Abstract
Study Objectives:
The majority of active-duty service members obtain insufficient sleep, which can influence diagnostic evaluations for sleep disorders, including disorders of hypersomnolence. An incorrect diagnosis of hypersomnia may be career ending for military service or lead to inappropriate medical care. This study was conducted to assess the rates at which narcolepsy (Nc) and idiopathic hypersomnia (IH) are diagnosed by military vs civilian sleep disorders centers.
Methods:
This retrospective study utilized claims data from the Military Health System Data Repository. The analyses compared diagnostic rates of military personnel by provider type—either civilian provider or military provider—from January 1, 2016 to December 31, 2019. Three diagnostic categories for Nc and IH: Nc or IH, Nc only, and IH only, were assessed with multivariate logistic regression models.
Results:
We found that among service members evaluated for a sleep disorder, the odds ratios of a positive diagnosis at a civilian facility vs a military facility for Nc or IH was 2.1, for Nc only was 2.1, and IH only was 2.0 over the 4-year period.
Conclusions:
Civilian sleep specialists were twice as likely to diagnose central disorders of hypersomnolence compared to military specialists. Raising awareness about this discrepancy is critical given the occupational and patient care-related implications of misdiagnoses.
Citation:
Thomas CL, Vattikuti S, Shaha D, et al. Central disorders of hypersomnolence: diagnostic discrepancies between military and civilian sleep centers. J Clin Sleep Med. 2022;18(10):2433–2441.
Keywords: narcolepsy, idiopathic hypersomnia, multiple sleep latency test, insufficient sleep syndrome, circadian rhythm disorders, obstructive sleep apnea
BRIEF SUMMARY
Current Knowledge/Study Rationale: This study was conducted to determine whether, and the extent to which, differences exist in the rate at which military service members—who constitute a chronically sleep-restricted population—are diagnosed with narcolepsy and idiopathic hypersomnia at military vs civilian sleep disorders facilities. It was hypothesized that because chronic sleep restriction can complicate the interpretation of clinical sleep studies and because civilian providers may not fully appreciate the extent to which chronic sleep restriction is endemic in the service member population, they may fail to appropriately screen for and address these confounders. This could lead to overdiagnosis of rare, career-limiting conditions.
Study Impact: A diagnosis of narcolepsy can impact quality of life and restrict occupational options. In addition, misdiagnosis can dramatically impact medical care (ie, result in inappropriate prescription of psychoactive medications to include anti-depressant medications, stimulants, or sodium oxybate). In the military, narcolepsy is not compatible with continued service, and thus, misdiagnosis can result in unwarranted medical separation.
INTRODUCTION
The military engages in continuous operations. There is inherent risk associated with personnel working during periods of high sleep propensity. To complete a mission, individual service members and their commanders regularly accept sleep loss-incurred risks. In the operational context, sleep itself may be viewed as a barrier to productivity, and the need for sleep as a weakness. Throughout history, falling asleep on guard duty has been an offense, in some cases punishable by court martial or execution. Military culture has often equated the ability to sustain cognitive and physical function in the context of sleep deprivation to “manliness.”1 While coping with sleep loss has always been a part of military service, it has been particularly salient in the post-9/11 era, with significant increases in rates of common sleep disorders among service members (SMs), namely obstructive sleep apnea (OSA) and insomnia.2–7 Most military members habitually sleep fewer than 6 hours per night, and nearly one-third sleep 5 hours or less.8,9 Modern combat operations (eg, in Iraq and Afghanistan) have been characterized by night operations and reverse cycle shifts, which maximize the advantages conferred by US military’s superiority in night vision and other related technologies. In fact, some warfighters spend their entire deployment on a reverse cycle—working at night and trying to sleep during the day. In a study of previously deployed military personnel, it was found that 88% had a diagnosable sleep disorder, with nearly half of these experiencing 2 or more service-related sleep conditions.3
Sleep disorders are common among active-duty and reserve SMs. Recent data from the military health care system reveals that over 50% of SMs in the Army have a documented sleep disorder diagnosis in their electronic health record.4 Factors that likely contribute to these disorders include 24-hour operations, unpredictable sleep opportunities, frequent deployments, early morning operations, and physical fitness training at times that interfere with the ability to obtain adequate sleep. In fact, excessive daytime sleepiness (EDS) is prevalent in this population: It has been reported that SMs have an average Epworth Sleepiness Scale score of 13, a level of sleepiness that requires medical attention (Epworth Sleepiness Scale scores greater than 10 represent significant levels of sleepiness).3
Many service members present with symptoms of EDS.5 Evaluation for confounders is exceedingly important in the military population given the high burden of service-related sleep stressors and conditions,8 including insufficient sleep, shift work, and delayed sleep phase disorder. Insufficient sleep is virtually ubiquitous in the military, with only 37.4% of active-duty SMs reporting that they average 7 or more hours of sleep a night compared with 63% of civilians reporting 7–8 hours of sleep a night (ie, the minimum amount of nightly sleep recommended by both the American Academy of Sleep Medicine and the National Sleep Foundation).8–12 In addition, SMs with a deployment history report shorter sleep times than SMs without a deployment history.6 Insufficient sleep in SMs is also positively associated with depressive symptoms, post-traumatic stress disorder, tobacco/alcohol abuse, and suicide attempts.7 Insomnia, fatigue, psychomotor deficits like motor and cognitive slowing, and other sleep-related symptoms are also manifestations of underlying mental health conditions that may perpetuate insufficient sleep if left untreated. Indeed, psychiatric conditions, such as depression and post-traumatic stress disorder, have been associated with shortened mean sleep onset latency and the presence of sleep onset rapid eye movement periods (SOREMs) during the multiple sleep latency test (MSLT), suggesting that psychiatric hypersomnolence may resemble central disorders of hypersomnolence during objective testing.13–15
Shift work is also common in the military, especially in deployed settings, because operational effectiveness must be maintained 24 hours per day.3 Shift work is a major contributor to insufficient sleep and daytime sleepiness, which may lead to degraded performance and vigilance in active-duty SMs.16 Additionally, delayed sleep phase disorder—a circadian rhythm disorder characterized by difficulty initiating sleep at night (eg, until the early morning hours) and difficulty awakening in the morning (eg, until the late morning/early afternoon hours)—can cause daytime sleepiness, particularly when individuals are forced into a schedule requiring with early morning wake-up times.17 Delayed sleep phase disorder commonly presents in young adults.18 In the military, over half of enlisted SMs are 25 years of age or younger.19 Early morning formations (ie, 6 A.M. or earlier) to conduct physical training, mission-related tasks, or accountability are culturally sanctioned practices, making the military a high-risk group for sleepiness associated with delayed sleep phase disorder.
