Abstract
We conducted 2 analyses using administrative data to understand whether more family physicians in Ontario, Canada stopped working during the COVID-19 pandemic compared with previous years. First, we found 3.1% of physicians working in 2019 (n = 385/12,247) reported no billings in the first 6 months of the pandemic; compared with other family physicians, a higher portion were aged 75 years or older (13.0% vs 3.4%, P <0.001), had fee-for-service reimbursement (37.7% vs 24.9%, P <0.001), and had a panel size under 500 patients (40.0% vs 25.8%, P <0.001). Second, a fitted regression line found the absolute increase in the percentage of family physicians stopping work was 0.03% per year from 2010 to 2019 (P = 0.042) but 1.2% between 2019 to 2020 (P <0.001). More research is needed to understand the impact of physicians stopping work on primary care attachment and access to care.
Key words: primary health care; COVID-19; workforce; health services, general practitioners; family physicians
INTRODUCTION
The COVID-19 pandemic disrupted how care was delivered by family physicians. To limit transmission, practices adopted a range of measures including active and passive screening, cleaning, strict use of personal protective equipment, and reducing the number of staff and patients in the office. In the first few weeks of the pandemic, nonessential care was deferred1 and total visits to primary care decreased by nearly 30%.2 At the same time, there was a dramatic shift to virtual care2 and primary care physicians were tasked with other system roles.3
These changes placed extraordinary stress on family physicians, particularly in Canada and the United States, where many operate as small business owners and rely on fee-for-service billings for revenue.4 Surveys of family physicians during the first wave of the pandemic detail numerous challenges including reduced revenue, retention of office staff, and difficulty obtaining personal protective equipment; many physicians also worried about their own personal safety.5,6 These challenges may have led some family physicians to prematurely stop working7–9 but more research is needed in different settings.
In Ontario, physicians are primarily paid through the provincial health insurance plan which provides coverage to all provincial residents for physician visits. Roughly 80% of family physicians work in a patient enrollment model where they formally enroll patients and between 15% and 70% of payment is based on age-sex adjusted capitation.10,11 The remaining 20% largely operate independent, fee-for-service practices with many working in walk-in clinics or doing focused practice.12 We sought to understand the number and characteristics of physicians stopping work in the first 6 months of the pandemic in Ontario, Canada.
METHODS
We conducted 2 analyses using routinely collected data including billing claims. Data sets only included de-identified data that were linked using unique encrypted identifiers and analyzed at ICES. ICES is an independent, nonprofit research institute whose legal status under Ontario’s health information privacy law allows it to collect and analyze health care and demographic data, without consent, for health system evaluation and improvement. Patients were attributed to physicians based on enrollment data; patients who were not enrolled were attributed to a physician using virtual rostering according to the highest billings for that patient.
First, we calculated the ratio of total visits (office, virtual, and home) from March 11, 2020 to September 29, 2020 to total visits in the same period in 2019 for each family physician who had at least 50 billing days in 2019; we assessed variation in the ratio within and across physician groups. We identified physicians who had 0 visits from March 11, 2020 to September 29, 2020 and compared their characteristics to those who had any visits during that time period using a t-test for mean and χ2 test for categorical variables.
Second, we conducted a repeated cross-sectional analysis. For each year from 2010 to 2020, we examined the cohort of physicians practicing in the first quarter of the year and noted the number and percent who stopped practicing (ie, had no billings) between April 1 and September 30. We fit a linear regression line to the number of physicians per 1,000 who stopped practicing in each year from 2010 to 2019 and used this to predict the expected 2020 outcome; we compared this to the observed 2020 outcome. Analysis was done in SAS Enterprise Guide (SAS Institute Inc) and graphs were produced in R v4.0.5 (the R Foundation).
