Abstract
Hepatocellular carcinoma (HCC) is the most common type of liver cancer and the third leading cause of cancer-related death worldwide. Factors including carcinogens, infection of hepatitis viruses, alcohol abuse, and metabolic disorders such as non-alcoholic fatty liver disease mainly contribute to HCC initiation and progression. Immunotherapy is one of the most powerful tools for unresectable HCC treatment in patients. CD8+ T cells are a major immune component in the tumor microenvironment with cytotoxic effects against cancer cells. However, these CD8+ T cells commonly display an exhaustion phenotype with high expression of programmed cell death protein 1, T-cell immunoglobulin and mucin-domain containing-3, and/or lymphocyte-activation gene 3, producing low levels of perforin (PRF1) and granzyme B (GZMB), as well as anti-tumor cytokines, such as interferon gamma and tumor necrosis factor alpha. In the referenced study, the authors also showed that deprivation of glutamine decreased the antitumor function of CD8+ T cells, as well as the production of PRF1 and GZMB. However, the role of each amino acid in T cell function and exhaustion may depend on tumor type and tumor microenvironment, including the source of other nutrients. Overall, amino acids or other nutrient metabolites in the tumor microenvironment play a pivotal role in both tumor growth and immune response.
Keywords: Hepatocellular carcinoma, Metabolism, Amino acids, Tumor microenvironment, T cell function
Core Tip: Immunotherapy is one of the most powerful tools for patients with unresectable hepatocellular carcinoma. CD8+ T cells are a major immune component in the tumor microenvironment with cytotoxic effects against tumor cells. However, these CD8+ T cells commonly display an exhaustion phenotype with high expression of immune checkpoints such as programmed cell death protein 1, producing less anti-tumor proteins and cytokines, such as perforin and granzyme B. Here, we show that the roles of amino acids such as glutamine in T cell activation and function are dependent on tumor types and nutrients in the tumor microenvironment. Overall, nutrient metabolism reprogramming in the tumor microenvironment plays a pivotal role in both tumor growth and immune response.
TO THE EDITOR
We read a basic study recently published by Wang et al[1] with great interest, which shows that glutamine deprivation impairs the cytotoxic function of tumor-infiltrating CD8+ T cells in hepatocellular carcinoma (HCC) by inducing mitochondrial dysfunction and apoptosis. HCC is the primary liver cancer and the third leading cause of cancer-related death worldwide[2]. Factors including carcinogens, infection of hepatitis viruses, alcohol abuse, and metabolic disorders such as non-alcoholic fatty liver disease mainly contribute to HCC initiation and progression[3].
Immunotherapy is one of the most powerful tools for unresectable HCC treatment in patients[4]. CD8+ T cells are a major immune component in the tumor microenvironment with cytotoxic effects against tumor cells. However, these CD8+ T cells commonly display an exhaustion phenotype with high expression of programmed cell death protein 1 (PD-1), T-cell immunoglobulin and mucin-domain containing-3, and/or lymphocyte-activation gene 3, which produce low levels of anti-tumor cytokines, such as interferon gamma (IFN-γ) and tumor necrosis factor alpha (TNF-α)[5,6]. In the referenced study, the authors also showed that deprivation of glutamine decreased the secretion of perforin and granzyme B in CD8+ T cells in HCC[1]. Treatment of immune checkpoint inhibitors by targeting PD-1, programmed death protein-ligand-1 (PD-L1), or cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4) has shown clinical effects in HCC patients[7,8]. For example, the U.S. Food and Drug Administration approved the use of nivolumab (anti-PD1) or in combination with ipilimumab or ipilimumab (anti-CTLA-4) for the treatment of patients with HCC in certain conditions[9-11]. Furthermore, the state-art chimeric antigen receptor-engineered T-cell therapy has displayed the promise for HCC treatment[12,13].
