Abstract
Background
Growth monitoring (GM) is a preventive activity that serves as the core function in an integrated child health and nutrition programme. In most developing nations, including Ethiopia, however, the use of GM service is insufficient. Hence, the purpose of this study was to evaluate the use of GM services and associated characteristics among mothers of infants in Mettu town, Southwest Ethiopia.
Objective
To assess the utilisation of GM service by mothers of infants in Mettu town, Southwest Ethiopia, 2021.
Method
A community-based cross-sectional study was conducted among 354 randomly selected mothers with children aged 0–23 months old from 25 June to 27 July 2021 in Mettu town. EpiData V.4.6.0 was used to enter data, which were then exported to SPSS V.25 for analysis. Simple binary and multivariable logistic regression analyses were performed to identify factors associated with GM service utilisation.
Results
A total of 354 study participants were included in the study, yielding a response rate of 95.2%. The proportion of GM service utilisation was 25.2% (95% CI: 20.24% to 29.33%). In multivariable regression analysis, age of index child 0–11 months (AOR (adjusted OR)=1.58; 95% CI: 1.052 to 3.713), early postnatal care (PNC) (AOR=1.72; 95% CI: 1.657 to 6.467), middle tertile wealth status (AOR=0.108; 95% CI: 0.047 to 0.319) and lower tertile wealth status (AOR=0.073; 95% CI: 0.013 to 0.874), utilisation of family health cards (AOR=2.09; 95% CI: 1.384 to 5.343) and taking ≤30 min to reach the nearest health facility (AOR=2.23; 95% CI: 2.061 to 7.350) were significantly associated with GM service utilisation.
Conclusion and recommendation
In this study, only one-fourth of mothers with children aged 0–23 months old were using GM services. GM service utilisation was found to be significantly associated with child age, early PNC visit, wealth status, utilisation of family health cards and time taking ≤30 min to reach the nearest health facility. Hence, appropriate strategies that promote and encourage GM service utilisation should be designed.
Keywords: Adolescent Health, Growth, Obesity, Growth Monitoring, Utilization, Mettu town, Children Aged 0-23 months
WHAT IS ALREADY KNOWN ON THIS TOPIC
GM service is one of the several preventive programs aimed at combating early childhood growth faltering and malnutrition.
WHAT THIS STUDY ADDS
In the current study, only one-fourth of mothers with a 0-23 month-old child were attended GM serves.
HOW THIS STUDY MIGHT AFFECT RESEARCH, PRACTICE OR POLICY
Hence, appropriate strategies that promote and encourage GM service utilization should be designed.
Introduction
Growth monitoring (GM) is defined as the regular measurement, plotting and interpreting of a child’s growth on a regular basis in order to respond when abnormal growth is noticed, with the aim of improving the child’s nutritional status. Improved nutritional status, increased utilisation of healthcare services and subsequent reduction in mortality are the main potential advantages of GM service.1 2
The majority of GM services are provided in health institutions or in communities. The main advantages of GM are that it helps families and community workers to identify children with growth failure early, when it is easier to intervene.3–5
Child growth and development is one of the major public health problems in low/middle-income countries.6 Poor child growth is attributed to a greater childhood mortality as a result of severe infections and increased susceptibility to common childhood illnesses, which account for the majority of deaths among children under the age of 5 years.7 Malnutrition is directly or indirectly responsible for about half of all childhood deaths worldwide.8 In 2019, there were 149 million children under the age of 5 years in the world. Out of those, 49 million were stunted, 17 million were severely wasted and 40 million were overweight.9
In Ethiopia, child malnutrition is a serious public health concern. According to the Ethiopian Mini Demographic and Health Survey of 2019, 37% of children under the age of 5 years were stunted, 21% were underweight and 7% were wasted. Similarly, in the Oromia region, 35.6% of children were stunted, 16.1% were underweight and 4.7% were wasted.10 In terms of the country’s economic losses, the estimated annual cost of child malnutrition is 55.5 billion Ethiopian birr, or 16.5% of gross domestic product.11
The most cost-effective method for tracking the challenging public health problem of malnutrition is through various preventive techniques, including GM service. This includes ensuring that all children who had normal weight at birth remain in that range, and that those who had low weight at birth are quickly brought into a healthy growth range.3
It is critical to promote and improve a child’s health during the window of opportunity that lasts from conception to the child’s second birthday.12 Despite the fact that GM is one of the activities that the Ethiopian government is currently focusing on to combat child malnutrition, only a few mothers brought their children for this service.13 14 Studies done in different parts of Ethiopia revealed that only 16.9%–38.9% of mothers were attending GM services.14–19 Lack of appropriate information about GM service, lack of support from husbands, distance from the health facility, pastoral lifestyle and cultural issues such as the fear of ‘evil eye’ were factors contributing to the utilisation of GM service.17 20
The irregularity of the GM session due to health extension workload, not recording the age and weight of the child accurately, the mother’s wrong belief and the skill gap of health extension workers were challenges to GM service utilisation.17 Since 2008, Ethiopia has adopted GM as a nutrition-specific intervention, but utilisation of GM services has been limited.13
However, limited evidence is available on the level of utilisation of the GM services in Mettu town. Hence, this study is intended to find out how widely GM services are being used and what factors have affected the programme in Mettu town.
