Abstract
BACKGROUND AND AIM:
Vaccination has been appraised to be one of the most significant public health achievements in human history. However, in countries like Nigeria, vaccine hesitancy is a public health challenge that has consistently forestalled concerted efforts made by health authorities to curb the spread of communicable diseases such as COVID-19. To improve COVID-19 vaccine acceptance via targeted interventions, it is imperative to examine the public's perception. Thus, this study aims to evaluate vaccine hesitancy among university students in Southwestern Nigeria.
MATERIALS AND METHODS:
The study utilized a descriptive cross-sectional design. A self-administered questionnaire was administered to a total of 366 respondents who were recruited using the convenience sampling technique and snowball approach. Data were entered and analyzed using SPSS.
RESULTS:
The majority of the respondents were over 18 years (88%) and were between their first and third years (81%). Over a tenth of the respondents reported having at least a loved one that had tested positive for the virus, while only 88% believed the virus is real. Furthermore, only 17% of the students had a positive attitude toward the vaccine. Although 90% of the respondents were aware of the administration of COVID-19 vaccine in Nigeria, only around a quarter were willing to take the vaccine, while 5.5% had been vaccinated. The major reasons for COVID-19 vaccine hesitancy highlighted by the respondents were concerns about vaccine side effects (21.3%), lack of trust in the authorities (26.5%), vaccine efficacy (13.1%), and diverse mystical possibilities (39.1%).
CONCLUSION:
The results indicate that a significant communication gap exists between the respondents and local health authorities. To enhance the acceptance of COVID-19 vaccines, extensive and targeted health promotion campaigns are required to allay specific concerns raised by the public.
Keywords: COVID-19, Nigeria, students, vaccine hesitancy, vaccines
Introduction
It has been noted that the protocols, guidelines, and prevention measures put in place to curtail the COVID-19 pandemic have not effectively stopped the spread of the virus. This has resulted in the world enacting an alternative approach. As of February 2021, approximately 70 vaccines had been tested in clinical trials on humans, and 20 in phase III clinical trials.[1,2] Over the years, immunization has proven to be one of the most successful ways to prevent infectious diseases.[3,4] However, vaccine hesitancy remains a rising challenge for immunization and has been cited by the World Health Organization (WHO) as the top 10 major threats to global health in 2019.[3,5]
Several studies have shown that vaccine hesitancy is a common phenomenon worldwide, with variability in mentioned reasons behind vaccine acceptance and refusal, such as misinterpretation of the need for a vaccine, misbelief in the government and the health system, and concerns regarding the potency and possible side effects of the vaccine.[5,6] Unfortunately, vaccine hesitancy does not only affect the individual undecided about taking the vaccine but also the community, thereby posing a great difficulty in achieving herd immunity.[7]
Although countries worldwide are making efforts to improve vaccination coverage and reduce the transmission of the COVID-19 virus, studies have shown that vaccine hesitancy globally is still quite high majorly due to mistrust, miscommunication, and lack of knowledge and health education about vaccine safety, which in turn has given rise to declining compliance with public health-related guidelines.[3,7] Recent data from seven OECD countries has revealed that around 25% of the population in France, Germany, and the United States are likely to refuse vaccination, with a higher number of young adults. In addition, approximately 33% of Dutch and over 50% of French residents between 25 and 34 years of age have refused to get vaccinated owing to a lack of trust in institutions responsible for vaccination.[8]
Recent literature has reported that COVID-19 vaccine hesitancy in Sub-Saharan Africa is a significant public health challenge stalling the concerted efforts made so far to curb the virus.[9] It was revealed that around 20%–50% of residents in countries such as South Africa, Ghana, and Zimbabwe have outrightly rejected the vaccine citing reasons such as religious beliefs, fear of government surveillance via microchips in the vaccine, lack of information about vaccine side effects, and mistrust and uncertainty about the vaccine preventing COVID-19 contraction.[9]
Unfortunately, the vaccine uptake among adults in Nigeria is reportedly poor.[10,11] Although Nigeria received over three million doses of the Oxford-AstraZeneca COVID-19 vaccine in March 2021, the acceptance of the vaccine is still low due to concerns about vaccine safety and effectiveness, as well as misinformation, which has been especially rampant in the context of the COVID-19 pandemic.[12] A recent study revealed that only a simple majority (58.2%) of adult Nigerians, aged 18 years and over, were willing to take a COVID-19 vaccine when available.[13] Another survey in six states found that most of the respondents dismissed the possibility of getting vaccinated because they did not believe that the COVID-19 virus exists in Nigeria, which was attributed to the fact that none of their loved ones had knowingly contracted the virus. Although over 84% of the respondents knew about the existence of the vaccine, only 68.3% were ready for vaccination as religious beliefs were another strong reason for unwillingness to take the vaccine.[12]
A global systematic review recommended the need for more studies in Africa to address COVID-19 vaccine hesitancy due to the limited availability of related articles.[6] In Nigeria, very few studies have been conducted about COVID-19 vaccine hesitancy before and after the vaccines were administered, with a major focus on the general adult population. To the best of our knowledge, there is yet to be an article that examined COVID-19 hesitancy among young adults since the ongoing vaccination processes began. On this note, this research was done to understand the perception of students toward vaccine hesitancy across Southwest, Nigeria.
