Abstract
Objectives
Contributing factors to COVID-19 vaccination intention in low-income and middle-income countries have received little attention. This study examined COVID-19-related anxiety and obsessive thoughts and situational factors associated with Pakistani postpartum women’s intention to get COVID-19 vaccination.
Design
Cross-sectional study administering a survey by a telephone interview format between 15 July and 10 September 2020.
Setting
Four centres of Aga Khan Hospital for Women and Children—Garden, Kharadar, Karimabad and Hyderabad—in Sindh Province, Pakistan.
Participants
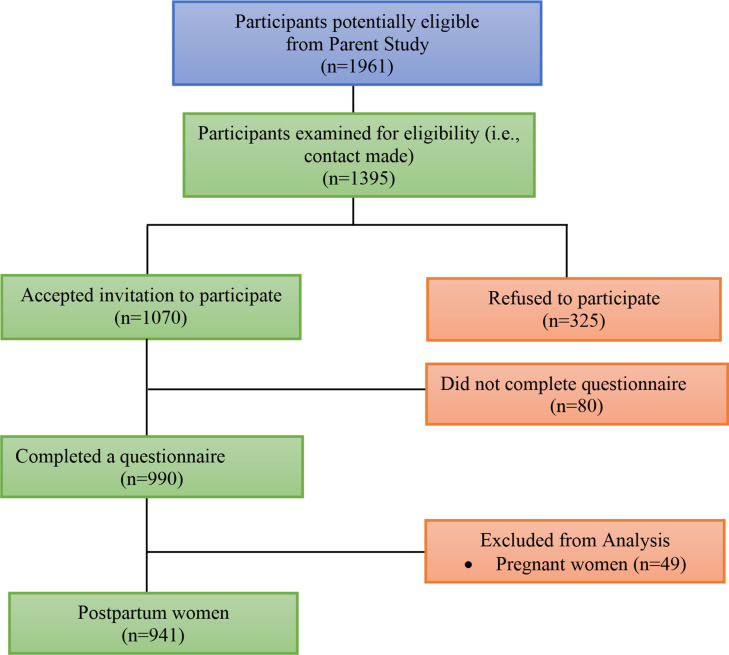
Women who were enrolled in our longitudinal Pakistani cohort study were approached (n=1395), and 990 women (71%) participated in the survey, of which 941 women who were in their postpartum period were included in the final analysis.
Primary outcome measure and factors
COVID-19 vaccine intention, sociodemographic and COVID-19-related factors, Coronavirus anxiety, obsession with COVID-19 and work and social adjustment were assessed. Multiple multinomial logistic regression analysis was used to identify factors associated with women’s intentions.
Results
Most women would accept a COVID-19 vaccine for themselves (66.7%). Only 24.4% of women were undecided about vaccination against COVID-19, and a small number of women rejected the COVID-19 vaccine (8.8%). Women with primary education were less likely to take a COVID-19 vaccine willingly than those with higher education. COVID-19 vaccine uncertainty and refusal were predicted by having no experience of COVID-19 infection, childbirth during the pandemic, having no symptoms of Coronavirus anxiety and obsession with COVID-19. Predictors for women’s intention to vaccinate themselves and their children against COVID-19 were similar.
Conclusion
Understanding the factors shaping women’s intention to vaccinate themselves or their children would enable evidence-based strategies by healthcare providers to enhance the uptake of the COVID-19 vaccine and achieve herd immunity against Coronavirus.
Keywords: COVID-19, perinatology, anxiety disorders, depression & mood disorders, public health
Strengths and limitations of this study.
In this study, we examined COVID-19-related anxiety and obsessive thoughts associated with Pakistani postpartum women’s intention to get COVID-19 vaccination.
The reliability and validity of Coronavirus anxiety and Obsession with COVID-19 Scales have not been tested in the population of Pakistani women, thus we categorised the participant responses rather than using a cutpoint of the questionnaire.
Our study did not examine knowledge, attitudes and beliefs about COVID-19 which promotes the actual health behaviour (ie, vaccine uptake), thus actual behaviour may differ from responses to surveys.
Although our study participants were from three sites in Karachi and one in Hyderabad, which represent sociocultural diversity in Pakistani women, the findings may not be generalised to the rest of Pakistan or other countries.
Introduction
In the context of the COVID-19 pandemic, maternity care for women is particularly complex given birth-related psychophysiological changes and our evolving understanding of the health risk of COVID-19 and the benefits of immunisation for both the mother and baby.1–3 Breastfeeding women were excluded from COVID-19 vaccine primary trials;4 hence, there are limited data on the safety of COVID-19 vaccines in lactating women and their effects on the baby or breast milk excretion.5 Recent studies reported the presence of antibodies in breastmilk of lactating women who have received the mRNA COVID-19 vaccines.6 7 However, more research is needed to determine the protective role for babies of these antibodies. Nevertheless, based on the knowledge of other mRNA vaccines, COVID-19 vaccines are presumed safe for both mothers and breastfed babies.8 Leading authorities, such as the USA Centers for Disease Control and Prevention (CDC), WHO and Advisory Committee on Immunization Practices (ACIP), in collaboration with the American College of Obstetricians and Gynecologists (ACOG), indicated in their guidelines that COVID-19 vaccines should not be withheld from lactating mothers.9–11
A requisite to achieving herd immunity and protection of the community against COVID-19, however, is the acceptability and uptake of the vaccine among the majority of the population.12 Children seem to have a low symptomatic COVID-19 infection rate than adults but may have a similar risk of infection.13 As of October 2019, only persons aged over 12 years are eligible to receive available COVID-19 vaccines.14–16 Since women play an important role in decision-making for the vaccination of their children,17 evaluating their intention and predicting factors is an essential factor for optimising their vaccination intake.
Vaccination of 60%–70% of the population is usually considered the threshold to achieve herd immunity,18 although this number might differ according to the community, the type of vaccine and populations prioritised for immunisation.19–21 Vaccinating the majority of the community can significantly reduce the likelihood of the spread of disease and infection of those who lack immunity (eg, babies).22 The intention of receiving COVID-19 vaccines is influenced by individual behaviour, which depends on several factors.22 Several studies on the general population in different countries suggest that individuals from ethnic minorities, lower-income households and those with lower education, who are aged under 25 years, are more likely to reject current COVID-19 vaccines.23 24 Intention towards vaccination can also be affected by geographic regions, for example, Middle East countries, Africa, Russia and some European countries such as France are more likely to reject the COVID-19 vaccine.23 25–27 The perceived rapid development and limited evidence about the safety of COVID-19 vaccinations on women’s and child health and the cost of vaccines may impact vaccine uptake.25 Social pressure (actual or perceived) from family may also influence vaccine willingness.22 The association between vaccine intention and mental health has remained controversial. Some studies showed that depression and anxiety were associated with more acceptability of vaccination.28 29 In contrast, others reported the association of psychological distress and vaccine hesitancy.30 31 Vaccination intention is also affected by demographic factors (eg, age, sex, marital status, monthly income and literacy level), diagnosis of COVID-19 infection in individuals or their family members and friends and the belief of being naturally immune to COVID-19 after being infected.32 Lack of knowledge, and fear of unknown side effects can also influence acceptance of COVID-19 vaccination.24 33
In low-income and middle-income countries, contributing factors to COVID-19 vaccination acceptance or refusal, especially among women in the postpartum period, have received little attention in the literature. We asked Pakistani postpartum women about their intention to uptake a COVID-19 vaccine for themselves or their children when it becomes available in the future. We examined the situational factors (eg, demographic, financial) that may influence intent to uptake a COVID-19 vaccine once available. Since psychological health appears to be a determinant of vaccine intention and remains to be investigated, we also assessed psychological factors, specifically anxiety and obsession associated with COVID-19, in our study.
