Abstract
Introduction
The use of high-flow nasal oxygen (HFNO) is a simple method that can reduce intubation in patients with hypoxemic acute respiratory failure (ARF). Early and prolonged prone position has demonstrated benefits on mortality in mechanically ventilated patients and on intubation in awake patients with ARF. However, strategies to achieve adherence to awake prone positioning (APP) have not been previously described.
Case and outcomes
We present six patients with ARF due to COVID-19 treated with HFNO and APP. The median (p25–75) of PaFiO2 upon admission was 121 (112–175). The average duration of APP on the first day was 16 h (SD 5 h). Duration (median p25–75) in APP for the following 20 days was 13 (10–18) h/day. Several strategies such as the presence of a health care team, recreational activities, adaptation of the circadian rhythm, oral nutritional support, and analgesics were used to improve prone tolerance. None of the patients suffered from delirium, all were ambulating on discharge from the ICU and none require intubation.
Conclusion
The case series presented show the feasibility of prolonged use of HFNO and APP in patients with COVID-19 and severe persistent hypoxemia and described strategies to enhance adherence.
Keywords: acute respiratory failure, awake prone positioning, adherence, COVID-19, endotracheal intubation
INTRODUCTION
SARV-CoV-2 infection triggers an immune response that manifests itself clinically in different ways, from mild respiratory symptoms to the development of acute hypoxemic respiratory failure and acute respiratory distress syndrome (ARDS), which may require invasive mechanical ventilation (IMV). In the light of the risks associated with IMV, several studies have assessed the role of a non-invasive approach in this scenario. The use of high-flow nasal oxygen (HFNO) could reduce the need for intubation compared to supplemental oxygen in subjects with ARF [1]. In COVID-19, the use of HFNO has gained popularity for being a simple method, easy to implement and well tolerated by patients, which allows the delivery of high fractions of humidified oxygen, thus improving efficiency and ventilatory pattern. However, at the onset of the pandemic its application was limited due to the potential risk of aerosolization and infection of health care personnel, as well as the possible delay in intubation and development of self-inflicted lung injury (P-SILI) [2]. Early and prolonged prone positioning is one of the techniques that has shown to reduce mortality in patients with moderate to severe ARDS on IMV [3]. This benefit can be attributed to a combination of alveolar recruitment with a more homogeneous ventilation distribution, the improvement of the ventilation-to-perfusion ratio (V/Q) and the reduction of ventilator-induced lung injury [4]. In patients with ARF due to COVID-19 who ventilate spontaneously, prone positioning substantially improved overall V/Q matching mainly through decreased dead space, although this effect was lost after reverting to the supine position [5]. Recently a meta-trial by Ehrmann et al. [6] performed in six countries demonstrated that awake prone positioning (APP) in combination with HFNO reduced the need for intubation or death [6]; however, subsequent published studies demonstrated low adherence to APP. The objective of this descriptive study (case series) was to describe the strategies used to achieve prolonged APP in a group of severely hypoxemic patients with HFNO.
CASE AND RESULTS
The four institutions involved in this study implemented a protocol of HFNO and APP on adult patients (>17 years) with ARF during the COVID-19 pandemic. The Internal Review Board from the four centers approved the study and written informed consent was obtained from all the patients for publication while preserving their identity. The criteria to start using this therapy were: (i) supplemental oxygen requirement >35% for oxygen saturation by pulse oximetry (SpO2) >90%, or (ii) increased work of breathing (WoB) assessed through recruitment of respiratory accessory muscles, or (iii) respiratory rate (RR) >30 respirations per minute (rpm). Intubation criteria were RR >30 for more than 5 min, increased WoB at rest, SpO2 < 90% despite FiO2 100%, the logarithm of the reciprocal of hydrogen ion concentration in gram atoms per liter (ph) < 7.25, hemodynamic instability or deterioration of neurological status. The HFNO was initially set at 60 L/min and FiO2 was that required for a target of SpO2 >90%. Weaning from HFNO was performed by initially decreasing FiO2 and flow until ≤40 with SpO2 >92%. To describe the characteristics of the patients, the numerical variables are presented as mean or median with their dispersion measures (standard deviation or 25%–75% percentiles, respectively) according to the normal distribution or not and categorical variables such as absolute frequency (n) and percentage (%). Every test was two-sided, and a P value <0.05 was considered statistically significant. All analyses were performed with STATA version 15.1.