Accumulating data indicate that tumor cells can compete with immune cells for nutrition in a nutrient-poor tumor microenvironment, especially for cytotoxic effective CD8+ T cells to suppress their anti-tumor immunity[14]. For example, restriction of dietary asparagine (Asn), asparaginase administration, or inhibition of the asparagine transporter solute carrier family 1 member 5 (SLC1A5) impaired the function of CD8+ T cells[15]. In contrast, increased Asn levels enhance CD8+ T-cell activation and function against tumor cells (e.g., B16-OVA) in vitro and in vivo[15]. Supplementation of creatine significantly inhibited tumor growth in multiple mouse tumor models (e.g., B16-OVA melanoma) by activating T cells, which had a synergistic with a PD-1/PD-L1 blockade treatment[16]. Some non-essential amino acids such as serine are required for T cell proliferation by promoting nucleotide biosynthesis[17]. Additionally, nutrients are also required for CD8+ T cell differentiation into effector and memory subsets, such as glucose, lactate, glutamine, methionine, and neutral amino acids[18]. Under a low-glucose tumor microenvironment, due to the consumption of glucose by tumor cells, the function of effector CD8+ T cells was impaired and the expression of PD-1 was enhanced in regulatory T cells, resulting in treatment failure of PD-1 blockade[19]. In addition, tumor cell-derived metabolites such as lactate can also inhibit CD8+ T cell cytotoxicity[20]. Another study also showed that accumulation of long-chain fatty acids (LCFAs) due to downregulation of regulating enzymes can impair CD8+ T cell function by causing their mitochondrial dysfunction and reducing fatty acid catabolism[21]. Tumor cells can reprogram their metabolic pathways to compete with CD8+ T cells for nutrients such as fatty acids[22]. Therefore, regulation of nutrient metabolism can impact the function of T cells. Inhibiting glutaminase, an amidohydrolase enzyme that can generate glutamate from glutamine, can also suppress CD8+ T cell activation induced by anti-PD-1 immunotherapy[23].
Different nutrients show diverse functions in CD8+ T cells. Regulation of tryptophan metabolism impacts the cytotoxic effect of CD8+ T cells. For example, inhibiting tryptophan catabolism using indoleamine 2,3-dioxygenase inhibitors can activate CD8+ T cells and suppress their expression of PD-1 by elevating intracellular tryptophan levels[24]. Meanwhile, tryptophan supplementation also promoted the cytotoxic function of CD8+ T cells against co-cultured B16F10 tumor cells in vitro and increased tumor-infiltration of CD8+ T cells and their functions in mouse lung cancer model[24]. In contrast, another study also showed that depletion of dietary tryptophan decreased aryl hydrocarbon receptor activity in tumor-associated macrophages and increased tumor infiltration of tumor necrosis factor alpha (TNFα)+IFNγ+CD8+ T cells in pancreatic ductal adenocarcinoma, while supplementation of dietary indoles inhibited this effect[25].
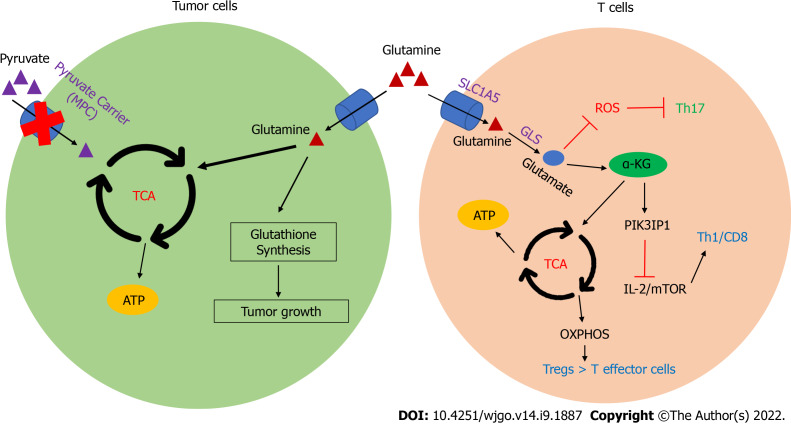
