Abstract
The COVID-19 pandemic has been particularly difficult for mothers. Women with a history of peripartum depression (PPD) may be vulnerable to relapse. We sought to understand changes in depressive and anxious symptoms throughout the pandemic and which stressors increased symptoms in women with a history of PPD. In June 2020, all US participants with a history of PPD (n = 12,007) in the global MomGenes Fight PPD study were invited to the COVID-19 follow-up study. Respondents (n = 2163, 18%) were sent biweekly and then monthly surveys until January 31, 2022. We employed time-varying effects models to evaluate trajectories of depressive (patient health questionnaire, PHQ-9) and anxious (generalized anxiety disorder, GAD-7) symptoms and to estimate longitudinal associations between perceived stress, fears, COVID-19 case rates, and symptoms. Peaks of PHQ-9, GAD-7, PSS, and perceived COVID-19 risk scores corresponded with timing of national COVID-19 case surges. High perceived stress was the strongest predictor of PHQ-9 (beta = 7.27; P = 1.48e − 38) and GAD-7 (beta = 7.73; P = 6.19e − 70). Feeling lack of control and unlikely to survive increased PHQ-9 and GAD-7 scores by 2 points. COVID-19 case rates, pandemic restrictions, and region were not independently associated with symptoms. This study suggests that the collective trauma of the pandemic has significantly affected mothers with a history of PPD, exemplified by high levels of perceived stress and the strong association with depressive and anxious symptoms. The next pandemic phase is uncertain, but will continue to influence mental health collectively and dynamically. Interventions must be flexible and responsive and should address fear, trauma, and feelings of control, particularly for mothers with a history of PPD.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00737-022-01265-1.
Keywords: Depression, Anxiety, COVID-19, Postpartum, Stress, Longitudinal
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has widely impacted society, causing health risks, economic vulnerability, food insecurity, school and business closures, and disruption of social support networks (Guo et al. 2021). Over one million people in the US have died of COVID-19 (Centers for Disease Control and Prevention 2022b), and nine times that have lost a family member (Verdery et al. 2020). Adverse life events increase risk of mental illness and the collective stress and trauma of the COVID-19 pandemic has increased prevalence of mental illness (Kessler et al. 2022). Meta-analyses suggest depressive and anxious symptoms have increased two- to threefold worldwide (Arora et al. 2022; Ettman et al. 2020) resulting in 53.2 million additional cases of major depressive disorder and 76.2 million additional cases of anxiety disorders globally (Santomauro et al. 2021).
The lives of mothers have been notably disrupted by lack of childcare, supervising at-home learning, and caregiving of family members at risk of COVID-19 complications (Frank et al. 2021; MCGoron et al. 2021). In a meta-analysis of 18 studies of 8981 mothers of children under 5 years old during the first year of the pandemic, 26.9% (95% CI: 21.3–33.4) experienced clinically significant depressive symptoms and 41.9% (95% CI: 26.7–58.8) experienced anxious symptoms (Racine et al. 2022). Several studies show large declines in mental health after the pandemic onset. In a cohort of low-income mothers in Toronto, 83% reported decreases in at least one indicator of mental health between the data collection wave prior to the pandemic and during the pandemic (May–November 2020) (Saleem et al. 2022). A large study in the UK found clinically relevant depressive symptoms in mothers increased from 11% prior to the pandemic (January 2016–March 2020) to 20% during the pandemic (March–June 2020) and anxious symptoms increased from 10 to 16% (Dickerson et al. 2022). Postpartum women are particularly vulnerable; pooled prevalence of postpartum depression in a meta-analysis of pandemic studies was 34% (95% CI: 21–46) (Chen et al. 2022), though as many as 75% reported symptoms in a small US sample (Goyal et al. 2022). In the few studies of perinatal mental health during COVID-19, there were pandemic increases in depressive (Zhang et al. 2022) and anxious (Overbeck et al. 2022; Zhang et al. 2022) symptoms for postpartum women, but not pregnant women. The diverse and pervasive effects of pandemic parenting-related stressors may pose particular risk for women with a past history of peripartum depression (PPD) and put them at significant risk of relapse.
Few large studies have focused on mental health of mothers during the pandemic, and those that do are mostly cross-sectional or have a brief length of follow-up. Although there have been many longitudinal COVID-19 mental health studies (COVID-Minds Network 2021; Unnarsdóttir et al. 2021), few focus on maternal mental health; all take place in Canada, Denmark, and the UK; and none specifically assess PPD history (Dickerson et al. 2022; Ladekarl et al. 2021; Overbeck et al. 2022; Racine et al. 2022; Saleem et al. 2022; Zhang et al. 2022). Only one Danish cohort examines symptom trajectories at multiple timepoints throughout the pandemic, and they found no differences (Overbeck et al. 2022). Depressive and anxious symptoms can be dynamic, and understanding how symptoms and perceptions change over time in response to population-level events can help us predict and prepare for waves of distress.
Our study of mothers with a history PPD is the largest US national study of PPD to date. To our knowledge, it is also the only national longitudinal US sample following mothers throughout the COVID-19 pandemic. In this study, we aimed to (1) describe psychiatric and sociodemographic factors during the COVID-19 pandemic among women with a history of PPD; (2) examine trajectories of depressive symptoms, anxious symptoms, perceived stress, and pandemic-related fears; and (3) assess the extent to which COVID-19 prevalence and pandemic-related stressors are associated with depressive and anxious symptom trajectories.
Methods
Participants for this study were recruited from the MomGenes Fight PPD study (http://momgenesfightppd.org/), which is a global collaboration to understand the biological basis of PPD. MomGenes Fight PPD began recruitment in March 2016 and is ongoing. Women enroll in the study through a mobile app designed for Apple iOS and Android devices to screen for PPD and obtain information about mood, childbirth, and demography. Participants are assessed at enrollment with the lifetime version of the Edinburgh Postnatal Depression Scale (EPDS), which has been validated in this cohort (Meltzer-Brody et al. 2013). The 10-item EPDS (Cox et al. 1987) is the most commonly used PPD instrument (Boyd et al. 2005; Hewitt & Gilbody 2009; Hewitt et al. 2009) and is scored on a scale of 0–30 with higher scores indicating greater symptom severity. PPD cases are defined as EPDS score ≥ 13 (a standard threshold for PPD) (Cox et al. 1987; Wisner et al. 2002), with symptom onset during pregnancy or < 3 months postpartum, and symptom duration > 2 weeks. Participants are excluded if the child is > 6 weeks preterm, mother or child experienced a perinatal life-threating illness, or the child died. A description of the MomGenes Fight PPD study protocol and cohort description from the first year of recruitment has been previously published (Guintivano et al. 2018).
