Abstract
Despite numerous challenges, Montefiore Medical Center in New York City implemented a program aimed at providing comprehensive, evidence-based medical cannabis certifications to patients, including those who have been historically disenfranchised, and shares insights from five years of operation.
Summary
Bronx, New York–based Montefiore Medical Center established the Montefiore Medical Cannabis Program in 2016. The program was designed to increase access to such care, with a special focus on marginalized populations that have encountered particular barriers to care. In the first five years, MMCP has expanded the number of providers and has certified more than 1,600 patients. Yet, in many cases, patients have not been able to acquire cannabis at the regulated dispensaries. The academic medical center continues research in this developing care delivery service, and describes its experience over the years.
The Challenge
Medical cannabis is increasingly used to treat a variety of medical conditions, including chronic pain, epilepsy, post-traumatic stress disorder, multiple sclerosis, and others.1–4 Currently, 36 states and the District of Columbia provide lawful access to medical cannabis,5 and its use is supported by large majorities of the U.S. public as well as American physicians.6,7 Despite the widespread implementation of medical cannabis programs by state governments and an evidence base supporting its use as an effective treatment for multiple medical conditions,8,9 its classification under the Controlled Substances Act as a Schedule I substance — with no currently accepted medical use and a high potential for abuse10 — has limited development of clinical guidelines and hindered its entry into routine clinical practice.
Cannabis’s Schedule I classification creates barriers for patients and has resulted in inequitable access. In all states, individuals interested in medical cannabis must first find a practitioner who is able to certify patients, which in some states is limited to providers who have completed content-relevant medical education. Often, patients are limited to private practitioners, including online certifiers, who may charge substantial fees for certification. Because it is not covered by health insurance, cannabis must be purchased from a state-regulated cannabis dispensary, often at considerable cost to patients: a one-month supply of medical cannabis in New York State (NYS) can range from $75–$150 or more depending upon the amount used. For Black and Hispanic individuals, who have historically faced structural barriers to health care and suffered from years of disproportionately aggressive enforcement of cannabis laws,11,12 access to medical cannabis remains even more limited, in part due to lack of access to practitioners who certify patients, and to medical cannabis dispensaries in their neighborhoods.1,13,14
Interest in and demand for medical cannabis will almost certainly continue to increase as the evidence base expands and the political landscape evolves. Currently, patients who could benefit from it may be unsure how to access medical cannabis, and may continue riskier therapies such as opioids or turn to unregulated, non-medical cannabis to treat their symptoms. There is a pressing need for safe and rigorous incorporation of medical cannabis into medical education and clinical care in ways that can minimize harms and maximize benefits for patients. Academic medical centers are well-positioned to deliver evidence-based patient care and clinician training in this area, yet we are not aware of any other academic medical centers that have developed a coordinated medical cannabis program.
In this manuscript we describe the Montefiore Medical Cannabis Program (MMCP), implemented in a large academic medical center in Bronx, New York.
The Goal
Montefiore Medical Center (Montefiore) is an integrated academic health care delivery system in Bronx, New York. The Bronx, one of New York City’s five boroughs, had a 26% unemployment rate and a per capita income of less than $22,000 in 2019.15 Borough residents are overwhelmingly Black (43.6%) and Hispanic or Latino (56.4%); residents who are white and not Hispanic or Latino make up 9.0% of the population.15 Montefiore’s network in the Bronx includes four acute-care hospitals and more than 50 ambulatory care practices that deliver primary care to more than 300,000 patients each year.
Shortly after NYS authorized medical cannabis in 2016,16 we began to develop and implement the MMCP within Montefiore’s ambulatory care network. The goal in initiating the program was to provide access to medical cannabis certification for patients in a rigorous and safe manner and to serve a population that has historically suffered from delayed and limited access to innovative medical interventions and that has disproportionately felt the impact of criminal justice enforcement of cannabis. We believed that establishing a medical cannabis program within a large, integrated health system would be an important resource for our community that would offer several advantages compared to individual, for-profit medical cannabis certifiers. As providers in the health system, MMCP physicians have access to patients’ full medical records and can communicate directly with their other physicians, allowing a more complete understanding of patients’ medical histories for assessing potential benefits and risks of medical cannabis use. Providing cannabis certification within Montefiore’s primary care clinics would enable patients to access this service in a familiar setting that accepts their insurance plans, without extra out-of-pocket costs. By providing comprehensive assessments and evidence-based, non-judgmental guidance, our program would offer a highly valuable service to patients in the Bronx.
