Abstract
Several techniques for patellar fixation for reconstruction of the medial patellofemoral ligament (MPFL) have been described in the literature. Despite the success of MPFL reconstruction reported in the literature, there is insufficient evidence to recommend a standard method of patellar fixation. A hybrid 2-point fixation technique allows for increased contact area and contact pressure between the insertion of the graft and the patella and offers a broad insertion of the graft onto the width of the patella, thus allowing for a more native attachment site to be re-created. The technique involves 2 suture anchors to increase graft compression onto the patella. This construct increases the primary load to failure of the repair, increases the surface contact area, and increases the stability of the MPFL reconstruction. These mechanical advantages decrease the chance of recurrent patellar instability and the chance of patellar fracture by avoiding transpatellar fixation.
Technique Video
Patellar graft fixation during medial patellofemoral ligament reconstruction using hybrid 2-point fixation technique of senior author. The step-by-step process for the open portion of the procedure is outlined. After visualization of the joint space arthroscopically, a 3- to 4-cm longitudinal incision is made over the superior border of the patella, and dissection is performed past layers 1 and 2. By use of a 2.4-mm drill bit, the proximal anchor is placed at the superior one-third of the proximal patella. The drill bit is used to create a blind tunnel, and a 3.0-mm suture is then drilled into the blind tunnel until it is fully seated. Biplanar intraoperative fluoroscopy is used to confirm the anchor position with the bone and assess the height of the anchor. On the basis of the position of the first anchor, the second anchor can then be placed appropriately to re-create the anatomy. This process is repeated for placement of the distal anchor, which is about 0.75 cm distal to the proximal anchor. During placement of the proximal and distal suture anchors, counterpressure is placed on the lateral border of the patella for increased stability. Once the suture anchors on the patella are placed, the semitendinosus allograft is sutured onto the medial border of the patella to create a “parachute.” The graft is then transferred between layers 2 and 3 of the medial knee toward the distal femoral insertion site. Under fluoroscopic guidance, the Schöttle point is determined for graft placement at the femoral attachment site. An interference screw is then placed within the reamed tunnel while the knee is positioned at between 30° and 45° of flexion.
Various techniques for patellar fixation for reconstruction of the medial patellofemoral ligament (MPFL) have been described in the literature, each with its advantages and disadvantages. The techniques described vary by the use of suture anchors, interference screws, and transpatellar bone tunnels.1 Despite the success of MPFL reconstruction reported in the literature, there is insufficient evidence to recommend a standard method of patellar fixation.2 Transpatellar bone tunneling is the most common technique used by surgeons, but recent studies have shown an increase in the incidence of patellar instability and patellar fracture in patients who undergo MPFL reconstruction with transpatellar bone tunnels.3,4 Parikh et al.5 reported patellar fractures in 6 of 179 young patients who underwent MPFL reconstruction via a transpatellar bone tunnel approach for patellar fixation. These findings suggest that other approaches for patellar fixation that do not violate the patellar cortex should be considered for MPFL reconstruction.
Biomechanical studies have shown that a nonanatomic surgical reconstruction can cause aberrant restraining forces and nonphysiological patellofemoral kinematics.6, 7, 8 Therefore, restoring the native load distribution seen on the patella is critical during patellar fixation in MPFL reconstruction. The MPFL fans out and has multiple attachments along the medial border of the patella.9 Current patellar fixation techniques use 1 or 2 points of fixation to anchor the graft to the patella. These constructs are mechanically different from the native MPFL insertion on the patella and can prevent the patella from experiencing an optimal force distribution. Proper patellar fixation should include a graft-to-bone insertion that spans an area similar to the area of the native MPFL patellar insertion site.
The contact surface area of graft on bone contributes to the process of “ligamentization,” which is seen in anterior cruciate ligament graft fixation. This phenomenon involves the integration of tendon grafts through tissue composed of fibers anchored to the mineralized bone in a Sharpey fiber–like pattern.10 The contact surface area between graft and bone is critical for the formation of this tissue that allows for integration of the graft. Therefore, increasing the contact surface area during MPFL reconstruction can lead to an optimal environment for graft integration and increased patellar stability.
We present a hybrid 2-point fixation technique that allows for increased contact area and contact pressure between the insertion of the graft and the patella and offers a broad insertion of the graft onto the width of the patella, thus allowing for a more native attachment site to be re-created. The technique involves 2 suture anchors to increase graft compression onto the patella. This construct increases the primary load to failure of the repair, increases the surface contact area, and increases the stability of the MPFL reconstruction. These mechanical advantages decrease the chance of recurrent patellar instability and the chance of patellar fracture by avoiding transpatellar fixation.
Surgical Technique
Preoperative Assessment
History and Physical Examination
Lateral patellar dislocations comprise most patellar dislocations, with a predilection for younger female patients aged less than 25 years.11 Patients who experience a subsequent patellar dislocation after an initial dislocation have a 50% chance of recurrent episodes.12 There may be a history of direct trauma to the medial aspect of the knee in younger patients who experience recurrent dislocations during athletic activity. The physical examination may show a patella palpable laterally with the knee held in 20° to 30° of flexion. Additionally, there may be a positive patellar apprehension test finding, a positive J-sign finding, and more than 2 quadrants of lateral patellar translation.
