Abstract
Objective
The objective of this review was to identify barriers and facilitators related to self-management from the perspectives of people with shoulder pain and clinicians involved in their care.
Data sources
CINAHL, MEDLINE, PsycINFO, SPORTDiscus, Embase, ProQuest Health, Web of Science, and Scopus were searched from inception to March 2022.
Review methods
A meta-aggregative approach to the synthesis of qualitative evidence was used. Two independent reviewers identified eligible articles, extracted the data, and conducted a critical appraisal. Two reviewers independently identified and developed categories, with validation by two further researchers. Categories were discussed among the wider research team and a comprehensive set of synthesized findings was derived.
Results
Twenty studies were included. From the perspective of patients, three synthesized findings were identified that influenced self-management: (1) support for self-management, including subthemes related to patient-centred support, knowledge, time, access to equipment, and patient digital literacy; (2) personal factors, including patient beliefs, patient expectations, patient motivation, pain, and therapeutic response; and (3) external factors, including influence of the clinician and therapeutic approach. From the perspective of clinicians, two synthesized findings were identified that influenced self-management: (1) support for self-management, including education, patient-centred support, patient empowerment, time, and clinician digital literacy; and (2) preferred management approach, including clinician beliefs, expectations, motivation, therapeutic approach, and therapeutic response.
Conclusion
The key barriers and facilitators were patient-centred support, patient beliefs, clinician beliefs, pain, and therapeutic response. Most of the included studies focused on exercise-based rehabilitation, and therefore might not fully represent barriers and facilitators to broader self-management.
Keywords: Shoulder pain, self-management, qualitative synthesis, systematic review
Introduction
The current management of the majority of shoulder pain presentations is varied and inconsistent, with little standardization of best practice.1,2 While there are clinical guidelines to inform practice,3,4 the optimal treatment for these shoulder pain presentations is unknown. 5 Several systematic reviews have been conducted to identify the most effective treatment for these conditions.5–7 At best, the results of these reviews indicate only short-term benefits for different treatments, over no treatment or placebo. The research to date suggests that shoulder pain is resistant to treatment and possibly recurrent in nature. 8 Therefore, self-management programmes that equip patients with the necessary tools to manage their condition on an ongoing basis may assist them in maximizing their quality of life in the longer term.
Self-management programmes for shoulder pain have produced similar findings to clinician-led interventions for the treatment of several shoulder conditions.9–11 However, similar to clinician-led interventions, self-management programmes tend to show only short-term benefits.9,10,12 A reason for limited success with self-management may be poor patient engagement with the programme.
To identify the barriers and facilitators that may influence patient engagement with self-management of shoulder pain, we conducted a systematic review and qualitative synthesis. As our aim was to perform an aggregative, rather than an interpretive, synthesis of findings from qualitative studies, 13 and to develop practice recommendations, 14 we adopted the principles of meta-aggregation. 15 Accordingly, the aim of this review was to identify and summarize barriers and facilitators related to self-management from the perspectives of people with shoulder pain and clinicians involved in the care of this cohort of patients.
Methods
This review followed the Enhancing Transparency in Reporting the Synthesis of Qualitative Research guidelines, 16 and was registered with the International Prospective Register of Systematic reviews, registration number CRD42018106024. One reviewer (AOS) performed the systematic search (the last search was completed on 7 March 2022). No funding was received to undertake this systematic review.
Eight electronic databases (CINAHL, MEDLINE, PsycINFO, SPORTDiscus, Embase, ProQuest Health, Web of Science, and Scopus) were systemically searched. The search strategy comprised the keywords in Supplemental Appendix 1. The search of Medline is detailed in Supplemental Appendix 2. Grey literature sources were also searched, namely OpenGrey, ProQuest Dissertations & Theses Global, Canadian Agency for Drugs and Technologies in Health, and Google Scholar (limited to the first 100 hits). Reference lists of all included studies were searched using backward and forward citation screening; in addition, experts in the field were contacted to identify additional relevant studies.
The eligibility criteria are detailed in Box 1. We defined barriers as factors that obstruct adherence to, or engagement with, self-management of shoulder pain. We defined facilitators as factors that enable adherence to, or engagement with, self-management of shoulder pain. For the purpose of this review, self-management was defined as ‘the active participation by a person living with a shoulder condition in managing the symptoms, treatment, physical and psychological consequences and lifestyle changes inherent in living with that condition’. 17 Two reviewers (AOS and JMcV) independently screened titles and abstracts to determine whether the papers merited a full-text review, and then independently screened potentially relevant full-text papers by applying the inclusion criteria. Any disagreements that occurred in determining the relevance of a full-text paper were resolved by discussion between these reviewers.
Box 1.
Eligibility criteria
Design
Qualitative studies
Full-text article in English
Mixed-methods studies that reported qualitative data, if the qualitative findings could be extracted separately.
Participants
Adults (aged ≥18 years) with primary shoulder pain, irrespective of diagnostic label
Clinicians involved in the care of adults with primary shoulder pain
- Specific exclusions were participants with:
- – rheumatoid arthritis
- – polymyalgia rheumatica
- – hemiplegic shoulders
- – shoulder pain due to cervical or thoracic spine pathology.
Phenomenon of interest
Barriers and facilitators related to self-management of shoulder pain
The data extraction process was carried out by one reviewer (AOS). A second reviewer (JMcV) completed extraction for 20% of the articles and the information extracted was then compared to ensure consistency in the process. The Joanna Briggs Institute data extraction tool was used (Supplemental Appendix 3). The extraction process included findings from each of the included studies. A finding was defined as ‘a theme, category, or metaphor reported by authors of original papers’. 15 Each finding was then assigned a level of evidence depending on the capacity of the data to adequately support that finding (credibility). Using the ConQual criteria, findings were rated as unequivocal (relates to evidence beyond reasonable doubt and not open to challenge), credible (findings that are, albeit interpretations, plausible in light of data; because the findings are interpretive, they can be challenged) or unsupported (findings that are not supported by the data). 15
Qualitative research findings were synthesized using the Joanna Briggs Institute meta-aggregative approach. 15 An aggregative approach allowed a descriptive thematic mapping and synthesis of barriers and facilitators that lends itself to the formulation of specific recommendations for practice. 14 The first stage in the meta-aggregation involved the aggregation of findings with similarities in meaning to generate categories. Two reviewers (AOS and JMcV) independently categorized the findings from the 20 included studies.18–37 These reviewers then met to reach a consensus on the name and content of each category. Two reviewers (JD and CL) who were not involved in the categorization process validated these categories following discussion and refinement.
The second stage of meta-aggregation involved reviewing the full list of categories and identifying similarities in meaning to generate a comprehensive set of synthesized findings. The categories were discussed between three reviewers (AOS, JMcV and JD) and a consensus was reached on the set of synthesized findings. These synthesized findings were then discussed with the whole research team and feedback was provided by the other three reviewers (HS, CL and JS); this process resulted in the generation of a comprehensive set of synthesized findings.
The final stage involved the development of practice recommendations. AOS developed the practice recommendations. These recommendations were discussed with the whole research team and feedback was provided by the other five reviewers. The consensus was then reached on the set of practice recommendations.
