Restrictive measures adopted worldwide against COVID-19 (e.g., wearing masks, frequent hand washing, and social distancing) produced not only a decrease in SARS-CoV-2 diffusion but also a drastic reduction in respiratory diseases caused by other pathogens, as reported by many authors [1, 2]. The spread of respiratory viruses, particularly respiratory syncytial virus (RSV), has been completely changed during the winter of 2020–2021 [3, 4], but an unusual resurgence of RSV infection has been recently reported in different countries [3–7]. A drastic reduction in bronchiolitis hospitalizations also occurred during the winter of 2020–2021, with RSV being the main etiologic agent of bronchiolitis [3, 6].
We described the unusual RSV bronchiolitis outbreak in young infants in autumn 2021 and the difference in RSV bronchiolitis epidemiology during the COVID-19 pandemic season (March 2020–September 2021) compared to previous seasons.
We retrospectively analyzed all infants aged < 6 months with acute bronchiolitis admitted to the Pediatric Emergency Department (PED) of our tertiary teaching children’s hospital from October to November 2021 compared to those admitted during the same period from 2017 to 2020. Data about demographics, triage priority codes, oxygen supplementation, and outcomes were collected. The diagnosis of RSV infection was made by RNA detection on a nasal swab. The study was approved by our local ethics committee. Informed consent to participate in the study was obtained from participants’ parents or legal guardians. Statistical analysis was performed using R software (version 4.0.2). The results were reported as medians and interquartile ranges (IQRs) or frequencies and percentages, as appropriate. All tests were two-sided; P value < 0.05 was considered significant.
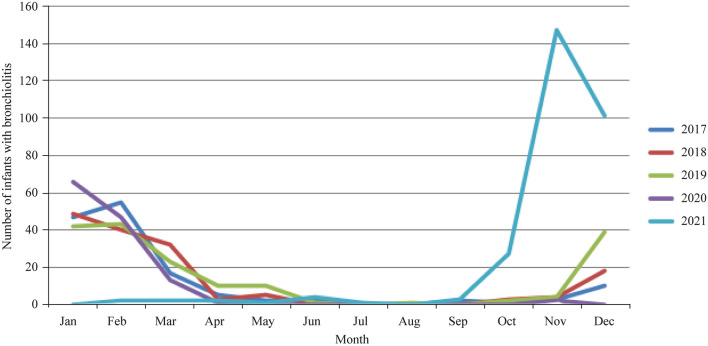
Comparing October–November 2021 to October–November 2017–2020, we observed an impressive outbreak of acute bronchiolitis in the first six months of life, especially due to RSV (159 vs. 1; P < 0.001) but also a lower hospital admission rate (P = 0.001) and shorter length of hospitalization (P = 0.016). No significant difference was observed for the need of oxygen supplementation (P = 0.120) or admission rate to Pediatric Intensive Care Unit (PICU) (P = 0.999), suggesting similar severity (Table 1). To address the great number of patients coming to the PED, a temporary short observation unit with six beds was opened in November 2021, and 9.2% of patients were moved to other hospitals due to a lack of beds. We did not observe any outbreaks of RSV bronchiolitis during spring and summer 2021 (Fig. 1) or a higher percentage of prematurity and PICU admissions, as otherwise reported by other authors [6].
Table 1.
Epidemiological and clinical features of infants with acute bronchiolitis
| Variables | October–November 2021 | October–November 2017–2020 | P value |
|---|---|---|---|
| Total admissions for acute bronchiolitis, n (%) | 174 (100.0) | 18 (100.0) | |
| RSV positive, n (%) | 159 (91.3) | 1 (5.5) | < 0.001 |
| Males, n (%) | 107 (61.5) | 9 (5.2) | 0.448 |
| Prematurity, n (%) | 21 (12.1) | 5 (2.9) | 0.075 |
| Median age, d, n (IQR) | 58 (34.0–95.5) | 69.5 (32.7–116.2) | 0.212 |
| Triage priority code, n (%) | |||
| Red (emergency) | 30 (17.2) | 5 (27.8) | 0.332 |
| Yellow (high priority) | 128 (73.6) | 13 (72.2) | 0.999 |
| Green (low priority) | 16 (9.2) | 0 (0.0) | 0.999 |
| White (very low priority) | 0 (0.0) | 0 (0.0) | 0.999 |
| Need for respiratory support, n (%) | 111 (63.8) | 15 (83.3) | 0.120 |
| Low-flow nasal cannulae, n (%) | 109 (62.6) | 7 (4.0) | |
| High-flow nasal cannulae, n (%) | 55 (31.6) | 10 (5.7) | |
| NIV/cPAP, n (%) | 7 (4.0) | 1 (0.6) | |
| Mechanical ventilation, n (%) | 3 (1.7) | 0 (0.0) | |
| Admission to hospital, n (%) | 107 (61.5) | 18 (100.0) | 0.001 |
| Admission to PICU, n (%) | 12 (6.8) | 1 (5.5) | 0.999 |
| Median length of hospitalization, d, n (IQR) | 5 (1.0–9.0) | 8 (6.0–11.5) | 0.016 |
| Moved to other Hospitals, n (%) | 16 (9.2) | 0 (0.0) |
RSV respiratory syncytial virus, IQR interquartile range, NIV noninvasive ventilation, cPAP continuous positive air pressure, PICU pediatric intensive care unit
Fig. 1.
