Abstract
With the increasing incidence and prevalence of end-stage liver disease, demand for donor grafts continues to increase. Approaches on maximizing the potential donor grafts vary depending on the region. This review aims to summarize the current practice of liver transplantation with an emphasis on challenges encountered in developing countries.
Keywords: Deceased-donor liver transplantation, end-stage liver disease, living-donor liver transplantation
Introduction
Liver transplantation (LT) is an established and only definitive treatment for end-stage liver disease (ESLD). With the increasing incidence and prevalence of ESLD, demand for donor liver grafts continues to increase, making the liver a scarce resource.[1,2] Despite the exponential increase in patients requiring liver, available organ donors have increased minimally.[1] Challenges arise when there is a shortage of suitable donor organs to supply the patients requiring the LT. Deceased-donor liver transplantation (DDLT) is the ideal and preferred method for LT. However, with the scarcity of deceased-donor organs to meet the need of patients, several solutions were developed to expand the donor pool and to maximize the utilization of liver allografts, such as using extended criteria donor grafts, split LT, donation after cardiac death (also known as non-heart beating donors), auxiliary transplants, domino LT, and living-donor liver transplantation (LDLT).[2–6]
From the first successful LT performed in 1967 to the late 1980s, only deceased-donor grafts were used.[2] However, as deceased organs from pediatric donors are rarely available, and liver size mismatch from deceased adult donors leads to longer waiting-list times, a reduced-size technique was developed by Bismuth et al. to increase the donor pool for pediatric patients.[5,7] Later, Pichlmayr et al.[8] developed a split technique using a deceased donor liver graft to use it for two pediatric patients. Even these approaches, which were aimed to widen and expand the deceased liver donor pool, were not adequate to meet the needs of patients in need of the liver. In many countries, a deceased liver donation was not widely adopted.
Living-Donor Liver Transplantation
To increase the donor pool, LDLT was introduced by Strong et al. in 1989.[9] Although LDLT was developed initially to decrease the gap between patients waiting for the liver and the scarcity of deceased organs in Western countries, it has become the primary form of LT in most Asian countries.[2] LDLT is a sophisticated and complex surgical procedure with a substantial risk of donor morbidity and mortality.[5,10,11] Intraoperative and postoperative complication rates for living donors are reported to be between 9% and 67%, respectively, and the mortality rate is estimated to be 0.08%–0.5%.[12] In addition, complications such as hepatic artery thrombosis, biliary leaks, and strictures are more common in LDLT than in DDLT.[12] LDLT offers several advantages including shorter wait times, lower dropout rates, and lower waitlist mortality.[1,13]
LDLT rates are low in most Western countries.[14] Of all LT activities, LDLT accounts for more than 90% of the transplantations in most Asian countries, 5% in the USA, and 4.3% in Europe.[1,2,15] One reason why LDLT is not being widely adopted in Northern America and Europe is the risk of morbidity and mortality in living donors. Another reason for low LDLT rates in Western societies is the high baseline levels of deceased organ supply due to increased awareness of organ donation compared with most Asian countries.[16]
Countries performing high volumes of LDLT developed new techniques. They made innovations such as left lateral segment graft use in pediatric patients to left lobe graft use in adults, right lobe graft use in LDLT, and dual graft use to overcome the organ shortage, whereas Western countries focused on promoting deceased organ donations.[1] In addition, some centers challenge the traditional 0.8% of graft/recipient weight ratio, suggesting that 0.6% can be safely adapted with portal pressure control, increasing the LDLT donor pool.[1,17] However, this ratio alone is not solely considered when determining the suitability because ideal graft size varies between the patients and depends on multiple factors including the recipient’s status.[2] Previously, aberrant biliary duct in the donor was considered a contraindication for LDLT because of the high risk of biliary complications. Advances in surgical approaches in biliary reconstruction with the use of routine microsurgical techniques have greatly decreased the risk of biliary complications from 21% to 5%, thereby increasing the number of potential donors for LDLT.[1]
Indications of Liver Transplantation Vary by Region
Indications of LT across the globe change depending on the region. In the West, the most common indications for LT are hepatitis C virus (HCV) and alcohol-related liver disease (ALD), whereas, in the East, hepatitis B virus (HBV), HCV, and associated hepatocellular carcinoma (HCC) are the predominant cause.[2,18] Although preventive measures such as vaccination, screening and antiviral treatment for HBV, and screening and treatment for HCV decreased the burden of chronic liver disease in some parts of the world, the prevalence of nonalcoholic fatty liver disease (NAFLD) and ALD increases globally.[19] The incidence of NAFLD increases in parallel with the increasing rates of obesity.