Two reviewers (AOS and JMcV) independently assessed the included studies using the Joanna Briggs Institute critical appraisal instrument for qualitative research (Supplemental Appendix 4). Reviewers were blinded to each other's assessment, and assessments were only compared once the initial appraisal of an article had been completed by both reviewers. Any disagreements were resolved through discussion. No study was excluded based on an assessment of methodological quality, as weak studies may still offer relevant findings. 38
The ConQual 39 tool was used to assess the confidence in the synthesized findings, generating an overall score, for each synthesized finding, of ‘high’ (it is highly likely that the review finding is a reasonable representation of the phenomenon of interest), ‘moderate’ (it is likely that the review finding is a reasonable representation of the phenomenon of interest), ‘low’ (it is possible that the review finding is a reasonable representation of the phenomenon of interest), or ‘very low’ (it is not clear whether the review finding is a reasonable representation of the phenomenon of interest). 40
Results
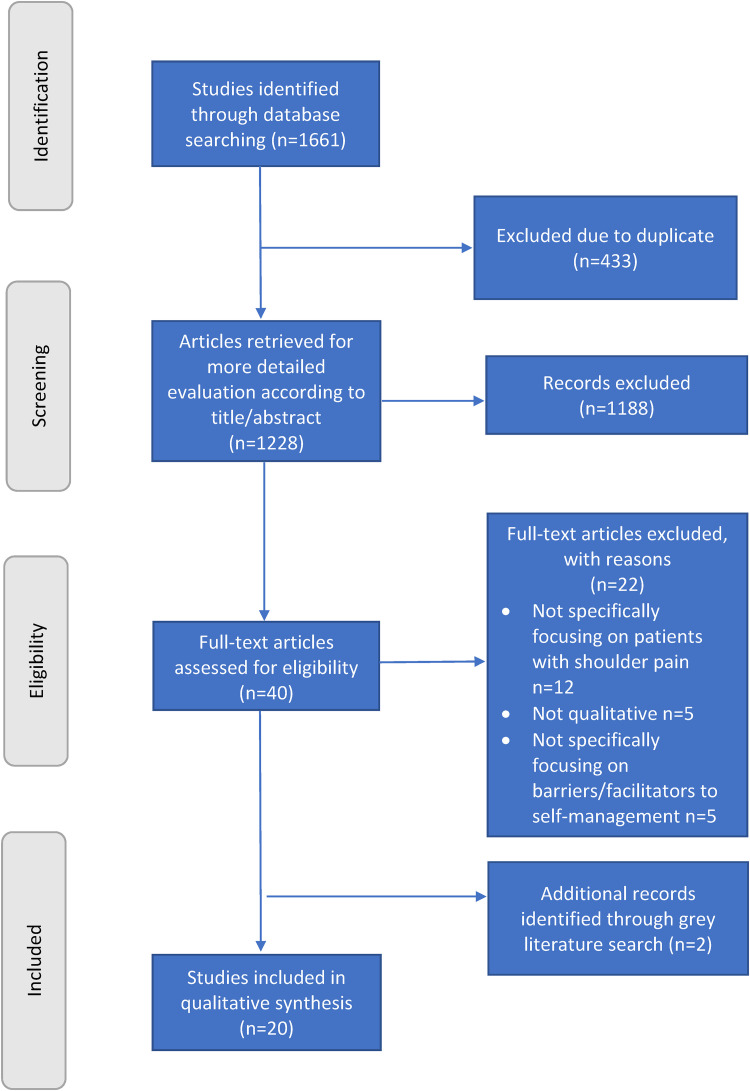
The identification and selection of studies are summarized in Figure 1. 41 Overall, 20 studies were included in this review.18–37 Characteristics of the included studies are described in Table 1. Quality assessment of the included studies, using the Joanna Briggs Institute critical appraisal checklist for qualitative research, is presented in Table 2. In the evaluation of confidence in the synthesized findings, 39 each finding was assigned a ConQual score of ‘moderate’ (Supplemental Appendix 5).
Figure 1.
PRISMA flow diagram. 41
Table 1.
Description of included studies.
| Study | Phenomena of interest | Country | Participants (number; diagnosis; clinical/professional characteristics) | Methods (data collection and analysis) | Key findings on factors influencing engagement with self-management interventions |
|---|---|---|---|---|---|
| Barrett et al. 18 | Subjective experiences of participating in a group-based exercise class for people with non-specific shoulder pain. | Republic of Ireland |
n = 23 patients; non-specific shoulder pain; 15 females and 8 males, aged 44–84 years. |
Semi-structured telephone interviews; inductive thematic analysis. | The group setting increased the participants’ determination to
follow their home exercise programme and increased their
adherence to their home exercise programme. The classes were found to facilitate self-management as they reinforced the exercises and provided advice on self-management. A favourable therapeutic response was found to facilitate adherence to the home exercise programme. The role of the physiotherapist was seen to facilitate self-management. |
| Gilbert et al. 20 | Whether or not the Multiple Joint System was acceptable to patients with shoulder dysfunction and their rehabilitation professionals. | United Kingdom |
n = 17 (7 physiotherapists and 10
patients); shoulder instability or rotator cuff related pain; 5 female and 5 male patients, aged 19–54 years. |
Semi-structured interviews; directed content analysis. | Access to equipment was found to facilitate
self-management. The therapist has been appropriately trained in the use of the equipment to facilitate self-management. Loss of income for private physiotherapists was found to be a barrier to self-management. The ability to monitor patients from a distance (via an online portal) was found to facilitate patient adherence to self-management. Reminders through the patient app were found to facilitate patient adherence to self-management. Ongoing support (follow-up appointments) was found to be a facilitator for self-management. |
| Hanratty et al. 21 | Physiotherapists’ perceptions regarding the use and types of exercise commonly used in the management of subacromial impingement syndrome and their views on the appropriate dosage of such exercises. | Northern Ireland and Republic of Ireland |
n = 20 musculoskeletal
physiotherapists; subacromial impingement syndrome; >5 years’ postgraduate experience working with musculoskeletal conditions. |
Focus groups (semi-structured); thematic content analysis. | Providing short-term pain relief was found to facilitate patient
adherence to their exercise program. Patient education (use of visual tools, advice re benefits of exercise) was found to facilitate self-management. Therapists facilitated self-management by putting the onus back on the patient to be proactive. Patients who are motivated are better at self-managing their condition. Experienced therapists were more confident about gaining patient buy-in to self-management strategies. |
| Lau et al. 22 | Factors that facilitate or hinder the implementation of a patient-facing app in routine clinical care following rotator cuff surgery. | Australia |
n = 12 (4 clinicians and 8
patients); following rotator cuff surgery; 5 female and 3 male patients, aged 42–67 years. |
Implementation records and semi-structured interviews; constant comparative method and thematic analysis. | Patients’ digital health literacy affects adherence to an
app-based self-management programme. Therapists’ digital health literacy affects their willingness to offer the app-based self-management programme to patients. Patients experiencing high levels of pain were disengaged during the app usability session leading to unfamiliarity with the app. Self-management programmes that are too tedious or do not reflect the patient recovery journey act as a barrier to patient adherence. Privacy concerns (sharing of information with insurance and workers’ compensation) when using the app acted as a barrier to the uptake of the self-management app. Patients’ caregivers were found to facilitate adherence to the app-based self-management programme. Lack of communication between clinicians resulted in some clinicians not knowing about the new app-based programme. Clinicians were too busy to introduce the app. |
| Littlewood et al. 23 | Barriers that might prevent implementation of a self-managed loaded exercise intervention. | United Kingdom |
n = 8 (6 patients and 2
physiotherapists); rotator cuff tendinopathy; 3 female and 3 male patients, aged 51–74 years. |
Semi-structured interviews; framework method. | Patients expected hands-on therapist-led treatment and were
demoralised when they were allocated to the self-management
exercise group. Therapists delivering the self-management exercise programme wanted to offer hands-on treatment. Patients believed that exercise was an inadequate intervention to manage their problem. Lack of an early and appreciable response to the therapy acted as a barrier to self-management. Pain was both a facilitator and a barrier to adherence to the self-management programme. The attitude of the therapist towards self-management had an impact on patient adherence to the self-management programme. Ongoing support from the therapist and the patients’ partner facilitated adherence to the self-management programme. Certain Personal traits facilitated self-management (self-efficacy, motivation, positivity). |
| Littlewood et al. 24 | Implementation barriers and facilitators with regard to the self-managed loaded exercise programme from the perspective of the physiotherapists delivering the programme. | United Kingdom |
n = 13 physiotherapists who delivered the
self-managed exercise intervention; rotator cuff tendinopathy; years qualified ranged from 1 to 32 years. |
Semi-structured interviews; framework method. | Manual therapy was the preferred treatment option and
self-management did not align with their usual
practice. Experienced therapists found the rationale underpinning the self-managed loaded exercise programme a challenge whereas less experienced therapists’ beliefs were less developed. Therapists agreed that patient education on the benefits of self-management was important to get patients on board with the self-management programme. Ongoing support and monitoring were important to facilitate patient adherence to the self-management programme. The simplicity of the self-management programme was both a barrier and a facilitator. |
| Minns Lowe et al. 25 | Why participants recruited within the United Kingdom Rotator Cuff Tear trial did not remain within their allocated treatment arm, from the perspective of trial participants. | United Kingdom |
n = 18 patients; degenerative rotator cuff tears; 3 females and 15 males, age 54–75. |
Semi-structured interviews; in accordance with interpretative phenomenological analysis. | Patients with a longer duration of pain were not interested in
conservative management and just wanted to progress to
surgery. Patients with improving symptoms were more likely to continue managing their condition without surgery. Patients reported that the surgeon influenced their decision to cross over to the surgical group by telling them that tears need to be repaired. Participants with previous unsuccessful conservative care, expected surgery to fix their shoulder. Patients viewed rest then exercise negatively, thinking it would take too long. People opted for surgery over conservative management based on their scan findings. |
| Nyman et al. 26 | What it entails to be a patient suffering from shoulder problems and patients’ situations both prior to and following medical intervention. | Finland |
n = 21 patients; supraspinatus tendinitis; 9 females and 12 males, aged 43–63 years. |
Focus group interviews; thematic analysis. | Patients expected that the treatment would be therapist-led and
would “fix” them. Patients are expected to receive hands-on treatment. Previous experiences, other illnesses, and current life situations appeared to influence the respondents’ attitudes toward their own role in the management of their condition. Ongoing support from the therapist facilitated self-management. Patients who experience meaningfulness and life satisfaction have a greater belief in their ability to manage. |
| Palenius and Nyman 27 | How do physiotherapists in different contexts face shoulder problems and what determines the physiotherapists’ choice of approach to their patients? | Finland | n = 36 physiotherapists with experience in treating shoulder problems. | Focus group interviews; thematic analysis. | Patients expected hands-on treatment. Susceptibility to instructions and motivation for self-training varies among patients and affects their ability to self-manage. Regular check-ups are important to motivate patients to follow their exercise programme. Older age, general feelings of unease and long waiting times have a restrictive influence on self-training. Private physiotherapists take into consideration the customers’ own wishes to a large extent. Some customers expect the physiotherapist to be the one who is primarily active in the therapy. |