Methods
Study design and participants
Participants in this cross-sectional study were recruited from an ongoing prospective longitudinal Pakistani cohort study (ie, parent study) assessing psychosocial distress during pregnancy and pathways to preterm birth. Women in the parent study were healthy women with a naturally conceived singleton pregnancy, attended antenatal clinics at 10–19 weeks’ and 22–29 weeks’ gestational age and intended to deliver or delivered at the same recruitment site, and could speak Urdu, Sindhi or English. The sample size was based on participants available from our parent study who provided informed consent (grade 4 reading level, witnessed or verbal in Urdu, Sindhi or English) and completed a questionnaire (a telephone interview format given varied literacy levels).
Setting
Our parent study was based in four centres of Aga Khan Hospital for Women and Children, three in Karachi (ie, Garden, Kharadar and Karimabad) and one in Hyderabad, representing ethnically diverse Pakistani women. During the study period, 15 July to 10 September 2020, the COVID-19 vaccines were still in their early stages of development.34 35
Measures
Participants had already completed a self-report questionnaire in the parent study with items related to sociodemographic information, obstetric characteristics, perinatal distress and covariates of preterm birth. The COVID-19 specific data collected through this observational study included (a) our outcome variable, which was women’s lack of willingness to vaccinate themselves, (b) symptoms of COVID-19, (c) dimensions of emotional well-being specific to COVID-19 which were assessed with the Coronavirus Anxiety Scale (CAS) and the Obsession with COVID-19 Scale (OCS) and (d) impact of COVID-19 on work and social adjustment and ability to meet financial needs. The list of variables from both the parent and the current study are presented in table 1.
Table 1.
List of collected variables through the parent study and current study
| Parent study | This study | |
| Sociodemographic factors | Obstetric characteristics | COVID-19-related factors |
| Age | Baby’s health-related issues at birth | Intention to vaccinate themselves against COVID-19 when the vaccine is available |
| Ethnic group | Pregnancy outcome (preterm/term) | COVID-19 symptom and/or exposure |
| Location | Breastfeeding | Period of childbirth (prepandemic/during pandemic) |
| Women and their husband’s education | Sex of baby | Coronavirus anxiety symptom (CAS) |
| Employment | Constant and troubled thinking about Coronavirus (OCS) | |
| Socioeconomic status | Work and social adjustment because of COVID-19 | |
| Impact of COVID-19 on the ability to meet financial obligations | ||
CAS, Coronavirus Anxiety Scale; OCS, Obsession with COVID-19 Scale children.
Two questions were used to determine women’s willingness to take a vaccine for themselves or their children: (1) if an approved COVID-19 vaccine becomes available, would you plan to receive this vaccine and (2) if an approved COVID-19 vaccine becomes available, would you plan to have your child (children) receive this vaccine? The response options were the same for both questions, namely no (lack of willingness to vaccinate), yes (willingness to vaccinate), undecided (undecided) or have not thought about it (undecided). From the exploratory data analysis, we found that almost all women indicated the same intention for themselves and their children; thus, we only present the intention to take an approved COVID-19 vaccine for themselves if it becomes available with three categories (willing, unwilling and undecided).
We assessed whether the participants had any symptoms of COVID-19 disease using the WHO case definitions as a guide (eg, fever, cough, shortness of breath categorised as yes/no). Two dimensions of emotional well-being specific to COVID-19 were assessed: (a) COVID-19-related anxiety assessed the frequency of the psychological effects (eg, disturbances in sleep and appetite) that participants experienced due to the Coronavirus pandemic. This was measured using the CAS consisting of five items on a four-point scale (0=not at all to 4=nearly every day over the last 2 weeks); score ranging from 0 to 20 with high scores suggesting greater COVID-19-related anxiety of the individuals. Cronbach’s α=0.93, 90% sensitivity, 85% specificity).36 (b) Obsession with COVID-19 that determined how often women had constant and troubled thinking about Coronavirus. This was measured using OCS consisting of four items; score ranging from 0 to 16 with high scores suggesting irrational thinking about COVID-19, Cronbach’s α=0.0.84 to 0.85, 81% to 93% sensitivity, 73% to 76% specificity.37 Following exploratory data analysis, we categorised the participant responses as women with one or more Coronavirus anxiety and obsession with COVID-19 symptoms and those who did not mention any symptom for COVID-19-related anxiety and obsession with COVID-19.
Work and Social Adjustment Scale (WSAS) identified day-to-day impediments to work and social functioning as a result of worries and fears of the Coronavirus.36 The WSAS uses five Likert type items (0 for not at all to 8 for very severely) related to the ability to work or study; home management; social leisure activities; private leisure activities and the ability to maintain close relationships (Cronbach’s α=0.70–0.94, correlation 0.76 and 0.61 to depression severity and symptoms of an obsessive compulsion disorder, respectively).36 The WSAS scores range from 0 to 40, and higher scores indicate higher levels of functional impairment (scores >21 suggest moderately severe to worse psychopathology; scores between 10 and 20 suggest significant functional impairment but less severe clinical symptomatology; scores <10 suggest mild or no clinical symptomatology).36 The impact of COVID-19 on the ability to meet financial obligations was asked with four possible response options including major impact, moderate impact, minor impact, or no impact.
Analysis
We used SPSS V.25 for analysis and statistical modelling. Descriptive statistics (number and percentages) for all variables were generated according to their responses to COVID-19 vaccines acceptability questions. χ2 tests were used to compare group differences in study variables that were categorical. Responses to COVID-19 vaccine intention, which were either ‘undecided’ or ‘have not thought about it’, were grouped into one category as undecided. Multiple multinomial logistic regression analysis was conducted to compare the odds of being undecided to vaccinate and unwilling to vaccinate with vaccine intention of women for themselves as an outcome, if a save vaccine became available. Women’s sociodemographic and psychological characteristics were used as predictor variables to compute the OR with 95% CI for vaccine willingness. Only significant variables were included in the models using the stepwise backward method. The level of significance was set at p<0.05. We hypothesised that younger women with lower level of education and socioeconomic status would be more likely to be undecided or unwilling to take the vaccine compared with older, more educated and wealthier women. Furthermore, women who have had previous experience with COVID-19 or exhibited anxiety symptoms regarding COVID-19 would be less likely to be unwilling or undecided about accepting the vaccine than women with no prior experience and no anxiety.
Results
Participants
Of the 1395 women in the parent study who could be reached, complete data were available for 990 women. Figure 1 details the flow of participants through the study which included refusals, and participants who accepted the invitation to participate but did not complete the questionnaire. In this paper, we present data on the 941 women who were in the postpartum period and delivered either before or during the pandemic. The remaining 49 women were excluded for various reasons: (a) their views of acceptability would be different from postpartum women, (b) some women became pregnant during the pandemic, thus their unique pregnancy experience would likely impact their attitudes and responses regarding COVID-19, and vaccine hesitancy and/or (c) to ensure consistency in terms of timing of measures of prenatal variables as for some women this was not their index pregnancy and the prenatal variables measured related to the child already delivered (ie, index pregnancy) and not the current pregnancy.
