Abstract
Medial collateral ligament (MCL) injuries are typically managed non-operatively, with high rates of clinical success. However, patients who present with medial knee laxity with valgus stress testing of a fully extended knee, anteromedial rotatory instability, associated tibial plateau fracture, or multiligament injury or those who continue to be symptomatic after non-operative treatment may benefit from surgical intervention. Patients with a history of total knee arthroplasty who suffer MCL and posterior oblique ligament (POL) injuries represent a challenging patient population and often require surgical attention. In this Technical Note, we describe the preoperative assessment, decision making, and surgical technique for anatomic reconstruction of the superficial MCL and POL with an Achilles allograft in young, active patients with medial-sided knee injuries after total knee arthroplasty.
Technique Video
In this Technical Note, we describe the preoperative evaluation, decision making, and surgical technique for a left knee anatomic reconstruction of the superficial medial collateral ligament and posterior oblique ligament with an Achilles allograft in young, active patients after a valgus injury who had previously undergone a total knee arthroplasty.
The medial complex of the knee consists of a series of capsular thickenings, tendinous attachments, and ligaments. The primary structures providing valgus stability of the knee are the superficial medial collateral ligament (sMCL), posterior oblique ligament (POL), and deep medial collateral ligament (dMCL).1 The sMCL has an oval-shaped femoral attachment 3.2 mm proximal and 4.8 mm posterior to the medial epicondyle.2 Distally, it has 2 attachments on the tibia, with the more proximal insertion of soft tissue that belongs to the anterior arm of the semimembranosus tendon, located about 10 to 12 mm distal to the joint line.3,4 The more distal insertion lies 60 mm distal to the tibial joint line and is located just anterior to the posteromedial crest of the tibia.1,5 Additionally, the POL is a fibrous extension of the distal aspect of the semimembranosus and reinforces the posteromedial capsule. Three arms of the POL have been described: the superficial, central, and capsular arms, with the central considered the main structural and functional component.6,7 The POL has a femoral attachment that is 1.4 mm distal and 2.9 mm anterior to the gastrocnemius tubercle and a distal attachment that blends into the posterior joint capsule and the posterior medial meniscus.5 The dMCL is a thickening of the medial joint capsule that runs parallel and deep to the sMCL and consists of the meniscofemoral and meniscotibial ligaments.1,8
The proximal division of the sMCL is the primary valgus stabilizer from 0° to 90° of flexion.9,10 Comparatively, the distal division of the sMCL plays a role as a primary restraint to external rotation at 30° of flexion and to internal rotation at all degrees of flexion.10 Additionally, the POL is a primary stabilizer for internal rotation from 0° to 30° of flexion.4 As a result, external rotation of the knee in patients with a POL tear can result in anteromedial subluxation of the tibial plateau and thus anteromedial rotatory instability of the knee.11 Furthermore, the POL acts as a secondary stabilizer to prevent posterior tibial translation and valgus abduction with the knee in full extension, regardless of the integrity of the posterior cruciate ligament (PCL).6 The main mechanism of POL injury involves a combination of valgus and external rotation forces, while an isolated lesion of the MCL often occurs from a pure valgus load.12
MCL injuries are typically managed non-operatively with success due to a high innate healing ability from the vast blood supply from branches of the superior and inferior genicular arteries.5 With non-operative treatment, early introduction of range of motion exercises, early weightbearing, and progressive strengthening have been shown to be successful for grade I and II and some isolated grade III MCL injuries.13 Several animal models have highlighted the need for early, progressive range of motion with conservative therapy, as prolonged immobilization after MCL tear has been shown to result in a reduction of collagen mass and increased collagen degradation.14, 15, 16 Comparatively, patients who present with medial knee laxity with valgus stress testing of a fully extended knee, anteromedial rotatory instability, associated tibial plateau fracture, or multiligament injury and those who continue to be symptomatic after non-operative treatment may benefit from surgical intervention.17,18 Furthermore, patients with a total knee arthroplasty (TKA) and subsequent MCL tear represent a unique subset of patients with significantly altered knee biomechanics and instability that may require medial-sided reconstruction.19
In this Technical Note, we describe the preoperative assessment, decision making, and surgical technique for anatomic reconstruction of the sMCL and POL with an Achilles allograft after a posteromedial knee injury in young, active patients who have previously undergone TKA (Video 1).
Technique
Preoperative Evaluation and Surgical Decision-Making
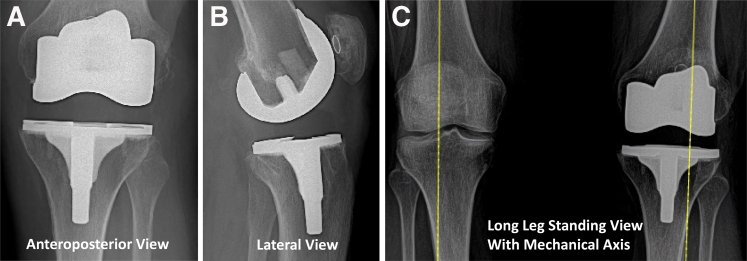
Patients with TKA who present with medial-sided instability after an acute injury should be evaluated for aseptic loosening or periprosthetic fracture. Radiographs should be performed in the anteroposterior (AP), lateral, merchant, and long leg standing views to assess for acute prosthetic pathology (Fig. 1A–C). Physical examination should include range of motion, the presence or absence of swelling, and the stability of the collateral ligaments compared with the contralateral extremity. Medial gapping on valgus stress testing at 20° to 30° of flexion can be seen in an isolated MCL tear, whereas gapping with 0° of knee flexion suggests injury to the POL. Anteromedial rotatory instability is suggestive of combined sMCL and POL injury and can be evaluated using the dial test. The dial test identifies anteromedial subluxation of the tibia with increasing tibial external rotation.20
Fig 1.