Materials and Methods
Study design and setting
The study utilized a descriptive cross-sectional design, and a self-administered online questionnaire was employed for obtaining information from the respondents. The target population comprised active university students in the southwestern zone of Nigeria.
Study participants and sampling
A total of 366 respondents were recruited using the convenience sampling technique and snowball approach. The inclusion criteria necessitated that the participants must be over 16 years of age and must be registered students in a southwestern university. Non-consenting and non-registered students were exempted from participating in the study.
Data collection tool and technique
The instrument utilized for this study is a semi-structured questionnaire, and the questions were categorized into four sections. The first section was designed to obtain questions on respondents' sociodemographic variables, the second assessed the perception of COVID-19, the third section assessed respondents' perception of the COVID-19 vaccine, and the fourth section was used to determine the participants' acceptance of COVID-19. To ensure the validity of the instrument, the questionnaire was drafted after extensively reviewing relevant works of literature and questions were formulated based on research objectives.
The questionnaire was developed using Google Forms, and a convenience sampling technique was used to select the respondents, that is, the form was made available through a link for the respondents on social media platforms such as WhatsApp and Telegram. It was also requested of them to share with their colleagues/networks; in all, 366 respondents completed the survey.
After completion of the survey, all participants' responses were downloaded in excel format, and the data were further imported to Statistical Package for Social Science (SPSS version 21) for analysis. The data were analyzed using descriptive statistics (such as frequency, mean, and percentage), and the association between variables was tested using statistics such as Chi-square and Fisher's exact test at P ≤ 0.05. Perception and acceptance variables were categorized based on the authors' discretion. Respondents' perception of the COVID-19 vaccine was measured on an 8-point scale, and it was categorized as ≤4 (negative perception) and scores >4 as (positive perception). Respondent's acceptance of the COVID-19 vaccine was measured on a 5-point scale, and it was categorized as <2 (poor acceptance) and >2 (good acceptance).
Ethical consideration
Ethical approval for this study was obtained from Ekiti State University Teaching Hospital (EKSUTH), with the protocol code EKSUTH/A67/2021/04/003. The purpose of the research was duly communicated to the research participants and every participant gave their consent before completing the survey.
Results
In total, 366 responses were received during the survey period. The highest proportion of respondents (88%) was within 18–24 years, 22 (6%) 25–33 years, and 19 (5.2%) less than 18 years. Of the respondents, 154 (42.1%) were females, 207 (56.6%) were males, and five (1.3%) preferred not to say. Moreover, the majority (86.1%) were Christians, 12.8% were Muslims, and the remainders were traditional worshippers (0.3%) and other religions (0.8%), respectively. The majority of respondents (82%) were Yoruba, 8.7% were Igbo, 1.6% Hausa, and 7.7% were from other ethnic groups. Furthermore, 297 (81%) were from year 1 to 3, while 25 (6.9%) were between 4th and 5th year.
Perception of COVID-19 and COVID-19 vaccine
As shown in Table 1, the majority of the respondents (88%) believed that COVID-19 is real, while around 8% were in doubt and 3.8% did not believe that COVID-19 is real. The majority of the students had never tested positive for COVID-19, while only around 2% had. In addition, 10.7% reported having family and friends who had tested positive for COVID-19. Almost half (49.5%) of the students had a neutral attitude toward the COVID-19 vaccine, while 17.2% had positive attitudes, 10.1% had negative attitudes, and around 13% could not describe their attitude toward the vaccine.
Table 1.
Perception of COVID-19 and COVID-19 vaccine
| Characteristics | Yes | No | No response |
|---|---|---|---|
| Have you tested positive for COVID-19? | 8 (2.2%) | 354 (96.7%) | 4 (1.1%) |
| Do you have family and friends that have tested positive for COVID-19? | 39 (10.7%) | 321 (87.7%) | 6 (1.6%) |
|
| |||
| Agree | Disagree | Neutral | |
|
| |||
| I do not believe the vaccine will work because COVID-19 is not real | 23 (63%) | 235 (64.2%) | 108 (29.5%) |
| I have concerns about the vaccine’s efficacy | 178 (48.6) | 39 (10.7%) | 149 (40.7%) |
| I believe the vaccine will have a negative side effect on my health | 116 (31.7%) | 82 (22.4%) | 168 (45.9%) |
| The new strains make the vaccine useless | 51 (13.9%) | 116 (31.7%) | 199 (54.4%) |
| The vaccine is a way for powerful people to control the world | 74 (20.2%) | 153 (41.8%) | 139 (38.0%) |
| COVID-19 vaccine goes against my religious belief | 21 (5.7%) | 261 (71.3%) | 84 (23.0%) |
| The vaccine invention is a way for some people to make more money | 123 (33.6%) | 99 (27.0%) | 144 (39.4%) |
The majority (64.2%) of the respondents believe in the vaccine's effectiveness, while around 29% were neutral, and less than 7% doubted the effectiveness of the vaccine because they did not believe that the vaccine is real. Furthermore, over 30% of respondents believed that the vaccine would harm their health, while 20.2% believed that the vaccine is a scheme for powerful people to control the world, and 33.6% believe that the vaccine invention is a scheme for certain persons to make more money. Overall, most participants had a negative perception of the COVID-19 vaccine, as shown in Figure 1. However, only 5.5% of respondents have been vaccinated, while a majority (37.2%) are yet to decide if they would take the vaccine. Additionally, 33% would allow their family and friends to take the vaccine, and 37.5% would welcome the vaccination team to their religious houses [see Table 3]. Furthermore, almost 90% of respondents were aware that the COVID-19 vaccine was available in the country, with a majority (42.4%) getting their information from social media platforms, as shown in Table 2.