The Execution
Building the MMCP
Prior to launching the MMCP, in February and March 2016, we met with key institutional stakeholders in the departments of medical affairs, legal affairs, and risk management to discuss the scope of the program and ensure it could fully operate within the institution’s regulatory environment. The program launched in April 2016.
Over the program’s first year, five internal medicine physicians interested in participating registered as providers under the NYS Medical Marijuana Program; they began to evaluate patients seeking certification in three ambulatory care sites. To develop and promote best practices, the MMCP providers met regularly to review patient cases, discuss new or complex issues that arose during certification, and create standardized tools to guide medical cannabis evaluations and care within our environment. These included creating electronic health record (EHR) templates for conducting both comprehensive initial evaluations as well as follow-up appointments, establishing protocols for dosing recommendations and patient monitoring, and developing an EHR-based referral system to facilitate scheduling of patients across the network (Appendix).
To disseminate information about the MMCP, including indications and contraindications for certification and processes for referral, we delivered medical cannabis information sessions to primary care and sub-specialty providers throughout Montefiore’s network and developed a brochure describing the program. We aimed to establish connections with programs providing care to patients who have been historically disenfranchised within the health care system; in particular, we connected with those providing Montefiore’s large HIV, sickle cell disease, and opioid use disorder treatment services. The MMCP is fully integrated in Montefiore’s primary care practices and, as such, MMCP providers accept Medicare and Medicaid.
Developing visit protocols
The NYS medical cannabis program is unique in several ways. It is among the most highly regulated of all of the medical cannabis programs in the United States, with strict laws regarding the patient-clinician relationship and distribution of products by dispensaries.17 Products sold in NYS are tested to ensure the specified delta-9-tetrahydrocannabinol (THC) and cannabidiol (CBD) content and to detect potential contaminants. In this context, providers in NYS give recommendations on appropriate use of cannabis products for individual patients who then purchase it in medical cannabis dispensaries.18
MMCP providers are internal medicine, family medicine, and infectious diseases physicians situated in Montefiore’s six primary care teaching practices. Patients referred from other Montefiore providers or self-referred from outside the institution are scheduled for 30-minute appointments, either within the provider’s regular template or in dedicated cannabis patient care sessions. Visits are billed as primary care visits, typically under codes pertaining to the patient’s indication for medical cannabis, and generate an average of 1.5–2.0 physician work RVUs per encounter. Because the MMCP is integrated in primary care sites and staffed by physicians already working in these sites, additional operational costs have been minimal. While cannabis visits are billable to insurance under NYS regulations, medical cannabis products purchased at dispensaries are not covered by public or commercial insurance and must be purchased out of pocket.
Following existing standards for controlled substance prescribing, we developed a set of best practices for clinical visits to ensure that patients were rigorously evaluated and safely certified, informed by harm reduction principles and our expertise in opioid prescribing for chronic pain and buprenorphine prescribing for opioid use disorder. This approach included a review of substance use and mental health history, screening for cannabis use disorder, and using a “start low and go slow” approach aiming to guide patients towards use of appropriate products (Appendix).
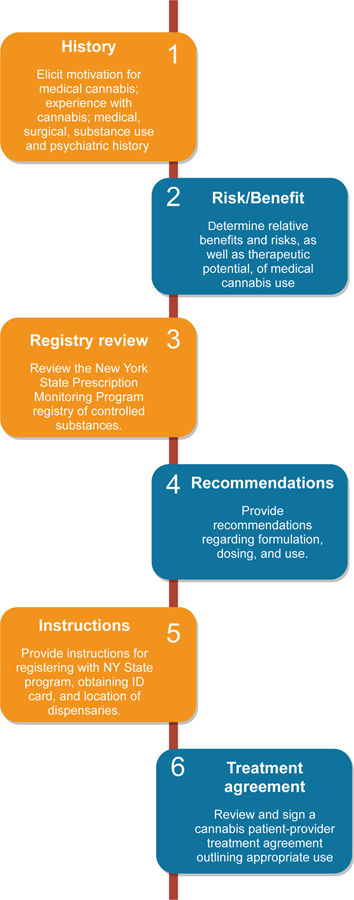
These practices (Figure 1), which will be disseminated in forthcoming guidelines from the NYS Department of Health AIDS Institute, include:
Eliciting patients’ motivation for medical cannabis; their experience with cannabis including current use; and their medical, surgical, substance use, and psychiatric history, including current medications.