Another notable sleep disorder is OSA. Some studies suggest that OSA rates are as high as 65% in those active duty SMs who have been referred for polysomnography, compared to a prevalence of 10–15% in female and 15–30% in male civilian samples.3,7,20,21 OSA can cause clinical symptoms that resemble narcolepsy (Nc), including EDS and sleep fragmentation. Additionally, untreated OSA can result in objective findings on the and MSLT that are similar to Nc with SOREMs occurring in 21% of patients with OSA in 1 study.22 Consequently, diligent exclusion of OSA and other potential confounders is of even greater necessity in this population.
While Nc and idiopathic hypersomnia (IH) should be considered as part of the differential diagnosis for EDS, they are relatively rare diseases among both civilians and military populations. Prevalence has previously been cited as 0.014% for Nc type I with cataplexy and 0.065% for Nc type II without cataplexy.23 Nc is typically diagnosed based on clinical history and completion of a polysomnography and MSLT. Few epidemiologic studies have examined the prevalence of IH, although 2 studies have estimated 0.03% in the general population of the United Kingdom and Italy.24,25 Although the diagnostic criteria differs, there is significant overlap in the treatments of Nc and IH.26
Accurately diagnosing Nc and IH is critical given potential impacts on quality of life and occupational functioning. Previous studies suggest that as many as 50% of patients may be misdiagnosed with Nc due to a confounding disorder.27 The treatments for these diagnoses are expensive and medications for these disorders have significant side effects.
Nc diagnoses carry particular significance in the military. Individuals cannot join the military if they have a diagnosis of Nc or if they use certain medications prescribed for treatment.28 A disqualification for military accession includes the use of a single dose of stimulants for 24 consecutive months after the age of 14 or use in the previous year.29 Additionally, SMs who are diagnosed with this condition while on active duty undergo a medical evaluation board to determine continued suitability to serve in the military.30 Although it is possible that a SM is reclassified to a different occupational field as a result of an medical evaluation board, these evaluations typically result in separation from military service. Consequently, a Nc diagnosis can have profound and lasting occupational effects on military personnel—a much greater impact than it has on civilians with comparable job requirements in the nonmilitary government or private sectors.
The present study was conducted to determine whether, and the extent to which, the rate at which Nc and IH are diagnosed by military vs civilian providers differs. Military providers are often consulted when SMs who have been diagnosed with Nc at a civilian sleep clinic and are being evaluated for medical separation from the military. Often civilian evaluations fail to utilize wrist actigraphy or another objective measures of habitual nighttime sleep duration and timing, which, as mentioned previously, is an important consideration when evaluating EDS in SMs since chronic sleep restriction is common in this population. Accordingly, it is hypothesized civilian providers who are less familiar with the increased prevalence of confounding sleep conditions in the military often overdiagnose Nc and IH.
METHODS
Participants and study design
Claims data were obtained from the Military Health System Data Repository (MDR). This MDR is a centralized repository for Department of Defense claims data worldwide and includes the Managed Care Support Contract.31 We obtained counts and the majority of statistical results (unless otherwise detailed in the in this section) from the Defense Health Agency Analytics and Evaluation Division (J-5). Based on guidance from the authors, J-5 designed and implemented the final analysis plan. The MDR was queried for all active-duty personnel with claims from January 1, 2016 to December 31, 2019. The timeframe determination was made to include only claims with an International Classification of Diseases-10 code before the start of the COVID-19 pandemic. Personnel with no prior diagnosis of Nc or IH were included based on absence of International Classification of Diseases-9/ International Classification of Diseases-10 diagnostic codes prior to January 01, 2016. Nc codes were 347, 3470, 34700, 34701, 3471, 34710, 34711, G47411, G47419, G47421, G47429. IH codes were 32711, 32712, G4711, G4712.
