Abstract
Melanotic schwannoma (MS) is a rare peripheral nerve sheath tumor commonly found in the thoracic paraspinal region. It is present in an intracranial location rarely, with 18 out of 105 MS cases described in the literature. Trigeminal nerve was involved in only six of these cases. Fifty percent of psammomatous melanotic schwannoma (PMS) patients have Carney complex. Carney complex is an autosomal dominant disorder featuring peripheral nerve tumors (schwannomas), myxomas (heart, skin, and breast), skin pigmentation (lentigines and blue nevi), and endocrine tumors (adrenal, testicular, and pituitary). We present a case of left trigeminal nerve PMS as a part of Carney complex. Patient had diffuse lentiginosis. Magnetic Resonance Imaging revealed enhancing lesion along left trigeminal nerve with widened Meckel's cave and foramen ovale. Final diagnosis of PMS was derived on clinical, radiological, and histopathological findings with immunohistochemistry correlation.
Key Message
Trigeminal nerve can be rarely involved in melanotic schwannoma (MS). Knowledge of typical radiological features of MS is crucial for its diagnosis. Its association with Carney complex should be sought.
Keywords: melanotic schwannoma, psammoma bodies, intracranial, Meckel's cave, trigeminal nerve, mandibular, foramen ovale, CT, MRI
Introduction
Melanotic schwannoma (MS) is a rare variant of schwannoma arising from sympathetic nervous system with malignant potential. 1 They can occur in unusual sites such as stomach, bone, soft tissue, heart, bronchus, and skin. 2 Two variants are described, psammomatous and nonpsammomatous. Half of psammomatous melanotic schwannoma (PMS) patients have Carney complex. 2 We present computed tomography (CT) and magnetic resonance imaging (MRI) features of a rare case of left trigeminal PMS as a part of Carney complex in a 36-year-old woman who presented with imbalance while walking and diffuse lentiginosis. MS is present in an intracranial location rarely, with 18 out of 105 MS cases described in the literature according to our knowledge. Trigeminal nerve was involved in only six of these cases.
Case History
A 36-year-old woman presented with imbalance while walking. There was remote history of sharp object injury to left eye during her childhood. She complained of left eye vision loss since then. There was no documented history of intervention or surgery in left eye. Presently, there was no perception to light on clinical examination.
She had diffuse lentigines on skin ( Fig. 1g ). Hyperdense lesion at the left cerebellopontine angle was noted. Widening of left Meckel's cave and foramen ovale was also appreciated on CT ( Fig. 1e, f ).On MRI, there was an extra-axial T1 hyperintense and T2 hypointense lesions in the left cerebellopontine angle, following the mandibular division of left trigeminal nerve trajectory, which was extending to and widening the ipsilateral Meckel's cave and foramen ovale ( Fig. 1a–c ). There was no blooming on susceptibility-weighted imaging ( Fig. 1c ). There was no evidence of diffusion restriction. Homogenous enhancement was noted on T1 postcontrast study ( Fig. 1d ). Mass effect was noted on the brain stem with perilesional vasogenic white matter edema tracking along the corticospinal tract. Fatty atrophy of left masticator muscles was seen. Incidentally, deformed left globe was noted with hyperdense content on CT, mild T1 hyperintensity, and T2 hypointensity in the posterior chamber suggestive of incidental chronic vitreous hemorrhage which was unrelated to Carney complex. Diagnosis of left trigeminal (mandibular division) nerve MS as a part of Carney complex was made. She underwent left retromastoid suboccipital craniectomy and for en bloc total removal of the mass. Intraoperatively, black-colored tumor was noted.
Fig. 1.
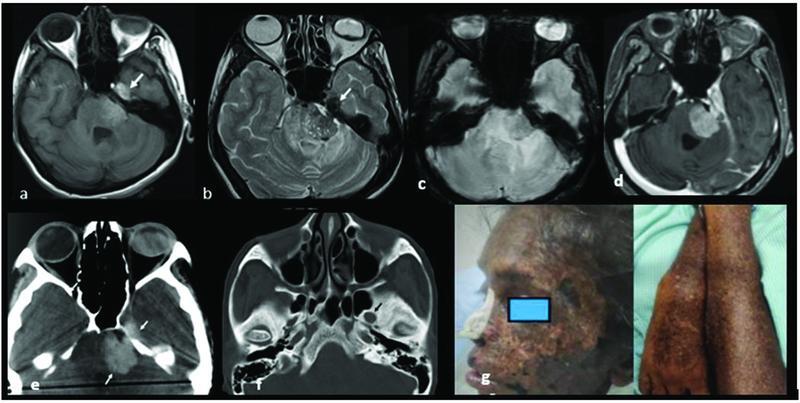
( a, b ) Axial T1WI and T2WI show T1 hyperintense and T2 hypointense lesions in left cerebellopontine angle extending to Meckel's cave ( white arrow ) suggestive of melanotic component in the lesion. Incidental finding: Deformed left globe is noted with hyperdense content on CT, mild T1 hyperintensity, and T2 hypointensity in the posterior chamber suggestive of incidental chronic vitreous hemorrhage. ( c ) SWI shows no evidence of blooming within the lesion. ( d ) Axial T1 postcontrast shows homogenous enhancement. ( e ) Axial NCCT brain shows hyperdense mass ( white arrow ). ( f ) Axial NCCT brain bone window shows smooth widening of left foramen ovale ( black arrow ). ( g ) Diffuse lentigines. CT, computed tomography; NCCT, noncontrast CT; T1WI, T1-weighted imaging; T2WI, T2-weighted imaging; SWI, susceptibility-weighted imaging.
