ABSTRACT
This review is based on a multiple database survey on published literature to determine the effects on health following voluntary exposure to cold-water immersion (CWI) in humans. After a filtering process 104 studies were regarded relevant. Many studies demonstrated significant effects of CWI on various physiological and biochemical parameters. Although some studies were based on established winter swimmers, many were performed on subjects with no previous winter swimming experience or in subjects not involving cold-water swimming, for example, CWI as a post-exercise treatment. Clear conclusions from most studies were hampered by the fact that they were carried out in small groups, often of one gender and with differences in exposure temperature and salt composition of the water. CWI seems to reduce and/or transform body adipose tissue, as well as reduce insulin resistance and improve insulin sensitivity. This may have a protective effect against cardiovascular, obesity and other metabolic diseases and could have prophylactic health effects. Whether winter swimmers as a group are naturally healthier is unclear. Some of the studies indicate that voluntary exposure to cold water has some beneficial health effects. However, without further conclusive studies, the topic will continue to be a subject of debate.
KEYWORDS: Cold-water immersion, winter swimming, ice bathing, insulin resistance, cardiovascular disease, brown adipose tissue
Introduction
Cold-water immersion (CWI) in the form of cold-water/ice bathing is a popular activity. There are many different forms of this activity and some have been clearly defined. For example, winter swimming is defined as the activity of swimming in cold water during the winter season [1]. In countries with colder winter climates, it may be synonymous with ice swimming, where the frozen ice layer has been removed to expose the water. The International Ice Swimming Associations (IISA) and the International Winter Swimming Association (IWSA) have similar competition guidelines [2,3]. These guidelines differentiate between swimming in ice water of −2 to +2°C, freezing water of +2.1 to 5°C and cold water of +5.1 to +9°C [2,3]. While swimming in icy/winter conditions has attracted a lot of focus, it is important to note that many swim regularly in water temperatures throughout the year that are not so extreme. As can be seen in Table 1 this review includes CWI articles in water temperatures up to 20°C
Table 1.
Exclusion criteria in database survey.
| Animal studies (with a few exceptions where it was felt they were relevant for humans) |
| Cold stress without water immersion |
| Aggravations of medical conditions when exposed to seawater |
| Accidental cold-water immersions |
| Water temperatures greater than 20°C |
| Treatment of hyperthermia |
| Therapy in general |
| Studies investigating the effect of a medication on CWI |
| Research on people with conditions such as diabetes, Raynauds, cardiovascular disease, homozygous sickle cell disease |
| Studies using wet suits |
| Studies on cold weather altitude acclimatisation |
| Publications were there was only a title with an abstract or publications with only a title. |
| Studies only including the title |
Ice bathing has been suggested to have many health benefits. For example, in the popular literature it has been claimed that it can boost the immune system, treat depression, enhance peripheral circulation, increase libido, burn calories and reduce stress [4]. However, many of the proclaimed health benefits are based on subjective claims and anecdotal cases.
A few studies give some scientific insight on the health benefits of ice bathing and exposure to cold air. These studies suggest that regular cold exposure can be effective in treatment of chronic autoimmune inflammation [5], reduce hypercholesterolaemia by brown adipose tissue activation [6] and have a positive effect on stress regulation [5]. However, many of the health benefits claimed from regular cold-water exposure may not be causal and may, instead, be explained by other factors. Such factors could include, for example, an active lifestyle, trained stress handling (meditation, breathing techniques, mindfulness), social interactions, aesthetic environmental surroundings, healthy food and healthy food intake patterns and a positive mindset.
While the details above describe some of the proposed benefits of CWI there is still much debate concerning this topic. From recent articles in the popular press, there has been an upsurge of interest in cold-water bathing in recent years worldwide in all age groups, although there are always special concerns with regard to the elderly [7]. In the light of this there is a clear need for evidence-based scientific research documenting the potential health benefits. While there are a few published reviews on the subject [8], most of them have only concentrated on certain types of cold-water exposure, for example, extreme cold exposure.
The purpose of this review article was to make a thorough examination of the available published scientific documentation on recreational cold-water exposure without any input from the large volume of articles in the popular press.
Methods
The review starts with an explanation of the literature search procedure and the narrowing down of the relevant publications. Based on the relevant selected articles, the physiological effects connected with regular cold-water immersion (CWI) are discussed in detail.
As a starting point, a detailed multiple database survey of the available published medical literature related to immersion in cold water and its health benefits was carried out. The search was restricted to the databases medline, embase and pubmed and required different advanced searches for each database.
Medical subject headings MeSH terms were discovered by using the function “explode” after typing in pre-established terms related to the review. This function suggested different MeSH-terms related to the established terms. The pre-established search terms (Figure 1) were chosen from exploring claims from scientific articles found in the popular press and internet.
Figure 1.
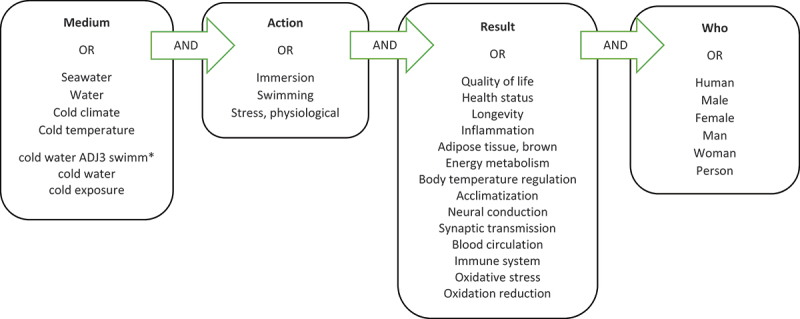
MEDLINE and EMBASE literature review medical subject MeSH terms (Medium, Action, Result, who) and functions (OR and AND) used in the literature survey.
MEDLINE and EMBASE are both OVID databases and have the same search functions. Using the function ADJ with a number, it is possible to find research papers mentioning terms that are placed adjacent to each other, within the distance of the number of words or sentences typed next to “ADJ”. Three main terms: “cold”, “water” and “swimming” were selected in an advanced search consisting of this function; “cold water adj3 swimm*”. Using the function “*” the search included every term beginning with “swimm”. This advanced search resulted in a total of 131 relevant research papers in MEDLINE and 204 relevant research papers in EMBASE.
In the database PUBMED, the strategy consisted of using a combination of MeSH terms related to the subject combined by the function OR, and later combined in groups by the function AND (Figure 1). The MeSH terms were divided in four groups related to either the medium, action, effects/results or population. Group 1 consisted of MeSHs describing the medium; seawater, water, cold climate, cold temperature. Group 2 consisted of MeSHs describing the action; immersion, swimming, physiological stress. Group 3 consisted of keywords describing the results; Quality of life, health status, longevity, inflammation, brown adipose tissue, energy metabolism, body temperature regulation, acclimatisation, neural conduction, synaptic transmission, blood circulation, immune system, oxidative stress, and oxidation reduction. Group 4 consisted of MeSHs describing the population of interest; humans, females, males. The advanced search in PUBMED resulted in a total of 405 research papers.
Many of the published research articles concerned animals, which were included in the initial search, although most were later filtered out (see exclusion criteria below).
In order to focus on the health effects of CWI in humans, it was necessary to employ some exclusion criteria (Table 1). After employing the exclusion criteria, the number of studies was narrowed down from 728 to 265. Following a more thorough examination of these 265 studies, many more were regarded as being irrelevant due to factors, such as double publication, non-regular cold-water exposure, not focusing on health effects, research that is no longer valid and no available online research paper. Following this procedure, 104 studies were relevant for the review. The main findings of these 104 articles are described and categorised for convenience using different organ systems. Before these findings are described, a brief general introduction into human cold thermoregulation physiology is presented, with reference to the 104 selected publications where appropriate.
Results
Physiological responses to cold
As in exercise and hypoxia, cold-water exposure is a physiological challenge to the body organ systems. The body has to adjust to the cool environment to maintain the temperature in the brain and organs of the core by appropriately regulating heat production and heat loss mechanisms. The main effects of acute cold exposure on human body physiology are shown in Figure 2 and are described in more detail below.
Figure 2.
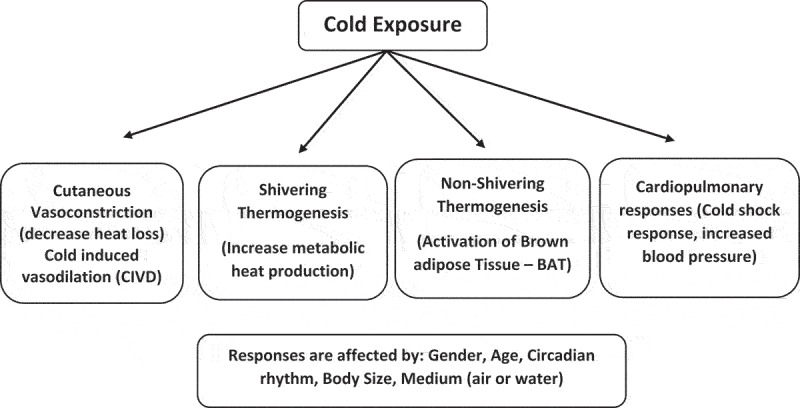
The acute effects of cold exposure on human body physiology.