In the USA, the most common causes of LT were HCV, HCC, and ALD previously; however, recent reports indicate that in patients without HCC, ALD and NASH became the leading etiologies for LT.[20–22] In addition, NASH is becoming the leading cause of HCC, surpassing HCV, in the USA.[21,22]
Although the prevalence of HBV is declining, HBV is still intermediate to highly endemic in Asia.[1,23,24] Countries including China, India, Nigeria, and Indonesia consist of approximately half of the HBV infections worldwide.[24] In addition, the Western Pacific region consists of 60% of the HCCs worldwide, and China, Pakistan, India, Egypt, Russia, and the USA account for more than half of all HCV infections.[24–26]
In Turkey, although HBV has been the predominant cause of LT for the past 15 years, its frequency is decreasing. However, the frequency of NASH leading to LT is increasing, with reports indicating that 20% of patients having LT had NASH as opposed to 4% in the last decade.[27] NASH is the fastest growing cause of LT in Turkey and in many countries, with increasing incidence seen as parallel to increasing obesity rates.[27]
Living-Donor Liver Transplantation in Hepatocellular Carcinoma
The approach and selection of the donors for HCC vary between the regions, largely based on the differences between the use of LDLT and DDLT.[2] LT is indicated in patients with HCC within the Milan criteria (a single lesion ≤5 cm in diameter or no more than three lesions, none exceeding 3 cm in diameter).[28] Patients within Milan criteria undergoing LT have similar 4-year survival (75%) as patients with cirrhosis without HCC.[29] The University of California San Francisco (UCSF) criteria proposed that LT can be performed in HCC cases of only solitary tumors up to 6.5 cm or ≤3 nodules with the largest less than 4.5 cm and a total <8 cm.[30] However, these criteria are designed primarily to allocate deceased organs to maximize utilization and might be too restrictive.[2] In countries with high LDLT rates, the selection of patients can be expanded to include a select group of patients outside of Milan or UCSF criteria.[1,31] One advantage of LDLT in these conditions is that it does not affect the limited deceased donor pool and offers similar overall survival between DDLT and LDLT recipients.[1,32,33] Approximately 25% of the patients with cirrhosis and HCC are removed from the waiting list with the progression of the diseases, and LDLT offers the advantage of LT to be performed in an elective setting, thereby optimizing the timing of the operation and reducing waiting time.[2,12] However, the risk of morbidity and mortality of the donor should be considered while expanding the criteria to maximize the LT and protect both donor and recipient.[2]
Practice of Liver Transplantation Differs between the Developed and Developing Countries
The country’s legal framework determines the use and transplantation of deceased organs, which differs in most Asian countries compared with Europe and the USA. The practice of LT differs between the countries, reflecting their own health care policy, health expenditure per capita, socioeconomic status, cultural norms, religious beliefs, and societal attitudes toward LT.[1,2,34,35] Figure 1 shows the LDLT and DDLT activities in select countries in 2020.
Figure 1.