Figure 1.
Flow of participants through the study.
Majority of respondents were in the 26–30 years age group (45.2%) and had a college or university education (74.3%) (table 2). Women of upper-medium socioeconomic status made up 51.6% of the sample, while only 6.4% came from low-medium socioeconomic backgrounds.
Table 2.
Intention to vaccinate for COVID-19 by characteristics of postnatal women
| Characteristics | Total N | Willingness, n (%) | Unwillingness n (%) | Undecided, n (%) | p value |
| 941 | 628 (66.7) | 83 (8.8) | 230 (24.4) | ||
| Maternal age (years) | |||||
| 18–25 | 237 | 151 (63.7) | 27 (11.4) | 59 (24.9) | 0.192 |
| 26–30 | 425 | 289 (68) | 38 (8.9) | 98 (23.1) | |
| 31–35 | 214 | 142 (66.4) | 11 (5.1) | 61 (28.5) | |
| 36–40 | 65 | 46 (70.8) | 7 (10.8) | 12 (18.5) | |
| Ethnic group | |||||
| Memon | 121 | 90 (74.4) | 12 (9.9) | 19 (15.7) | <0.001 |
| Sindhi | 215 | 123 (57.2) | 19 (8.8) | 73 (34) | |
| Urdu-Muhajir | 294 | 187 (63.6) | 26 (8.8) | 81 (27.6) | |
| Other | 311 | 228 (73.3) | 26 (8.4) | 57 (18.3) | |
| Location | |||||
| Karimabad | 243 | 152 (62.6) | 24 (9.9) | 67 (27.6) | <0.001 |
| Garden | 244 | 230 (94.3) | 1 (0.4) | 13 (5.3) | |
| Hyderabad | 278 | 127 (45.7) | 38 (13.7) | 113 (40.6) | |
| Kharadar | 176 | 119 (67.6) | 20 (11.4) | 37 (21) | |
| Woman’s education | |||||
| Primary school | 75 | 34 (45.3) | 7 (9.3) | 34 (45.3) | <0.001 |
| Secondary/high school | 166 | 114 (68.7) | 19 (11.4) | 33 (19.9) | |
| College/university | 699 | 480 (68.7) | 57 (8.2) | 162 (23.2) | |
| Husband’s education | |||||
| Primary school | 48 | 31 (64.6) | 4 (8.3) | 13 (27.1) | 0.896 |
| Secondary/high school | 117 | 76 (65) | 9 (7.7) | 32 (27.4) | |
| College/university | 774 | 521 (67.3) | 70 (9) | 183 (23.6) | |
| Socioeconomic status | |||||
| Low | 60 | 32 (53.3) | 6 (10) | 22 (36.7) | 0.097 |
| Middle | 486 | 320 (65.8) | 47 (9.7) | 119 (24.5) | |
| High | 394 | 276 (70.1) | 30 (7.6) | 88 (22.3) | |
| Sex of the child | |||||
| Boy | 471 | 302 (64.1) | 44 (9.3) | 125 (26.5) | 0.411 |
| Girl | 385 | 261 (67.8) | 37 (9.6) | 87 (22.6) | |
| Infant health issues at birth | |||||
| No | 807 | 532 (65.9) | 77 (9.5) | 198 (24.5) | 0.770 |
| Yes | 47 | 32 (68.1) | 3 (6.4) | 12 (25.5) | |
| Pregnancy outcome | |||||
| Preterm | 113 | 80 (70.8) | 7 (6.2) | 26 (23) | 0.36 |
| Term | 738 | 480 (65) | 72 (9.8) | 186 (25.2) | |
| Breastfeeding | |||||
| No | 25 | 9 (36) | 4 (16) | 12 (48) | 0.004 |
| Yes | 907 | 614 (67.7) | 79 (8.7) | 214 (23.6) | |
There was ethnic diversity in the sample with almost a third representing Urdu-Muhajir (ie, largest ethnic group), followed by Sindhi (22.8%) and then Memon (12.9%). Almost a third of the sample were from minority ethnic groups (eg, Katchi, Gujrati, Punjabi, Balochi, Pathan or mixed ethnicity). The rate of preterm birth in our sample was 12%. Majority of women (85.8%) had a healthy baby at birth (85.8%) and were breastfeeding their baby (96.4%).
Women’s intention to get COVID-19 vaccination
Bivariate associations between characteristics of women and intention to receive the COVID-19 vaccine for themselves are presented in table 2. Overall, two-thirds of the women in our sample (66.7%, n=628) reported that they would accept a future COVID-19 vaccine for themselves, while 8.8% (n=83) would refuse and 24.4% (n=230) were undecided about receiving a vaccine.
As shown in table 2, background factors associated with women’s intention to vaccinate were ethnicity (p<0.001), location (p<0.001), women’s education (p<0.001) and breastfeeding (p<0.004). Willingness to vaccinate was highest at Garden (94.3%) and lowest at Hyderabad (45.7%). However, 40.6% of women at Hyderabad were undecided, and only 13.7% were unwilling. Only one woman at Garden was unwilling to vaccinate. Differences were noted between ethnic categories in the percentage of women who were willing to vaccinate and those who were still undecided. Similarly, differences in the percentage of women who were unwilling to vaccinate and those who were still undecided was more pronounced for women with higher levels of education.
Table 3 shows an association between willingness to vaccinate and exposure to, the experience of, and feelings about COVID-19. As evident from table 3, Coronavirus anxiety symptoms (p<0.001), obsession with COVID-19 symptoms (p<0.001), level of work and social adjustment to COVID-19 pandemic (p=0.008) and the impact of COVID-19 on the ability to meet financial obligations (p<0.00), were highly associated with intention to vaccinate. When comparing women who gave birth before the pandemic to women who gave birth during the pandemic, women who gave birth during the pandemic tended to be more willing to get the COVID-19 vaccine (68.3% vs 60.1%) and less likely to be unwilling to vaccinate themselves (7.9% vs 14.2%). Similarly, women who had the experience of COVID-19-related symptoms were more likely (82.1% vs 65.6%) to get the vaccine and less likely to refuse it (6.0% vs 9.0%) than women who had not experienced any symptoms.
Table 3.
