Abstract
Objective:
Change talk, or client language that is consistent with making a behavioral change, has been found to improve the efficacy of motivational interviewing (MI). It is not known, however, if change talk helps to explain MI’s effect on instigating a quit attempt in smokers with serious mental illness.
Methods:
We measured change talk in smokers with a serious mental illness (SMI) randomized to receive either a single session adaptation of motivational interviewing or an interactive education intervention. We evaluated relationships between treatment condition, proportion of change talk, and study outcomes of quit attempts and willingness to follow up on treatment provider referrals.
Results:
Participants receiving the adaptation of motivational interviewing had higher proportions of change talk than participants in the interactive education condition. However, total proportion of change talk did not mediate the relationship between treatment and outcome, nor did it predict making a quit attempt or following up on a referral to contact a treatment provider.
Conclusions:
Our study found that motivational interviewing has the same change talk augmenting effect in individuals with SMI as those without SMI. Given that anhedonia, negative affect, and depressive symptoms are a major part of serious mental illnesses, it is encouraging that MI can generate change talk in this population. Future smoking cessation intervention trials with larger samples should investigate whether greater amounts of change talk lead to increased quit attempts in this population.
Keywords: Motivational interviewing, serious mental illness, smoking, cessation, change talk
Introduction
Smoking continues to be the main preventable cause of death in the United States, with approximately fourteen percent of US adults continuing to smoke cigarettes (Wang et al., 2018). Individuals who smoke cigarettes have a greater likelihood of experiencing a heart attack, stroke, developing lung disease, or various types of cancer (National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health, 2014). In particular, this is an issue in individuals with bipolar disorder and schizophrenia, where smoking rates exceed fifty percent (Garcia-Portilla et al., 2016). Smoking can greatly elevate the risk of death from heart disease in individuals with schizophrenia (Kelly et al., 2011) and has been found to be the main contributor to premature mortality in this population (Dickerson et al. 2016). For these reasons, it is imperative that we improve cessation rates among smokers with serious mental illness (SMI). SMI consists of psychological or behavioral disorders that cause severe impairment in day-to-day activities (National Institute of Mental Health, 2021). Motivational interviewing (MI) has been investigated as a potential way to do so (Steinberg et al., 2004. Steinberg et al., 2016).
MI is a client-centered counseling style used to treat substance use disorders and improve health behaviors (Miller & Rollnick, 2012). MI therapists seek to generate change talk (CT), which is defined as language consistent with making a behavior change (Amrhein et al., 2003) because it is considered one of MI’s main mechanisms of change (Amrhein et al., 2003). In a seminal study, Amrhein et al. (2003) coded the MI sessions of 84 clients who had participated in a substance use outcome trial and demonstrated that expressed commitment strength predicts drug use outcomes. For the purpose of the analyses, they divided the study participants into four groups based on patterns of use: maintainers, changers, strugglers, and discrepants. Maintainers reported high levels of abstinence at baseline and the follow-up period. Changers reported low levels of abstinence at baseline but maintained high levels of abstinence throughout the follow-up period. Strugglers reported low levels of abstinence at baseline and only low-to-moderate levels throughout the follow-up period. Discrepants reported complete abstinence but provided a positive urine sample. They examined the pattern of CT in each group by dividing the MI session into ten deciles and comparing patterns of CT between groups in each decile. Amrhein et al. (2003) stated that the tenth decile was the most important because the strength of CT during this decile most reliably discriminated treatment responders from non-treatment responders. This separation likely occurred because it is in the tenth decile that clients assessed the impact of their change plan and considered barriers to its implementation.
Since then, numerous studies have found that MI consistent behaviors are positively related to the amount of CT (Catley et al., 2006; Dobber et al., 2020; Magill et al., 2018; Pace et al., 2017), and the strength and frequency of CT predicts future outcomes (Carpenter et al., 2016; Gaume et al., 2016; Moyers et al., 2007; Romano & Peters, 2016; Vader et al., 2010). Sustain talk (ST) consists of statements made by the client in favor of continued drug use and negatively impacts treatment outcome (Apodaca et al., 2014; Magill et al., 2014, 2018; Magill & Hallgren, 2019; Pace et al., 2017).
Adaptations of MI retain the core principles of MI while integrating them with techniques from other treatments (Steinberg et al., 2016) and have been shown to be effective in helping individuals quit smoking (Borrelli et al., 2010; Bredie et al., 2011). To our knowledge only two studies have examined the impact of motivational interviewing or adaptations of motivational interviewing on tobacco use in individuals with SMI. In both studies, adaptations of motivational interviewing were more effective than an education-only intervention in motivating smokers with serious mental illness to make quit attempts and/or to seek formal treatment for tobacco use disorder (Steinberg et al., 2004, 2016). Although more research is needed, these two studies provide preliminary support for MI’s ability to generate quit attempts in individuals with serious mental illness.