Preoperative radiographs of the left knee. Preoperative anteroposterior (A) and preoperative lateral view (B) radiographs of a total knee arthroplasty with well-positioned tibial and femoral components before surgery for medial collateral ligament and posterior oblique ligament reconstruction. (C) Preoperative long leg standing radiographs demonstrating significant valgus malalignment of the left knee compared with the right knee.
Initial treatment of MCL injuries consists of bracing and activity modifications. Patients who have continued symptoms of instability, pain, and functional decline despite conservative therapy may be indicated for surgery. Surgical options in patients with medial-sided knee injuries with a preexisting TKA include revision of total knee replacement with a higher level of constraint or a ligament reconstruction. When deciding between these options, one must consider the patient’s age, bone quality, activity level, comorbid conditions, and functional limitations associated with a constrained prosthesis. In young, active TKA patients presenting with a complete medial-sided knee injury, an open superficial medial collateral ligament (sMCL) and POL reconstruction using a split Achilles tendon allograft should be considered as an alternative to revision TKA.
Patient Positioning, Anesthesia, and Graft Preparation
The patient is taken to the operating room, and general anesthesia is administered along with preoperative antibiotic prophylaxis. The patient is positioned supine on an operating room table with the leg of the bed removed. A tourniquet is placed high on the operative extremity, and the operative leg is positioned in a leg holder (AliMed Fluid-Proof Arthroscopic Leg Holder; AliMed, Dedham, MA). The non-operative extremity is placed in a stirrup (Allen YellowFin Lift Assist Stirrups; Allen Medical Systems, Acton, MA). A preoperative examination under anesthesia is performed, confirming 3+ valgus instability in both full extension and 30° of flexion. The operative extremity is subsequently prepped and draped in a sterile fashion.
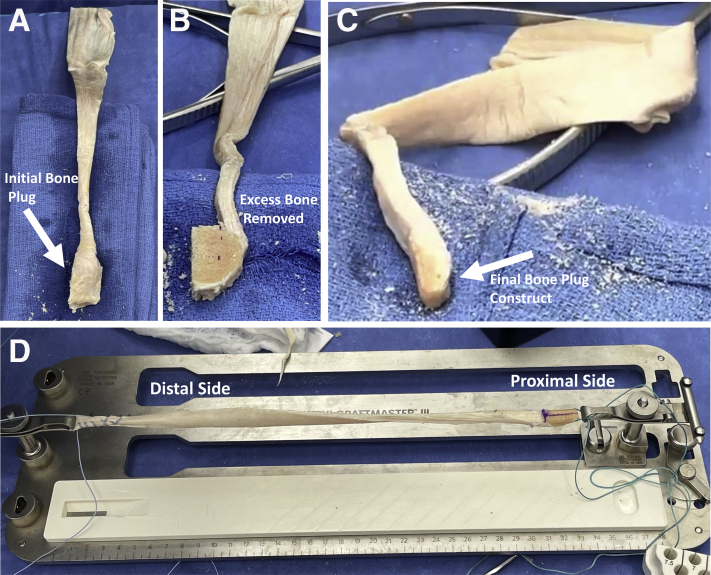
On the back table, an Achilles tendon allograft (JRF Ortho, Englewood, CO) is thawed and prepared as 2 separate 11 × 25-mm bone plugs to be used on the femoral side to reconstruct the sMCL and POL (Fig. 2A–C). A single hole is drilled in each bone block, and a passing suture is passed through the bone plug to help with graft passing later in the procedure. The free, soft tissue end of the graft is whipstitched, and the graft is tensioned to remove any inherent creep (Fig. 2D).
Fig 2.
Achilles allograft preparation for use as the superficial medial collateral ligament (sMCL) and posterior oblique ligament (POL). (A) An Achilles tendon allograft (JRF Ortho) is thawed and (B) prepared as 2 separate 11 × 25-mm bone plugs to be used on the femoral side to reconstruct the sMCL and POL. (C) The bone plug of the allograft is shaped in a cylindrical fashion to fit inside the femoral tunnels. (D) Each Achilles tendon allograft is whipstitched to form a strong construct, a single hole is drilled in each bone block, and a passing suture is passed through the bone plug to help with graft passing later in the procedure.