| Palenius and Nyman 28 | How patients with shoulder problems, especially supraspinatus tendinitis, experience physiotherapy practice. | Finland |
n = 26 patients; supraspinatus tendinitis; 12 females and 14 males, aged 43–63 years. |
Individual interviews and focus group interviews; thematic analysis. | Patients expect hands-on therapist-led
treatment. Patients need ongoing support from the therapist to facilitate adherence to self-management. Most of the respondents agreed that the main responsibility for exercising lies with the individual patient. A functioning interaction between the patient and the physiotherapist can influence the patient's motivation for self-training. |
| Sandford et al. 29 | Factors affecting adherence to a prescribed home- and class-based exercise program for those with rotator cuff tendinopathy. | United Kingdom |
n = 12 patients; rotator cuff tendinopathy; 6 females and 6 males, the majority were between 50 and 69 years of age. |
Semi-structured interviews; inductive thematic analysis. | Participation in a research study increased the patient's
motivation to adhere to the prescribed
treatment. Scheduling of an additional review appointment to progress their exercise programme facilitated increased adherence to the programme. Patients with greater self-efficacy are more likely to adhere to home-based programmes. Lack of an early response reduces patient adherence to a home-based exercise programme. Pain was a motivator, enabler, facilitator and for some a barrier to exercise. The right equipment needs to be provided to facilitate adherence. Participants found it difficult to find time to complete their home exercise programme. Patients who incorporate the exercises into their daily routine are more likely to adhere to their home exercise programme. Personal traits (motivation and self-discipline) influence adherence to a home-based exercise programme. |
| Stamp et al. 31 | The experienced benefit of psychomotor therapy. | Denmark |
n = 12 patients; shoulder pain (visual analogue scale > 2 at rest, visual analogue scale > 5 in activity) lasting more than 3 months; 4 females and 8 males, aged 38–67 years. |
Face-to-face interviews; theoretical sampling and constant comparative analysis. | Advice from the therapist facilitated self-management at
home. Psychomotor therapy helped patients to change behaviours and manage their shoulder pain. Incorporating advice from the therapist into their daily routine facilitated self-management. Patients realised that they themselves could affect the intensity of their shoulder pain. Pain was a reminder to the patient that they needed to take action. Psychomotor therapy helps patients become more aware of body signals and how to respond to them. |
| Franz and Uhazie 32 | Barriers to home exercise programme adherence among patients with shoulder pathology. | USA |
n = 8 patients; unilateral musculoskeletal shoulder pathologies; 5 females and 3 males, aged 49–87 years. |
One-on-one interviews; comparative analysis. | Pain had an influence on home exercise programme adherence (both
a barrier and a facilitator). One's belief in full recovery (positive or negative) was not associated with increased home exercise programme adherence. Having a social support system was not associated with completion of all of ones set & reps assigned in their home exercise programme. Having enough time to complete the home exercise programme was not associated with complete set and repetition of home exercise programme adherence. Those who self-reported themselves as active individual was not associated with complete home exercise programme adherence to assigned sets and repetitions. Being limited in one's normal activities was associated with decreased home exercise programme adherence to all sets and repetitions. Positive satisfaction with a therapist, understanding of instructions, and positive perception of rehabilitation was not associated with higher or lower rates of adherence to home exercise programme assigned sets & repetitions. |
| Cuff and Littlewood 19 | How do patients rationalise their shoulder pain following a diagnosis of subacromial impingement syndrome and how this understanding might impact their perception of physiotherapy and engagement with exercise. | UK |
n = 9 patients; subacromial impingement syndrome; 5 females and 4 males, mean age of 56.5 years. |
Semi-structured interviews; framework method. | The biomedical approach to diagnosis, which impacts how patients
understand their problem, has implications for their
management. Therapists continue to use a biomedical approach to diagnosis despite a lack of evidence for this approach. The language used by the therapists led patients to believe that surgery was the only option. Some participants questioned the appropriateness of physiotherapy. The message delivered by the attending clinician influences subsequent expectations of what physiotherapy can achieve. Patients display a lack of understanding of what physiotherapy might help a patient to achieve. |
| Sole et al. 30 | Participants’ perceptions of pain neuroscience education as an intervention for their shoulder pain. | New Zealand |
n = 10 patients; persistent rotator cuff related pain; 5 females and 5 males, aged 47–68 years. |
Semi-structured interviews; general inductive approach. | Most of the participants found the pain education session
helpful. Participants’ understanding of pain was reconceptualised, evident by their ability to describe the role of neurophysiological mechanisms, stress and general well-being in their pain. Participants still sought a pathoanatomical explanation of their pain and individual-specific exercises. Participants recommended integrating pain neuroscience education with pathoanatomical knowledge. Participants also recommended educating other health professionals about pain neuroscience education. |
| White et al. 33 | Expert shoulder clinician's experiences with managing rotator cuff tendinopathy including practice beliefs towards providing education. | Australia |
n = 8 clinicians; shoulder tendinopathy; shoulder clinicians who had published about shoulder tendinopathy within the past 5 years and had a minimum of 10 years of clinical experience. |
Semi-structured interviews; inductive thematic analysis. | Most clinicians reported that the first consultation was
critical for engaging patients in the overall rotator cuff
tendinopathy management plan in order to facilitate patient
education and understanding. Clinicians prioritised understanding patient expectations and provided an education that clarified misconceptions about treatment, pain and structure, and treatment philosophies. All clinicians highlighted that developing trust and an early therapeutic relationship was closely linked with achieving better treatment outcomes. Clinicians expressed that it was important for patients to understand what is involved with exercise management in rotator cuff tendinopathy, given that it can be a substantial commitment and required significant behaviour change. Promoting behaviour change through education took time and many clinicians reported that their work setting did not recognize the value of taking extra time in consultations to have a long conversation with the patient. All clinicians expressed concerns about having had no formal training concerning how to best educate their patients in order to form a collaborative partnership and address many of the patient education issues raised. |
| Cridland et al. 34 | The experiences and perspectives of people with RCRSP about education for their condition. | Australia | n = 8 patients; rotator cuff related shoulder pain; 5 females and 3 males, aged 49–67 years. | Semi-structured telephone interviews; inductive thematic analysis. | A therapeutic alliance leads to a trust in
education. Education designed for rotator cuff related shoulder pain patients should be individualized and practical. Delivery of educational interventions should be varied and multi-modal. |
| Kiely 35 | The experience of attending either individual or group physiotherapy for the management of rotator cuff tendinopathy in primary care. | Ireland | n = 10 patients; rotator cuff tendinopathy; 8 females and 2 males; aged 46–86 years. | Semi-structured telephone interviews; thematic analysis. | Patients valued support from their therapist or peers, and
received an explanation about their condition, receiving
feedback on their exercise performance and advice on how to
manage their condition. Participants from both treatment groups reported a strong positive belief in exercise and the main were convinced that exercise was key to recovery. Laziness, meaning a lack of motivation due to lack of symptoms, was cited as the reason for discontinuing exercises. Participants identified a successful outcome as an improvement in function and acquired confidence in their ability to manage their condition independently. |
| Stutz 36 | Whether an app can support physiotherapy and whether an app is feasible in the context of home-based physiotherapy. | Austria | n = 10 patients; adhesive capsulitis; 7 females and 3 males. | Semi-structured interview; qualitative content analysis. | Both interventions showed that an app can sustainably support
physiotherapy for frozen-shoulder patients. The ShoulderApp-based intervention was well accepted by the frozen-shoulder users. Patients would appreciate automatic feedback on their progress. The usability of the automatic mobility measurement process has to be improved. |
| Ulack et al. 37 | What is it like to live with rotator cuff tendinopathy? What are the barriers and facilitators of a healthy lifestyle with an ageing shoulder? What are the outcomes that matter most to people seeking care for rotator cuff tendinopathy? | USA | n = 19 patients; rotator cuff tendinopathy; 10 females and 9 males; aged 31–75 years. | Experience group sessions; a hybrid of initial inductive coding of themes and subsequent deductive consideration of these themes within the capability, comfort, and calm framework. | Patients with rotator cuff tendinopathy experienced less restful
sleep, difficulty with work and life transitions, loss of
baseline abilities, limitation in social roles, physical pain,
despair, loneliness, lack of direction or progress and feeling
uncared for. Barriers to a healthy lifestyle with an ageing shoulder included the sense that rotator cuff tendinopathy is something correctable rather than age-associated, the sense that painful activities will make the tendinopathy worse, tenuous relationships and limited trust with clinicians, loss of hope, and a sense that care is directionless. The outcomes that mattered most to patients seeking care were feeling that they were receiving effective care and not being dismissed; maintaining meaningful activity and life roles; and replacing despair and frustration with hope and progress. |
Table 2.
