Abstract
Background
Metabolic profiles differ between healthy humans and those with inflammatory bowel disease. Few studies have examined metabolic profiles in dogs with chronic enteropathy (CE).
Hypothesis
Serum metabolic profiles of dogs with CE are significantly different from those of healthy dogs.
Animals
Fifty‐five dogs with CE and 204 healthy controls.
Methods
A cross‐sectional study. The serum concentrations of 99 metabolites measured using a canine‐specific proton nuclear magnetic resonance spectroscopy platform were studied. A 2‐sample unpaired t‐test was used to compare the 2 study samples. The threshold for significance was set at P < .05 with a Bonferroni correction for each metabolite group.
Results
Nineteen metabolites and 18 indices of lipoprotein composition were significantly different between the CE and healthy dogs. Four metabolites were significantly higher in dogs with CE, including phenylalanine (mean and SD) (healthy: 0.0417 mmol/L; [SD] 0.0100; CE: 0.0480 mmol/L; SD: 0.0125; P value: <.001) and lactate (healthy: 1.8751 mmol/L; SD: 0.7808; CE: 2.4827 mmol/L; SD CE: 1.4166; P value: .003). Fifteen metabolites were significantly lower in dogs with CE, including total fatty acids, and glycine (healthy: 0.2273 mmol/L; SD: 0.0794; CE: 0.1828 mmol/L; SD CE: 0.0517; P value: <.001).
Conclusions and Clinical Importance
The metabolic profile of dogs with CE is significantly different from that of healthy dogs, this opens novel research avenues to develop better diagnostic and prognostic approaches as well as therapeutic trials.
Keywords: amino acid, canine, glycoprotein acetyls, lipid, metabolomics
Abbreviations
- 1H NMR
proton nuclear magnetic resonance
- ACTH
adrenocorticotrophic hormone
- APTT
activated partial thromboplastin time
- CE
chronic enteropathy
- CI
confidence interval
- cPLI
canine pancreas specific lipase
- GC‐MS
gas chromatography coupled to mass spectrometry
- GPA
glycoprotein acetyls
- HDL
high density lipoproteins
- HfSA
Hospital for Small Animals
- IBD
inflammatory bowel disease
- LC‐MS
liquid chromatography coupled with single‐stage or tandem mass spectrometry
- PT
prothrombin time
- PUFAs
polyunsaturated fatty acids
- R(D)SVS
Royal (Dick) School of Veterinary Studies
- TLI
trypsin‐like immunoreactivity
- VLDL
very low‐density lipoprotein
1. INTRODUCTION
Chronic enteropathy (CE) is a common cause of gastrointestinal disease in dogs. It is characterized by a several week history of signs of gastrointestinal (GI) disease, and histopathological evidence of inflammatory infiltrates in the GI tract, in the absence of any underlying metabolic, infectious, or neoplastic causes. 1 It is subtyped based upon response to treatment as either food‐responsive, 2 antibiotic‐responsive, 3 immunosuppression‐responsive, 4 or nonresponsive. 5
The etiology of CE is hypothesized to be a series of complex interactions between the host genome, microbiome, lack of immune tolerance and intraluminal dietary components. 1 , 6 The degree of inflammation shows marked interobserver variability dependant on scoring system used, 7 does not consistently correlate with clinical signs, 8 nor does it predict the response to treatment, 9 and clinical remission often does not correlate with histological remission. 10 Therefore, it remains challenging for the clinician to both diagnose and prognosticate based on current diagnostic approaches. In an effort to improve the diagnostic accuracy, reduce invasive testing and to better predict and monitor the response to treatment of dogs with CE, the clinical utility of measuring multiple biomarkers has been explored. 11 Of these, few are routinely used in clinical practice, mainly because of limitations concerning availability of testing and individual variation. 11 , 12
Similar challenges exist in the human field, where the clear need to noninvasively assess and personalize treatment for diseases such as ulcerative colitis and Crohn's disease resulted in the extensive study of metabolic profiling. Several serum metabolites consistently differ between healthy individuals and those suffering from inflammatory bowel disease (IBD), which might allow differentiation between subtypes. 13 , 14 , 15 This not only provides a series of potential biomarkers, but also offers insights into the potential pathogenesis of these conditions. This gives rise to the hope that measuring serum metabolites might be able to reduce the clinical need of more invasive testing such as endoscopic biopsies in dogs.
Assessment of serum metabolites can be undertaken using a wide range of analytical platforms. In contrast to other commonly used metabolomics techniques such as gas chromatography coupled to mass spectrometry (GC‐MS) and liquid chromatography coupled with mass spectrometry (LC‐MS), proton nuclear magnetic resonance (1H NMR) spectroscopy provides a high speed, high throughput, and highly reproducible method. 16 Increased availability of these techniques has facilitated the recent expansion of metabolomic studies in both human and veterinary medicine.
Metabolomic profiles between dogs with CE and healthy individuals are not well characterized. Several recent studies documented differences in lipid and amino acid profiles in dogs with CE, 17 , 18 however comprehensive metabolomic studies are lacking. Significant variance has been identified in the phospholipid profiles of dogs with IBD and food responsive enteropathy, and before and after treatment. 17 Alterations in amino acid profiles are identified in dogs with IBD, and whilst correlating with clinical disease severity, these did not reflect the histological inflammation or C‐reactive protein concentrations. 18
This study measures a large panel of serum metabolites in dogs with a CE using a canine‐specific 1H NMR metabolomics platform. We hypothesize that serum metabolic profiles of dogs with CE are significantly different from healthy dogs. The aim of this study is to, therefore, compare the metabolomic profiles between healthy dogs and dogs with histopathologically confirmed CE.
