Abstract
PURPOSE
Practice facilitation is an evidence-informed implementation strategy to support quality improvement (QI) and aid practices in aligning with best evidence. Few studies, particularly of this size and scope, identify strategies that contribute to facilitator effectiveness.
METHODS
We conducted a sequential mixed methods study, analyzing data from EvidenceNOW, a large-scale QI initiative. Seven regional cooperatives employed 162 facilitators to work with 1,630 small or medium-sized primary care practices. Main analyses were based on facilitators who worked with at least 4 practices. Facilitators were defined as more effective if at least 75% of their practices improved on at least 1 outcome measure—aspirin use, blood pressure control, smoking cessation counseling (ABS), or practice change capacity, measured using Change Process Capability Questionnaire—from baseline to follow-up. Facilitators were defined as less effective if less than 50% of their practices improved on these outcomes. Using an immersion crystallization and comparative approach, we analyzed observational and interview data to identify strategies associated with more effective facilitators.
RESULTS
Practices working with more effective facilitators had a 3.6% greater change in the mean percentage of patients meeting the composite ABS measure compared with practices working with less effective facilitators (P <.001). More effective facilitators cultivated motivation by tailoring QI work and addressing resistance, guided practices to think critically, and provided accountability to support change, using these strategies in combination. They were able to describe their work in detail. In contrast, less effective facilitators seldom used these strategies and described their work in general terms. Facilitator background, experience, and work on documentation did not differentiate between more and less effective facilitators.
CONCLUSIONS
Facilitation strategies that differentiate more and less effective facilitators have implications for enhancing facilitator development and training, and can assist all facilitators to more effectively support practice changes.
Key words: practice facilitation, quality improvement, large-scale initiative, capacity building, implementation facilitation, organizational change, organizational innovation
INTRODUCTION
Practice facilitators are trained individuals who build medical practices’ capacity to make meaningful operational changes aligned with current evidence.1,2 Facilitators provide education, motivation, accountability, and guidance on organizational processes.3 Facilitators increase practices’ awareness about needs for change, prioritize Plan-Do-Study-Act (PDSA) cycles and quality improvement (QI) activities, promote relationship building and communication, train staff to use data for monitoring and evaluation,1,3,4 and/or provide technical advice.5
Facilitators have been particularly used in primary care settings4–7 to help practices improve process and outcome measures6 and adopt evidence-based guidelines.7 Research suggests that facilitation can be effective8–10 and that use of facilitators is growing,5 as policies and guidelines affecting primary care rapidly change.11
Studies suggest that facilitators use varied interpersonal communication and health information technology skills to help practices make incremental process improvements,9,12–15 and facilitators benefit from training and other supportive structures, including peer support.16 Research examining the strategies facilitators use that contribute to organizational change and clinical outcome improvement,17–19 which would benefit the change management field more broadly, is limited.20,21 This study begins to fill this important research gap5,20 by addressing a key research question: what characteristics and strategies distinguish between more and less effective facilitators?
METHODS
Setting
Advancing Heart Health, funded by the Agency for Healthcare Research and Quality (AHRQ), was a large-scale practice change initiative launched in mid-2015 that focused on improving practice capacity and cardiovascular preventive care clinical outcomes. Seven regional grantees, called cooperatives, participated; the cooperatives spanned 12 states and brought together a range of partners to implement this initiative, launching work with practices in 2016.22 Facilitation was a core implementation strategy delivered to all practices, across all cooperatives, in conjunction with other implementation support (ie, expert consultation, learning collaboratives, data feedback, and benchmarking)23 that varied by cooperative.24–26 Cooperative intervention details are described elsewhere.24–27
Cooperatives worked with a range of facilitator organizations, including Area Health Education Centers, Regional Extension Centers, and practice-based research networks, to develop a workforce to engage more than 200 practices in each region and 1,630 practices overall. To assess the initiative’s impact, we conducted the EvidenceNOW national evaluation called Evaluating System Change to Advance Learning and Take Evidence to Scale (ESCALATES).28 The Oregon Health & Science University Institutional Review Board approved this study.
Sample
The sample for this study included cooperative leaders, facilitators, and practices. All cooperatives and their practices that submitted quantitative data both before and after the initiative were included. A subset of facilitators participated in this study. To be included, facilitators had to have participated in qualitative data collection (observation and/or interview); had to have worked with at least 4 practices, resulting in a stable caseload that allowed assessment of effectiveness; had to be external facilitators, meaning they were part of the cooperative workforce and not employees of the primary care organization; and had to be either more or less effective as facilitators, according to criteria described in detail below. Figure 1 and Table 1 show the numbers of practices and facilitators included in this sample.
Figure 1.
