of a smartphone-based just-in-time adaptive intervention (JITAI) for reducing alcohol use among people experiencing homelessness–Smart-T Alcohol (Businelle et al., 2020). Like A-CHESS, Smart-T Alcohol provides on-demand motivational messages to help people avoid or reduce drinking. In addition, Smart-T Alcohol assesses momentary risk factors for imminent drinking via EMA and automatically delivers tailored messages at the end of each EMA based on individual and contextual factors, including current drinking goal (if any), time of day, and imminent risk factors for drinking (Walters et al., 2021). This approach directly targets real-time influences on alcohol use without having to rely on treatment providers or a sober social support network, neither of which may be present for these individuals.
The Smart-T Alcohol trial had three phases. In the first phase previously reported, we collected EMA data from 78 adults experiencing homelessness (mean age [SD] = 46.6 [9.2]; 15.4% women) who reported hazardous drinking (Walters et al., 2021). Participants completed up to five EMAs per day for 4 weeks. The first assessment was prompted 30 min after the participant's self-reported waking time, and four were prompted at random times throughout the day. Participants were also asked to self-initiate an assessment if/when they were about to drink.
In Phase 2, we used Phase 1 data to develop algorithms and messages that could be used in real-time to predict and intervene with drinking. First, we used a predictive machine learning model to test 36 potential event-level covariates, which were reduced to the following seven variables: urge to drink, alcohol easily available, confidence that alcohol would improve mood, feeling depressed, low commitment to being alcohol-free, not interacting with someone drinking alcohol, and being indoors. The final prediction model correctly predicted 82% (i.e., sensitivity) of imminent alcohol use episodes within 4 h of the first drink of the day and correctly identified 76% of nondrinking episodes (i.e., specificity).
We then developed a database of 839 messages that provided both automated and on-demand content. Automated messages were tailored to a person's current risk of drinking as determined by the risk algorithm which took into account the probability of drinking based on the prediction model (i.e., Low vs. High Risk), participants' self-assessment of their drinking probability (i.e., likely to drink today) or actual drinking (i.e., already drank), and leading momentary imminent risk indicators (i.e., urge to drink, negative mood, and social/availability of alcohol). Individuals with low imminent drinking risk received Level-1 messages, which were focused on general wellness, for instance, spending time with supportive people, setting and achieving goals, and engaging in healthy behaviors. Individuals who were deemed at risk of imminent drinking received Level-2 messages that were tailored to (1) the person's imminent risk indicators and (2) current drinking goal. People whose drinking goal was to stay sober versus moderate their drinking received appropriate messages that were tailored to that goal. People who were at high risk of imminent drinking but did not have a current drinking goal received Level-4 messages that encouraged them to reconsider their need for change. Participants who already drank that day received either Level-4 messages focused on motivation (if they indicated no current drinking goal) or Level-3 messages focused on reframing the drinking episode as a learning experience and offering strategies to handle situations differently in the future. We further refined messages based on time of day (i.e., morning messages focused on planning, mid-day messages focused on immediate activities, and evening messages focused on reflection on the day's activities). For instance, if a person's risk of imminent drinking was estimated to be high (Level 2), the highest-rated drinking trigger was negative mood, and the person's drinking goal for the day was to stay sober (e.g., avoid all drinking), a message in the morning might be phrased:
Make sure you are avoiding “dead time” today. Keep yourself busy with things you enjoy and take your time to do things well. If you are busy and engaged in your work, you are more likely to stay sober.
On the contrary, if a person's imminent risk was estimated to be high, the leading risk indicator was social/availability, and the person's drinking goal was to cut back or moderate their drinking, a message might be phrased:
Try to avoid people, places, and things that remind you of drinking. Seek out people and situations that make it easier for you to cut down on drinking.
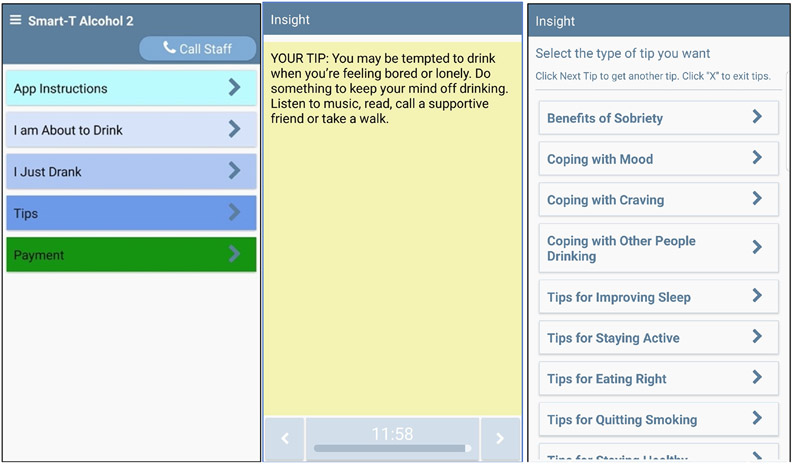
Finally, on-demand messages (“tips”) could be accessed at any time on a variety of topics, such as the benefits of sobriety and ways to manage urges, mood, availability of alcohol, diet, physical activity, sleep, and safety. Figure 1 shows screenshots of the Smart-T Alcohol homescreen, a sample message, and the tips menu.