2. MATERIALS AND METHODS
This study was performed at the Royal (Dick) School of Veterinary Studies and was approved by the University of Edinburgh Veterinary Ethics Review Committee.
Dogs were classified as having a CE if they had a >3‐wk history of signs of GI disease, confirmation of an inflammatory infiltrate of the lamina propria on histopathology from endoscopic intestinal biopsies, and exclusion of other causative processes. Signs of GI disease were classified as 1 or more of: vomiting, diarrhea, increased borborygmi or flatus, abdominal pain, increased or decreased appetite and weight loss or bloating. In order to exclude other causative processes, dogs were required to have no clinically relevant abnormalities on hematology, biochemistry, abdominal ultrasound, fecal parasitology including giardia antigen and a resting or post ACTH stimulated cortisol >2 μg/dL (>55 nmol/L) to exclude hypoadrenocorticism. Other investigations performed at the discretion of the clinician included canine pancreas‐specific lipase, trypsin‐like immunoreactivity, urine analysis +/− urine protein: creatinine ratio, abdominal and/or thoracic radiographs, T4 and TSH, and coagulation parameters (PT and APTT). A canine IBD activity index (CIBDAI) score was recorded in all dogs with a CE, where this was not available it was calculated from clinical records. 19 Empiric deworming was performed at the discretion of the clinician but was not considered an exclusion criterion.
Healthy controls were defined as dogs presenting for an annual vaccination to the university teaching hospital without any abnormalities detected on history or physical examination. Samples were collected between November 2014 and July 2018.
After sampling, blood was placed into plain blood collection tubes (as per manufacturer's instructions), which were refrigerated immediately after collection. Serum was separated by centrifugation within 4 hours of collection and aliquoted. Samples were stored frozen at −80°C until analysis. Before analysis samples were inspected for any evidence of hemolysis, or lipemia and sample quality noted.
All samples were analyzed using a Bruker AVANCE III HD 500 1H NMR spectrometer (Bruker Biospin, Rheinstetten, Germany). The canine‐specific platform has been recently validated and reference intervals for the individual metabolites determined by Ottka et al. 20 Ninety‐nine metabolites were analyzed, from 8 metabolite group, consisting of amino acids, cholesterols, fatty acids, glycolysis related metabolites, inflammatory markers, ketone bodies, lipoprotein subclass particles, and triglycerides, as outlined in Figure 1.
FIGURE 1.
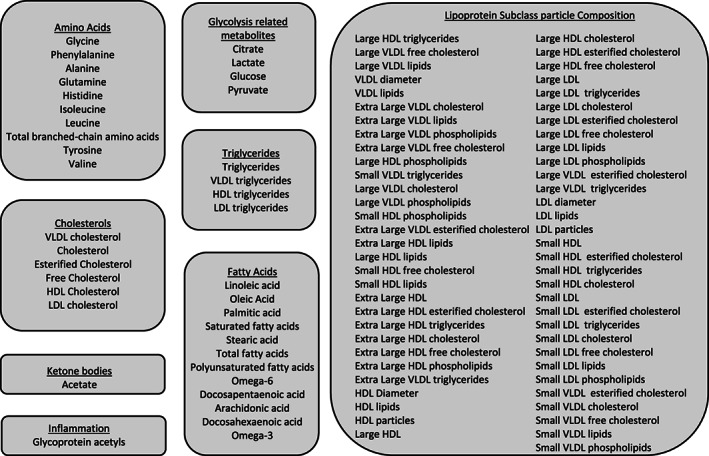
Metabolite subgroups tested in dogs with 55 dogs with chronic enteropathy compared to a healthy study sample of 204 dogs, measured using 1NMR Spectroscopy
Statistical analysis was performed using the R statistical system (R version 4.0.3 [October 10, 2020]). An unpaired 2‐sample t‐test was used to compare the 2 study samples as group sizes were sufficient, under the central limit theorem, to assume that sample means were normally distributed. The threshold for significance was set at P < .05 with a Bonferroni correction for each metabolite group by setting the critical P‐value for multiple comparisons to be .05 divided by the number of comparisons in each metabolite group.
3. RESULTS
3.1. Dogs
Fifty‐five dogs with CE were included in the analysis. The median age was 6 y (range, 6 mo‐12.5 y). These were from 25 breeds, and 7 dogs were mixed breed. The CIBDAI scores ranged from 1 to 15 with a median of 7. Five entire females, 19 neutered females, 13 entire males and 18 neutered male dogs were included in the CE cohort. The median weight was 22.25 kg (range, 4.3‐80 kg). The 10 most prevalent breeds included are outlined in Table 1. Drugs used before referral included: histamine blockers (famotidine, cimetidine, and ranitidine), antibiotics (metronidazole, enrofloxacin, trimethoprim sulfonamide, and potentiated amoxicillin), hyoscine butylbromide, probiotics, omeprazole, meloxicam, tramadol, metoclopramide, phenylpropanolamine, oclacitinib, maropitant, thyroxine, and chlorphenamine. One dog was receiving prednisolone orally at physiological dose (0.2 mg/kg q24 hours). Empiric deworming with fenbendazole at 50 mg/kg orally for 5 consecutive days was performed in 38 dogs.
TABLE 1.