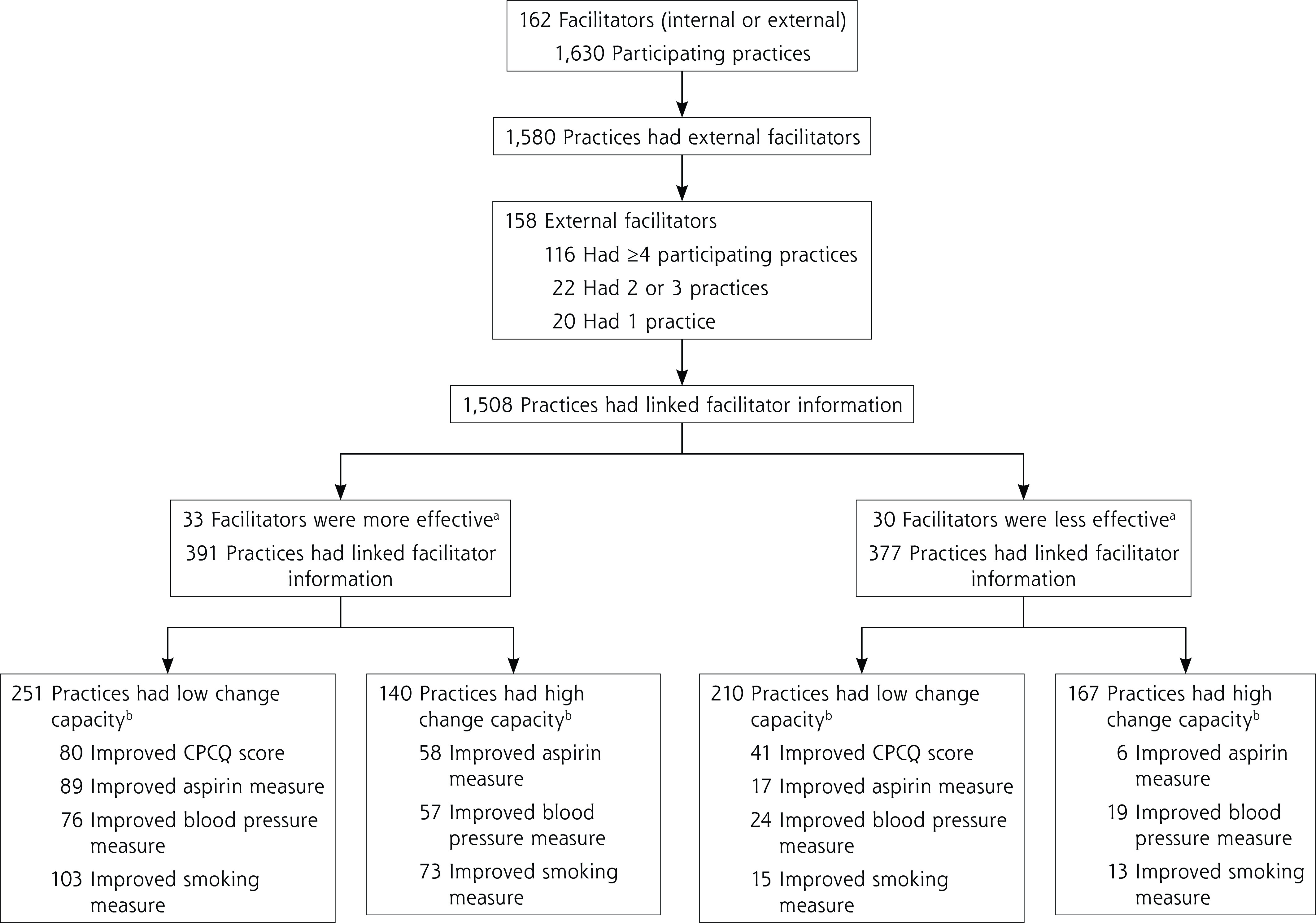
Numbers of facilitators and practices.
ABS = aspirin use for high-risk patients; CPCQ = Change Process Capability Questionnaire.
Notes: Numbers of practices that improved on the CPCQ score and on the aspirin, blood pressure, and smoking measures are not mutually exclusive and add up to more than the total number of practices with high change capacity or low change capacity.
a More effective: ≥75% of facilitator’s practices had improved CPCQ scores and/or ABS performance; less effective: <50% of facilitator’s practices had improved CPCQ scores and/or ABS performance. A total of 53 facilitators with 740 practices were neither more nor less effective, and were excluded from effectiveness analyses.
b Assessed from baseline CPCQ score, dichotomized at the median value as high (score ≥11) or low (score <11).
Table 1.
Practice and Facilitator Numbers by Cooperative
| Group and Measure | Coop 1 | Coop 2 | Coop 3 | Coop 4 | Coop 5 | Coop 6 | Coop 7 | Total |
|---|---|---|---|---|---|---|---|---|
| Practices | ||||||||
| Number participating | 245 | 225 | 274 | 205 | 216 | 211 | 254 | 1,630 |
| Number having external facilitator | 245 | 225 | 274 | 205 | 166 | 211 | 254 | 1,580 |
| Facilitators | ||||||||
| Number | 31 | 17 | 17 | 16 | 15 | 39 | 23 | 158 |
| Number having ≥4 practices | 18 | 16 | 17 | 15 | 12 | 19 | 19 | 116 |
| Effectiveness of facilitators having ≥4 practicesa | ||||||||
| Number more effective | 12 | 5 | 6 | 2 | 0 | 6 | 2 | 33 |
| Number less effective | 2 | 3 | 2 | 2 | 11 | 3 | 7 | 30 |
ABS = aspirin use for high-risk patients, blood pressure control, smoking cessation counseling; Coop = cooperative; CPCQ = Change Process Capability Questionnaire.
More effective: ≥75% of facilitator’s practices had improved CPCQ scores and/or ABS performance; less effective: <50% of facilitator’s practices had improved CPCQ scores and/or ABS performance. A total of 53 facilitators who were neither more effective nor less effective were excluded from effectiveness analyses.
Study Design
This study used a sequential mixed methods design (Table 2). Qualitative data collection and analysis preceded quantitative analyses that identified more and less effective facilitators. Once both data sources were independently assessed, the team integrated these data and analyzed the complete data set further.