Materials and methods
Study area and period
The study was conducted in Mettu town from 25 June to 27 July 2021, which is located in the I/A/Bor Zone, Oromia region, Southwest Ethiopia and is 542 km from Addis Ababa, the capital city of Ethiopia. Mettu is a market town with six administrative kebeles. One health centre, one specialised hospital and three health posts are found in the town. The total population of the town is estimated to be 49 538. The under 5 and under 2 age groups were estimated to be 8139 and 2828, respectively.
Study design and population
A community-based cross-sectional study was employed from 25 June to 27 July 2021. All mothers who have children aged 0–23 months old and live in Mettu town were the source population, whereas mothers who have children aged 0–23 months and selected by simple random sampling from the sampling frame were the study population and included in the study.
Eligibility criteria
Inclusion criteria
Mothers with children aged 0–23 months old who have lived in Mettu town for at least 6 months were included in the study.
Exclusion criteria
Mothers who were unable to respond due to medical or psychiatric illness were excluded.
Sample size determination
The minimum required sample size was calculated using a double population proportion formula using Epi Info V.7 by considering the assumptions, 80% power of the study, 95% confidence level, 1:1 ratio and proportion of outcome for the variable, and place of delivery (33.33% exposed and 10.33% non-exposed). After adding a 10% non-response rate, the final sample size for the study was 372 (table 1).
Table 1.
Sample size determination to assess the utilisation of growth monitoring service by mothers of infants in Mettu town, Southwest Ethiopia, 2021
| S/N | Variable | Assumptions | Sample size | Reference | |||||
| CI (%) | Power (%) | Ratio | AOR | Proportion of outcome | |||||
| Exposed | Non-exposed | ||||||||
| 1 | Place of delivery | 95 | 80 | 1:1 | 3.0 | 33.33% | 10.33% | 372 | 18 |
| 2 | Family health card | 95 | 80 | 1:1 | 5.09 | 57.86% | 11.14% | 139 | 20 |
| 3 | Distance from nearby health facility | 95 | 80 | 1:1 | 4.53 | 33.90% | 8.0% | 359 | 19 |
AOR, adjusted OR.
Sampling techniques and procedures
To achieve the desired sample size, all six urban kebeles were included in the study. Initially, a sampling frame consisting a list of 2828 mother–child pairs with children aged 0–23 months old, along with the child’s date of birth and house number, was obtained from the respective health posts. Then samples representing each kebele were calculated using a proportional to population size allocation.
Finally, a simple random sampling technique was employed using a computer-generated program (Microsoft Excel) to select a total of 372 samples from the six urban kebeles.
Data collection procedures and tools
Data were collected from mothers using a semistructured interviewer-administered questionnaire. The questionnaire was adapted from previous similar studies.17 20 21 The questionnaire was first prepared in English and then translated to Afan Oromo and back to English to check the consistency by an expert who had good ability in both languages. The questionnaire was divided into five sections: sociodemographic and economic information; child and maternal health characteristics; mother–child feeding knowledge; maternal knowledge of the WHO growth chart and GM service; and the availability and accessibility of health services.
Data were collected by six diploma clinical nurses and two BSc nurses were recruited as supervisors during data collection. The younger child from the household was taken as an index child, and if twin children were found within one household, data were taken from one of them using the lottery method. If an eligible mother was absent during the data collection period, a revisit was done three times, and mothers absent on the third visit were considered non-respondent.
Data quality control
Before data collection, the questionnaires were pretested on a 5% (20) sample size in another town, which was not part of the actual data collection area. Based on the pretest, some modifications, such as unclear or vague questions and wrong skip patterns, were corrected. Two days of training was given for data collectors and supervisors by the principal investigator on data collection tools, data collection techniques, approach to the interviews, and maintaining the privacy and confidentiality of the respondents. Every day after data collection, the questionnaires were reviewed and checked for completeness by the supervisors and the principal investigator.
Patient and public involvement
No patient involved in this study.
