Abstract
Introduction
Both coil and hook-wire localization techniques are commonly employed prior to video-assisted thoracic surgery (VATS) resection in patients with lung nodules (LNs), but the relative advantages of each remain uncertain.
Aim
This meta-analysis was performed to explore the relative safety and efficacy of coil localization (CL) and hook-wire localization (HWL) for patients with LNs.
Material and methods
The PubMed, Embase, Cochrane Library, Wanfang, and CINK databases were searched to identify relevant studies published as of February 2022, after which pooled analyses of study outcomes were conducted.
Results
In total, 8 studies met the inclusion criteria for the present meta-analysis. Successful localization rates were higher for the CL group relative to the HWL group (p = 0.0001). The CL group additionally exhibited significantly lower pooled total complication, pneumothorax, and lung hemorrhage rates relative to the HWL group (p = 0.01, p = 0.0001, p = 0.0009). Pooled duration of localization, VATS procedure duration, and wedge resection duration values were comparable in both groups (p = 0.69, p = 0.16, p = 0.76), as were chest pain scores (p = 0.06). When specifically analyzing the subset of patients with ground-glass LNs, pooled pneumothorax rates were significantly lower in the CL group relative to the HWL group (p = 0.03). Significant publication bias was detected with respect to rates of lung hemorrhage (Egger test, p = 0.029), but was not evident for other analyzed variables.
Conclusions
These results suggest that the coil-based localization of LNs before VATS resection is safer and more effective than hook-wire localization.
Keywords: coil, hook-wire, localization, lung nodule
Introduction
Computed tomography (CT) is routinely used throughout the world as an approach to screening for early-stage lung cancer, leading to the frequent detection of lung nodules (LNs) [1–3]. In individuals with clinical and radiological evidence that places them at a moderate to high risk of malignancy, these LNs tend to be malignant in 62–72% of cases [4]. Video-assisted thoracic surgery (VATS) is the standard approach to resecting LNs suspected of being malignant [5–7]. When these LNs are small (< 10 mm in diameter) or located in a deep site > 5 mm from the pleura, a failure to accurately identify these nodules can lead to the conversion of VATS to thoracotomy in ~63% of cases [8]. Hence, the preoperative localization of such LNs is critical as a means of guiding accurate VATS resection procedures [9, 10].
The two most common LN localization approaches are coil localization (CL) and hook-wire localization (HWL) [9, 10], with prior meta-analyses having demonstrated both of these strategies to be associated with similarly high rates of successful LN localization (92–99%) [9, 10]. Despite comparable efficacy, HWL has been reported to result in higher complication rates relative to CL [9, 10]. The rates in these prior meta-analyses, however, were derived from indirect comparisons based on single-arm studies. There thus remains a need to conduct an additional meta-analysis specifically focused on comparative studies examining the relative safety and efficacy of CL and HWL prior to VATS-based LN resection.
Aim
The aim of this meta-analysis was to compare the relative safety and efficacy of coil- and hook-wire-based approaches to LN localization.
Material and methods
Study selection
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines were used to conduct the present systematic review and meta-analysis [11], which was registered at INPLASY.COM (No. INPLASY202230128).
The PubMed, Embase, Cochrane Library, Wanfang, and CNKI databases were searched to identify relevant articles published as of February 2022 using the following strategy: (((((coil) OR (microcoil)) AND (((hook wire) OR (hookwire)) OR (hook-wire))) AND ((lung) OR (pulmonary))) AND (localization)) AND ((nodule) OR (lesion)).
Studies eligible for inclusion met the following criteria:
types of studies: comparative studies;
diseases: patients with LNs;
types of interventions: CL versus HWL prior to VATS;
languages: not limited.
Studies were excluded if they were:
non-comparative studies;
studies without English titles and/or abstract;
case reports, letters, and reviews.