Table 2.
Trial Data Collection and Analysis Timeline
| Phase and Components | Specific Activities |
|---|---|
| Preintervention phase: Sep 2015-Mar 2017 | |
| Quantitative data collection | Baseline surveys (practice survey, practice member survey) |
| Intervention phase: Dec 2015-Nov 2017 | |
| Quantitative data collection: Dec 2015-Nov 2017a | Quarterly ABS reports |
| Qualitative data collection: Jul 2016-Apr 2017 | Interviews with 80 study participants:
|
| Postintervention phase: Nov 2016-Apr 2018 | |
| Quantitative data collection: Nov 2016-Dec 2017 | Postintervention surveys (practice survey, practice member survey) |
| Qualitative data collection: Sep 2017-Aug 2018 | Interviews with 74 facilitators:
|
| Analysis phase: Mar 2020-Dec 2021 | |
| Quantitative data analyses | Analyses of descriptive data from 162 facilitators (158 external, 4 internal) |
| Qualitative data analyses | Analyses based on interviews with 36 of 87 facilitators interviewed:
|
ABS = aspirin use for high-risk patients, blood pressure control, smoking cessation counseling.
The active interventions ranged in duration from 3 to 18 months.
Data Collection
Clinical Quality Measures
We collected 3 outcomes defined by the Centers for Medicare and Medicaid Services as measures of the quality of clinical care: aspirin use in high-risk individuals, blood pressure control, and smoking cessation counseling (ABS). Possible values ranged from 0% (no eligible patients met the measure) to 100% (all eligible patients met the measure). These measures, detailed elsewhere, were collected quarterly from all practices (Supplemental Table 1) from baseline until the end of intervention.28 ABS outcomes, abstracted from electronic health records, were collected by cooperatives at the practice level and shared with the ESCALATES team.
Practice Capacity for Change
Practice capacity for change was measured at baseline and at the end of the intervention by the Change Process Capability Questionnaire (CPCQ), which assessed the extent to which practices engaged in specific QI strategies during the previous year.29 Possible scores range from −28 (lowest capacity) to 28 (highest capacity).30
Observation and Interviews
A multidisciplinary team having expertise in qualitative methods, primary care, and practice improvement conducted the observations and interviews. During the active intervention, we observed facilitators, selected by cooperative leadership, working with their practices for at least 7 QI meetings, paying particular attention to the strategies facilitators used. Researchers (S.M.S., A.B., J.D.H., D.J.C.) took notes during these meetings, and later developed these into detailed field notes that described the observed activities. After observation, facilitators were interviewed using a semistructured guide (Supplemental Appendix 1) to explore professional background, training, education, skills, and facilitation approach.
After the intervention, we conducted semistructured interviews by telephone with facilitators who worked with at least 1 practice that made a positive change in ABS outcome measures. Facilitators worked with practices that varied on size, ownership, and geography. These interviews were similar to those conducted during the active intervention, but focused on the specific changes practices made to improve metrics and the facilitator’s role in fostering improvements (Supplemental Appendix 2). We also conducted interviews with 39 individuals responsible for hiring and supporting facilitators to learn about facilitator training and monitoring.
Defining Facilitator Effectiveness
Using quantitative data, we purposively selected a group of more effective and a group of less effective facilitators. Facilitators were defined as more effective if at least 75% of their practices improved on an ABS and/or CPCQ outcome. Facilitators were defined as less effective if less than 50% of their practices improved on these measures. Data from facilitators who achieved improvements in 50% or more but less than 75% of their practices were not considered further (Figure 1).
A practice was defined as improved if (1) it had a below-median baseline change capacity (assessed from CPCQ score) and, with the intervention, achieved an increase of at least 6 points in CPCQ score or an increase of at least 5 percentage points in 1 or more ABS measures, or (2) it had an above-median baseline change capacity and, with the intervention, achieved an improvement of at least 5 percentage points in 1 or more ABS measures. We selected this definition for several reasons. First, previous research has shown that a 6-point positive change in CPCQ score represents a moderate-level improvement, as determined by the Cohen d effect size.31 Second, an improvement of at least 5 percentage points in an ABS measure was clinically meaningful and achievable. In addition, our prior work showed that EvidenceNOW interventions were associated with average ABS improvements ranging from +3.39 percentage points (aspirin use) to +7.73 percentage points (smoking cessation counseling).32 Third, in practices with below-median baseline CPCQ scores, facilitators might prioritize foundational QI work (which this questionnaire assessed) over ABS change, whereas practices already having higher CPCQ scores may be deemed better positioned to immediately begin work implementing QI strategies to improve ABS outcomes.
Data Management
Interviews, which generally lasted an hour, were audio recorded, professionally transcribed, and reviewed for accuracy. The quantitative analyst provided the qualitative team with identification numbers for more and less effective facilitators, without identifying the group to which facilitators belonged. All qualitative data were deidentified and organized into Atlas.ti 7 (Scientific Software Development GmbH) for management and analysis.
Analysis
Qualitative data analysis preceded our selection of more and less effective facilitators. During this early analysis stage, 2 to 3 cooperative facilitators joined group analysis sessions. Together, we read field notes and interview transcripts to develop an understanding of facilitators’ work using an immersion crystallization approach.33 We developed an initial codebook that identified a range of strategies facilitators used. In teams of 2, we used this codebook to analyze incoming data, comparing each team’s findings, discussing differences, and refining the codebook, as needed.