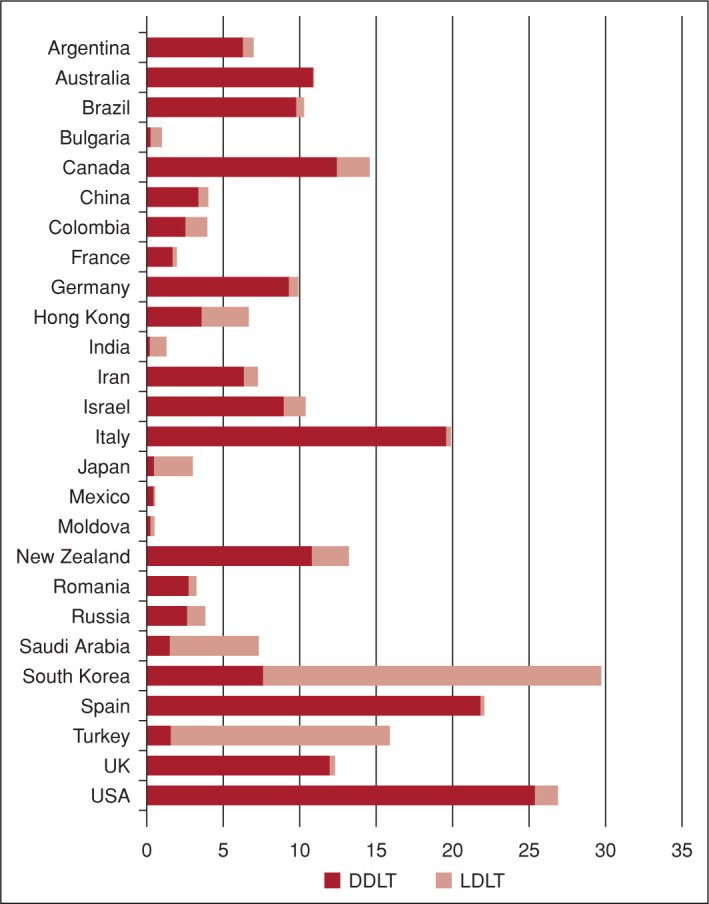
Liver transplantation activity in 2020 (per million population).[54]
The United Nations uses Human Development Index (HDI) to determine the development of the countries. HDI metric includes various factors, including gross national income per capita, life expectancy, and education. Many developing countries have a heterogeneous population, differing levels of education, and financial wealth among their residents with various religious compositions. Developing countries often have a poor collection of organ transplantation activity and limited resources to make the LT data publicly available. This is particularly evident in most countries in Africa and in some countries in Asia.[36] This nontransparent activity and the public lack of awareness prevent organ donation from reaching its maximum potential in these regions.
Despite the modern views encouraging and supporting deceased organ donation, traditional views still influence the majority of people.[1] In many Asian countries, traditions and religious beliefs play a major role in an individual’s life and in shaping the decision of organ donation.[1] Religions including Buddhism, Taoism, Confucianism, Shintoism, and Islam cautiously approach deceased organ donation.[1,15,16]
Many Southeast Asian countries, except Singapore, have low-to-middle income and have similar challenges as faced by other developing countries, such as the lack of infrastructure required for an organized and well-coordinated organ transplantation network, registering potential donors to national programs for coordinating organ procurement and promoting awareness in public.[37]
In Asia, the first successful LT was performed in Taiwan in 1984 by Chen et al.[38] Among Asian countries, China is the only country with DDLT being more common than LDLT, with 95% of donated livers originating from deceased donors.[1,15] This practice stems from China’s prior use of organs from nonvoluntaries, mainly from executed prisoners, which led to concerns over human rights and organ trafficking. Eventually, starting from 2005, with continuous improvements in legislation, China revised its organ transplantation practice on LDLT and implemented WHO guiding principles. In 2015, China completely left the practice of using organs from executed prisoners.[1,15,39]
Singapore has a developed economy with large health care expenditures.[37] Singapore started using an opt-out system in 1987 with restrictive inclusion criteria such as only including those between 21 and 60 years old after a traumatic cause of death and allowing only kidney procurement. This system has been modified multiple times over the years and now allows a wide range of potential donors to be included while allowing procurement of liver and other organs.[37]
Despite these legislations, DDLT remains very low in Singapore compared with other developed countries (approximately 6 per million population [pmp] per year).[37,40] Main barriers are lack of awareness of organ donation, discrepancies between donor referral and transplantation, and cultural or religious beliefs.[37] To overcome organ scarcity, LDLT plays a major role in Singapore.