Methodological quality of included studies.
| Study | Question number | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Q1 a | Q2 b | Q3 c | Q4 d | Q5 e | Q6 f | Q7 g | Q8 h | Q9 i | Q10 j | |
| Barrett et al. 18 | No | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| Cuff and Littlewood 19 | No | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| Gilbert et al. 20 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes |
| Hanratty et al. 21 | No | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| Lau et al. 22 | No | Yes | Yes | Yes | Yes | No | No | No | Yes | Yes |
| Littlewood et al. 23 | No | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes |
| Littlewood et al. 24 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes |
| Minns Lowe et al. 25 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| Nyman et al. 26 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes |
| Palenius and Nyman 27 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes |
| Palenius and Nyman 28 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Sandford et al. 29 | No | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes |
| Sole et al. 30 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Stamp et al. 31 | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes |
| Franz and Uhazie 32 | Yes | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes |
| White et al. 33 | No | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| Cridland et al. 34 | Yes | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| Kiely 35 | No | Yes | Yes | Yes | Yes | No | Yes | Yes | Yes | Yes |
| Stutz 36 | No | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes |
| Ulack et al. 37 | No | Yes | Yes | Yes | Yes | No | No | Yes | Yes | Yes |
Q1: Is there congruity between the stated philosophical perspective and the research methodology?
Q2: Is there congruity between the research methodology and the research question or objectives?
Q3: Is there congruity between the research methodology and the methods used to collect data?
Q4: Is there congruity between the research methodology and the representation and analysis of data?
Q5: Is there congruity between the research methodology and the interpretation of results?
Q6: Is there a statement locating the researcher culturally or theoretically?
Q7: Is the influence of the researcher on the research, and vice-versa, addressed?.
Q8: Are participants, and their voices, adequately represented?
Q9: Is the research ethical according to current criteria or for recent studies, and is there evidence of ethical approval by an appropriate body?
Q10: Do the conclusions drawn in the research report flow from the analysis, or interpretation, of the data? 39
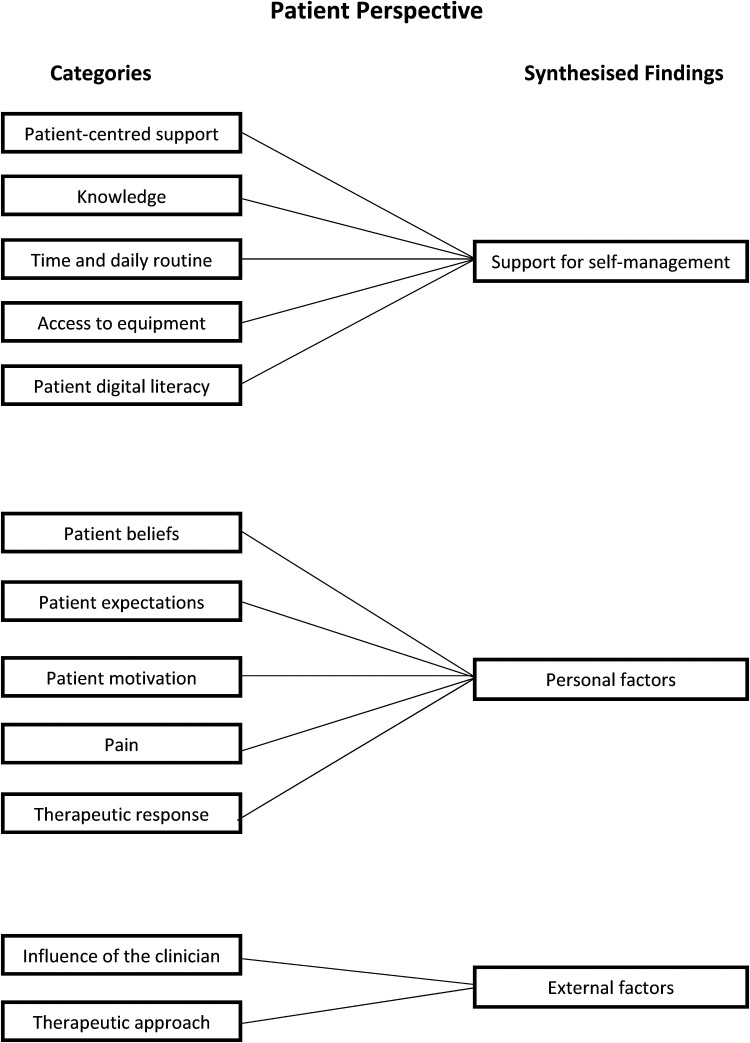
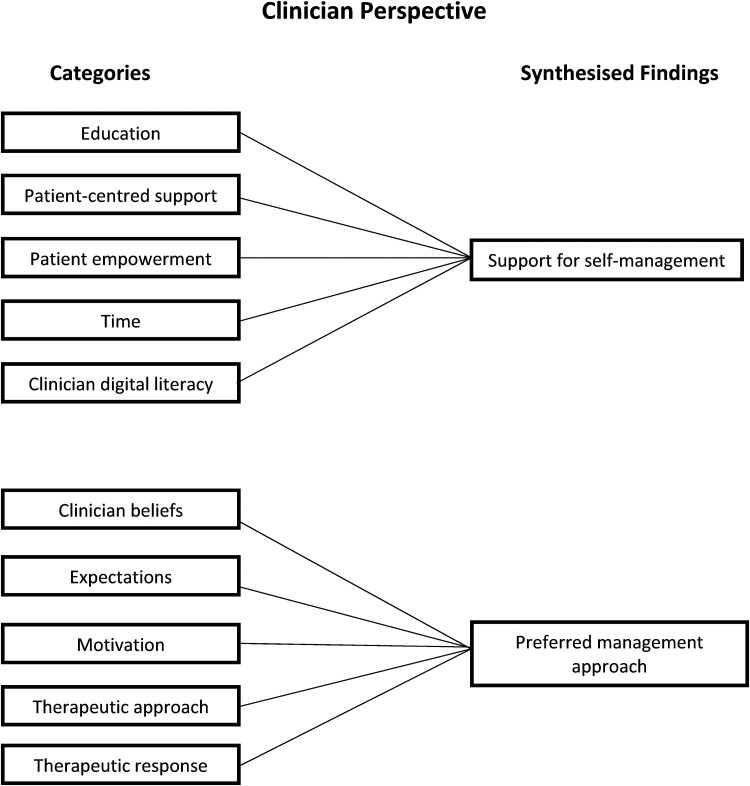
In total, 305 findings were extracted from the 20 included studies and were organized into 12 categories that related to the patients’ perspective and 10 categories that related to the clinicians’ perspective. Further analysis of the categories led to the generation of three synthesized findings relating to the patients’ perspective and two synthesized findings relating to the clinicians’ perspective (Figures 2 and 3). Examples of supporting evidence are provided in Supplemental Appendices 6 to 10.
Figure 2.
Patient perspective.
Figure 3.
Clinician perspective.
Patient perspective
Support for self-management
People with shoulder pain identified support for self-management as being important; specifically, categories related to (1) patient-centred support, (2) knowledge, (3) time and daily routine, (4) access to equipment, and (5) patient digital literacy (Supplemental Appendix 6).