Thermoregulation and skin blood perfusion
The vasomotor control of skin blood perfusion through vasoconstriction and vasodilation and its role in body thermoregulation is a well-established physiological mechanism. Heat is mainly distributed to the outer layer of the skin by blood flow. The warm blood from the core is transported to the dermis of the skin through a network of blood vessels, after have penetrated the subcutaneous tissue. The venous plexus in the subcutaneous skin layer plays an important role in temperature regulation. The large volume capacity of the venous plexus makes it possible to lose heat when necessary, depending on the arterial inflow, which is regulated by the core temperature. The skin receives a continuous supply of blood from the core through the skin capillaries. While skin blood perfusion is important for tissue viability, the large changes in skin blood perfusion from full vasoconstriction to full vasodilation, especially in the acral parts of the body, are used for heat exchange between the skin surface and the environment. In the acral parts like the hands, feet, nose and ear helix, the blood from the subcutaneous arteries can be transmitted directly to the venous plexi through a network of small blood vessels called arteriovenous anastomosis, or AVAs. The AVAs are surrounded by smooth muscle that contracts and dilates to regulate the blood flow and therewith regulates the temperature in the respective skin areas they supply. These short circuit vessels are open in situations when the body needs to lose heat and are closed during heat conservation in the cold. Their function in thermoregulation from the hands and feet can nicely be demonstrated with infrared thermography [9–11].
In thermoneutral or warm environments (25–30°C) the skin, especially in the acral parts of the body, is overly perfused when compared with the nutritive needs of the skin [12]. The purpose of the extra blood flow is considered to be mainly connected to thermoregulation, by increased radiative and convective heat loss. The control of the blood flow is influenced by both neurogenic reflexes and local factors [13]. Neural control of human skin circulation is regulated by vasomotor control (vasoconstriction and vasodilation) by the sympathetic nervous system. In thermoneutral environments this system is tonically active, altering slight changes in blood flow to maintain a constant body temperature. This automatic regulative effect is mainly controlled by cardiovascular homoeostatic reflexes activated by carotid sinus pressure receptors and atrial volume receptors. In response to changes in environmental temperature, thermoregulatory hypothalamic neurons release norepinephrine with other co-transmitters. In addition, local endothelium mediated factors also contribute to adjustments in vasoconstriction. This mechanism of vasoconstriction reduces heat loss of the skin, blood flow and nerve conduction velocity [14].
Under normal environmental conditions the vasomotor response (vasodilation/vasoconstriction) is used to regulate body core temperature within the thermoneutral zone. Under these conditions, the skin is fully vasoconstricted at the lower critical temperature (lower limit of the thermoneutral zone) [15].
The vasoconstriction of the peripheral blood vessels sets in at an estimated core temperature of 37.1°C when immersed in cold water and a temperature of 37.5°C when immersed in cold water post-exercise [16]. It should be noted that these participants were at the high side of normal deep body temperature. A thermal drive from the cooling skin temperatures also contribute to invoking shivering thermogenesis [17].
When body core temperature falls below the lower critical temperature [18], the body is unable to prevent a further fall by vasomotor control alone. In order to prevent a further fall, it has to invoke its second heat defence system, namely increasing heat production by shivering (see below). The core temperature threshold for shivering was estimated to be 36.2°C pre-exercise and 36.5°C post-exercise, when immersed in cold water [16].
There are large individual variations in the physiological response to CWI. This was nicely demonstrated in a recent study using dynamic infrared thermography (DIRT) [19]. In this study, Norheim et al. were able to demonstrate the differences in rewarming ability in a cohort of 255 healthy Norwegian army conscripts exposed to a mild cold provocation test (immersion of the hands for one minute in water at 20°C). While the majority were able to rewarm their hands passively, to pre-test peripheral temperature within 4 minutes, 10% had a slow or decreased rewarming.
The slower rewarmers tended to have lower pre-cooling average hand skin temperatures compared to the normal and fast rewarmers. This indicates that even among a group of largely heterogeneous healthy individuals, some individuals might have a different physiological response to immersion in cold water.
Shivering and nonshivering thermogenesis
In addition to the production of body heat by normal basal metabolic processes, the body is, in addition to physical exercise, able to generate extra heat through the process of shivering and nonshivering thermogenesis.
Shivering is the process of continuous and asynchronous contraction of skeletal muscles in the body. Peripheral and central thermal receptors stimulate the hypothalamic thermoregulatory control centre, which mediates an effector response through supraspinal- and peripheral motor neurons. The increased muscle activity is highly energy dependent and, in consequence, causes an elevated metabolic rate. The maximum amount of heat that the body can produce by shivering thermogenesis is about 5 times greater than the basal metabolic heat production [20]. Metabolic energy production, or cell respiration, is an exothermic reaction and is the chief generator of additional heat production in cold environments [21].
While considerably more heat can be produced by physical activity than by shivering, shivering in a CWI situation is more effective than exercise at producing heat because the individual remains relatively immobile and less heat is lost by convection [17].
Brown adipose tissue (BAT) is capable of producing excess heat through the process of non-shivering thermogenesis. The heat is generated by the action of free fatty acids in uncoupling mitochondrial electron transport, and by noradrenaline-induced membrane depolarisation and sodium pumping. These adipocytes have a higher number of mitochondria compared to white adipocytes. Through a chemical process involving loose coupling of oxidative phosphorylation the mitochondria in BAT are able to burn triglycerides and produce large quantities of heat, which are released directly into the bloodstream. In response to cold stress, the blood flow to BAT increases, indicating a physiological response of heat generation rather than the insulative blood flow reduction related to white adipose tissue (WAT) [22]. While BAT deposits and its role in heat production in humans by non-shivering thermogenesis is well established in the newborn, its role in thermoregulation in the adult has, for many years, been a subject of debate [23]. As actual brown fat deposits in adult humans are only a few grams, Muzik et al [24] showed that BAT thermogenesis only accounts for metabolic energy consumption of <20kcal/day, equivalent to only 2 minutes moderate-intensity running. The important role of mitochondria in the regulation of WAT remodelling and energy balance is increasingly appreciated [22] and browning of white fat is therefore necessary to show a physiological relevant effect on whole body metabolism [25].
Adipose tissue as a body thermal insulator
Subcutaneous fat is an important insulator of heat during cold exposure. Its insulating effect depends on the thickness of the fat layer. Hayward et al [26] performed an experiment comparing the importance of fat thickness to thermoregulatory reflexes in determining the ability to stabilise the body core temperature in cold water. It was concluded that the importance varies in different parts of the body. The thorax was measured to be the main site for heat loss and that the subcutaneous fat accounted for half of the insulation. By contrast, the subcutaneous fat accounted for less than a third of the insulation in the muscular limbs, and only about 3% of insulation in the hands and feet. Total body insulation by unit surface area was closely determined by mean subcutaneous fat thickness, regardless of fat distribution differences among genders [25].
Gender, age and time of day responses to CWI
When body fatness and the body surface area to volume ratio are taken into account, there appears to be no differences in responses to CWI between men and women [27]. However, when comparing gender-specific cold-water responses, Solianic et al [28] found that there was a significant difference in the thermoregulatory response to CWI between men and women. It was observed that men tended to exhibit a greater metabolic response and shivering thermogenesis to CWI, whereas women had a greater insulative response. The cooling rate was similar in both genders.
As Solianic et al. were investigating the differences of CWI between the two genders, it was noted that although the experience of cold stress was similar in men and women, the neuroendocrine and immune responses were larger in men [28].
Another important predictor of how the physiology of our body is influenced by cold is age. Hypothermia still remains one of the leading causes of death among older individuals [29]. A study exploring the difference in thermoregulatory response between old and young individuals observed a higher mean skin temperature in old subjects compared to the younger subjects [30]. This suggests a deficit of thermoregulation, which may contribute to a loss in core temperature and development of hypothermia in older adult. On the other hand in a thermographic study comparing the response to local cooling of the hands and feet in young and elderly subjects, the elderly were found to have lower pre-cooling skin temperatures [9].
Body core temperature in humans has a well-established circadian rhythm, where temperature varies by about 1°C throughout the day, reaching its lowest temperature at night [31]. This raises the possibility that morning CWI may increase the risk of hypothermia because of lower initial core temperature. However, there are no indications of circadian temperature rhythm affecting the thermoregulatory response to CWI in terms of shivering and vasoconstriction [31].
Cold exposure
The Lewis hunting reaction is one of four possible responses to immersion of the hand in cold water [15]. When extremities are immersed in cold water, the peripheral blood vessels alternate between vasoconstriction and vasodilation. The initial response is a vasoconstriction to reduce the heat loss, but this results also in reduced temperature of the extremities. After approximately 5–10 minutes of cold exposure, the sympathetic response causes blood vessels to vasodilate, a process called cold-induced vasodilation (CIVD). The CIVD response is related to a cold-induced decrease of sympathetic activity around the sphincter muscle of the arteriovenous anastomosis. A new phase of vasoconstriction follows the vasodilation, after which the process repeats itself in a cyclic fashion.
