Abstract
Magnetic resonance imaging (MRI) is a technique useful for the diagnosis of cartilage damage due to high sensitivity to identify subchondral bone abnormalities and full-thickness cartilage lesions. The lack of a study on knee cartilage changes over time in patients with osteoarthritis (OA) by MRI technique led us to investigate the accuracy of MRI in identifying knee cartilage changes over time in patients with OA in a systematic review. In the present systematic review, started from the beginning of 2020 in one of the University Hospitals in Iran, the databases of CINAHL, Ovid, Elsevier, Scopus, PubMed, Science Direct, and Web of Science were searched using the keywords MRI, OA, Cartilage Lesion, Imaging Techniques. A total of 169 articles were retrieved in the initial search, and after reviewing the titles, abstracts, and full-texts, finally, seven were enrolled in the systematic review. Review of the selected papers showed that a total of 1091 subjects were studied, of which 355 were males. The results of all the studies, except one, indicated the high accuracy of MRI to identify knee cartilage changes over time. MRI technique can show cartilage changes with high accuracy in patients with knee OA over time. We proved the potential of MRI to identify articular cartilage injuries in patients with OA and its importance to the evaluation of articular cartilage lesions along with other available techniques.
Keywords: Cartilage lesion, imaging techniques, knee cartilage, magnetic resonance imaging, osteoarthritis
Highlight key points
MRI is a high sensitive technique useful for the diagnosis of cartilage damage.
MRI is a low sensitive modality for examining small abnormalities and injuries.
MRI is a common non-invasive technique along with other invasive methods to evaluate cartilage injuries.
MRI is high capable in the early and timely identification of soft, cartilaginous, and hard tissue changes.
It opened a promising window to the timely diagnosis of joint destruction.
The use of MRI can reduce the need for invasive measures, such as surgery.
Osteoarthritis (OA) is a common degenerative disorder that affects the synovial joint [1]. The main pathological findings in OA include irregularities in local joint changes, changes in the repair process of intra-articular tissue, and involvement of large joints, as well as extensive degenerative changes with loss of joint cartilage, capsule hypertrophy, subchondral bone, and joint margins [2, 3]. Inflammation of the synovia with varying degrees of joint destruction occurs with the disease progression. OA symptoms intensify and cause disability and dysfunction by age increase. This disorder is followed by pain, swelling, joint dryness, joint deformities, and decreased range of motion [4, 5]. In knee OA, patellar displacement, changes in the instant center of rotation, abnormal weight transfer, and several other biomechanical factors cause damage to cartilage and lead to OA [6].
The thickness of cartilage at the joint surface is heterogeneous, which is attributed to the biomechanical function of the joint. The highest thickness of cartilage is observed in areas, where the load is increased. Articular cartilage disorders are caused by weight transfer in the affected joint and stimulation of nerve endings in the subchondral bone. Destruction of articular cartilage to varying degrees is one of the major disorders associated with OA [7, 8].
There are various imaging techniques, including magnetic resonance imaging (MRI), to evaluate joints, the surrounding, intra-articular tissue, cartilage, and their injuries [2]. MRI as a gold standard method is a technique useful for the diagnosis of cartilage damage and assessment of OA in knee. It has a high sensitivity to identify subchondral bone abnormalities and full-thickness cartilage lesions, and low sensitivity for examining small abnormalities and injuries [9, 10]. The most advanced MRI technique presents multiple planes of articular cartilage. In terms of signal strength, the 3 Tesla MRI has a high diagnostic sensitivity compared to the 1.5 Tesla one. It is a common non-invasive technique that, along with other invasive methods, used to evaluate and diagnose cartilage injuries; however, it currently has diagnostic limitations, calling its accuracy into question [11]. Due to advantages of MRI in the evaluation of structural changes, it allows us to visualize all the tissues involved in OA, such as cartilage, subchondral bone, meniscus, and soft tissue.
Knee cartilage changes are found in patients with knee OA over time, and the results of MRI cannot prove the utility of this technique as a diagnostic tool; hence, knee specialists do not have enough information about the accuracy and specificity of MRI.