Patient-centred support
Support from the clinician20,23,26,28,31,34,35 and from family members,23,36 and social support18,35,36 were mentioned as facilitating participant adherence to self-management strategies. Early support from clinicians was valued and as participants progressed through treatment and their condition improved, this high level of support was reduced, and participants were encouraged to self-manage their shoulder pain. 18 Follow-up appointments with the clinician were also reported to facilitate self-management.23,27,29,36 Participants also mentioned that group classes increased adherence to their home exercise programmes.18,35
Knowledge
Participants reported that advice from the clinician on how to manage their shoulder condition,18,34 what to do when it hurts, 23 how to exercise,31,34 advice on rehabilitation timelines,29,34 and pain education30,34 were all seen to facilitate a self-management approach. However, when participants received advice that aligned with the biomedical model of pain, it tended to reinforce ideas of a specific biomedical remedy, including surgery. 19
Time/daily routine
Lack of time was frequently mentioned by participants as a barrier to completing their home exercise programme.23,29,32 Incorporating exercises into their daily routine – for example, doing their exercises while waiting for the kettle to boil – was a strategy that they utilized in order to increase their adherence to a home exercise programme. 29
Access to equipment
Ease of access to equipment facilitated adherence to self-management. 20 When participants lived some distance away from where the equipment was located, they reported that this was a barrier to their engagement with the equipment and therefore a barrier to adhering to their self-management programme. Simple equipment such as resistance bands for exercise was a facilitator, as they could be used anywhere.29,36
Patient digital literacy
Poor patient digital literacy was reported to be a barrier to a self-management programme for shoulder pain based on a web-based application (‘app’). 22 Participants forgot passwords, were unfamiliar with their Wi-Fi setup at home and had difficulty downloading the app, all of which hindered their ability to engage with the app-based programme. Suggestions that were made to facilitate engagement with the app were to introduce it as part of pre-operative care and to have a practice app. It is important to note, however, that only one study focused on patient digital literacy.
Personal factors
People with shoulder pain described several personal factors as being important. Categories identified related to (1) patient beliefs, (2) patient expectations, (3) patient motivation, (4) pain, and (5) therapeutic response (Supplemental Appendix 7).
Patient beliefs
A number of participants who had engaged with a self-management programme, and where outcomes were unsatisfactory, expressed concerns about the nature of their problem and questioned whether a self-managed approach was appropriate for them.23,30 These negative beliefs about self-management were reinforced if the clinician was also sceptical about the potential benefit of a self-managed approach. 23 However, participants who had previously received clinician-led interventions that were unsuccessful were receptive to engaging with self-management. 23
Patient expectations
Some participants who were offered a self-managed exercise programme were disappointed, as they anticipated a poor outcome with this approach. 23 Some attended physiotherapy assuming that it would be unsuccessful, but they had to complete a course of physiotherapy before being referred for surgery. 25 Many of these participants perceived their shoulder problem to be mechanical in nature and so expected an intervention that would fix their problem quickly.26,37 A number of these participants expected hands-on treatment,23,27 while others who had received previous unsuccessful conservative treatment expected surgery. 25
Patient motivation
Some participants admitted to being too lazy to follow their home exercise programme, and some accepted that they did not take responsibility for the programme as they hoped that the clinician would get them better.23,26,35 However, it appears that participants largely agreed that it was their responsibility to adhere to their home exercise programme and to establish new habits that would reduce the impact of their shoulder symptoms.26,30,31,34,35
Pain
Pain was found to have been both a facilitator of, and a barrier to, exercise. 29 Some participants who completed regular exercise reported a reduction in their shoulder pain and, as a result, their motivation to continue to exercise increased. 29 Those whose shoulder condition caused the most difficulty with functional activities demonstrated greater adherence to home exercise programmes. 29 However, others found pain to be a barrier to exercise.29,30,35,37 These participants used pain as a guiding factor to decide when to adjust or skip their home exercise programme and as an indication of when to stop exercise.30,32
Therapeutic response
When participants experienced a favourable therapeutic response with a self-managed approach, they reported being more likely to adhere.18,23,29,36 When previous clinician-led interventions yielded a poor therapeutic response, participants were amenable to engaging with a self-managed approach. 23
External factors
People with shoulder pain described external factors as being important; specifically, categories related to the (1) influence of the clinician and (2) therapeutic approach (Supplemental Appendix 8).
Influence of the clinician
Some participants described the physiotherapist as facilitating increased self-management by gradually getting the patient to take greater responsibility for the management of his or her shoulder condition.18,34 Some medical personnel may also have facilitated a self-management approach by encouraging patients to trial conservative treatment before surgery. 19 However, when the clinician expressed doubt over the benefit of self-managed approaches, this negatively affected the patient's attitude towards self-management.19,23,37
Therapeutic approach
When the home exercise programme only consisted of one exercise, some participants doubted the potential benefit of the programme. 23 However, others found the simplicity of the exercise programme to be a facilitator, as it was easily incorporated into their daily routine. 23 Many participants expected to receive hands-on treatments, which did not align with a self-management approach and could act as a barrier to engagement. 28
Clinicians’ perspectives
Support for self-management
Clinicians identified support for self-management as being important; specifically, categories related to (1) education, (2) patient-centred support, (3) patient empowerment, (4) time, and (5) clinician digital literacy (Supplemental Appendix 9).
Education
Clinicians agreed that early patient education was essential to get patient buy-in to the home exercise programme and to facilitate long-term self-management.21,33 Clinicians reported that education that focused on clarifying misconceptions about treatment, pain and anatomical structure, and explanation of treatment philosophies were important to engage patients in the management plan. 33 Despite this, clinicians expressed some disquiet about having had no formal training on how best to educate their patients. 33
Patient-centred support
Clinicians recognized the importance of providing ongoing support and monitoring in order to facilitate adherence to a self-managed exercise programme.23,24,33 One way to monitor patient adherence was via an online app, and the app reminded patients to complete their home exercise programme. 20 Clinicians also reported that follow-up appointments were beneficial in facilitating patients’ comply with home exercise programmes in the long term. 29
Patient empowerment
Clinicians reported that it was important to encourage patients to take responsibility for the management of their shoulder condition21,27 and for patients to understand the substantial commitment and significant behaviour change required for exercise management of shoulder pain to be successful. 33
Time
Clinicians reported that limited time was a barrier to supporting a self-management approach.20,22,33 For an app-based self-management programme, clinicians found it difficult to find the time to set up the patient app and explain how to use it during the consultation. 22
Clinician digital literacy
For some clinicians, digital literacy was a barrier. These clinicians were not confident about using new technologies and this affected their willingness to offer an app-based self-management programme to their patients. 22 It was noted that strategies to improve clinicians’ digital literacy and help them to incorporate the app into their everyday practice were important. Clinicians also noted that older patients often have poor digital literacy and might therefore not be suitable candidates for the app-based programme. 22 A practice app was suggested as a way of overcoming this barrier. It is important to note that only one study focused on clinician digital literacy.
Preferred management approach
Clinicians reported that the management approach they preferred in the treatment of shoulder pain was important; specifically, categories related to (1) clinician beliefs, (2) expectations, (3) motivation, (4) therapeutic approach, and (5) therapeutic response (Supplemental Appendix 10).
Clinician beliefs
Physiotherapists reported that they could identify patients during the assessment who they believed would not engage with a self-managed approach.23,33 For a number of physiotherapists, a self-managed approach did not align with their usual practice and they therefore found it challenging to embrace. 24 These physiotherapists expressed disquiet when they were unable to offer hands-on treatments. 24 Similarly, several surgeons believed that rotator cuff tears would not heal without surgery, and consequently believed that surgery was the only effective option. 25
Expectations
Clinicians mentioned that some patients expected the clinician to be more active than the patient during treatment 27 and they thought it unlikely that these patients would engage with a self-managed approach. Clinicians reported that it was important to understand the patient's expectations from the start27,33 and that when patient expectations do not align with self-management, it is a challenge for the clinician to offer this approach.27,33
Motivation
Clinicians described patients with shoulder pain as two distinct groups: those who are highly motivated and adhere to their home exercise programme, and those who need a lot of encouragement to engage and adhere.21,23,27 For the latter group, clinicians reported that it was important that these patients understood their role in the management of their shoulder pain.21,33 Clinicians discussed shared responsibility, whereby the clinician demonstrated exercises and motivated patients and patients were responsible for adhering to their home exercise programme.21,28,33 Regular check-ups were frequently mentioned as a way to motivate patients and increase adherence to their home exercise programme.27,29 Clinicians also mentioned that patients who pay for treatment were often motivated to engage in self-management. 27
Therapeutic approach
The simplicity of a self-managed exercise programme that consisted of one exercise was perceived as both positive and negative. 24 However, when clinicians who were previously sceptical about a self-management exercise programme of this type saw its success, this challenged their current practice. 24 More experienced clinicians were less likely to offer a temporary solution and were more likely to offer education, to obtain patient buy-in to long-term self-management.21,33 Most clinicians would offer hands-on treatment as part of their approach to the management of shoulder pain, which would obviously not align with a self-management approach.23,24
Therapeutic response
Clinicians agreed that providing short-term pain relief assisted in increasing patient engagement with the exercise programme. 21 Clinicians reported that they might use taping to achieve this short-term relief, and such relief demonstrated to the patient the long-term benefits of exercise. 21 When comparing the self-managed exercise programme to other treatment interventions, clinicians reported that it took longer to achieve a worthwhile clinical outcome when implementing the self-managed exercise programme 24 ; this represents a potential barrier to the self-managed approach.
