Abstract
OBJECTIVES
Previous studies have demonstrated the safety and excellent short-term and mid-term survival after minimally invasive direct coronary artery bypass (MIDCAB). We reviewed the long-term outcomes up to 20 years, including overall survival and freedom from reintervention.
METHODS
Consecutive patients who underwent MIDCAB between February 1997 and August 2020 were identified. Demographic details, operative information and long-term outcomes were obtained. The Australian National Death Index database was accessed to obtain long-term mortality data.
RESULTS
A total of 271 patients underwent an MIDCAB procedure during the study period. There were no intraoperative deaths and only one 30-day mortality (0.4%). The mean length of follow-up was 9.82 ± 8.08 years. Overall survival at 5-, 10-, 15- and 20-year survival was 91.9%, 84.7%, 71.3% and 56.5%, respectively. Patients with single-vessel disease [left anterior descending artery (LAD) only] had significantly better survival compared to patients with multivessel disease (P = 0.0035). During long-term follow-up, there were no patients who required repeat revascularization of the LAD territory. Sixty-nine patients died with the cause of death in 15 patients (21.7%) being attributable to ischaemic heart disease. An analysis comparing the isolated LAD disease MIDCAB cohort survival with the expected survival among an age/gender/year matched sample of the Australian reference population, using the standardized mortality ratio, demonstrated that the rate of survival returned to that of the reference population (standardized mortality ratio = 0.94).
CONCLUSIONS
MIDCAB is a safe and effective revascularization strategy which can be successfully performed in a carefully selected patient population with low morbidity and excellent long-term results. The survival of MIDCAB patients returns to that of their age/gender/year-matched counterparts within the normal population and hence should be offered as an alternative to coronary stenting when counselling patients with ischaemic heart disease.
Keywords: Minimally invasive direct coronary artery bypass, Minimally invasive, Coronary artery bypass grafting
Coronary artery bypass grafting (CABG) remains the gold standard treatment for complex multivessel coronary artery disease, resulting in superior long-term symptom relief and improved survival when compared to medical therapy and percutaneous coronary intervention (PCI) [1, 2].
INTRODUCTION
Coronary artery bypass grafting (CABG) remains the gold standard treatment for complex multivessel coronary artery disease, resulting in superior long-term symptom relief and improved survival when compared to medical therapy and percutaneous coronary intervention (PCI) [1, 2]. Significant short-, medium- and long-term survival benefit follows grafting of the internal mammary artery to the left anterior descending artery (LAD), with demonstrated graft patency of >90% at 15 years, and protection of the LAD territory from recurrent ischaemic injury [1, 3]. Over the last 20 years with the development of percutaneous revascularization strategies, patients with more limited disease have been managed with angioplasty instead of surgery, without long-term data (>10 years) to show superiority over established surgical techniques. Minimally invasive direct coronary artery bypass (MIDCAB), first described in 1964 with Kolesov completing LIMA to LAD grafting via a thoracotomy, was re-introduced by Calafiore in 1994, and involves grafting of the coronary arteries through a small left anterior thoracotomy, avoiding sternotomy and cardiopulmonary bypass [4]. The development of modern revascularization procedures allows complex anastomoses to be performed through a minimally invasive approach, ranging from internal mammary artery harvesting with hand-sewn anastomoses via an anterior thoracotomy (MIDCAB), to totally endoscopic coronary artery bypass grafting, either on- or off-pump [5, 6].
MIDCAB has demonstrated comparable complication and long-term patency rates to conventional sternotomy among several studies, with additional benefits of decreased postoperative pain, improved cosmesis, reduced surgical site infection rate, reduced surgical trauma, decreased requirement for blood transfusions, shortened recovery time and hospital length of stay [7, 8]. Moreover, medium-term studies have affirmed that potential increased operative times with minimally invasive approaches have no bearing on postoperative outcomes and success—with no difference in survival or cardiac and cerebrovascular complications [9, 10]. Clinical outcomes of MIDCAB have been outstanding, with excellent procedural results, a low morbidity profile, and a significantly lower rate of target vessel revascularization (1.5% vs 20%, P < 0.001) compared to PCI [11, 12]. However, long-term data regarding the outcomes and graft patency for minimally invasive coronary procedures is limited, and there are currently no randomized control trials to support their adoption over conventional open procedures [10]. Barriers to widespread adoption of robotic and minimally invasive cardiac procedures include cost increased learning curve for surgeons undertaking the procedure, institutional infrastructure and the lack of recognized training programmes [8]. We thus aimed to assess the long-term outcomes at 20 years after MIDCAB surgery including overall survival benefit of the LIMA–LAD graft and freedom from reintervention. In addition, we performed a survival analysis to determine if MIDCAB restored patients to their age-expected survival.
