Abstract
Objectives
To examine the views and experiences of community pharmacists in Northern Ireland (NI) regarding changes in community pharmacy practice/processes in preparation for, and response to, the COVID-19 pandemic.
Design
Cross-sectional telephone-administered questionnaire.
Setting and participants
Geographically stratified representative sample of 130 community pharmacists in NI between March and May 2021.
Outcome measures
Community pharmacists’ responses to questions focusing on their preparation, experience and response to the COVID-19 pandemic. Descriptive analysis was conducted including frequencies and percentages. Free-text comments were summarised using thematic analysis.
Results
One hundred and thirty pharmacists completed the questionnaire. Pharmacists responded comprehensively to implementing infection control measures, for example, management of social distancing in the shop (96.2%), making adjustments to premises, for example, barriers/screens (95.4%), while maintaining medicines supply (100.0%) and advice to patients (93.1%). Newly commissioned services were provided, for example, emergency supply service (93.1%), influenza vaccination for healthcare workers (77.7%) and volunteer deliveries to vulnerable people (54.6%). Pharmacists were least prepared for the increased workload and patients’ challenging behaviour, but the majority (96.9%) reported that they felt better prepared during the second wave. Pharmacists agreed/strongly agreed that they would be able to re-establish normal services (87.7%), were willing to administer COVID-19 vaccines (80.7%) and provide COVID-19 testing (60.8%) in the future.
Conclusions
Community pharmacists remained accessible and maintained supply of essential medicines and advice to patients throughout the pandemic. Provision of modified and additional services such as vaccination reinforced the clinical and public health role of pharmacy
Keywords: COVID-19, Quality in health care, PRIMARY CARE
STRENGTHS AND LIMITATIONS OF THIS STUDY
Large representative sample of community pharmacists attained.
Method of questionnaire administration ensured there was very little missing data.
Focus on Northern Ireland making the results less generalisable.
Method of questionnaire administration limited the number of pharmacists who could be contacted due to time and resource constraints.
Introduction
Since March 2020, healthcare provision has faced one of its greatest challenges in responding to the COVID-19 pandemic. Health services have been under immense pressure to provide information, prevent and manage COVID-19 infection and deal with the long-term sequalae of infection, while trying to maintain care for other patients with acute and long-term conditions. Community pharmacy is one of the most accessible health sectors and has played a vital front-line role during key stages of the current COVID-19 pandemic (ie, prevention, preparedness, response and recovery).1–4 However, community pharmacy had to markedly adapt its usual working practices.
Community pharmacies typically provide a wide range of core services (eg, dispensing, supply of over the counter medication and health promotion activities), with some providing locally commissioned services (eg, smoking cessation) that are delivered by choice or driven by local need. At the outset of the pandemic, the commissioners stood down a number of additional patient-facing services, for example, medicines use reviews; some of these were reintroduced at a later date, for example, Minor Ailments and Smoking Cessation (September 2020) with appropriate COVID-safe modifications. Most of the non-core services were stood down during March–May 2020, with the notable exception of needle and syringe exchange services, which were modified to reduce the COVID-19 transmission risk.5
Amid the restrictions imposed following the onset of the pandemic, community pharmacy was deemed an essential service that reflects the importance of medicine-taking in everyday life,6 especially at a time when other services were not readily accessible.2 4 Governments and professional organisations in various countries have specifically acknowledged the need to support and maximise pharmacy as a resource in maintaining delivery of patient care.7
As society begins to emerge from the worst of the pandemic, it is important to learn from the experience so that health services can appropriately prepare for the next pandemic or emergency health crisis. This requires a consideration of the experiences of healthcare professionals who have worked during COVID-19. A three-phase research project was undertaken in Northern Ireland (NI) to assess community pharmacy’s preparedness for and response to the pandemic, using Donabedian’s overarching three-pillar model of quality of care: structure, process and outcome.8 Phase 1 (representing structure) was a documentary analysis of guidance and policy documents released over the initial months of the pandemic,5 this current paper describes the findings of a telephone-administered questionnaire with community pharmacist participants (phase 2, process) while phase 3 was a series of semistructured interviews with community pharmacists and key stakeholders (outcomes).9 The aim of this study was to examine the immediate views and experiences of the community pharmacy workforce in NI regarding changes in community pharmacy practice/processes in preparation for, and response to the COVID-19 pandemic.
Method
A cross-sectional study was undertaken involving administration of a brief telephone questionnaire with community pharmacists in NI to examine their immediate views and experiences of changes in community pharmacy practice/processes in preparation for, and in response to, COVID-19.
Patient and public involvement
Two patient and public involvement representatives were recruited to the Study Advisory Group via the Patient Involvement Enhancing Research NI network from the Health and Social Care Research and Development division. The Study Advisory Group also included members of the pharmacy profession representing practice, regulation and professional advocacy, along with a methodological advisor. The group contributed to the development of the telephone questionnaire (see below) and advised on other aspects of the study, including providing commentary on the findings.
