Abstract
Purpose
Rapidly progressive osteoarthritis of the hip is an uncommon and poorly understood condition. No universal definition of RPOH exists, however, a loss of joint space of 2 mm or more per year or 50% or more in one year with no other cause can be classed as RPOH. Due to the rapid loss of joint space and associated bone loss, total hip arthroplasty is the only viable treatment option. The aim of this systematic review is to assess the outcomes of THA in RPOH.
Methods
A systematic search of Embase, Medline and CINAHL databases was performed for studies reporting on the outcomes of patients with RPOH as their primary diagnosis for undergoing THA. Patient demographics, surgical techniques, implant selection, blood loss, morbidity and mortality, length of stay and patient-reported outcomes were amongst the data collected.
Results
Eight studies were found to be eligible, reporting on the outcomes of 270 patients with a mean age of 71. The majority of patients (88.1%) were female and the mean Body Mass Index was 27.6 kg/m2. Six of the eight studies reported on the need for additional reconstructive devices and procedures including the use of acetabular roof augmentation, acetabular reinforcement devices and revision acetabular components. Two studies reported increased blood loss in RPOH patients compared with non-RPOH patients (945 ml vs. 578 ml and 473.9 g vs. 353.9 g, respectively).
Conclusion
RPOH leads to significant pre-operative morbidity and THA for RPOH has been shown to result in greater blood loss, prolonged operative time and increased complexity of the procedure all of which result in increased cost. There is a paucity of data on the long-term outcomes for these patients and more well-constructed studies are therefore required.
Keywords: Rapidly progressive osteoarthritis of the hip, Total hip arthroplasty, Acetabular reconstruction, PROMS, RPOH
Introduction
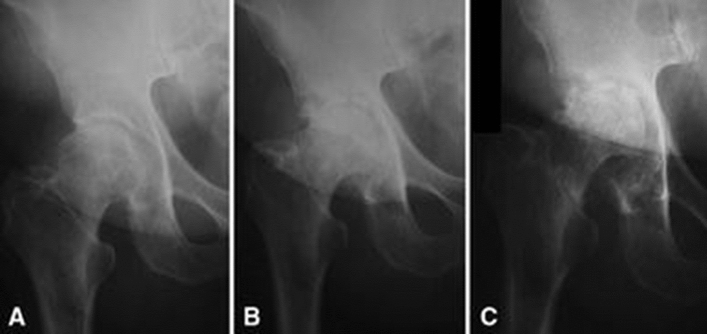
Rapidly progressive osteoarthritis of the hip (RPOH) is an uncommon condition first described by Forestier in 1957 [1]. Whilst no standard definition for RPOH exists, the loss of joint space at a rate of 2 mm or greater per year, or a loss of joint space of 50% or more in one year, with no other cause for a destructive arthropathy, as proposed by Lequesne, has been widely adopted [2]. Clinically, RPOH presents as rapidly worsening severe hip pain due to the destruction of the femoral head, with or without acetabular involvement (Fig. 1). The radiographic changes associated with RPOH typically manifest within 12 months of the onset of symptoms [3–5], and the reported incidence is between 7.2 and 15.7% [4, 6].
Fig. 1.
Example of RPOH. A – Radiographs initially normal 3 months pre-presentation; B – joint space narrowing and lateral fragmentation 2 months pre-presentation; C – destruction of the femoral head and acetabulum at presentation.
Source Reproduced with permission from [8]
In light of the increasing recognition of RPOH, many studies have attempted to identify a cause despite which its aetiology remains unclear [7–9]. It has been suggested that subchondral insufficiency fractures (SIFs) contribute to the development of RPOH, although this remains unproven [9–11]. The patient is more commonly female, older than the typical osteoarthritic patient, and with unilateral disease [8, 12–14].
Total hip arthroplasty (THA) has been hailed as the operation of the century [15] and the number of primary THAs performed in 2019, the year prior to the COVID-19 pandemic, stood at 95,677 [16]. The number of THAs being performed in the United Kingdom (UK) was predicted to rise year on year [17], but, as a result of the COVID-19 pandemic, all non-urgent elective surgeries were initially suspended [18] and the number of primary THA performed in 2020 fell by 43% to 54,858 [19]. Despite many centres resuming elective services, the waiting list for elective orthopaedic surgery is estimated to continue rising with 1.4 million patients waiting as of November 2020 [20]. This poses a significant problem as pre-pandemic, patients waiting for elective hip replacement often experienced a health state worse than death [21] and this number has only increased since the pandemic [22]. At current estimates, expanding the provision of THA by 5% compared to 2019 levels would eliminate the deficit in 10 years and a 10% expansion in 5 years [19].
