Abstract
BACKGROUND
Paraduodenal hernia (PDH) is a mesenteric-parietal hernia with retroperitoneal and retrocolic herniation of the small bowel into a sac, which is formed by a peritoneal fold located near the fourth portion of the duodenum. The present case revealed that PDH was a possible reason for hydronephrosis, and that the carful laparoscopic exploration surgery was necessary to find infrequent causes of hydronephrosis to avoid invalid Anderson–Hynes pyeloplasty surgery and its injury.
CASE SUMMARY
An 8-year-old boy presented to the pediatric department with a chief complaint of cryptorchidism. Afterwards, laparoscopy confirmed hydronephrosis secondary to left PDH with cryptorchid. Then, he received laparoscopic surgery, fixed operation for left PDH, release of the ureteropelvic junction obstruction, and treatment for hydronephrosis. It is necessary to perform secondary surgery for cryptorchidism and long-term follow-up.
CONCLUSION
The case revealed an extremely rare cause of hydronephrosis in children, suggesting a potential correlation between PDH and hydronephrosis.
Keywords: Paraduodenal hernia, Hydronephrosis, Cryptorchidism, Laparoscopic surgery, Case report
Core Tip: Paraduodenal hernia (PDH) is a kind of mesenteric-parietal hernia accompanied by retroperitoneal and retrocolic hernia. The small intestine hernia enters the sac, which is formed by peritoneal folds located near the fourth part of the duodenum. The present case revealed that PDH was a possible reason for hydronephrosis, and that the carful laparoscopic exploration surgery was necessary to find infrequent causes of hydronephrosis to avoid invalid Anderson-Hynes pyeloplasty surgery and its injury.
INTRODUCTION
Internal hernia refers to the outward protrusion of internal organs through the peritoneum or mesentery, and accounts for less than 1% of all abdominal hernias[1]. Of all the internal hernias, paraduodenal hernia (PDH) is the most common. Left PDH accounts for about 75% of all cases. PDH can cause small bowel obstruction and hydronephrosis[2]. Currently, diagnosing internal hernia is challenging.
Cryptorchidism is a common congenital disease, with an incidence of 2%–5% in male births. When the testis is missing or dysfunctional, the temperature of the inguinal canal and inside the abdomen increases, which harms the germinal epithelium and can lead to malignancy. Only 7% of pediatric patients with inguinal hernia present with cryptorchidism, and PDH combined with cryptorchidism is rare. The present case revealed that PDH was a possible reason for hydronephrosis, and the careful laparoscopic exploration surgery was necessary to find infrequent causes of hydronephrosis to avoid invalid Anderson-Hynes pyeloplasty surgery and its injury.
CASE PRESENTATION
Chief complaints
An 8-year-old boy was admitted to our hospital because of enuresis and missing right testis.
History of present illness
The patient had been diagnosed with cryptorchidism at another hospital.
History of past illness
The boy was healthy.
Personal and family history
The patient had no family history of reproductive and urinary disease.
Physical examination
The body mass index was 14.2 kg/m2, and physical and rectal examinations were unremarkable. The left testis was topical without alterations, and the right testis was imperceptible in the scrotum.
Laboratory examinations
No abnormality was found in routine blood and urine analyses.
Imaging examinations
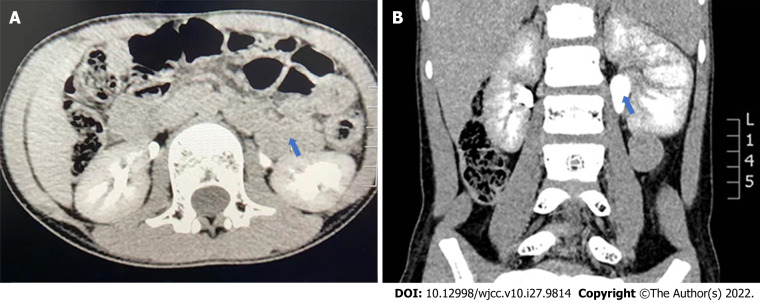
Urinary B-ultrasound revealed left hydronephrosis. Serum creatinine and blood urea nitrogen levels were normal. Contrast-enhanced computed tomography (CT) confirmed left hydronephrosis and left ureteropelvic junction obstruction (UPJO), but not PDH (Figure 1).
Figure 1.
Contrast-enhanced computed tomography. A: Computed tomography section at the level of renal vessels shows a horseshoe appearance of the bowel loops that contain the jejunal vessels radiating inside the hernial sac; B: Left hydronephrosis.