Surgical Approach
Dissection and Identification of Anatomic Landmarks
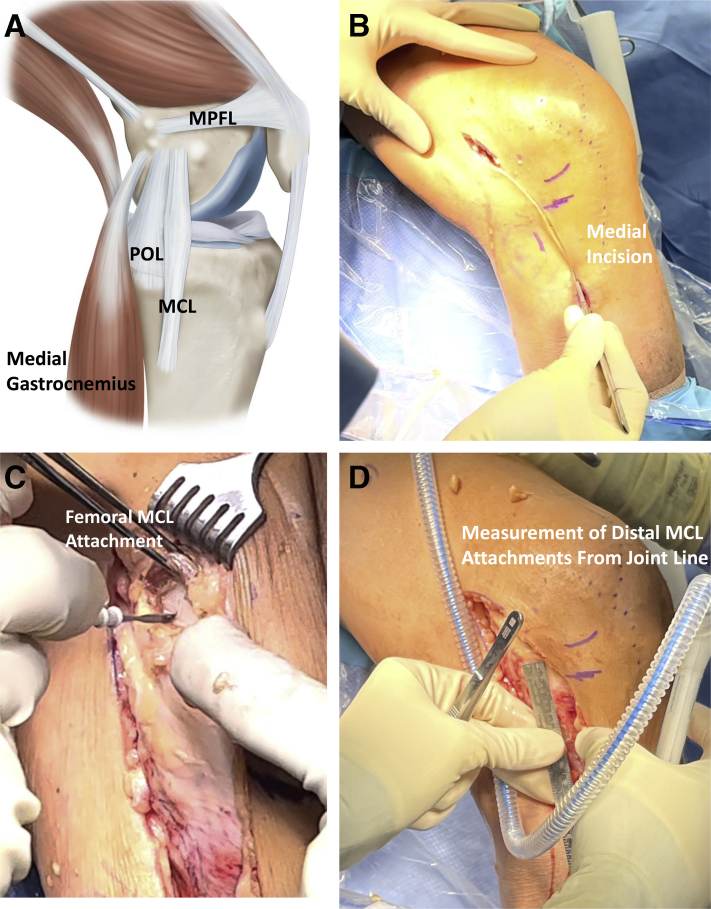
The medial femoral condyle, medial tibial plateau, and medial epicondyle are marked as anatomic landmarks, in addition to a point 7 cm distal to the joint line on the tibia (Fig. 3A).
Fig 3.
Dissection and anatomic landmark identification of the medial side of the left knee. (A) An illustrative depiction of the medial collateral ligament (MCL) and posterior oblique ligament (POL) in relation to the medial gastrocnemius and medial patellofemoral ligament (MPFL) complexes. (B) A 10-cm posteriorly based curvilinear incision centered over the medial femoral epicondyle is made and extended distally to the mark placed 7 cm distal to the tibial joint line. (C) The origin of the superficial MCL (sMCL) is identified by first palpating and identifying the adductor tubercle and medial epicondyle. This point on the femur is further exposed with electrocautery to facilitate subsequent drilling of the femoral tunnel of the sMCL. (D) A point 60 mm distal to the joint line and the midline between the medial aspect of the tibia is identified as the most distal insertion site of the sMCL on the tibia.
A 10-cm posteriorly based curvilinear incision centered over the medial femoral epicondyle is made and extended distally to the mark placed 7 cm distal to the tibial joint line (Fig. 3B). Large skin flaps are made, and dissection is carried down until the vastus medialis muscle fibers are visualized. The adductor tubercle is then identified by following the insertion of the adductor tendon. From here, the medial epicondyle can be palpated 12 mm distal and 8 mm anterior from the adductor tubercle.2 The origin of the sMCL is finally found 3.2 mm proximal and 4.8 mm posterior to the medial epicondyle. This point on the femur is further exposed with electrocautery to facilitate subsequent drilling of the femoral tunnel of the sMCL (Fig. 3C).
Attention is then turned to prepare the distal attachment of the sMCL on the tibia. A point 60 mm distal to the joint line, and midline between the AP distance on the medial aspect of the tibia is identified (Fig. 3D). This point is often at the insertion of the pes tendons that were previously elevated and tagged. Care is taken to leave a sleeve of sartorial fascia attached to the tendons for repair at the end of the procedure. The distal sMCL attachment on the tibia is then marked with electrocautery and cleared of periosteum and overlying soft tissue. The more proximal sMCL tibial insertion is also identified just anterior to the semimembranosus insertion on the proximal tibia. At the same AP position on the tibia, and at the level of the semimembranosus on the proximal tibia, the tibia is marked with electrocautery and cleared of overlying periosteum.