Questionnaire development
The telephone questionnaire was developed based on documentary analysis of key policy publications from health policy, commissioning and professional organisations in NI, and relevant literature describing a framework of activities that pharmacy personnel can undertake in preparation/response to crises such as COVID-19.10 11 The questionnaire included items on demographics, followed by six main sections encompassing community pharmacists’ experiences of working during the pandemic and specifically during March–May 2020 (wave 1) and September–December 2020 (wave 2), that is: (1) prevention of infection spread, (2) maintaining pharmacy services, (3) preparedness for and response to the COVID-19 pandemic, (4) communicating with others (5) updating professional knowledge and (6) looking to the future. To minimise the impact of administering the questionnaire on daily practice, the content was designed to ensure that the questionnaire was concise. Respondents could skip any questions that they preferred not to answer. It was piloted with volunteer community pharmacists (n=5) to assess face and content validity and was refined on the basis of their responses. This piloting indicated that completion time for the questionnaire was approximately 15 min. Pilot responses were not included in the final analysis. A copy of the questionnaire is provided in online supplemental file 1.
bmjopen-2022-064545supp001.pdf (1.5MB, pdf)
Sampling
A purposive and geographically stratified sample of community pharmacists was recruited for the study. Using the publicly available information on contact details of registered pharmacies in NI, community pharmacies were stratified according to Local Commissioning Group (LCG) areas, of which there are five. LCGs commission health and social care services based on the needs of local populations. The numbers sampled were in proportion to the number of registered pharmacies in each locality to ensure representation across NI.
In November 2020, there were 528 community pharmacies in NI. In order to attain a statistically representative sample of pharmacists across NI, and to estimate the percentage response to any questions in the questionnaire with a 95% confidence level to within ±7.5% (ie, a 95% confidence level to within ±7.5% of any questionnaire responses), a sample of n=130 respondents to the questionnaire was required. Based on the total number of pharmacies across NI (n=528) and an anticipated response rate of 30%, up to a maximum number of 433 pharmacies were contacted (from the 528) to achieve the required sample size (n=130). This equated to a sampling fraction of 24% of the total number of pharmacies. Within each LCG area, a random list of pharmacies was generated. Pharmacies were telephoned sequentially in each LCG area by the researcher (SMP) using the random list until the required number within each LCG area was achieved.
Recruitment and consent
To raise awareness in advance of recruitment, summary information about the study was made available to all community pharmacies through a number of pharmacy organisations, for example, pharmacy forum, community pharmacy NI, with close links with the community pharmacy sector.
Pharmacies were contacted by telephone in random order across the LCGs by the researcher (SMP). SMP briefly outlined the study and referred to the summary information circulated to pharmacies in advance to determine if a pharmacist would be interested in taking part. SP advised that the questionnaire would take approximately 15 min to complete. Community pharmacists were offered the opportunity to complete the questionnaire during the telephone call or to arrange a later time and date that was more convenient. Further information about the study, if requested, was provided via email. Community pharmacists interested in taking part were asked to provide verbal consent over the telephone; this was documented and audiorecorded. The explicit yes/no responses for consent were documented on the telephone questionnaire form. The records of consent were stored separately from the completed questionnaire responses.
Data collection
A unique study ID number was assigned to each community pharmacist participant and recorded on a hard copy of the questionnaire. The study IDs were stored in a password-protected Microsoft Excel spreadsheet which acted as a log, linking ID numbers to respondents known only to the researcher and stored on the researcher’s secure and password-protected laptop. Verbal responses to the questions were recorded by the researcher (SMP) on the form. If the community pharmacist was interrupted during the questionnaire data collection, they were asked if they were willing to complete the questionnaire at a later time and an appointment was arranged. All participants completed the questionnaire only once.
Data analysis
Data were analysed descriptively using SPSS V.27,12 reporting frequencies, percentages and 95% CIs. Free-text responses to questions were recorded, and grouped into broad themes.
Results
During March–May 2021, the researcher initially invited 175 community pharmacists. Just under 80% (79.4%; n=139) of community pharmacists agreed to participate and 74.3% (n=130) completed the questionnaire by telephone with the researcher (representing 130 pharmacies). Nine community pharmacists were unable to complete the survey due to interruptions during administration and could not be contacted again. Completion of the telephone questionnaires took 46 working days, with 62.9% (n=110) community pharmacists deferring the call to another day due to work pressures at the time of the arranged call.
The demographic characteristics of the 130 participating community pharmacists are reported in table 1 and the characteristics of the pharmacies in which they worked are reported in table 2. There was a higher percentage (55.4%; n=72) of pharmacist respondents who were female, most participants were aged between 25 and 54 years old, and 36.2% (n=47) been in practice for more than 11 years. The majority of respondents were employees (80.8%; n=105) and just over 50% (51.5%; n=67) were dispensary managers. The pharmacies in which the respondents worked were located in largely urban (43.1%; n=56) or suburban settings (37.7%; n=38); just over 30% (32.3%; n=42) were independently owned and 38.5% (n=50) were part of a large chain (group of more than 20 pharmacies).
Table 1.
Demographic characteristics of community pharmacists who completed the telephone questionnaire
| Characteristic | n (%) |
| Gender | |
| Female | 72 (55.4) |
| Male | 58 (44.6) |
| Age | |
| < 25 years | 6 (4.6) |
| 25–34 years | 53 (40.8) |
| 35–44 years | 38 (29.2) |
| 45–54 years | 21 (16.2) |
| ≥ 55 years | 12 (9.2) |
| No of years in community pharmacy practice | |
| ≤ 5 years | 36 (27.7) |
| 6–10 years | 22 (16.9) |
| 11–15 years | 25 (19.2) |
| ≥ 15 years | 47 (36.2) |
| Status | |
| Owner/contractor | 25 (19.2) |
| Employee | 105 (80.8) |
| Usual role | |
| Owner manager | 17 (13.1) |
| Responsible pharmacist | 12 (9.2) |
| Dispensary manager | 67 (51.5) |
| Locum pharmacist | 13 (10.0) |
| Pharmacist team member | 15 (11.5) |
| Superintendent | 6 (4.6) |
| Shielding during wave 1* | 8 (6.2) |
*Measures taken by those at highest risk of severe illness from COVID-19 (eg, self-isolation).
