Abstract
Background and Aims:
Robotic surgeries often require a relatively long duration of pneumo-peritoneum and trendelenburg position which may accentuate changes in endo-tracheal tube (ETT) cuff pressure leading to pressure related complications. The aim of this study was to analyze changes in ETT cuff pressures during various stages of pneumo-peritoneum and surgical positioning and its correlation with airway pressure changes.
Material and Methods:
A prospective observational study was planned after approval of institutional review board on 60 patients undergoing elective robotic pelvic surgery requiring head down position. Baseline cuff pressure was adjusted to 25 cm H2O. ETT cuff pressure, peak airway pressure and end tidal CO2 (ETCO2) was measured at various time intervals before and after pneumo-peritoneum and head down. Ventilatory parameters were kept fixed after baseline setting. Those requiring any change were excluded. Pearson’s coefficient was used for correlation and ANOVA for trend of parameters at different time intervals (P value <0.05 was considered significant).
Results:
Baseline cuff pressure after manual inflation was 46.2 ± 17.4 cm H2O. Significant correlation was observed between change in cuff pressure and increase in peak airway pressure at the end of the surgery (r = 0.4, P < 0.05). Serial measurements of ETT cuff pressure, peak airway pressure and ETCO2 were significantly increased compared to baseline (P < 0.05).
Conclusion:
Significant increases in ETT cuff pressure may be seen in robotic surgeries, with a positive correlation between change in cuff pressure and increase in airway pressures. Objective adjusted measurement of cuff pressure and airway pressures is recommended for such surgeries.
Keywords: Cuff pressure, peak airway pressure, pneumoperitoneum, robotic pelvic surgery, trendelenburg position
Introduction
Changes in endo-tracheal tube (ETT) cuff pressure during elective surgeries may lead to neuropraxia of recurrent laryngeal nerve or ischemia of tracheal mucosa, especially in longer duration surgeries. This may lead to minor symptoms like sore throat and hoarseness to more distressing complications like ulceration, nerve palsy and sub-glottic stenosis.[1] A safe range of 20 to 30 cm H2O cuff pressure is advised to be maintained using a cuff manometer; although on most occasions and in majority of centers this is still done by manual palpation and “feel” of the pilot balloon.[1,2,3] Studies have shown significantly higher cuff pressures when inflated manually compared to use of cuff pressure monitors or automated pressure controllers with fewer pressure related side effects seen in the latter.[2,3,4]
Robotic surgeries have revolutionized surgical technique and access to difficult areas like the pelvis.[5,6,7] Such surgeries often require a relatively long duration of pneumo-peritoneum and trendelenburg position. These changes in physiology may accentuate increases in ETT cuff pressure. It has been found that there is a linear relationship between cuff pressure changes and increase in airway pressure[1,8] although this has not been established definitively. Various other factors have also been studied such as, correlation to body mass index (BMI), patient position, duration of pneumo-peritoneum and use of nitrous oxide.[8,9,10,11,12]
The aim of the present study was to analyze changes in ETT cuff pressures during various stages of pneumo-peritoneum and surgical positioning. The primary objective was to assess the correlation between change in ETT cuff pressure and increase in peak airway pressure. Secondary objectives were to assess the changes in ETT cuff pressure and other airway parameters at different stages of robotic pelvic surgeries.
Material and Methods
A prospective observational study was conducted on patients posted for elective pelvic robotic surgeries after approval from the institutional ethics committee (12.04.2019). A total of 60 patients were finally analyzed after excluding all ineligible participants over a time period of 7 months. The manuscript was prepared according to STROBE guidelines for observational studies. Written informed consent for was taken for participation in the study along with consent for surgery. Inclusion criteria was patients of age above 18 years and below 60 years, both genders, American society of anesthesiology physical status 1 and 2, patients undergoing robotic gynecological and urological procedures requiring trendelenburg positioning. Exclusion criteria was patients with preexisting pulmonary or cardiac disease, patients with preexisting vocal cord palsy, goiter or any other airway or thoracic pathology, pregnant or lactating females, smokers, BMI more than 25 or less than 18.5, and those participants who were initially recruited in the study but required change in ventilator parameters after pneumo-peritoneum or change in angle of head down tilt of table due to crossing of determined ventilator limits described later.
