Abstract
Observational studies have indicated an association between iron status and risk of sepsis and COVID-19. We estimated the effect of genetically-predicted iron biomarkers on risk of sepsis and risk of being hospitalized with COVID-19, performing a two-sample Mendelian randomization study. For risk of sepsis, one standard deviation increase in genetically-predicted serum iron was associated with odds ratio (OR) of 1.14 (95% confidence interval [CI] 1.01–1.29, P = 0.031). The findings were supported in the analyses for transferrin saturation and total iron binding capacity, while the estimate for ferritin was inconclusive. We found a tendency of higher risk of hospitalization with COVID-19 for serum iron; OR 1.29 (CI 0.97–1.72, P = 0.08), whereas sex-stratified analyses showed OR 1.63 (CI 0.94–2.86, P = 0.09) for women and OR 1.21 (CI 0.92–1.62, P = 0.17) for men. Sensitivity analyses supported the main findings and did not suggest bias due to pleiotropy. Our findings suggest a causal effect of genetically-predicted higher iron status and risk of hospitalization due to sepsis and indications of an increased risk of being hospitalized with COVID-19. These findings warrant further studies to assess iron status in relation to severe infections, including the potential of improved management.
Subject terms: Genetics, Immunology, Diseases, Medical research
Introduction
Iron is an essential element in various physiological processes, including immune function, metabolism and erythropoiesis1,2. Deviations in iron status (e.g. iron deficiency or iron overload) can have considerable health implications and iron status deviations show substantial sex differences with women more at risk of iron deficiency1,3. Iron status can be assessed clinically by using serum iron, transferrin saturation (TSAT), total iron binding capacity (TIBC) and ferritin3,4. A growing body of evidence has demonstrated an essential role of systemic and cellular iron-regulating mechanisms in protecting hosts from infections and most pathogens depend on iron for their pathogenicity2. Observational studies have indicated an association between iron status and risk of severe infections, where both low iron status5,6 and high iron status7–9 have been linked to increased risk10,11. Sepsis is the life-threatening dysregulated host response to infection often leading to multi-organ failure and death12. Patients with severe COVID-19 are defined as septic because they share pathophysiological and clinical features with sepsis patients13. Studies related to COVID-19 found evidence that iron deficiency measured at hospitalization14, or low serum iron and TSAT but high ferritin15, were linked to severe COVID-19. On the other hand, excess serum iron, TSAT and lower TIBC (i.e. indication of iron overload) and hyperferritinemia have been associated with critical illness from COVID-1916,17. In a study examining nutritional status in European populations, there were indications of low iron status linked to higher mortality from COVID-1918. There is evidence of sex differences in incidence and outcomes of COVID-19 infection19–21. Few studies have evaluated sex differences in iron status at time of infection. In a small study iron status was lower in female patients when measured at hospitalization due to COVID-1917.
A key limitation of observational studies is that they are prone to bias due to confounding and reverse causation. Mendelian randomization (MR) studies can overcome these limitations by using genetic variants associated with the exposures as instrumental variables. Because genetic variants are distributed randomly at conception, the risk of confounding (e.g. from lifestyle factors) and reverse causation (i.e. that the disease affects levels of the exposure) is greatly reduced22. A recent MR study found a positive association between genetically-predicted high levels of iron biomarkers and risk of sepsis23, but a more recent set of genetic instruments for iron status has since been published24. No study has evaluated the role of iron status on the risk of COVID-19 in an MR framework and there is a lack of studies assessing sex differences25 using sex-stratified MR analyses.
Leveraging data from large genome-wide association studies (GWAS), we aimed to evaluate the association between genetically-predicted iron status biomarkers and risk of being hospitalized with sepsis or COVID-19. In addition, by using sex specific summary-level data on iron status and COVID-19 outcomes, we assessed sex differences in the associations between genetically-predicted iron status and risk of hospitalization due to COVID-19.
Methods
We performed a two-sample MR study to estimate the effect of genetically-predicted markers of iron status on risk of sepsis and COVID-19 outcomes. None of the iron biomarkers reflect iron status perfectly and iron status in populations is challenging to assess3,4. Ferritin is widely used to assess global iron stores but is heavily influenced by inflammation3,4. Serum iron is a measure of the fraction of iron that circulates which is readily available and most of it is bound to transferrin. Serum iron is subject to diurnal variation and is affected by fasting status. By measuring the total number of binding sites for iron atoms on transferrin, we calculate the TIBC. TSAT reflects the amount of binding sites on transferrin occupied with iron (calculated as [Serum iron]/[TIBC]%). The normal range is narrow, which is attributed to lower physiological variation than the other iron biomarkers. Low serum iron, low TSAT, low ferritin and high TIBC reflect low iron status. Elevated serum iron, TSAT and ferritin and low TIBC indicate high iron status. The iron in circulation turns over very quickly, especially during infection and inflammation and in clinical conditions with tissue destruction or repeated transfusions4.
