Abstract
Previous research supports a link between school-related factors, such as bullying and school connectedness, and suicidal thoughts and behaviors. To deepen understanding of how school experiences may function as both protective and risk factors for youth struggling with suicidal thoughts and behaviors, this qualitative study explored multiple perspectives. Specifically, in-depth interviews were conducted with adolescents previously hospitalized for a suicidal crisis (n = 19), their parents (n = 19), and the professionals they may interact with in schools and hospitals (i.e., school professionals [n = 19] and hospital providers [n = 7]). Data were analyzed using applied thematic analysis revealing three main themes related to perceptions of how school experiences can positively or negatively impact mental health: School activities, school social experiences, and school interventions. An emergent theme related to the complexity of suicide-related risk identified the ways in which school experiences may intersect with other environmental, biological, and psychological factors. Findings underscore the need for school-based approaches to address the unique academic, social, and emotional needs of students with suicide-related risk that complement the supports and services provided in their home and community.
Keywords: Suicidal thoughts and behaviors, qualitative research, school, adolescent, parent, professional
Schools have been called upon to provide systematic suicide prevention programs that span from upstream approaches for bolstering protective factors against suicide to tertiary services for youth with heightened risk for suicide (e.g., Miller, 2021; Singer et al., 2019). School mental health professionals (e.g., psychologists, counselors, social workers, nurses) may be charged with delivering universal suicide prevention programs, providing targeted interventions for social and emotional concerns, formulating risk assessments, providing referrals to care, communicating with community providers, supporting school re-entry following a mental health crisis, and coordinating postintervention following a student death (Joshi et al., 2015; Surgenor et al., 2016). Although these supports and services vary in scope, frequency, and intensity, inherent to all these practices is the aim of mitigating risk related to suicide and reinforcing protective factors against suicide.
Although varying across cultural context (Marraccini, Griffin, et al., 2022; Marraccini, Ingram, et al., 2022), school-related risk and protective factors of suicide can be considered within an ideation-to-action framework. Ideation-to-action theories of suicide postulate distinct pathways of suicidal thoughts (i.e., suicidal ideation, including thinking about or making a plan about suicide) to suicidal behaviors (i.e., action, including attempting suicide; Klonsky et al., 2018). For example, the interpersonal theory of suicide posits that hopelessness about feelings of disconnect and burdensomeness may contribute to suicidal ideation, with reduced fear of death, increased pain tolerance, and access to means facilitating the move from thinking about suicide to acting on suicide (Van Orden et al., 2010). Aligned within this model, schools can contribute protective effects against suicidal ideation by enhancing feelings of belongingness and connectedness between school community members (Marraccini & Brier, 2017), but can also confer risk for suicidal ideation if negative experiences such as bullying, social difficulties, and discrimination are not prevented (Assari et al., 2017; Holt et al., 2015; van Geel et al., 2022; Walker et al., 2017). Moreover, school-based mental health preventions and interventions, school referrals to care, and school structures that prevent access to means may play a role in disrupting the shift from ideation to action.
Few studies have addressed school factors that may influence risk for suicidal thoughts and behaviors in clinical samples of adolescents. However, preliminary findings suggest that feeling connected to school is associated with improved recovery from a mental health crisis (King et al., 2019; Marraccini, Resnikoff, et al., 2021). Conversely, stressors such as bullying experiences and academic difficulties can confer risk for suicidal thoughts and behaviors and rehospitalization (Luukkonen et al., 2009; Marraccini, Resnikoff, et al., 2021; Tossone et al., 2014). Although this formative work helps establish the significance of school-related relationships for recovery from a mental health crisis, missing from this work is an exploration of the mechanisms linking school-related experiences with mental health outcomes in adolescents with suicidal thoughts and behaviors.
Drawing on previous work that has identified social (e.g., having to describe to their peers where they have been), academic (work remediation), and emotional (management of mental health symptoms) concerns for adolescents returning to school following psychiatric hospitalization (Marraccini & Pittleman, 2022; Preyde et al., 2017, 2018), the present study aimed to deepen understanding of how school-related experiences may influence suicidal thoughts and behaviors in adolescents with suicide-related risk. By exploring the lived experiences of adolescents previously hospitalized for a suicide-related crisis, as well as their parents, school professionals, and clinical providers, this study complements previous work that has identified a link in school-related experiences with suicide-related risk and protective factors. The primary aim of this qualitative study was to explore multiple perspectives of how school may intersect with suicide-related risk and recovery.
Theoretical Framework
From an ecological perspective, school environment and school experiences may influence both the development of suicidal ideation and the shift from ideation to action. Ecological systems theory posits that a child’s environment transacts with their development across multiple levels (Bronfenbrenner, 1996). Thus, consideration of how school may influence suicide-related risk spans all layers of a student’s ecology: schools may play a role in supporting student identity development (ontosystem), creating safe and inclusive spaces for students to learn and thrive (microsystem), building school-family-community partnerships to support student development (mesosystem), being part of safe communities for schools to actualize supports (macrosystem), and accounting for how social norms that include or exclude youth with diverse identities and mental health needs may shape schools (exosystem; Marraccini, Ingram, et al., 2022).
When considered within the cognitive-behavioral model of adolescent suicide (Spirito et al., 2012), proximal influences of schools (e.g., school values, structures, processes, relationships) can serve as stressors or protective factors of suicide when intersecting with a student’s internal processes (i.e., maladaptive cognition, behavior, and affective responses may lead to suicide risk). Risk for suicide, and the relationship between school and a student’s internal processes influencing risk, are also influenced by other microsystem level influences (e.g., family cohesiveness, community networks). Thus, school experiences and school environment are among many potential contributors to risk that must be considered within the unique context of a student (including both internal and external processes).
Consideration of cultural variation in risk factors and the ways in which they intersect with school norms and values is also critical for understanding school context and risk for suicide (Marraccini, Griffin, et al., 2022; Marraccini, Ingram, et al., 2022). Culture not only influences risk for suicide, but it is also shapes how suicide, associated risk factors, and associated protective factors are defined and expressed (Chu et al., 2010). For example, acculturative stress and racial discrimination are associated with suicidal thoughts and behaviors in racial and ethnic minoritized youth, and collaborative religion and spirituality may play a protective role against it (Goldston et al., 2008). Cultural interpretations and expressions (e.g., acceptability of stressors and suicidality) can influence the development of suicidal thoughts and behaviors (Chu et al., 2010).
A student’s identity, including their gender, sexuality, race, ethnicity, disability, and more, is at the center of a student’s ontosystem. It may be impacted by both proximal and distal stressors unique to ethnic, racial, sexual, and gender minoritized and economically disadvantaged individuals (Meyer, 2003). As outlined by the minority stress model, these may include experienced and expected discrimination and prejudice, which may be internalized and intersect with other risk and protective factors for suicide (Fulginiti et al., 2020; Meyer, 2003). Although originally proposed for understanding health risk in individuals identifying as lesbian, gay, bisexual, transgender, questioning, intersex, two spirit, and queer (LGBTQ+), a rich body of work suggests that these stressors are salient to suicide-related risk across a wide range of identities associated with societal disadvantages (Chu et al., 2010). Thus, a holistic understanding of school context and risk for suicide accounts for the intersectional experiences of multiple disadvantages. Such understanding must take an intersectionality lens, which acknowledges how interlocking systems of privilege, power, and oppression may interact to shape experiences according to a combination of identities (Crenshaw, 1989).
Building from intersectionality theory, along with critical race and disability theories, Disability Critical Race Theory (DisCrit) centers the intersection of the social constructs of race and disability (Sabnis & Bueno Martinez, 2022). Specifically, “DisCrit seeks to understand ways that macrolevel issues of racism and ableism, among other structural discriminatory processes, are enacted in the day-to-day lives of students of color with dis/abilities” (Annamma et al., 2013. p. 8). Because suicide is transdiagnostic – that is, risk for suicide has been found to associate with nearly all major mental health disorders (Schechter & Goldblatt, 2020) – and individuals with suicidal thoughts and behaviors represent a wide range in severity of symptoms, DisCrit helps frame how an understanding of school influences of suicide-related risk must acknowledge how intersecting identities, inclusive of identifying as having a mental health disorder, interact with cultural and contextual variations of suicide risk. For each unique identity, school experiences and norms can relate to development of or protection from suicide-related risk differently. For example, acceptance of LGBTQ+ identity and severity of symptoms related to suicide-related risk may be interpreted differently by school professionals and student families (Marraccini, Griffin, et al., 2022; Marraccini, Ingram, et al., 2022).
School Related Risk and Protective Factors of Suicide
Recent reviews of school-related risk and protective factors of suicidal thoughts and behaviors focused on LGBTQ+ (Marraccini, Ingram, et al., 2022) and ethnic and racial minoritized (Marraccini, Griffin, et al., 2022) students have identified the significance of multiple components of school for understanding suicide-related risk in youth. Key factors may include school relationships (e.g., bullying that can occur in and out of schools, feelings of connectedness to teachers and peers), academic stressors and difficulties, and school processes (e.g., comprehensive suicide prevention programs; inclusive programs and policies that are welcoming to diverse students).
Although most research aimed at understanding school-related risk and protective factors of suicidal thoughts and behaviors has employed quantitative approaches, a rich literature based on qualitative research has explored experiences and perceptions of suicide in adolescents more generally. For example, Grimmond and colleagues (2019) conducted a systematic review of 27 qualitative inquiries focused on understanding youth and young adult suicide attempts, categorizing findings according to (a) triggers and risks leading to suicidality (including peer influences and academic challenges), (b) factors involved in recovery, (c) needs for institutional treatment/prevention strategies (including education in schools and specialized support and education for parents), and (d) beliefs about suicide within the wider culture. In the following sections we expand on quantitative and qualitative research exploring each of these school-specific components (school social supports and school connectedness, social difficulties and bullying, academic stressors and difficulties, and school processes for preventing suicide) as they relate to suicide-related risk in youth.
School Relationships and Connectedness
School connectedness has emerged as a potential protective factor against suicidal thoughts and behaviors. Findings from a 2017 meta-analysis indicated that when students feel connected to their school (by way of teachers and peers), they are approximately half as likely to report past suicidal thoughts or suicide attempts (Marraccini & Brier, 2017). Students feeling connected to their schools also appear less likely to report a suicide attempt in the months following an emergency department visit (King et al., 2019). Moreover, positive student teacher relationships (Marraccini, Resnikoff, et al., 2021) and connectedness to peers (Czyz et al., 2012) can support student recovery following a suicide related crisis.
When findings from quantitative studies are stratified by race, ethnicity, and gender identity, the protective effects of school connectedness are less consistent. Although school connectedness appears to play a protective role among American Indian and Hispanic students, its protective effects appear less consistent among Asian, Black, and LGBTQ+ students (Marraccini, Griffin, et al., 2022; Marraccini, Ingram, et al., 2022). Qualitative findings have largely pointed to peer supports (in and out of schools) as a salient theme for understanding recovery from suicide-related crises among adolescents globally (Bostik & Everall, 2007; Shilubane et al., 2012; Strickland & Cooper, 2011), but have less frequently explored the potential for adults in school to play a supportive role towards prevention and recovery (although the dearth of research focused on Black and African American and LGBTQ+ youth is consistent in qualitative studies).
Bullying and Peer Conflict
Bullying experiences and peer conflict may also confer risk for suicide. Several meta-analyses suggest that students reporting bullying victimization, bullying perpetration, or both, are approximately two to three times more likely to report suicidal thoughts and behaviors as compared to those without a history of bullying experiences or behaviors (Holt et al., 2015; Van Geel et al., 2014). They are also approximately one and a half to two times more likely to report suicidal thoughts and behaviors over time (Van Geel et al., 2022). Bullying appears to serve as a risk-factor for suicidal thoughts and behaviors among most ethnic, racial, sexual, and gender minoritized youth (Marraccini, Griffin, et al., 2022; Marraccini, Resnikoff et al., 2021). Several qualitative inquiries have identified bullying experiences as a perceived contributor to distress or risk for suicide, including Zayas and colleagues’ (2010) study exploring perspectives of Latina youth with a history of suicidal thoughts and behaviors and Matel-Anderson and Bekhet’s (2016) study focused on provider (i.e., nurses) perspectives.
Academic Stress and Pressure
Compared to research focused on school connectedness and bullying experiences, fewer studies have investigated how academic difficulties (and, conversely, academic successes) are associated with suicidal thoughts and behaviors. However, the relationship between academic performance and mental health more generally has been demonstrated in a recent meta-analysis (Bas, 2021), suggesting a bidirectional relationship of academic success and mental health functioning. A few studies have also supported this relationship for suicidal thoughts and behaviors specifically. Higher grades were shown to associate with lower scores on a measure of suicide-related risk (including indicators of depression and suicidal thoughts and behaviors) in a national sample of African American and Asian American students (Whaley & Noel, 2003). In a sample of students in New Mexico, students with plans for postsecondary education were approximately 60% less likely to report having made a suicide attempt compared to those without plans (Hall et al., 2018). Qualitative studies have also illustrated the ways in which academics may play a role in recovery from suicide-related crises, including concerns about academic pressure, academic difficulties, and overly focusing on academics (Gulbas & Zayas, 2015; Gulbas et al., 2015; Keyvanara & Haghshenas, 2011; Shilubane et al., 2014).