FINAL DIAGNOSIS
Hydronephrosis and cryptorchism.
TREATMENT
Laparoscopic exploration and Anderson-Hynes pyeloplasty are often used for intraoperative diagnosis and correction of UPJO. A 10-mm port was inserted in the infraumbilical direction using the Hasson technique, and the other ports were placed below the umbilicus and epigastric region. Laparoscopic examination showed dilation of the left renal pelvis, and some adjacent intestines and rings surrounding the duodenal recess, forming PDH. The PDH compressed the upper part of the left ureter, causing hydronephrosis (Figure 2).
Figure 2.

Intraoperative image. The patient was lying on the right side while we performed the surgery. The observation hole was near the umbilicus. Intra-operatively, it was observed that small-bowel loops were lying within a hernial sac. The upper end of the ureter was located in the retroperitoneum, behind the hernia sac. The sac was opened with an ultrasonic shear, and the bowel was freed up. The hernia sac compressed the upper ureter of the left ureter and induced hydronephrosis. A: Small intestine; B: Hernia sac; C: Lateral peritoneum.
The small intestine is smaller in patients with PDH than in normal children of the same age, and the hernia can be reduced by incision and traction of the hernia sac. An incision on the hernia sac wall releases the hernia sac. After placing the bowel in the hernia sac at the correct position, we found that the anterior wall of the hernia sac neck (the branches of the inferior mesenteric vein and left colonic artery) blocked the blood supply of some bowel tubes. To make sure that the blood vessel (the branches of the inferior mesenteric vein and left colonic artery) was not necessary, we had been occluding it for 20 min. We made sure that the intestinal color, peristalsis, and blood supply were normal, so the blood vessel was cut off. We concluded that some UPJOs were caused by external compression and did not perform pyeloplasty. No local or systemic complications were noted.
OUTCOME AND FOLLOW-UP
After 12 wk of follow-up, hydronephrosis and calyceal dilatation disappeared. Three months later, the patient underwent laparoscopic testicular descent and fixation under general anesthesia to treat cryptorchidism. Two years later, CT showed that the hydronephrosis had subsided (Figure 3). Blood urea nitrogen and serum creatinine levels were normal.
Figure 3.

Computed tomography performed 2 years after laparoscopic paraduodenal hernia repair showed that the hydronephrosis was remitted and the paraduodenal hernia had been recovered.
DISCUSSION
Since PDH was first described in 1857 and classified in 1889[3], studies have shown that poor rotation is a potential mechanism of PDH. Midgut rotation occurs in gestational weeks 5–11, and the mesentery fuses the posterior abdominal structure from the right iliac fossa to the Trez ligament[4,5]. PDH can present as asymptomatic, recurring abdominal pain, or acute obstruction[6].
Left PDH develops secondarily to midgut rotation failure[7], which can lead to small bowel obstruction or other clinical manifestations. It is difficult to diagnose because of complex clinical features[8]. Laboratory tests are of little diagnostic value, and physical examination cannot lead to a diagnosis unless the hernia is sufficiently large to form an abdominal mass. Currently, about 50% of internal hernias are confirmed by imaging examinations, autopsy, or surgeries[9]. Although CT is good for diagnosis of PDH in patients without a specific presentation[10], only 10%–15% of cases are diagnosed preoperatively[11].
Surgical repair is the conventional treatment for left PDH, and approximately 50% of patients present with complications[12]. Surgery resects the ischemic intestinal segment, returns the contents of the hernia to the normal position, and closes the hernia hole. Preventing hernia recurrence remains a challenge. It is rare to implant prosthesis to repair defects. Mesh implants are used to repair recurrent hernia and large defects[13]. Open surgery was a traditional method for treatment of left PDH. Until 1998, Uematsu et al[14] first reported laparoscopic surgery for PDH, which is now often used to diagnose and repair PDH[14].
In this case, the preoperative examination did not reveal the presence of PDH, so we planned to perform laparoscopic pyeloplasty, with an operation time of about 1.5 h. Because the stent needs to be removed again 6-8 wk after pyeloplasty, we planned to perform testicular descent and fixation at the same time during the second stent removal operation, which takes approximately 1 h. Thus, patients do not have to undergo long-term general anesthesia multiple times, and the number of operations does not increase. However, PDH was accidentally found during hydronephrosis surgery. It is inferred that hydronephrosis may be caused by PDH, but the real cause remains to be further discovered. We have never seen the PDH during the operation of hydronephrosis. After observation and analysis during the operation, we concluded that the patient's UPJO was not obvious and the location of the PDH was close to the ureteropelvic junction, so hydronephrosis caused by the compression of the ureteropelvic junction by the PDH was suspected. Although this was not certain, we decided to repair the PDH first to avoid irreversible damage caused by blind treatment of the ureteropelvic junction. The follow-up results confirmed that our decision was correct.