Histopathology showed tumor cells heavily laden with brownish black melanotic pigment with few interspersed psammoma bodies. Tumor cells were immunoreactive for S100 and HMB45 ( Fig. 2 ). Final diagnosis of PMS was derived on clinical, radiological, and histopathological findings with immunohistochemistry correlation.
Fig. 2.
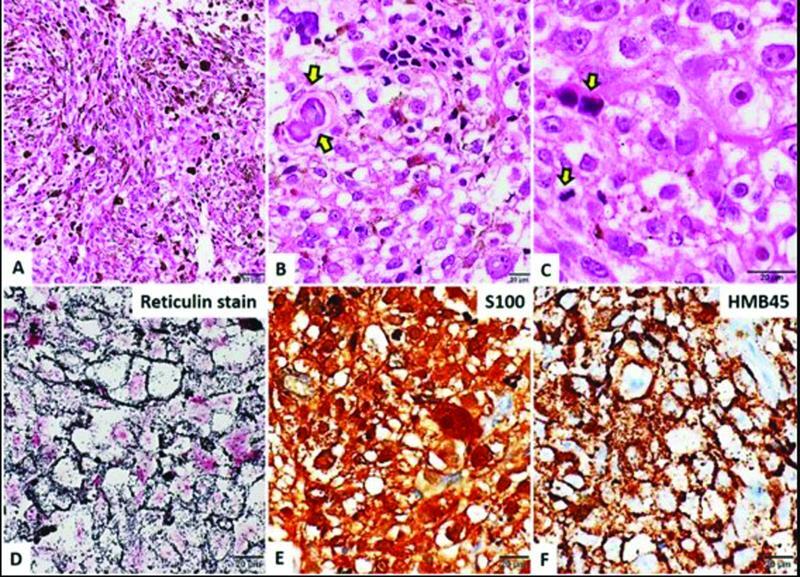
( a ) Microphotograph showing a moderately cellular neoplasm composed of spindled to epithelioid cells arranged in interlacing fascicles which are heavily laden with brownish black melanotic pigment. ( b ) Interspersed few psammoma bodies. ( c ) Cells have vesicular nuclei with prominent macronucleoli. Mitotic figures were evident ( arrow ). ( d ) Tumor shows rich pericellular reticulin as highlighted by Gordon and Sweet's method for reticulin fibers. ( e ) Tumor cells were immunoreactive for S100. ( f ) Tumor cells were immunoreactive for HMB45. Magnification as shown in bar.
Discussion
MS is a rare nerve sheath tumor commonly found in thoracic paraspinal region. They arise from posterior spinal nerve roots or from sympathetic ganglia but are also known to involve in cranial nerves. 3 Only six cases of trigeminal nerve involvement are documented. 4 PMS is a nerve sheath tumor containing melanin-producing cells and psammoma bodies. The mean age of presentation is decade earlier than the conventional schwannoma with peak incidence between fourth and fifth decades of life and no sex predilection. 4 Earlier studies have shown slightly more than 10% of MSs follow a malignant course and show local recurrence after surgery. 5 6
MS is associated with Carney complex, a rare multiple neoplasia syndrome with an unknown prevalence. It can be diagnosed as early as in the second year of life and as late as in the fifth decade of life, usually seen more commonly in females. It is inherited in an autosomal dominant manner or occurring sporadically as a result of a de novo genetic defect. It is characterized by multiple endocrine and nonendocrine neoplasms, pigmented lesions of the skin and mucosa, cardiac, cutaneous, and other myxomatous tumors. The diagnostic criteria for Carney complex are (1) at least two manifestations out of spotty skin pigmentation with a typical distribution (lips, conjunctiva and inner or outer canthi, vaginal and penile mucosa), myxoma (cutaneous and mucosal), cardiac myxoma, PMS, primary pigmented nodular adrenocortical disease (paradoxical positive response of urinary glucocorticosteroid excretion to dexamethasone administration during Liddle's test), acromegaly due to growth hormone-producing adenoma, large-cell calcifying Sertoli cell tumor, thyroid carcinoma, blue nevus, breast myxomatosis, breast ductal adenoma, and osteochondromyxoma or (2) one of these manifestations plus one of the supplemental criteria (an affected first-degree relative or an inactivating mutation of the PRKAR1A gene). 7 8 Our patient had diffuse lentiginosis (spotty skin pigmentation) and PMS (trigeminal nerve MS and psammomatous bodies at histopathology examination). She has two major diagnostic criteria for Carney complex. Thus, the diagnosis of Carney complex was made. Her family history was negative for Carney complex stigmata.