Although there are a large number of studies measuring CT in substance using populations without serious mental illness, there are only a few studies (see Dobber et al., 2020) on the effect of CT on treatment efficacy in populations with serious mental illness. Language deficits are a key part of schizophrenia (Brown & Kuperberg, 2015) and individuals with serious mental illness, many of whom have a schizophrenia spectrum disorder, may have different speech patterns. Therefore, it is important to determine whether CT follows similar patterns and is as influential across populations, so future adaptations of motivational interviewing can better target relevant mechanisms of change.
In the present study we analyzed patterns and the impact of within-session CT on treatment outcomes using session tapes from Steinberg et al. (2016). We hypothesized that smokers with serious mental illness randomized to receive an adaptation of motivational interviewing would produce a higher proportion of CT than smokers with serious mental illness who received psychoeducation. We also predicted that smokers with serious mental illness who made a quit attempt would produce a higher proportion of CT than smokers who did not make a quit attempt. In addition, we predicted that CT would mediate the relationship between intervention and outcome. Consistent with Amrhein et al. (2003), we predicted that the proportion of CT in the tenth decile would most strongly predict treatment outcome. Additionally, in Steinberg et al. (2016), the final minutes of the session which would fall in the tenth decile included the therapists’ discussion regarding the treatment referral. Therefore, we hypothesized that this was the decile where the most influential CT would be generated. Finally, we ran post-hoc exploratory analyses looking at the relationship between contacting a treatment provider and the proportion of CT.
Methods
Participants
This analysis of client speech consisted of a subsample of 82 participants from a previous study assessing the efficacy of an adaptation of motivational interviewing for addressing tobacco use in individuals with schizophrenia, schizoaffective disorder, and bipolar disorder (Steinberg et al., 2016). Participants’ age ranged from 22–63 years old (M = 42.56, SD = 10.148). We were unable to use the full sample (N = 98) from the original study because several poor-quality recordings could not be coded. The sample was 45.1% female, 58.5% white, 79.3% regular cigarette smokers, 62.2% menthol cigarette smokers, 62.2% never married, and 90.2% unemployed. The mean age that participants regularly began smoking was 16.52 years old (range 7–43, SD = 5.938). Smokers reported attempting to quit an average of 2.79 times (SD = 2.696). See Table 1 for a complete list of demographic characteristics.
Table 1.
Demographic Characteristics Within Each Treatment Condition.
| Characteristic | Motivational interviewing (n=41) | Interactive education (n=41) |
|---|---|---|
| Gender | ||
| Female | 46.3% (19) | 43.9% (18) |
| Male | 53.7% (22) | 56.1% (23) |
| Diagnosis | ||
| Bipolar disorder | 20.7% (17) | 22.0% (18) |
| Schizoaffective | 14.6% (12) | 11.0% (9) |
| Schizophrenia | 14.6% (12) | 17.1% (14) |
| Race/Ethnicity | ||
| Black | 26.8% (11) | 31.7% (13) |
| White | 61.0% (25) | 56.1% (23) |
| Latino | 2.4% (1) | 9.8% (4) |
| Asian | 2.4% (1) | 0.0% (0) |
| Other | 7.3% (3) | 2.4% (1) |
| Marital status | ||
| Never married | 73.2% (30) | 51.2% (21) |
| Married | 7.3% (3) | 12.2% (5) |
| Separated | 2.4% (1) | 9.8% (4) |
| Divorced | 12.2% (5) | 24.4% (10) |
| Other or unknown | 4.9% (2) | 2.4% (1) |
| Employment status | ||
| Unemployed | 87.8% (36) | 92.7% (38) |
| Employed part-time | 9.8% (4) | 4.9% (2) |
| Employed full-time | 2.4% (1) | 1.2% (1) |
| Type of cigarette | ||
| Ultra light | 4.9% (2) | 4.9% (2) |
| Light | 19.5% (8) | 12.2% (5) |
| Regular | 75.6% (31) | 82.9% (34) |
| Flavor | ||
| No menthol | 39.0% (16) | 36.6% (15) |
| Menthol | 61.0% (25) | 63.4% (26) |
Interventions
Both conditions were manualized, 45-minute, individual, single session interventions. Therapists provided treatment in both conditions to control for therapist effects. In the adaptation of Motivational Interviewing (MI plus personalized feedback) condition, smokers with serious mental illness were given feedback about their carbon monoxide reading, spending on cigarettes, and information about health conditions that were personally relevant. An MI consistent style was used to deliver the information.