Determining the relative benefits and risks of cannabis use for each patient, including potential for therapeutic improvement and potential for abuse. This includes screening for substance use disorders, including cannabis use disorder, and providing counseling on reduction or cessation of cannabis if indicated.
Reviewing the NYS Prescription Monitoring Program Registry of controlled substances.
For patients determined to be appropriate medical cannabis candidates, providing recommendations regarding formulation (e.g., pill, tincture), dosing (e.g., ratio of delta-9 tetrahydrocannabinol (THC) to cannabidiol (CBD), amount to use, how to titrate), and anticipatory guidance regarding potential adverse effects. These recommendations include informed discussions on potential cardiac and psychiatric effects of THC, potential acute and chronic adverse effects of cannabis use, how to minimize risk of adverse events, and how to use cannabis within the scope of state and federal regulations (e.g., not to cross state lines with cannabis products).
Providing patients with an overview of the NYS Medical Marijuana Program, including instructions for registering and obtaining their identification card, the location and procedures of dispensaries providing cannabis, and estimated cost.
Reviewing and signing a Cannabis Patient-Provider Agreement (based on existing opioid patient-provider agreements) outlining appropriate use, limitations of medical cannabis, and expectations for ongoing care.
Figure 1. Clinical Procedures for Evaluating Patients Interested in Medical Cannabis.
This six-step process is designed to assess the patient’s motivation for medical cannabis, determine relative risks and benefits of certification, and establish parameters for appropriate use.
Source: The author
Patients are seen for follow-up appointments three to six months after initial certification and at least annually. At that time, providers assess the type and frequency of cannabis used, response to treatment, any change in other medication use; probe for side effects and adverse events; and review medical cannabis products purchased in the NYS Prescription Monitoring Program Registry.
Ongoing Program Refinement
Over the course of the MMCP’s existence, we have developed the program in ways that continue to expand access to certification for patients while maintaining clinical rigor. In order to improve institutional knowledge about the benefits and risks of cannabis use and the availability of this resource for patients, MMCP providers continue to disseminate information about the program through conference presentations and departmental grand rounds. These efforts aim to encourage patient referrals and expand awareness of how to obtain training in medical cannabis certification. Recently, an electronic consult — an EHR-based asynchronous communication between health care providers — was launched to provide primary care and specialty clinicians access to medical cannabis experts who can answer clinical questions about individual patients.
For patients evaluated by MMCP providers, care is often coordinated with their primary care and subspecialty physicians through EHR-based communications (e.g., sharing visit notes), and by phone when necessary. In addition, each month, MMCP providers meet to discuss complex cases and ensure standardization (e.g., refining EHR templates). These conferences allow providers to obtain peer input on the relative risks and benefits of cannabis for patients who may be particularly vulnerable to adverse effects, such as patients who are pregnant, with comorbid cardiac disease, or have substance use disorders.
To provide an option for certified patients to use medical cannabis during hospitalization, in November 2019, we developed policies and procedures for inpatient use. This process included engaging stakeholders in nursing, medical affairs, pharmacy, legal affairs, and information technology; creating a policy for patients’ self-administration of medical cannabis consistent with federal and state law; and establishing a medical cannabis inpatient consult service to facilitate use. Inpatient use is allowable only by self-administration by the certified patient or designated caregiver, who keeps medical cannabis (purchased by the patient from a dispensary) in a locked safe at the bedside. A physician needs to authorize medical cannabis use after review of the patient’s certification documentation, the cannabis products, and NYS Prescription Monitoring Program data. A nurse assesses for contraindications (e.g., sedation) prior to dosing, then observes and documents self-administration.