Figure 1.
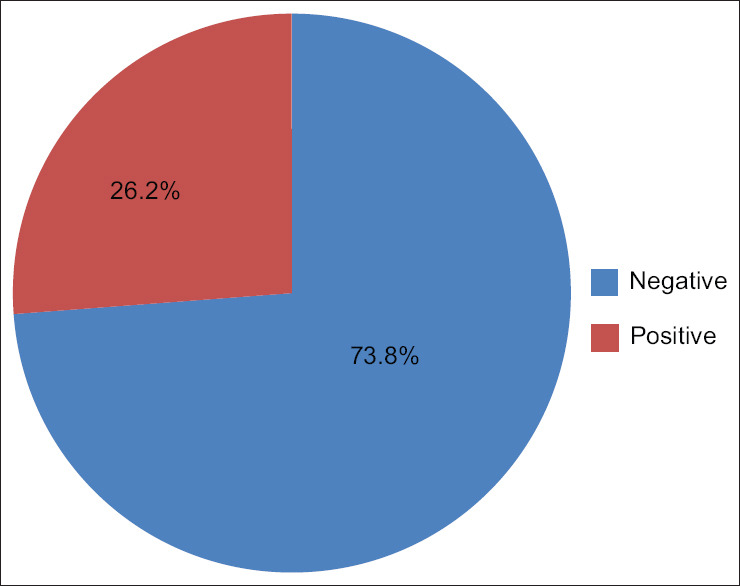
Perception of COVID-19 vaccine
Table 3.
Respondents’ attitude toward the acceptance of COVID-19 vaccine
| Characteristics | No | Yes | |
|---|---|---|---|
| Have you taken the COVID-19 vaccine? | 346 (94.5%) | 20 (5.5%) | |
|
| |||
| No | Undecided | Yes | |
|
| |||
| Now that COVID-19 is available free, would you take it? | 128 (35.0%) | 136 (37.2%) | 102 (27.8%) |
| Will you allow your family or friends to take the COVID-19 vaccine? | 101 (27.6%) | 144 (39.3%) | 121 (33.1%) |
| Will you be willing to support the campaign for the uptake of the COVID-19 vaccine? | 126 (34.4%) | 126 (34.4%) | 114 (31.2%) |
| Would you welcome the COVID-19 vaccination team to your religious house? | 107 (29.2%) | 122 (33.3%) | 137 (37.5%) |
Table 2.
Respondents’ source of awareness on COVID-19 vaccine
| Characteristics | Frequency | Percentage |
|---|---|---|
| Are you aware that the COVID-19 vaccine is now available in Nigeria? | ||
| No | 38 | 10.4 |
| Yes | 328 | 89.6 |
| Source of information on COVID-19 | ||
| NCDC/Ministry of Health website | 85 | 23.2 |
| WHO Website | 47 | 12.9 |
| Social media platforms (Facebook, Instagram, YouTube, WhatsApp. Twitter) | 155 | 42.4 |
| Official statements or press releases (news channels, newspapers, emails, SMS, etc.) | 43 | 11.7 |
| Other internet sources | 36 | 9.8 |
| Respondents’ source of information on COVID-19 Vaccine | ||
| NCDC/Ministry of Health website | 82 | 22.4 |
| WHO Website | 59 | 16.1 |
| Social media platforms (Facebook, Instagram, YouTube, WhatsApp. Twitter) | 45 | 12.3 |
| Official statements or press releases (news channels, newspapers, emails, SMS, etc.) | 143 | 39.1 |
| Other internet sources | 37 | 10.1 |
As shown in Figure 2, the majority of the respondents (26%) expressed a lack of trust in the COVID-19 vaccine as their reason for not taking the vaccine, while less than 5% did not believe that the vaccine is real.
Figure 2.
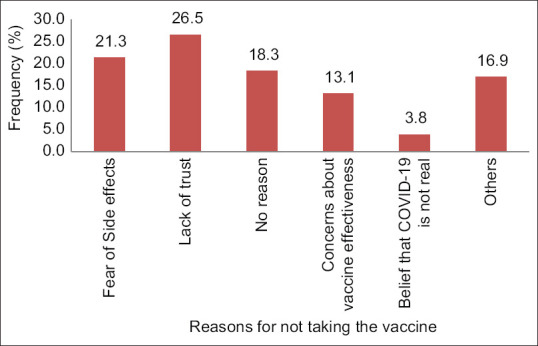
Reasons for vaccine hesitancy
Bivariate analysis of sociodemographic characteristics of respondents and COVID-19 vaccine perception (as shown in Table 4 revealed only a significant association for marital status (P < 0.05); other variables tested were insignificant (P > 0.05). Moreover, respondents' age, ethnic group, and year of study were associated with acceptance of the COVID-19 vaccine (P < 0.05), as shown in Table 5. The bivariate analysis further revealed a significant association between COVID-19 perception and COVID-19 vaccine perception (P < 0.05) [Table 6]. In addition, a significant association was found between respondents' perception of COVID-19 and acceptance of COVID-19 vaccine (P < 0.05) as well as respondents' perceived realness of COVID-19 (P < 0.05), respectively.