In the Interactive Education condition, smokers with serious mental illness were given non-personalized, psychoeducational material about the impact of cigarette smoking. The information was provided didactically, although visual aids were used and participant interaction was encouraged. See Steinberg et al. (2016) for further details.
Measures
Structured Clinical Interview for DSM-IV Disorders (SCID; First et al., 2002): This is a semi-structured interview used to determine DSM-IV Axis I diagnoses. The scale has strong inter-rater reliability and was used to confirm schizoaffective, schizophrenia, and bipolar disorder diagnoses (Steinberg et al., 2016). Modules A-D were administered to confirm diagnoses.
Timeline Follow Back (TLFB) (Sobell & Sobell 1996): The TFLB was used to assess daily cigarette use and the study authors defined cessation as self-reported 7-day point prevalence abstinence, biochemically confirmed with expired carbon monoxide less than 10 ppm at 1-month follow-up.
Steps to Quitting Questionnaire: The questionnaire was designed by Steinberg et al. (2016)’s research group. It assessed various non-cessation treatment outcomes, including quit attempts and seeking professional assistance to quit smoking. They defined “a quit attempt” as a client reporting a “serious” attempt to stop smoking as recommended by Hughes and Callas (2010). See Steinberg et al. (2016) for more details about the Steps to Quitting Questionnaire.
Client Language Easy Rating (CLEAR) Coding System (Glynn & Moyers, 2012): The CLEAR is a coding system used to calculate the proportion, or frequency, of CT and ST in an MI session. The instruction manual includes information on how to train and assess rater reliability, how to code each session, how to classify speech as CT or ST, and guidelines for times the rater is unsure of how to code a statement.
Procedure
The study was conducted in accordance with the Declaration of Helsinki and approved by the Rutgers Robert Wood Johnson Medical School Institutional Review Board (IRB). Three raters were trained in the CLEAR coding system and supervised by the first author. Training involved studying the CLEAR manual, coding motivational interviewing sessions, and passing quizzes on the coding system (Gaume et al., 2016). Coders were then asked to independently code non-study motivational interviewing sessions until they reached an inter-rater reliability of at least 0.60, which is deemed adequate by the CLEAR manual. A total of 82 tapes were coded for instances of CT or ST with 24% of tapes double coded. Reliability was determined as follows: 1) each column in SPSS corresponded to a specific rater, 2) each set of twenty cells within a column corresponded to a specific participant’s session, 3) each cell within the set of twenty contained the amount of CT or ST spoken in a specific decile during that session. Cells were matched across the three raters, allowing us to confirm that all three raters were listening and parsing client speech similarly. An average ICC range between raters was calculated, 95% CI [0.866, 0.914]. The average ICC range for the 10th decile codes was also calculated, 95% CI [0.508, 0.884].
When raters listened to session tapes, session length was determined by a cassette tape counter. They then divided the tape’s total count by ten to determine the length of one decile. For example, if a final session count was 590, each decile would be composed of 59 counts (590/10); for example, decile 1 would correspond to count 0–59, decile 2 count 60–118, etc. To calculate total proportion of CT, each utterance of CT was noted, summed and divided by total number of CT and ST utterances (Glynn & Moyers, 2012), as shown below. To calculate proportion of CT in the tenth decile, each utterance of CT in the tenth decile was noted, summed and divided by total number of CT and ST utterances in the tenth decile, as shown below.
Analyses
We ran bivariate correlations to identify confounding relationships between demographic and dependent variables. We ran a mediation analysis using PROCESS, which is a macro that uses linear or logistic regression and a path analytic framework to assess mediation (Hayes & Rockwood, 2017). The PROCESS macro specifies the indirect effect as a measure of whether a variable exerts a mediating effect (Hayes & Rockwood, 2017). The indirect effect is quantified as (a*b). If it is found to be significant, then we canreject the null hypothesis and assert that the variable under consideration is a mediator even if none of the other relationships in the analysis are significant.
We ran a mediation model with treatment condition as the independent variable (coded as MI = 1, psychoeducation = 2) quit attempt as the dependent variable (coded as no quit attempt = 0, quit attempt = 1), and proportion of change talk as the mediator (see Figure 1). Diagnosis was entered as a covariate in all models. We then ran a logistic regression with total proportion of change talk and proportion of change talk in the tenth decile entered as independent variables and following up with a smoking cessation treatment provider entered as the dependent variable. We also ran a logistic regression with treatment condition, total proportion of change talk, and proportion of change talk in the tenth decile as independent variables and following up with a smoking cessation treatment provider as the dependent variable.
Figure 1.