On CT, they appear isodense or hyperdense and show bone changes. They show variable amount of calcification. On MRI, they appear hyperintense on T1-weighted images, iso/hypointense on T2-weighted images, because of intracellular storage of melanin. In contrast, nonmelanotic type of schwannomas are hypoisointense on T1 and hyperintense on T2. Homogeneous or heterogeneous enhancement is seen based on degree of tumor cellularity. 9 With typical MRI features, differentials include other melanotic lesions such as malignant melanoma, pigmented meningioma, meningeal melanocytomas, melanotic medulloblastoma, melanotic carcinomas.
Most of these tumors are highly cellular composed of spindled-shaped cells and epitheloid cells. The cells stain positive for reticulum, melanin, and periodic acid–Schiff. They express neurol-specific enolase, vimentin, S100 protein and stain variably with HMB45 and other melanocytic markers. Antigen K i -67 shows variable mitotic index ranging between 1 and 20%. 10
In Carney complex, each specific complication/tumor should be addressed separately. Radical surgical resection is the treatment of choice for MS. Adjuvant radiotherapy remains controversial. Adjuvant radiotherapy is considered after histological confirmation of malignant nature of the tumor. 6
Conclusion
In conclusion, MS is a rare form of pigmented neural tumor. MRI is crucial for diagnosis of intracranial MS and CT provides additional information on bony changes. MS in the trigeminal nerve is rare, and has be suspected based on typical MRI findings. MS should be considered in a patient with nerve sheath tumor which appears hyperdense on CT, hyperintense on T1-weighted images, and hypointense on T2-weighted images. Its associations in Carney complex has to be sought by further diagnostic work-up. Complete surgical resection is the treatment of choice and is essential to prevent recurrence. Long-term follow-up is recommended as they carry the risk of recurrence and metastases.
Acknowledgment
The authors would like to acknowledge Dr. Radhika Mhatre, DM, consultant pathologist, National Institute of Mental Health and Neuro-Sciences, Bengaluru.
Conflict of Interest None declared.
Source(s) of Support
Nil.
References
- 1.Chikkannaiah P, Boovalli M M, Nathiyal V, Venkataramappa S. Morphological spectrum of peripheral nerve sheath tumors: an insight into World Health Organization 2013 classification. J Neurosci Rural Pract. 2016;7(03):346–354. doi: 10.4103/0976-3147.182768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shanmugam S, Ghosh M, Niamathullah S, Ghosh S. Psammomatous melanotic schwannoma as a component of Carney complex. Indian J Pathol Microbiol. 2015;58(03):368–370. doi: 10.4103/0377-4929.162903. [DOI] [PubMed] [Google Scholar]
- 3.De Cerchio L, Contratti F, Fraioli M F.Dorsal dumb-bell melanotic schwannoma operated on by posterior and anterior approach: case report and a review of the literature Eur Spine J 200615(5, suppl 5):664–669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Spina A, Gagliardi F, Boari N, Terreni M R, Mortini P. Intracranial melanotic schwannomas. J Neurol Surg A Cent Eur Neurosurg. 2015;76(05):399–406. doi: 10.1055/s-0034-1393926. [DOI] [PubMed] [Google Scholar]
- 5.Shields L B, Glassman S D, Raque G H, Shields C B. Malignant psammomatous melanotic schwannoma of the spine: a component of Carney complex. Surg Neurol Int. 2011;2:136. doi: 10.4103/2152-7806.85609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Collart J, Vandeponseele M, Bosschaert P. Intracranial melanotic schwannomas: rare and distinctive tumors to know due to their risk of recurrence and metastases. J Belg Soc Radiol. 2018;102(01):15. doi: 10.5334/jbsr.1359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Li S, Duan L, Wang F D, Lu L, Jin Z Y. Carney complex: two case reports and review of literature. World J Clin Cases. 2018;6(14):800–806. doi: 10.12998/wjcc.v6.i14.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carney J A, Stratakis C A. Epithelioid blue nevus and psammomatous melanotic schwannoma: the unusual pigmented skin tumors of the Carney complex. Semin Diagn Pathol. 1998;15(03):216–224. [PubMed] [Google Scholar]
- 9.Hoover J M, Bledsoe J M, Giannini C, Krauss W E. Intramedullary melanotic schwannoma. Rare Tumors. 2012;4(01):e3. doi: 10.4081/rt.2012.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Alexiev B A, Chou P M, Jennings L J. Pathology of melanotic schwannoma. Arch Pathol Lab Med. 2018;142(12):1517–1523. doi: 10.5858/arpa.2017-0162-RA. [DOI] [PubMed] [Google Scholar]