FIGURE 1.
Example screens of the Smart-T Alcohol App
The current study reports the results of a single-arm pilot trial (Phase 3) of the Smart-T Alcohol JITAI using an independent but similar sample to the one used to develop the prediction model, algorithms, and treatment messages (for more information, see Appendix S1). Since this was a single-arm trial, we report changes in the probability of any drinking, probability of heavy drinking, and drinks per day during the 28 days of the intervention period.
MATERIALS AND METHODS
Participants and procedures
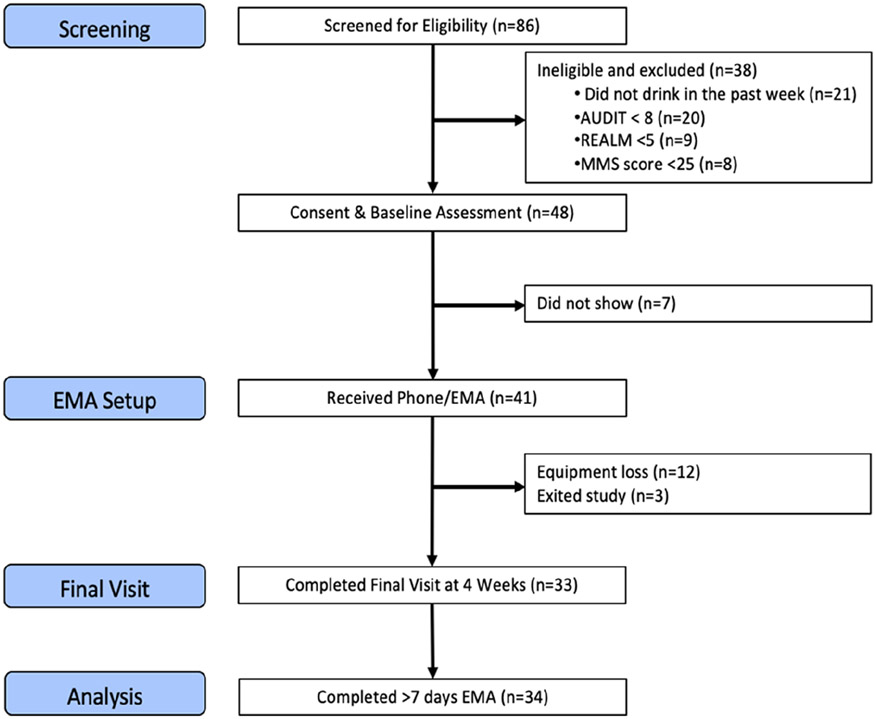
Participants were recruited from a homeless shelter in a major metropolitan area of the United States. Eligible participants (1) scored eight or more on the Alcohol Use Disorders Identification Test (AUDIT; Saunders et al., 1993); (2) consumed at least one standard drink in the past week; (3) were receiving services at the homeless shelter; (4) agreed to complete the baseline and follow-up visits; (5) scored >6th-grade English literacy on the REALM-SF (Arozullah et al., 2007); and (6) scored ≥24 on the Mini-Mental State Exam (Tombaugh & McIntyre, 1992). Approximately 5 days after the baseline interview, participants attended a setup visit where they received the phone. Phones were Samsung S3 or S7 models preloaded with an app developed using the Insight™ mHealth platform (https://healthpromotionresearch.org/Mobile-Health-Technology). We provided phones because at the outset of the study, smartphone ownership and model compatibility were not always assured. Thereafter, participants completed up to five EMAs each day for 28 days. Figure 2 shows the CONSORT participant flowchart.
FIGURE 2.
CONSORT diagram
A total of 41 participants (mean age [SD] = 45.2 [11.5]; 19.5% women) completed the setup visit where they received the phone. There were no significant differences between those who completed the setup visit and those who did not. Participants were paid $25 for completing the baseline assessment, $25 for completing the 4-week follow-up assessment, up to $25 per week for completing EMA assessments (based on percent completed), and $25 for returning the equipment at the end of the study. Data collection took place from August 2020 to July 2021. This study was registered at ClinicalTrials.gov (NCT03746808), and the North Texas Regional IRB approved the research protocol.