Creation of sMCL and POL Femoral Bone Tunnels
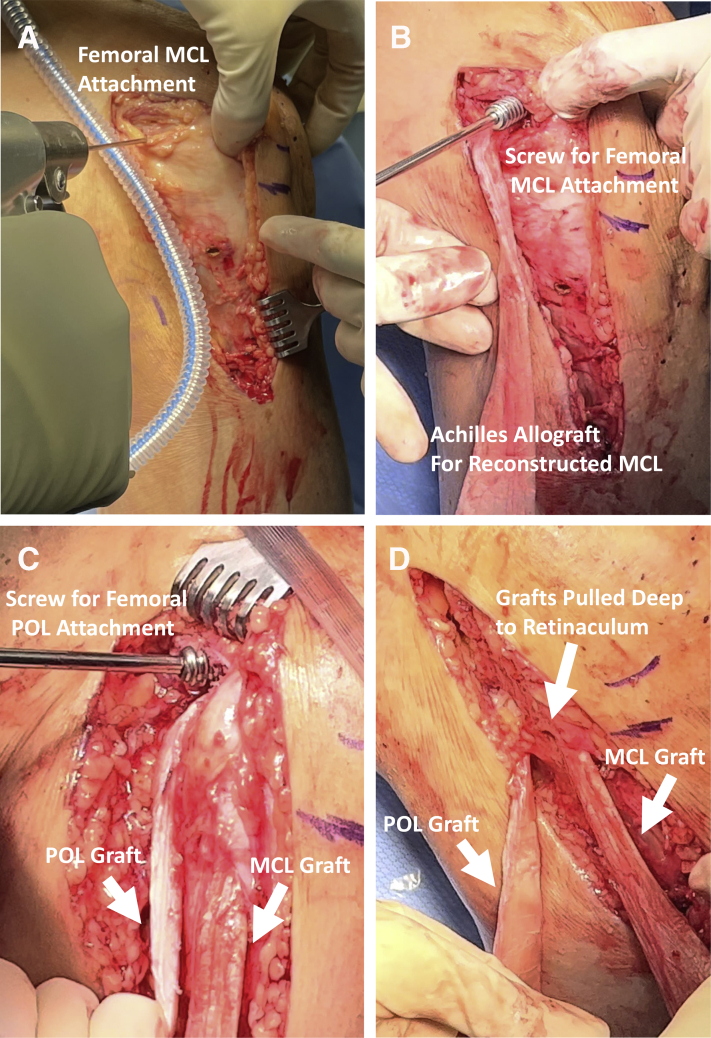
Drilling of the femoral origin of the sMCL is performed with a guide pin introduced at the previously exposed origin on the femur (Fig. 4A). Drilling is performed bicortically and oriented 20° anteriorly and proximally. The pin is over-reamed with a size 11 half reamer to a depth of 30 mm, and a passing stitch is placed at the end of the pin, pulled through to the lateral femoral cortex, and used to deliver one of the Achilles tendon graft bone blocks into the tunnel. The graft is then secured with an 8 × 25-mm interference screw (SoftSilk 1.5 Fixation Screws; Smith & Nephew, Andover, MA) on the femur (Fig. 4B).
Fig 4.
Preparation of the femoral side for the left knee superficial medial collateral ligament (sMCL) and posterior oblique ligament (POL) tunnels and graft placement. (A) The femoral origin of the sMCL is performed with a guide pin introduced at the previously exposed point on the femur bicortically. (B) Once the Achilles tendon allograft bone block is pulled into the tunnel, the graft is secured with an 8 × 25-mm interference screw (SoftSilk 1.5 Fixation Screws; Smith & Nephew) on the femur. (C) Using the second prepared portion of the split Achilles allograft, the 11 × 25-mm bone block and associated soft tissue for the new POL is delivered into the previously established bone tunnel and secured with an 8 × 25-mm interference screw. (D) A plane is made deep to the medial retinacular tissues, but superficial to the semimembranosus, to deliver the POL graft distally. In a similar fashion, the free end of the sMCL graft is passed distally, deep to the medial retinacular tissues.
A second tunnel is then drilled at the femoral origin of the posterior oblique ligament (POL) 1.4 mm distal and 2.9 mm anterior to the gastrocnemius tubercle, bicortically across the distal femur to avoid tunnel convergence with the now fixed femoral sMCL allograft bone block. The pin is over-reamed with an 11-mm half reamer, and a passing stitch is placed through the guide pin to help with subsequent graft passage. Using a curved clamp, a plane is created deep to the medial retinacular tissues, and the free end of the sMCL graft is passed distally. A ruler is used again to measure and confirm the location of the distal sMCL tibial attachment.
Using the second, prepared portion of the split Achilles allograft, the POL is reconstructed at the proximal femur. The 11 × 25-mm bone block is delivered into the previously established bone tunnel and secured with an 8 × 25-mm interference screw (SoftSilk 1.5 Fixation Screws; Smith & Nephew) (Fig. 4C). The tibial insertion of the POL is then identified along the same AP position along the medial tibia and just proximal to the upper border of the semimembranosus insertion approximately 10 to 12 mm distal to the joint line. Similar to the steps taken with the sMCL graft, a plane is made deep to the medial retinacular tissues but superficial to the semimembranosus, to deliver the POL graft distally (Fig. 4D).
