Abstract
Purpose
The stress-sensitization hypothesis posits that individuals with prior trauma are at elevated risk for poor mental health when faced with subsequent stressors. Little work has examined whether those who have demonstrated psychological resilience to prior trauma would show either increased resilience or vulnerability to subsequent stressors. We examined pre-pandemic psychological resilience to lifetime trauma in relation to mental health outcomes amid the coronavirus disease 2019 (COVID-19) pandemic, a major societal stressor.
Methods
The sample included 16,900 trauma-exposed women from the Nurses’ Health Study II. Pre-pandemic resilience was defined by psychological health in 2017–2019 (characterized by levels of both distress and positive emotional well-being) relative to lifetime trauma. Resilience was defined categorically by cross-classifying unfavorable, adequate, and favorable psychological health by higher versus lower trauma burden, and continuously as the residual difference in predicted versus actual psychological health regressed on trauma burden. Mental health outcomes as of May–August 2020 included psychological distress symptoms and overall positive emotional well-being. Associations were assessed using covariate-adjusted regression models.
Results
Pre-pandemic resilience was associated with lower distress and higher well-being early in the COVID-19 pandemic. Relative to the women showing highest resilience (favorable psychological health despite higher trauma), only those with lower trauma and favorable prior psychological health had significantly lower distress and higher positive emotional well-being during the pandemic. Higher continuous pre-pandemic resilience was also significantly associated with lower distress and higher positive emotional well-being during the pandemic.
Conclusion
Preventing mental health problems following trauma may contribute to protecting population well-being amid major stressors.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00127-022-02367-y.
Keywords: COVID-19, Longitudinal, Mental health, Psychological resilience, Trauma
Introduction
The stress-sensitization hypothesis posits that individuals who previously experienced major life stressors (e.g., traumas) may be particularly sensitive to adverse impacts of later stressors, with lower thresholds for developing subsequent psychopathology [1–3]. The coronavirus disease 2019 (COVID-19) pandemic represents a highly stressful and potentially traumatic event, negatively impacting mental health in the general population and even more so among healthcare workers [4]. The stress-sensitization hypothesis suggests that individuals with prior trauma history may be at higher risk for mental health morbidity in the context of a pandemic [1, 5]. Despite this, there are likely differences in mental health responses to the pandemic even among individuals at higher risk due to prior trauma. A better understanding of such differences could inform strategies to promote favorable outcomes amid widespread stressful experiences among those at elevated risk.
One differentiating factor may be psychological resilience prior to the COVID-19 pandemic, evidenced for example by the absence of psychopathology and/or presence of positive psychological functioning after trauma exposure [6, 7]. If individuals previously experienced trauma but then demonstrated relatively favorable psychological health, i.e., showed resilience, we might expect them to avoid negative mental health consequences of future stressors like the pandemic, or even to adapt more positively than individuals who never encountered such challenges. Studies suggest that fostering effective coping with stressful experiences may help inoculate against distress to later stressors [8]. However, based on recent evidence from other contexts such as post-disaster settings [9], it is also possible that pre-pandemic resilience would not confer mental health protection from a subsequent stressful experience, such that individuals showing resilience to prior trauma may still be at heightened risk of mental health problems during the pandemic and benefit from targeted support. Addressing such clinically relevant questions requires knowledge about trauma exposure and psychological health ideally obtained before the COVID-19 pandemic.
To examine the association between pre-pandemic resilience and mental health early in the COVID-19 pandemic, the present study drew on data from the Nurses’ Health Study II (NHS II), a longitudinal cohort of US women where pre-pandemic trauma and psychological health are well characterized. NHS II participants also reported current mental health symptoms during the pandemic. We characterized pre-pandemic resilience to lifetime trauma using two standard definitions from the literature and examined its relationship to mental health outcomes, specifically depression, anxiety, posttraumatic stress, and positive emotional well-being, early in the pandemic. We focused particularly on initial mental health outcomes given this was when acute effects of the pandemic (e.g., lockdown, uncertainty) may be most pronounced. The stress-sensitization hypothesis would suggest that individuals who experienced prior trauma may be at heightened risk of poor mental health in the pandemic compared to those who had not previously experienced such trauma. Even if this general model holds, as a more-nuanced extension, we hypothesized heterogeneity among these trauma-exposed individuals, such that those showing pre-pandemic resilience would be relatively less susceptible to adverse mental health consequences of the pandemic.
To test this hypothesis, we compared women who showed evidence of pre-pandemic psychological resilience to trauma (i.e., more favorable psychological health despite higher trauma exposure) to peers who showed lower levels of resilience (i.e., similarly high trauma exposure but poorer psychological health), as well as with peers who had previously faced lower trauma exposure with more or less favorable psychological health. Based on prior literature, we identified and adjusted for multiple socio-demographic factors that may represent confounders (e.g., race/ethnicity, childhood socio-economic status).
Methods
Participants and procedure
Data are from the NHS II, a longitudinal cohort of 116,429 US female registered nurses aged 25–42 upon enrollment in 1989. Women complete biennial questionnaires and follow-up is ongoing. The 2017 biennial questionnaire included a range of psychological symptom measures. In 2018–2019, NHS II participants with known email addresses who were current active cohort participants (i.e., had completed the recent biennial questionnaire, had not opted out of any NHS II substudies, had not passed away) were invited to complete an online supplemental posttraumatic stress disorder (PTSD) questionnaire, which assessed lifetime trauma and psychological functioning; 33,846 women participated (65.7% response rate with repeated invitations) [10]. In 2020, the COVID-19 substudy was initiated and a series of supplemental questionnaires assessing health and well-being amid the pandemic was sent to 55,925 women who were current active cohort participants. Of note, while all participants were nurses upon cohort enrollment, not all were still active healthcare workers during the COVD-19 pandemic. A total of 39,564 participants (70.7% response rate) completed the COVID-19 baseline questionnaire in May–August 2020, and subsequently received monthly questionnaires (follow-ups were administered 1 month after an individual’s prior questionnaire). During that time, there were roughly 3 million COVID-19 cases in the US (July 2020), with most states lifting formal stay-at-home orders by May/June but many local restrictions still in place. Because we were interested in examining individual differences among the trauma-exposed group, and since resilience by definition implies the presence of adversity or challenge [11], we included only women who reported at least one lifetime traumatic event. Thus, women were included in current analyses if they had complete trauma and psychological symptom data from the 2017 biennial questionnaire and 2018–2019 supplemental PTSD questionnaire; reported at least one lifetime traumatic event; and had complete mental health data on the 2020 COVID-19 questionnaires, resulting in an analytic sample of 16,900 (Online Resource Fig. 1). This study was approved by the Partners Healthcare Human Research Committee and return of questionnaires implied consent.