School Processes: Comprehensive Suicide Prevention Programs
Beyond the influence of school experiences and environments, schools are increasingly called upon to deliver comprehensive suicide prevention programs. Schools are ethically, and, in more than half of the states in the US, legally, required to provide training for suicide prevention (American Foundation for Suicide Prevention, 2020). The most effective suicide prevention programs are postulated to be those that (a) include a mechanism for identifying students at risk; (b) are embedded across all levels of the multitiered systems of support (including general education curriculum); (c) employ a gatekeeping approach wherein school faculty, staff, and students are aware of referral processes; and (d) efficiently connect youth with risk to suicide to school and community services (King et al., 2018; Miller & Mazza, 2018; Singer et al., 2019).
Despite growing interest in such programs, indicators of efficacy are limited due to both implementation and evaluation challenges, with research tending to rely on intermediate indicators such as knowledge and attitudes related to help-seeking and suicide, with less understanding about program effects on behavior (e.g., reducing risk for suicide; Klimes-Dougan et al., 2013; Singer et al., 2019). Still, several programs that can be considered within a multitiered systems of support (MTSS) framework have emerged as best practice. These may include (a) promoting protective factors and preventing risk factors for suicide and screening for suicide-related risk at the universal (tier 1) level, (b) identifying and intervening in suicide-related risk and enacting crisis protocols at the selected (tier 2) level, and (c) delivering intensive supports and interventions for youth identified with suicide-related risk, as well as enacting postvention interventions following death due to suicide at the indicated (tier 3) level (Singer et al., 2019). Recent findings have also prioritized “upstream” approaches that aim to address risk factors for suicide prior to the onset of risk for suicide (Singer et al., 2019; Wyman, 2014) as promising universal prevention associated with lower likelihood for suicidal ideation and attempts (Wilcox et al., 2008).
Several qualitative studies that involve community samples of adolescents and care providers (Coggan et al., 1997; Schwartz et al., 2010), as well as samples of youth with peers who had attempted or died of suicide (Shilubane et al., 2014), have identified the need for increased access to services and resources dedicated to suicide prevention in schools. Yet, there may be a chasm between family and school professional perspectives regarding standard procedures for risk assessment. Families have voiced concerns about assessments feeling intrusive and disciplinary, but professionals have shared their appreciation for the structured nature of standardized protocols (Kodish et al., 2020). School professionals delivering school-based suicide prevention programs have also described the difficulty in engaging in dialogue with students when expressions of suicide emerge (White & Morris, 2010).
Such findings align to those reported in a qualitative analysis of 22 quantitative and 30 qualitative datasets addressing barriers and facilitators to adolescent help seeking for mental health care, the majority of which took place in school settings (Radez et al., 2021). Radez and colleagues described barriers to help seeking in and out of schools to include social (e.g., stigma) and therapeutic relationships (e.g., confidentiality concerns), as well as personal factors (e.g., limited knowledge) and structural barriers (e.g., logistical, financial). Thus, even with dedicated resources and interventions addressing suicide prevention, there are additional structural, systemic, and interpersonal obstacles to accessing mental health care in schools.
The Present Study
Risk for suicide is complex and stems from a combination of biological, environmental, and psychological risk factors. Although research to date suggests that there are multiple ways in which schools can help to prevent suicide, the majority of studies have used quantitative methods to identify general predictors or have explored qualitative perceptions of risk more generally, without focusing explicitly on school context. In sum, this work has yet to elucidate the mechanisms or ways in which these school specific risk and protective factors may relate to suicidal thoughts and behaviors. The present study aimed to deepen understanding of school-related risk and protective factors of suicidal thoughts and behaviors among youth with suicide-related crises. Specifically, we aimed to address the following research question: How do adolescents with a history of suicide-related crises, their parents, school professionals, and hospital professionals describe school-related influences of suicidal thoughts and behaviors and mental health?
Material and Method
This qualitative research is part of a larger mixed-methods study that is developing school re-entry guidelines for adolescents hospitalized for suicidal thoughts and behaviors. The larger study involved three phases of data collection, including (a) a survey of school professionals across one state (n = 133); (b) in-depth interviews with adolescents previously hospitalized for suicidal thoughts and behaviors (n=19), their parents (n = 19), school professionals (n = 19), and hospital professionals (n = 7); and (c) iterative development of school re-entry guidelines based on feedback from representative participants completing focus group and one-on-one interviews. In our previous analyses addressing data as part of Phases 1 and 2, we focused on adolescent and school professional descriptions and experiences related to school reintegration following psychiatric hospitalization and informing the types of supports adolescents may require as they return to school (see Marraccini & Pittleman, 2022; Marraccini, Pittleman, et al., 2022). The present study also focused on qualitative data collected from the interviews conducted during Phase 2, but explored adolescent, parent, school professional, and hospital professional perceptions of school influences of suicide-related risk more generally (as opposed to focusing on school reintegration only).
Participants
Participants included four cohorts consisting of adolescent (n = 19) and parent (n = 19) dyads, school professionals (n = 19), and hospital professionals (n = 7). Each cohort was selected to enhance understanding of adolescent school experiences. We focused on adolescents because they are the individuals interfacing with schools as students experiencing suicidal thoughts and behaviors. We included parents because they are often a primary caregiver of adolescents and may have an indirect understanding of school experiences by way of their adolescent and direct experiences with school by advocating for their adolescent and interacting with school through meetings and events. We included school professionals because they can be involved in supporting adolescents with suicidal thoughts and behaviors and may directly observe adolescent experiences in schools. Finally, we included hospital professionals, because they deliver acute treatment to adolescents that involves understanding and assessing suicide-related risk and protective factors, drivers, and triggers; and because they integrate school assessments into treatment decision making.
Final sample sizes for each cohort were based on assessment of data saturation by monitoring debrief summaries following interview completion with consideration of representativeness within each cohort. Specific representativeness considerations included (a) severity of suicidal thoughts and behaviors among adolescent and parent dyad participants, (b) school demographic characteristics among school professional participants, and (c) professional roles among school and hospital professional participations. All participants completed consent and/or assent procedures prior to participating in the study and were informed of ethical protections for their participation (i.e., a certificate of confidentiality provided by National Institute of Mental Health). As compensation for their time, adolescent participants received $30, parent participants received $25, and school and hospital professional participants received $20.
Adolescent/Parent Dyads
Adolescent and parent participants were identified from medical records of adolescent patients with a hospital billing code related to suicidal thoughts and behaviors within a large hospital located in the southeast United States. Adolescent eligibility criteria were (a) hospitalization for suicidal thoughts and behaviors at a psychiatric inpatient facility, (b) ages 13–18 years (Mage = 15.7, SD = 1.3), (c) return to school following hospitalization, and (d) ability to speak, read, and understand English sufficiently to complete study procedures. One legal guardian of each participating adolescent was eligible to participate.
A total of 1399 records were extracted at three different times over a 16-month window. After removing records that indicated patients were not admitted to an inpatient hospital (n = 1198; e.g., they were seen in the emergency department or a medical unit only), a total of 231 records were screened for eligibility on an ongoing basis. Records were excluded if they were identified as duplicates (n = 10), identified as requiring interpreter services during hospital interactions (n = 11), or no longer met eligibility criteria (n = 87). Note that because the records were static and our recruitment was ongoing, records in the latter category primarily reflected those that were no longer eligible to participate based on date of discharge or age at the time of recruitment.
In total, we mailed 123 “opt-out” letters to families, following up by phone to describe study procedures. A total of 19 (15.4%) adolescent/parent dyads (n = 17 mothers and n = 2 fathers; ages 29–56 years, Mage = 45.7, SD = 7.7) participated in the study and completed consent and assent procedures in-person or virtually (depending on safety during the pandemic). The remaining families did not participate because they (a) indicated that they were not interested in participating (n = 22, 17.9%), (b) did not return our phone calls or no longer had the same contact information as indicated in their medical records (n = 60, 48.8%), or (c) were not eligible to participate based on eligibility criteria (n = 19 [15.4%], of whom three [2.4%] were ineligible because they were not proficient in English to complete study procedures).
School Professionals
We also conducted in-depth interviews with a purposive sample of school professionals (n = 19) participating in Phase 1 of the study, in which we recruited school professionals providing school-based mental health services across one southeastern state to complete surveys about school reintegration (n = 133). School professional participants, as part of Phase 1, were recruited within 35 participating school districts using an email invitation. When completing the consent process during Phase 1, school professionals indicated their interest in completing qualitative interviews and researchers followed up with interested participants by email and phone. The final sample of school professional participants as part of Phase 2 was selected to represent individuals working in a range of school-based roles in different districts across the state. School professional participants included school psychologists (n = 4), school counselors (n = 4), social workers (n = 4), nurses (n = 2), one principal, one special education teacher, and one professional who identified as “other.”
Hospital Professionals
Hospital professionals were recruited by way of email invitations to one psychiatric inpatient facility in the same state. Any hospital professionals working in the facility supporting adolescents hospitalized for suicide-related crises at the facility were eligible. Hospital professionals included two individuals working in the hospital’s school, with the remaining participants working in treatment as occupational therapists, recreational therapists, or attending physicians. Note that although the hospital professionals worked in a hospital or the hospital’s school setting and did not directly observe adolescents in their community school environments, they described a range of relevant experiences. These included speaking with adolescents about school experiences, planning for adolescent return to school settings, and integrating school-based reports into their treatment planning.
Procedure
Study procedures were approved by the Institutional Review Board. Following parent permission for adolescents under the age of 18 years, adolescents completed informed assent procedures. All adult participants (i.e., adult adolescents, parents, school professionals, and hospital professionals) completed informed consent prior to participation. Following consent and assent procedures, all participants completed interviews; adolescent, parent, and school professional participants also completed a brief set of questionnaires that varied according to cohort.
Instrumentation
Self-Report Measures and Clinical Interviews
Demographic data were collected using a self-report survey for adolescent, parent, and school professional participants and by using verbal prompts for hospital professionals. Although specific questions varied by cohort (i.e., adolescents and parents were asked about household income, attendance, grades, and special education services; school and hospital professionals were asked about their profession and number of years working in the profession), all participants were asked about their race, ethnicity, and gender. The questions asking about ethnicity and race adhered to a two-question format, addressing ethnicity and race separately.1 To address ethnicity, participants were asked: “Are you Hispanic or Latinx?” Response options on the survey for race included American Indian or Alaska Native, Asian, Black or African American, Native Hawaiian or Pacific Islander, White, or Other. If adolescent and parent participants selected “Other” an open-ended text box allowed them to self-describe their race. This option to self-describe race was not included for school or hospital professional participants.
To assess gender, hospital and school professional participants were asked “Which of the following describes your gender?” Response options included male, female, or other. The questions asking adolescent and parent participants about their gender were selected based on recommendations from the Gender Identity in U.S. Surveillance (GenIUSS) group for identifying transgender and other gender minoritized individuals (The GenIUSS Group, 2014) and youth specifically (Greytak et al., 2014). Accordingly, we used a two-step procedure wherein we first asked participants to identify sex as described on their birth certificate and next asked participants to select or identify their gender. Parent participants were asked the question, “How do you describe yourself? (check one),” and response options included female, male, transgender, and I do not identify as female, male, or transgender. Adolescents were provided with the following prompt: “When a person’s sex and gender do not match, they might think of themselves as transgender. Sex is what a person is born with. Gender is how a person feels. What one response best describes you?” Response options included I identify as a boy or man, I identify as a girl or woman, I identify in some other way, I do not know what this question is asking, or I do not know if I am transgender. Adolescent and parent participants also identified their sexual orientation by selecting from the following response options: Heterosexual or straight, bisexual, gay or lesbian. They identified their sexual attraction to others by selecting from only attracted to females, mostly attracted to females, equally attracted to females and males, mostly attracted to males, only attracted to males, or not sure.
Although the present study was focused on qualitative interviews and demographic information collected from participants, additional measures completed by participants included the School Reintegration Survey and the School and Community Mental Health Services Questionnaire (Marraccini et al., 2019; Marraccini, Vanderburg, et al., 2022; completed by school professionals), the Authoritative School Climate Survey (Konald & Cornell, 2015; completed by adolescents, parents, and school professionals), and the Self-Injurious Thoughts and Behaviors Interview (Nock et al., 2007; completed by adolescents).
In-Depth Interviews
Masters and doctoral-level interviewers completed a 2-day qualitative training addressing qualitative in-depth interview approaches, the interview protocol, and applied thematic analysis. The training was provided by a senior researcher with expertise in qualitative methods for applied health behaviors and other patient-oriented research. The senior researcher also provided ongoing consultation throughout the project.
The semi structured qualitative interview guide addressed four main areas: (a) school experiences prior to hospitalization, (b) school experiences and considerations during hospitalization, (c) school re-entry experiences and processes, and (d) information sharing between hospitals and schools. The interview guide allowed for adaptations and flexibility based on individual differences across interview and included sample questions to address each area. For example, a sample interview question particularly relevant to the present study aims that was included in the first section of the interview (school experiences prior to hospitalization) asked “How do you think your [or your adolescent’s] school may have influenced suicidal thoughts and behaviors?” (directed to adolescents and parents), and “How do you think school may influence students with suicidal thoughts and behaviors?” (directed to school and hospital professionals). Because each topic could be addressed in any order to follow the logical flow of the interview, and questions were informed by participant responses, specific questions addressed to individual participants varied according to individual interviews.
The majority (18 of 19) of one-on-one interviews with adolescent and parent participants were conducted in-person in private interview rooms located within a teaching laboratory and clinic. The final adolescent/parent interview was conducted virtually due to safety concerns during the pandemic. A total of four interviews conducted with school professionals were conducted in-person (e.g., at the participant’s workplace), with the remaining interviews with both school (n = 15) and hospital (n = 7) professionals conducted virtually.