In June 2020, we contacted participants enrolled in the US-based arm of the MomGenes Fight PPD study. All 12,007 participants with a history of PPD who had previously enrolled in the MomGenes Fight PPD study were invited to participate in the COVID-19 pandemic follow-up study. Participants in the COVID-19 pandemic follow-up study consented to participate and received questionnaires via email inquiring about mental health outcomes, sociodemographic characteristics, and pandemic-specific stressors. Surveys began June 30, 2020, and were completed biweekly for the first 3 months and then monthly thereafter. The MomGenes Fight PPD study is in concordance with the Helsinki Declaration and was approved by the Institutional Review Board of the University of North Carolina at Chapel Hill (IRB Number: 15–2165). The study protocol was amended to include the COVID-19 follow-up questionnaires, and the modification was approved by the IRB in May 2020.
Measures
Outcomes
Primary outcomes of interest were depressive and anxious symptoms. We measured depressive symptoms with the Patient Health Questionnaire-9 (PHQ-9) (Kroenke and Spitzer 2002). Scores range from 0 to 27 and standard symptom categories are defined as none (0–4), mild (5–9), moderate (10–14), moderately severe (15–19), and severe (≥ 20). Scores of ≥ 10 were considered clinically significant for binary outcomes (Kroenke and Spitzer 2002). We assessed anxious symptoms with the 7-item Generalized Anxiety Disorder Questionnaire (GAD-7) (Spitzer et al. 2006). Scores range 0 to 21, and standard categories are defined as none (0–5), mild (6–10), moderate (11–15), and severe (> 15). GAD-7 scores of ≥ 10 were considered clinically significant (Spitzer et al. 2006). The PHQ-9 and GAD-7 are widely used and validated in peripartum populations (Simpson et al. 2014).
Demographic characteristics, environment, and health status
Baseline demographic information about maternal age, race/ethnicity, parity, age at worst PPD episode, time since worst PPD episode, EPDS score, and psychiatric history was obtained from survey responses at time of enrollment into the MomGenes Fight PPD study prior to the pandemic. Because participants may have moved or changed jobs due to pandemic-related factors, we asked about zip code, household membership, employment status, and occupation in the first COVID-19 survey. In each follow-up survey during the COVID-19 pandemic, we also asked about ongoing health status, including whether the participant was currently pregnant, smoking status, any current treatment for major depressive disorder (MDD), COVID-19 risk factors (lung disease or asthma, heart condition, immunocompromise, diabetes, renal failure, liver disease, HIV/AIDS, high blood pressure), COVID-19 symptoms, and COVID-19 diagnosis.
Perceived stress, life events, and perceived risk of COVID-19
We were interested in how perceived stress varied over the course of the pandemic, and the extent to which stressful life events and perceived risk of COVID-19 were associated with depressive and anxious symptoms. We used the Perceived Stress Scale (Sheldon Cohen et al. 1983) to quantify how unpredictable, uncontrollable, and overloaded respondents found their lives. Scores range from 0 to 40 and scores > 13 indicate a high degree of perceived stress (S Cohen and Williamson 1988). We asked about major life events, including change in employment, change in household membership, and knowing someone who died of COVID and their relationship to the participant. We asked about COVID prevention measures occurring in their area that may have disrupted regular routines, including stay-at-home/shelter-in-place ordinances, school closings, or remote work. To assess perceived risk of specific COVID-19 threats, we asked questions adapted from the Perceived SARS-Related Risk Scale (Wu et al. 2009) which inquires about fears, worries, and control about infection, transmission and survival of COVID-19. We aggregated these responses into a total COVID-19 risk perception score to enable us to assess change in risk perception continuously over time.
COVID-19 metrics
We plotted national daily COVID-19 cases and 7-day rolling averages obtained from the CDC (Centers for Disease Control and Prevention 2022b). We then geographically linked participant data with covid metrics. Using Housing and Urban Development/US Postal Service zip code crosswalk files (US Department of Housing and Urban Development 2010), we joined geographic Federal Information Processing System county code and date to obtain local case and vaccination rates for each individual at each time point. County level rolling averages of COVID-19 cases per 100,000 population were obtained from the New York Times (The New York Times 2021) and county level vaccination data came from the CDC (Centers for Disease Control and Prevention 2022a).
Statistical analysis
We described characteristics of participants who completed our baseline COVID-19 survey. To visualize changes in depressive symptoms, anxious symptoms, perceived stress, and perceived risk across time, we plotted smoothed mean PHQ-9, GAD-7, PSS, and COVID-19 risk perception scores from June 30, 2020, to January 31, 2022. We also plotted US national COVID-19 case numbers and smoothed mean local COVID-19 case rates for the same time period to observe how symptom trajectories corresponded to the trajectory of the pandemic. Based on peaks and troughs of COVID-19 case trajectories, we selected five distinct timepoints to investigate in more detail: July 2020 (baseline), January 2021 (winter peak of COVID-19 cases), June 2021 (low COVID-19 cases), August 2021 (rising COVID-19 cases due to Delta variant and school reopenings), and December 2021 (rising COVID-19 cases due to initial Omicron variant). We calculated descriptive statistics at each timepoint to understand how depressive and anxious symptoms, stress, life events, and COVID-specific factors differed. To observe time trends, we plotted percentages of participants meeting clinically significant symptom thresholds, specific COVID-19 fears and concerns, experiences with COVID-19 illness, and presence of local pandemic-related restrictions.
We were particularly interested in whether specific pandemic-related stressors increase depressive or anxiety symptoms, but both predictors and outcomes change significantly over time. To account for dynamic relationships and correlation among individuals across time, we employed time-varying effects models (TVEM) using the tvem package in R (https://github.com/dziakj1/TvemPackage_development) to estimate associations between predictors of interest and PHQ-9 and GAD-7 scores. TVEMs are particularly well-suited for intensive longitudinal data and apply penalized B-spline models as an extension of generalized estimating equations with sandwich standard errors to allow flexibility across time and account for within-subject correlation (Tan et al. 2012). We selected predictors for our final adjusted multivariate model based on data visualization and known risk factors for MDD and GAD. Maternal age, race, time since worst PPD episode, EPDS at worst PPD episode, and history of suicidal ideation were included as time-invariant predictors. County-level COVID-19 case rates per 100,000, high stress (PSS ≥ 14), local COVID-19 restrictions (stay-at-home/shelter-in-place ordinances, school closures, or work-from-home recommendations), feeling lack of control over getting infected, thinking survival unlikely if infected, US census region, and parity were modeled as time-varying predictors. A stringent Bonferroni corrected significance threshold of p < 0.001 accounted for multiple comparisons.
To check for informative missingness, we applied Little’s test for missing completely at random (MCAR) data (Little 1988). As expected, data were not MCAR, so we plotted patterns of PHQ-9 and GAD-7 outcomes by completed visits to check for systematic variation. Because time-varying effect models use listwise deletion for missing data, we used random forest imputation (missForest, R 4.1.2) for missing data.