The study of these patients was aimed to evaluate the knee cartilage changes in patients with knee OA with radiography and MRI measurement techniques. All studies were cohorts except one performed by Ding et al. (2005) [12], which was a longitudinal study, in this study, other studies are also studied, the variables studied and the duration of the study, as well as the quality of the article and the follow-up period, like other budget studies, and hence. The largest and smallest sample sizes belonged to the studies by Ding et al. [12], (n=325) and Hunter (2010) [13] (n=29 female patients). The measurement techniques were radiography and MRI (1, 1.5, and 3 Tesla, respectively) in three studies, and only MRI in four other studies (1 Tesla in two studies and 3 Tesla in the rest two ones). Only in the study by Cibere et al. (2011) [18], the radiographic results were more accurate than those of MRI, and in the rest articles, MRI could accurately identify articular cartilage changes.
The current systematic review aimed at evaluating the accuracy of MRI in identifying knee cartilage changes over time in patients with OA.
MATERIALS AND METHODS
The present systematic review was conducted from the beginning of 2020 in one of the University Hospitals in Iran. Concerning the study objectives, articles published in English were searched in CINAHL, Ovid, Elsevier, Scopus, PubMed, ScienceDirect, and Web of Science databases based on the keywords selected from MeSH terms, including MRI, OA, Cartilage Lesion, and Imaging Techniques. Articles published from 2000 to the year of the study were searched. The keywords were extracted based on the study objectives by the researchers, and the search for articles was performed by a librarian not included in the research team.
To find all the eligible articles, the resources of the retrieved papers were also evaluated manually. Inclusion criteria were as follows: Articles used keywords in the title or presented them in the keywords section of the abstract, articles available with full-texts, published in English, and performed on knee joint using human patients with OA with and without a control group. It should be noted that to review the articles with inclusion criteria, studies that were similar in terms of homogeneity were included in the study, and it was the epidemiologist who helped us with that. To do this, only articles were included in the study that had the necessary criteria and quality by two researchers who were in charge of searching articles based on the checklist, they had prepared. The exclusion criteria were as follows: Summary of articles presented in conferences, letters to the editor, and papers published in other than the English language.
If the author(s) reported that they could identify articular cartilage lesions using MRI or it is a reliable technique in the examination of cartilage lesions, the study results were considered positive. If the author(s) reported that the MRI has not adequate validity and reliability to evaluate articular cartilage lesions or fails to detect such lesions, the study results were considered negative.
RESULTS
A total of 169 articles were retrieved in the initial search (160 from databases and nine through manual search). In the next step, 29 papers were deleted due to duplication. In the review of titles and abstracts, 110 irrelevant papers were excluded, and 30 remained. The remaining articles were thoroughly reviewed, and after removing the irrelevant ones (n=23), seven papers were finally enrolled in the present systematic review. The PRISMA flowchart of the study selection process is shown in Figure 1.
Figure 1.
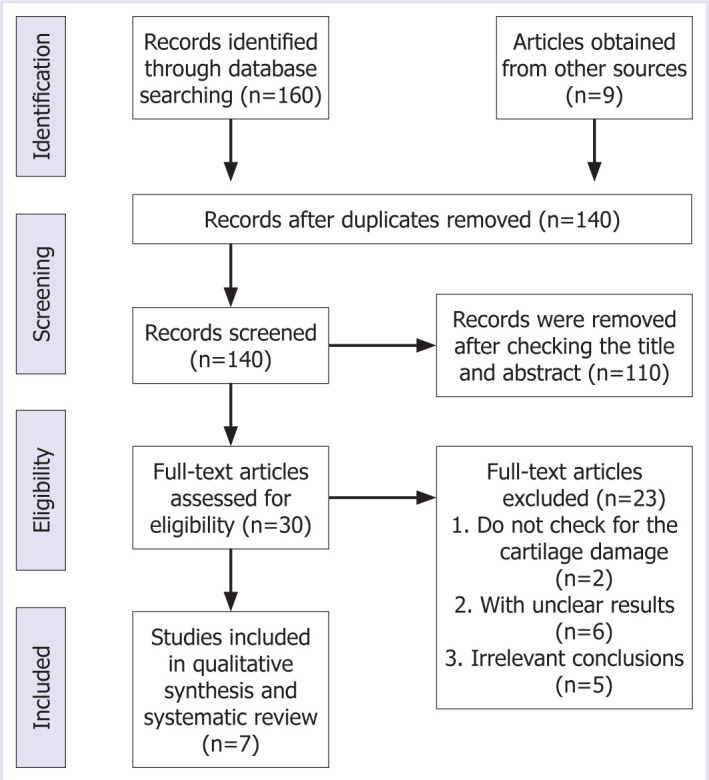
Prisma flowchart of the study selection process.