Genetic instruments for iron status
Iron status was the exposure of interest and we ran the analyses for the four iron biomarkers serum iron, TSAT, TIBC and ferritin. The genetic instruments for the iron biomarkers were collected from a GWAS published in 2021 of 246,139 participants of European ancestry24. To validate a genetic instrument for the use in MR analysis the three MR assumptions must be met. Assumption (1) The SNPs are directly associated with the exposure (i.e. strongly associated (P-value < 5e−8) with at least one iron biomarker). Assumption (2) The SNPs are not related to exposure-outcome confounders (i.e. they should share no common cause with sepsis or COVID-19). Assumption (3) the SNPs affect the outcome only through the risk factor referred to as “no pleiotropy”22. F statistic above 10 was required for sufficient strength to limit bias due to weak instrumental variables26. Both exposure and outcome cohorts included individuals of European ancestry to reduce possible bias due to population stratification. Independence between SNPs were ensured by using the LD-reference panel of European populations in 10,000 kb windows and R2 < 0.01 that is included in the TwoSampleMR (version 0.5.6) package in R27. As a supplemental correction for correlated SNPs, the MendelianRandomization package (version 0.6.0) in R was implemented using generalized weighted linear regression28. Sex-specific effects for each biomarker were extracted from the same iron status GWAS using similar precautions for correlation between SNPs24. We estimated R2 in the TwoSampleMR package and calculated F-statistics using the formula F = ([n – k − 1]/k)([R2/1 − R2]), where n is the sample size, k is the number of included SNPs and R2 is the proportion of variance in the iron biomarkers explained by the genetic variance26. The included numbers of SNPs with F-statistics and explained variance of the iron biomarkers is presented for all and separately for men and women, in Supplementary Table S1.
Genetic susceptibility to sepsis and COVID-19
The genetic susceptibility to sepsis was collected from the IEU OpenGWAS with summary-level data obtained from the UK Biobank which included 10,154 sepsis cases, defined as explicit sepsis29 and 454,764 controls27,30. For COVID-19, we used data from the COVID-19 Host Genetics Initiative (HGI), which is an international collaboration to facilitate COVID-19 genetics research, release 5 (18 Jan 2021). We evaluated two different COVID-19 outcomes: Hospitalized COVID-19 patients (n = 4829) compared with non-hospitalized COVID-19 patients (n = 11,816), and hospitalized COVID-19 patients (n = 9986) compared with population-based controls (n = 1,877,672)31. For iron status related SNPs missing in the COVID-19 HGI GWASs, we used the LDproxy Tool32 to find potential LD proxy SNPs in European populations applying a threshold of R2 > 0.933. To ensure the selected proxy SNPs did not show any important pleiotropic associations, we used the PhenoScanner version 2. Additionally, we used the sex specific summary-level data on the two COVID-19 outcomes from UKBiobank only, using the NHLBI GRASP catalogue (18 June 2021). As with the non-stratified analyses, we used two different COVID-19 outcomes: Hospitalized COVID-19 cases compared with non-hospitalized COVID-19 patients (female cases: n = 1181, controls n = 7586; male cases: 1703, male controls: n = 6081), and hospitalized with COVID-19 compared to non-hospitalized population (female cases = 1181, controls = 248,118; male: cases = 1703, controls = 208,248)34. Unfortunately, we were not able to find sex-stratified summary-level on sepsis.
MR analyses
The main analysis was the inverse variance weighted (IVW) method which assumes all genetic instruments to be valid35 and a P-value of 0.05 was used for statistical significance. Three sensitivity analyses were conducted: weighted median, weighted mode and MR Egger regression. The weighted median orders MR estimates produced by each SNP by their magnitude weighted for their precision and gives an overall MR estimate based on the median value with standard errors estimated by bootstrapping. This method allows for some of the IVs to be invalid36. The weighted mode assumes that the most common causal effect is consistent with the true causal effect and allows some invalid instruments without biasing the MR estimate37. Directional horizontal pleiotropy refers to the presence of SNP effects on the outcome of interest through other biological pathways independent of the studied exposure38. MR Egger allows directional pleiotropic effects where some SNPs could be acting on the outcome through another pathway than the exposure of interest, but at the cost of statistical power. The MR Egger intercept test is a statistical test to evaluate the presence of unbalanced pleiotropy39. A consistent effect across these three sensitivity analyses and the IVW analysis suggests that pleiotropy did not bias the IVW estimate.
We used leave-one-out analyses to evaluate whether the IVW estimates were strongly driven by single SNPs35. To investigate potential heterogeneity and outliers, the MR PRESSO (Mendelian randomization Pleiotropy RESidual Sum and Outlier) was applied. MR PRESSO is a simulation-based heterogeneity and outlier test and computes a global test for horizontal pleiotropy. If horizontal pleiotropy is present MR PRESSO performs an outlier test for each genetic instrument with removal of all offending IVs that are due to horizontal pleiotropy before repeating the IVW without the outliers (distortion test). If both horizontal pleiotropy and outliers are detected the method applies a distortion test to investigate any difference in the causal estimate before and after outlier removal38,40. Additionally we used PhenoScanner version 241 to check if any of the genetic instruments had important pleiotropic associations, including sensitivity analyses where we omitted SNPs associated with potential pleiotropic pathways. To assess the theoretical potential of reverse causation, we performed bi-directional MR for sepsis and hospitalized COVID-19 applying the IWV MR method. For sepsis, we extracted four SNPs with a P-value < 5e−8. For COVID-19 HGI GWAS used as outcome in the main analysis only yielded one SNP as potential genetic instrument, instead we extracted 17 SNPs associated with risk of critical COVID-19 identified by Kousathanas et al.42.