Data extraction
Relevant data were independently extracted from eligible studies by two authors, with discrepancies being resolved through discussion with a third author. Extracted baseline data included the first author, year of publication, country, study design, number of patients, number of LNs, age, gender ratio, LN diameter, and LN-pleura distance values. Extracted outcome data included technical success rates for localization, localization procedure duration, total rates of complications, pneumothorax rates, lung hemorrhage rates, chest pain scores, VATS duration, and the duration of wedge resection.
Quality assessment
The Cochrane risk-of-bias tool was used to establish the quality of randomized controlled trials (RCTs), with each of the following being assigned a low, high, or unclear risk of bias: performance, attrition, detection, selection, reporting, and other bias.
Observational study quality was assessed using the Newcastle-Ottawa scale (NOS) [12], which assigns points to each study based on selection (4 points), comparability (2 points), and outcome (3 points) criteria. A NOS score ≥ 7 was considered indicative of a high-quality study.
Endpoints
The primary endpoint for the present analysis was the technical success rate of LN localization. Secondary endpoints included the duration of localization, the duration of the VATS procedure, wedge resection duration, chest pain scores, and rates of pneumothorax, lung hemorrhage, and total complications. The technical success of localization procedures was defined by the visibility of the coil or hook-wire when performing the VATS procedure such that these materials were not dislodged during the VATS procedure, with the target LN being successfully located in the resected segment of pulmonary tissue [9].
Statistical analysis
Pooled analyses were conducted using RevMan v5.3. For dichotomous variables, pooled odds ratios (ORs) with 95% confidence intervals (CIs) were calculated, while continuous variables were compared using mean differences (MD) values with 95% CIs. The I2 statistic and Q test were used to assess heterogeneity, with an I2 > 50% being considered indicative of significant heterogeneity. When heterogeneity was significant, random-effects models were used, whereas fixed-effect models were otherwise used. Sensitivity analyses were conducted via a “leave one out” approach in an effort to detect sources of heterogeneity. Subgroup analyses of studies focused specifically on ground glass nodules (GGNs) were additionally conducted. Publication bias was analyzed using Egger’s test by Stata v12.0, with p < 0.05 as the significance threshold.
Results
Study selection
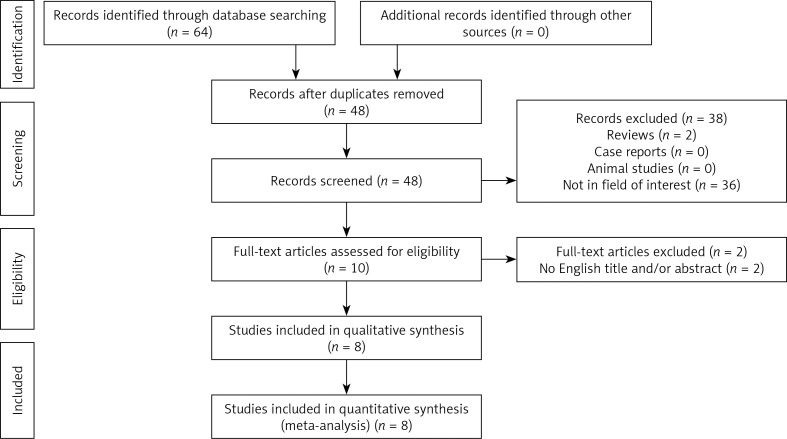
In total, 64 potentially relevant studies were initially identified, of which 8 were ultimately included in the present study [13–20]. The study selection process is detailed in Figure 1. Of these studies, 7 were retrospective [13–16, 18–20] and one article was an RCT [17] (Table I). Six studies were performed in China [13, 14, 16, 17, 19, 20], one study was performed in the USA [18], and one study was performed in Korea [15]. In total, the coil group contained 467 patients with 470 LNs and the hook-wire group contained 400 patients with 401 LNs (Table II). The number of patients in each included study ranged from 43 to 198. Two of these studies specifically focused on patients with GGNs [16, 19].