Measures
Alcohol outcomes
Alcohol outcomes included (1) whether participants drank (i.e., any drinking); (2) how many drinks they had (i.e., number of drinks); and (3) whether they reported heavy episodic drinking (HED) on each day during 28 days. These outcomes were determined based on EMA responses.
Alcohol use on a given day was determined based on any positive answer to the following questions: (1) “Have you consumed alcohol today?,” which was scheduled up to five times per day (daily diary and random EMAs); (2) “Did you just drink or are you about to drink alcohol?,” which was asked when participants self-initiated drinking-related EMAs; and (3) “Did you drink any alcohol yesterday?,” which was asked during the daily morning assessment about drinking the previous day. We counted a day as a drinking day (coded as 1) if there was a positive answer to the “any alcohol use” question. In the absence of a valid positive answer for the morning diary question, alcohol use was coded as 0 only when participants answered “No” to all alcohol use EMA questions (e.g., random EMAs without any self-initiated drinking-related EMAs) the previous day. If a participant reported no drinking for some EMAs but had missing values/nonresponse for other EMAs within the same day and the next day's daily diary was not completed, alcohol use was coded as missing for that day.
The number of drinks per day was assessed during the morning assessment each day (i.e., “How many standard drinks did you have yesterday?”). Heavy episodic drinking (HED) was determined by the number of drinks per day reported (i.e., 5 or more drinks for men; 4 or more drinks for women).
Covariates
Baseline scores on the AUDIT, sex assigned at birth, and age in years were included as covariates in all analyses. A 30-day timeline follow-back (TLFB; Sobell & Sobell, 1992) provided an estimate of baseline drinking.
Analysis plan
We limited the analysis to participants (n = 34) who had at least 8 days of either EMA or daily diary reports. Because this pilot study aimed to examine the preliminary effectiveness of a new app, we deemed it necessary to have more than one week of exposure to the Smart-T Alcohol JITAI (out of a maximum of 28 days) to reasonably test whether the app was efficacious. However, an intention-to-treat (ITT) analytic approach without any minimum app use (i.e., receiving EMA or daily diary) and a more stringent filter of at least 2 weeks of app use were also analyzed as a sensitivity check.
We conducted growth curve analyses with generalized linear mixed-effects models to examine trajectories of alcohol outcomes for participants over the entire 4-week course of the study. EMA data were aggregated to the day-level data following the procedure described in Mun et al. (2021) and detailed in the Measures section. Generalized linear mixed-effects models can better handle missing EMA data and data clustering due to repeated measures than repeated measures ANOVA. This analysis allowed more flexible modeling of outcomes in-process and at the study endpoint, while retaining the most granular data.
A mixed-effects negative binomial regression model was used for the number of drinks per day to account for overdispersion, and a mixed-effects logistic regression was used for any drinking and HED on a given day. Trajectories were examined with sequential model comparisons to determine the most appropriate form among models representing no change, linear change, and quadratic change over the 28 days. Time trends were specified (i.e., a linear change noted as “day,” a quadratic change noted as “day × day”). All models included AUDIT score, self-identified sex, and age as covariates to adjust for between-person differences. Within-person effects and within-by-between-person effects were accounted for by modeling random effects of the intercept and slope(s) across individuals. Chi-square difference tests and relative model fit comparisons were used to determine the most parsimonious and well-fitting model. Finally, inference was made on the individual effect estimates from the best-fitting growth curve model. Missing data were assumed missing at random and handled with maximum likelihood estimation. Models were fitted using the lme4 package (Bates et al., 2015) in the R statistical program (R Core Team, 2021). Results were visualized using the sjPlot and sjstats packages (Lüdecke, 2021a, 2021b).
RESULTS
Baseline descriptives
Table 1 shows baseline characteristics of participants who completed the EMA setup visit. At baseline, participants reported relatively high AUDIT scores (23.8; SD = 8.7) and an average of 3.6 drinks per day (SD = 2.9). We subsequently included age, sex, and AUDIT scores as covariates to adjust for baseline individual differences.
TABLE 1.
Characteristics of participants who completed the EMA setup visit (n = 41)
| Variable | |
|---|---|
| Age (M, SD) | 45.2 (11.5) |
| Sex (Male, %) | 80.5 |
| Race | |
| White, % | 70.7 |
| Black, % | 24.4 |
| AUDIT score (mean, SD) | 23.8 (8.7) |
| Alcohol consumption | |
| Drinking days, % | 55.5 |
| Number of drinks per day (mean, SD) | 3.6 (2.9) |
| Heavy episodic drinking days, % | 31.4 |
Abbreviation: AUDIT, alcohol use disorders identification test.