The review of the articles indicated that a total of 1091 patients were studied, of which 355 were male (patients’ gender was not determined in one study); all the studies aimed at evaluating knee cartilage changes in patients with knee OA. All studies were cohorts except one performed by Ding et al. (2005) [12], which was a longitudinal study. In this study, other studies are also studied, the variables studied and the duration of the study, as well as the quality of the article and the follow-up period, like other budget studies, and hence. The largest and smallest sample sizes belonged to the studies by Ding et al., (n=325) and Hunter (2010) [13] (n=29 female patients). The measurement techniques were radiography and MRI (1, 1.5, and 3 Tesla, respectively) in three studies, and only MRI in four other studies (1 Tesla in two studies and 3 Tesla in the rest two ones). Only in the study by Cibere et al. (2011) [18], the radiographic results were more accurate than those of MRI, and in the rest articles, MRI could accurately identify articular cartilage changes.
DISCUSSION
The current systematic review aimed at evaluating the accuracy of MRI in assessing articular cartilage changes over time in patients with OA, and after the search, seven papers were finally evaluated. In studies by Boegard et al. [14], Ding et al. [12], Davies-Tuck et al. [15], and Wirth et al. [16], MRI could identify cartilage changes in patients with OA during 2 years. They reported that knee cartilage changes were extensive within the studied period, and the progression of OA was closely correlated with this change. In the study by Ding et al., in addition to indicating common cartilage injuries, the results showed an association between an increase or decrease in joint damage and the percentage of change in cartilage volume.
Hunter et al. [17] examined the rate of cartilage changes in patients with knee OA during 1 year using radiography and MRI techniques and stated that the annual rate of changes was low in the medial and central femoral regions. Furthermore, in a follow-up study performed 1 year later by the same authors [13], extensive changes were observed in the thickness of articular cartilage over time.
Cibere et al. [18], in a study on patients with OA and knee pain, evaluated the rate of OA progression during 3 years using radiography and MRI techniques. Their results showed that the disease progression rate was low during the studied period; the radiographic findings confirmed the MRI results; but in this study, results of MRI study was confirmed with a cheaper and easier imaging which is not in favor of MRI.
Radiography was the technique used formerly to identify cartilage injuries in patients with knee OA, in which its validity was questioned due to various reasons; the point that should not be overlooked [19, 20]. Therefore, the use of more modern imaging techniques, for example, MRI, with added capabilities to evaluate soft-tissue opened new windows to OA diagnosis [21]. MRI was first used to indicate the role of knee MRI in focal pathologies-for example, meniscus rupture, osteochondritis dissecans, avascular necrosis, and ligament injury. Concerning the fact that OA involves all the joint components, MRI becomes very important in its identification, because it can show the subchondral bone and soft tissue, in great detail. This feature helps a lot in discovering the link between structural components and pain, as well as finding the source of pain [8, 9]. These different and accurate features of MRI were sometimes used to assess knee cartilage changes in patients with OA but, unfortunately, due to the lack of summarizing the studies’ results or the lack of informing and applying the findings, the use of this method remained unknown for the experts. Due to the high capability of MRI in the early and timely identification of tissue (soft, cartilaginous, and hard) changes, its application to detect articular cartilage changes in patients with OA opened a promising window to the timely diagnosis of joint destruction. The use of this technique can reduce the need for invasive measures, such as surgery. However, despite several years of using MRI, its application is not common yet and needs more elaboration and informing.
Limitations
One of the limitations of the research was the lack of access to all articles in this field considering non-English papers and the lack of access to dissertations, which may contain more accurate information.
The results of the articles reviewed in the current systematic review are shown in, since different studies had different homogeneity, this study could not be converted to meta-analysis and only the results were presented in a systematic review, which is one of the limitations of this study (Table 1).
Table 1.