Figure 1.
Meta-analysis flow chart
Table I.
Baseline data of the included studies
| No. | First author | Year | Country | Design | NOS |
|---|---|---|---|---|---|
| 1 | Deng [13] | 2020 | China | Retrospective | 8 |
| 2 | Hu [14] | 2019 | China | Retrospective | 8 |
| 3 | Hwang [15] | 2018 | Korea | Retrospective | 8 |
| 4 | Liu [16] | 2020 | China | Retrospective | 8 |
| 5 | Lu [17] | 2018 | China | Randomized controlled trial | – |
| 6 | Rostambeigi [18] | 2019 | USA | Retrospective | 8 |
| 7 | Wu [19] | 2021 | China | Retrospective | 8 |
| 8 | Yang [20] | 2020 | China | Retrospective | 8 |
NOS – Newcastle-Ottawa Scale.
Table II.
Baseline data of the patients in the included studies
| Author | Groups | Patients (n) | Nodules (n) | Age [years] | Gender (M/F) | Diameter [mm] | Lesion-pleura distant [mm] |
|---|---|---|---|---|---|---|---|
| Deng [13] | Coil | 22 | 22 | 56 | 7/15 | 8.9 | 19 |
| Hook-wire | 21 | 21 | 62 | 11/10 | 8.9 | 18 | |
| Hu [14] | Coil | 79 | 79 | 53.9 | 34/45 | 8.7 | 9.4 |
| Hook-wire | 33 | 33 | 52.6 | 13/20 | 8.0 | 7.9 | |
| Hwang [15] | Coil | 54 | 54 | 62.2 | 29/25 | 12.6 | 9.4 |
| Hook-wire | 45 | 45 | 63.6 | 26/19 | 13.0 | 9.1 | |
| Liu [16] | Coil | 76 | 76 | 56.79 | 38/38 | 9.58 | 21.84 |
| Hook-wire | 122 | 122 | 57.47 | 59/63 | 8.28 | 19.82 | |
| Lu [17] | Coil | 60 | 60 | 52 for all | Not given | Not given | Not given |
| Hook-wire | 52 | 52 | Not given | Not given | Not given | ||
| Rostambeigi [18] | Coil | 20 | 20 | 62 | 13/7 | 10.9 | 12 |
| Hook-wire | 26 | 26 | 60.5 | 16/10 | 9.9 | 18 | |
| Wu [19] | Coil | 85 | 88 | 54.3 | 33/52 | 14.0 | 15.3 |
| Hook-wire | 30 | 31 | 54.5 | 14/16 | 14.1 | 13.7 | |
| Yang [20] | Coil | 71 | 71 | 55.4 | 24/47 | 9.3 | 12.3 |
| Hook-wire | 71 | 71 | 56.4 | 26/45 | 9.4 | 12.3 |
M – male, F – female.
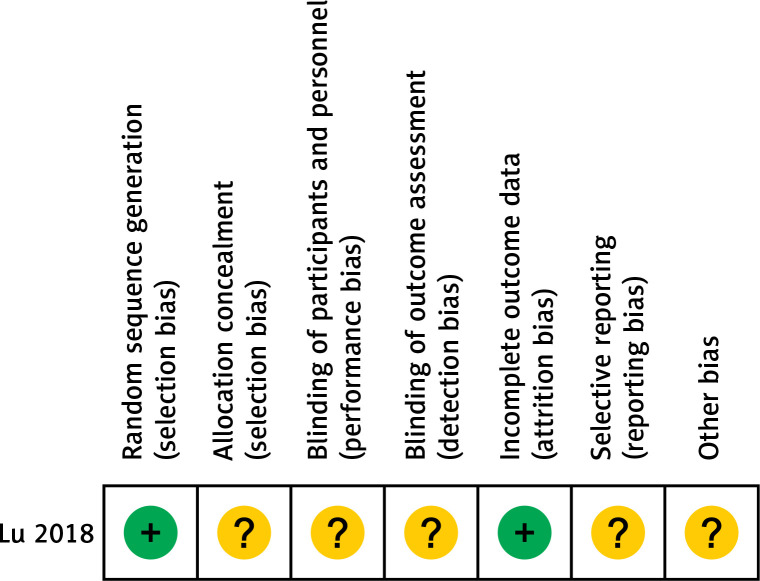
All 7 retrospective studies included in this analysis exhibited NOS scores of 7-8, consistent with a high degree of quality. The details of the NOS assessment are shown in the Table III. The included RCT exhibited an unclear risk of bias with respect to selection, performance, detection, reporting, and other bias criteria (Figure 2).
