Abstract
Introduction and Objectives:
Research suggests that perceived immigration policy vulnerability has important health implications. Coupled with the mental and physical stressors accompanying the postpartum period and a growing awareness of the discrimination and structural racism experienced by marginalized communities globally, the coronavirus disease 2019 period may have exacerbated stress among vulnerable populations, specifically postpartum Hispanic/Latina women. This study evaluated perceived immigration policy vulnerability (i.e. discrimination, social isolation, and family threats) in early postpartum Hispanic/Latina women in Los Angeles before and during the coronavirus disease 2019 pandemic.
Methods:
The Perceived Immigration Policy Effects Scale (PIPES) was administered cross-sectionally at 1 month postpartum to 187 Hispanic/Latina women in the MADRES cohort. Respondents between September 2018 and March 2020 were classified as “pre-pandemic” (N = 128), between March 2020 and July 2020 as “early pandemic” (N = 38), and between August 2020 and November 2021 as “later pandemic” (N = 21). Average PIPES subscale scores were dichotomized into “higher” and “lower” groups (⩽median, >median) and logistic regression models were performed.
Results:
Approximately half of participants had incomes of <$50,000 (50.3%) and were Latin American born (54.6%). After adjusting for age, nativity, education, income, postpartum distress, and employment status, early pandemic respondents had 5.05 times the odds of a higher score on the perceived discrimination subscale (95% CI: 1.81, 14.11), 6.47 times the odds of a higher score on the social isolation subscale (95% CI: 2.23, 18.74), 2.66 times the odds of a higher score on the family threats subscale (95% CI: 0.97, 7.32), and 3.36 times the odds of a higher total score (95% CI: 1.19, 9.51) when compared to pre-pandemic respondents. There were no significant subscale score differences between later pandemic and pre-pandemic periods.
Conclusion:
Higher perceived immigration policy vulnerability was reported among postpartum women during the early coronavirus disease 2019 pandemic versus pre-pandemic periods. This suggests greater social inequities during the early pandemic period.
Keywords: COVID-19, immigration policy concerns, postpartum mental health, public health, women’s health
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has been characterized as a stressful and uncontrollable event which has resulted in distressing health and financial consequences, such as chronic illness, death, loss of income, and housing insecurity, particularly among communities of color.1–5 Alongside the COVID-19 pandemic period, a host of political and social events have occurred which have intensified anti-immigration rhetoric and shown a national spotlight on the structural racism experienced by marginalized communities, further increasing social inequities. 6 Coupled with the disproportionate burden of COVID-19 infection prevalence among minority groups, the pandemic has intensified existing social, economic, and health disparities.7–10 These simultaneous events during the pandemic period have placed a high mental burden among immigrant communities who report increased perceptions of vulnerabilities to COVID-19 as well as higher levels of perceived discrimination.6,11 Such perceived vulnerabilities may impact the overall psychological well-being and utilization of health care resources among postpartum women of color12–15 as the COVID-19 pandemic period has also been associated with a disproportionate increase in symptoms of distress and anxiety among postpartum women from marginalized communities.16–23
Elevated levels of perceived vulnerability to immigration policies, such as increased perceptions of discrimination, social isolation, and familial threats due to their immigration status and related policies, could increase psychological distress among perinatal Hispanic/Latina women. 24 The perinatal and early postpartum periods are characterized by neuroendocrine shifts (such as hypothalamic–pituitary–adrenal axis dysregulation) and dramatic life changes which may exacerbate stress responses and place postpartum mothers in a particularly vulnerable position.25,26 Psychosocial stressors and anxiety among postpartum women impact their quality of life, alter their interactions with their infants and partners, and can lower the quality of the home environment.27,28 Moreover, postpartum distress can have intergenerational consequences, impacting child behavioral, cognitive, and social emotional developmental outcomes.27,29 Latina women have a high risk of developing perinatal anxiety and postpartum depression.30,31 As a result, factors which may contribute to psychological postpartum distress, such as immigration-related stressors, are of concern.
Since immigration-related concerns may place a high mental burden among postpartum Latina women, they are important to understand within the context of the highly stressful COVID-19 pandemic period. In this study, we examined differences in perceived discrimination, social isolation, and family threats due to immigration policies between early postpartum Hispanic/Latina women in Los Angeles before and during two timepoints within the COVID-19 pandemic. Given the many political and social stressors experienced during the COVID-19 pandemic period and the heightened anti-immigration climate, we hypothesized that participants would have higher perceived vulnerabilities to immigration during the COVID-19 pandemic timepoints as compared to before the pandemic.
Methods
Study sample
The Maternal And Developmental Risks from Environmental and Social Stressors (MADRES) study is an ongoing prospective pregnancy cohort of low-income, predominantly Hispanic women residing in Los Angeles, CA. The methods and protocol of this cohort have been described elsewhere. 32 In brief, MADRES participants were recruited beginning in 2015 to the present, from four prenatal clinic sites, including two community health clinics, one county hospital prenatal clinic, one private obstetrics and gynecology practice, and through self-referrals from community meetings and local advertisements. Eligible participants at time of recruitment were: (1) less than 30-week gestation, (2) over 18 years of age, and (3) fluent in English or Spanish. Exclusion criteria included: (1) multiple gestation, (2) having a physical, mental, or cognitive disability that prevented participation or ability to provide consent, (3) current incarceration, and (4) HIV-positive status. Written informed consent was obtained at study entry for each participant and the study was approved by the University of Southern California’s Institutional Review Board (ethics approval number = HS-15-00498).