Ten most prevalent breeds of 55 dogs with chronic enteropathy and 204 healthy controls used in metabolomic analysis using 1NMR Spectroscopy
| Ten most prevalent breeds of 55 dogs with chronic enteropathy | Number of Dogs | Percentage | Ten most prevalent breeds of 204 healthy controls | Number of Dogs | Percentage |
|---|---|---|---|---|---|
| Labrador | 13 | 24 | Mixed Breed | 52 | 26 |
| Mixed Breed | 7 | 13 | Labrador | 28 | 14 |
| Border terrier | 3 | 5 | English Cocker Spaniel | 17 | 8 |
| Border Collie | 3 | 5 | English Springer Spaniel | 13 | 6 |
| Irish Setter | 3 | 5 | Golder Retriever | 8 | 4 |
| Lurcher | 2 | 4 | Jack Russel Terrier | 6 | 3 |
| Golder Retriever | 2 | 4 | Greyhound | 6 | 3 |
| Jack Russel Terrier | 2 | 4 | Border Terrier | 5 | 2 |
| Rottweiller | 2 | 4 | Whippet | 4 | 2 |
| Rhodesian Ridgeback | 2 | 4 | Hungarian Vizsla | 4 | 2 |
Two hundred four healthy controls were used. These were from 47 breeds, and 52 dogs were mixed breed. Of the healthy controls, 96 were neutered females, 10 were entire females, 72 were neutered males, 26 were entire males. They had a median age of 3 y (range, 6 mo‐16 y). The median weight of control dogs was 20.95 kg (range, 3.1‐70 kg). The 10 most prevalent breeds from the healthy control group are outlined in Table 1. An unpaired t‐test did not identify a significant difference between the ages of the 2 groups of dogs (P = .15) or the weights of the 2 groups (P = .26).
3.2. Metabolites
A significant difference was identified in 19 metabolites and 18 indices of lipoprotein composition between the healthy and CE groups. Four metabolites were significantly higher in dogs with CE than healthy controls: the amino acid phenylalanine, the ketone body acetate, and the glycolysis related metabolites citrate and lactate. Fifteen metabolites were significantly lower in dogs with CE than healthy dogs, outlined in Table 2, including several fatty acids; the amino acid glycine, total triglycerides, very low‐density lipoprotein triglycerides and high‐density lipoprotein triglycerides, glycoprotein acetyls and very low‐density lipoprotein cholesterol. The 18 indices of lipoprotein subclass particle composition that showed statistical significance are outlined in Table 3. No samples were recorded to be grossly lipemic or hemolytic.
TABLE 2.
Metabolite concentrations with significant differences in dogs with chronic enteropathy compared to a healthy study sample, measured using 1NMR Spectroscopy
| Metabolite | Group | Unit | Reference interval | Mean Healthy | SD Healthy | Range Healthy | Mean CE | SD CE | Range CE | P value | Critical Value |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Acetate | Ketone Bodies | mmol/L | 0.021‐0.037 | 0.0227 | 0.0054 | 0.013‐0.047 | 0.0256 | 0.0077 | 0.011‐0.052 | .010 | 0.05 |
| Citrate | Glycolysis related metabolites | mmol/L | 0.061‐0.123 | 0.0871 | 0.0249 | 0.053‐0.302 | 0.1000 | 0.0284 | 0.056‐0.158 | .003 | 0.0125 |
| Docosapentaenoic acid | Fatty Acids | mmol/L | 0.125‐0.361 | 0.2447 | 0.0724 | 0.107‐0.579 | 0.2057 | 0.0801 | 0.062‐0.481 | .0016 | 0.0041 |
| Glycine | Amino Acids | mmol/L | 0.130‐0.454 | 0.2273 | 0.0794 | 0.074‐0.631 | 0.1828 | 0.0517 | 0.100‐0.353 | <.001 | 0.005 |
| Glycoprotein acetyls | Inflammation | mmol/L | 0.597‐1.028 | 0.8230 | 0.2207 | 0.506‐1.829 | 0.7656 | 0.1626 | 0.546‐1.297 | .034 | 0.05 |
| HDL triglycerides | Triglycerides | mmol/L | 0.003‐0.076 | 0.0517 | 0.0348 | 0.000‐0.186 | 0.0327 | 0.0254 | 0.000‐0.120 | <.001 | 0.0125 |
| Lactate | Glycolysis related metabolites | mmol/L | 1.184‐3.581 | 1.8751 | 0.7808 | 0.553‐6.846 | 2.4827 | 1.4166 | 0.792‐9.441 | .0033 | 0.0125 |
| Linoleic acid | Fatty Acids | mmol/L | 2.495‐5.892 | 4.2844 | 1.0007 | 2.350‐8.203 | 3.4460 | 1.1153 | 2.039‐7.757 | <.001 | 0.0041 |
| Oleic Acid | Fatty Acids | mmol/L | 1.265‐2.796 | 2.1554 | 0.7010 | 1.056‐4.662 | 1.5565 | 0.5276 | 0.796‐3.271 | <.001 | 0.0041 |
| Omega‐6 | Fatty Acids | mmol/L | 4.148‐9.810 | 6.8996 | 1.5983 | 3.678‐12.890 | 5.9244 | 1.8162 | 3.261‐13.036 | <.001 | 0.0041 |
| Palmitic acid | Fatty Acids | mmol/L | 1.837‐3.616 | 2.9405 | 0.7081 | 1.760‐5.668 | 2.3799 | 0.5846 | 1.592‐4.413 | <.001 | 0.0041 |