RESULTS
We analyzed data for 12,247 family physicians practicing in Ontario in 2019 (Table 1). During the week of September 29, 2019 there were 916,831 total visits in 2019, of which 97% were in-office, compared with 903,402 total visits in 2020, of which 40% were in-office (Supplemental Figure 1). Most family physicians had 0 to 50% fewer total visits post-pandemic compared with the same period in 2019 (Supplemental Figure 2) but there was considerable variation both between and within groups (Supplemental Figure 3).
Table 1.
Characteristics of All Family Physicians in Ontario, Canada Active in 2019 and Comparison of Characteristics Between Those With No Outpatient Visits During the First 6 Months of the COVID-19 Pandemic (March-September 2020) and Those With Any Visits
| Characteristic | All Family Physicians Active in 2019 |
Family Physicians With Any Outpatient Visits From March to September 2020 |
Family physicians With No Outpatient Visits March to September 2020 |
P Value |
|---|---|---|---|---|
| Physician age group, y | n = 12,247 (%) | n = 11,862 (%) | n = 385 (%) | |
| ≤44 | 4,320 (35.3) | 4,188 (35.3) | 132 (34.3) | <0.001 |
| 45-64 | 5,746 (46.9) | 5,644 (47.6) | 102 (26.5) | |
| 65-74 | 1,718 (14.0) | 1,618 (13.6) | 100 (26.0) | |
| ≥75 | 454 (3.7) | 404 (3.4) | 50 (13.0) | |
| Missing | 9 (0.1) | 8 (0.1) | 1 (0.3) | |
| Physician age, y | ||||
| Mean ± SD | 51 ± 13 | 51 ± 13 | 56 ± 16 | <0.001 |
| Physician sex | ||||
| Female | 5,861 (47.9) | 5,674 (47.8) | 187 (48.6) | 0.775 |
| Male | 6,386 (52.1) | 6,188 (52.2) | 198 (51.4) | |
| Model of care | ||||
| PEM: Non-team capitation | 3,114 (25.4) | 3,052 (25.7) | 62 (16.1) | <0.001 |
| PEM: Enhanced fee-for-service | 2,854 (23.3) | 2,769 (23.3) | 85 (22.1) | |
| PEM: Team-based capitation | 2,893 (23.6) | 2,825 (23.8) | 68 (17.7) | |
| Non-PEM: Straight fee-for-service | 3,099 (25.3) | 2,954 (24.9) | 145 (37.7) | |
| Missing | 287 (2.3) | 262 (2.2) | 25 (6.5) | |
| Rurality (RIO) | ||||
| Big cities (0) | 5,971 (48.8) | 5,773 (48.7) | 198 (51.4) | 0.399 |
| Smaller cities (1 – 9) | 3,338 (27.3) | 3,245 (27.4) | 93 (24.2) | |
| Small towns (10 – 39) | 1,817 (14.8) | 1,756 (14.8) | 61 (15.8) | |
| Rural (≥40) | 1,111 (9.1) | 1,079 (9.1) | 32 (8.3) | |
| Missing | 10 (0.1) | 9 (0.1) | 1 (0.3) | |
| Physician panel size group | ||||
| <100 | 1,847 (15.1) | 1,761 (14.8) | 86 (22.3) | <0.001 |
| 100-499 | 1,378 (11.3) | 1,310 (11.0) | 68 (17.7) | |
| 500-999 | 2,369 (19.3) | 2,287 (19.3) | 82 (21.3) | |
| 1,000-1,499 | 2,980 (24.3) | 2,917 (24.6) | 63 (16.4) | |
| 1,500-1,999 | 1,899 (15.5) | 1,858 (15.7) | 41 (10.6) | |
| ≥2,000 | 1,487 (12.1) | 1,467 (12.4) | 20 (5.2) | |
| Missing | 287 (2.3) | 262 (2.2) | 25 (6.5) | |
| Physician panel size | ||||
| Mean ± SD | 1,097 ± 829 | 1,106 ± 829 | 788 ± 741 | <0.001 |
| Median (IQR) | 1,059 (417-1,580) | 1,069 (437-1,588) | 673 (114-1,259) | <0.001 |
| Days with ≥1 billing, no. | ||||
| March – Sept 2019 Mean ± SD | 100 ± 35 | 101 ± 35 | 73 ± 35 | <0.001 |
| March – Sept 2020 Mean ± SD | 109 ± 42 | 109 ± 42 | 0 ± 0 | |
| Total visits, no. | ||||
| March – Sept 2019 Mean ± SD | 2,061 ± 1,795 | 2,087 ± 1,803 | 1,266 ± 1,281 | <0.001 |
| March – Sept 2020 Mean ± SD | 1,703 ± 1,674 | 1,758 ± 1,672 | 0 ± 0 | <0.001 |
| Percent of virtual visits | ||||
| March – Sept 2019 | 2.0 | 2.0 | 0.07 | <0.001 |
| March – Sept 2020 | 66.0 | 66.0 | ||
PEM = patient enrollment model; RIO = Rurality Index of Ontario.