The quantitative analyst (D.E-H.) identified 33 more effective and 30 less effective facilitators (28% and 26% of the sample, respectively). We had qualitative data for 23 more effective and 13 less effective facilitators.
Analysts (J.D.H., A.B., D.J.C.), who were blinded to the facilitators’ group assignment, reanalyzed the field notes and interviews from these 36 facilitators. For each facilitator, we identified the strategies we observed them using, as well as their professional characteristics. We unblinded the facilitator’s effectiveness group, clustered findings of more and less effective facilitators, and conducted within- and across-group comparisons. We performed confirming-disconfirming analyses34 to further refine our results, considering features of their cooperative infrastructure that might have shaped facilitators’ work.
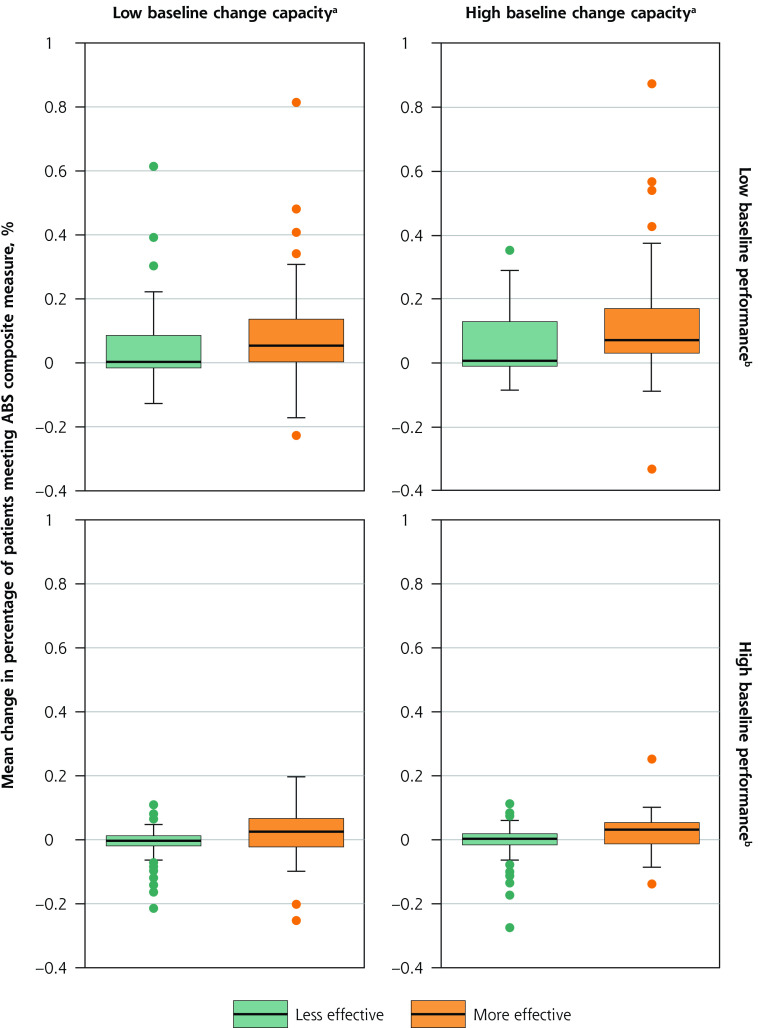
We thought it was possible that facilitators working with practices with lower baseline ABS measures and CPCQ scores may have been placed in the more effective group because their practices had more room to improve and might do so faster. As a result, we created a composite ABS score, calculated as the mean ABS change from baseline to follow-up, and created plots showing the distribution of mean ABS change between more and less effective facilitators stratified by baseline CPCQ score and baseline ABS measure. We then conducted a simple linear regression analysis modeling the outcome change as a function of facilitator effectiveness (more vs less), baseline change capacity (CPCQ score above vs below median), and composite baseline performance (ABS measure above vs below median). Quantitative analyses were performed using R version 4.1.1 (the R Foundation).
RESULTS
Sample Characteristics
Table 2 enumerates the practice and facilitator cohorts for this study by cooperative. Cooperatives operated in different contexts, had varied geographies and prior experience with large-scale change initiatives and facilitation, and offered different levels of support to facilitators with some cooperatives standardizing facilitator skillsets. There was good cooperative representation in both facilitator groups, however, with all but 1 cooperative contributing at least 1 facilitator to each group.
Facilitator Effectiveness and Practice Improvement
Practices working with more effective facilitators had higher changes in the composite ABS performance outcome (Figure 2 and Table 3), regardless of whether their baseline change capacity was low or high (based on a CPCQ score of less than the median of 11 points vs 11 points or greater) and regardless of whether their baseline performance was low vs high (based on an ABS composite measure of less the median of 65% of patients meeting any of the 3 measures vs 65% or greater). In our regression model, when adjusting for baseline ABS measure and CPCQ score, practices working with a more effective facilitator had a 3.6% greater change in mean composite ABS performance (P <.001).
Figure 2.
Distribution of mean change in ABS composite measure between more and less effective facilitators, stratified by practice baseline change capacity and baseline performance.
ABS = aspirin use, blood pressure control, smoking cessation counseling. CPCQ = Change Process Capability Questionnaire.