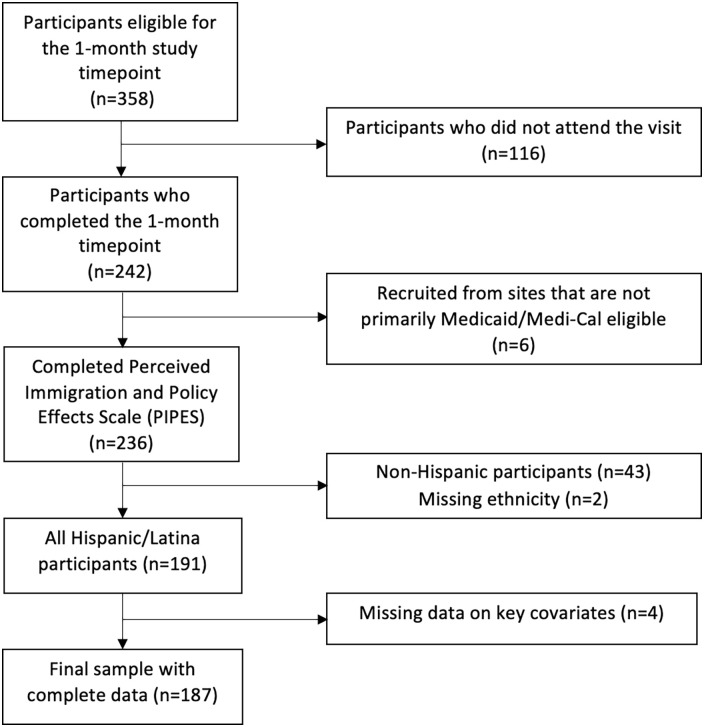
This cross-sectional study was performed on a subset of participants from the MADRES study, with our outcome of interest, perceived vulnerabilities to immigration policies, measured using the Perceived Immigration Policy Effects Scale (PIPES), and our exposure of interest, COVID-19 pandemic periods, created using the date the PIPES questionnaire was administered. Within the MADRES cohort, a total of 358 participants were eligible for the one-month study timepoint. A total of 242 MADRES participants completed the 1-month questionnaire, including the PIPES questionnaire. The 187 Hispanic participants included in this analysis were: (1) of Hispanic ethnicity, (2) recruited from primarily Medicaid/Medi-Cal eligible clinics, and (3) had complete data on our exposure, key covariates, and outcome of interest (Figure 1). This subset of 187 participants were recruited into the MADRES study from April 10, 2018, to June 17, 2021, and were administered the PIPES questionnaire from September 1, 2018, to November 8, 2021.
Figure 1.
Consort diagram of maternal participants included in the analyses.
Data collection
All data were collected by well-trained, bilingual MADRES staff. Participant demographic data were collected through interviewer-administered questionnaires at study entry during pregnancy. The Postpartum Distress Measure (PDM) 33 and PIPES 34 were administered in-person or via telephone questionnaire using participants’ preferred language (English or Spanish) at the 1-month postpartum study timepoint.
COVID-19 pandemic periods
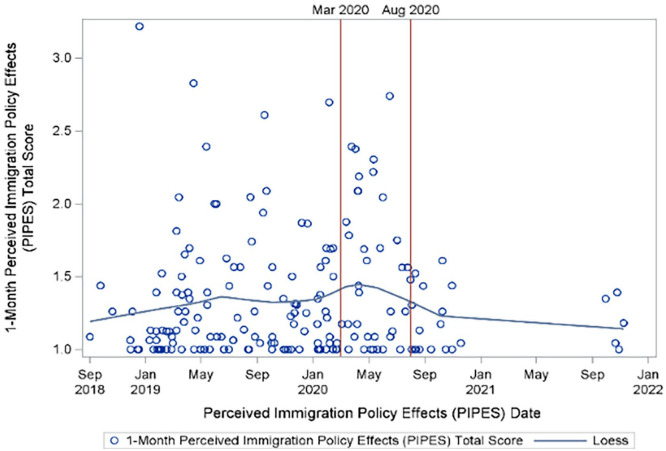
Three COVID-19 pandemic periods were identified for this analysis based on the regional progression of the pandemic in Los Angeles. Since March 2020 marked the first announced LA County COVID-19 cases and deaths as well as the initiation of rapid social distancing measures and subsequent lockdowns, 35 questionnaire responses prior to March 1, 2020 were classified as “pre-pandemic” and those between March 1, 2020 and July 31, 2020 were classified as the “early pandemic” period. The period between August 1, 2020 and November 8, 2021 coincided with a general easing of the pandemic lockdown restrictions and announcements of long-term reopening plans in California, prior to the resurgence of cases due to the Delta and Omicron variants. 36 Thus, this period was classified as a separate timepoint labeled the “later pandemic” period. As shown in Figure 2, we additionally explored total PIPES scores in our population across time using a Locally Weighted Scatterplot Smoothing (LOWESS) plot and visually evaluated the three distinct timepoints. There was a noticeable increase in total PIPES scores between March 2020 and July 2020 compared to the other periods. These three timepoints provided the opportunity to examine participant stressors before the pandemic, during the early isolation phase of the pandemic, and during the period of easing of pandemic restrictions to compare shifts of the COVID-19 impacts on participant stressors.
Figure 2.
Locally Weighted Scatterplot Smoothing (LOWESS) of total PIPES scores across date the PIPES questionnaire was administered.
The Perceived Immigration Policy Effects Scale
The PIPES questionnaire was originally developed and validated to evaluate the impacts of state-level immigration policies among Latino immigrant parents. 34 There are a total of 24 items in the PIPES questionnaire that can be summed together to create a total score scale. The 24 items additionally represent four subscales including discrimination (11 items), social isolation (5 items), children’s vulnerability (5 items), and threats to the family (3 items). Participants respond to each PIPES question on a Likert-type scale ranging from 1 (Never) to 5 (Always) and each subscale and the total scale is scored by summing together participant responses.
Participants in this study were administered 23 of the 24 items on the PIPES questionnaire at the 1-month postpartum study timepoint using participants’ preferred language (English or Spanish). Since not all participants who were originally administered the questionnaire were Hispanic/Latina, we removed one item from the discrimination scale which inquired about treatment from other Latinos. Although the PIPES questionnaire was originally developed for use among immigrant Latinos, both foreign-born and US-born Latina postpartum women were administered the questionnaire given the large number of US Hispanic families with mixed documentation status which could result in similar unique immigration stressors and concerns about their family.37,38 Furthermore, participants without other children were not administered the children’s vulnerability subscale (5 items) and two child specific questions included in the discrimination subscale since they were only applicable to participants with school-aged children. As a result of these adaptations, only the perceived discrimination, social isolation, family threats, and total PIPES scores were analyzed in this study. In addition, the scores for each PIPES subscale were calculated by averaging together responses from each corresponding item on the Likert-type scale (ranging from 1 through 5) and the total PIPES score was computed by averaging together responses from all PIPES questions.