Intention to vaccinate for COVID-19 by different characteristics of postnatal women
| Characteristics | Total N | Willingness n (%) |
Unwillingness n (%) |
Undecided n (%) |
p value |
| 941 | 628 (66.7) | 83 (8.8) | 230 (24.4) | ||
| Period of childbirth | |||||
| Prepandemic | 786 | 537 (68.3) | 62 (7.9) | 187 (23.8) | 0.030 |
| During pandemic | 148 | 89 (60.1) | 21 (14.2) | 38 (25.7) | |
| Women’s experience of COVID-19 symptoms | |||||
| No | 874 | 573 (65.6) | 79 (9) | 222 (25.4) | 0.020 |
| Yes | 67 | 55 (82.1) | 4 (6) | 8 (11.9) | |
| Family member experience of COVID-19 symptoms | |||||
| No | 890 | 588 (66.1) | 80 (9) | 222 (24.9) | 0.219 |
| Yes | 50 | 39 (78) | 3 (6) | 8 (16) | |
| Impact of COVID-19 on ability to meet financial obligations | |||||
| Major impact | 128 | 75 (58.6) | 15 (11.7) | 38 (29.7) | 0.001 |
| Moderate impact | 256 | 166 (64.8) | 23 (9) | 67 (26.2) | |
| Minor impact | 329 | 250 (76) | 18 (5.5) | 61 (18.5) | |
| No impact | 228 | 137 (60.1) | 27 (11.8) | 64 (28.1) | |
| Obsession with COVID-19 | |||||
| No OC symptoms | 241 | 155 (64.3) | 36 (14.9) | 50 (20.7) | <0.001 |
| ≥1 OC symptoms | 700 | 473 (67.6) | 47 (6.7) | 180 (25.7) | |
| Coronavirus anxiety symptoms | |||||
| No CA symptom | 495 | 271 (54.7) | 65 (13.1) | 159 (32.1) | <0.001 |
| ≥1 CA symptoms | 446 | 357 (80) | 18 (4) | 71 (15.9) | |
| Work and social adjustment | |||||
| 0–9 | 502 | 358 (71.3) | 43 (9.6) | 101 (20.1) | 0.008 |
| 10–20 | 283 | 171 (60.4) | 30 (10.6) | 82 (29) | |
| 21–40 | 156 | 99 (63.5) | 10 (6.4) | 47 (30.1) | |
CA, Coronavirus anxiety; OC, obsessive compulsive.
Predictors of unwillingness and indecision to take COVID-19 vaccine
The ORs for unwilling to vaccinate versus willing, and undecided about vaccination versus willing to vaccinate given significant baseline and COVID-19-related factors, were obtained using the multinomial logistic regression models as shown in table 4.
Table 4.
Predictors of women’s intentions to accept future COVID-19 vaccination*
| Characteristics | Unwilling | Undecided | ||
| OR (95% CI) | p value | OR (95% CI) | p value | |
| Ethnic group | ||||
| Memon | 1.56 (0.69 to 3.54) | 0.289 | 1.03 (0.53 to 1.98) | 0.934 |
| Sindhi | 0.43 (0.20 to 0.93) | 0.031 | 0.73 (0.43 to 1.25) | 0.246 |
| Urdu-Muhajir | 1.00 (0.50 to 2.00) | 0.995 | 1.39 (0.86 to 2.24) | 0.177 |
| Other | Reference | Reference | ||
| Location | ||||
| Karimabad | 1.32 (0.58 to 3.00) | 0.505 | 1.60 (0.88 to 2.91) | 0.127 |
| Garden | 0.03 (0 to 0.25) | 0.001 | 0.19 (0.09 to 0.38) | <0.001 |
| Hyderabad | 2.81 (1.29 to 6.07) | 0.009 | 3.24 (1.81 to 5.80) | <0.001 |
| Kharadar | Reference | Reference | ||
| Woman’s education | ||||
| Primary school | 2.24 (0.85 to 5.91) | 0.103 | 3.83 (2.09 to 7.05) | <0.001 |
| Secondary/high school | 1.66 (0.86 to 3.20) | 0.135 | 1.32 (0.80 to 2.18) | 0.271 |
| College/university completed | Reference | Reference | ||
| Period of childbirth | ||||
| During pandemic | 2.16 (1.17 to 4.00) | 0.014 | 1.37 (0.85 to 2.21) | 0.194 |
| Prepandemic | Reference | Reference | ||
| Women’s experience of COVID-19 symptoms | ||||
| No | 1.87 (0.62 to 5.65) | 0.269 | 3.30 (1.36 to 6.64) | 0.007 |
| Yes | Reference | Reference | ||
| Coronavirus anxiety symptoms | ||||
| No CA symptom | 2.32 (1.26 to 4.28) | 0.007 | 1.55 (1.05 to 2.28) | 0.026 |
| ≥1 CA symptoms | Reference | Reference | ||
| Obsession with COVID-19 symptoms | ||||
| Never OC symptoms | 2.22 (1.30 to 3.77) | 0.003 | 0.92 (0.61 to 1.39) | 0.683 |
| ≥1 OC symptom | Reference | Reference | ||
*The reference category is: willingness to receive the COVID-19 vaccine.
CA, Coronavirus anxiety; OC, obsessive compulsive; OR, odds ratio.
The odds of Sindhi women being unwilling to vaccinate (OR=0.43, 95% CI 0.20 to 0.93) were 57% lower than the corresponding odds for women of other minorities ethnic category. Women from Memon, Sindhi and Urdu-Muhajir ethnic groups did not differ from other minorities ethnic category in their likelihood of being unwilling to vaccinate or undecided about vaccinating.
Women recruited from Karimabad had a similar likelihood of being unwilling (p=0.505) or undecided (p=0.127) about vaccinating compared with women from Kharadar. The odds of a woman recruited from Hyderabad being unwilling to vaccinate were 2.81 (95% CI 1.29 to 6.07), and the odds of being undecided about vaccinating were 3.24 (CI 1.81 to 5.80), which were significantly higher than the corresponding odds for a women recruited from Kharadar. Virtually none of the women from Garden was unwilling to vaccinate, and the odds of a woman from Garden being undecided were 81% (OR=0.19, 95% CI 0.09 to 0.38) lower than for women recruited from Kharadar. Women with primary education were more likely to be undecided about COVID-19 vaccination than those with higher education (OR=3.83; 95% CI: 2.09 to 7.05).
Women who gave birth during the pandemic had significantly higher odds (OR=2.16, 95% CI 1.17 to 4.0) of being unwilling to vaccinate compared with women who gave birth before the pandemic. However, both groups of women had a similar likelihood (p=0.194) of being undecided. Women who had not experienced COVID-19 disease symptoms had 3.30 (95% CI 1.36 6.64) times higher odds of being uncertain about vaccinating against COVID-19 than women who had experienced symptoms, but both groups had a similar likelihood (p=0.267) of being unwilling to vaccinate.
Women’s emotional distress related to COVID-19 was also associated with unwillingness and uncertainty about future intent to vaccinate against COVID-19. The odds of a woman who had no Coronavirus anxiety symptoms rejecting vaccination were 2.32 (95% CI 1.26 to 4.28), and odds of being undecided were 1.55 (95% CI 1.05 to 2.28) times compared with those for a woman who reported one or more symptoms. Women who reported at least one symptom of obsession with COVID-19 were significantly more likely to be unwilling to vaccinate (OR=2.22, 95% CI 1.30 to 3.77, p=0.003) compared with those with no obsession with COVID-19 symptom but being obsessed with COVID-19 symptoms did not change the likelihood (p=0.683) of being undecided to vaccinate relative to being willing to vaccinate.
Discussion
We explored postnatal Pakistani women’s intention to vaccinate against COVID-19 at a time when large-scale vaccination, globally, had yet to begin. Two-thirds (66.7%) of women in our study would accept a COVID-19 vaccine for themselves, while 24.4% were undecided, and 8.8% said that they would not take the vaccine. All but two of the women selected the same intention for their children and for themselves. Our study determined that some sociodemographic characteristics (primary education, being from Hyderabad) can negatively affect women’s intention to vaccinate themselves against COVID-19. Women’s intention to accept the COVID-19 vaccine were also influenced by COVID-19-related factors such as the experience of COVID-19 infection, Coronavirus anxiety symptoms and obsession with COVID-19 and childbirth before the COVID-19 pandemic.