In the reviewed study, the authors showed that mitochondrial damage and apoptosis caused CD8+ T cell dysfunction. These findings shed light on the need for further investigation into the molecular mechanisms of glutamine metabolism impacting T cell functions. Glutamine metabolism has been shown to regulate the T helper 17 cell differentiation but restrict Th1 and CD8+ T cell differentiation through glutaminolysis (GLS) by regulating the production of reactive oxygen species and expression of phosphoinositide-3-kinase interacting protein 1 (Figure 1), respectively. SLC1A5, also known as alanine-serine-cysteine transporter 2, mediates glutamine transportation, as well as other solute carriers (SLCs) including SLC6A14, 19, and SLC38A1-5[26]. Increasing GLS leads to a proinflammatory effector phenotype, while restriction of GLS results in a slanted Treg differentiation through the inhibition of oxidative phosphorylation[27]. In addition, hepatocyte mitochondrial pyruvate carrier disruption redirected glutamine from glutathione synthesis into the tricarboxylic acid cycle, which impaired HCC by limiting glutathione synthesis[28]. Another study showed that inhibition of glutamine metabolism can reduce T-cell exhaustion and increase the antitumor activity of tumor-specific CD8+ T cells against mouse lymphoma[29]. Overall, the function of glutamine on CD8+ T cells is dependent on tumor microenvironment and tumor type. Meanwhile, regulation of nutrient metabolism could be a synergetic strategy for cancer treatment.
Figure 1.
Glutamine metabolism impacts T cell differentiation and tumor growth. Glutamine metabolism can be transferred into cells by solute carriers, such as Solute carrier family 1 member 5 (also known as alanine-serine-cysteine transporter 2). It can be metabolized into glutamate through glutaminolysis (GLS) to impact T helper 17 (Th17) cells, Th1, and CD8 T cell differentiation by regulating the production of reactive oxygen species and expression of phosphoinositide-3-Kinase Interacting Protein 1, respectively. Increasing GLS leads to a proinflammatory effector phenotype, while restriction of GLS causes a slanted Treg differentiation by inhibiting oxidative phosphorylation. In addition, hepatocyte mitochondrial pyruvate carrier disruption redirects glutamine from glutathione synthesis into the tricarboxylic acid cycle, which impaired hepatocellular carcinoma by limiting glutathione synthesis. MPC: Mitochondrial pyruvate carrier; TCA: Tricarboxylic acid; SLC1A5: Solute carrier family 1 member 5; GLS: Glutaminolysis; OXPHOS: Oxidative phosphorylation; TOR: Target of Rapamycin; Th1: T helper 1; PIK3IP1: Phosphoinositide-3-Kinase Interacting Protein 1; ROS: Reactive oxygen species.
Footnotes
Conflict-of-interest statement: All authors declare no conflicts of interest.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: June 18, 2022
First decision: July 19, 2022
Article in press: August 16, 2022
Specialty type: Oncology
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Liao R, China; Lu H, China; Yang L, China S-Editor: Wang LL L-Editor: A P-Editor: Wang LL
Contributor Information
Chun-Ye Zhang, Department of Veterinary Pathobiology, University of Missouri, Columbia, MO 65211, United States.
Shuai Liu, The First Affiliated Hospital, Zhejiang University, Hangzhou 310006, Zhejiang Province, China.
Ming Yang, Department of Surgery, University of Missouri, Columbia, MO 65211, United States. yangmin@health.missouri.edu.
