Abstract
Point-of-care ultrasound (POCUS) has evolved in recent years in clinical practice, helping in early bedside diagnosis of important etiologies. Many medical schools and training programs are integrating POCUS into their curriculum. Especially with the technological advances of newer handheld ultrasound devices, POCUS has now become a component adjunct to clinical examination, in the clinic and bedside in critical care units. The diagnostic utility of POCUS lies both in early identification of critical kidney disease, and also extra-renal pathologies from a focused cardiac ultrasound, lung ultrasound, and integrated fluid assessment. There is a need to incorporate POCUS in training in pediatric nephrology and establish competency standard criteria. This review shall cover how POCUS helps in enhancing patient care in pediatric kidney disorders and critical children, and the recent advances.
Keywords: Ultrasonography, Nephrology, Pediatrics, Kidney, Urinary tract, Point-of-care systems, POCUS
Background
Ultrasonography has evolved as a first-line imaging tool for the diagnosis of a wide range of ailments owing to its enhanced portability, availability, low cost, and lack of radiation exposure. An increasing number of clinicians are incorporating multi-organ point-of-care ultrasonography (POCUS) into their practice as a bedside diagnostic tool to supplement physical examination. Accordingly, several medical schools and post-graduate training programs including pediatric specialties have integrated POCUS into their curricula [1, 2].
Studies have shown that clinician-performed ultrasound frequently changes the diagnosis and leads to appropriate management compared to conventional physical examination in various clinical settings. In addition, POCUS has the potential to reduce further diagnostic workup and unnecessary radiation exposure [3]. Moreover, when the treating physician performs ultrasound at the bedside and discusses the findings with patients, their understanding of the diagnosis and contributing factors is enhanced. Nephrologist- or urologist-performed kidney POCUS allows assessment of renal parenchymal characteristics, structural renal abnormalities, stone disease, congenital urinary tract abnormalities, and the progression of cystic kidney diseases in the clinic and facilitates timely management [4, 5]. However, POCUS is a limited ultrasound examination intended to answer focused clinical questions and must not be viewed as an alternative to radiologist-performed comprehensive ultrasound.
This current educational review focuses on the POCUS equipment; technology; outpatient and inpatient assessment of the kidney, urinary tract, and hemodynamic status; and the use of POCUS-related interventions in pediatric nephrology practice. The current review shall also serve as a guide for the pediatric nephrologist to implement a POCUS program at the departmental level.
Equipment and technology
Ultrasound probes—conventional and the newer point-of-care devices
Over the past several decades, technological advances have aided in the development of compact, portable, and high-quality ultrasound machines [6]. Clinical ultrasound essentially involves conversion of electrical energy into sound energy and vice versa using piezoelectric crystals in the transducer (probe). When stimulated by an electric current, these crystals vibrate and produce ultrasound waves. The ultrasound waves are then transmitted into the tissues, which reflect them back. The returning echoes are converted into electrical signals by the crystals and displayed as a 2-dimensional gray-scale image. While the detailed description of ultrasound physics is beyond the scope of this manuscript, key principles behind wave generation and propagation are summarized in Fig. 1. The commonly used ultrasound probes and their uses in pediatric practice are shown in Table 1 and Figs. 2, 3, and 4. In addition to conventional probes, specialized probes with a smaller footprint (shape and the size of the face) and higher frequency (resolution) are available for use in the pediatric population [6–8].
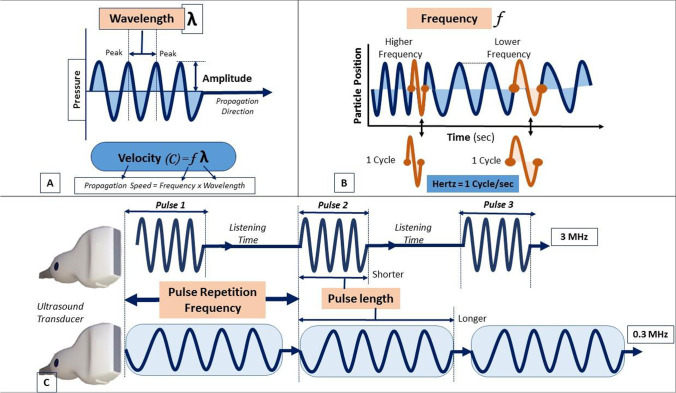
Fig. 1.
Physics behind ultrasound: basic physics concepts behind ultrasound imaging. A, B Depict the ultrasound wave as a sine wave. The wave travels through the tissue at a specified wavelength determined by the frequency (to which it is inversely related) at a specified amplitude. Frequency is the pitch, whereas amplitude is referred to as the loudness of the tone. C Denotes pulse length, or duration, which is associated with the transducer frequency (to which it is inversely related). The rate at which the pulses are emitted is referred to as pulse repetition frequency
Table 1.
Characteristics of common ultrasound transducers
| Transducer | Configuration | Imaging depth | Frequency (Hz) | Application |
|---|---|---|---|---|
| Standard linear | Long, narrow rectangular probe face | 9 cm | 5–13 | Visualization of superficial structures—pleural ultrasound, procedural guidance such as dialysis catheter placement |
| Neonatal/pediatric linear | Hockey stick configuration | 7–22 | Lungs in neonates and infants along with superficial structures. Fits in better between the ribs in smaller children | |
| Phased array | Small, square probe face | 35 cm | 1–5 | Deeper penetration, primarily used for cardiac ultrasound. Abdominal structures can be visualized but not optimal |
| Neonatal/pediatric phased array | Square or rectangular probe face | 4–8 | It has a smaller footprint to fit better between rib spaces | |
| Curvilinear | Curved or rectangular probe face | 30 cm | 1–5 |
Deeper penetration, provides a wider field of view Abdominal and thoracic face visualization, including renal, aorta, IVC, bladder, bowel Procedural guidance such as kidney biopsy |
Fig. 2.

Micro-convex array ultrasound transducer with frequency of 4 to 10 MHz, indicated for pediatric use as it has a small footprint
Fig. 3.

Convex and linear transducer. Left image: convex transducer with frequency of 3 to 5 MHz. They have a curved array that allows wider field of view. These are used for abdominal scans and have deeper penetration due to low frequency. Right image: linear transducers have a flat array and appearance. They have high frequency and are useful for small parts and shallow structures near the surface of the body. They produce a rectangular image with frequency ranging from 9 to 14 MHz
Fig. 4.
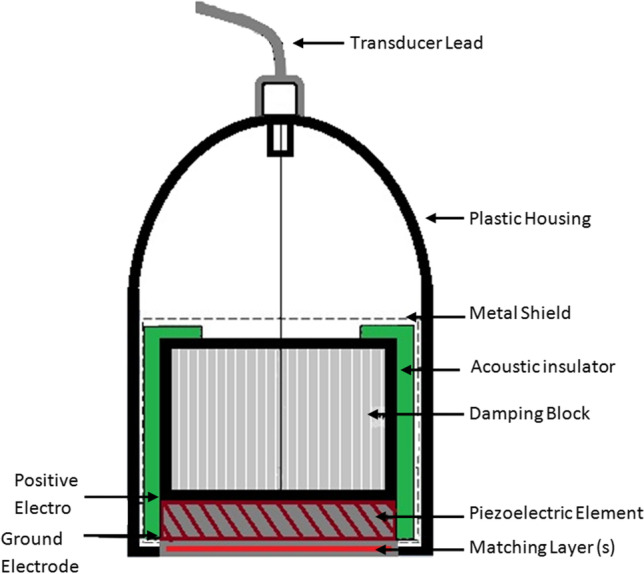
Cross section of the transducer
The advent of handheld ultrasound devices (HUD) in the recent past has revolutionized the landscape of POCUS. As the name suggests, these devices are ultraportable and can often be carried in a coat pocket and use a tablet or cellphone for image display. Moreover, HDUs are much cheaper than the traditional cart-based machines. While most of these devices use the same piezoelectric crystal technology as the cart-based systems, some such as Butterfly® use capacitive micro-machined ultrasound transducers on complementary metal oxide semiconductors (CMUT-on-CMOS technology). This new technology allows a single probe to operate at multiple frequencies and hence image different parts of the body without having to switch transducers [8, 9]. Image quality varies with the type and cost of the device, though, in general, it is inferior to that of traditional systems. Nevertheless, it is sufficient to answer most of the focused clinical questions encountered in day-to-day nephrology practice. Some HUDs offer artificial intelligence (AI)-based features such as automatic calculation of the urinary bladder volume and left ventricular ejection fraction, which save time in the point-of-care settings, such as a busy clinic. AI-guided image acquisition is another attractive feature, particularly for institutions where the availability of POCUS-trained faculty is limited. Like traditional portable ultrasound machines, most HUDs have the capability to save images to the picture archiving and communications system (PACS) used by the hospitals or separate cloud-based secure servers. This streamlines the process of image archiving, which is vital for providing feedback to trainees, sharing images with experts as well as facilitates billing for the scans. In addition, some of the HUD companies provide innovative audio-visual platforms that facilitate remote ultrasound instruction to trainees as well as interact with experts at a different institution. This offers a unique advantage in the setting of travel restrictions and physical distancing requirements during the COVID-19 pandemic [8–10].
However, HUDs are not without limitations. First of all, the user must have a good understanding of the sonographic applications they want to perform, and whether their HUD offers the necessary image quality and modes/options. For example, while the image quality of most HUDs is adequate to exclude hydronephrosis, it is not optimal for reliable assessment of renal parenchymal characteristics or identification of small lesions such as stones. Depending on the options purchased, it might not be possible to perform assessments such as renal artery resistive index or venous congestion. Secondly, technical issues such as low battery life/limited scan time, overheating, and financial aspects such as recurring subscription must be taken into consideration while purchasing a HUD. In addition, using personal display devices such as physicians’ cellphone may pose problems related to patient confidentiality and data breach, especially if the device is lost. We strongly recommend using hospital-provided encrypted tablets/phones with HUDs and not to enter any identifiable patient data unless the device is connected to institutional PACS [8–10].
Ultrasound modes/image display
There are several modes of ultrasound display used for various purposes [10]. B-mode, or brightness mode, denotes the regular 2-dimensional gray-scale display. M-mode, or motion/time mode, is a uni-dimensional image obtained by plotting the movement of a structure over time used to evaluate excursion of the cardiac valves, pleural sliding, respiratory variation of inferior vena cava, etc. Color Doppler allows the detection of blood flow and its direction by analyzing the frequency information of returning signal from the blood vessels. Red color indicates flow towards the transducer whereas blue denotes away from it. Spectral Doppler, on the other hand, provides a graphical representation of the blood flow. It has two variants, namely pulsed wave Doppler (PWD) and continuous wave Doppler (CWD). PWD allows measurement of blood velocity at a particular location and CWD allows gauging peak velocity across cardiac valves [10–12].