The acceptance rate in our study was consistent with a multinational study conducted on women in 16 countries throughout the world (average acceptance rate: 73.4%) and another study of six European nations (acceptance rate: 60%–70%) that investigated the vaccine acceptance among mothers of young children.38 39 However, a study conducted in 10 low-income and middle-income countries in Asia, Africa and South America, Russia (an upper-middle-income country) showed an average rate of acceptance of 80.3% (range: 66.5%–96.6%; median: 78%) which was higher than women in our study;40 while a national survey of the general population in Pakistan reported only 48.2% acceptance to receive a COVID-19 vaccine.41 The difference in the rate of acceptance between this national survey and our study can be due to differences in responded characteristics. Those who completed the web-based questionnaire were predominantly male (55.2%) and students without gainful employment (71.8%). Rates of acceptance of COVID-19 vaccine are higher among postpartum women than pregnant women given fear of adverse consequences on fetus.25 Our sample comprised women in the postpartum period who are in close contact with their physician following childbirth and could be informed by them and became more motivated to receive the vaccine.42 Moreover, there are important qualifying differences in the way some of the vaccine intention questions were asked across studies. For example, by adding terms such as ‘Safe’, ‘free’ and ‘efficacy of 90%’ to the vaccine intention questions, significant change in acceptance can occur.39 Finally, the stage of COVID-19 pandemic, containment measures in place and incidence rates of new cases can result in differences in how participants respond between countries and different parts of a country.27 40 43
We found an association between geographic location and intention to receive a COVID-19 vaccine, with women from Kharadar being more inclined to receive COVID-19 vaccination for themselves and women from Hyderabad being undecided. Kharadar is different from other study sites with respect to infrastructure, poverty level, maternal education and sociocultural context.44 Pakistani women’s decision-making is related to the complex intersection between the sociodemographic and economic context and cultural milieu in which they live.45–47 Women living in urban areas have a greater say in the household, while in the rural area, husbands and other family members have a significant role in making decisions, especially with regard to medical care for their children.47 However, the social position of the women, her education level and earning potential are also determinants of women’s autonomy in decision-making.45 Anecdotal evidence from our clinician colleagues suggests that information from authoritative sources such as physicians, influences women and family’s decision-making in Kharadar. In addition, the Aga Khan Hospital for Women and Children’s service is more accessible to women and children in Karimabad, and Garden compared with Hyderabad and Kharadar due to its location, which provides women with more health education thus more latitude with decision-making. A study conducted on awareness and acceptance of the influenza vaccine in Pakistan has shown that only a few people vaccinate themselves or their children despite the presence of vaccines.48 Community healthcare providers, local stakeholders and partners must design strategies to manage problems associated with people who are reluctant to get the COVID-19 vaccine in the rural parts of the country24 but also ensure intention leads to uptake of vaccine.
In our study, individuals with a lower level of education were more likely to be undecided about vaccination, whether for themselves or their children. These findings are consistent with prior studies conducted in Ethiopia, Saudi Arabia, the UK, Australia and the Punjab region in Pakistan as part of a global study.40 49–52 People with a lower level of education might not be completely aware of the health benefit of receiving COVID-19 vaccination on the individual and society levels.53 Their uncertainty or lack of willingness to vaccinate may be related to safety concern (ie, side effects),40 which our clinician colleagues explain is based on what family members, relatives or friends tell perinatal women. Women in Kharadar, who are generally less educated, may also be more inclined to trust information received from authoritative sources such as their postpartum care provider and be willing to accept their recommendations to vaccinate.40 People with a higher level of education spend more time improving their knowledge of understanding the severity of the disease and the positive impact of vaccination, making them more receptive to a new vaccine.54 These findings suggest the importance of targeting women from lower academic status and improving their understanding through targeted messages from physicians or healthcare providers that are understandable to encourage vaccination uptake.50 52
In line with previous reports,55 56 having no symptoms of COVID-19-related anxiety and obsession were linked to women’s uncertainty and unwillingness about vaccination against COVID-19. Women with more than one symptom of Coronavirus anxiety or obsession with COVID-19 were more likely to be vaccinated than those without any symptom. Anxiety is a defence response to a possible danger that encourages people to deal with a detected threat such as the COVID-19 pandemic and its related risks.57 In our study, being more willing to receive a vaccine in women with a higher level of anxiety can be due to this adaptive function of anxiety that has evolved to lower the risk of mortality and reflect one’s fear of protecting oneself.58 However, these findings were inconsistent with some other studies, which reported more likelihood of suffering from vaccine hesitancy in individuals with psychological distress.31 59 These discordances can be due to their different measurement tools (ie, generalised anxiety, depression, and peritraumatic distress) compared with our study.
In this study, we separately looked at predictor factors for women’s uncertainty and unwillingness to vaccinate themselves or their children against COVID-19. Uncertainty is an important factor regarding health-related decisions.60 The uncertainty is usually caused by conflicting information and contributes to negative emotions, which can impact individuals’ attitudes toward health-related behaviour such as vaccination.61 62 Programmes and interventions that help to interpret conflicting information and cope with uncertainty are necessary.63 Based on WHO recommendation, individuals who are undecided about receiving vaccination are potential target groups for future interventions that encourage vaccination.64 These interventions for improving the vaccine uptake are not likely to affect the attitude of those who are entirely against vaccination, and better to not target these groups primarily.65
According to the theory of reasoned action, the major predictors of intentions are attitude towards the behaviour, subjective norms concerning the behaviour and perceived behavioural control.66 Attitude towards a health-related behaviour such as getting a vaccine is positively related to intention to perform that behaviour.67 Although the uptake of health behaviours such as vaccination is highly related to the individual’s intention,68 69 based on previous experience with influenza vaccination, intention towards receiving a vaccine is usually greater than the actual vaccine uptake rate.70 71 Hence, those who intend to uptake a vaccine also benefit from these public health programmes designed to increase vaccine uptake.64 The Government implemented several strategies (eg, blocking citizen’s cell phone SIMs, restricting access to transport, public spaces such as restaurants and shopping if they are not vaccinated) that changed individual’s behaviour to promote uptake of vaccine.72
Strengths and limitations
To the best of our knowledge, this is the first study to comprehensively investigate factors affecting uncertainty and unwillingness of postpartum Pakistani women to vaccinate themselves and their children against COVID-19 as separate outcomes. The reliability and validity of Coronavirus anxiety and OCS have not been tested before in the Pakistani women population, thus we categorised the participant responses rather than using a cutpoint of the questionnaire. Although the uptake of health behaviours such as vaccination uptake is highly related to the individual’s intention, actual behaviours may differ from responses to surveys. Our study did not examine knowledge, attitudes and beliefs about COVID-19 which promotes the actual health behaviour (ie, vaccine uptake). We recruited through convenience sampling from three sites in Karachi and one in Hyderabad. Although our sample represents sociocultural diversity in Pakistani women, the findings may not be generalised to the rest of Pakistan or other countries. We did not investigate the interrelationship between common mental disorders (eg, depression, anxiety) and COVID-19 vaccine intention, thus findings need to be interpreted and applied with caution. We assessed vaccine intention at a time when the vaccine was not available. The ongoing pandemic, increasing knowledge of COVID-19 and access (or lack thereof) to COVID-19 vaccination(s) will influence vaccine attitudes, intensions and behaviours. The interventions to promote vaccine uptake will need to consider the unique backgrounds, conditions, and contexts of postpartum women.