Results
Of the 12,007 women with PPD who previously participated in MomGenes Fight PPD, 2163 (18%) individuals responded at least once. Responders were slightly older, less racially and ethnically diverse, older at age of worst PPD episode, and more often sought depression or anxiety treatment than non-responders (Supplementary Table S1). There was significant loss to follow-up, and 24.8% of participants only completed the baseline survey (Supplementary Fig. S1a). Participants completed five surveys on average, but half of all surveys were completed within the first 6 months of the study (Supplementary Fig. S1b). Only 38 participants completed surveys through the end of the study period. We did not observe any strong evidence for differential loss to follow-up by outcome (Supplementary Figs. S1c, S1d).
Participant characteristics are described in Table 1. Mean age of participants was 34 years, and most were White (92%) and lived in urban environments (91%). Respondents resided throughout all 50 US states, the District of Columbia, and Guam. Participants were well-distributed throughout the USA, but most (34%) resided in the US South (US Census Bureau defined regions (US Census Bureau 2010)). Most participants (72%) had 2–3 children. Most women (55%) were within 2 years of their worst PPD episode, but nearly 10% had PPD over 10 years ago. Sixty-two percent of women were being treated for depression at baseline.
Table 1.
Characteristics of the study population at baseline (n = 2163)
| Characteristica | ||
|---|---|---|
| Maternal age (years) | ||
| Mean (SD) | 34.1 (6.3) | |
| Median (IQR) | 33 (30–37) | |
| Range | 18–82 | |
| Race/ethnicity (n, %) | ||
| White | 1973 | 91.5 |
| Black | 14 | 0.6 |
| Hispanic | 114 | 5.3 |
| Asian | 32 | 1.5 |
| Native American, Pacific Islander, Other | 22 | 1.0 |
| US census region (n, %) | ||
| Northeast | 374 | 17.4 |
| Midwest | 439 | 20.4 |
| South | 745 | 34.7 |
| West | 586 | 27.3 |
| Urban (n, %) | 1941 | 90.5 |
| Parity | ||
| Mean (SD) | 2.1 (0.9) | |
| Median (IQR) | 2 (2–2) | |
| Range | 1–8 | |
| Age at worst episode (years) | ||
| Mean (SD) | 30.1 (4.4) | |
| Median (IQR) | 30 (27–33) | |
| Range | 15–44 | |
| Time since worst episode (years) | ||
| Mean (SD) | 4.0 (5.5) | |
| Median (IQR) | 2 (1–5) | |
| Range | 0–52 | |
| EPDS score | ||
| Mean (SD) | 22.5 (3.7) | |
| Median (IQR) | 23 (20–25) | |
| Range | 0–30 | |
| Current treatment for depression (n, %) | 1331 | 61.5 |
| History of professional help for depression/anxiety (n, %) | 1638 | 75.7 |
| History of medication for depression/anxiety (n, %) | 1366 | 63.2 |
| History of hospitalization for depression/anxiety (n, %) | 131 | 6.1 |
| History of suicidal ideation (n, %) | 382 | 17.6 |
| History of postpartum psychosis (n, %) | 255 | 11.8 |
US Census Region residence, urban residence, and current treatment for depression were obtained from the first COVID-19 survey sent in July 2020. All other characteristics were obtained from responses to the survey at enrollment into the larger MomGenes Fight PPD study prior to the COVID-19 pandemic
aMissing values: race (8), region (19), urbanicity (19), parity (729), age at worst episode (1), time since worst episode (1), history of professional help (1), history of medication (1), history of hospitalization (1), history of suicidal ideation (1323)
Women in our study experienced relatively severe depression during their worst peripartum episode (EPDS mean = 22.5, SD = 3.7); mothers scoring 13 or greater are likely to be suffering from a depressive episode. Of these women, 76% had previously sought professional help for depression or anxiety, 63% had taken medication for depression or anxiety, 6% had a psychiatric hospitalization, and 18% experienced peripartum suicidal ideation (Table 1).
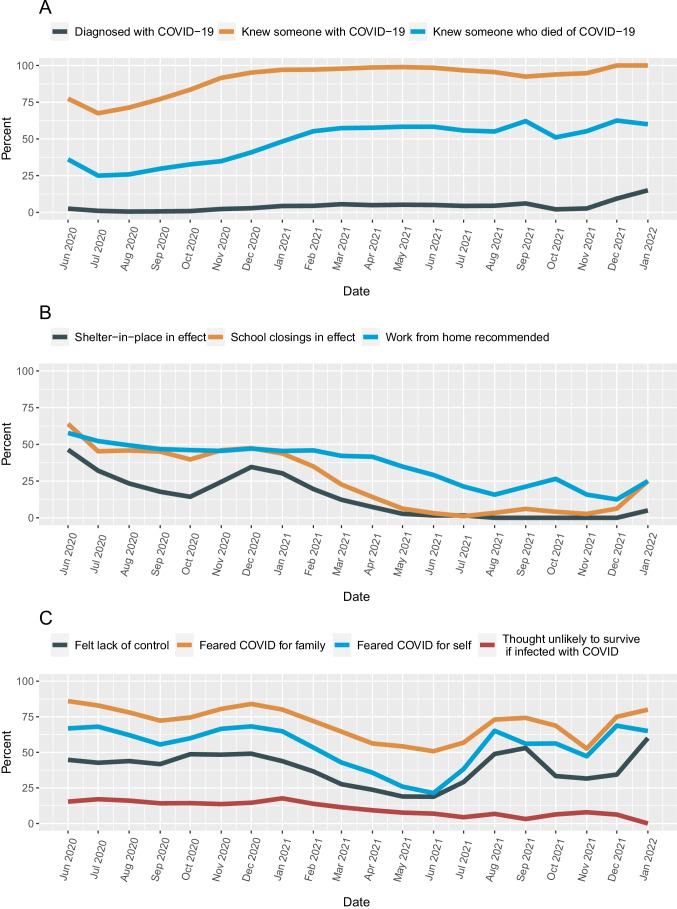
PHQ-9, GAD-7, PSS, and perceived COVID-19 risk score trajectories all corresponded with COVID-19 case trajectory. Scores for all instruments were high in July 2020, decreasing as COVID-19 cases waned in June 2021, and rising again as cases increased during the SARS-CoV-2 Delta variant wave in late summer 2021 and subsequent Omicron variant wave in winter 2021–2022 (Fig. 1). Table 2 describes participant responses in July 2020, January 2021, June 2021, August 2021, and December 2021. Over a third of participants met clinically significant thresholds for depressive and anxious symptoms during the first year of the pandemic. Those numbers decreased to a fifth of participants in June 2021 but later rose again to early pandemic levels (Table 2).
Fig. 1.
Trajectories of COVID-19 cases, depressive symptoms (PHQ-9), anxious symptoms (GAD-7), and stress (PSS), and COVID-related fears and concerns score, June 30, 2020 to January 31, 2022
Table 2.