Discussion
The aim of this systematic review and qualitative synthesis was to identify barriers and facilitators related to self-management from the perspectives of people with shoulder pain and clinicians involved in their care. Three synthesized findings were identified by patients as the issues that influenced self-management: support for self-management, personal factors, and external factors. Support for self-management and the preferred therapeutic approach were identified by clinicians as the main influences on engagement with self-management. Similar to the results of this review, education, health beliefs, patient-centred support, social support, therapeutic response, and shared decision-making have all been found to influence adherence to self-management for non-communicable diseases such as asthma, 42 chronic obstructive pulmonary disease, 43 and type 1 diabetes. 44 The findings of our review are also consistent with known theories of behavioural change. Determinants of behaviour change such as professional role, knowledge, skills, beliefs about consequences, and motivation are common components of behavioural change theories, and these determinants are consistent with the findings identified in our review. 45
An important consideration when interpreting the results of this review is that most of the included studies focused on home exercise programmes, and therefore might not fully represent barriers and facilitators related to broader self-management programmes for people living with shoulder pain. The term ‘self-management’ was rarely used in the studies included in this review; interventions that supported self-management were discussed but were not explicitly described as such. These interventions often involved exercise-based rehabilitation. Self-management encompasses more than advice and a home exercise programme, and goes beyond simple dissemination of information on diagnosis and exercise prescription. 46 Rotheram-Borus et al. 47 describe five essential elements required for successful self-management: (1) activate motivation for change; (2) apply information from education and self-monitoring; (3) develop skills; (4) acquire environmental resources; and (5) build social support. Most of the interventions discussed in our review were aimed at providing patients with the knowledge and skills to self-manage. However, most of the included studies did not address critical elements of self-management such as problem-solving, activating the motivation for change, initiating and reinforcing behaviour change, and building social support. Future research studies for shoulder pain should incorporate a broader framework for self-management to investigate the effectiveness and explore patient perceptions of a more person-centred approach.
The findings of this synthesis suggest that educational interventions focused on self-management strategies, such as home exercise, facilitated a self-managed approach. However, most of the education provided was based on the biomedical model of pain. Diagnosis of shoulder pain based on this model tends to reflect a narrow understanding of shoulder pain and is informed by a pathoanatomical diagnosis.48,49 A biomedically oriented educational approach was perceived as acting as a barrier to patient engagement with self-management. Only one of the included studies incorporated a formal education component, which consisted of a one-hour presentation. 30 Patients found this educational session overwhelming and suggested that this information should be delivered over several sessions. In contrast, education programmes for non-communicable diseases such as asthma, 50 chronic obstructive pulmonary disease 51 and diabetes 52 involve several educational sessions. Clinicians involved in the design of self-management programmes for shoulder pain need to take this ‘temporal chunking’ into consideration.
Patients appreciated the responsiveness of clinicians when questions and problems arose and reported that it was important that follow-up appointments were scheduled. Similar to our review, Campbell et al. 53 highlighted that follow-up support for effective type 1 diabetes self-management should be a combination of both structured and responsive individualized follow-up support. Patient-centred support should provide patients with the opportunity to troubleshoot problems as they arise, with appropriately trained clinicians.
Shared decision-making emerges as a common theme across systematic reviews investigating self-management for several chronic conditions.42,54–56 As part of this decision-making process, clinicians need to be aware of patient beliefs and expectations. This current review found that patients’ understanding of their shoulder pain was based on the biomedical model and patients expected hands-on treatment and had an expectation that clinicians will ‘fix’ them.23,25,26 This belief that the patient was a passive recipient of care was identified as a barrier to engagement with self-management for shoulder pain. Main et al. 57 report that patient concerns and mistaken beliefs should be addressed from the outset, which facilitates the development of a mutually agreed management plan. They highlighted that all explanations provided to patients must be in a language and terminology that they understand, as this helps to shape their beliefs and expectations and optimize their coping strategies. 57
Patient motivation was also a key factor underpinning adherence to exercise-based rehabilitation.42,43,53 Clinicians reported that they could identify patients who were not motivated and where self-management would not be effective. However, these studies did not investigate the validity of these expressed preconceptions. Future research should investigate if clinicians can validly identify patients who are not motivated and will not adhere to self-management and require a different approach that aligns with their needs.
The findings from our review suggest that clinicians’ preferred approach to the management of shoulder pain does not align with self-management. Their approach is more consistent with the biomedical model and comprises clinician-led interventions. Given that the evidence to date suggests that shoulder pain is resistant to treatment, clinicians should consider self-management programmes that focus on providing patients with the necessary tools to self-manage their shoulder pain and focus on keeping the patient active. In this context, clinicians are encouraged to switch from the biomedical model to the biopsychosocial model and a model of care based on shared decision-making to facilitate self-management support. 58 Furthermore, Wade et al. 48 report that the biomedical model cannot fully explain many forms of illness and that when patients are provided with a diagnosis they assume that a specific treatment will be provided by the health service, despite contemporary evidence for the use of active self-management in chronic condition care.
This synthesis found that patients and clinicians experience barriers and facilitators relating to engaging with self-management that are reflected in 14 domains of the theoretical domains framework. This framework was originally developed to identify influences on health professional behaviour related to the implementation of evidence-based recommendations. 59 The use of the theoretical domains framework has been extended and it is now used to inform the implementation of behavioural change in patient populations. Behavioural change interventions are increasingly recognized as an essential component of self-management. 60 The theoretical domains framework has also been used to guide the choice of behaviour change techniques and intervention components. 61 Therefore, future studies may benefit from using the theoretical domains framework to inform study design when exploring self-management approaches for shoulder pain. By adopting this framework, the barriers and facilitators relating to self-management can be explored, within the context of behaviour change, thereby identifying how barriers can be avoided or addressed through appropriate intervention strategies.
Strengths of the review include that, through exploring both patient and clinician perspectives, a more comprehensive understanding of the barriers and facilitators related to self-management is provided; in addition, the number of studies in this review provided sufficient evidence to answer the research question. Multiple reviewers carried out each stage of the review to address any potential areas of subjectivity, which enhances the credibility of the review. A range of approaches exist within qualitative synthesis, 62 but as our pragmatic concern was to identify ‘lines of action’ for clinical practice, rather than a more phenomenological understanding of the experience and management of shoulder pain, we adopted an aggregative rather than an interpretive approach.
There were also some limitations in the review process. Given how broad self-management is and the multiple elements encompassed by self-management, it is possible that the keywords searched may not have found all the relevant studies. However, reference lists of all included studies were searched using backward and forward citation screening, and experts in the field were contacted to identify additional relevant studies. Our use of the Joanna Briggs Institute critical appraisal checklist for qualitative research was not assessed for reliability; however, studies were assessed independently, and agreement was reached for all studies. Finally, our review only sought to identify the barriers and facilitators that are related to self-management approaches for shoulder pain. Further research is needed to examine whether overcoming these barriers and extending the framework towards a more person-centred approach will increase adherence to self-management programmes for shoulder pain and improve patient outcomes.
Practice recommendations
From the results of this synthesis, three key recommendations were derived that are intended to help to inform the design and implementation of self-management programmes for shoulder pain.
Recommendation 1
Patients’ beliefs, goals and expectations must be considered when developing and implementing a self-management programme. Patients should be involved in the decision-making progress, and accordingly, the benefits and limitations of each treatment option should be explained to them so that they can make informed decisions. If patients’ beliefs, goals and expectations do not align with a self-management approach, then the aims of self-management, such as equipping patients with the necessary tools to manage their condition on an ongoing basis and enabling them to keep active, should be explained to the patient or these aims should be re-oriented to more appropriately support their needs and goals. Similarly, patients should be provided with an education that aligns with their goals and needs. Patient digital literacy should also be considered when developing online or application-based self-management programmes.
Recommendation 2
To increase patient adherence to exercise-based rehabilitation, self-management programmes might consider the potential value, or otherwise, of follow-up support, aimed at empowering the patient, through assessment of progress, goal setting, and problem-solving support. For patients who lack motivation, group exercise classes and alternatives identified by the patient might be appropriate. Where pain is a barrier to adherence, a graded approach to exercise-based rehabilitation could be considered in tandem with recognition of the patient's acceptable symptom response. Programmes should also ensure that patients have adequate access to resources and are provided with strategies to allow them to incorporate the approach into their daily routine.
