Abstract
Arthritis patients may show little motivation for physical activity (PA), resulting in a sedentary lifestyle. The primary objective of the study was to investigate whether motivation for PA and fulfillment of PA recommendations were associated with cardiorespiratory fitness in patients with RA. The exploratory objective was to study whether university students could be used as controls for RA patients in future studies of PA motivation. Peak oxygen uptake (VO2peak) was measured in 93 RA patients. The patients and 354 students filled in the Behavioral Regulation in Exercise Questionnaire-2 (BREQ-2). Data were analyzed using structural equation modeling with adjustment for age and sex. The BREQ-2 scores were also compiled to an overall motivational style “Relative Autonomy Index” as previously published. Mean VO2peak for the RA patients was 32.2 (SD: 9.6) mL × min−1 × kg−1. Only 29 patients (31%) fulfilled the current recommendations for PA. BREQ-2 scores were associated with measured VO2peak (standardized coefficient 0.33, p < 0.001). Whether a person fulfilled the current recommendations for PA was a significant mediator of this effect (standardized coefficients: mediated effect; 0.22, p = 0.001, remaining direct effect; 0.11, p = 0.18). The Relative Autonomy Index also significantly predicted measured VO2peak (standardized coefficient 0.30, p < 0.001). The underlying BREQ-2 factor structure was significantly different between RA patients and university students, and comparison of scores would not be adequate. Motivation for PA was significantly associated with measured VO2peak in RA patients. The effect was mediated by whether the patient fulfilled the current recommendations for PA. Addressing and stimulating motivation is important when intervening to increase PA and cardiovascular fitness in RA patients.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00296-021-05079-9.
Keywords: Arthritis, rheumatoid; Motivation; Physical fitness; Exercise test; Physical exercise
Introduction
Around 0.5–1% of the population suffers from rheumatoid arthritis (RA), a chronic inflammatory disease which may affect any synovial joint, but most often affects the small joints of the hands and feet [1]. Without treatment, joint destruction may ensue over time, so early medical treatment guided by the aim of achieving complete remission has become the standard. Even with treatment, patients often experience pain, fatigue, and reduced quality of life [2].
Previous research has shown that RA patients still have an increased mortality rate compared to the general population [3–6]. Low cardiorespiratory fitness is an important mediator, with direct and indirect effects accounting for 23% of the totally 28% excess relative risk of mortality [6]. Thus, in addition to adequate medication, stimulating RA patients to improve their fitness level should be an important goal in the overall treatment plan [7].
Current guidelines for RA include similar recommendations for aerobic PA as given for the general population by the American College of Sports Medicine (ACSM) and the American Heart Association (AHA): namely moderate-intensity PA ≥ 30 min on ≥ 5 days a week (≥ 150 min per week), high-intensity PA ≥ 20 min ≥ 3 times a week (≥ 75 min per week), or a combination of PA at these intensities [8, 9].
Uptake of exercise recommendations is relatively low in the general population, and several studies show that many RA patients are physically inactive and spend numerous sedentary hours daily [10, 11]. This may have many reasons in addition to physical restrictions, including lack of knowledge about the helpful effects of PA, suitable and accessible exercise programs, and social support [12]. Such barriers may act through effects on motivation to perform PA, and the motivational aspects probably differ between RA patients and the general population.
Motivation comprises a person’s reasons for acting or behaving in a specific way. According to self-determination theory, motivation is a multidimensional concept ranging from intrinsic regulation (completely self-determined behavior regulation) through various intermediate styles (extrinsic regulation, namely behavior performed to obtain an external outcome) to amotivation (no intention to perform a behavior, i.e., completely non-self-determined behavior regulation) [13, 14]. The proposed motivational styles cannot be measured directly, and the instrument Behavioral Regulation in Exercise Questionnaire-2 (BREQ-2) has therefore been developed to enable assessment [14, 15]. The psychological needs for competence in dealing with one’s surroundings, relatedness through satisfying social relationships, and autonomy by doing things from self-determination and not from external control or obligation are proposed as important underlying factors [13]. A substantial body of evidence supports self-determination theory in settings like learning and health-related activities including PA [17].
For studies of motivation for PA in arthritis patients, comparison with a "normal" control group is useful to identify areas where fitness programs would need to differ from those intended for the general population. Previous literature has confirmed good performance of BREQ-2 in diverse groups like students [16, 17], office workers [18], blue-collar workers, white-collar workers and members of a bridge club [19], participants in an Internet-based exercise program [20], and female hospital workers and members of a community church group [21].
We hypothesized that motivation for PA is associated with cardiorespiratory fitness. The gold-standard method to measure cardiorespiratory fitness is using cardiopulmonary exercise testing (CPET) [22]. We further hypothesized that whether the patient fulfills the ACSM/AHA recommendations for PA acts as a mediator between motivation and fitness. The primary aim of the present observational study was therefore to investigate the associations among motivation for PA, fulfillment of PA guidelines, and cardiorespiratory fitness measured using treadmill-based CPET in patients with RA. The secondary aim was to translate the BREQ-2 questionnaire to Norwegian and confirm the psychometric properties of the translated version. We also included an exploratory test of whether university students could be used as controls for RA patients with respect to motivational styles for PA measured using BREQ-2 in future studies. For the exploratory study, we hypothesized that the underlying structure of BREQ-2 would be robust to differences between arthritis patients and students.