Table III.
Assessment of non-randomized study quality
| Studies | Quality indicators from Newcastle-Ottawa Scale | Score | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Selection | Comparability | Outcome | |||||||
| Representativeness of the exposed cohort | Selection of the non-exposed cohort | Ascertainment of exposure | Demonstration the outcome of interest was not present at start of study | Comparability of cohorts on the basis of the design or analysis | Assessment of outcome | Whether follow-up was long enough for outcomes to occur | Adequacy of followup of cohorts | ||
| Deng [13] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Hu [14] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Hwang [15] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Liu [16] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Rostambeigi [18] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Wu [19] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
| Yang [20] | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 8 |
Figure 2.
Cochrane risk-of-bias tool for the included RCT
Localization rates
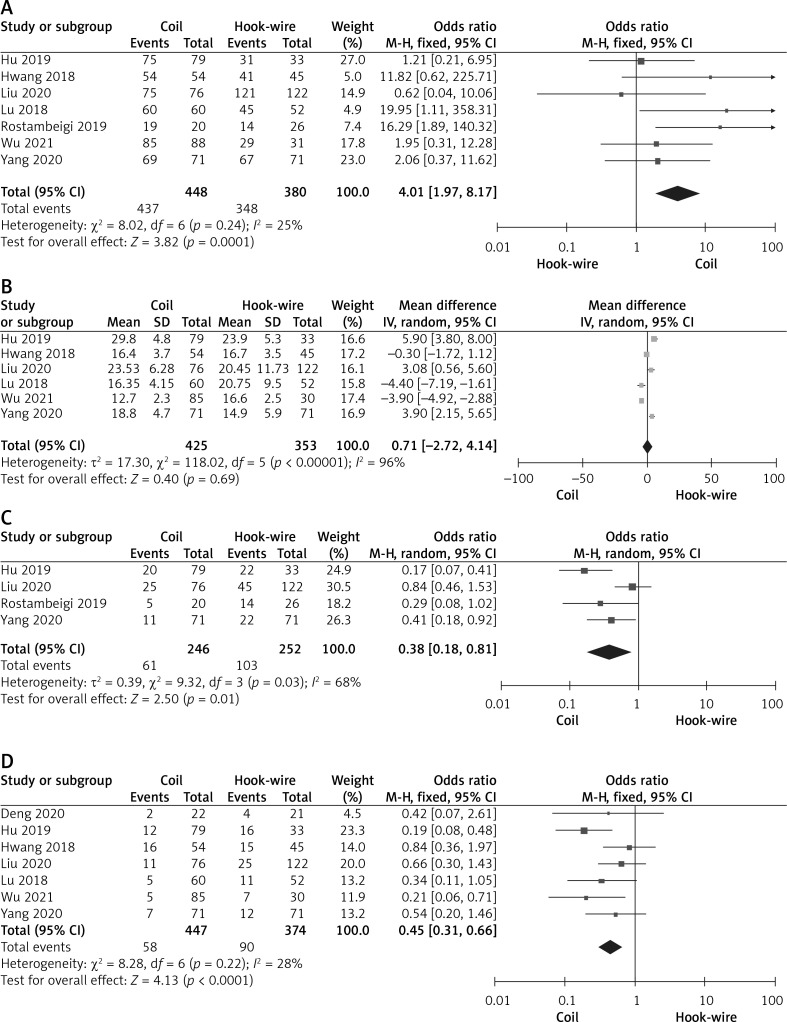
In total, 7 articles reported the rates of successful LN localization [14–20], with 448 and 380 LNs having been successfully localized via the CL and HWL approaches, respectively. Pooled rates of successful LN localization were higher in the CL group (97.5%) relative to the HWL group (91.6%) (OR = 4.01; 95% CI: 1.97, 8.17; p = 0.0001, Figure 3 A). There was no significant heterogeneity among these studies (I2 = 25%).