Following completion of interviews, interviewers completed debrief summaries to provide a summary of the interview and monitor data saturation. Debrief summaries described tone and demeanor of the participant, a summary of responses for each segment of the interview, conceptual lessons learned, notes about the interview set up, interruptions or problems during the interview, and areas for follow-up or change. Interviews ranged in length from 33 to 120 min for all participants (M = 68). By cohort, interviews ranged from 42 to 90 min for adolescents (M = 64), 44 to 120 minutes for parents (M = 76), 33 to 101 minutes for school professionals (M = 65), and 45 to 94 minutes for hospital professionals (M = 63).
Data Analysis
Qualitative interviews were audio recorded, transcribed, reviewed for accuracy, and redacted of identifying information. Final interviews were entered into NVivo and Nvivo 12 Pro qualitative data analysis software (depending on the date of analysis), which is a qualitative software tool that helps organize and manage qualitative data into analytic themes (QSR International Pty Ltd, 2018, 2020).
We conducted applied thematic analysis on transcribed interviews. Applied thematic analysis is a systematic and inductive approach that draws from multiple theoretical foundations, such as basic inductive thematic analysis, grounded theory, and phenomenology (Guest et al., 2012). Although coding structures were developed separately for each cohort, we first developed the adolescent coding structure and used it as the basis for developing the coding structure for other cohorts. Initially based on the interview agenda, we iteratively refined and developed the adolescent coding structure to include emergent themes throughout the coding process, following a similar process for other cohorts. We prioritized the adolescent coding structure as a guide for other structures because they represent the population of focus. For the present study, we focused on an emergent code related to the study’s aim, which addresses perceptions of school experiences in relation to adolescent functioning. The first author further reduced the data to identify themes related to perceptions of school influences of mental health, discussing them with the second author throughout the process. Note that there are additional codes outside the scope of the present study (e.g., focused on school reintegration procedures) that have been summarized elsewhere (see Marraccini & Pittleman, 2022; Marraccini, Pittleman, et al., 2022) and are currently under analysis to address other research questions.
Trustworthiness
We enhanced trustworthiness in our data analysis by addressing issues related to credibility, transparency, and transferability. Interview procedures involved a form of member checking, wherein the researchers regularly summarized participant responses to confirm understanding. To ensure credibility, two trained researchers read transcripts and identified emergent codes separately, and then met regularly to come to agreement about the coding structure. An “audit trail” identifying changes to the coding structure was maintained to ensure transparency. A total of 53% (10 of 19) of adolescent transcripts were double coded (i.e., two independent researchers coded interviews separately), with assessment of internal reliability (percent agreement above .80) assessed during the final stages of coding. To prevent drift from occurring during independent coding of the final nine transcripts, wherein the researcher may begin to apply codes inconsistently over time, two of the nine transcripts were double coded. All other transcriptions (collected from parents, school professionals, and hospital professionals) were double coded to ensure credibility. In the case of disagreements, researchers engaged in discussions to come to consensus, documenting reasonings for agreement. To support transferability of findings, illustrative quotes were selected to represent common themes.
Researcher Positionality
We considered the background of each researcher, including privilege and underrepresented statuses conferred by our unique racial, ethnic, sexual, and gender identities, when interpreting study findings and included a diverse group of researchers to help manage the influence of our prior experiences and perspectives. The first author is the principal investigator of the study and has focused on research aimed at supporting adolescents with suicidal thoughts and behaviors in the context of school settings. Trained as a school psychologist and licensed as a psychologist, she is committed to identifying ways for schools to play a supportive role in recovery from suicide-related crises. Accordingly, the first author applied an ecological lens when engaged in this work, remaining open to the potential for schools to play a complex role in adolescent recovery (having both positive and negative influences on recovery).
The second, third, and fifth authors are doctoral level graduate students, each with experiences working in schools. Collectively, they have worked with a wide age range of both neurotypical and neurodiverse students from varied socioeconomic, racial, and cultural backgrounds across school-based and/or clinical settings. They also applied an ecological lens focused on societal, environmental, cultural, familial, and internal factors to both clinical conceptualizations and research.
Finally, the fourth and sixth authors are psychiatrists with fellowship training in child and adolescent psychiatry. They both work clinically with children and adolescents with suicidal thoughts and behaviors, in inpatient and outpatient settings. Additionally, the sixth author conducts independent research examining a task-shifting model of providing mental health care in schools in resource-limited areas. The fourth and sixth authors have applied a biopsychosocial lens to this work, taking into consideration biological underpinnings of mental health, psychological contributions to mental health, and social and environmental influences on mental health.
Results
Results are presented in three sections. First, we describe descriptive data identifying participant demographic characteristics. Second, we describe themes related to perceptions of how school experiences can positively or negatively relate to mental health. Third, an emergent theme related to the complexity of suicide-related risk and how school may intersect with other environmental, biological, and psychological risk and protective factors, is presented. Sections are organized according to subthemes and cohorts are described together.
Participant Characteristics
Demographic Characteristics
Demographic characteristics for the four participant cohorts, including gender, race, and ethnicity, are shown in Table 1. Only adolescent and parent participants were asked questions about sex and gender separately, of whom only adolescents identified a gender inconsistent with sex identified on their birth certificate. More specifically, most adolescents selected their gender to be girl or boy, aligning to the sex identified on their birth certificate and were considered cisgender (n = 16); two adolescents identified in some other way than boy, man, girl, or woman (n = 2); and one indicated they did not know if they were transgender (n = 1). Regarding race, adolescents were White (n = 11), Asian American and White (n = 4), Black or African American (n = 2), or other (n= 2). Four adolescents identified their ethnicity as Latinx or Hispanic.
Table 1.
Demographic Characteristics of Study Participants by Cohort
| Adolescents | Parents | School Professionals | Hospital Professionals | |
|---|---|---|---|---|
|
| ||||
| Gender† | ||||
| Girl, woman, or female | 14 (73.7) | 17 (89.5) | 15 (78.9) | 7 (100) |
| Boy, man, or male | 2 (11.8) | 2 (11.8) | 4 (21.1) | 0 |
| Something other than boy, man, girl, or woman | 2 (11.8) | |||
| Do not know if transgender | 1 (5.3) | |||
| Race | ||||
| American Indian/Alaska Native†† | 0 | 1 (5.3) | 0 | 0 |
| Asian American†† | 4 (21.0) | 1 (5.3) | 0 | 1 (14.3) |
| Black or African American | 2 (10.5) | 2 (10.5) | 2 (10.5) | 1 (14.3) |
| White | 11 (57.9) | 14 (73.7) | 15 (79.0) | 5 (71.4) |
| Other††† | 2 (10.5) | 1 (5.3) | 1 (5.3) | 0 |
| Ethnicity | ||||
| Latinx/Hispanic | 4 (21.0) | 2 (10.5) | 1 (5.3) | 1 (14.3) |
| Non-Latinx/Hispanic | 13 (79.0) | 17 (89.5) | 17 (89.5) | 6 (85.7) |
Note.
Response options for gender varied according to participant cohort
All adolescents and parents identifying as American Indian/Alaska Native or Asian American also identified as White
One adolescent selecting “other” self-described their race as “Latino” and the other adolescent did not describe their race; the parent identifying as “other” self-described their race as Brazilian; the school professional identifying as “other” did not have an option to self-describe their race. Numbers represent frequency with percent shown in parentheses. Total percent may be less than 100 in cases where participants chose not to answer.
Fifteen parents identified as women and four identified as men. Parents were White (n = 14), Black or African American (n = 2), American Indian/Alaska Native and White (n = 1), Asian American and White (n = 1), or other (n = 1). Two parents identified their ethnicity as Latinx or Hispanic. Fifteen school professionals identified as female and four identified as male. School professionals were White (n = 15), Black or African American (n = 2), or “other” (n = 1), with one identifying as Latinx or Hispanic. Finally, all hospital professionals were female (n = 7), identifying their race as White (n = 5), Asian American (n = 1), or Black or African American (n = 1). One hospital professional identified their ethnicity as Latinx or Hispanic.
Adolescent and Parent Characteristics
Only adolescents and parents were asked about sexual orientation and attraction. Of the adolescent participants answering the question (n = 18), seven adolescents (38.9%) identified as heterosexual or straight, two (11.1%) identified as gay or lesbian, and nine (50.0%) identified as bisexual. When asked about sexual attraction to other people, only four adolescents (21.0%) indicated they were only attracted to the other sex. The remaining adolescents indicated they were mostly attracted to the other or same sex (n = 12, 63.2%), equally attracted to females and males (n = 1, 5.3%), or not sure about their attraction (n = 1, 5.3%). Most parents (n = 18, 95%) identified as heterosexual, and one parent (5%) identified as bisexual. Most also indicated they were only attracted to the other sex (n = 15, 83%), whereas two (10.5%) indicated they were mostly attracted to the other sex and one (5.3%) indicated they were equally attracted to females and males. Taking both gender and sexuality in account, 14 adolescents (70%) and one parent (5%) identified in a way that can be considered under the umbrella identity of LGBTQ+.
All adolescents attended public school and 26% of parents (n = 5) reported that their child received special education or remedial services in school. Adolescents described receiving “Mostly A’s” (n = 5, 26%), “Mostly A’s and B’s” (n = 8, 42%), “Mostly B’s” (n = 1, 5%), “Mostly B’s and C’s” (n = 2, 11%) and “Mostly C’s” (n = 3, 16%). Annual household income was reported by 16 parent participants, ranging from $0 to $500,000 (M = $115,703; Mdn = $105,500).
Perceptions of Positive and Negative School Experiences
Figure 1 displays common themes related to participant views of how school experiences may positively or negatively relate to psychological functioning in adolescents with suicidal thoughts and behaviors. Themes included (1) participation in school activities, (2) school social experiences, and (3) school interventions. For each theme, we first present descriptions of how school experiences may positively relate to mental health and next present descriptions of how school experiences may negatively relate to mental health. Illustrative quotes are presented to enhance understanding of each theme and are displayed in Supplementary Tables 1–3.
Figure 1.
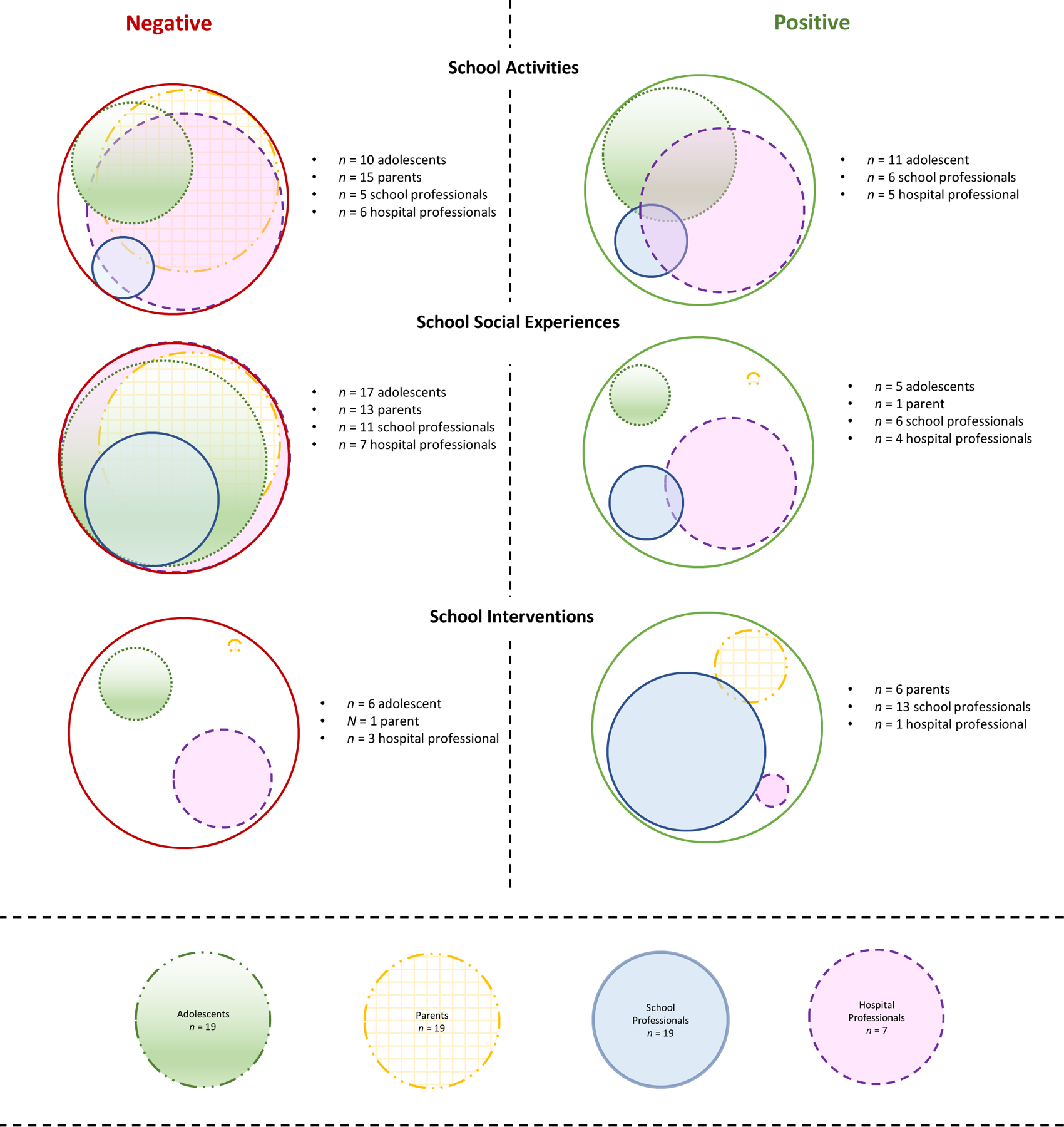
School Experiences Perceived to Negatively and Positively Influence Mental Health
Note. Size of circle indicates proportion of participants within cohort describing an experience or perspective that aligns with each theme.
