Abstract
A male in his late 70s with a history of an uncomplicated kidney transplantation 20 years prior was brought to the Emergency Department after experiencing blunt abdominal trauma following a motor vehicle collision. Imaging revealed a large perinephric haematoma, a retroperitoneal haematoma and multiple fractures. He was admitted to the intensive care unit where a renal haematoma was found to be expanding with ultrasonography (US) and developed renal dysfunction including anuria and hyperkalemia. His creatinine rose to twice his baseline and Doppler US showed elevated resistive indices, confirming extrinsic compression and causing a Page phenomenon. An open surgical exploration through the upper aspect of his Gibson incisional scar was performed followed by evacuation of the haematoma. An intraoperative US was done demonstrating good flow in the renal vessels. His postoperative course was uncomplicated and was discharged home with renal function back to baseline. On follow-up, he continued to have a good renal function.
Keywords: Transplantation, Ultrasonography, Renal transplantation, Dialysis, Renal medicine
Background
Page kidney or Page phenomenon is a rare but treatable phenomenon resulting from extrinsic compression of the renal parenchyma due to mass effect and often leads to secondary hypertension. The mechanism seems to begin with resultant hypoperfusion of the kidney leading to activation of the renin–angiotensin–aldosterone system (RAAS), as evidenced by elevated renin in the plasma and venous blood from the affected kidney and normalization of blood pressure following nephrectomy.1 Since the kidneys are surrounded by a fibrous capsule with little space, any fluid collection under it can easily cause compression of the parenchyma and reduced blood flow. It was first described by Irving Page in 1939 in a series of experiments wrapping canine kidneys in cellophane to avoid direct damage to the renal tissue where he discovered that hypertension developed in these animals after wrapping caused a perinephritic inflammatory response that facilitated the formation of a fibrocollagenous shell leading to compression and ischemia.2 In 1955, Engel and Page described the first case of Page kidney in a 19-year-old football player presenting withflank trauma and a 2-year history of hypertension, who was found to have a subcapsular haematoma that was subsequently resolved after resection of the kidney. This phenomenon is most commonly seen in traumatic cases, usually due to a buildup of blood or other fluid source.3 More common scenarios leading to this phenomenon are usually due to blunt trauma (ie, sports injuries) or iatrogenic (ie, biopsies), while spontaneous (ie, anticoagulation, aneurysms and vasculitis) are less common. Other rarer non-bleeding causes due to extrinsic compression include lymphoceles, cysts and retroperitoneal paragangliomas.4–8
Page kidney can present insidiously or acutely as a new-onset hypertensive event. Workup usually includes an ultrasound of the kidneys and contrast-enhanced CT to visualise perinephric fluid collections. Creatinine can be used to aid in the diagnosis in cases where the patient is dependent solely on one kidney (ie, transplanted kidney patients) as the other normal kidney can usually compensate.4
Though management can often restore renal function in most Page kidney patients, in the setting of renal transplants, the graft is commonly lost if immediate surgical intervention is not performed. Page kidney after kidney transplantation was first described in 1976 and was shown to cause an acute deterioration in graft function seemingly mimicking rejection but was coined as ‘pseudorejection’.9 Because of its rarity, most of the literature discussing Page kidney consists of case reports investigating different risk factors and treatments that lead to better outcomes. Here, we report one case of Page phenomenon following trauma in a renal allograft patient at our institution. The literature was also reviewed.
To our knowledge, this is the third case reported of Page kidney that was able to be saved after blunt trauma through early surgical intervention. Given that these patients rely solely on their renal graft, we recommend that immediate diagnosis be made with either CT imaging or Doppler US and to maintain a low threshold for early surgical intervention in renal transplant patients with confirmed Page kidney following blunt trauma considering the high risk of graft loss and the excellent prognosis seen in patients with early surgical management.
Case presentation
A male in his late 70 s with a medical history significant for diabetes mellitus (DM), hypertension, hyperparathyroidism and end-stage renal disease secondary to focal segmental glomerulosclerosis status post-transplant of a deceased-donor kidney (on the right iliac fossa) 20 years prior was brought to the Emergency Department after experiencing blunt trauma.
