Abstract
Sleep is an ancient and evolutionarily conserved biological process that, when disturbed, increases the risk for a variety of diseases in people, including diabetes, cardiovascular disease, kidney disease, and cancer. Although results from epidemiological studies support the link between insufficient sleep and an increased risk of obesity, the directionality of this link is unknown. Results from short‐term controlled clinical studies, conducted almost exclusively in people who are normal weight, demonstrate that sleep restriction increases hunger, appetite, energy intake, and body weight. However, the authors are not aware of any studies that have evaluated the effect of more than 3 weeks of experimental sleep restriction on obesity risk factors, and few studies have been conducted in people with preexisting obesity. This Perspective reviews the link between insufficient sleep and obesity risk and the potential therapeutic effects of sleep extension in people with chronic sleep insufficiency.
INTRODUCTION
Insufficient sleep can be defined as a failure to obtain the adequate amount of sleep needed to support optimal mental and physiological function. Insufficient sleep is common in modern society and is likely caused by a variety of factors, including work, social and family obligations, stress, sleep disorders, and other medical illnesses. The American Academy of Sleep Medicine defines acute insufficient sleep as a reduction in total sleep time, usually lasting less than 1 week, whereas chronic insufficient sleep is defined as curtailed sleep that persists for 3 months or longer [1].
Insufficient sleep is associated with an increased risk of developing obesity, characterized by an inverse dose–response association between sleep duration and obesity risk. Data from a meta‐analysis of prospective cohort studies demonstrate that each 1‐hour decrease in sleep from a sleep duration of 7 h/d is associated with a 9% increased risk of obesity [2]. However, epidemiological studies are unable to determine causality, and it is not clear whether insufficient sleep causes obesity or obesity causes insufficient sleep and/or additional sleep disturbances, or both (Figure 1).
FIGURE 1.
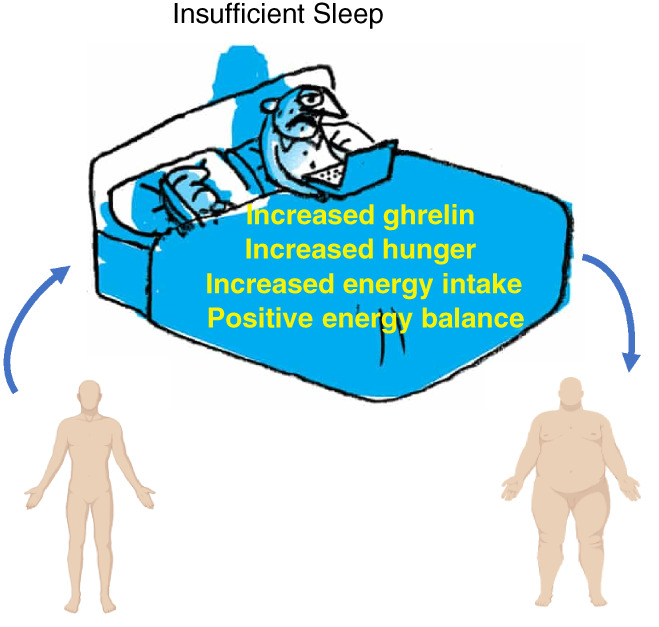
Conceptual model linking insufficient sleep to weight gain and obesity risk
INSUFFICIENT SLEEP
Data from controlled clinical studies conducted in lean participants demonstrate that short‐term experimental sleep restriction (e.g., 1 night of total sleep deprivation; 2 days of 4‐hour time‐in‐bed [TIB]; 4 days of 5‐hour TIB) increases appetite and cravings for high‐carbohydrate‐rich foods, which causes increased food consumption and weight gain [3], despite an increase in energy expenditure associated with sleep restriction [4]. A meta‐analysis of 41 randomized controlled trials found that experimental sleep restriction (4‐ to 5‐hour as compared with 8‐ to 9‐hour TIB for 1‐14 days) in healthy adults increases subjective feelings of hunger and increases brain activity in response to food stimuli in central reward centers [5]. As little as 2 days of sleep restriction (4‐hour vs. 10‐hour TIB) induces changes in plasma concentrations of appetitive hormones, including a decrease in the satiety hormone leptin and an increase in the hunger hormone ghrelin [3]. Furthermore, 1 week of 8.5‐hour versus 4.5‐hour TIB in a controlled inpatient setting increases fasting plasma ghrelin concentration and blunts the normal postprandial decline in ghrelin [3]. Finally, 2 weeks of a similar reduction in sleep duration (4‐hour TIB) leads to an increase in energy intake of more than 300 kcal/d, a 0.5 kg increase in body weight, and an 11% increase in visceral fat volume [6]. Controlled studies of slightly longer sleep restriction also demonstrate that sleep loss induces weight gain. Reducing habitual sleep duration by 1.5 h/night for 3 weeks in free‐living healthy men is associated with an approximate 1‐kg increase in body weight [7]. Together, these data suggest that alterations in energy balance, appetitive hormones, hunger, and appetite, as well as subsequent eating behavior induced by acute sleep restriction in people who are normal weight, can induce weight gain. However, we are not aware of any studies that have evaluated the effects of more than 3 weeks of experimental sleep restriction or impaired sleep quality on body weight.