School Activities
Positive Perceptions: Engagement and Distraction.
Eleven adolescents (58%), six school professionals (32%), and five hospital professionals (71%) described how engagement in school experiences (e.g., academics, extracurricular activities) and the consistent routine and structure provided by school can serve as a form of coping, connection, or distraction for adolescents. School professionals indicated the significance of school as a safe place that can also serve as an escape from difficult home experiences, and individuals across cohorts described how they believed engagement in school activities can have a positive influence on adolescent health. A school counselor provided an example of one student who, despite having a difficult home life, made school “her safe place” by engaging in Future Farmers of America activities “where she feels important and a leader.”
Adolescents (n = 9, 47%) also identified the potential for school to serve as a form of distraction from other pain and stressors. For example, this 17-year-old girl explained how school helped served as a form of distraction: “Distraction. Just like, ‘Okay. I’m not gonna be in the house being depressed and doing stupid sh*t all day. Great.’” Another 16-year-old girl explained the push and pull they felt from feeling stressed in school while also benefiting from it as a distraction:
Cause I was like, oh my gosh, I’m missing school. Why am I missing school, like. Oh, it was, like, just—sometimes I had to break myself out of it. You have scars all over your arm. Like, you need to not think about school. But then, I don’t know. It was also good, though, for a distraction sometimes to just make me, like—I’d tell myself, like, no I need to do this homework cause I need to, like, think about something in the future. Like, I’m gonna turn this assignment in. Like, have that.
For some adolescents, distraction was the only aspect of school they felt had a positive effect on them.
Negative Perceptions: Academic and Performance Pressure.
Perceptions of how academic pressure, as well as pressure to perform well in other areas, may have a negative influence on mental health emerged as a common theme across cohorts (adolescents, n = 10 [53%]; parents, n = 15 [79%]; school professionals, n = 5 [26%]; hospital professionals, n = 6 [86%]). Several participants (two adolescents [10%], two parents [10%], and two hospital professionals [29%]) described how the combination of academic pressure and being a “perfectionist” or high achiever can be particularly challenging. For example, this 16-year-old girl explained:
…I was putting the pressure on myself that I had to do every assignment perfectly, get perfect grades, um, everything like that. And, of course, there’s benefits to being a perfectionist in school because it drives me to do well but—um, it really took a toll on my mental health. And I think that it was kind of that attitude about the [advanced] program that was hard because it was kind of like you go, go, go. There’s no slack. Like, everyone, the teachers-it’s not just solely the teachers, but the students as well. Like, it’s kinda the environment, that everyone puts the school before their mental health.
A related issue, in which adolescents may compare their performance to their peers, was described by three parents. A father explained how attending a school with high-performing students may have influenced their adolescent’s mental health:
I think generalized anxiety about performance. There’s all the usual cultural sh*t of body image and the whole Snapchat, Instagram culture of comparing yourself to—and she’s going to a school with a lot of really high-performing, amazing people. If you’re feeling like your life’s not going well, that can really wear you down.
Others (two adolescents) described how academic pressure can exacerbate additional risk factors for them, for example not getting enough sleep or spending too little time with friends. One 16-year-old adolescent girl simply described how academic stress minimized their fear of death: “Well, I guess what I’m trying to say is like, school, because of the stress load from school, it made, like, thinking of suicide not as scary of a thing.”
Pressure to succeed was not limited to academics; for example, one adolescent noted the pressure they faced in sports. Indeed, a hospital professional described how for some adolescents, doing less in school may be one of the solutions for recovery:
I think each kid probably is different. I think sometimes things that have been helpful have been really specific things…some of that could be like, “Okay, you’re in ROTC [Junior Reserve Office Training Corps program], and you play on the soccer team, and you do this, and you do that. Which of those roles do you—you’re telling me that you don’t have enough time. Which of those roles are most fulfilling to you? What benefits are you getting from those activities? How can we make sure you’re still getting those benefits but you still have enough time to care of yourself?”
Finally, when describing how schools may influence suicidal thoughts and behaviors, a school psychologist described how school-related pressures may intersect with student backgrounds, including economic privilege, to influence mental health and suicide-related risk. They described how patterns of school factors contributing to mental health may differ across demographic groups, with college and advanced coursework pressure more salient to some, but economic constraints more salient to others:
I think it really is across all of our demographic groups. I see some differences. I see that the kids that are taking those AP classes and they really are pushed to college and stuff, it’s more the anxiety, it’s more the stress and the anxiety. Some of our other kids, our Hispanic kids, there’s been a fear of, “Have you been coming to school over recent years?” Then when you start getting on them about attendance because they’re trying to work a job on top of coming to school, you see them dropping out in this homeroom.
School Social Experiences
Positive Perceptions: School Relationships.
Positive in-school relationships with adults and peers were described as supporting adolescent mental health by a handful of adolescents (n = 5 [26%]), school professionals (n = 6 [32%]), and hospital professionals (n = 4 [57%]), as well as one parent (5%). Positive in-school adult relationships were especially emphasized by school professionals. A school psychologist described how teachers shared information about students of concern simply to provide emotional support to them:
They were aware of some really significant depression, anxiety, and internalizing concerns. They had just talked about how they tracked the student on their own. From semester to semester, they made sure they talked about this student and her background to the next set of teachers. Said, “Keep an eye out, and check in with this student a little bit more. Talk to her and see what she needs.”
A more general sense of connectedness to school was also expressed by hospital professionals. This hospital school professional explained:
I’ve been happily surprised to hear that it seems like most students feel like there is someone in the school that they can talk to. It can be different people, but I do feel like overall, maybe 80 % or something of the students that I actually ask—I don’t always ask that to every kid. If I do happen to ask them, they feel like there is someone that they can identify as someone that they’re comfortable talking to at their school.
Adolescents also expressed gratitude for adult relationships, as this 14-year-old girl described:
But my SRO [school resource officer], you know, like, if I looked sad or mad or something like that, you know, she always knew what it was. And she would always, you know, like, talk to me, like take me up to her office. You know, she’d make me laugh somehow. And so did my counselor. So during that time, you know, I felt safe going to school, you know? I felt good, you know? I was like, “You know, even though this is happening, you know, I still got these people to talk to.”
In addition to adult relationships, a few adolescents reported that they appreciated having school as a place they could connect with peers. A 15-year-old girl expressed the positives of school this way: “It was the only way I could really see my friends.”
Negative Perceptions: Difficult Social Interactions.
Difficult social interactions were identified as a perceived stressor for adolescents with suicide-related risk by most adolescents (n = 17 [90%]), parents (n = 15 [79%]), school professionals (n = 11 [58%]), and hospital professionals (n = 7 [100%]). Because of the breadth of this theme, we present findings related to difficult social interactions in separate categories that include (a) challenging peer relationships or feelings of social isolation, (b) concerns about large numbers of students in school, (c) bullying and harassment experiences, and (d) difficult school adult-student relationships. As noted by this 15-year-old girl, however, social difficulties across these categories can overlap to make students feel isolated:
I think that being in school, it made me feel more isolated. That really intensified my suicidal thoughts where I was like, nobody likes you. You’re weird. You’re awkward. That made things harder. How little teachers seemed to care about you. It’d be like, this is their job, is to help develop students and care for them. The teachers that I had that actually did that made me realize how little they—you know what I’m sayin’? I don’t know how to describe it.
Challenges with Peers.
Ongoing challenges with peers in school were identified by several participants across all cohorts (8 [42%] adolescents, 9 [47%] parents, 6 [32%] school professionals, and 4 [57%] hospital professionals). Participants described experiences of social isolation and peer comparisons (e.g., academics, financial), leading to feelings of inadequacy. A special education teacher stated “That kid who is perpetually, always 100% alone, who is shunned when he or she tries to join in so they don’t even bother anymore, that’s a huge problem.” The special education teacher explained how for some kids, not feeling like they fit into the group leads to feelings of alienation, and for others, issues related to hygiene (because “they don’t want to take a shower” or their “moms had another boyfriend over last night, and [they’re] afraid to go in the bathroom”) can lead to other students not wanting to be around them.
One adolescent-mother dyad noted the feeling of disconnect among members of the school. For example, the mother described the psychosocial “culture” or climate of school as uncaring compared to that of their home:
Her struggles were in the school level. Her struggles were the overwhelming amount of children, older children, girls that she couldn’t relate to, the culture. She came from one culture that was safe, open, holistic, caring, everybody knew everybody’s name, blah, blah, blah to a culture of nobody cares about you at all.
Another parent and adolescent (dyad) each described the exhaustion the adolescent felt from having to pretend that everything was okay with friends and teachers, when it really was not.
Still, one hospital school professional explained that when school is described as a stressor or trigger in a patient’s chart (which they review to identify interests and dislikes related to school to better engage them as a learner), it was rarely because of “peer relationships,” but more often because “they’re not doing well in school, and that causes a lot of stress.” As noted by a hospital recreational therapist, the significance of social (and all) stressors varies across patients.
School professionals also identified the intersection of peer difficulties with social media. A school counselor explained:
Kids and adults, for that matter, society and special social media has created this image of what we should be like. When kids are coming to school, and they’re comparing themselves against other people, a lotta times we think somebody else has it all together when they really don’t. I think just comparing, and why can’t I be as smart as her? Why can’t I be as pretty as her? Why can’t I drive a car like she does? I think that creates in their mind what their life is supposed to be like and where they are versus where they think they should be. I think coming to school makes that more prominent in their mind of the differences.
In addition, two school professionals and one parent noted how careful they had to be to contain social contagion, where kids may reinforce each other’s negative coping responses.
Large Numbers of Students.
Five adolescents (26%), five parents (26%), four school professionals (21%), and two hospital professionals (29%) also described how being with a large group of people (e.g., in classrooms, in crowded hallways) was something that could be challenging more generally and difficult to avoid in school. Put simply by this adolescent, “…there’s a lot of people, and I get really anxious when there’s a lot of people.” A mother described it in more detail:
But it’s very overwhelming. It’s just too crowded. It is massive people there, and just… to changing classes, it’s very anxiety-inducing for her. I mean, school is, but she has to go. It’s her biggest trigger is her high school. That’s it. It sums it up right there.
In some cases, these stressors appeared to overlap with student perceptions of the school’s psychosocial support. For example, this 16-year-old girl described it this way:
Anxiety was really bad at [my school] because when that bell rings, your anxiety is like whoo ‘cause you have to run out the class. There’s a horde of people who just push you on—if you stop, they’ll push you to the ground. … Nobody stops when they see that. You just kind of feel like, oh, thanks. I guess I’m just a piece of garbage. They don’t even give you a second glance. They don’t care.
Bullying and Harassment.
Victimization and bystander experiences to incidents of bullying, rumors, and harassment were described by six adolescents (32%), five parents (26%), four school professionals (21%), and six hospital professionals (86%). This 14-year-old girl explained how they felt bullying experiences and rumors contributed to their suicidal thoughts and behaviors:
The bullying was not too bad, but it was bad enough to kind of make me very, very just tired of life and just—I just didn’t want to be here anymore ‘cause I just—I was just so tired of the BS and all the lies and stuff like that. …I think maybe it was a little bit of a contributor to what happened, but I don’t think it was necessarily a big reason.
A 15-year-old girl described how sexual comments in school could be upsetting: “Cause I’ll be havin’ a good day, and I’ll hear something disgusting and gross about somebody else’s—what somebody else would like to violate about someone else’s body.” Still another described the challenge they faced in seeing their perpetrator at school.
A hospital professional described how mental health issues such as “low self-esteem, not liking themselves, social anxiety, rumination, all those sorts of things” can be “wrapped up in” bullying. Note, however, that one hospital professional and one school professional explained that bullying may be relevant in some cases, but that it is not talked about by patients at a frequency that matches how media portrays the issue. Another hospital professional described that although patients may describe their experience as bullying, oftentimes, it may be more aligned to feelings of social isolation:
I would say also the other thing that came to mind is that sometimes, we do have kids who say they’re bullied, but when we ask more, it sounds like what they describe does not involve bullying behavior. It’s more of loneliness at school and then feeling isolated and describing that as being bullied, when in reality, it’s really more poor social skills, lack of peer relationships, which is sad. It’s just not the same as what we call bullying.
Relationships with School Adults.
Finally, tension experienced in relation to negative adult relationships or simply having too few adult relationships was described by seven adolescents (37%), three parents (16%), and four school professionals (21%) as a stressor. Adolescents identified specific teachers they found to be “triggering”, with several explaining that they felt unwelcome by counselors when seeking help. A 17-year-old girl described reaching out to counselors for help and being told “All right. Cool. Go to class.”
Parents also described the difficulties their adolescents faced from negative interactions with teachers and school professionals, with one describing an incident of their adolescent being picked on by a teacher. Although school professionals largely described positive student-adult relationships (detailed in the previous section), some also noted the difficulties students faced when they lacked close connections to school adults. A school psychologist explained, “I think that not having those relationships and not taking the time to form those relationships with kids is detrimental.” Another school psychologist noted how the shift from having school connections while in high school, to being disconnected following high school graduation, can exacerbate isolation, with a specific example of a student dying of suicide after graduation.