The patient was admitted directly to the trauma bay as a level 1 after a high-speed motor vehicle collision. Standardised Advanced Trauma Life Support (ATLS) algorithm was performed.10–12 Primary survey was intact, secondary survey revealed severe chest and abdominal tenderness. After resuscitation and stabilisation, a pan-CT scan showed multiple fractures in the pelvis, ribs and sternum in addition to a large perinephric haematoma (9.8 cm) and a retroperitoneal haematoma with signs of active bleeding (figures 1–3).13 14 Patient was transferred to the burn and trauma intensive care unit. After a few hours, the patient showed deterioration of renal function with hyperkalemia, rising creatinine, haematuria and oliguria. An ultrasonography (US) was performed showing reversal of diastolic flow in the main renal artery and signs of compression, consistent with increasing resistance to inflow secondary to pressure from the haematoma (figure 4A–B), and the decision was made to go to the operating room.
Figure 1.
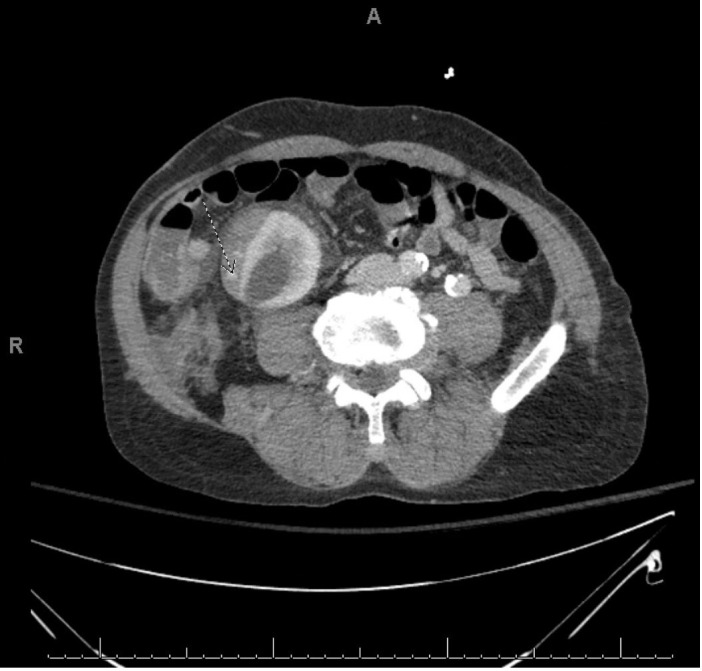
CT image showing perinephric subcapsular haematoma measuring 9.8 cm in diameter located over the right iliac fossa with signs of active contrast extravasation, consistent with active haemorrhage.
Figure 2.

CT image highlighting the retroperitoneal haematoma with foci of contrast extravasation suggestive of active haemorrhage, which could be either venous or arterial.
Figure 3.

Coronal CT image showing the large 9.8 cm subcapsular haematoma over the transplanted renal allograft.
Figure 4.
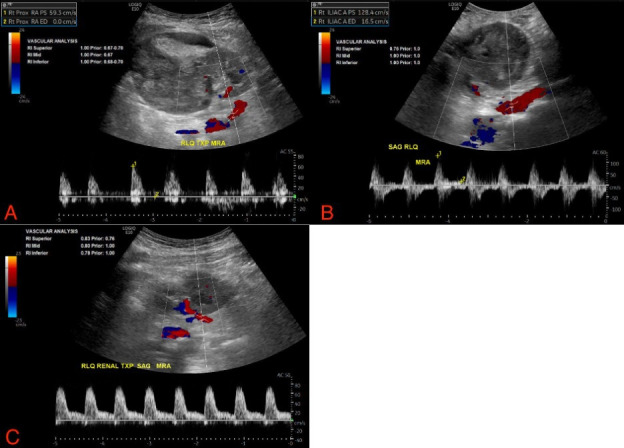
US at the time of admission (A), followed by a few hours prior to surgery (B) showing loss of forward diastolic flow and US postoperatively (C) with downtrending resistive indices.
Differential diagnosis
New-onset hypertension with flank trauma should always raise concern for Page kidney, as was the case discussed here. However, with the history of trauma, recent use of contrast for CT imaging, rising creatinine and a dropping haematocrit, consideration of active bleeding from the haematoma as well contrast-induced nephropathy is necessary. Imaging is crucial to identifying this phenomenon. Less likely, the differential also includes renal artery stenosis, nephrosclerosis, juxtaglomerular cell tumour or malignant hypertension in the differential diagnosis. In a transplant patient, the differential should also include organ rejection, acute tubular necrosis and renal vein thrombosis.