Notes: Plots show absolute changes in percentages, so the magnitude of the difference is small, but across the baseline characteristics, practices with more effective facilitators tended to have higher changes in the ABS composite measure.
a Assessed from baseline CPCQ score, dichotomized at the median value as high (score ≥11) or low (score <11).
b Assessed from percentage of patients meeting composite ABS outcome at baseline, dichotomized at the median value as high (≥65%) or low (<65%).
c More effective: ≥75% of facilitator’s practices had improved CPCQ scores and/or ABS performance; less effective: <50% of facilitator’s practices had improved CPCQ scores and/or ABS performance.
Table 3.
Outcomes by Facilitator Effectiveness and Practice Baseline Change Capacity
| Outcome | More Effective Facilitator | Less Effective Facilitator | All | ||
|---|---|---|---|---|---|
| High Capacity | Low Capacity | High Capacity | Low Capacity | ||
| Change in percentage of patients meeting ABS measurea | |||||
| Aspirin, mean (SD) % | 10 (22) | 6 (16) | 0 (10) | 1 (10) | 4 (16) |
| Blood pressure, mean (SD) % | 4 (14) | 2 (14) | 2 (9) | 2 (13) | 2 (13) |
| Smoking, mean (SD) % | 11 (17) | 9 (22) | 1 (14) | 0 (11) | 6 (18) |
| Change in CPCQ score, mean (SD) pointsb | −2.7 (9.8) | 17.8 (13.9) | −3.1 (9.5) | 11.7 (10.6) | 5.9 (14.5) |
ABS = aspirin use for high-risk patients, blood pressure control, smoking cessation counseling; CMS = Centers for Medicare and Medicaid Services; CPCQ = Change Process Capability Questionnaire.
Notes: See Table 1 footnotes for definitions of more and less effective facilitators. See Figure 1 footnotes for definitions of practice baseline change capacity.
Absolute difference between percentage of patients meeting metric at follow-up and at baseline. Theoretical range: −100% (practice went from all eligible patients meeting CMS performance measure at baseline to none at follow-up) to 100% (practice went from no eligible patients meeting CMS performance measure at baseline to all at follow-up).
Difference between score at follow-up and at baseline. Theoretical range following above logic: −56 (practice went from highest to lowest change capacity) to 56 (practice went from lowest to highest change capacity).
Facilitator Differentiators
Professional Background
Facilitator professional background and experience did not distinguish between more and less effective facilitators. Both groups had facilitators with prior relevant work experience, including clinical backgrounds or familiarity working in clinical settings, technical expertise, and previous facilitation experience.
Strategies Used
In contrast, several strategies for supporting practice change differentiated between more and less effective facilitators across the cooperatives. More effective facilitators helped cultivate motivation by tailoring QI work, addressing practice resistance, and guiding practices through the change process, regardless of practice focus (Table 4). These strategies were not mutually exclusive; in fact, more effective facilitators used these strategies in combination. Less effective facilitators rarely used these strategies or, if they did, used a single strategy exclusively.
Table 4.
Summary of Strategies Used and Articulation of Strategies by More and Less Effective Facilitators
| Facilitator Effectiveness | Cultivating Motivation, Tailoring, and Addressing Resistance | Guiding Practices Though the Change Process | Articulating Strategies to Help Practices |
|---|---|---|---|
| More effective | Aligned EvidenceNOW work with other payer initiatives or practice goals. Used formal assessment tools or casual conversations to assess practice readiness to change and QI capacity. Addressed resistance directly and worked with practice to overcome barriers (eg, suggesting smaller tests of change, working with EHR vendors, helping reallocate tasks among team members). |
Identified pain points through conversation with the practice and discussed next steps. Shared ideas from other practices (cross-pollination) such as on workflows and patient education and helped tailor to the local context to make changes appropriate across diverse practice settings. Provided project management support (eg, agenda setting, note-taking, summarizing action items, assigning tasks to team members, providing reminders). |
Yes—were able to speak in detail about the work they did in specific practices, how this work was tailored, and which changes likely led to improvements. |
| Less effective | Showed less evidence of motivating and tailoring. Cited practice resistance as preventing work from being done. Described not wanting to push the practice too hard. |
Held didactic meetings with education alone. Did the work for the practice. Presented options for the change process, but did not push the practice to identify their next steps. Some did not have structured meetings; emphasis was on just being present in the practice. |
No—when asked about work done in specific practices, answers were limited to the facilitator’s overall approach and to description of presentations and materials used. |
EHR = electronic health record; QI = quality improvement.
More effective facilitators tailored QI work to practices’ experience, needs, and preferences, and directly addressed resistance when encountered. To learn about motivators, they asked open-ended questions about practice goals and challenges, or used motivational interviewing to identify and stimulate enthusiasm for practice change.
Facilitators who were more effective also approached practices individually based on their experience and interests, and fostered change by being flexible about what the practice worked on. We observed and heard more effective facilitators describe how EvidenceNOW aligned with other payer initiatives or unique practice goals:
Keeping an open mind is important. And not going in with your own agenda, but going in and helping them find what works for them… because you have to understand people dynamics while you’re doing this, and you’re helping them find what’s meaningful to them. – Facilitator Interview, Cooperative 6
Less effective facilitators described rigidity in their approach and were less adept at surfacing and leveraging motivation to customize possible practice changes.
Despite tailoring QI efforts, some practices remained resistant to change. When this situation arose, more effective facilitators addressed resistance directly. This trait was a notable differentiator, widely displayed among more effective facilitators and absent among less effective facilitators. The former identified specific barriers to the change (ie, limited staff capacity, the need for better data) and focused on minimizing them. We saw and heard less effective facilitators describe their role in more passive terms such as providing education without guiding practices to make a plan:
From my end, it was a lot of just education on what does the blood pressure metric mean, and then they came up with the plan of remeasuring anyone that was close. – Facilitator Interview, Cooperative 2
Less effective facilitators described not wanting to push the practice too hard or be in the practice’s way, citing resistance as an insurmountable roadblock.