Table 2.
Characteristics of participating community pharmacies
| Geographical location (LCG area) | n (%) |
| Belfast | 32 (24.6) |
| Northern | 28 (21.5) |
| South-Eastern | 24 (18.5) |
| Southern | 22 (16.9) |
| Western | 24 (18.5) |
| Location type | |
| Urban | 56 (43.1) |
| Rural | 36 (27.7) |
| Suburban | 38 (29.2) |
| Pharmacy type | |
| Independent | 42 (32.3) |
| Small chain <5 | 18 (13.8) |
| Medium chain 5–20 | 20 (15.4) |
| Large chain >20 | 50 (38.5) |
LCG, Local Commissioning Group.
Preventing the spread of COVID-19
During the first wave, the most common measure was the management of social distancing in the pharmacy (96.2%; n=125), including one-way systems, limiting capacity within the pharmacy and queue management (table 3). Adjustments, such as the erection of barriers or screens, were made to premises in 95.4% (n=124) of pharmacies to reduce the risk of contact between staff and patients. Cleaning and disinfection of premises became a routine task during the pandemic first wave, implemented in 93.8% (n=122) of pharmacies and performed at least twice a day in most. Public health information was displayed in 92.3% (n=120) pharmacies, using materials from the public health campaigns that focused on COVID-19-related issues.
Table 3.
Measures taken during the onset of the pandemic (March–May 2020) to prevent the spread of COVID-19 in community pharmacies
| Prevention of infection measures | Implemented in March–May 2020 |
Stopped in June–August 2020 |
Started at a later date (after September 2020) n (%) |
||
| Yes n (%) | No n (%) | Yes n (%) | No n (%) | ||
| Management of social distancing | 125 (96.2) | 5 (3.8) | * | 122 (93.8) | * |
| Premises adjustments such as barriers, screens | 124 (95.4) | 6 (4.6) | 115 (88.5) | 9 (6.9) | 5 (3.8) |
| Protocols for disinfection of pharmacy surfaces | 122 (93.8) | 8 (6.2) | 5 (3.8) | 122 (93.8) | 0 (0.0) |
| Public health information on preventing COVID-19 displayed | 120 (92.3) | 10 (7.7) | * | 119 (91.5) | * |
| Reduced face-to-face contact | 120 (92.3) | 10 (7.7) | 6 (4.6) | 116 (89.2) | 0 (0.0) |
| Lunchtime closing | 119 (91.5) | 11 (8.5) | 63 (48.5) | 55 (42.3) | * |
| Use of PPE by pharmacy staff | 115 (88.5) | 15 (11.5) | * | 116 (89.2) | 11 (8.5) |
| Changes to the use of the available space | 98 (75.4) | 32 (24.6) | 7 (5.4) | 92 (70.8) | * |
| Shorter opening hours | 87 (66.9) | 43 (33.1) | 69 (53.1) | 17 (13.1) | 0 (0.0) |
| Changes to staff working patterns | 64 (49.2) | 66 (50.8) | 9 (6.9) | 57 (43.8) | * |
*Not reported as less than 5, and potentially identifiable
PPE,personal protective equipment.
During the first wave, 88.5% (n=115), community pharmacists reported that staff were using personal protective equipment (PPE). When asked for further comments, pharmacists reported how government advice on PPE had changed and there was conflicting advice from other sources. Community pharmacists were concerned about protecting their staff, especially those with vulnerable family members and some introduced early protection measures, for example, making visors when PPE was in short supply, ensuring adequate ventilation, setting up dispensary workstations two metres apart and asking delivery drivers to wear protective clothing.
Many pharmacies (75.4%; n=98) closed the shop floor space entirely or reduced it and reused the space to prepare and check prescriptions, monitored dosage system boxes and orders for delivery. Working patterns and break times were changed in 49.2% (n=64) pharmacies to reduce the number of staff working at any one time. Many staff worked longer hours and started early to manage the increased volume of prescriptions. Many of the changes outlined in table 4 were maintained over the time periods assessed, except lunchtime closing, which was stopped in almost 50% of pharmacies (48.5% n=63) in June–August 2020.
Table 4.