Alcohol outcomes over 4 weeks
Trajectories of all alcohol outcomes were best characterized by a quadratic model in which drinking behaviors initially increased before significantly decreasing in the latter half of the study (Figure 3). Table 2 provides estimates from the generalized mixed-effects models with up to quadratic change. The significant main effects of Day and Day × Day indicated a decline in drinking outcomes over the course of the study, with the rate of decline accelerating as the study went on. As shown in Figure 3, participants generally showed a flat trajectory or a slight increase in drinking outcomes over the first 2 weeks, followed by declines below initial levels. There were relatively large variance components for the random intercept, and the conditional R2 (which accounts for both fixed and random effects) was quite large, indicating substantial individual differences in drinking between participants. AUDIT score at baseline was a significant covariate, but age and sex were not statistically significant (see limitations for a note on sex). Note that uncertainty surrounding the average trajectory became smaller as the study went on, which suggests that participants' drinking became more similar over time.
FIGURE 3.
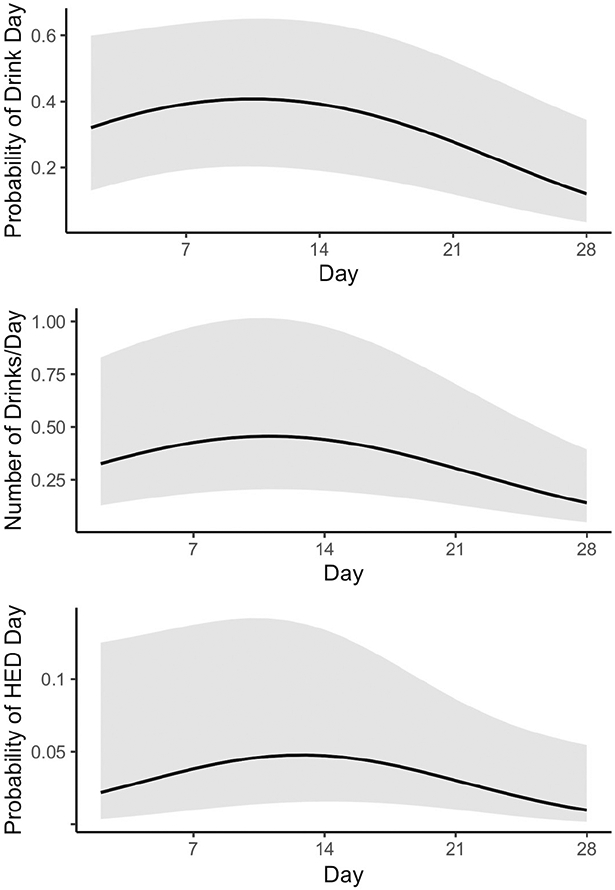
Model-implied trajectories of alcohol outcomes. The top panel plots the probability of drinking on a given day. The mid panel plots the number of drinks per day. The bottom panel plots the probability of heavy episodic drinking on a given day.
TABLE 2.
Generalized linear mixed-effects models estimating the 4-week trajectories of alcohol outcomes
| Drink day probability (NID = 77, Ndays = 1493) |
Number of drinks/day (NID = 77, Ndays = 1336) |
HED day probability (NID = 77, Ndays = 1336) |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | RR | 95% CI | p | OR | 95% CI | p | |
| Intercept | 0.00 | 0.00, 0.11 | <0.001 | 0.01 | 0.00, 0.08 | <0.001 | 0.00 | 0.00, 0.01 | <0.001 |
| Day | 0.27 | 0.10, 0.69 | 0.007 | 0.38 | 0.22, 0.65 | <0.001 | 0.21 | 0.05, 0.95 | 0.043 |
| Day × Day | 0.77 | 0.61, 0.96 | 0.023 | 0.82 | 0.73, 0.92 | 0.001 | 0.70 | 0.49, 1.00 | 0.048 |
| AUDIT | 1.07 | 1.00, 1.14 | 0.012 | 1.14 | 1.04, 1.25 | 0.004 | 1.18 | 1.06, 1.31 | 0.003 |
| Sex (female = 1) | 1.41 | 0.13, 15.3 | 0.780 | 1.03 | 0.15, 7.12 | 0.978 | 2.72 | 0.31, 23.86 | 0.368 |
| Age | 1.98 | 0.91, 4.31 | 0.083 | 1.34 | 0.71, 2.55 | 0.369 | 1.44 | 0.72, 2.89 | 0.305 |
| Random effects | |||||||||
| σ2 | 3.29 | 1.53 | 3.29 | ||||||
| τ00 | 6.01ID | 3.79ID | 1.81ID | ||||||
| τ11 | 0.18ID.Day | 0.12ID.Day | 0.28ID.Day | ||||||
| ρ01 | 0.41ID | 0.41ID | 0.04ID | ||||||
| ICC | 0.62 | 0.69 | 0.48 | ||||||
| Marginal R2/Cond. R2 | 0.192/0.690 | 0.219/0.755 | 0.220/0.596 | ||||||
Abbreviations: AUDIT, alcohol use disorders identification test; CI, confidence interval; HED, heavy episodic drinking; Ndays, total reported days; NID, number of subjects; OR, odds ratio; RR, incidence rate ratio.
