Short abstract
Content available: Author Interview and Audio Recording
Watch the interview with the author.
Listen to an audio presentation of this article.
INTRODUCTION
Hepatic encephalopathy (HE) is a common and serious symptom of advanced liver disease. The goal of this article is to explain HE and treatments for patients and their caregivers. It is not intended to give medical advice and cannot replace the role of a patient's medical team. This article is based on the 2014 guidelines by the American Association for the Study of Liver Diseases, the primary professional medical society for liver disease in the United States (the guidelines can be found online at: https://www.aasld.org/sites/default/files/2019‐06/hepaticencephalopathy82014.pdf). 1
WHAT IS HE?
HE is changes in brain function in patients with severe liver disease. It results in a wide range of nerve and mood symptoms, which range from mild confusion to coma.
Some important things to know include the following:
1. HE can develop in patients with any cause of liver disease.
2. Most people with HE have very severe liver disease, or cirrhosis.
3. HE is the most frequent complication of cirrhosis that leads to hospitalization.
4. People with cirrhosis can have other reasons (besides HE) that can lead to similar symptoms.
5. HE symptoms can improve if the liver gets healthier (or with a liver transplant).
Besides changes in thinking, other symptoms of HE include poor appetite, sleep, and mood, as well as trouble with self‐care and work. 2 The West Haven Criteria, listed in Table 1, are a scale used by health care providers to grade the seriousness of HE. Grade I on this scale is difficult for physicians to detect, but people who know the patient well might be able to see confusion or forgetfulness. Physicians look for difficulty thinking with simple questions and check for hand flapping, called asterixis, as in Figure 1.
TABLE 1.
West haven criteria for HE
| Grade | Description |
|---|---|
| Grade I |
|
| Grade II |
|
| Grade III |
|
| Grade IV |
|
FIGURE 1.
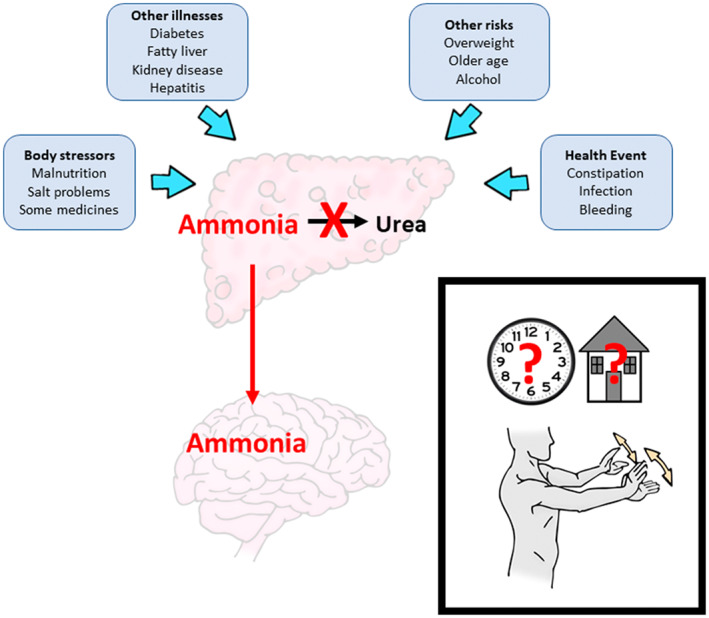
Why HE happens. A diseased liver is unable to change toxic ammonia into urea to leave the body in the urine. This is worsened by a patient's other illnesses and risks, and is also made worse by body stressors and sudden health events. Ammonia then builds up in the blood and gets to the brain, where it causes the findings of HE (boxed inset): confusion about time, date, and place, as well as asterixis or hand flapping. 1 , 3
WHY DOES HE HAPPEN?
The cause of HE is an active area of research. HE can be triggered by one reason or a combination of multiple reasons. A damaged liver struggles with the breakdown products of the protein we eat. Ammonia is a key breakdown product of proteins, and the change of ammonia to urea, which can be removed more easily from the body, happens mostly by the urea cycle, which is found only in the liver. In a diseased liver, ammonia builds up in the blood, where it can then injure nerves in the brain. 3 , 4 Extra stress on the liver, such as alcohol, obesity, hepatitis infection, diabetes, certain medications, and aging, can increase the risk for HE developing, as in Figure 1.
Remember, other disease processes can present with symptoms similar to that of HE. That is why when patients present with symptoms of HE, they are examined and tested for other possible causes that can add to their confusion. This includes new medications and drugs (prescribed and over the counter), pain medications, a recent injury or trauma, bleeding, kidney problems, and infections in the blood, urine, or lungs.
WHAT IS THE TREATMENT FOR HE?