PATIENTS AND METHODS
Ethics statement
The study was approved by the Northern Sydney Local Health District Human Research Ethics Committee (Sydney, Australia, 2019/ETH12964) and the need for individual patient consent was waived.
Study cohort
A total of 271 consecutive patients who had undergone MIDCAB procedures between February 1997 and August 2020 were identified from institutional databases at Prince of Wales Hospital, Prince of Wales Private Hospital and Liverpool Hospital. Patients who underwent MIDCAB or robotically assisted MIDCAB were included. All patients had prospectively collected data with the first 60 cases undergoing day 1 graft angiography, with initial results published in 1999 [13]. The Australian National Death Index database was accessed in September 2020 to obtain long-term mortality data.
Patient selection and surgical technique
Patients were selected initially with isolated proximal LAD disease, but later included multivessel disease patients with either ungraftable territories, conditions which precluded sternotomy, or as part of a planned hybrid procedure with post-MIDCAB stenting of less critical non-LAD disease. To be suitable for a MIDCAB approach, the angiogram must demonstrate a good quality mid-distal LAD, that is, without diffuse calcific disease or an intramyocardial course. Some patients with concurrent diagonal disease received sequential grafting.
Under general anaesthesia and utilizing double lumen intubation, the patient is placed in the supine position with a pack placed behind the left scapula. A left anterior mini thoracotomy is performed through the 4th intercostal space, centred on the expected course of the LAD as assessed by cardiac position on chest X-ray. The pericardium is opened, the LAD identified and assessed as suitable for grafting off-pump and then the LIMA harvested. The LIMA was harvested in initial cases with a small thoracotomy retractor, later a specialized LIMA harvest retractors (Thoralift) was utilized. More recently, the DaVinci robot has allowed for LIMA harvesting on larger patients, also increasing the LIMA length for sequential grafting. Intercostal nerve blocks are placed prior to administering 10 000 units of heparin and treating the LIMA with intraluminal papaverine and blood as routine for CABG. Coronary grafting was performed with a variety of stabilizing techniques prior to the availability of the currently utilized Platypus (compression) stabilizer with a carbon dioxide blower and intraluminal shunt. The anastomosis is completed with a 7–0 prolene. Heparin is reversed at the conclusion of the case and the patient extubated on the table.
Statistical analysis
Categorical variables were summarized as frequencies and percentages. Kaplan–Meier curves were used to describe the overall survival among the full sample, in addition to comparing survival among patients with LAD disease and those who received a hybrid procedure, with log-rank tests use to assess whether survival differed significantly (P < 0.05). Kaplan–Meier curves and one-sided log-rank tests were used to compare the overall survival among the patient sample with the survival among a standard population. This was done following the approach outlined by Finkelstein, Muzikansky and Schoenfeld [14]. Below, we briefly outline the approach with regards to our sample.
Firstly, Australian life tables were downloaded from the Australian Bureau of Statistics [15], which included life tables from 2002 to 2019 broken down by age (0–100 by 1-year intervals) and gender. Next, each patient’s follow-up period was matched to the survival they would have experienced if they were a member of the Australian general population (the reference population). For example, if a 60-year-old male underwent a MIDCAB in 2015 and was followed for 5 years, the cumulative death rate was estimated for this patient by summing the death rate for a male in the 2015 life tables from age 60 to 65 years. In this way, an expected death rate was obtained for each patient, which when summed across all patients equalled the number of deaths that would be expected in an age/gender/year matched sample in the reference population. The ratio of deaths observed in the sample versus expected deaths [] in the matched reference population indicates the excess death experienced by the patient sample. The test for equality of mortality is obtained by the formula , for which the null hypothesis is distributed chi-square with 1 degree of freedom [14].