Characteristics of participants at five timepoints throughout the pandemic: July 2020, January 2021, June 2021, August 2021, and December 2021
| Characteristic | July 2020 (n = 1691) | January 2021 (n = 578) | June 2021 (n = 319) | August 2021 (n = 89) | December 2021 (n = 32) |
|||||
|---|---|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | N | % | |||
| PHQ-9 (mean, SD) | 7.8 (5.4) | 7.9 (5.8) | 5.7 (4.8) | 7.1 (5.5) | 7.2 (5.0) | |||||
| GAD-7 (mean, SD) | 8.3 (5.6) | 7.8 (5.6) | 5.8 (5.1) | 7.6 (5.8) | 7.8 (5.4) | |||||
| PSS (mean, SD) | 19.2 (7.5) | 18.3 (8.6) | 15.4 (8.7) | 17.6 (8.3) | 20.3 (8.6) | |||||
| PTSD (mean, SD) | 1.4 (1.4) | 1.4 (1.4) | 0.7 (1.1) | 1.4 (1.5) | 1.0 (1.3) | |||||
| PHQ-9 ≥ 10 (clinical threshold) | 541 | 32.0 | 197 | 34.1 | 62 | 19.4 | 25 | 28.1 | 10 | 31.2 |
| GAD-7 ≥ 10 (clinical threshold) | 618 | 36.5 | 196 | 33.9 | 65 | 20.4 | 31 | 34.8 | 11 | 34.5 |
| Local case rate/100 K population | 15.8 (13.8) | 58.5 (27.6) | 3.9 (2.9) | 33.9 (20.6) | 51.8 (68.7) | |||||
| Local vaccination rate | – | 3.3 (3.7) | 53.7 (25.4) | 57.6 (29.8) | 74.8 (23.1) | |||||
| School closings in effect in area | 741 | 43.8 | 253 | 43.8 | 10 | 3.1 | 3 | 3.3 | 2 | 6.3 |
| Work from home advised by workplace | 872 | 51.6 | 263 | 45.5 | 93 | 29.2 | 14 | 15.7 | 4 | 12.5 |
| Stay at home or shelter in place in effect in area | 500 | 29.5 | 175 | 30.2 | 5 | 1.6 | 0 | 0.0 | 0 | 0.0 |
| Been diagnosed with COVID | 9 | 0.5 | 25 | 4.3 | 16 | 5.0 | 4 | 4.5 | 3 | 9.4 |
| Knew someone with COVID | 1062 | 62.8 | 561 | 97.1 | 314 | 98.4 | 85 | 95.5 | 32 | 100.0 |
| Knew someone who died of COVID | 348 | 20.6 | 279 | 48.2 | 186 | 58.3 | 49 | 55.1 | 20 | 62.5 |
| Experienced change in household | 161 | 9.5 | 82 | 14.2 | 40 | 12.5 | 24 | 26.9 | 15 | 46.9 |
| Experienced change in employment | 106 | 6.3 | 116 | 20.0 | 79 | 24.8 | 19 | 21.3 | 4 | 12.5 |
| Afraid of falling ill with COVID | 1141 | 67.5 | 374 | 64.7 | 68 | 21.3 | 58 | 65.2 | 22 | 68.8 |
| Felt had little control over whether would get infected or not | 723 | 42.8 | 252 | 43.6 | 60 | 18.8 | 43 | 48.3 | 11 | 34.4 |
| Thought would be unlikely to survive if were to get COVID | 294 | 17.4 | 102 | 17.6 | 22 | 6.9 | 6 | 6.7 | 2 | 6.3 |
| Thought about resigning because of COVID | 220 | 13.0 | 46 | 8.0 | 11 | 3.4 | 11 | 12.4 | 2 | 6.3 |
| Afraid would pass COVID to others | 1072 | 63.4 | 365 | 63.1 | 97 | 30.4 | 56 | 62.9 | 23 | 71.9 |
| Family and friends were worried they might get infected through me | 336 | 19.9 | 147 | 25.4 | 26 | 8.2 | 14 | 15.7 | 4 | 12.5 |
| Afraid of a loved one falling ill with COVID | 1397 | 82.6 | 463 | 80.1 | 162 | 50.8 | 65 | 73.0 | 24 | 75.0 |
Table 3 presents adjusted time-varying effects models of longitudinal associations with PHQ-9 and GAD-7 scores. High perceived stress was the strongest predictor of both PHQ-9 (beta = 7.27; 95% CI: 6.22, 8.31; P = 1.48e − 38) and GAD-7 (beta = 7.73; 95% CI: 6.92, 8.54; P = 6.19e − 70). Feeling a lack of control about getting infected and feeling unlikely to survive if infected were both associated with an approximately 2-point increase in PHQ-9 and GAD-7 (Table 3). History of suicidal ideation and EPDS at worst PPD episode were time-invariant predictors associated with PHQ-9 and GAD-7. COVID-19 case rates, COVID-19 restrictions, and geographic region were not associated PHQ-9 or GAD-7. Parity was associated with PHQ-9 but not GAD-7 scores. Coefficients for associations between time-varying predictors and symptoms remained fairly constant, though there were some slight variations across time (Supplementary Figure S2). Table 3 presents results for data with missing values imputed. Findings for the unimputed data were similar in magnitude and significance of association, but less precise, and are reported in Supplementary Table S2.
Table 3.