Our intention was to compare the frequency of hypersomnolence diagnoses by civilian (CIV) and military (MIL) providers. First, this involved identifying providers that perform such evaluations. This generally includes primary care physicians, sleep disorder specialists, and pulmonologists, and somewhat less frequently, other specialties (eg, neurologists, psychiatrists).27 Although lists of providers who are board certified in sleep medicine exist, not all sleep medicine providers are board certified, making identification of all providers difficult. We also wanted to capture instances in which SMs were incidentally diagnosed with a sleep disorder, eg, based on a routine physical. Thus, we adopted a liberal definition of eligible providers. We inferred “sleep medicine providers” and then defined CIV- and MIL-exposed SMs. First, we defined the set of providers for both CIV and MIL cohorts by inspecting their diagnostic histories. If a provider ever gave a diagnosis of hypersomnolence, we included them in our analysis. This inclusion criteria were specific to the targeted diagnosis group for each analysis. We examined 3 such diagnosis groups: Nc or IH, Nc only, and IH only. Once the set of providers was selected, we used only SMs who visited these providers for any reason as identified by a medical claim/record by the provider for this SM. These individuals were then assigned to 1 or both CIV and MIL groups as defined in the next section. Using Nc only as an example, all providers who had at least 1 claim with an Nc code were part of the Nc provider cohort. Then all beneficiaries within that Nc provider cohort were included in the Nc only model.
Provider-type and case definitions
Using an exposure-type statistical analysis, we identified SMs who were exposed to CIV providers with a history of diagnosing hypersomnolence disorders as described above. Although the primary reason for a visit may not be for a sleep complaint, we counted this as an exposure if the provider’s history included having previously diagnosed disorders of hypersomnolence. Analyses were conducted to compare diagnosis rates of military personnel by provider-type—either CIV provider using purchase-care claims or MIL provider using direct-care claims. A beneficiary was assigned to 1 or both groups depending on whether they had any claim for that provider-type during the observation window. For example, if “beneficiary A” had a claim by a civilian provider then they are assigned to the CIV-provider group. If a beneficiary had a MIL-provider claim at any point during treatment, they were also assigned to the MIL-provider group. We took this approach to avoid eliminating too many data points. (Using a strict criterion of CIV- and MIL-only provider exposure for the entire 4-year period could have eliminated many cases.) In addition, we assumed that many SMs had both CIV and MIL visits. Selecting SMs who only had 1 or the other in the 4-year period would not have been representative of the population.
Cases were defined within each group (CIV or MIL) if a beneficiary received a new diagnosis by that provider type. A new diagnosis was defined as the first occurrence of the diagnostic code in the primary or secondary diagnosis claims fields. Double-counting was avoided by identifying instances when the same patient received the same diagnosis from CIV and MIL providers.
Statistical analysis
Incidence rates were estimated by dividing the number of newly diagnosed SMs (n) by the total number of at-risk members (N) within a group as defined by provider type and diagnosis group. Standard errors were estimated as:
A 1-tailed Student’s t-test was used to estimate P values. Unadjusted (without covariates) odds ratios (ORs) were estimated using the R library fmsb.
Adjusted ORs were calculated using multiple variable logistic regression for provider type and previously reported covariates (sex, age, race, and geographical region).32 All covariates and the main predictor (CIV vs MIL) were treated as binary variables, except the intercept. Significance of each parameter was assessed using a Wald chi-squared test, which assesses whether a parameter is zero given all other parameters in the model.33 Odds ratios and confidence intervals (CIs) were then derived from the exponentiated regression coefficients. Data pull and regression modeling was implemented by the Military Health System Research Program system.
RESULTS
The incidence rates for hypersomnolence diagnoses were higher in the CIV-provider than MIL-provider group (Table 1, Table 2, and Table 3). Across diagnosis types (Nc or IH, Nc only, and IH only), the mean incidence rates for CIV-provider cohort ranged from 0.004 to 0.007 vs 0.0008 to 0.001 in the MIL group. We summarize the results for the Nc or IH analyses here, since the results were similar across diagnosis definitions (see Table 1 and Table 2 for details). The odds of being diagnosed with Nc or IH if exposed to a CIV provider at first diagnosis was 4.9 (95% CI: 4.6–5.1, P < .001). To assess the robustness of the estimates to cofounders, we performed a multivariable logistic regression analysis controlling for age, sex, race, and geographic region. Including confounders lowered the OR by more than a half. However, the provider-type effects were still large, with an OR of 2.07 (95% CI: 2.02–2.13, P < .001).
Table 1.
Counts and incidence rates across provider-types and diagnosis groups.
| Diagnosis | Provider-type | No Dx | Dx | Total | Rate (SE) |
|---|---|---|---|---|---|
| Nc or IH | CIV | 768,039 | 5,377 | 773,416 | *0.0070 (0.0001) |
| MIL | 1,673,963 | 2,414 | 1,676,377 | *0.00144 (0.00003) | |
| Nc | CIV | 719,059 | 3,842 | 722,901 | *0.0053 (0.0001) |
| MIL | 1,609,258 | 1,750 | 1,611,008 | *0.00109 (0.00003) | |
| IH | CIV | 529,906 | 2,187 | 532,093 | *0.0041 (0.0001) |
| MIL | 1,001,404 | 766 | 1,002,170 | *0.00076 (0.00003) |
*P < .001. CIV = civilian, Dx = diagnosis, IH = idiopathic hypersomnia, MIL = military, Nc = narcolepsy, SE = standard error.
Table 2.
Odds ratios for each diagnosis group.
| Diagnosis | OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|
| Nc-or-IH | *4.9 (4.6–5.1) | *2.07 (2.02–2.13) |
| Nc | *4.9 (4.6–5.2) | *2.15 (2.08–2.22) |
| IH | *5.3 (5–5.9) | *2.02 (1.92–2.11) |
*P < .001. CI = confidence interval, IH = idiopathic hypersomnia, Nc = narcolepsy, OR = odds ratio.
Table 3.