Table 4.
Chi-square test showing the association between sociodemographic characteristics and perception of COVID-19 vaccine
| Sociodemographic Characteristics | Perception of COVID-19 Vaccine | DF | X 2 | P | ||
|---|---|---|---|---|---|---|
|
| ||||||
| Negative (n%) | Positive (n%) | Total | ||||
| Gender | ||||||
| Female | 71 (19.4%) | 83 (22.7) | 154 | 0.441** | 0.817 | |
| Male | 101 (27.6%) | 106 (29.0%) | 207 | |||
| Prefer not to say | 2 (0.5%) | 3 (0.8) | 5 | |||
| Age | ||||||
| Less than 18 years | 12 (3.3%) | 7 (1.9%) | 19 | |||
| 18-24 years | 153 (41.8%) | 172 (47.0%) | 325 | 2 | 2.274 | 0.321 |
| 25-33 years | 9 (2.5%) | 13 (3.6%) | 22 | |||
| Marital status | ||||||
| Single | 166 (45.4%) | 191 (52.2%) | 357 | |||
| Engaged | 2 (0.5%) | 1 (0.3) | 3 | 6.862** | 0.035 | |
| Married | 4 (1.1) | 0 | 4 | |||
| Others | 2 (0.5%) | 0 | 2 | |||
| Ethnic group | ||||||
| Yoruba | 140 (38.3%) | 160 (43.7%) | 300 | |||
| Igbo | 15 (4.1%) | 17 (4.6%) | 32 | 2.517** | 0.492 | |
| Hausa | 2 (0.5%) | 4 (1.1%) | 6 | |||
| Others | 17 (4.6%) | 11 (3.0%) | 28 | |||
| Religion | ||||||
| Christianity | 149 (40.7%) | 166 (45.4%) | 315 | 3.614** | 0.285 | |
| Islam | 24 (6.6%) | 23 (6.3) | 47 | |||
| Traditional | 1 (0.3%) | 0 | 1 | |||
| Others | 0 | 3 (0.8%) | 3 | |||
| University by Location | ||||||
| Lagos | 31 (8.5%) | 33 (9.0%) | 64 | |||
| Osun | 31 (8.5%) | 25 (6.8%) | 56 | |||
| Oyo | 10 (2.7%) | 18 (4.9%) | 28 | 8.960** | 0.109 | |
| Ogun | 4 (1.1%) | 9 (2.5%) | 13 | |||
| Ondo | 30 (8.2%) | 19 (5.2%) | 49 | |||
| Ekiti | 68 (18.6%) | 88 (24.0%) | 156 | |||
| Year of study | ||||||
| Year 1 | 18 (4.9%) | 26 (7.1%) | 44 | |||
| Year 2 | 67 (18.3%) | 57 (15.6%) | 124 | |||
| Year 3 | 45 (12.3%) | 51 (13.9%) | 96 | 5.945** | 0.287 | |
| Year 4 | 35 (9.6%) | 42 (11.5%) | 77 | |||
| Year 5 | 8 (2.2%) | 16 (4.4%) | 24 | |||
| Year 6 | 1 (0.3%) | 0 | 1 | |||
**Fisher’s exact test
Table 5.