Methods
This was an observational study.
Participants
For a previously published study regarding cardiorespiratory fitness in RA patients, a convenience sample of 94 individuals performed cardiopulmonary exercise testing (CPET) on a treadmill in 2017–2018 as described below [23]. Diagnosis was confirmed according to the 2010 American College of Rheumatology /European League against Rheumatism 2010 classification criteria [24], and their clinical status was registered. Patients with unstable heart conditions, chronic pulmonary disease necessitating use of oxygen therapy, or physical disability making a treadmill test impossible were excluded. As a pilot test, the participants also filled in a Norwegian version of the BREQ-2 questionnaire, which is further described below. Power calculations were performed for the original study and were therefore not suitable for the present pilot study. The 93 individuals with complete BREQ-2 data were included in the present study. Most patients (n = 87) were recruited from the rheumatology outpatient clinic at St. Olavs University Hospital where they either came for regular follow-up visits or participated in a patient-centered follow-up program. Six patients were included after reading a newsletter from the local arthritis association.
For the exploratory aim, students from the Faculty of Medicine and Health Sciences (n = 248, Student group 1) and Faculty of Information Technology and Electrical Engineering (n = 106, Student group 2) at NTNU—Norwegian University of Science and Technology were included. Students from both faculties were included to achieve a more diverse total control sample. The students were approached before leaving the lecture hall for an intermission and were given oral and written information. Those who wished to participate filled in an anonymous version of the Norwegian BREQ-2 questionnaire, and there were no exclusion criteria.
Main outcome variable
The main outcome variable was measured cardiorespiratory fitness in the RA patients. Performance of CPET has been described in detail previously [23]. In brief, participants had a 6-min warm-up period, whereafter the walking or running speed of the treadmill (Woodway PPS 55, Waukesha, Wisconsin, USA) was adjusted using an individualized protocol to account for any RA-related physical limitations. The participants were fitted with a facemask (7450 Series V2 CPET mask, Hans Rudolph, Shawnee, Kansas, USA) and a heart rate monitor (H7, Polar Electro, Kempele, Finland), and perceived exertion was rated using the RPE Borg Scale [25]. Gas measurements were recorded every 10 s using a mixing chamber ergospirometry system (Metalyzer II, Cortex Biophysik Gmbh, Leipzig, Germany) and workload was increased gradually until exhaustion. The following criteria were used to define maximal oxygen uptake (VO2max): (1) VO2 leveling off (< 2 mL × min−1 × kg−1) despite increase in workload and (2) respiratory exchange ratio ≥ 1.05. If these criteria were not met, the participant’s VO2peak was determined, defined as the mean of the three successive highest VO2 registrations achieved during the CPET. The term VO2peak is used for all patients for simplicity even if 83% qualified for VO2max.
Study factors
The main study factor was the assessed motivation for physical activity as measured by the BREQ-2 questionnaire [15]. The 19 items of the English version of the BREQ-2 questionnaire were translated to Norwegian by a bilingual person and back-translated to English by another bilingual person (Online Resource 1—Norwegian version of the BREQ-2 questionnaire). A style of Norwegian close to everyday language was chosen as opposed to more formal written language. The motivational styles are denoted as (1) intrinsic regulation, where PA is performed because the person finds it enjoyable in itself (for example, “I enjoy my exercise sessions”), (2) identified regulation, where PA may help a person achieve his or her goals (for example, “I value the benefits of exercise”), (3) introjected regulation, where PA is performed to increase one’s self-esteem or avoid negative feelings (for example, “I feel ashamed when I miss an exercise session”), (4) external regulation, where PA is performed due to rewards or punishments given by someone else (for example, “I feel under pressure from my friends/family to exercise"), and (5) amotivation, where the person has no intention to perform PA (for example, “I think exercising is a waste of time”) [15, 18, 26]. The complete list of items is given in Table 1.
Table 1.