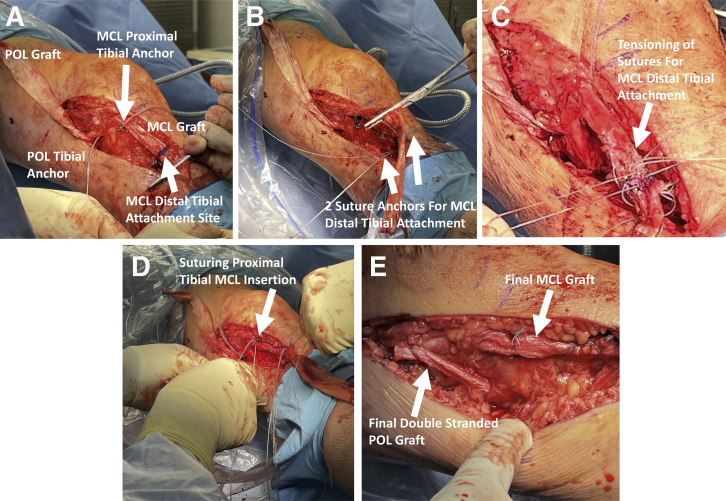
Tibial Fixation of the sMCL and POL grafts
At this point, focus is turned to fixation of both grafts on the tibia. A 2.8-mm all-suture anchor (Q-FIX; Smith & Nephew, Watford, UK) is placed at the previously identified proximal sMCL as well as at the POL attachment on the tibia. A final measurement of the sMCL graft is taken to ensure adequate graft length extending to the distal sMCL attachment site, and the graft is marked with a surgical marker (Fig. 5A).
Fig 5.
Tibial fixation of the left knee superficial medial collateral ligament (sMCL) and posterior oblique ligament (POL) allografts. (A) A 2.8-mm all-suture anchor (Q-FIX; Smith & Nephew) is placed at the previously identified proximal sMCL as well as at the POL attachments on the tibia. (B) If loosening of the staple at the distal sMCL insertion site is appreciated, the sMCL graft is secured with two 2.8-mm all-suture anchors. (C) The matching suture limbs of the two 2.8-mm all-suture anchors are passed from distal to proximal through the tendon in a Krakow fashion, tension is applied to the post limbs, the graft is reduced to the tibia, and suture limbs are tied. (D) The proximal tibial sMCL attachment is then secured using sutures from the previously placed anchor. Sutures are passed through the Achilles allograft in a mattress fashion and tied. (E) The POL graft is secured to the tibia with the suture limbs passed in a mattress fashion through the graft and tied with the knee in full extension while a varus force is applied. The free POL graft limb is folded on top of itself to produce a double-stranded reconstruction of the POL. A high-strength suture (no. 2 FiberWire; Arthrex) is used to secure the 2 folded limbs of the graft together and reinforce the posterior capsule.
It is the senior author’s preferred technique to use a staple (Richards Staple System; Smith & Nephew) to fix the distal sMCL to the tibia owing to the lower implant costs and strong fixation method. However, during this step of the procedure, if there is evidence of loosening of the staple in the proximal tibial bone, the decision can be made to secure the sMCL graft with two 2.8-mm all-suture anchors (Q-FIX; Smith & Nephew) (Fig. 5B).
From each double-loaded 2.8-mm all-suture anchor, 2 free limbs are selected and marked as the post limbs. The matching suture limbs are passed from distal to proximal through the tendon in a Krakow fashion. The sMCL graft is tensioned and pulled distally, in line with its fibers, during suture passage. The post limbs are then passed from deep to superficial through the tendon at the anatomic insertion point on the tibia. Tension is applied to the post limbs, the graft is reduced to the tibia, and suture limbs are tied with the knee in 30° of flexion and a varus stress (Fig. 5C).
The proximal tibial sMCL attachment is then secured using sutures from the previously placed anchor (Fig. 5D). Sutures are passed through the Achilles allograft in a mattress fashion and tied. Sutures limbs are cut, and any additional graft is excised.
Finally, the POL graft is secured to the tibia with the suture limbs passed in a mattress fashion, through the graft, and tied with the knee in full extension while a varus force is applied. The knee is examined and found to have improved stability with the application of a valgus force. Given the extent of residual allograft remaining, the free graft limb is folded on top of itself to produce a double-stranded reconstruction of the POL. A high-strength suture (no. 2 FiberWire; Arthrex, Naples, FL) is used to secure the 2 folded limbs of the graft together and reinforce the posterior capsule (Fig. 5E). The wound is thoroughly irrigated, and care is taken to repair the previously elevated pes tendons distally to the remaining sartorial fascia. The wound is then closed in a layered fashion.
Rehabilitation
Postoperatively, the patient is made weightbearing as tolerated with crutches and placed in a hinged knee brace locked in extension. The patient is provided with DVT prophylaxis for a period of 4 weeks postoperatively. Physical therapy is started after surgery to focus on gait mechanics, range of motion, and isometric strengthening, with the goal of achieving 90° of knee flexion by 2 weeks postoperatively. At the first postoperative appointment, 10 to 14 days after surgery, radiographs are obtained to ensure proper hardware placement and confirm there is no disruption to the TKA prosthesis. At 6 weeks postoperatively, the brace can be discontinued, and the patient is allowed to initiate closed chain strengthening and biking, with an expected return to running or higher-level activities at 24 weeks.