Lastly, to produce the survival curve for the reference population, the expected death rate was obtained for each patient as described above, but this time each patient’s death rate was calculated cumulatively at each age greater than MIDCAB for as many years as the longest length of follow-up. Individual expected cumulative death rates were then converted to expected survival rates using the formula given in [14]. These were then summed to give the expected survival curve for the age/gender/year matched sample which was plotted against the observed survival curve. All analyses were undertaken in the R statistical package.
RESULTS
Patient characteristics
226 (83.4%) patients were men with a mean age of 60.31 ± 11.07 (Table 1). Indications for surgery were stable angina or positive exercise stress test in 219 (80.8%) and non-ST elevation myocardial infarction in 52 (19.2%). Commonly associated cardiac risk factors included previous PCI (20.7%), family history of cardiac disease (21.4%), hypertension (25.5%) and dyslipidaemia (38.4%). One hundred and ninety-seven patients had single-vessel disease (72.3%), 59 (21.8%) patients had double-vessel disease and 16 (5.9%) had triple vessel disease. Revascularization was performed to the LAD only in 251 patients (92.6%), diagonal only in 1 patient, and both the diagonal and LAD in 19 (7%) patients. Twenty-seven patients (10%) underwent a hybrid procedure with stenting following their MIDCAB operation. Twenty-two patients (8.1%) underwent robotic harvest of the LIMA. Of the multivessel cohort, 9% of patients had pre-existing conditions that made a conventional sternotomy approach unfavourable, including previous radiotherapy, paraplegia or poor mobility, active malignancy, immunosuppressive medications, previous stroke, and requiring dialysis. Case load has varied over the study period (Fig. 1) with initial higher case volumes falling with the introduction of drug-eluting stents, before a more gradual increase recently after greater appreciation of benefits of LIMA conduit longevity, need for reintervention with PCI, and a desire to avoid long-term dual antiplatelet therapy. Recent advancements and access to robotic technology has helped with LIMA harvest and minimally invasive approaches in larger patients.
Table 1:
Characteristics of patients undergoing minimally invasive direct coronary artery bypass grafting (n = 271)
| Patient demographics, n (%) | |
|---|---|
| Male | 226 (83.4) |
| Mean age | 60.31 ± 11.07 |
| Angina functional class | |
| 1 | 38 (14.0) |
| 2 | 127 (46.9) |
| 3 | 93 (34.3) |
| 4 | 13 (4.8) |
| Indication for surgery | |
| Stable angina/positive exercise stress test | 219 (80.8) |
| Non-ST elevation myocardial infarction | 52 (19.2) |
| Previous percutaneous coronary intervention | 56 (20.7) |
| Previous cardiac surgery | 3 (1.1) |
| Diabetes | 25 (9.2) |
| Smoking status | |
| Never | 79 (10.7) |
| Current | 42 (15.5) |
| Ex-smoker | 19 (7.0) |
| Family history | 58 (21.4) |
| Hypertension | 69 (25.5) |
| Dyslipidaemia | 104 (38.4) |
| Body mass index >30 | 14 (5.2) |
| Previous cerebrovascular accident/transient ischaemic attack | 4 (1.5) |
| Number of vessel disease | |
| 1 | 196 (72.3) |
| 2 | 59 (21.8) |
| 3 | 16 (5.9) |
| Distal anastomoses | |
| Left anterior descending only | 251 (92.6) |
| Diagonal only | 1 (0.4) |
| Left anterior descending and diagonal | 19 (7.0) |
| Hybrid procedure | 27 (10.0) |
| Left circumflex | 16 (5.9) |
| Left circumflex + right coronary artery | 4 (1.5) |
| Right coronary artery | 7 (2.6) |
| Robotic procedure | 22 (8.1) |
| Conversion to sternotomy | 5 (1.8) |
| 30-Day reoperation for bleeding | 3 (1.1) |
| 30-Day reoperation for re-grafting | 2 (0.7) |
| 30-Day mortality | 1 (0.4) |
| Mean length of follow-up | 9.82 ± 8.08yrs |
Figure 1:
Number of minimally invasive direct coronary artery bypass grafting operations performed within study period stratified by year (note: 2020 January–August only).