School Interventions
Positive Perceptions: School-Based Mental Health
Thirteen school professionals (68%), six parents (32%), one adolescent (5%), and one hospital professional (14%) identified the potential for school-based mental health supports to help adolescents with suicide-related risk. Participants described a variety of school-based mental health supports and services, such as monitoring of suicide-related risk, access to resources, and connection to care. As a school social worker explained:
There’s been a tremendous focus on trauma-informed schools these last 2 years. I think your staff are more in tune with some of the things that are maybe going on with students. Many things that maybe didn’t come to light before are now. That, I’m positive, has an impact. I can’t tell you empirically what that impact is, but I can tell you that we’ve definitely seen an increase.
School professionals emphasized how schools may be well equipped to monitor the safety of these high-risk adolescents, as did this hospital professional, explaining: “Teachers or school staff are a lot more apt to notice something that’s going on with them potentially.” A few school professionals also noted that they felt that their schools could continue to improve screening efforts and ways of reinforcing coping skills. For example, a school psychologist described that although they’ve “done well educating students about the mental health services available at the school,” they could do better at “addressing topics proactively rather than reacting when things come up.”
Negative Perceptions: Minimal Supports for Mental Health.
Six adolescents (32%), one school professional (5%), and three hospital professionals (43%) indicated concerns about minimal support for mental health interventions in schools or the limitations of school rules to allow for flexibility in supporting students with mental health concerns. A 17-year-old girl explained:
I think that our school definitely does not take mental health seriously. If I had cancer, they would be like, “Oh, what can I do to help since you’re getting treatment today,” or “you’re sick because you’re just sore and tired, so it’s fine for you to take a day off. We’ll help you make up your work.” Then, if it’s “I couldn’t sleep last night because I was having a panic attack or I’ve been having consistent panic attacks and, mentally, I cannot handle today. I need a day,” then they’d be like, “Just skippin’. You’re just lazy.”
A 16-year-old girl described how when they sought counseling during a panic attack, they called their dad to take them home because “there was no support” as they were only told “to sit here for 5 minutes and go back to class.”
Finally, three participants (one adolescent, one hospital professional, and one school professional) described how the rigidity of school rules can interfere with mental health supports. A school counselor described how although a student with suicide-related risk was previously engaged in several extracurricular programs, when she began to face problems due to absences related to her mental health, the teachers did not allow the student to continue with those supports. A hospital professional further emphasized this point, identifying “the inflexibility of what happens for kids who are slow to wake up or who have a lot of difficulty socially” as difficult to modify.
Intersecting Bio-Psycho-Social Influences with School and Psychological Functioning
A notable theme across cohorts was the recognition that risk and resilience for adolescents with suicidal thoughts and behaviors is complex and driven by multiple, intersecting factors. School experiences were often considered a secondary influencer of health and well-being, and sometimes described as transacting with other risk factors (i.e., other problems led to school problems, which together lead to worse outcomes). These observations are evident within each of the previous themes, for example, how bullying has been portrayed in the media, but is rarely the sole driver of suicide.
For parents and adolescents, descriptions often related to the interaction of personality characteristics (e.g., perfectionism) and academic pressure, as well as the role of medications, substance use, and underlying psychopathology conferring risk for suicide. After describing how their son was “sneakily smoking pot on campus every single night,” this mother explained how drugs, learning differences, and peer comparisons converged in a problematic way for her son:
It’s not about the school, but the chemicals in his brain while he was trying to survive at this incredibly rigorous school. He’s used to being one of the smartest people in the room, but he never feels that smart because, again, when you take longer to answer a question, you feel like you might not be as smart as the person who answered it quickly even though you might do a better job of answering it. I think he thinks he’s really smart and thinks he’s stupid, and there’s a lot of things with him where he’s here and there at the same time, and that’s almost more painful than just thinking, “Oh, I’m okay.” Being in that, it’s like, “Am I dumbest person here? Am I the—,” I think it made him question himself even more.
For school professionals, some of these observations hinged around how the home environment and economic diversity played a role in student risk, obstructing access to care and making school-based supports and services more essential. For example, a special education teacher explained how remote learning was important for students while they were isolating during the pandemic, “especially the ones whose home life sucks because… even though they can’t get outta there, at least it’s a mental distancing for a few minutes.” When describing how the structure of school can be helpful for students, a school counselor reflected on their own experiences to point to its significance for those with less resources:
Definitely better is the structure. I think that for so long, I grew up in a very stable, safe house. I had both my parents. They were both employed. We didn’t deal with a whole lotta financial hardships. I’m speaking of me, of my own life. I think that has been the hardest thing. I’ve worked with kindergarten through 12th grade, and I think kids feel stuck in where they are. Unfortunately, so often, and good gracious, just research shows this. The cycle continues. Poverty is a cycle.
Hospital professionals perhaps emphasized this theme the most, considering their role in conceptualizing adolescent functioning and care. For example, one stated:
I would say every kid’s probably struggling with school on some level for the most part. It doesn’t mean it’s like—it seems like it contributes in some way. For other kids, it’s more, there’s a really difficult home situation or, in my mind, when you think of that psychopathology, there’s a difference between pure biological psychopathology and then biological that’s been really, really induced by the environment. Then there’s a subset of kids in the former where everything’s mostly, actually, fine. They just have true biological MDD [Major Depressive Disorder]. That’s what it is. School might be stressful, but, really, it’s a very clear pattern…It’s either impacted and/or a secondary exacerbator where things aren’t going well. Then they have to deal with school.
Discussion
Although previous research has demonstrated the significance of school-related experiences for enhancing protective factors (e.g., connectedness) and mitigating risk factors (e.g., bullying) of suicide, few studies have addressed these factors in clinical samples or explored the lived experiences of individuals representative of multiple roles. To address this gap, this qualitative study explored adolescent, parent, school professional, and hospital professional perceptions of how school may relate to adolescents’ suicidal thoughts, behaviors, and mental health. Participants included a diverse sample of adolescents, with 47% representing a racial or ethnic minoritized group and 70% identifying their gender or sexuality in a way that can considered under the umbrella identity of LGBTQ+. Accordingly, special consideration is given to how school psychologists can engage in culturally grounded practices and affirm the sexual and gender identity of youth to enhance their safety and psychological wellbeing in the context of suicide risk (Schultz et al., 2021).
Findings illustrate how school experiences may transact with other risk and protective factors of suicide to impact adolescent mental health. The nature of these influences not only appears to vary across individuals, but also across home and school communities. In the following sections we expand on the themes emerging from adolescent, parent, school professional, and hospital professional perceptions of positive and negative school influences of mental health (i.e., school activities, school social experiences, and school interventions), integrating consideration of the cross-cutting theme pertaining to how intersecting bio-psycho-social factors may contribute to risk. Findings inform how school psychologists can partner with families and other professionals to enhance supports for students with suicidal thoughts and behaviors in school settings, tailoring interventions to the unique needs of each student.
School Activities
Adolescents, school professionals, and hospital professionals, but not parents, noted some of the ways in which participation in school activities, including extracurriculars and school more generally, may help students struggling with suicidal thoughts and behaviors. Participants across cohorts also identified the negative effects of overinvolvement in activities, especially in the context of a culture that reinforces high-performance expectations. Accordingly, supportive practices that foster positive school engagement in youth with suicide-related risk may look different based on the unique needs of each student. Although some students may benefit from supports that increase their school involvement, others may benefit from a change in the type of activities they are involved in or interventions that help mitigate internalized messages of pressures to be perfect.
Enhancing Student Engagement
Although adolescents primarily described the ways that schools can distract them from their other problems or their own internal pain, school and hospital professionals described how students may become more connected and feel more supported when engaged in school. Indeed, positive emotions in school have been found to associate with behavioral engagement (i.e., involvement in learning and participation in school-related activities; Fredricks et al., 2019) through the use of effective coping skills (Reschly et al., 2008). Thus, school engagement may also help to promote positive affect.
In their review of evidence-based interventions addressing student engagement, Archambault and colleagues (2019) provided an extensive list of interventions across a multitiered system of support (MTSS). Although few of these identified interventions focus exclusively on intensive (tier 3) interventions targeting behavioral engagement for at-risk adolescents, Check and Connect (Evelo, 1996) has perhaps the most research support. Findings from several studies have demonstrated Check and Connect as effective for supporting student engagement across multiple contexts (Archambault et al., 2019; Heppen et al., 2018) and it is recommended as an intervention to specifically address suicide-related risk (Miller, 2021).
Most interventions addressing student engagement (including Check and Connect) tend to integrate family partnerships for increasing school participation in students (Archembault et al., 2019), with research supporting a link between family involvement in school and student engagement (Simons-Morton & Crump, 2003). The present study’s findings that no parent participants identified school activities or school engagement as a potential positive school experience for their adolescent provides additional credibility to the importance of connecting with families to engage students with suicide-related risk. Thus, as school psychologists work to enhance school engagement among adolescents facing suicide-related risk, an important first step involves partnering with student families.
Professionals in both hospitals and schools acknowledged the strengths of supports provided in each setting. School psychologists and outside clinicians can facilitate home-school partnerships by engaging outside providers and other school professionals in a collaborative problem-solving process, each reinforcing the importance of working with the other entity to support the adolescent’s recovery. Outside clinicians may be particularly helpful in reinforcing the importance of making connections or engaging in school, or for alerting the family and school when adolescents may be over- (as opposed to under) engaged in activities and need to scale back their involvement. Note that such partnerships require adherence to both the Family Educational Rights and Privacy Act and the Health Insurance Portability and Accountability Act, with information only shared between sites when families have granted authorization.
Because interventions and research addressing family involvement in schools have predominantly relied on hegemonic notions of what family involvement means (e.g., checking homework, attending school events, participating in the parent-teacher association), partnering with families to enhance school engagement must also address diversity in culture, language, socioeconomic status, employment, and technology literacy (Watson & Bagotch, 2015) and involve shared decision-making between schools and families (Lazarus et al., 2021). Drawing from DisCrit, Matute-Chavarria (2021) outlined a model for engaging families by holding an aspirational meeting with parents of youth with disabilities. By facilitating a critical dialogue with families that centers family values and focuses on the family’s aspirations for their child, the school and family can partner to enact a visionary plan that addresses strategies and supports consistent across school and home. School psychologists can integrate such approaches into interventions aimed at enhancing school engagement and further support family involvement by offering flexible meeting times (e.g., during unconventional work hours such as late evenings and on weekends) and ensuring that school events for families and students are culturally inclusive (Watson & Bagotch, 2015).
It is also important to note that although the majority (70%) of adolescent participants identified their sexual or gender identity in a way that could be considered under the umbrella of LGBTQ+, none described a Gender and Sexuality Alliance (GSA) in their school. It is unclear if adolescents did not have access to such supports or simply did not identify them as influential. Nonetheless, the potential for GSAs to build from the strengths of LGBTQ+ students and serve as a safe and inclusive place (Poteat et al., 2020) makes it an important consideration for school psychologists working to support student engagement. GSAs have been shown to help mitigate bullying victimization (Marx & Kettrey, 2016) and when combined with a positive school climate that integrates inclusive approaches such as health curricula relevant to LGBTQ+ youth, they may also play a protective role against suicide-related risk among LGBTQ+ students (Hatzenbuehler et al., 2014; Marraccini, Ingram et al., 2022). Such inclusive approaches are particularly important to consider for increasing school engagement in adolescents with suicide-related risk, given that as compared to youth identifying as cisgender and heterosexual, LGBTQ+ youth are at increased risk of having suicidal thoughts or attempting suicide (Johns et al., 2020) and are overrepresented among adolescents who receive treatment for suicidal ideation, attempts, and other forms of self-harm (Berona et al., 2020).
Mitigating Performance Pressure
Although increased engagement in school may be especially important for youth struggling with school attendance and school avoidance, school psychologists must also attend to the ways in which a culture that pressures adolescents to succeed – in academics and beyond – can exacerbate mental health problems (Gulbas & Zayas, 2015; Gulbas et al., 2015; Keyvanara et al., 2011; Shilubane et al., 2014). Adolescents, parents, school professionals, and hospital professionals emphasized how high academic expectations set by schools and families may be particularly problematic for adolescents already internalizing a need to be perfect. Perfectionism is associated with commonly identified disorders (e.g., depression, anxiety; Hewitt et al., 2002) among individuals with suicide-related risk (Goldston et al., 2008) and is identified as a core feature of other comorbid disorders, such as obsessive-compulsive disorder (Halmi et al., 2005) and eating disorders (Lloyd et al., 2014). Adolescents identified both the strengths (e.g., high rates of success) and limitations (e.g., feeling like they cannot stop) of their need to be perfect.
Participants also described this pressure as difficult for adolescents struggling with suicidal thoughts and behaviors more generally. Although the use of cognitive behavioral strategies to address perfectionism may be clinically merited for some adolescents (Flett & Hewitt, 2008) in school, these findings intimate the need for motivational approaches that balance high performance expectations with emotional well-being. Schools have begun to embrace strategies that prioritize reinforcement of effort and growth instead of fixed measures of achievement (i.e., growth mindset; Yeager et al., 2019), demonstrating preliminary support for improvements in both academic outcomes and well-being (Zeng et al., 2016). For high-achievement oriented youth struggling with suicidal thoughts and behaviors whose key issues relate to internalized pressure for academic success, school-based interventions that integrate growth mindset approaches could complement evidenced-based clinical interventions (e.g., cognitive behavioral therapy, dialectical behavioral therapy) to support recovery. Moreover, adoption of such approaches may preempt the development of internalized pressure for academic success from occurring to begin with.