Discussion
The MCL, POL, and associated posteromedial structures are essential to valgus and rotational stability of the knee.4,9,10 A number of studies in the non-arthroplasty literature have suggested that the MCL demonstrates considerable capacity to heal following injury.21 However, in the setting of multiligament knee injury, nonoperative treatment can result in recurrent valgus and rotational instability.22 The MCL is critical for the function and longevity of a primary, non-constrained total knee prosthesis.23 Loss of integrity and stability provided by the MCL can lead to reduced function, early loosening, and accelerated polyethylene wear.24
Injury to the posteromedial complex of the knee in the setting of TKA is not well understood. In a standard medial release for varus osteoarthritis during primary TKA, the deep MCL is partially released off of the proximal tibia during the initial exposure. This is usually followed by removal of osteophytes from the medial tibia and femur, all of which decrease tension on the MCL, with the goal of reconstructing balance of the knee and maintaining coronal stability.24 The reported incidence of complete MCL injury in the setting of TKA varies greatly, ranging from 0.8% to 2.7%,24, 25, 26 with higher risk of intraoperative injury in revision procedures or morbidly obese patients.26 The optimal management of intraoperative iatrogenic MCL injury remains controversial, and even less literature exists regarding MCL injury after TKA. In general, most options are surgical and include an increase in polyethylene liner thickness, primary repair, augmentation with a graft, fixation with screw and washer techniques, or an increase in prosthetic constraint.19,25,27
Primary repair of the MCL can be performed intraoperatively at the time of TKA if an iatrogenic injury occurs. These repairs are usually in the form of direct suture repair or suture anchor fixation for midsubstance tears or avulsion injuries, respectively. Bohl et al. reported 48 cases of primary repair of intraoperative MCL injuries with no subjective or objective instability at 2 years.25 Other studies suggest less favorable outcomes after primary repair, as Lee and Lotke28 noted that 4 of 7 knees underwent revision for instability at an average of 50 months after primary MCL repair. Some argue that primary repair results are superior in cruciate retaining knee designs, since the posterior cruciate ligament acts as a secondary medial stabilizer, conferring additional stability.25
In patients with a history of varus osteoarthritis, the MCL can be contracted and shortened, making direct repair difficult after injury. Augmentation or reconstruction with allograft, autograft, or synthetic tendon techniques have been described, with good results reported in small series.27,29 Wierer et al. reported a single case of early valgus instability after primary TKA treated with MCL reconstruction using a semitendinosus autograft.30 At 24 months, the patient had no clinical or radiographic valgus instability, with an improvement in Lysholm score from 27 to 86.30
Conversion to a more constrained prosthesis typically involves using a larger polyethylene with a post to substitute for the MCL and provide varus-valgus balance.31 While the use of constrained implants has the advantage of providing immediate stability without the need for ligamentous healing and bracing, these implants have several disadvantages.19 Such constrained implants require augmented fixation through stemmed components and a larger resection of intercondylar bone to make room for the post, resulting in significant bone loss should additional revision surgery be required.25 Additional constraint also increases both polyethylene wear and stress at the bone-cement and cement-implant interfaces, thus potentially increasing the risk of aseptic loosening and limiting the longevity of reconstruction. The use of constrained implants is generally discouraged in the primary setting when less constrained options are available and can adequately restore knee stability, particularly in young, active patients.31
Data are sparse regarding management of posteromedial ligament complex injures after TKA. The case presented here illustrates the role for MCL and POL reconstruction with Achilles allograft for valgus instability in young patients after TKA. Table 1 lists the salient pearls and pitfalls of this technique. Patients presenting with valgus instability after TKA should consider the risks, benefits, and their own long-term functional goals when deciding between revision arthroplasty and ligament reconstruction options.
Table 1.
Pearls and pitfalls
| Pearls |
|
|
|
|
|
|
| Pitfalls |
|
|
|
|
When performing an examination under anesthesia, it is crucial to test for valgus instability at both full extension and 30° flexion to delineate between an isolated MCL tear or the presence of a concomitant POL injury. During the initial dissection of the posteromedial side of the knee, the more proximal sMCL tibial insertion is identified using the semimembranosus as an anatomic landmark. The Achilles allograft should be accurately marked for the new sMCL graft length to ensure proper valgus restraint. While securing the POL graft back to the tibia, the knee should be placed in full extension while a varus force is applied. The surgeon should anticipate poor fixation in osteoporotic bone, and suture anchors should be available if Richards staples are not adequate. Furthermore, preoperative planning must consider the location of the femoral prosthesis and avoid femoral tunnel convergence for POL and sMCL tunnels.
Table 2 outlines the major advantages and disadvantages of this surgical technique. This technique is a viable option in young, active patients hoping to avoid the risks associated with revision arthroplasty and restore valgus stability. The large Achilles allograft for the POL can be folded, producing a double-stranded reconstruction, further reinforcing the posterior capsule of the knee. Multidisciplinary orthopaedic care is often required in these situations, given the relative lack of experience TKA surgeons may have in managing POL injuries. Lastly, despite reconstruction of the posteromedial structures, any remaining valgus instability may accelerate the need for revision arthroplasty through accelerated wear.
Table 2.
Advantages and limitations
| Advantages |
|
|
|
| Limitations |
|
|
|
Patients with POL and MCL injury in the setting of a previous TKA represent a unique subset of patients with multiple treatment options. Shared decision making prioritizing the patient’s functional goals is needed to maximize clinical outcomes and limit the need for revision arthroplasty.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: J.C. reports paid consultant, Conmed Linvatec, Ossur, Smith & Nephew; board or committee member, American Orthopaedic Society for Sports Medicine, Arthroscopy Association of North America, International Society of Arthroscopy, Knee Surgery, and Orthopedic Sports Medicine. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
In this Technical Note, we describe the preoperative evaluation, decision making, and surgical technique for a left knee anatomic reconstruction of the superficial medial collateral ligament and posterior oblique ligament with an Achilles allograft in young, active patients after a valgus injury who had previously undergone a total knee arthroplasty.
