Abstract
Pyelolymphatic backflow is a rare type of pyelolymphatic fistula that occurs in cases of urinary obstruction. This phenomenon may help to decompress an acutely obstructed kidney, and therefore, alleviate renal function from deteriorating. Pyelolymphatic backflow has specific imaging characteristics best shown on CT urography. Our case study aims to improve the understanding and diagnosis of pyelolymphatic backflow by presenting a case of pyelolymphatic backflow seen on CT urography, including discussions on the pathophysiology, clinical relevance and management of this phenomenon. Our case study demonstrates the opacification of landmark lymphatic structures including the retroperitoneal para-aortic lymphatic chain, cisterna chyli and thoracic duct, which have not been demonstrated previously.
Keywords: Pyelolymphatic backflow, Pyelolymphatic fistula, Computed tomography
Introduction
Pyelolymphatic backflow is a subtype of pyelolymphatic fistula which occurs in cases of urinary obstruction. This phenomenon may help to decompress an acutely obstructed kidney by acting as an alternative drainage pathway [1,2]. Cross-sectional techniques are the mainstay of investigation of pyelolymphatic backflow. To our knowledge, there is only one published case report of pyelolymphatic backflow depicted on CT, which was presented by Durhan et al. [1]. In their case report, Durhan et al. showed the opacification of periureteral lace-like densities.
Our case study aims to further the understanding and diagnosis of this rare phenomenon by presenting a case of pyelolymphatic backflow demonstrated on CT. Additionally, our case study demonstrates the opacification of the downstream lymphatic drainage pathway which have not been previously demonstrated.
Case report
Our patient was a 63-year-old male who was seen for an episode of Enterococcus faecalis urinary tract infection. His symptoms resolved following a course of antibiotics. The prostate was smooth and nontender on digital rectal examination. Serum creatinine was within normal limits (86 µmol/L). CT urography was performed to evaluate possible underlying causes for urinary tract infection in a male patient.
CT urography demonstrated evidence of pyelolymphatic backflow on the excretory phase of the study. There was opacification of retroperitoneal tubular structures, which were directed toward the hilum of the kidneys. These formed lace-like structures (shown in Figs. 1a–d indicated by orange arrows) with resultant opacification of the retroperitoneal para-aortic lymph node chain (shown in Figs. 1a–d indicated by red arrows). Subsequent opacification of the cisterna chyli (shown in Fig. 2 indicated by a blue arrow) and thoracic duct (shown in Fig. 2 indicated by a yellow arrow) are also demonstrated, which confirms that the opacified structures are the renal lymphatic networks.
Fig. 1.
(a, b) Axial CT urography in the excretory phase. (c, d) Coronal CT urography in the excretory phase. The orange arrows denote the opacified lace-like pararenal lymphatics. The red arrows denote the opacified para-aortic lymph node chains. Black asterisks denote the opacified urinary tract.
Fig. 2.
Coronal CT urography in the excretory phase. The blue arrow denotes the opacified cisterna chyli and yellow arrow denotes the opacified thoracic duct. Black asterisks denote the opacified urinary tract.