Characteristics and outcomes of the whole population have been published elsewhere [7] and included 335 patients. A small subgroup of six patients required HFNO and APP for very prolonged periods due to persistent hypoxemia. Table 1 shows the patients’ characteristics. The median (p25–75) of Pa/FiO2 upon admission was 121 (112–175). The mean duration on prone position on the first day was 16 h (SD 5). Duration (median (p25–75)) in APP for the following 20 days was 13 (10–18) h/day.
TABLE 1.
Patient’s characteristics
| Patient | Sex | Age | BMI | Frailty | LDH | CRP | Ferritin | Days HFNO | Days APP | Analgesia | Dexme | Delirium | Discharge with O2 | Ambu-late |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| P1 | M | 37 | 30.5 | 2.well | 682 | 17 | 4186 | 32 | 34 | YES | YES | NO | YES | YES |
| P2 | M | 66 | 31 | 2.well | 252 | 114 | 3610 | 24 | 20 | NO | YES | NO | YES | YES |
| P3 | F | 35 | 29.7 | 2.well | 250 | 28 | 124 | 20 | 15 | YES | YES | NO | YES | YES |
| P4 | M | 41 | 36.7 | 3.managing well | 404 | 121 | 841 | 21 | 20 | NO | NO | NO | NO | YES |
| P5 | M | 82 | 32.9 | 4. vulnerable | 345 | 205 | 889 | 20 | 20 | NO | NO | NO | NO | YES |
| P6 | M | 53 | 34.6 | 1.very fit | 828 | 149 | 26 | 29 | NO | NO | NO | YES | YES |
Note: Characteristics of patients included in the case studies. Frailty was assessed through the Rockwood clinical frailty scale. BMI = body mass index; LDH = lactate dehydrogenase; CRP = C-reactive protein; HFNO = high-flow nasal oxygen; APP = awake prone position.
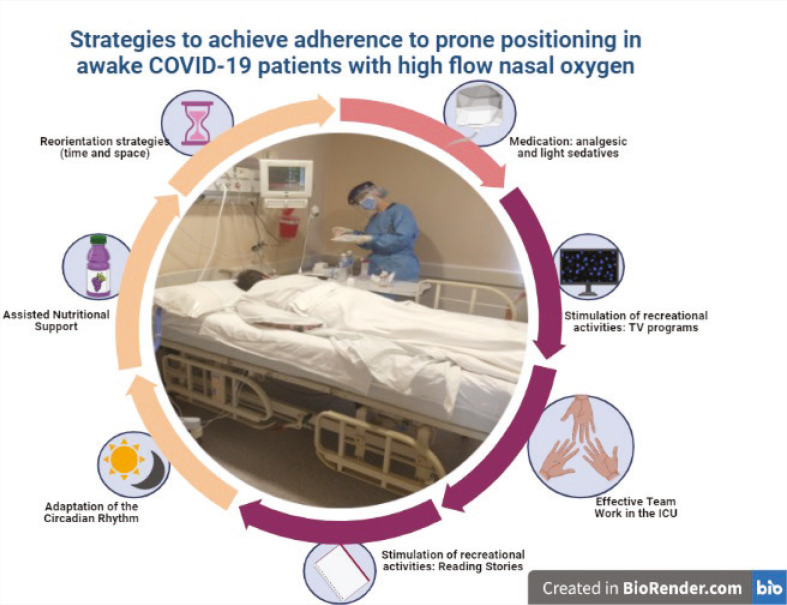
Patients were instructed to maintain the prone positioning for as many hours as possible, minimizing movements in bed to avoid episodes of desaturation and increased WoB. Continuously infused analgesics and light sedatives (fentanyl and dexmedetomidine, respectively) were used to improve prone tolerance. Codeine was utilized to limit coughing. They also received bladder catheterization and assisted feeding with textured modified diet and oral nutritional support with four hypercaloric and hyperproteinic liquid supplements per day to reduce the effort associated with ingestion and, thus, the impact on energy expenditure and dyspnea during APP. Among other relevant measures implemented were the adaptation of the circadian rhythm, the continuous monitoring of body temperature, assistance in daily activities, and the stimulation of recreational activities such as reading stories, positioning to watch TV, and the presence of the health team trained for this approach. The respiratory therapists assisted in the clearance of nostrils which, despite active humidification, often had plugs with hematic secretions as a result of mucosal lesions. They also assessed pain and delirium with validated tools. When changing position (from prone to lateral decubitus), a reservoir mask was placed above the HFNO on those with FiO2 100% to prevent desaturation. All these measures were intended to promote patient adherence to prone position for prolonged periods of time (Figure 1).