30-Day outcomes
There were no in-hospital deaths and only one 30-day mortality (0.4%). There were 5 patients (1.8%) who required conversion to sternotomy: all due to difficulties harvesting the LIMA. Two patients early in the series required reoperation for re-grafting (0.7%) following unsatisfactory intraoperative flows and immediate post-operative angiogram, and 3 patients (1.1%) requiring reoperation for bleeding via thoracotomy. The first 60 cases all had day 1 angiography of grafts with 100% patency [13].
Long-term survival
The mean length of follow-up was 9.82 ± 8.08 years. At the time of accessing the National Death Index, 69 patients had died with the cause of death in 15 patients (21.7%) being attributable to cardiac disease (Table 2). Malignancy accounted for the largest number of deaths (29%), with chronic diseases including diabetes, renal failure and chronic obstructive pulmonary disease (COPD) totalling 15.9%.
Table 2:
Cause of death after minimally invasive direct coronary artery bypass grafting (n = 69)
| Cause of death | n (%) |
|---|---|
| Cardiac | 15 (21.7) |
| Malignancy | 20 (29.0) |
| Infection | 6 (8.7) |
| Degenerative neurological disease (including neurocognitive) | 7 (10.1) |
| Chronic disease (i.e. diabetes, renal failure, COPD) | 11 (15.9) |
| Other (i.e. trauma) | 3 (4.3) |
| Unknown | 7 (10.1) |
Overall survival at 5, 10, 15 and 20 years was 91.9%, 84.7%, 71.3% and 56.5% (Fig. 2). Due to small cohort numbers, there was no significant difference in overall survival between patients receiving the hybrid procedure (MIDCAB + PCI) compared to those who underwent MIDCAB only (P = 0.180) (Fig. 3). Overall survival after the hybrid procedure (MIDCAB + PCI) at 5, 10, 15 and 20 years was lower at 90.7%, 66.1%, 44.1% and 44.1%. In contrast, MIDCAB-only survival rates were higher at 5, 10, 15 and 20 years (92.1%, 85.9%, 72.7% and 57.3%). Of note, patients with single-vessel disease (LAD only) had significantly better survival compared to patients with multivessel disease (P = 0.0035) (Fig. 4). Overall survival in patients with single-vessel LAD disease at 5, 10, 15 and 20 years was 92.6%, 87.7%, 76.6% and 62.2%, whilst overall survival in patients with multivessel disease (2 or more vessels) at 5, 10, 15 and 20 years was 90.7%, 74.5%, 50.4% and 32.2%.
Figure 2:

Overall survival after minimally invasive direct coronary artery bypass grafting. Survival at 5, 10, 15 and 20 years was 91.9%, 84.7%, 71.3% and 56.5%.
Figure 3:

Overall survival after minimally invasive direct coronary artery bypass grafting stratified by patients who underwent a hybrid procedure (minimally invasive direct coronary artery bypass + percutaneous coronary intervention) compared to patients who underwent minimally invasive direct coronary artery bypass only.
Figure 4:

Overall survival after minimally invasive direct coronary artery bypass grafting stratified by patients with single-vessel disease (left anterior descending artery only) compared to patients with multivessel disease.
Survival analysis comparing isolated LAD disease (Fig. 5) with the expected survival among an age/gender/year matched sample of the Australian reference population revealed that isolated LAD patients had equivalent survival compared to the reference population (standardized mortality ratio = 0.94; P = 0.651). However, a similar survival analysis comparing multivessel MIDCAB patients (Fig. 6) to an age/gender/year matched sample of the Australian reference population, revealed the multivessel cohort died at an increased rate compared to the reference population (standardized mortality ratio = 1.37; P = 0.161).