All summary data used in this work are publicly available and with relevant ethical approvals24,30,31, and follow recommendations of reporting MR studies according to STROBE-MR guidelines43.
Results
The workflow of the MR analyses performed is summarized in Supplementary Fig. S1. We assured independence between SNPs using the LD reference panel from the 1000 Genomes project, which excluded two SNPs for serum iron and TSAT (rs748587164 and rs773570300), for TIBC we removed two SNPs (rs748587164 and rs1495743), and for ferritin we removed eight SNPs (rs551459670, rs762752083, rs750717575, rs745795585, rs535064984, rs34216132 and rs143041401) and rs2954029 for being palindromic. For the sex-specific analyses rs1799945 was removed from the TSAT analyses, for TIBC three SNPs were removed (rs1799945, rs17580, rs1495743) for both sexes for being palindromic. For the MR analyses using the COVID-19 HGI GWASs, we extracted two LD proxy SNPs for TIBC and four SNPs for ferritin. The list of SNPs included in each MR analysis is included in Supplementary Table S2A,B.
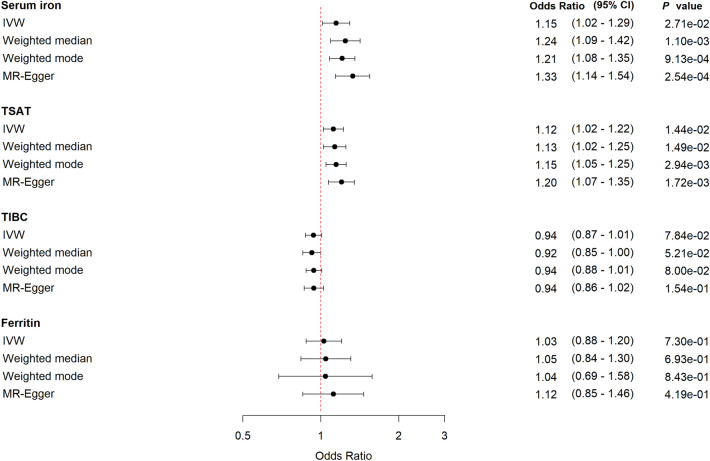
Sepsis
Increasing genetically-predicted levels of serum iron and TSAT levels point in the direction of increased risk of sepsis: Odds ratio (OR) 1.15 (95% confidence interval (CI) 1.01–1.29, P = 0.03) for each standard deviation (SD) (7.76 µmol/L) increase in serum iron; and OR 1.12 (95% CI 1.02–1.23, P = 0.01) per SD increase in TSAT (13.25%) (Fig. 1). The direction of effect for TIBC showed evidence of lower TIBC (i.e. indicating increased iron status) being associated with sepsis OR 0.94 (95% CI 0.87–1.01, P = 0.09). Ferritin showed inconclusive results. The sensitivity analyses supported the findings from the IVW analyses.
Figure 1.
Forest plot with MR estimates for risk of sepsis. CI confidence interval, IVW inverse variance weighted, TSAT transferrin saturation, TIBC total iron binding capacity.
Using PhenoScanner, we identified the SNP rs2228145, an instrument for serum iron, to be strongly associated with the IL6-receptor, and SNPs related to white blood cell count, which we considered a potential biasing pathway due to pleiotropy (Supplementary Table S3). In addition, some of the SNPs used were associated with BMI, CRP, coronary artery disease, triglyceride levels, cholesterol levels, blood pressure, diabetes 2 and glycosylated hemoglobin. MR estimates after omitting these SNPs for serum iron and ferritin on risk of sepsis and being hospitalized with COVID-19 versus non-hospitalized cases, rendered the same results for both iron biomarkers and both outcomes, but with reduced precision (Supplementary Tables S4,S5). The leave-one-out analyses yielded similar results, suggesting that the different potentially pleiotropic pathways did not substantially affect the results (Supplementary Fig. S1), and the MR Egger intercepts or MR PRESSO did not detect aggregated directional pleiotropy or outliers (Supplementary Tables S8, S9).
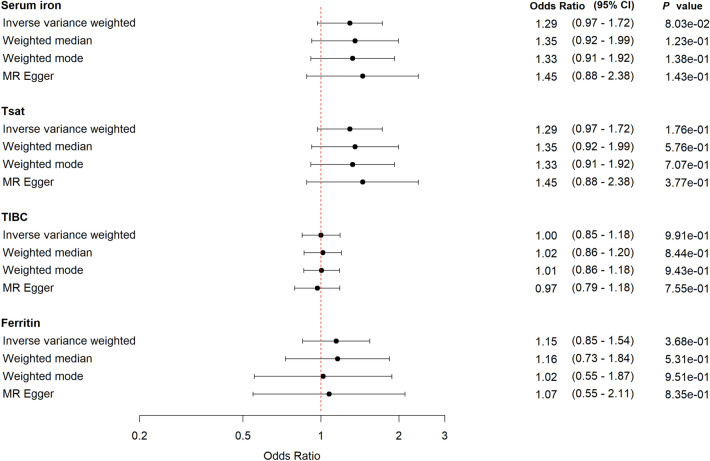
COVID-19
We found a suggestive relationship between genetically-predicted higher levels of serum iron and risk of being hospitalized with COVID-19 compared with non-hospitalized COVID cases; OR 1.29 (95% CI 0.97–1.72, P = 0.08) (Fig. 2). We show corresponding results for TSAT, but less pronounced. The sensitivity analyses supported the IVW analyses, leave-one-out plots, MR Egger intercepts and MR PRESSO suggested no pleiotropic effects or heterogeneity (Supplementary Fig. S2, Supplementary Tables S10, S11).