Although current federal regulations restrict the conduct of randomized, controlled, and other therapeutic trials of cannabis, several MMCP providers are conducting observational and quasi-experimental clinical research on the use of medical cannabis, including federally funded projects.19–21 Findings from these studies have been incorporated directly into patient care protocols at Montefiore, and are contributing to the wider evidence base on appropriate medical cannabis use.
Finally, the MMCP has adapted procedures based on evolving regulations. Recent and pending changes to cannabis laws in NYS include legalization and sale of recreational cannabis as well as an expansion of indications for medical cannabis certification. For example, with whole flower products now being offered at dispensaries, we have incorporated increased counseling on the risks involved in smoking combustible cannabis (e.g., exposure to carcinogens, damage to bronchi) into visits. The expected plan to expand indications for medical cannabis as well as offset the cost of medical cannabis through sale recreational cannabis will likely lead to additional patients seeking certification. MMCP providers will need to adapt counseling to these changes.
Hurdles
As the MMCP has grown and patient demand has expanded, one challenge has been appointment availability. The number of medical providers offering certifications has grown over the past five years (from 5 in 2016 to 13 in 2021), and some physicians conduct weekly sessions dedicated exclusively to medical cannabis patients, allowing a total of 20–25 available MMCP appointments weekly. Nonetheless, interest from patients and providers has increased with expanding awareness of the program and exceeds availability. Appointment capacity is also impacted by other administrative and clinical responsibilities MMCP providers have that limit their clinic sessions (e.g., inpatient teaching service, protected research time). As a result, patients often wait several months for an initial evaluation; wait times for appointments have increased as the program has grown and are now as much as 4–5 months.
Scheduling medical cannabis patients within the practices has also presented difficulties. Most providers in the program are primary care physicians in practices that are not accustomed to receiving referrals. Therefore, initially, each practice developed its own workflows about which patients could be seen, by whom, and the length of the visit. This created logistical challenges for appointment scheduling, as patients often had to call multiple clinics to try to schedule an appointment with an available cannabis provider. Additionally, the 30 minutes allotted in primary care templates for new patients is not always sufficient to fully evaluate a patient, provide appropriate counseling on medical cannabis use, and provide instruction on completing the certification process and obtaining cannabis products. Training clinic support staff to assist patients with certification and use of follow-up telemedicine appointments can help address this hurdle.
The process of obtaining medical cannabis is not straightforward, and multiple patient-level barriers have emerged. Many patients within Montefiore’s health system have limited health and technological literacy, impacting their ability to navigate and complete the online process necessary to become registered as a NYS medical cannabis patient. MMCP has limited resources available to help patients with this process and, as a result, approximately 14% of patients who saw a medical cannabis provider since the program’s inception never registered in the state system. Because cannabis is not covered by any medical insurance and the cost can be prohibitive (e.g., a 25ml bottle of 1:1 THC:CBD tincture, equivalent to 20–30 doses, can cost from $75–$150),22,23 many patients who are certified cannot regularly access medical cannabis products, although some dispensaries offer reduced price for certain products. Indeed, approximately half of patients certified by MMCP providers never purchased cannabis products from a medical dispensary. NYS’s plan to offset medical cannabis costs through sales of recreational cannabis may address this barrier. Additionally, patients are often hesitant to disclose non-medical cannabis use prior to certification, and providers who are unaware of their existing tolerance may recommend products that are ineffective because of low potency. Our approach emphasizes inquiring about patients’ cannabis use and its impact on their symptoms in a nonjudgmental way, facilitating a therapeutic alliance.
Provider-level barriers have also negatively impacted uptake of medical cannabis as well. Many providers in the institution are not aware of the ability to refer to a medical cannabis provider for evaluation and certification. Among those that do know of the program, a substantial number of referrals are inappropriate (e.g., the patient does not qualify under NYS regulations). Finally, for medical cannabis providers, fully evaluating the benefits and risks of cannabis for complex patients often requires input from other physicians (e.g., psychiatrists, cardiologists), which can be difficult to coordinate in a timely manner, and sometimes requires a second appointment to complete the certification.