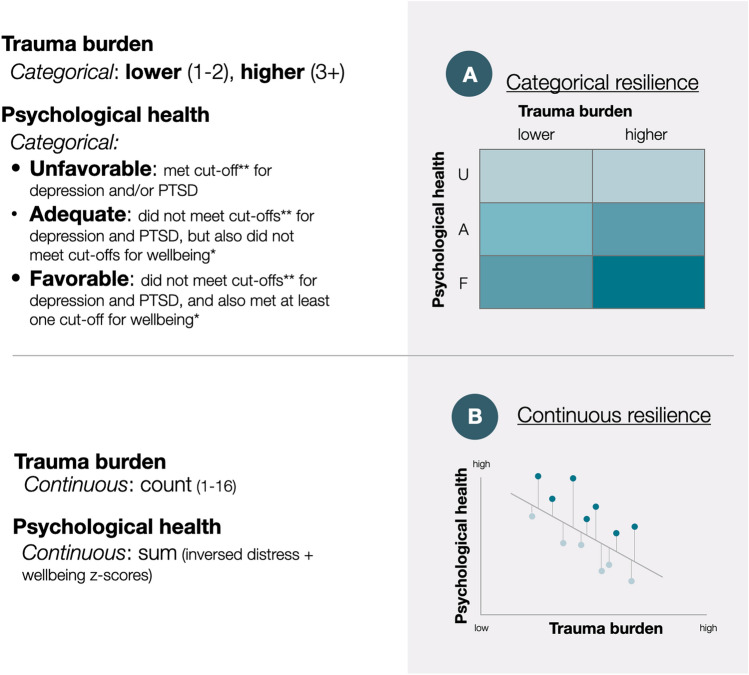
Fig. 1.
Two operational definitions of pre-pandemic resilience to trauma in our sample, based on lifetime trauma burden and pre-pandemic psychological health indicators: A categorical resilience and B continuous resilience. **Cut-off for elevated depression (CES-D score ≥ 10); cut-off for elevated anxiety (GAD-7 score ≥ 10); cut-off for probable PTSD (DSM-5 symptom criteria). *Cut-off for each form of elevated positive emotional well-being (score > median). U = unfavorable, A = adequate, F = favorable. Darker blue in the figure represents conceptually higher levels of resilience
Measures
Predictor: pre-pandemic resilience
Pre-pandemic psychological resilience was defined based on two domains assessed in 2017–2019: 1) lifetime trauma exposure and 2) psychological health indicators (see Online Resource Fig. 2 for timeline of measures). Lifetime trauma exposure was assessed using a modified Brief Trauma Questionnaire [12], a measure developed to assess exposure to traumatic events according to the Diagnostic and Statistical Manual of Mental Disorders, fourth edition (DSM-IV) Criterion A.1. Specifically, the measures query 16 potentially traumatic events, such as life-threatening illness, natural disaster, physical assault, car accidents, and unwanted sexual contact. To index trauma burden, we calculated the count of endorsed event types (potential range 1–16) as a continuous indicator and also created a dichotomous variable reflecting lower (1–2 traumas) and higher (≥ 3 traumas) burden. Categorization of relatively lower versus higher trauma burden is often necessarily sample-specific [13, 14], as no validated thresholds have been proposed given trauma burden can vary greatly by sample population and trauma assessment. Following prior work [13, 14], we chose the cut-point (≥ 3 traumas) based on mean trauma count (m = 2.64, SD = 2.2; n = 20,480) among women who completed the 2017 biennial, 2018–2019 supplemental PTSD, and 2020 COVID-19 questionnaires. To test an alternative cut-point that dichotomized “higher” trauma count using a higher threshold, we defined lower trauma as 1–4 traumas and higher trauma as ≥ 5 traumas (21.4% of the analytic sample) in an alternative measure of categorical resilience.
Psychological health was indexed by a combination of distress and positive emotional well-being measures to encompass negative and positive ends of the mental health spectrum. Such a measure recognizes that simply identifying the absence of poor functioning and distress may not signal healthy functioning or emotional well-being per se [15]. Distress was characterized using measures of three forms of distress, including self-reported past-month depressive, anxiety, and PTSD symptoms (Online Resource Table 1) [16–18]. Each distress measure was operationalized in two ways: as dichotomous variables based on established clinical thresholds [16–18] or as continuous severity scores. Positive emotional well-being was characterized using separate measures of three forms of emotional well-being, including life satisfaction, optimism, and purpose (Online Resource Table 1) [19–23]. Notably, anxiety, optimism, and purpose were assessed on the 2017 biennial questionnaire, and thus were reported prior to lifetime trauma reporting. Each emotional well-being measure was operationalized in two ways: as dichotomous variables reflecting higher versus lower levels for each form based on a median cut-off in the sample distribution (i.e., above the median considered higher, at or below the median considered lower) [24, 25] or as continuous sum scores. To assess the robustness of this empirically derived approach, we also conducted sensitivity analyses in which we defined the cut-off for higher versus lower emotional well-being for each form as the top tercile rather than median. We then combined dichotomous measures of distress and positive emotional well-being to define categorical psychological health in three tiers: unfavorable psychological health (meets clinical criteria for depression, anxiety, or PTSD), adequate psychological health (does not meet clinical criteria for depression, anxiety, or PTSD, but shows lower levels in all forms of positive emotional well-being), and favorable psychological health (does not meet clinical criteria for depression, anxiety, or PTSD, and shows higher levels on ≥ 1 forms of positive emotional well-being), similar to prior work [24]. To assess the robustness of our approach, we also conducted sensitivity analyses in which we defined favorable psychological health as meeting criteria for ≥ 2 (rather than 1) forms of positive emotional well-being. Finally, we derived continuous psychological health scores by summing the separate measures of depression, anxiety, and PTSD symptoms using z-scores (reversed, with higher scores representing lower distress) with the separate measures of life satisfaction, optimism, and purpose using z-scores [26, 27]. This continuous measure thereby reflects a spectrum of general distress and positive functioning to broadly capture psychological health, rather than focusing on specific clinical presentations [24].
Pre-pandemic resilience was operationalized by combining trauma burden and psychological health in two ways (Fig. 1), informed by prior approaches which define high resilience as occurring in the context of high trauma burden [28–30]. Categorical resilience was defined by cross-classifying trauma burden (lower versus higher) by psychological health (unfavorable, adequate, and favorable psychological health). This yielded six groups representing a conceptual gradient of psychological resilience across 4 working levels (very high, high, moderate, and low): very high resilience is represented by those with higher trauma burden but favorable psychological health; high resilience is represented by either those with higher trauma burden but adequate psychological health, or those with lower trauma burden and favorable psychological health; moderate resilience is represented by those with lower trauma burden and adequate psychological health; and finally, low resilience is represented by those showing unfavorable psychological health with either higher or lower trauma burden. Continuous resilience was defined by regressing continuous psychological health scores on continuous trauma burden. Standardized residuals from this regression model were used as a continuous resilience measure, with higher values indicating better psychological functioning relative to level of trauma [31, 32].
Outcome: mental health during the COVID-19 pandemic
Mental health early in the pandemic was assessed using four separate measures: three of distress and one of overall positive emotional well-being. Distress measures included self-reported depression, anxiety, and posttraumatic stress symptoms specific to COVID-19-related trauma (Online Resource Table 1) [33–35], defined as either dichotomous variables based on established clinical thresholds or continuous severity scores. Each distress measure was considered as a separate outcome across models. Overall positive emotional well-being was defined both continuously and dichotomously based on self-reported items assessing positive affect, optimism, and purpose in life, each measured with the same 7-point Likert scale response option (see Online Resource Table 1) [20, 36]. Following prior work [37], overall positive emotional well-being was considered as a composite of all these forms of well-being. Continuous overall positive emotional well-being was derived by summing all items, and a dichotomous measure defined the top quartile of the continuous measure as “higher” versus “lower” emotional well-being. Due to the design and timing of COVID-19 questionnaires, women reported psychological symptoms at different times depending on their current healthcare worker status. Women who were not current healthcare workers (n = 11,361, 76.5%) completed all four measures at baseline, while current healthcare workers (n = 3488, 23.5%) completed items assessing depression and anxiety at baseline, posttraumatic stress at the 1 month follow-up, and overall positive emotional well-being at the 3 month follow-up. Comparing current versus not current healthcare workers, early pandemic depression and anxiety did not significantly differ, while posttraumatic stress was lower and overall positive emotional well-being higher among current healthcare workers (Online Resource Table 2).