Time-varying effect models of predictors of PHQ-9 and GAD-7 scores (n = 2163). Multivariate models were mutually adjusted by all other covariates, and missing data were imputed
| Beta | SE | 95% CI | P-value | ||
|---|---|---|---|---|---|
| a. Associations with depressive symptoms (PHQ-9) | |||||
| Time-invariant predictors | |||||
| Maternal age | − 0.07 | 0.023 | − 0.11, − 0.02 | 2.39E − 03 | |
| Race | 0.28 | 0.123 | 0.04, 0.52 | 0.02 | |
| Time since worst episode | 0.07 | 0.029 | 0.01, 0.12 | 0.02 | |
| EPDS at worst episode | 0.18 | 0.026 | 0.13, 0.23 | 6.42E − 12 | |
| History of suicidal ideation | 2.86 | 0.271 | 2.33, 3.39 | 3.53E − 24 | |
| Time-varying predictors (averaged over all time points) | |||||
| County cases/100 k population | − 0.00 | 0.006 | − 0.02, 0.01 | 0.99 | |
| High stress (PSS ≥ 14) | 7.27 | 0.533 | 6.22, 8.31 | 1.48E − 38 | |
| COVID-19 restrictions in place | 0.37 | 0.297 | − 0.21, 0.95 | 0.22 | |
| Felt lack of control over whether would get infected | 1.53 | 0.255 | 1.03, 2.03 | 3.97E − 09 | |
| Thought unlikely to survive if were to get COVID-19 | 2.10 | 0.450 | 1.21, 2.98 | 4.11E − 06 | |
| Region | − 0.01 | 0.235 | − 0.47, 0.45 | 0.97 | |
| Parity | 0.60 | 0.225 | 0.16, 1.04 | 7.63E − 03 | |
| b. Associations with anxious symptoms (GAD-7) | |||||
| Time-invariant predictors | |||||
| Maternal age | − 0.07 | 0.021 | − 0.11, − 0.03 | 9.01E − 04 | |
| Race | 0.05 | 0.109 | − 0.17, 0.26 | 0.68 | |
| Time since worst episode | 0.02 | 0.028 | − 0.03, 0.08 | 0.38 | |
| EPDS at worst episode | 0.14 | 0.026 | 0.09, 0.19 | 9.48E − 08 | |
| History of suicidal ideation | 2.11 | 0.276 | 1.57, 2.65 | 9.85E − 14 | |
| Time-varying predictors (averaged over all time points) | |||||
| County cases/100 k population | − 0.00 | 0.003 | − 0.01, 0.00 | 0.99 | |
| High stress (PSS ≥ 14) | 7.73 | 0.413 | 6.92, 8.54 | 6.19E − 70 | |
| COVID-19 restrictions in place | 0.29 | 0.156 | − 0.02, 0.60 | 0.06 | |
| Felt lack of control over whether would get infected | 2.07 | 0.148 | 1.78, 2.36 | 3.21E − 40 | |
| Thought unlikely to survive if were to get COVID-19 | 1.96 | 0.547 | 0.89, 3.03 | 3.73E − 04 | |
| Region | − 0.05 | 0.166 | − 0.38, 0.27 | 0.78 | |
| Parity | 0.10 | 0.240 | − 0.37, 0.57 | 0.69 | |
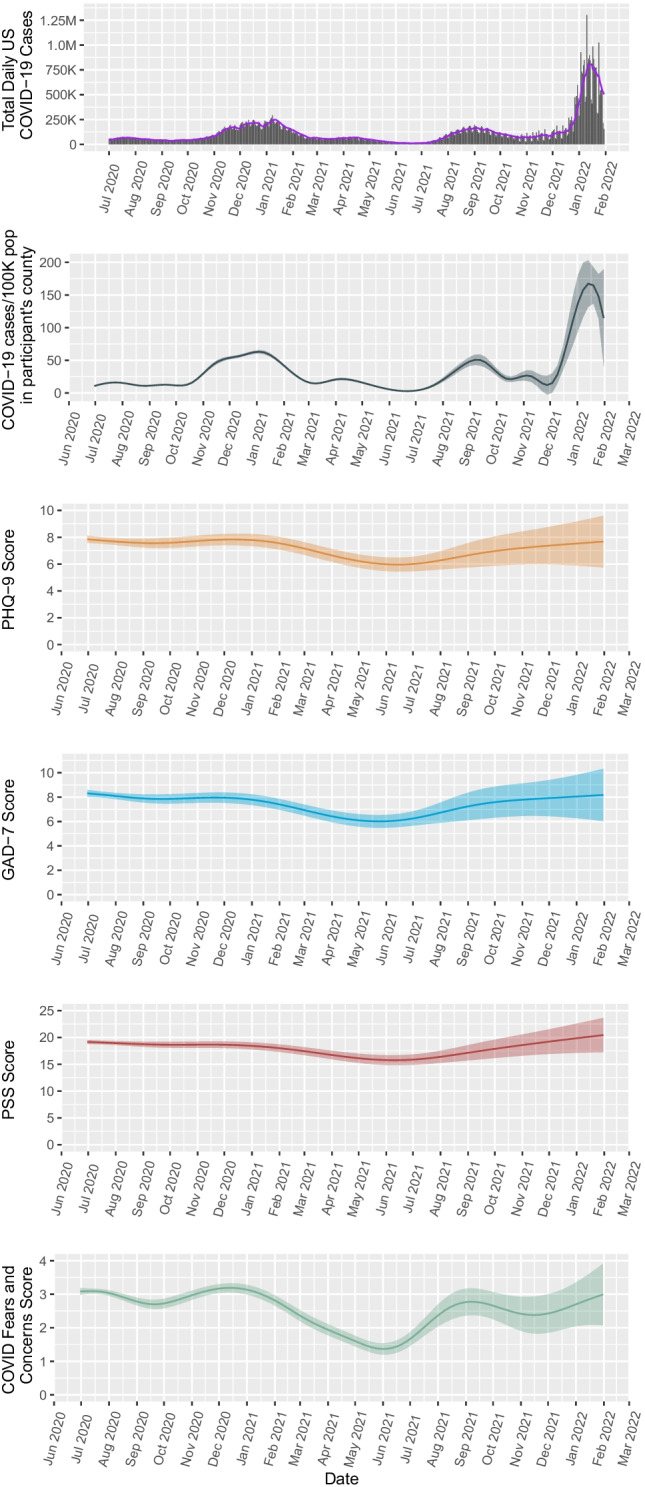
Participants experienced numerous external stressors. Average PSS scores were 19.2 (SD = 7.5) in July 2020 and after a slight decline in summer 2021 rose again (Table 2). In July 2020, about a third of participants had stay-at-home or shelter-in-place ordinances in place in their area. Approximately 50% of respondents were being advised to work from home and had school closings in effect in their area in January 2021. By August 2021, about 15% of participants were still advised to work from home by their workplace, but nearly all schools had reopened. A sizable proportion of participants experienced a change in people living in their household (27%) and a change in employment (25%). Most people were also directly affected by the consequences of COVID-19 illness. By January 2021, 97% knew someone who had been diagnosed with COVID-19. By December 2021, 63% knew someone who had died of COVID-19. Most people were afraid that they or a loved one would fall ill with COVID-19 and felt they had little control over getting infected. These fears particularly increased during times of COVID-19 case rates in December 2020, August 2021, and December 2021 (Fig. 2).
Fig. 2.
Percentage of respondents (A) affected by COVID-19 illness, (B) experiencing local COVID-19 disruptions, and (C) expressing COVID-19-related fears and concerns
Discussion
In this large, national, longitudinal study of mothers with a history of PPD, we found that depressive symptoms, anxious symptoms, perceived stress, and pandemic-related fears followed trends of COVID-19 caseload severity throughout the pandemic. Although population-level symptom trajectories aligned with pandemic trajectory, local COVID-19 prevalence was not associated with PHQ-9 or GAD-7 scores. Most participants experienced significant life stressors. High perceived stress was the factor most strongly associated with both depressive symptoms and anxious symptoms throughout the pandemic. History of suicidal ideation or high peripartum EPDS score also increased PHQ-9 and GAD-7 scores.