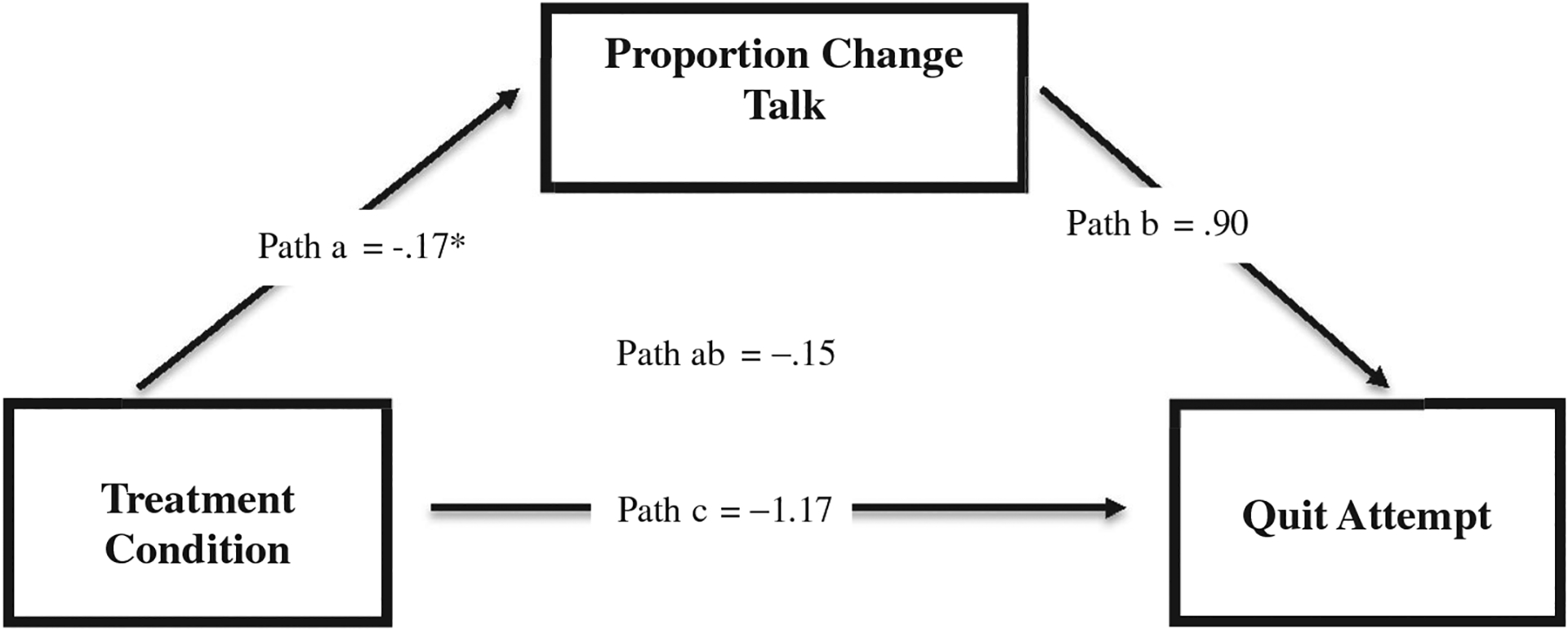
Mediation model. *p < .05.
Results
Quit attempts and treatment seeking
Individuals in the MI condition made more quit attempts by the 1-month follow-up than individuals in the psychoeducation condition (34.2% vs. 12.2%), t(71.05) = 2.41, p = .019. Although there was no statistically significant difference t(71.31) = 1.46, p = .148, 37.8% of individuals in the MI condition and 22.5% of individuals in the psychoeducation condition followed up with a treatment provider for tobacco dependence treatment. For more details about study outcomes with the whole treatment sample, see Steinberg et al. (2016).
Mechanisms of change
In our mediation model (see Figure 1), controlling for diagnosis, only path a was significant, β = −0.17, t(79) = −3.89, p = .002. Path b was not significant β = 0.90, z = 0.58, p = .5591, and neither was path ab, β = −0.15, 95% CI [0.88, 0.58]. In addition, we ran a stepwise logistic regression to see whether proportion of change talk in the 10th decile would predict quit attempts above total proportion of change talk. There was no significant effect for either total proportion of change talk, OR = 11.17, Wald(1) = 2.33, p = .127, 95% CI [0.51, 247.33] or proportion of change talk in the 10th decile, OR = 0.56, Wald(1) = 0.35, p = .654, 95% CI [0.16, 2.69].
Treatment seeking and change talk
We examined the proportion of change talk produced among those who did and did not follow up on a referral to contact a treatment provider. We found there was no significant difference in the proportion of change talk, t(75) = −1.14, p = .260, produced between those who did and did not contact a treatment provider.