After selection of suitable study participants and obtaining appropriate consent, a thorough pre-anesthetic examination was done. All participants were given anxiolysis medication in the evening prior to surgery in the form of oral alprazolam (0.5 mg) and were kept nil per oral as per existing guidelines. On the morning of surgery, surgical safety check list was confirmed. After securing intravenous access and injection fentanyl (1-1.5 mcg/kg), anesthesia was induced by propofol (1-1.5 mg/kg) and the trachea intubated with an appropriately sized ETT (7.5 mm in females and 8.5 mm in males, Portex®) facilitated with vecuronium (0.1 mg/kg). The ETT cuff (polyvinyl chloride) was inflated by a technician or a resident guided by manual palpation. Baseline cuff pressure was measured at this time using an ETT cuff manometer (Ambu™) and adjusted to 25 cm of H2O. Other baseline values of peak airway pressure and end tidal CO2 (ETCO2) were also recorded. Neuromuscular monitoring was done to prevent any bucking due to inadequate blockade. Maintenance was with sevoflurane, air and oxygen along with maintenance dose of fentanyl and vecuronium. Nitrous oxide was not used. Cushioned straps were applied to chest and arms for securing the patient to the operating table along with padded shoulder supports fixed to the table to prevent slipping.
Baseline ventilator parameters were set after intubation prior to pneumo-peritoneum insufflation (tidal volume of 8 ml/kg, respiratory rate of 15/min, positive end expiratory pressure of 5 cm). No changes were made in the ventilator parameters thereafter unless ETCO2 and peak airway pressures rose above the described values (ETCO2 above 45 mm Hg and peak airway pressure above 40 cm H2O). The degree of head down tilt was fixed at 30 degrees[13,14] and the intra-abdominal pressure was kept set at 12 mm Hg unless airway pressures exceeded the described limit. Those who required change of set parameters were excluded from study. All values (ETT cuff pressure, peak airway pressure and ETCO2) were recorded again 5 minutes after establishing pneumo-peritoneum, 5 minutes after final head down position and lastly, 5 minutes prior to releasing pneumo-peritoneum and return to horizontal position. The trachea was extubated at the end of the procedure after objective neuro-muscular recovery (train of four ratio of more than 0.9). Outcome modifiers not being analyzed in the present study were either excluded or standardized (only ideal weight BMI category was included; nitrous oxide was not used and angle of table tilt was fixed for all patients).
Statistical analysis
Sample size was calculated from MedCalc® software for correlation calculation. To obtain a correlation of at least 0.4 (observed in a pilot study with 15 subjects conducted by us), a minimum of 47 participants were required to achieve 80% power and 5% alpha error. The data was entered in MS EXCEL spreadsheet and analysis was done using GraphPad InStat version 3.05. Categorical variables were presented in number and percentage (%) and continuous variables were presented as mean ± SD and median. Normality of data was tested by Kolmogorov-Smirnov test. Correlation between change in ETT cuff pressure and change in peak airway pressure was done using Pearson’s correlation coefficient. Repeated measures analysis of variance (ANOVA) with post hoc test was used to compare baseline study parameters at different stages of surgery. A P value of <0.05 was considered statistically significant.
Results
A final number of 60 participants were analyzed for statistical analysis after initially considering 75 participants for inclusion in the study over a period of 7 months. 8 participants were excluded due to exceeding 40 cm H2O airway pressures requiring change in set parameters. Similarly, 7 patients were excluded due to rise in ETCO2 above 45 mm Hg [Figure 1]. The mean age of the study sample was 42.7 ± 7.1 years. All participants in the study (100%) were female patients as all the pelvic surgeries included gynecological pathologies. Baseline cuff pressure after manual inflation was 46.2 ± 17.4 cm H2O (range; 25-90 cm H2O). The cuff was overinflated (>30 cm H2O) in 86% of the participants. These pressures were adjusted to 25 cm H2O using the cuff manometer. Mean duration of surgeries was 2.0 ± 0.4 hours.
Figure 1.