Finally, MMCP operations were severely interrupted during the Covid-19 surge of March-May 2020, as outpatient practices were closed and providers were working on inpatient Covid-19 wards. During these months, the NYS Department of Health issued guidance allowing telemedicine for medical cannabis certification and classifying dispensaries as essential businesses. As outpatient practices began seeing patients by telemedicine and eventually for in-person appointments, MMCP visit volume began to return to pre-pandemic levels.
The Team
Initial parameters for the MMCP were developed by a team of primary care–based general internists, one of whom is the Chief of the Division of General Internal Medicine, as well as medical directors of two of Montefiore’s ambulatory care clinics. Additional input was obtained from the Vice President of the Montefiore Medical Group (the ambulatory care network), Chief Legal Officer, and Vice President for Medical Affairs, with approval of the program by Montefiore’s Chief Executive Officer. Development of a policy for inpatient use of medical cannabis included additional contributions from the Vice President of Nursing as well as the Senior Director of Pharmacy Services.
Metrics
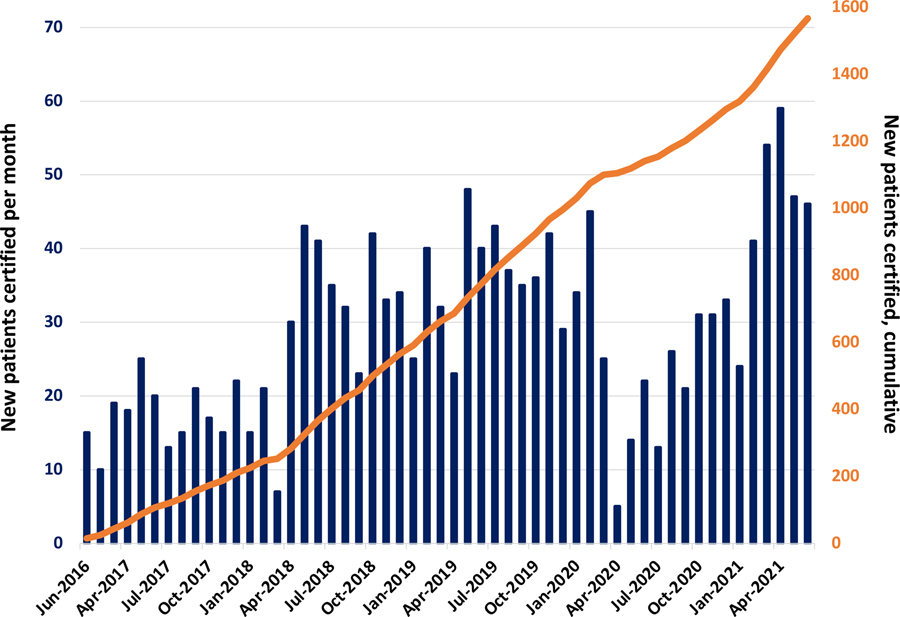
Over five years, through 2021, MMCP has expanded throughout the institution. Initially launched in three out of Montefiore’s ambulatory care sites in the Bronx, the program now includes 13 internal medicine, family medicine, and infectious diseases physicians in all six of the teaching practices where faculty provide direct care and supervise residents. A total of 1,965 EHR referrals have been made within the institution, with 1,567 unique patients certified as of June 2021 (Figure 2). Common indications for certification included chronic pain (78%), HIV (7%), neuropathies (6%), and post-traumatic stress disorder (4%).
FIGURE 2: Number of Patients Newly Certified for Medical Cannabis Through the Montefiore Medical Cannabis Program, By Month and Cumulatively, 2016–2021.
Over five years of program implementation, capacity for certification has increased with higher numbers of monthly certifications as additional providers joined the MMCP. During the Covid-19 surge in New York City in early 2020, operations were severely impacted, with certifications returning to pre-pandemic levels after several months.
Source: The authors
Among 1,417 patients with available demographic and clinical data, 529 (37%) were Black and 632 (45%) Hispanic, median age was 56 years, and 605 were enrolled in Medicaid (Table 1).
Table 1.