Siginificance of bold indicates the p < 0.05.
As a sensitivity analysis, the models were refit in an ITT analytic framework with no filtering for number of days that participants interacted with the Smart-T alcohol app. The pattern of results from the additional analyses (significance of quadratic trend, direction of effects, etc.) was consistent with the results reported (Table S2).
Perceived usefulness
Most participants who attended the final follow-up visit (N = 33) reported that the number of prompted assessments was appropriate (12.1% “Too High”; 12.1% “Not Enough”; 75.8% “About Right”) and felt the app increased their awareness of their thoughts, feelings, and behaviors (90.9% “Mostly Yes” or “Definitely Yes”). Participants also reported that the on-demand “Tips” feature was useful (M = 3.9, SD = 1.0; 1 to 5 scale where 1 = Not at all Useful and 5 = Extremely Useful), that the app as a whole helped reduce alcohol consumption (M = 3.6, SD = 1.1; 1 to 5 scale where 1 = Not at all Helpful, and 5 = Extremely Helpful), that they were generally interested in using the app in the future (M = 3.8, SD = 1.5; 1 to 5 scale where 1 = Not at all Interested and 5 = Extremely Interested), and that they would likely recommend the app to a friend (M = 4.0, SD = 1.4; 1 to 5 scale where 1 = Very Unlikely and 5 = Very Likely). Finally, app use data indicated that of those who received the phone (n = 41), over 95% used the on-demand “tips” feature at least once. The most commonly viewed tips were related to the benefits of sobriety (27.4% of views), strategies for improving sleep (17.6%), coping with cravings (11.6%), and coping with other people drinking (11.1%).
DISCUSSION
This paper summarizes alcohol use outcomes among adults experiencing homelessness while they were using the Smart-T Alcohol JITAI. Over 4 weeks, participants showed a decline in the probability of any drinking, heavy episodic drinking, and drinks per day. Moreover, participants reported high levels of perceived usefulness of the JITAI and an overwhelming majority accessed the on-demand tips features.
To our knowledge, this is the first JITAI specifically designed for adults with alcohol misuse who are experiencing homelessness. Prior JITAIs for alcohol use have most often been designed for young adults (O'Donnell et al., 2019; Suffoletto et al., 2018; Wright et al., 2018) or domiciled adults (Attwood et al., 2017; Dulin et al., 2014; Gonzalez & Dulin, 2015), both of whom tend to be more stable populations with better access to traditional treatment services. This study is also unique in that real-time risk assessments of imminent drinking were derived from a machine learning algorithm that incorporated empirically established risk factors for drinking, including urge to drink, negative mood, and social/availability of alcohol (Walters et al., 2021). Prior JITAIs for alcohol use have utilized geographic location (i.e., GPS) (Attwood et al., 2017; Dulin et al., 2014; Gonzalez & Dulin, 2015) or a single factor (e.g., self-reported drinking or low self-efficacy to avoid drinking) to determine when to deliver treatment messages (Suffoletto et al., 2018; Weitzel et al., 2007). Finally, Smart-T Alcohol is the first JITAI to deliver treatment messages based on participants' real-time motivation, drinking goal, and risk factors.
This study had a number of limitations, notably the small sample size and a single-arm repeated measures design. Because this study was not a randomized controlled trial, the preliminary effectiveness evidence should be cautiously interpreted. In addition, we report comparisons between Phase 1 and Phase 3 participants only in the supplemental materials because of potentially systematic differences between the phase conditions. Furthermore, the sample only included a small number of women, leading to large variability (i.e., wide CIs) and instability in the estimates of sex differences. However, the proportion of women in this study is comparable with the proportion of women who experience homelessness (Statista Research Department, 2021). Larger samples with more female participants are needed. An additional limitation of this study is the reliance on self-reported drinking, psychosocial context, motivation, and environmental variables needed to tailor treatment messages. While our prior work found good concordance between EMA reports and transdermal alcohol readings (Mun et al., 2021), frequent EMAs may be burdensome to some participants. Although a majority of participants (75.8%) in this study believed that the amount of EMAs was “about right,” future studies may consider ways to reduce the number of questions or assessment points and/or collect data passively (e.g., via independent biosensors or integrated phone sensors) to reduce participant burden (Perski et al., 2021). Payment for participants to engage in the mHealth app and EMA completion is an inherent limitation with unclear implementation implications. Given that this was a treatment development trial, it was critical to provide subject payment to keep people engaged. However, an app can be optimized to stand on its own without the need to pay people to complete EMAs. The advantage of app-based interventions is the relatively low effort that is required to receive assistance (e.g, multiple 1 to 2 min surveys), rather than arranging transportation to attend hour-long sessions (with additional barriers such as stigma). Telehealth and online options for alcohol treatment have become more important in recent years following the COVID-19 pandemic experience. Hence, identifying optimal strategies for engaging people in our and similar apps without payment remains a critical future research direction.