Notes: The total number of billing days for the study period including weekends and holidays was 203 days (29 weeks). Rurality categorized using the Rurality Index of Ontario. See Kralj B. Measuring Rurality — RIO2008 BASIC: Methodology and Results. Ontario Medical Association; 2009. Accessed Sep 22, 2020. https://content.oma.org//wp-content/uploads/2008rio-fulltechnicalpaper.pdf
There were 3.1% (n = 385) of physicians practicing in 2019 who had no primary care visits during the first 6 months of the pandemic (Table 1). Compared with other family physicians, a higher portion of physicians with no primary care visits were aged 75 years or older (13.0% vs 3.4%, P <0.001), practicing fee-for-service (37.7% vs 24.9%, P <0.001), had a panel size under 500 patients (40.0% vs 25.8%, P <0.001), had fewer billing days in 2019 (mean 73 vs 101, P <0.001), and had fewer total visits in 2019 (1,266 vs 2,087, P <0.001). Fifty-six percent (n = 215) of those who stopped working practiced in a patient enrollment model (PEM). The percentage of all family physicians who stopped work ranged from 0% to 14% in a given subregion with higher percentages in both urban and rural areas (Supplemental Figure 4).
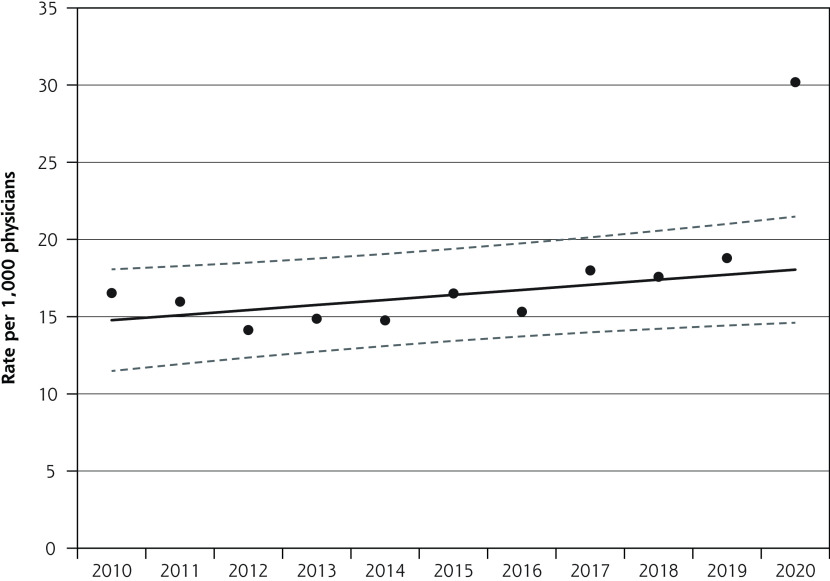
In each year between 2010 and 2019, an average of 1.6% of family physicians who were working from January to March stopped work between April and September; in contrast, 3.0% stopped work in 2020 (Supplemental Figure 5). Figure 1 depicts the observed and fitted data. The fitted regression line estimated 1.48% of family physicians stopped working in 2010. The absolute increase in the percentage of family physicians stopping work was 0.03% per year from 2010 to 2019 (P = 0.042) but 1.2% between 2019 to 2020 (P <0.001).