We observed more effective facilitators guide practices through the change process by helping them think critically to identify solutions at pain points, and by providing structure and accountability to implement those solutions. They leveraged ideas from other practices (a process called cross-pollination) to stimulate thinking and provide options. By doing this, practices not only improved a specific clinical quality measure, but also built their capacity to address future changes. This strategy sometimes led to new workflows or expanded practice member roles:
You can’t walk in and take over and do things for practices, because they’ve got to be able to go forward long term. What if I’m not here forever? They’ve got to be able to understand what it is that they need to do, and it’s our role, in my opinion, to help guide them to get them there so that they can function on their own. – Facilitator Interview, Cooperative 1
We noted that less effective facilitators educated without helping practice members apply lessons and did work for the practice.
More effective facilitators also provided project management and organizational support to practices by creating an agenda and providing reminders. These facilitators discussed setting goals and tracking progress. During meetings, we observed them allocating concrete tasks to specified individuals (even for members not present) with target dates for completion, and providing accountability by routinely asking for updates:
They know next time they see me, I’m gonna ask about it. They often would beat me to the question. “This is what we did. What we’ve been working on. You’re gonna be so proud.” – Facilitator Interview, Cooperative 7
We saw less effective facilitators use meetings to present clinical guidelines or check-in. Some less effective facilitators did not hold meetings with individuals or groups, but instead, emphasized being available for assistance, limiting the structure or accountability provided.
A subset of both more and less effective facilitators focused on building electronic health record efficiencies and making documentation changes. This strategy improved specific measures (primarily aspirin use and smoking cessation counseling) by moving data to the appropriate electronic health record location. Although this strategy did not require clinical or process changes, it often led to an immediate improvement in outcome. Cleaning data and documentation changes were not distinguishing features between more and less effective facilitators; however, more effective facilitators who worked on documentation changes did so in conjunction with other strategies such as cultivating motivation and addressing resistance.
Articulation of Strategies
More effective facilitators could specifically describe how they helped their practice make improvements (Table 4). This description included describing their role, how they approached practices (and how they approached practices differently), and specific changes practices made that likely led to observed improvements. Less effective facilitators struggled to provide details about their work and the changes practices made. They spent more time describing materials without discussing how the practice used those resources or translated this information into action, even when probed.
DISCUSSION
Our findings show that practices that worked with a more effective facilitator had significantly larger improvements in cardiovascular disease preventive care than practices that worked with a less effective facilitator. Although backgrounds did not distinguish more and less effective facilitators, their strategies did. These strategies included cultivating motivation by tailoring work, directly addressing resistance, guiding practices through the change process by problem solving, and providing structure and accountability to help practices implement changes. This study’s findings echo some of the existing research describing facilitator work,1,3,5 and connect the strategies that we observed facilitators using to effectiveness.7,20
All but 1 cooperative contributed at least 2 facilitators to the more effective group. This finding suggests that the strategies we identified were generalizable and transcended differences among the EvidenceNOW cooperatives. There are, however, a few cooperative variations worth exploring. For example, Goldberg et al35 reported that an overly ambitious timeline negatively affected cooperative 5. This finding likely explains why this cooperative did not contribute facilitators to the more effective group: they did not have sufficient time to engage practices using the identified strategies. Similarly, our prior work shows facilitators benefit from training and ongoing support.16 Cooperatives that intentionally and consistently assess and address facilitators’ learning needs may produce facilitators who are more able to make practice changes, thereby minimizing the effect of facilitator background and experience.
Our results also have implications for facilitator trainings. The technical skills associated with facilitation (conducting record audits and PDSA cycles)1,5,9 were not sufficient for practice change. Facilitator training would benefit from a greater focus on complex skills, such as fostering motivation, addressing resistance, and creating dynamics in which practices can engage in self-assessment and think critically to address weaknesses. These skills, which are arguably more difficult to teach, may require ongoing support and hands-on training through activities such as shadowing and peer learning.16 One way of knowing whether facilitators are absorbing these skills is their ability to thoroughly describe their work. Although it was a somewhat unexpected finding that more effective facilitators were also better at describing their work, this ability may be important for those recruiting, hiring, and supporting facilitators, as well as for practices deciding whether to work with a particular facilitator.
There are several limitations to this study. First, although the criteria to be considered a more effective facilitator had multiple pathways, it is possible that some facilitators were effective at making changes outside the scope of the ABS and CPCQ measures. Second, individual practice characteristics such as size, ownership, disruptions, and internal motivation for change can influence the strategies a facilitator uses36 and a facilitator’s ability to make practice changes.37–39 Although practice characteristics vary in all studies, some facilitators reported having more challenging (eg, larger or less engaged) practices and believed that despite their best efforts, these issues were insurmountable. This perception may be true, but our study was not designed to examine it. We thus might have excluded some effective facilitators from our sample.
In conclusion, practices that worked with more effective facilitators made significantly larger improvements in cardiovascular disease preventive care than practices that worked with less effective facilitators. Facilitator experience and background and use of documentation changes did not distinguish more and less effective facilitators, but a range of strategies, including cultivating motivation, addressing resistance, helping practices to think critically, and providing accountability, did. Practices considering working with a facilitator and organizations that employ facilitators should seek out these qualities.