Characteristics of Patients Referred for and Certified for Medical Cannabis Among Patients With Available Demographic and Clinical Data, 2016–2021
| Bronx population (N=1.4 million) | Patients referred through EHR (N=1,965) | Patients certified by a medical cannabis provider* (N=1,417) | |
|---|---|---|---|
|
| |||
| Median age (IQR) | 34a | 54 (41–62) | 56 (45–65) |
| Female gender | 53%a | 1,270 (65%) | 882 (62%) |
| Hispanic ethnicity | 56%a | 884 (45%) | 632 (45%) |
| Race | |||
| Black | 35%a | 775 (39%) | 529 (37%) |
| White | 22%a | 195 (10%) | 154 (11%) |
| Other | 43%a | 815 (41%) | 626 (44%) |
| Declined or missing | 0 | 180 (9%) | 108 (8%) |
| Medicaid insurance | 36%b | 945 (48%) | 605 (43%) |
| Medical conditions | |||
| HIV | 2%c | 288 (15%) | 218 (15%) |
| Sickle cell disease | 0.1%d | 121 (6%) | 61 (4%) |
| Opiate use disorder | Uncertain | 189 (10%) | 208 (15%) |
Abbreviations: EHR = electronic health record; IQR = interquartile range.
not all patients were linked to a provider through an EHR-based referral
Sources: The authors. Bronx demographic data as noted.
= U.S. Census Bureau. American Community Survey, 2019. Bronx County, New York. Table DP05. https://data.census.gov/cedsci/table?tid=ACSDP5Y2019.DP05&g=0400000US36_0500000US36005.
= New York City Department of Health. Community Health Survey 2019. https://www1.nyc.gov/site/doh/data/data-sets/community-health-survey-public-use-data.page.
= New York City Department of Health and Mental Hygiene. HIV/AIDS Annual Surveillance Statistics 2019. Table 1.1. https://www1.nyc.gov/assets/doh/downloads/pdf/ah/surveillance2019-tables-all.pdf.
= Estimate based on Wang Y, Kennedy J, Caggana M, et al. Sickle cell disease incidence among newborns in New York State by maternal race/ethnicity and nativity. Genet Med. 2013 March; 15(3): 222–228. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4453875/pdf/nihms-693235.pdf.
Among those certified, many have not successfully accessed medical cannabis: an analysis of a subset of 562 MMCP patients who were certified between 2017–2019 demonstrated that 254 (45%) subsequently purchased cannabis at a NYS dispensary (unpublished data). Additional metrics of interest that will be examined as part of ongoing program evaluation include average wait time for an appointment with an MMCP provider, the proportion of patients seen by an MMCP provider who were subsequently certified, and the proportion of patients certified who were seen for a recertification visit, which is required at least annually in the NYS Medical Marijuana Program.
Where To Start
Implementing an academic medical center–based medical cannabis program has been a complex and iterative effort. Replicating such efforts elsewhere will likely require early support from institutional stakeholders including administrative and clinical leadership, legal affairs, and information technology. Establishing a multidisciplinary team that can review existing best practices and adapt them to the local setting, including state-specific medical cannabis laws, in an evidence-based manner can ensure safety and clinical rigor. Plans for provider education about indications for and risks and benefits of medical cannabis, as well as outreach to communities served by the medical center, should be developed to ensure that patients who most stand to benefit from medical cannabis will be able to access it.
Supplementary Material
Key Takeaways.
Academic medical centers and integrated health systems can play a leading role in delivering rigorous, evidence-based, and equitable treatment for patients seeking medical cannabis.
There is substantial patient demand for medical cannabis, but providers and patients need education about appropriate referrals, and the risks and benefits of medical cannabis use.
Establishment of health system–based medical cannabis programs requires coordination among clinical providers, hospital leadership, and legal affairs.
Integrating medical cannabis into clinical care can be accomplished in academic medical centers using measures similar to those developed for other controlled substances.
Disclosures
Jonathan Ross is supported by the National Institute of Mental Health (K23MH114752).
Deepika Slawek and Joanna L. Starrels are supported by the National Institute on Drug Abuse (K23DA053997, K24DA046309).
Jaclyn Yamada, Chinazo O. Cunningham, and Julia H. Arnsten have nothing to disclose.