Another response observed in the fingers after CWI is that the blood vessel diameter remains constant after an initial phase of vasoconstriction [15]. However, of the vast majority of vascular responses to immersion of the fingers in cold water, the hunting reaction is the most important.
While the genetic component influencing the strength of this response is largely unknown, individuals living or working in cold environments seem to have a well-developed hunting reaction. Krog et al [32] and Leblanc et al found that arctic fishermen and Norwegian Sami had an increased blood flow to the hands in the cold [33]. Also, Nelms and Soper [34] noted a shorter time onset of CIVD in British acclimatised fish filleters working in cold and wet conditions. The genetic influence on the ability to respond to cold temperature is unknown. It has been shown that Inuits recover faster to control temperature values after a CWI of the hand, when compared to arctic Caucasian residents, and especially when compared to individuals from a warmer climate [35]. It is uncertain whether this is caused by a genetic adaptation or an acclimatisation to cold environments. On the other hand, endothelial function and sensory thresholds in the peripheral appendages do not seem to be altered by previous recreational exposure to cold [36].
CWI
This review focuses on cold-water immersions and excludes research regarding exposure to other cold mediums. For example, one of the well-described differences regarding the impact of a medium on heat loss from the skin relates to heat loss in air compared to water. This is related to the fact that heat conduction is superior to convection in terms of temperature exchange to the environment [14]. Heat conductance is about 3.34 times greater in water compared to air, depending largely on the skinfold thickness [37].
With CWI, the body experiences two mechanistically different autonomic responses, namely the cold shock response and the diving response. The diving response is activated by the wetting and cooling of the face- and nostrils while breath holding. This causes a profound sinus bradycardia, peripheral vasoconstriction, inhibition of respiratory neurons, and redirection of blood to vital organs and release of red blood cells stored in the spleen [38]. The cold shock response is a series of reflexes triggered by signals from cutaneous cold thermoreceptors and causes sympathetically mediated tachycardia, respiratory gasping, uncontrollable hyperventilation, peripheral vasoconstriction and hypertension [39]. In a study by Shattock and Tipton, they proposed that this conflict of autonomic response could be a major contributor to the high incidence of cardiac arrhythmias among healthy individuals when immersed in cold water [39].
Without the antagonising autonomic responses to CWIs, the cold shock response in itself can have a major impact on the body and is connected to an increased risk of drowning [40]. In this study, a link was found between the initial respiratory gasping and hyperventilation to a decrease in cerebral blood flow velocity in the middle cerebral artery and was associated with disorientation and loss of consciousness among the participants.
Effects of regular cold-water exposure on different organ systems
The main effects of regular exposure to cold-water are shown in Figure 3 and are described in more detail below
Figure 3.
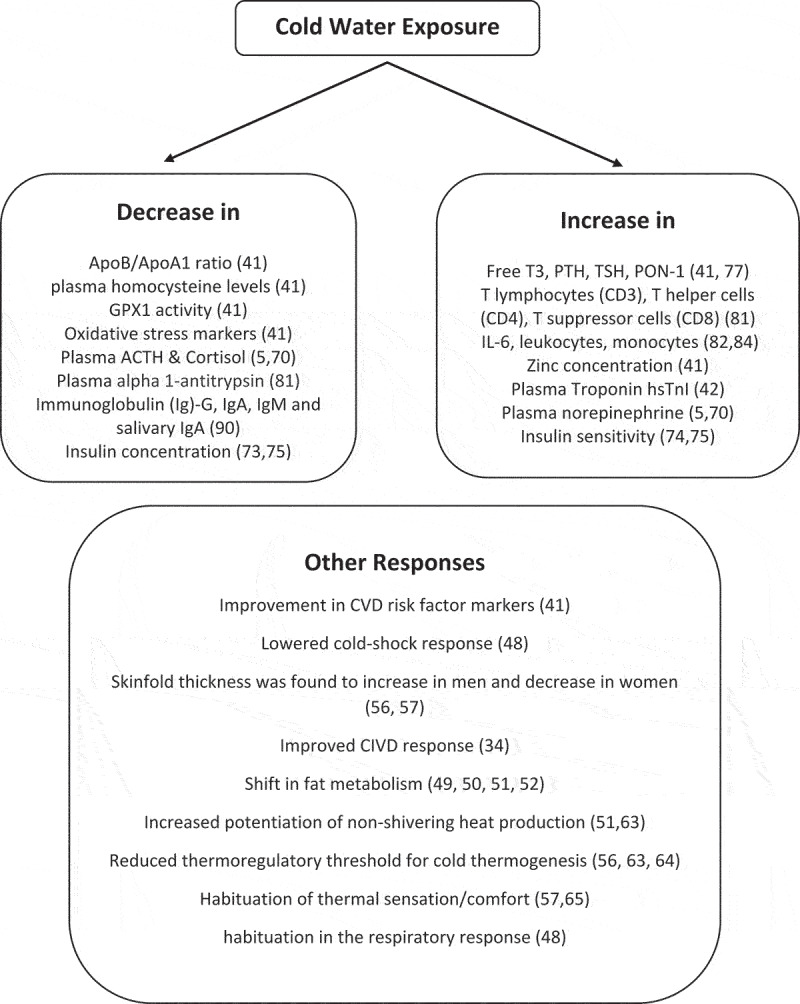
The effects of cold-water exposure on body systems physiology (References in parentheses).
Respiratory and cardiovascular response
There are, as discussed above, some risk factors connected to CWI. The cold shock response initiates an increase in respiratory rate, heart rate, blood pressure and decreases the cerebral blood perfusion. In a study by Lesna et al [41], a group of cold-adapted winter swimmers were investigated and compared to a control group to determine the effect of cold adaptation on cardiovascular risk factors, thyroid hormones and the capacity of humans to reset the damaging effects of oxidative stress. The cold adapted group had a significant reduction in apolipoprotein B/apolipoprotein A1 (ApoB/ApoA1) ratio, plasma homocysteine levels, glutathione peroxidase 1 (GPX1) activity and oxidative stress markers. They also had an increase in triiodothyronine (T3) values, paraoxonase (PON)-1 activity and zinc concentration when compared to the control group. This study demonstrated that cold-adapted individuals showed an improvement in cardiovascular risk factor markers not seen in the non-adapted group. These findings imply a positive cardio-protective effect of regular CWI.
Even though there is evidence of reduced cardiovascular risk factors in cold-adapted subjects, the act of CWI still increases the workload of the heart and thus has a large stress impact on the heart. During a winter swimming competition among elite swimmers, a group of Czech scientists [42] investigated the relationship between swimming in cold water and the following cardiac markers; high-sensitivity troponin I (hsTnI), high-sensitivity troponin T (hsTnT), and aminoterminal pro-brain natriuretic peptide (at-pro-BNP). Blood samples were collected one day before, right after, two hours after and 24 hours after the competition. They found a significant increase in plasma hsTnI concentration two hours after the competition, while hsTnT and at-pro-BNP remained unchanged. Generally, having an elevated level of troponin is associated with a worse overall cardiac prognosis. Although the exercise in cold water caused a release of hsTnI, it is not clear if this is connected to an increased risk of developing acute coronary syndromes. Elevation of troponins is mainly an indication of damage to the cardiac muscle, most commonly caused by a mismatch between oxygen supply and demand [43]. However, high-intensity exercise in thermoneutral environments is also known to cause elevation of troponins [44]. Even when the previous cited study by Lesna [41] shows that adaptation to CWI contributes to an improvement in cardiovascular risk factors, the findings in the study by Baker et [44] could link cold adapted swimmers to an increased risk for coronary syndrome. If cold adaptation causes an increase in troponin, it would be interesting to know what would occur during CWI in non-adapted individuals. More research is therefore necessary to conclude whether CWI is linked to an increased risk of acute coronary syndrome among adapted cold-water swimmers.
Another important factor to evaluate on the effects of regular CWI is its effect on blood pressure. If repeated cold-water immersion causes elevation of blood pressure, this could be linked to several heart conditions, such as ventricular hypertrophy. A group of 28 regular winter swimmers underwent a study to investigate the cardiovascular responses to cold [45]. In this study, clinical examination of the subjects was performed and their medical history was recorded. Most of the subjects were healthy individuals. However, one subject had hypertension (180/105 mmHg) and three subjects had a diastolic pressure of 95 mmHg. A significant increased blood pressure was found in all undressed subjects, while they waited in the cold winter air before CWI. Neither immersion nor swimming in the cold water caused further increase in blood pressure and the pressure returned to control values 4 min after the experience. Electro and vector cardiographic signs remained unchanged among the subjects. No signs of ventricular hypertrophy, cardiovascular or cerebrovascular damage could be detected. Similar findings were also found when a group of healthy men were put through a cold acclimation programme for five weeks [46]. Blood pressure in the subjects increased significantly during the first CWI, but were normal after the cold acclimation program, indicating that an adaptive process had taken place.
With regard to the initial respiratory response to CWI, both experienced and inexperienced cold-water swimmers had a positive effect of acclimatising to CWI [47]. Furthermore, it has been shown that skin cooling through CWI caused a significant habituation in the respiratory response and lowered the cold-shock response [48].