Because we had no previous experience in surgical repair of PDH, the operation was long (about 3 h), and the anesthesia time for the patient was longer than 3 h. The position and incision of testicular descent fixation are quite different from those of PDH surgery. If testicular descent fixation had been performed at this time, the patient would have endured a longer period of general anesthesia and bear the risk of changes in position and incision during the operation. Considering these disadvantages, we decided to wait for the recovery of this operation before performing testicular descent fixation.
We extracted 23 cases from PubMed , Google Scholar, and Reference Citation Analysis (https:// www.referencecitationanalysis.com/) databases using the keywords “hydronephrosis,” “PDH,” and “internal hernia,” and found that only two cases required conversion to laparotomy (Table 1). Overall, laparoscopic diagnosis and repair surgery were used to treat left PDH.
Table 1.
Cases of left paraduodenal hernia reported in the literature
|
Ref.
|
Sex
|
Age
|
Size of defect (cm)
|
Sac excised
|
Defect closed
|
Postoperative LOS (d)
|
Laparoscopy completed
|
| Lee and Choi[15] | F | 74 | 3 | N | Y | 4 | Y |
| Jeong et al[16] | M | 52 | 5 | N | Y | 5 | Y |
| Jeong et al[16] | F | 58 | 6 | N | Y | 5 | Y |
| Cundy et al[17] | M | 55 | 6 | N | Y | 6 | N |
| Palanivelu et al[18] | M | 44 | 7 | N | Y | 5 | Y |
| Palanivelu et al[18] | M | 49 | 8 | N | Y | 2 | Y |
| Palanivelu et al[18] | F | 54 | 9 | N | Y | 2 | Y |
| Nam et al[19] | M | 1 | 3 | N | Y | 5 | Y |
| Nam et al[19] | F | 12 | 5 | N | Y | 5 | Y |
| Fukunaga et al[20] | M | 51 | 5 | N | Y | 9 | Y |
| Coakley et al[21] | M | 25 | 6 | Y | N | 3 | N |
| Parmar and Parmar[10] | M | 38 | 8 | Y | NM | 3 | Y |
| Shoji et al[22] | M | 60 | 3 | N | Y | 6 | Y |
| Siddika et al[23] | M | 35 | 3 | N | Y | 6 | Y |
| Khalaileh et al[24] | F | 53 | 4 | N | Y | 3 | Y |
| Rollins and Glasgow[25] | M | 21 | 4 | N | Y | 2 | Y |
| Uematsu et al[14] | M | 44 | 5 | N | Y | 28 | Y |
| Hussein et al[26] | M | 59 | 5 | N | Y | 3 | Y |
| Moon et al[27] | M | 18 | 2 | Y | Y | 2 | Y |
| Assenza et al[11] | M | 67 | 3 | N | N | 4 | Y |
| Uchiyama et al[28] | F | 80 | 5 | N | N | 3 | Y |
| Kulkarni et al[29] | M | 36 | 4 | N | Y | 3 | Y |
| Kulkarni et al[29] | M | 42 | 4 | Y | Y | 3 | Y |
LOS: Length of hospital stay; F: Female; M: Male; N: No; Y: Yes.
In our case, long-term postoperative follow-up showed that hydronephrosis was cured. This finding provides indirect evidence that hydronephrosis is caused by PDH. This case could help to avoid similar surgical risks and introduce a possible cause of hydronephrosis. It revealed that PDH was a possible reason for hydronephrosis. And the carful laparoscopic exploration surgery was necessary to find infrequent causes of hydronephrosis to avoid invalid Anderson-Hynes pyeloplasty surgery and its injury.
CONCLUSION
The case revealed that PDH is a possible reason for hydronephrosis. Laparoscopic exploration is useful for diagnosis and treatment. The carful laparoscopic exploration surgery is necessary to find infrequent causes of hydronephrosis to avoid invalid Anderson-Hynes pyeloplasty surgery and its injury. Attention should be paid to these unusual findings in long-term follow-up studies.
ACKNOWLEDGEMENTS
We thank the patient and all the rest doctors and nurses in our department.
Footnotes
Informed consent statement: Written informed consent was obtained from the patient's legal guardian for publication of this case report and any accompanying images.