Recommendation 3
Clinicians should consider their own current beliefs and the extent to which they might facilitate or compromise support for self-management of people living with shoulder pain. As shoulder pain is recurrent in nature and often resistant to current treatments, optimal management should include equipping patients with the necessary tools that align with their goals and needs, and assist them to return to valued life activities. Clinicians may require new skills to support person-centred care and longer consultation times to enable them to incorporate self-management strategies into the management of people with shoulder pain.
Conclusion
This qualitative synthesis identified barriers and facilitators relating to self-management approaches for shoulder pain that might explain, in part, why existing self-management programmes are not always effective. Most of the included studies focused on home exercise adherence and therefore might not fully represent barriers and facilitators related to broader self-management programmes for shoulder pain. Adherence to self-management programmes might be improved by better education of both patients and clinicians to shape helpful contemporary evidence-informed beliefs and expectations about management of shoulder pain as well as shared planning and behavioural support. A greater focus should be placed on the limitations of currently available treatments and the potential to maximize the quality of life over the long term through adherence to a self-management programme. A supportive environment, motivation, adequate resources, and using educational methods that build self-care skills increase engagement with self-management of shoulder pain. Clinicians should review and consider whether any of their current beliefs might compromise support for self-management of people living with shoulder pain. Critically, the results of this review could stimulate informed discussion for the future delivery of self-management programmes for people with shoulder pain and the requirement to upskill clinicians to effectively support patients and implement behaviour change strategies. The challenge now is to incorporate these findings into routine practise and to develop novel interventions to support effective self-management.
Clinical messages.
Patients’ expectations and goals must be considered when developing and implementing a self-management programme.
To increase patient adherence to exercise-based rehabilitation, follow-up support, and the patient's acceptable symptom response should be considered.
Clinicians should consider their own beliefs and the extent to which they might compromise support for self-management.
Supplemental Material
Supplemental material, sj-docx-1-cre-10.1177_02692155221108553 for Barriers and facilitators related to self-management of shoulder pain: a systematic review and qualitative synthesis by Aidan O'Shea, Jonathan Drennan, Chris Littlewood, Helen Slater, Julius Sim, and Joseph G. McVeigh in Clinical Rehabilitation
Footnotes
Author Contributions: AOS and JMcV assessed eligibility for inclusion; AOS and JMcV undertook data extraction; AOS and JMcV undertook critical appraisal of the included studies; AOS, JD, CL, HS, JS and JMcV undertook data analysis and data synthesis. All authors contributed to and approved the final draft of the manuscript.
Declaration of conflicting interests: The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: C. Littlewood was a co-author of three of the studies and J. Sim was co-author of one of the studies included in this review, but neither author was involved in study selection. J. McVeigh was co-author of one included study, and was involved in study selection.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs: Aidan O’Shea https://orcid.org/0000-0003-2780-2380
Chris Littlewood https://orcid.org/0000-0002-7703-727X
Helen Slater https://orcid.org/0000-0002-4868-4988
Supplemental material: Supplemental material for this article is available online.
References
- 1.Artus M, van der Windt DA, Afolabi EK, et al. Management of shoulder pain by UK general practitioners (GPs): A national survey. BMJ Open 2017; 7: e015711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Doiron-Cadrin P, Lafrance S, Saulnier M, et al. Shoulder rotator cuff disorders: A systematic review of clinical practice guidelines and semantic analyses of recommendations. Arch Phys Med Rehabil 2020; 101: 1233–1242. [DOI] [PubMed] [Google Scholar]
- 3.Vandvik PO, Lähdeoja T, Ardern C, et al. Subacromial decompression surgery for adults with shoulder pain: A clinical practice guideline. Br Med J 2019; 364: 1294. [DOI] [PubMed] [Google Scholar]
- 4.Diercks R, Bron C, Dorrestijn O, et al. Guideline for diagnosis and treatment of subacromial pain syndrome: A multidisciplinary review by the Dutch Orthopaedic Association. Acta Orthop 2014; 85: 314–322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Littlewood C, May S, Walters S. A review of systematic reviews of the effectiveness of conservative interventions for rotator cuff tendinopathy. Shoulder Elbow 2013; 5: 151–167. [Google Scholar]
- 6.Steuri R, Sattelmayer M, Elsig S, et al. Effectiveness of conservative interventions including exercise, manual therapy and medical management in adults with shoulder impingement: A systematic review and meta-analysis of RCTs. Br J Sports Med 2017; 51: 13401347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hanratty CE, McVeigh JG, Kerr DP, et al. The effectiveness of physiotherapy exercises in subacromial impingement syndrome: A systematic review and meta-analysis. Semin Arthritis Rheum 2012; 42: 297–316. [DOI] [PubMed] [Google Scholar]
- 8.Croft P, Pope D, Silman A. The clinical course of shoulder pain: Prospective cohort study in primary care. Primary Care Rheumatology Society Shoulder Study Group. Br Med J 1996; 313: 601–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Granviken F, Vasseljen O. Home exercises and supervised exercises are similarly effective for people with subacromial impingement: A randomised trial. J Physiother 2015; 61: 135–141. [DOI] [PubMed] [Google Scholar]
- 10.Kuhn JE. Exercise in the treatment of rotator cuff impingement: A systematic review and a synthesized evidence-based rehabilitation protocol. J Shoulder Elbow Surg 2009; 18: 138–160. [DOI] [PubMed] [Google Scholar]
- 11.Robinson PM, Norris J, Roberts CP. Randomized controlled trial of supervised physiotherapy versus a home exercise program after hydrodilatation for the management of primary frozen shoulder. J Shoulder Elbow Surg 2017; 26: 757–765. [DOI] [PubMed] [Google Scholar]
- 12.Hayes K, Ginn KA, Walton JR, et al. A randomised clinical trial evaluating the efficacy of physiotherapy after rotator cuff repair. Aust J Physiother 2004; 50: 77–83. [DOI] [PubMed] [Google Scholar]
- 13.Paterson B. “It looks great but how do I know it fits?”: An introduction of meta-synthesis research. In: Hannes K, Lockwood C. (eds) Synthesizing qualitative research: Choosing the right approach. Chichester: Wiley, 2012, pp. 1–20. [Google Scholar]
- 14.Hannes K, Lockwood C. Pragmatism as the philosophical foundation for the Joanna Briggs meta-aggregative approach to qualitative evidence synthesis. J Adv Nurs 2011; 67: 1632–1642. [DOI] [PubMed] [Google Scholar]
- 15.Lockwood C, Porrit K, Munn Z, et al. Chapter 2: systematic reviews of qualitative evidence. In: Aromataris E, Munn Z. (eds) JBI manual for evidence synthesis. Adelaide: Joanna Briggs Institute, 2020. Available at: https://synthesismanual.jbi.global [Google Scholar]
- 16.Tong A, Flemming K, McInnes E, et al. Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Med Res Methodol 2012; 12: 181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barlow J, Wright C, Sheasby J, et al. Self-management approaches for people with chronic conditions: A review. Patient Educ Couns 2002; 48: 177–187. [DOI] [PubMed] [Google Scholar]
- 18.Barrett E, Hayes A, Kelleher M, et al. Exploring patient experiences of participating in a group exercise class for the management of nonspecific shoulder pain. Physiother Theory Pract 2018; 34: 464–471. [DOI] [PubMed] [Google Scholar]
- 19.Cuff A, Littlewood C. Subacromial impingement syndrome – what does this mean to and for the patient? A qualitative study. Musculoskelet Sci Pract 2018; 33: 24–28. [DOI] [PubMed] [Google Scholar]
- 20.Gilbert AW, Hauptmannova I, Jaggi A. The use of assistive technology in shoulder exercise rehabilitation – a qualitative study of acceptability within a pilot project. BMC Musculoskelet Disord 2018; 19: 133–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hanratty CE, Kerr DP, Wilson IM, et al. Physical therapists’ perceptions and use of exercise in the management of subacromial shoulder impingement syndrome: Focus group study. Phys Ther 2016; 96: 1354–1363. [DOI] [PubMed] [Google Scholar]
- 22.Lau AY, Piper K, Bokor D, et al. Challenges during implementation of a patient-facing mobile app for surgical rehabilitation: Feasibility study. JMIR Hum Factors 2017; 4: e31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Littlewood C, Malliaras P, Mawson S, et al. Patients with rotator cuff tendinopathy can successfully self-manage, but with certain caveats: A qualitative study. Physiotherapy 2014; 100: 80–85. [DOI] [PubMed] [Google Scholar]