| Phenylalanine | Amino Acids | mmol/L | 0.030‐0.065 | 0.0417 | 0.0100 | 0.024‐0.098 | 0.0480 | 0.0125 | 0.024‐0.095 | <.001 | 0.005 |
| Polyunsaturated fatty acids | Fatty Acids | mmol/L | 4.723‐11.141 | 7.8617 | 1.7837 | 4.100‐15.413 | 6.7669 | 2.0155 | 3.783‐14.517 | <.001 | 0.0041 |
| Saturated fatty acids | Fatty Acids | mmol/L | 3.588‐7.431 | 5.7232 | 1.3384 | 3.241‐10.381 | 4.6880 | 1.2452 | 2.749‐9.034 | <.001 | 0.0041 |
| Stearic acid | Fatty Acids | mmol/L | 1.744‐3.842 | 2.7828 | 0.6501 | 1.482‐5.077 | 2.3082 | 0.6817 | 1.041‐4.621 | <.001 | 0.0041 |
| Total fatty acids | Fatty Acids | mmol/L | 9.741‐20.972 | 15.7403 | 3.7177 | 8.773‐30.089 | 13.0114 | 3.7015 | 7.805‐26.747 | <.001 | 0.0041 |
| Triglycerides | Triglycerides | mmol/L | 0.190‐1.004 | 0.7942 | 0.5226 | 0.152‐3.790 | 0.5067 | 0.3379 | 0.124‐1.584 | <.001 | 0.0125 |
| VLDL cholesterol | Cholesterol | mmol/L | 0.027‐0.311 | 0.1970 | 0.1529 | 0.004‐0.925 | 0.1261 | 0.1356 | 0.013‐0.905 | .0012 | 0.0083 |
| VLDL triglycerides | Triglycerides | mmol/L | 0.000‐0.705 | 0.5540 | 0.4832 | 0.030‐3.304 | 0.2822 | 0.3086 | 0.000‐1.291 | <.001 | 0.0125 |
TABLE 3.
Lipoprotein subclass particle composition with significant differences in dogs with chronic enteropathy compared to a healthy study sample measured using 1NMR Spectroscopy
| Metabolite | Unit | Reference Interval | Mean Healthy | SD Healthy | Range Healthy | Mean CE | SD CE | Range CE | P value | Critical Value |
|---|---|---|---|---|---|---|---|---|---|---|
| Extra Large VLDL esterified cholesterol | mmol/L | 0.001‐0.028 | 0.0193 | 0.02 | 0.001‐0.094 | 0.01 | 0.01 | 0.001‐0.048 | <0.0008 | 0.0008 |
| Extra Large VLDL cholesterol | mmol/L | 0.000‐0.060 | 0.0452 | 0.0544 | 0.000‐0.284 | 0.0167 | 0.0263 | 0.000‐0.127 | <0.0008 | 0.0008 |
| Extra Large VLDL free cholesterol | mmol/L | 0.001‐0.045 | 0.0340 | 0.0364 | 0.001‐0.191 | 0.0139 | 0.0180 | 0.001‐0.087 |
<0.0008 |
0.0008 |
| Extra Large VLDL lipids | mmol/L | 0.001‐0.264 | 0.2205 | 0.2594 | 0.001‐1.394 | 0.0911 | 0.1294 | 0.002‐0.653 | <0.0008 | 0.0008 |
| Extra Large VLDL phospholipids | mmol/L | 0.001‐0.054 | 0.0405 | 0.0485 | 0.001‐0.275 | 0.0146 | 0.0205 | 0.001‐0.106 | <0.0008 | 0.0008 |
| Large HDL lipids | mmol/L | 4.966‐8.260 | 6.1179 | 0.7381 | 3.986‐8.349 | 5.5368 | 1.0208 | 2.915‐7.441 | <0.0008 | 0.0008 |
| Large HDL phospholipids | mmol/L | 2.481‐3.936 | 2.9923 | 0.3259 | 2.174‐3.851 | 2.7367 | 0.3796 | 1.853‐3.447 | <0.0008 | 0.0008 |
| Large HDL triglycerides | mmol/L | 0.003‐0.028 | 0.0200 | 0.0106 | 0.004‐0.060 | 0.0127 | 0.0081 | 0.001‐0.039 | <0.0008 | 0.0008 |
| Large VLDL cholesterol | mmol/L | 0.004‐0.132 | 0.0877 | 0.0762 | 0.002‐0.410 | 0.0468 | 0.0586 | 0.002‐0.314 | <0.0008 | 0.0008 |
| Large VLDL free cholesterol | mmol/L | 0.002‐0.080 | 0.0587 | 0.0532 | 0.003‐0.284 | 0.0277 | 0.0310 | 0.002‐0.132 | <0.0008 | 0.0008 |
| Large VLDL lipids | mmol/L | 0.010‐0.600 | 0.4304 | 0.3815 | 0.004‐2.414 | 0.2047 | 0.2468 | 0.005‐1.173 | <0.0008 | 0.0008 |
| Large VLDL phospholipids | mmol/L | 0.001‐0.105 | 0.0676 | 0.0666 | 0.001‐0.333 | 0.0367 | 0.0370 | 0.001‐0.154 | <0.0008 | 0.0008 |
| Small HDL free cholesterol | mmol/L | 0.093‐0.193 | 0.1283 | 0.0240 | 0.068‐0.224 | 0.1098 | 0.0341 | 0.022‐0.191 | <0.0008 | 0.0008 |
| Small HDL lipids | mmol/L | 1.268‐2.174 | 1.5239 | 0.2230 | 0.941‐2.288 | 1.3557 | 0.3217 | 0.432‐1.865 | <0.0008 | 0.0008 |
| Small HDL phospholipids | mmol/L | 0.724‐1.187 | 0.8549 | 0.1123 | 0.572‐1.205 | 0.7657 | 0.1524 | 0.332‐1.020 | <0.0008 | 0.0008 |
| Small VLDL triglycerides | mmol/L | 0.016‐0.157 | 0.1350 | 0.0795 | 0.023‐0.539 | 0.0884 | 0.0598 | 0.001‐0.288 | <0.0008 | 0.0008 |
| VLDL diameter | mmol/L | 35.261‐43.770 | 41.6472 | 3.0774 | 35.358‐57.942 | 39.0502 | 3.5107 | 35.005‐57.046 | <0.0008 | 0.0008 |
| VLDL lipids | mmol/L | 0.087‐1.154 | 0.8901 | 0.7528 | 0.107‐4.750 | 0.4684 | 0.4844 | 0.075‐2.503 | <0.0008 | 0.0008 |
4. DISCUSSION
This study highlights a significant difference in the metabolomic profile between dogs with CE and healthy controls, using a recently validated 1H NMR metabolomics platform. Alterations were identified in the serum concentrations of amino acids, fatty acids, glycolysis related metabolites, and lipid subclass composition.