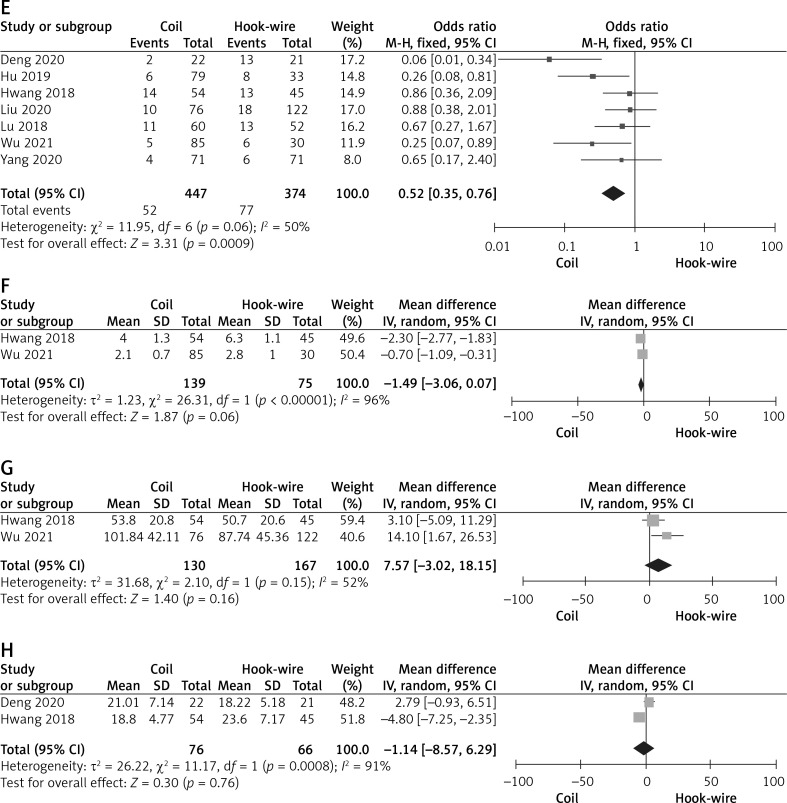
Figure 3.
Pooled results for successful localization rates (A), the duration of localization (B), total complication rates (C), pneumothorax rates (D), lung hemorrhage rates (E), chest pain scores (F), VATS procedure duration (G), and the duration of wedge resection (H) in the CL and HWL groups
Duration of localization
Of the included articles, 6 reported the duration of localization [14–17, 19, 20], including 425 and 353 patients who underwent CL and HWL, respectively. There were no significant differences in the pooled duration of localization between these groups (MD = 0.71; 95% CI: –2.72, 4.14; p = 0.69, Figure 3 B). While significant heterogeneity was detected (I2 = 96%), sensitivity analyses did not identify any study as the source of such heterogeneity.
Total complication rates
Total complication rates were reported in 4 studies [14, 16, 18, 20], including 246 and 252 patients in the CL and HWL groups, respectively. Pooled total complication rates were significantly lower in the CL group (24.8%) relative to the HWL group (40.9%) (OR = 0.38; 95% CI: 0.18, 0.81; p = 0.01, Figure 3 C). Significant heterogeneity was detected pertaining to these results (I2 = 68%), and sensitivity analyses indicated that this heterogeneity was absent (I2 = 3%) when omitting the study conducted by Liu et al. [16]. Even with this study having been omitted, pooled total complication rates remained significantly lower in the CL group relative to the HWL group (p < 0.00001).