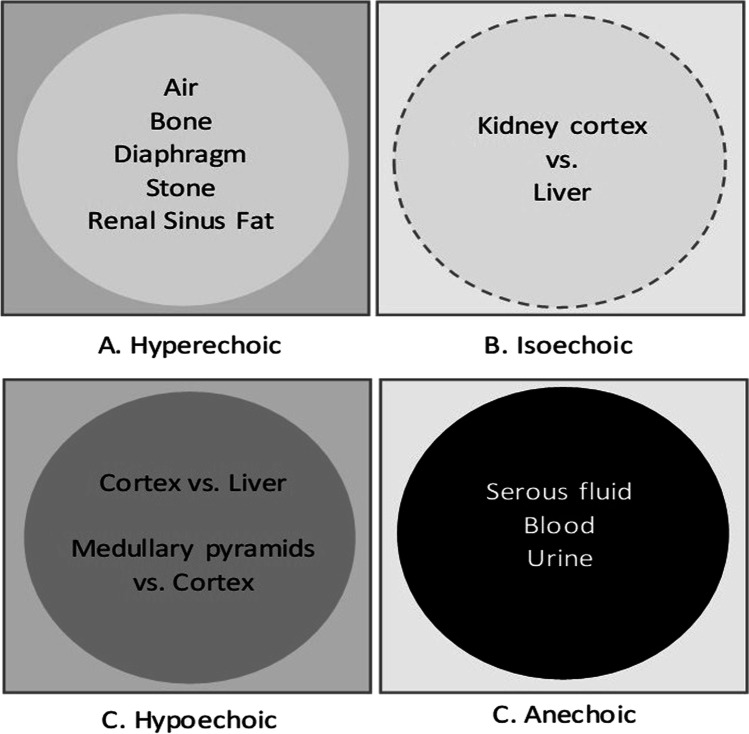
On B-mode imaging, structures appear in various shades of gray ranging from white to black. An ultrasound image is described in terms of “relative echogenicity,” which essentially means how bright or dark a structure appears compared to the adjacent area (Fig. 5). A bright structure (more reflective to ultrasound waves) is described as hyperechoic, darker structures as hypoechoic and black structures (good transmitters of ultrasound waves) as anechoic. Structures that are of similar brightness to the area being compared are labeled as isoechoic. For example, fibrous structures such as the renal capsule, diaphragm, renal sinus fat, stones, and bones are hyperechoic. The renal cortex is either isoechoic or hypoechoic compared to that of the liver and spleen (older children); medullary pyramids are hypoechoic relative to the renal cortex. Clear fluids such as urine, flowing blood, and ascites are typically anechoic [11, 12]. It is notable that air appears as a bright structure on ultrasound image, as it scatters the sound waves. Therefore, evaluation of a structure containing air is a limitation of ultrasound, because air does not allow proper visualization of the underlying pathology.
Fig. 5.
Relative differences between hyperechoic, isoechoic, hypoechoic, and anechoic ultrasound images
In ultrasonography, image quality is determined by the distance between the area of interest and the transducer; the smaller the distance, the better the quality. In addition, frequency of the ultrasound beam is inversely related to the depth of penetration and directly related to image resolution. A high-frequency linear transducer is typically used in neonates and small children as the depth of penetration is relatively short, which results in high-resolution images. For older children, lower frequency probes are optimal for transabdominal imaging while higher frequency probes are used to image superficial structures such as neck vessels [13]. Sometimes, it helps to switch probes; for example, using a linear transducer to assess renal parenchyma and changing to curvilinear to measure accurate kidney length.
Clinical uses
Renal ultrasonography is commonly used as the initial screening examination in pediatric nephrology and urology patients to assess congenital anatomical variants of the kidney and urinary tract, urolithiasis, nephrocalcinosis, renal fusion, bladder outlet obstruction, cystic kidney diseases, hydronephrosis, and vascular anomalies (Table 2) [14, 15]. It is imperative that the POCUS-performing clinician has thorough understanding of the pediatric pathology as it can be quite different compared to adults. Some of the commonly encountered abnormalities in day-to-day clinical practice are discussed below. Notably, current handheld ultrasound technology is not optimized for detailed assessment of the kidneys, although adequate for identifying hydronephrosis and large cysts/stones. Nephrologists must be aware of the limitations of the equipment they are using, particularly when excluding a pathology at the bedside.
Table 2.
Renal pathologies in relation to their generalized ultrasound findings
| Pathology | Generalized Ultrasound Imaging | |
|---|---|---|
| Congenital anatomical variants | Horseshoe kidney | The upper portion of each kidney in the low paraspinal location |
| Ureteropelvic junction obstruction | Abnormal dilatation of the pelvicalyceal system | |
| Bladder outlet obstruction | Bilateral hydroureteronephrosis and bladder wall thickening | |
| Cystic kidney disease | Multicystic dysplastic kidney | Multiple cysts of various sizes that do not communicate |
| Autosomal dominant polycystic kidney disease | Small bilateral simple renal cysts with or without kidney enlargement | |
| Autosomal recessive polycystic kidney disease | A sponge-like kidney appearance with small uniform cysts | |
| Nephronophthisis | Small kidneys with increased echogenicity and loss of corticomedullary differentiation | |
| Kidney stone disease | Radiopaque and nonopaque urinary tract stones with acoustic shadowing | |
| Nephrocalcinosis | Medullary | Loss of normal papillary hypoechogenicity and increased medullary echogenicity |
| Cortical | Hyper-echogenic cortex | |
| Hydronephrosis | Antenatal | Urinary tract dilation |
| Postnatal | Collecting system dilation | |
| Vascular anomalies | Renovascular hypertension | Turbulent flow and aliasing, slow systolic acceleration, and diminished peak systolic velocity |
| Renal vein thrombosis | Elevation of the arterial resistive index | |
| Arteriovenous malformation and fistula | Turbulent flow and arterial velocity in the draining veins | |
| Nutcracker syndrome | Elevated velocity of the narrowed left renal vein or retro-aortic left renal vein | |
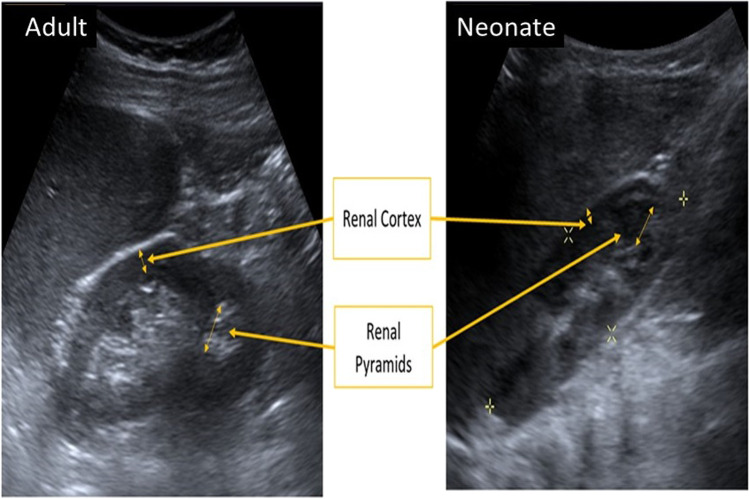
Certain differences exist between the kidneys of older children and adults compared to that of neonates. Firstly, fetal lobulations are prominent in neonates compared to older children and adults. Secondly, neonates have a lower sinus fat content and as a result, central renal echogenicity is not as readily observed. Thirdly, the renal cortex of neonates tends to be hyperechoic compared to the liver, whereas, it gradually decreases by the age of 4–6 months and eventually becomes hypoechoic. In all age groups, the renal pyramids are hypoechoic when compared with the cortex. The anatomical vasculature of the cortex contributes to the appearance of the renal cortex as striations visible on high-frequency transducers, whereas the collecting ducts contribute to the appearance of striations in the renal medulla. Also, in neonates, the renal cortex is much thinner, making the pyramids look larger as compared to those visualized in older children (Fig. 6) [13, 16, 17].
Fig. 6.
Ultrasound images highlighting differences in echogenicity in adults [left image] as compared to neonates [right image]. In neonates, the renal cortex is much thinner, therefore it makes the pyramids larger as compared to those visualized in the older children
Bedside assessment of the kidneys and urinary tract with POCUS
Horseshoe kidney
Horseshoe kidney is the most common renal fusion anomaly, with fusion at the lower poles being the predominant variant. Bedside ultrasound can quickly establish the diagnosis by demonstrating the presence of the isthmus and its continuity with the lower kidney poles. In addition, complications associated with horseshoe kidney such as stones, hydronephrosis, and cysts may also be detected using POCUS. Nevertheless, caution must be exercised in obese patients and horseshoe kidney with fibrous isthmus, as ultrasound is not sensitive in such cases [18].