Figure 2.
Forest plot with MR estimates for risk of being hospitalized with COVID-19 compared to non-hospitalized COVID-19. CI confidence interval, IVW inverse variance weighted, TSAT transferrin saturation, TIBC total iron binding capacity.
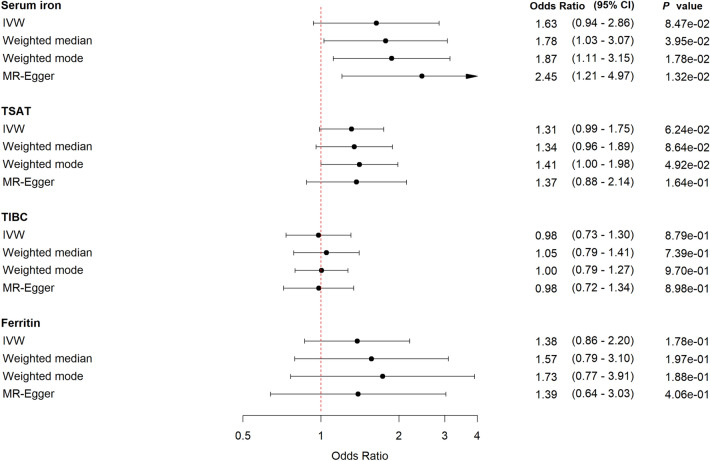
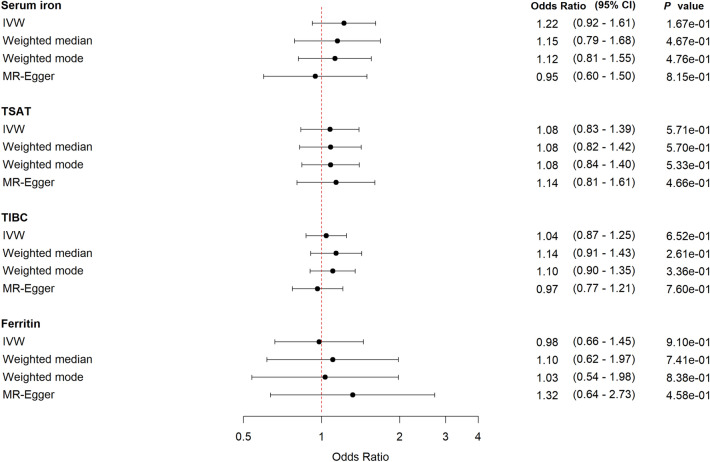
In the sex-stratified analyses, we show a tendency among women of a harmful effect of increasing genetically-predicted levels of serum iron; OR 1.63 (95% CI 0.94–2.86, P = 0.09) and TSAT; OR 1.31 (95% CI 0.99–1.75, P = 0.06). For TIBC and ferritin the estimates were uncertain (Fig. 3). The corresponding results for men were less pronounced and the wide confidence intervals made comparison between the sexes inappropriate (Fig. 4). The sensitivity analyses supported the main findings (Figs. 3, 4, Supplementary Tables S12, S13, Supplementary Figs. S3, S4).
Figure 3.
Forest plot for women with MR estimates for risk of being hospitalized with COVID-19 compared to non-hospitalized COVID-19. CI confidence interval, IVW inverse variance weighted, TSAT transferrin saturation, TIBC total iron binding capacity.
Figure 4.
Forest plot for men with MR estimates for risk of being hospitalized with COVID-19 compared to non-hospitalized COVID-19. CI confidence interval, IVW inverse variance weighted, TSAT transferrin saturation, TIBC total iron binding capacity.
There was no clear evidence that genetically-predicted levels of iron status biomarkers were associated with risk of being hospitalized with COVID-19 compared with the population including the sex-stratified analyses (Supplementary Figs. S5–S7).
Additionally, we performed two bi-directional MR analyses to assess the potential causal effect of sepsis on serum iron status and hospitalized COVID-19 on serum iron. The bi-directional MR analyses showed no significant relationship (Supplementary Tables S14, S15), leaving no evidence of a reverse causation.
Discussion
In this study we performed two-sample MR analyses to estimate the unconfounded effect of iron status on risk of sepsis and severe COVID-19 using data from large GWASs. The MR results provided some evidence that higher genetically-proxied iron load—reflected in higher levels of serum iron and TSAT, and lower levels of TIBC—were associated with increased risk of sepsis. For COVID-19, we found a trend for increased risk of being hospitalized with COVID-19 compared to non-hospitalized COVID-19 cases in subjects with genetically-predicted higher levels of serum iron. We included sex stratified analyses to assess potential sex differences in the effect of iron status on risk of COVID-19 hospitalizations, which provided some indication of a more pronounced harmful effect of high iron status among women compared with men, but with too little precision to strongly support a difference. The sensitivity analyses supported the overall findings. Genetic predisposition to sepsis or severe COVID-19 did not show any evidence of effect on serum iron levels.