Operational definition
GM utilisation: if the mother participated in the GM services at least once for her 0-month-old child, at least two times for her child 1–3 months old, at least five times for her child 4–11 months and at least four times per year for her child 12–23 months old. In addition, it should be plotted or recorded on the child’s growth chart.18 22
Family health card utilisation: the mother is considered to have used the family health card if she had the card at home, plotted and able to interpret information displayed on the weight-for-age child growth chart during every GM session.
Early postnatal care (PNC): the care given to the woman and her newborn at least once from the second day through the seventh day after delivery.23
Family health card: a book which contains the weight-for-age child growth chart for both sexes and used to plot the growth pattern of the child attending GM session and would need to be held by the mother.
Wealth index: measured using fixed household asset. Factor score was derived using the Principal Component Analysis (PCA) then the composite score was ranked into three tertiles.24
Data processing and analysis
All data were checked visually, coded and entered into EpiData V.4.6.0 before being exported to SPSS V.25 for analysis. Descriptive statistics (frequency and cross-tabulation) were calculated for variables. The results were presented in the form of tables and text using frequencies and summary statistics such as mean, SD and percentage to describe the study population with relevant variables.
Before performing PCA for variables explaining the household wealth index, all the necessary assumptions and prerequisites were checked. The degree of association between independent and dependent variables was assessed using an OR with a 95% CI. A simple binary logistic regression analysis was performed to select candidate variables for multivariable regression analysis. Variables with a p value of <0.25 were taken as a cut-off point to select eligible variables for the multivariable regression analysis, and a p value of <0.05 was declared as statistically significant in the final model.
Pseudo-regression was performed to check multicollinearity between independent variables. The minimum tolerance and maximum variance inflation factor were found to be 0.80 and 1.89, respectively. For the finally fitted multivariable logistic regression model, the adequacy of the model to predict the outcome variables was checked by Hosmer-Lemeshow goodness-of-fit and p>0.05.
Result
Sociodemographic and economic characteristics of households
In this study, a total of 354 mother–child pairs were included, yielding a response rate of 95.2%. The mean age of the children was 11.25 (6.433) months and more than half of the children (187, 52.8%) belonged to the age category below 11 months. Regarding the age of respondents, the majority (329, 92.9%) of them were in the age category below 30 years. The mean age of the mothers was 24.91 (3.472) years. More than half of the respondents (181, 51.2%) had secondary and above education. Nearly half (160, 45.3%) of the respondents were housewives. In terms of wealth status, 116 (32.8%) and 93 (26.2%) ranked in the higher and lower tertiles, respectively (table 2).
Table 2.
Demographic and socioeconomic characteristics of mothers of infants in Mettu town, 2021 (n=354)
| Variable | Categories | Frequency | Percentage |
| Sex of child | Male | 184 | 51.98 |
| Female | 170 | 48.02 | |
| Age of child (months) | 0–11 | 187 | 52.8 |
| 12–23 | 167 | 47.2 | |
| Maternal age | <30 | 329 | 92.9 |
| ≥30 | 25 | 7.1 | |
| Religion of mother | Orthodox | 136 | 38.5 |
| Muslim | 111 | 31.4 | |
| Protestant | 96 | 27 | |
| Others* | 11 | 3.1 | |
| Ethnicity of mother | Oromo | 289 | 81.7 |
| Amhara | 36 | 10.1 | |
| Gurage | 14 | 4 | |
| Others† | 15 | 4.2 | |
| Level of education | No formal education | 32 | 9 |
| Primary | 141 | 39.8 | |
| Secondary and above | 181 | 51.2 | |
| Occupational status | Housewife | 160 | 45.3 |
| Merchant | 36 | 10.2 | |
| Government employee | 53 | 14.9 | |
| Private employee | 48 | 13.7 | |
| Student | 39 | 10.9 | |
| Others†‡ | 18 | 4.97 | |
| Current marital status | Married | 321 | 90.7 |
| Single | 20 | 5.6 | |
| Divorced | 11 | 3.1 | |
| Widowed | 2 | 0.6 | |
| Family size | <3 | 96 | 27.2 |
| 4–5 | 165 | 46.5 | |
| >5 | 93 | 26.3 | |
| Wealth status | Lower tertile | 93 | 26.2 |
| Middle tertile | 145 | 41 | |
| Higher tertile | 116 | 32.8 |
*Catholic, Wakefata and Jiohava.
†Kambata, Hadiya, Tigre, Agnuak and Nuer.
‡Daily labourerand farmer.
Information on availability of health facilities with specific health services
In this study, nearly half (168, 47.5%) of the study participants took 30 min or less to reach the nearest health facility. More than two-thirds (272, 76.7%) of the respondents prefer to go to health centres for their children’s care. Regarding the perceived awareness of the respondents to the availability of GM services, half of (187, 52.8%) of the respondents were aware of the availability of GM services at health facilities (table 3).