Covariates
Covariates included age (in years in 2020); race/ethnicity (white or non-white) reported on the 1989 NHS II biennial questionnaire; markers of socio-economic status including parental education attainment (highest completed by either parent: high school graduate, 1–3 years of college, or 4 years of college or greater, missing) reported on the 2005 biennial questionnaire and median household income of residential census tract (in quartiles) for residential locations in 2009; marital status (married, divorced/separated, widowed, single, other/missing) reported on the supplemental PTSD questionnaire; living situation (with others versus alone) reported on the COVID-19 baseline questionnaire; presence of chronic health conditions (history of cancer, stroke, or heart attack) reported on biennial questionnaires through 2017; and current healthcare worker status (current healthcare worker yes/no) reported on the COVID-19 baseline questionnaire.
Data analyses
For descriptive purposes, we first examined the distribution of covariates among the full sample and by categorical resilience groups.
To address our primary hypotheses, we used separate logistic regression models to examine associations between pre-pandemic resilience (separate models considering resilience defined categorically or continuously) and odds of exhibiting clinically elevated symptoms of depression, anxiety, or posttraumatic stress, or high overall emotional well-being during the pandemic, adjusting for all covariates. To determine how each group was functioning relative to those most highly “resilient,” the group with higher trauma and favorable psychological health was used as the referent for categorical resilience models [30]. To provide more-nuanced insight into these relationships, we also used linear regression models to evaluate associations between pre-pandemic resilience (categorical and continuous resilience, separately) and continuous measures for each mental health outcome separately, adjusting for all covariates. For interpretability, we calculated standardized beta estimates by standardizing all continuous variables (i.e., predictors and outcomes). As healthcare workers may be at particularly high risk during the pandemic and timing of assessment for some mental health outcomes differed, we examined effect modification of pre-pandemic resilience by current healthcare worker status in each primary model and conducted follow-up analyses stratifying by current healthcare worker status. Finally, to determine the potential added explanatory value of the combined pre-pandemic resilience definition above and beyond its separate components (i.e., trauma, distress, and emotional well-being), we conducted post hoc analyses comparing the proportion of variance explained by pre-pandemic resilience in primary models described above with that explained by each pre-pandemic resilience component in separate models (Online Resource Methods).
Results
Table 1 presents covariates among the trauma-exposed sample and by levels of pre-pandemic resilience. Women were 66.3 (SD = 4.5) years old on average and a large majority were white (96.0%), with varied levels of parental education attainment. Most women (82.8%) reported living with others and 23.4% were current healthcare workers (of these, 632 reported working in an emergency room, operating room, or intensive care unit, 86 in a dedicated COVID-19 unit, and 30 in a temporary COVID-19 facility).
Table 1.
Distribution of covariates in the analytic sample and by categorical pre-pandemic psychological resilience groups (n = 16,900)
| Pre-pandemic psychological resilience | |||||||
|---|---|---|---|---|---|---|---|
| Full Sample | Higher trauma, unfavorable psych health, n = 2787, 16.5% | Lower trauma, unfavorable psych health, n = 1274, 7.5% | Higher trauma, adequate psych health, n = 1314, 7.8% | Lower trauma, adequate psych health, n = 1026, 6.1% |
Higher trauma, favorable psych health, n = 5132, 30.4% | Lower trauma, favorable psych health, n = 5367, 31.8% | |
| N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | N (%) | |
| Age, mean (SD) | 66.3 (4.5) | 66.0 (4.5) | 65.9 (4.6) | 66.7 (4.4) | 66.3 (4.3) | 66.5 (4.4) | 66.4 (4.5)*** |
| Race/ethnicity | |||||||
| White | 16,217 (96.0) | 2689 (96.5) | 1231 (96.6) | 1261 (96.0) | 984 (95.9) | 5151 (96.0) | 4900 (95.5) |
| Non-White | 501 (3.0) | 74 (2.6) | 30 (2.3) | 42 (3.2) | 27 (2.6) | 159 (3.0) | 170 (3.3) |
| Parental education | |||||||
| High school or less | 7832 (46.3) | 1295 (46.5) | 617 (48.4) | 648 (49.3) | 514 (50.1) | 2396 (44.6) | 2368 (46.1)** |
| 1–3 Years of college | 3931 (23.3) | 640 (23.0) | 292 (22.9) | 285 (21.7) | 229 (22.3) | 1295 (24.1) | 1187 (23.1) |
| 4 Years of college plus | 4105 (24.3) | 205 (7.3) | 77 (6.0) | 93 (7.1) | 50 (4.9) | 334 (6.2) | 276 (5.4) |
| Median household income | |||||||
| Quartile 1 | 4215 (24.9) | 780 (28.0) | 321 (25.2) | 339 (25.8) | 240 (23.4) | 1343 (25.0) | 1187 (23.1)** |
| Quartile 2 | 4209 (24.9) | 708 (25.4) | 326 (25.6) | 359 (27.3) | 254 (24.8) | 1316 (24.5) | 1245 (24.3) |
| Quartile 3 | 4248 (25.1) | 679 (24.4) | 312 (24.5) | 324 (24.7) | 276 (26.9) | 1,343 (25.0) | 1321 (25.7) |
| Quartile 4 | 4,200 (24.9) | 617 (22.1) | 311 (24.4) | 289 (22.0) | 253 (24.7) | 1356 (25.3) | 1371 (26.7) |
| Marital status | |||||||
| Married | 12,718 (75.3) | 1837 (65.9) | 878 (68.9) | 901 (68.5) | 722 (70.4) | 4186 (78.0) | 4198 (81.8)*** |
| Separated/divorced | 2132 (12.6) | 528 (18.9) | 174 (13.7) | 209 (15.9) | 135 (13.2) | 640 (11.9) | 446 (8.7) |
| Widowed | 1109 (6.6) | 223 (8.0) | 117 (9.2) | 108 (8.2) | 79 (7.7) | 321 (6.0) | 262 (5.1) |
| Single | 838 (5.0) | 176 (6.3) | 99 (7.7) | 84 (6.4) | 84 (8.2) | 192 (3.6) | 198 (3.9) |
| Any chronic conditions | 2450 (14.5) | 461 (16.5) | 158 (12.4) | 222 (16.9) | 113 (11.1) | 859 (16.0) | 633 (12.3)*** |
| Living arrangement | |||||||
| With others | 13,991 (82.8) | 2127 (76.3) | 984 (77.2) | 1023 (77.9) | 826 (80.5) | 4578 (85.3) | 4450 (86.7)*** |
| Alone | 2601 (15.4) | 587 (21.1) | 262 (20.6) | 255 (19.4) | 173 (16.8) | 699 (13.0) | 628 (12.2) |
| Current healthcare worker | 3962 (23.4) | 599 (21.5) | 266 (20.9) | 336 (25.6) | 262 (25.5) | 1315 (24.5) | 1203 (23.4) |
All variables besides age are standardized to the age distribution of the study population. Values of polytomous variables may not sum to 100% due to rounding. Missingness was 1.1% for race/ethnicity, 6.1% for parental education, 0.2% for median census tract household income, 0.6% for marital status, and 1.8% for living arrangement
***p < 0.0001, **p < 0.01, *p < 0.05, +p < 0.10 for ANOVA or Χ2 tests of homogeneity
Among the sample, 44.0% had reported relatively lower levels (1–2 trauma types) and 56.0% had higher levels (≥ 3 trauma types) of lifetime trauma burden before the pandemic. Regarding pre-pandemic psychological health, 24.0% of the sample were considered to have unfavorable psychological health, 13.9% to have adequate psychological health, and 62.1% to have favorable psychological health. Among women with favorable psychological health, 43.3% were high on one, 48.9% were high on two, and 7.8% were high on all three forms of positive emotional well-being. Those showing highest resilience per our definition (higher trauma burden but favorable psychological health) represented 30.4% of the sample.