Our results were consistent with previous observational studies on sepsis, including a prospective study from Turkey found higher serum iron in septic patients compared to healthy volunteers8. There is a substantial lack of prospective studies investigating the effect of iron status measured before the onset of the infection. In a prospective population-based cohort study from Norway, we found low iron status to be associated with increased risk of future bloodstream infections6. This is discordant to our MR results where higher genetically-predicted iron status is related to increased risk of sepsis and being hospitalized due to COVID-19, and could be attributed to differences in the epidemiological methods applied, such as residual confounding, but also limitations with the two-sample MR method used that is restricted to assess linear models44.
Few MR studies have explored iron status and risk of severe infections. An MR-study using iron related SNPs identified in the Genetics of Iron Status-consortia45 found evidence that higher serum-iron, TSAT and ferritin were related to increased risk of sepsis23. Using a more updated set of genetic instruments for iron status biomarkers, we replicated these findings for serum iron and TSAT, a tendency for TIBC, but not for ferritin. Another MR study found evidence of increased risk of skin and soft-tissue infections with higher serum iron levels46.
Patients with severe COVID-19 share many pathophysiological and clinical features with septic patients, and we found the COVID-19 HGI GWAS with the comparison of hospitalized COVID-19 patients to non-hospitalized COVID-19 patients to be most similar to sepsis patients as most septic patients are hospitalized in industrialized countries13,47. In a large-scale two-sample MR analysis aimed to evaluate the causal effects of a vast number of traits in severe COVID-19, they report in supplemental data that serum iron levels (using SNPs from the Genetics of Iron Status-consortia) yielded the same direction of effect as our results for risk of being hospitalized with COVID-19 versus non-hospitalized cases in the release five of the COVID-19 HGI dataset48. Observational studies that have investigated iron status at the time of infection, found evidence of low iron status being a risk factor for a severe course of COVID-1914. A case–control study with COVID-19 patients compared to non-COVID-19 patients showed lower serum iron and TSAT levels in patients with COVID-19 independently of severity. Whereas COVID-19 patients defined as severe and critical had substantially higher ferritin levels49. Some have linked COVID-19 to the hyperferritinemic syndromes which is associated with hyperinflammation50. We identified a tendency towards an increased risk of being hospitalized with COVID-19 in persons with genetically proxied higher iron status. Differences between our findings and those reported in observational studies could reflect the fact that associations between iron status and COVID-19 may be confounded by factors difficult to adjust for such as poor nutritional status4 or medical comorbidities associated with functional iron deficiency51. Despite numerous observational studies in COVID-19 patients, the role of iron status before the time of infection as well as changes in iron status during infection has not been ruled out and the same applies to sepsis. We hypothesize that individuals with higher iron status could be less able to handle the acute iron load seen during severe infections, leaving them more vulnerable to be hospitalized with sepsis and COVID-19.
The role of iron status in the context of infectious diseases has long been noted1,2,10,11. Both iron deficiency5,6, iron overload8 and iron fortification programs without adequate infection surveillance52, have been linked to increased risk of infections. To date, treatment with iron chelators in sepsis or COVID-19 have not been studied in any large RCT, although suggested as potential adjuvant therapy in several reviews53,54. Experimental models of sepsis studying different iron chelators, report promising anti-inflammatory and anti-bacterial effects55. One pilot study in 92 COVID-19 patients using oral and intranasal lactoferrin have shown promising results with faster clinical symptoms recovery and lower serum ferritin levels in patients with mild to moderate COVID-19 compared to controls56.
The pathway from iron status to risk of severe infections like sepsis and COVID-19 could be multifactorial, including long-term effects of iron status on immune functions and susceptibility to pathogens, but also adaptations in iron status at the time of infection2,11,53. We identified that iron status affects the risk of sepsis and the risk of being hospitalized with COVID-19, indicating that iron status before the time of infection interfere with the response to infection.
It is well established that iron status varies according to sex3,4. Observational studies have shown that men are more prone to a severe course of COVID-1920,21, leaving sex-stratified investigations important to reveal potential explanations for the sex differences25. We assessed sex specific summary-level data on iron status and COVID-19 outcomes and showed that there was some tendency that the effect of serum iron and TSAT was more pronounced among women. Another study looking at iron status at time of hospitalization for COVID-19 identified sex differences where female patients had significantly lower serum iron, TSAT and ferritin levels and higher TIBC levels compared to men, whereas the association with severity between serum iron and TSAT was observed in both sexes17.
Major strengths with our study include the use of large GWAS summary data for both iron status, sepsis and severe COVID-19. Our main MR estimates were similar using IVW, weighted median, weighted mode and MR Egger methods. We included bi-directional MR to ensure that there were no reverse causation. As MR studies could carry the risk of pleiotropy, we used various strategies to detect and account for the potential pleiotropy. Taken together, the overall conclusions of our study were less likely to be affected by bias due to pleiotropy. We used GWAS summary data from European ancestry to reduce confounding due to population stratification. The slight difference in estimation and confidence intervals between the different MR methods were expected and most likely do not represent actual differences57.