Immediate future directions for this work include a randomized controlled trial of the efficacy of Smart-T Alcohol in a larger sample of adults experiencing homelessness that also includes longer-term follow-up. In a larger test, we would likely be able to install the app directly on the participant's personal device and assist them with obtaining one if necessary. Additionally, continued efforts to refine the prediction algorithm and improve message tailoring may bolster treatment effects. Recent studies on cigarette smoking suggest images of the current environment may have particular value in predicting behavioral outcomes and integration of a similar approach may be particularly helpful for improving risk predictions (Engelhard et al., 2019, 2021). This approach could also be extended to other intervention targets relevant to this population (e.g., opioid use) or other at-risk populations that might benefit from such an approach (e.g., people who were recently housed). Overall, the results of this study suggest that smartphone-based JITAIs may be feasible and potentially efficacious in this population that has substantial barriers to entering and completing traditional AUD treatments. A majority of people experiencing homelessness already have and use cell phones, a number that will undoubtedly increase in the coming years (Rhoades et al., 2017). Indeed, a number of ongoing and recently completed studies are exploring the utility of mobile health interventions for this population (Gonzalez et al., 2018; Sheoran et al., 2016; Thompson Jr et al., 2020). Accordingly, JITAIs for alcohol use may offer a promising and timely method for improving drinking outcomes, quality of life, and overall health for this highly disadvantaged and understudied population.
Supplementary Material
ACKNOWLEDGMENT
We would like to thank Charles Williams, Shelly Li, and the staff at the Bridge Homeless Recovery Center for their help with participant recruitment and engagement.
FUNDING INFORMATION
This study was supported by NIAAA grant R34AA024584 to MSB and STW; NIAAA grants R01AA019511 and K02AA028630 awarded to E-YM; the Oklahoma Tobacco Settlement Endowment Trust (TSET) grant R21-02 to MSB; and used the Stephenson Cancer Center's mHealth Shared Resource (NCI grant P30CA225520).
Footnotes
CONFLICT OF INTEREST
MSB is an inventor of the Insight mHealth Platform and receives royalties related to use of this platform. However, MSB did not receive royalties for the use of the platform for this study.
SUPPORTING INFORMATION
Additional supporting information can be found online in the Supporting Information section at the end of this article.
REFERENCES
- Ali EE, Chew L & Yap KY-L (2016) Evolution and current status of mhealth research: a systematic review. BMJ Innovations, 2, 33–40. [Google Scholar]
- Arozullah AM, Yarnold PR, Bennett CL, Soltysik RC, Wolf MS, Ferreira RM et al. (2007) Development and validation of a short-form, rapid estimate of adult literacy in medicine. Medical Care, 45(11), 1026–1033. [DOI] [PubMed] [Google Scholar]
- Attwood S, Parke H, Larsen J & Morton KL (2017) Using a mobile health application to reduce alcohol consumption: a mixed-methods evaluation of the drinkaware track & calculate units application. BMC Public Health, 17(1), 394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bates D, Maechler M, Bolker B & Walker S (2015) Fitting linear mixed-effects models using lme4. Journal of Statistical Software, 67(1), 1–48. [Google Scholar]
- Brubaker MD, Amatea EA, Torres-Rivera E, Miller MD & Nabors L (2013) Barriers and supports to substance abuse service use among homeless adults. Journal of Addictions and Offender Counseling, 34(2), 81–98. [Google Scholar]
- Businelle MS, Walters ST, Mun E-Y, Kirchner TR, Hébert ET & Li X (2020) Reducing drinking among people experiencing homelessness: protocol for the development and testing of a just-in-time adaptive intervention. JMIR Research Protocols, 9(4), e15610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carreiro S, Newcomb M, Leach R, Ostrowski S, Boudreaux ED & Amante D (2020) Current reporting of usability and impact of mHealth interventions for substance use disorder: a systematic review. Drug and Alcohol Dependence, 215, 108201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colbert S, Thornton L & Richmond R (2020) Smartphone apps for managing alcohol consumption: a literature review. Addiction Science & Clinical Practice, 15(1), 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dulin PL, Gonzalez VM & Campbell K (2014) Results of a pilot test of a self-administered smartphone-based treatment system for alcohol use disorders: usability and early outcomes. Substance Abuse, 35(2), 168–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engelhard MM, Oliver JA, Henao R, Hallyburton M, Carin LE, Conklin C et al. (2019) Identifying smoking environments from images of daily life with deep learning. JAMA Network Open, 2(8), e197939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engelhard MM, D'Arcy J, Oliver JA, Kozink R & McClernon FJ (2021) Prediction of smoking risk from repeated sampling of environmental images: model