Specific thermoregulative adaptations to regular exposure to cold air and/or cold water exposure
While this review focuses mainly on CWI, it is also relevant to briefly mention how exposure to cold air impacts body physiology since some of the findings in these two different media are similar. Thermal stress due to exposure to cold air has a direct effect on progenitor cell plasticity [49]. Cold adaptation induces BAT biogenesis in adipose tissue. The acute cold stress upregulates thermogenic gene expression through a complex process that requires both β-adrenergic-dependent phosphorylation of S265 and demethylation of H3K9me2 by JMJD1A [50]. This stimulates the formation of BAT with enhanced glucose oxidation, which, as described in section “Shivering and non-shivering thermogenesis” above, is required to maintain thermal homoeostasis in a cold environment. In a recent study on BAT during CWI, it was shown that winter swimmers have a lower core temperature at a thermal comfort state than controls and had no BAT glucose uptake. In addition, winter swimmers have a higher cold-induced thermogenesis than control subjects [51]. Some research suggests that the molecular mechanism of transition between acute and chronic adaptation to cold stress might prove to be a novel molecular target for the treatment of metabolic disorders, via promoting biogenesis of BAT [50]. Although the “browning” of adipose tissue has a positive effect on long-term energy homoeostasis and body-weight regulation, the thermogenic response needs to be maintained to keep these changes in the transition process of fat cells [52].
Adiponectin is a key protein produced by adipose tissue and plays an important role in protecting against insulin resistance, diabetes, atherosclerosis and other age-related diseases [53]. Some research, looking at the plasma adiponectin levels in centenarians and their offspring, suggest that elevated plasma adiponectin levels may promote increased longevity [53]. Cold exposure in air or water seems to increase the production of adiponectin in adipose tissue through the process of shivering and non-shivering thermogenesis [54] and could, as such, be seen as a positive health effect.
Another study looked into the combination of moderate exercise and facial cooling that induced substantial fat loss in men, with an associated ketonuria, proteinuria, and increase of body mass [55]. This was linked to several factors, such as small energy deficit, energy cost of synthesising new lean tissue, energy loss through the storage and excretion of ketone bodies, catecholamine-induced “futile” metabolic cycles with increased resting metabolism and a specific reaction to cold dehydration. The associated mobilisation of free fatty acids suggests the possibility of using winter sport as a pleasant method of treating obesity. The study still recognises the limitations of implementing this as a clinical treatment of weight loss due to possible pathological reactions to cold and the less evident fat mobilisation seen in female patients undergoing winter swimming activities [55]. Gender differences were also found when comparing skinfold thickness to regular CWI. Skinfold thickness was found to increase in men [56] and decrease in women [57].
The effect of local cooling on skin temperature and blood flow in peripheral limbs were studied in a group of 64 men living in an Antarctic environment for 8 weeks [58]. There was a significant fall in skin temperature and an increase in finger blood flow. It was hypothesised, based on these observations, that continuous cold exposure results in vasodilation to prevent cold injuries, such as in the case of the Inuits [35]. This may be regarded as a positive adaptation with positive health effects. Although not included in the results of our original database search, an article comparing substrate utilisation during exercise and shivering during cold water immersion showed that there was a shift from the metabolism of fat during moderate shivering when compared to exercise of an equivalent intensity in air. Hepatic glucose output was higher during exercise in air compared to shivering whereas free fatty acid levels were higher during shivering in water [59].
A cold water immersion study of the hands conducted by LeBlanc et al [33] in fishermen showed that the fishermen maintained a higher finger temperature and complained less of pain as well as a greater heat flow compared to a control group. They suggested that this may increase the dexterity of the limbs in a cold environment, but this may only be possible when the core temperature remains unchanged. If the core temperature decreases, as seen with whole-body immersion in cold water, the acclimatisation causes the opposite effect, with decreased CIVD reaction. Daanen [15] hypothesised that hypothermic acclimatisation leads to reduced CIVD responses due to the reduced body core temperature and that insulative acclimatisation has less impact on CIVD.
Cold acclimatisation through the process of CWI has been shown to alter the onset of metabolic responses to cold [56]. The metabolic response to cold is delayed and subjective shivering attenuated. In the same study, shivering was found to be delayed during CWI by about 40 minutes in winter swimmers compared to the control group, suggesting the importance of non-shivering thermogenesis in early thermogenic response. Because of this induced potentiation of nonshivering heat production in cold-water swimmers, it is hypothesised that CWI increases the thermogenic capacity. This is largely influenced by catecholamine-induced heat production. In a study on metabolic habituation to cold-water immersion it was found that subjects who had repeated deep tissue cooling a habituation of the metabolic response was induced but that repeated skin cooling alone had no effect [60]. Cold acclimation causes increased noradrenaline-induced secretion of glucagon contributing to improved cold tolerance by non-shivering thermogenesis [61].
In cold-adapted winter swimmers, cold thermogenesis is solely related to changes in rectal temperature, indicating the predominance of the central temperature input in activation of heat production mechanisms [62]. This is in contrast to non-cold-adapted controls, where a significant part of cold thermogenesis during the early phase of cooling was induced by changes in peripheral temperature input, while in the late phase of cooling it was the central temperature input, which was mainly engaged in induction of cold thermogenesis. In cold-adapted winter swimmers the thermoregulatory threshold for induction of cold thermogenesis is lowered, but the apparent hypothalamic thermosensitivity remains the same as in non-cold-adapted subjects. These differences indicate an adaptation in the threshold for induction of cold thermogenesis by peripheral vasoconstriction [56,63,64].
Research examining the thermal sensation and thermal comfort associated with regular winter swimming, indicates that thermal sensation and comfort become habituated after a few short-lasting whole-body immersions in cold water [57,65]. This is a temporary change in the cold sensation and regulation lasting some weeks after cessation of cold-water exposure [56,62], meaning that winter swimmers undergo an acclimatisation of thermal sensation and comfort, and not a permanent adaptation. Similar findings were found in a group of Korean-women-divers, called Ama. These women are exposed to regular CWI from a young age, as they dive for pearls. In older cold-water adapted Korean women, the response to cold is heat loss reduction, rather than increased metabolic rate [66]. They also show an increase in resting metabolism, which is speculated to be a shift from shivering to non-shivering thermogenesis [67]. It was found that the acclimatisation of these women divers slowly disappeared after they changed from diving with a thin cotton garment to an insulative diving suit [68].
As a side issue, an important aspect of assessing cold sensation is the level of discomfort. While CWI is pleasurable to some, it is discomforting for many, although, cold pain sensation is difficult to assess both quantitatively and qualitatively [69].
Hormone system
Plasma adrenocorticotropic hormone (ACTH) and cortisol levels seem to decrease significantly after a short time of regular cold-water exposure, probably due to acclimation or adaptation, suggesting that regular cold-water exposure has little effect on stimulating the pituitary-adrenal cortex axis [5,70]. However, the plasma concentration of norepinephrine has a significant increase after each, CWI, even after 3 months of regular CWI. The increase in norepinephrine suggest that it might play a role in pain alleviation [5,70], as well as improving the cold tolerance by non-shivering thermogenesis [71] and insulative peripheral vasoconstriction, as discussed earlier [56,63,64].
While the hormonal changes by CWI in regard to pain alleviation seem to be largely positive [5,70], there is little data regarding the effects on other hormonal systems in the body. Measurements of serum levels of growth hormone, prolactin, follicle-stimulating hormone (FSH) and luteinising hormone (LH) in healthy females indicates an unaltered hormonal balance after regular CWI [72,73], although one study noted an increase in basal prolactin levels in late season winter swimming [73].
As discussed earlier, regular cold-water swimming may have an impact on fat loss in men [55]. The physiological reasons explaining this are not fully understood, although adiponectin secretion by non-shivering thermogenesis may contribute to this [53]. If regular winter swimming leads to increased levels of plasma adiponectin, it would be expected to have a positive impact on insulin resistance, diabetes, atherosclerosis and other age-related diseases. Such findings have been observed in several studies. For example, repeated cold-water immersions during the winter months of both inexperienced and experienced subjects significantly increased insulin sensitivity and decreased insulin concentrations [73–75]. Such could be interpreted as a positive health effect although, it is difficult to predict the clinical implications of this finding.
Leptin is an adipose tissue hormone that maintains homoeostatic control of the adipose tissue mass, and it has been shown that acute and repeated CWI have separate and opposing effects on circulating leptin concentrations in humans [75]. In this study, they reported a reduction in plasma leptin concentration in acute CWI compared to pre-immersion. Although, in another study, this decline was shown to be reduced after regular CWI [76].
When looking at the effect of regular cold-water exposure on parathyroid- and thyroid hormones, a study by Kovaničová et al. suggests that regulation of PTH and thyroid hormones during cold exposure in humans varies by cold acclimatisation level and/or cold stimulus intensity. After 15 min of swimming in ice water, an increase in parathyroid hormone (PTH) and thyroid-stimulating hormone (TSH), as well as free T3, has been reported [41,75]. There were indications of a positive correlation between systemic PTH and nonshivering thermogenesis as shown by whole-body metabolic preference for lipids, as well as increased BAT volume and uncoupling protein 1 (UCP1) content. Increasing the UCP1 content ameliorates BAT function, as it is an important mitochondrial carrier in BAT [77]. It is well established that BAT prefers metabolising lipids as triglycerides and that regular cold-water exposure increases browning of fat [22]. This finding might implicate that elevated PTH is involved in this browning of white adipose tissue.