Table 3.
Information on availability and accessibility of health services among mother–child pairs, Mettu town, 2021 (n=354)
| Variable | Category | Frequency | Percentage | |
| Time it takes to the nearest health facility | ≤30 min | 168 | 47.5 | |
| >30 min | 186 | 52.5 | ||
| The most frequently visited health facility for childcare | Health centre | 272 | 76.7 | |
| Health post | 9 | 2.5 | ||
| Private clinic | 51 | 14.3 | ||
| Hospital | 23 | 6.5 | ||
| Perceived awareness on availability of specific health services |
ANC | Yes | 318 | 89.8 |
| No | 36 | 10.2 | ||
| Delivery | Yes | 301 | 85.1 | |
| No | 53 | 14.9 | ||
| PNC | Yes | 242 | 68.3 | |
| No | 112 | 31.7 | ||
| GMP | Yes | 187 | 52.8 | |
| No | 167 | 47.2 | ||
ANC, antenatal care; GMP, growth monitoring and promotion; PNC, postnatal care.
Information on utilisation of maternal and child health service
Among 354 mothers who participated in this study, more than half (181, 55.5%) had antenatal care follow-up with a frequency of four or more visits. The majority of the mothers (334, 94.4%) delivered at health institutions, but only one-third (123, 34.8%) of the mothers had early PNC (table 4).
Table 4.
Variables used to assess the information on MCH service among mothers and their children, Mettu, Ethiopia, 2021 (n=354)
| Variable | Category | Frequency | Percentage |
| ANC follow-up | No | 25 | 7.1 |
| Yes | 329 | 92.9 | |
| Frequency of ANC follow-up | <4 visits | 147 | 44.8 |
| ≥4 visits | 181 | 55.5 | |
| Place of delivery | Home | 20 | 5.6 |
| Health institution | 334 | 94.4 | |
| Early PNC | No | 231 | 65.2 |
| Yes | 123 | 34.8 | |
| Vaccination status of the child | Not vaccinated | 9 | 2.5 |
| Vaccinating | 137 | 38.8 | |
| Defaulter | 6 | 1.6 | |
| Fully vaccinated | 202 | 57.1 | |
| Reason for not getting vaccinated | Distance to EPI sites | 1 | 12.5 |
| Do not know the benefit | 8 | 87.5 |
ANC, antenatal care; EPI, Extended Programm of Immunization; MCH, maternal and child health; PNC, postnatal care.
Reasons for frequent health facility visits by mothers
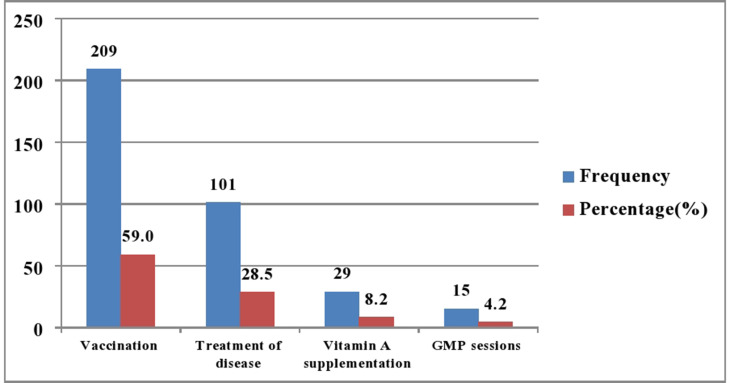
This study revealed that nearly two-thirds (209, 59.0%) of the mothers frequently visit health facilities to have their children vaccinated, but only 15 (4.3%) of the mothers who participated in the study took their children for weighing or GM service (figure 1).
Figure 1.
Mothers’ most common reasons to visit health facilities, Mettu town, 2021 (n=354). GMP, growth monitoring and promotion.
Child feeding and GM knowledge of mothers
The finding of this study reported that the majority of the respondents (310, 87.6%) were counselled on child feeding. Almost all respondents (347, 98.1%) provided breast milk to their babies immediately after birth. Nearly half (166, 46.9%) of the study participants were using family health cards, and the majority (153, 92.05%) of those mothers were able to read and interpret information displayed on the growth chart (table 5).
Table 5.