Several limitations should be considered in our study. First, the participants in our study are restricted to European ancestry and as both severe infections and iron deficiency are global concerns, our findings should be examined in other populations. Second, the sepsis phenotype has proven to be heterogeneous depending on how the causal pathogen act on the host immune functions and factors within the host58. Timing and correct treatment of infections before they evolve to sepsis, further access to organ supportive treatment in intensive care units and severity of sepsis might also be different. During the COVID-19 pandemic limited hospital resources and capacity might have influenced on hospitalizations. Third, iron status changes substantially during infection and inflammation, further exacerbated by tissue destruction and cell death. Iron status fluctuates during a lifetime, during periods of higher demand and need such as pregnancy and growth, in situations with increased losses (i.e. blood loss or critical illness), and due to chronical medical disorders4. Genetically-predicted iron status may not perfectly reflect this time-varying exposure59. The U-shaped risk relationship that has been proposed for the extremes of iron status10,17 might cause an attenuated association when evaluated in a linear model as in the two-sample MR methods. Non-linear MR methods could be more suitable to explore this U-shaped relationship but requires large GWAS with both measurements of iron biomarkers as well as the outcomes of interest44. However, observational studies measuring iron status at time of infection might be biased by the acute phase response leading to iron depletion and hyperferritinemia (i.e. reverse causation) which we avoided using an MR framework. Due to the MR methods’ use of genetic instruments, the possibility of confounding was limited. Using sex stratified summary-level data for both exposure and COVID-19 outcomes we were able to investigate potential sex differences in the associations.
In conclusion, our study leveraged large-scale summary data to explore the effects of iron status on risk of sepsis and severe COVID-19. Our findings suggest a causal association between high iron status and increased risk of sepsis and in verified cases of COVID-19 we identified a tendency of higher risk of being hospitalized in persons with higher iron status. We highlight the importance of sex specified summary-level data to assess potential sex differences in the associations. For being hospitalized with COVID-19 there were indications of a more pronounced effect of higher iron status in women compared to men. Future studies are needed to explore the exact mechanisms of iron status and severe infections with the potential of prevention management and treatment strategies.
Supplementary Information
Author contributions
R.M.M. and T.R. originated the research hypothesis and conceptual design. R.M.M. analyzed the data, R.M.M. and H.M.F. prepared tables and figures. R.M.M. drafted the manuscript. H.M.F., K.V.L., A.T.D., E.S., J.K.D., B.O.Å., L.T.G. and T.R. revised the manuscript. L.T.G., B.O.Å. and T.R. provided critical inputs in study methods and analyses. J.K.D. and T.R. supervised the study. All authors revised and approved the submission.
Funding
Open access funding provided by Norwegian University of Science and Technology. This work was supported by a grant from The Liaison Committee for education, research and innovation in Central Norway.
Data availability
The datasets used during the current study are publicly available using the provided web links: Sepsis GWAS: www.gwas.mrcieu.ac.uk/. COVID-19 Host Genetics Initiative: www.covid19hg.org. Sex disaggregated COVID-19 GWAS: NHLBI GRASP catalogue, release date 06.18.21, www.grasp.nhlbi.nih.gov/covid19GWASResults.aspx. COVID-19 GWAS for bi-directional MR (release 2): https://genomicc.org/data/.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-022-20679-6.
References
- 1.Beard JL. Iron biology in immune function, muscle metabolism and neuronal functioning. J. Nutr. 2001;131:568S–579S. doi: 10.1093/jn/131.2.568S. [DOI] [PubMed] [Google Scholar]
- 2.Ganz T, Nemeth E. Iron homeostasis in host defence and inflammation. Nat. Rev. Immunol. 2015;15:500–510. doi: 10.1038/nri3863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO . WHO Guideline on Use of Ferritin Concentrations to Assess Iron Status in Individuals and Populations. World Health Organization; 2020. [PubMed] [Google Scholar]
- 4.WHO . Assessing the Iron Status of Populations: Including Literature Reviews. World Health Organization; 2007. [Google Scholar]
- 5.Tansarli GS, Karageorgopoulos DE, Kapaskelis A, Gkegkes I, Falagas ME. Iron deficiency and susceptibility to infections: Evaluation of the clinical evidence. Eur. J. Clin. Microbiol. Infect. Dis. 2013;32:1253–1258. doi: 10.1007/s10096-013-1877-x. [DOI] [PubMed] [Google Scholar]
- 6.Mohus RM, et al. Association of iron status with the risk of bloodstream infections: Results from the prospective population-based HUNT study in Norway. Intensive Care Med. 2018;44:1276–1283. doi: 10.1007/s00134-018-5320-8. [DOI] [PubMed] [Google Scholar]
- 7.Brandtner A, et al. Linkage of alterations in systemic iron homeostasis to patients’ outcome in sepsis: A prospective study. J. Intensive Care. 2020;8:76. doi: 10.1186/s40560-020-00495-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akkaş İ, Ince N, Sungur MA. Serum trace element and heavy metal levels in patients with sepsis. Aging Male. 2020;23:222–226. doi: 10.1080/13685538.2020.1740200. [DOI] [PubMed] [Google Scholar]
- 9.Lan P, et al. High serum iron level is associated with increased mortality in patients with sepsis. Sci. Rep. 2018;8:11072. doi: 10.1038/s41598-018-29353-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Swenson ER, Porcher R, Piagnerelli M. Iron deficiency and infection: Another pathway to explore in critically ill patients? Intensive Care Med. 2018;44:2260–2262. doi: 10.1007/s00134-018-5438-8. [DOI] [PubMed] [Google Scholar]