Cystic kidney disease
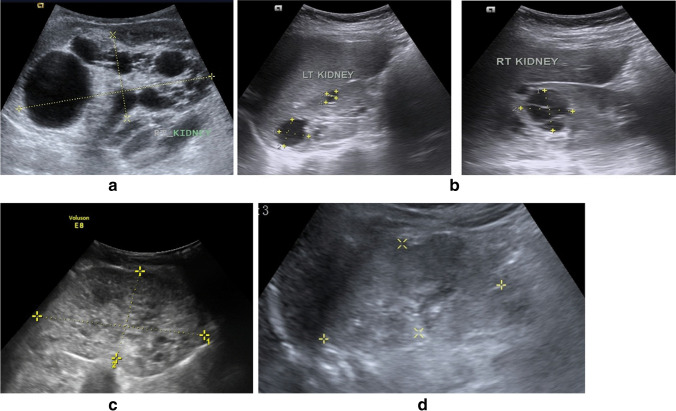
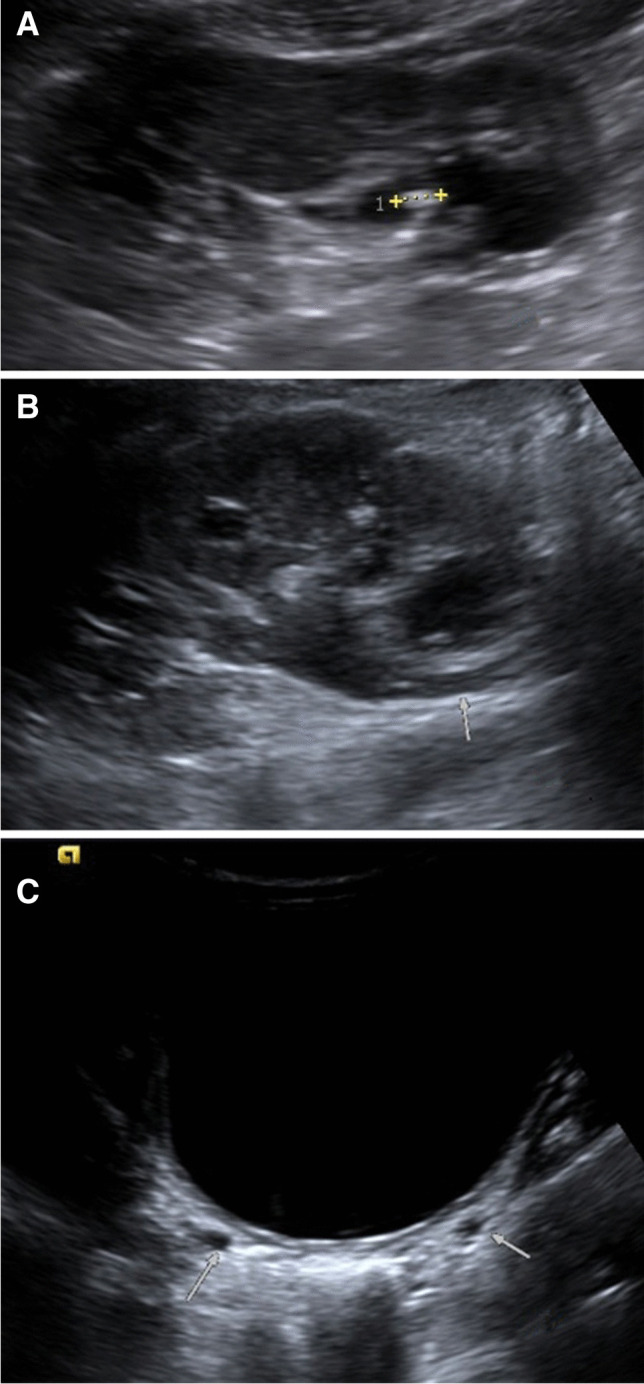
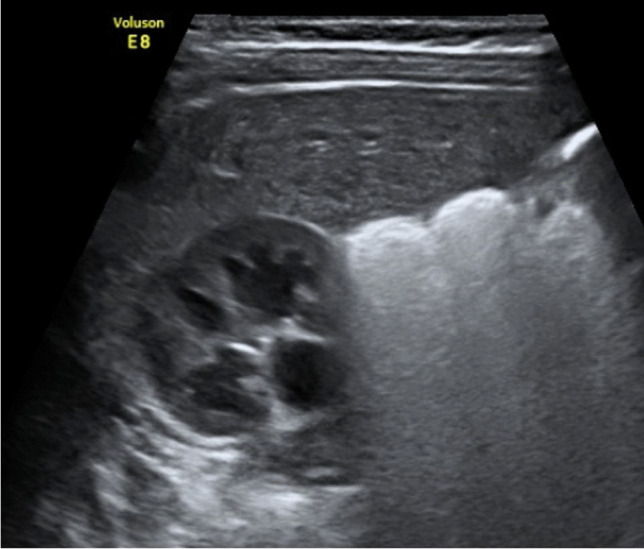
Kidney cysts can be unilateral or bilateral and focal or diffuse. In children, hereditary cystic diseases are more common than acquired cystic diseases, unlike adults. Cysts generally appear as well-circumscribed anechoic structures on ultrasound. Some key entities are discussed below. In multicystic dysplastic kidney (MCDK), renal parenchyma is echogenic, dysplastic, and interspersed with numerous noncommunicating cysts of various sizes (ranging from ≥ 1 mm to a few centimeters) [19] (Fig. 7a). Hypertrophy of the contralateral kidney can be often noted on POCUS. On the other hand, autosomal dominant polycystic kidney disease (ADPKD) is generally associated with bilateral cysts (though not a rule) and a positive family history (Fig. 7b). In autosomal recessive polycystic kidney disease (ARPKD), the kidneys are enlarged with retention of the reniform shape. The cysts are small and POCUS with curvilinear transducer does not necessarily demonstrate them but just increased parenchymal echogenicity with loss of cortico-medullary differentiation (Fig. 7c). A high-frequency transducer is often necessary to identify the cysts, which appear as elliptical anechoic structures oriented perpendicular to the cortex [20]. POCUS findings in nephronophthisis are nonspecific and include normal to small-sized kidneys with increased echogenicity bilaterally (Fig. 7d). Cysts are usually located at the corticomedullary junction and may or may not be detected on POCUS depending on the size. Based on the above discussion, it is conceivable that POCUS allows detection of gross abnormalities such as larger cysts, parenchymal characteristics, and kidney size, which should prompt further evaluation. It must not be perceived as a rule out test.
Fig. 7.
POCUS in cystic kidney disease in childhood. a Multicystic dysplastic kidney: the right kidney shows multiple cysts with intervening parenchyma showing increased echogenicity. b Autosomal dominant polycystic kidney disease: normal-sized kidneys showing multiple cysts. Some of the cysts show internal septation. There is mildly increased cortical echogenicity. Left kidney on left, right kidney shown on the right. c Autosomal recessive polycystic kidney disease: bilaterally enlarged kidneys with increased cortical echogenicity and multiple cysts involving both the cortex and medulla. No hydronephrosis is present. d Nephronophthisis: normal-sized kidneys showing increased cortical echogenicity with poor corticomedullary differentiation in a 2-year-old child with a pathogenic mutation. No sizable cysts could be appreciated
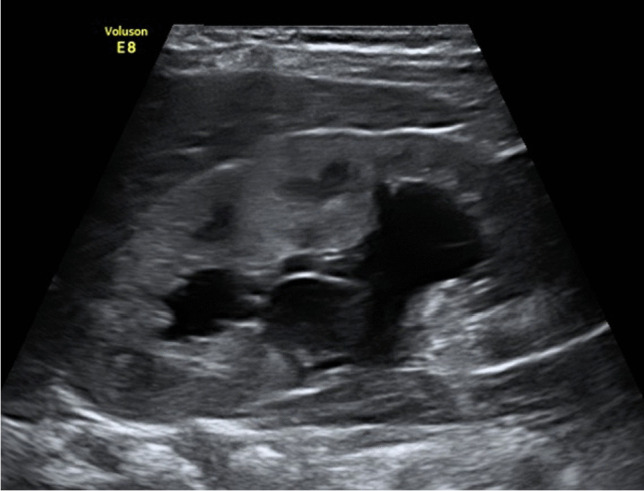
Kidney stone disease
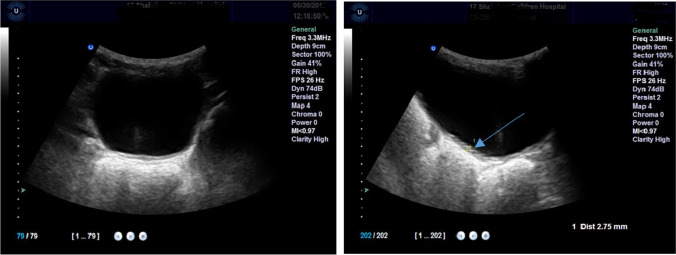
POCUS identifies both radiopaque and radiolucent urinary tract stones (calculi) which appear as echogenic foci with acoustic shadowing. Ultrasound is more sensitive for identifying calculi > 3 mm and cannot rule out smaller stones; hence alternative imaging such as CT scan must be considered when the suspicion is high, but POCUS is negative (Fig. 8). POCUS can be extremely useful in emergent conditions of children presenting to emergency with colic and even anuria, as in the case shown in Fig. 8. Most stones, particularly the rougher ones demonstrate twinkling artifact on color Doppler that appears similar to turbulent blood flow with mixed colors. Knowledge of this artifact is particularly useful when the acoustic shadowing is not apparent on greyscale images. However, its sensitivity and specificity in children are relatively low compared to that of adults [21].
Fig. 8.
Ultrasound of a 10-year-old boy with cystinuria and recurrent urolithiasis needing multiple procedures. POCUS in this child revealed bilateral calculi and suspicion of bilateral vesicoureteric calculi causing colic and anuria: (A) ultrasound image of the right kidney showing an echogenic calculus in the lower calyx, (B) hydroureteronephrosis in the right kidney, (C) transverse view of the ultrasound of the urinary bladder showing prominent bilateral distal ureters just before the vesicoureteric junction
Nephrocalcinosis
Nephrocalcinosis can either be medullary or cortical in nature, though medullary involvement is more common given the concentrating effects in the loops of Henle. Ultrasonography of medullary nephrocalcinosis is characterized by increased medullary echogenicity in addition to the presence of calcifications within the renal parenchyma or outside the collecting system (Fig. 9). Cortical calcinosis is simply defined with a hyperechogenic cortex when diffuse.
Fig. 9.

Nephrocalcinosis: normal-sized kidneys with diffusely echogenic medullary region including pyramids along with punctate echogenic foci in the medulla, some of which are conglomerate in places and show acoustic shadowing. No evidence of hydronephrosis
Vascular abnormalities
Abnormalities such as large arteriovenous malformations and post-biopsy arteriovenous fistula may be readily detectable on POCUS using color Doppler [22, 23]. On the other hand, diagnosis of renal artery stenosis and renal vein thrombosis involves expertise in using spectral Doppler and is generally considered beyond the scope of POCUS. However, clues such as differences in the size of the kidneys in severe renovascular hypertension or absence of flow with visible echogenicity in the main renal vein may still be picked up on bedside evaluation [22, 23].
Allograft dysfunction
POCUS is a valuable adjunct in managing patients with suspected allograft dysfunction. In the immediate postoperative period, a dysfunctional allograft typically shows hypoechoic and swollen parenchyma with a loss of normal corticomedullary differentiation and poor color flow; PWD evaluation may reveal elevated arterial resistive indices [14, 15, 24–26]. In addition, special attention must be paid to peri-nephric areas for collections such as hematoma, urinoma, lymphocele, etc.
Urinary tract obstruction
The uretero-pelvic junction is a frequent site of congenital urinary tract obstruction leading to hydronephrosis, which can be readily detected on POCUS. In one study, the sensitivity and the specificity of POCUS were 76.5% and 97.2% respectively to detect hydronephrosis in a pediatric population [24]. Pelvicalyceal dilatation can be of varying degrees with or without associated hydroureter depending on the site of obstruction (Figs. 10 and 11). In children presenting with hydronephrosis and fever or hematuria, the presence of echogenicities within the dilated collecting system should raise the concern for pyonephrosis or hemorrhage. Ability to identify such abnormalities in the nephrology clinic using POCUS without having to wait for formal imaging quickly changes the management.
Fig. 10.
Pelvic-ureteric junction obstruction: hydronephrosis (SFU-3) including dilated renal pelvis in a 2-year-old child. Cortical thickness is maintained
Fig. 11.
Antenatally diagnosed hydronephrosis: ultrasound image showing hydronephrosis [SFU-3] in a 3-month-old child followed since the antenatal period
Similarly, bladder outlet obstruction can occur in children from several causes including posterior urethral valves and neurogenic bladder, which eventually could lead to vesicoureteric reflux, recurrent infections, hydronephrosis, and renal parenchymal damage [25]. In such cases, POCUS findings in conjunction with relevant history can alert the nephrologist to obtain further investigations; urgently catheterize the child before the surgeon arrives in the neonatal intensive care.