FIGURE 1.
Strategies to achieve adherence to awake prone positioning.
Presence of health care team, recreational activities, adaptation of the circadian rhythm, oral nutritional support, and analgesics.
A large variability of the ROX index was observed not only during the first hours of treatment, but also during the following days (Figure 2). These measures aimed at prolonging tolerance to prone positioning may cause complications such as catheter displacement, bradycardia due to the drugs used or urinary tract infection, among others; therefore, close monitoring of these patients is recommended. In this case series, we did not record any relevant adverse effects; none suffered delirium and all of them were ambulating on discharge from the ICU, they also did not require intubation or IMV.
FIGURE 2.
ROX index.
Daily ROX index of patients included in the case studies. The red line represents a ROX index value of 5. ROX index=((SaO2/FiO2)/RR). SaO2/FiO2 = ratio of arterial oxygen saturation to fraction of inspired oxygen; RR = respiratory rate.
DISCUSSION
The case series presented show the feasibility of prolonged use of HFNO and APP in patients with COVID-19 and severe persistent hypoxemia and described the strategies developed to achieve adherence.
In 2013, the PROSEVA trial showed the impact on mortality associated with early and prolonged prone position in patients with moderate to severe ARDS under IMV [3]. Previous randomized controlled studies had evaluated the prolonged prone position (17/20 h) in patients with ARDS, but they failed to find significant differences in mortality.
In spontaneously ventilated patients, APP became relevant during the COVID-19 pandemic due to its easy implementation and impact on oxygenation, particularly in a setting with limited material resources. The retrospective APRONOX [8] study included 932 patients with ARF due to COVID-19 found a decrease in the intubation rate (38% vs 21%) and mortality (36% vs 19%) in the prone versus supine group (matched cohort). It was not possible to specify the daily duration of prone positioning. Furthermore, in the study by Ehrmann et al. [6], the only subgroup of patients where a decrease in the need for intubation was observed was in Mexico (hazard ratio (HR) 0.62 (95%CI 0.45; 084)), which obtained a higher mean of APP duration than the rest of the countries (9 vs 3 h). However, subsequent randomized control trials testing APP could not achieve a prolonged duration (4.8 h/d) [9]. Our case series reached an average of 13 h/day for 20 consecutive days demonstrating its feasibility and safety along with HFNO. The use of pharmacological treatments that favor tolerance to this position, such as dexmedetomidine [10] and opioids, have been previously described.
The P-SILI is perhaps the main limitation in maintaining patients with severe hypoxemic ARF supported by non-invasive measures. The APP has been proposed not only as a strategy for improving oxygenation but also for homogenization of ventilation and, thus, the feasibility of limiting the risk of lung injury in both IMV and spontaneously ventilated patients. The challenge lies in recognizing the right time for intubation and IMV to avoid delay and the development of P-SILI. Monitoring the use of respiratory accessory muscles is perhaps one of the valid tools; in turn, the persistence of elevated RR, and not only the events of increased RR or low ROX index, could also be useful in their monitoring. Roca et al. [11] found that ROX index <3.85 at 12 h was predictive of HFNO failure. However, that cut-off point does not seem to be useful in patients with COVID-19 as was described in a recent review about the ROX index [12]; cut-off points ranged from 2.7 to 5.9 and were assessed at different times (<4 to 12 h); the optimal cut-off point found in that review was 5–12 h for prediction of failure. In this case series, we observe the variability of the ROX index may be due to the variability of the physiological parameters (RR and SpO2) that these patients suffer from when faced with minimal stimuli such as limb movements, coughing, fluid intake, etc. Based on the above, we consider that the applicability of this index is limited in the subgroup of patients with severe hypoxemia due to COVID-19.
The limitations of this study include a small number of subjects. Future studies are needed to assess adherence to APP and thus evaluate the replicability of these results.