Conclusions
In summary, the results indicated that situational factors such as location, education and the experience of COVID-19, and psychological factors including Coronavirus anxiety and obsession could affect the intention to uptake a COVID-19 vaccine for women and their children. Our findings can inform healthcare planners when strategising targeted approaches to positively affect the intention of vaccination, considering the positive association between intention to receive a vaccine and getting vaccinated. Future studies on vaccine hesitancy need to consider the complex (eg, temporal trends in COVID-19) and multifactorial (eg, sociodemographic) influences on vaccine hesitancy to guide evidence informed approaches given the continued pandemic and need for repeated boosters.
Supplementary Material
Acknowledgments
We wish to thank all the participants for generously contributing their time and experience to this study. We are grateful to the research support received through the Canadian Institutes of Health Research Grant (Application #376731) and York University, Faculty of Health, Startup Grant. Maternal–infant Global Health Team (MiGHT) Collaborators in Research members: Lead Shahirose Sadrudin Premji (premjis@yorku.ca); Members (alphabetical): Saher Aijaz, Naureen Akber Ali, Shahnaz Shahid Ali, Neelofur Babar, Aliyah Dosani, Christine Dunkel Schetter, Fazila Faisal, Ntonghanwah Forcheh, Farooq Ghani, Fouzia Hashmani, Imtiaz Jehan, Nasreen Ishtiaq, Arshia Javed, Nigar Jabeen, Rabia Khoja, Sharifa Lalani, Nicole Letourneau, Heeramani Lohana, Mohamoud Merali, Ayesha Mian, Qamarunissa Muhabat, Joseph Wangira Musana, Suneeta Namdave, Christopher T Naugler, Sidrah Nausheen, Christine Okoko, Geoffrey Omuse, Almina Pardhan, Erum Saleem, Pauline Samia, Kiran Shaikh, Nazia Shamim, Sana Asif Siddiqui, Salima Sulaiman, Afia Tariq, Sikolia Wanyonyi, Ilona S Yim.
Footnotes
Twitter: @PremjiShahirose
SSP and SK contributed equally.
Contributors: SSP, SK, NF, KS and SL identified the secondary question. SSP, SK and NF analysed the data and interpreted the results, and KS, AJ, ES, NB, QM, NJ, SN and SSA provided critical interpretations of the findings. SSP, SK and NF had the primary responsibility to draft the manuscript, and KS, AJ, ES, NB, QM, NJ, SN and SSA reviewed it for critical intellectual content. All authors approved the final version of the manuscript for submission. MiGHT Collaborators in Research is an interdisciplinary team that includes investigators, collaborators, programme managers and research associates/assistants who contributed to this work. SSP, SK, and NF are acting as guarantors for this article.
Funding: Canadian Institutes of Health Research Project Grant (PJT 153021, Application Number 376731); Startup Grant, Faculty of Health, York University.
Competing interests: SK and NF were supported to work as research team members through the Canadian Institutes of Health Research Project Grant and Startup Grant.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Contributor Information
Maternal-infant Global Health Team (MiGHT) Collaborators in Research:
Saher Aijaz, Naureen Akber Ali, Aliyah Dosani, Christine Dunkel Schetter, Fazila Faisal, Farooq Ghani, Fouzia Hashmani, Imtiaz Jehan, Nasreen Ishtiaq, Nigar Jabeen, Rabia Khoja, Nicole Letourneau, Heeramani Lohana, Mohamoud Merali, Ayesha Mian, Joseph Wangira Musana, Suneeta Namdave, Christopher T. Naugler, Christine Okoko, Geoffrey Omuse, Almina Pardhan, Pauline Samia, Nazia Shamim, Sana Asif Siddiqui, Salima Sulaiman, Afia Tariq, Sikolia Wanyonyi, and Ilona S Yim
Data availability statement
Data are available upon reasonable request. All data relevant to the study are included in the article or uploaded as supplementary information. For more information, collaborations or data access inquiries please contact Principal Investigator Dr. Shahirose Sadrudin Premji at premjis@yorku.ca
Ethics statements
Patient consent for publication
Not required.
Ethics approval
This study involves human participants and was approved by Aga Khan University (2020-4955-11327); Mount Royal University (102574); University of Calgary (REB 17-132148 MOD8) and York University Research Ethics Board (2020-184). Participants gave informed consent to participate in the study before taking part.
References
- 1. Rasmussen SA, Jamieson DJ. Pregnancy, postpartum care, and COVID-19 vaccination in 2021. JAMA 2021;325:1099–100. 10.1001/jama.2021.1683 [DOI] [PubMed] [Google Scholar]
- 2. Fahey JO, Shenassa E. Understanding and meeting the needs of women in the postpartum period: the perinatal maternal health promotion model. J Midwifery Womens Health 2013;58:613–21. 10.1111/jmwh.12139 [DOI] [PubMed] [Google Scholar]
- 3. Dekel S, Ein-Dor T, Ruohomäki A, et al. The dynamic course of Peripartum depression across pregnancy and childbirth. J Psychiatr Res 2019;113:72–8. 10.1016/j.jpsychires.2019.03.016 [DOI] [PubMed] [Google Scholar]
- 4. Riley LE, Jamieson DJ. Inclusion of pregnant and lactating persons in COVID-19 vaccination efforts. 174. American College of Physicians, 2021: 701–2. 10.7326/M21-0173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Food U, Administration D. Development and licensure of vaccines to prevent COVID-19: guidance for industry. Docket FDA-2020-D-1137. FDA, 2020. [Google Scholar]
- 6. Kelly JC, Carter EB, Raghuraman N, et al. Anti-Severe acute respiratory syndrome coronavirus 2 antibodies induced in breast milk after Pfizer-BioNTech/BNT162b2 vaccination. Am J Obstet Gynecol 2021;225:101–3. 10.1016/j.ajog.2021.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Gray KJ, Bordt EA, Atyeo C, et al. Coronavirus disease 2019 vaccine response in pregnant and lactating women: a cohort study. Am J Obstet Gynecol 2021;225:303.e1–303.e17. 10.1016/j.ajog.2021.03.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sculli MA, Formoso G, Sciacca L. COVID-19 vaccination in pregnant and lactating diabetic women. Nutr Metab Cardiovasc Dis 2021;31:2151-2155. 10.1016/j.numecd.2021.04.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Centers for Disease Control and Prevention . Interim clinical considerations for use of mRNA COVID-19 vaccines currently authorized in the United States, 2020. Available: https://www.cdc.gov/coronavirus/2019ncov/vaccines/recommendations/pregnancy.html#anchor_1628692641537
- 10. Pfizer BioNTech COVID-19 vaccine: what you need to know. Available: https://www.who.int/news-room/feature-stories/detail/who-can-take-the-pfizer-biontech-covid-19-vaccine
- 11. Vaccinating pregnant and lactating patients against COVID-19 | ACOG. Available: https://www.acog.org/clinical/clinical-guidance/practice-advisory/articles/2020/12/vaccinating-pregnant-and-lactating-patients-against-covid-19
- 12. World Health Organization . Coronavirus disease (COVID-19): herd immunity, lockdowns and COVID-19, 2020. Available: https://www.who.int/news-room/q-a-detail/herd-immunity-lockdowns-and-covid-19