Key similarities, differences, and contextual factors to consider when evaluating military sleep medicine patients.
| Factors for Consideration | Civilian Patients | Military Patients |
|---|---|---|
| Disease prevalence, Narcolepsy |
0.014–0.07% may be at risk for narcolepsy type I with cataplexy23,34 0.065–0.2% may be at risk for narcolepsy type II without cataplexy23,34 |
Unknown; might mirror civilian estimates but chronic sleep insufficiency, circadian misalignment, erratic shift work schedules, and psychiatric conditions confound such estimates |
| Disease prevalence, Idiopathic Hypersomnia | 0.03% may be at risk24,25 | Unknown; might mirror civilian estimates but chronic sleep insufficiency, circadian misalignment, shift work, and psychiatric conditions confound such estimates |
| Disease prevalence, OSA | Middle aged adults are at risk for OSA (based on an AHI of 5 events/h or greater)20,21
|
9–12% across the Department of Defense.51–52 Some studies reporting 65% at risk among those screened with PSG; but rates are variable and pretest probability using standard metrics such as STOP-BANG and ESS are less useful due to chronic insufficient sleep and disability incentive3,7 |
| Insufficient sleep | ||
| < 6 h/night habitually | 29%11 | 62.7–72%3,7,8 |
| < 5 h/night habitually | 8%11 | 31.4–43%3,7,8 |
| Occupational culture surrounding sleep | Variable; many professions that endorse a culture of productivity at expense of sleep include:
|
Long standing traditions surrounding extended workdays and early start times (earlier than 6 A.M.) for unit physical fitness. Many service members have long commute times to work, especially in urban areas where military income does not match housing costs close to work. |
| Shift Work | Variable; although many professions have established patterns of shift work, engagement in these occupations varies:
|
Extensive and sometimes hidden shift work schedules. Field training and deployment operations requiring 24/7 manning. Many leadership rolls encompass 24/7 responsibility by phone. Senior leaders may have several separate leadership jobs due to personnel shortages. Early work start times that are outside a normal 9 A.M.-5 P.M. schedule in addition to evening meetings, night-work and weekends. |
| Disability, OSA |
No specific disability rating. Potential disincentives (ie, driving license restrictions in some states) |
There is a Veterans Affairs disability rating for the diagnosis of OSA
|
| Disability, Narcolepsy |
No specific disability rating. Potential disincentives (ie, driving license restrictions in some states) |
There is a Veterans Affairs disability rating for the diagnosis of Narcolepsy:
|
| Implications for Future Employment | A diagnosis of narcolepsy or OSA does not impact your occupational capability for many jobs. | A diagnosis of narcolepsy or OSA can render a Service member limited in the following ways, depending on final diagnosis and response to treatment:
|
| Take Home Points |
|
|
AHI = apnea-hypopnea index, CPAP = continuous positive airway pressure, ESS = Epworth Sleepiness Scale, PSG = polysomnography.
Among the covariates, factors that increased the odds of hypersomnolence diagnosis were female vs male (OR: 1.09, 95% CI:1.06–1.12, P < .001), black vs non-Hispanic white personnel (OR: 1.33, 95% CI:1.26–1.42, P < .001) and Midwest vs South (OR: 1.07, 95% CI: 1.01–1.14, P = .025). Lower odds of diagnosis were found for Hispanic (OR: 0.83, 95% CI: 0.77–0.90, P < .001) and Asian or Pacific Islander (OR: 0.90, 95% CI: 0.81–1.0, P < .001) vs non-Hispanic white and the West vs South geographic region (OR: 0.72, 95% CI: 0.68–0.77, P < .001). Our findings for covariates were consistent with those obtained in a prior study of Nc in the US military using medical records from 2004 to 2013.32
DISCUSSION
Our study revealed that, compared to MIL providers, CIV providers were at least 2 times more likely to diagnose Nc or IH, Nc only, or IH only in active duty SMs. Numerous factors may contribute to this discrepancy. By far, the most common disorder masquerading as Nc is insufficient sleep syndrome. Military practitioners understand the cultural context in which active-duty SMs operate and the increased likelihood that members of this population will be chronically sleep restricted. Civilian providers may not be aware of the prevalence of insufficient sleep syndrome in the military, and this may not be fully addressed with the clinical history, sleep logs, and actigraphy prior to administration of the MSLT.
The rate of Nc diagnosis in the CIV-provider group was also higher than expected, based on previously published prevalence data from the civilian population. In a medical claims database of 8.4 million people that included children, Nc type I with cataplexy was present in 0.014% and Nc type II without cataplexy was present in NT2 0.065% of the population.23 In the Wisconsin sleep cohort, Nc type I with cataplexy was present in 0.07% and Nc type II was present in 0.2% of the general population.34 Our study revealed a 0.5% diagnostic rate for Nc only (combined Nc type I and type II), which is considerably higher than has been reported in these large studies. This suggests that civilian providers are over diagnosing Nc in the military population.
Much of the Nc literature focuses on delays in recognition, under-diagnosis, and the need to educate providers to improve awareness.35,36 It is possible that this educational emphasis may skew the differential diagnosis of clinicians who evaluate patients for EDS. Our findings suggest that civilian providers probably over diagnose Nc, and it is notable that 100% of the overturned diagnoses came from civilian sleep clinics.
False positive diagnoses of Nc may contribute to excessive prescription of stimulants and other wake-promoting agents, which is discouraged in the military. Stimulant prescriptions for fatigue reduction and/or performance enhancement is guided by military policies and are reserved for select aviation professionals and special operators under operational constraints.37 Stimulants are known drugs of misuse and abuse, can cause several side effects that may impact occupational performance, and may compromise safety while operating specialized equipment and weapons. On an anonymous survey, 2.3% of active-duty SM respondents reported misusing prescription stimulants at least once within the past year.38 Misuse of prescription pain relievers, tranquilizers, and sedatives ranged from 2 to 17%. Diligent efforts to ensure diagnostic accuracy are important in this patient population, given the potential implications for performance, safety, and prescription misuse.