Our findings are comparable to global estimates of depressive and anxious symptoms. In a cross-sectional study of 64 countries in May–June 2020 (Basu et al. 2021), 31% of participants were experiencing significant symptoms, similar to the 20–40% of our sample meeting clinically significant thresholds. In that multi-country study, 86% reported being worried or very worried about COVID-19. Similarly, 70–80% of participants in our sample were worried about a loved one falling ill with COVID-19.
Surprisingly, local pandemic-related stressors such as working from home and school closings were not independently associated with depression and anxiety symptoms. Likewise, although disruptions such as household and employment changes were common, they also were not directly associated with symptoms. Conversely, high perceived stress, fear of not surviving, and lack of a sense of control were strongly associated with depressive and anxious symptoms. It is possible that response to the stressors rather than the specific stressors themselves most greatly influences symptoms (Puyané et al. 2022). We see evidence of this as COVID-19 case rate is not directly associated with depressive symptoms, but case rate is associated with perceived COVID-19 risk score, which is subsequently associated with depressive symptoms. Thus, COVID risk perception in response to changing case rates may act as a mediator. Number of children in the home may also be a factor, as parity was strongly associated with depressive symptoms. Parity was not associated with anxiety symptoms, likely due to a more uniform distribution of GAD-7 scores and low variability of parity (i.e., most mothers had two children). The relationships between difficult life events, community resources, social support, family composition, and emotional wellbeing are complex and there are likely interactions that make mothers especially susceptible to depression or anxiety during the pandemic (Racine et al. 2022).
Mental health experts have been warning of a “mental health tsunami” (American Psychological Association 2021a; Roxby 2020), and we are just beginning to understand its magnitude. Many studies showed an increase in psychiatric symptoms at the pandemic onset (American Physological Association 2020; Arora et al. 2022; Ettman et al. 2020; Kessler et al. 2022). Some longitudinal studies show consistent increases over time, though a few also suggest symptoms are stabilizing (Shevlin et al. 2021a, b; Sommerlad et al. 2021). Our study demonstrates psychiatric symptoms do not increase or decrease in a consistent manner. Symptoms broadly ebb and flow within the context of the pandemic, consistent with results of a recent multi-national European study (Unnarsdóttir et al. 2021). These fluctuations may be particularly enhanced in women with a history of PPD.
This cohort of over 2000 women is drawn from the largest study of women with PPD in the USA, which includes participants from all 50 states and Guam. Participants have been carefully phenotyped and validated for PPD. This study is unique as it contains longitudinal data at many timepoints across the past two years of the COVID-19 pandemic, enabling us to employ TVEM to address time-varying questions and empirically observe that symptoms both increase and decrease at different points in time. Although TVEM is flexible and allows for non-uniform data structures such as unequal spacing of measurements (Lanza et al. 2016), low response rate and high loss to follow-up hinder our ability to make generalizable conclusions. Of invited participants, 18% completed the baseline survey, and respondents were significantly different than non-respondents, indicating some selection bias is likely. Additionally, only 38 participants completed surveys through the end of the study period, and most surveys were completed in 2020, limiting interpretation of findings from the latter half of the study. Completion of regular questionnaires throughout a pandemic is challenging, and severe depressive or anxious symptoms likely reduce response. Like most longitudinal methods, TVEM assumes random entry and dropout. While we detected no differential dropout and used modern imputation methods to impute missing data, we did detect some non-random missingness, which may also bias results. TVEM can assess variability and associations across time, but these cannot be interpreted as causal associations (Lanza et al. 2016), and thus, findings must be interpreted with care.
MomGenes Fight PPD is an innovative study that recruited, phenotyped, and obtained genetic samples through an app-based platform. Digital health research, education, and interventions have the benefit of being adaptive and unconstrained by geographic barriers. All women in MomGenes Fight PPD remain eligible, and we are continuing surveys as we transition from the acute phase of the pandemic to COVID-19 endemicity. Digital interventions are particularly well-suited to the field of psychiatry, and the COVID-19 pandemic has already demonstrated success of a shift to virtual care for many outpatient psychiatric and psychotherapy visits (American Psychological Association 2021b). As demand for psychiatric services increases (American Physological Association 2020; American Psychological Association 2021a), digital approaches show great promise for delivering population based mental health interventions and improving access to care.
Conclusions
In our study of mothers with a history of PPD, we observed dynamic changes in depressive and anxious symptoms throughout the pandemic and, in particular, saw increases in stress and pandemic-related fear when COVID-19 cases increased. Psychiatric symptoms and national COVID-19 cases followed similar trajectories, but local COVID-19 case rates and restrictions were not independently associated with psychiatric symptoms. High perceived stress and more severe PPD (i.e., higher EPDS and suicidal ideation) had stronger associations with depressive and anxious symptoms. Although the low response rate and high loss to follow-up in this study reduce our ability to make strong recommendations, this study suggests that the collective trauma of the pandemic has significantly affected women with a history of PPD, exemplified by high levels of perceived stress and its effect on depressive and anxious symptoms. Thus, pandemic-related fear must be contextualized to enable people to regain a feeling of control over their life circumstances. Interventions to mitigate stress and prevent worsening symptoms or relapse in this vulnerable group are needed. The COVID-19 pandemic has brought large-scale, community-level effects on mental health, which will require innovative, scalable interventions to reach large numbers of people (Van Lieshout et al. 2021). Although the exact trajectory of the next phase of the COVID-19 pandemic is unknown, it will certainly influence mental health collectively and dynamically and will require flexible, responsive solutions, particularly for mothers with a history of PPD (Hermann et al. 2021).
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
We thank the MomGenes Fight PPD participants, who continue to take part in this ongoing study.
Funding
This work was supported by the Foundation of Hope and the National Institute of Mental Health (AB, grant number 5K01MH120352-03; JG, grant number 5K01MH116413-04).
Declarations
Conflict of interest
SMB receives research grant funding from Sage Therapeutics and has done educational consulting with MedScape (WebMD).