Data from the national joint registry (NJR) show that the majority of patients (60%) undergoing THA are female and most are in their 70 s (37%) [16] both of which place them at risk of RPOH. THA for RPOH has been shown to lead to increased blood loss, a prolonged operative time and greater complexity of the procedure, as well as the need for adjuncts such as cages and revision implants [23–25]. Non-operative management in the hopes of delaying or avoiding THA altogether has been attempted. Intra-articular steroid injection and or weight bearing modification did not prevent the need for THA [26] with some indications that intra-articular injection may increase the risk of developing RPOH [27]. Delays to treating patients with RPOH can lead to significant bone loss, particularly acetabular, being present at the time of surgery. The outcomes following THA in bone loss are variable with survivorship ranging from 75 to 96% depending on fixation method [28–30]. However, the available literature on THA in the presence of bone loss predominantly relates to revision surgery or hip dysplasia. The purpose of this review is to assess the available literature on the patient demographics, surgical techniques and outcomes of THA in RPOH.
Methods
Search strategy and criteria
Embase, Medline and, CINAHL databases were searched for all relevant articles from inception until December 2021. The search combined the keywords “rapid” OR “rapidly” AND “progressive” OR “progressing” OR “destructive” AND “arthrosis” OR “ARTHRITIS”/ OR “OSTEOARTHRITIS”/. The searches were performed in duplicate by two authors (VA and KB) with citations of the included articles also screened for further relevant studies. All articles meeting the inclusion criteria were evaluated.
Articles were included if they featured patients with RPOH who underwent primary THA and reported on the outcomes of this, either peri-operatively or post-operatively. Articles were excluded if they contained no outcome data, cohorts other than primary THA, datasets where RPOH cohorts could not be delineated from others, biochemical or histological studies, abstracts and case reports. Study types eligible for inclusion were randomised and non-randomised controlled trials, cohort or case–control studies and case series, which we defined as five or more cases.
Any disagreements were resolved through discussion in the first instance, and where this failed, the senior author was the final arbiter.
Data collection and analysis
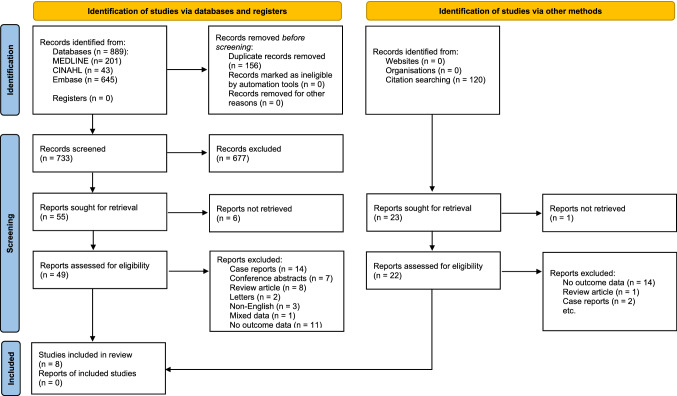
This review was performed in line with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidance [31]. Search results were reviewed using their full titles and those deemed relevant underwent a review of their abstracts. Abstracts were assessed against the inclusion and exclusion criteria and those still considered relevant had the full article reviewed. Full articles meeting inclusion criteria were included in the study (Fig. 2).
Fig. 2.
PRISMA flow chart. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 2021;372:n71. https://doi.org/10.1136/bmj.n71. For more information, visit: http://www.prisma-statement.org/
Data collected included study details, the number of patients and number of hips, as well as demographic data including sex, age and Body Mass Index (BMI). Patient-reported outcome measures (PROMs) included, Japanese Orthopaedic Association score (JOA) [32], Harris hip score (HHS) [33], Oxford hip score (OHS) [34]. Data on blood loss, transfusion requirements, length of stay, revisions and mortality were recorded. Surgical considerations such as approach, implants used, surgical time the need for bone grafting and any additional procedures required were also recorded.
Data were extracted from the papers by systematic analysis of each article and summation in Microsoft Excel for Microsoft 365 (Microsoft, Redmond, WA, USA).
Quality appraisal
The methodological index for non-randomised studies (MINORS) score [35] was used to evaluate the quality of evidence. Eight criteria were assessed with scores of between zero and two being allocated to each. A further four criteria were available for the assessment of comparative studies making the maximum score for non-comparative studies 16 and for comparative studies 24. Each study was independently evaluated by two of the authors and their independent scores were averaged for each study.