Covariates
We considered various sociodemographic variables as potential covariates based on previous literature and if a variable resulted in a material change (> 10%) in estimated model parameters for the exposure of interest. Maternal recruitment site was included as a study design covariate. Household income (less than US$50,000, US$50,000 or more), age at 30 days postpartum (quartiles), and nativity (foreign born, the US born) were included as demographic covariates based on previous research, while maternal education (⩽high school education, ⩾some college or technical school), employment (employed, on leave and expected to return, homemaker, unemployed), and PDM scores (continuous) were adjusted for as confounders since they all met confounding criteria and resulted in a material change (>10%) in our estimated model parameter for the exposure of interest (i.e. COVID-19 pandemic periods). The PDM is a 10-item questionnaire that assesses symptoms of maternal postpartum depression and anxiety symptoms. 33 Additional covariates evaluated in sensitivity analyses included maternal depression during pregnancy, measured using the Center for Epidemiologic Studies-Depression (CES-D) scale administered at each trimester (yes (defined as having a clinically suggestive cutoff score of ⩾16 for at least one trimester), no), maternal pregnancy complications (yes (defined as having one or more of the following: preeclampsia–eclampsia, chronic hypertension and preeclampsia, gestational hypertension, and postpartum preeclampsia), no), and calendar month the PIPES questionnaire was administered (continuous).
Statistical analysis
We calculated means, medians, and frequencies to summarize key maternal characteristics and PIPES scores across each scale by COVID-19 pandemic period and across all participants analyzed. Average PIPES scores across each scale were right skewed so univariate relationships between potential covariates and total PIPES scores were assessed using non-parametric Kruskal–Wallis tests for categorical covariates and Spearman’s correlations for continuous covariates. Univariate associations between COVID-19 timepoints and average PIPES scores were assessed using Kruskal–Wallis tests. Since linear regression assumptions were not met for our association of interest given the right skewed nature of our residuals, even after log transformation, PIPES scores were dichotomized (⩽median, >median) for each PIPES subscale before modeling and unadjusted logistic regressions performed to assess the association between COVID-19 timepoints and “higher” and “lower” PIPES subscale scores.
We performed multivariable logistic regression models across each dichotomized PIPES subscale group to evaluate the association between COVID-19 pandemic time periods and PIPES groups. Hosmer–Lemeshow goodness-of-fit (GOF) measures were assessed across models, generally suggesting good model fit (p > 0.05). Logistic model linearity assumptions for continuous covariates were assessed using lowess plots and variables categorized if the assumption was not met. PDM total scores at 1 month postpartum met the logistic model linearity assumption for continuous independent variables and were thus modeled continuously; however, maternal age at 1-month postpartum questionnaire administration did not appear linear and was categorized into quartiles. Final models were adjusted for recruitment site, age, nativity, household income, education, employment status, and postpartum distress scores. Sensitivity analyses were performed to assess the robustness of results and included additionally adjusting for possible maternal depression during pregnancy and maternal pregnancy complications. We also performed sensitivity analyses to assess possible seasonality or latent trends, including additionally adjusting for calendar month of PIPES questionnaire administration and subsetting the pre-pandemic period to the same calendar period used in the two post-pandemic periods. Since responses to the PIPES questionnaires during the post-pandemic periods ranged from March 1 to November 18, 2020 and 2021, the pre-pandemic period was subset to include responses to the PIPES questionnaire between March 1 and November 18, 2018 and 2019.
All data were analyzed using SAS Version 9.4 and all analyses assumed a two-sided alternative hypothesis with an alpha level of 0.05.
Results
Descriptive statistics
Maternal characteristics are shown in Table 1 by COVID-19 pandemic period and across all participants analyzed in this study. Overall, participants were primarily Hispanic White (95.7%), and approximately, half were born in Latin America (54.6%), with a large frequency of foreign-born participants born in Mexico (31.0%) and residing in the United States between 11 and 20 years (28.9%). Most participants had a high school education or less (62.0%) and were either married (33.2%) or living with a partner (39.0%). Approximately half of participants had an annual household income of less than US$50,000 (50.3%) and were not employed at 1 month postpartum (homemakers (36.9%), unemployed (31.0%)). However, the sociodemographic profiles of participants’ education level, household income, and employment status varied across pandemic period since respondents differed across time periods resulting in variations in participant characteristics over the course of the study. Most participants during the early pandemic period reported having some college or technical education or more (65.8%) while most participants in the pre-pandemic period (67.2%) and later pandemic period (81.0%) reported having at most a high school education. Although the majority of participants across pandemic periods reported annual household incomes of less than US$50,000, there were a higher percentage of participants during the later pandemic period reporting household incomes of less than US$50,000 (61.9%). There were a higher percentage of employed participants during the pre-pandemic period (32.0%), compared to employment during the early pandemic (7.9%) and later pandemic (4.8%) periods.
Table 1.
Sociodemographic characteristics of 187 Hispanic/Latina mothers in the MADRES study.