validation. Journal of Medical Internet Research, 23(11), e27875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fazel S, Khosla V, Doll H & Geddes J (2008) The prevalence of mental disorders among the homeless in western countries: systematic review and meta-regression analysis. PLoS Medicine, 5(12), e225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez VM & Dulin PL (2015) Comparison of a smartphone app for alcohol use disorders with an internet-based intervention plus bibliotherapy: a pilot study. Journal of Consulting and Clinical Psychology, 83(2), 335–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez G & Rosenheck RA (2002) Outcomes and service use among homeless persons with serious mental illness and substance abuse. Psychiatric Services, 53(4), 437–446. [DOI] [PubMed] [Google Scholar]
- Gonzalez JMR, Businelle MS, Kendzor D, Staton M, North CS & Swartz M (2018) Using mHealth to increase treatment utilization among recently incarcerated homeless adults (Link2Care): protocol for a randomized controlled trial. JMIR Research Protocols, 7(6), e9868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafson DH, McTavish FM, Chih MY, Atwood AK, Johnson RA, Boyle MG et al. (2014) A smartphone application to support recovery from alcoholism: a randomized clinical trial. JAMA Psychiatry, 71(5), 566–572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E & Grant BF (2007) Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry, 64(7), 830–842. [DOI] [PubMed] [Google Scholar]
- Heaslip V, Richer S, Simkhada B, Dogan H & Green S (2021) Use of technology to promote health and wellbeing of people who are homeless: a systematic review. International Journal of Environmental Research and Public Health, 18(13), 6845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazemi DM, Borsari B, Levine MJ, Li S, Lamberson KA & Matta LA (2017) A systematic review of the mHealth interventions to prevent alcohol and substance abuse. Journal of Health Communication, 22(5), 413–432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kertesz SG, Larson MJ, Cheng DM, Tucker JA, Winter M, Mullins A et al. (2006) Need and non-need factors associated with addiction treatment utilization in a cohort of homeless and housed urban poor. Medical Care, 44(3), 225–233. [DOI] [PubMed] [Google Scholar]
- Lüdecke D (2021a) sjPlot: data visualization for statistics in social science (version 2.8.10) [Computer Program]. [Google Scholar]
- Lüdecke D (2021b) sjstats: statistical functions for regression models (version 0.18.1) [Computer Program]. [Google Scholar]
- Maisto SA, Kirouac M & Witkiewitz K (2014) Alcohol use disorder clinical course research: informing clinicians' treatment planning now and in the future. Journal of Studies on Alcohol and Drugs, 75(5), 799–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcolino MS, Oliveira JAQ, D'Agostino M, Ribeiro AL, Alkmim MBM & Novillo-Ortiz D (2018) The impact of mHealth interventions: systematic review of systematic reviews. JMIR mHealth and uHealth, 6(1), e23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos RH & Moos BS (2007) Treated and untreated alcohol-use disorders: course and predictors of remission and relapse. Evaluation Review, 31(6), 564–584. [DOI] [PubMed] [Google Scholar]
- Morgenstern J, Kuerbis A & Muench F (2014) Ecological momentary assessment and alcohol use disorder treatment. Alcohol Research: Current Reviews, 36(1), 101–109. [PMC free article] [PubMed] [Google Scholar]
- Morrison DS (2009) Homelessness as an independent risk factor for mortality: results from a retrospective cohort study. International Journal of Epidemiology, 38(3), 877–883. [DOI] [PubMed] [Google Scholar]
- Mun E-Y, Li X, Businelle MS, Hebert ET, Tan Z, Barnett NP et al. (2021) Ecological momentary assessment of alcohol consumption and its concordance with transdermal alcohol detection and timeline follow-back self-report among adults experiencing homelessness. Alcoholism: Clinical and Experimental Research, 45(4), 864–876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neisler J, Shree S, Reitzel LR, Chen T-A, Kendzor DE, Obasi EM et al. (2019) Characterizing alcohol use behaviors among homeless men and women. American Journal of Health Behavior, 43(1), 37–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- North CS, Pollio DE, Smith EM & Spitznagel EL (1998) Correlates of early onset and chronicity of homelessness in a large urban homeless population. The Journal of Nervous and Mental Disease, 186(7), 393–400. [DOI] [PubMed] [Google Scholar]
- O'Donnell R, Richardson B, Fuller-Tyszkiewicz M & Staiger PK (2019) Delivering personalized protective behavioral drinking strategies via a smartphone intervention: a pilot study. International Journal of Behavioral Medicine, 26(4), 401–414. [DOI] [PubMed] [Google Scholar]
- Perski O, Hébert ET, Naughton F, Hekler EB, Brown J & Businelle MS (2021) Technology-mediated just-in-time adaptive interventions (JITAIs) to reduce harmful substance use: a systematic review. Addiction, 2021, 1–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Core Team. (2021) R: a language and environment for statistical computing [Computer Program].