Characteristics and final results of the selected studies on articular cartilage changes over time
| Author/Year | Study methodology | Purpose of the study | Sample size gender | Measurement method | Conclusion |
|---|---|---|---|---|---|
| Boegård et al. | Cohort study | Evaluation of changes in cartilage, subcutaneous bone and meniscus injuries during 2 years | n=47 Male: 22 (46.8%) | 1 Tesla MRI | MRI was able to show the appearance or absence, increase or decrease of damage |
| Ding et al. | Longitudinal study | Investigating the relationship between the prevalence of knee joint cartilage injuries and cartilage loss in young men and women | n=325 Men: 135 (41.5%) | 1 Tesla MRI and Radiography | MRI has better diagnostic power than radiography. |
| Davies-Tuck et al. | Cohort study | Evaluation of the progression of cartilage damage during 2 years MRI-assisted assessment and determination of injury-related factors | n=117 Male: 49 (41.9%) | 3 Tesla MRI | This technique can be useful in early diagnosis. |
| Hunter et al. | Cohort study | Evaluation of cartilage morphology and disease progression during 1 year MRI atrial fibrillation in patients with osteoarthritis | n=150 Male: 74 (49.3%) | 3 Tesla MRI | MRI can detect changes and has good results for early detection. |
| Wirth et al. | Cohort study | Evaluation of changes in tibial femoral joint cartilage thickness by observation in a 2-year period compared to a 1-year period | n=80 Male: Unknown | 1 Tesla MRI | It was found that MRI technique can show cartilage changes correctly. |
| Hunter et al. | Cohort study | Examination of cartilage thickness in the medial and central part of the femur with MRI | n=29 Men: 0 | Radiography and 3 Tesla MRI Radiography and 1.5 Tesla | No quantitative agreement was observed with changes in the medial and central part of the joint in the short term with the help of MRI |
| Cibere et al. | Cohort study | Evaluation of joint cartilage damage and progression of osteoarthritis by MRI | n=163 Male: 75 (46%) | MRI | Radiography had more diagnostic value than MRI. |
Conclusion
By reviewing, the literature in this field, adequate, accurate, and strong evidence was obtained to prove the potential of MRI to identify articular cartilage injuries in patients with OA and its importance to the evaluation of articular cartilage lesions along with other available techniques.
Footnotes
Cite this article as: Aghdam YH, Moradi A, Großterlinden LG, Jafari MS, Heverhagen JT, Daneshvar K. Accuracy of magnetic resonance imaging in assessing knee cartilage changes over time in patients with osteoarthritis: A systematic review. North Clin Istanb 2022;9(4):414–418.
Conflict of Interest
No conflict of interest was declared by the authors.
Financial Disclosure
The authors declared that this study has received no financial support.
Authorship Contributions
Concept – YHA, AM, KD; Design – YHA, AM, LGG, JTH, KD; Supervision – AM, LGG, JTH; Fundings – KD, YHA; Materials – MSJ, YHA, KD; Data collection and/or processing – MSJ, YHA, KD; Analysis and/or interpretation – MSJ, YHA, KD; Literature review – KD, YHA; Writing – YHA, KD; Critical review – LGG, AM, JTH.
References
- 1.Bilge A, Ulusoy RG, Üstebay S, Öztürk Ö. Osteoartrit. Kafkas Tıp Bilimleri Dergisi. 2018;8:133–42. [Google Scholar]
- 2.Hart HF, Stefanik JJ, Wyndow N, Machotka Z, Crossley KM. The prevalence of radiographic and MRI-defined patellofemoral osteoarthritis and structural pathology: a systematic review and meta-analysis. Br J Sports Med. 2017;51:1195–208. doi: 10.1136/bjsports-2017-097515. [DOI] [PubMed] [Google Scholar]
- 3.McCulloch K, Litherland GJ, Rai TS. Cellular senescence in osteoarthritis pathology. Aging Cell. 2017;16:210–8. doi: 10.1111/acel.12562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hügle T, Geurts J. What drives osteoarthritis?-synovial versus subchondral bone pathology. Rheumatology (Oxford) 2017;56:1461–71. doi: 10.1093/rheumatology/kew389. [DOI] [PubMed] [Google Scholar]