Additional considerations are warranted for high-achieving ethnic and racial minoritized students and high-achieving economically-disadvantaged students. Pressure for educational attainment may also be driven by economic instability and other systemic factors, so interventions that only target internal processes (such as growth mindset and other skills commonly addressed in social and emotional learning curriculums) may do more harm than good. Indeed, previous work has indicated that academic success can be viewed by ethnic and racial minoritized families as a mechanism for overcoming the obstructions of racism (Suizzo et al., 2008). Without acknowledging and addressing the socio-cultural conditions that obstruct academic opportunities – systemic oppression and discrimination – these approaches can reinforce the myth that economically disadvantaged and ethnic and racial minoritized students should be able to “pull themselves up by their bootstraps, despite being in an environment that is designed to knock them down” (Marraccini, Lindsey, et al., 2022, p. 3). Note, however, that the systemic obstructions to academic success vary from person to person, so school psychologists must be careful not to make assumptions about the specific discriminatory and economic barriers of students based on their racial and ethnic identify or socio-economic status.
Culturally inclusive approaches for supporting youth social and emotional development prioritize an understanding of critical consciousness. Critical consciousness involves critical analysis of the social conditions that economically disadvantaged, ethnic and racial minoritized, and other disadvantaged students face, empowering students to affect change towards social justice (Watts et al., 2011). In schools, transformative social emotional learning (TSEL) has gained attention for its potential to facilitate supportive and lasting relationships between and across students and school adults that are built from a collective understanding of and action towards critical consciousness (Jagers et al., 2019). TSEL, which prioritizes both adult and student learning, may be particularly well suited for addressing the concerns raised by the present study’s participants considering both adolescents and adults voiced concerns about a “climate” of overachievement, indicating a need to intervene at the school level. As researchers have only begun to explore the effectiveness of TSEL for supporting the social and emotional development of students, future research addressing how schools can enhance clinical care and integrate the tenets of critical consciousness into existing and new supports such as TSEL is merited. In the meantime, school psychologists can draw from TSEL approaches to center critical consciousness when supporting students identifying school and family pressure as a stressor for their mental health.
In summary, school activities emerged as a prominent theme for understanding school-related risk and protective factors of suicide. There is a need to balance efforts for enhancing student engagement in school while attending to the potential for academic and performance pressure to worsen student mental health. Findings underscore the significance of school approaches that cultivate culturally inclusive practices and prioritize student wellbeing.
School Social Experiences
Participants described how social stressors in school can be challenging for youth struggling with varying degrees of social anxiety, and for those with a history of trauma or victimization. Yet, the extent to which social difficulties, such as peer rejection and bullying, can be distinguished from symptoms of depression and other internalizing disorders, such as feelings of isolation and disconnect, is unclear. Although bullying was certainly emphasized as a stressor by multiple participants, in some cases adolescent and parent descriptions of bullying victimization experiences may better reflect deficits in social skills or underlying feelings of disconnect. These findings align with concerns about the way bullying can be presented as a cause (as opposed to a contributor) to suicide in the media (Assistant Secretary for Public Affairs, 2020), reinforcing bullying as one of many possible contributors to suicide-related risk.
As interpersonal stressors increase during adolescence, those with limited biological resources to manage such social stress may be especially vulnerable for a suicide-related crisis (Miller & Prinstein, 2019). Thus, in addition to school-wide bullying prevention initiatives (Gaffney et al., 2021; Holt et al., 2020), adolescents struggling with suicidal thoughts and behaviors may benefit from interventions addressing social skill learning, as well as some of the in-school activities facilitating connections to peers, activities, teachers, and other adults in school we previously described (e.g., Check and Connect, GSAs, structured extracurricular activities; Miller, 2021). Although these activities may be beneficial for some, other students described the exhaustion they felt from feeling sad or depressed while interacting with “typical” peers, underscoring the need to tailor interventions for individual students. Research addressing peer-based mentoring (i.e., providing support by peers who have faced similar crises and recovered) is worthy of exploration; however, school psychologists should remain cautious to such approaches considering the potential for social contagion among social networks involving peers with depression and suicide-related risk (Singer et al., 2019).
Other social stressors appeared to overlap with internal and external pressure for adolescents to succeed, achieve, and fit in. Participants across cohorts identified peer comparisons (e.g., to grades, clothing, sports) as a challenge in school, with multiple sociocultural conditions at play (e.g., socioeconomic and cultural diversity impacting availability and access to resources and opportunities). Several participants emphasized the stress caused by the large number of students who adolescents may face within classrooms and hallways, especially for students struggling more generally with social anxiety or phobias. These challenging peer interactions were identified as occurring within the physical space of the school and extending into school by way of social media exchanges. Although infrequently mentioned by adolescents or parents, school professionals identified the social challenges wrought by social media platforms, showcasing the overlap of virtual and in-school social experiences.
Notably, relationships with adults in school were identified as helpful in some instances and problematic in others. Difficulties between students and adults involved performance pressure, as well as prioritization of procedural supports above emotional ones (e.g., counselors adhering to re-entry plans by holding brief check-ins with students and prioritizing sending them back to class). This finding speaks to the tension within the work of student support professionals, which involves prioritizing student access to the academic curriculum but also supporting their emotional needs as students face interpersonal stressors in and out of school. School professionals can prioritize small actions during student interactions, having conversations that are sensitive to student mental health needs and that are gender affirming, for example, by respecting student gender identity pronouns (Schultz et al., 2021).
Collectively, findings related to perceptions of social experiences and suicide-related risk point to the significance of schools as a social microcosm for adolescents and the need for school professionals to support students as they navigate an increasingly complex social environment.
School Interventions
Although schools have been increasingly relied upon to provide mental health care to children and adolescents (Costello et al., 2014), and school-based supports addressing suicide prevention have been identified as a need by adolescents and care providers (Coggan et al., 1997; Schwartz et al., 2010; Shilubane et al., 2014), school-based mental health supports for youth with suicide-related risk were only minimally identified by adolescents, parents, and hospital professionals. Although most school professionals described the significance of these services and programs for supporting adolescent mental health, several adolescents and parents indicated that the school provided limited access to quality mental health supports and services. This discrepancy may reflect an emphasis on universal prevention programs and skill-based interventions delivered in schools (Singer et al., 2019), with more intensive psychological treatments for youth with severe mental health difficulties typically provided by outside clinicians. Yet, this discrepancy may also speak to the barriers faced by adolescents seeking mental health care in school reported by previous researchers (Kodish et al., 2020 Radez et al., 2021; White & Morris, 2010).
A growing body of work has identified promising interventions for addressing mental health symptoms commonly associated with suicide (e.g., depression, anxiety, conduct disorders) that can be implemented by school psychologists and other school support staff across all tiers of MTSS (from universal to intensive; Arora et al., 2019; Miller, 2021). To date, however, limited research has addressed school-based interventions for youth with suicidal thoughts and behaviors at the tertiary level, and instead, is primarily focused on universal suicide prevention programs (Singer et al., 2019). In addition to the need for investments in school-based mental health supports and services that address serious emotional concerns (Arora et al., 2019), this finding indicates a need to consider collaborative efforts between school and community providers that tailor services in schools to reinforce outside interventions for youth struggling with suicide-related risk (Radez et al., 2021). Moreover, school based mental health services, involving dedicated school staff who can provide mental health services, as well as wrap around services involving community partnerships, have been called for to address barriers to access to care (Arora et al., 2019; Duong et al., 2021). Several promising psychotherapy practices for treating suicidal ideation in clinical settings (e.g., dialectical behavioral therapy, cognitive behavioral therapy; King et al., 2018) could be integrated into these school services (Martinez et al., 2021; Mazza et al., 2016; Miller, 2021; Singer et al., 2019). As experts in school-based interventions, mental health, and consultation, school psychologists are well positioned to help liaison between community and school supports for these high-risk youth.
Beyond the formal interventions addressed within comprehensive suicide prevention programs, adolescents expressed concerns about ongoing supports provided by counselors and other school support professionals when they experienced emotional distress in school. Thus, there is also a need for brief treatment approaches that fit within the workflow of school student support professionals to support adolescents throughout their day, beyond simply allowing students to take a short break from class before returning to school. School psychologists may consider integrating mobile Health (mHealth) tools designed to teach adolescents skills, such as affect regulation or mindfulness, into their practice and preparing to reinforce aspects of their treatment provided in the community within the school day. Preliminary research supports the feasibility and acceptability of these tools for use with adolescents in schools (Newton et al., 2020; Puhy et al., 2021); however, at present, there is limited research addressing the efficacy of these tools for increasing skill utilization and leading to improved outcomes (Grist et al., 2017). As mHealth tools are tested and shown to be effective for supporting youth with mental health concerns, school psychologists may consider integrating them into their suite of tools for supporting students struggling with symptoms associated with suicide-related risk.
In sum, school interventions that span from universal to targeted remain an important aspect of suicide prevention, with collaborative approaches between schools, communities, and families essential for youth with more intensive mental health needs.
Implications
Applying a DisCrit lens to understanding comprehensive suicide prevention programs requires attention to “the voices of those who have been marginalized” (Sabnis & Martinez, 2022, p. 38). Voices from adolescents experiencing suicide-related crises, as well as the adults supporting them during and following crisis, echo some of the key tenets of DisCrit and intersectionality in the context of suicide prevention. Findings reinforce the multidimensional nature of identity and the significance of decentralizing (but not ignoring) intraindividual influences of mental health, and instead, centralizing mutable factors related to mental health (Edyburn et al., 2022; Sabnis & Martinez, 2022). Accordingly, school psychologists and other school professionals charged with implementing comprehensive suicide prevention programs may draw on intersectionality, DisCrit, and other diversity, equity, and inclusion (DEI) frameworks to provide school-based mental health in a way that honors student identities.
Edyburn and colleagues (2022) presented a model informed by DisCrit and related theories that prioritizes three areas of reflective practice that may help guide school psychologists in a DEI-informed approach to school-based mental health service. First, the authors point out how an emphasis on psychodiagnostic assessment can overlook the complex influences of mental health that may be mutable, such as those identified by participants in the current study (e.g., social interactions, academic pressure, school supports), and instead place the onus of a mental health concern within the child. Thus, in addition to decentralizing psychodiagnostic assessments, Edyburn et al. next called on school psychologists to centralize systems-level work, including self-reflective school personnel practices and the implementation of universal screenings of resilience factors such as coping skills that may help destigmatize mental health. The authors concluded with an emphasis on strengths and healing, which in the context of the present study’s findings, reflects the need to move beyond considering student recovery from suicide-related crises as overcoming a deficit, but instead considering the strength and resiliency that is embedded within recovery.
Limitations
This qualitative study contributes a more nuanced understanding of how school experiences may contribute to the mental health of adolescents with suicidal thoughts and behaviors. Although the nature of this research design helps to elucidate a more detailed description of lived and observed experiences, this work is limited to descriptions and does not provide insight on causality of school influences of mental health. Although the perspectives of four different cohorts (i.e., adolescents, parents, school professionals, and hospital professionals) were considered to provide a more holistic understanding of this phenomena, findings should be considered within the context of each cohort’s positionality, with bias inherent to all participant views. For example, hospital professional perceptions are based on secondary information, such as information shared by adolescents and schools. Likewise, as compared to adolescents and school professionals, parents have limited access to the school environment.
Because we did not employ member checking at the conclusion of the study, which is a validation technique to assess accuracy and appropriateness of results by participants (Birt et al., 2016), results may not accurately reflect participant experiences. Moreover, this study’s sample was limited to one southeastern state, so findings may not generalize to other locations or settings. Although school professionals represented diverse school districts across the state (see Marraccini, Pittleman, et al., 2022), hospital providers, adolescents, and parents were recruited from only one hospital. The majority of participating adolescents identified as a girl or woman, limiting understanding of school-related experiences in those identifying as boys and men or non-binary. Because we only recruited families proficient in English, parent and adolescent perspectives do not represent those facing language barriers when navigating school and hospital systems, which intersect with other cultural considerations not addressed in the present study. Additionally, stressors such as economic pressures, as well as other stressors stemming from ethnic and racial discrimination, require additional considerations not addressed in this study. Further research that prioritizes the voices of ethnic, racial, sexual, and/or gender minoritized youth struggling with suicidal thoughts and behaviors are critically needed. Of note, findings are not meant to be representative of all families and providers. Instead, they reflect deep insight from specific samples who may have commonalities with other families and providers facing similar concerns.
Conclusion
Adolescents spend a substantial portion of their time in school settings and schools are a primary referral source for hospitalization due to a suicide-related crisis (Crepeau-Hobson, 2013; Soto et al., 2009). School-related factors, such as school connectedness and bullying, have been shown to link to suicide-related risk (Holt et al., 2015; Marraccini & Brier, 2017; Marraccini, Resnikoff, et al., 2021; van Geel et al., 2022; Walker et al., 2017). As such, understanding the lived experiences of adolescents with suicidal thoughts and behaviors, as well as the adults supporting adolescents with suicide-related risk, provides insight into areas that school and health providers can collaborate to address. Findings from the present study also underscore the complexity of factors that contribute to suicide by identifying the ways in which experiences in school may converge with other risk and protective factors of suicide to influence perceived mental health. The circumstances of an adolescent’s home life and the context of school can intersect to determine if and how school can be a safe place for youth. For example, the potential for schools to provide a safe, structured, and secure environment, serving as a healthy distraction for some teens, can present as an inflexible or even rigid system incompatible to the needs of other teens in crisis, conferring negative effects. Attention to access to means and school-related triggers requires school-family-community partnerships for establishing relevant safety planning procedures appropriate to school context. Instead of solely placing blame on the school or on the family, schools, community providers, and families can partner to deliver a holistic treatment plan that leverages the strengths in each environment to support adolescent recovery.