BREQ-2 items and scores
| BREQ-2 factor | BREQ-2 itemsa | Persons with rheumatoid arthritis (n = 93) | Student group 1 (n = 248) |
Student group 2 (n = 106) |
|---|---|---|---|---|
| Intrinsic regulation | 3.91 (0.90) | 4.02 (0.87) | 4.05 (0.80) | |
| 4. I exercise because it’s fun | ||||
| 10. I enjoy my exercise sessions | ||||
| 15. I find exercise a pleasurable activity | ||||
| 18. I get pleasure and satisfaction from participating in exercise | ||||
| Identified regulation | 3.91 (0.78) | 4.04 (0.82) | 4.02 (0.89) | |
| 3. I value the benefits of exercise | ||||
| 8. It’s important to me to exercise regularly | ||||
| 14. I think it is important to make the effort to exercise regularly | ||||
| 17. I get restless if I don’t exercise regularly | ||||
| Introjected regulation | 2.36 (0.81) | 2.77 (0.98) | 2.78 (1.06) | |
| 2. I feel guilty when I don’t exercise | ||||
| 7. I feel ashamed when I miss an exercise session | ||||
| 13. I feel like a failure when I haven’t exercised in a while | ||||
| External regulation | 1.34 (0.57) | 1.60 (0.68) | 1.69 (0.63) | |
| 1. I exercise because other people say I should | ||||
| 6. I take part in exercise because my friends/family/partner say I should | ||||
| 11. I exercise because others will not be pleased with me if I don’t | ||||
| 16. I feel under pressure from my friends/family to exercise | ||||
| Amotivation | 1.19 (0.46) | 1.15 (0.37) | 1.20 (0.45) | |
| 5. I don’t see why I should exercise | ||||
| 9. I can’t see why I should bother exercising | ||||
| 12. I don’t see the point in exercising | ||||
| 19. I think exercising is a waste of time | ||||
| Relative autonomy index | NA | 10.9 (5.4) | 10.7 (5.4) | 10.4 (4.8) |
BREQ-2 Behavioral Regulation in Exercise Questionnaire-2, NA not applicable
a[15]
The BREQ-2 items have 5-point Likert scales ranging from 0 (“not true for me”) to 4 (“very true for me”). The mean score of the three to four items related to each factor was calculated, giving the individual’s score for each of the five types of motivation for exercise [15]. A relative autonomy index (RAI) was also calculated where the score for each of the five factors was weighted, and the resulting numbers were summed. The weightings are: Intrinsic regulation: 3, identified regulation: 2, introjected regulation: − 1, external regulation: − 2, amotivation: − 3. The possible RAI values range from − 24 to 20 with higher scores indicating more self-determined motivation [26].
Other variables
The RA patients provided information about the frequency, duration, and intensity of the physical activity they usually perform, which was used to evaluate whether they fulfilled the ACSM/AHA recommendations for PA [8]. For descriptive purposes, RA disease activity was measured by Disease Activity Score 20 (DAS28) including the high-sensitivity C-reactive protein concentration [27]. Assessment of functional status was measured by the modified Health Assessment Questionnaire (mHAQ), which includes eight questions regarding the ability to perform common daily activities during the last week with answers given on a 4-point Likert scale [29]. Use of disease-modifying antirheumatic drugs was registered.
In addition to the BREQ-2 questionnaire, the included students also provided information about their sex and age, but not other demographical or social data.
Procedures
The study was performed in compliance with the Helsinki Declaration and was approved by the Regional Committee for Medical and Health Research Ethics (#20734). All participants gave informed consent.
Statistical analysis
Data are given as frequency (percentage) or mean (standard deviation), and descriptive statistics were compared among groups using the Chi-square test or T test. p values < 0.05 were considered significant.
In the RA patients, associations between motivation, fulfillment of the ACSM/AHA guidelines for PA and VO2peak as outcome were analyzed using Structural Equation Modeling (SEM) [30]. For these analyses, n = 92 due to missing questionnaire data on performed PA for one person. In SEM, a model showing the proposed relationships among the variables is drawn, and the method then tests whether the observed data fit with the model, using a series of common fit indices (Online Resource 2—Common fit indices for structural equation models) [30]: the Chi-square test, root mean squared error of approximation (RMSEA), Tucker Lewis index (TLI), comparative fit index (CFI), and standardized root mean square residual (SRMR). In a standardized model, all variables are measured in the same unit, namely standard deviations. This makes the coefficient sizes directly comparable, which would not be so when for example BREQ-2 scores are measured in numbers from 0 to 4 and age in years. Due to non-normal distributions, standard errors were calculated using the Satorra–Bentler method [15].
The proposed models for the primary aim are shown in Fig. 1. The first model proposed that the five BREQ-2 factors were measurements of a latent variable Motivation for PA, which in turn was associated with the measured VO2peak. The second model was similar, but further proposed that whether the person fulfilled the ACSM/AHA recommendations for PA (yes/no) acted as a mediator between Motivation for PA and the measured VO2peak. Because analysis in a real-world setting would be easier using RAI instead of the five separate BREQ-2 factors, a third model proposed that the calculated RAI was associated with the measured VO2peak, thus not assuming any latent Motivation for PA factor. All models included adjustment for sex and age, which are known to influence VO2peak [11]. Model fit was assessed using the fit indices mentioned above. The sample size was small for SEM, so a sensitivity analysis was performed where the main models were run in bootstrap samples (n = 300) for bias correction of coefficients and standard errors.
Fig. 1.