Neural connectivity and thermal sensation
Little is known about the effect of regular cold-water swimming on the nervous system in humans, although some studies concerning this have been made in animals. For example, a number of cold-shock proteins, including ribonucleic acid (RNA) binding protein (RBM3), are involved in the regeneration of synapses (reassembly of synapses) after cooling, for example, after hibernation [78]. Overexpression of RBM3 resulted in sustained synaptic protection in mice with neurodegenerative disease, as indicated from findings in both prion disease infected mice and Alzheimers mutated mice [78]. If this is applicable to regular CWI in humans, this may enhance cold-shock pathways and potentially function as a protective therapy in neurodegenerative disorders. Also in rats, the combination of mesenchymal stem cell transplantation and cold-water swimming was more effective in functional recovery following peripheral nerve injury than the mesenchymal stem cell transplantation alone [79]. This may be connected to the capacity for synapse regeneration seen in the enhancement of cold-shock pathways [78].
Inflammation and stress
There is an expanding body of evidence linking inflammation with health and disease. It has been shown that centenarians have lower levels of inflammation than community‐living elderly (85‐ to 99‐year‐old) [80]. Arai et al. also showed that although centenarians and their offspring were able to maintain long telomeres, telomere length was not a predictor of successful ageing, whereas a low inflammation score was. CWI increases the metabolic rate and spikes plasma concentrations of catecholamines [5,70], which in turn affects the immune system. Regular CWI has, as mentioned above [41], caused adaptations influencing oxidative stress markers giving some cardio-protective effect.
There are several studies, which have investigated how the immune system responds to regular non-infectious stress stimuli after CWI. For example, in one study [81] involving 6 weeks of regular 1 hour CWI (14°C), increases in plasma concentration of interleukin (IL)-6, total T lymphocytes (CD3), T helper cells (CD4), T suppressor cells (CD8), activated T and B lymphocytes (HLA-DR) were found. In the same study, they found a decrease in the plasma concentration of alpha 1-antitrypsin. In another study, which compared habitual and inexperienced winter swimmers, the authors reported significantly higher concentrations of plasma IL-6, leukocytes and monocytes in winter swimmers compared to inexperienced subjects. This indicates that adaptive mechanisms occur in habitual winter swimmers [82]. In a study investigating the effects of a short-term immersion in cold water following a bout of exercise, IL-6 levels were found to be significantly higher compared to post-exercise rest at room temperature [83]. As increased levels of the cytokine IL-10 are known to be anti-inflammatory [84], it would be interesting to see whether this cytokine is increased during CWI. However, no research on this was found.
There are indications of decreased plasma uric acid concentration, an important plasma antioxidant, following CWI in regular winter swimmers [85]. This is hypothesised to be caused by its consumption after formation of oxygen radicals, which is further supported by the measured increase in erythrocytic level of oxidised glutathione and the ratio of oxidised glutathione to total glutathione following cold exposure. However, the baseline concentration of activated glutathione is increased and the concentration of oxidised glutathione is decreased in the erythrocytes of winter swimmers as compared to those of non-winter swimmers. Similar findings were observed in other studies [86,87]. This is most likely connected to an adaptive response to repeated oxidative stress, or “body hardening”, following cold stress, resulting in increased tolerance to stress [85,88] and could be interpreted as a positive health effect of CWI.
A clinical study of upper respiratory tract infections (URTI) in cold-water swimmers compared to pool swimmers found no significant difference in the prevalence of these infections, although there was some evidence of less URTI in cold-water swimmers compared to non-swimmers [89]. Interestingly, the same study showed that both cold swimmers and pool swimmers who had partners that were non-swimmers, and that the latter had significantly more URTIs than their swimming partners.
Although not strictly within the definitions of CWI as defined by IISA and IWSA [2,3], the effect on the immune system response of long-distance swimming (LDS) in open water with temperatures ranging from 18°C to 21°C has been investigated based on salivary and serum antibody concentration [90]. Kormanovski A et al [84] found that at the end of six months of training, the average pre-exercise levels of serum immunoglobulin (Ig)-G, IgA, IgM and salivary IgA, decreased significantly. In the same study, it was found that there was a significant suppression of pre-exercise serum and salivary antibody levels, although these changes did not affect the resistance of the swimmers to respiratory infections.
Psychology and mental health
Mental health is among the 10 leading causes of disability in both developed and developing countries, and depression is the leading cause of years lost due to disability worldwide, projected to be ranked the number one global burden of disease within 2030 [91]. Even though winter swimming is an exposure to an extreme stress, it is voluntarily practised by many people. It is commonly described as a joyful and positively experienced leisure activity by experienced individuals. One hypothesis proposes that a lifestyle without certain physiological stressors may cause inadequate functioning of the brain and lead to mental health problems, such as depression [92]. The known increases in plasma noradrenaline, beta-endorphin and synaptic release of noradrenaline in the brain due to stress induced by CWI, may therefore have a positive effect on mental health and brain development [92]. In this study, it was hypothesised that the strong afferent input to the brain from the stimulation of cold receptors in the skin during cold-water immersion could result in an anti-depressive effect. The practical testing of the hypothesis indicated that regular cold-water exposure could relieve depressive symptoms rather efficiently. However, the testing did not include a significant number of participants to make a firm conclusion. In a case study concerning a patient who wished to cease medication for a severe post-partum depressive disorder, regular CWI had a remarkable positive effect [93].
The general implication regarding the positive mental health aspect of regular winter swimmers is mostly based on questionnaires. For example, a questionnaires looking into the mental health of regular winter swimmers indicates relieved physical symptoms and positive mood, but no significant difference when compared to a control group [94]. Another questionnaire-based study looked into general well-being and indicated a reduction of tension, fatigue and an improvement in mood and memory in winter swimmers [95]. In addition, the participants reported to be more energetic, active and brisk, compared to the control group. All swimmers in the study who suffered from rheumatism, fibromyalgia or asthma reported that winter swimming relieved pain.
Exercise and cold water
Athletes competing in sports are exposed to physical stress, often multiple times each day, and especially during tournaments where they have to perform many times over a relatively short period of time. CWI could, according to some studies [96–98], play a role in preventing injuries and maintaining performance of athletes, when applied in the recovery period following a bout of exercise. A study by Leeder et al [96] compared competing professional athletes recovering with and without post exercise CWI, and assessed recovery using markers of sprint performance, muscle function, muscle soreness and measured biochemical markers associated with damage (creatine kinase (CK)), inflammation (IL-6 and C-Reactive Protein (CRP)) and oxidative stress (lipid hydroperoxides and activity of lipid-soluble antioxidants). The CWI group was associated with improved recovery time of sprint speed 24 hours post-exercise and an attenuated efflux of CK. The reduction in CK associated with reduced muscle damage may be due to reduced muscle blood flow [97]. Similar findings were found in another study, and may be explained by a decreased muscle metabolic activity without affecting the tissue oxygenation necessary for normal muscle recovery [98].
Negative health effects of cold-water immersion
While this review has concentrated on the possible health benefits of CWI, the possible negative health effects also need to be mentioned. The negative health risks to CWI are complex and include many factors such as age, general health condition, body size/composition, experience, water temperature and immersion duration. These have been dealt with in many previous publications and are discussed in some detail in the narrative review on cold water swimming by Knechtle et al [99]. The effect of accidental immersion in cold-water, particularly in extreme situations such as falling overboard from a boat into very cold water is beyond the scope of this review although, many of the potential negative effects of recreational swimming in cold water are similar. The most prevalent risks are related to cardiorespiratory problems that are often related to the initial cold shock when entering cold water [39,100–102]. The risk of hypothermia and its well-known consequences is very prevalent. Understanding the risk of hypothermia and its consequences are nicely described in a popular article [103]. In more extreme situations, both freezing and non-freezing cold injuries are possible, although these are more common in cold related activities not related to immersion in cold water [104].
Discussion
The main aim of this review was to carry out a detailed search of the scientific literature in order to try and determine whether voluntary exposure to cold water has health effects in humans. The literature research was deliberately restricted to include studies within a strict keyword-based framework. After a strict selection process, the number of studies regarded as being relevant was narrowed down to 104. It has to be recognised that the exclusion criteria used to narrow down the number of relevant studies was based on a subjective evaluation and thus may have caused the exclusion of other relevant research, although due to the selection process for the selected search criteria this is regarded as being unlikely.