Supplementary Material
Acknowledgments
This project was supported by Grant SRG-0-093-17 awarded to Marisa Marraccini from the American Foundation for Suicide Prevention. The project described was also supported by the National Center for Advancing Translational Sciences (NCATS), National Institutes of Health, through Grant Award Number UL1TR002489. Marisa Marraccini’s effort was supported by the National Institute of Mental Health (K23MH122775; L30MH117655; Marraccini). The efforts of and/or resources used by Amanda Tow, Juliana Vanderburg, and Christina Cruz were also supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant KL2TR002490. The content is solely the responsibility of the authors and does not necessarily represent the official views of the American Foundation for Suicide Prevention or NIH.
The researchers would like to acknowledge the families and professionals who donated their time to this project and the Qualitative Science and Methods Training Program (QSMTP) of the Department of Psychiatry and Human Behavior, Warren Alpert Medical School of Brown University, which provided training in qualitative research methods for this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Note that because hospital professional participants did not complete any questionnaires, demographic questions were asked verbally and responses were recorded based on verbal responses without providing response options (all of which matched response option categories included in the questionnaire for other adult cohorts).
References
- American Foundation for Suicide Prevention (AFSP). (2020, May 09). Model school district policy on suicide prevention Retrieved January 15, 2022, from https://afsp.org/model-school-policy-on-suicide-prevention.
- Annamma SA, Connor D, & Ferri B (2013). Dis/ability critical race studies (DisCrit): Theorizing at the intersections of race and dis/ability. Race Ethnicity and Education, 16(1), 1–31. [Google Scholar]
- Archambault I, Janosz M, Goulet M, Dupéré V, & Gilbert-Blanchard O (2019). Promoting student engagement from childhood to adolescence as a way to improve positive youth development and school completion. In Fredricks JA, Reschly AL, & Christenson SL (Eds.), Handbook of student engagement interventions: Working with disengaged students (pp. 13–29). Academic Press. [Google Scholar]
- Arora PG, Collins TA, Dart EH, Hernández S, Fetterman H, & Doll B (2019). Multitiered systems of support for school-based mental health: A systematic review of depression interventions. School Mental Health, 11(2), 240–264. [Google Scholar]
- Assari S, Moghani Lankarani M, & Caldwell CH (2017). Discrimination increases suicidal ideation in black adolescents regardless of ethnicity and gender. Behavioral Sciences, 7, 75–85. 10.3390/bs7040075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Assistant Secretary for Public Affairs (ASPA). (2020, July 21). Media Guidelines for Bullying Prevention Retrieved February 01, 2021, from https://www.stopbullying.gov/resources/media-guidelines
- Bas G (2021). Relation between student mental health and academic achievement revisited: A meta-analysis. In Health and Academic Achievement-New Findings IntechOpen. [Google Scholar]
- Berona J, Horwitz AG, Czyz EK, & King CA (2020). Predicting suicidal behavior among lesbian, gay, bisexual, and transgender youth receiving psychiatric emergency services. Journal of Psychiatric Research, 122, 64–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Birt L, Scott S, Cavers D, Campbell C, & Walter F (2016). Member checking: a tool to enhance trustworthiness or merely a nod to validation? Qualitative Health Research, 26(13), 1802–1811. [DOI] [PubMed] [Google Scholar]
- Bostik KE & Everall RD (2007). Healing from suicide: Adolescent perceptions of attachment relationships. British Journal of Guidance & Counselling, 35(1), 79–96. 10.1080/03069880601106815 [DOI] [Google Scholar]
- Bronfenbrenner U (1996). The ecology of human development: Experiments by nature and design Harvard University Press. [Google Scholar]
- Chu JP, Goldblum P, Floyd R, & Bongar, B. (2010). The cultural theory and model of suicide. Applied & Preventative Psychology, 14, 25–40. 10.1016/j.appsy.2011.11.001 [DOI] [Google Scholar]
- Coggan C, Patterson P, & Fill J (1997). Suicide: qualitative data from focus group interviews with youth. Social Science & Medicine, 45(10), 1563–1570. 10.1016/S0277-9536(97)00098-1 [DOI] [PubMed] [Google Scholar]
- Costello EJ, He JP, Sampson NA, Kessler RC, & Merikangas KR (2014). Services for adolescents with psychiatric disorders: 12-month data from the National Comorbidity Survey–Adolescent. Psychiatric Services, 65(3), 359–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crenshaw K (1989). Demarginalizing the intersection of race and sex: Black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. University of Chicago Legal Forum, 1989, 139–168. [Google Scholar]
- Crepeau-Hobson F (2013). An exploratory study of suicide risk assessment practices in the school setting. Psychology in the Schools, 50(8), 810–822. [Google Scholar]
- Czyz EK, Liu Z, & King CA (2012). Social connectedness and one-year trajectories among suicidal adolescents following psychiatric hospitalization. Journal of Clinical Child & Adolescent Psychology, 41(2), 214–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duong MT, Bruns EJ, Lee K, Cox S, Coifman J, Mayworm A, & Lyon AR (2021). Rates of mental health service utilization by children and adolescents in schools and other common service settings: A systematic review and meta-analysis. Administration and Policy in Mental Health and Mental Health Services Research, 48(3), 420–439. [DOI] [PubMed] [Google Scholar]
- Edyburn KL, Bertone A, Raines TC, Hinton T, Twyford J, & Dowdy E (2022). Integrating intersectionality, social determinants of health, and healing: A new training framework for school-based mental health. School Psychology Review, Advanced Online Publication, 1–23. [Google Scholar]
- Evelo D (1996). Keeping kids in school: Using Check & Connect for dropout prevention [Google Scholar]
- Flett GL, & Hewitt PL (2008). Treatment interventions for perfectionism—A cognitive perspective: Introduction to the special issue. Journal of Rational-Emotive & Cognitive-Behavior Therapy, 26, 127–133. [Google Scholar]
- Fredricks JA, Reschly AL, & Christenson SL Interventions for student engagement: Overview and state of the field. 2019. In Fredricks JA, Reschly AL, & Christenson SL (Eds.), Handbook of student engagement interventions: Working with disengaged students (pp. 1–11). Academic Press. [Google Scholar]
- Fulginiti A, Goldbach JT, Mamey MR, Rusow J, Srivastava A, Rhoades H, … & Marshal MP (2020). Integrating minority stress theory and the interpersonal theory of suicide among sexual minority youth who engage crisis services. Suicide and Life- Threatening Behavior, 50(3), 601–616. 10.1111/sltb.12623 [DOI] [PubMed] [Google Scholar]
- Gaffney H, Ttofi MM, & Farrington DP (2021). What works in ant-bullying programs? Analysis of effective intervention components. Journal of School Psychology, 85, 37–56. [DOI] [PubMed] [Google Scholar]
- Goldston DB, Molock SD, Whitbeck LB, Murakami JL, Zayas LH, & Hall GCN (2008). Cultural considerations in adolescent suicide prevention and psychosocial treatment. American Psychologist, 63, 14–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greytak EA, Gill A, Conron KJ, Matthews PA, Scout Reisner SL, & Tamar-Mattis A (2014). Identifying transgender and other gender minority respondents on population-based surveys: Special considerations for adolescents, race/ethnicity, socioeconomic status, and intersex status. In Herman JL (Ed.), Best practices for asking questions to identify transgender and other gender minority respondents on population-based surveys (29–34). The Williams Institute. [Google Scholar]
- Grimmond J, Kornhaber R, Visentin D, & Cleary M (2019). A qualitative systematic review of experiences and perceptions of youth suicide. PloS One, 14(6), e0217568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grist R, Porter J, & Stallard P (2017). Mental health mobile apps for preadolescents and adolescents: A systematic review. Journal of Medical Internet Research, 19(5), e176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guest G, MacQueen KM, & Namey EE (2012). Applied thematic analysis SAGE Publications. [Google Scholar]
- Gulbas LE, Hausmann-Stabile C, De Luca SM, Tyler TR & Zayas LH (2015). An exploratory study of nonsuicidal self-injury and suicidal behaviors in adolescent Latinas. American Journal of Orthopsychiatry, 85(4), 302–314. 10.1037/ort0000073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gulbas LE, & Zayas LH (2015) Examining the interplay among family, culture, and Latina teen suicidal behavior. Qualitative Health Research, 25(5), 689–699. 10.1177/1049732314553598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall M, Fullerton L, FitzGerald C, & Green D (2018). Suicide risk and resiliency factors among Hispanic teens in New Mexico: Schools can make a difference. Journal of School Health, 88(3), 227–236. 10.1111/josh.12599 [DOI] [PubMed] [Google Scholar]
- Halmi KA, Tozzi F, Thornton LM, Crow S, Fichter MM, Kaplan AS, … & Bulik CM (2005). The relation among perfectionism, obsessive-compulsive personality disorder and obsessive-compulsive disorder in individuals with eating disorders. International Journal of Eating Disorders, 38(4), 371–374. [DOI] [PubMed] [Google Scholar]
- Hatzenbuehler ML, Birkett M, Van Wagenen A, & Meyer IH (2014). Protective school climates and reduced risk for suicide ideation in sexual minority youths. American Journal of Public Health, 104(2), 279–286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heppen JB, Zeiser K, Holtzman DJ, O’Cummings M, Christenson S, & Pohl A (2018). Efficacy of the Check & Connect mentoring program for at-risk general education high school students. Journal of Research on Educational Effectiveness, 11(1), 56–82. [Google Scholar]
- Hewitt PL, Caelian CF, Flett GL, Sherry SB, Collins L, & Flynn CA (2002). Perfectionism in children: Associations with depression, anxiety, and anger. Personality and Individual Differences, 32(6), 1049–1061. [Google Scholar]
- Holt MK, Bowman C, Alexis A, & Murphy A (2020). Bullying, suicide, and suicide prevention in education. In Shapiro H (Ed.), The Wiley handbook on violence in education (pp. 449–464). John Wiley & Sons, Inc. [Google Scholar]
- Holt MK, Vivolo-Kantor AM, Polanin JR, Holland KM, DeGue S, Matjasko JL, … & Reid G (2015). Bullying and suicidal ideation and behaviors: A meta-analysis. Pediatrics, 135(2), e496–e509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jagers RJ, Rivas-Drake D, & Williams B (2019). Transformative Social and Emotional Learning (SEL): Toward SEL in service of educational equity and excellence. Educational Psychologist, 54, 162–184. 10.1080/00461520.2019.1623032 [DOI] [Google Scholar]
- Johns MM, Lowry R, Haderxhanaj LT, Rasberry CN, Robin L, Scales L, … & Suarez NA (2020). Trends in violence victimization and suicide risk by sexual identity among high school students—Youth Risk Behavior Survey, United States, 2015–2019. MMWR supplements, 69(1), 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joshi SV, Hartley SN, Kessler M, & Barstead M (2015). School-based suicide prevention: Content, process, and the role of trusted adults and peers. Child and Adolescent Psychiatric Clinics, 24(2), 353–370. [DOI] [PubMed] [Google Scholar]
- Keyvanara M, & Haghshenas A (2011). Sociocultural contexts of attempting suicide among Iranian youth: A qualitative study. East Mediterr Health Journal, 17(6), 529–535. [PubMed] [Google Scholar]
- King CA, Arango A, & Foster CE (2018). Emerging trends in adolescent suicide prevention research. Current Opinions in Psychology, 22, 89–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King CA, Grupp-Phelan J, Brent D, Dean JM, Webb M, Bridge JA, … & Pediatric Emergency Care Applied Research Network. (2019). Predicting 3-month risk for adolescent suicide attempts among pediatric emergency department patients. Journal of Child Psychology and Psychiatry, 60(10), 1055–1064.https://doi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonsky DE, Saffer BY, & Bryan CJ (2018). Ideation-to-action theories of suicide: A conceptual model and empirical update. Current Opinion in Psychology, 22, 38–43, 10.1016/j.copsyc.2017.07.020 [DOI] [PubMed] [Google Scholar]
- Kodish T, Kim JJ, Le K, Yu SH, Bear L, & Lau AS (2020). Multiple stakeholder perspectives on school-based responses to student suicide risk in a diverse public school district. School Mental Health, 12(2), 336–352. [Google Scholar]
- Konold T, & Cornell D (2015). Measurement and structural relations of an Authoritative School Climate model: A multi-level latent variable investigation. Journal of School Psychology, 53(6), 447–461. 10.1016/j.jsp.2015.09.001 [DOI] [PubMed] [Google Scholar]
- Klimes-Dougan B, Klingbeil DA, & Meller SJ (2013). The impact of universal suicide-prevention programs on the help-seeking attitudes and behaviors of youths. Crisis: The Journal of Crisis Intervention and Suicide Prevention, 34(2), 82–97. [DOI] [PubMed] [Google Scholar]
- Lazarus PJ, Doll B, Song SY, & Radliff K (2021). Transforming school mental health services based on a culturally responsible dual-factor model. School Psychology Review, Advance Online Publication, 1–16. [Google Scholar]
- Lloyd S, Yiend J, Schmidt U, & Tchanturia K (2014). Perfectionism in anorexia nervosa: novel performance based evidence. PLoS One, 9(10), e111697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luukkonen AH, Räsänen P, Hakko H, & Riala K (2009). Bullying behavior is related to suicide attempts but not to self-mutilation among psychiatric inpatient adolescents. Psychopathology, 42(2), 131–138. [DOI] [PubMed] [Google Scholar]