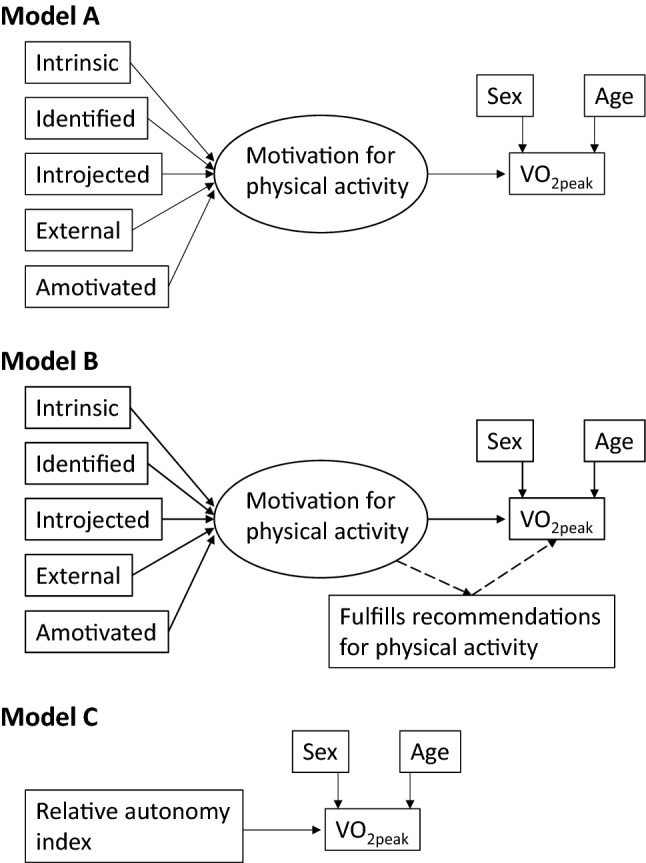
Models for associations of motivation for physical activity and cardiorespiratory fitness. Model A assumes that the BREQ-2 factors together define a latent factor Motivation for physical activity, which in turn predicts the measured VO2peak. Model B assumes that whether the person fulfills the ACSM/AHA recommendations for physical activity (yes/no) is a mediator for the effect of this predictive latent factor. Model C assumes that the calculated relative autonomy index from the BREQ-2 factors may substitute for the individual BREQ-2 factors and the latent Motivation factor. All models were adjusted for sex (0 = woman, 1 = man) and age (years). Coefficients were standardized and their size is therefore directly comparable. ACSM American College of Sports Medicine, AHA American Heart Association, BREQ-2 Behavioral Regulation in Exercise Questionnaire-2, VO2peak peak oxygen uptake
For the secondary aim, namely, to test whether the original BREQ-2 5-factor structure fit well in our data using the translated items, confirmatory factor analysis by means of SEM was employed [29]. Based on item correlations, they are reduced into a set of underlying latent factors, in this case those indicated in the original BREQ-2 publication [15]. The item correlations with these factors are denoted their factor loadings. Model fit was assessed using the fit indices mentioned above. Different models were compared using the likelihood ratio (LR) test. Internal consistency (reliability) of the factors was measured using Cronbach’s alpha, where values > 0.7 are considered good [30].
Details regarding the SEM methods used in the exploratory study to evaluate whether the five BREQ-2 factors could be compared between students and RA patients are given in Online Resource 3—Supplementary methods—Comparison of BREQ-2 factor structure between RA patients and students.
Statistical analysis was performed using Stata/MP (v.16.1, StataCorp, College Station, TX, USA).
Results
Table 2 shows the participant characteristics. Most of the patients were seropositive and had long-standing RA. As expected, the RA patients were significantly older than the students (p < 0.001) (Online Resource 4—Participant characteristics in exploratory study). Only 29 patients (31%) fulfilled the ACSM/AHA recommendations for PA. BREQ-2 results are given in Table 1. Both RA patients and students scored highest on intrinsic and identified regulation and low on amotivation. Mean RAI was between 10 and 11 for both groups.
Table 2.
Participant characteristics
| Variable | Persons with rheumatoid arthritis (n = 93) |
|---|---|
| Women | 68 (73%) |
| Age (years) | 59 (12) |
| Height (m) | 1.69 (0.90) |
| Weight (kg) | 76.4 (12.3) |
| Smoking | |
| Never smoked | 35 (38%) |
| Previous smoker | 51 (55%) |
| Present smoker | 7 (8%) |
| Fulfills ACSM/AHA recommendations | 29 (31%) |
| Disease duration (years) | 12 (9) |
| Seropositive (anti-citrullinated peptide antibody and/or rheumatoid factor positive) | 75 (81%) |
| Uses conventional DMARD | 74 (80%) |
| Uses biological DMARD | 54 (58%) |
| DAS28 | 2.56 (1.04) |
| mHAQ | 0.26 (0.31) |
| Peak oxygen uptake (mL × min−1 × kg−1) | 32.2 (9.6) |
Data are given as number (percent) or mean (SD). Some of the data for persons with rheumatoid arthritis have been published previously [23]
ACSM American College of Sports Medicine, AHA American Heart Association, DAS28 disease activity score including high-sensitivity C-reactive protein concentration, DMARD disease-modifying antirheumatic drug, mHAQ modified Health Assessment Questionnaire
For the main aim regarding motivation and VO2peak in the RA patients, Model A (Fig. 1) had good fit and was therefore compatible with the hypothesis that a latent factor Motivation for PA based on the five BREQ-2 factors was associated with the measured VO2peak (Chi square 15.18, df = 15, p = 0.44, RMSEA = 0.01, TLI = 1.00, CFI = 1.00, SRMR = 0.06). The associations with Motivation for PA were positive and significant for intrinsic and identified regulation, non-significant for introjected regulation, and negative and significant for external motivation and amotivation (Table 3).