Covariate distribution across pre-pandemic resilience categories is presented in Table 1. Distributions of age, parental education, median census tract household income, marital status, and chronic conditions significantly differed across pre-pandemic resilience categories. Higher parental education, higher median household income, and being married were associated with more favorable psychological health, largely regardless of trauma burden, whereas having chronic conditions was associated with higher trauma burden, mostly regardless of psychological health.
Regarding mental health outcomes early in the pandemic, 10.3% of the sample met clinical criteria for depression, 16.7% for anxiety, and 15.5% for posttraumatic stress, and these distress symptoms were positively correlated (rdepression-anxiety = 0.64, rdepression-posttraumatic stress = 0.49, ranxiety-posttraumatic stress = 0.54). Overall positive emotional well-being scores had a mean of 35.7 (SD = 7.5) and were negatively correlated with distress symptoms (rwell-being-depression = – 0.58, rwell-being-anxiety = – 0.46, rwell-being-posttraumatic stress = − 0.45).
Pre-pandemic resilience and mental health outcomes during the pandemic
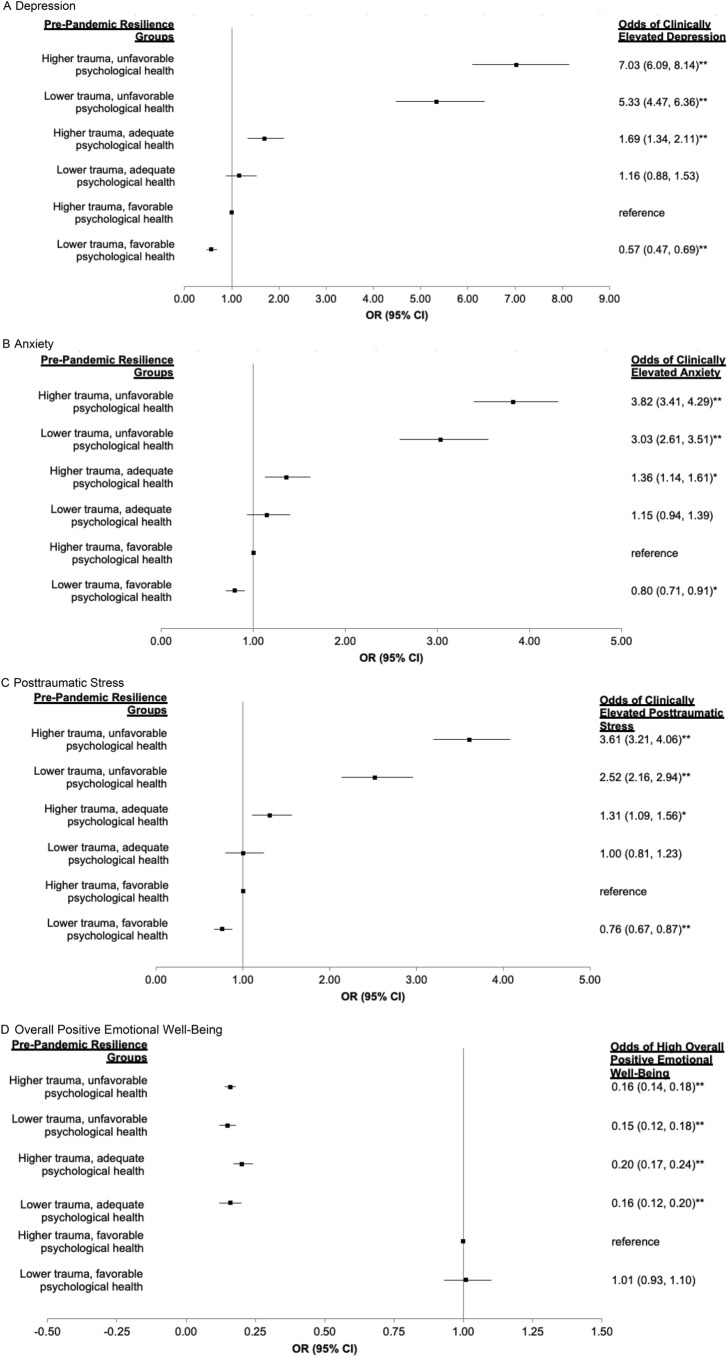
Categorical pre-pandemic resilience status was associated with clinically elevated distress early in the pandemic in hypothesized directions (Fig. 2; Online Resource Table 3). Resilience categories were associated in a graded fashion with depression, anxiety, and posttraumatic stress outcomes during the pandemic; groups exhibiting less pre-pandemic resilience showed increased odds of distress compared to the highest resilience reference group. For example, odds of depression early in the pandemic were increased across the following groups, relative to the highest resilience group: ORs ranged from 1.16 (95%CI 0.88–1.53) to 1.69 (95%CI 1.34–2.11) for higher resilience, OR = 5.33 (95%CI 4.47–6.36) for moderate resilience, and OR = 7.03 (95%CI 6.09–8.14) for lowest resilience. With respect to the overall positive emotional well-being outcome during the pandemic, higher pre-pandemic resilience was generally associated with higher well-being; however, prior trauma burden largely did not influence associations. For example, associations were almost identical for women reporting either lower trauma OR = 0.15 (95%CI 0.12–0.18) and higher trauma OR = 0.16 (95%CI 0.14–0.18) with unfavorable psychological health, relative to the highest resilience group. Patterns were largely consistent when examining associations between categorical resilience and continuous mental health outcomes during the pandemic (Table 2).
Fig. 2.
Odds ratios for pre-pandemic psychological resilience in relation to lifetime trauma on categorical mental health outcomes amid the COVID-19 pandemic. **< 0.0001, * < 0.05; adjusted for age, race/ethnicity, parental education, census tract household income, marital status, chronic conditions, living arrangement, and current healthcare worker status. Categorical mental health outcomes: clinically elevated depression (Patient Health Questionnaire PHQ-2 sum score ≥ 3), anxiety (Generalized Anxiety Disorder GAD-2 sum score ≥ 3), and posttraumatic stress (adapted Impact of Events Scale-6 item IES-6; mean scores ≥ 1.75); and high overall positive emotional well-being (top quartile of positive emotional well-being scores)
Table 2.