In addition, we ran a logistic regression to see if proportion of change talk in the tenth decile would predict contacting a treatment provider, above total proportion of change talk and treatment condition. There was no significant effect for treatment group, OR = 0.59, Wald(1) = 0.93, p =.336, 95% CI [0.20, 1.74], total proportion of change talk, OR = 0.93, Wald(1) = 0.002, p = .964, 95% CI [0.04, 19.91], or proportion of change talk in the 10th decile, OR = 2.93 Wald(1) = 1.60, p = .206, 95% CI [0.55, 15.48].
Discussion
To the best of our knowledge, this is one of the few studies to look at the frequency of change talk and its effect on treatment outcome in individuals with SMI. We coded tapes of a single session adaptation of motivational interviewing, and a time-matched interactive education intervention for frequency of change talk. As hypothesized, participants receiving an adaptation of motivational interviewing produced a higher proportion of change talk compared to participants receiving an interactive educational intervention (Table 2).
Table 2.
Process and Outcome Variables.
| Variable | Motivational interviewing | Interactive education | t |
|---|---|---|---|
| Session time (min) | 45 - | 45 - | – |
| Utterances CT | 27.9 (10.3) | 8.5 (6.2) | 10.39* |
| Utterances ST | 8.1 (7.9) | 4.7 (2.7) | 2.64* |
| Total proportion % CT | 78.2 (16.3) | 61.0 (22.9) | 3.92* |
| Total proportion % ST | 21.8 (16.3) | 39.0 (22.9) | −3.92* |
| Smoking at follow-up | |||
| CPD | 15.3 (8.4) | 16.58 (8.2) | −0.67 |
| Time to first cig (min) | 24.7 (48.1) | 13.03 (20.8) | 1.31 |
| % Quit attempts | 34.2 (48.1) | 12.2 (33.1) | 2.41* |
| Contacted Tx provider | 37.8 (49.2) | 22.5 (42.3) | 1.46 |
Note. The counseling sessions were scheduled for 45 min each.
p < .05.
This finding is consistent with research investigating the relationship between motivational interviewing, motivational interviewing consistent behaviors, and change talk in patients with (Dobber et al., 2020) and without serious mental illness (Catley et al. 2006; Gaume et al., 2008; Magill et al., 2018; Magill & Hallgren, 2019; Moyers et al., 2007; Vader et al., 2010). Catley et al. (2006) analyzed process data from a smoking cessation trial comparing MI plus bupropion versus MI plus placebo in African American smokers. The authors found that the quantity of MI consistent behaviors was positively correlated with quantity of change talk. Additionally, a meta-analysis of 36 process studies of MI for alcohol use, other drug use, and problematic health behaviors (Magill et al., 2018) found a consistent positive relationship between proportion of MICO and proportion of within-session change talk. Most relevant to the current study of smokers with serious mental illness, Dobber et al. (2020) found that a higher level of MI consistent behaviors employed by clinicians was followed by greater quantities of change talk in individuals with schizophrenia receiving an intervention to increase medication adherence. Specifically, the authors found that change talk often followed reflections and open-ended questions, and that this was enabled by a strong therapeutic alliance.
The adaptation of motivational interviewing produced almost three times more total utterances than the interactive education intervention, which is in line with previous research (Magill et al., 2019). This finding is noteworthy because the education intervention was developed to be engaging, however, the adaptation of motivational interviewing intervention was significantly more productive at generating client speech.Based on these findings, our study shows that motivational interviewing exerts the same effects on client language in individuals with serious mental illness, as it does in individuals without serious mental illness.
Contrary to hypotheses, proportion of change talk did not mediate the relationship between treatment and outcome. This contradicts previous research in populations without serious mental illness (Eaton et al., 2018; Houck et al., 2018; Moyers et al., 2009; Pirlott et al., 2012). In three of these studies, the amount of change talk explained the relationship between motivational interviewing consistent behaviors and reduced drinking (Eaton et al., 2018; Houck et al., 2018; Moyers et al., 2009). In a fourth study looking at MI for health behaviors, change talk mediated the relationship between MI counselors’ skills and increased fruit and vegetable consumption (Pirlott et al., 2012).
Although we did not find a relationship between the proportion of change talk and treatment outcome, there are several significant implications that can still be drawn from these data. Individuals with serious mental illness suffer from interpersonal, affective, and speech deficits (American Psychiatric Association, 2013) which, in this population, could impact a patient’s ability to generate change talk. Our study is one of the few intervention studies to find that motivational interviewing has the same change talk augmenting effect in individuals with serious mental illness as for those without serious mental illness. Given that anhedonia, negative affect and depressive symptoms are a major part of schizophrenia, schizoaffective disorder, and bipolar disorder (American Psychiatric Association, 2013), it is encouraging that MI can generate change talk in this population. Another implication is the potential for MI to be added to other interventions developed for this population, such as being added as an adjunct to physical health care protocols for this population (Spoelstra et al., 2015) or within cognitive behavioral therapy sessions (Marker & Norton, 2018).