Table 3.
Analysis of associations with cardiorespiratory fitness
| Associations with latent factor Motivation for PAa Coefficient (p value) |
Associations with VO2peak Coefficient (p value) |
|||
|---|---|---|---|---|
| Model A | Intrinsic regulation | 0.92 (p < 0.001) | Motivation for PA | 0.33 (p < 0.001) |
|
Identified regulation |
0.78 (p < 0.001) | Sexb | 0.51 (p < 0.001) | |
| Introjected regulation | 0.08 (p = 0.49) | Age | − 0.62 (p < 0.001) | |
| External regulation | − 0.31 (p = 0.01) | |||
| Amotivation | − 0.60 (p < 0.001) | |||
| Model B | Intrinsic regulation | 0.89 (p < 0.001) | Motivation for PA | |
| Direct effect | 0.11 (p = 0.18) | |||
| Indirect effect | 0.22 (p = 0.001) | |||
|
Identified regulation |
0.81 (p < 0.001) | Sex | 0.52 (p < 0.001) | |
| Introjected regulation | 0.09 (p = 0.46) | Age | − 0.61 (p < 0.001) | |
| External regulation | − 0.33 (p = 0.01) | |||
| Amotivation | − 0.61 (p < 0.001) | |||
| Model C | Relative autonomy index | 0.54 (p < 0.001) | ||
| Sex | 0.51 (p < 0.001) | |||
| Age | − 0.63 (p < 0.001) | |||
BREQ-2 Behavioral Regulation in Exercise Questionnaire-2, PA physical activity, RA rheumatoid arthritis
aThe latent factor Motivation for PA is illustrated in Fig. 1
bSex: 0 = female, 1 = male
Model B (Fig. 1, Table 3) showed that whether a person fulfills the recommendations for PA was a significant mediator of the association of Motivation for PA with VO2peak, whereas the direct effect became non-significant. There were minimal changes for the associations of the BREQ-2 factors with motivation for PA. Model B had good fit (Chi square 22.77, df = 21, p = 0.30, RMSEA = 0.026, TLI = 0.99, CFI = 0.99, SRMR = 0.06).
In Model C (Fig. 1, Table 3), RAI was significantly positively associated with VO2peak. The coefficient (0.30) was close to that of Motivation for PA (0.33) in Model A. All variables were treated as observed in this saturated model, which had excellent fit (Chi-square test: not applicable, RMSEA p = 1.00, TLI = 1.00, CFI = 1.00, SRMR = 0.00). The coefficients for the adjustment variables sex and age were essentially equal in all three models (Table 3), confirming the well-known findings of higher VO2peak in men and lower VO2peak with older age.
The sensitivity analysis in bootstrap samples confirmed that the models had little bias despite the sample size, with small differences in coefficients or CI (data not shown).
For the secondary aim of testing the psychometric properties of the original BREQ-2 factors in our population, all items correlated with their proposed latent factors and the overall model fit was good (Chi square 304.27, df = 136, p < 0.01, RMSEA = 0.053, CFI = 0.94, TLI = 0.92, SRMS = 0.057) (Online Resource 5—BREQ-2 psychometric properties). A significant Chi-square test is common in large studies [30] and has been found in other studies of BREQ-2 [20]. The factors were partly correlated in accordance with self-determination theory that the regulatory styles form a continuum from intrinsic regulation to amotivation, and with strongest correlation between factors more closely related [15]. Because the correlation between intrinsic and identified regulation was very high (0.93), we tested a model where the items belonging to these factors were pooled as one factor. The fit for this 4-factor model was significantly worse than the original 5-factor model (LR test Chi square 96.56, df = 4, p < 0.001). Internal consistency (reliability) of the five factors was good (Cronbach’s alphas from 0.73 to 0.87) (Online Resource 5—BREQ-2 psychometric properties).
In the exploratory study, the results showed that using the students as a control population for the RA patients would not be adequate, as the factor structure of BREQ-2 was significantly different in these two populations. Further details are given in Online Resource 6 (LR tests for measurement invariance between students and patients with RA).
Discussion
The study confirmed that the latent factor Motivation for PA was significantly associated with measured VO2peak in RA patients. Furthermore, whether the patient fulfilled the ACSM/AHA recommendations for PA mediated the effect of Motivation for PA on VO2peak. The study also showed that the RAI could act as useful summary measure for BREQ-2, with a similar effect size as Motivation for PA, and with stable coefficients for the adjustment variables age and sex. The original 5-factor BREQ-2 model had retained its psychometric properties following translation into everyday Norwegian. However, despite overall good fit, the factor structure was significantly different between RA patients and university students, indicating that choice of control group for BREQ-2 scores in arthritis patients is not trivial.