Treatment
The transplant surgery team decided to perform surgical evacuation of the subcapsular haematoma due to concern of the Page kidney syndrome and requirement of prompt intervention. The patient was scheduled as an emergency case, where an intraoperative US was first performed to localise the perirenal haematoma. We then entered using the previous renal incision. The retroperitoneum was accessed and the perirenal haematoma successfully visualised. Clots around the kidney were removed with irrigation and gentle dissection. Intraoperative US was performed showing improvement in resistive indices and better perfusion of the kidney. Renal biopsy was not considered given that there was no suspicion for acute rejection and the increased risk of bleeding in a patient with a disrupted renal capsule.
Postoperatively, the patient underwent another US, which revealed downtrending resistive indices (figure 4C). Immediately, there was return of good urine output and further US showing improving patency of the renal vessels. In his follow-up US, his resistive indices and creatinine levels normalised to his baseline and the patient subsequently recovered from his multiple fractures requiring rehabilitation services.
Outcome and follow-up
At his 2-week follow-up with transplant nephrology, the patient continued to be well within his baseline range creatinine. His incision was clean, dry and intact and staples were removed at this time. At his 5-month follow-up, creatinine continued to be within his baseline.
Discussion
Despite its rarity, some of the few cases of Page kidney have been reported in the transplanted population. However, most of these cases are due to iatrogenic causes, mainly biopsies, and, less frequently, trauma.4 Surgical decompression has been found to be the intervention of choice and has resolved it successfully in about 80% of the cases reported in the literature.5 15–24 However, even with surgical evacuation, the results could be unfavourable with still a high risk of losing the graft. There have been very few cases reporting successful resolution in Page kidney due to blunt trauma. We believe that a high suspicion for this diagnosis as well as rapid surgical decompression is the best approach for success, as in our case. We present the third successful rescue of a Page kidney due to blunt trauma in a transplant patient. In our case, we report an older male whose total dependence on his graft resulted in a quick deterioration over the span of a few hours on arrival to the hospital. We demonstrate how quickly and progressive a subcapsular haematoma can impair renal functioning and cause electrolytic abnormalities in a renal allograft patient
CT of the abdomen and pelvis is the preferred modality as it is more sensitive for detecting smaller haematomas. US of the abdomen is more useful to track for any changes in the growth of the haematoma which can help guide surgeons in determining the need for evacuation. In addition, we also used Doppler US to monitor for reversal of diastolic blood flow keep track of any changes to resistive indices in the renal vessels both preoperatively and postoperatively. The management approach to Page kidney varies according to the patient and includes medical antihypertensive therapy with observation, percutaneous drainage of the renal haematoma and, ultimately decompression via open surgical evacuation of the haematoma if renal deterioration is rapid and unmanageable. Hypertension can be managed medically though there are no official guidelines on the duration of therapy in these cases. Elevations in blood pressure are permanent in some patients and lifelong treatment is the best approach.25 Theoretically, it would be best to use an antihypertensive inhibiting the RAAS system such as an angiotensin-converting enzyme inhibitor or angiotensin receptor blockers.3 Percutaneous drainage is most recommended in subcapsular haematomas that are relatively new, often less than 3 weeks duration as it has shown better success rates.26 In some cases, a chronic subcapsular haematoma can develop often with a fibrotic pseudocapsule leading to long-term hypertension that would warrant capsulectomy or even total nephrectomy in patients who still possess another kidney as it has been shown to cure hypertension in most patients.26
If renal function is stable even with imaging findings consistent with a subcapsular haematoma, the benefits of waiting for spontaneous reabsorption should be weighed against the risk of allograft loss if surgical evacuation is not performed immediately. In our experience, if there was an obvious cause of new perirenal bleeding with evidence of renal dysfunction, then we should minimise any delay and proceed to surgical evacuation immediately as even a small amount of extrinsic compression can hinder renal perfusion due to reduced elasticity and graft capsule thickening.8 Our case is one of the few demonstrating that early surgical drainage can restore and save a renal graft with an excellent prognosis. As the incidence rate of renal transplants rises worldwide, there is a higher risk of Page kidney both due to blunt trauma as well from postprocedural biopsies and it is essential to consider the specific signs discussed here as well as the imaging modalities used to prevent loss of the renal allograft and restore renal function. Immediate surgical evacuation is currently the best management approach when a renal transplant patient begins to develop renal dysfunction symptoms including anuria, increasing creatinine levels, localised pain over the graft and haemodynamic instability due to active haemorrhaging into the haematoma.