Supplementary Material
Acknowledgments
We are grateful to all of the EvidenceNOW Cooperatives and facilitators who made this work possible. In addition, the entire ESCALATES study team, especially William L. Miller, MD, MA, and Leif I. Solberg, MD, willingly contributed their thoughtful feedback.
Footnotes
Conflicts of interest: authors report none.
Funding support: This work was supported by the Agency for Healthcare Research and Quality (grant No. R01HS023940-01).
Disclaimer: The views expressed are solely those of the authors and do not necessarily represent official views of the authors’ affiliated institutions or funder.
Previous presentation: Facilitation Characteristics That Lead to Improvement in Practice Capacity and Clinical Quality. Presented at the 48th Annual North American Primary Care Research Group meeting; November 2020; virtual.
Trial registration: Registered as Observational Study at www.clinicaltrials.gov (NCT02560428).
References
- 1.Taylor EF, Machta RM, Meyers DS, Genevro J, Peikes DN.. Enhancing the primary care team to provide redesigned care: the roles of practice facilitators and care managers. Ann Fam Med. 2013; 11(1): 80-83. 10.1370/afm.1462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Agency for Healthcare Research and Quality . AHRQ Practice Facilitation Training Modules. Last reviewed Apr 2022. Accessed Aug 2, 2022. https://www.ahrq.gov/ncepcr/tools/transform-qi/deliver-facilitation/modules/index.html
- 3.Dogherty EJ, Harrison MB, Graham ID.. Facilitation as a role and process in achieving evidence-based practice in nursing: a focused review of concept and meaning. Worldviews Evid Based Nurs. 2010; 7(2): 76-89. 10.1111/j.1741-6787.2010.00186.x [DOI] [PubMed] [Google Scholar]
- 4.Knox L, Brach C.. The Practice Facilitation Handbook. Training Modules for New Facilitators and Their Trainers. Agency for Healthcare Research and Quality Publication 13-0046-EF. Last reviewed May 2018. Accessed Mar 7, 2022. https://www.ahrq.gov/ncepcr/tools/pf-handbook/index.html
- 5.Nagykaldi Z, Mold JW, Aspy CB.. Practice facilitators: a review of the literature. Fam Med. 2005; 37(8): 581-588. [PubMed] [Google Scholar]
- 6.Baskerville NB, Liddy C, Hogg W.. Systematic review and meta-analysis of practice facilitation within primary care settings. Ann Fam Med. 2012; 10(1): 63-74. 10.1370/afm.1312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang A, Pollack T, Kadziel LA, et al. . Impact of practice facilitation in primary care on chronic disease care processes and outcomes: a systematic review. J Gen Intern Med. 2018; 33(11): 1968-1977. 10.1007/s11606-018-4581-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nutting PA, Crabtree BF, Stewart EE, et al. . Effect of facilitation on practice outcomes in the National Demonstration Project model of the patient-centered medical home. Ann Fam Med. 2010; 8(Suppl 1): S33-S44, S92. 10.1370/afm.1119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ritchie MJ, Parker LE, Edlund CN, Kirchner JE.. Using implementation facilitation to foster clinical practice quality and adherence to evidence in challenged settings: a qualitative study. BMC Health Serv Res. 2017; 17(1): 294. 10.1186/s12913-017-2217-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Grumbach K, Bainbridge E, Bodenheimer T.. Facilitating improvement in primary care: the promise of practice coaching. Issue Brief (Commonw Fund). 2012; 15(1): 1-14. [PubMed] [Google Scholar]
- 11.Chen LM, Epstein AM, Orav EJ, Filice CE, Samson LW, Joynt Maddox KE.. Association of practice-level social and medical risk with performance in the Medicare Physician Value-Based Payment Modifier Program. JAMA. 2017; 318(5): 453-461. 10.1001/jama.2017.9643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harvey G, Loftus-Hills A, Rycroft-Malone J, et al. . Getting evidence into practice: the role and function of facilitation. J Adv Nurs. 2002; 37(6): 577-588. 10.1046/j.1365-2648.2002.02126.x [DOI] [PubMed] [Google Scholar]
- 13.Harvey G, Lynch E.. Enabling continuous quality improvement in practice: the role and contribution of facilitation. Front Public Health. 2017; 5: 27. 10.3389/fpubh.2017.00027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Webne-Behrman H. The Practice of Facilitation: Managing Group Process and Solving Problems. Greenwood Publishing Group; 1998. [Google Scholar]
- 15.Coleman KF, Krakauer C, Anderson M, et al. . Improving quality improvement capacity and clinical performance in small primary care practices. Ann Fam Med. 2021; 19(6): 499-506. 10.1370/afm.2733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sweeney SM, Hemler JR, Baron AN, et al. . Dedicated workforce required to support large-scale practice improvement. J Am Board Fam Med. 2020; 33(2): 230-239. 10.3122/jabfm.2020.02.190261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Walunas TL, Ye J, Bannon J, et al. . Does coaching matter? Examining the impact of specific practice facilitation strategies on implementation of quality improvement interventions in the Healthy Hearts in the Heartland study. Implement Sci. 2021; 16(1): 33. 10.1186/s13012-021-01100-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cranley LA, Cummings GG, Profetto-McGrath J, Toth F, Estabrooks CA.. Facilitation roles and characteristics associated with research use by healthcare professionals: a scoping review. BMJ Open. 2017; 7(8): e014384. 10.1136/bmjopen-2016-014384 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nutting PA, Crabtree BF, Miller WL, Stewart EE, Stange KC, Jaén CR.. Journey to the patient-centered medical home: a qualitative analysis of the experiences of practices in the National Demonstration Project. Ann Fam Med. 2010; 8(Suppl 1): S45-S56, S92. 10.1370/afm.1075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Moussa L, Garcia-Cardenas V, Benrimoj SI.. Change facilitation strategies used in the implementation of innovations in healthcare practice: a systematic review. J Change Manag. 2019; 19(4): 283-301. 10.1080/14697017.2019.1602552 [DOI] [Google Scholar]