Newly commissioned services and community pharmacy initiatives during the COVID-19 pandemic.
| New services or initiatives | Implemented in March–May 2020 n (%) |
Stopped in June–August 2020 n (%) |
Started at a later date n (%) |
||
| Yes | No | Yes | No | ||
| Emergency supply during a pandemic service | 121 (93.1) | 9 (6.9) | * | 117 (90.0) | 0 (0.0) |
| Influenza vaccination service (front-line health and social care workers) | 101 (77.7) | 29 (22.3) | 101 (77.7) | 0 (0.0) | 0 (0.0) |
| Situation reporting (staffing/stock) to the health and social care board | 74 (56.9) | 56 (43.1) | 10 (7.7) | 64 (49.2) | 0 (0.0) |
| Measures to flag/assist patients with sensitive issues such as domestic violence reporting | 73 (56.2) | 57 (43.8) | 0 (0.0) | 73 (56.2) | 6 (4.6) |
| Prescription delivery by volunteers in the local community | 71 (54.6) | 59 (45.4) | 32 (24.6) | 39 (30.0) | 0 (0.0) |
| Referrals to test and trace services | 70 (53.8) | 60 (46.2) | * | 68 (52.3) | 0 (0.0) |
| Employment of additional staff, for example, dentists, volunteers, students, retired pharmacists | 49 (37.7) | 81 (62.3) | 22 (16.9) | 27 (20.8) | 0 (0.0) |
| Drive-through (or equivalent) pharmacy services | 33 (25.4) | 97 (74.6) | * | 32 (24.6) | 0 (0.0) |
| Replenishment of care home pandemic packs | 19 (14.6) | 107 (82.4) | * | 15 (11.5) | * |
| Palliative care on-call services | 19 (14.6) | 111 (85.4) | * | 17 (13.1) | 0 (0.0) |
| Supply of medicines usually supplied in the hospital setting (eg, oncology, antiretroviral drugs, ‘Healthcare at Home’) | 11 (8.5) | 119 (91.5) | 0 (0.0) | 11 (8.5) | 0 (0.0) |
| Medicines delivery service (to vulnerable people) (commissioned September 2020) | n/a | n/a | n/a | n/a | 95 (73.1) |
*Not reported as less than 5, and potentially identifiable.
Maintaining pharmacy services during the pandemic
Core pharmacy services, principally dispensing, continued to be provided from all pharmacies throughout March–December 2020, while over-the-counter medicines advice and supply were available from 128 (98.5%) and 121 (93.1%) pharmacies, respectively (table 4). Prescription collection and delivery services were maintained (and increased) by the majority of pharmacies (95.4%; n=124 and 88.5%; n=115, respectively). Of the 84 (64.6%) pharmacies that provided out-of-hours dispensing services, two stopped service provision during March-May 2020 and one restarted with a modified service during September–December 2020. Some pharmacies did not restart services until September–December 2020 and then provided them in a modified format, for example, nursing home advice was provided by telephone or videocall by 12 (9.2%) pharmacies during wave 2. All participating pharmacies, except one, normally provided Living Well campaigns (provision of key public health messages and advice through community pharmacies); 55 (42.3%) stopped this service at the onset of the pandemic, but by June–August 2020, 44 (33.8%) had restarted modified campaigns providing COVID-19 information to the public.
Just over 70% (71.5%; n=93) of community pharmacies stopped smoking cessation services, 56.2% (n=73) restarted the service during June-August 2020 and 16.1% (n=21) reported providing a modified service by September–December 2020. Pharmacists reported that opioid substitution treatment supervision was initially stopped, but then as patients’ needs were reassessed, it was recommenced in a modified format, for example, increased supervision by addiction team staff. Most private travel vaccination services did not restart as there was little demand for them.
During the pandemic, a number of new services were commissioned and provided by community pharmacies. In addition, many new initiatives were undertaken as the pandemic progressed such as ‘drive-through’ pharmacies or the equivalent such as ‘call and collect’ and measures to flag/assist patients with sensitive issues such as domestic violence reporting. The new services/initiatives and their status over time are presented in table 4.
The Emergency Supply Service (allowing a month’s supply of medicines to be provided in the absence of a prescription) was widely implemented from the onset of the pandemic. It was initially provided by 93.1% (n=121) of community pharmacies, four of whom stopped provision in June-August 2020. Pharmacists commented that this was due to an inappropriately excessive demand for pain medication in urban areas. The ‘influenza vaccination campaign was provided by 77.7% (n=101) of community pharmacies. Only 56.9% (n=74) reported participation in the Situation Reporting scheme (updating health officials on staffing and stock issues) and 56.2% (n=73) implemented measures to flag domestic violence (‘Ask for ANI’ initiative). Almost 55% (54.6%; n=71) used volunteer delivery services but by June–August 2020, 24.6% (n=32) had stopped and by September–December 2020, 73.1% (n=95) of pharmacies had switched to commissioned Home Delivery services. From free-text comments, pharmacists commented that the volunteer services were invaluable but that in some cases, they had encountered problems with insurance and confidentiality issues.
Preparedness for and response to the COVID-19 pandemic
Pharmacists were asked to recall the initial outbreak of the pandemic (March–May 2020) and to reflect on their level of preparedness. The responses are shown in table 5 and illustrate the changes in preparedness over time. Initially, 74.6% (n=97) of pharmacies reported having had appropriate working patterns in place and 66.2% (n=86) had sufficient PPE available for staff at the onset of the pandemic, but after 6 months, this increased to 95.4% (n=124) and 99.2% (n=129), respectively. Increases were also seen over the time period in the number of pharmacies reporting that business continuity plans were in place in their premises for prolonged staff absences or for the eventuality of pharmacy closure. Employee pharmacists in pharmacy multiples reported that they did not know or were unsure about the existence of business continuity plans or financial resources available during the pandemic, for example, 54 (41.5%) were unaware of financial resources during March–May 2020. Pharmacies having sufficient information about PPE increased from 53.1% (n=69) during March–May 2020 to 99.2% (n=129) in September–December 2020, reflecting the increasing amount of advice relevant to community pharmacy available from Public Health England and the Department of Health in NI. Sufficient stocks and supplies of medicines and hand sanitisers increased over the same time periods from 65.4% (n=85) to 94.6% (n=123) and 35.4% (n=46) to 99.2% (n=129), respectively.