Standardized effect estimates of pre-pandemic psychological resilience (considered as a categorical and as a continuous measure) as a predictor of continuous mental health outcomes early in the COVID-19 pandemic
| N (%) | β (95% CI) | ||||
|---|---|---|---|---|---|
| Depressive symptoms | Anxiety symptoms | Posttraumatic stress symptoms | Overall positive emotional well-being | ||
| Categorical pre-pandemic resilience | |||||
| A. Higher trauma, unfavorable psych health | 2787 (16.5) | 0.98 (0.94, 1.03)** | 0.76 (0.72, 0.81)** | 0.70 (0.66, 0.74)** | – 1.07 (– 1.11, – 1.03)** |
| B. Lower trauma, unfavorable psych health | 1274 (7.5) | 0.82 (0.76, 0.88)** | 0.64 (0.58, 0.70)** | 0.50 (0.44, 0.56)** | – 1.02 (– 1.07, – 0.96)** |
| C. Higher trauma, adequate psych health | 1314 (7.8) | 0.28 (0.23, 0.34)** | 0.19 (0.14, 0.25)** | 0.14 (0.08, 0.20)** | – 0.71 (– 0.77, – 0.66)** |
| D. Lower trauma, adequate psych health | 1026 (6.1) | 0.17 (0.11, 0.24)** | 0.09 (0.03, 0.16)* | 0.02 (– 0.04, 0.09) | – 0.72 (– 0.78, – 0.66)** |
| E. Higher trauma, favorable psych health | 5132 (30.4) | ref | ref | ref | ref |
| F. Lower trauma, favorable psych health | 5367 (31.8) | – 0.10 (– 0.13, – 0.06)** | – 0.09 (– 0.13, – 0.05)** | – 0.10 (– 0.14, – 0.07)** | 0.01 (– 0.02, 0.04) |
| Continuous pre-pandemic resilience | |||||
| Relative psychological resilience | – 0.46 (– 0.47, – 0.44)** | – 0.36 (– 0.38, – 0.35)** | – 0.32 (– 0.33, – 0.30)** | 0.57 (0.56, 0.58)** | |
** < 0.0001, * < 0.05; adjusted for age, race/ethnicity, parental education, census tract household income, marital status, chronic conditions, living arrangement, current healthcare worker status; Betas are standardized and separate models were conducted for each resilience measure (i.e., categorical and continuous resilience) with each outcome
Like findings with categorical resilience, continuous pre-pandemic resilience was significantly associated with all mental health measures early in the pandemic in expected directions (Table 2, Online Resource Table 3). Greater continuous pre-pandemic resilience was consistently associated with lower distress across measures, most strongly with depression (β = – 0.46, 95%CI – 0.47– – 0.44), followed by anxiety (β = – 0.36, 95%CI – 0.38, – 0.35) and posttraumatic stress (β = – 0.32, 95%CI – 0.33, – 0.30) symptoms. Greater continuous pre-pandemic resilience was also associated with higher overall positive emotional well-being early in the pandemic (β = 0.57, 95%CI 0.56– 0.58), to an even greater opposite magnitude than associations with distress.
Sensitivity analyses examining the robustness of a priori criteria for defining pre-pandemic resilience are presented in Online Resource Table 4, indicating generally consistent findings across methodological decisions, e.g., when using a higher threshold cut-point for “higher trauma” (≥ 5 traumatic event types), when varying criteria for the cut-off for pre-pandemic positive emotional well-being across the three forms (top tercile), or characterizing pre-pandemic positive emotional well-being according to the three forms that were assessed (≥ 2 forms). There was limited evidence of effect modification by current healthcare worker status; the only statistically significant interactions between continuous resilience and healthcare worker status were found for anxiety symptoms (β = – 0.04, 95%CI – 0.07, 0.00, p = 0.04) and overall positive emotional well-being (β = 0.06, 95%CI 0.04, 0.10, p < 0.0001) during the pandemic. Interactions suggested that continuous resilience was more protective against subsequent anxiety, and more promotive of higher subsequent overall positive emotional well-being among current versus not current healthcare workers. In stratified models, associations between categorical and continuous pre-pandemic resilience with continuous mental health outcomes during the pandemic were strikingly similar across healthcare worker status (Online Resource Table 5).
Finally, in post hoc analyses examining the proportion of variance explained by each resilience component versus categorical resilience, pre-pandemic dichotomous distress (meeting clinical criteria vs not) accounted for most variance in pandemic mental health outcomes, followed by dichotomous positive emotional well-being (higher vs lower), and then by dichotomous trauma exposure (higher vs lower) (Online Resource Results and Table 6). Composite categorical resilience explained nominally more variance than dichotomous positive emotional well-being and distress alone. This is consistent with the main findings in which, across all three distress-related mental health outcomes, the biggest difference in odds ratios was observed when contrasting groups according to prior psychological health, although considering whether groups differed by trauma burden was also informative. Distinguishing groups primarily by pre-pandemic trauma burden largely did not provide insight into overall positive emotional well-being during the pandemic.
Discussion
The stress-sensitization model posits that exposure to stressful life events primes individuals for heightened risk of developing mental health symptoms in the context of future stressors [1, 37, 38]. Here, we extend the stress-sensitization model by considering not only stressful life events as a priming exposure for future adaptation, but also psychological health following that exposure. This study leveraged prospective data from almost 17,000 older-adult women in an established cohort followed prior to and during the COVID-19 pandemic to examine the relationship between pre-pandemic resilience to lifetime trauma and mental health responses during the pandemic. Using two empirical definitions of resilience informed by previous literature, we observed converging evidence that among trauma-exposed women, pre-pandemic psychological resilience—evidenced by more favorable psychological health despite such exposure—was associated with healthier mental health outcomes early in the pandemic, including lower depressive, anxiety, and posttraumatic stress symptoms, and higher overall positive emotional well-being. The size of these associations is notable, with up to three-to-seven-fold lower odds of depression, anxiety, and posttraumatic stress and eightfold higher odds of elevated overall positive emotional well-being among women who demonstrated pre-pandemic resilience. Of note, psychological health measures used to classify pre-pandemic resilience, though distinct, were similar to mental health outcomes assessed in the pandemic, and thus, one would expect pre-pandemic psychological health to generally correlate with later mental health. However, we were particularly interested in how prior lifetime trauma might impact mental health amid the pandemic, which is a significant disruption, influencing what we could otherwise expect as a natural trajectory of psychological functioning.
Several explanations for our results are possible. First, as psychological resilience is influenced by multiple intrapersonal and contextual assets [39], individuals with earlier access to protective resources may also draw on these resources to face future stressors. For example, women showing pre-pandemic resilience to trauma may have used coping skills and/or had socio-economic or other assets to maintain favorable psychological health despite elevated trauma exposure, which may also help protect mental health against challenges such as the pandemic [40, 41]. Second, some individuals may have an underlying resistance to psychopathology that explains both past and future mental health. Indeed, a prior longitudinal study observed that individuals who did not develop PTSD after a trauma were unlikely to develop it after exposure to subsequent trauma [5]. Third, restoring adequate or favorable levels of psychological health following initial trauma may create conditions for future adaptive coping and better mental health, increasing the likelihood of a more resilient trajectory and potentially mitigating otherwise more pronounced negative mental health responses under future stress. To this end, individual- and structural-level efforts to support mental health following trauma (e.g., financial assistance, psychological support) may have the potential to interrupt a cycle of distress in trauma-exposed individuals and promote better adjustment to future stressors, which could reduce the impact of future disasters and therefore improve or bolster population mental health.