Treatment for HE starts with checking for possible triggers that can be treated. For example, if the patient has a new infection in the lungs or urine, treating the infection with antibiotics will help the HE. Another example is when there are problems with electrolytes in the blood. This can be treated with adjusting certain medications. A third common example is bleeding. Sometimes patients with cirrhosis can present with obvious or silent bleeding that worsens HE. Finding and stopping the source of bleeding can improve HE.
The ultimate goal of HE treatment is to decrease the number of severe confusion episodes and to prevent patients from being admitted to the hospital. It is difficult to predict when HE will happen. However, patients and especially caregivers should watch for little and big changes in personality or thinking. If they notice these changes, they should let their medical care team know.
There are many parts to the management of HE. For example:
HE is treated by prevention, early diagnosis, and care of emergencies and causes.
Patients with HE must stop activities such as driving.
Patients with HE should document their wishes, such as in an advance directive, and choose a person to speak for them, such as a surrogate decision maker, in case they cannot speak for themselves.
HE treatment focuses on ridding the body of ammonia through laxatives such as lactulose.
Nutrition is very important in cirrhosis care.
HE can improve if the liver gets healthier (or with a liver transplant).
The medicines for HE work by slowing ammonia creation and uptake in the gut. Lactulose is a laxative that works this way by pulling out toxic ammonia from the body through the stool (Table 2). Lactulose can be combined with rifaximin, an antibiotic the gut cannot absorb that fights gut bacteria that produce ammonia. The goal of treatment is to reduce serious HE episodes and hospitalizations.
TABLE 2.
Medications and therapies used to treat HE
| Therapy | How it works | Goal |
|---|---|---|
| Lactulose | Laxative (causes frequent bowel movements that make you “poop out” the ammonia from your body) | First line to treat HE |
| Goal is to have 3–4 loose bowel movements per day | ||
| May cause bloating | ||
| Rifaximin | Antibiotic not absorbed from the gut | Use with lactulose |
| Take one tablet twice a day | ||
| Nutrition | High‐calorie and ‐protein meals to maintain muscle | Goal is to build muscle, which helps process ammonia, because many patients with cirrhosis lose muscle |
The key treatment, other than medicines such as lactulose, is nutrition, as listed in Table 2. Serious muscle loss (called sarcopenia) is common in cirrhosis. This can make HE worse because healthy muscle can help break down ammonia. It is important to get enough calories and protein to build muscle, which decreases the risk for HE. High‐protein diets are recommended in patients with cirrhosis to help build muscle. The average needs for calories and protein are listed in Table 3. For example, there is 6 g of protein in an egg and 80 g in a salmon fillet. These high numbers of calories and protein usually mean special nutrition drinks are needed. Small, frequent meals and snacks before bedtime is good because a lot of muscle building happens while you sleep at night.
TABLE 3.
Recommended calorie and protein intake for those with cirrhosis
| Patient | Calories needed: 35–40 kcal/kg | Protein needed: 1.2–1.5 g of protein/kg/day |
|---|---|---|
| Average woman 130 pounds (59 kg) | 2360 calories | 88.5 g of protein |
| Average man 160 pounds (73 kg) | 2920 calories | 110 g of protein |
Liver transplantation can cure HE but may take time. Continued confusion may be seen, especially shortly after surgery, often as a result of stress on the body from the surgery, new medications to prevent rejection of the new liver (called immunosuppressants), or other new and old illnesses that are diagnosed.
HE is very hard for patients with cirrhosis and their families. HE symptoms often change. It is important to work with your medical care team to adjust the amount of lactulose you are taking and to identify possible things that can sometimes make HE worse. Please be patient with your loved ones and yourself.
CONFLICT OF INTEREST
Nothing to report.
ACKNOWLEDGMENTS
The authors thank Nancy Reau, MD, for her contributions to this Patient Page.
Green EW, Mitra A. Diagnosis and management of hepatic encephalopathy: A summary for patients. Clinical Liver Disease. 2022;20:90–92. 10.1002/cld.1236
REFERENCES
- 1. Vilstrup H, Amodio P, Bajaj J, Cordoba J, Ferenci P, Mullen KD, et al. Hepatic encephalopathy in chronic liver disease: 2014 practice guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the liver. Hepatology. 2014;60:715–35. [DOI] [PubMed] [Google Scholar]
- 2. Elsaid MI, John T, Li Y, Pentakota SR, Rustgi VK. The health care burden of hepatic encephalopathy. Clin Liver Dis. 2020;24:263–75. [DOI] [PubMed] [Google Scholar]
- 3. Rose CF, Amodio P, Bajaj JS, Dhiman RK, Montagnese S, Taylor‐Robinson SD, et al. Hepatic encephalopathy: novel insights into classification, pathophysiology and therapy. J Hepatol. 2020;73:1526–47. [DOI] [PubMed] [Google Scholar]
- 4. Wijdicks EF. Hepatic encephalopathy. N Engl J Med. 2016;375:1660–70. [DOI] [PubMed] [Google Scholar]