Additional support was provided to Albert Einstein College of Medicine by the National Institute on Drug Abuse (R01DA044171).
Contributor Information
Jonathan Ross, Assistant Professor of Medicine, Montefiore Health System, Division of General Internal Medicine, Bronx, New York, USA; Assistant Professor of Medicine, Albert Einstein College of Medicine, Division of General Internal Medicine, Bronx, New York, USA.
Jaclyn Yamada, Resident, Northwell Health, New Hyde Park, New York, USA; Former medical student, Albert Einstein College of Medicine, Division of General Internal Medicine, Bronx, New York, USA.
Deepika Slawek, Assistant Professor of Medicine, Montefiore Health System, Division of General Internal Medicine, Bronx, New York, USA; Assistant Professor of Medicine, Albert Einstein College of Medicine, Division of General Internal Medicine, Bronx, New York, USA.
Joanna L. Starrels, Associate Professor of Medicine, Montefiore Health System, Division of General Internal Medicine, Bronx, New York, USA; Associate Professor of Medicine, Albert Einstein College of Medicine, Division of General Internal Medicine, Bronx, New York, USA.
Chinazo O. Cunningham, Professor of Medicine, Family and Social Medicine, and Psychiatry and Behavioral Sciences, Albert Einstein College of Medicine, Division of General Internal Medicine, Bronx, New York, USA.
Julia H. Arnsten, Professor of Medicine, Epidemiology & Population Health, and Psychiatry and Behavioral Sciences, Montefiore Health System, Division of General Internal Medicine, Bronx, New York, USA; Professor of Medicine, Epidemiology & Population Health, and Psychiatry and Behavioral Sciences, Albert Einstein College of Medicine, Division of General Internal Medicine, Bronx, New York, USA.
References
- 1.Mahabir VK, Merchant JJ, Smith C, Garibaldi A. Medical cannabis use in the United States: a retrospective database study. J Cannabis Res 2020;2:32 https://jcannabisresearch.biomedcentral.com/articles/10.1186/s42238-020-00038-w https://doi.org/10.1186/s42238-020-00038-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Piper BJ, DeKeuster RM, Beals ML, et al. Substitution of medical cannabis for pharmaceutical agents for pain, anxiety, and sleep. J Psychopharmacol 2017;31:569–75 https://journals.sagepub.com/doi/10.1177/0269881117699616 https://doi.org/10.1177/0269881117699616. [DOI] [PubMed] [Google Scholar]
- 3.Hill KP. Medical marijuana for treatment of chronic pain and other medical and psychiatric problems: a clinical review. JAMA 2015;313:2474–83 https://jamanetwork.com/journals/jama/article-abstract/2338266 https://doi.org/10.1001/jama.2015.6199. [DOI] [PubMed] [Google Scholar]
- 4.Boehnke KF, Gangopadhyay S, Clauw DJ, Haffajee RL. Qualifying conditions of medical cannabis license holders in the United States. Health Aff (Millwood) 2019;38:295–302 https://www.healthaffairs.org/doi/10.1377/hlthaff.2018.05266 https://doi.org/10.1377/hlthaff.2018.05266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.ProCon.Org (Encyclopaedia Britannica). Legal medical marijuana states and DC. Updated June 22, 2021. Accessed July 9, 2021. https://medicalmarijuana.procon.org/legal-medical-marijuana-states-and-dc/.
- 6.Van Green T Americans overwhelmingly say marijuana should be legal for recreational or medical use. Pew Research Center. April 16, 2021. Accessed July 16, 2021. https://www.pewresearch.org/fact-tank/2021/04/16/americans-overwhelmingly-say-marijuana-should-be-legal-for-recreational-or-medical-use/. [Google Scholar]
- 7.Frellick M Medical, recreational marijuana should be legal, most clinicians say. Medscape. September 12, 2018. Accessed July 16, 2021. https://www.medscape.com/viewarticle/901761. [Google Scholar]
- 8.National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division; Board on Population Health and Public Health Practice; Committee on the Health Effects of Marijuana: An Evidence Review and Research Agenda. The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. Washington (DC): National Academies Press (US), 2017. https://www.nap.edu/catalog/24625/the-health-effects-of-cannabis-and-cannabinoids-the-current-state. [PubMed] [Google Scholar]
- 9.Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA 2015;313:2456–73 https://jamanetwork.com/journals/jama/fullarticle/2338251 https://doi.org/10.1001/jama.2015.6358. [DOI] [PubMed] [Google Scholar]
- 10.Department of Justice/Drug Enforcement Administration. Marijuana/Cannabis. April 2020. Accessed November 16, 2021. https://www.dea.gov/sites/default/files/2020-06/Marijuana-Cannabis-2020_0.pdf.