Child feeding and growth chart knowledge of mothers, Mettu town, 2021 (n=354)
| Variable | Category | Frequency | Percentage |
| Counselled by HCWs on child feeding | No | 44 | 12.4 |
| Yes | 310 | 87.6 | |
| The first thing given after birth | Breast milk | 347 | 98.1 |
| Other* | 7 | 1.86 | |
| Time for BF initiation immediately after birth | Within 1 hour | 342 | 96.7 |
| Greater than 1 hour | 11 | 3.1 | |
| Duration of EBF | 3 months | 7 | 1.9 |
| 6 months | 344 | 97.2 | |
| 1 year | 3 | 0.9 | |
| Total duration of BF | Below 2 years | 33 | 9.33 |
| 2 years and greater | 321 | 90.68 | |
| Use family health card at home | No | 188 | 53.1 |
| Yes | 166 | 46.9 | |
| Can read information displayed on growth chart | No | 13 | 7.95 |
| Yes | 153 | 92.05 | |
| Who thought you | HCWs | 99 | 64.95 |
| By myself | 46 | 30.01 | |
| HEWs | 8 | 5.04 | |
| What does it mean if growth curve flattens | Child not growing well | 72 | 46.8 |
| Child may be sick | 31 | 20.3 | |
| Child not eating well | 50 | 32.9 | |
| What does it mean if growth curve rises | Child gaining weight | 89 | 58.4 |
| Child is healthy | 16 | 10.6 | |
| Child is eating well | 48 | 31.0 | |
| What does it mean if growth curve is falling | Child is not gaining weight | 66 | 43.2 |
| Child may be sick or has been sick | 36 | 23.4 | |
| Child is not eating well | 51 | 33.4 |
*Formula milk, water or cow milk.
BF, breast feeding; EBF, exclusive breast feeding; HCWs, healthcare workers; HEWs, health extension workers.
Utilisation of GM services
This study revealed that one-fourth of (89, 25.2%) mothers used GM service (95% CI: 20.24 to 29.33). Of those respondents who participated in this study, nearly two-thirds (196, 60.9%) knew the benefit of GM. Regarding the benefits of the GM service, half (108, 50.5%) of the respondents reported the GM service is used ‘to monitor the child’s growth’. More than two-thirds (59, 66.7%) of the respondents followed GM sessions at health centres (table 6).
Table 6.
Variables to assess utilisation of GM, Mettu town, 2021 (n=354)
| Variable | Category | Frequency | Percentage |
| GM utilisation status | Used | 89 | 25.2 |
| Not used | 265 | 74.8 | |
| Know benefit of regular GM session | Yes | 216 | 60.9 |
| No | 138 | 29.1 | |
| Benefit of regularly taking the child for GM session | To monitor growth | 108 | 50.0 |
| To seek medical care | 7 | 3.06 | |
| To know health status | 101 | 46.94 | |
| Place where GM service is given | Health centre | 59 | 66.7 |
| EPI outreach sites | 8 | 8.45 | |
| Health posts | 22 | 24.85 | |
| Who provides the service | HEWs | 30 | 33.15 |
| HCWs | 59 | 66.8 |
EPI, Extended Programm of Immunization; GM, growth monitoring; HCWs, healthcare workers; HEWs, health extension workers.
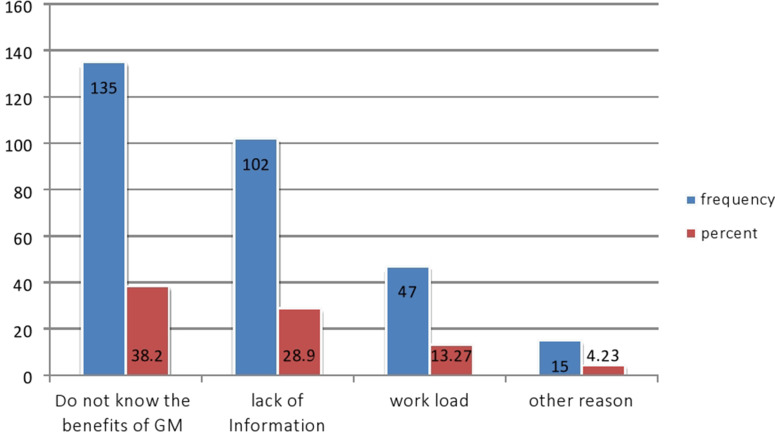
Reasons for not taking the child for GM session
This study reported that more than one-third (135, 38.2%) of the respondents who missed taking the child for GM sessions did not know the benefits of the GM services, and 102 (28.9%) of the mothers lacked information about the services (figure 2).
Figure 2.
Reasons for not regularly taking the child for GM session, Mettu town, 2021 (n=354). GM, growth monitoring.