Urinary bladder
The utility of bladder POCUS includes evaluation of structural abnormalities, including wall thickness (Fig. 12) and abnormal contents. A thickened bladder wall may be indicative of abnormalities such as a neurogenic bladder or distal obstruction. While echogenic contents maybe expected in dehydrated children, they may also indicate debris or hemorrhage depending on the clinical context. Other abnormalities such as bladder stones and ureteroceles must be watched for. Stones appear as hyperechoic structures whereas ureterocele is a thin-walled intra-vesicular cystic structure. Assessment of bladder volume and post-void residual (PVR) prior to attempting urethral catheterization may prevent failed attempts. A full bladder allows optimal assessment of all these parameters; it might be worthwhile to examine the bladder before kidneys in small children as probe manipulation on the abdomen might stimulate micturition [27–31].
Fig. 12.
Bladder: left transverse, right sagittal view (arrow, bladder thickness)
Evaluation of hemodynamic status in critical illnesses
Assessment of fluid and hemodynamic status is crucial for evaluating the derangements in blood pressure and fluid–electrolyte balance seen in critical children with AKI and stage 5 chronic kidney disease (CKD 5). Information gleaned from the sonographic assessment of the lungs, heart, and abdominal veins addresses the frequent dilemma in nephrology practice: “to fill or not to fill” (Table 3) [32].
Table 3.
Typical sonographic findings in different types of shock
| Sepsis | Focused cardiac ultrasound imaging | Lung ultrasound imaging |
|---|---|---|
| Hypovolemic |
Hyperdynamic LV ↓ Cardiac output* Small collapsible IVC |
A-lines |
| Cardiogenic |
↓ LV function ↓ Cardiac output Dilated IVC |
B-lines Pleural effusions |
| Obstructive |
Pericardial effusion Dilated right ventricle with interventricular septal flattening (in pulmonary embolism) ↓Cardiac output Dilated IVC |
A-lines Focal B-lines may be seen with large lung infarcts |
| Distributive |
Varying LV function (usually hyperdynamic) ↑ Cardiac output Variable IVC |
A-lines Focal B-lines/hepatization in case of pneumonia |
*Measurement of cardiac output involves spectral Doppler imaging, which requires a higher operator skill level
Lung ultrasound
In the past several years, lung ultrasound (LUS) has emerged as a reliable tool for the assessment of extravascular lung water (EVLW), particularly in adult patients with critical illness, heart failure, and CKD 5 [32–38]. Because of its technical simplicity and proven superiority over conventional physical examination, pediatric nephrologists are increasingly adopting this technique as a bedside diagnostic aid. As mentioned, air scatters the ultrasound beam and does not allow proper visualization of underlying structures. Therefore, air-filled lung tissue cannot be seen on ultrasound and LUS essentially involves interpretation of artifacts. The pleural line appears as a bright linear structure with a shimmer (rhythmic to-and-fro movement) that represents pleural sliding. Normal lung demonstrates horizontal hyperechoic artifacts placed equidistantly called the A-lines that are created by ultrasound reverberation from the pleural interface (Fig. 13a). On the other hand, vertical hyperechoic artifacts called the B-lines represent interlobular septal thickening (typically but not exclusively due to EVLW) (Fig. 13b). B-lines arise from the pleural line, extend to the bottom of the screen without fading, and move synchronously with lung sliding [39–41]. In general, the presence of three or more B-lines per intercostal space is considered significant; interstitial syndrome/pulmonary edema is characterized by B-lines in multiple scan zones bilaterally. Further, counting the total number of B-lines using a pre-defined scanning protocol allows semi-quantitative estimation of EVLW, which in turn can be used to titrate ultrafiltration or diuretic dosing in patients with AKI and CKD 5 [26, 31–33]. It is of note that B-lines are not specific for pulmonary edema. They can be seen in conditions such as pneumonia, parenchymal lung disease, and lung contusion; B-lines must be interpreted in the right clinical context together with corroborating sonographic parameters, for example, irregular pleural line in non-cardiogenic causes. Moreover, as the fetal lung has high fluid content, B-lines are often seen in neonates without respiratory distress and usually disappear by the third day [42]. The zones/regions of evaluation vary widely in the literature. In adult patients, an 8-zone method is widely popular (4 zones in each hemithorax) though most studies in hemodialysis patients used a more comprehensive 28-zone method [43]. In pediatric literature, a 12-zone method is commonly described in stable patients where each hemithorax is divided into 6 regions using 3 longitudinal lines—anterior axillary, posterior axillary, and spine, and a horizontal line just above the nipple [44].
Fig. 13.
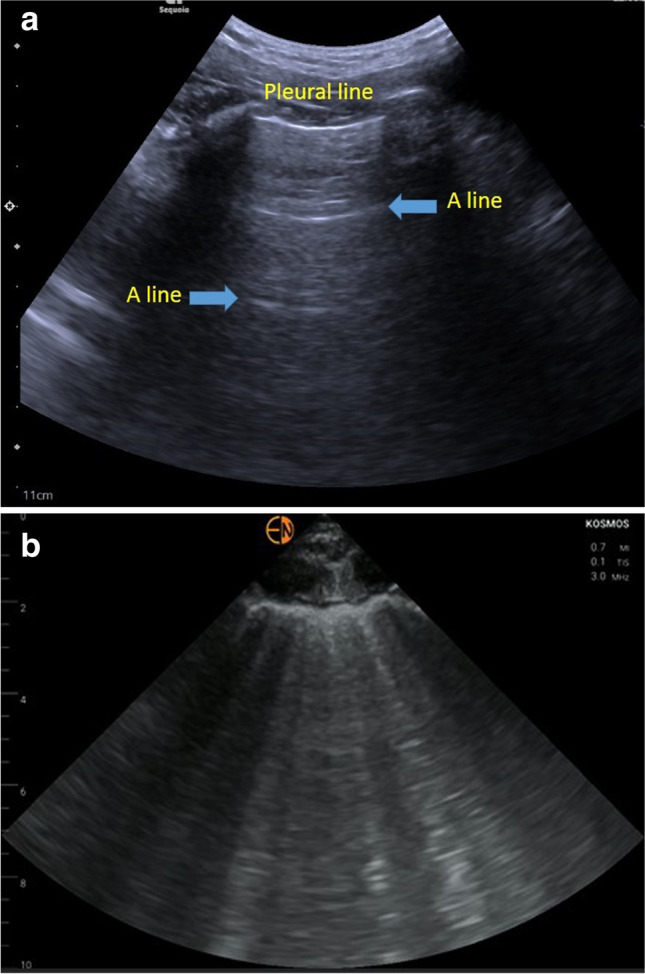
Lung ultrasound. a Lung ultrasound showing A-lines. b Lung ultrasound showing multiple B lines
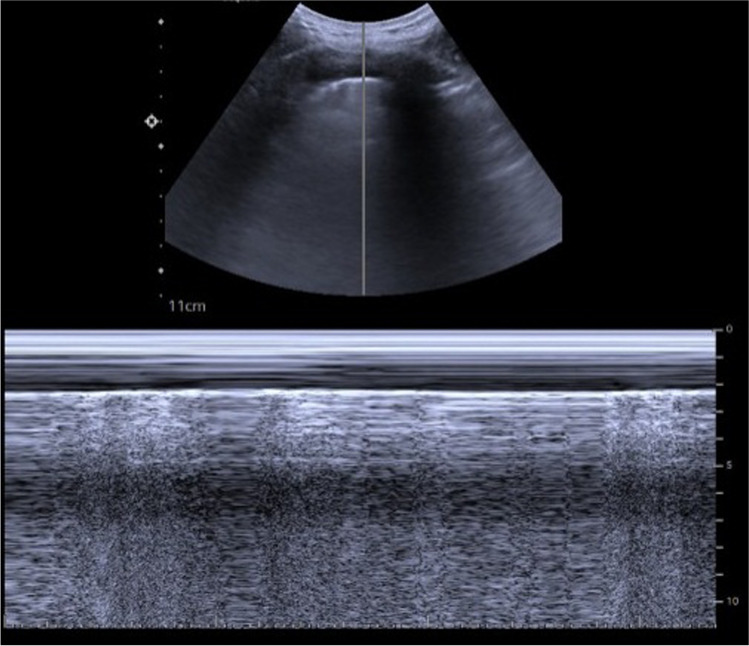
The M-mode of the lung ultrasound helps to understand that the to-and-fro sliding movement of the lung at the pleural line relative to superficial tissue. The seashore sign indicates to the clinician that the pleural line also is the visceral pleura and is present in a normal lung (Fig. 14). Both the seashore sign and the A-lines make the A-profile, giving information at the level of capillary pressure. In pneumothorax, a pattern involving M-mode, which is for motion, existence of A-lines, non-appearance of B-lines, and visualization of lung point, which is a specific indicator, is seen [41].
Fig. 14.
M-mode images of the lungs depicting the typical “seashore sign.” Above the pleura, the ultrasound scan reveals wave-like lines, which are generated by the movement of muscles (“waves”) and the skin (“sky”)
LUS is also a sensitive tool to diagnose pneumonia and significantly outperforms auscultation in pediatric patients [45]. In adult patients with acute respiratory distress syndrome (ARDS), the diagnostic accuracy of LUS has shown to be higher than that of auscultation as well as chest radiography for the diagnosis of alveolar consolidation and alveolar-interstitial syndrome [33]. A consolidated lung appears like the liver in echotexture (hepatization); branching, mobile, echogenic foci may be seen within the consolidation representing dynamic air bronchograms. In addition, the utility of LUS in identifying pleural effusions is well established. LUS can detect effusions as small as 10–20 mL, while chest radiograph needs about 200 mL [33, 46, 47]. Sonographically, effusion appears as an anechoic area above the diaphragm (Fig. 15) and the atelectatic lung is frequently seen floating within. Pneumothorax is another pathology that may be encountered by pediatric nephrologists, especially in the context of procedural complications, and another indication for learning LUS-POCUS especially for pediatric nephrologists. The diagnostic accuracy of LUS for detection of pneumothorax is comparable to that of CT and exceeds that of plain radiographs [48]. The absence of pleural sliding on LUS has a specificity and sensitivity of 91.1 and 95.3%, respectively for the detection of pneumothorax [44]. The specificity approaches 100% when a lung point is identified (junction between the non-sliding and sliding pleura) [49]. LUS can also be used for procedural guidance to drain pleural effusion and chest tube placement, which reduces the rate of complications [50].
Fig. 15.