| Overall freq. (%) (N = 187) | Pre-pandemic freq. (%) (N = 128) |
Early pandemic freq. (%) (N = 38) |
Later pandemic freq. (%) (N = 21) |
|
|---|---|---|---|---|
| Age at 30 days postpartum | ||||
| Quartile 1 (18.8–24.2 years) | 46 (24.6) | 30 (23.4) | 10 (26.3) | 6 (28.6) |
| Quartile 2 (24.3–28.1 years) | 47 (25.1) | 29 (22.7) | 11 (29.0) | 7 (33.3) |
| Quartile 3 (28.2–32.7 years) | 47 (25.1) | 39 (30.5) | 7 (18.4) | 1 (4.8) |
| Quartile 4 (32.8–46.2 years) | 47 (25.1) | 30 (23.4) | 10 (26.3) | 7 (33.3) |
| Nativity | ||||
| US-born Hispanic | 85 (45.5) | 58 (45.3) | 18 (47.4) | 9 (42.9) |
| Foreign-born Hispanic | 102 (54.6) | 70 (54.7) | 20 (52.6) | 12 (57.1) |
| Country of origin | ||||
| El Salvador | 21 (11.2) | 14 (10.9) | 5 (13.2) | 2 (9.5) |
| Guatemala | 21 (11.2) | 14 (10.9) | 3 (7.9) | 4 (19.1) |
| Honduras | 2 (1.1) | 0 (0.0) | 1 (2.6) | 1 (4.8) |
| Mexico | 58 (31.0) | 42 (32.8) | 11 (29.0) | 5 (23.8) |
| The United States | 85 (45.5) | 58 (45.3) | 18 (47.4) | 9 (42.9) |
| Years living in the United States | ||||
| ⩽10 years | 31 (16.6) | 18 (14.1) | 7 (18.4) | 6 (28.6) |
| 11–20 years | 54 (28.9) | 41 (32.0) | 9 (23.7) | 4 (19.1) |
| >20 years | 16 (8.6) | 10 (7.8) | 4 (10.5) | 2 (9.5) |
| Lifetime resident | 85 (45.5) | 58 (45.3) | 18 (47.4) | 9 (42.9) |
| Missing | 1 (0.5) | 1 (0.8) | 0 (0.0) | 0 (0.0) |
| Race (all Hispanic ethnicity) | ||||
| White | 179 (95.7) | 122 (95.3) | 37 (97.4) | 20 (95.2) |
| Asian | 1 (0.5) | 1 (0.8) | 0 (0.0) | 0 (0.0) |
| Black/African American | 2 (1.1) | 2 (1.6) | 0 (0.0) | 0 (0.0) |
| American Indian/Alaska native | 5 (2.7) | 3 (2.3) | 1 (2.6) | 1 (4.8) |
| Education | ||||
| ⩽High school education | 116 (62.0) | 86 (67.2) | 13 (34.2) | 17 (81.0) |
| ⩾Some college or technical school | 71 (38.0) | 42 (32.8) | 25 (65.8) | 4 (19.1) |
| Household income | ||||
| Less than US$50,000 | 94 (50.3) | 63 (49.2) | 18 (47.4) | 13 (61.9) |
| US$50,000 or more | 12 (6.4) | 7 (5.5) | 4 (10.5) | 1 (4.8) |
| Do not know | 81 (43.3) | 58 (45.3) | 16 (42.1) | 7 (33.3) |
| Marital status | ||||
| Married | 62 (33.2) | 44 (34.4) | 9 (23.7) | 9 (42.9) |
| Living together | 73 (39.0) | 51 (39.8) | 16 (42.1) | 6 (28.6) |
| Never married, single | 37 (19.8) | 22 (17.2) | 10 (26.3) | 5 (23.8) |
| Divorced or separated | 6 (3.2) | 5 (3.9) | 1 (2.6) | 0 (0.0) |
| Decline to answer | 9 (4.8) | 6 (4.7) | 2 (5.3) | 1 (4.8) |
| Employment | ||||
| Employed | 45 (24.1) | 41 (32.0) | 3 (7.9) | 1 (4.8) |
| On leave and expected to return | 15 (8.0) | 0 (0.0) | 11 (29.0) | 4 (19.1) |
| Homemaker | 69 (36.9) | 52 (40.6) | 9 (23.7) | 8 (38.1) |
| Unemployed | 58 (31.0) | 35 (27.3) | 15 (39.5) | 8 (38.1) |
Median PIPES subscale scores across COVID-19 timepoints are presented in Table 2. Early pandemic respondents had significantly higher median scores for the discrimination subscale, social isolation subscale, and total PIPES when compared to pre-pandemic and later pandemic respondents. There were no significant associations between COVID-19 period and threat to family subscale scores. Respondents during the later pandemic period had similar median PIPES scores across scales to pre-pandemic respondents, but lower median scores when compared to respondents during the early pandemic period.
Table 2.
Median perceived immigration and policy effects scores across subscales by pandemic time period and overall (N = 187).
| Discrimination subscale scores | Social isolation subscale scores | Threat to family subscale scores | Total PIPES scores | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pandemic time period | Median | Min. –max. | % >Overall median | Median | Min.–max. | % >Overall median | Median | Min.–max. | % >Overall median | Median | Min.–max. | % >Overall median |
| Overall (N = 187) | 1.0 | 1.0–2.7 | 41.7 | 1.0 | 1.0–3.8 | 39.6 | 1.3 | 1.0–5.0 | 47.1 | 1.2 | 1.0–3.2 | 48.7 |
| Pre-pandemic (N = 128) | 1.0 | 1.0–2.7 | 36.7 | 1.0 | 1.0–3.8 | 32.0 | 1.3 | 1.0–5.0 | 46.1 | 1.1 | 1.0–3.2 | 46.9 |
| Early pandemic (N = 38) | 1.4 | 1.0–2.6 | 63.2 | 1.5 | 1.0–3.0 | 68.4 | 1.5 | 1.0–4.7 | 50.0 | 1.4 | 1.0–2.7 | 57.9 |
| Later pandemic (N = 21) | 1.0 | 1.0–1.5 | 33.3 | 1.0 | 1.0–2.4 | 33.3 | 1.3 | 1.0–2.3 | 47.6 | 1.1 | 1.0–1.6 | 42.9 |
| P value* | <0.01 | <0.01 | 0.4 | 0.02 | ||||||||
PIPES: Perceived Immigration Policy Effects Scale.
The associations between average PIPES subscale scores and COVID-19 timepoints were evaluated using the Kruskal–Wallis tests.