- 11.Golub A, Johnson BD, Dunlap E. The race/ethnicity disparity in misdemeanor marijuana arrests in New York City. Criminol Public Policy 2007;6:131–64 https://onlinelibrary.wiley.com/doi/10.1111/j.1745-9133.2007.00426.x https://doi.org/10.1111/j.1745-9133.2007.00426.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Solomon R Racism and its effect on cannabis research. Cannabis Cannabinoid Res 2020;5:2–5 https://www.liebertpub.com/doi/10.1089/can.2019.0063 https://doi.org/10.1089/can.2019.0063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Salazar CA, Tomko RL, Akbar SA, Squeglia LM, McClure EA. Medical cannabis use among adults in the southeastern United States. Cannabis 2019;2:53–65 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6388700/ https://doi.org/10.26828/cannabis.2019.01.005. [PMC free article] [PubMed] [Google Scholar]
- 14.Cooke A, Freisthler B, Mulholland E. Examination of market segmentation among medical marijuana dispensaries. Subst Use Misuse 2018;53:1463–7 https://www.tandfonline.com/doi/abs/10.1080/10826084.2017.1413391?journalCode=isum20 https://doi.org/10.1080/10826084.2017.1413391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.U.S. Census Bureau. QuickFacts: Bronx County, New York. July 1, 2019. Accessed November 16, 2021. https://www.census.gov/quickfacts/fact/table/bronxcountynewyork/PST045219.
- 16.New York State Department of Health. Press Release. NYS Department of Health Announces; January 7 Launch of Medical Marijuana Program. January 5, 2016. Accessed December 21, 2021. https://www.health.ny.gov/press/releases/2016/2016-01-05_launch_of_medical_marijuana_program.htm. [Google Scholar]
- 17.Richard EL, Althouse AD, Arnsten JH, et al. How medical are states’ medical cannabis policies?: proposing a standardized scale. Int J Drug Policy 2021;94:103202 https://www.sciencedirect.com/science/article/abs/pii/S0955395921001006?via%3Dihub10.1016/j.drugpo.2021.103202 https://doi.org/10.1016/j.drugpo.2021.103202. [DOI] [PubMed] [Google Scholar]
- 18.New York State, Department of Health. The New York State Medical Marijuana Program. Revised November 2021. Accessed November 24, 2021. https://www.health.ny.gov/regulations/medical_marijuana/. [Google Scholar]
- 19.Cunningham CO, Starrels JL, Zhang C, et al. Medical Marijuana and Opioids (MEMO) Study: protocol of a longitudinal cohort study to examine if medical cannabis reduces opioid use among adults with chronic pain. BMJ Open 2020;10:e043400 https://bmjopen.bmj.com/content/10/12/e043400 https://doi.org/10.1136/bmjopen-2020-043400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Slawek DE, Arnsten J, Sohler N, et al. Daily and near-daily cannabis use is associated with HIV viral load suppression in people living with HIV who use cocaine. AIDS Care 2021;33:1350–7 https://www.tandfonline.com/doi/abs/10.1080/09540121.2020.1799922?journalCode=caic20 https://doi.org/10.1080/09540121.2020.1799922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.First-year trajectories of medical cannabis use among adults taking opioids for chronic pain: an observational cohort study. Pain Med 2021. December 11;22(12):3080–3088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Verilife. Bronx Dispensary Product Menu. Accessed September 23, 2021. https://www.verilife.com/ny/menu/verilife-bronx-ny.
- 23.Vireo. Medical Marijuana Dispensary & Products. Accessed September 23, 2021. https://shop.vireohealth.com/.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.