We have previously shown that the average fitness level is lower in RA patients and declines more rapidly with age than in healthy individuals of the same age [11]. The present study points at motivation as a key factor to address when promoting PA for RA patients, which has important clinical implications. The results also contribute to strengthening the evidence for the recent EULAR (European Alliance of Associations for Rheumatology) recommendations, which focus on the need to base interventions on individual aims and consider barriers and facilitators [9]. In a recent randomized controlled trial addressing PA motivation in RA patients, training was equal for both groups, and a self-determination theory-based psychological intervention resulted in higher autonomous motivation [31]. In turn, autonomous motivation predicted self-reported PA and subjective vitality after 3 months. These results support our present findings and demonstrate that motivation may be modified using appropriate methods. However, self-reported PA may be biased. A strength of our study is that we used CPET to quantify VO2peak instead of self-reported PA or indirect measurements to quantify of fitness [32].
Our study also showed that it is plausible to assume that a person's different forms of motivational regulation for PA come together as an overall underlying factor, which influences the performed activities that in turn may modify measured fitness. The direction of the association was positive as expected, indicating that patients with higher intrinsic motivation had higher VO2peak. The interpretation was strengthened by the finding that the effect of motivation was mediated through fulfillment or not of widely accepted recommendations for a clinically relevant level of PA, which take both frequency, duration, and intensity into consideration. These aspects of PA are important, as high-intensity activities more efficiently increase fitness and there is a PA dose effect as well [33]. Our study may also be considered an external validation of the BREQ-2 questionnaire by demonstrating an association of the motivational styles with a relevant outcome, i.e., VO2peak.
The present study also confirmed that the summary measure RAI may be useful in studies where the detailed motivational regulation of PA is of less importance. Using the RAI leads to loss of detail and the proposed weighting may not be correct, but statistical analysis becomes easier when latent variables are not included. Several published studies have used the RAI for this reason [19, 26, 27, 32], but to our knowledge, the validity of RAI has not previously been confirmed based on CPET results. Filling in the BREQ-2 questionnaire only takes a few minutes and use of the RAI may be a simple way to evaluate motivation for PA in future studies of patients with inflammatory arthritis.
The exploratory part of our study has important consequences regarding the choice of control population for future studies of motivation for PA in arthritis patients. We used university students because a sufficiently large number of participants could easily be recruited, but also as a "stress test" because they were different in age from most of the RA patients. Showing a similar factor structure in these two diverse groups would have simplified selection of controls in future studies. Our findings are somewhat different from an investigation of participants in an Internet-based exercise program, where there were no differences between the 18–45 years and 47–78 years age groups or between men and women [20].
The study has some limitations. There may be a selection bias regarding which RA patients who sign up for a CPET study. However, the VO2peak measurements covered a wide range and only 1/3 of the patients fulfilled the current PA recommendations, which argues against a strong selection bias toward the more fit persons. The sample of RA patients was small for SEM and too small for more detailed analysis, including of the potential influence of disease-modifying antirheumatic drugs or disease activity. However, the sensitivity analysis indicated little bias. A weakness using SEM is that other models may fit the data equally well or better, and that only associations are measured, not causation.
In conclusion, the study demonstrated that motivation for PA was significantly associated with measured VO2peak in RA patients. The effect was mediated by whether the patient fulfilled the current recommendations for PA. The results should be confirmed in a larger future study, which would also permit more detailed analysis. Addressing and stimulating motivation is important when intervening to increase PA and cardiorespiratory fitness in RA patients, and further studies using interventions aimed at strengthening the intrinsic motivation for PA in RA patients are needed.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
Cardiopulmonary exercise testing was provided by NeXt Move, NTNU—Norwegian University of Science and Technology. We are grateful to Thomas Fremo for excellent technical assistance.
Author contributions
Study conception and design: VV, MH, MHL. Acquisition and analysis of data: VV, MHL. Interpretation of data: VV, MH, MHL. Drafting the manuscript: VV. Revising the manuscript critically for important intellectual content: MH, MHL, VV. All authors approved the final version of the manuscript.
Funding
Open access funding provided by NTNU -- Norwegian University of Science and Technology (incl St. Olavs Hospital - Trondheim University Hospital). This project was funded by a grant to Marthe Halsan Liff from The Central Norway Regional Health Authority, allocated via The Liaison Committee for Education, Research and Innovation in Central Norway (2016/29014). NeXt Move is funded by the Faculty of Medicine at NTNU and Central Norway Regional Health Authority.
Data availability
No additional data are available.
Declarations
Conflict of interest
None declared.
Ethical approval
The study was performed in compliance with the Helsinki Declaration and was approved by the Regional Committee for Medical and Health Research Ethics (20734).