Results
Study characteristics
Following the application of inclusion and exclusion criteria, eight studies were selected [14, 23, 25, 36–40] reporting on the outcomes of 270 patients. One study was conducted prospectively [38] and two included a comparison group [14, 25].
Quality assessment
Each study was assigned a MINORS score, with an average score of 11 (9–15) (Table 1).
Table 1.
Quality assessment of studies using MINORS score
| Study | Year of publication | Study type | MINORS score |
|---|---|---|---|
| Charrois et al.a | 2001 | Retrospective | 15 |
| Karayiannis et al. | 2020 | Retrospective | 10 |
| Kawai et al. | 2009 | Retrospective | 9.5 |
| Kuo et al. | 2009 | Retrospective | 9 |
| Peters and Doets | 2009 | Prospective | 10 |
| Postel and Kerboull | 1970 | Retrospective | 9 |
| Thompson et al. | 2004 | Retrospective | 12.5 |
| Yuasa et al.a | 2016 | Retrospective | 13 |
aComparative study therefore scored out of 24
Patient characteristics
All studies included the number of patients, with seven reporting on the number of hips analysed [14, 25, 36–40]. The mean age of patients across all eight studies was 71 years (68–74). Six studies [14, 25, 36–38, 40] detailed the numbers of male and female patients and three studies [14, 23, 40] included the mean BMI 27.6 (25.8 – 29.1). Two studies [14, 38] reported on the duration of symptoms prior to THA, which averaged 15 months (Table 2).
Table 2.
Summary of patient characteristics
| Study | Patients | Hips | Male | Female | Age (range) | BMI (Kg/m2) | Duration of symptoms (months) |
|---|---|---|---|---|---|---|---|
| Charrois et al. | 100 | 100 | 14 | 86 | 71 | – | – |
| Karayiannis et al. | 49 | – | – | – | 72.7 (51–88) | 29.1 | – |
| Kawai et al. | 17 | 20 | 1 | 16 | 68.3 (60–77) | – | – |
| Kuo et al. | 8 | 10 | 1 | 7 | 70 (60–86) | - | – |
| Peters and Doets | 6 | 8 | 0 | 6 | 74.8 (64–83) | – | 21 (4–35) |
| Postel and Kerboull | 44 | 51 | – | – | 68 | – | – |
| Thompson et al. | 34 | 35 | 5 | 29 | 72 (51–88) | 28 (20–41) | – |
| Yuasa et al. | 12 | 12 | 0 | 12 | 72.3 (50–80) | 25.8 | 9 (4–11) |
| Total | 270 | 236 | 21 | 156 |
Surgical details
Approach
Six studies detailed the surgical approach used [14, 25, 36–39]. Three studies [14, 37, 39] utilised the posterolateral approach and two [25, 36] used a trans-trochanteric approach. The remaining study [38] utilised a transgluteal approach in all but two patients, where a posterior approach was used due to “substantial acetabular bone loss”.
Implants
Seven studies included detail on the implants used [14, 23, 25, 36–39]. Three studies [25, 36, 39] performed cemented THAs and one [38] performed cementless. One study [23] used solely cementless cups, with 39 cementless stems and 10 cemented stems. One study [37] used hybrid THAs for all patients bar one, where a cementless configuration was used. One study [14] used cementless stems in combination with cementless cups where little bone loss had occurred, or cemented cups where bone loss was deemed significant.
Additional procedures/changes to technique
Six studies [14, 23, 25, 36–38] reported on the need for the use of additional procedures or techniques as a result of the encountered bone loss. One study [25] reported that no additional bone reconstruction was required and another [23] used a standard technique for all procedures irrespective of bone loss.
Four studies [14, 36–38] reported the use of acetabular reconstruction or reinforcement. Kawai et al. used a reinforcement device in all patients included in their study [36]. Kuo et al. used an oblong acetabular component for two patients with superior acetabular bone loss [37]. Yuasa et al. used a Kerboull-type plate for acetabular roof reconstruction in one patient [14]. Peters and Doets report on one patient requiring ‘structural’ reconstruction but did not provide further detail [38].
Duration of surgery
Four studies [14, 23, 25, 40] reported on operative time, which averaged 91.4 min (58 – 127 min).
A summary of surgical details can be found in Table 3.
Table 3.