- 13. Mehta NS, Mytton OT, Mullins EWS, et al. SARS-CoV-2 (COVID-19): what do we know about children? A systematic review. Clin Infect Dis 2020;71:2469–79. 10.1093/cid/ciaa556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Oliver SE, Gargano JW, Marin M, et al. The Advisory Committee on Immunization Practices' Interim Recommendation for Use of Pfizer-BioNTech COVID-19 Vaccine - United States, December 2020. MMWR Morb Mortal Wkly Rep 2020;69:1922. 10.15585/mmwr.mm6950e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Pfizer-BioNTech announce positive Topline results of pivotal COVID-19 vaccine study in adolescents. Available: https://www.pfizer.com/news/press-release/press-release-detail/pfizer-biontech-announce-positive-topline-results-pivotal
- 16. Canada H. Available: https://www.canada.ca/en/health-canada/news/2021/05/health-canada-authorizes-use-of-the-pfizer-biontech-covid-19-vaccine-in-children-12-to-15-years-of-age.html
- 17. Benin AL, Wisler-Scher DJ, Colson E, et al. Qualitative analysis of mothers' decision-making about vaccines for infants: the importance of trust. Pediatrics 2006;117:1532–41. 10.1542/peds.2005-1728 [DOI] [PubMed] [Google Scholar]
- 18. Aschwanden C. Five reasons why COVID herd immunity is probably impossible. Nature 2021;591:520–2. 10.1038/d41586-021-00728-2 [DOI] [PubMed] [Google Scholar]
- 19. Kadkhoda K. Herd immunity to COVID-19: alluring and elusive. American Journal of Clinical Pathology 2021;155:471–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Anderson RM, Vegvari C, Truscott J, et al. Challenges in creating herd immunity to SARS-CoV-2 infection by mass vaccination. Lancet 2020;396:1614–6. 10.1016/S0140-6736(20)32318-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Britton T, Ball F, Trapman P. A mathematical model reveals the influence of population heterogeneity on herd immunity to SARS-CoV-2. Science 2020;369:846–9. 10.1126/science.abc6810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Dubé E, Laberge C, Guay M, et al. Vaccine hesitancy. Hum Vaccin Immunother 2013;9:1763–73. 10.4161/hv.24657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Sallam M. COVID-19 vaccine Hesitancy worldwide: a Concise systematic review of vaccine acceptance rates. Vaccines 2021;9:160. 10.3390/vaccines9020160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Hawlader MDH, Rahman ML, Nazir A, et al. COVID-19 vaccine acceptance in South Asia: a multi-country study. Int J Infect Dis 2022;114:1–10. 10.1016/j.ijid.2021.09.056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Skirrow H, Barnett S, Bell S. Women’s views on accepting COVID-19 vaccination during and after pregnancy, and for their babies: A multi-methods study in the UK. medRxiv 2021:2021.04.30.21256240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Verger P, Scronias D, Dauby N, et al. Attitudes of healthcare workers towards COVID-19 vaccination: a survey in France and French-speaking parts of Belgium and Canada, 2020. Euro Surveill 2021;26. 10.2807/1560-7917.ES.2021.26.3.2002047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Szilagyi PG, Thomas K, Shah MD, et al. National Trends in the US Public’s Likelihood of Getting a COVID-19 Vaccine—April 1 to December 8, 2020. JAMA 2021;325:396–8. 10.1001/jama.2020.26419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lawrence T, Zubatsky M, Meyer D. The association between mental health diagnoses and influenza vaccine receipt among older primary care patients. Psychol Health Med 2020;25:1083–93. 10.1080/13548506.2020.1717557 [DOI] [PubMed] [Google Scholar]
- 29. Mohammed H, Roberts CT, Grzeskowiak LE, et al. Psychosocial determinants of pertussis and influenza vaccine uptake in pregnant women: a prospective study. Vaccine 2020;38:3358–68. 10.1016/j.vaccine.2020.02.020 [DOI] [PubMed] [Google Scholar]
- 30. Savas E, Tanriverdi D. Knowledge, attitudes and anxiety towards influenza A/H1N1 vaccination of healthcare workers in turkey. BMC Infect Dis 2010;10:1–6. 10.1186/1471-2334-10-281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Xu Y, Zhang R, Zhou Z, et al. Parental psychological distress and attitudes towards COVID-19 vaccination: a cross-sectional survey in Shenzhen, China. J Affect Disord 2021;292:552–8. 10.1016/j.jad.2021.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Tahir MJ, Saqlain M, Tariq W, et al. Population preferences and attitudes towards COVID-19 vaccination: a cross-sectional study from Pakistan. BMC Public Health 2021;21:1759. 10.1186/s12889-021-11814-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Kashif M, Fatima I, Ahmed AM, et al. Perception, willingness, barriers, and Hesitancy towards COVID-19 vaccine in Pakistan: comparison between healthcare workers and general population. Cureus 2021;13:e19106. 10.7759/cureus.19106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Jackson LA, Anderson EJ, Rouphael NG, et al. An mRNA Vaccine against SARS-CoV-2 - Preliminary Report. N Engl J Med 2020;383:1920–31. 10.1056/NEJMoa2022483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Mulligan MJ, Lyke KE, Kitchin N, et al. Phase I/II study of COVID-19 RNA vaccine BNT162b1 in adults. Nature 2020;586:589–93. 10.1038/s41586-020-2639-4 [DOI] [PubMed] [Google Scholar]
- 36. Mundt JC, Marks IM, Shear MK, et al. The work and social adjustment scale: a simple measure of impairment in functioning. Br J Psychiatry 2002;180:461–4. 10.1192/bjp.180.5.461 [DOI] [PubMed] [Google Scholar]
- 37. Lee SA. How much "Thinking" about COVID-19 is clinically dysfunctional? Brain Behav Immun 2020;87:97–8. 10.1016/j.bbi.2020.04.067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Ceulemans M, Foulon V, Panchaud A, et al. Vaccine Willingness and Impact of the COVID-19 Pandemic on Women’s Perinatal Experiences and Practices—A Multinational, Cross-Sectional Study Covering the First Wave of the Pandemic. Int J Environ Res Public Health 2021;18:3367. 10.3390/ijerph18073367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Skjefte M, Ngirbabul M, Akeju O, et al. COVID-19 vaccine acceptance among pregnant women and mothers of young children: results of a survey in 16 countries. Eur J Epidemiol 2021;36:197–211. 10.1007/s10654-021-00728-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Solís Arce JS, Warren SS, Meriggi NF, et al. COVID-19 vaccine acceptance and hesitancy in low- and middle-income countries. Nat Med 2021;27:1385–94. 10.1038/s41591-021-01454-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Arshad MS, Hussain I, Mahmood T, et al. A national survey to assess the COVID-19 vaccine-related conspiracy beliefs, acceptability, preference, and willingness to pay among the general population of Pakistan. Vaccines 2021;9:720. 10.3390/vaccines9070720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Davis CJ, Golding M, McKay R. Efficacy information influences intention to take COVID-19 vaccine. Br J Health Psychol 2022;27:300–19. 10.1111/bjhp.12546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. de Figueiredo A, Simas C, Karafillakis E, et al. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: a large-scale retrospective temporal modelling study. Lancet 2020;396:898–908. 10.1016/S0140-6736(20)31558-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Viqar S. ‘We are your brothers, we will know where you are at all times’: risk, violence and positionality in Karachi. Contemp Soc Sci 2018;13:386–96. 10.1080/21582041.2017.1418526 [DOI] [Google Scholar]