References
- 1.Wang W GM, Li N, Pang DQ, Wu JH. Glutamine deprivation impairs function of infiltrating CD8+ T cells in hepatocellular carcinoma by inducing mitochondrial damage and apoptosis. World J Gastrointest Oncol. 2022;14:1124–1140. doi: 10.4251/wjgo.v14.i6.1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71:209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 3.Zhang C, Liu S, Yang M. Hepatocellular Carcinoma and Obesity, Type 2 Diabetes Mellitus, Cardiovascular Disease: Causing Factors, Molecular Links, and Treatment Options. Front Endocrinol (Lausanne) 2021;12:808526. doi: 10.3389/fendo.2021.808526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sangro B, Sarobe P, Hervás-Stubbs S, Melero I. Advances in immunotherapy for hepatocellular carcinoma. Nat Rev Gastro Hepat. 2021;18:525–543. doi: 10.1038/s41575-021-00438-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim HD, Song GW, Park S, Jung MK, Kim MH, Kang HJ, Yoo C, Yi K, Kim KH, Eo S, Moon DB, Hong SM, Ju YS, Shin EC, Hwang S, Park SH. Association Between Expression Level of PD1 by Tumor-Infiltrating CD8+ T Cells and Features of Hepatocellular Carcinoma. Gastroenterology. 2018;155:1936–1950.e17. doi: 10.1053/j.gastro.2018.08.030. [DOI] [PubMed] [Google Scholar]
- 6.Shi F, Shi M, Zeng Z, Qi RZ, Liu ZW, Zhang JY, Yang YP, Tien P, Wang FS. PD-1 and PD-L1 upregulation promotes CD8(+) T-cell apoptosis and postoperative recurrence in hepatocellular carcinoma patients. Int J Cancer. 2011;128:887–896. doi: 10.1002/ijc.25397. [DOI] [PubMed] [Google Scholar]
- 7.Jin H, Qin S, He J, Xiao J, Li Q, Mao Y, Zhao L. New insights into checkpoint inhibitor immunotherapy and its combined therapies in hepatocellular carcinoma: from mechanisms to clinical trials. Int J Biol Sci. 2022;18:2775–2794. doi: 10.7150/ijbs.70691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.El-Khoueiry AB, Sangro B, Yau T, Crocenzi TS, Kudo M, Hsu C, Kim TY, Choo SP, Trojan J, Welling TH Rd, Meyer T, Kang YK, Yeo W, Chopra A, Anderson J, Dela Cruz C, Lang L, Neely J, Tang H, Dastani HB, Melero I. Nivolumab in patients with advanced hepatocellular carcinoma (CheckMate 040): an open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet. 2017;389:2492–2502. doi: 10.1016/S0140-6736(17)31046-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saung MT, Pelosof L, Casak S, Donoghue M, Lemery S, Yuan M, Rodriguez L, Schotland P, Chuk M, Davis G, Goldberg KB, Theoret MR, Pazdur R, Fashoyin-Aje L. FDA Approval Summary: Nivolumab Plus Ipilimumab for the Treatment of Patients with Hepatocellular Carcinoma Previously Treated with Sorafenib. Oncologist. 2021;26:797–806. doi: 10.1002/onco.13819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fessas P, Kaseb A, Wang Y, Saeed A, Szafron D, Jun T, Dharmapuri S, Rafeh Naqash A, Muzaffar M, Navaid M, Khan U, Lee C, Bulumulle A, Yu B, Paul S, Nimkar N, Bettinger D, Benevento F, Hildebrand H, Pressiani T, Abugabal YI, Personeni N, Huang YH, Rimassa L, Ang C, Marron T, Pinato DJ. Post-registration experience of nivolumab in advanced hepatocellular carcinoma: an international study. J Immunother Cancer. 2020;8 doi: 10.1136/jitc-2020-001033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.D'Alessio A, Rimassa L, Cortellini A, Pinato DJ. PD-1 Blockade for Hepatocellular Carcinoma: Current Research and Future Prospects. J Hepatocell Carcinoma. 