Pneumothorax rates
Pneumothorax rates were reported in 7 studies [13–17, 19, 20], including 447 and 374 patients in the CL and HWL groups, respectively. Significantly lower pneumothorax rates were observed in the CL group (13.0%) relative to the HWL group (24.1%) (OR = 0.45; 95% CI: 0.31, 0.66; p < 0.0001, Figure 3 D), with no significant heterogeneity (I2 = 28%).
Lung hemorrhage rates
Lung hemorrhage rates were reported in 7 studies [13–17, 19, 20], including 447 and 374 patients who underwent CL and HWL, respectively. Pooled rates of lung hemorrhage were significantly lower in the CL group (11.6%) relative to the HWL group (20.6%) (OR = 0.52; 95% CI: 0.35, 0.76; p = 0.0009, Figure 3 E), with no significance heterogeneity (I2 = 50%).
Chest pain scores
Chest pain scores were reported for 2 studies [15, 19], incorporating 139 and 75 patients in the CL and HWL groups, respectively. No significant differences in chest pain scores were observed between these groups (MD = –1.49; 95% CI: –3.06, 0.07; p = 0.06, Figure 3 F). While significant heterogeneity was detected among studies (I2 = 96%), sensitivity analyses could not be performed as only two studies were included.
VATS duration
VATS duration was reported in two studies [15, 17], including 130 and 167 patients in the CL and HWL groups, respectively. Pooled VATS duration values were similar in both groups (MD = 7.57; 95% CI: –3.02, 18.15; p = 0.16, Figure 3 G). While significant heterogeneity was detected among studies (I2 = 52%), sensitivity analyses could not be performed as only two studies were included.
Duration of wedge resection
The duration of wedge resection was reported in two studies [13, 15], including 76 and 66 patients in the CL and HWL groups, respectively. Pooled wedge resection duration values were comparable between groups (MD = –1.14; 955 CI: –8.57, 6.29; p = 0.76, Figure 3 H). While significant heterogeneity was detected among studies (I2 = 91%), sensitivity analyses could not be performed as only two studies were included.
Publication bias
Egger’s test did not detect any significant bias associated with the localization technical success rate, duration of localization, total complication rate, or pneumothorax rate endpoints (p = 0.108, p = 0.408, p = 0.494, p = 0.909). The lung hemorrhage rate endpoint was associated with significant publication bias (p = 0.029). Funnel plots revealed significant publication bias with respect to chest pain score, duration of VATS, and duration of wedge resection.
Subgroup analyses
Of the included studies, two specifically focused on patients with GGNs [16, 19]. When comparing different parameters included in both of these articles (Table IV), it was evident that there were no significant differences in pooled localization technical success rates, duration of localization, or lung hemorrhage rates between these groups (p = 0.71, p = 0.88, p = 0.18), while pooled pneumothorax rates remained lower in the CL group (p = 0.03).
Table IV.
Meta-analytic pooled results based on the GGNs
| Variable | Number of studies | OR/MD (95% CI) | Heterogeneity | Favored |
|---|---|---|---|---|
| Technical success of localization | 2 | 1.35 (0.29, 6.36), p = 0.71 | I2 = 0% | – |
| Time of localization | 2 | –0.51 (–7.35, 6.33), p = 0.88 | I2 = 96% | – |
| Pneumothorax rate | 2 | 0.49 (0.25, 0.95), p = 0.03 | I2 = 59% | Coil |
| Pulmonary hemorrhage rate | 2 | 0.62 (0.31, 1.25), p = 0.18 | I2 = 62% | – |
OR – odds ratio, MD – mean difference, GGN – ground-glass nodule.