- Marraccini ME, & Brier ZMF (2017). School connectedness and suicidal thoughts and behaviors: A systematic meta-analysis. School Psychology Quarterly, 32(1), 5–21. 10.1037/spq0000192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marraccini ME, Lee S, & Chin AJ (2019). School reintegration post-psychiatric hospitalization: protocols and procedures across the nation. School Mental Health, 11(3), 615–628. [Google Scholar]
- Marraccini ME, Ingram KM, Naser SC, Grapin SL, Toole EN, O’Neill JC, … & Griffin D (2022). The roles of school in supporting LGBTQ+ youth: A systematic review and ecological framework for understanding risk for suicide-related thoughts and behaviors. Journal of School Psychology, 91, 27–49. 10.1016/j.jsp.2021.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marraccini ME, Griffin D, O’Neill C, Martinez R, Chin A, Toole E, Grapin SL, & Naser SC (2022). School risk and protective factors of suicide: A cultural model of suicide risk and protective factors in schools. School Psychology Review, 51(3), 266–289. DOI: 10.1080/2372966X.2020.1871305 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marraccini ME, Lindsay CA, Griffin D, Greene MJ, Simmons KT, & Ingram KM (2022). A trauma-and justice, equity, diversity, and inclusion (JEDI)-informed approach to suicide prevention in school: Black boys’ lives matter. School Psychology Review, 1–24. 10.1080/2372966X.2021.2010502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marraccini ME, & Pittleman C (2022) Returning to school following hospitalization for suicide-related behaviors: Recognizing student voices for improving practice. School Psychology Review, 51(3), 370–385. DOI: 10.1080/2372966X.2020.1862628 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marraccini ME, Pittleman C, Toole EN, & Griffard MR (2022). School supports for reintegration following a suicide-related crisis: A mixed methods study informing hospital recommendations for schools during discharge. Psychiatric Quarterly, 93(1), 347–383. 10.1007/s11126-021-09942-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marraccini ME, Vanderburg JL, Martinez RR Jr, Knotek SE, Pittleman C, & Neshkes R (2022). Development and psychometric evaluation of a brief measure of school and community mental health supports and services. Professional School Counseling, 26(1). [Google Scholar]
- Marraccini ME, Resnikoff A, Brick LA, Brier ZMF, & Nugent NR (2021). Adolescent perceptions of school before and after psychiatric hospitalization: Predicting suicidal ideation. School Psychology, 37(2), 119–132. 10.1037/spq0000487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez RR, Marraccini ME, Knotek SE, Neshkes RA, & Vanderburg J (2021). Effects of dialectical behavioral therapy skills training for emotional problem solving for adolescents (DBT STEPS-A) program of rural ninth-grade students. School Mental Health, Advance online publication, 1–14. [Google Scholar]
- Marx RA, & Kettrey HH (2016). Gay-straight alliances are associated with lower levels of school-based victimization of LGBTQ+ youth: A systematic review and meta-analysis. Journal of Youth and Adolescence, 45(7), 1269–1282. [DOI] [PubMed] [Google Scholar]
- Matel-Anderson DM, & Bekhet AK (2016). Resilience in adolescents who survived a suicide attempt from the perspective of registered nurses in inpatient psychiatric facilities. Issues in Mental Health Nursing, 37(11), 839–846. 10.1080/01612840.2016.1193578 [DOI] [PubMed] [Google Scholar]
- Matute-Chavarria M (2021). Giving voice to aspirations: Engaging African American parents with children with disabilities. Intervention in School and Clinic, 57, 211–218. [Google Scholar]
- Mazza JJ, Dexter-Mazza ET, Miller AL, Rathus JH, & Murphy HE (2016). DBT? Skills in schools: Skills training for emotional problem solving for adolescents Dbt Steps-a Guilford Publications. [Google Scholar]
- Meyer IH (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. Psychological Bulletin, 129(5), 674–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller DN (2021) Child and adolescent suicidal behavior: School-based prevention, assessment, and intervention (2nd ed.). Guilford Publications. [Google Scholar]
- Miller DN, & Mazza JJ (2018). School-based suicide prevention, intervention, and postvention. In Leschied AW, Saklofske DH, & Flett GL (Eds.), Handbook of school-based mental health promotion (pp. 261–277). Springer. 10.1007/978-3-319-89842-1_15 [DOI] [Google Scholar]
- Miller AB, & Prinstein MJ (2019). Adolescent suicide as a failure of acute stress-response systems. Annual Review of Clinical Psychology, 15, 1076–1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newton A, Bagnell A, Rosychuk R, Duguay J, Wozney L, Huguet A, … & Curran J (2020). A mobile phone-based app for use during cognitive behavioral therapy for adolescents with anxiety (MindClimb): User-centered design and usability study. JMIR mHealth and uHealth, 8(12), e18439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Holmberg EB, Photos VI, & Michel BD (2007). Self-injurious thoughts and behaviors interview: Development, reliability, and validity in an adolescent sample. Psychological Assessment, 19(3), 309–317. 10.1037/1040-3590.19.3.309 [DOI] [PubMed] [Google Scholar]
- Poteat VP, Rivers I, & Vecho O (2020). Membership experiences in gender-sexuality alliances (GSAs) predict increased hope and attenuate the effects of victimization. Journal of School Psychology, 79, 16–30. 10.1016/j.jsp.2020.02.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preyde M, Parekh S, Warne A, & Heintzman J (2017). School reintegration and perceived needs: The perspectives of child and adolescent patients during psychiatric hospitalization. Child and Adolescent Social Work Journal, 34(6), 517–526. 10.1007/s10560-017-0490-8 [DOI] [Google Scholar]
- Preyde M, Parekh S, & Heintzman J (2018). Youths’ experiences of school re-integration following psychiatric hospitalization. Journal of the Canadian Academy of Child and Adolescent Psychiatry, 27(1), 22–32. [PMC free article] [PubMed] [Google Scholar]
- Puhy CE, Litke SG, Silverstein MJ, Kiely JR, Pardes A, McGeoch E, & Daly BP (2021). Counselor and student perceptions of an mHealth technology platform used in a school counseling setting. Psychology in the Schools, 58, 1284–1298. [Google Scholar]
- QSR International Pty Ltd. (2020) NVivo (released in March 2020), https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home
- QSR International Pty Ltd. (2018) NVivo (Version 12), https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/home
- Radez J, Reardon T, Creswell C, Lawrence PJ, Evdoka-Burton G, & Waite P (2021). Why do children and adolescents (not) seek and access professional help for their mental health problems? A systematic review of quantitative and qualitative studies. European Child & Adolescent Psychiatry, 30(2), 183–211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reschly AL, Huebner ES, Appleton JJ, & Antaramian S (2008). Engagement as flourishing: The contribution of positive emotions and coping to adolescents’ engagement at school and with learning. Psychology in the Schools, 45(5), 419–431. [Google Scholar]
- Sabnis S, & Martinez CB (2022). DisCrit: Disability critical race theory. In Proctor SL & Rivera DP (Eds), Critical theories for school psychology and counseling (pp. 33–47). Routledge. [Google Scholar]
- Schechter MA, & Goldblatt MJ (2020). Suicide: A transdiagnostic phenomenon. Psychiatric Annals, 50(4), 136–137. [Google Scholar]
- Schultz TR, Zoucha R, & Sekula LK (2021). The intersection between youth who identify as LGBTQ+ and emergency care for suicidality: an integrative review. Journal of Pediatric Nursing, 63, e82–e94. [DOI] [PubMed] [Google Scholar]
- Schwartz KA, Pyle SA, Dowd MD, & Sheehan K (2010). Attitudes and beliefs of adolescents and parents regarding adolescent suicide. Pediatrics, 125(2), 221–227. [DOI] [PubMed] [Google Scholar]
- Shilubane HN, Ruiter RA, Bos AE, van den Borne B, James S, & Reddy PS (2012). Psychosocial determinants of suicide attempts among black South African adolescents: A qualitative analysis. Journal of Youth Studies, 15(2), 177–189. 10.1080/13676261.2011.634400 [DOI] [Google Scholar]
- Shilubane HN, Ruiter RAC, Bos AER, Reddy PS & van den Borne B (2014). High school students’ knowledge and experience with a peer who committed or attempted suicide: A focus group study. BMC Public Health, 14(1), 1–9. 10.1186/1471-2458-14-1081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons-Morton BG, & Crump AD (2003). Association of parental involvement and social competence with school adjustment and engagement among sixth graders. Journal of School Health, 73(3), 121–126. [DOI] [PubMed] [Google Scholar]
- Singer JB, Erbacher TA, & Rosen P (2019). School-based suicide prevention: A framework for evidence-based practice. School Mental Health, 11(1), 54–71. 10.1007/s12310-018-9245-8 [DOI] [Google Scholar]
- Soto EC, Frederickson AM, Trivedi H, et al. (2009). Frequency and correlates of inappropriate pediatric psychiatric emergency room visits. Journal of Clinical Psychiatry, 70(8), 1164–1177. [DOI] [PubMed] [Google Scholar]
- Spirito A, Esposito-Smythers C, Weismoore J, & Miller A (2012). Adolescent suicidal behavior. Child and adolescent therapy: Cognitive-behavioral procedures (pp. 234–256). Guilford Press. [Google Scholar]
- Strickland CJ, & Cooper M (2011). Getting into trouble: Perspectives on stress and suicide prevention among Pacific Northwest Indian Youth. Journal of Transcultural Nursing, 22(3), 240–247. 10.1177/1043659611404431 [DOI] [PubMed] [Google Scholar]
- Suizzo MA, Robinson C, & Pahlke E (2008). African American mothers’ beliefs and practices with young children: Relations between academic and racial socialization. Journal of Family Issues, 29(3), 287–316. [Google Scholar]
- Surgenor PW, Quinn P, & Hughes C (2016). Ten recommendations for effective school-based, adolescent, suicide prevention programs. School Mental Health, 8(4), 413–424. [Google Scholar]
- The GenIUSS Group. (2014). Best practices for asking questions to identify transgender and other gender minority respondents on population-based surveys Herman JL (Ed.). Los Angeles, CA: The Williams Institute. [Google Scholar]
- Tossone K, Jefferis E, Bhatta MP, Bilge-Johnson S, & Seifert P (2014). Risk factors for rehospitalization and inpatient care among pediatric psychiatric intake response center patients. Child Adolescent Psychiatry Mental Health, 8(27), 1–10. 10.1186/1753-2000-8-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Geel M, Goemans A, Zwaanswijk W, & Vedder P (2022). Does peer victimization predict future suicidal ideation? A meta-analysis on longitudinal studies. Aggression and Violent Behavior, 64, Article 101577. 10.1016/j.avb.2021.101577 [DOI] [Google Scholar]
- van Geel M, Vedder P, & Tanilon J (2014). Relationship between peer victimization, cyberbullying, and suicide in children and adolescents: a meta-analysis. JAMA Pediatrics, 168(5), 435–442. [DOI] [PubMed] [Google Scholar]
- Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, & Joiner TE Jr. (2010). The interpersonal theory of suicide. Psychological Review, 117(2), 575–600. 10.1037/a0018697 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walker R, Francis D, Brody G, Simons R, Cutrona C, & Gibbons F (2017). A longitudinal study of racial discrimination and risk for death ideation in African American youth. Suicide and Life-Threatening Behavior, 47(1), 86–102. 10.1111/sltb.12251 [DOI] [PubMed] [Google Scholar]
- Watson TN, & Bogotch I (2015). Reframing parent involvement: What should urban school leaders do differently? Leadership and Policy in Schools, 14(3), 257–278. [Google Scholar]
- Watts RJ, Diemer MA, & Voight AM (2011). Critical consciousness: Current status and future directions. New Directions for Child and Adolescent Development, 134, 43–57. [DOI] [PubMed] [Google Scholar]
- Whaley AL, & Noel L (2003). Academic achievement and behavioral health among Asian American and African American adolescents: testing the model minority and inferior minority assumptions. Social Psycholology of Education 16(1) 23–43. 10.1007/s11218-012-9206-2 [DOI] [Google Scholar]
- White J, & Morris J (2010). Precarious spaces: Risk, responsibility and uncertainty in school-based suicide prevention programs. Social Science & Medicine, 71(12), 2187–2194. [DOI] [PubMed] [Google Scholar]
- Wilcox HC, Kellam SG, Brown CH, Poduska JM, Ialongo NS, Wang W, & Anthony JC (2008). The impact of two universal randomized first-and second-grade classroom interventions on young adult suicide ideation and attempts. Drug and Alcohol Dependence, 95, S60–S73. 10.1016/j.drugalcdep.2008.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wyman PA (2014). Developmental approach to prevent adolescent suicides: Research pathways to effective upstream preventive interventions. American Journal of Preventive Medicine, 47(3), S251–S256. 10.1016/j.amepre.2014.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeager DS, Hanselman P, Walton GM, Murray JS, Crosnoe R, Muller C, … & Dweck CS (2019). A national experiment reveals where a growth mindset improves achievement. Nature, 573(7774), 364–369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zayas L, Gulbas LE, Fedoravicius N, & Cabassa LJ (2010). Patterns of distress, precipitating events, and reflections on suicide attempts by young Latinas. Social Science & Medicine, 70(11), 1773–1779. 10.1016/j.socscimed.2010.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeng G, Hou H, & Peng K (2016). Effect of growth mindset on school engagement and psychological well-being of Chinese primary and middle school students: The mediating role of resilience. Frontiers in Psychology, 7, 1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