The present study had a number of limitations. First, our sample size and number of quit attempts made by participants were modest. This may have impacted our ability to find a significant relationship between change talk and treatment outcome. In addition, some of the tapes had poor audio quality. Although raters noted when the quality was extremely poor, it is possible that some of the language may have been misunderstood. However, our raters had good reliability (ICC = .73), so the probability of poor audio quality accounting for unexpected outcomes is small. We also may have lost the ability to test more granular hypotheses because of our decision to use the CLEAR to examine change talk because of the CLEAR’s simplicity. Data from the CLEAR did not allow us to parse change talk into specific subcategories (e.g., “desire” or “ability” talk) or measure its strength. We ultimately chose to use the CLEAR because it did not require extensive training or written session transcripts for coding (Glynn & Moyers, 2012), and because it has been used in previous studies to successfully predict alcohol outcomes (Glynn & Moyers, 2010; Moyers et al., 2007).
Future research should address the methodological limitations of the current study. Sessions should be recorded digitally to improve recording quality and ensure that minimal data are lost. The results should be replicated using other coding systems with more established reliability, such as the Motivational Interviewing Skill Code (MISC). Future studies should also investigate the effect of conducting multiple sessions of motivational interviewing to see whether this increases the number of quit attempts in this population. In conclusion, this study documents the relationship between MI and change talk in individuals with SMI and highlights the need for more studies of change talk in this population.
Acknowledgments
The authors would like to express their appreciation to Ylana Lopez, Savannah Chapa, and Sherese Case for serving as raters on the study, and to Drashya Shah and Nicole Weickert for reading the final version of the manuscript and providing feedback.
Funding
Research reported in this publication was supported by National Institute of Drug Abuse (NIDA) of the National Institutes of Health under the following award numbers [R33DA041163, K23DA018203].
Footnotes
Disclosure statement
The authors report no conflict of interests.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Author. 10.1176/appi.books.9780890425596 [DOI] [Google Scholar]
- Amrhein PA, Miller WR, Yahne CE, Palmer M, & Fulcher L (2003). Client commitment language during motivational interviewing predicts drug use outcomes. Journal of Consulting and Clinical Psychology, 71(5), 862–878. 10.1037/0022-006X.71.5.862 [DOI] [PubMed] [Google Scholar]
- Apodaca TR, Borsari B, Jackson KM, Magill M,Longabaugh R, Mastroleo NR, & Barnett NP (2014). Sustain talk predicts poorer outcomes among mandated college student drinkers receiving a brief motivational intervention. Psychology of Addictive Behaviors, 28(3), 631–638. 10.1037/a0037296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Borrelli B, McQuaid E, Novak SP, Hammond SK, & Becker B (2010). Motivating Latino caregivers of children with asthma to quit smoking: A randomized trial. Journal of Consulting and Clinical Psychology, 78(1), 34–43. 10.1037/a0016932 [DOI] [PubMed] [Google Scholar]
- Bredie SJH, Fouwels AJ, Wollersheim H, &Schipper GM (2011). Effectiveness of nurse based motivational interviewing for smoking cessation in high risk cardiovascular outpatients: A randomized trial. European Journal of Cardiovascular Nursing, 10(3), 174–179. 10.1016/j.ejcnurse.2010.06.003 [DOI] [PubMed] [Google Scholar]
- Brown M, & Kuperberg GR (2015). A hierarchical generative framework of language processing: Linking language perception, interpretation, and production abnormalities in schizophrenia. Frontiers in Human Neuroscience, 9(643), 643–623. 10.3389/fnhum.2015.00643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter KM, Amrhein PC, Bold KW, Mishlen K,Levin FR, Raby WN, Evans SM, Foltin RW, & Nunes EV (2016). Derived relations moderate the association between changes in the strength of commitment language and cocaine treatment response. Experimental and Clinical Psychopharmacology, 24(2), 77–89. 10.1037/pha0000063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Catley D, Harris KJ, Mayo MS, Hall S, Okuyemi KS, Boardman T, & Ahluwalia JS (2006). Adherence to principles of motivational interviewing and client within-session behavior. Behavioural and Cognitive Psychotherapy, 34(1), 43–56. 10.1017/S1352465805002432 [DOI] [Google Scholar]