References
- 1.LaPrade R.F., Chahla J. Nova Science Publishers; Hauppauge, NY: 2018. The medial collateral ligament and the posteromedial corner: A comprehensive analysis. [Google Scholar]
- 2.LaPrade R.F., Engebretsen A.H., Ly T.V., Johansen S., Wentorf F.A., Engebretsen L. The anatomy of the medial part of the knee. J Bone Joint Surg Am. 2007;89:2000–2010. doi: 10.2106/JBJS.F.01176. [DOI] [PubMed] [Google Scholar]
- 3.Wijdicks C.A., Griffith C.J., LaPrade R.F., et al. Radiographic identification of the primary medial knee structures. J Bone Joint Surg Am. 2009;91:521–529. doi: 10.2106/JBJS.H.00909. [DOI] [PubMed] [Google Scholar]
- 4.Wijdicks C.A., Griffith C.J., Johansen S., Engebretsen L., LaPrade R.F. Injuries to the medial collateral ligament and associated medial structures of the knee. J Bone Joint Surg Am. 2010;92:1266–1280. doi: 10.2106/JBJS.I.01229. [DOI] [PubMed] [Google Scholar]
- 5.LaPrade M.D., Kennedy M.I., Wijdicks C.A., LaPrade R.F. Anatomy and biomechanics of the medial side of the knee and their surgical implications. Sports Med Arthrosc Rev. 2015;23:63–70. doi: 10.1097/JSA.0000000000000054. [DOI] [PubMed] [Google Scholar]
- 6.Tibor L.M., Marchant M.H., Jr., Taylor D.C., Hardaker W.T., Jr., Garrett W.E., Jr., Sekiya J.K. Management of medial-sided knee injuries, part 2: Posteromedial corner. Am J Sports Med. 2011;39:1332–1340. doi: 10.1177/0363546510387765. [DOI] [PubMed] [Google Scholar]
- 7.Griffith C.J., LaPrade R.F., Johansen S., Armitage B., Wijdicks C., Engebretsen L. Medial knee injury: Part 1, static function of the individual components of the main medial knee structures. Am J Sports Med. 2009;37:1762–1770. doi: 10.1177/0363546509333852. [DOI] [PubMed] [Google Scholar]
- 8.Wijdicks C.A., Ewart D.T., Nuckley D.J., Johansen S., Engebretsen L., Laprade R.F. Structural properties of the primary medial knee ligaments. Am J Sports Med. 2010;38:1638–1646. doi: 10.1177/0363546510363465. [DOI] [PubMed] [Google Scholar]
- 9.D’Ambrosi R., Corona K., Guerra G., Rubino M., Di Feo F., Ursino N. Biomechanics of the posterior oblique ligament of the knee. Clin Biomech (Bristol, Avon) 2020;80:105205. doi: 10.1016/j.clinbiomech.2020.105205. [DOI] [PubMed] [Google Scholar]
- 10.Griffith C.J., Wijdicks C.A., LaPrade R.F., Armitage B.M., Johansen S., Engebretsen L. Force measurements on the posterior oblique ligament and superficial medial collateral ligament proximal and distal divisions to applied loads. Am J Sports Med. 2009;37:140–148. doi: 10.1177/0363546508322890. [DOI] [PubMed] [Google Scholar]
- 11.Engebretsen L., Lind M. Anteromedial rotatory laxity. Knee Surg Sports Traumatol Arthrosc. 2015;23:2797–2804. doi: 10.1007/s00167-015-3675-8. [DOI] [PubMed] [Google Scholar]
- 12.Wijdicks C.A., Griffith C.J., LaPrade R.F., et al. Medial knee injury: Part 2, load sharing between the posterior oblique ligament and superficial medial collateral ligament. Am J Sports Med. 2009;37:1771–1776. doi: 10.1177/0363546509335191. [DOI] [PubMed] [Google Scholar]
- 13.Giannotti B.F., Rudy T., Graziano J. The non-surgical management of isolated medial collateral ligament injuries of the knee. Sports Med Arthrosc Rev. 2006;14:74–77. doi: 10.1097/01.jsa.0000212307.54947.e4. [DOI] [PubMed] [Google Scholar]
- 14.Walsh S., Frank C., Hart D. Immobilization alters cell metabolism in an immature ligament. Clin Orthop Relat Res. 1992;277:277–288. [PubMed] [Google Scholar]
- 15.Padgett L.R., Dahners L.E. Rigid immobilization alters matrix organization in the injured rat medial collateral ligament. J Orthop Res. 1992;10:895–900. doi: 10.1002/jor.1100100619. [DOI] [PubMed] [Google Scholar]
- 16.Amiel D., Akeson W.H., Harwood F.L., Frank C.B. Stress deprivation effect on metabolic turnover of the medial collateral ligament collagen. A comparison between nine- and 12-week immobilization. Clin Orthop Relat Res. 1983;172:265–270. [PubMed] [Google Scholar]