Our findings nonetheless suggest that preventing trauma exposure should remain a priority for ensuring optimal mental health. Although promising that prior psychological resilience seems to confer protection against poor mental health sequelae amid later stress, there may be some residual effects of trauma that cannot be fully mitigated. Compared to women showing the highest levels of pre-pandemic resilience to trauma, women with relatively lower levels of lifetime trauma who also had favorable psychological health showed even healthier psychological responses during the pandemic. This is consistent with most research, whereby prior trauma tends to predict poorer responses to later trauma. For example, a prospective study of 1,160 Chilean adults found that more prior lifetime stressors predicted higher odds of developing PTSD or major depression after subsequent exposure to a disaster [9].
Our study offers numerous strengths, including its prospective design in a large, well-characterized cohort of women, many of whom were at heightened risk for distress by virtue of being healthcare workers during the pandemic. We also move beyond confirming the negative impacts of the COVID-19 pandemic on mental health to examine the extent to which even vulnerable groups such as trauma-exposed individuals may be protected from poor mental health. Moreover, we utilize a nuanced definition of resilience that is not defined solely by the absence of psychopathology [11, 42, 43]. Rather, we also accounted for the presence of positive functioning by considering positive emotional well-being assessed according to both subjective (e.g., life satisfaction) and eudaimonic (e.g., meaning and purpose) aspects of well-being. Furthermore, our sensitivity analyses suggest that integrating trauma exposure and pre-pandemic psychological health simultaneously into a single resilience measure could provide greater explanatory value. We were able to move beyond a sole focus on psychiatric morbidity and adverse outcomes during the COVID-19 pandemic to also assess overall positive emotional well-being as an outcome. Assessing positive emotional well-being can provide insight into coping and general functioning during the pandemic [44], but has received relatively limited attention. Only individuals with pre-pandemic favorable mental health (including positive emotional well-being) showed high levels of overall positive emotional well-being during the pandemic, whereas those with unfavorable or even adequate pre-pandemic mental health reported lower levels of emotional well-being. This suggests that positive emotional well-being may be relatively stable even in the face of a stressor, consistent with prior literature on the stability of optimism and other psychological attributes [45, 46].
This study has several limitations to note. Trauma information used to classify pre-pandemic resilience was indexed to the number of traumatic event types; while this is a reasonable proxy of trauma burden and complexity, we could not incorporate information about specific events, some of which may have been severe even if isolated. We additionally lacked information on whether traumatic events were experienced multiple times and on the severity of specific events, and thus, the trauma burden variable may not fully capture the complexity of trauma experience. Similarly, we considered the pandemic as a universal stressor, but there was likely wide variation in how individuals were impacted by the pandemic. Moreover, lifetime trauma was retrospectively reported by participants who were, on average, approximately 64 years old at the time of assessment. It is possible recall bias might have influenced reporting and reports of trauma may also be influenced by concurrent psychological status, though retrospective recall on life events is generally reliable [47]. We adjusted for a range of confounders that may influence pandemic impact (e.g., healthcare worker status, socio-economic factors), but more work examining experiences of COVID-19 is needed to explore coping and adjustment at a granular level. Additionally, pre-pandemic anxiety, optimism, and purpose were queried in 2017 and lifetime trauma was reported in 2018–2019, so traumas post-2017 may have been captured. Unfortunately, women did not report timing of all traumas, and thus, there may have been lack of temporal ordering regarding trauma and some aspects of distress and well-being in the resilience definition. For example, the lack of temporality may have resulted in misclassification (e.g., higher positive well-being in 2017, but experienced and reported a trauma in 2018, thus misclassified as having higher trauma plus more favorable psychological functioning). To define categorical pre-pandemic resilience, we used established cut-offs for the presence of clinically elevated depression, anxiety, and PTSD, but such cut-offs have not been established for trauma burden or positive emotional well-being measures. Therefore, we used rational methods (e.g., mean or median split) to divide individuals into higher versus lower levels within each measure. Of note, it is encouraging that results were robust when considering different cut-offs for each form of positive emotional well-being and trauma burden. Pre-pandemic psychological health was only assessed at one time point, potentially resulting in misclassification as psychological health is dynamic over time. There has been attrition in NHS II over time, and women who participated in all questionnaires required for the current study may differ (e.g., be healthier) from those lost to follow-up. Generalizability may be limited, as our sample was largely white, older, professional women who were motivated for health-oriented research. Perhaps surprisingly, given high rates of burnout among healthcare workers [48], current healthcare workers in our sample showed largely comparable mental health outcomes to women who were previously healthcare workers (but were not practicing during the pandemic). As noted, there were slight differences in timing of assessment by healthcare worker status, which could have influenced mental health. Despite these differences in assessment timing, associations between pre-pandemic resilience and mental health amid the pandemic were largely similar across current versus non-current healthcare workers.
In conclusion, drawing on longitudinal data from almost 17,000 women with detailed mental health data before and after the onset of the COVID-19 pandemic, we found converging evidence that pre-pandemic psychological resilience, as well as lower lifetime trauma burden with favorable psychological health, were associated with better mental health outcomes early in the pandemic. Findings were evident among both frontline and prior healthcare workers in the initial phases of the pandemic, during a time of great uncertainty. Our study has important implications for interventions to support the mental health of individuals with prior trauma histories before and during a highly stressful event such as the pandemic. Future studies should examine how psychological resilience may predict physical health and other long-term outcomes of the pandemic. Promoting mental health and recovery among individuals following trauma is important in its own right. However, it may also yield additional health dividends as a strategy for reducing risk and protecting enduring mental health in the face of future stressors.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
The authors would like to acknowledge the Channing Division of Network Medicine, Department of Medicine, Brigham and Women’s Hospital, and Harvard Medical School for managing the NHS II. Data and/or research tools used in the preparation of this manuscript were submitted to the National Institute of Mental Health (NIMH) Data Archive (NDA). NDA is a collaborative informatics system created by the National Institutes of Health to provide a national resource to support and accelerate research in mental health. Dataset identifier(s): 10.15.154/1522870. This manuscript reflects the views of the authors and may not reflect the opinions or views of the NIH or of the Submitters submitting original data to NDA.
Author contributions
All authors contributed to the study conception and design. Material preparation and data analysis were performed by KN. The first draft of the manuscript was written by KC and KN, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by the National Institutes of Health (NHS II infrastructure, U01 CA176726), National Institute of Mental Health (KCK and LDK, R01MH101269), National Institute of Mental Health (KCK, R01MH078928), Department of Defense (LDK, W81XWH-17–1-0153), and Harvard TH Chan School of Public Health Dean’s Fund for Scientific Advancement (KCK and LDK, COVID-19, Social Unrest, and Health in the Harvard Cohorts). KWC was supported in part by a NARSAD Young Investigator Grant from the Brain & Behavior Research Foundation and funding from the National Institute of Mental Health (K08MH127413). KN was supported by the National Institute of Mental Health (T32 MH017119-33) and the Department of Veterans Affairs Office of Academic Affiliations Advanced Fellowship Program in Mental Illness Research and Treatment, the Medical Research Service of the SFVAHCS, and the Department of Veterans Affairs Sierra-Pacific Mental Illness Research, Education, and Clinical Center (MIRECC). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or the Department of Veterans Affairs. The authors have no competing interests to declare that are relevant to the content of this article.