Additionally, the MSLT, the gold standard used to diagnose Nc, is an imperfect test. When the American Academy of Sleep Medicine changed the MSLT sleep onset latency threshold signifying pathological sleepiness from 5 minutes to 8 minutes in 2005, differences in sensitivity and specificity were considered.39 MSLT sleep onset latency had a sensitivity of 80.9% and specificity of 89.8% with a < 5-minute cut-off. Under an 8-minute cut-off, sleep onset latency had a higher sensitivity of 94.5%. On the other hand, specificity, or the probability that a person not having a disease will be correctly identified by a clinical test, was 73.3%.40 The possibility of false positive diagnoses is further exacerbated by accruing evidence that SOREMS during the MSLT—long considered a hallmark and unique indicator of Nc—are actually found in a variety of conditions characterized by high sleep pressure.41–44 For example, the Wisconsin Sleep Cohort study revealed that some shift workers without Nc exhibit both short sleep latencies and SOREMs on the MSLT.34 Likewise, SOREMs during the MSLT have been observed in patients with untreated OSA, particularly in those with apnea who exhibit severe deoxygenation events.45 In a study by Aldrich et al,43 a large number of controls with EDS who did not have a diagnosis of Nc demonstrated multiple SOREMs on the MSLT, which contributed to a drop in the positive predictive value from 98–100% observed in previous studies to 63%. As a result, it may be that the overall number of false positive MSLTs outnumber the true positives when testing all patients who present with EDS if confounding conditions that present with high sleep pressure are not carefully excluded. Coelho et al45 recommends conducting a second MSLT in clinically uncertain cases to avoid missing the diagnosis of Nc. Given the possibility of false positive MSLTs (ie, the presence of SOREMs or shortened sleep onset latency that typically represent findings of Nc when other disorders like insufficient sleep or obstructive sleep apnea may better account for the findings), performing a second MSLT may also be prudent to confirm Nc if the previously made diagnosis has come into question. In military sleep labs, it is common to repeat sleep studies after a civilian diagnosis is made, because they lack the work-up that is required to make that diagnosis according to military regulations. In the Army, Nc can be diagnosed after only 1 week of actigraphy with an average sleep period of 7 or more hours without circadian variability.47 The Air Force guidelines are more stringent, requiring 2 weeks of actigraphy with 7 or more hours of average sleep and a wash-out of sedating medication and stimulants 2 weeks prior to the MSLT.48 In contrast, the International Classification of Sleep Disorders, third edition, which is used by all providers to classify sleep disorders, recommends that “the sleep-wake schedule must have been standardized and, if necessary, extended to a minimum of seven hours in bed each night (longer for children) for at least seven days before polysomnography (preferably documented by sleep log and, whenever possible, actigraphy).”49 Actigraphy is not considered mandatory to complete an MSLT according to current International Classification of Sleep Disorders, third edition guidelines and is often not reimbursed in the civilian setting. However, there can be a difference in the quality of data obtained by sleep log compared with actigraphy, particularly in patients with insomnia and/or severely disrupted nocturnal sleep (the latter is characteristic of Nc, albeit not unique to Nc). In a sleep log, providers rely on self-reporting, but the patient can be a major source of bias due to problems in recall, a desire to seek approval or to provide socially desirable responses, or secondary gain (ie, a SM desires to be medically boarded). Having objective evidence of sleep onset, duration, and fragmentation via actigraphy helps clinicians rule out confounders such as insufficient sleep or circadian rhythm abnormalities that may lead to false positive diagnoses of Nc. Military clinicians may be more likely to utilize clinical resources, such as actigraphy, repeat an MSLT altogether, or cautiously interpret positive MSLT findings, because of their understanding of the operational culture and the contextual factors that influence an individual to seek testing (Table 3).
In a retrospective analysis, Villarreal and colleagues49 examined 23 patients aged 18–65 years who were previously diagnosed with Nc at an outside civilian facility. They were referred for a repeat evaluation at a military sleep disorders center that included actigraphy, in-laboratory polysomnography, and MSLT. Of the 23 patients, 9% maintained a diagnosis of Nc after repeat testing, 43% had insufficient sleep syndrome, 22% had a circadian rhythm sleep-wake disorder, and 39% had mild OSA with nearly half of these cases having supine predominant OSA. Clearly, patients who have previously been diagnosed with Nc and who subsequently have repeat testing at a military facility that utilizes at-home actigraphy as part of the evaluation are often diagnosed with conditions that better explain the presenting symptoms.