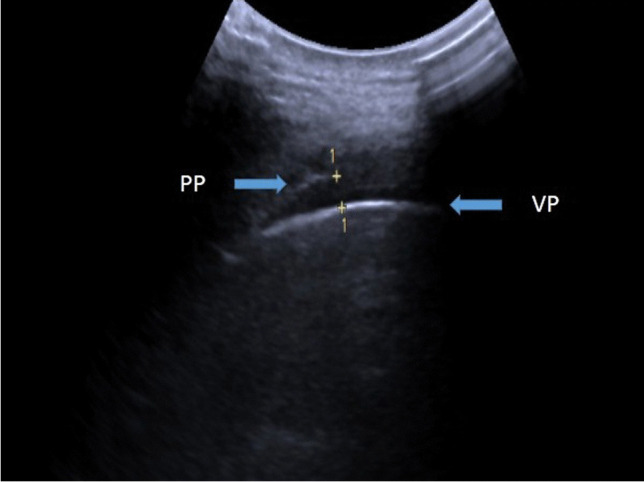
Ultrasound lung depicting pleural effusion between visceral pleura (VP) and parietal pleura (PP)
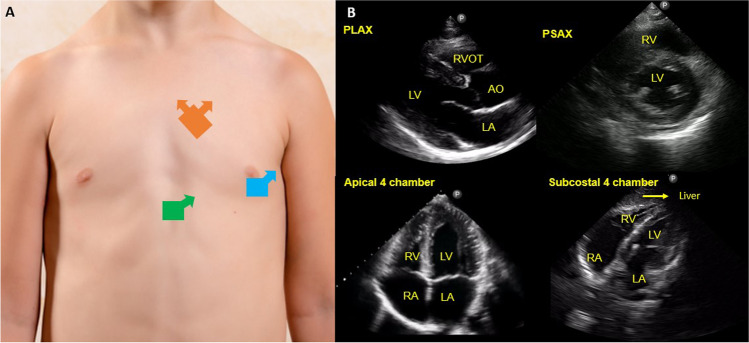
Focused cardiac ultrasound
Focused cardiac ultrasound is a limited sonographic examination of the heart to answer a focused clinical question and/or guide a procedure such as pericardiocentesis [51–55]. Comprehensive echocardiogram performed by the cardiology department typically involves acquisition of multiple cardiac views and documentation of various measurements according to a pre-specified protocol. On the other hand, FoCUS is a simplified study performed by the clinician (typically a non-cardiologist) as an adjunct to physical examination to guide immediate management [56, 57]. When used in conjunction with LUS and careful history taking/physical examination, FoCUS can provide valuable, real-time insights into a child’s hemodynamics. It allows bedside assessment of pericardial effusion, cardiac preload, pump function, forward flow, chamber enlargement, and facilitates timely management [58]. It usually involves acquiring cross-sectional images of the heart from three windows or spaces, namely parasternal, apical, and subcostal (Fig. 16).
Fig. 16.
The figure illustrates four standard views of focused cardiac ultrasound (FoCUS). A Illustration of transducer positions (orange-parasternal window, blue-apical and green-subcostal) and orientation of probe indicator (direction of the arrow). B Corresponding sonographic images. PLAX, parasternal long axis, PSAX parasternal short axis, LA, left atrium, RA, right atrium, LV, left ventricle, RV, right ventricle, RVOT, right ventricle outflow tract, AO, aorta. Chest photograph is licensed from Shutterstock
Assessment of left ventricular systolic function or left ventricular ejection is a key component of FoCUS in a patient with hemodynamic instability. In pediatrics, increased left ventricular end-diastolic dimensions either suggest volume overload or can be a sign of left ventricular dysfunction due to dilated cardiomyopathy. As the condition worsens, transmittance of the overload to the right ventricle causes similar dilation and the interventricular septum is flattened during diastole. Under these conditions, an increase in wall thickness may indicate pressure loading or infiltrative disorders [53, 54]. Pericardial effusion is another well-recognized cause of hypotension and hemodynamic compromise. On FoCUS, it appears as an anechoic space between the two pericardial layers, best visualized from the parasternal and subcostal windows. Careful attention must be exercised to detect hemodynamic effects of the effusion such as right-sided chamber collapse. In addition, cardiac preload can be assessed by inferior vena cava (IVC) ultrasound [59, 60]. While FoCUS also helps to diagnose congenital heart defects and regional wall motion abnormalities and assess stroke volume and pulmonary artery pressure at the bedside, these require a higher operator skill level and training [61, 62].
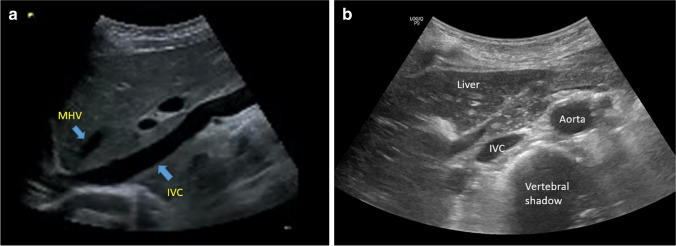
IVC assessment
IVC ultrasound is generally considered a component of FoCUS and isolated interpretation may lead to erroneous conclusions. It indicates right atrial pressure (RAP) or central venous pressure, which is a surrogate for cardiac preload. Figure 17 illustrates long and short axis view of a normal IVC. In spontaneously breathing adults, IVC diameter at end-expiration and collapsibility with inspiration are used to estimate RAP. A dilated IVC (> 2.1 cm) with less than 50% collapse suggests high RAP (as in heart failure) while a small collapsing IVC suggests low RAP (as in volume depletion or normal state depending on the context). However, in children, it is not that straightforward as the baseline IVC size is smaller and it is not possible to establish a universal cut-off for these values accounting for normal growth-related changes. Aorta to IVC ratio is a good alternative in the pediatric population based on the rationale that as opposed to aorta diameter, IVC diameter varies before and after intravenous hydration. This ratio is obtained by dividing the largest aorta diameter (during systole) by the largest IVC diameter (end-expiration) in the transverse plane [63]. In one study, based on a cutoff of 1.22, aorta to IVC ratio had a sensitivity and specificity of 93% and 59% respectively for detecting severe dehydration [64]. On the other hand, a plethoric IVC bigger than the aorta indicates high RAP, in other words, volume intolerance. While much of the earlier research on IVC ultrasound focused on assessing volume responsiveness, it has been recognized that IVC is an unreliable indicator for this. Moreover, as exhausting fluid responsiveness is not the goal of intravenous fluid therapy, most experts advocate using IVC to assess fluid tolerance rather than responsiveness. IVC ultrasound can be error-prone in patients on mechanical ventilation and those with congenital heart disease.
Fig. 17.
Inferior vena cava. a Long axis view of the inferior vena cava (IVC) obtained from the subxiphoid window. MHV denotes the middle hepatic vein draining into the IVC. b Short axis view of inferior vena cava (IVC)
In adult patients, there is growing interest in the assessment of venous congestion using Doppler as an extension to IVC ultrasound. In a cohort of cardiac surgery patients [65], severe flow abnormalities in multiple Doppler patterns (2 of 3—hepatic, portal, and intra-renal veins) with a dilated IVC (≥ 2 cm) predicted the development of AKI with a hazard ratio of 3.69. Utility of these Doppler waveforms has also been reported in the management of hyponatremia [66], which is one of the common electrolyte disorders encountered in nephrology practice. Furthermore, these waveforms are dynamic and aid in monitoring the efficacy of decongestive therapy in patients with volume overload [42, 43]. Future studies are needed to investigate whether these findings can be replicated in pediatric patients.
Multiorgan POCUS
The use of multiorgan POCUS at the bedside can potentially narrow the differential diagnoses being considered or even suggest an entirely new diagnosis. For example, the presence of a diffuse B-line pattern on LUS and decreased left ventricular ejection on FoCUS suggests heart failure and warrants decongestive and/or ionotropic therapy. On the other hand, a child with focal B-line pattern adjacent to a subpleural consolidation on LUS and hyperdynamic left ventricle on FoCUS would likely benefit from fluid resuscitation. Clinical integration of data provided by POCUS can be realized in the context of undifferentiated shock, where rapid categorization of the precise etiology as distributive, cardiogenic, and hypovolemic shock is crucial to rapidly intervene and lead to the best patient outcomes [67–70].
Utility of POCUS in interventional nephrology
POCUS in ultrasound-guided procedures in the PICU
The advent of real-time ultrasound guidance has reduced the complication rate of kidney biopsies as well as increased the chances of successful sampling. Instinctively, clinicians perform kidney biopsies in regions that are most accessible and visible, which most frequently is the lower pole of the left kidney. The use of ultrasound provides real-time visualization of the needle track (Fig. 18) and gives an accurate estimate of the depth of the kidney from the skin surface. A high-frequency/linear transducer is the preferred probe in children as it offers higher resolution to assess subcutaneous structures and renal parenchyma traversed by the needle. If the depth is inadequate due to patient size, a curvilinear probe is used [71].
Fig. 18.
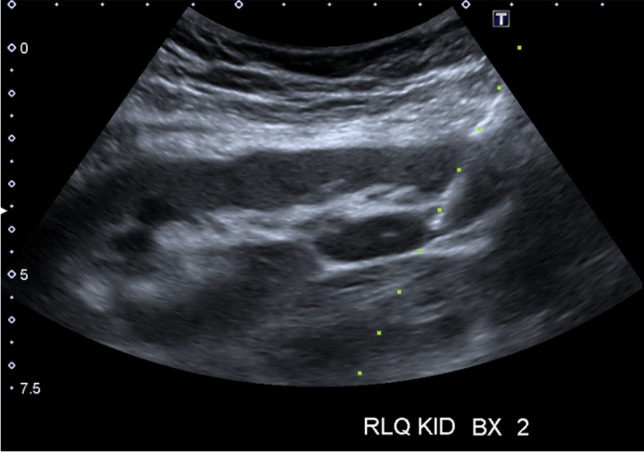
Ultrasound-guided real-time visualization of needle track during kidney biopsy
POCUS in dialysis access
Hemodialysis vascular access
The most common sites for placement of tunneled and non-tunneled hemodialysis catheters are the central veins. POCUS guidance for central venous catheter placement minimizes complications and is considered a standard of care, at least in developed countries. POCUS not only helps to confirm the needle entry into the vein but also allows the catheter to be used prior to obtaining a chest radiograph by (1) confirming appropriate catheter position and (2) excluding pneumothorax. Once the catheter is placed, it is flushed with 10 mL of saline (preferably agitated); if it is in the correct position, the right atrium immediately opacifies (within 2 s), which can be observed in the subcostal or apical cardiac views using POCUS. This is called the rapid atrial swirl sign (RASS) [72]. Similarly, upper lung zones are scanned to assess pleural sliding and rule out pneumothorax.
Arteriovenous access
POCUS allows evaluation of vessel diameters and blood flow in an arteriovenous fistula (AVF) and expedites care when abnormalities are detected. It is often used for vein mapping prior to the placement of AVF, assessment of maturation, and complications such as aneurysm/pseudoaneurysm, peri-AVF infiltration [73]. PWD evaluation allows assessment of the flow pattern and velocities, which helps in diagnosing stenosis; however, this requires a higher skill level and potentially beyond the scope of a non-interventional nephrologist.