In some developing countries with two-tier health care systems, such as South Africa and India, wealthy patients often have easier access to transplants than those with limited resources.[36] This modality also augments the public mistrust of organ transplantation in those countries. Apart from religious beliefs, in some developing countries such as India, the Philippines, Thailand, Indonesia, and Vietnam, DDLT rates remain low. Other factors including lack of awareness of organ donation, lack of organized networks and national policies to facilitate organ transplantations, and poverty are some other explanations.[1]
In India, the Transplantation of Human Organ Bill became law in 1995; however, DDLT was not widely adopted, with most centers performing LDLT to meet the needs of the patients.[2] In India, approximately 85% of LT is derived from LDLT.[2] The low rates of DDLT in India are thought to be a result of limited government policies across the country, better understanding of brain death, limited identification of potential donors, and lack of awareness and education of the public regarding organ donation.[2]
The first DDLT in Turkey was performed by Haberal et al. in 1988.[41] In addition, the same team performed the first left lobe LDLT procedure in the world in an adult patient in 1990.[42] In Turkey, a study reported that families of 23.4% of patients with brain death were permitted to use the deceased organs to be used for transplantation between 2011 and 2014.[16] Only one-fourth of LT in Turkey is derived from DDLT; however, as a result of efforts to create public awareness of organ donation, 0.9 pmp in 2001 increased to 7 pmp in 2019.[15,16]
Despite being a developed country, Japan shows low DDLT rates. First, the use of a deceased donor in Japan in 1968 aroused public mistrust because of the lack of proper documentation of the brain death of the donor.[1,43] South Korea and China have been more successful in promoting DDLT awareness and increasing the numbers of LT from deceased donors over the last decade, and Iran and India are following this trend slower.[18]
Consent Systems for Organ Donation
Opt-in (explicit consent) and opt-out (presumed consent) are two systems that exist for organ donation after death. In an opt-in system, potential donors need to actively give their consent for their organs to be used after death, whereas in an opt-out system, no active consent is needed, and individuals are presumed to give the consent unless they specifically indicate the opposite.[36,44] Opt-out systems may increase donation rates and may overcome challenges in deceased organ donation including culture and religious beliefs and transplant awareness.[34,36] However, this system requires governmental support in building the public infrastructure and may not be feasible in many countries with limited resources.
In addition, hard consent, soft consent, and mandated consent exist and are used in many countries.[36] Hard consent leaves no involvement of family in the donation process, whereas soft consent involves family. Mandated consent requires individuals to register their intent to donate or not donate. This approach gives individuals to make a decision for themselves.
Spain is an example of a country with a successful opt-out system (despite it being practiced as a hybrid opt-in and opt-out), with the highest number of donors per pmp (49.6 in 2019, compared with 36.8 in the USA).[36,44] However, this highest pmp in Spain is not only a result of the opt-out system but also a result of early identification of organ donors by transplant coordinators, successful coordination of organ transplant network, and an effective communication system with family members with specifically trained professionals.[2]
Some reports argue that opt-in versus opt-out systems alone do not differ greatly in terms of increasing donor numbers; an opt-out system is not imperative in all countries.[35,36] Multifaceted approaches, such as legislative adaptation and consideration of health care resources and population dynamics in each country, are necessary to overcome the barriers to organ donation and maximize deceased organ utilization.[36,44]
Liver Transplant Registries
Compared with LLDT, DDLT requires a widespread organization from coordination of organ procurement to allocating a recipient, and agencies to oversee these activities, and requires more financial resources to establish a successful network.[15] In the USA, National Organ Transplant Act established the Organ Procurement and Transplantation Network (OPTN) in 1984 to develop policies around waiting list, organ donation and procurement, organ allocation, and transplantation. United Network Organ Sharing (UNOS) is a nonprofit, federally funded organization that manages the OPTN.[2,29,44] In Europe, European Liver Transplant Registry was established in 1985, and similar organizations exist in China, Korea, and Japan.[2] In Europe, the European Directive, Declaration of Istanbul, and the WHO guiding principles are implemented to ensure the safety of living organ donors and report any adverse effects after donation.[4,45,46] In some countries in Asia, the lack of national LT registries and limited collection and uniform reporting of data prevent having accurate outcomes of LT activity.[18] Despite successful organizations in Europe (ELTR) and in the USA (UNOS), establishing a regional registry in Asia might be more difficult given the available financial resources and geopolitical situation.
Liver Transplantation Center Volume on Outcomes
Transplant center volume is an important factor in LT outcome, with only a few reports investigating this topic.[47–50] The majority of LDLT in Asia are performed in centers with high volume transplant numbers and having multidisciplinary care staff, given the complexity of the operation.[37] High-volume transplant centers usually have less unfavorable outcomes compared with low-to-middle volume transplant centers.[47–49] However, with the acuity of LT in certain conditions such as acute liver failure and socioeconomic and geographic limitations, access to such centers may not be feasible. In addition, it has been reported that patients are less likely to have LT in those programs and have a higher risk of mortality after LT.[47,49] Narrowing this outcome gap is important to minimize the disparities across the transplant centers and to improve overall outcomes after LT at the national level.