Associations between COVID-19 pandemic periods and PIPES scores
The results of the four unadjusted and adjusted logistic regression models evaluating the association between COVID-19 pandemic timepoint and PIPES score groups across subscales and total PIPES score are shown in Table 3. In the unadjusted models, respondents during the early pandemic period had 2.95 times the odds of a higher score on the perceived discrimination subscale (95% CI: 1.40, 6.26) and 4.60 times the odds of a higher score on the social isolation subscale (95% CI: 2.11, 10.01) when compared to pre-pandemic respondents. There were no significant unadjusted associations between early- and pre-pandemic respondents for the threat to family subscale and total PIPES, and no significant associations between later pandemic respondents and pre-pandemic respondents for any of the PIPES. After adjusting for recruitment site, age, education, nativity, household income, employment status, and postpartum distress scores, participants at 1 month postpartum during the early pandemic period (March 1, 2020–July 31, 2020) had 5.05 times the odds of a higher score on the perceived discrimination subscale (95% CI: 1.81, 14.11), 6.47 times the odds of a higher score on the social isolation subscale (95% CI: 2.23, 18.74), and 2.66 times the odds of a higher score on the threat to family subscale (95% CI: 0.97, 7.32) than those responding to the questionnaire at 1 month postpartum before the pandemic. Similarly, early pandemic period participants had 3.36 times the odds of a higher score on the total PIPES (95% CI: 1.19, 9.51). Participants at 1 month postpartum during the late pandemic period (August 1, 2020–November 8, 2021) did not have any significant associations with PIPES subscales groups when compared to those responding to the questionnaire at 1 month postpartum before the pandemic, after adjusting for recruitment site, age, education, nativity, household income, employment status, and postpartum distress scores.
Table 3.
Associations between pandemic time periods and Perceived Immigration and Policy Effects Scale (PIPES) scores (higher/lower a ) among early postpartum Hispanic women in Los Angeles, CA.
| N | Unadjusted models OR (95% CI) |
Adjusted
b
OR (95% CI) |
|
|---|---|---|---|
| Discrimination subscale | |||
| Pre-pandemic | 128 | 1.00 (reference) | 1.00 (reference) |
| Early pandemic | 38 | 2.95 (1.40, 6.26) | 5.05 (1.81, 14.11) |
| Later pandemic | 21 | 0.86 (0.33, 2.29) | 0.84 (0.28, 2.52) |
| Social isolation subscale | |||
| Pre-pandemic | 128 | 1.00 (reference) | 1.00 (reference) |
| Early pandemic | 38 | 4.60 (2.11, 10.01) | 6.47 (2.23, 18.74) |
| Later pandemic | 21 | 1.06 (0.40, 2.83) | 1.49 (0.48, 4.58) |
| Threat to family subscale | |||
| Pre-pandemic | 128 | 1.00 (reference) | 1.00 (reference) |
| Early pandemic | 38 | 1.17 (0.57, 2.41) | 2.66 (0.97, 7.32) |
| Later pandemic | 21 | 1.06 (0.42, 2.68) | 1.61 (0.54, 4.78) |
| Total PIPES | |||
| Pre-pandemic | 128 | 1.00 (reference) | 1.00 (reference) |
| Early pandemic | 38 | 1.56 (0.75, 3.24) | 3.36 (1.19, 9.51) |
| Later pandemic | 21 | 0.85 (0.34, 2.16) | 1.06 (0.36, 3.11) |
OR: odds ratio; CI: confidence interval; PIPES: Perceived Immigration Policy Effects Scale.
Higher and lower PIPES scores were defined as above or below the overall median values for each subscale. For discrimination and social isolation subscale, the median score = 1.0; for threat to family subscale, the median score = 1.3; and for the total PIPES, the median score = 1.2.
Models were adjusted for recruitment site, maternal age, maternal nativity, maternal education, household income, postpartum distress score, and employment status.
The results of the sensitivity analyses additionally adjusting for maternal depression during pregnancy and maternal pregnancy complications are shown in Supplemental Table 1. Overall, effect estimates across COVID-19 pandemic periods were similar to those in the final adjusted models. Similarly, sensitivity analyses additionally adjusting for calendar month of PIPES questionnaire administration and subsetting the pre-pandemic period to the exact calendar period used for the post-pandemic periods moved in similar directions to our final adjusted models; however, effect estimates for the latter were attenuated (Supplemental Table 2).
Discussion
Relative to pre-pandemic periods, we found elevated perceptions of discrimination, social isolation, and total PIPES scores due to immigration policies among Hispanic/Latina participants at one-month postpartum during the early COVID-19 pandemic in a low-income cohort in Los Angeles, California. Perceived threats to family subscores during the early COVID-19 pandemic were similarly elevated when compared to pre-pandemic periods; however, this association was not statistically significant. Perceptions of discrimination, social isolation, and threats to family due to immigration policies after lockdown periods ended (i.e. later pandemic period) were not significantly elevated, suggesting the immigration-related stressors observed during the early pandemic period may have eased alongside COVID-19 restrictions.
The early COVID-19 period coincided with an increase in anti-immigration rhetoric experienced in the United States, uncovering social and political fractures within communities and resulting in discriminatory responses and a doubling down on border policies. 39 Anti-immigration rhetoric and policies have important implications toward the mental and physical well-being of Hispanic communities, generally increasing feelings of fear, confusion, and anxiety and decreasing self-reported health.40,41 This is particularly important among early postpartum Hispanic/Latina women as previous research suggests that stressors, such as perceived discrimination, isolation, and anxiety regarding immigration policy concerns may contribute to the prevalence of distress, depression, and anxiety.13,40,42–45
Early postpartum mothers are in a uniquely vulnerable position with the recent delivery of their newborn infants, changing household dynamics, and corresponding shifts in their physical and mental health.46,47 As a result of the COVID-19 pandemic, postpartum Hispanic mothers were faced with the unprecedented disadvantage of having to navigate a global pandemic within the context of an exceedingly hostile immigration and discriminatory climate while simultaneously caring for a newborn infant. Immigration policy concerns and the perceptions of discrimination, social isolation, and family threats experienced by postpartum Hispanic mothers are unique stressors which may contribute to the mental health disparities observed during the COVID-19 pandemic.19,23,48 Previous studies have found associations between perceptions of discrimination, social isolation, and familial threats and increased psychological distress and mental health issues among Latina mothers13,49but, this association has not been explored within the context of the COVID-19 pandemic or other natural disaster. However, a study by Mollard et al. 17 explored the impacts of COVID-19 on stress and resilience factors, finding higher levels of stress and lower levels of resilience during the pandemic among postpartum women of color when compared to pre-pandemic norms. In addition, previous studies have found increased associations between perceived discrimination and familial threats and increased avoidance strategies, such as decreased visits to health care providers.14,50 This is of high concern given the important role health care visits play in maternal and infant health during the first year postpartum. 14 A more thorough understanding of the immigration policy-related stressors impacting postpartum women during the COVID-19 pandemic can support the development of resources and strategies tailored to support the psychosocial well-being of Hispanic mothers and children.