Chi-square test showing the association between sociodemographic characteristics and acceptance of COVID-19 vaccine
| Socio-Demographic Characteristics | Acceptance of COVID-19 vaccine | DF | X 2 | P | ||
|---|---|---|---|---|---|---|
|
| ||||||
| Poor n (%) | Good n (%) | Total (n) | ||||
| Gender | ||||||
| Female | 94 (25.7%) | 60 (16.4%) | 154 | |||
| Male | 127 (34.7%) | 80 (21.9%) | 207 | 2 | 1.019** | 0.635 |
| Prefer not to say | 2 (0.5%) | 3 (0.8%) | 5 | |||
| Age | ||||||
| Less than 18 years | 17 (4.6%) | 2 (10.5%) | 19 | |||
| 18-24 years | 189 (51.6%) | 136 (37.2%) | 325 | 2 | 10.432** | 0.005* |
| 25-33 years | 17 (4.6%) | 5 (1.4%) | 22 | |||
| Marital status | ||||||
| Single | 215 (58.7%) | 142 (38.8%) | 357 | |||
| Engaged | 2 (0.5%) | 1 (0.3%) | 3 | 3.595** | 0.449 | |
| Married | 4 (1.1%) | 0 | 4 | |||
| Others | 2 (0.6%) | 0 | 2 | |||
| Ethnic group | ||||||
| Yoruba | 174 (47.5%) | 126 (34.4%) | 300 | |||
| Igbo | 26 (7.1%) | 6 (1.6%) | 32 | 8.481** | 0.032* | |
| Hausa | 3 (0.8%) | 3 (0.8%) | 6 | |||
| Others | 20 (5.5%) | 8 (2.2%) | ||||
| Religion | ||||||
| Christianity | 193 (52.7) | 122 (33.3) | 315 | |||
| Islam | 28 (7.7) | 19 (5.2) | 47 | 0.780** | 1.711 | |
| Traditional | 1 (0.3) | 0 | 1 | |||
| Others | 1 (0.3) | 2 (0.5) | 3 | |||
| University by Location | ||||||
| Lagos | 31 (8.5) | 33 (9.0) | 64 | |||
| Osun | 37 (10.1) | 19 (5.2) | 56 | |||
| Oyo | 17 (4.6) | 11 (3.0) | 28 | |||
| Ogun | 7 (1.9) | 6 (1.6) | 13 | 5 | 9.497 | 0.086 |
| Ondo | 37 (10.1) | 12 (3.3) | 49 | |||
| Ekiti | 94 (25.7) | 62 (16.9) | 156 | |||
| Year of study | ||||||
| Year 1 | 29 (7.9) | 15 (4.1) | 44 | |||
| Year 2 | 79 (21.6) | 45 (12.3) | 124 | |||
| Year 3 | 63 (17.2) | 33 (9.0) | 96 | 15.049** | 0.007* | |
| Year 4 | 45 (12.3) | 32 (8.7) | 77 | |||
| Year 5 | 6 (1.6) | 18 (4.9) | 24 | |||
| Year 6 | 1 (0.3) | 0 | 1 | |||
*Significant **Fisher’s exact test
Table 6.
Chi-square test showing the association between perception of COVID-19 and perception of COVID-19 vaccine
| Perception of COVID-19 | Perception of COVID-19 Vaccine | DF | X 2 | P | ||
|---|---|---|---|---|---|---|
|
| ||||||
| Negative n (%) | Positive n (%) | Total (n) | ||||
| Do you believe COVID-19 is real? | ||||||
| Maybe | 22 (6.0) | 4 (1.1) | 26 | |||
| No | 13 (3.6) | 1 (0.3) | 14 | 34.939** | 0.000* | |
| Not sure | 4 (1.0) | 0 | 4 | |||
|
| ||||||
| Poor n (%) | Good n (%) | Total (n) | ||||
|
| ||||||
| Do you believe COVID-19 is real? | ||||||
| Maybe | 22 (6.0) | 4 (1.1) | 26 | |||
| No | 14 (3.8) | 0 | 14 | 21.311** | 0.000* | |
| Not sure | 4 (1.0) | 0 | 4 | |||
| Negative | 141 (81.0%) | 33 (19.0%) | 322 | |||
| Positive | 82 (42.7%) | 110 (57.3%) | 1 | 56.332 | 0.000* | |
| Total | 223 (60.9%) | 143 (39.1%) | ||||
*Significant **Fisher’s exact test
Discussion
The global spread and emergence of new variants of COVID-19 in different nations have necessitated the need for effective vaccines and other therapeutic solutions for the menace. However, COVID-19 vaccine hesitancy among the population threatens adequate vaccination coverage necessary for COVID-19 control. This study investigated COVID-19 vaccine hesitancy among undergraduate students.
Although more than half of the respondents believed that COVID-19 is real, a few of them were still in doubt, while about 4% do not believe that COVID-19 is real. People in doubt or disbelief may take safety precautions less seriously than those with strong awareness and who believe that the disease is real. While this study did not directly investigate the effect of doubt and unbelief of COVID-19 vaccine acceptance and hesitancy, Oyeoku et al.[14] ascertained that perceived realness is among the predictors of health behavior initiation, consistency, interruption, and discontinuation. Unsafe health practices of a group of people based on their perceptions during a pandemic potentially contribute to the continuous circulation of the disease, especially in populations where herd immunity has not been achieved. Sadly, COVID-19 is indiscriminate and varying perceptions about its existence do not stop its spread.
Our study also revealed a low COVID-19 prevalence of 2% (8) among the students, although 10.7% reported having family and friends who had tested positive. This is similar to the findings of a study among students in New York City (NYC) where 0.4% (948) of the total 234,132 students tested during the pandemic tested positive for the coronavirus.[15] The study by Varma et al.[15] also reported a higher prevalence in the general population among older people (45 years and above). Although limited studies have explored COVID-19 prevalence among students in Nigeria, it can be hypothesized that the closing of schools during the pandemic contributed to the low preponderance of COVID-19 infection among the students. The low prevalence may have also contributed to the doubt about the existence of the disease.
Three hundred and twenty-eight respondents in our study reported being aware of the COVID-19 vaccine in Nigeria. Nevertheless, more than half of the respondents were neutral about the vaccine, while 17.2% were positive and 9.8% were uneasy about the subject. Although our evaluation did not explore the associated reasons, Mheidly and Fares suggested that public perception of the COVID-19 vaccination is linked to the kind of information the public is exposed to regarding the subject.[16] Most students (39.1%) in our study got their information from social media platforms, 23.2% got information from NCDC/Ministry of Health, 12.9% from the WHO website, 11.7% from official statements/press releases, and 9.8% from other internet sources. Social media has been reported as the most frequent source of vaccine information particularly among youths, and a low visit to government websites has been associated with diminished trust in the government concerning the COVID-19 vaccine by the public.[17,18] For instance, a recent media report indicated that Nigeria had up to a million expired COVID-19 vaccines and some Nigerians might have taken the expired vaccines unaware. This can further increase mistrust and hence COVID-19 hesitancy.[19] The government needs to rebuild trust in its people by exploring target messaging around the COVID-19 vaccine to further enlighten people and positively influence perception.