STROBE flowchart for patient recruitment
Pearson’s correlation between change in peak airway pressure and change in ETT cuff pressure did not show any significant correlation at 5 minutes after pneumo-peritoneum and 5 minutes after final head down position, but showed statistically significant positive correlation towards the end of surgery (5 minutes prior to releasing pneumo-peritoneum and return to horizontal position) (r = 0.4, P < 0.05) [Figure 2, Table 1]. Repeated measures ANOVA for ETT cuff pressure showed statistically significant increase at various time intervals overall and also individually compared to baseline (P < 0.05). Similar results were seen with peak airway pressure and ETCO2 at various time intervals compared to baseline (P < 0.05), [Table 2].
Figure 2.
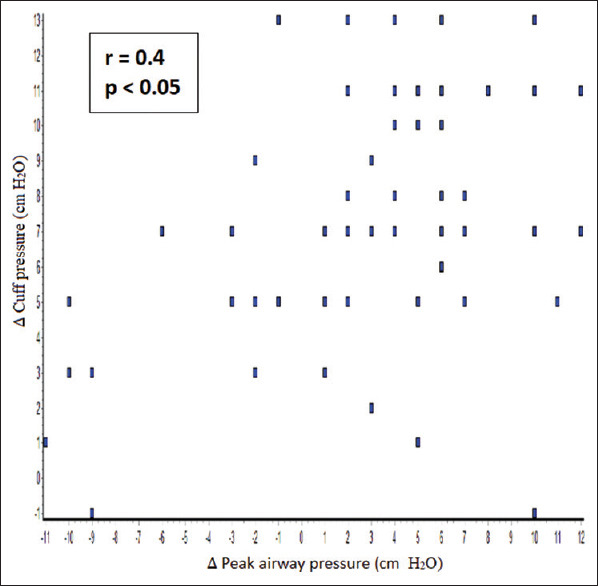
Correlation between change in cuff pressure and change in peak airway pressure (5 minutes before pneumoperitoneum release)
Table 1.
Correlation coefficient between change in cuff pressure and change in peak airway pressure at different time intervals
| Time intervals (compared to baseline) | Correlation coefficient (r) | P* |
|---|---|---|
| 5 min after establishing pneumo-peritoneum | −0.05 | 0.6 |
| 5 min after final head down position | 0.05 | 0.7 |
| 5 min prior to releasing pneumo-peritoneum | 0.4 | 0.001 |
*Pearson’s correlation, P<0.05 is significant
Table 2.
Comparison of ETT cuff pressure, ETCO2 and peak airway pressure at different time intervals
| Measured parameter | Mean±SD | P* |
|---|---|---|
| Cuff pressure (cm H2 O) | ||
| Baseline (adjusted to 25 cm H2 0) | 25±0 | - |
| 5 mins after pneumo-peritoneum | 29.97±3.79 | <0.001 |
| 5 mins after head down | 32.7±3.2 | <0.001 |
| 5 mins prior to pneumo-peritoneum release | 32.28±3.57 | <0.001 |
| Peak airway pressure (cm H2 O) | ||
| Baseline | 16.87±2.62 | - |
| 5 mins after pneumo-peritoneum | 23.08±3.62 | <0.001 |
| 5 mins after head down | 26.88±4.16 | <0.001 |
| 5 mins prior to pneumo-peritoneum release | 25.3±5.4 | <0.001 |
| End tidal CO2 (mm Hg) | ||
| Baseline | 30.93±2.11 | - |
| 5 mins after pneumo-peritoneum | 33.33±2.57 | <0.001 |
| 5 mins after head down | 35.77±2.47 | <0.001 |
| 5 mins prior to pneumo-peritoneum release | 34.2±3.04 | <0.001 |
*Repeated measures ANOVA with post hoc test, P<0.05 is significant
Discussion
Robot assisted procedures offer numerous advantages such as lesser peri-operative pain, earlier recovery, smaller surgical incisions and reduced hospital stay, but at the same time may offer unique challenges to the anesthesiologist. One of these is the management of airway pressures and possible effects on cuff pressure during the extremes of position as well as the patho-physiological effects of pneumo-peritoneum.