To our knowledge, no studies have explored the impacts of COVID-19 on immigration policy concerns and perceptions of discrimination, social isolation, and threats to family safety among Hispanic women at 1 month postpartum. However, a cross-sectional study by Janevic et al. 51 explored the impacts of the COVID-19 pandemic on birth satisfaction and perceived health care discrimination during childbirth and the influence of these experiences on the postpartum health of 237 predominately non-Hispanic White women (61.7%) through a bilingual web survey administered at two hospitals in New York City. This study found that Black (8.5%) and Latina women (14.5%) had higher perceived health care discrimination. In addition, one or more experiences of health care discrimination were associated with higher levels of postpartum stress and birth-related post-traumatic stress disorder (PTSD) among all study participants. Since Black/Latina women reported a higher frequency of perceived health care discrimination, this study suggests that increased mental health issues among Black/Latina women may result from a myriad of different factors. Our results suggest that immigration-related concerns, coupled with social isolation and stressful life events, may be an additional compounding factor.
The many strengths of this study include an ongoing, established prospective cohort study, with participants experiencing the postpartum period before and during the pandemic. We were able to explore pre-pandemic perceptions of immigration policy effects using a validated scale, compared to periods during the pandemic at a vulnerable window for mental health effects in postpartum women. An additional strength of this study was the ability to assess these impacts in a predominantly Hispanic/Latina population residing in Los Angeles, with approximately, 50% US-born and 50% foreign-born Latinas which allowed us to explore specific stressors related to this population. Finally, this study was able to evaluate distinct pandemic episodes in Los Angeles, providing the opportunity to explore the impacts of specific COVID-19 timepoints on postpartum stressors.
This study has some limitations. Since the PIPES questionnaire was administered at a single timepoint within the MADRES cohort study, we were unable to explore changes in PIPES scores within participants across timepoints. This study also had a small sample size, particularly for the early and later pandemic periods, given that the analysis was performed on an existing cohort which constrained our sample size to the number of participants who had already completed the questionnaire prior to the time of analysis. This likely limited statistical power to detect significant differences in the threat to family subscale during the early pandemic period and across all subscales during the later pandemic period. However, despite these small sample sizes, we observed significantly elevated scores in perceived discrimination, social isolation, and total PIPES scores during the early pandemic period relative to the pre-pandemic period. Another limitation is that although we adjusted for various possible confounders in our analysis, it is possible that there was still some residual confounding in our results. For example, important demographic variables, such as education, varied by COVID-19 pandemic timepoint, with participants who responded during the early pandemic having higher education levels. This may have occurred by chance or as a result of lower participation during more stressful pandemic periods. Regardless, we adjusted for education and income in our models to account for these differences. An additional limitation is that various historical and political events occurred alongside the pandemic and resulted in heightened racism; therefore, it was impossible to separate entirely the early social isolation period of the pandemic from the various sociopolitical events to assess their independent effects, particularly given our small sample sizes. Furthermore, although the PIPES questionnaire was originally intended for use among immigrant Latinos, both foreign-born and US-born Latina postpartum women were administered the questionnaire. However, many US Hispanic families have mixed documentation status which could similarly result in unique immigration stressors and concerns about their family. 37 In addition, anti-immigration policies and rhetoric have been found to impact the overall mental health of Hispanic/Latino US residents independent of nativity or immigration status. 38
Conclusion
This study found higher perceived discrimination, social isolation, and total PIPES scores at 1 month postpartum during the early COVID-19 pandemic period when compared to the pre-pandemic period. These results suggest increased social inequities during the pandemic among US Hispanic/Latina women, stressing the importance of understanding the possible health implications of these unique stressors in Hispanic/Latina women and their children.
Supplemental Material
Supplemental material, sj-docx-1-whe-10.1177_17455057221125103 for Perceived vulnerability to immigration policies among postpartum Hispanic/Latina women in the MADRES pregnancy cohort before and during the COVID-19 pandemic by Ixel Hernandez-Castro, Claudia M Toledo-Corral, Thomas Chavez, Rima Habre, Brendan Grubbs, Laila Al-Marayati, Deborah Lerner, Nathana Lurvey, Isabel Lagomasino, Sandrah P Eckel, Genevieve F Dunton, Shohreh F Farzan, Carrie V Breton and Theresa M Bastain in Women’s Health
Acknowledgments
The authors are indebted to the MADRES study families, nurses, midwives, physicians, and staff at each of our study sites for their cooperation and participation, and especially to the members of the MADRES study team for their efforts to improve the health of underserved communities.
Footnotes
ORCID iD: Ixel Hernandez-Castro  https://orcid.org/0000-0002-4572-4163
https://orcid.org/0000-0002-4572-4163
Supplemental material: Supplemental material for this article is available online.
Declarations
Ethics approval and consent to participate: Written informed consent was obtained at study entry for each participant and the study was approved by the University of Southern California’s Institutional Review Board (ethics approval number= HS-15-00498).
Consent for publication: Not applicable.
Author contribution(s): Ixel Hernandez-Castro: Formal analysis; Writing – original draft; Writing – review & editing.
Claudia M Toledo-Corral: Conceptualization; Writing – review & editing.
Thomas Chavez: Data curation; Writing – review & editing.
Rima Habre: Conceptualization; Funding acquisition; Writing – review & editing.
Brendan Grubbs: Conceptualization; Writing – review & editing.
Laila Al-Marayati: Conceptualization; Writing – review & editing.
Deborah Lerner: Conceptualization; Writing – review & editing.
Nathana Lurvey: Conceptualization; Writing – review & editing.
Isabel Lagomasino: Conceptualization; Writing – review & editing.
Sandrah P Eckel: Conceptualization; Writing – review & editing.
Genevieve F Dunton: Conceptualization; Writing – review & editing.
Shohreh F Farzan: Conceptualization; Writing – review & editing.
Carrie V Breton: Conceptualization; Funding acquisition; Methodology; Writing – review & editing.