Figure 5:
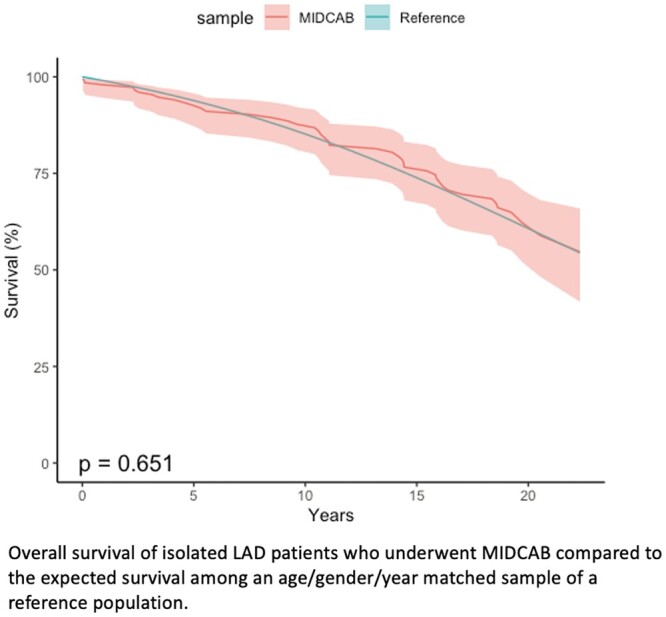
Overall survival of isolated left anterior descending artery patients who underwent minimally invasive direct coronary artery bypass compared to the expected survival among an age/gender/year matched sample of a reference population.
Figure 6:

Overall survival of multivessel patients who underwent minimally invasive direct coronary artery bypass compared to the expected survival among an age/gender/year matched sample of a reference population.
COMMENT
This retrospective single-surgeon study reports on the perioperative and long-term survival of patients undergoing MIDCAB revascularization over a 22-year period. MIDCAB offers the benefits of surgical revascularization with the left internal mammary artery (LIMA) in several patient cohorts: patients with isolated LAD disease, patients suitable for hybrid revascularization, and patients with significant comorbidities that preclude a sternotomy and cardiopulmonary bypass [16]. The results of our study confirm that MIDCAB is a viable and safe revascularization strategy across all cohorts. The 10-year survival of the entire MIDCAB cohort of 84.7% compares favourably to the existing literature reporting on single and multivessel results, ranging from 76.6% to 84.3% [17–19]. Moreover, the short-term results are in keeping with current literature with an early mortality of 0.4% (0–4.9%), conversion to sternotomy 1.8% (0–6.2%) and reoperation for bleeding 1.1% (0–8%) [20, 21]. The 10-year long-term survival of multivessel MIDCAB patients of 74.5% is also superior to the rates in the literature for conventional CABG, with Chikwe et al. [22] reporting a 10-year survival in over 40 000 patients of 66.6% in off-pump CABG and 70.4% in on-pump CABG.
Importantly, our survival analysis comparing isolated LAD disease MIDCAB patients to the expected age/gender/year matched Australian reference population demonstrated that their long-term survival had been restored to the normal population curve. The Leipzig experience [20] demonstrates a very similar survival curve to our observations, only in a much larger series of 2667 patients. Their survival was statistically better than their age-matched population, however, had a lower age-matched survival expectation than exhibited in the Australian population. The authors also noted a decrease in case numbers as drug-eluting stents dominated the market. Despite this, there has been a gradual increase in cases at our centre in recent years as the efficacy of the LIMA–LAD graft has become better understood.
Multiple randomized control trials and recent meta-analyses have reaffirmed the survival advantage of CABG over contemporary medical therapy, demonstrating the impact of revascularization over the natural survival curve of patients with coronary disease [23, 24]. Van Lierde et al. [25] retrospectively reviewed the long-term prognosis of medically managed isolated LAD disease, discovering that over an 8-year follow-up period there was a significantly greater number of cardiac death, myocardial infarction and revascularization procedures in men with LAD occlusion versus minor insignificant coronary disease (P < 0.0001, P = 0.001, P = 0.04). From this, it can be inferred that patients with LAD disease inherently have a negative impact on their survival curve, reiterating the benefits of our MIDCAB results in returning patients to mortality rate equivalent of the average population, which is attributable to the LIMA–LAD graft.
Previous meta-analyses comparing MIDCAB to both on-pump CABG and off-pump CABG have demonstrated similar outcomes [16, 26]. A review with the longest follow-up of 12.95 ± 0.47 years revealed there was no difference between MIDCAB and traditional CABG in terms of complications or survival, reaffirming its safety but failing to demonstrate superiority over the conventional approach [21]. The benefits of MIDCAB in a selective high-risk surgical population has been studied by Jacob et al., demonstrating that incomplete revascularization via MIDCAB is a safe procedure compared with conventional CABG with a lower incidence of hospital mortality, neurological events, and perioperative myocardial infarction with comparable midterm results at 4 years [27].
