Abstract
A 1-day-old late preterm, small-for-gestational-age female presented with a caudal appendage—a rare finding—and abnormalities in all 4 limbs most consistent with amniotic band syndrome. The caudal appendage was lateral to midline, measured 3 cm × 0.5 cm, and had no bony abnormalities or spinal cord tethering. Limb abnormalities consisted of brachydactyly, oligodactyly, and syndactyly. Renal and head ultrasounds and an echocardiogram were normal. Chromosomal microarray showed deletion of EPHA3, which is not associated with a known phenotype. The multidisciplinary approach of managing this infant with the rare finding of a caudal appendage and limb abnormalities is presented.
Keywords: caudal appendage, amniotic band syndrome, brachydactyly, spinal dysraphism, human tail
Introduction
Amniotic band syndrome (ABS) describes a spectrum of presentations from a single finding to a constellation of findings, and the pathogenesis is not clearly understood. Most infants with ABS have limb deformities—nearly 80% in a 1982-2012 review. 1 The prevalence of ABS is 1 in 1200 to 15 000 live births 2 and affects both sexes nearly equally. There are 3 main categories of ABS: isolated limb deformities, craniofacial deformities, and limb–body wall deformities. 3 Neonates with isolated limb deformities can have a defect in a single extremity or defects in multiple extremities; such deformities can appear as an amputation of a distal digit or extremity or as webbing of finger and/or toes. Craniofacial deformities can manifest as cleft lip and/or palate, hypertelorism, or microphthalmia. The most severe category of ABS is characterized by limb–body wall deformities. Infants with such deformities can have skull defects that allow the brain to protrude or defects in the abdominal wall that release the abdominal contents. Because the infant described here had limb abnormalities and a caudal appendage, this case does not fall strictly into the ABS categories described above. Having a caudal appendage with ABS has not been clearly recorded in the literature.
There are 2 theories describing the etiology of ABS—the intrinsic and extrinsic models. In the extrinsic model, the amniotic sac ruptures, causing constriction rings that disrupt fetal development. Rarely, these bands can be visualized with prenatal ultrasound. 2 The intrinsic model seeks to explain cases of ABS that are not consistent with the extrinsic model. In these cases, the amniotic sac is not disrupted, but changes in blood flow during development result in tissue loss.
This report describes an infant with a caudal appendage and limb abnormalities whose presentation was most consistent with amniotic band syndrome.
Case Presentation
A female infant was born at 35 5/7 weeks gestation to a 26-year-old gravida 2, para 2 mother. The infant was small for gestational age, born at 1.984 kg (ninth percentile on the Fenton growth chart for preterm girls).
The pregnancy was complicated by maternal tobacco use. The mother was positive for group B streptococcus, and she received clindamycin for intrapartum prophylaxis due to penicillin allergy. She was also late to acquire prenatal care, having been seen initially at 20 weeks gestation. The remainder of the mother’s prenatal testing was unremarkable, and there was no other pertinent maternal history. There were no abnormalities noted on prenatal imaging.
The mother presented to the outside (referring) hospital with spontaneous preterm labor. The delivery was complicated by vacuum assistance. The infant was vigorous at delivery and did not require resuscitation.
The referring hospital contacted the tertiary care facility after multiple congenital anomalies were noted on physical examination. The infant was transferred to the level 4 neonatal intensive care unit (NICU).
Upon arrival at the NICU, the infant was noted to have multiple congenital anomalies. Both hands exhibited brachydactyly and hypoplasia of the nail beds of the fifth digits the left hand lacked the distal phalanx of the second digit. Both feet exhibited oligodactyly of the fifth digits, with right 2-3 syndactyly and left 2-3-4 syndactyly. Bilaterally, the medial malleolus at the tibial insertion was abnormal, with circumferential narrowing of the lower leg. In the lumbosacral region, there was a caudal appendage, 3 cm × 0.5 cm, lateral and 2.5 cm to the right of midline with no apparent bony involvement (Figure 1).
Figure 1.

Caudal appendage lateral and 2.5 cm to the right of midline, measuring 3 cm × 0.5 cm, with no apparent bony involvement. Image taken during newborn hospital stay.