2021;8:887–897. doi: 10.2147/JHC.S284440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rochigneux P, Chanez B, De Rauglaudre B, Mitry E, Chabannon C, Gilabert M. Adoptive Cell Therapy in Hepatocellular Carcinoma: Biological Rationale and First Results in Early Phase Clinical Trials. Cancers (Basel) 2021;13 doi: 10.3390/cancers13020271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang C, Yang M. Targeting T Cell Subtypes for NAFLD and NAFLD-Related HCC Treatment: An Opinion. Front Med (Lausanne) 2021;8:789859. doi: 10.3389/fmed.2021.789859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang T, Gnanaprakasam JNR, Chen X, Kang S, Xu X, Sun H, Liu L, Rodgers H, Miller E, Cassel TA, Sun Q, Vicente-Muñoz S, Warmoes MO, Lin P, Piedra-Quintero ZL, Guerau-de-Arellano M, Cassady KA, Zheng SG, Yang J, Lane AN, Song X, Fan TW, Wang R. Inosine is an alternative carbon source for CD8+-T-cell function under glucose restriction. Nat Metab. 2020;2:635–647. doi: 10.1038/s42255-020-0219-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wu J, Li G, Li L, Li D, Dong Z, Jiang P. Asparagine enhances LCK signalling to potentiate CD8+ T-cell activation and anti-tumour responses. Nat Cell Biol. 2021;23:75–86. doi: 10.1038/s41556-020-00615-4. [DOI] [PubMed] [Google Scholar]
- 16.Di Biase S, Ma X, Wang X, Yu J, Wang YC, Smith DJ, Zhou Y, Li Z, Kim YJ, Clarke N, To A, Yang L. Creatine uptake regulates CD8 T cell antitumor immunity. J Exp Med. 2019;216:2869–2882. doi: 10.1084/jem.20182044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ma EH, Bantug G, Griss T, Condotta S, Johnson RM, Samborska B, Mainolfi N, Suri V, Guak H, Balmer ML, Verway MJ, Raissi TC, Tsui H, Boukhaled G, Henriques da Costa S, Frezza C, Krawczyk CM, Friedman A, Manfredi M, Richer MJ, Hess C, Jones RG. Serine Is an Essential Metabolite for Effector T Cell Expansion. Cell Metab. 2017;25:482. doi: 10.1016/j.cmet.2017.01.014. [DOI] [PubMed] [Google Scholar]
- 18.Reina-Campos M, Scharping NE, Goldrath AW. CD8+ T cell metabolism in infection and cancer. Nat Rev Immunol. 2021;21:718–738. doi: 10.1038/s41577-021-00537-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kumagai S, Koyama S, Itahashi K, Tanegashima T, Lin YT, Togashi Y, Kamada T, Irie T, Okumura G, Kono H, Ito D, Fujii R, Watanabe S, Sai A, Fukuoka S, Sugiyama E, Watanabe G, Owari T, Nishinakamura H, Sugiyama D, Maeda Y, Kawazoe A, Yukami H, Chida K, Ohara Y, Yoshida T, Shinno Y, Takeyasu Y, Shirasawa M, Nakama K, Aokage K, Suzuki J, Ishii G, Kuwata T, Sakamoto N, Kawazu M, Ueno T, Mori T, Yamazaki N, Tsuboi M, Yatabe Y, Kinoshita T, Doi T, Shitara K, Mano H, Nishikawa H. Lactic acid promotes PD-1 expression in regulatory T cells in highly glycolytic tumor microenvironments. Cancer Cell. 2022;40:201–218.e9. doi: 10.1016/j.ccell.2022.01.001. [DOI] [PubMed] [Google Scholar]