While many of the studies demonstrated significant effects of CWI on various physiological and biochemical parameters, the question as to whether these are beneficial or not for health is difficult to assess. One of the problems is that some of the studies involve passive CWI [46,47,52,54,56,58,61,63–65,71,72,76,77,81,85,96–98], while others deal with active CWI [42,45,50,55,57,62,66–68,73–75,79,82,86–90,93–95]. Many of the research studies were based on cold adapted winter swimmers [41,67,68,71,75,77,82,85,86,88–90,94,95]. Other investigations on the beneficial effects of regular CWI were performed on subjects with no previous experience [46,47,52,54,56–58,63–65,69,70,72–74,76,81,87,92,93]. Some research was based on subjects not involved in cold-water swimming, for example, as a post-exercise treatment following sports activities [55,96–98]. However, as mentioned in the introduction and based on the results from this review, many of the health benefits claimed from regular cold exposure may not be causal and may, instead, be explained by other factors including an active lifestyle, trained stress handling, social interactions, as well as a positive mindset. In addition, clear conclusions from the majority of studies was hampered by the fact that they were carried out in small groups, often of one gender, and with differences in exposure temperature and salt composition of the water.
Although approached from different angles in different studies, one positive effect worth highlighting is the effect that CWI has on the reduction and/or transformation of body adipose tissue [49,50,52,55,61,77]. This can be considered to be protective against diabetes [54,74,75] and cardiovascular disease [41,54] and therefore potentially could have prophylactic effects on health. The reported findings regarding the effects of CWI on the immune system, especially concerning tolerance to stress [70,71,81,82,85–88] and respiratory infections [89,90] as a beneficial effect of CWI, are promising. If CWI has a positive effect on health this would be an interesting finding since it would be an intervention not requiring the use of medication, without financial costs. However, new studies are necessary to provide further scientific support for these findings. It is also felt that detailed and well thought out questionnaires concerning individuals’ experiences in relation to CWI, such as those reported in section. Psychology and mental health [94,95], can provide useful indicators for further research topics.
Conclusion
From this review, it is clear that there is increasing scientific support that voluntary exposure to cold water may have some beneficial health effects. However, it is also clear that there is a need for new controlled research studies that are specifically focused on the topic. There are several specific areas regarding the potential preventive health effect of CWI that need further investigation. For example, its effect on the immune system (e.g. tolerance to stress and respiratory infections), potential prophylactic effects on the cardiovascular system and prophylaxis against insulin resistance and improved insulin sensitivity and mental health, are areas that are promising and warrant further investigation. In addition, the educational aspects in respect to both carrying out this activity in a responsible way and learning more about specific beneficial effects also need addressing. In conclusion, it would seem that the question proposed in the introduction to this review concerning the health effects of CWI, based on the published scientific literature described above, has only been partly answered. Until we have more concrete scientific evidence the topic will continue to be a subject of debate.
Acknowledgments
The authors wish to thank senior Academic Librarian Eirik Reierth, Faculty of Health Sciences, UiT The Arctic University of Norway for assistance in carrying out the detailed research of the scientific literature.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Abbreviations
| ACTH | Adrenocorticotropic hormone |
| ApoB | Apolipoprotein B |
| ApoA1 | Apolipoprotein A1 |
| at-pro-BNP | Aminoterminal pro-brain natriuretic peptide |
| AVA | Arteriovenous anastomosis |
| BAT | Brown adipose tissue |
| CD | Cluster of differentiation |
| CIVD | Cold induced vasodilation |
| CK | Creatine Kinase |
| CRP | C-reactive protein |
| CWI | Cold-water immersion |
| DIRT | Dynamic infrared thermography |
| FSH | Follicle-stimulating hormone |
| GPX1 | Glutathione peroxidase 1 |
| HLA-DR | Human Leukocyte Antigen-DR isotype |
| hsTnI | High sensitivity troponin I |
| hsTnT | High sensitivity troponin T |
| Ig | Immunoglobulin |
| IISA | The International Ice Swimming Associations |
| IL | Interleukin |
| IWSA | The International Winter Swimming Association |
| LDS | Long distance swimming |
| LH | Luteinizing hormone |
| PON-1 | Paraoxonase-1 |
| PTH | Parathyroid hormone |
| RBM3 | RNA binding protein 3 |
| RNA | Ribonucleic acid |
| T3 | Triiodothyronine |
| TSH | Thyroid-stimulating hormone |
| UCP1 | Uncoupling protein 1 |
| URTI | Upper respiratory tract infections |
| WAT | White adipose tissue |
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- [1].Wikipedia. Winter swimming. wikipediaorg. 2020. .
- [2].The International Ice Swimming Asssociation, Rules and Regulations. 2021. https://internationaliceswimming.com/wp-content/uploads/2021/08/IISA-Swimming-Rules-and-Regulations-Aug-2021.pdf.
- [3].International Winter Swimming Association Water Classification. 2019. https://iwsa.world/water-classification/.
- [4].Hsaio A. 6 amazing health benefits of cold water swimming. Lifehack. https://www.lifehack.org/288238/6-amazing-health-benefits-cold-water-swimming. [Google Scholar]
- [5].Leppaluoto J, Westerlund T, Huttunen P, et al. Effects of long-term whole-body cold exposures on plasma concentrations of ACTH, beta-endorphin, cortisol, catecholamines and cytokines in healthy females. Scand J Clin Lab Invest. 2008;68(2):145–16. [DOI] [PubMed] [Google Scholar]
- [6].Berbee JF, Boon MR, Khedoe PP, et al. Brown fat activation reduces hypercholesterolaemia and protects from atherosclerosis development. Nat Commun. 2015;6(1):6356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Bøkenes L, Alexandersen TE, Østerud B, et al. Physiological and haematological responses to cold exposure in the elderly. Int J Circumpolar Health. 2000;59(3–4):216–221. [PubMed] [Google Scholar]
- [8].Tipton MJ, Collier N, Massey H, et al. Cold water immersion: kill or cure? Exp Physiol. 2017;102(11):1335–1355. [DOI] [PubMed] [Google Scholar]
- [9].Rasmussen L, Mercer J. A comparison of thermal responses in hands and feet of young and elderly subjects in response to local cooling as determined by infared imaging. Thermol Int. 2004;14:71–76. [Google Scholar]
- [10].Stikkbakke, Einar, Mercer, James B. An infrared thermographic and Laser Doppler flowmetric investigation of skin perfusion in the forearm and finger tip following a short period of vascular stasis. Thermology International. 2008. ;18:107–111 . [Google Scholar]
- [11].Nielsen SB, Mercer J. Dynamic thermography in vascular finger disease A methodological study of arteriovenous anastomoses. Thermol Int. 2010;20:93–99. [Google Scholar]
- [12].Lossius K, Eriksen M, Walløe L. Fluctuations in blood flow to acral skin in humans: connection with heart rate and blood pressure variability. J Physiol. 1993;460(1):641–655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Miland ÅO, Mercer JB. Effect of a short period of abstinence from smoking on rewarming patterns of the hands following local cooling. Eur J Appl Physiol. 2006;98(2):161–168. [DOI] [PubMed] [Google Scholar]
- [14].Hohenauer E, Deliens T, Clarys P, et al. Perfusion of the skin’s microcirculation after cold-water immersion (10°C) and partial-body cryotherapy (−135°C). Skin Res Technol. 2019;25(5):677–682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Daanen HA. Finger cold-induced vasodilation: a review. Eur J Appl Physiol. 2003;89(5):411–426. [DOI] [PubMed] [Google Scholar]
- [16].Kenny GP, Denis PM, Proulx CE, et al. The effect of dynamic exercise on resting cold thermoregulatory responses measured during water immersion. Eur J Appl Physiol Occup Physiol. 1999;79(6):495–499. [DOI] [PubMed] [Google Scholar]
- [17].Haman F, Blondin DP. Shivering thermogenesis in humans: origin, contribution and metabolic requirement. Temperature (Austin). 2017;4(3):217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Mercer, James B. Hypothermia and Cold Injuries in Man Blatteis, Clark M. Editor. Physiology and pathophysiology of temperature regulation (Singapore.New Jersey.London.Hong Kong: World Scientific; ). 1998:246–257 . [Google Scholar]