Discussion
In the present meta-analysis, the relative safety and efficacy of coil- and hook-wire-based approaches to LN localization prior to VATS resection were evaluated. There are certain advantages to this meta-analysis relative to other prior meta-analyses [9, 10]. For one, this analysis specifically included only comparative studies with balanced baseline data, reducing the potential for bias affecting the pooled results, in contrast to prior meta-analyses that compared successful localization rates based only on single-arm studies [9, 10]. Balanced baseline data cannot be guaranteed when comparing data from multiple centers. The present meta-analysis also compared certain variables not included in these prior meta-analyses, including operative duration and chest pain scores [9, 10].
The results of this meta-analysis suggest that CL was associated with significantly higher successful localization rates relative to HWL. This may be a consequence of higher hook-wire dislodgement or migration rates [9, 18]. When used, the hook-wire is placed within the lung parenchyma such that it extends through the chest wall, leaving it susceptible to dislodgement or migration in response to respiratory movement [19]. In contrast, CL entails the partial insertion of the coil into the lung parenchyma with the coil tail on the visceral pleura [4–6], making the coils less susceptible to dislodgement.
The CL and HWL procedures were associated with a similar duration of localization in this study, but significant heterogeneity was detected pertaining to this endpoint (I2 = 96%), suggesting that these results were not stable. The variability in duration of localization values across studies may be attributable to differences in the experience of the radiologists performing these procedures at different centers.
Analyses of the complication rates associated with these two procedures revealed that the CL approach was associated with a better safety profile than the HWL approach. This is consistent with the results of a prior study demonstrating that HWL was associated with a high frequency of pneumothorax [21]. Nakashima et al. similarly found hook-wire dislodgement to be associated with the incidence of pneumothorax, hemorrhage, and chest pain [22]. While pooled chest pain scores did not differ significantly between the HWL and CL groups in the present study, the p-value of 0.06 suggests a trend towards better safety outcomes in the CL group.
Pooled VATS and wedge resection procedure durations were comparable between the CL and HWL groups in the present study, suggesting that these two localization materials did not adversely interfere with these operative parameters.
This meta-analysis is subject to several limitations. For one, only a single RCT was included in this analysis, with all other studies having been retrospective in design, potentially biasing the results of this analysis. Second, the majority of the included studies exhibited multiple types of LNs, including solid LNs, GGNs, and mixed GGNs, potentially contributing to further bias. Third, some studies exhibited a lack of balance between the numbers of patients in the CL and HWL groups [14, 16, 19]. Additional well-designed RCTs focused on this research topic are still required. As most of the studies in this meta-analysis were conducted in Asian countries, future meta-analyses should seek to incorporate additional data from around the world.
Conclusions
The results of this meta-analysis suggest that CL is safer and more successful than HWL for patients undergoing VATS-based LN resection.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Toumazis I, Bastani M, Han SS, Plevritis SK. Risk-based lung cancer screening: a systematic review. Lung Cancer 2020; 147: 154-86. [DOI] [PubMed] [Google Scholar]
- 2.Wood DE, Kazerooni EA, Baum SL, et al. Lung Cancer Screening, Version 3.2018, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 2018; 16: 412-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Becker N, Motsch E, Trotter A, et al. Lung cancer mortality reduction by LDCT screening – results from the randomized German LUSI trial. Int J Cancer 2020; 146: 1503-13. [DOI] [PubMed] [Google Scholar]