- 24.Littlewood C, Mawson S, May S, et al. Understanding the barriers and enablers to implementation of a self-managed exercise intervention: A qualitative study. Physiotherapy 2015; 101: 279–285. [DOI] [PubMed] [Google Scholar]
- 25.Minns Lowe CJ, Moser J, Barker KL. Why participants in the United Kingdom Rotator Cuff Tear (UKUFF) trial did not remain in their allocated treatment arm: A qualitative study. Physiotherapy 2018; 104: 224–231. [DOI] [PubMed] [Google Scholar]
- 26.Nyman P, Palenius K, Panula H, et al. Patients’ experiences of shoulder problems prior to and following intervention. Physiother Theory Pract 2012; 28: 221–231. [DOI] [PubMed] [Google Scholar]
- 27.Palenius K, Nyman P. Physiotherapists’ perceptions of their work with shoulder patients: A focus group study in Finland. Eur J Physiother 2015; 17: 132–137. [Google Scholar]
- 28.Palenius KG, Nyman PC. Expectations and experiences of physiotherapeutic practice among patients with shoulder problems. Eur J Physiother 2018; 20: 58–64. [Google Scholar]
- 29.Sandford FM, Sanders TAB, Lewis JS. Exploring experiences, barriers, and enablers to home- and class-based exercise in rotator cuff tendinopathy: A qualitative study. J Hand Ther 2017; 30: 193–199. [DOI] [PubMed] [Google Scholar]
- 30.Sole G, Mącznik AK, Ribeiro DC, et al. Perspectives of participants with rotator cuff-related pain to a neuroscience-informed pain education session: An exploratory mixed method study. Disabil Rehabil 2020; 42: 1870–1879. [DOI] [PubMed] [Google Scholar]
- 31.Stamp AS, Pedersen LL, Ingwersen KG, et al. Behavioural typologies of experienced benefit of psychomotor therapy in patients with chronic shoulder pain: A grounded theory approach. Complement Ther Clin Prac 2018; 31: 229–235. [DOI] [PubMed] [Google Scholar]
- 32.Franz E, Uhazie R. Barriers to adherence of home exercise programs in patients with shoulder pathology. Florida, USA: Florida Gulf Coast University, 2018. [Google Scholar]
- 33.White J, Auliffe SM, Jepson M, et al. ‘There is a very distinct need for education’ among people with rotator cuff tendinopathy: An exploration of health professionals’ attitudes. Musculoskelet Sci Pract 2020; 45: 102103. [DOI] [PubMed] [Google Scholar]
- 34.Cridland K, Pritchard S, Rathi S, et al. ‘He explains it in a way that I have confidence he knows what he is doing’: A qualitative study of patients’ experiences and perspectives of rotator-cuff-related shoulder pain education. Musculoskelet Care 2021; 19: 217–231. [DOI] [PubMed] [Google Scholar]
- 35.Kiely D. Group versus individual treatment in the management of rotator cuff tendinopathy in primary care. Masters thesis, University of Limerick, 2021. [Google Scholar]
- 36.Stutz T. (How) can an app support physiotherapy for frozen shoulder patients? In Proceedings of INTERACT 2019: 17th IFIP TC13 international conference on human–computer interaction, Paphos, Cyprus, 2019, Part 1, pp. 163–183. [Google Scholar]
- 37.Ulack C, Suarez J, Brown L, et al. What are people that seek care for rotator cuff tendinopathy experiencing in their daily life? J Patient Exp 2022; 9: 23743735211069811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pawson R. Digging for nuggets: how ‘bad’ research can yield ‘good’ evidence. Int J Soc Res Methodol 2006; 9: 127–142. [Google Scholar]
- 39.Munn Z, Porritt K, Lockwood C, et al. Establishing confidence in the output of qualitative research synthesis: the ConQual approach. BMC Med Res Methodol 2014; 14: 108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lewin S, Glenton C, Munthe-Kaas H, et al. Using qualitative evidence in decision making for health and social interventions: An approach to assess confidence in findings from qualitative evidence syntheses (GRADE-CERQual). PLoS Med 2015; 12: e1001895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med 2009; 6: e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Miles C, Arden-Close E, Thomas M, et al. Barriers and facilitators of effective self-management in asthma: Systematic review and thematic synthesis of patient and healthcare professional views. NPJ Prim Care Respir Med 2017; 27: 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.O’Connell S, McCarthy VJC, Savage E. Self-management support preferences of people with asthma or chronic obstructive pulmonary disease: A systematic review and meta-synthesis of qualitative studies. Chronic Illn 2019; 1742395319869443. [DOI] [PubMed] [Google Scholar]
- 44.Frost J, Garside R, Cooper C, et al. A qualitative synthesis of diabetes self-management strategies for long term medical outcomes and quality of life in the UK. BMC Health Serv Res 2014; 14: 348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Michie S, Johnston M, Francis J, et al. From theory to intervention: Mapping theoretically derived behavioural determinants to behaviour change techniques. Appl Psychol 2008; 57: 660–680. [Google Scholar]
- 46.Dineen-Griffin S, Garcia-Cardenas V, Williams K, et al. Helping patients help themselves: A systematic review of self-management support strategies in primary health care practice. PLoS One 2019; 14: e0220116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rotheram-Borus MJ, Ingram BL, Swendeman D, et al. Adoption of self-management interventions for prevention and care. Prim Care 2012; 39: 649–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wade DT, Halligan PW. Do biomedical models of illness make for good healthcare systems? Br Med J 2004; 329: 1398–1401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Dean BJ, Gwilym SE, Carr AJ. Why does my shoulder hurt? A review of the neuroanatomical and biochemical basis of shoulder pain. Br J Sports Med 2013; 47: 1095–1104. [DOI] [PubMed] [Google Scholar]
- 50.Cicutto L. Review: Self-management education improves outcomes in children and adolescents with asthma. Evid Based Nurs 2003; 6: 106. [PubMed] [Google Scholar]
- 51.Stoilkova A, Janssen DJA, Wouters EFM. Educational programmes in COPD management interventions: A systematic review. Respir Med 2013; 107: 1637–1650. [DOI] [PubMed] [Google Scholar]
- 52.Mohamed A, Staite E, Ismail K, et al. A systematic review of diabetes self-management education interventions for people with type 2 diabetes mellitus in the Asian Western Pacific (AWP) region. Nurs Open 2019; 6: 1424–1437. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Campbell F, Lawton J, Rankin D, et al. Follow-up support for effective type 1 diabetes self-management (the FUSED model): A systematic review and meta-ethnography of the barriers, facilitators and recommendations for sustaining self-management skills after attending a structured education programme. BMC Health Serv Res 2018; 18: 898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Russell S, Ogunbayo OJ, Newham JJ, et al. Qualitative systematic review of barriers and facilitators to self-management of chronic obstructive pulmonary disease: Views of patients and healthcare professionals. NPJ Prim Care Respir Med 2018; 28: 2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Yadav UN, Lloyd J, Hosseinzadeh H, et al. Facilitators and barriers to the self-management of COPD: A qualitative study from rural Nepal. BMJ Open 2020; 10: e035700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Lewinski AA, Shapiro A, Gierisch JM, et al. Barriers and facilitators to implementation of epilepsy self-management programs: A systematic review using qualitative evidence synthesis methods. Syst Rev 2020; 9: 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Main CJ, Buchbinder R, Porcheret M, et al. Addressing patient beliefs and expectations in the consultation. Best Pract Res Clin Rheumatol 2010; 24: 219–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vallis M. Are behavioural interventions doomed to fail? Challenges to self-management support in chronic diseases. Can J Diabetes 2015; 39: 330–334. [DOI] [PubMed] [Google Scholar]
- 59.Atkins L, Francis J, Islam R, et al. A guide to using the theoretical domains framework of behaviour change to investigate implementation problems. Implement Sci 2017; 12: 77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Araújo-Soares V, Hankonen N, Presseau J, et al. Developing behavior change interventions for self-management in chronic illness: An integrative overview. Eur Psychol 2019; 24: 7–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.French SD, Green SE, O’Connor DA, et al. Developing theory-informed behaviour change interventions to implement evidence into practice: A systematic approach using the theoretical domains framework. Implement Sci 2012; 7: 38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Barnett-Page E, Thomas J. Methods for the synthesis of qualitative research: A critical review. BMC Med Res Methodol 2009; 9: 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-cre-10.1177_02692155221108553 for Barriers and facilitators related to self-management of shoulder pain: a systematic review and qualitative synthesis by Aidan O'Shea, Jonathan Drennan, Chris Littlewood, Helen Slater, Julius Sim, and Joseph G. McVeigh in Clinical Rehabilitation