Barriers to Liver Transplantation
Societal Beliefs, Traditions, and Religion
Traditions, beliefs, and religion play a strong role in daily life and decision-making in many countries and are important in public attitude toward organ transplantation, particularly deceased-organ donation.[1,31]
Mistrust of Health Care System
Mistrust of the health care system and policymakers are another barrier in LT, with the belief that professionals have control over the organ transplantation process and legalities involving brain death for DDLT.[15,44] Financial incentives and manipulation of transplant systems, as seen in South Africa in 2002 and Germany in 2013, resulted in dramatic decreases in donor numbers.[36,51] In China, unethical procurement of donor organs from prisoners without informed consent has disrupted the public trust in organizations.[52]
It was reported in 2007 that up to 10% of organ transplants worldwide are involved in organ trafficking or patients who travel abroad to buy organs from vulnerable people.[45,53] Declaration of Istanbul was developed to prevent human organ trafficking and to prevent the exploitation of poor individuals/countries being organ donors to recipients of wealthy individuals/countries in 2008.[1] To overcome these barriers and regain public trust, we recommend transparency in every step of organ transplantation.[36]
Conclusion
With the success of the LT, the demand for liver exponentially increases while the number of donors remains relatively stable. The practice of LT varies widely depending on the region. To maximize the pool of available organs, the East should focus on improving deceased liver donation, whereas the West needs to improve living-donor liver donation. Efforts must be made to approach the barriers in LT in multifaceted ways as LT is a life-saving treatment.
Footnotes
How to cite this article: Ozturk NB, Muhammad H, Gurakar M, Aslan A, Gurakar A, Dao D. Liver transplantation in developing countries. Hepatology Forum 2022; 3(3):103–107.
Peer-review
Externally peer-reviewed.
Author Contributions
Concept – DD, AG; Design – NBO, AG, HM, DD; Supervision – AG; Literature Search – NBO, AA, HM; Writing – NBO, AA, HM, MG, AG; Critical Reviews – DD, MG, AG.
Conflict of Interest
The authors have no conflict of interest to declare.
Financial Disclosure
The authors declared that this study has received no financial support.
References
- 1.Chen CL, Kabiling CS, Concejero AM. Why does living donor liver transplantation flourish in Asia? Nat Rev Gastroenterol Hepatol. 2013;10(12):746–751. doi: 10.1038/nrgastro.2013.194. [DOI] [PubMed] [Google Scholar]
- 2.Shukla A, Vadeyar H, Rela M, Shah S. Liver Transplantation: East versus West. J Clin Exp Hepatol. 2013;3(3):243–253. doi: 10.1016/j.jceh.2013.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cameron AM, Ghobrial RM, Yersiz H, Farmer DG, Lipshutz GS, Gordon SA, et al. Optimal utilization of donor grafts with extended criteria: A single-center experience in over 1000 liver transplants. Ann Surg. 2006;243(6):748–755. doi: 10.1097/01.sla.0000219669.84192.b3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lennerling A, Lovén C, Dor FJ, Ambagtsheer F, Duerinckx N, Frunza M, et al. Living organ donation practices in Europe-results from an online survey. Transpl Int. 2013;26(2):145–153. doi: 10.1111/tri.12012. [DOI] [PubMed] [Google Scholar]
- 5.Lobritto S, Kato T, Emond J. Living-donor liver transplantation: Current perspective. Semin Liver Dis. 2013;32(4):333–40. doi: 10.1055/s-0032-1329900. [DOI] [PubMed] [Google Scholar]
- 6.Muhammad H, Zaffar D, Tehreem A, Ting PS, Simsek C, Turan I, et al. an update on usage of high-risk donors in liver transplantation. J Clin Med. 2021;11(1):215. doi: 10.3390/jcm11010215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bismuth H, Houssin D. Reduced-sized orthotopic liver graft in hepatic transplantation in children. Surgery. 1984;95(3):367–370. [PubMed] [Google Scholar]