Table 5.
Community pharmacists’ reflections on how prepared they felt they were for working during a pandemic
| Did you have…. | During March–May 2020 | During September–December 2020 | ||||
| Yes n (%) |
No n (%) |
Don’t know/Unsure n (%) |
Yes n (%) |
No n (%) |
Don’t know/unsure n (%) |
|
| Appropriate staff working patterns in place | 97 (74.6) | 33 (25.4) | 0 (0.0) | 124 (95.4) | 6 (4.6) | 0 (0.0) |
| Enough supply of PPE for staff | 86 (66.2) | 44 (33.8) | 0 (0.0) | 129 (99.2) | * | 0 (0.0) |
| A business continuity plan in place for use in the event of staff absence over a prolonged period | 85 (65.4) | 26 (20) | 19 (14.6) | 101 (77.7) | 10 (7.7) | 19 (14.6) |
| A business continuity plan in place for use in the event of pharmacy closure | 85 (65.4) | 21 (16.2) | 24 (18.5) | 100 (76.9) | 7 (5.4) | 23 (17.7) |
| Enough stock and supply of essential prescription and OTC medicines | 85 (65.4) | 43 (33.1) | * | 123 (94.6) | 6 (6 (4.6) | * |
| Enough information about PPE requirements for staff | 69 (53.1) | 60 (46.2) | * | 129 (99.2) | 0 (0.0) | * |
| Enough financial resources to cover the additional demands on your pharmacy business | 63 (48.5) | 13 (10.0) | 54 (41.5) | 76 (58.5) | * | 53 (40.8) |
| A system to manage quantity limits for patients for the supply of individual medicines | 56 (43.1) | 73 (56.2) | * | 38 (29.2) | 91 (70.0) | * |
| Enough stock and supply of hand sanitisers | 46 (35.4) | 83 (63.8) | * | 129 (99.2) | 1 (0.8) | 0 (0.0) |
*Not reported as less than 5, and potentially identifiable.
OTC, over-the-counter; PPE, personal protective equipment.
Pharmacists were asked (using open questions) about what single aspect of their work they felt most prepared for and what they felt least prepared for. Forty-three pharmacists commented that they felt most prepared for continuing core services, that is, normal dispensary work with the help of a good staff team (n=17) who demonstrated resilience and were able to keep going. They were least prepared for the surge in the workload and the increased demand for medicines (n=73), the behaviour (eg, aggression) exhibited by the public (n=33) and wearing PPE and dealing with the risk of COVID-19 infection (n=21).
Almost all participating pharmacists (96.9%; n=126) reported that they felt better prepared for working during the second wave of the pandemic (September–December 2020) compared with the first wave (March–May 2020).
Communicating with others during the pandemic
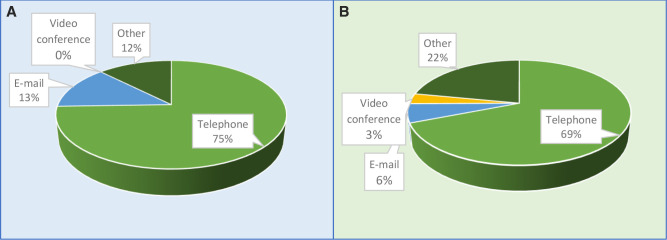
During the pandemic, 84.6% (n=110) pharmacists said that they communicated differently with general practitioner (GP) practices and 86.9% (n=113) reported communicating differently with patients during the pandemic compared with beforehand. The dominance of telephone communication is evident, representing 75% (figure 1A) and 69% (figure 1B) of the communication methods used for GPs and patients, respectively.
Figure 1.
(A) Pharmacists’ methods of communication with GP practices during the pandemic. (B) Pharmacists’ methods of communication with patients during the pandemic. GP, general practitioner.
Updating professional knowledge during the pandemic
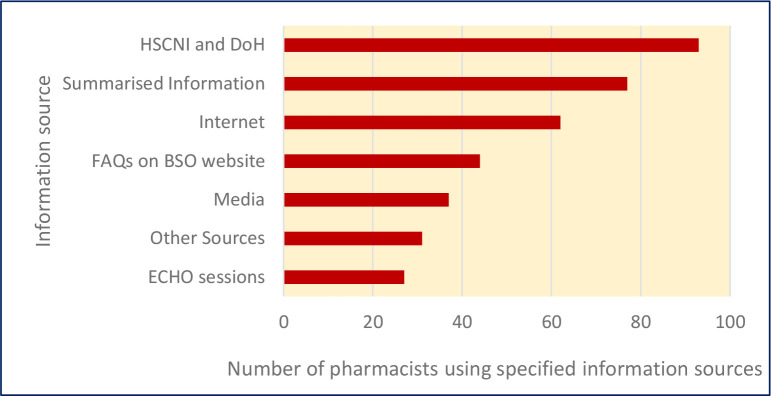
Almost 90% of community pharmacists (86.9%; n=113) reported that sufficient training resources were available to them during the pandemic to maintain their professional knowledge. The reported use of COVID-19 resources is illustrated in figure 2.
Figure 2.