Peritoneal dialysis catheter placement
Interventional radiologists/nephrologists place and maintain peritoneal dialysis (PD) catheters with image-guided techniques of fluoroscopy and/or ultrasound. As opposed to laparoscopic or open surgical techniques, the percutaneous approach is less invasive and does not require conventional surgical clearance, thus increasing availability to wider patient populations and also expediting care by being able to be performed at the bedside or ambulatory setting.
During the initial evaluation of the patient, superficial structures and vessels can be evaluated with a linear probe, while evaluation of the bladder and deeper abdominal cavity is performed with a curvilinear probe. To ensure the needle entry site is safe and to minimize the risk of bowel injury or peritonitis, ultrasound is used to assess the abdominal cavity and associated peristaltic bowel movements against the abdominal wall. Given the difficult nature of achieving hemostasis within vessels of the rectus muscle, epigastric vessels, or accessory vessels of the subcutaneous layer, assessing the location and patency of vessels with Doppler ultrasound helps to minimize risk of hemorrhage into the peritoneal cavity and improve success of placing the deep cuff [74, 75].
Training and competency standards
POCUS is an adjunct to physical examination and enhances patient care by reducing diagnostic uncertainty and potentially healthcare cost burden [76]. Regardless, formal training and establishment of standards is lacking in most specialties outside of emergency medicine and critical care. A recent survey of US pediatric critical care divisions reported that diagnostic POCUS training is offered in 67% of the institutions. However, availability of trained faculty, proper image archiving, documentation, credentialing, and quality assessment were limited/underdeveloped in most of the programs [77]. There was also wide heterogeneity in organization of the curricular content among programs. In adult nephrology, there are very few fellowship programs that offer structured diagnostic POCUS training at this time [78, 79]. Training faculty in the fellowship programs and physicians who are already in practice is another challenge. While short POCUS courses are offered during professional society meetings, it must be recognized that mastering any new skill is a long-term process. Learning POCUS involves understanding multiple components including formulating the right clinical questions, knowing what sonographic parameter to assess, possessing the necessary skill to perform the scan and interpreting the findings in the right clinical context. Fellowship programs should identify faculty champions who are willing to dedicate time to POCUS and provide them with administrative support. Responsibilities of POCUS faculty include but are not limited to development of the curricular content, organization of hands-on workshops, training other faculty, longitudinal mentoring and supervised scholarship, oversight of documentation, fostering multidisciplinary collaborations, quality assessment, and improvement. All these components take substantial time and effort, and as such experts recommend providing a protected time of about 0.15–0.25 full-time equivalent (FTE) to the POCUS director depending on the size of the fellowship program [80]. It is vital to establish a workflow for image archiving and retrieval for the purposes of billing, comparison with formal imaging, provide learner feedback, and quality assurance. Billing for POCUS scans helps to offset the costs of ultrasound equipment over time. Nevertheless, successful incorporation of POCUS into clinical practice requires proper training and establishment of rigorous certification process to avoid unintentional patient harm from under- or overdiagnosis. There is paucity of data in the area of POCUS education regarding the effectiveness of existing curricula and competency assessment. Key steps in the development of a POCUS program including faculty training are summarized in Fig. 19. At a national and international level, there is a pressing need to establish standards for POCUS training in pediatric nephrology fellowships, competency assessment and uniform reporting guidelines. It is also important to set guidelines for conducting POCUS workshops and certification processes for physicians in private practice to facilitate incorporation of POCUS. We believe that the best way to undertake this is to form a working group consisting of pediatric nephrologists and intensivists, as well as experts from adult POCUS-performing specialties and formulate a consensus guideline endorsed by pediatric nephrology societies. The authors of this review are currently in process of developing and formulating the same.
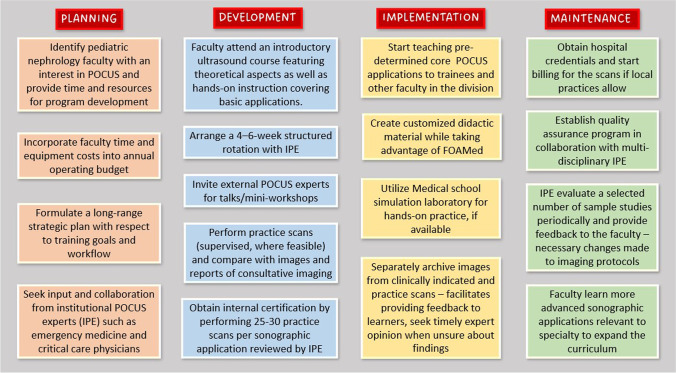
Fig. 19.
Key elements of developing a point-of-care ultrasound (POCUS) program at the departmental level. Figure adapted from NephroPOCUS.com, with kind permission of the author
Future directions
Enhanced portability of the equipment combined with progressive improvement in image quality has enabled non-radiologist physicians to use ultrasonography at the point-of-care as an adjunct to physical examination. In pediatric nephrology, POCUS can be used to answer a number of focused clinical questions at the bedside ranging from structural renal abnormalities to hemodynamic status, facilitating timely diagnosis and management. Moreover, despite well-established diagnostic accuracy of bedside ultrasound, the data on its impact on the patient outcomes is sparse. Further, novel hemodynamic applications of POCUS such as Doppler-assisted venous congestion assessment have not been studied in the pediatric population. Future research should aim to address these knowledge gaps and develop standardized POCUS-guided management protocols in various clinical scenarios. The impact of POCUS on the outcome essentially depends on how effectively we use the information provided by it to manage patients; indeed, application of a diagnostic modality cannot improve outcomes by itself.
Key summary points
Point-of-care ultrasound (POCUS) has rapidly evolved as a very valuable adjunct to physical examination, especially in sick children for the pediatric nephrologist.
POCUS can help a pediatric nephrologist in multiple ways, ranging from bedside assessment of urinary tract, fluid assessment, focused cardiac ultrasound, and interventions.
Successful application of POCUS includes proficiency in image acquisition, interpretation, integrating the sonographic data with the clinical picture to guide therapy and effectively communicating with patients and colleagues.
There is a need for a taskforce to guide consensus on POCUS curriculum, competency evaluation, and application of POCUS in routine pediatric nephrology practice.
Multiple choice questions (answers can be found after the reference list)
- What is the advantage to POCUS?
-
aLack of ionizing radiation
-
bNon-invasive
-
cPortable
-
dAll of the Above
-
a
- What is POCUS able to assess?
-
aRenal parenchymal characteristics
-
bKidney stone progression
-
cBladder catheterization for urine sample collection
-
dFluid assessment in pediatric intensive care
-
eAll of the Above
-
a
- Which ultrasound mode is most often used?
-
aA mode
-
bM mode
-
cB mode
-
dD mode
-
a
Declarations
Conflict of Interest
The authors declare no competing interests.
Footnotes
Dr. Sidharth Kumar Sethi and Dr. Rupesh Raina shall be first authors.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Answers: 1-d; 2-e; 3-c.
References
- 1.Conlon TW, Nishisaki A, Singh Y, Bhombal S, De Luca D, Kessler DO, Su ER, Chen AE, Fraga MV. Moving beyond the stethoscope: diagnostic point-of-care ultrasound in pediatric practice. Pediatrics. 2019;144:e20191402. doi: 10.1542/peds.2019-1402. [DOI] [PubMed] [Google Scholar]
- 2.Finkel L, Ghelani S, Paladugu K, Sanyal S, Colla JS. General pediatric clinical applications of POCUS: part 2. Pediatr Ann. 2020;49:e196–e200. doi: 10.3928/19382359-20200319-02. [DOI] [PubMed] [Google Scholar]
- 3.Colli A, Prati D, Fraquelli M, Segato S, Vescovi PP, Colombo F, Balduini C, Della Valle S, Casazza G (2015) The use of a pocket-sized ultrasound device improves physical examination: results of an in- and outpatient cohort study. PLoS One 10:e0122181. 10.1371/journal.pone.0122181 [DOI] [PMC free article] [PubMed]
- 4.Hassanzadeh Rad A, Badeli H. Point-of-care ultrasonography: is it time nephrologists were equipped with the 21th century’s stethoscope? Iran J Kidney Dis. 2017;11:259–262. [PubMed] [Google Scholar]
- 5.Cox EGM, Koster G, Baron A, Kaufmann T, Eck RJ, Veenstra TC, Hiemstra B, Wong A, Kwee TC, Tulleken JE, Keus F, Wiersema R, van der Horst ICC (2020) Should the ultrasound probe replace your stethoscope? A SICS-I sub-study comparing lung ultrasound and pulmonary auscultation in the critically ill. Crit Care 24:14. 10.1186/s13054-019-2719-8 [DOI] [PMC free article] [PubMed]
- 6.Akkus Z, Cai J, Boonrod A, Zeinoddini A, Weston AD, Philbrick KA, Erickson BJ. A survey of deep-learning applications in ultrasound: artificial intelligence-powered ultrasound for improving clinical workflow. J Am Coll Radiol. 2019;16(9 Pt B):1318–1328. doi: 10.1016/j.jacr.2019.06.004. [DOI] [PubMed] [Google Scholar]
- 7.Sharma KV, Yarmolenko PS, Eranki A, Partanen A, Celik H, Kim A, Oetgen M, Kim PCW. Magnetic resonance imaging-guided high-intensity focused ultrasound applications in pediatrics: early experience at Children’s National Medical Center. Top Magn Reson Imaging TMRI. 2018;27:45–51. doi: 10.1097/RMR.0000000000000163. [DOI] [PubMed] [Google Scholar]