Declarations
Ethical approval and consent to participate
The study was approved by the Partners Healthcare Human Research Committee and return of questionnaires implied consent, and was conducted in compliance with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Footnotes
Karmel W. Choi and Kristen Nishimi have contributed equally as co-first authors.
Contributor Information
Karmel W. Choi, Email: kwchoi@mgh.harvard.edu
Kristen Nishimi, Email: kristen.nishimi@ucsf.edu.
References
- 1.McLaughlin KA, Conron KJ, Koenen KC, Gilman SE. Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: a test of the stress sensitization hypothesis in a population-based sample of adults. Psychol Med. 2010;40(10):1647–1658. doi: 10.1017/S0033291709992121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bandoli G, Campbell-Sills L, Kessler RC, Heeringa SG, Nock MK, Rosellini AJ, Sampson NA, Schoenbaum M, Ursano RJ, Stein MB. Childhood adversity, adult stress, and the risk of major depression or generalized anxiety disorder in US soldiers: a test of the stress sensitization hypothesis. Psychol Med. 2017;47(13):2379–2392. doi: 10.1017/S0033291717001064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hammen C, Henry R, Daley SE. Depression and sensitization to stressors among young women as a function of childhood adversity. J Consult Clin Psychol. 2000;68(5):782–787. doi: 10.1037//0022-006X.68.5.782. [DOI] [PubMed] [Google Scholar]
- 4.Twenge JM, Joiner TE. US Census Bureau-assessed prevalence of anxiety and depressive symptoms in 2019 and during the 2020 COVID-19 pandemic. Depress Anxiety. 2020;37(10):954–956. doi: 10.1002/da.23077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Breslau N, Chilcoat HD, Kessler RC, Davis GC. Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit Area Survey of Trauma. Am J Psychiatry. 1999;156(6):902–907. doi: 10.1176/ajp.156.6.902. [DOI] [PubMed] [Google Scholar]
- 6.Luthar SS, Cicchetti D, Becker B. The construct of resilience: a critical evaluation and guidelines for future work. Child Dev. 2000;71(3):543–562. doi: 10.1111/1467-8624.00164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bonanno GA, Diminich ED. Annual Research Review: Positive adjustment to adversity–trajectories of minimal-impact resilience and emergent resilience. J Child Psychol Psychiatry. 2013;54(4):378–401. doi: 10.1111/jcpp.12021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Snijders C, Pries L-K, Sgammeglia N, Al Jowf G, Youssef NA, de Nijs L, Guloksuz S, Rutten BPF. Resilience against traumatic stress: current developments and future directions. Front Psychiatry. 2018;9:676. doi: 10.3389/fpsyt.2018.00676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fernandez CA, Choi KW, Marshall BD, Vicente B, Saldivia S, Kohn R, Koenen KC, Arheart KL, Buka SL. Assessing the relationship between psychosocial stressors and psychiatric resilience among Chilean disaster survivors. Br J Psychiatry. 2020;217(5):630–637. doi: 10.1192/bjp.2020.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sampson L, Jha SC, Roberts AL, Lawn RB, Nishimi KM, Ratanatharathorn A, Sumner JA, Kang JH, Kubzansky LD, Rimm EB, Koenen KC. Trauma, post-traumatic stress disorder, and treatment among middle-aged and older women in the Nurses’ Health Study II. Am J Geriatr Psychiatry. 2022;30(5):588–602. doi: 10.1016/j.jagp.2021.10.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choi KW, Stein MB, Dunn EC, Koenen KC, Smoller JW. Genomics and psychological resilience: a research agenda. Mol Psychiatry. 2019;24(12):1770–1778. doi: 10.1038/s41380-019-0457-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schnurr P, Vielhauer M, Weathers F, Findler M (1999) The Brief Trauma Questionnaire (BTQ) [Measurement instrument]. Available from http://www.ptsd.va.gov.
- 13.Kaspersen M, Matthiesen SB, Götestam KG. Social network as a moderator in the relation between trauma exposure and trauma reaction: A survey among UN soldiers and relief workers. Scand J Psychol. 2003;44(5):415–423. doi: 10.1046/j.1467-9450.2003.00362.x. [DOI] [PubMed] [Google Scholar]
- 14.Moore TM, Risbrough VB, Baker DG, Larson GE, Glenn DE, Nievergelt CM, Maihofer A, Port AM, Jackson CT, Ruparel K, Gur RC. Effects of military service and deployment on clinical symptomatology: The role of trauma exposure and social support. J Psychiatr Res. 2017;95:121–128. doi: 10.1016/j.jpsychires.2017.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kubzansky LD, Segerstrom SC, Boehm JK. Positive psychological functioning and the biology of health. Soc Personal Psychol Compass. 2015;9(12):645–660. doi: 10.1111/spc3.12224. [DOI] [Google Scholar]
- 16.Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10(2):77–84. doi: 10.1016/S0749-3797(18)30622-6. [DOI] [PubMed] [Google Scholar]
- 17.Blevins CA, Weathers FW, Davis MT, Witte TK, Domino JL. The posttraumatic stress disorder Checklist for DSM-5 (PCL-5): development and initial psychometric evaluation. J Trauma Stress. 2015;28(6):489–498. doi: 10.1002/jts.22059. [DOI] [PubMed] [Google Scholar]
- 18.Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–1097. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 19.Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. J Pers Assess. 1985;49(1):71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- 20.Feller SC, Castillo EG, Greenberg JM, Abascal P, Van Horn R, Wells KB, University of California, Los Angeles Community Translational Science Team Emotional well-being and public health: proposal for a model national initiative. Public Health Rep. 2018;133(2):136–141. doi: 10.1177/0033354918754540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Keyes CL, Shmotkin D, Ryff CD. Optimizing well-being: the empirical encounter of two traditions. J Pers Soc Psychol. 2002;82(6):1007–1022. doi: 10.1037/0022-3514.82.6.1007. [DOI] [PubMed] [Google Scholar]
- 22.Ryff CD, Keyes CL. The structure of psychological well-being revisited. J Soc Psychol. 1995;69(4):719–727. doi: 10.1037//0022-3514.69.4.719. [DOI] [PubMed] [Google Scholar]
- 23.Scheier MF, Carver CS, Bridges MW. Distinguishing optimism from neuroticism (and trait anxiety, self-mastery, and self-esteem): A reevaluation of the Life Orientation Test. J Pers Soc Psychol. 1994;67(6):1063–1078. doi: 10.1037//0022-3514.67.6.1063. [DOI] [PubMed] [Google Scholar]
- 24.Keyes CL. The mental health continuum: from languishing to flourishing in life. J Health Soc Behav. 2002;43(2):207–222. doi: 10.2307/3090197. [DOI] [PubMed] [Google Scholar]