Learning points.
Page kidney is a rare cause of new-onset hypertension. A patient with evidence of abdominal trauma, new-onset hypertension and evidence of haemodynamic instability should always raise concern for Page kidney.
A high degree of suspicion of this phenomenon is especially warranted in patients with transplanted kidneys due to their sole reliance on their graft for renal function. Acute pain over the graft can often be an early symptom in these patients.
Prompt surgical intervention is crucial to save the graft and avoid long-term complications such as restarting haemodialysis.
Imaging with either ultrasonography or CT is crucial in an atypical patient without trauma or hypertension along with the use of Doppler US resistive indices, which are elevated in those with renal parenchymal compression.
In a renal transplant patient, serum levels of creatinine and electrolytic imbalances are more apparent given the sole dependence on the allograft.
Footnotes
Twitter: @kareninaqx
Contributors: KP-S first proposed the idea to report this rare case seen at our institution to Mr. RC. Mr. RC was the primary author involved in drafting the case report, acquisition of data, literature review and analysis/interpretation of data. Mr. RC is the guarantor who controlled the decision to publish and accepts full responsibility for the finished case report. Dr KP-S also aided in several aspects of the case report including analysis and/or interpretation of data, literature search and revision of the manuscript critically for important intellectual content. Dr KP-S, Dr RK and Dr AN were the primary team involved in the management of this patient during their hospitalisation. All authors approved the version of the case report to be published.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Consent obtained directly from patient(s).
References
- 1.Dopson SJ, Jayakumar S, Velez JCQ. Page kidney as a rare cause of hypertension: case report and review of the literature. Am J Kidney Dis 2009;54:334–9. 10.1053/j.ajkd.2008.11.014 [DOI] [PubMed] [Google Scholar]
- 2.PAGE IH. The production of persistent arterial hypertension by cellophane perinephritis. J Am Med Assoc 1939;113:2046–8. 10.1001/jama.1939.02800480032008 [DOI] [Google Scholar]
- 3.Vaidya PN, Rathi BM, Finnigan NA. In: StatPearls Internet. Treasure Island FL: StatPearls Publishing, 2022. http://www.ncbi.nlm.nih.gov/books/NBK482486/ [Google Scholar]
- 4.Morgan TA, Chandran S, Burger IM, et al. Complications of ultrasound-guided renal transplant biopsies. Am J Transplant 2016;16:1298–305. 10.1111/ajt.13622 [DOI] [PubMed] [Google Scholar]
- 5.Takahashi K, Prashar R, Putchakayala KG, et al. Allograft loss from acute page kidney secondary to trauma after kidney transplantation. World J Transplant 2017;7:88–93. 10.5500/wjt.v7.i1.88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gibney EM, Edelstein CL, Wiseman AC, et al. Page kidney causing reversible acute renal failure: an unusual complication of transplant biopsy. Transplantation 2005;80:285–6. 10.1097/01.TP.0000165097.42243.3F [DOI] [PubMed] [Google Scholar]
- 7.Kliewer MA, Carroll BA. Ultrasound case of the day. page kidney phenomenon in a transplanted kidney after biopsy. Radiographics 1991;11:336–7. 10.1148/radiographics.11.2.2028069 [DOI] [PubMed] [Google Scholar]
- 8.Mak J, He B. Page kidney phenomenon following kidney graft biopsy: a medical emergency. Int J Surg Surgical Proced 2017;2 https://www.graphyonline.com/archives/IJSSP/2017/IJSSP-127/index.php?page=abstract 10.15344/2456-4443/2017/127 [DOI] [Google Scholar]
- 9.Cromie WJ, Jordan MH, Leapman SB. Pseudorejection: the page kidney phenomenon in renal allografts. J Urol 1976;116:658–9. 10.1016/S0022-5347(17)58953-3 [DOI] [PubMed] [Google Scholar]