- 17.Vosoughi F., Rezaei Dogahe R., Nuri A., Ayati Firoozabadi M., Mortazavi J. Medial collateral ligament injury of the knee: A review on current concept and management. Arch Bone Joint Surg. 2021;9:255–262. doi: 10.22038/abjs.2021.48458.2401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.LaPrade R.F., DePhillipo N.N., Dornan G.J., et al. Comparative outcomes occur after superficial medial collateral ligament augmented repair vs reconstruction: A prospective multicenter randomized controlled equivalence trial. Am J Sports Med. 2022 doi: 10.1177/03635465211069373. [DOI] [PubMed] [Google Scholar]
- 19.Shahi A., Tan T.L., Tarabichi S., Maher A., Della Valle C., Saleh U.H. Primary repair of iatrogenic medial collateral ligament injury during TKA: A modified technique. J Arthroplasty. 2015;30:854–857. doi: 10.1016/j.arth.2014.12.020. [DOI] [PubMed] [Google Scholar]
- 20.D’Ambrosi R., Corona K., Guerra G., et al. Posterior oblique ligament of the knee: State of the art. EFORT Open Rev. 2021;6:364–371. doi: 10.1302/2058-5241.6.200127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smyth M.P., Koh J.L. A review of surgical and nonsurgical outcomes of medial knee injuries. Sports Med Arthrosc Rev. 2015;23:e15–e22. doi: 10.1097/JSA.0000000000000063. [DOI] [PubMed] [Google Scholar]
- 22.Dwyer T., Whelan D. Anatomic considerations in multiligament knee injury and surgery. J Knee Surg. 2012;25:263–274. doi: 10.1055/s-0032-1326996. [DOI] [PubMed] [Google Scholar]
- 23.Iizawa N., Mori A., Majima T., Kawaji H., Matsui S., Takai S. Influence of the medial knee structures on valgus and rotatory stability in total knee arthroplasty. J Arthroplasty. 2016;31:688–693. doi: 10.1016/j.arth.2015.09.027. [DOI] [PubMed] [Google Scholar]
- 24.Cheung A., Yan C.H., Chan P.K., Chiu K.Y. The medial collateral ligament in primary total knee arthroplasty: Anatomy, biomechanics, and injury. J Am Acad Orthop Surg. 2020;28:e510–e516. doi: 10.5435/JAAOS-D-19-00355. [DOI] [PubMed] [Google Scholar]
- 25.Bohl D.D., Wetters N.G., Del Gaizo D.J., Jacobs J.J., Rosenberg A.G., Della Valle C.J. Repair of intraoperative injury to the medial collateral ligament during primary total knee arthroplasty. J Bone Joint Surg Am. 2016;98:35–39. doi: 10.2106/JBJS.O.00721. [DOI] [PubMed] [Google Scholar]
- 26.Rajkumar N., Soundarrajan D., Dhanasekararaja P., Rajasekaran S. Influence of intraoperative medial collateral ligament bony avulsion injury on the outcome of primary total knee arthroplasty. J Arthroplasty. 2021;36:1284–1294. doi: 10.1016/j.arth.2020.10.051. [DOI] [PubMed] [Google Scholar]
- 27.Jung K.A., Lee S.C., Hwang S.H., Jung S.H. Quadriceps tendon free graft augmentation for a midsubstance tear of the medial collateral ligament during total knee arthroplasty. Knee. 2009;16:479–483. doi: 10.1016/j.knee.2009.04.007. [DOI] [PubMed] [Google Scholar]
- 28.Lee G.C., Lotke P.A. Management of intraoperative medial collateral ligament injury during TKA. Clin Orthop Relat Res. 2011;469:64–68. doi: 10.1007/s11999-010-1502-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shahi A., Kheir M.M., Tarabichi M., Hosseinzadeh H.R.S., Tan T.L., Parvizi J. Serum D-dimer test is promising for the diagnosis of periprosthetic joint infection and timing of reimplantation. J Bone Joint Surg Am. 2017;99:1419–1427. doi: 10.2106/JBJS.16.01395. [DOI] [PubMed] [Google Scholar]
- 30.Wierer G., Runer A., Hoser C., Gföller P., Fink C. Anatomic MCL reconstruction following TKA. Knee. 2016;23:911–914. doi: 10.1016/j.knee.2016.06.006. [DOI] [PubMed] [Google Scholar]
- 31.Adravanti P., Vasta S. Varus-valgus constrained implants in total knee arthroplasty: Indications and technique. Acta Biomed. 2017;88(2 suppl):112–117. doi: 10.23750/abm.v88i2-S.6521. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
In this Technical Note, we describe the preoperative evaluation, decision making, and surgical technique for a left knee anatomic reconstruction of the superficial medial collateral ligament and posterior oblique ligament with an Achilles allograft in young, active patients after a valgus injury who had previously undergone a total knee arthroplasty.
In this Technical Note, we describe the preoperative evaluation, decision making, and surgical technique for a left knee anatomic reconstruction of the superficial medial collateral ligament and posterior oblique ligament with an Achilles allograft in young, active patients after a valgus injury who had previously undergone a total knee arthroplasty.