Theresa M Bastain: Conceptualization; Funding acquisition; Methodology; Supervision; Writing – review & editing.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This work was supported by the Maternal and Developmental Risks from Environmental and Social Stressors (MADRES) Center (grant nos. P50ES026086, 83615801-0, and P50MD015705) funded by the National Institute of Environmental Health Sciences, the National Institute for Minority Health and Health Disparities and the Environmental Protection Agency; the Southern California Environmental Health Sciences Center (grant no. P30ES007048) funded by the National Institute of Environmental Health Sciences, and the Lifecourse Approach to Developmental Repercussions of Environmental Agents on Metabolic and Respiratory health (LA DREAMERs) (grant no. UH3OD023287) funded by the National Institutes of Health Office of the Director ECHO Program.
Competing interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of data and materials: The datasets generated and/or analyzed during the current study are not publicly available due to participant confidentiality but are available from the corresponding author on reasonable request.
References
- 1. Salari N, Hosseinian-Far A, Jalali R, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health 2020; 16: 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Shaw B, Daskareh M, Gholamrezanezhad A. The lingering manifestations of COVID-19 during and after convalescence: update on long-term pulmonary consequences of coronavirus disease 2019 (COVID-19). Radiol Med 2021; 126(1): 40–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hertz-Palmor N, Moore TM, Gothelf D, et al. Association among income loss, financial strain and depressive symptoms during COVID-19: evidence from two longitudinal studies. J Affect Disord 2021; 291: 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Decerf B, Ferreira FHG, Mahler DG, et al. Lives and livelihoods: estimates of the global mortality and poverty effects of the Covid-19 pandemic. World Dev 2021; 146: 105561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Couch KA, Fairlie RW, Xu H. The impacts of COVID-19 on minority unemployment: first evidence from April 2020 CPS microdata. NBER working paper no. 27246, May 2020, Cambridge, MA: NBER. [Google Scholar]
- 6. Lu Y, Kaushal N, Huang X, et al. Priming COVID-19 salience increases prejudice and discriminatory intent against Asians and Hispanics. Proc Natl Acad Sci U S A 2021; 118: e2105125118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Singu S, Acharya A, Challagundla K, et al. Impact of social determinants of health on the emerging COVID-19 pandemic in the United States. Front Public Health 2020; 8: 406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Reitsma MB, Claypool AL, Vargo J, et al. Racial/ethnic disparities in COVID-19 exposure risk, testing, and cases at the subcounty level in California. Health Aff 2021; 40(6): 870–878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Lo CH, Nguyen LH, Drew DA, et al. Race, ethnicity, community-level socioeconomic factors, and risk of COVID-19 in the United States and the United Kingdom. EClinicalMedicine 2021; 38: 101029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Sze S, Pan D, Nevill CR, et al. Ethnicity and clinical outcomes in COVID-19: a systematic review and meta-analysis. EClinicalMedicine 2020; 29–30: 100630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jamieson T, Caldwell D, Gomez-Aguinaga B, et al. Race, ethnicity, nativity and perceptions of health risk during the COVID-19 pandemic in the US. Int J Environ Res Public Health 2021; 18: 11113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Oaten M, Stevenson RJ, Case TI. Disease avoidance as a functional basis for stigmatization. Philos Trans R Soc Lond B Biol Sci 2011; 366: 3433–3452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Santos HP, Adynski H, Harris R, et al. Biopsychosocial correlates of psychological distress in Latina mothers. J Affect Disord 2021; 282: 617–626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Wouk K, Morgan I, Johnson J, et al. A systematic review of patient-, provider-, and health system-level predictors of postpartum health care use by people of color and low-income and/or uninsured populations in the United States. J Womens Health 2021; 30(8): 1127–1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Ryan D, Tornberg-Belanger SN, Perez G, et al. Stress, social support and their relationship to depression and anxiety among Latina immigrant women. J Psychosom Res 2021; 149: 110588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Hessami K, Romanelli C, Chiurazzi M, et al. COVID-19 pandemic and maternal mental health: a systematic review and meta-analysis. J Matern Neonatal Med 2020; 1–8: 4014–4021. [DOI] [PubMed] [Google Scholar]
- 17. Mollard E, Kupzyk K, Moore T. Postpartum stress and protective factors in women who gave birth in the United States during the COVID-19 pandemic. Womens Health 2021; 17: 17455065211042190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Perzow SED, Hennessey EP, Hoffman MC, et al. Mental health of pregnant and postpartum women in response to the COVID-19 pandemic. J Affect Disord Rep 2021; 4: 100123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Suárez-Rico BV, Estrada-Gutierrez G, Sánchez-Martínez M, et al. Prevalence of depression, anxiety, and perceived stress in postpartum Mexican women during the COVID-19 lockdown. Int J Environ Res Public Health 2021; 18: 4627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Vigod SN, Brown HK, Huang A, et al. Postpartum mental illness during the COVID-19 pandemic: a population-based, repeated cross-sectional study. CMAJ 2021; 193: E835–E843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gur RE, White LK, Waller R, et al. The disproportionate burden of the COVID-19 pandemic among pregnant black women. Psychiatry Res 2020; 293: 113475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Iyengar U, Jaiprakash B, Haitsuka H, et al. One year into the pandemic: a systematic review of perinatal mental health outcomes during COVID-19. Front Psychiatry 2021; 12: 674194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hibel LC, Boyer CJ, Buhler-Wassmann AC, et al. The psychological and economic toll of the COVID-19 pandemic on Latina mothers in primarily low-income essential worker families. Traumatology 2021; 27: 40–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Lara-Cinisomo S, Fujimoto EM, Oksas C, et al. Pilot study exploring migration experiences and perinatal depressive and anxiety symptoms in immigrant Latinas. Matern Child Health J 2019; 23(12): 1627–1647. [DOI] [PubMed] [Google Scholar]