- 21.Møller L, Goduscheit RC.. Facilitation as a management discipline to support organisational development processes. Danish Journal of Management & Business. 2015; 79(2): 7-19. [Google Scholar]
- 22.Agency for Healthcare Research and Quality . EvidenceNOW Cooperatives. Last reviewed Apr 2022. Accessed Aug 2, 2022. https://www.ahrq.gov/evidencenow/projects/heart-health/about/cooperatives/index.html
- 23.Taylor EF, Genevro J, Peikes D, Geonnotti K, Wang W, Meyers D.. Building Quality Improvement Capacity in Primary Care: Supports and Resources. Agency for Healthcare Research and Quality: 2013. [Google Scholar]
- 24.Perry CK, Damschroder LJ, Hemler JR, Woodson TT, Ono SS, Cohen DJ.. Specifying and comparing implementation strategies across seven large implementation interventions: a practical application of theory. Implement Sci. 2019; 14(1): 32. 10.1186/s13012-019-0876-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Parchman ML, Fagnan LJ, Dorr DA, et al. . Study protocol for “Healthy Hearts Northwest”: a 2 × 2 randomized factorial trial to build quality improvement capacity in primary care. Implement Sci. 2016; 11(1): 138. 10.1186/s13012-016-0502-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Weiner BJ, Pignone MP, DuBard CA, et al. . Advancing heart health in North Carolina primary care: the Heart Health NOW study protocol. Implement Sci. 2015; 10(1): 160. 10.1186/s13012-015-0348-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ono SS, Crabtree BF, Hemler JR, et al. . Taking innovation to scale in primary care practices: the functions of health care extension. Health Aff (Millwood). 2018; 37(2): 222-230. 10.1377/hlthaff.2017.1100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cohen DJ, Balasubramanian BA, Gordon L, et al. . A national evaluation of a dissemination and implementation initiative to enhance primary care practice capacity and improve cardiovascular disease care: the ESCALATES study protocol. Implement Sci. 2016; 11(1): 86. 10.1186/s13012-016-0449-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Solberg LI, Asche SE, Margolis KL, Whitebird RR.. Measuring an organization’s ability to manage change: the change process capability questionnaire and its use for improving depression care. Am J Med Qual. 2008; 23(3): 193-200. 10.1177/1062860608314942 [DOI] [PubMed] [Google Scholar]
- 30.Agency for Healthcare Research and Quality . EvidenceNOW: Change Process Capability Questionnaire Scoring. Last reviewed May 2017. Accessed Aug 2, 2022. https://www.ahrq.gov/evidencenow/projects/heart-health/research-results/research/cpcq-scoring.html
- 31.Balasubramanian BA, Marino M, Cohen DJ, et al. . Use of quality improvement strategies among small to medium-size US primary care practices. Ann Fam Med. 2018; 16(Suppl 1): S35-S43. 10.1370/afm.2172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Marino M, Solberg L, Springer R, et al. . Cardiovascular disease preventive services among smaller primary care practices. Am J Prev Med. 2022; 62(5): e285-e295. 10.1016/j.amepre.2021.10.011 [DOI] [PubMed] [Google Scholar]
- 33.Borkan J. Immersion/crystallization In: Crabtree BF, Miller WL, eds. Doing Qualitative Research. Sage Publications, Inc; 1999. [Google Scholar]
- 34.Patton MQ. Qualitative Research & Evaluation Methods: Integrating Theory and Practice. Sage Publications; 2014. [Google Scholar]
- 35.Goldberg DG, Soylu TG, Grady VM, Kitsantas P, Grady JD, Nichols LM.. Indicators of workplace burnout among physicians, advanced practice clinicians, and staff in small to medium-sized primary care practices. J Am Board Fam Med. 2020; 33(3): 378-385. 10.3122/jabfm.2020.03.190260 [DOI] [PubMed] [Google Scholar]
- 36.Nguyen AM, Cuthel A, Padgett DK, et al. . How practice facilitation strategies differ by practice context. J Gen Intern Med. 2020; 35(3): 824-831. 10.1007/s11606-019-05350-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Russell G, Lane R, Parker S, et al. ; Preventive Evidence into Practice (PEP) Partnership Group . Preventive Evidence into Practice: what factors matter in a facilitation intervention to prevent vascular disease in family practice? BMC Fam Pract. 2019; 20(1): 113. 10.1186/s12875-019-0995-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Parchman ML, Anderson ML, Coleman K, et al. . Assessing quality improvement capacity in primary care practices. BMC Fam Pract. 2019;20(1):103. 10.1186/s12875-019-1000-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Liddy C, Rowan M, Valiquette-Tessier S-C, Drosinis P, Crowe L, Hogg W.. Improved delivery of cardiovascular care (IDOCC): findings from narrative reports by practice facilitators. Prev Med Rep. 2016; 5: 214-219. 10.1016/j.pmedr.2016.12.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.