Figure 1.
Number of family physicians per 1,000 who were actively practicing from January to March in a given year but who had 0 primary care visits between April and September of that year, 2010-2020. Observed numbers and fitted regression line with 95% CIs.
DISCUSSION
We found that roughly 3% of the 12,000 practicing family physicians in Ontario, Canada stopped working during the first 6 months of the pandemic—approximately twice as many as in previous years. Our estimate of the proportion stopping work was consistent using 2 different analytic methods. Physicians stopping work were more likely to be aged 75 years or over, practice fee-for-service, have a panel size under 500, and work less than other physicians in the previous year—factors that are likely correlated and consistent with physicians heading into retirement.
Although the absolute number of physicians stopping work was small, the impact on patients and communities is likely substantial. Just over one-half of the physicians who stopped working were practicing in a patient enrollment model and responsible for care of formally rostered patients. Using the mean panel size of 788, we can estimate these physicians cared for approximately 170,000 patients who may now be unattached. The number of unattached is likely even higher as some physicians who practiced outside a patient enrollment model and who stopped working were also providing comprehensive primary care. These health human resource challenges are occurring in a province where approximately 10% of the population does not have a family physician.13,14
Although we cannot directly attribute causation, we hypothesize that some family physicians accelerated their retirement plans because of the pandemic. Possible reasons include the concerns about health, increased practice costs due to recommended infection prevention and control measures, drop in revenue due to the reduction in total visits,15,16 and burnout.17,18 More research is needed to understand the long-standing impact on primary care attachment and access to care and the broader impact on population health.
Supplementary Material
Acknowledgments
Thank you to Peter Gozdyra for creating the map of percentage of physicians stopping work by subregion.
Footnotes
Conflicts of interest: authors report none.
Author contributions: T.K. and R.H.G. conceived of the study. All authors helped design the study. F.C.W., A.K., and L.L. conducted the analysis. All authors helped interpret the data. T.K. drafted the manuscript and all authors critically reviewed it. All authors read and approved the final manuscript.
Funding support: This study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health (MOH) and the Ministry of Long-Term Care (MLTC). This study also received funding from the Canadian Institutes of Health Research funding reference number SOP 162662 and also received some support from the INSPIRE Primary Health Care Research Program which is funded through the Health Systems Research Program of the Ontario Ministry of Health and Long-Term Care. Parts of this material are based on data and information compiled and provided by Ontario Ministry of Health (MOH). The analyses, conclusions, opinions, and statements expressed herein are solely those of the authors and do not reflect those of the funding or data sources; no endorsement is intended or should be inferred.
T.K. and R.H.G. are supported as Clinician Scientists by the Department of Family and Community Medicine at the University of Toronto and at St Michael’s Hospital. T.K. is the Fidani Chair of Improvement and Innovation in Family Medicine at the University of Toronto. M.E.G. is supported by the Brian Hennen Chair in Family Medicine at Queen’s University.