There is significant paucity in the literature with regard to long-term outcomes of MIDCAB procedures in comparison to PCI [19]. Benedetto et al. [12] performed a propensity-matched study which demonstrated a similar 30-day mortality; however, at 10 years drug-eluting PCI was associated with a 2.19-fold increased risk of late death and a 2.0-fold increase in repeat revascularization, demonstrating improved long-term survival in MIDCAB patients. Controversy remains regarding the use of PCI for proximal LAD disease with multiple randomized control trials and meta-analyses demonstrating comparable rates of death, myocardial infarction and stroke in comparison to MIDCAB, but with significantly increased rate of repeat revascularization after PCI (1.5% vs 20%, P < 0.001) [11, 12, 28]. A recent meta-analysis pooling 7710 patients demonstrated the superiority of MIDCAB in terms of freedom from repeat intervention and decreased target vessel revascularization when compared to both first and second-generation drug-eluting stents [29]. However, the majority of studies in this analysis had a limited follow-up of only 1 year, hence the long-term durability of stents remains unproven [1]. In addition, an earlier meta-analysis demonstrated 2.62 times more angina, 2.86 times more adverse coronary and cerebral events, and 4.63 times greater repeat revascularization when comparing PCI to MIDCAB [30].
Limitations
This study is limited by its retrospective, observational nature and has been undertaken over 2 surgical centres. This population is the entire surgical experience and thereby incorporates the initial learning curve and early complications associated with performing a new procedure. Moreover, the population contains patients with various patterns of disease, with both single and multivessel coronary disease, potentially confounding comparisons of long-term survival given the inherent disease state. In statistical analysis, due to the lack of life table data prior to 2002, patients who underwent MIDCAB prior to 2002 were matched to the 2002 life table data (rather than data from their year of surgery). This resulted in a reference population with slightly better survival than would have been expected from the general population in the years prior to 2002. However, improvements in death rates between 1997 (the earliest year of surgery in our data) and 2002 are minimal, and are unlikely to have substantially biased our results [15].
CONCLUSION
This study reconfirms the safety of the MIDCAB procedure in a carefully selected patient population with minimal post-operative complications, low morbidity, and excellent grafting results. Importantly, we have demonstrated that post-revascularization isolated LAD disease MIDCAB patients return to their expected survival for their age-/gender-/year-matched counterparts within the Australian population. This, particularly in combination with corroborating literature, raises questions concerning the management of proximal LAD disease with either PCI or surgery in patients with >10-year expected survival. Direct comparison between isolated LAD stenting and MIDCAB is required in the future to further analyse the benefits of a surgical approach in this patient cohort as currently, nothing else compares favourably to the LIMA–LAD graft beyond 10 years.
Conflict of interest: none declared.
Glossary
ABBREVIATIONS
- CABG
Coronary artery bypass grafting
- LAD
Left anterior descending artery
- MIDCAB
Minimally invasive direct coronary artery bypass
- PCI
Percutaneous coronary intervention
Contributor Information
Lucy Manuel, Cardiothoracic Surgery Department, Royal North Shore Hospital, St Leonards, Australia.
Laura S Fong, Cardiothoracic Surgery Department, Prince of Wales Hospital, Randwick, Australia.
Kim Betts, School of Public Health, Curtin University, Perth, Australia.
Levi Bassin, Cardiothoracic Surgery Department, Royal North Shore Hospital, St Leonards, Australia; Cardiothoracic Surgery Department, Prince of Wales Hospital, Randwick, Australia.
Hugh Wolfenden, Cardiothoracic Surgery Department, Prince of Wales Hospital, Randwick, Australia.
Data Availability
The data underlying this article will be shared on reasonable request to the corresponding author.
Author contributions
Lucy Manuel: Data curation; Investigation; Writing – original draft; Writing – review & editing. Laura S. Fong: Supervision; Writing—review & editing. Kim Betts: Data curation; Formal analysis. Levi Bassin: Supervision; Writing—review & editing. Hugh Wolfenden: Conceptualization; Methodology; Project administration; Supervision; Writing—review & editing.
Reviewer information
Interactive CardioVascular and Thoracic Surgery thanks Stefano Schena and the other, anonymous reviewer(s) for their contribution to the peer review process of this article.