Factors associated with GM service utilisation
On multivariable logistic regression analysis, mothers with children aged 0–11 months old (adjusted OR (AOR)=1.58; 95% CI: 1.052 to 3.713), mothers who had early PNC (AOR=1.72; 95% CI: 1.657 to 6.467), mothers from households with middle (AOR=0.108; 95% CI: 0.047 to 0.319) and lower tertiles (AOR=0.073; 95% CI: 0.013 to 0.874), mothers using family health cards at home (AOR=2.09; 95% CI: 1.384 to 5.343), and mothers who took 30 min and below to reach the nearest health facility (AOR=2.24; 95% CI: 2.061 to 7.350) were factors significantly associated with utilisation of GM service (table 7).
Table 7.
Bivariable and multivariable logistic regression analyses of utilisation of growth monitoring (GM) service by mothers of infants in Mettu town, 2021 (n=354)
| Variable | Category | Utilisation of GM service | 95% CI | ||
| Yes (%) | No (%) | COR | AOR | ||
| Age of index child | 12–23 months | 32 (9.01) | 135 (38.2) | 1 | 1 |
| ≤11 months | 57 (16.15) | 130 (36.6) | 1.87 (1.112 to 3.143) | 1.58 (1.052 to 3.713)* | |
| Frequency of ANC visit | <4 | 28 (7.91) | 107 (30.22) | 1 | |
| ≥4 | 61 (17.23) | 110 (31.07) | 2.12 (1.204 to 3.519) | 1.16 (0.579 to 2.305) | |
| Early PNC | No | 46 (13.04) | 185 (52.2) | 1 | |
| Yes | 43 (12.1) | 80 (22.7) | 2.14 (1.277 to 3.577) | 1.72 (1.657 to 6.467)* | |
| Maternal level of education | No formal education | 6 (1.60) | 26 (7.40) | 1 | |
| Primary | 27 (7.51) | 114 (32.25) | 1.17 (0.404 to 3.356) | 0.645 (0.179 to 2.320) | |
| Secondary and above | 56 (15.8) | 125 (35.4) | 2.15 (0.775 to 5.946) | 0.319 (0.088 to 1.160) | |
| Wealth status | Higher tertile | 62 (17.5) | 54 (15.25) | 1 | 1 |
| Middle tertile | 17 (4.80) | 128 (36.16) | 0.116 (0.016 to 0.311) | 0.108 (0.047 to 0.319)* | |
| Lower tertile | 10 (2.82) | 83 (23.45) | 0.099 (0.012 to 0.697) | 0.073 (0.013 to 0.874)* | |
| Family health card utilisation | No | 33 (9.31) | 155 (43.8) | 1 | |
| Yes | 56 (15.8) | 110 (31.1) | 2.40 (1.427 to 4.027) | 2.09 (1.384 to 5.343)* | |
| Perceived awareness on GMP availability | No | 27 (7.76) | 133 (37.6) | 1 | |
| Yes | 62 (17.4) | 132 (37.3) | 2.26 (1.323 to 3.858) | 1.67 (0.871 to 3.203) | |
| Time to reach nearby health facility | >30 min | 31 (8.76) | 155 (43.78) | 1 | |
| ≤30 min | 58 (16.38) | 110 (31.07) | 2.64 (2.410 to 7.297) | 2.23 (2.061 to 7.350)* | |
*Denote statistically significant variables in multivariable logistic regression at p<0.05.
ANC, antenatal care; AOR, adjusted OR; COR, crude OR; GMP, growth monitoring and promotion; PNC, postnatal care.
Discussion
GM services are essential until the child’s second birthday in order to have a healthy and well-nourished child and to break the intergenerational cycle of malnutrition. Hence, this study was aimed to assess utilisation of GM services and associated factors among mothers of children aged 0–23 months old in Mettu town. The proportion of GM service utilisation in this study area was found to be 25.2% (95% CI: 20.24% to 29.33%). This finding is comparable with a study conducted in rural lower parts of Ghana (28.5%) and Northern Ethiopia (30.7%).20 25
The finding of this study is lower compared with a study conducted in the Lawra district of Ghana (70%) and Nyamira county of Kenya (53.3%).16 26 The inconsistency might be due to differences in socioeconomic characteristics among the study population, study design and study period.
However, the finding of the current study was higher compared with a study done in Thika subcity of Kenya (20%), Mareka district, Southern Ethiopia (16.9%) and Butajira district, Southern Ethiopia (11%).17 18 27 Differences in study setting, socioeconomic and demographic characteristics of study participants, and study period could all explain the disparity.