- 20.Elia I, Rowe JH, Johnson S, Joshi S, Notarangelo G, Kurmi K, Weiss S, Freeman GJ, Sharpe AH, Haigis MC. Tumor cells dictate anti-tumor immune responses by altering pyruvate utilization and succinate signaling in CD8+ T cells. Cell Metab. 2022 doi: 10.1016/j.cmet.2022.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Manzo T, Prentice BM, Anderson KG, Raman A, Schalck A, Codreanu GS, Nava Lauson CB, Tiberti S, Raimondi A, Jones MA, Reyzer M, Bates BM, Spraggins JM, Patterson NH, McLean JA, Rai K, Tacchetti C, Tucci S, Wargo JA, Rodighiero S, Clise-Dwyer K, Sherrod SD, Kim M, Navin NE, Caprioli RM, Greenberg PD, Draetta G, Nezi L. Accumulation of long-chain fatty acids in the tumor microenvironment drives dysfunction in intrapancreatic CD8+ T cells. J Exp Med. 2020;217 doi: 10.1084/jem.20191920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ringel AE, Drijvers JM, Baker GJ, Catozzi A, García-Cañaveras JC, Gassaway BM, Miller BC, Juneja VR, Nguyen TH, Joshi S, Yao CH, Yoon H, Sage PT, LaFleur MW, Trombley JD, Jacobson CA, Maliga Z, Gygi SP, Sorger PK, Rabinowitz JD, Sharpe AH, Haigis MC. Obesity Shapes Metabolism in the Tumor Microenvironment to Suppress Anti-Tumor Immunity. Cell. 2020;183:1848–1866.e26. doi: 10.1016/j.cell.2020.11.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Best SA, Gubser PM, Sethumadhavan S, Kersbergen A, Negrón Abril YL, Goldford J, Sellers K, Abeysekera W, Garnham AL, McDonald JA, Weeden CE, Anderson D, Pirman D, Roddy TP, Creek DJ, Kallies A, Kingsbury G, Sutherland KD. Glutaminase inhibition impairs CD8 T cell activation in STK11-/Lkb1-deficient lung cancer. Cell Metab. 2022;34:874–887.e6. doi: 10.1016/j.cmet.2022.04.003. [DOI] [PubMed] [Google Scholar]
- 24.Qin R, Zhao C, Wang CJ, Xu W, Zhao JY, Lin Y, Yuan YY, Lin PC, Li Y, Zhao S, Huang Y. Tryptophan potentiates CD8+ T cells against cancer cells by TRIP12 tryptophanylation and surface PD-1 downregulation. J Immunother Cancer. 2021;9 doi: 10.1136/jitc-2021-002840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hezaveh K, Shinde RS, Klötgen A, Halaby MJ, Lamorte S, Ciudad MT, Quevedo R, Neufeld L, Liu ZQ, Jin R, Grünwald BT, Foerster EG, Chaharlangi D, Guo M, Makhijani P, Zhang X, Pugh TJ, Pinto DM, Co IL, McGuigan AP, Jang GH, Khokha R, Ohashi PS, O'Kane GM, Gallinger S, Navarre WW, Maughan H, Philpott DJ, Brooks DG, McGaha TL. Tryptophan-derived microbial metabolites activate the aryl hydrocarbon receptor in tumor-associated macrophages to suppress anti-tumor immunity. Immunity. 2022;55:324–340.e8. doi: 10.1016/j.immuni.2022.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang W, Zou W. Amino Acids and Their Transporters in T Cell Immunity and Cancer Therapy. Mol Cell. 2020;80:384–395. doi: 10.1016/j.molcel.2020.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Desdín-Micó G, Soto-Heredero G, Mittelbrunn M. Mitochondrial activity in T cells. Mitochondrion. 2018;41:51–57. doi: 10.1016/j.mito.2017.10.006. [DOI] [PubMed] [Google Scholar]
- 28.Tompkins SC, Sheldon RD, Rauckhorst AJ, Noterman MF, Solst SR, Buchanan JL, Mapuskar KA, Pewa AD, Gray LR, Oonthonpan L, Sharma A, Scerbo DA, Dupuy AJ, Spitz DR, Taylor EB. Disrupting Mitochondrial Pyruvate Uptake Directs Glutamine into the TCA Cycle away from Glutathione Synthesis and Impairs Hepatocellular Tumorigenesis. Cell Rep. 2019;28:2608–2619.e6. doi: 10.1016/j.celrep.2019.07.098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nabe S, Yamada T, Suzuki J, Toriyama K, Yasuoka T, Kuwahara M, Shiraishi A, Takenaka K, Yasukawa M, Yamashita M. Reinforce the antitumor activity of CD8+ T cells via glutamine restriction. Cancer Sci. 2018;109:3737–3750. doi: 10.1111/cas.13827. [DOI] [PMC free article] [PubMed] [Google Scholar]