The primary objective of the current study was to analyze the correlation between change in cuff pressure and increase in peak airway pressure. In the current study a significant correlation was seen between changes in airway pressure and cuff pressure with readings taken towards the end of the surgery, but not in the initial 2 stages (change compared to baseline readings). In a similar study by Wu CY et al. they reported a significant correlation between changes in airway pressure and endotracheal tube cuff pressure by abdominal insufflation (r = 0.68, P < 0.05).[8] Rosero EB, et al. also conducted a multilevel mixed regression analyses in which increased peak airway pressures were significantly associated with increased pressures in the ETT cuff. Each 1 cm H2O increase in peak airway pressures produced an increase in the ETT cuff pressures of 0.25 cm H2O (P < .0001).[1] The correlation findings in the current study is in keeping with the above two studies. As readings were taken at different time points of surgery, the change observed in the first two reading in the initial phases were perhaps not adequate enough to reflect the correlation, compared to the overall change towards the end of surgery [Table 1].
In the current study, significant increase in cuff pressure were observed at various time intervals of pneumo-peritoneum and head down position across the surgery. Similar trends were observed by Wu CY, et al. who conducted their study on patients undergoing elective laparoscopic colorectal tumor resection and laparoscopic cholecystecomy comparing it to open abdominal surgery. The cuff pressure increased from 26 ± 3 to 32 ± 6 cm H2O in laparoscopic cholecystecomy patients and from 27 ± 3 to 33 ± 5 cm H2O in laparoscopic colorectal tumor resection after insufflation (P < 0.001). The head-down tilt further increased cuff pressure from 33 ± 5 to 35 ± 5 cmH2O (P < 0.001).[8] Findings of Rosero EB, et al.[1] are also in keeping with the above findings, in their study on adult obese patients undergoing elective laparoscopic gynecologic procedures. The peak airway pressures significantly increased from 23.2 ± 0.84 cm H2O before peritoneal insufflations (phase 1) to 32.1 ± 0.46 cm H2O after peritoneal insufflations and Trendelenburg positioning (phase 2), (P < .0001). ETT cuff pressures also increased significantly from 29.6 ± 1.30 cm H2O during phase 1 to 35.6 ± 0.68 cm H2O during phase 2, (P < .0001).
In the current study baseline cuff pressure after manual inflation by the technician or anesthesia resident was significantly higher (46.2 ± 17.4 cm H2O) than the prescribed safe range (20–30 cm H2O), with 86% of the values being above 30 cm H2O cuff pressure. A wide range of baseline cuff pressures was also noted (25-90 cm H2O). Similar findings were observed by Rosero EB, et al.[1] (89% over-inflated) and in 46% patients it was above 100 cm H2O. In a study by Jain and Tripathi,[3] manual and automated techniques of cuff inflation were analyzed which showed significantly high mean cuff pressure 50.1 ± 11.7 cm H2O after manual inflation and complication rate was lower in automated controlled group. Cuff pressure monitor should thus be a minimal requirement in elective surgeries with endo-tracheal intubation. Alternatively, training of technicians or residents can be done to accurately predict appropriate amount of air required to be inflated by palpation or feel of pilot balloon, as was done by Chan SM, et al.[15] although it should not replace use of manometer.
Limitations
Firstly, the duration of surgery was relatively short in the study; inclusion of longer urological surgeries would provide further insight into the extent and correlation of the cuff pressure changes with airway pressures. Secondly, analyzing other variables like BMI, degree of head down tilt etc., was not within the scope of this study, the authors plan to conduct a future research on similar subjects taking different angles of head down and effect of weight and BMI into consideration.