Informed consent
All participants gave informed consent.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Smolen JS, Aletaha D, McInnes IB. Rheumatoid arthritis. Lancet. 2016;388:2023–2038. doi: 10.1016/S0140-6736(16)30173-8. [DOI] [PubMed] [Google Scholar]
- 2.Pope JE. Management of fatigue in rheumatoid arthritis. RMD Open. 2020;6:e001084. doi: 10.1136/rmdopen-2019-001084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Holmqvist M, Ljung L, Askling J. Mortality following new-onset rheumatoid arthritis: has modern rheumatology had an impact? Ann Rheum Dis. 2018;77:85–91. doi: 10.1136/annrheumdis-2017-212131. [DOI] [PubMed] [Google Scholar]
- 4.Abhishek A, Nakafero G, Kuo CF, Mallen C, Zhang W, Grainge MJ, Doherty M. Rheumatoid arthritis and excess mortality: down but not out. A primary care cohort study using data from Clinical Practice Research Datalink. Rheumatology. 2018;57:977–981. doi: 10.1093/rheumatology/key013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Houge IS, Hoff M, Thomas R, Videm V. Mortality is increased in patients with rheumatoid arthritis or diabetes compared to the general population—the Nord-Trøndelag Health Study. Sci Rep. 2020;10:3593. doi: 10.1038/s41598-020-60621-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Liff MH, Hoff M, Wisløff U, Videm V. Reduced cardiorespiratory fitness is a mediator of excess all-cause mortality in rheumatoid arthritis: the Trøndelag Health Study. RMD Open. 2021;7:e001545. doi: 10.1136/rmdopen-2020-001545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agca R, Heslinga SC, Rollefstad S, Heslinga M, McInnes IB, Peters MJ, Kvien TK, Dougados M, Radner H, Atzeni F, Primdahl J, Södergren A, Wallberg Jonsson S, van Rompay J, Zabalan C, Pedersen TR, Jacobsson L, de Vlam K, Gonzalez-Gay MA, Semb AG, Kitas GD, Smulders YM, Szekanecz Z, Sattar N, Symmons DP, Nurmohamed MT. EULAR recommendations for cardiovascular disease risk management in patients with rheumatoid arthritis and other forms of inflammatory joint disorders: 2015/2016 update. Ann Rheum Dis. 2017;76:17–28. doi: 10.1136/annrheumdis-2016-209775. [DOI] [PubMed] [Google Scholar]
- 8.Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007;39:1423–1434. doi: 10.1249/mss.0b013e3180616b27. [DOI] [PubMed] [Google Scholar]
- 9.Rausch Osthoff AK, Niedermann K, Braun J, Adams J, Brodin N, Dagfinrud H, Duruoz T, Esbensen BA, Günther KP, Hurkmans E, Juhl CB, Kennedy N, Kiltz U, Knittle K, Nurmohamed M, Pais S, Severijns G, Swinnen TW, Pitsillidou IA, Warburton L, Yankov Z, Vliet Vlieland TPM. 2018 EULAR recommendations for physical activity in people with inflammatory arthritis and osteoarthritis. Ann Rheum Dis. 2018;77:1251–1260. doi: 10.1136/annrheumdis-2018-213585. [DOI] [PubMed] [Google Scholar]
- 10.Pinto AJ, Roschel H, de Sá Pinto AL, Lima FR, Pereira RMR, Silva CA, Bonfá E, Gualano B. Physical inactivity and sedentary behavior: overlooked risk factors in autoimmune rheumatic diseases? Autoimmun Rev. 2017;16:667–674. doi: 10.1016/j.autrev.2017.05.001. [DOI] [PubMed] [Google Scholar]
- 11.Liff MH, Hoff M, Wisløff U, Videm V. Faster age-related decline in cardiorespiratory fitness in rheumatoid arthritis patients: an observational study in the Trøndelag Health Study. Rheumatol Int. 2021;41:369–379. doi: 10.1007/s00296-020-04713-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Veldhuijzen van Zanten JJ, Rouse PC, Hale ED, Ntoumanis N, Metsios GS, Duda JL, Kitas GD. Perceived barriers, facilitators and benefits for regular physical activity and exercise in patients with rheumatoid arthritis: a review of the literature. Sports Med. 2015;45:1401–1412. doi: 10.1007/s40279-015-0363-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deci EL, Ryan RM. The «What” and “Why” of goal pursuits: human need and the self-determination of behaviour. Psychol Inq. 2000;11:227–268. doi: 10.1207/S15327965PLI1104_01. [DOI] [Google Scholar]
- 14.Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55:68–78. doi: 10.1037//0003-066x.55.1.68. [DOI] [PubMed] [Google Scholar]
- 15.Markland D, Tobin V. A modification to the Behavioural Regulation in Exercise Questionnaire to include an assessment of amotivation. J Sport Exerc Psychol. 2004;26:191–196. doi: 10.1123/jsep.26.2.191. [DOI] [Google Scholar]
- 16.Haerens L, Kirk D, Cardon G, Bourdeaudhuij ID, Vansteenkiste M. Motivational profiles for secondary school physical education and its relationship to the adoption of a physically active lifestyle among university students. Eur Phys Educ Rev. 2010;16:117–139. doi: 10.1177/1356336X10381304. [DOI] [Google Scholar]