- [19].Norheim AJ, Borud E, Wilsgaard T, et al. Variability in peripheral rewarming after cold stress among 255 healthy Norwegian army conscripts assessed by dynamic infrared thermography. Int J Circumpolar Health. 2018;77(1):1536250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Swift RW. The effects of low environmental temperature upon metabolism: II. the influence of shivering, subcutaneous fat, and skin temperature on heat production. J Nutr. 1932;5(3):227–249. [Google Scholar]
- [21].Martin S, Cooper KE. Factors which affect shivering in man during cold water immersion. Pflügers Archiv. 1981;391(1):81–83. [DOI] [PubMed] [Google Scholar]
- [22].Muzik O, Mangner TJ, Leonard WR, et al. Sympathetic innervation of cold-activated brown and white fat in lean young adults. J Nucl Med. 2017;58(5):799–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Gilsanz V, Hu HH, Kajimura S. Relevance of brown adipose tissue in infancy and adolescence. Pediatr Res. 2013;73(1):3–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Muzik O, Mangner TJ, Granneman JG. Assessment of oxidative metabolism in brown fat using PET imaging. Front Endocrinol (Lausanne). 2012;3:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Heinonen I, Laukkanen JA. Effects of heat and cold on health, with special reference to Finnish sauna bathing. Am J Physiol Regul Integr Comp Physiol. 2018;314(5):R629–r38. [DOI] [PubMed] [Google Scholar]
- [26].Hayward MG, Keatinge WR. Roles of subcutaneous fat and thermoregulatory reflexes in determining ability to stabilize body temperature in water. J Physiol. 1981;320(1):229–251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Glickman-Weiss EL, Cheatham C, Caine N, et al. The influence of gender and menstrual phase on thermosensitivity during cold water immersion. Aviat Space Environ Med. 2000;71(7):715–722. [PubMed] [Google Scholar]
- [28].Solianik R, Skurvydas A, Vitkauskienė A, et al. Gender-specific cold responses induce a similar body-cooling rate but different neuroendocrine and immune responses. Cryobiology. 2014;69(1):26–33. [DOI] [PubMed] [Google Scholar]
- [29].Reingardiene D. Hypothermia. Medicina (Kaunas). 2003;39(1):90–97. [PubMed] [Google Scholar]
- [30].Potkanowicz ES, Caine-Bish N, Otterstetter R, et al. Age effects on thermal, metabolic, and perceptual responses to acute cold exposure. Aviat Space Environ Med. 2003;74(11):1157–1162. [PubMed] [Google Scholar]
- [31].Castellani JW, Young AJ, Kain JE, et al. Thermoregulatory responses to cold water at different times of day. J Appl Physiol. 1999;87(1):243–246. Bethesda, Md: 1985. [DOI] [PubMed] [Google Scholar]
- [32].Krog J, Folkow B, Fox RH, et al. Hand circulation in the cold of Lapps and North Norwegian fishermen. J Appl Physiol. 1960;15(4):654–658. [DOI] [PubMed] [Google Scholar]
- [33].LeBlanc J, Hildes JA, Héroux O. Tolerance of Gaspé fishermen to cold water. J Appl Physiol. 1960;15(6):1031–1034. [DOI] [PubMed] [Google Scholar]
- [34].Nelms JD, Soper DJG. Cold vasodilatation and cold acclimatization in the hands of British fish filleters. J Appl Physiol. 1962;17(3):444–448. [DOI] [PubMed] [Google Scholar]
- [35].Livingstone SD, Grayson J, Reed LD, et al. Effect of a local cold stress on peripheral temperatures of Inuit, Oriental, and Caucasian subjects. Can J Physiol Pharmacol. 1978;56(5):877–881. [DOI] [PubMed] [Google Scholar]
- [36].Eglin CM, Costello JT, Tipton MJ, et al. Previous recreational cold exposure does not alter endothelial function or sensory thermal thresholds in the hands or feet. Exp Physiol. 2021;106(1):328–337. [DOI] [PubMed] [Google Scholar]
- [37].Smith RM, Hanna JM. Skinfolds and resting heat loss in cold air and water: temperature equivalence. J Appl Physiol. 1975;39(1):93–102. [DOI] [PubMed] [Google Scholar]
- [38].Lindholm P, Lundgren CE. The physiology and pathophysiology of human breath-hold diving. J Appl Physiol. 2009;106(1):284–292. [DOI] [PubMed] [Google Scholar]
- [39].Shattock MJ, Tipton MJ. Autonomic conflict’: a different way to die during cold water immersion? J Physiol. 2012;590(14):3219–3230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Mantoni T, Belhage B, Pedersen LM, et al. Reduced cerebral perfusion on sudden immersion in ice water: a possible cause of drowning. Aviat Space Environ Med. 2007;78(4):374–376. [PubMed] [Google Scholar]
- [41].Kralova Lesna I, Rychlikova J, Vavrova L, et al. Could human cold adaptation decrease the risk of cardiovascular disease? J Therm Biol. 2015;52:192–198. [DOI] [PubMed] [Google Scholar]
- [42].Broz P, Rajdl D, Racek J, et al. Relationship between cold water swimming and increased cardiac markers: a pilot study. Klin Biochem Metab. 2017;25:27–31. [Google Scholar]
- [43].Stark Matthew , Kerndt, Connor C., Sharma , Sandeep. Troponin StatPearls [Internet]. 2022. Updated 2020 Jul 10 https://www.ncbi.nlm.nih.gov/books/NBK507805/. updated 2022 May 8.
- [44].Baker P, Leckie T, Harrington D, et al. Exercise-induced cardiac troponin elevation: an update on the evidence, mechanism and implications. Int J Cardiol Heart Vasc. 2019;22:181–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Zenner RJ, De Decker DE, Clement DL. Blood-pressure response to swimming in ice-cold water. Lancet. 1980;1(8160):120–121. [DOI] [PubMed] [Google Scholar]
- [46].Muza SR, Young AJ, Sawka MN, et al. Respiratory and cardiovascular responses to cold stress following repeated cold water immersion. Undersea Biomed Res. 1988;15(3):165–178. [PubMed] [Google Scholar]
- [47].Mantoni T, Rasmussen JH, Belhage B, et al. Voluntary respiratory control and cerebral blood flow velocity upon ice-water immersion. Aviat Space Environ Med. 2008;79(8):765–768. [DOI] [PubMed] [Google Scholar]
- [48].Tipton MJ, Mekjavic IB, Eglin CM. Permanence of the habituation of the initial responses to cold-water immersion in humans. Eur J Appl Physiol. 2000;83(1):17–21. [DOI] [PubMed] [Google Scholar]
- [49].Chen Y, Ikeda K, Yoneshiro T, et al. Thermal stress induces glycolytic beige fat formation via a myogenic state. Nature. 2019;565(7738):180–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Abe Y, Fujiwara Y, Takahashi H, et al. Histone demethylase JMJD1A coordinates acute and chronic adaptation to cold stress via thermogenic phospho-switch. Nat Commun. 2018;9(1):1566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Søberg S, Löfgren J, Philipsen FE, et al. Altered brown fat thermoregulation and enhanced cold-induced thermogenesis in young, healthy, winter-swimming men. Cell Reports Medicine. 2021;2(10):100408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Jankovic A, Golic I, Markelic M, et al. Two key temporally distinguishable molecular and cellular components of white adipose tissue browning during cold acclimation. J Physiol. 2015;593(15):3267–3280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Atzmon G, Pollin TI, Crandall J, et al. Adiponectin levels and genotype: a potential regulator of life span in humans. J Gerontol A Biol Sci Med Sci. 2008;63(5):447–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [54].Imbeault P, Dépault I, Haman F. Cold exposure increases adiponectin levels in men. Metabolism. 2009;58(4):552–559. [DOI] [PubMed] [Google Scholar]
- [55].Shephard RJ. Adaptation to exercise in the cold. Sports medicine. (Auckland, NZ). 1985;2(1):59–71. [DOI] [PubMed] [Google Scholar]
- [56].Janský L, Janáková H, Uličný B, et al. Changes in thermal homeostasis in humans due to repeated cold water immersions. Pflügers Archiv. 1996;432(3):368–372. [DOI] [PubMed] [Google Scholar]
- [57].Smolander J, Mikkelsson M, Oksa J, et al. Thermal sensation and comfort in women exposed repeatedly to whole-body cryotherapy and winter swimming in ice-cold water. Physiol Behav. 2004;82(4):691–695. [DOI] [PubMed] [Google Scholar]
- [58].Naidu M, Sachdeva U. Effect of local cooling on skin temperature and blood flow of men in Antarctica. Int J Biometeorol. 1993;37(4):218–221. [DOI] [PubMed] [Google Scholar]
- [59].Tipton MJ, Franks GM, Meneilly GS, et al. Substrate utilisation during exercise and shivering. Eur J Appl Physiol Occup Physiol. 1997;76(1):103–108. [DOI] [PubMed] [Google Scholar]
- [60].Tipton MJ, Wakabayashi H, Barwood MJ, et al. Habituation of the metabolic and ventilatory responses to cold-water immersion in humans. J Therm Biol. 2013;38(1):24–31. [DOI] [PubMed] [Google Scholar]
- [61].Kuroshima A. Regulation of thermoregulatory thermogenesis. [Hokkaido Igaku Zasshi] the Hokkaido Journal of Medical Science. 1995;70(1):1–8. [PubMed] [Google Scholar]
- [62].Vybíral S, Lesná I, Jansky L, et al. Thermoregulation in winter swimmers and physiological significance of human catecholamine thermogenesis. Exp Physiol. 2000;85(3):321–326. [PubMed] [Google Scholar]