Summary of surgical technique
| Study | Patients | Approach | Femoral implant | Acetabular implant | Additional requirements | Surgical time (minutes) | Length of stay (days) | Complications | Revisions | Length of follow-up | Blood loss | Transfusion | PROMs |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Charrios et al. | 100 | Trans-trochanteric | Cemented | Cemented | None | 119 | - | Not recorded | Not recorded | Not recorded | 945 ml | 100 patients | Not recorded |
| Karayiannis et al. | 49 | Not recorded |
39 Uncemented 10 Cemented |
Uncemented | None | 61.7 | 5.9 (1–34) | Not recorded |
1 × early acetabular loosening and periacetabular fracture (day 10) 1 × infection (day 21) 1 × stem only revision for peri-prosthetic fracture (13.3 years) |
2.3 years (61 days – 12.9 years) | Not recorded |
19 patients (9 patients required 1 unit; 6 patients required 2 units; 2 patients required 3 units; and 2 patients required 4 units.) |
Mean pre-op OHS 7.7 (1–15) (available for 43 patients) Mean post-op OHS 36.6 (6–48) (available for 42 patients at 1 year) |
| Kawai et al. | 17 | Lateral approach with trochanteric osteotomy | Cemented | Cemented |
Kerboull-type acetabular reinforcement devices in all patients Bone grafting in all patients |
Not recorded | – | None | None | 6.3 years (3.6 – 11.8 years) | Not recorded | Not recorded |
Mean pre-op JOA hip score 38.1 (13–62) Mean post-op JOA hip score 84.6 (70–93) (post-op score at last follow-up) |
| Kuo et al. | 8 | Posterolateral |
8 Cemented 1 Uncemented |
Uncemented | 2 × oblong acetabular device | Not recorded | – | 1 loose femoral stem at 12 years | None | 6 years (4 – 12 years) | Not recorded | Not recorded |
Mean post-op HHS 85.7 (at last follow-up) |
| Peters and Doets | 6 |
6 Transgluteal 2 Posterior approach |
Uncemented | Uncemented |
Acetabular roof reconstruction in 1 patient Bone grafting in all patients Acetabular screws 7 hips Oversized cup in 6 hips |
Not recorded | – |
2 patients cystitis 1 patient post-op delirium |
None | 69 months (24 – 104 months) | Not recorded | Not recorded |
Mean pre-op HHS 25.8 Mean post-op HHS 88.3 (Post-op score at last follow-up) |
| Postel and Kerboull | 44 | Posterolateral | Cemented | Cemented | Not recorded | Not recorded | – | 4 loose acetabulum | 1 × acetabular loosening (6 weeks) | 6 months to 3 years | Not recorded | Not recorded | Not recorded |
| Thompson et al. | 34 | Not recorded | Not recorded | Not recorded | Not recorded | 58 | – | Not recorded | None | 18 months (13 – 36 months) | Not recorded |
Yes Mean transfusion requirement of 3.5 units (1—9 units) |
Mean pre-op OHS 50 (36–59) Mean post-op OHS 27 (12–41) (Post-op score at last follow-up) |
| Yuasa et al. | 12 | Posterolateral | Uncemented |
7 Uncemented 5 Cemented |
1 acetabular roof reconstruction | 127 | – | None | None | 9.3 years | 473.9 g (286 g – 780 g) | Not recorded |
Mean pre-op HHS 38.3 Mean post-op HHS 81.1 (Post-op score at last follow-up) |
PROMs – patient reported outcome measures, OHS – Oxford hip score, HHS – Harris hip score, ml – millilitres, g–grams
Post-operative outcomes
Blood loss and transfusion
Two studies reported on blood loss following surgery [14, 25]. Charrois et al. calculated blood loss in millilitres (ml) of red blood cells with the RPOH group having a mean of 945 ml [25]. Yuasa et al. calculated blood loss in grams (g) with a mean in the RPOH group of 473.9 g [14].
Three studies reported on transfusion requirement [23, 25, 40]. Karayiannis et al. reported on 19 patients with a mean transfusion requirement of 1.8 units (1–4 units) [23]. Charrois et al. reported all 100 patients required transfusions but did not specify the amount [25]. Thompson et al. reported a mean transfusion requirement of 3.5 units (1–9 units) [40].
Mortality and revision
Two studies reported on deaths during their respective study periods [23, 37]. Kuo et al. reported two deaths at a mean of 7.5 years post-operatively [37]. Karayiannis et al. reported on 11 deaths at a mean of 7.7 years [23]. Seven studies reported on revisions during the study periods [14, 23, 36–40]. Amongst the studies, five [14, 36–38, 40] reported no revisions at a mean follow-up of 69.2 months (18–111.6 months). Karayiannis et al. reported on three revisions at a mean follow-up of 2.3 years [23]. One revision was for early cup loosening, one for a periacetabular fracture following a fall and one had a washout and liner exchange due to infection. Postel and Kerboull reported on 1 revision at 6 weeks for acetabular loosening [39] (Table 3).