- 25. Glynn LM, Davis EP, Sandman CA. New insights into the role of perinatal HPA-axis dysregulation in postpartum depression. Neuropeptides 2013; 47(6): 363–370. [DOI] [PubMed] [Google Scholar]
- 26. McEwen BS. Stress, adaptation, and disease. Allostasis and allostatic load. Ann N Y Acad Sci 1998; 840: 33–44. [DOI] [PubMed] [Google Scholar]
- 27. Letourneau NL, Dennis CL, Benzies K, et al. Postpartum depression is a family affair: addressing the impact on mothers, fathers, and children. Issues Ment Health Nurs 2012; 33(7): 445–457. [DOI] [PubMed] [Google Scholar]
- 28. Lutkiewicz K, Bieleninik Cieślak ŁM, et al. Maternal-infant bonding and its relationships with maternal depressive symptoms, stress and anxiety in the early postpartum period in a polish sample. Int J Environ Res Public Health 2020; 17: 5427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kingston D, Tough S, Whitfield H. Prenatal and postpartum maternal psychological distress and infant development: a systematic review. Child Psychiatry Hum Dev 2012; 43(5): 683–714. [DOI] [PubMed] [Google Scholar]
- 30. Preciado A, D’Anna-Hernandez K. Acculturative stress is associated with trajectory of anxiety symptoms during pregnancy in Mexican-American women. J Anxiety Disord 2017; 48: 28–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Howell EA, Mora PA, Horowitz CR, et al. Racial and ethnic differences in factors associated with early postpartum depressive symptoms. Obstet Gynecol 2005; 105(6): 1442–1450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Bastain TM, Chavez T, Habre R, et al. Study design, protocol and profile of the Maternal and Developmental Risks from Environmental and Social Stressors (MADRES) pregnancy cohort: a prospective cohort study in predominantly low-income Hispanic women in urban Los Angeles. BMC Pregnancy and Childbirth 2019; 19: 189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Allison KC, Wenzel A, Kleiman K, et al. Development of a brief measure of postpartum distress. J Womens Health 2011; 20(4): 617–623. [DOI] [PubMed] [Google Scholar]
- 34. Ayón C. Perceived immigration policy effects scale: development and validation of a scale on the impact of state-level immigration policies on Latino immigrant families. Hispanic J Behav Sci 2016; 39: 19–33. [Google Scholar]
- 35. Health CoLAP. Los Angeles county announces first death related to 2019 novel coronavirus (COVID-19)- public health confirms first death from COVID-19 and six additional cases in Los Angeles county, http://publichealth.lacounty.gov/phcommon/public/media/mediapubhpdetail.cfm?prid=2261
- 36. Gov C. Office of governor Gavin Newsom 2022, https://www.gov.ca.gov/2020/08/28/governor-newsom-unveils-blueprint-for-a-safer-economy-a-statewide-stringent-and-slow-plan-for-living-with-covid-19/ [Google Scholar]
- 37. Taylor P, Lopez M, Passel J, Motel S. Unauthorized immigrants: length of residency, patterns of parenthood. 2011. Pew research center, https://www.pewresearch.org/hispanic/wp-content/uploads/sites/5/2011/12/Unauthorized_Characteristics.pdf [Google Scholar]
- 38. Pinedo M, Valdez CR. Immigration enforcement policies and the mental health of US citizens: findings from a comparative analysis. Am J Community Psychol 2020; 66(1–2): 119–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Conzo P, Fuochi G, Anfossi L, et al. Negative media portrayals of immigrants increase ingroup favoritism and hostile physiological and emotional reactions. Sci Rep 2021; 11: 16407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Vernice NA, Pereira NM, Wang A, et al. The adverse health effects of punitive immigrant policies in the United States: a systematic review. Plos One 2020; 15(12): e0244054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hatzenbuehler ML, Prins SJ, Flake M, et al. Immigration policies and mental health morbidity among Latinos: a state-level analysis. Soc Sci Med 2017; 174: 169–178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Pineros-Leano M, Yao L, Simonovich SD, et al. “I don’t have time to be sad”: experiences and perceptions of sadness among Latina mothers. Soc Work 2021; 66: 119–127. [DOI] [PubMed] [Google Scholar]
- 43. Molina KM, Little TV, Rosal MC. Everyday discrimination, family context, and psychological distress among Latino adults in the United States. J Community Psychol 2016; 44: 145–165. [Google Scholar]
- 44. Heilemann MV, Coffey-Love M, Frutos L. Perceived reasons for depression among low income women of Mexican descent. Arch Psychiatr Nurs 2004; 18(5): 185–192. [DOI] [PubMed] [Google Scholar]
- 45. Becerra D, Hernandez G, Porchas F, et al. Immigration policies and mental health: examining the relationship between immigration enforcement and depression, anxiety, and stress among Latino immigrants. J Ethn Cult Divers Soc Work 2020; 29: 43–59. [Google Scholar]
- 46. Barba-Müller E, Craddock S, Carmona S, et al. Brain plasticity in pregnancy and the postpartum period: links to maternal caregiving and mental health. Arch Womens Ment Health 2019; 22(2): 289–299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Gammie SC, Driessen TM, Zhao C, et al. Genetic and neuroendocrine regulation of the postpartum brain. Front Neuroendocrinol 2016; 42: 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Liu J, Hung P, Alberg AJ, et al. Mental health among pregnant women with COVID-19–related stressors and worries in the United States. Birth 2021; 48(4): 470–479. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Levine JW, Ferrer P, De Witte AJ, et al. The association between social support and psychological distress in Latina mothers living in Miami-Dade County, Florida. Cureus 2020; 12: e10848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Williams DR, Lawrence JA, Davis BA, et al. Understanding how discrimination can affect health. Health Serv Res 2019; 54(Suppl. 2): 1374–1388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Janevic T, Maru S, Nowlin S, et al. Pandemic birthing: childbirth satisfaction, perceived health care bias, and postpartum health during the COVID-19 pandemic. Matern Child Health J 2021; 25(6): 860–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-whe-10.1177_17455057221125103 for Perceived vulnerability to immigration policies among postpartum Hispanic/Latina women in the MADRES pregnancy cohort before and during the COVID-19 pandemic by Ixel Hernandez-Castro, Claudia M Toledo-Corral, Thomas Chavez, Rima Habre, Brendan Grubbs, Laila Al-Marayati, Deborah Lerner, Nathana Lurvey, Isabel Lagomasino, Sandrah P Eckel, Genevieve F Dunton, Shohreh F Farzan, Carrie V Breton and Theresa M Bastain in Women’s Health