Amino acid profiling has been widely investigated in human inflammatory enteropathies, and more recently has been studied in dogs with CE. Investigation of alterations in the amino acid signature of dogs with CE has highlighted tryptophan and serine as potential biomarkers in IBD. 18 , 21 , 26 In this study, glycine was significantly lower in dogs with CE than healthy dogs. This is in contrast to previous studies, in which no significant difference was identified in glycine levels between dogs with IBD or protein losing enteropathy and healthy controls. 18 , 21 Glycine is a simple amino acid, which functions as an anti‐inflammatory, immunomodulatory and cytoprotective molecule. 22 It suppresses TLR4 and NOD2 signaling in piglets challenged with lipopolysaccharide. 23 mRNA expression of TLR4 and NOD2 is dysregulated in CE. 24 , 25 Supplementation with glycine also decreases the clinical severity and inflammatory infiltrates in animal models of inflammatory enteropathies. 22 A possible explanation for the discordance between our findings and those of previous studies might lie in the smaller number of dogs used in one of these previous cohorts, or the differences in study samples analyzed, as previous studies included only dogs with immunosuppressive ‐ responsive enteropathy 26 and protein‐losing enteropathy. 21
In our study, in contrast to a previous pilot study, 26 phenylalanine concentration was found to be significantly higher in dogs with CE. This is also identified in humans, as people with ulcerative colitis have higher blood levels of phenylalanine than healthy controls. 27 The metabolism of phenylalanine relates to the enzyme phenylalanine hydroxylase, which is functionally reduced by inflammation, therefore this increased serum level might be an indirect result of inflammatory cytokines. 28
Aberrations in glycolysis related metabolites are documented in many disease states, driven by alterations in energy requirements. In this study, lactate was significantly higher in dogs with CE compared to the healthy study sample. Lactate measured by this 1H NMR spectrometer encompasses both L‐lactate and D‐lactate. Within human IBD, serum D‐Lactate has been identified to be significantly higher in peoples with Crohn's disease than healthy controls, because of increased intestinal production, and absorption facilitated by abnormal intestinal barrier function. 29 Within veterinary medicine, significant increases in fecal lactate concentrations are observed in dogs with CE. 30 Down‐regulation of genes responsible for maintaining intestinal barrier function is identified in dogs with CE, therefore the pathogenesis of increased lactate might mirror that seen in human medicine. 31 Alternatively, the increase in serum lactate might be a result of L‐lactate production, because of tissue hypoperfusion.
Total fatty acids were significantly lower in dogs with CE than healthy controls. Essential fatty acids are important mediators of inflammation, acting as both pro‐ and anti‐inflammatory intermediaries. Pro‐inflammatory mediators are metabolized via arachidonic acid and the cyclooxygenase pathway to form prostaglandins, thromboxanes, and leukotrienes. 32 In contrast, specialized pro‐resolving mediators are synthesized from omega‐3 essential fatty acids (eicosopentanoic acid and docosahexaenoic acid) to resolvins, protectins, and maresins and from omega‐6 fatty acids to lipoxins. 33 Dysregulation in these mediators in the face of chronic inflammation, is a feature of CE in people but has not been extensively investigated in dogs with CE. Interestingly, in comparison to that of amino acids, evidence of therapeutic response to essential fatty acids in people is limited, 34 However there is some evidence that supplementation of eicosopentanoic acid can improve inflammation and affect colonic differentiation markers and microbiota in people with ulcerative colitis. 35
Lipoprotein particle composition analysis is an emerging tool in human medicine. Whilst primarily used to look for dyslipidemias surrounding cardiovascular disease, there is some emerging data that dyslipidemias in human IBD might be an important potential focus for profiling and treating these patients. 36 , 37 Dyslipidemias are widely reported in dogs with CE, 17 and the role of proinflammatory cytokines on mediators of lipolysis such as lipoprotein lipase are suggested to have a role in these pathways in human medicine. 38
Glycoprotein acetyls (GPA) were significantly lower in dogs with CE than healthy controls. Glycoprotein acetyls are a novel NMR biomarker, which reflect the concentrations of certain acute‐phase glycoproteins, and in human medicine correlate with chronic inflammation. A recent NMR study in people identified GPA to be significantly higher in people with active IBD compared with healthy controls. 39 In addition, they accurately reflected the mucosal recovery to a healthy state in people with both Crohn's disease and ulcerative colitis. 39 The lower level of GPA in dogs with CE, compared with healthy controls is unexpected, although the literature surrounding the use of GPA as biomarkers in dogs is limited. Glycoprotein acetyl profiles in dogs differ from human profiles, and are affected by various medications. 40 , 41 As the medications before referral were not standardized the impact of these cannot be excluded. Equally, the lower level of GPA in dogs with CE might represent GI protein loss in our cohort.