CONCLUSION
To summarize, the supports measures and personalized therapeutics seem to be relevant in the implementation of APP and HFNO in patients with persistent severe hypoxemia secondary to COVID-19. The impact of such interventions in patients with hypoxemic ARF of different etiologies remains to be studied.
DISCLOSURES
Acknowledgments
The authors acknowledge Nutricia Bago for their translation support.
Contributors
MB, MML, JGU, MEA, DV, SS and AG contributed to the design of the work, the acquisition, analysis, and interpretation of the data. MB and AWT were involved in drafting and commenting on the paper. All authors approved the final version.
Funding information
This study did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interests
All authors have completed the ICMJE uniform disclosure form and declare: no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval
The Internal Review Board from the 4 centers approved the study and written informed consent was obtained from all the patients for publication while preserving their identity.
REFERENCES
- 1.Grieco DL, Maggiore SM, Roca O, et al. Non-invasive ventilatory support and high-flow nasal oxygen as first-line treatment of acute hypoxemic respiratory failure and ARDS. Intensive Care Med 2021. Aug;47(8):851–66. doi: 10.1007/s00134-021-06459-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brochard L, Slutsky A, Pesenti A. Mechanical ventilation to minimize progression of lung injury in acute respiratory failure. Am J Respir Crit Care Med 2017. Feb 15;195(4):438–42. doi: 10.1164/rccm.201605-1081CP. [DOI] [PubMed] [Google Scholar]
- 3.Guérin C, Reignier J, Richard J-C, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med 2013. Jun 6;368(23):2159–68. doi: 10.1056/NEJMoa1214103. [DOI] [PubMed] [Google Scholar]
- 4.Cornejo RA, Díaz JC, Tobar EA, et al. Effects of prone positioning on lung protection in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med 2013. Aug 15;188(4):440–8. doi: 10.1164/rccm.201207-1279OC. [DOI] [PubMed] [Google Scholar]
- 5.Liu L, Xie J, Wang C, et al. Prone position improves lung ventilation-perfusion matching in non-intubated COVID-19 patients: A prospective physiologic study. Crit Care 2022. Jun 29;26(1):193. doi: 10.1186/s13054-022-04069-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ehrmann S, Li J, Ibarra-Estrada M, et al. Awake prone positioning for COVID-19 acute hypoxaemic respiratory failure: A randomised, controlled, multinational, open-label meta-trial. Lancet Respir Med 2021. Dec 1;9(12):1387–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Esperatti M, Busico M, Fuentes NA, et al. Impact of exposure time in awake prone positioning on clinical outcomes of patients with COVID-19-related acute respiratory failure treated with high-flow nasal oxygen: A multicenter cohort study. Crit Care 2022. Jan 7;26(1):16. doi: 10.1186/s13054-021-03881-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perez-Nieto OR, Escarraman-Martinez D, Guerrero-Gutierrez MA, et al. Awake prone positioning and oxygen therapy in patients with COVID-19: The APRONOX study. Eur Respir J 2022. Feb 24;59(2):2100265. doi: 10.1183/13993003.00265-2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Alhazzani W, Parhar KKS, Weatherald J, et al. Effect of awake prone positioning on endotracheal intubation in patients with covid-19 and acute respiratory failure: A randomized clinical trial. JAMA 2022. Jun 7;327(21):2104–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Taboada M, Baluja A, Santos LD, et al. Effectiveness of dexmedetomidine combined with high flow nasal oxygen and long periods of awake prone positioning in moderate or severe COVID-19 pneumonia. J Clin Anesth 2021. Sep;72:110261. doi: 10.1016/j.jclinane.2021.110261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roca O, Caralt B, Messika J, et al. An index combining respiratory rate and oxygenation to predict outcome of nasal high-flow therapy. Am J Respir Crit Care Med 2019;199(11):1368–76. doi: 10.1164/rccm.201803-0589OC. [DOI] [PubMed] [Google Scholar]
- 12.Prakash J, Bhattacharya PK, Yadav AK, Kumar A, Tudu LC, Prasad K. ROX index as a good predictor of high flow nasal cannula failure in COVID-19 patients with acute hypoxemic respiratory failure: A systematic review and meta-analysis. J Crit Care 2021;66:102–8. doi: 10.1016/j.jcrc.2021.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]