- 11.Drakesmith H, Prentice AM. Hepcidin and the iron-infection axis. Science. 2012;338:768–772. doi: 10.1126/science.1224577. [DOI] [PubMed] [Google Scholar]
- 12.Singer M, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3) JAMA. 2016;315:801–810. doi: 10.1001/jama.2016.0287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.da Silva Ramos FJ, de Freitas FGR, Machado FR. Sepsis in patients hospitalized with coronavirus disease 2019: How often and how severe? Curr. Opin. Crit. Care. 2021;27:474–479. doi: 10.1097/MCC.0000000000000861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lv Y, et al. Association between iron status and the risk of adverse outcomes in COVID-19. Clin. Nutr. 2021;40:3462–3469. doi: 10.1016/j.clnu.2020.11.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hippchen T, Altamura S, Muckenthaler MU, Merle U. Hypoferremia predicts hospitalization and oxygen demand in COVID-19 patients. MedRxiv. 2020;8(4):420. doi: 10.1097/HS9.0000000000000492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Perricone C, et al. COVID-19 as part of the hyperferritinemic syndromes: The role of iron depletion therapy. Immunol. Res. 2020;68:213–224. doi: 10.1007/s12026-020-09145-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tojo K, et al. The U-shaped association of serum iron level with disease severity in adult hospitalized patients with COVID-19. Sci. Rep. 2021;11:13431. doi: 10.1038/s41598-021-92921-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Galmés S, Serra F, Palou A. Current state of evidence: Influence of nutritional and nutrigenetic factors on immunity in the COVID-19 pandemic framework. Nutrients. 2020;12(9):2738. doi: 10.3390/nu12092738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mohus RM, et al. Explaining sex differences in risk of bloodstream infections using mediation analysis in the population-based HUNT study in Norway. Sci. Rep. 2022;12:8436. doi: 10.1038/s41598-022-12569-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alwani M, et al. Sex-based differences in severity and mortality in COVID-19. Rev. Med. Virol. 2021;31:e2223. doi: 10.1002/rmv.2223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Peckham H, et al. Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission. Nat. Commun. 2020;11:6317. doi: 10.1038/s41467-020-19741-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davies NM, Holmes MV, Davey Smith G. Reading Mendelian randomisation studies: A guide, glossary and checklist for clinicians. BMJ. 2018;362:k601. doi: 10.1136/bmj.k601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hu Y, et al. Causal effects of genetically predicted iron status on sepsis: A two-sample bidirectional Mendelian randomization study. Front. Nutr. 2021;8:747547. doi: 10.3389/fnut.2021.747547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bell S, et al. A genome-wide meta-analysis yields 46 new loci associating with biomarkers of iron homeostasis. Commun. Biol. 2021;4:156. doi: 10.1038/s42003-020-01575-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mauvais-Jarvis F, et al. Sex and gender: Modifiers of health, disease and medicine. Lancet. 2020;396:565–582. doi: 10.1016/S0140-6736(20)31561-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Burgess S, Thompson SG. Avoiding bias from weak instruments in Mendelian randomization studies. Int. J. Epidemiol. 2011;40:755–764. doi: 10.1093/ije/dyr036. [DOI] [PubMed] [Google Scholar]
- 27.Hemani G, et al. The MR-Base platform supports systematic causal inference across the human phenome. Elife. 2018 doi: 10.7554/eLife.34408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Yavorska OO, Burgess S. MendelianRandomization: An R package for performing Mendelian randomization analyses using summarized data. Int. J. Epidemiol. 2017;46:1734–1739. doi: 10.1093/ije/dyx034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Rudd KE, et al. Global, regional and national sepsis incidence and mortality, 1990–2017: Analysis for the global burden of disease study. Lancet. 2020;395:200–211. doi: 10.1016/S0140-6736(19)32989-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Elsworth B, et al. The MRC IEU OpenGWAS data infrastructure. BioRxiv. 2020;35:99. [Google Scholar]
- 31.Niemi MEK, Karjalainen J, Neale BM, Daly M, Andrea G. Mapping the human genetic architecture of COVID-19. Nature. 2021;600:472–477. doi: 10.1038/s41586-021-03767-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Machiela MJ, Chanock SJ. LDlink: A web-based application for exploring population-specific haplotype structure and linking correlated alleles of possible functional variants. Bioinformatics. 2015;31:3555–3557. doi: 10.1093/bioinformatics/btv402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Hartwig FP, Davies NM, Hemani G, Davey Smith G. Two-sample Mendelian randomization: Avoiding the downsides of a powerful, widely applicable but potentially fallible technique. Int. J. Epidemiol. 2016;45:1717–1726. doi: 10.1093/ije/dyx028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Leslie R, O’Donnell CJ, Johnson AD. GRASP: Analysis of genotype-phenotype results from 1390 genome-wide association studies and corresponding open access database. Bioinformatics. 2014;30:i185–i194. doi: 10.1093/bioinformatics/btu273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Burgess S, et al. Guidelines for performing Mendelian randomization investigations. Wellcome Open Res. 2019;4:186. doi: 10.12688/wellcomeopenres.15555.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bowden J, Davey Smith G, Haycock PC, Burgess S. Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet. Epidemiol. 