- 8.Pichlmayr R, Ringe B, Gubernatis G, Hauss J, Bunzendahl H. Transplantation einer Spenderleber auf zwei Empfänger (Splitting-Transplantation)--Eine neue Methode in der Weiterentwicklung der Lebersegmenttransplantation [Transplantation of a donor liver to 2 recipients (splitting transplantation)--a new method in the further development of segmental liver transplantation] Langenbecks Arch Chir. 1988;373(2):127–130. [German] [PubMed] [Google Scholar]
- 9.Strong RW, Lynch SV, Ong TH, Matsunami H, Koido Y, Balderson GA. Successful liver transplantation from a living donor to her son. N Engl J Med. 1990;322(21):1505–1507. doi: 10.1056/NEJM199005243222106. [DOI] [PubMed] [Google Scholar]
- 10.Cheah YL, Simpson MA, Pomposelli JJ, Pomfret EA. Incidence of death and potentially life-threatening near-miss events in living donor hepatic lobectomy: A world-wide survey: Death and near-miss events. Liver Transpl. 2013;19(5):499–506. doi: 10.1002/lt.23575. [DOI] [PubMed] [Google Scholar]
- 11.Kornberg A. Liver transplantation for hepatocellular carcinoma beyond Milan criteria: Multidisciplinary approach to improve outcome. ISRN Hepatol. 2014;2014:706945. doi: 10.1155/2014/706945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wakade VA, Mathur SK. Donor safety in live-related liver Transplantation. Indian J Surg. 2012;74(1):118–126. doi: 10.1007/s12262-011-0385-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kaido T, Uemoto S. Does living donation have advantages over deceased donation in liver transplantation? J Gastroenterol Hepatol. 2010;25(10):1598–603. doi: 10.1111/j.1440-1746.2010.06418.x. [DOI] [PubMed] [Google Scholar]
- 14.Trotter JF, Cárdenas A. Liver transplantation around the world. Liver Transpl. 2016;22(8):1059–1061. doi: 10.1002/lt.24508. [DOI] [PubMed] [Google Scholar]
- 15.Rela M, Rammohan A. Why are there so many liver transplants from living donors in Asia and so few in Europe and the US? J Hepatol. 2021;75(4):975–980. doi: 10.1016/j.jhep.2021.05.036. [DOI] [PubMed] [Google Scholar]
- 16.Akbulut S, Yilmaz S. Liver transplantation in Turkey: Historical review and future perspectives. Transplant Rev. 2015;29(3):161–167. doi: 10.1016/j.trre.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 17.Kaido T, Mori A, Ogura Y, Hata K, Yoshizawa A, Iida T, et al. Lower limit of the graft-to-recipient weight ratio can be safely reduced to 0.6% in adult-to-adult living donor liver transplantation in combination with portal pressure control. Transplant Proc. 2011;43(6):2391–2393. doi: 10.1016/j.transproceed.2011.05.037. [DOI] [PubMed] [Google Scholar]
- 18.Hibi T, Wei Chieh AK, Chi-Yan Chan A, Bhangui P. Current status of liver transplantation in Asia. Int J Surg. 2020;82S:4–8. doi: 10.1016/j.ijsu.2020.05.071. [DOI] [PubMed] [Google Scholar]
- 19.Moon AM, Singal AG, Tapper EB. Contemporary epidemiology of chronic liver disease and cirrhosis. Clin Gastroenterol Hepatol. 2020;18(12):2650–2666. doi: 10.1016/j.cgh.2019.07.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alqahtani SA, Larson AM. Adult liver transplantation in the USA. Curr Opin Gastroenterol. 2011;27(3):240–247. doi: 10.1097/MOG.0b013e3283457d5d. [DOI] [PubMed] [Google Scholar]
- 21.Goldberg D, Ditah IC, Saeian K, Lalehzari M, Aronsohn A, Gorospe EC, et al. Changes in the prevalence of hepatitis c virus infection, nonalcoholic steatohepatitis, and alcoholic liver disease among patients with cirrhosis or liver failure on the waitlist for liver Transplantation. Gastroenterology. 2017;152(5):1090–1099.e1. doi: 10.1053/j.gastro.2017.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wong RJ, Singal AK. Trends in liver disease etiology among adults awaiting liver transplantation in the United States, 2014-2019. JAMA Netw Open. 2020;3(2):e1920294. doi: 10.1001/jamanetworkopen.2019.20294. [DOI] [PubMed] [Google Scholar]