REFERENCES
- 1. Pasrija C, Kon ZN, Ghoreishi M, Lehr EJ, Gammie JS, Griffith BP. et al. Cost and outcome of minimally invasive techniques for coronary surgery using robotic technology. Innovations (Phila) 2018;13:282–6. [DOI] [PubMed] [Google Scholar]
- 2. Leyvi G, Forest SJ, Srinivas VS, Greenberg M, Wang N, Mais A. et al. Robotic coronary artery bypass grafting decreases 30-day complication rate, length of stay, and acute care facility discharge rate compared with conventional surgery. Innovations (Phila) 2014;9:361–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cameron A, Davis KB, Green G, Schaff HV.. Coronary bypass surgery with internal-thoracic-artery grafts—effects on survival over a 15-year period. N Engl J Med 1996;334:216–9219. [DOI] [PubMed] [Google Scholar]
- 4. Calafiore AM, Di Giammarco G, Teodori G, Gallina S, Maddestra N, Paloscia L. et al. Midterm results after minimally invasive coronary surgery (last operation). J Thorac Cardiovasc Surg 1998;115:763–71. [DOI] [PubMed] [Google Scholar]
- 5. Cao C, Indraratna P, Doyle M, Tian DH, Liou K, Munkholm-Larsen S. et al. A systematic review on robotic coronary artery bypass graft surgery. Ann Cardiothorac Surg 2016;5:530–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Ishikawa N, Watanabe G.. Robot-assisted cardiac surgery. Ann Thorac Cardiovasc Surg 2015;21:322–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Christidis NK, Fox SA, Swinamer SA, Bagur R, Sridhar K, Lavi S. et al. Reason and timing for conversion to sternotomy in robotic-assisted coronary artery bypass grafting and patient outcomes. Innovations (Phila) 2018;13:423–7. [DOI] [PubMed] [Google Scholar]
- 8. Sepehripour AH, Garas G, Athanasiou T, Casula R.. Robotics in cardiac surgery. Ann R Coll Surg Engl 2018;100:22–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Kofler M, Stastny L, Johannes Reinstadler S, Dumfarth J, Kilo J, Friedrich G. et al. Robotic versus conventional coronary artery bypass grafting: direct comparison of long-term clinical outcome. Innovations (Phila) 2017;12:239–46. [DOI] [PubMed] [Google Scholar]
- 10. Harky A, Chaplin G, Chan JSK, Eriksen P, MacCarthy-Ofosu B, Theologou T. et al. The Future of open heart surgery in the era of robotic and minimal surgical interventions. Heart Lung Circ 2020;29:49–61. [DOI] [PubMed] [Google Scholar]
- 11. Blazek S, Rossbach C, Borger MA, Fuernau G, Desch S, Eitel I. et al. Comparison of sirolimus-eluting stenting with minimally invasive bypass surgery for stenosis of the left anterior descending coronary artery: 7-year follow-up of a randomized trial. JACC Cardiovasc Interv 2015;8:30–8. [DOI] [PubMed] [Google Scholar]
- 12. Benedetto U, Raja SG, Soliman RF, Albanese A, Jothidasan A, Ilsley CD et al; Harefield Cardiac Outcomes Research Group. Minimally invasive direct coronary artery bypass improves late survival compared with drug-eluting stents in isolated proximal left anterior descending artery disease: a 10-year follow-up, single-center, propensity score analysis. J Thorac Cardiovasc Surg 2014;148:1316–22. [DOI] [PubMed] [Google Scholar]
- 13. Wolfenden H, Pitney M.. In-hospital angiographic review of 32 consecutive MIDCAB-LAST procedures. Asia Pac Heart J 1999;8:61. [Google Scholar]
- 14. Finkelstein DM, Muzikansky A, Schoenfeld DA.. Comparing survival of a sample to that of a standard population. J Natl Cancer Inst 2003;95:1434–9. [DOI] [PubMed] [Google Scholar]
- 15. Statistics ABo. Life Tables, 2021. https://www.abs.gov.au/statistics/people/population/life-tables (9 September 2021, date last accessed).