The age of the index child was found to be significantly associated with the utilisation of GM and promotion services. Mothers with index children under 11 months were 1.5 times more likely to use the service compared with mothers with index children aged 12–23 months old. The possible explanation might be that children under 11 months old are recommended going to a health facility for several doses of immunisation. Thus, most mothers will continue to send them to weighing centres until completion of the immunisation. However, as the child’s age advances, attendance at GM sessions decreases. This finding is similar to a study conducted in rural Ghana, which discovered a negative correlation between child age and GM service utilisation.25 In contrast to this finding, a study conducted in the Legambo district of South Wollo zone and Mareka found that mothers with index children aged 12–24 months were more likely to use GM services than those with children aged 11 months or less.18 19 The inconsistency might be due to the differences in study design and sampling technique employed. The study conducted in Legambo district used an unmatched case–control study design, which may have contributed to this variation.
This study found that mothers who had early PNC were 1.7 times more likely to use GM services compared with those mothers who had no early PNC. This relationship between early PNC service and higher utilisation of GM could be explained by the child nutrition and health counselling that is provided as part of the PNC service. As a result, they could get more opportunities to receive child growth and development counselling. This study is supported by a study conducted in Benin that reported mothers who had early PNC were more likely to use maternal and child health services.28
Utilisation of family health cards was another predictor of GM services in this study. Those mothers using family health cards were two times more likely to use GM services compared with those who were not. This might be due to the possibility of family health cards motivating mothers to get GM service. This finding is congruent with a study done in Yilmana woreda of Northern Ethiopia.20
Compared with mothers from households with higher tertile wealth status, mothers from households with lower and middle tertile wealth status were 89% and 92% less likely to use GM services, respectively. The study done in Southern Ethiopia supports this finding.18 The possible explanation could be that people with lower household tertile might be busy fulfilling their day-to-day livelihood needs and have limited time to attend the GM service.
The time it takes to reach a nearby health facility was found to be significantly associated with GM service utilisation. Those mothers who took less than 30 min to reach a nearby health facility were two times more likely to use GM than those mothers who took more than 30 min to reach a nearby health facility. This finding was in line with the studies conducted in Yilmana Dedisa and Butajira district.17 20 This could be because mothers who live near a health facility can bring their children for GM service quickly and return to work, even if they are busy at work.
Strength and limitation of the study
There are certain limitations to this research. First, since the data were collected by the verbal report of the participants, there might be a possibility of response bias. Data collectors were trained on some techniques of reducing response bias during the interview. Second, the study did not assess the qualitative perspective of GM service utilisation.
Conclusions and recommendation
The study found that only one-fourth of mothers with children aged 0–23 months in Mettu town were using GM services. GM service utilisation was significantly associated with index child age, early PNC, use of family health cards, wealth status and time to reach nearby health facilities. Hence, appropriate strategies that promote and encourage GM service utilisation should be designed.
Supplementary Material
Acknowledgments
We would like to acknowledge Mettu University, the Department of Public Health and Mettu town health office for their support throughout the study period. We are also grateful to data collectors, supervisors and study participants for their valuable contributions.
Footnotes
Contributors: YT developed the research idea, design and analysis, and drafted the manuscript. AM, SS and KB conceived the study, supervised the data collectors, interpreted the result and reviewed the manuscript. All authors read and approved the final manuscript. YT is responsible for the overall content as the guarantor.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement
Data are available upon reasonable request. Not applicable.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Ethical clearance was obtained from the ethical review board of Mettu University, College of Health Science (reference no. RPG 42/20) submitted to Mettu town health office. The letter of permission was obtained from Mettu town health office. Before beginning the data collection, written consent was obtained from the study participants after clear information was provided about the objectives of the study. The study was conducted in accordance with the Helsinki Declaration.