- 5.Rockel JS, Kapoor M. The metabolome and osteoarthritis: possible contributions to symptoms and pathology. Metabolites. 2018;8:92. doi: 10.3390/metabo8040092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dell’Isola A, Allan R, Smith SL, Marreiros SS, Steultjens M. Identification of clinical phenotypes in knee osteoarthritis: a systematic review of the literature. BMC Musculoskelet Disord. 2016;17:425. doi: 10.1186/s12891-016-1286-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Messina OD, Vidal Wilman M, Vidal Neira LF. Nutrition, osteoarthritis and cartilage metabolism. Aging Clin Exp Res. 2019;31:807–13. doi: 10.1007/s40520-019-01191-w. [DOI] [PubMed] [Google Scholar]
- 8.MacKay JW, Low SBL, Smith TO, Toms AP, McCaskie AW, Gilbert FJ. Systematic review and meta-analysis of the reliability and discriminative validity of cartilage compositional MRI in knee osteoarthritis. Osteoarthritis Cartilage. 2018;26:1140–52. doi: 10.1016/j.joca.2017.11.018. [DOI] [PubMed] [Google Scholar]
- 9.Culvenor AG, Øiestad BE, Hart HF, Stefanik JJ, Guermazi A, Crossley KM. Prevalence of knee osteoarthritis features on magnetic resonance imaging in asymptomatic uninjured adults: a systematic review and meta-analysis. Br J Sports Med. 2019;53:1268–78. doi: 10.1136/bjsports-2018-099257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chaudhari AS, Kogan F, Pedoia V, Majumdar S, Gold GE, Hargreaves BA. Rapid knee MRI acquisition and analysis techniques for imaging osteoarthritis. J Magn Reson Imaging. 2020;52:1321–39. doi: 10.1002/jmri.26991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Atkinson HF, Birmingham TB, Moyer RF, Yacoub D, Kanko LE, Bryant DM, et al. MRI T2 and T1ρ relaxation in patients at risk for knee osteoarthritis: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2019;20:182. doi: 10.1186/s12891-019-2547-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ding C, Cicuttini F, Scott F, Boon C, Jones G. Association of prevalent and incident knee cartilage defects with loss of tibial and patellar cartilage: a longitudinal study. Arthritis Rheum. 2005;52:3918–27. doi: 10.1002/art.21474. [DOI] [PubMed] [Google Scholar]
- 13.Hunter DJ, Bowes MA, Eaton CB, Holmes AP, Mann H, Kwoh CK, et al. Can cartilage loss be detected in knee osteoarthritis (OA) patients with 3-6 months’ observation using advanced image analysis of 3T MRI? Osteoarthritis Cartilage. 2010;18:677–83. doi: 10.1016/j.joca.2010.02.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Boegård TL, Rudling O, Petersson IF, Jonsson K. Magnetic resonance imaging of the knee in chronic knee pain. A 2-year follow-up. Osteoarthritis Cartilage. 2001;9:473–80. doi: 10.1053/joca.2001.0414. [DOI] [PubMed] [Google Scholar]
- 15.Davies-Tuck ML, Wluka AE, Wang Y, Teichtahl AJ, Jones G, Ding C, et al. The natural history of cartilage defects in people with knee osteoarthritis. Osteoarthritis Cartilage. 2008;16:337–42. doi: 10.1016/j.joca.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 16.Wirth W, Benichou O, Kwoh CK, Guermazi A, Hunter D, Putz R, et al. OAI Investigators Spatial patterns of cartilage loss in the medial femoral condyle in osteoarthritic knees: data from the Osteoarthritis Initiative. Magn Reson Med. 2010;63:574–81. doi: 10.1002/mrm.22194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hunter DJ, Niu J, Zhang Y, Totterman S, Tamez J, Dabrowski C, et al. OAI Investigators Change in cartilage morphometry: a sample of the progression cohort of the Osteoarthritis Initiative. Ann Rheum Dis. 2009;68:349–56. doi: 10.1136/ard.2007.082107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cibere J, Sayre EC, Guermazi A, Nicolaou S, Kopec JA, Esdaile JM, et al. Natural history of cartilage damage and osteoarthritis progression on magnetic resonance imaging in a population-based cohort with knee pain. Osteoarthritis Cartilage. 2011;19:683–8. doi: 10.1016/j.joca.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 19.Shrestha S, Dave AJ, Losina E, Katz JN. Diagnostic accuracy of administrative data algorithms in the diagnosis of osteoarthritis: a systematic review. BMC Med Inform Decis Mak. 2016;16:82. doi: 10.1186/s12911-016-0319-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Flemming DJ, Gustas-French CN. Rapidly progressive osteoarthritis: a review of the clinical and radiologic presentation. Curr Rheumatol Rep. 2017;19:42. doi: 10.1007/s11926-017-0665-5. [DOI] [PubMed] [Google Scholar]
- 21.Boesen M, Ellegaard K, Henriksen M, Gudbergsen H, Hansen P, Bliddal H, et al. Osteoarthritis year in review 2016: imaging. Osteoarthritis Cartilage. 2017;25:216–26. doi: 10.1016/j.joca.2016.12.009. [DOI] [PubMed] [Google Scholar]