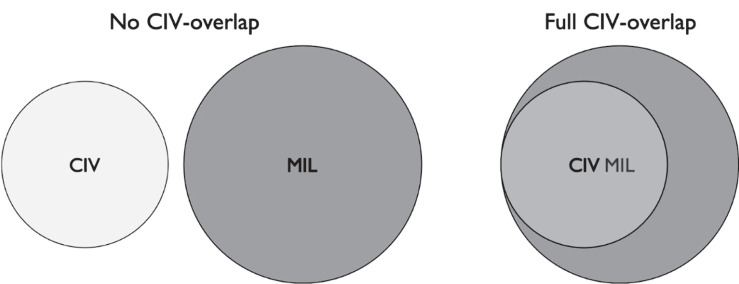
Our goal was to compare the rates of diagnosis of Nc by civilian vs military providers who diagnose hypersomnolence. In many cases, these are not sleep medicine specialists, and a considerable number are primary care providers.27 It is the diagnoses by this broad group of physicians including specialists and nonspecialists that we wished to evaluate. Our analysis involved identification sleep medicine providers and determination of the appropriate denominators for assessment of the relative rates of diagnoses by CIV and MIL physicians. In other words, we needed to account for the disparate numbers of individuals visiting CIV vs MIL sleep physicians, representing opportunities for new diagnoses. For each group (CIV or MIL), we defined the at-risk populations as any service members without a prior diagnosis who were under the care of such providers evidenced by any type of medical claim (ie, the care was not necessarily sleep related). Thus, it is possible that some SMs were included in both CIV and MIL groups. Using the counts provided by MDR (see Table 1 and Figure 1), at most 50% of the MIL pool were also counted in the CIV pool. More information is needed to evaluate the impact on our analysis. The use of medical records can help further define exposure and alternative models.
Figure 1. Possible overlaps between at-risk groups.
On one extreme, there may be no overlap between individuals who had CIV-provider claim and those who had MIL-provider claims. On the other extreme, there could be complete overlap. Because the MIL group was approximately 2-fold larger than CIV, it is possible that all the CIV group had exposure to CIV and MIL providers and were also part of the MIL group. CIV = civilian, MIL = military.
An additional limitation is the possibility that both CIV and MIL providers misdiagnosed some of the same patients. Likewise, we do not know with certainty that all MIL providers performed actigraphy in accordance with military policies. Despite these limitations, this is the first large scale study to assess discrepancies between MIL and CIV providers in the rates of diagnoses of disorders of central nervous system hypersomnolence. Future research should include more detailed information about how CIV and MIL providers code and bill for visits (ie, to determine how many sleep evaluations included actigraphy based on provider type).
CONCLUSIONS
The present study was conducted to assess differences in the rates at which MIL vs CIV providers diagnose Nc and IH in SMs—a population with a high incidence of chronic sleep restriction. We found that active-duty SMs evaluated by CIV providers were twice as likely to be newly diagnosed with Nc or IH, Nc only, or IH only compared to MIL providers during a 4-year period. Accurately diagnosing Nc is paramount given potential impacts on quality of life and occupational implications, particularly in the military where Nc is not compatible with continued service.
ACKNOWLEDGMENTS
The authors thank Wilford Hall, Madigan Army Medical Center, and Walter Reed National Military Medical Center for their collaborations on this study.
ABBREVIATIONS
- CI
confidence interval
- CIV
provider, civilian provider
- EDS
excessive daytime sleepiness
- IH
idiopathic hypersomnia
- MIL
provider, military provider
- MDR
Military Health System Data Repository
- MSLT
Multiple Sleep Latency Test
- Nc
narcolepsy
- OR
odds ratio
- OSA
obstructive sleep apnea
- SM
service member
- SOREM
sleep onset rapid eye movement
DISCLOSURE STATEMENT
All authors have seen and approved this manuscript. The opinions and assertions in this manuscript are those of the authors and do not represent those of the Department of the Army, Department of Defense, or the US government. The investigators have adhered to the policies for protection of human participants as prescribed in AR 70–25. There is no financial support to disclose. The authors report no conflicts of interest.
AVAILABILITY OF DATA AND MATERIALS
The datasets generated and/or analyzed during the current study are not publicly available due to the potential sensitive nature of military health care data.
REFERENCES
- 1. Derickson , A . “No Such Thing as a Night's Sleep”: the Embattled Sleep of American Fighting Men from World War II to the Present . J Social History. 2013. ; 47 ( 1 ): 1 – 26 . [Google Scholar]
- 2. Mysliwiec V , McGraw L , Pierce R , Smith P , Trapp B , Roth BJ . Sleep disorders and associated medical comorbidities in active duty military personnel . Sleep. 2013. ; 36 ( 2 ): 167 – 174 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Devine JK , Collen J , Choynowski JJ , Capaldi V . Sleep disturbances and predictors of nondeployability among active-duty Army soldiers: an odds ratio analysis of medical healthcare data from fiscal year 2018 . Mil Med Res. 2020. ; 7 ( 1 ): 10 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Trimmel K , Żebrowska M , Böck M , et al . Wanted: a better cut-off value for the Epworth Sleepiness Scale . Wien Klin Wochenschr. 2018. ; 130 ( 9-10 ): 349 – 355 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Foster SN , Brock MS , Hansen S , et al . Sleep disorders related to deployment in active duty service members and veterans . Curr Pulmonol Rep. 2016. ; 5 ( 2 ): 101 – 110 . [Google Scholar]