COVID-19 information sources used by community pharmacists (n=130) Health and Social Care Northern Ireland (HSCNI) and department of health (DoH): Advisory letters/emails were provided regularly by the health and social care board, the department of health and related agencies. Summarised information: Distilled information provided by the contractor/head office or a professional organisation for example, community pharmacy NI, pharmacy forum. Frequently asked questions (FAQs) updated daily on the Business Services Organisation (BSO) website. ECHO sessions: Online video sessions provided by DoH and health and social care board. NI, Northern Ireland.
Other information sources used by pharmacists were online professional courses (n=20), COVID-19 vaccine training courses (n=6) and miscellaneous resources, for example, pharmacy publications. Pharmacists commented that they were overwhelmed by the volume of information (n=19), but sometimes they needed more, for example, clinical information (n=18), and that information changed frequently which was confusing (n=16).
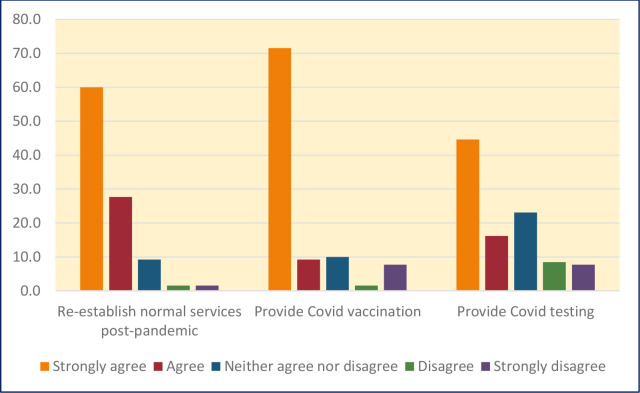
Looking to the future
Using a five-point Likert scale, pharmacists were asked for their views on three postpandemic activities, ranging from ‘strongly agree’ to ‘strongly disagree’. The activities related to re-establishing normal patient care services, COVID-19 vaccinations and COVID-19 testing. The responses are summarised in figure 3.
Figure 3.
Views of pharmacists (n=130) on selected postpandemic activities.
Almost 90% (87.7%; n=114) pharmacists agreed or strongly agreed that they would be able to establish normal patient care services postpandemic. Eighty per cent (80.7%; n=105) agreed or strongly agreed that they would be willing to provide and administer COVID-19 vaccinations when they were available through community pharmacies in NI. Sixty per cent (60.8%; n=79) agreed or strongly agreed that they would be willing to provide COVID-19 testing within the pharmacy if available in the future.
Discussion
This study has provided an overview of experience and activities of NI community pharmacists over the early waves of the pandemic. Pharmacists responded comprehensively to implementing infection control measures, while maintaining medicines supply and advice to patients and providing newly commissioned services. They were least prepared for the increased workload and patients’ challenging behaviour, but the majority reported that they felt better prepared during the second wave of the pandemic. Pharmacists agreed/strongly agreed that they would be able to re-establish normal services, were willing to administer COVID-19 vaccines and provide COVID-19 testing in the future.
In the early stages of the pandemic, pharmacies introduced a range of public health measures (social distancing, barriers, one-way systems, cleaning), and tried to provide PPE for staff. Many of these measures have been noted in other community pharmacy studies which highlighted the need to change the physical environment and protect staff as far as possible.2 13 Working patterns also changed to allow pharmacies to manage workload and to reduce the number of staff working at any one time. By introducing such measures, pharmacists were able to maintain a range of core pharmacy services. However, it was deemed necessary to discontinue some services temporarily to allow critical tasks such as dispensing to continue. There was also an increase in collection and delivery services, particularly for vulnerable patients who were not in a position to come to a pharmacy personally. In circumstances such as these, priority will be given to what is deemed essential.14
The onset of the pandemic also provided an opportunity to innovate and introduce new services. Of particular note was the widespread introduction of a new emergency supply system for medicines and a ‘influenza vaccination service specifically for front-line health workers (thus paving the way for COVID-19 vaccinations later). Many of these services reinforced the public health role of pharmacists and reflected the accessibility of the profession at a time when many other services were not available to patients.4 15
As might be expected, there was an increase in the reported perceived level of preparedness by pharmacists on most aspects of practice from March to May 2020 compared with September–December 2020. Notable increases were observed in having sufficient PPE (and relevant information) and hand sanitiser stock, and supplies of medicines. As pharmacists gained experience of working under pandemic conditions, there would have been growing awareness of where to access supplies such as PPE, and how to manage workload.2 Although they felt most prepared for maintaining core services such as dispensing, the increase in requirements for medicines and resultant increase in workload was somewhat unexpected.15 These issues have been previously reported.4 15 A time-trend analysis of data from community pharmacies in Portugal revealed an increase in the demand for medicines, and accompanying shortages in the early stages of the pandemic.16 Bhamra et al4 who undertook a cross-sectional study of a range of community pharmacy staff noted that 94% of participants reported an increase in workload, partly driven by a higher volume of medication dispensing activities.
Methods of communication needed to change with GPs and patients due to practices being closed, or patients isolating or being unable to come to the pharmacy in person. Telephone contact was the most common mode of communication. Although the use of online platforms for remote consultations has increased within general practice,17 based on the findings of this survey, this does not seem to have been replicated to the same extent in community pharmacy, and which has also been noted elsewhere.18 Carpenter et al noted that digital connectivity issues can impact on the ability to provide online consultations.18
Community pharmacists continued to maintain their professional knowledge over the course of the pandemic, largely in relation to COVID-19, using resources from the Department of Health, or professional organisations. Some pharmacists reported that the volume of information was overwhelming, contradictory or unclear, for example, advice in relation to PPE, which has been noted in other countries (eg, Netherlands, USA).2 18 The evidence base relating to COVID-19 changed rapidly, and other health professionals have reported how difficult it was to keep up-to-date.19 An important lesson for future pandemic planning is the need to rationalise the amount of information being released to healthcare professionals and to ensure consistency across different sources.