The infant had multiple imaging studies while in the NICU. Head ultrasound, renal ultrasound, and echocardiogram were normal. A skeletal survey confirmed the limb abnormalities noted at the physical exam. A spine ultrasound showed that the conus medullaris terminated at L2-3 (lower limit of normal) and had a thickened filum with decreased oscillation. Magnetic resonance imaging of the spine revealed a small syrinx at the distal thoracic cord. There was an elongated soft tissue appendage (caudal appendage) emanating from the level of the right iliac crest and extending inferiorly along the right gluteal region. It did not appear to involve or extend from the ileum or iliac crest. There was evidence of a central fibrous structure, but likely not fascial nor cartilaginous.
Pediatrics subspecialties including genetics, orthopedics, neurosurgery, general surgery, and plastic surgery were consulted during the NICU hospitalization. Genetics recommended obtaining a chromosomal microarray and outpatient follow-up. The surgical subspecialists recommended no acute interventions and outpatient follow-up. The remainder of the patient’s 6-day hospitalization was unremarkable. She had jaundice but did not require phototherapy. She fed well and was near birth weight at the time of discharge.
The infant had multiple follow-up appointments with pediatric subspecialists over the first year of life. At 6 months of age, she was seen by a pediatric plastic surgeon, at which time the caudal appendage measured 6.5 cm × 1.5 cm (Figure 2). Additionally, there was a diffuse soft tissue mass deep to the appendage measuring 7.5 cm in diameter. Excision of the caudal appendage was scheduled for 1 year of age. Repair of the syndactyly on the left and right feet was not recommended at the time because the risks outweighed any benefit. She was noted to have plagiocephaly and torticollis, which were being treated with physical therapy.
Figure 2.
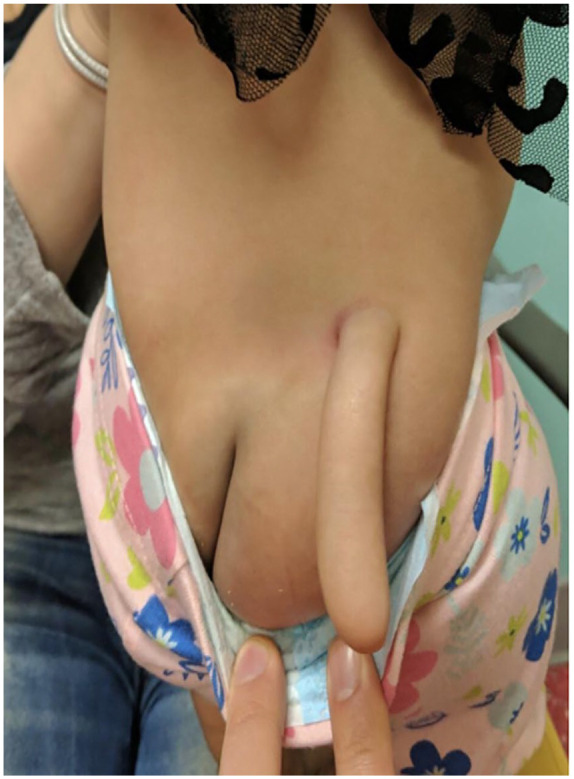
Caudal appendage at 6 months of age measuring 6.5 cm × 1.5 cm. Image taken at 6-month follow-up.
At 6 months of age, she was also seen by an orthopedic hand surgeon. Repeat X-rays of both hands were obtained and showed no change in the abnormalities previously seen on imaging. Upon evaluation, the decision was made to offer surgical webspace deepening with syndactyly release and possible full-thickness skin grafting involving the left ring and small fingers—to be coordinated with the caudal appendage excision.
Chromosomal microarray results were non-diagnostic but showed a small deletion that included EPHA3, which has no associated phenotype. There was no consanguinity. At the 6-month follow-up, the geneticist concluded that findings were consistent with amniotic band syndrome.
At 1 year of age, plastic surgery removed the caudal appendage and underlying soft tissue mass. Skin was taken from the appendage for grafting during the hand surgery repair. Gross and histologic examination of the excised caudal appendage and underlying mass revealed skin and subcutaneous mature fibroadipose tissue. After the appendage and mass were excised, the orthopedic hand surgeon performed full separation of the fourth and fifth digits of the left hand, with full-thickness skin grafting; a cast was placed on the left upper extremity.