- Dickerson F, Origoni A, Schroeder J, Schweinfurth LAB, Stallings C, Savage CLG, Katsafanas E, Banis M, Khushalani S, & Yolken R (2016). Mortality in schizophrenia and bipolar disorder: Clinical and serological predictors. Schizophrenia Research, 170(1), 177–183. 10.1016/j.schres.2015.11.010 [DOI] [PubMed] [Google Scholar]
- Dobber J, Latour C, van Meijel B, Ter Riet G, Barkhof E, Peters R, Scholte Op Reimer W, & de Haan L (2020). Active ingredients and mechanisms of change in motivational interviewing for medication adherence. A mixed methods study of patient-therapist interaction in patients with schizophrenia. Frontiers in Psychiatry, 11(78), 78–12. 10.3389/fpsyt.2020.00078 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eaton EM, Magill M, Capone C, Cramer MA,Mastroleo NR, Reavy R, & Borsari B (2018). Mechanisms of behavior change within peer-implemented alcohol interventions. Journal of Studies on Alcohol and Drugs, 79(2), 208–216. 10.15288/jsad.2018.79.208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW(2002). Structured clinical interview for DSM-IV-TR axis 1 disorders, research version, patient edition. (SCID-I-P). Biometrics Research. New York State Psychiatric Institute. [Google Scholar]
- Garcia-Portilla MP, Garcia-Alvarez L, Sarramea F,Galvan G, Diaz-Mesa E, Bobes-Bascaran T, Al-Halabi S, Elizagarate E, Iglesias C, Martinez PAS, & Bobes J (2016). It is feasible and effective to help patients with severe mental disorders to quit smoking: An ecological pragmatic clinical trial with transdermal nicotine patches and varenicline. Schizophrenia Research, 176(2–3), 272–280. 10.1016/j.schres.2016.05.011 [DOI] [PubMed] [Google Scholar]
- Gaume J, Gmel G, Faouzi M, & Daeppen J (2008). Counsellor behaviours and patient language during brief motivational interventions: A sequential analysis of speech. Addiction (Abingdon, England), 103(11), 1793–1800. 10.1111/j.1360-0443.2008.02337.x [DOI] [PubMed] [Google Scholar]
- Gaume J, Magill M, Mastroleo NR, Longabaugh R,Bertholet N, Gmel G, & Daeppen J (2016). Change talk during brief motivational intervention with young adult males: Strength matters. Journal of Substance Abuse Treatment, 65, 58–65. 10.1016/j.jsat.2016.01.005 [DOI] [PubMed] [Google Scholar]
- Glynn LH, Moyers TB (2012). Manual for the Client Language Easy Rating (CLEAR) coding system: Formerly “motivational interviewing skill code (MISC) 1.1”. http://casaa.unm.edu/download/CLEAR.pdf
- Glynn LH, & Moyers TB (2010). Chasing change talk:The clinician’s role in evoking client language about change. Journal of Substance Abuse Treatment, 39(1), 65–70. 10.1016/j.jsat.2010.03.012 [DOI] [PubMed] [Google Scholar]
- Hayes AF, & Rockwood NJ (2017). Regression-based statistical mediation and moderation analysis in clinical research: Observations, recommendations, and implementation. Behaviour Research and Therapy, 98, 39–57. 10.1016/j.brat.2016.11.001 [DOI] [PubMed] [Google Scholar]
- Houck JM, Manuel JK, & Moyers TN (2018). Short- and long-term effects of within-session client speech on drinking outcomes in the COMBINE study. Journal of Studies on Alcohol and Drugs, 79(2), 217–222. 10.15288/jsad.2018.79.217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, & Callas PW (2010). Definition of a quit attempt: A replication test. Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco, 12(11), 1176–1179. 10.1093/ntr/ntq165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly DL, McMahon RP, Wehring HJ, Liu F,Mackowick KM, Boggs DL, Warren KR, Feldman S, Shim J-C, Love RC, & Dixon L (2011). Cigarette smoking and mortality risk in people with schizophrenia. Schizophrenia Bulletin, 37(4), 832–838. 10.1093/schbul/sbp152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magill M, & Hallgren KA (2019). Mechanisms of behavior change in motivational interviewing: Do we undertand how MI works? Current Opinion in Psychology, 30, 1–5. 10.1016/j.copsyc.2018.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magill M, Borsari B, Hoadley A, Gordon REF,Apodaca TR, Gaume J, Tonigan JS, & Moyers T (2018). A meta-analysis of motivational interviewing process: Technical, relational, and conditional process models of change. Journal of Consulting and ClinicalPsychology, 86(2), 140–157. 10.1037/ccp0000250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magill M, Gaume J, Apodaca TR, Walthers J,Mastroleo NR, Borsari B, & Longabaugh R (2014). The technical hypothesis of motivational interviewing: A meta-analysis of MI’s key causal model. Journal of Consulting and Clinical Psychology, 82(6), 973–983. 10.1037/a0036833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magill M, Janssen T, Mastroleo N, Hoadley A,Walthers J, Barnett N, & Colby S (2019). Motivational interviewing technical process and moderated relational process with underage young adult heavy drinkers. Psychology of Addictive Behaviors: Journal of the Society of Psychologists in Addictive Behaviors, 33(2), 128–138. 10.1037/adb0000440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marker I, & Norton PJ (2018). The efficacy of incorporating motivational interviewing to cognitive behavior therapy for anxiety disorders: A review and meta-analysis. Clinical Psychology Review, 62, 1–10. 10.1016/j.cpr.2018.04.004 [DOI] [PubMed] [Google Scholar]