- 23.Wong MCS, Huang JLW, George J, Huang J, Leung C, Eslam M, et al. The changing epidemiology of liver diseases in the Asia-Pacific region. Nat Rev Gastroenterol Hepatol. 2019;16(1):57–73. doi: 10.1038/s41575-018-0055-0. [DOI] [PubMed] [Google Scholar]
- 24.Razavi H. Global epidemiology of viral hepatitis. Gastroenterol Clin North Am. 2020;49(2):179–189. doi: 10.1016/j.gtc.2020.01.001. [DOI] [PubMed] [Google Scholar]
- 25.Jefferies M, Rauff B, Rashid H, Lam T, Rafiq S. Update on global epidemiology of viral hepatitis and preventive strategies. World J Clin Cases. 2018;6:589–599. doi: 10.12998/wjcc.v6.i13.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blach S, Terrault NA, Tacke F, Gamkrelidze I, Craxi A, Tanaka J, et al. Global change in hepatitis C virus prevalence and cascade of care between 2015 and 2020: a modelling study. Lancet Gastroenterol Hepatol. 2022;7(5):396–415. doi: 10.1016/S2468-1253(21)00472-6. [DOI] [PubMed] [Google Scholar]
- 27.Serin A, Sahin T, Arikan BT, Emek E, Bozkurt B, Tokat Y. A changing etiologic scenario in liver transplantation: A single-center cohort study from Turkey. Transplant Proc. 2019;51(7):2416–2419. doi: 10.1016/j.transproceed.2019.01.190. [DOI] [PubMed] [Google Scholar]
- 28.Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, et al. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334(11):693–700. doi: 10.1056/NEJM199603143341104. [DOI] [PubMed] [Google Scholar]
- 29.Mahmud N. Selection for liver transplantation: Indications and evaluation. Curr Hepatol Rep. 2020;19(3):203–212. doi: 10.1007/s11901-020-00527-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yao FY, Ferrell L, Bass NM, Watson JJ, Bacchetti P, Venook A, et al. Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology. 2001;33(6):1394–1403. doi: 10.1053/jhep.2001.24563. [DOI] [PubMed] [Google Scholar]
- 31.Petrowsky H, Kim KH, Tokat Y, editors. Editorial: Living-donor liver transplantation: why the Sun rises in the East and sets in the West? Curr Opin Organ Transplant. 2019;24(5):620–622. doi: 10.1097/MOT.0000000000000700. [DOI] [PubMed] [Google Scholar]
- 32.Florman S, Miller CM. Live donor liver transplantation. Liver Transpl. 2006;12(4):499–510. doi: 10.1002/lt.20754. [DOI] [PubMed] [Google Scholar]
- 33.Muhammad H, Gurakar M, Ting PS, Alsughayer AM, Luu H, Zaffar D, et al. Long-term outcomes of living donor versus deceased donor liver transplant for hepatocellular carcinoma in the United States. Exp Clin Transplant. 2022;20(3):279–284. doi: 10.6002/ect.2021.0479. [DOI] [PubMed] [Google Scholar]
- 34.Ezaz G, Lai M. How the. “Opt-In” option optimizes organ donation rates. Dig Dis Sci. 2019;64(5):1067–1069. doi: 10.1007/s10620-019-05483-z. [DOI] [PubMed] [Google Scholar]
- 35.Saab S, Saggi SS, Akbar M, Choi G. Presumed consent: A potential tool for countries experiencing an organ donation crisis. Dig Dis Sci. 2019;64(5):1346–1355. doi: 10.1007/s10620-018-5388-6. [DOI] [PubMed] [Google Scholar]
- 36.Etheredge HR. Assessing global organ donation policies: Opt-in vs opt-out. Risk Manag Healthc Policy. 2021;14:1985–1998. doi: 10.2147/RMHP.S270234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yeow M, Bonney GK, Kow WCA, Wee P, Madhavan K, Iyer SG. Liver transplantation in Singapore: Challenges and strategies of low-to mid-volume centers. Transplantation. 2022;106(5):895–897. doi: 10.1097/TP.0000000000003925. [DOI] [PubMed] [Google Scholar]