To conclude; significant increases in ETT cuff pressure may be caused by changes in body position such as trendelenburg and effect of pneumo-peritoneum. This effect is maximum shortly after achieving head down position. There exists a significant positive correlation between the change in cuff pressure versus the increase in airway pressure, which appears to be more pronounced as the surgery progresses. In this context strict monitoring and management of airway pressures and ongoing adjustment of cuff pressure using a manometer is essential and advised, especially for this subset of surgeries.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Rosero EB, Ozayar E, Eslava-Schmalbach J, Minhajuddin A, Joshi GP. Effects of increasing airway pressures on the pressure of the endotracheal tube cuff during pelvic laparoscopic surgery. Anaesth Analg. 2018;127:120–5. doi: 10.1213/ANE.0000000000002657. [DOI] [PubMed] [Google Scholar]
- 2.Coelho RD, Paiva TT, Mathias LA. In vitro evaluation of the method effectiveness to limit inflation pressure cuffs of endotracheal tubes. Rev Bras Anaestesiol. 2016;66:120–5. doi: 10.1016/j.bjan.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 3.Jain MK, Tripathi CB. Endotracheal tube cuff pressure monitoring during neurosurgery-Manual vs. automatic method. J Anaesthesiol Clin Pharmacol. 2011;27:358–61. doi: 10.4103/0970-9185.83682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Koo C-H, Sohn H-M, Choi E-S, Choi J-Y, Oh A-Y, Jeon Y-T, et al. The effect of adjustment of endotracheal tube cuff pressure during scarless remote access endoscopic and robotic thyroidectomy on laryngo-pharyngeal complications:Prospective randomized and controlled trial. J Clin Med. 2019;8:1787. doi: 10.3390/jcm8111787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ashrafian H, Clancy O, Grover V, Darzi A. The evolution of robotic surgery:Surgical and anaesthetic aspects. Br J Anaesth. 2017;119(suppl_1):i72–84. doi: 10.1093/bja/aex383. [DOI] [PubMed] [Google Scholar]
- 6.Kakar PN, Das J, Roy PM, Pant V. Robotic invasion of operation theatre and associated anaesthetic issues:A review. Indian J Anaesth. 2011;55:18–25. doi: 10.4103/0019-5049.76577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McLarney JT, Rose GL. Anaesthetic implications of robotic gynecologic surgery. J Gynecol Endosc Surg. 2011;2:75–8. doi: 10.4103/0974-1216.114077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu C-Y, Yeh Y-C, Wang M-C, Lai C-H, Fan S-Z. Changes in endotracheal tube cuff pressure during laparoscopic surgery in head-up or head-down position. BMC Anaesthesiol. 2014;14:75. doi: 10.1186/1471-2253-14-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Athiraman U, Gupta R, Singh G. Endotracheal cuff pressure changes with change in position in neurosurgical patients. Int J Crit Illn Inj Sci. 2015;5:237–41. doi: 10.4103/2229-5151.170841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Godoy AC, Vieira RJ, Capitani EM. Endotracheal tube cuff pressure alteration after changes in position in patients under mechanical ventilation. J Bras Pneumol. 2008;34:294–7. doi: 10.1590/s1806-37132008000500008. [DOI] [PubMed] [Google Scholar]
- 11.Kim D, Jeon B, Son J-S, Lee J-R, Ko S, Lim H. The changes of endotracheal tube cuff pressure by the position changes from supine to prone and the flexion and extension of head. Korean J Anaesthesiol. 2015;68:27–31. doi: 10.4097/kjae.2015.68.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mogal SS, Baliarsing L, Dias R, Gujjar P. Comparison of endotracheal tube cuff pressure changes using air versus nitrous oxide in anaesthetic gases during laparoscopic abdominal surgeries. Braz J Anaesthesiol. 2018;68:369–74. doi: 10.1016/j.bjane.2018.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ghomi A, Kramer C, Askari R, Chavan NR, Einarsson JI. Trendelenburg position in gynecologic robotic-assisted surgery. J Minim Invasive Gynecol. 2012;19:485–9. doi: 10.1016/j.jmig.2012.03.019. [DOI] [PubMed] [Google Scholar]
- 14.Gould C, Cull T, Wu YX, Osmundsen B. Blinded measure of Trendelenburg angle in pelvic robotic surgery. J Minim Invasive Gynecol. 2012;19:465–8. doi: 10.1016/j.jmig.2012.03.014. [DOI] [PubMed] [Google Scholar]
- 15.Chan S-M, Wong C-S, Cherng C-H. Determining an optimal tracheal tube cuff pressure by the feel of the pilot balloon:A training course for trainees providing airway care. Acta Anaesthesiol Taiwan. 2009;47:79–83. doi: 10.1016/S1875-4597(09)60028-X. [DOI] [PubMed] [Google Scholar]