Almost half of the respondents in our study raised concerns about the vaccine's efficacy, while 20.2% believed that it is a scheme for powerful people to control the world. This is not surprising as many conspiracy theories existed on social media ahead of the availability of the vaccine. Our evaluation also revealed that respondents' concerns about the vaccines majorly revolved around negative health impact and ineffectiveness against new COVID strains. This corroborates the findings of a study on public perception of the COVID-19 vaccine in Nigeria where respondents doubted vaccine effectiveness and believed that the vaccine is not safe.[20] While research has shown that religious leaders potentially contributed to conspiracy theories affecting the public perceptions of vaccines,[18,21] 71.3% of the students in our study do not believe that the COVID-19 vaccine is against their religious beliefs. Overall, most participants had a negative perception of the COVID-19 vaccine. This outlook is neither good for a nation with increasing COVID-19 cases nor for the goal to combat the disease.[22]
The level of vaccination coverage and acceptance was low in this study as only 5% of respondents had received it and 27.8% would take it for free. On the contrary, a study in Nigeria reported an estimated 74% vaccine acceptance, which is higher than the 27.8% willingness reported in our study.[20] Similarly, another study reported a high COVID-19 vaccine acceptance (50%) among respondents.[18] The differences observed may be due to the variation in the respondent type; over 70% of respondents in the other study were over 24 years of age compared to 6% in our study. A study in the Democratic Republic of Congo, however, reported a similar proportion of acceptance (28%) as in our study.[23]
Although our data reveal a wide gap in vaccine coverage, it is worthy of note that from the time this data was collected until now, there is a likelihood that the gap has since reduced due to interventions such as mass vaccination campaigns for employees by their organizations; compulsive vaccination for international travel has also significantly enhanced vaccine uptake. Nonetheless, it is baffling that about 35% of our respondents would not take the vaccine even if the vaccine were to be free. This implies that if cost were to be added, the unwillingness level would skyrocket.
Many other studies have also reported high unwillingness to receive the COVID-19 vaccine among different populations. For instance, unwillingness to receive the COVID-19 vaccine was reported in Russia, Poland, Hungary, France, South Africa, and Germany to be 47%, 45%, 44%, 36%, and 33%, respectively, in a report by IPSOS.[24] However, up to 5%, 7%, and 35% were unwilling to take the vaccine in Ethiopia, Niger, and Senegal, respectively.[25] Although more than half of the participants in this study believed in the efficacy of the vaccine, not many are willing to take it. Besides, only 33% of our respondents would allow their family and friends to take the vaccine. Tobin et al.[18] also reported that less than half of respondents in their study would allow vaccines for their elderly and above half for their school children. Youths are generally susceptible to peer influences. Thus, chances are that youths who uptake or do not uptake the vaccine might be able to influence their friends and families to do the same.
The bivariate analysis to test the association between sociodemographic characteristics of respondents and COVID-19 vaccine perception was only significant for marital status (P < 0.05); other variables tested were insignificant (P > 0.05). This result is perhaps due to chance as most participants were single. Age, ethnic group, and student's level of study were significantly associated with respondents' perception of the COVID-19 vaccine (P < 0.05). A previous study reported associated factors such as education level and socioeconomic status. Soares et al.[26] found no significant difference between sex and willingness to take the vaccine. The bivariate tests revealed a significant association between COVID-19 perception and COVID-19 vaccine perception (P < 0.05). For instance, the belief that COVID-19 is not real as reported by some of our respondents potentially has a role to play in respondents' vaccine perception. Lastly, a significant association was discovered between respondents' perception of COVID-19 and acceptance of the COVID-19 vaccine (P < 0.05) as well as respondents' perception of acceptance of the COVID-19 vaccine (P < 0.05). The perception that COVID-19 is not real or not deadly would preclude respondents from accepting the vaccine. However, recent studies have reported that over 90% of university students believed COVID-19 is real, with a significant portion even predisposed to mental health challenges.[27,28] A study in Indonesia revealed that a high COVID-19 risk perception influenced respondents' willingness to accept the vaccine.[29] Similarly, Al-Mohaithef et al.[30] suggested that if individuals perceive that they are at increased danger of getting COVID-19 or that the vaccine is highly effective against the disease, they would be less hesitant to take the vaccine.
Limitations and Recommendations
Results' generalizability to the wider population and the informal sector youths may be inaccurate as the survey sample was small and did not consider other regions of the country. There is also a dearth of literature exploring the associated factors with the perception of COVID-19 vaccine acceptance. In addition, the kind of analysis conducted prevented the exploration of the degree of association of factors. Consider also that data obtained were self-reported and are likely prone to social desirability bias. Finally, being a cross-sectional survey, the cause-and-effect association between variables could not be ascertained.