The patient was evaluated by a general pediatric orthopedic surgeon shortly after the procedures described above. Radiographic imaging at that time showed no changes in the abnormalities of her feet bilaterally. Given that the patient was not experiencing functional limitations due to the toe abnormalities, observation was recommended. Of note, she was found to have bilateral acetabular dysplasia, for which she was fitted with an abduction brace.
Postoperative follow-up with the pediatric orthopedic hand surgeon showed appropriate wound healing at the site of the syndactyly release and skin grafting, with no evidence of infection. She had full digital range of motion at that time.
Discussion
Amniotic band syndrome (ABS) is a heterogeneous collection of congenital, fetal malformations that typically affect the limbs but can also affect internal organs and craniofacial areas. 4 The incidence is estimated to be 1 in 1000 to 1 in 15 000 births, and there is no known inheritance pattern. The most common manifestations are constriction rings and limb/digit amputations, which combined comprise 80% of cases. In rare cases, spinal defects and scoliosis occur. 5
While ABS is rare, it is especially rare for ABS to occur with a caudal appendage. In the literature, there are just over 60 cases of true caudal appendages, or “human tails.” A true tail is benign and composed of vessels, adipose tissue, connective tissue, nerves, and muscle. True tails are distinguished from pseudo-tails by the lack of an associated spinal dysraphism. 6 In our case, after excision, the appendage was found to be composed of fibroadipose tissue and skin. Most cases reported in the literature are actually pseudo-tails. Pseudo-tails are thought to result from the development of abnormal tissue (bone, cartilage, and remnants of the notochord) in non-fused portions of the neural tube, leading to tethering of the spinal cord or other dysraphisms. 7
Conclusion
Here, we described a neonate with a true human tail, without bony elements or underlying spinal dysraphism, and ABS. Her ABS was treated symptomatically. She had additional limb abnormalities that were not repaired because they did not affect limb function. The caudal appendage was removed via simple excision with no complications. When facing the rare occurrence of ABS and a caudal appendage, it is critical to assemble a multi-disciplinary team because there are no guidelines for treatment. This team should include specialists in pediatric genetics, orthopedics, neurosurgery, surgery, and plastic surgery. A thorough physical exam should dictate imaging studies and any necessary procedures.
Footnotes
Authors’ Note: This case study examines the case of 1 pediatric patient. This patient was treated Arkansas Children’s Hospital, Little Rock, AR. Case study contains approximately 1460 words.
Author Contributions: CB, MB, and GW conceived and designed the paper and wrote the paper. All of the authors reviewed approve the final manuscript.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Gwenevere White  https://orcid.org/0000-0001-9801-079X
https://orcid.org/0000-0001-9801-079X
References
- 1. Lowry RB, Bedard T, Sibbald B. The prevalence of amnion rupture sequence, limb body wall defects and body wall defects in Alberta 1980-2012 with a review of risk factors and familial cases. Am J Med Genet A. 2017;173(2):299-308. [DOI] [PubMed] [Google Scholar]
- 2. Barzilay E, Harel Y, Haas J, et al. Prenatal diagnosis of amniotic band syndrome - risk factors and ultrasonic signs. J Matern Fetal Neonatal Med. 2015;28(3):281-283. [DOI] [PubMed] [Google Scholar]
- 3. Holmes LB. Amniotic band syndrome. NORD (National Organization for Rare Disorders). 2018. Accessed June 23, 2022. https://rarediseases.org/rare-diseases/amniotic-band-syndrome/ [Google Scholar]
- 4. Seeds JW, Cefalo RC, Herbert WN. Amniotic band syndrome. Am J Obstet Gynecol. 1982;144(3):243-248. [DOI] [PubMed] [Google Scholar]
- 5. Singh AP, Gorla SR. Amniotic Band Syndrome. Stat Pearls; 2022. [PubMed] [Google Scholar]
- 6. Islam MN, Adhikari SB, Alam MM, Dilshad Munmun UH. Experience with human tail and its outcome. Afr J Paediatr Surg. 2021;18(1):43-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pillai MK, Nair ST. A true human tail in a neonate: case report and literature review. Sultan Qaboos Univ Med J. 2017;17(1):e109-e111. [DOI] [PMC free article] [PubMed] [Google Scholar]