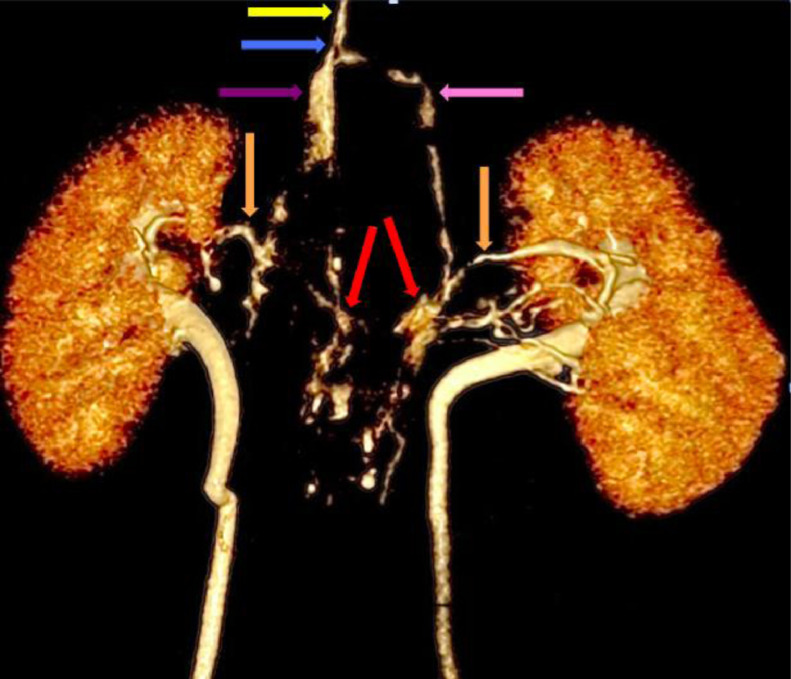
3D reconstruction of the opacified urinary tracts and lymphatics shows the periureteral lace-like lymphatic network (shown in Fig. 3 indicated by orange arrows) and the retroperitoneal para-aortic lymph node chain (shown in Fig. 3 indicated by red arrows). 3D reconstruction clearly demonstrates landmark lymphatic structures including the right lumbar trunk (shown in Fig. 3 indicated by purple arrow) and the left lumbar trunk (shown in Fig. 3 indicated by pink arrow). These converge and drain into the cysterna chyli (shown in Fig. 3 indicated by blue arrow), which continues cranially as the thoracic duct (shown in Fig. 3 indicated by yellow arrow).
Fig. 3.
3D reconstruction of the urinary tract and lymphatic network. The orange arrows denote the opacified lace-like pararenal lymphatics. The red arrows denote the opacified para-aortic lymph node chains. The purple arrow denotes the right lumbar trunk and the pink arrow denotes the left lumbar trunk. The blue arrow denotes the cisterna chyli and yellow arrow denotes the thoracic duct.
Discussion
Pyelolymphatic fistulas have been reported in cases of upper urinary tract obstruction, infection, inflammatory disease, neoplasm, or trauma [1,3]. Two main pathophysiological processes give rise to pyelolymphatic fistulas. The first occurs due to the rupture of lymphatic channels into the urinary tract, allowing the reflux of chyle into the urinary system. This is usually seen in cases of parasitic infections or renal tuberculosis [3]. It may be caused by an accumulation of toxic metabolites or an inflammatory immune reaction, causing regurgitation of chyle into the urinary tract [4]. Another theory is that it occurs due to obstruction of the peri-renal lymphatic system resulting in obliterative lymphangitis and collateralization, with the development of a fistula [5].
The other process is pyelolymphatic backflow, an uncommon phenomenon. Pyelolymphatic backflow refers to the reflux of urine into the lymphatic system. This occurs in cases of urinary obstruction due to the rupture of the renal fornices with subsequent interstitial extravasation and filling of forniceal lymphatics [1]. The elevation of intrapelvic pressure may then result in the backflow of urine via one of the following pathways: pyelotubular or pyelocanalicular backflow, pyelovenous backflow, pyelointerstitial backflow, pyelosinus backflow, and lastly pyelolymphatic backflow [6,7].
Microlymphatic channels originate in the cortical interstitium near the glomeruli, forming networks that closely parallel afferent arterioles and encircle interlobular arteries as a rete. Animal studies have demonstrated that subsequent to forniceal rupture, lymphatic filling occurs initially in the periarcuate plexus at the corticomedullary junction. Following this, interlobular, interlobar and perihilar lymphatics are then visualized [2].
It has been suggested that pyelolymphatic backflow may help to decompress an obstructed kidney by serving as an alternative drainage pathway and preventing renal function from deteriorating [1,2,8]. Renal damage due to urinary tract obstruction has been demonstrated to be markedly more rapid and severe in cases where intrarenal lymphatics are destroyed by infection [2].