PROMs
Three studies reported on the HHS [14, 34, 35]. Two of these studies [14, 38] reported on both the pre-operative and post-operative scores, increasing from an average of 32.1 to an average of 84.7. Kuo et al. reported only the post-operative which averaged 85.7 [37].
Two studies [23, 40] reported on the OHS with scores increasing from an average of 8.85 pre-operatively to 34.8 post-operatively.
One study [36] reported on the JOA score, which increased from 38.1 to 84.6 post-operatively.
Length of stay
Only one study reported on post-operative duration of hospital stay [23], which averaged 5.9 days with a range of 1–34 days.
A summary of post-operative outcomes can be found in Table 3.
Discussion
RPOH remains a poorly understood entity despite first being described in 1957 [1]. Whilst the aetiology is unclear, RPOH primarily affects female patients, with unilateral disease at an average age greater than those undergoing THA for osteoarthritis or other pathologies [12, 13]. The NJR suggests that the demographics of the patients undergoing THA in the UK make them more likely to be affected by RPOH, i.e., females in their 70 s [16], which is further compounded by lengthening waiting lists, given that the time from the onset of symptoms to bony destruction can be as little as 12 months [8, 12, 13]. Given the increasing elective waiting lists for THA and the potential increase in patients developing RPOH whilst on them, the paucity of data on the outcomes following THA for RPOH needs to be addressed. This review has found that patients undergoing THA for RPOH are of greater complexity, often require adjunctive procedures due to bone loss and therefore greater operative time, lose a greater amount of blood requiring transfusion, and may be at greater risk of early revision.
Due to the nature of the disease, RPOH can present additional complexities due to the degree of bone loss and the need to perform complex reconstructions, which can directly impact operative time and blood loss. Kawai et al. used Kerboull acetabular reinforcement devices and bone grafting in all cases [36], but did not comment specifically on the operative time. Two other studies [14, 38] reported on the need for acetabular roof reconstruction with a further study [37] reporting the use of an acetabular component usually reserved for revision THA. Despite the clear surgical complexity of many patients with RPOH and the need for procedures that reflect this, one study used a standard technique and implants regardless of bone loss [23] reporting three revisions, one of which one was secondary to trauma.
Another factor shown to result in poorer outcomes following THA is the duration of surgery. Several studies have shown an increase in both minor and major complications with increasing operative time [41–43]. Four studies [14, 23, 25, 40] included in this review reported on the duration of surgery. Charrois et al. and Yuasa et al. compared the duration of surgery between patients with RPOH and those without, concluding that there was no statistically significant difference [14, 25]. Conversely, Karayiannis et al. reported that there was a significant difference in the duration of surgery between RPOH and non-RPOH groups (61.7 vs. 57.7 min p = 0.01) [23], and although Charrois et al. reported an increased duration of surgery, this was not statistically significant (127.9 vs. 110.6 min (p = 0.268) [25].
One of the most immediately obvious features of THA in patients with RPOH is the increase in blood loss compared to THA for other indications. Charrois et al. compared the blood loss in patients undergoing THA for RPOH with those undergoing THA for other indications, reporting significantly higher loss in the RPOH group (945 vs. 578 ml p < 0.001) [25], with similar findings reported by Yuasa et al. with a mean blood loss of 473.9 vs. 353.9 g, although this did not reach statistical significance [14]. For comparison, 1 g of blood is equivalent to 1 ml of blood [44]. Possible explanations for the increased blood loss in RPOH are the presence of increased amounts of vascularised synovial tissue which are more prone to bleeding [4, 9] in conjunction with increased operative time.
Blood transfusion following THA has been demonstrated to increase adverse outcomes including death, pneumonia and infection [45, 46]. In the study by Charrois et al., all 100 patients in the RPOH group required blood transfusion compared with 84 of 100 in the non-RPOH group [25]. Studies by Karayianis et al. and Thompson et al. also reported on transfusion requirements in RPOH patients but did not have a non-RPOH group for comparison. Karayiannis et al. reported transfusion requirements ranging from 1 to 4 units [23], whilst Thompson et al. reported on transfusion requirements ranging from 1 to 9 units [40].
Amongst the studies included in this review, all reported on revisions with the exception of Charrois et al. [25]. Five of the studies [14, 36–38, 40] reported no revisions, at an average follow-up of 5.7 years (1.5–9.3 years). Karayiannis et al. reported on three revisions two of which were acetabular revisions and occurred within 21 days. The other revision was a stem only revision for aseptic loosening at 13.3 years [23]. Postel et al. reported one revision for acetabular failure within 6 weeks of operation [39]. The number of revisions reported, most of which occurred early, is relatively small and this may provide a false sense of reassurance on the outcomes following THA for RPOH. The heterogeneous nature of the data, with small numbers of patients, limited duration of follow-up and non-standardised reporting means that it is difficult to draw any conclusions.