- 38.Chen YS, Chen CL, de Villa VH, Wang CC, Wang SH, Liu PP, et al. Living-Donor Liver Transplantation in Taiwan. In: Kitajima M, Shimazu M, Wakabayashi G, Hoshino K, Tanabe M, Kawachi S, editors. Current Issues in Liver and Small Bowel Transplantation. Tokyo: Springer Japan; 2002. pp. 13–21. (Keio University International Symposia for Life Sciences and Medicine) [Google Scholar]
- 39.Shi BY, Liu ZJ, Yu T. Development of the organ donation and transplantation system in China. Chin Med J (Engl) 2020;133(7):760–765. doi: 10.1097/CM9.0000000000000779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kwek TK, Lew TWK, Tan HL, Kong S. The transplantable organ shortage in Singapore: has implementation of presumed consent to organ donation made a difference? Ann Acad Med Singap. 2009;38(4):346–348. [PubMed] [Google Scholar]
- 41.Haberal M, Sert S, Aybasti N, Gulay H, Gokce O, Arslan G, et al. Living donor kidney transplantation. Transplant Proc. 1988;20(1 Suppl 1):353–355. [PubMed] [Google Scholar]
- 42.Haberal M, Buyukpamukcu N, Telatar H, Bilgin N, Arslan G, Simsek H, et al. Segmental living liver transplantation in children and adults. Transplant Proc. 1992;24(6):2687–2689. [PubMed] [Google Scholar]
- 43.Kimura R. Organ transplantation and brain-death in Japan. Cultural, legal and bioethical background. Ann Transplant. 1998;3(3):55–58. [PubMed] [Google Scholar]
- 44.Lewis A, Koukoura A, Tsianos GI, Gargavanis AA, Nielsen AA, Vassiliadis E. Organ donation in the US and Europe: The supply vs demand imbalance. Transplant Rev. 2021;35(2):100585. doi: 10.1016/j.trre.2020.100585. [DOI] [PubMed] [Google Scholar]
- 45.The Declaration of Istanbul on Organ Trafficking and Transplant Tourism (2018 Edition) Transplantation. 2019;103(2):218–219. doi: 10.1097/TP.0000000000002540. [DOI] [PubMed] [Google Scholar]
- 46.World Health Organization WHO guiding principles on human cell, tissue and organ transplantation. Transplantation. 2010;90(3):229–233. doi: 10.1097/TP.0b013e3181ec29f0. [DOI] [PubMed] [Google Scholar]
- 47.Alqahtani SA, Stepanova M, Kabbara KW, Younossi I, Mishra A, Younossi Z. Liver transplant center size and the impact on clinical outcomes and resource Utilization. Transplantation. 2022;106(5):988–996. doi: 10.1097/TP.0000000000003915. [DOI] [PubMed] [Google Scholar]
- 48.Axelrod DA, Guidinger MK, McCullough KP, Leichtman AB, Punch JD, Merion RM. Association of center volume with outcome after liver and kidney transplantation. Am J Transplant. 2004;4(6):920–927. doi: 10.1111/j.1600-6143.2004.00462.x. [DOI] [PubMed] [Google Scholar]
- 49.Edwards EB, Roberts JP, McBride MA, Schulak JA, Hunsicker LG. The effect of the volume of procedures at transplantation centers on mortality after liver transplantation. N Engl J Med. 1999;341(27):2049–2053. doi: 10.1056/NEJM199912303412703. [DOI] [PubMed] [Google Scholar]
- 50.Ozhathil DK, Li YF, Smith JK, Tseng JF, Saidi RF, Bozorgzadeh A, Shah SA. Impact of center volume on outcomes of increased-risk liver transplants. Liver Transpl. 2011;17(10):1191–1199. doi: 10.1002/lt.22343. [DOI] [PubMed] [Google Scholar]
- 51.Sidley P. South African doctors charged with involvement in organ trade. BMJ. 2004;329(7459):190. doi: 10.1136/bmj.329.7459.190-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Paul NW, Caplan A, Shapiro ME, Els C, Allison KC, Li H. Human rights violations in organ procurement practice in China. BMC Med Ethics. 2017;18(1):11. doi: 10.1186/s12910-017-0169-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Shimazono Y. The state of the international organ trade: a provisional picture based on integration of available information. Bull World Health Organ. 2007;85(12):955–962. doi: 10.2471/BLT.06.039370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.International registry in organ donation and transplantation (Internet) 2022. Accessed on April 28 2022. Available at: https://www.irodat.org/