SLEEP EXTENSION
Extending sleep duration in people who have chronic sleep insufficiency may reverse some of the deleterious consequences of sleep loss. However, the effect of sleep extension on food intake and body weight is not clear because of conflicting results from studies that have reported decreases in appetite and sugar intake or no effect on appetite, diet selection, appetitive hormones, energy expenditure, and body weight [8]. The reason for the discordance in outcomes among studies is not clear but it could be related to the amount of the increase in sleep duration. It is possible that the clinical benefits of sleep extension require a minimum threshold of daily sleep of at least 6 h/night. In a recently completed randomized controlled clinical trial, the effects of increasing sleep duration to 8.5 h/night for 2 weeks were evaluated in people with overweight who habitually slept less than 6.5 h/night [9]. During sleep extension, participants reduced their estimated daily energy intake by 270 kcal, without a measurable change in total energy expenditure (assessed by using the doubly labeled water technique), resulting in a small (0.5 kg), but statistically significant, decrease in body weight [9].
CONCLUSION
Acute insufficient sleep combined with ad libitum access to food increases energy expenditure, food intake, and body weight in people who are lean. However, the long‐term effects of experimental sleep restriction (>3 weeks) on the risk of developing obesity are not known. In addition, we are not aware of studies that have evaluated the effect of experimental sleep restriction without dietary manipulations on body weight, hunger and appetite, or neuroendocrine hormones in people with overweight or obesity. Additional studies are needed to do the following: 1) evaluate the effect of longer duration sleep restriction and reduced sleep quality on energy balance and body composition; 2) determine the effect of experimental sleep restriction on body weight in people with overweight/obesity; 3) provide a better understanding of the importance of reduced sleep quality in the pathogenesis of obesity; 4) provide a better understanding of the potential health benefits of sleep extension in people with obesity and chronic sleep insufficiency; and 5) determine whether optimizing sleep as part of a weight management program enhances weight loss.
CONFLICT OF INTEREST
Josiane L. Broussard reports consulting fees from Cellular Longevity, Inc., and Everlywell, Inc., outside the submitted work. Samuel Klein serves on the scientific advisory board for Altimmune and as a consultant for B2M Medical.
Broussard JL, Klein S. Insufficient sleep and obesity: cause or consequence. Obesity (Silver Spring). 2022;30(10):1914‐1916. doi: 10.1002/oby.23539
Funding information National Institutes of Health, Grant/Award Numbers: R01DK125653, R01DK115502, P30DK020579, UL1TR000448
REFERENCES
- 1. American Academy of Sleep Medicine . International Classification of Sleep Disorders. 3rd ed. American Academy of Sleep Medicine; 2014.
- 2. Zhou Q, Zhang M, Hu D. Dose‐response association between sleep duration and obesity risk: a systematic review and meta‐analysis of prospective cohort studies. Sleep Breath. 2019;23:1035‐1045. [DOI] [PubMed] [Google Scholar]
- 3. Hanlon EV, Van Cauter E, Tasali E, Broussard JL. Endocrine physiology in relation to sleep and sleep disturbances. In: Kryger MH, Roth T, Goldstein CA, eds. Principles and Practice of Sleep Medicine. 7th ed. Elsevier; 2021:284‐300. [Google Scholar]
- 4. Markwald RR, Melanson EL, Smith MR, et al. Impact of insufficient sleep on total daily energy expenditure, food intake, and weight gain. Proc Natl Acad Sci USA 2013;110:5695‐5700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Zhu B, Shi C, Park CG, Zhao X, Reutrakul S. Effects of sleep restriction on metabolism‐related parameters in healthy adults: a comprehensive review and meta‐analysis of randomized controlled trials. Sleep Med Rev. 2019;45:18‐30. [DOI] [PubMed] [Google Scholar]
- 6. Covassin N, Singh P, McCrady‐Spitzer SK, et al. Effects of experimental sleep restriction on energy intake, energy expenditure, and visceral obesity. J Am Coll Cardiol. 2022;79:1254‐1265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Robertson MD, Russell‐Jones D, Umpleby AM, Dijk DJ. Effects of three weeks of mild sleep restriction implemented in the home environment on multiple metabolic and endocrine markers in healthy young men. Metabolism. 2013;62:204‐211. [DOI] [PubMed] [Google Scholar]
- 8. Hoddy KK, Potts KS, Bazzano LA, Kirwan JP. Sleep extension: a potential target for obesity treatment. Curr Diab Rep. 2020;20:81. doi: 10.1007/s11892-020-01360-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Tasali E, Wroblewski K, Kahn E, Kilkus J, Schoeller DA. Effect of sleep extension on objectively assessed energy intake among adults with overweight in real‐life settings: a randomized clinical trial. JAMA Intern Med. 2022;182:365‐374. [DOI] [PMC free article] [PubMed] [Google Scholar]