The limitations of this study include a lack of standardized diets, lack of subtyping of CE, and the smaller number of dogs with CE than healthy controls. Six dogs had a serum albumin level below the lower reference limit which could have impacted the metabolome. The dogs were also exposed to different medications before referral including antibiotics and probiotics. Two dogs did not have a trypsin like immunoreactivity performed to exclude exocrine pancreatic insufficiency, and not all cases had empirical deworming. The body condition score of the healthy controls was not available to compare with the CE group, which could have impacts on the metabolome.
A number of animal and sample factors can influence the metabolome, and clinicians should endeavor to standardize these in follow up experiments. 42 Animal factors which could have affected the metabolome include a difference in the fasting status between the CE and control dogs, differences in medication exposure, and time of day of sampling. The dogs were not subdivided into age categories to enhance the statistical power, however again this represents a potential for variance. Sample factors which could have impacted the metabolome include the potential for different brand of serum tubes to be used over the 4 y collection period, differences in clotting time between dogs, and a difference in time to centrifugation. Whilst most amino acids are stable for 4 hours, there is some evidence that others might be affected. 43 There was also a difference in storage times between the samples before analysis. Samples were stored at −80°C for several years before analysis. In a previous study validating the NMR platform, all sample metabolites were stable at −80°C for 12 mo, 20 however evidence into the impact of longer storage on canine samples is lacking. Studies looking at human metabolites, however, have shown negligible effects after storage at −80°C for 2.5 y when using an NMR platform, 44 despite this, the effect of storage on the current study's samples cannot be excluded. No freeze thaw cycles were performed.
In conclusion, dogs with CE have significant alterations in lipid, amino acid, fatty acid and glycolysis related metabolites compared to healthy dogs. This study might open novel research avenues which could explore the diagnostic and prognostic utility of metabolite changes and guide the development of future therapeutic trials.
CONFLICT OF INTEREST
Claudia Ottka was an employee and Hannes Lohi is a shareholder and the chairman of the board of PetBIOMICS Ltd, who developed and provides the metabolomics test. No other authors have a conflict of interest.
OFF‐LABEL ANTIMICROBIAL DECLARATION
Authors declare no off‐label use of antimicrobials.
INSTITUTIONAL ANIMAL CARE AND USE COMMITTEE (IACUC) OR OTHER APPROVAL DECLARATION
Approved by the University of Edinburgh Animal Welfare and Ethics Review Board.
HUMAN ETHICS APPROVAL DECLARATION
Authors declare human ethics approval was not needed for this study.
ACKNOWLEDGMENT
Study was partially supported by PetBIOMICS Ltd. Preliminary data was presented in abstract form at the 31st ECVIM‐CA Online Congress. The authors thank Dr. Jenni Puurunen for her helpful input to the manuscirpt.
Walker HK, Boag AM, Ottka C, et al. Serum metabolomic profiles in dogs with chronic enteropathy. J Vet Intern Med. 2022;36(5):1752‐1759. doi: 10.1111/jvim.16419
Funding information Partially supported by PetBIOMICS Ltd
REFERENCES
- 1. Dandrieux JR. Inflammatory bowel disease versus chronic enteropathy in dogs: are they one and the same? J Small Anim Pract. 2016;57(11):589‐599. doi: 10.1111/jsap.12588 [DOI] [PubMed] [Google Scholar]
- 2. Allenspach K, Culverwell C, Chan D. Long‐term outcome in dogs with chronic enteropathies: 203 cases. Vet Rec. 2016;178(15):368. doi: 10.1136/vr.103557 [DOI] [PubMed] [Google Scholar]
- 3. Hall EJ. Antibiotic‐responsive diarrhea in small animals. Vet Clin North Am Small Anim Pract. 2011;41(2):273‐286. doi: 10.1016/j.cvsm.2010.12.004 [DOI] [PubMed] [Google Scholar]
- 4. Allenspach K, Rüfenacht S, Sauter S, et al. Pharmacokinetics and clinical efficacy of cyclosporine treatment of dogs with steroid‐refractory inflammatory bowel disease. J Vet Intern Med. 2006;20(2):239‐244. doi: 10.1892/0891-6640(2006)20[239:paceoc]2.0.co;2 [DOI] [PubMed] [Google Scholar]
- 5. Allenspach K, Wieland B, Gröne A, Gaschen F. Chronic enteropathies in dogs: evaluation of risk factors for negative outcome. J Vet Intern Med. 2007;21(4):700‐708. doi: 10.1892/0891-6640(2007)21[700:ceideo]2.0.co;2 [DOI] [PubMed] [Google Scholar]
- 6. German AJ, Hall EJ, Day MJ. Chronic intestinal inflammation and intestinal disease in dogs. J Vet Intern Med. 2003;17(1):8‐20. doi: [DOI] [PubMed] [Google Scholar]
- 7. Willard MD, Jergens AE, Duncan RB. Interobserver variation among histopathologic evaluations of intestinal tissues from dogs and cats. J Am Vet Med Assoc. 2002;220(8):1177‐1182. doi: 10.2460/javma.2002.220.1177 [DOI] [PubMed] [Google Scholar]