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- American Physological Association (2020) Patients with depression and anxiety surge as psychologists respond to the coronavirus pandemic. Retrieved from https://www.apa.org/news/press/releases/2020/11/anxiety-depression-treatment. Accessed 10 Apr 2022
- American Psychological Association (2021a) Demand for mental health treatment continues to increase, say psychologists. Press Release. Retrieved from https://www.apa.org/news/press/releases/2021a/10/mental-health-treatment-demand. Accessed 10 Apr 2022
- American Psychological Association (2021b) Worsening mental health crisis pressures psychologist workforce: 2021b COVID-19 Practitioner Survey. Retrieved from https://www.apa.org/pubs/reports/practitioner/covid-19-2021b. Accessed 10 Apr 2022
- Arora T, Grey I, Östlundh L, Lam KBH, Omar OM, Arnone D. The prevalence of psychological consequences of COVID-19: a systematic review and meta-analysis of observational studies. J Health Psychol. 2022;27(4):805–824. doi: 10.1177/1359105320966639. [DOI] [PubMed] [Google Scholar]
- Basu A, Kim HH, Basaldua R, Choi KW, Charron L, Kelsall N, …, Koenen KC (2021) A cross-national study of factors associated with women’s perinatal mental health and wellbeing during the COVID-19 pandemic. PLoS ONE 16(4):e0249780. 10.1371/journal.pone.0249780 [DOI] [PMC free article] [PubMed]
- Boyd RC, Le HN, Somberg R. Review of screening instruments for postpartum depression. Archives of Women’s Mental Health. 2005;8(3):141–153. doi: 10.1007/s00737-005-0096-6. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2022a) COVID-19 vaccinations in the United States, County. Retrieved March 2, 2022a, from https://data.cdc.gov/Vaccinations/COVID-19-Vaccinations-in-the-United-States-County/8xkx-amqh
- Centers for Disease Control and Prevention (2022b) COVID data tracker. Retrieved March 25, 2022b, from https://covid.cdc.gov/covid-data-tracker
- Chen Q, Li W, Xiong J, Zheng X. Prevalence and risk factors associated with postpartum depression during the COVID-19 pandemic: a literature review and meta-analysis. Int J Environ Res Public Health. 2022;19(4):2219. doi: 10.3390/ijerph19042219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S, Williamson G. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, editors. The social psychology of health. Newbury Park: Sage; 1988. [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385. doi: 10.2307/2136404. [DOI] [PubMed] [Google Scholar]
- COVID-Minds Network (2021) Global mental health in the COVID-19 pandemic. Retrieved March 25, 2022, from https://www.covidminds.org/
- Cox J, Holden J, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh postnatal depression scale. Br J Psychiatry. 1987;150:782–786. doi: 10.1007/978-94-007-1694-0_2. [DOI] [PubMed] [Google Scholar]
- Dickerson J, Kelly B, Lockyer B, Bridges S, Cartwright C, Willan K, Shire K, Crossley K, Bryant M, Siddiqi N, Sheldon TA, Lawlor DA, Wright J, McEachan RRC, Pickett KE, on behalf of the Bradford Institute for Health Research COVID-19 Scientific Advisory Group (2022) ‘When will this end? Will it end?’ The impact of the March-June 2020 UK COVID-19 lockdown response on mental health: a longitudinal survey of mothers in the Born in Bradford study. BMJ Open 12:e047748. 10.1136/bmjopen-2020-047748 [DOI] [PMC free article] [PubMed]
- Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S (2020) Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Network Open 3(9):e2019686. 10.1001/jamanetworkopen.2020.19686 [DOI] [PMC free article] [PubMed]
- Frank E, Zhao Z, Fang Y, Rotenstein LS, Sen S, Guille C. Experiences of work-family conflict and mental health symptoms by gender among physician parents during the COVID-19 pandemic. JAMA Netw Open. 2021;4(11):1–12. doi: 10.1001/jamanetworkopen.2021.34315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goyal D, Beck CT, Webb R, Ayers S (2022) Postpartum depressive symptoms and experiences during COVID-19. MCN Am J Matern Child Nurs 47(2):77–84. 10.1097/nmc.0000000000000802 [DOI] [PMC free article] [PubMed]
- Guintivano J, Krohn H, Lewis C, Byrne EM, Henders AK, Ploner A, …, Meltzer-Brody S (2018) PPD ACT: an app-based genetic study of postpartum depression. Transl Psychiatry 8(1):260. 10.1038/s41398-018-0305-5 [DOI] [PMC free article] [PubMed]
- Guo J, De Carli P, Lodder P, Bakermans-Kranenburg MJ, Riem MME (2021) Maternal mental health during the COVID-19 lockdown in China, Italy, and the Netherlands: a cross-validation study. Psychol Med 1–11. 10.1017/S0033291720005504 [DOI] [PMC free article] [PubMed]
- Hermann A, Fitelson EM, Bergink V. Meeting maternal mental health needs during the COVID-19 pandemic. JAMA Psychiat. 2021;78(2):123. doi: 10.1001/jamapsychiatry.2020.1947. [DOI] [PubMed] [Google Scholar]
- Hewitt CE, Gilbody SM (2009) Is it clinically and cost effective to screen for postnatal depression: a systematic review of controlled clinical trials and economic evidence. BJOG Int J Obstet Gynaecol 116(8):1019–1027. 10.1111/j.1471-0528.2009.02148.x [DOI] [PubMed]
- Hewitt CE, Gilbody SM, Brealey S, Paulden M, Palmer S, Mann R, Green J, Morrell J, Barkham M, Light K, Richards D (2009) Methods to identify postnatal depression in primary care: an integrated evidence synthesis and value of information analysis. Health Technol Assess 13(36). 10.3310/hta13360 [DOI] [PubMed]
- Kessler RC, Chiu WT, Hwang IH, Puac-Polanco V, Sampson NA, Ziobrowski HN, Zaslavsky AM. Changes in prevalence of mental illness among US adults during compared with before the COVID-19 pandemic. Psychiatr Clin North Am. 2022;45(1):1–28. doi: 10.1016/j.psc.2021.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann. 2002;32(9):509–515. doi: 10.3928/0048-5713-20020901-06. [DOI] [Google Scholar]
- Ladekarl M, Olsen NJ, Winckler K, Brødsgaard A, Nøhr EA, Heitmann BL, Specht IO (2021) Early postpartum stress, anxiety, depression, and resilience development among Danish first-time mothers before and during first-wave COVID-19 pandemic. Int J Environ Res Public Health 18(22):11734. 10.3390/ijerph182211734 [DOI] [PMC free article] [PubMed]
- Lanza ST, Vasilenko SA, Russell MA. Time-varying effect modeling to address new questions in behavioral research: examples in marijuana use. Psychology of Addictive Behaviors : Journal of the Society of Psychologists in Addictive Behaviors. 2016;30(8):939. doi: 10.1037/ADB0000208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little RJA. A test of missing completely at random for multivariate data with missing values. J Am Stat Assoc. 1988;83(404):1198–1202. doi: 10.1080/01621459.1988.10478722. [DOI] [Google Scholar]