Conflict-of-interest statement: All the authors report no relevant conflicts of interest for this article.
CARE Checklist (2016) statement: The authors have read the CARE Checklist (2016), and the manuscript was prepared and revised according to the CARE Checklist (2016).
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Peer-review started: April 23, 2022
First decision: June 16, 2022
Article in press: August 15, 2022
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Basu S, India; Sultan AAEA, Egypt S-Editor: Fan JR L-Editor: Wang TQ P-Editor: Fan JR
Contributor Information
Xin Wang, Department of Pediatric Surgery, Tianjin Children's Hospital, Tianjin 300014, China.
Yong Wu, Department of Pediatric Surgery, Tianjin Children's Hospital, Tianjin 300014, China.
Yong Guan, Department of Pediatric Surgery, Tianjin Children's Hospital, Tianjin 300014, China. guan_lab@126.com.
References
- 1.Husain A, Bhat S, Roy AK, Sharma V, Dubey SA, Faridi MS. Internal Hernia through Paraduodenal Recess with Acute Intestinal Obstruction: A Case Report. Indian J Surg. 2012;74:354–355. doi: 10.1007/s12262-011-0243-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Winder JS, Pauli EM, Haluck RS. Laparoscopic repair of a left-sided paraduodenal hernia. Surg Endosc. 2016;30:3636–3637. doi: 10.1007/s00464-015-4648-1. [DOI] [PubMed] [Google Scholar]
- 3.Schizas D, Apostolou K, Krivan S, Kanavidis P, Katsaros I, Vailas M, Koutelidakis I, Chatzimavroudis G, Pikoulis E. Paraduodenal hernias: a systematic review of the literature. Hernia. 2019;23:1187–1197. doi: 10.1007/s10029-019-01947-3. [DOI] [PubMed] [Google Scholar]
- 4.Akbulut S. Unusual cause of intestinal obstruction: left paraduodenal hernia. Case Rep Med. 2012;2012:529246. doi: 10.1155/2012/529246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Manfredelli S, Andrea Z, Stefano P, Giovanni L, Maria M, Angelo F, Alberto A, Renato M. Rare small bowel obstruction: Right paraduodenal hernia. Case report. Int J Surg Case Rep. 2013;4:412–415. doi: 10.1016/j.ijscr.2012.11.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yun MY, Choi YM, Choi SK, Kim SJ, Ahn SI, Kim KR. Left paraduodenal hernia presenting with atypical symptoms. Yonsei Med J. 2010;51:787–789. doi: 10.3349/ymj.2010.51.5.787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Târcoveanu E, Angelescu N. A European surgeon: Thoma Ionescu (Thomas Jonnesco)--founder of the Romanian school of surgery (1860-1926) Acta Chir Belg. 2009;109:824–828. doi: 10.1080/00015458.2009.11680550. [DOI] [PubMed] [Google Scholar]
- 8.Kabbani D, Salem A, Holloway DK. Paraduodenal herniation: An internal herniation in a virgin abdomen. Int J Surg Case Rep. 2014;5:1148–1150. doi: 10.1016/j.ijscr.2014.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kuzinkovas V, Haghighi K, Singhal R, Andrews NJ. Paraduodenal hernia: a rare cause of abdominal pain. Can J Surg. 2008;51:E127–E128. [PMC free article] [PubMed] [Google Scholar]
- 10.Parmar BP, Parmar RS. Laparoscopic management of left paraduodenal hernia. J Minim Access Surg. 2010;6:122–124. doi: 10.4103/0972-9941.72601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Assenza M, Rossi D, Rossi G, Reale C, Simonelli L, Romeo V, Guerra F, Modini C. Laparoscopic management of left paraduodenal hernia. Case report and review of literature. G Chir. 2014;35:185–189. [PMC free article] [PubMed] [Google Scholar]
- 12.Falk GA, Yurcisin BJ, Sell HS. Left paraduodenal hernia: case report and review of the literature. BMJ Case Rep. 2010;2010 doi: 10.1136/bcr.04.2010.2936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fukada T, Mukai H, Shimamura F, Furukawa T, Miyazaki M. A causal relationship between right paraduodenal hernia and superior mesenteric artery syndrome: a case report. J Med Case Rep. 2010;4:159. doi: 10.1186/1752-1947-4-159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Uematsu T, Kitamura H, Iwase M, Yamashita K, Ogura H, Nakamuka T, Oguri H. Laparoscopic repair of a paraduodenal hernia. Surg Endosc. 1998;12:50–52. doi: 10.1007/s004649900591. [DOI] [PubMed] [Google Scholar]