Six studies [14, 23, 36–38, 40] looked at PROMs including the JOA, HHS and OHS. Kawai et al. reported on pre- and post-operative JOA score with the mean score increasing from 38.1 to 84.6 at final follow-up (mean follow-up 6.3 years) [36]. Three studies [14, 37, 38] reported on the HHS, however, only two of these included both pre- and post-operative scores [14, 38]. The two studies reported an increase in HHS from 32.1 pre-operatively to 81.1 post-operatively at an average follow-up of 7.5 years. Karayiannis et al. reported on the OHS pre-operatively and at one year post-operatively with an increase from an average of 7.7–36.6 [23]. This study reported that following THA for RPOH, PROMS increased in the short and medium terms, but there were no long-term studies available.
This review does have some limitations which make its interpretation difficult. The total number of patients from the studies is small at 270, reflecting the paucity of data on RPOH and highlighting the need for further studies on this pathology. The limited follow-up period in the studies meant that any potential conclusions could only be applied in the short to mid-term. This reinforces the need for further well-constructed long-term studies, with standardised reporting into the outcome of THA for RPOH. Because of the heterogeneity of the data and the relatively small numbers, meaningful statistical analysis was not possible. Despite these limitations, the included studies were of generally good quality and the majority had low rates of attrition in the data presented.
Conclusion
As patients languish on ever lengthening waiting lists, the population at risk of developing RPOH is increasing, with the typical patient being female, having unilateral disease and being typically older than those undergoing THA for other pathologies. RPOH is a disease which causes a rapid worsening of symptoms and significant morbidity and results in increased complexity of THA. This has been reported to result in greater blood loss, increased transfusion requirements, longer duration of surgery and the need for further procedures, particularly acetabular reconstruction. The literature on the results of THA for RPOH remains lacking and in order to establish the results, well-constructed long-term studies of larger patient numbers with standardised reporting of surgical techniques and complications are required.
Funding
The authors declare that no funding was received for this manuscript.
Declarations
Conflicts of interest
The authors declare no conflicts of interests.
Availability of data and material
Data and material available on request.
Code availability
Not applicable.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Forestier F (1957) Coxite rhumatismales subaigues et chroniques. Thesis
- 2.Lequesne M. Coxarthrose destructive rapide. Rev Rhum. 1970;37:721–733. [PubMed] [Google Scholar]
- 3.Abe H, Sakai T, Ando W, et al. Synovial joint fluid cytokine levels in hip disease. Rheumatol (United Kingdom) 2014;53:165–172. doi: 10.1093/rheumatology/ket334. [DOI] [PubMed] [Google Scholar]
- 4.Batra S, Batra M, McMurtrie A, Sinha AK. Rapidly destructive osteoarthritis of the hip joint: a case series. J Orthop Surg Res. 2008;3:1–6. doi: 10.1186/1749-799X-3-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nelson FRT, Bhandarkar VS, Woods TA. Using hip measures to avoid misdiagnosing early rapid onset osteoarthritis for osteonecrosis. J Arthroplast. 2014;29:1243–1247. doi: 10.1016/j.arth.2013.11.010. [DOI] [PubMed] [Google Scholar]
- 6.Boutin RD, Pai J, Meehan JP, et al. Rapidly progressive idiopathic arthritis of the hip: incidence and risk factors in a controlled cohort study of 1471 patients after intra-articular corticosteroid injection. Skelet Radiol. 2021;50:2449–2457. doi: 10.1007/s00256-021-03815-7. [DOI] [PubMed] [Google Scholar]
- 7.Okano K, Aoyagi K, Enomoto H, et al. Bone mineral density in patients with destructive arthrosis of the hip joint. J Bone Miner Metab. 2014;32:312–316. doi: 10.1007/s00774-013-0501-6. [DOI] [PubMed] [Google Scholar]
- 8.Mavrogenis AF, Flevas DA, Panagopoulos GN, et al. Rapid destructive arthritis of the hip revisited. Eur J Orthop Surg Traumatol. 2015;25:1115–1120. doi: 10.1007/s00590-015-1676-4. [DOI] [PubMed] [Google Scholar]