- 16. Garg S, Raja SG.. Minimally invasive direct coronary artery bypass (MIDCAB) grafting. AME Med J 2020;5:19. [Google Scholar]
- 17. Holzhey DM, Cornely JP, Rastan AJ, Davierwala P, Mohr FW.. Review of a 13-year single-center experience with minimally invasive direct coronary artery bypass as the primary surgical treatment of coronary artery disease. Heart Surg Forum 2012;15:E61–8. [DOI] [PubMed] [Google Scholar]
- 18. Repossini A, Di Bacco L, Nicoli F, Passaretti B, Stara A, Jonida B. et al. Minimally invasive coronary artery bypass: twenty-year experience. J Thorac Cardiovasc Surg 2019;158:127–38.e1. [DOI] [PubMed] [Google Scholar]
- 19. Davierwala PM, Verevkin A, Bergien L, von Aspern K, Deo SV, Misfeld M. et al. Twenty-year outcomes of minimally invasive direct coronary artery bypass surgery: the Leipzig experience. J Thorac Cardiovasc Surg 2021. 10.1016/j.jtcvs.2020.12.149. [DOI] [PubMed] [Google Scholar]
- 20. Hammal F, Nagase F, Menon D, Ali I, Nagendran J, Stafinski T.. Robot-assisted coronary artery bypass surgery: a systematic review and meta-analysis of comparative studies. Can J Surg 2020;63:E491–E508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Raja SG, Garg S, Rochon M, Daley S, De Robertis F, Bahrami T.. Short-term clinical outcomes and long-term survival of minimally invasive direct coronary artery bypass grafting. Ann Cardiothorac Surg 2018;7:621–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Chikwe J, Lee T, Itagaki S, Adams DH, Egorova NN.. Long-term outcomes after off-pump versus on-pump coronary artery bypass grafting by experienced surgeons. J Am Coll Cardiol 2018;72:1478–86. [DOI] [PubMed] [Google Scholar]
- 23. Fearon WF, Harrington RA.. Coronary artery bypass surgery is not underutilized! Circulation 2016;133:1027–35. [DOI] [PubMed] [Google Scholar]
- 24. Hueb W, Lopes N, Gersh BJ, Soares PR, Ribeiro EE, Pereira AC. et al. Ten-year follow-up survival of the Medicine, Angioplasty, or Surgery Study (MASS II). Circulation 2010;122:949–57. [DOI] [PubMed] [Google Scholar]
- 25. Van Lierde J, Piessens J, Glazier JJ, Vrolix M, De Geest H, Willems JL.. Long-term prognosis of male patients with an isolated chronic occlusion of the left anterior descending coronary artery. Am Heart J 1991;122:1542–7. [DOI] [PubMed] [Google Scholar]
- 26. Stanbridge RD, Hadjinikolaou LK.. Technical adjuncts in beating heart surgery comparison of MIDCAB to off-pump sternotomy: a meta-analysis. Eur J Cardiothorac Surg 1999;16:S24–S33. [PubMed] [Google Scholar]
- 27. Jacobs S, Holzhey D, Falk V, Garbade J, Walther T, Mohr FW.. High-risk patients with multivessel disease–is there a role for incomplete myocardial revascularization via minimally invasive direct coronary artery bypass grafting? Heart Surg Forum 2007;10:E459–62. [DOI] [PubMed] [Google Scholar]
- 28. Patel AJ, Yates MT, Soppa GK.. What is the optimal revascularization technique for isolated disease of the left anterior descending artery: minimally invasive direct coronary artery bypass or percutaneous coronary intervention? Interact CardioVasc Thorac Surg 2014;19:144–8. [DOI] [PubMed] [Google Scholar]
- 29. Raja SG, Uzzaman M, Garg S, Santhirakumaran G, Lee M, Soni MK. et al. Comparison of minimally invasive direct coronary artery bypass and drug-eluting stents for management of isolated left anterior descending artery disease: a systematic review and meta-analysis of 7,710 patients. Ann Cardiothorac Surg 2018;7:567–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Aziz O, Rao C, Panesar SS, Jones C, Morris S, Darzi A. et al. Meta-analysis of minimally invasive internal thoracic artery bypass versus percutaneous revascularisation for isolated lesions of the left anterior descending artery. BMJ 2007;334:617. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data underlying this article will be shared on reasonable request to the corresponding author.