Seasonal trends of respiratory syncytial virus bronchiolitis between 2017 and 2022
Our analysis confirmed previous observations of different new epidemiological trends of RSV bronchiolitis worldwide during the COVID-19 pandemic [1, 5, 8]. In New Zealand, the incidence rate during the bronchiolitis peak in 2021 was higher than the average of peaks in 2015–2019 but without more severe cases [8]. Hatter et al. hypothesized that in countries with a higher COVID-19 burden in the Northern Hemisphere, the RSV epidemic might have been more severe during the winter season of 2021 than in the prepandemic years due to the immunity debt secondary to long periods of low exposure to RSV [8]. This prediction has come true in our area in autumn 2021, when school, kindergarten, and work social activities fully reprised. On the other hand, we have not observed any summer peak, as reported in Japan and Spain [5, 6]. We fully agree with Bermúdez Barrezueta et al. about the necessity of potentiating the epidemiological surveillance systems that control RSV circulation for a better management of health resources, including the better timing of palivizumab prophylaxis [6].
In conclusion, we observed an unusual early RSV outbreak in autumn 2021, suggesting a possible change in the epidemiology of the virus during the COVID-19 pandemic. Despite the noticeable increase, no more severe cases were recorded compared to 2017–2020.
Author contributions
IR and CE contributed to conceptualization, formal analysis, and writing –original draft. MF was involved in data curation and writing–original draft. BC and GS contributed to writing–original draft, and writing–review and editing.
Funding
No funding was received for this paper.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Conflict of interest
No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Ethical approval
The study was approved by our local Ethical Committee (approval number: 0049894, May 3, 2022). Informed consent to participate in the study has been obtained from participants’ parents or legal guardians.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Agca H, Akalin H, Saglik I, Hacimustafaoglu M, Celebi S, Ener B. Changing epidemiology of influenza and other respiratory viruses in the first year of COVID-19 pandemic. J Infect Public Health. 2021;14:1186–1190. doi: 10.1016/j.jiph.2021.08.004. [DOI] [PubMed] [Google Scholar]
- 2.Di Mattia G, Nenna R, Mancino E, Rizzo V, Pierangeli A, Villani A, et al. During the COVID-19 pandemic where has respiratory syncytial virus gone? Pediatr Pulmonol. 2021;56:3106–3109. doi: 10.1002/ppul.25582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Van Brusselen D, De Troeyer K, ter Haar E, Vander Auwera A, Poschet K, Van Nuijs S, et al. Bronchiolitis in COVID-19 times: a nearly absent disease? Eur J Pediatr. 2021;180:1969–1973. doi: 10.1007/s00431-021-03968-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vittucci AC, Piccioni L, Coltella L, Ciarlitto C, Antilici L, Bozzola E, et al. The disappearance of respiratory viruses in children during the COVID-19 pandemic. Int J Environ Res Public Health. 2021;18:9550. doi: 10.3390/ijerph18189550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ujiie M, Tsuzuki S, Nakamoto T, Iwamoto N. Resurgence of respiratory syncytial virus infections during COVID-19 pandemic, Tokyo. Japan Emerg Infect Dis. 2021;27:2969–2970. doi: 10.3201/eid2711.211565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bermúdez Barrezueta L, Matías Del Pozo V, López-Casillas P, Brezmes Raposo M, Gutiérrez Zamorano M, Pino Vázquez MA. Variation in the seasonality of the respiratory syncytial virus during the COVID-19 pandemic. Infection. 2022;22:1–5. doi: 10.1007/s15010-022-01794-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cason C, Zamagni G, Cozzi G, Tonegutto D, Ronfani L, Oretti C, et al. Spread of respiratory pathogens during the COVID-19 pandemic among children in the northeast of Italy. Front Microbiol. 2022;24:804700. doi: 10.3389/fmicb.2022.804700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hatter L, Eathorne A, Hills T, Bruce P, Beasley R. Respiratory syncytial virus: paying the immunity debt with interest. Lancet Child Adolesc Health. 2021;5:e44–e45. doi: 10.1016/S2352-4642(21)00333-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.