Beyond cost, policymakers and key stakeholders should begin to explore tackling factors such as ascertaining the vaccine effectiveness in addition to transparent and right communication of the same to improve the perception of people and increase acceptance. In addition, we urge the government to employ grassroots measures by using local, traditional/religious leaders, local radio stations, and other decentralized measures to encourage the masses to uptake effective COVID-19 vaccines. Similarly, tertiary institution authorities should work alongside the government and health professionals to enhance vaccination communication and engagement among their students to build trust and increase acceptance. Moreover, it is necessary for the Government of Nigeria and Africa in general to fund its epidemiologists, scientists, and everyone involved in the healthcare sector to build the needed capability to manufacture effective COVID-19 vaccines, thereby reducing heavy reliance on imported vaccines on the verge of expiration. Finally, more effort is required by the government to ensure quality data on COVID-19 mortality and COVID-19 vaccine-related adverse effects are available to enhance transparency and public trust.
Conclusion
COVID-19 vaccine hesitation is real in Nigeria amidst other countries of the world. Our study found 35% hesitancy and 37.2% undecidedness toward the COVID-19 vaccination even if offered freely. This is largely due to the kind of information the people are exposed to, which in turn influenced their decision on taking up the vaccine. Therefore, more attention should be paid to advocacy and health awareness by the government and health workers to improve COVID-19 vaccine uptake.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
We appreciate the Ethics and Research Committee of Ekiti state University Teaching Hospital (EKSUTH) and the respondents (students) for support as well as their responses during the survey. Special thanks to the Research assistants involved with data collection.
References
- 1.Sharpe HR, Gilbride C, Allen E, Belij-Rammerstorfer S, Bissett C, Ewer K, et al. The early landscape of coronavirus disease 2019 vaccine development in the UK and rest of the world. Immunology. 2020;160:223–32. doi: 10.1111/imm.13222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.The New York Times. Coronavirus Vaccine Tracker. 2020. [Last accessed on 2021 Feb 18]. Available from: https://www.nytimes.com/interactive/2020/science/coronavirus-vaccine-tracker.html .
- 3.Kerr JR, Schneider CR, Recchia G, Dryhurst S, Sahlin U, Dufouil C, et al. Predictors of COVID-19 vaccine acceptance across time and countries. MedRxiv. 2020 doi: 10.1136/bmjopen-2020-048025. doi: 10.1101/2020.12.09.20246439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wang K, Wong ELY, Ho KF, Cheung AWL, Chan EYY, Yeoh EK, et al. Intention of nurses to accept coronavirus disease 2019 vaccination and change of intention to accept seasonal influenza vaccination during the coronavirus disease 2019 pandemic: A cross-sectional survey. Vaccine. 2020;38:7049–56. doi: 10.1016/j.vaccine.2020.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alfageeh E, Alshareef N, Angawi K, Alhazmi F, Chirwa G. Acceptability of a COVID-19 vaccine among the Saudi population. Vaccines (Basel) 2021;9:226. doi: 10.3390/vaccines9030226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sallam M. COVID-19 vaccine hesitancy worldwide: A concise systematic review of vaccine acceptance rates. Vaccines. 2021;9:160. doi: 10.3390/vaccines9020160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sharun K, Tiwari R, Iqbal Yatoo M, Patel SK, Natesan S, Dhama J, et al. Antibody-based immunotherapeutics and use of convalescent plasma to counter COVID-19: Advances and prospects. Expert Opin Biol Ther. 2020;20:1033–46. doi: 10.1080/14712598.2020.1796963. [DOI] [PubMed] [Google Scholar]
- 8.Organisation for Economic Co-operation and Development. Enhancing public trust in COVID-19 vaccination: The role of governments. OECD. 2021. [Last accessed on 2021 Sep 08]. Available from: https://www.oecd.org/coronavirus/policy-responses/enhancing-public-trust-incovid-19-vaccination-the-role-of-governments-eae0ec5a/
- 9.Acheampong T, Akorsikumah EA, Osae-Kwapong J, Khalid M, Appiah A, Amuasi JH. Examining vaccine hesitancy in Sub-Saharan Africa: A survey of the knowledge and attitudes among adults to receive COVID-19 vaccine in Ghana. Vaccines (Basel) 2021;9:814. doi: 10.3390/vaccines9080814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ochu CL, Beynon CM. Hepatitis B vaccination coverage, knowledge and sociodemographic determinants of uptake in high risk public safety workers in Kaduna State, Nigeria: A cross sectional survey. BMJ Open. 2017;7:e015845. doi: 10.1136/bmjopen-2017-015845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Omotowo IB, Meka IA, Ijoma UN, Okoli VE, Obienu O, Nwagha T, et al. Uptake of hepatitis B vaccination and its determinants among health care workers in a tertiary health facility in Enugu, South-East, Nigeria. BMC Infect Dis. 2018;18:1–9. doi: 10.1186/s12879-018-3191-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Baiye B, Oguntola I. Will you take the COVID-19 vaccine? A household survey on the perception of Nigerians toward COVID-19 vaccine. Nigeria Health Watch. 2021. [Last accessed on 2021 Oct 18]. Available from: https://nigeriahealthwatch.com/will-you-take-the-covid-19-vaccine-a-household-survey-on-the-perception-of-nigerians-towards-a-covid-19-vaccine/