- 45. Abbas S, Isaac N, Zia M, et al. Determinants of women's empowerment in Pakistan: evidence from demographic and health surveys, 2012-13 and 2017-18. BMC Public Health 2021;21:1328. 10.1186/s12889-021-11376-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Wilson RJ, Paterson P, Jarrett C, et al. Understanding factors influencing vaccination acceptance during pregnancy globally: a literature review. Vaccine 2015;33:6420–9. 10.1016/j.vaccine.2015.08.046 [DOI] [PubMed] [Google Scholar]
- 47. Mahmood N. Women’s Role In Domestic Decisionmaking In Pakistan: Implications For Reproductive Behaviour. The Pakistan Development Review 2002;41:121–48. 10.30541/v41i2pp.121-148 [DOI] [Google Scholar]
- 48. Bukhsh A, Rehman H, Mallhi TH, et al. Parents' attitude, awareness and behaviour towards influenza vaccination in Pakistan. Hum Vaccin Immunother 2018;14:952–7. 10.1080/21645515.2017.1415686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Rhodes A, Hoq M, Measey M-A, et al. Intention to vaccinate against COVID-19 in Australia. Lancet Infect Dis 2021;21:e110. 10.1016/S1473-3099(20)30724-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Paul E, Steptoe A, Fancourt D. Attitudes towards vaccines and intention to vaccinate against COVID-19: implications for public health communications. The Lancet Regional Health - Europe 2021;1:100012. 10.1016/j.lanepe.2020.100012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Al-Mohaithef M, Padhi BK. Determinants of COVID-19 vaccine acceptance in Saudi Arabia: a web-based national survey. J Multidiscip Healthc 2020;13:1657–63. 10.2147/JMDH.S276771 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Abebe H, Shitu S, Mose A. Understanding of COVID-19 vaccine knowledge, attitude, acceptance, and Determinates of COVID-19 vaccine acceptance among adult population in Ethiopia. Infect Drug Resist 2021;14:2015–25. 10.2147/IDR.S312116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Truong J, Bakshi S, Wasim A, et al. What factors promote vaccine hesitancy or acceptance during pandemics? A systematic review and thematic analysis. Health Promot Int 2022;37:daab105. 10.1093/heapro/daab105 [DOI] [PubMed] [Google Scholar]
- 54. Hilyard KM, Freimuth VS, Musa D, et al. The vagaries of public support for government actions in case of a pandemic. Health Aff 2010;29:2294–301. 10.1377/hlthaff.2010.0474 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55. Yurttas B, Poyraz BC, Sut N, et al. Willingness to get the COVID-19 vaccine among patients with rheumatic diseases, healthcare workers and general population in turkey: a web-based survey. Rheumatol Int 2021;41:1105–14. 10.1007/s00296-021-04841-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Salali GD, Uysal MS. COVID-19 vaccine hesitancy is associated with beliefs on the origin of the novel coronavirus in the UK and turkey. Psychol Med 2020:1–3. 10.1017/S0033291720004067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Bateson M, Brilot B, Nettle D. Anxiety: an evolutionary approach. Can J Psychiatry 2011;56:707–15. 10.1177/070674371105601202 [DOI] [PubMed] [Google Scholar]
- 58. Nesse RM. Natural selection and the regulation of defenses: a signal detection analysis of the smoke detector principle. Evolution and Human Behavior 2005;26:88–105. [Google Scholar]
- 59. Palgi Y, Bergman YS, Ben-David B, et al. No psychological vaccination: vaccine hesitancy is associated with negative psychiatric outcomes among Israelis who received COVID-19 vaccination. J Affect Disord 2021;287:352–3. 10.1016/j.jad.2021.03.064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Hunink MGM, Weinstein MC, Wittenberg E. Decision making in health and medicine: integrating evidence and values, 2014. [Google Scholar]
- 61. Van den Bos K, Lind EA. Uncertainty management by means of Fairness judgments. Adv Exp Soc Psychol 2002;34:1–60. [Google Scholar]
- 62. Lee C-J, Nagler RH, Wang N. Source-specific exposure to contradictory nutrition information: documenting prevalence and effects on adverse cognitive and behavioral outcomes. Health Commun 2018;33:453–61. 10.1080/10410236.2016.1278495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Li J-Y, Wen TJ, McKeever R, et al. Uncertainty and negative emotions in parental decision-making on childhood vaccinations: extending the theory of planned behavior to the context of conflicting health information. J Health Commun 2021;26:215–24. 10.1080/10810730.2021.1913677 [DOI] [PubMed] [Google Scholar]
- 64. Schmid P, MacDonald NE, Habersaat K, et al. Commentary to: how to respond to vocal vaccine deniers in public. Vaccine 2018;36:196–8. 10.1016/j.vaccine.2016.09.065 [DOI] [PubMed] [Google Scholar]
- 65. Briñol P, Rucker DD, Petty RE. Naïve theories about persuasion: implications for information processing and consumer attitude change. Int J Advert 2015;34:85–106. 10.1080/02650487.2014.997080 [DOI] [Google Scholar]
- 66. Fishbein M, Ajzen I. Belief, attitude, intention, and behavior: an introduction to theory and research. Philosophy and Rhetoric 1977;10. [Google Scholar]
- 67. Stühlinger M, Schmutz JB, Grote G, et al. To get vaccinated or not? psychological safety as a catalyst for the alignment between individual beliefs and behavior. Group Organ Manag 2021;46:38–69. 10.1177/1059601120983964 [DOI] [Google Scholar]
- 68. Rogers R, Prentice-Dunn S, Gochman D. Handbook of health behavior research 1: personal and social determinants. 505. New York, NY, US: Plenum Press, Xxviii, 1997: 113–32. [Google Scholar]
- 69. Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process 1991;50:179–211. 10.1016/0749-5978(91)90020-T [DOI] [Google Scholar]
- 70. Sniehotta FF, Scholz U, Schwarzer R. Bridging the intention–behaviour gap: planning, self-efficacy, and action control in the adoption and maintenance of physical exercise. Psychol Health 2005;20:143–60. 10.1080/08870440512331317670 [DOI] [Google Scholar]
- 71. Zeng Y, Yuan Z, Yin J, et al. Factors affecting parental intention to vaccinate kindergarten children against influenza: a cross-sectional survey in China. Vaccine 2019;37:1449–56. 10.1016/j.vaccine.2019.01.071 [DOI] [PubMed] [Google Scholar]
- 72. Shahzad A. Threats of cellphone blocks, work bans boost Pakistan’s vaccination rate Asia Pacific, 2021. Available: https://www.reuters.com/world/asia-pacific/threats-cellphone-blocks-work-bans-boost-pakistans-vaccination-rate-2021-08-05/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request. All data relevant to the study are included in the article or uploaded as supplementary information. For more information, collaborations or data access inquiries please contact Principal Investigator Dr. Shahirose Sadrudin Premji at premjis@yorku.ca