As pharmacists looked to a postpandemic future, they were confident that they could re-establish normal services, but also participate in ongoing public health efforts such as COVID-19 vaccination and testing. Indeed, the latter two activities have become part of practice, with community pharmacy making a significant contribution to the vaccination programme,20 and playing a critical role in the supply of lateral flow tests.21 22
The study has a number of strengths. We attained our target sample, and the mode of administration (which was novel in this context) ensured that there was very little missing data. The sample was stratified ensuring broad geographical representation from across NI. However, the focus on NI is one of the limitations as the findings may not be generalisable to other regions within or beyond the UK. Telephone administration also meant that we were limited in the number of pharmacists who could be contacted due to time and resource constraints. Other modes of administration of the questionnaire had been considered, for example, postal or online, but in view of the busyness of community pharmacies during the pandemic, we concluded that direct contact by telephone might yield a better response rate. Experience with postal questionnaires to community pharmacists has indicated that response rates rarely exceed 30%,23 and online response rates are also extremely variable, therefore, we feel that our choice of telephone administration is justified. The timing of administration was fortuitous as pharmacists appeared to have had sufficient time to reflect on how practice had changed over that time period. Attempting to administer the questionnaire at an earlier time point may have been difficult as pharmacists were still adjusting to new ways of working and coping with increased workload demands, which has been reported in other pharmacy studies.24
The results from this study have provided a snapshot of how pharmacy practice changed over the early phases of the COVID-19 pandemic, with essential services being maintained, other services suspended and new services being introduced. The survey aligned with the ‘process’ aspect of Donabedian’s model of quality of care, focusing on how practice (processes) had changed.8 Despite feeling unprepared during the first wave, this improved with time, which although not unexpected, appears not to have been reported before. It has been generally recognised that community pharmacy made an immense contribution to healthcare during the pandemic when many other services were not available to patients.4 25 This has been recognised by other key stakeholders (eg, other health professions, professional and governing organisations), and is reported in an accompanying paper.9 These findings need to inform ongoing and future planning for community pharmacy services, and especially in the context of another pandemic.26 Public health measures need to be instigated quickly, along with prioritisation of essential services. It may be necessary to have access to additional staff to deal with the observed increase in workload, or redeploy from sectors that are not under immediate pressure (this was done to some extent using dentists). Careful attention needs to be given to the volume and consistency of key information to avoid confusion, with greater coordination.4 27 Important lessons have been learnt as to the pressures that community pharmacists have faced, and these must be integral to future planning and implementation of services in preparation for the next crisis.4 16 25
Supplementary Material
Acknowledgments
The authors wish to acknowledge the contribution of the community pharmacists who participated in the study. We also wish to thank the members of the Study Advisory Group for their advice and support and those pharmacists who helped to pilot the questionnaire.
Footnotes
Twitter: @cathalcadogan, @pharmacoepircsi
Contributors: CC, HEB, KEB, CH: acquisition, analysis or interpretation of the data: SMP, CC, HEB, KEB, CH: manuscript drafting, revision, approval: SMP, CC, HEB, KEB, CH. Overall guarantors: CH. The guarantor accepts full responsibility for the work and/or the conduct of the study, had access to the data and controlled the decision to publish.
Funding: This work was funded by the Health and Social Care Research and Development Division of the Public Health Agency, NI, under its COVID-19 Rapid Response Funding Call (Ref. No. COM/5601/20).
Disclaimer: The content or views expressed are those of the authors/presenters and do not necessarily reflect the official views of the HSC R&D Division.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were involved in the design, or conduct, or reporting, or dissemination plans of this research. Refer to the Methods section for further details.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available on reasonable request.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study involves human participants and was approved by Name of ethics committee-Queen’s University Belfast Faculty of Medicine, Health and Life Sciences Research Ethics Committee (Ref. No. MHLS 21_21). Participants gave informed consent to participate in the study before taking part.