- 13.Olomofe CO, Soyemi KV, Udomah BF, Owolabi AO, Ajumuka EE, Igbokwe MC, et al. Predictors of uptake of a potential Covid-19 vaccine among Nigerian adults. J Vaccines Vaccin. 2021;12:442. [Google Scholar]
- 14.Oyeoku EK, Talabi FO, Oloyede D, Boluwatife AA, Gever VC, Ebere I. Predicting COVID-19 health behaviour initiation, consistency, interruptions, and discontinuation among social media users in Nigeria. Health Promot Int. 2021;37:daab059. doi: 10.1093/heapro/daab059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Varma JK, Thamkittikasem J, Whittemore K, Alexander M, Stephens DH, Arslanian K, et al. COVID-19 infections among students and staff in New York City public schools. Pediatrics. 2021;147:e2021050605. doi: 10.1542/peds.2021-050605. [DOI] [PubMed] [Google Scholar]
- 16.Mheidly N, Fares J. Leveraging media and health communication strategies to overcome the COVID-19 infodemic. J Public Health Policy. 2020;41:410–20. doi: 10.1057/s41271-020-00247-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mohamed NA, Solehan HM, Mohd Rani MD, Ithnin M, Che Isahak CI. Knowledge, acceptance and perception on COVID-19 vaccine among Malaysians: A web-based survey. PLoS One. 2021;16:e0256110. doi: 10.1371/journal.pone.0256110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tobin EA, Okonofua M, Azeke A. Acceptance of a COVID-19 vaccine in Nigeria: A population-based cross-sectional study. Ann Med Health Sci Res. 2021;11:1445–52. [Google Scholar]
- 19.Reuters. Exclusive: Up to 1 million COVID vaccines expired in Nigeria last month. [Last accessed on 2022 Feb 01]. Available from: https://www.reuters.com/business/healthcare-pharmaceuticals/exclusive-up-1-million-covid-vaccines-wasted-nigeria-last-month-2021-12-08/
- 20.Adebisi YA, Alaran AJ, Bolarinwa OA, Akande-Sholabi W, Lucero-Prisno DE. When it is available, will we take it? Public perception of hypothetical COVID-19 vaccine in Nigeria. medRxiv. 2020 doi: 10.11604/pamj.2021.38.230.27325. doi: 10.1101/2020.09.24.20200436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Garcia LL, Yap JF. The role of religiosity in COVID-19 vaccine hesitancy. J Public Health (Oxf) 2021;43:e529–30. doi: 10.1093/pubmed/fdab192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ohia C, Bakarey AS, Ahmad T. COVID-19 and Nigeria: Putting the realities in context. Int J Infect Dis. 2020;95:279–81. doi: 10.1016/j.ijid.2020.04.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nzaji MK, Ngombe LK, Mwamba GN, Ndala DB, Miema JM, Lungoyo CL, et al. Acceptability of vaccination against COVID-19 among healthcare workers in the Democratic Republic of the Congo. Pragmat Obs Res. 2020;11:103–9. doi: 10.2147/POR.S271096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.IPSOS. Three in four adults globally say they would get a vaccine for COVID-19. 2020. [Last accessed on 2021 Jan 12]. Available from: https://www.ipsos.com/sites/default/files/ct/news/documents/2020-09/global-attitudes-on-a-covid-19-vaccine-ipsos-survey-for-wef-2020.pdf .
- 25.Africa CDC. Majority of Africans would take a safe and effective COVID-19 vaccine. [Last accessed on 2021 Jan 12]. https: //africacdc.org/news-item/majority-of-africans-would-take-a-safe-and-effective-covid-19-vaccine/
- 26.Soares P, Rocha JV, Moniz M, Gama A, Laires PA, Pedro AR, et al. Factors associated with COVID-19 vaccine hesitancy. Vaccines (Basel) 2021;9:300. doi: 10.3390/vaccines9030300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Olawade DB, Wada OZ, Asaolu FT, Odetayo A, Akeju OO, Olorunsogbon OF. COVID-19 and students' mental wellbeing: A cross-sectional study across selected Nigerian universities. J Educ Soc Behav Sci. 2021;34:176–86. [Google Scholar]
- 28.Olawade DB, Olorunfemi OJ, Wada OZ, Afolalu TD, Enahoro MA. Internet addition among university students during COVID-19 Lockdown: Case study of institutions in Nigeria. J Educ Hum Dev. 2020;9:165–73. [Google Scholar]
- 29.Harapan H, Wagner AL, Yufika A, Winardi W, Anwar S, Gan AK, et al. Acceptance of a COVID-19 vaccine in Southeast Asia: A cross-sectional study in Indonesia. Front Public Health. 2020;8:381. doi: 10.3389/fpubh.2020.00381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Al-Mohaithef M, Padhi BK. Determinants of COVID-19 vaccine acceptance in Saudi Arabia: A web-based national survey. J Multidiscip Healthc. 2020;13:1657–63. doi: 10.2147/JMDH.S276771. [DOI] [PMC free article] [PubMed] [Google Scholar]