- 8.Baribeau Y, Sharkey A, Chaudhary O, Krumm S, Fatima H, Mahmood F, Matyal R. Handheld point-of-care ultrasound probes: the new generation of POCUS. J Cardiothorac Vasc Anesth. 2020;34:3139–3145. doi: 10.1053/j.jvca.2020.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Malik AN, Rowland J, Haber BD, Thom S, Jackson B, Volk B, Ehrman RR. The use of handheld ultrasound devices in emergency medicine. Curr Emerg Hosp Med Rep. 2021;9:73–81. doi: 10.1007/s40138-021-00229-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koratala A, Bhattacharya D, Kazory A. Point of care renal ultrasonography for the busy nephrologist: a pictorial review. World J Nephrol. 2019;8:44–58. doi: 10.5527/wjn.v8.i3.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lawrence JP. Physics and instrumentation of ultrasound. Crit Care Med. 2007;35:S314–322. doi: 10.1097/01.CCM.0000270241.33075.60. [DOI] [PubMed] [Google Scholar]
- 12.Kelahan LC, Desser TS, Troxell ML, Kamaya A. Ultrasound assessment of acute kidney injury. Ultrasound Q. 2019;35:173–180. doi: 10.1097/RUQ.0000000000000389. [DOI] [PubMed] [Google Scholar]
- 13.Markowitz J (2011) Chapter 4. Probe selection, machine controls, and equipment. Carmody KA, Moore CL, Feller-Kopman D (eds) Handbook of critical care and emergency ultrasound. McGraw Hill. https://accessanesthesiology.mhmedical.com/content.aspx?bookid=517§ionid=41066790. Accessed 15 Sept 2022
- 14.Wolters K, Herget-Rosenthal S, Langenbeck M. Renal sonography. Internist. 2012;53:282–290. doi: 10.1007/s00108-011-2960-y. [DOI] [PubMed] [Google Scholar]
- 15.Stock KF. Klinischer Ultraschall in der Nephrologie. Nephrology. 2021;16:189–199. doi: 10.1007/s11560-021-00499-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cosgrove DO, Chan KE. Renal transplants: what ultrasound can and cannot do. Ultrasound Q. 2008;24:77–87. doi: 10.1097/RUQ.0b013e31817c5e46. [DOI] [PubMed] [Google Scholar]
- 17.Parri N, Berant R, Giacalone M, Corsini I, Titomanlio L, Connolly J, Kwan C, Teng D, European Society of Emergency Pediatrics (EUSEP), the Ultrasound Section of the European Society for Emergency Medicine (EUSEM), and the Pediatric Emergency Medicine Point-of-Care Ultrasound (P2) Network Point-of-care ultrasonography in pediatrics. Pediatr Radiol. 2021;51:1271–1272. doi: 10.1007/s00247-021-05077-w. [DOI] [PubMed] [Google Scholar]
- 18.Shah HU, Ojili V. Multimodality imaging spectrum of complications of horseshoe kidney. Indian J Radiol Imaging. 2017;27:133–140. doi: 10.4103/ijri.IJRI_298_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gimpel C, Avni EF, Breysem L, Burgmaier K, Caroli A, Cetiner M, Haffner D, Hartung EA, Franke D, König J, Liebau MC, Mekahli D, Ong ACM, Pape L, Titieni A, Torra R, Winyard PJD, Schaefer F. Imaging of kidney cysts and cystic kidney diseases in children: an International Working Group consensus statement. Radiology. 2019;290:769–782. doi: 10.1148/radiol.2018181243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Thomas CC, Jana M, Sinha A, Bagga A, Ramachandran A, Sudhakaran D, Gupta AK. Ultrasound imaging of renal cysts in children. J Ultrasound Med. 2021;40:621–635. doi: 10.1002/jum.15435. [DOI] [PubMed] [Google Scholar]
- 21.Puttmann K, Dajusta D, Rehfuss AW. Does twinkle artifact truly represent a kidney stone on renal ultrasound? J Pediatr Urol. 2021;17:475.e1–475.e6. doi: 10.1016/j.jpurol.2021.03.026. [DOI] [PubMed] [Google Scholar]
- 22.Koratala A, Bhattacharya D, Chamarthi G. Point-of-care renal ultrasound: interpret with care. Clin Case Rep. 2019;7:233–235. doi: 10.1002/ccr3.1934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bejjanki H, Santos AH, Koratala A. Postbiopsy arteriovenous fistula in renal allograft: an ultrasound case study. Clin Case Rep. 2019;7:834–835. doi: 10.1002/ccr3.2059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guedj R, Escoda S, Blakime P, Patteau G, Brunelle F, Cheron G. The accuracy of renal point of care ultrasound to detect hydronephrosis in children with a urinary tract infection. Eur J Emerg Med. 2015;22:135–138. doi: 10.1097/MEJ.0000000000000158. [DOI] [PubMed] [Google Scholar]
- 25.Hsieh YC, Tsai WS, Tsau YK. Urinary bladder outlet obstruction in children. Zhonghua Minguo Xiao Er Ke Yi Xue Hui Za Zhi. 1998;39:376–379. [PubMed] [Google Scholar]
- 26.Qi R, Yang C, Zhu T. Advances of contrast-enhanced ultrasonography and elastography in kidney transplantation: from microscopic to microcosmic. Ultrasound Med Biol. 2021;47:177–184. doi: 10.1016/j.ultrasmedbio.2020.07.025. [DOI] [PubMed] [Google Scholar]
- 27.Wheeler J, O’Riordan M, Allareddy V, Speicher D. Would the use of bedside bladder ultrasound decrease the necessity of invasive bladder catheterization in the pediatric intensive care unit? Clin Pediatr (Phila) 2015;54:800–802. doi: 10.1177/0009922814547566. [DOI] [PubMed] [Google Scholar]
- 28.Marin JR, Abo AM, Arroyo AC, Doniger SJ, Fischer JW, Rempell R, Gary B, Holmes JF, Kessler DO, Lam SH, Levine MC, Levy JA, Murray A, Ng L, Noble VE, Ramirez-Schrempp D, Riley DC, Saul T, Shah V, Sivitz AB, Tay ET, Teng D, Chaudoin L, Tsung JW, Vieira RL, Vitberg YM, Lewiss RE. Pediatric emergency medicine point-of-care ultrasound: summary of the evidence. Crit Ultrasound J. 2016;8:16. doi: 10.1186/s13089-016-0049-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chan H. Noninvasive bladder volume measurement. J Neurosci Nurs. 1993;25:309–312. doi: 10.1097/01376517-199310000-00007. [DOI] [PubMed] [Google Scholar]
- 30.Chen L, Hsiao AL, Moore CL, Dziura JD, Santucci KA. Utility of bedside bladder ultrasound before urethral catheterization in young children. Pediatrics. 2005;115:108–111. doi: 10.1542/peds.2004-0738. [DOI] [PubMed] [Google Scholar]
- 31.Witt M, Baumann BM, McCans K. Bladder ultrasound increases catheterization success in pediatric patients. Acad Emerg Med. 2005;12:371–374. doi: 10.1197/j.aem.2004.11.023. [DOI] [PubMed] [Google Scholar]
- 32.Argaiz ER, Koratala A, Reisinger N (2021) Comprehensive assessment of fluid status by point-of-care ultrasonography. Kidney360 2:1326–1338. 10.34067/KID.0006482020 [DOI] [PMC free article] [PubMed]
- 33.Lichtenstein D, Goldstein I, Mourgeon E, Cluzel P, Grenier P, Rouby JJ. Comparative diagnostic performances of auscultation, chest radiography, and lung ultrasonography in acute respiratory distress syndrome. Anesthesiology. 2004;100:9–15. doi: 10.1097/00000542-200401000-00006. [DOI] [PubMed] [Google Scholar]
- 34.Reisinger N, Koratala A (2022) Quantitative lung ultrasonography for the nephrologist: applications in dialysis and heart failure. Kidney360 3:176–184. 10.34067/KID.0003972021 [DOI] [PMC free article] [PubMed]
- 35.Jiang C, Patel S, Moses A, DeVita MV, Michelis MF. Use of lung ultrasonography to determine the accuracy of clinically estimated dry weight in chronic hemodialysis patients. Int Urol Nephrol. 2017;49:2223–2230. doi: 10.1007/s11255-017-1709-5. [DOI] [PubMed] [Google Scholar]
- 36.Noble VE, Murray AF, Capp R, Sylvia-Reardon MH, Steele DJR, Liteplo A. Ultrasound assessment for extravascular lung water in patients undergoing hemodialysis. Time course for resolution. Chest. 2009;135:1433–1439. doi: 10.1378/chest.08-1811. [DOI] [PubMed] [Google Scholar]
- 37.Cortellaro F, Ceriani E, Spinelli M, Campanella C, Bossi I, Coen D, Casazza G, Cogliati C. Lung ultrasound for monitoring cardiogenic pulmonary edema. Intern Emerg Med. 2017;12:1011–1017. doi: 10.1007/s11739-016-1510-y. [DOI] [PubMed] [Google Scholar]
- 38.Lichtenstein DA. Lung ultrasound in the critically ill. Ann Intensive Care. 2014;4:1. doi: 10.1186/2110-5820-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Volpicelli G, Elbarbary M, Blaivas M, Lichtenstein DA, Mathis G, Kirkpatrick AW, Melniker L, Gargani L, Noble VE, Via G, Dean A, Tsung JW, Soldati G, Copetti R, Bouhemad B, Reissig A, Agricola E, Rouby JJ, Arbelot C, Liteplo A, Sargsyan A, Silva F, Hoppmann R, Breitkreutz R, Seibel A, Neri L, Storti E, Petrovic T, International Liaison Committee on Lung Ultrasound (ILC-LUS) for International Consensus Conference on Lung Ultrasound (ICC-LUS) International evidence-based recommendations for point-of-care lung ultrasound. Intensive Care Med. 2012;38:577–591. doi: 10.1007/s00134-012-2513-4. [DOI] [PubMed] [Google Scholar]
- 40.Picano E, Pellikka PA. Ultrasound of extravascular lung water: a new standard for pulmonary congestion. Eur Heart J. 2016;37:2097–2104. doi: 10.1093/eurheartj/ehw164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lichtenstein DA, Mezière GA. Relevance of lung ultrasound in the diagnosis of acute respiratory failure: the BLUE protocol. Chest. 2008;134:117–125. doi: 10.1378/chest.07-2800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Buonsenso D, Soldati G, Curatola A, Morello R, De Rose C, Vacca ME, Lazzareschi I, Musolino AM, Valentini P. Lung ultrasound pattern in healthy infants during the first 6 months of life. J Ultrasound Med. 2020;39:2379–2388. doi: 10.1002/jum.15347. [DOI] [PubMed] [Google Scholar]
- 43.Covic A, Siriopol D, Voroneanu L. Use of lung ultrasound for the assessment of volume status in CKD. Am J Kidney Dis. 2018;71:412–422. doi: 10.1053/j.ajkd.2017.10.009. [DOI] [PubMed] [Google Scholar]
- 44.Musolino AM, Tomà P, De Rose C, Pitaro E, Boccuzzi E, De Santis R, Morello R, Supino MC, Villani A, Valentini P, Buonsenso D. Ten years of pediatric lung ultrasound: a narrative review. Front Physiol. 2021;12:721951. doi: 10.3389/fphys.2021.721951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lovrenski J, Petrović S, Balj-Barbir S, Jokić R, Vilotijević-Dautović G. Stethoscope vs. ultrasound probe - which is more reliable in children with suspected pneumonia? Acta Med Acad. 2016;45:39–50. doi: 10.5644/ama2006-124.155. [DOI] [PubMed] [Google Scholar]