- 8. Allenspach KA, Mochel JP, Du Y, et al. Correlating gastrointestinal histopathologic changes to clinical disease activity in dogs with idiopathic inflammatory bowel disease. Vet Pathol. 2019;56(3):435‐443. doi: 10.1177/0300985818813090 [DOI] [PubMed] [Google Scholar]
- 9. Day MJ, Bilzer T, Mansell J, et al. Histopathological standards for the diagnosis of gastrointestinal inflammation in endoscopic biopsy samples from the dog and cat: a report from the World Small Animal Veterinary Association Gastrointestinal Standardization Group. J Comp Pathol. 2008;138(Suppl 1):S1‐S43. doi: 10.1016/j.jcpa.2008.01.001 [DOI] [PubMed] [Google Scholar]
- 10. García‐Sancho M, Rodríguez‐Franco F, Sainz A, et al. Evaluation of clinical, macroscopic, and histopathologic response to treatment in nonhypoproteinemic dogs with lymphocytic‐plasmacytic enteritis. J Vet Intern Med. 2007;21(1):11‐17. doi: 10.1892/0891-6640(2007)21[11:eocmah]2.0.co;2 [DOI] [PubMed] [Google Scholar]
- 11. Heilmann RM, Steiner JM. Clinical utility of currently available biomarkers in inflammatory enteropathies of dogs. J Vet Intern Med. 2018;32(5):1495‐1508. doi: 10.1111/jvim.15247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Heilmann RM. Important and novel laboratory parameters and biomarkers for canine chronic enteropathy. Adv Small Animal Care. 2020;1:111‐125. doi: 10.1016/j.yasa.2020.07.009 [DOI] [Google Scholar]
- 13. Storr M, Vogel HJ, Schicho R. Metabolomics: is it useful for inflammatory bowel diseases? Curr Opin Gastroenterol. 2013;29(4):378‐383. doi: 10.1097/MOG.0b013e328361f488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Williams HR, Willsmore JD, Cox IJ, et al. Serum metabolic profiling in inflammatory bowel disease. Dig Dis Sci. 2012;57(8):2157‐2165. doi: 10.1007/s10620-012-2127-2 [DOI] [PubMed] [Google Scholar]
- 15. Schicho R, Shaykhutdinov R, Ngo J, et al. Quantitative metabolomic profiling of serum, plasma, and urine by (1)H NMR spectroscopy discriminates between patients with inflammatory bowel disease and healthy individuals. J Proteome Res. 2012;11(6):3344‐3357. doi: 10.1021/pr300139q [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Emwas AH, Roy R, McKay RT, et al. NMR spectroscopy for metabolomics research. Metabolites. 2019;9(7):123. doi: 10.3390/metabo9070123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kalenyak K, Heilmann RM, van de Lest CHA, Brouwers JF, Burgener IA. Comparison of the systemic phospholipid profile in dogs diagnosed with idiopathic inflammatory bowel disease or food‐responsive diarrhea before and after treatment. PLoS One. 2019;14(4):e0215435. doi: 10.1371/journal.pone.0215435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tamura Y, Ohta H, Kagawa Y, et al. Plasma amino acid profiles in dogs with inflammatory bowel disease. J Vet Intern Med. 2019;33(4):1602‐1607. doi: 10.1111/jvim.15525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Jergens AE, Schreiner CA, Frank DE, et al. A scoring index for disease activity in canine inflammatory bowel disease. J Vet Intern Med. 2003;17(3):291‐297. doi: 10.1111/j.1939-1676.2003.tb02450.x [DOI] [PubMed] [Google Scholar]
- 20. Ottka C, Vapalahti K, Puurunen J, et al. A novel canine nuclear magnetic resonance spectroscopy‐based metabolomics platform: validation and sample handling. Vet Clin Pathol. 2021;50(3):410‐426. doi: 10.1111/VCP.12954 [DOI] [PubMed] [Google Scholar]
- 21. Kathrani A, Allenspach K, Fascetti AJ, Larsen JA, Hall EJ. Alterations in serum amino acid concentrations in dogs with protein‐losing enteropathy. J Vet Intern Med. 2018;32(3):1026‐1032. doi: 10.1111/jvim.15116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Liu Y, Wang X, Hu CA. Therapeutic potential of amino acids in inflammatory bowel disease. Nutrients. 2017;9(9):920. doi: 10.3390/nu9090920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Liu Y, Wang X, Wu H, et al. Glycine enhances muscle protein mass associated with maintaining Akt‐mTOR‐FOXO1 signaling and suppressing TLR4 and NOD2 signaling in piglets challenged with LPS. Am J Physiol Regul Integr Comp Physiol. 2016;311(2):R365‐R373. doi: 10.1152/ajpregu.00043.2016 [DOI] [PubMed] [Google Scholar]
- 24. Heilmann RM, Allenspach K. Pattern‐recognition receptors: signaling pathways and dysregulation in canine chronic enteropathies—brief review. J Vet Diagn Invest. 2017;29(6):781‐787. doi: 10.1177/1040638717728545 [DOI] [PubMed] [Google Scholar]
- 25. Aono K, Azuma YT, Nabetani T, et al. Correlation between toll‐like receptor 4 and nucleotide‐binding oligomerization domain 2 (NOD2) and pathological severity in dogs with chronic gastrointestinal diseases. Vet Immunol Immunopathol. 2019;210:15‐22. doi: 10.1016/j.vetimm.2019.03.003 [DOI] [PubMed] [Google Scholar]