- 6. Luxton DD , Greenburg D , Ryan J , Niven A , Wheeler G , Mysliwiec V . Prevalence and impact of short sleep duration in redeployed OIF soldiers . Sleep. 2011. ; 34 ( 9 ): 1189 – 1195 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Troxel WM , Shih RA , Pedersen ER , et al . Sleep in the Military: Promoting Healthy Sleep among U.S. SMs. Santa Monica, CA: : RAND Corporation; ; 2015. . [PMC free article] [PubMed] [Google Scholar]
- 8. Capaldi VF , Balkin TJ , Mysliwiec V . Optimizing sleep in the military: challenges and opportunities . Chest. 2019. ; 155 ( 1 ): 215 – 226 . [DOI] [PubMed] [Google Scholar]
- 9. Watson NF , Badr MS , Belenky G , et al . Recommended amount of sleep for a healthy adult: a joint consensus statement of the American Academy of Sleep Medicine and Sleep Research Society . Sleep. 2015. ; 38 ( 6 ): 843 – 844 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hirshkowitz M , Whiton K , Albert SM , et al . National Sleep Foundation’s updated sleep duration recommendations: final report . Sleep Health. 2015. ; 1 ( 4 ): 233 – 243 . [DOI] [PubMed] [Google Scholar]
- 11. Krueger PM , Friedman EM . Sleep duration in the United States: a cross-sectional population-based study . Am J Epidemiol. 2009. ; 169 ( 9 ): 1052 – 1063 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Bušková J , Novák T , Miletínová E , et al . Self-reported symptoms and objective measures in idiopathic hypersomnia and hypersomnia associated with psychiatric disorders: a prospective cross-sectional study . J Clin Sleep Med. 2022. ; 18 ( 3 ): 713 – 720 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Zhang Y , Li Y , Zhu H , et al . Characteristics of objective daytime sleep among individuals with earthquake-related posttraumatic stress disorder: a pilot community-based polysomnographic and multiple sleep latency test study . Psychiatry Res. 2017. ; 247 : 43 – 50 . [DOI] [PubMed] [Google Scholar]
- 14. Plante DT . Sleep propensity in psychiatric hypersomnolence: a systematic review and meta-analysis of multiple sleep latency test findings . Sleep Med Rev. 2017. ; 31 : 48 – 57 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shattuck N , Matsangas P , Saitzyk A . Improving work and rest patterns of military personnel in operational settings with frequent unplanned events . Proc Hum Fac and Erg Soc. Annu. Meet. 2018. ; 62 ( 1 ): 772 – 776 . [Google Scholar]
- 16. Schrader H , Bovim G , Sand T . The prevalence of delayed and advanced sleep phase syndromes . J Sleep Res. 1993. ; 2 ( 1 ): 51 – 55 . [DOI] [PubMed] [Google Scholar]
- 17. Sivertsen B , Pallesen S , Stormark KM , Bøe T , Lundervold AJ , Hysing M . Delayed sleep phase syndrome in adolescents: prevalence and correlates in a large population based study . BMC Public Health. 2013. ; 13 : 1163 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. U.S. Department of Defense (DoD) . 2017 Demographics: Profile of the Military Community. Washington, DC: : Department of Defense; ; 2017. . http://download.militaryonesource.mil/12038/MOS/Reports/2017-demographics-report.pdf . [Google Scholar]
- 19. Young T , Palta M , Dempsey J , Peppard PE , Nieto FJ , Hla KM . Burden of sleep apnea: rationale, design, and major findings of the Wisconsin Sleep Cohort study . WMJ. 2009. ; 108 ( 5 ): 246 – 249 . [PMC free article] [PubMed] [Google Scholar]
- 20. Peppard PE , Young T , Barnet JH , Palta M , Hagen EW , Hla KM . Increased prevalence of sleep-disordered breathing in adults . Am J Epidemiol. 2013. ; 177 ( 9 ): 1006 – 1014 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Paudel D , Lin Q , Yan C , Liu S , Zhang B . A false alarm of narcolepsy: obstructive sleep apnea masquerading as narcolepsy and depression . Sleep Breath. 2019. ; 23 ( 3 ): 873 – 877 . [DOI] [PubMed] [Google Scholar]
- 22. Scheer D , Schwartz SW , Parr M , Zgibor J , Sanchez-Anguiano A , Rajaram L . Prevalence and incidence of narcolepsy in a US health care claims database, 2008-2010 . Sleep. 2019. ; 42 ( 7 ): zsz091 . [DOI] [PubMed] [Google Scholar]
- 23. Ohayon MM , Caulet M , Philip P , Guilleminault C , Priest RG . How sleep and mental disorders are related to complaints of daytime sleepiness . Arch Intern Med. 1997. ; 157 ( 22 ): 2645 – 2652 . [PubMed] [Google Scholar]
- 24. Ohayon MM , Ferini-Strambi L , Plazzi G , Smirne S , Castronovo V . Frequency of narcolepsy symptoms and other sleep disorders in narcoleptic patients and their first-degree relatives . J Sleep Res. 2005. ; 14 ( 4 ): 437 – 445 . [DOI] [PubMed] [Google Scholar]
- 25. Maski K , Trotti LM , Kotagal S , et al . Treatment of central disorders of hypersomnolence: an American Academy of Sleep Medicine clinical practice guideline . J Clin Sleep Med. 2021. ; 17 ( 9 ): 1881 – 1893 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dunne L , Patel P , Maschauer EL , Morrison I , Riha RL . Misdiagnosis of narcolepsy . Sleep Breath. 2016. ; 20 ( 4 ): 1277 – 1284 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Department of Defense Medical Standards for Appointment . Enlistment, or Induction in the Military Services. Instruction Number 6130.03. http://www.dtic.mil/whs/directives/corres/pdf/613003p.pdf . Accessed April 28, 2010. .
- 28. Department of Defense Criteria and Procedure Requirements for Physical Standards for Appointment . Enlistment, or Induction in the Armed Forces. Instruction Number 6130.4. https://biotech.law.lsu.edu/blaw/dodd/corres/pdf2/i61304p.pdf . Accessed April 2, 2004. .
- 29. Department of Defense Medical Standards for Military Service . Retention. Instruction 6130.03, Volume 2. https://www.esd.whs.mil/Portals/54/Documents/DD/issuances/dodi/613003_vol02.PDF?ver=vx1spUpNVLcc-0-rov00Sg%3d%3d . Accessed September 4, 2020. .