2016;40:304–314. doi: 10.1002/gepi.21965. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hartwig FP, Davey Smith G, Bowden J. Robust inference in summary data Mendelian randomization via the zero modal pleiotropy assumption. Int. J. Epidemiol. 2017;46:1985–1998. doi: 10.1093/ije/dyx102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hemani G, Bowden J, Davey Smith G. Evaluating the potential role of pleiotropy in Mendelian randomization studies. Hum. Mol. Genet. 2018;27:R195–R208. doi: 10.1093/hmg/ddy163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bowden J, Davey Smith G, Burgess S. Mendelian randomization with invalid instruments: Effect estimation and bias detection through Egger regression. Int. J. Epidemiol. 2015;44:512–525. doi: 10.1093/ije/dyv080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Verbanck M, Chen CY, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat. Genet. 2018;50:693–698. doi: 10.1038/s41588-018-0099-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kamat MA, et al. PhenoScanner V2: An expanded tool for searching human genotype-phenotype associations. Bioinformatics. 2019;35:4851–4853. doi: 10.1093/bioinformatics/btz469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kousathanas A, et al. Whole-genome sequencing reveals host factors underlying critical COVID-19. Nature. 2022;607:97–103. doi: 10.1038/s41586-022-04576-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Skrivankova VW, et al. Strengthening the reporting of observational studies in epidemiology using mendelian randomisation (STROBE-MR): Explanation and elaboration. BMJ. 2021;375:n2233. doi: 10.1136/bmj.n2233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Burgess S, Davies NM, Thompson SG. Instrumental variable analysis with a nonlinear exposure-outcome relationship. Epidemiology. 2014;25:877–885. doi: 10.1097/EDE.0000000000000161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Benyamin B, et al. Novel loci affecting iron homeostasis and their effects in individuals at risk for hemochromatosis. Nat. Commun. 2014;5:4926. doi: 10.1038/ncomms5926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gill D, et al. Associations of genetically determined iron status across the phenome: A Mendelian randomization study. PLoS Med. 2019;16:e1002833. doi: 10.1371/journal.pmed.1002833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Alhazzani W, et al. Surviving sepsis campaign guidelines on the management of adults with coronavirus disease 2019 (COVID-19) in the ICU: First update. Crit. Care Med. 2021;49:e219–e234. doi: 10.1097/CCM.0000000000004899. [DOI] [PubMed] [Google Scholar]
- 48.Sun Y, Zhou J, Ye K. Extensive Mendelian randomization study identifies potential causal risk factors for severe COVID-19. Commun. Med. 2021;1:59. doi: 10.1038/s43856-021-00061-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Bastin A, et al. Iron chelator or iron supplement consumption in COVID-19? The role of iron with severity infection. Biol. Trace Elem. Res. 2021 doi: 10.1007/s12011-021-03048-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Colafrancesco S, Alessandri C, Conti F, Priori R. COVID-19 gone bad: A new character in the spectrum of the hyperferritinemic syndrome? Autoimmun. Rev. 2020;19:102573–102573. doi: 10.1016/j.autrev.2020.102573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Weiss G, Ganz T, Goodnough LT. Anemia of inflammation. Blood. 2019;133:40–50. doi: 10.1182/blood-2018-06-856500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Sazawal S, et al. Effects of routine prophylactic supplementation with iron and folic acid on admission to hospital and mortality in preschool children in a high malaria transmission setting: Community-based, randomised, placebo-controlled trial. Lancet. 2006;367:133–143. doi: 10.1016/S0140-6736(06)67962-2. [DOI] [PubMed] [Google Scholar]
- 53.Habib HM, Ibrahim S, Zaim A, Ibrahim WH. The role of iron in the pathogenesis of COVID-19 and possible treatment with lactoferrin and other iron chelators. Biomed. Pharmacother. 2021;136:111228. doi: 10.1016/j.biopha.2021.111228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Poonkuzhi Naseef P, et al. Therapeutic potential of induced iron depletion using iron chelators in Covid-19. Saudi J. Biol. Sci. 2022;29:1947–1956. doi: 10.1016/j.sjbs.2021.11.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lehmann C, Aali M, Zhou J, Holbein B. Comparison of treatment effects of different iron chelators in experimental models of sepsis. Life. 2021;11:57. doi: 10.3390/life11010057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Campione E, et al. Lactoferrin as potential supplementary nutraceutical agent in COVID-19 patients: In vitro and in vivo preliminary evidences. BioRxiv. 2020;47:4184. [Google Scholar]
- 57.Slob EAW, Burgess S. A comparison of robust Mendelian randomization methods using summary data. Genet. Epidemiol. 2020;44:313–329. doi: 10.1002/gepi.22295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Leligdowicz A, Matthay MA. Heterogeneity in sepsis: New biological evidence with clinical applications. Crit. care. 2019;23:80–80. doi: 10.1186/s13054-019-2372-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Labrecque JA, Swanson SA. Interpretation and potential biases of Mendelian randomization estimates with time-varying exposures. Am. J. Epidemiol. 2019;188:231–238. doi: 10.1093/aje/kwy204. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used during the current study are publicly available using the provided web links: Sepsis GWAS: www.gwas.mrcieu.ac.uk/. COVID-19 Host Genetics Initiative: www.covid19hg.org. Sex disaggregated COVID-19 GWAS: NHLBI GRASP catalogue, release date 06.18.21, www.grasp.nhlbi.nih.gov/covid19GWASResults.aspx. COVID-19 GWAS for bi-directional MR (release 2): https://genomicc.org/data/.