- 9.Zazgyva A, Gurzu S, Gergely I, et al. Clinico-radiological diagnosis and grading of rapidly progressive osteoarthritis of the hip. Med (United States) 2017;96:1–7. doi: 10.1097/MD.0000000000006395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flemming DJ, Gustas-French CN. Rapidly progressive osteoarthritis: a review of the clinical and radiologic presentation. Curr Rheumatol Rep. 2017 doi: 10.1007/s11926-017-0665-5. [DOI] [PubMed] [Google Scholar]
- 11.Porrino J, Carlson B, Kani KK, et al. Disappearing acts: the many causes of rapidly destructive arthritis. Curr Probl Diagn Radiol. 2017;46:63–73. doi: 10.1067/j.cpradiol.2016.02.012. [DOI] [PubMed] [Google Scholar]
- 12.Irwin LR, Gopalakrishnan RN, Chattopadhyay S, Roberts JA. Rapidly progressive osteoarthrosis of the hip. Curr Orthop. 1997;11:36–39. doi: 10.1016/S0268-0890(97)90049-9. [DOI] [Google Scholar]
- 13.Pivec R, Johnson AJ, Harwin SF, Mont MA. Differentiation, diagnosis, and treatment of osteoarthritis, osteonecrosis, and rapidly progressive osteoarthritis. Orthopedics. 2013;36:118–125. doi: 10.3928/01477447-20130122-04. [DOI] [PubMed] [Google Scholar]
- 14.Yuasa T, Maezawa K, Nozawa M, Kaneko K. Midterm outcome of total hip arthroplasty for rapidly destructive coxarthrosis. J Orthop Surg. 2016;24:27–30. doi: 10.1177/230949901602400108. [DOI] [PubMed] [Google Scholar]
- 15.Learmonth ID, Young C, Rorabeck C. The operation of the century: total hip replacement. Lancet. 2007;370:1508–1519. doi: 10.1016/S0140-6736(07)60457-7. [DOI] [PubMed] [Google Scholar]
- 16.Registry NJ (2020) National joint registry - 17th annual report. Natl Jt Regist [PubMed]
- 17.Culliford D, Maskell J, Judge A, et al. Future projections of total hip and knee arthroplasty in the UK: results from the UK clinical practice research datalink. Osteoarthr Cartil. 2015;23:594–600. doi: 10.1016/j.joca.2014.12.022. [DOI] [PubMed] [Google Scholar]
- 18.Iacobucci G. Covid-19: all non-urgent elective surgery is suspended for at least three months in England. BMJ Br Med J. 2020;368:m11106. doi: 10.1136/bmj.m1106. [DOI] [PubMed] [Google Scholar]
- 19.National Joint Registry for England Wales Northern Ireland and the Isle of Man (2021) NJR 18th annual report. Natl Jt Regist
- 20.Oussedik S, MacIntyre S, Gray J, et al. Elective orthopaedic cancellations due to the COVID-19 pandemic: where are we now, and where are we heading? Bone Jt Open. 2021;2:103–110. doi: 10.1302/2633-1462.22.bjo-2020-0161.r1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Scott CEH, MacDonald DJ, Howie CR. ‘Worse than death’ and waiting for a joint arthroplasty. Bone Jt J. 2019;101(B8):941–950. doi: 10.1302/0301-620X.101B8.BJJ-2019-0116.R1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Clement ND, Scott CEH, Murray JRD, et al. The number of patients “worse than death” while waiting for a hip or knee arthroplasty has nearly doubled during the COVID-19 pandemic: a UK nationwide survey. Bone Joint J. 2021;103:672–680. doi: 10.1302/0301-620X.103B.BJJ-2021-0104.R1. [DOI] [PubMed] [Google Scholar]
- 23.Karayiannis P, Walls A, Cassidy R, Beverland D. Rapidly progressive osteoarthritis and acetabular bone loss outcomes for patients undergoing primary total hip replacement. Arthroplast Today. 2020;6:289–295. doi: 10.1016/j.artd.2020.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hess SR, O’Connell RS, Bednarz CP, et al. Association of rapidly destructive osteoarthritis of the hip with intra-articular steroid injections. Arthroplast Today. 2018;4:205–209. doi: 10.1016/j.artd.2017.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Charrois O, Kahwaji A, Vastel L, et al. Blood loss in total hip arthroplasty for rapidly destructive coxarthrosis. Int Orthop. 2001;25:22–24. doi: 10.1007/s002640000210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Villoutreix C, Pham T, Tubach F, et al. Intraarticular glucocorticoid injections in rapidly destructive hip osteoarthritis. Jt Bone Spine. 2006;73:66–71. doi: 10.1016/j.jbspin.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 27.Okike K, King RK, Merchant JC, et al. Rapidly Destructive Hip Disease Following Intra-Articular Corticosteroid Injection of the Hip. J Bone Jt Surg. 2021;103(22):2070–2079. doi: 10.2106/JBJS.20.02155. [DOI] [PubMed] [Google Scholar]