- 30. Military Health System . Military Health System Data Repository. https://www.health.mil/Military-Health-Topics/Technology/Clinical-Support/Military-Health-System-Data-Repository . Accessed August 19, 2021.
- 31. Lee RU , Radin JM . A population-based epidemiologic study of adult-onset narcolepsy incidence and associated risk factors, 2004-2013 . J Neurol Sci. 2016. ; 370 : 29 – 34 . [DOI] [PubMed] [Google Scholar]
- 32. Introduction to SAS . UCLA: StatisticalConsulting Group. https://stats.oarc.ucla.edu/sas/modules/introduction-to-the-features-of-sas/. Accessed August 16, 2021.
- 33. Goldbart A , Peppard P , Finn L , et al . Narcolepsy and predictors of positive MSLTs in the Wisconsin Sleep Cohort . Sleep. 2014. ; 37 ( 6 ): 1043 – 1051 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Thorpy MJ , Krieger AC . Delayed diagnosis of narcolepsy: characterization and impact . Sleep Med. 2014. ; 15 ( 5 ): 502 – 507 . [DOI] [PubMed] [Google Scholar]
- 35. Morse AM . Narcolepsy in children and adults: a guide to improved recognition, diagnosis and management . Med Sci (Basel). 2019. ; 7 ( 12 ): 106 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Caldwell JA , Mallis MM , Caldwell JL , Paul MA , Miller JC , Neri DF ; Aerospace Medical Association Fatigue Countermeasures Subcommittee of the Aerospace Human Factors Committee . Fatigue countermeasures in aviation . Aviat Space Environ Med. 2009. ; 80 ( 1 ): 29 – 59 . [DOI] [PubMed] [Google Scholar]
- 37. Jeffery DD , Babeu LA , Nelson LE , Kloc M , Klette K . Prescription drug misuse among U.S. active duty military personnel: a secondary analysis of the 2008 DoD survey of health related behaviors . Mil Med. 2013. ; 178 ( 2 ): 180 – 195 . [DOI] [PubMed] [Google Scholar]
- 38. Krahn LE , Arand DL , Avidan AY , et al . Recommended protocols for the Multiple Sleep Latency Test and Maintenance of Wakefulness Test in adults: guidance from the American Academy of Sleep Medicine . J Clin Sleep Med. 2021. ; 17 ( 12 ): 2489 – 2498 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Johns MW . Sensitivity and specificity of the multiple sleep latency test (MSLT), the maintenance of wakefulness test and the Epworth sleepiness scale: failure of the MSLT as a gold standard . J Sleep Res. 2000. ; 9 ( 1 ): 5 – 11 . [DOI] [PubMed] [Google Scholar]
- 40. Murer T , Imbach LL , Hackius M , et al . Optimizing MSLT specificity in narcolepsy with cataplexy . Sleep. 2017. ; 40 ( 12 ): . [DOI] [PubMed] [Google Scholar]
- 41. Moscovitch A , Partinen M , Guilleminault C . The positive diagnosis of narcolepsy and narcolepsy’s borderland . Neurology. 1993. ; 43 ( 1 ): 55 – 60 . [DOI] [PubMed] [Google Scholar]
- 42. Mignot E , Lin L , Finn L , et al . Correlates of sleep-onset REM periods during the Multiple Sleep Latency Test in community adults . Brain. 2006. ; 129 ( Pt 6 ): 1609 – 1623 . [DOI] [PubMed] [Google Scholar]
- 43. Aldrich MS , Chervin RD , Malow BA . Value of the multiple sleep latency test (MSLT) for the diagnosis of narcolepsy . Sleep. 1997. ; 20 ( 8 ): 620 – 629 . [PubMed] [Google Scholar]
- 44. Chervin RD , Aldrich MS . Sleep onset REM periods during multiple sleep latency tests in patients evaluated for sleep apnea . Am J Respir Crit Care Med. 2000. ; 161 ( 2 Pt 1 ): 426 – 431 . [DOI] [PubMed] [Google Scholar]
- 45. Coelho FM , Georgsson H , Murray BJ . Benefit of repeat multiple sleep latency testing in confirming a possible narcolepsy diagnosis . J Clin Neurophysiol. 2011. ; 28 ( 4 ): 412 – 414 . [DOI] [PubMed] [Google Scholar]
- 46. Department of the Army . Army Regulation 40-501: Standards of Medical Fitness. https://armypubs.army.mil/epubs/DR_pubs/DR_a/pdf/web/ARN8673_AR40_501_FINAL_WEB.pdf . Accessed June 2019. .
- 47. Secretary of the Air Force . Air Force Instruction 48-123: Medical Examinations and Standards. https://dmna.ny.gov/hro/agr/air/files/1407787321–afi48-123.pdf . Accessed November 2013. .
- 48. American Academy of Sleep Medicine . International Classification of Sleep Disorders. 3rd ed. Darien, IL: : American Academy of Sleep Medicine; ; 2014. . [Google Scholar]
- 49. Villarreal B , Powell T , Brock MS , Hansen S . Diagnosing narcolepsy in the active duty military population . Sleep Breath. 2021. ; 25 ( 2 ): 995 – 1002 . [DOI] [PubMed] [Google Scholar]
- 50. Haynes ZA , Stewart IJ , Poltavskiy EA , et al . Obstructive sleep apnea among survivors of combat-related traumatic injury: a retrospective cohort study . J Clin Sleep Med. 2022. ; 18 ( 1 ): 171 – 179 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Defense Health Agency . ICD-9 327.23, ICD-10 G47.33, FY2020. Military Heath System Data Repository. Accessed February 18, 2021. .
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to the potential sensitive nature of military health care data.