- 25.Keyes CL, Simoes EJ. To flourish or not: positive mental health and all-cause mortality. Am J Public Health. 2012;102(11):2164–2172. doi: 10.2105/AJPH.2012.300918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Pimple P, Lima BB, Hammadah M, Wilmot K, Ramadan R, Levantsevych O, Sullivan S, Kim JH, Kaseer B, Shah AJ, Ward L, Raggi P, Bremner JD, Hanfelt J, Lewis T, Quyyumi AA, Vaccarino V. Psychological distress and subsequent cardiovascular events in individuals with coronary artery disease. J Am Heart Assoc. 2019;8(9):e011866. doi: 10.1161/JAHA.118.011866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Winefield HR, Gill TK, Taylor AW, Pilkington RM. Psychological well-being and psychological distress: is it necessary to measure both? Psychol Well- Theory Res Pract. 2012;2(1):1–14. doi: 10.1186/2211-1522-2-3. [DOI] [Google Scholar]
- 28.Masten AS, Burt KB, Roisman GI, Obradovic J, Long JD, Tellegen A. Resources and resilience in the transition to adulthood: continuity and change. Dev Psychopathol. 2004;16(4):1071–1094. doi: 10.1017/s0954579404040143. [DOI] [PubMed] [Google Scholar]
- 29.Jung SJ, Jeon YJ, Choi KW, Yang JS, Chae J-H, Koenen KC, Kim HC. Correlates of psychological resilience and risk: Prospective associations of self-reported and relative resilience with Connor-Davidson resilience scale, heart rate variability, and mental health indices. Brain Behav. 2021;11(5):e02091. doi: 10.1002/brb3.2091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Nishimi KM, Koenen KC, Coull BA, Chen R, Kubzansky LD. Psychological resilience predicting cardiometabolic conditions in adulthood in the Midlife in the United States Study. Proc Natl Acad Sci. 2021;118(32):e2102619118. doi: 10.1073/pnas.2102619118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Amstadter AB, Maes HH, Sheerin CM, Myers JM, Kendler KS. The relationship between genetic and environmental influences on resilience and on common internalizing and externalizing psychiatric disorders. Soc Psychiatry Psychiatr Epidemiol. 2016;51(5):669–678. doi: 10.1007/s00127-015-1163-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sheerin CM, Lind MJ, Brown EA, Gardner CO, Kendler KS, Amstadter AB. The impact of resilience and subsequent stressful life events on MDD and GAD. Depress Anxiety. 2018;35(2):140–147. doi: 10.1002/da.22700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kroenke K, Spitzer RL, Williams JB. The Patient Health Questionnaire-2: validity of a two-item depression screener. Med Care. 2003;41(11):1284–1292. doi: 10.1097/01.MLR.0000093487.78664.3C. [DOI] [PubMed] [Google Scholar]
- 34.Kroenke K, Spitzer RL, Williams JB, Monahan PO, Löwe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. 2007;146(5):317–325. doi: 10.7326/0003-4819-146-5-200703060-00004. [DOI] [PubMed] [Google Scholar]
- 35.Thoresen S, Tambs K, Hussain A, Heir T, Johansen VA, Bisson JI. Brief measure of posttraumatic stress reactions: Impact of Event Scale-6. Soc Psychiatry Psychiatr Epidemiol. 2010;45(3):405–412. doi: 10.1007/s00127-009-0073-x. [DOI] [PubMed] [Google Scholar]
- 36.VanderWeele TJ, Trudel-Fitzgerald C, Allin P, Farrelly C, Fletcher G, Frederick DE, Hall J, Helliwell JF, Kim ES, Lauinger WA, Lee MT, Lyubomirsky S, Margolis S, McNeely E, Messer N, Tay L, Viswanath V, Węziak-Białowolska D, Kubzansky LD. Current recommendations on the selection of measures for well-being. Prev Med. 2020;133:106004. doi: 10.1016/j.ypmed.2020.106004. [DOI] [PubMed] [Google Scholar]
- 37.Smid GE, Kleber RJ, Rademaker AR, van Zuiden M, Vermetten E. The role of stress sensitization in progression of posttraumatic distress following deployment. Soc Psychiatry Psychiatr Epidemiol. 2013;48(11):1743–1754. doi: 10.1007/s00127-013-0709-8. [DOI] [PubMed] [Google Scholar]
- 38.Nurius PS, Uehara E, Zatzick DF. Intersection of stress, social disadvantage, and life course processes: reframing trauma and mental health. Am J Psychiatr Rehabil. 2013;16(2):91–114. doi: 10.1080/15487768.2013.789688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ungar M. Resilience, trauma, context, and culture. Trauma Violence Abuse. 2013;14(3):255–266. doi: 10.1177/1524838013487805. [DOI] [PubMed] [Google Scholar]
- 40.Lock S, Rubin GJ, Murray V, Rogers MB, Amlôt R, Williams R. Secondary stressors and extreme events and disasters: a systematic review of primary research from 2010–2011. PLoS Curr. 2012 doi: 10.1371/currents.dis.a9b76fed1b2dd5c5bfcfc13c87a2f24f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lowe SR, Kwok RK, Payne J, Engel LS, Galea S, Sandler DP. Why does disaster recovery work influence mental health?: pathways through physical health and household income. Am J Community Psychol. 2016;58(3–4):354–364. doi: 10.1002/ajcp.12091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Almedom AM, Glandon D. Resilience is not the absence of PTSD any more than health is the absence of disease. J Loss Trauma. 2007;12(2):127–143. doi: 10.1080/15325020600945962. [DOI] [Google Scholar]
- 43.Southwick SM, Bonanno GA, Masten AS, Panter-Brick C, Yehuda R. Resilience definitions, theory, and challenges: interdisciplinary perspectives. Eur J Psychotraumatol. 2014;5(1):25338. doi: 10.3402/ejpt.v5.25338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Waters L, Algoe SB, Dutton J, Emmons R, Fredrickson BL, Heaphy E, Moskowitz JT, Neff K, Niemiec R, Pury C, Steger M. Positive psychology in a pandemic: buffering, bolstering, and building mental health. J Posit Psychol. 2021 doi: 10.1080/17439760.2021.1871945. [DOI] [Google Scholar]
- 45.Schou I, Ekeberg Ø, Sandvik L, Ruland CM. Stability in optimism-pessimism in relation to bad news: a study of women with breast cancer. J Pers Assess. 2005;84(2):148–154. doi: 10.1207/s15327752jpa8402_04. [DOI] [PubMed] [Google Scholar]
- 46.Fujita F, Diener E. Life satisfaction set point: stability and change. J Pers Soc Psychol. 2005;88(1):158–164. doi: 10.1037/0022-3514.88.1.158. [DOI] [PubMed] [Google Scholar]
- 47.Jivraj S, Goodman A, Ploubidis GB, de Oliveira C. Testing comparability between retrospective life history data and prospective birth cohort study data. J Gerontol Series B. 2020;75(1):207–217. doi: 10.1093/geronb/gbx042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Morgantini LA, Naha U, Wang H, Francavilla S, Acar Ö, Flores JM, Crivellaro S, Daniel Moreira D, Abern M, Eklund M, Vigneswaran HT, Weine SM. Factors contributing to healthcare professional burnout during the COVID-19 pandemic: A rapid turnaround global survey. PLoS ONE. 2020;15(9):e0238217. doi: 10.1371/journal.pone.0238217. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.