- 4.Fu YF, Zhang M, Wu WB, Wang T. Coil localization-guided video-assisted thoracoscopic surgery for lung nodules. J Laparoendosc Adv Surg Tech A 2018; 28: 292-7. [DOI] [PubMed] [Google Scholar]
- 5.Zheng YG, Wang T, Rong PH, Fu YF. Computed tomography-guided trans-pulmonary-hepatic approach coil localization for pulmonary nodules near the right lung base. Kardiochir Torakochirur Pol 2021; 18: 173-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xia FF, Shi YB, Wang T, Fu YF. Computed tomography-guided transfissural coil localization of lung nodules. Thorac Cardiovasc Surg 2020; 68: 545-8. [DOI] [PubMed] [Google Scholar]
- 7.Ai M, Xu J. Computed tomography-guided simultaneous coil localization of multiple pulmonary nodules before video-assisted thoracoscopic surgery. Videosurgery Miniinv 2022; 17: 245-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Suzuki K, Nagai K, Yoshida J, et al. Video-assisted thoracoscopic surgery for small indeterminate pulmonary nodules: indications for preoperative marking. Chest 1999; 115: 563-8. [DOI] [PubMed] [Google Scholar]
- 9.Park CH, Han K, Hur J, et al. Comparative effectiveness and safety of preoperative lung localization for pulmonary nodules: a systematic review and meta-analysis. Chest 2017; 151: 316-28. [DOI] [PubMed] [Google Scholar]
- 10.Tang X, Jian HM, Guan Y, et al. Computed tomography-guided localization for multiple pulmonary nodules: a meta-analysis. Videosurgery Miniinv 2021; 16: 641-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev 2015; 4: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cook DA, Reed DA. Appraising the quality of medical education research methods: the Medical Education Research Study Quality Instrument and the Newcastle-Ottawa Scale-Education. Acad Med 2015; 90: 1067-76. [DOI] [PubMed] [Google Scholar]
- 13.Deng B, Kong P. Clinical application of microspring coil location before thoracoscopic pulmonary tuberculectomy. Modem Oncol 2020; 28: 954-7. [Google Scholar]
- 14.Hu L, Gao J, Chen C, et al. Comparison between the application of microcoil and hookwire for localizing pulmonary nodules. Eur Radiol 2019; 29: 4036-43. [DOI] [PubMed] [Google Scholar]
- 15.Hwang S, Kim TG, Song YG. Comparison of hook wire versus coil localization for video-assisted thoracoscopic surgery. Thorac Cancer 2018; 9: 384-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu J, Wang X, Wang Y, et al. Comparison of CT-guided localization using hook wire or coil before thoracoscopic surgery for ground glass nodules. Br J Radiol 2020; 93: 20190956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lu Y, Ding Y, Wang MS, et al. Clinical research of two localization methods in small pulmonary nodules video-assisted thoracoscopic surgery. Lin Chuang Fei Ke Za Zhi 2018; 23: 591-4. [Google Scholar]
- 18.Rostambeigi N, Scanlon P, Flanagan S, et al. CT fluoroscopic-guided coil localization of lung nodules prior to video-assisted thoracoscopic surgical resection reduces complications compared to hook wire localization. J Vasc Interv Radiol 2019; 30: 453-9. [DOI] [PubMed] [Google Scholar]
- 19.Wu BX, Liu H, Liu HL, et al. Application of microcoil localization in video-assisted thoracic surgery for pulmonary ground-glass nodules. J Cancer Control Treat 2021; 34: 247-51. [Google Scholar]
- 20.Yang F, Zhao H, Sui X, et al. Comparative study on preoperative localization techniques using microcoil and hookwire by propensity score matching. Thorac Cancer 2020; 11: 1386-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Iguchi T, Hiraki T, Gobara H, et al. CT fluoroscopy-guided preoperative short hook wire placement for small pulmonary lesions: evaluation of safety and identification of risk factors for pneumothorax. Eur Radiol 2016; 26: 114-21. [DOI] [PubMed] [Google Scholar]
- 22.Nakashima S, Watanabe A, Obama T, et al. Need for preoperative computed tomography-guided localization in video-assisted thoracoscopic surgery pulmonary resections of metastatic pulmonary nodules. Ann Thorac Surg 2010; 89: 212-8. [DOI] [PubMed] [Google Scholar]