- Miller WR, & Rollnick S (2012). Motivational interviewing: Helping people change (3rd ed.). Guilford press. [Google Scholar]
- Moyers TB, Martin T, Christopher PJ, Houck JM,Tonigan JS, & Amrhein PC (2007). Client language as a mediator of motivational interviewing efficacy: Where is the evidence? Alcoholism, Clinical and Experimental Research, 31(10 Suppl), 40S–47S. 10.1111/j.1530-0277.2007.00492.x [DOI] [PubMed] [Google Scholar]
- Moyers TB, Martin T, Houck JM, Christopher PJ,& Tonigan JS (2009). From in-session behaviors to drinking outcomes: A causal chain for motivational interviewing. Journal of Consulting and Clinical Psychology, 77(6), 1113–1124. 10.1037/a0017189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Center for Chronic Disease Prevention and HealthPromotion (US) Office on Smoking and Health. (2014). The Health Consequences of Smoking—50 Years of Progress: A Report of the Surgeon General. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services. https://www.ncbi.nlm.nih.gov/books/NBK179276/ [Google Scholar]
- National Institute of Mental Health. (2021). Mental illness. https://www.nimh.nih.gov/health/statistics/mental-illness.shtml
- Pace BT, Dembe A, Soma CS, Baldwin SA, Atkins DC, & Imel ZE (2017). A multivariate meta-analysis of motivational interviewing process and outcome. Psychology of Addictive Behaviors: Journal of the Society of Psychologists in Addictive Behaviors, 31(5), 524–533. 10.1037/adb0000280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirlott AG, Kisbu-Sakarya Y, Defrancesco CA, Elliot DL, & Mackinnon DP (2012). Mechanisms of motivational interviewing in health promotion: A Bayesian mediation analysis. International Journal of Behavioral Nutrition and Physical Activity, 9(1), 69. 10.1186/1479-5868-9-69 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Romano M, & Peters L (2016). Understanding the process of motivational interviewing: A review of the relational and technical hypotheses. Psychotherapy Research: Journal of the Society for Psychotherapy Research, 26(2), 220–240. 10.1080/10503307.2014.954154 [DOI] [PubMed] [Google Scholar]
- Smedslund G, Berg RC, Hammerstrøm KT, Steiro A,Leiknes KA, Dahl HM, & Karlsen K (2011). Motivational interviewing for substance abuse. Campbell Systematic Reviews, 7(1), 1–126. 10.4073/csr.2011.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell L, & Sobell M (1996). Alcohol Timeline FollowBack (TLFB) user’s manual. Addiction Research Foundation. [Google Scholar]
- Spoelstra SL, Schueller M, Hilton M, & Ridenour K(2015). Interventions combining motivational interviewing and cognitive behavior to promote medication adherence: A literature review. Journal of Clinical Nursing, 24(9–10), 1163–1173. 10.1111/jocn.12738 [DOI] [PubMed] [Google Scholar]
- Steinberg ML, Williams JM, Stahl NF, Budsock PD, & Cooperman NA (2016). An Adaptation of Motivational Interviewing increases quit attempts in smokers with serious mental illness. Nicotine & Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco, 18(3), 243–250. 10.1093/ntr/ntv043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinberg ML, Ziedonis DM, Krejci JA, & Brandon TH (2004). Motivational interviewing with personalized feedback: A brief intervention for motivating smokers with schizophrenia to seek treatment for tobacco dependence. Journal of Consulting and Clinical Psychology, 72(4), 723–728. 10.1037/0022-006X.72.4.723 [DOI] [PubMed] [Google Scholar]
- Vader AM, Walters ST, Prabhu GC, Houck JM, & Field CA (2010). The language of motivational interviewing and feedback: Counselor language, client language, and client drinking outcomes. Psychology of Addictive Behaviors: journal of the Society of Psychologists in Addictive Behaviors, 24(2), 190–197. 10.1037/a0018749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang TW, Asman K, Gentzke AS, Cullen KA,Holder-Hayes E, Reyes-Guzman C, Jamal A, Neff L, & King BA (2018). Tobacco product use among adults—United States, 2017. MMWR. Morbidity and Mortality Weekly Report, 67(44), 1225–1232. 10.15585/mmwr.mm6744a2 [DOI] [PMC free article] [PubMed] [Google Scholar]