REFERENCES
- 1.World Health Organization . Maintaining Essential Health Services: Operational Guidance for the COVID-19 Context: Interim Guidance. World Health Organization; 2020. [Google Scholar]
- 2.Glazier RH, Green ME, Wu FC, Frymire E, Kopp A, Kiran T.. Shifts in office and virtual primary care during the early COVID-19 pandemic in Ontario, Canada. CMAJ. 2021; 193(6): E200-E210. 10.1503/cmaj.202303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barzin A, Wohl DA, Daaleman TP.. Development and implementation of a covid-19 respiratory diagnostic center. Ann Fam Med. 2020; 18(5): 464. 10.1370/afm.2558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goroll AH, Greiner AC, Schoenbaum SC.. Reform of payment for primary care—from evolution to revolution. N Engl J Med. 2021; 384(9): 788-791. 10.1056/NEJMp2031640 [DOI] [PubMed] [Google Scholar]
- 5.Lemire F, Slade S.. Reflections on family practice and the pandemic first wave. Can Fam Physician. 2020; 66(6): 468-468. [PMC free article] [PubMed] [Google Scholar]
- 6.Etz R, Larry A Green Center Advisory Group . Quick covid-19 primary care weekly survey, weeks 1-4. Published Apr 9, 2020. Accessed Aug 23, 2021. https://deepblue.lib.umich.edu/handle/2027.42/154717
- 7.Abelson Reed. Doctors are calling it quits under stress of the pandemic. The New York Times. November 15, 2020. https://www.nytimes.com/2020/11/15/health/Covid-doctors-nurses-quitting.html
- 8.Etz R, Group LAGCA . Quick covid-19 primary care weekly survey, series 21. Published Oct 2, 2020. Accessed Aug 23, 2021. https://deepblue.lib.umich.edu/handle/2027.42/162822
- 9.Neprash HT, Chernew ME.. Physician practice interruptions in the treatment of medicare patients during the covid-19 pandemic. JAMA. 2021; 326(13): 1325-1328. 10.1001/jama.2021.16324 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hutchison B, Glazier R.. Ontario’s primary care reforms have transformed the local care landscape, but a plan is needed for ongoing improvement. Health Aff (Millwood). 2013; 32(4): 695-703. 10.1377/hlthaff.2012.1087 [DOI] [PubMed] [Google Scholar]
- 11.Kiran T, Kopp A, Moineddin R, Glazier RH.. Longitudinal evaluation of physician payment reform and team-based care for chronic disease management and prevention. CMAJ. 2015; 187(17): E494-E502. 10.1503/cmaj.150579 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kiran T, Kopp A, RH G.. Those left behind from voluntary medical home reforms in Ontario, Canada. Ann Fam Med. 2016; 14(6): 517-525. 10.1370/afm.2000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Glazier R, Gozdyra P, Kim M, Bai L, Kopp A, Schultz S.. Geographic variation in primary care need, service use and providers in ontario, 2015/16. IC/ES. Published Aug 2018. https://www.ices.on.ca/Publications/Atlases-and-Reports/2018/Geographic-Variation-in-Primary-Care [Google Scholar]
- 14.Statistics Canada . Primary health care providers, 2019. Published Oct 22, 2020. Accessed Aug 23, 2021. https://www150.statcan.gc.ca/n1/pub/82-625-x/2020001/article/00004-eng.htm
- 15.Gold SB, Green LA, Westfall JM.. How payment reform could enable primary care to respond to covid-19. Milbank Memorial Fund. Published Apr 20, 2020. Updated Apr 30, 2020. https://www.milbank.org/publications/how-payment-reform-could-enable-primary-care-to-respond-to-covid-19/ [Google Scholar]
- 16.Phillips RL Jr, McCauley LA, Koller CF.. Implementing high-quality primary care: a report from the National Academies of Sciences, Engineering, and Medicine. JAMA. 2021; 325(24): 2437-2438. 10.1001/jama.2021.7430 [DOI] [PubMed] [Google Scholar]
- 17.Etz R, Larry A Green Center Advisory Group . Quick covid-19 primary care survey, series 29. Published Jul 27, 2021. Accessed Aug 23, 2021. https://deepblue.lib.umich.edu/handle/2027.42/168418
- 18.Zuber MC. Nearly 75 per cent of Ontario doctors experienced burnout during pandemic, survey finds. The Canadian Press. August 18, 2021. https://toronto.ctvnews.ca/nearly-75-per-cent-of-ontario-doctors-experienced-burnout-during-pandemic-survey-finds-1.5552218
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.