- 26. Benvenuti E, Pierini A, Gori E, et al. Serum amino acid profile in 51 dogs with immunosuppressant‐responsive enteropathy (IRE): a pilot study on clinical aspects and outcomes. BMC Vet Res 2020;16(1):117. doi: 10.1186/s12917-020-02334-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Santoru ML, Piras C, Murgia A, et al. Cross sectional evaluation of the gut‐microbiome metabolome axis in an Italian cohort of IBD patients. Sci Rep. 2017;7(1):9523. doi: 10.1038/s41598-017-10034-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Chen WS, Wang CH, Cheng CW, et al. Elevated plasma phenylalanine predicts mortality in critical patients with heart failure. ESC Heart Fail. 2020;7(5):2884‐2893. doi: 10.1002/ehf2.12896 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Cai J, Chen H, Weng M, Jiang S, Gao J. Diagnostic and clinical significance of serum levels of D‐lactate and diamine oxidase in patients with Crohn's disease. Gastroenterol Res Pract. 2019;2019:8536952‐8536957. doi: 10.1155/2019/8536952 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Blake AB, Guard BC, Honneffer JB, Lidbury JA, Steiner JM, Suchodolski JS. Altered microbiota, fecal lactate, and fecal bile acids in dogs with gastrointestinal disease. PLoS One. 2019;14(10):e0224454. doi: 10.1371/journal.pone.0224454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wilke VL, Nettleton D, Wymore MJ, et al. Gene expression in intestinal mucosal biopsy specimens obtained from dogs with chronic enteropathy. Am J Vet Res. 2012;73(8):1219‐1229. doi: 10.2460/ajvr.73.8.1219 [DOI] [PubMed] [Google Scholar]
- 32. Ma C, Vasu R, Zhang H. The role of long‐chain fatty acids in inflammatory bowel disease. Mediators Inflamm. 2019;2019:8495913‐8495910. doi: 10.1155/2019/8495913 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Serhan CN, Dalli J, Colas RA, Winkler JW, Chiang N. Protectins and maresins: new pro‐resolving families of mediators in acute inflammation and resolution bioactive metabolome. Biochim Biophys Acta. 2015;1851(4):397‐413. doi: 10.1016/j.bbalip.2014.08.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Charpentier C, Chan R, Salameh E, et al. Dietary n‐3 PUFA may attenuate experimental colitis. Mediators Inflamm. 2018;2018:8430614‐8430610. doi: 10.1155/2018/8430614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Prossomariti A, Scaioli E, Piazzi G, et al. Short‐term treatment with eicosapentaenoic acid improves inflammation and affects colonic differentiation markers and microbiota in patients with ulcerative colitis. Sci Rep. 2017;7(1):1‐10. doi: 10.1038/s41598-017-07992-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bjerrum JT, Steenholdt C, Ainsworth M, et al. Metabonomics uncovers a reversible proatherogenic lipid profile during infliximab therapy of inflammatory bowel disease. BMC Med. 2017;15(1):184. doi: 10.1186/s12916-017-0949-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Sappati Biyyani RS, Putka BS, Mullen KD. Dyslipidemia and lipoprotein profiles in patients with inflammatory bowel disease. J Clin Lipidol. 2010;4(6):478‐482. doi: 10.1016/j.jacl.2010.08.021 [DOI] [PubMed] [Google Scholar]
- 38. Romanato G, Scarpa M, Angriman I, et al. Plasma lipids and inflammation in active inflammatory bowel diseases. Aliment Pharmacol Ther. 2009;29(3):298‐307. doi: 10.1111/j.1365-2036.2008.03886.x [DOI] [PubMed] [Google Scholar]
- 39. Dierckx T, Verstockt B, Vermeire S, van Weyenbergh J. GlycA, a nuclear magnetic resonance spectroscopy measure for protein glycosylation, is a viable biomarker for disease activity in IBD. J Crohns Colitis. 2019;13(3):389‐394. doi: 10.1093/ecco-jcc/jjy162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Ottka C, Weber C, Müller E, et al. Serum NMR metabolomics uncovers multiple metabolic changes in phenobarbital‐treated dogs. Metabolomics. 2021;17(6):1‐11. doi: 10.1007/S11306-021-01803-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Behrens AJ, Duke RM, Petralia LM, et al. Glycosylation profiling of dog serum reveals differences compared to human serum. Glycobiology. 2018;28(11):825‐831. doi: 10.1093/glycob/cwy070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. González‐Domínguez R, González‐Domínguez Á, Sayago A, Fernández‐Recamales Á. Recommendations and best practices for standardizing the pre‐analytical processing of blood and urine samples in metabolomics. Metabolites. 2020;10(6):229. doi: 10.3390/metabo10060229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. An Z, Shi C, Li P, Liu L. Stability of amino acids and related amines in human serum under different preprocessing and pre‐storage conditions based on iTRAQ®‐LC‐MS/MS. Biol Open. 2021;10(2):bio055020. doi: 10.1242/bio.055020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Pinto J, Domingues MR, Galhano E, et al. Human plasma stability during handling and storage: impact on NMR metabolomics. Analyst. 2014;139(5):1168‐1177. doi: 10.1039/c3an02188b [DOI] [PubMed] [Google Scholar]