- Reitzel LR, Chinamuthevi S, Daundasekara SS, Hernandez DC, Chen T-A, Harkara Y et al. (2020) Association of problematic alcohol use and food insecurity among homeless men and women. International Journal of Environmental Research and Public Health, 17(10), 3631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhoades H, Wenzel SL, Golinelli D, Tucker JS, Kennedy DP, Green HD et al. (2011) The social context of homeless men's substance use. Drug and Alcohol Dependence, 118(2–3), 320–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhoades H, Wenzel SL, Rice E, Winetrobe H & Henwood B (2017) No digital divide? Technology use among homeless adults. Journal of Social Distress and Homeless, 26(1), 73–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR & Grant M (1993) Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction, 88(6), 791–804. [DOI] [PubMed] [Google Scholar]
- Sheoran B, Silva CL, Lykens JE, Gamedze L, Williams S, Ford JV et al. (2016) YTH StreetConnect: development and usability of a mobile app for homeless and unstably housed youth. JMIR mHealth and uHealth, 4(3), e82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC & Sobell MB (1992) Timeline follow-back: a technique for assessing self-reported alcohol consumption. In: Litten RZ & Allen JP (Eds.) Measuring alcohol consumption: psychosocial and biochemical methods. Totowa, NJ: Humana Press, pp. 41–72. [Google Scholar]
- Statista Research Department. (2021) Share of homeless individuals in the U.S. by gender 2020 [Online]. Available at: https://www.statista.com/statistics/962171/share-homeless-people-us-gender [Accessed 10th June 2022].
- Suffoletto B, Chung T, Muench F, Monti P & Clark DB (2018) A text message intervention with adaptive goal support to reduce alcohol consumption among non-treatment-seeking young adults: non-randomized clinical trial with voluntary length of enrollment. JMIR mHealth and uHealth, 6(2), e8530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson RG Jr., Aivadyan C, Stohl M, Aharonovich E & Hasin DS (2020) Smartphone application plus brief motivational intervention reduces substance use and sexual risk behaviors among homeless young adults: results from a randomized controlled trial. Psychology of Addictive Behaviors, 34(6), 641–649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tombaugh TN & McIntyre NJ (1992) The mini-mental state examination: a comprehensive review. Journal of the American Geriatrics Society, 40(9), 922–935. [DOI] [PubMed] [Google Scholar]
- United States Conference of Mayors. (2008) Hunger and homelessness survey: a status report on hunger and homelessness in America's cities. Washington, DC: United States Conference of Mayors. [Google Scholar]
- United States Department of Housing and Urban Development. (2021) The 2020 annual homeless assessment report (AHAR) to congress, part 1: point-in time estimates of homelessness. Washington, DC: United States Department of Housing and Urban Development. [Google Scholar]
- Upshur CC, Jenkins D, Weinreb L, Gelberg L & Orvek EA (2018) Homeless women's service use, barriers, and motivation for participating in substance use treatment. The American Journal of Drug and Alcohol Abuse, 44(2), 252–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters ST, Businelle MS, Suchting R, Li X, Hébert ET & Mun E-Y (2021) Using machine learning to identify predictors of imminent drinking and create tailored messages for at-risk drinkers experiencing homelessness. Journal of Substance Abuse Treatment, 127, 108417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weitzel JA, Bernhardt JM, Usdan S, Mays D & Glanz K (2007) Using wireless handheld computers and tailored text messaging to reduce negative consequences of drinking alcohol. Journal of Studies on Alcohol and Drugs, 68(4), 534–537. [DOI] [PubMed] [Google Scholar]
- Wenzel SL, Audrey Burnam M, Koegel P, Morton SC, Miu A, Jinnett KJ et al. (2001) Access to inpatient or residential substance abuse treatment among homeless adults with alcohol or other drug use disorders. Medical Care, 39(11), 1158–1169. [DOI] [PubMed] [Google Scholar]
- Wenzel SL, Green HD Jr., Tucker JS, Golinelli D, Kennedy DP, Ryan G et al. (2009) The social context of homeless women's alcohol and drug use. Drug and Alcohol Dependence, 105(1–2), 16–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright C, Dietze PM, Agius PA, Kuntsche E, Livingston M, Black OC et al. (2018) Mobile phone-based ecological momentary intervention to reduce young adults' alcohol use in the event: a three-armed randomized controlled trial. JMIR mHealth and uHealth, 6(7), e9324. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.