- 46.Ciumanghel A, Siriopol I, Blaj M, Siriopol D, Gavrilovici C, Covic A. B-lines score on lung ultrasound as a direct measure of respiratory dysfunction in ICU patients with acute kidney injury. Int Urol Nephrol. 2018;50:113–119. doi: 10.1007/s11255-017-1730-8. [DOI] [PubMed] [Google Scholar]
- 47.Coley BD. Chest sonography in children: current indications, techniques, and imaging findings. Radiol Clin North Am. 2011;49:825–846. doi: 10.1016/j.rcl.2011.06.008. [DOI] [PubMed] [Google Scholar]
- 48.Chen L, Zhang Z. Bedside ultrasonography for diagnosis of pneumothorax. Quant Imaging Med Surg. 2015;5:618–623. doi: 10.3978/j.issn.2223-4292.2015.05.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang Z. Double lung point in an 18-month-old child: a case report and literature review. J Thorac Dis. 2015;7:E50–53. doi: 10.3978/j.issn.2072-1439.2015.01.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.McLario DJ, Sivitz AB. Point-of-care ultrasound in pediatric clinical care. JAMA Pediatr. 2015;169:594–600. doi: 10.1001/jamapediatrics.2015.22. [DOI] [PubMed] [Google Scholar]
- 51.Kühn B, Peters J, Marx GR, Breitbart RE. Etiology, management, and outcome of pediatric pericardial effusions. Pediatr Cardiol. 2008;29:90–94. doi: 10.1007/s00246-007-9014-1. [DOI] [PubMed] [Google Scholar]
- 52.Mertens L, Seri I, Marek J, Arlettaz R, Barker P, McNamara P, Moon-Grady AJ, Coon PD, Noori S, Simpson J, Lai WW, Writing Group of the American Society of Echocardiography; European Association of Echocardiography; Association for European Pediatric Cardiologists Targeted neonatal echocardiography in the neonatal intensive care unit: practice guidelines and recommendations for training. Writing Group of the American Society of Echocardiography (ASE) in collaboration with the European Association of Echocardiography (EAE) and the Association for European Pediatric Cardiologists (AEPC) J Am Soc Echocardiogr. 2011;24:1057–1078. doi: 10.1016/j.echo.2011.07.014. [DOI] [PubMed] [Google Scholar]
- 53.Nidorf SM, Picard MH, Triulzi MO, Thomas JD, Newell J, King ME, Weyman AE. New perspectives in the assessment of cardiac chamber dimensions during development and adulthood. J Am Coll Cardiol. 1992;19:983–988. doi: 10.1016/0735-1097(92)90282-r. [DOI] [PubMed] [Google Scholar]
- 54.Howard LS, Grapsa J, Dawson D, Bellamy M, Chambers JB, Masani ND, Nihoyannopoulos P, Simon R, Gibbs J. Echocardiographic assessment of pulmonary hypertension: standard operating procedure. Eur Respir Rev. 2012;21:239–248. doi: 10.1183/09059180.00003912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Labovitz AJ, Noble VE, Bierig M, Goldstein SA, Jones R, Kort S, Porter TR, Spencer KT, Tayal VS, Wei K. Focused cardiac ultrasound in the emergent setting: a consensus statement of the American Society of Echocardiography and American College of Emergency Physicians. J Am Soc Echocardiogr. 2010;23:1225–1230. doi: 10.1016/j.echo.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 56.Yamada H, Ito H. Fujiwara M (2022) Cardiac and vascular point-of-care ultrasound: current situation, problems, and future prospects. J Med Ultrason. 2001 doi: 10.1007/s10396-021-01166-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Via G, Hussain A, Wells M, Reardon R, ElBarbary M, Noble VE, Tsung JW, Neskovic AN, Price S, Oren-Grinberg A, Liteplo A, Cordioli R, Naqvi N, Rola P, Poelaert J, Guliĉ TG, Sloth E, Labovitz A, Kimura B, Breitkreutz R, Masani N, Bowra J, Talmor D, Guarracino F, Goudie A, Xiaoting W, Chawla R, Galderisi M, Blaivas M, Petrovic T, Storti E, Neri L, Melniker L, International Liaison Committee on Focused Cardiac UltraSound (ILC-FoCUS); International Conference on Focused Cardiac UltraSound (IC-FoCUS) International evidence-based recommendations for focused cardiac ultrasound. J Am Soc Echocardiogr. 2014;27:683.e1–683.e33. doi: 10.1016/j.echo.2014.05.001. [DOI] [PubMed] [Google Scholar]
- 58.Singh Y. Commentary: echocardiographic evaluation of hemodynamics in neonates and children. Front Pediatr. 2018;6:76. doi: 10.3389/fped.2018.00076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kwon H, Jung JY, Lee JH, Kwak YH, Kim do K, Jung JH, Chang IW, Kim K. Sonographic aorta/IVC cross-sectional area index for evaluation of dehydration in children. Am J Emerg Med. 2016;34:1840–1844. doi: 10.1016/j.ajem.2016.06.060. [DOI] [PubMed] [Google Scholar]
- 60.Marbach JA, Almufleh A, Di Santo P, Simard T, Jung R, Diemer G, West FM, Millington SJ, Mathew R, Le May MR, Hibbert B. A shifting paradigm: the role of focused cardiac ultrasound in bedside patient assessment. Chest. 2020;158:2107–2118. doi: 10.1016/j.chest.2020.07.021. [DOI] [PubMed] [Google Scholar]
- 61.Burton L, Bhargava V, Kong M. Point-of-care ultrasound in the pediatric intensive care unit. Front Pediatr. 2022;9:830160. doi: 10.3389/fped.2021.830160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Spurney CF, Sable CA, Berger JT, Martin GR. Use of a hand-carried ultrasound device by critical care physicians for the diagnosis of pericardial effusions, decreased cardiac function, and left ventricular enlargement in pediatric patients. J Am Soc Echocardiogr. 2005;18:313–319. doi: 10.1016/j.echo.2004.10.016. [DOI] [PubMed] [Google Scholar]
- 63.Orso D, Paoli I, Piani T, Cilenti FL, Cristiani L, Guglielmo N. Accuracy of ultrasonographic measurements of inferior vena cava to determine fluid responsiveness: a systematic review and meta-analysis. J Intensive Care Med. 2020;35:354–363. doi: 10.1177/0885066617752308. [DOI] [PubMed] [Google Scholar]
- 64.Levine AC, Shah SP, Umulisa I, Munyaneza RB, Dushimiyimana JM, Stegmann K, Musavuli J, Ngabitsinze P, Stulac S, Epino HM, Noble VE. Ultrasound assessment of severe dehydration in children with diarrhea and vomiting. Acad Emerg Med. 2010;17:1035–1041. doi: 10.1111/j.1553-2712.2010.00830.x. [DOI] [PubMed] [Google Scholar]
- 65.Beaubien-Souligny W, Rola P, Haycock K, Bouchard J, Lamarche Y, Spiegel R, Denault AY. Quantifying systemic congestion with point-of-care ultrasound: development of the venous excess ultrasound grading system. Ultrasound J. 2020;12:16. doi: 10.1186/s13089-020-00163-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Samant S, Koratala A. Point-of-care Doppler ultrasound in the management of hyponatremia: another string to nephrologists’ Bow. Clin Case Rep. 2021;9:e04687. doi: 10.1002/ccr3.4687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Moore CL, Copel JA. Point-of-care ultrasonography. N Engl J Med. 2011;364:749–757. doi: 10.1056/NEJMra0909487. [DOI] [PubMed] [Google Scholar]
- 68.Spencer KT, Kimura BJ, Korcarz CE, Pellikka PA, Rahko PS, Siegel RJ. Focused cardiac ultrasound: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2013;26:567–581. doi: 10.1016/j.echo.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 69.Koratala A (2021) Lung and cardiac ultrasound for assessment of intravascular volume status in children. In: Sethi SK, Raina R, McCulloch M, Bunchman TE (eds) Advances in critical care pediatric nephrology: point of care ultrasound and diagnostics. Springer, Singapore. 10.1007/978-981-33-4554-6
- 70.Adler AC, Brown KA, Conlin FT, Thammasitboon S, Chandrakantan A. Cardiac and lung point-of-care ultrasound in pediatric anesthesia and critical care medicine: uses, pitfalls, and future directions to optimize pediatric care. Paediatr Anaesth. 2019;29:790–798. doi: 10.1111/pan.13684. [DOI] [PubMed] [Google Scholar]
- 71.Hunter RW, Ramaswamy R, Patel D, Dhaun N (2017) Ultrasound-guided renal biopsy. Br J Hosp Med (Lond) 78:C56–C59. 10.12968/hmed.2017.78.4.C56 [DOI] [PubMed]
- 72.Weekes AJ, Johnson DA, Keller SM, Efune B, Carey C, Rozario NL, Norton HJ. Central vascular catheter placement evaluation using saline flush and bedside echocardiography. Acad Emerg Med. 2014;21:65–72. doi: 10.1111/acem.12283. [DOI] [PubMed] [Google Scholar]
- 73.Ward F, Faratro R, McQuillan RF. Ultrasound-guided cannulation of the hemodialysis arteriovenous access. Semin Dial. 2017;30:319–325. doi: 10.1111/sdi.12603. [DOI] [PubMed] [Google Scholar]
- 74.Latich I, Luciano RL, Mian A. Image-guided approach to peritoneal dialysis catheter placement. Tech Vasc Interv Radiol. 2017;20:75–81. doi: 10.1053/j.tvir.2016.11.010. [DOI] [PubMed] [Google Scholar]
- 75.Ash S, Sequeira A, Narayan R. Imaging and peritoneal dialysis catheters. Semin Dial. 2017;30:338–346. doi: 10.1111/sdi.12607. [DOI] [PubMed] [Google Scholar]
- 76.Koratala A, Kazory A. An introduction to point-of-care ultrasound: Laennec to Lichtenstein. Adv Chronic Kidney Dis. 2021;28:193–199. doi: 10.1053/j.ackd.2021.07.002. [DOI] [PubMed] [Google Scholar]
- 77.Conlon TW, Kantor DB, Su ER, Basu S, Boyer DL, Haileselassie B, Petersen TL, Su F, Nishisaki A. Diagnostic bedside ultrasound program development in pediatric critical care medicine: results of a national survey. Pediatr Crit Care Med. 2018;19:e561–e568. doi: 10.1097/PCC.0000000000001692. [DOI] [PubMed] [Google Scholar]
- 78.Koratala A, Segal MS, Kazory A. Integrating point-of-care ultrasonography into nephrology fellowship training: a model curriculum. Am J Kidney Dis. 2019;74:1–5. doi: 10.1053/j.ajkd.2019.02.002. [DOI] [PubMed] [Google Scholar]
- 79.Koratala A, Olaoye OA, Bhasin-Chhabra B, Kazory A (2021) A blueprint for an integrated point-of-care ultrasound curriculum for nephrology trainees. Kidney360 2:1669–1676. 10.34067/KID.0005082021 [DOI] [PMC free article] [PubMed]
- 80.Koratala A, Reisinger N (2021) POCUS for nephrologists: basic principles and a general approach. Kidney360 2:1660–1668. 10.34067/KID.0002482021 [DOI] [PMC free article] [PubMed]