- 28.Sheth NP, Nelson CL, Paprosky WG. Femoral bone loss in revision total hip arthroplasty: evaluation and management. J Am Acad Orthop Surg. 2013;21:601–612. doi: 10.5435/JAAOS-21-10-601. [DOI] [PubMed] [Google Scholar]
- 29.Fröschen FS, Randau TM, Hischebeth GTR, et al. Mid-term results after revision total hip arthroplasty with custom-made acetabular implants in patients with paprosky III acetabular bone loss. Arch Orthop Trauma Surg. 2020;140:263–273. doi: 10.1007/s00402-019-03318-0. [DOI] [PubMed] [Google Scholar]
- 30.Kamada T, Imai H, Mahima N, et al. Acetabular reconstruction with the Kerboull-type plate at mid-term follow-up: survivorship analysis and prognostic factors for loosening. Eur J Orthop Surg Traumatol. 2018;28:485–491. doi: 10.1007/s00590-017-2060-3. [DOI] [PubMed] [Google Scholar]
- 31.Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Imura S. The japanese orthopaedic association: evaluation chart of hip joint functions. J Jpn Orthop Assoc. 1995;69:864–867. [Google Scholar]
- 33.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty: an end-result study using a new method of result evaluation. J Bone Jt Surg. 1969;51:13–17. doi: 10.2106/00004623-196951040-00012. [DOI] [PubMed] [Google Scholar]
- 34.Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br. 1996;78(B2):185–190. doi: 10.1302/0301-620X.78B2.0780185. [DOI] [PubMed] [Google Scholar]
- 35.Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 36.Kawai T, Tanaka C, Ikenaga M, et al. Total hip arthroplasty using kerboull-type acetabular reinforcement device for rapidly destructive coxarthrosis. J Arthroplast. 2010;25:432–436. doi: 10.1016/j.arth.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 37.Kuo A, Ezzet KA, Patil S, Colwell CW. Total hip arthroplasty in rapidly destructive osteoarthritis of the hip: a case series. HSS J. 2009;5:117–119. doi: 10.1007/s11420-009-9112-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Peters KS, Doets HC. Midterm results of cementless total hip replacement in rapidly destructive arthropathy and a review of the literature. HIP Int. 2009;19:352–358. doi: 10.1177/112070000901900409. [DOI] [PubMed] [Google Scholar]
- 39.Postel M, Kerboull M. 15 Total prosthetic replacement in rapidly destructive arthrosis of the hip joint. Clin Orthop Relat Res. 1970;72:138–144. [PubMed] [Google Scholar]
- 40.Thompson NW, Corr AM, Geddis CJ, et al. Rapidly progressive osteoarthrosis of the hip. HIP Int. 2004;14:217–222. doi: 10.5301/HIP.2008.1372. [DOI] [PubMed] [Google Scholar]
- 41.Nowak LL, Schemitsch EH. Duration of surgery affects the risk of complications following total hip arthroplasty. Bone Jt J. 2019;101(B6):51–56. doi: 10.1302/0301-620X.101B6.BJJ-2018-1400.R1. [DOI] [PubMed] [Google Scholar]
- 42.Wills BW, Sheppard ED, Smith WR, et al. Impact of operative time on early joint infection and deep vein thrombosis in primary total hip arthroplasty. Orthop Traumatol Surg Res. 2018;104:445–448. doi: 10.1016/j.otsr.2018.02.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Bohl DD, Ondeck NT, Darrith B, et al. Impact of operative time on adverse events following primary total joint arthroplasty. J Arthroplast. 2018;33:2256–2262.e4. doi: 10.1016/j.arth.2018.02.037. [DOI] [PubMed] [Google Scholar]
- 44.Vitello DJ, Ripper RM, Fettiplace MR, et al. Blood density is nearly equal to water density: a validation study of the gravimetric method of measuring intraoperative blood loss. J Vet Med. 2015;2015:1–4. doi: 10.1155/2015/152730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pedersen AB, Mehnert F, Overgaard S, Johnsen SP. Allogeneic blood transfusion and prognosis following total hip replacement: a population-based follow up study. BMC Musculoskelet Disord. 2009;10:1–13. doi: 10.1186/1471-2474-10-167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kim JL, Park JH, Han SB, et al. Allogeneic blood transfusion is a significant risk factor for surgical-site infection following total hip and knee arthroplasty: a meta-analysis. J Arthroplast. 2017;32:320–325. doi: 10.1016/j.arth.2016.08.026. [DOI] [PubMed] [Google Scholar]