Cross-sectional techniques are the mainstay of investigation of pyelolymphatic backflow. Durhan et al. [1] presented a case of pyelolymphatic backflow detected by CT, in which the backflow showed peri-ureteral thread-like structures. Our case study also demonstrates the opacification of the retroperitoneal para-aortic lymph node chain, cysterna chyli and thoracic duct. The opacification of these landmark structures have not been previously demonstrated, and indicate the normal flow direction in the lymphatic system.
One potential pitfall in the diagnosis of pyelolymphatic backflow on CT is that this may sometimes be confused with a urine leak on CT. However, the absence of urinoma, characteristic lace-like, beaded features of the lymphatic system and the opacification of landmark structures such as the cisterna chyli and thoracic duct more strongly favor the presence of pyelolymphatic backflow [1].
Treatment involves decompression of renal pelvic pressure via the deployment of a ureteric stent or percutaneous nephrostomy, and treating the cause of obstruction [1]. Another possible treatment option is sclerotherapy, which has been used to obliterate fistulous communications between the urinary tract and the lymphatic system [4]. In such cases, 1% silver nitrate is the sclerosing agent of choice [4]. When instilled into the renal pelvis, the sclerosing agent induces a chemical lymphangitis. The resultant edema and fibrosis then results in occlusion of the lymphatic channels [4].
In summary, pyelolymphatic backflow is one mechanism through which reflux of urine occurs in response to urinary tract obstruction. Pyelolymphatic backflow may serve to preserve renal function by acting as an alternative drainage pathway for urine. The characteristic imaging findings of pyelolymphatic backflow are best seen on CT urography. Treatment involves decompression of renal pelvic pressure and treating the cause of obstruction.
Patient consent
Written informed consent was obtained from the patient for publication of the details of their medical case and any accompanying images.
Footnotes
Competing Interests: The authors have no conflicts of interest to declare.
Funding Sources: No funding was acquired for this case report.
References
- 1.Gamze D, Veysel AA, Turkmen TC, Deniz A, Mustafa NO. Pyelolymphatic backflow demonstrated by an abdominal CT: a case report. Pol J Radiol. 2014;79:6–8. doi: 10.12659/PJR.889930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cuttino JT, Clark RL, Fried FA, Stevens PS. Microradiographic demonstration of pyelolymphatic backflow in the porcine kidney. Am J Roentgenol. 1978;131:501–505. doi: 10.2214/ajr.131.3.501. [DOI] [PubMed] [Google Scholar]
- 3.Yu NC, Raman SS, Patel M, Barbaric Z. Fistulas of the genitourinary tract: a radiologic review. RadioGraphics. 2004;24:1331–1352. doi: 10.1148/rg.245035219. [DOI] [PubMed] [Google Scholar]
- 4.Victoria S, Patrick J, Siri OJ, Rupert B, Amr H. Vol. 12. 2020. Chyluria: what does the clinician need to know? pp. 1–10. (Ther Adv Urol). [Google Scholar]
- 5.Goel TC, Goel A. Lymphatic filariasis. Springer; Singapore: 2016. Chyluria; pp. 273–300. [Google Scholar]
- 6.Prabudh G, Minu B, Devasenathipathy K. An enigmatic route to the contralateral pelvicalyceal system on antegrade pyelogram. J Indian Assoc Pediatr Surg. 2018;23(4):236–238. doi: 10.4103/jiaps.JIAPS_139_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Szewczyk W, Prajsner A, Szewczyk M. Pyelointerstitial, pyelovenous, and pyelosinus backflow during retrograde pyelography. Urol J. 2016;13:2932–2933. [PubMed] [Google Scholar]
- 8.Helin I, Okmian L, Olin T. Renal blood flow and function at elevated ureteric pressure. An experimental study in the pig. Scand J Urol Nephrol. 1975;(28 Suppl):53–69. [PubMed] [Google Scholar]