- 10.American College of Surgeons . Student Course Manual. In: Advanced trauma life support: student course manual. Tenth Chicago, 2018: 391 p. [Google Scholar]
- 11.Lalwani S, Gera S, Sawhney C, et al. Mortality profile of geriatric trauma at a level 1 trauma center. J Emerg Trauma Shock 2020;13:269–73. 10.4103/JETS.JETS_102_18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jacobs DG, Plaisier BR, Barie PS, et al. Practice management guidelines for geriatric trauma: the East practice management guidelines work group. J Trauma 2003;54:391–416. 10.1097/01.TA.0000042015.54022.BE [DOI] [PubMed] [Google Scholar]
- 13.Mohamed H, Teoh K. Outcome of selective CT vs. pan-CT scan in elderly trauma patients: a retrospective cohort study in a level 1 trauma center. Chin J Traumatol 2021;24:249–54. 10.1016/j.cjtee.2021.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Stengel D, Ottersbach C, Matthes G, et al. Accuracy of single-pass whole-body computed tomography for detection of injuries in patients with major blunt trauma. CMAJ 2012;184:869–76. 10.1503/cmaj.111420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pan G, Ahmed F, Campsen J. Page kidney phenomenon in kidney allograft following abdominal trauma. Urol Case Rep 2020;32:101274. 10.1016/j.eucr.2020.101274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sedigh O, Lasaponara F, Dalmasso E, et al. Subcapsular hematoma causing anuria after renal graft trauma. Exp Clin Transplant 2017;15:578–80. 10.6002/ect.2015.0073 [DOI] [PubMed] [Google Scholar]
- 17.Canllavi E, Teigell J, Trujillo H, et al. Acute page kidney after angioplasty in kidney transplant allografts. Clin Kidney J 2021;14:1980–2. 10.1093/ckj/sfab064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gambhir A, Elangovan I, Simon S, et al. Postrenal Transplant Allograft "Page Kidney" Identified and Salvaged using 99mTc-diethylenetriaminepentaacetic acid Renogram and Single-photon Emission-computed Tomography. Indian J Nucl Med 2018;33:161. 10.4103/ijnm.IJNM_155_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McFadden JD, Hawksworth JS. Page kidney: an unusual complication of a renal transplant biopsy. Case Rep Urol 2018;2018 ::e8768549 10.1155/2018/8768549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Iovino D, Ietto G, Soldini G, et al. Page kidney phenomenon following kidney transplant, secondary to acute postsurgical sub capsular hematoma compression: a case report. Transpl Rep 2017;2:15–18. 10.1016/j.tpr.2017.10.001 [DOI] [Google Scholar]
- 21.Howlader A, Thajudeen B, Kodali L, et al. Page kidney following Nephroureteral stent placement in a renal transplant allograft. Prog Transplant 2019;29:95–6. 10.1177/1526924818817014 [DOI] [PubMed] [Google Scholar]
- 22.Kapoor R, Zayas C, Mulloy L. Recurrence of acute page kidney in a renal transplant allograft. Case Rep Med 2016:e3898307. 10.1155/2016/3898307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bora F, Yılmaz F, Koçak H. Page Kidney After Traumatic Hematoma. Turk Nephrol Dial Transplant [Internet], 2016. Available: http://turkjnephrol.org/en/page-kidney-after-traumatic-hematoma-135741 [Accessed 04 Feb 2022].
- 24.Rajagopal P, Chughtai SA, Khan S. Traumatic injury to renal allograft, literature review and case series trauma in renal transplant Recipient- a case report, 2018. Available: https://www.iomcworld.org/articles/traumatic-injury-to-renal-allograft-literature-review-and-case-series-trauma-in-renal-transplant-recipient-a-case-report-18959.html [Accessed 04 Feb 2022].
- 25.Smyth A, Collins CS, Thorsteinsdottir B, et al. Page kidney: etiology, renal function outcomes and risk for future hypertension. J Clin Hypertens 2012;14:216–21. 10.1111/j.1751-7176.2012.00601.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Watts RA, Hoffbrand BI. Hypertension following renal trauma. J Hum Hypertens 1987;1:65–71. [PubMed] [Google Scholar]