References
- 1.Garner P, Panpanich R, Logan S. Is routine growth monitoring effective? A systematic review of trials. Arch Dis Child 2000;82:197–201. 10.1136/adc.82.3.197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ashworth A, Shrimpton R, Jamil K. Growth monitoring and promotion: review of evidence of impact. Matern Child Nutr 2008;4:86–117. 10.1111/j.1740-8709.2007.00125.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Griffiths M, Del Rosso J, Growth Monitoring and the Promotion of Healthy Young Child Growth . Evidence of effectiveness and potential to prevent malnutrition. Matern Child Nutr 2008:86–117. [Google Scholar]
- 4.UNICEF . Experts consultation on growth monitoring and promotion strategies : Program guidance for a way forward Recommendations from a Technical Consultation UNICEF Headquarters. New York, USA; 2008: 1–8. [Google Scholar]
- 5.Mangasaryan N, Arabi M, Schultink W. Revisiting the concept of growth monitoring and its possible role in community-based nutrition programs. Food Nutr Bull 2011;32:42–53. 10.1177/156482651103200105 [DOI] [PubMed] [Google Scholar]
- 6.Lu C, Black MM, Richter LM. Risk of poor development in young children in low-income and middle-income countries: an estimation and analysis at the global, regional, and country level. The Lancet Global Health 2016;4:e916–22. 10.1016/S2214-109X(16)30266-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.UNICEF . Tracking progress on child and maternal nutrition, 2009. [Google Scholar]
- 8.World Health Organization . Levels and trends in child malnutrition: key findings of the 2018 edition of the joint child malnutrition estimates. Geneva; 2018. [Google Scholar]
- 9.WHO, W Bank . Levels and trends in child malnutrition, 2019
- 10.Ethiopian . Mini demographic and health survey, 2019. [Google Scholar]
- 11.Afrirican development bank and agance frace development Wfp, the cost of hunger in Africa: Ethiopia WFP, 2014
- 12.Investing in nutrition the foundation for development. An investment framework to reach the global nutrition targets, 2015
- 13.Nutrition Program Planning and Supervision . For health and agriculture program managers reference manual July 2013 nutrition
- 14.Yeshaneh A, Fentahun T, Belachew T, et al. Utilization of growth monitoring and promotion services and associated factors among children aged 0-23 months in Banja district, Northwest Ethiopia 2020: a cross-sectional study. PLoS One 2021;16:e0259968. 10.1371/journal.pone.0259968 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bilal SM, Moser A, Blanco R. Practices and challenges of growth monitoring and promotion in Ethiopia: a qualitative study. J Heal Popul Nutr 2014;32:441–51. [PMC free article] [PubMed] [Google Scholar]
- 16.Tuobom Debuo D. Caregivers knowledge, attitude and practices on child growth monitoring and promotion activities in Lawra district, upper West region of Ghana. SJPH 2017;5:20. 10.11648/j.sjph.20170501.13 [DOI] [Google Scholar]
- 17.Desalegne L, Shiferaw S, Haile D. Assessment of knowledge and utilization of growth monitoring and promotion for under two children in Butajira, Ethiopia 2017, 2017. [Google Scholar]
- 18.Feleke FW, Adole AA, Bezabih AM. Utilization of growth monitoring and promotion services and associated factors among under two years of age children in southern Ethiopia. PLoS One 2017;12:e0177502. 10.1371/journal.pone.0177502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dagne S, Aliyu J, Menber Y, et al. Determinants of growth monitoring and promotion service utilization among children 0-23 months of age in northern Ethiopia: unmatched case-control study. BMC Nutr 2021;7:15–20. 10.1186/s40795-021-00470-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yeniew S. Utilization of growth monitoring and promotion service by mothers of children 0-23 months old in Yilmana Denisa Woreda, 2020. [Google Scholar]
- 21.Tekle M, Tariku B, Alagaw A, et al. Exploring reasons for low attendance of mothers to growth monitoring and promotion program at Loka Abaya district, southern Ethiopia: exploratory qualitative study. J Nutr Metab 2019;2019:1–7. 10.1155/2019/3510649 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Faber M, Phungula MA, Kvalsvig JD, et al. Acceptability of community-based growth monitoring in a rural village in South Africa. Food Nutr Bull 2003;24:350–9. 10.1177/156482650302400405 [DOI] [PubMed] [Google Scholar]
- 23.Gebreslassie Gebrehiwot T, Mekonen HH, Hailu Gebru T, et al. Prevalence and associated factors of early postnatal care service use among mothers who had given birth within the last 12 months in Adigrat town, Tigray, Northern Ethiopia, 2018. Int J Womens Health 2020;12:869–79. 10.2147/IJWH.S266248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.EDHS . Federal Democratic Republic of Ethiopia demographic and health survey, 2016. [Google Scholar]
- 25.Seidu F. Utilisation of Growth Monitoring and Promotion is Highest Among Children Aged 0-11 Months : A Survey Among Mother-Child Pairs From Rural [DOI] [PMC free article] [PubMed]
- 26.Jane Ilusa Nyabuti . Factors associated with the continuation of growth monitoring among children 10 to 59 months old. 1, 2015: 5–6. [Google Scholar]
- 27.Lucy Mwari K, Keraka Professor MN, University K. Care giver deteminants of utilization of growth monitoring clinic among children aged 12-59 months in urban Kiambu County, Kenya. Int J Innov Res Adv Stud 2017;4:334–8. [Google Scholar]
- 28.Budu E, et al. Maternal healthcare utilization and full immunization coverage among 12–23 months children in Benin: a cross sectional study using population-based data. Arch Public Heal 2021;79:1–12. 10.1186/s13690-021-00554-y [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available upon reasonable request. Not applicable.