References
- 1.Cadogan CA, Hughes CM. On the frontline against COVID-19: community pharmacists' contribution during a public health crisis. Res Social Adm Pharm 2021;17:2032–5. 10.1016/j.sapharm.2020.03.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Koster ES, Philbert D, Bouvy ML. Impact of the COVID-19 epidemic on the provision of pharmaceutical care in community pharmacies. Res Social Adm Pharm 2021;17:2002–4. 10.1016/j.sapharm.2020.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Costa S, Romao M, Mendes M. Pharmacy interventions on COVID-19 in Europe: mapping current practices and a scoping review. Res Social Adm Pharm. 10.1016/j.sapharm.2021.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bhamra SK, Parmar J, Heinrich M. Impact of the coronavirus pandemic (COVID-19) on the professional practice and personal well-being of community pharmacy teams in the UK. Int J Pharm Pract 2021;29:556–65. 10.1093/ijpp/riab062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Barry HE, Cadogan CA, O’Reilly E, et al. Changes to community pharmacy practice during the COVID-19 pandemic: a cross-country documentary analysis. Int J Pharm Pract 2022;30:i21–2. 10.1093/ijpp/riac019.029 [DOI] [Google Scholar]
- 6.Bahlol M, Dewey RS. Pandemic preparedness of community pharmacies for COVID-19. Res Social Adm Pharm 2021;17:1888–96. 10.1016/j.sapharm.2020.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.International Pharmaceutical Federation (FIP Health Advisory) . Coronavirus 2019- nCoV outbreak. information and interim guidelines for pharmacists and the pharmacy workforce. The Netherlands, 2020. https://www.fip.org/files/content/priorityareas/coronavirus/Coronavirus-guidance-update-ENGLISH.pdf [Google Scholar]
- 8.Donabedian A. The quality of care. JAMA 1988;260:1743–8. 10.1001/jama.1988.03410120089033 [DOI] [PubMed] [Google Scholar]
- 9.Patterson SM, Cadogan CA, Barry HE. 'It stayed there, front and centre': Perspectives on community pharmacy’s contribution to front-line health care services during the COVID-19 pandemic. BMJ Open 2022. 10.1136/bmjopen-2022-064549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alkhalili M, Ma J, Grenier S. Defining roles for pharmacy personnel in disaster response and emergency preparedness. Disaster Med Public Health Prep 2017;11:496–504. 10.1017/dmp.2016.172 [DOI] [PubMed] [Google Scholar]
- 11.Zaidi STR, Hasan SS. Personal protective practices and pharmacy services delivery by community pharmacists during COVID-19 pandemic: results from a national survey. Res Social Adm Pharm 2021;17:1832–7. 10.1016/j.sapharm.2020.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.SPSS Inc. Released . SPSS statistics for windows. Chicago: SPSS Inc, 2008. [Google Scholar]
- 13.World Health Organisation . Maintaining essential health services: operational guidance for the COVID-19 context. interim guidance 1 June 2020. World health organisation, 2020. https://www.who.int/publications/i/item/WHO-2019-nCoV-essential_health_services-2020.2 [Google Scholar]
- 14.Visacri MB, Figueiredo IV, Lima TdeM. Role of pharmacist during the COVID-19 pandemic: a scoping review. Res Social Adm Pharm 2021;17:1799–806. 10.1016/j.sapharm.2020.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wickware C. Pharmacies’ dispensing increases by up to a third as a result of COVID-19, survey finds. Pharm J 2020;306. 10.1211/PJ.2020.20207917 [DOI] [Google Scholar]
- 16.Romano S, Galante H, Figueira D, et al. Time-Trend analysis of medicine sales and shortages during COVID-19 outbreak: data from community pharmacies. Research in Social and Administrative Pharmacy 2021;17:1876–81. 10.1016/j.sapharm.2020.05.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Murphy M, Scott LJ, Salisbury C, et al. Implementation of remote consulting in UK primary care following the COVID-19 pandemic: a mixed-methods longitudinal study. Br J Gen Pract 2021;71:e166–77. 10.3399/BJGP.2020.0948 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Carpenter DM, Hastings T, Westrick S, et al. Rural community pharmacies’ preparedness for and responses to COVID-19. Res Social Adm Pharm 2021;17:1327–31. 10.1016/j.sapharm.2020.10.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rosenquist JN. The stress of Bayesian medicine — uncomfortable uncertainty in the face of Covid-19. N Engl J Med 2021;384:7–9. 10.1056/NEJMp2018857 [DOI] [PubMed] [Google Scholar]
- 20.Wickware C. Pharmacy leaders in ‘urgent talks’ with NHS as COVID-19 booster vaccination campaign is ramped up. Pharm J 2021;307. 10.1211/PJ.2021.1.12-231 [DOI] [Google Scholar]
- 21.Wickware C. Record numbers of lateral flow tests sent to pharmacies amid supply issues. Pharm J 2021;307. 10.1211/PJ.2021.1.121205 [DOI] [Google Scholar]
- 22.Wickware C. Community pharmacies fulfil 17 million lateral flow test requests, official data show. Pharm J 2022;308. 10.1211/PJ.2022.1.129133 [DOI] [Google Scholar]
- 23.Patton DE, Ryan C, Hughes CM. Enhancing community pharmacists' provision of medication adherence support to older adults: a mixed methods study using the theoretical domains framework. Res Social Adm Pharm 2021;17:406–18. 10.1016/j.sapharm.2020.03.004 [DOI] [PubMed] [Google Scholar]
- 24.Austin Z, Gregory P. Resilience in the time of pandemic: the experience of community pharmacists during COVID-19. Res Social Adm Pharm 2021;17:1867–75. 10.1016/j.sapharm.2020.05.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parkhurst C, Singh Purewal G, Donyai P. Community pharmacy and COVID-19-the unsung heroes on our high streets. J Patient Exp 2020;7:282–4. 10.1177/2374373520927638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maidment I, Young E, MacPhee M, et al. Rapid realist review of the role of community pharmacy in the public health response to COVID-19. BMJ Open 2021;11:e050043. 10.1136/bmjopen-2021-050043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lloyd-Smith M. The COVID-19 pandemic: resilient organisational response to a low-chance, high-impact event. BMJ Lead 2020;4:109–12. 10.1136/leader-2020-000245 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-064545supp001.pdf (1.5MB, pdf)
Data Availability Statement
Data are available on reasonable request.