- 17.Ingledew DK, Markland D. Three levels of exercise motivation. Appl Psychol Health Well-Being. 2009;1:336–355. doi: 10.1111/j.1758-0854.2009.01015.x. [DOI] [Google Scholar]
- 18.Ingledew DK, Markland D. The role of motives in exercise participation. Psychol Health. 2008;23:807–828. doi: 10.1080/08870440701405704. [DOI] [PubMed] [Google Scholar]
- 19.Mullan E, Markland D. Variations in self-determination across the Stages of Change for Exercise in adults. Motiv Emot. 1997;21:349–362. doi: 10.1023/A:1024436423492. [DOI] [Google Scholar]
- 20.Weman-Josefsson K, Lindwall M, Ivarsson A. Need satisfaction, motivational regulations and exercise: moderation and mediation effects. Int J Behav Nutr Phys Act. 2015;12:67. doi: 10.1186/s12966-015-0226-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Markland D. The mediating role of behavioural regulations in the relationship between perceived body size discrepancies and physical activity among women. Hell J Psychol. 2009;6:169–182. [Google Scholar]
- 22.Ross R, Blair SN, Arena R, Church TS, Després JP, Franklin BA, Haskell WL, Kaminsky LA, Levine BD, Lavie CJ, Myers J, Niebauer J, Sallis R, Sawada SS, Sui X, Wisløff U. Importance of assessing cardiorespiratory fitness in clinical practice: a case for fitness as a clinical vital sign: a scientific statement from the American Heart Association. Circulation. 2016;134:e653–699. doi: 10.1161/CIR.0000000000000461. [DOI] [PubMed] [Google Scholar]
- 23.Liff MH, Hoff M, Fremo T, Wisløff U, Thomas R, Videm V. Cardiorespiratory fitness in patients with rheumatoid arthritis is associated with the patient global assessment but not with objective measurements of disease activity. RMD Open. 2014;5:e000912. doi: 10.1136/rmdopen-2019-000912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO, 3rd, Birnbaum NS, Burmester GR, Bykerk VP, Cohen MD, Combe B, Costenbader KH, Dougados M, Emery P, Ferraccioli G, Hazes JM, Hobbs K, Huizinga TW, Kavanaugh A, Kay J, Kvien TK, Laing T, Mease P, Ménard HA, Moreland LW, Naden RL, Pincus T, Smolen JS, Stanislawska-Biernat E, Symmons D, Tak PP, Upchurch KS, Vencovsky J, Wolfe F, Hawker G. 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis. 2010;69:1580–1588. doi: 10.1136/ard.2010.138461. [DOI] [PubMed] [Google Scholar]
- 25.Borg GA. Perceived exertion. Exerc Sport Sci Rev. 1974;2:131–153. doi: 10.1249/00003677-197400020-00006. [DOI] [PubMed] [Google Scholar]
- 26.Verloigne M, Bourdeaudhuij ID, Tanghe A, D'Hondt E, Theuwis L, Vansteenkiste M, Deforche B. Self-determined motivation towards physical activity in adolescents treated for obesity: an observational study. Int J Behav Nutr Phys Act. 2011;8:97. doi: 10.1186/1479-5868-8-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Markland D, Ingledew DK. The relationships between body mass and body image and relative autonomy for exercise among adolescent males and females. Psychol Sport Exerc. 2007;8:836–853. doi: 10.1016/j.psychsport.2006.11.002. [DOI] [Google Scholar]
- 28.Prevoo ML, van’t Hof MA, Kuper HH, van Leeuwen MA, van de Putte LB, van Riel PL. Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum. 1995;38:44–48. doi: 10.1002/art.1780380107. [DOI] [PubMed] [Google Scholar]
- 29.Pincus T, Summey JA, Soraci SA, Jr, Wallston KA, Hummon NP. Assessment of patient satisfaction in activities of daily living using a modified Stanford Health Assessment Questionnaire. Arthritis Rheum. 1983;26:1346–1353. doi: 10.1002/art.1780261107. [DOI] [PubMed] [Google Scholar]
- 30.Mehmetoglu M, Jakobsen TG. Applied statistics using Stata. A guide for the social sciences. Thousand Oaks: Sage Publications; 2017. pp. 270–322. [Google Scholar]
- 31.Fenton SAM, Veldhuijzen van Zanten JJ, Metsios GS, Rouse PC, Yu CA, Ntoumanis N, Kitas GD, Duda JL. Testing a self-determination theory-based process model of physical activity behavior change in rheumatoid arthritis: results of a randomized controlled trial. Transl Behav Med. 2021;11:369–380. doi: 10.1093/tbm/ibaa022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Riiser K, Ommundsen Y, Småstuen MC, Løndal K, Misvær N, Helseth S. The relationship between fitness and health-related quality of life and the mediating role of self-determined motivation in overweight adolescents. Scand J Public Health. 2014;42:766–772. doi: 10.1177/1403494814550517. [DOI] [PubMed] [Google Scholar]
- 33.World Health Organization . WHO guidelines on physical activity and sedentary behaviour. Geneva: World Health Organization; 2020. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
No additional data are available.