- MCGoron L, Aikins JW, Trentacosta CJ, Gomez JM, Beeghly M. School support, chaos, routines, and parents’ mental health during COVID-19 remote schooling. School Psychology. 2021;37(2):173–182. doi: 10.1037/spq0000467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer-Brody S, Boschloo L, Jones I, Sullivan PF, Penninx BW. The EPDS-Lifetime: assessment of lifetime prevalence and risk factors for perinatal depression in a large cohort of depressed women. Arch Women’s Ment Health. 2013;16(6):465–473. doi: 10.1038/jid.2014.371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Overbeck G, Rasmussen IS, Siersma V, Kragstrup J, Ertmann RK, Wilson P. Mental well-being during stages of COVID-19 lockdown among pregnant women and new mothers. BMC Pregnancy Childbirth. 2022;22(1):1–7. doi: 10.1186/s12884-021-04374-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puyané M, Subirà S, Torres A, Roca A, Garcia-Esteve L, Gelabert E. Personality traits as a risk factor for postpartum depression: a systematic review and meta-analysis. J Affect Disord. 2022;298:577–589. doi: 10.1016/j.jad.2021.11.010. [DOI] [PubMed] [Google Scholar]
- Racine N, Eirich R, Cooke J, Zhu J, Pador P, Dunnewold N, Madigan S. When the bough breaks: a systematic review and meta-analysis of mental health symptoms in mothers of young children during the COVID-19 pandemic. Infant Ment Health J. 2022;43(1):36–54. doi: 10.1002/imhj.21959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roxby P (2020, May 16). Psychiatrists fear “tsunami” of mental illness after lockdown. BBC News. https://www.bbc.com/news/health-52676981
- Saleem S, Burns S, Falenchuk O, Varmuza P, Perlman M. Heterogeneity in maternal and child mental health responses to the COVID-19 pandemic. Early Child Res Q. 2022;59(January):203–214. doi: 10.1016/j.ecresq.2021.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Santomauro DF, Mantilla Herrera AM, Shadid J, Zheng P, Ashbaugh C, Pigott DM, …, Ferrari AJ (2021) Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the COVID-19 pandemic. The Lancet 398(10312):1700–1712. 10.1016/S0140-6736(21)02143-7 [DOI] [PMC free article] [PubMed]
- Shevlin M, Butter S, McBride O, Murphy J, Gibson-Miller J, Hartman TK, Levita L, Mason L, Martinez AP, McKay R, Stocks TVA, Bennett KM, Hyland P, Vallieres F, Bentall RP (2021a) Psychological responses to the COVID-19 pandemic are heterogeneous but have stabilised over time: 1 year longitudinal follow-up of the COVID-19 Psychological Research Consortium (C19PRC) study. Psychol Med 1–3. 10.1017/S0033291721004025 [DOI] [PMC free article] [PubMed]
- Shevlin M, Butter S, McBride O, Murphy J, Gibson-Miller J, Hartman TK, Levita L, Mason L, Martinez AP, McKay R, Stocks TVA, Bennett K, Hyland P, Bentall RP (2021b) Refuting the myth of a ‘tsunami’ of mental ill-health in populations affected by COVID-19: evidence that response to the pandemic is heterogeneous, not homogeneous. Psychol Med 1–9. 10.1017/S0033291721001665 [DOI] [PMC free article] [PubMed]
- Simpson W, Glazer M, Michalski N, Steiner M, Frey BN. Comparative efficacy of the generalized anxiety disorder 7-item scale and the Edinburgh Postnatal Depression Scale as screening tools for generalized anxiety disorder in pregnancy and the postpartum period. Can J Psychiat. 2014;59(8):434–440. doi: 10.1177/070674371405900806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sommerlad A, Marston L, Huntley J, Livingston G, Lewis G, Steptoe A, Fancourt D (2021) Social relationships and depression during the COVID-19 lockdown: longitudinal analysis of the COVID-19 Social Study. Psychol Med 1–10. 10.1017/S0033291721000039 [DOI] [PMC free article] [PubMed]
- Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- Tan X, Shiyko MP, Li R, Li Y, Dierker L. A time-varying effect model for intensive longitudinal data. Psychol Methods. 2012;17(1):61–77. doi: 10.1037/a0025814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The New York Times (2021) Coronavirus (Covid-19) data in the United States. Retrieved March 2, 2022, from https://github.com/nytimes/covid-19-data
- Unnarsdóttir AB, Lovik A, Fawns-Ritchie C, Ask H, Kõiv K, Hagen K, Didriksen M, Christoffersen LAN, Garòarsson AB, McIntosh A, Kähler AK, Campbell A, Hauksdóttir A, Krikstrup C, Mikkelsen DH, Altschul D, Thordardottir EB, Frans EM, Kvale G, Tómasson G, Kariis HM, Jónsdóttir HL, Rúnarsdóttir H, Magnúsdóttir I, Eid J, Jakobsdóttir J, Nielsen KR, Kaspersen KA, Milani L, Trogstad LS, Yi L, Bruun MT, Sullivan PF, Magnus PM, Shen Q, Nesvåg R, Brandlistuen RE, Mägi R, Ostrowski SR. Løkhammer S, Solem S, Reichborn-Kjennerud T, Hansen TF, Werge T, Aspelund T, Porteous DJ, Fang F, Lehto K, Andreassen OA, Pedersen OBV, Le Hellard S, Valdimarsdóttir UA (2021) Cohort profile: COVIDMENT: COVID-19 cohorts on mental health across six nations. Int J Epidemiol 51(3):e108–e122. 10.1093/ije/dyab234 [DOI] [PMC free article] [PubMed]
- US Census Bureau (2010) Census regions and divisions of the United States. Retrieved March 31, 2022, from https://www.census.gov/geographies/nce-maps/2010/geo/2010-census-regions-and-divisions-of-the-united-states.html
- US Department of Housing and Urban Development (2010) HUD USPS zip code crosswalk files. Retrieved March 30, 2022, from https://www.huduser.gov/portal/datasets/usps_crosswalk.html
- Van Lieshout RJ, Layton H, Savoy CD, Brown JSL, Ferro MA, Streiner DL, …, Hanna S (2021) Effect of online 1-day cognitive behavioral therapy-based workshops plus usual care vs usual care alone for postpartum depression: a randomized clinical trial. JAMA Psychiat 78(11):1200–1207. 10.1001/jamapsychiatry.2021.2488 [DOI] [PMC free article] [PubMed]
- Verdery AM, Smith-Greenaway E, Margolis R, Daw J. Tracking the reach of COVID-19 kin loss with a bereavement multiplier applied to the United States. Proc Natl Acad Sci USA. 2020;117(30):17695–17701. doi: 10.1073/pnas.2007476117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisner KL, Parry BL, Piontek CM. Postpartum depression. N Engl J Med. 2002;347(3):194–199. doi: 10.1056/NEJMcp011542. [DOI] [PubMed] [Google Scholar]
- Wu P, Fang Y, Guan Z, Fan B, Kong J, Yao Z, …, Hoven CW (2009) The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiat 54(5):302–311. 10.1177/070674370905400504 [DOI] [PMC free article] [PubMed]
- Zhang CXW, Okeke JC, Levitan RD, Murphy KE, Foshay K, Lye SJ, Matthews SG (2022) Evaluating depression and anxiety throughout pregnancy and postpartum: impact of the COVID-19 pandemic. Am J Obstet Gynecol MFM 4(3):100605. 10.1016/j.ajogmf.2022.100605 [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.