- 15.Lee SE, Choi YS. Left paraduodenal hernia combined with acute cholecystitis. Ann Surg Treat Res. 2014;86:217–219. doi: 10.4174/astr.2014.86.4.217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jeong GA, Cho GS, Kim HC, Shin EJ, Song OP. Laparoscopic repair of paraduodenal hernia: comparison with conventional open repair. Surg Laparosc Endosc Percutan Tech. 2008;18:611–615. doi: 10.1097/SLE.0b013e3181825733. [DOI] [PubMed] [Google Scholar]
- 17.Cundy TP, Di Marco AN, Hamady M, Darzi A. Giant left paraduodenal hernia. BMJ Case Rep. 2014;2014 doi: 10.1136/bcr-2013-202465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Palanivelu C, Rangarajan M, Jategaonkar PA, Anand NV, Senthilkumar K. Laparoscopic management of paraduodenal hernias: mesh and mesh-less repairs. A report of four cases. Hernia. 2008;12:649–653. doi: 10.1007/s10029-008-0376-y. [DOI] [PubMed] [Google Scholar]
- 19.Nam SH, Kim KW, Kim JS, Kim KH, Park SJ. Laparoscopic treatment of left paraduodenal hernia in two cases of children. Int J Surg Case Rep. 2012;3:199–202. doi: 10.1016/j.ijscr.2012.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fukunaga M, Kidokoro A, Iba T, Sugiyama K, Fukunaga T, Nagakari K, Suda M, Yosikawa S. Laparoscopic surgery for left paraduodenal hernia. J Laparoendosc Adv Surg Tech A. 2004;14:111–115. doi: 10.1089/109264204322973907. [DOI] [PubMed] [Google Scholar]
- 21.Coakley BA, Froylich D, Wong R, Khaitov S. Repair of primary bowel obstruction resulting from a left paraduodenal hernia. Am Surg. 2012;78:E422–E424. [PubMed] [Google Scholar]
- 22.Shoji T, Nishiyama R, Oba K, Azuma M. Left paraduodenal hernia successfully treated with laparoscopic surgery: a case report. Case Rep Gastroenterol. 2007;1:71–76. doi: 10.1159/000107595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Siddika A, Coleman AH, Pearson TE. Laparoscopic repair of left paraduodenal hernia. J Surg Case Rep. 2013;2013 doi: 10.1093/jscr/rjt079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Khalaileh A, Schlager A, Bala M, Abu-Gazala S, Elazary R, Rivkind AI, Mintz Y. Left laparoscopic paraduodenal hernia repair. Surg Endosc. 2010;24:1486–1489. doi: 10.1007/s00464-009-0794-7. [DOI] [PubMed] [Google Scholar]
- 25.Rollins MD, Glasgow RE. Left paraduodenal hernia. J Am Coll Surg. 2004;198:492–493. doi: 10.1016/j.jamcollsurg.2003.07.025. [DOI] [PubMed] [Google Scholar]
- 26.Hussein M, Khreiss M, Al-Helou G, Alaeddine M, Elias E, Abi Saad GS. Laparoscopic repair of a left paraduodenal hernia presenting with acute bowel obstruction: report of a case. Surg Laparosc Endosc Percutan Tech. 2012;22:e28–e30. doi: 10.1097/SLE.0b013e31823f3798. [DOI] [PubMed] [Google Scholar]
- 27.Moon CH, Chung MH, Lin KM. Diagnostic laparoscopy and laparoscopic repair of a left paraduodenal hernia can shorten hospital stay. JSLS. 2006;10:90–93. [PMC free article] [PubMed] [Google Scholar]
- 28.Uchiyama S, Imamura N, Hidaka H, Maehara N, Nagaike K, Ikenaga N, Hotokezaka M, Chijiiwa K. An unusual variant of a left paraduodenal hernia diagnosed and treated by laparoscopic surgery: report of a case. Surg Today. 2009;39:533–535. doi: 10.1007/s00595-008-3875-7. [DOI] [PubMed] [Google Scholar]
- 29.Kulkarni GV, Salgaonkar HP, Sharma PC, Chakkarvarty NR, Katara AN, Bhandarkar DS. Laparoscopic repair of left paraduodenal hernia: Report of two cases and review of the literature. Asian J Endosc Surg. 2016;9:157–160. doi: 10.1111/ases.12270. [DOI] [PubMed] [Google Scholar]