- [63].Janský L. Physiologic basis of human adaptation to cold. Ceskoslovenska Fysiologie. 2003;52(3):107–117. [PubMed] [Google Scholar]
- [64].Elkington EJ. Finger blood flow in Antarctica. J Physiol. 1968;199(1):1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Geurts CL, Sleivert GG, Cheung SS. Central and peripheral factors in thermal, neuromuscular, and perceptual adaptation of the hand to repeated cold exposures. Appl Physiol Nutr Metab = Physiologie Appliquee, Nutrition Et Metabolisme. 2006;31(2):110–117. [DOI] [PubMed] [Google Scholar]
- [66].Park J, Kim S, Kim DH, et al. Whole-body cold tolerance in older Korean female divers “haenyeo” during cold air exposure: effects of repetitive cold exposure and aging. Int J Biometeorol. 2018;62(4):543–551. [DOI] [PubMed] [Google Scholar]
- [67].Glickman EI, Caine-Bish N. Changes in body temperature and basal metabolic rate of the ama—A commentary. Wilderness Environ Med. 2003;14(3):191–192. [DOI] [PubMed] [Google Scholar]
- [68].Park YS, Rennie DW, Lee IS, et al. Time course of deacclimatization to cold water immersion in Korean women divers. J Appl Physiol Respir Environ Exerc Physiol. 1983;54(6):1708–1716. [DOI] [PubMed] [Google Scholar]
- [69].Lundgren P, Henriksson O, Kuklane K, et al. Validity and reliability of the cold discomfort scale: a subjective judgement scale for the assessment of patient thermal state in a cold environment. J Clin Monit Comput. 2014;28(3):287–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Huttunen P, Rintamäki H, Hirvonen J. Effect of regular winter swimming on the activity of the sympathoadrenal system before and after a single cold water immersion. Int J Circumpolar Health. 2001;60(3):400–406. [PubMed] [Google Scholar]
- [71].Kauppinen K, Pajari-Backas M, Volin P, et al. Some endocrine responses to sauna, shower and ice water immersion. Arct Med Res. 1989;48(3):131–139. [PubMed] [Google Scholar]
- [72].Smolander J, Leppäluoto J, Westerlund T, et al. Effects of repeated whole-body cold exposures on serum concentrations of growth hormone, thyrotropin, prolactin and thyroid hormones in healthy women. Cryobiology. 2009;58(3):275–278. [DOI] [PubMed] [Google Scholar]
- [73].Hermanussen M, Jensen F, Hirsch N, et al. Acute and chronic effects of winter swimming on LH, FSH, prolactin, growth hormone, TSH, cortisol, serum glucose and insulin. Arct Med Res. 1995;54(1):45–51. [PubMed] [Google Scholar]
- [74].Gibas-Dorna M, Chęcińska Z, Korek E, et al. Cold water swimming beneficially modulates insulin sensitivity in middle-aged individuals. J Aging Phys Act. 2016;24(4):547–554. [DOI] [PubMed] [Google Scholar]
- [75].Gibas-Dorna M, Checinska Z, Korek E, et al. Variations in leptin and insulin levels within one swimming season in non-obese female cold water swimmers. Scand J Clin Lab Invest. 2016;76(6):486–491. [DOI] [PubMed] [Google Scholar]
- [76].Zeyl A, Stocks JM, Taylor NA, et al. Interactions between temperature and human leptin physiology in vivo and in vitro. Eur J Appl Physiol. 2004;92(4–5):571–578. [DOI] [PubMed] [Google Scholar]
- [77].Kovaničová Z, Kurdiová T, Baláž M, et al. Cold exposure distinctively modulates parathyroid and thyroid hormones in cold-acclimatized and non-acclimatized humans. Endocrinology. 2020;161(7). DOI: 10.1210/endocr/bqaa051. [DOI] [PubMed] [Google Scholar]
- [78].Peretti D, Bastide A, Radford H, et al. RBM3 mediates structural plasticity and protective effects of cooling in neurodegeneration. Nature. 2015;518(7538):236–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Yang CC, Wang J, Chen SC, et al. Enhanced functional recovery from sciatic nerve crush injury through a combined treatment of cold-water swimming and mesenchymal stem cell transplantation. Neurol Res. 2015;37(9):816–826. [DOI] [PubMed] [Google Scholar]
- [80].Arai Y, Martin-Ruiz CM, Takayama M, et al. Inflammation, but not telomere length, predicts successful ageing at extreme old age: a longitudinal study of semi-supercentenarians. EBioMedicine. 2015;2(10):1549–1558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [81].Janský L, Pospísilová D, Honzová S, et al. Immune system of cold-exposed and cold-adapted humans. Eur J Appl Physiol Occup Physiol. 1996;72(5–6):445–450. [DOI] [PubMed] [Google Scholar]
- [82].Dugué B, Leppänen E. Adaptation related to cytokines in man: effects of regular swimming in ice-cold water. Clin Physioly (Oxford, England). 2000;20(2):114–121. [DOI] [PubMed] [Google Scholar]
- [83].Pawłowska M, Mila-Kierzenkowska C, Boraczyński T, et al. The effect of submaximal exercise followed by short-term cold-water immersion on the inflammatory state in healthy recreational athletes: a cross-over study. J Clin Med. 2021;10(18):4239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [84].Kessler B, Rinchai D, Kewcharoenwong C, et al. Interleukin 10 inhibits pro-inflammatory cytokine responses and killing of Burkholderia pseudomallei. Sci Rep. 2017;7(1):42791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [85].Siems WG, van Kuijk Fj, Maass R, et al. Uric acid and glutathione levels during short-term whole body cold exposure. Free Radic Biol Med. 1994;16(3):299–305. [DOI] [PubMed] [Google Scholar]
- [86].Mila-Kierzenkowska C, Woźniak A, Boraczyński T, et al. Thermal stress and oxidant–antioxidant balance in experienced and novice winter swimmers. J Therm Biol. 2012;37(8):595–601. [DOI] [PubMed] [Google Scholar]
- [87].Lubkowska A, Dołęgowska B, Szyguła Z, et al. Winter-swimming as a building-up body resistance factor inducing adaptive changes in the oxidant/antioxidant status. Scand J Clin Lab Invest. 2013;73(4):315–325. [DOI] [PubMed] [Google Scholar]
- [88].Siems WG, Brenke R, Sommerburg O, et al. Improved antioxidative protection in winter swimmers. Qjm. 1999;92(4):193–198. [DOI] [PubMed] [Google Scholar]
- [89].Collier N, Massey HC, Lomax M, et al. Cold water swimming and upper respiratory tract infections. Extrem Physiol Med. 2015;4(1):A36. [Google Scholar]
- [90].Kormanovski A, Ibarra F, Padilla E, et al. Resistance to respiratory illness and antibody response in open water swimmers during training and long distance swims. Int J Med Med Sci. 2010;2:80–87. [Google Scholar]
- [91].Malhi, Gin S., Mann, J. John, et al. Depression. Lancet. 2010. 392 2299–2312. doi: 10.1016/S0140-6736(18)31948-2. [DOI] [PubMed] [Google Scholar]
- [92].Shevchuk NA. Adapted cold shower as a potential treatment for depression. Med Hypotheses. 2008;70(5):995–1001. [DOI] [PubMed] [Google Scholar]
- [93].van Tulleken C, Tipton M, Massey H, et al. Open water swimming as a treatment for major depressive disorder. BMJ Case Rep. 2018;2018. DOI: 10.1136/bcr-2018-225007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [94].Lindeman S, Hirvonen J, Joukamaa M. Neurotic psychopathology and alexithymia among winter swimmers and controls–a prospective study. Int J Circumpolar Health. 2002;61(2):123–130. [DOI] [PubMed] [Google Scholar]
- [95].Huttunen P, Kokko L, Ylijukuri V. Winter swimming improves general well-being. Int J Circumpolar Health. 2004;63(2):140–144. [DOI] [PubMed] [Google Scholar]
- [96].Leeder JDC, Godfrey M, Gibbon D, et al. Cold water immersion improves recovery of sprint speed following a simulated tournament. Eur J Sport Sci. 2019;19(9):1166–1174. [DOI] [PubMed] [Google Scholar]
- [97].Mawhinney C, Jones H, Joo CH, et al. Influence of cold-water immersion on limb and cutaneous blood flow after exercise. Med Sci Sports Exerc. 2013;45(12):2277–2285. [DOI] [PubMed] [Google Scholar]
- [98].Ihsan M, Watson G, Lipski M, et al. Influence of postexercise cooling on muscle oxygenation and blood volume changes. Med Sci Sports Exerc. 2013;45(5):876–882. [DOI] [PubMed] [Google Scholar]
- [99].Knechtle B, Waśkiewicz Z, Sousa CV, et al. Cold water swimming-benefits and risks: a narrative review. Int J Environ Res Public Health. 2020;17(23):8984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [100].Keatinge WR, Evans M. The respiratory and cardiovascular response to immersion in cold and warm water. Q J Exp Physiol. 1961;46(1):83–94. [DOI] [PubMed] [Google Scholar]
- [101].Mekjavić IB, La Prairie A, Burke W, et al. Respiratory drive during sudden cold water immersion. Respiration Physiol. 1987;70(1):121–130. [DOI] [PubMed] [Google Scholar]
- [102].Tipton MJ. The initial responses to cold-water immersion in man. Clin sci. 1989;77(6):581–588. [DOI] [PubMed] [Google Scholar]
- [103].Radford Imogen, Harper, Mark, Rew, Kate. Understanding hypothermia. The Outdoor Swimming Society https://www.outdoorswimmingsociety.com/understanding-hypothermia/. [Google Scholar]
- [104].Heil K, Thomas R, Robertson G, et al. Freezing and non-freezing cold weather injuries: a systematic review. Br Med Bull. 2016;117(1):79–93. [DOI] [PubMed] [Google Scholar]