Imaging Studies
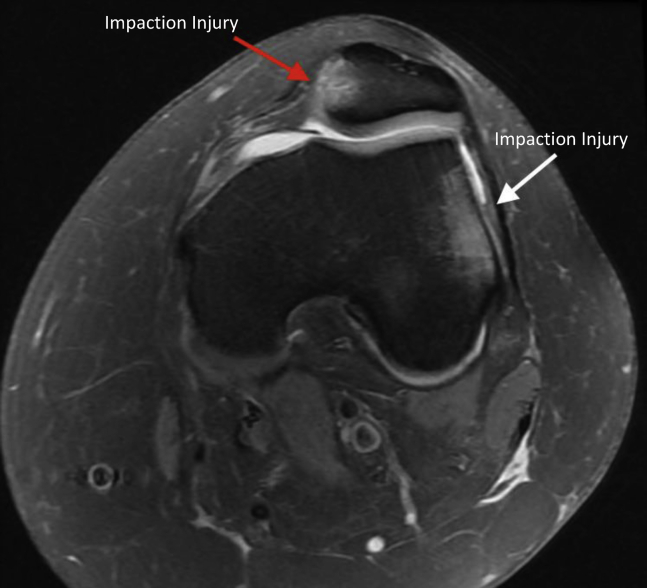
Plain radiographs of the knee are obtained and include anteroposterior, lateral, and skyline Laurin views. In our practice, advanced imaging consisting of magnetic resonance imaging (MRI) is used to evaluate the patient’s anatomy and associated injuries within the vicinity of the MPFL insertion site and the femoral condyle, as shown in Figure 1. MRI is useful for identifying additional chondral and osteochondral injuries, as well as any intra-articular fragments or other meniscal or ligamentous injuries. MRI may also reveal increased T2 signaling within the marrow of the patella’s corresponding femoral surface, indicative of impaction injuries.
Fig 1.
Preoperative cross-sectional view of the left knee on magnetic resonance imaging (T2 sequence) showing attenuation of the midsubstance of the medial patellofemoral ligament with surrounding edema. The increased T2 signal seen within the marrow of the medial patella (red arrow) and lateral femoral condyle (white arrow) is consistent with impaction injuries. Bone edema of the lateral femoral condyle is a result of impaction of the patella and is common in patients with a prior patellar dislocation. Magnetic resonance imaging is used to evaluate the patient’s anatomy and associated injuries within the vicinity of the medial patellofemoral ligament insertion site and the femoral condyle.
Surgical Setup and Preoperative Examination
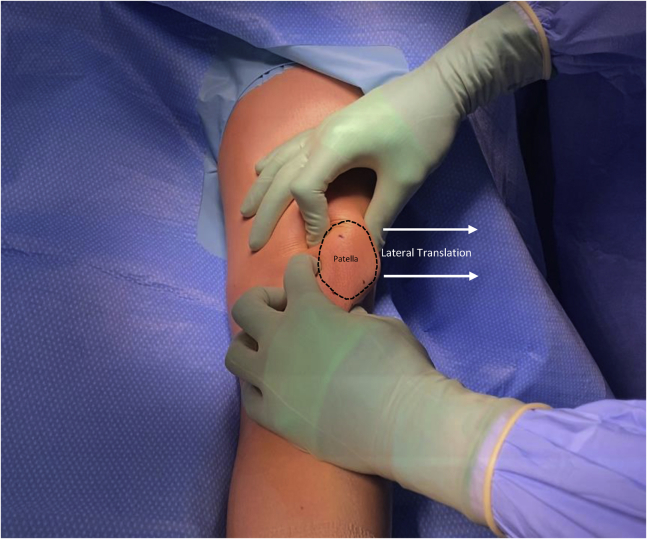
The patient is positioned supine on the operating room table, and general anesthesia is induced. The appropriate extremity is prepared and draped in the normal sterile fashion. An examination of the knee is performed, and patellar maltracking and instability are further assessed, as shown in Figure 2.
Fig 2.
Intraoperative examination of patellar maltracking and instability of the left knee showing more than 2 quadrants of lateral patellar translation. The black dashed line indicates the patella, and the white arrows indicate lateral translation. The examination is performed with the patient under anesthesia and positioned supine on the operative table. Medial and lateral patellar translation should be assessed at varying angles of flexion prior to surgery to further evaluate the degree of patellar maltracking. Other examinations that should be performed with the patient under anesthesia include assessments of patellar tilt, passive internal and external rotation of the hip, and the degree of knee flexion at which patellar instability is most appreciated.
Surgical Approach
A standard diagnostic arthroscopy is performed prior to reconstruction of the MPFL.13 A lateral port is used for the diagnostic arthroscopy and allows the surgeon to assess for any potential patellar maltracking and dynamic instability. Furthermore, any intra-articular pathology or loose bodies can be noted and treated prior to proceeding with the open procedure.14
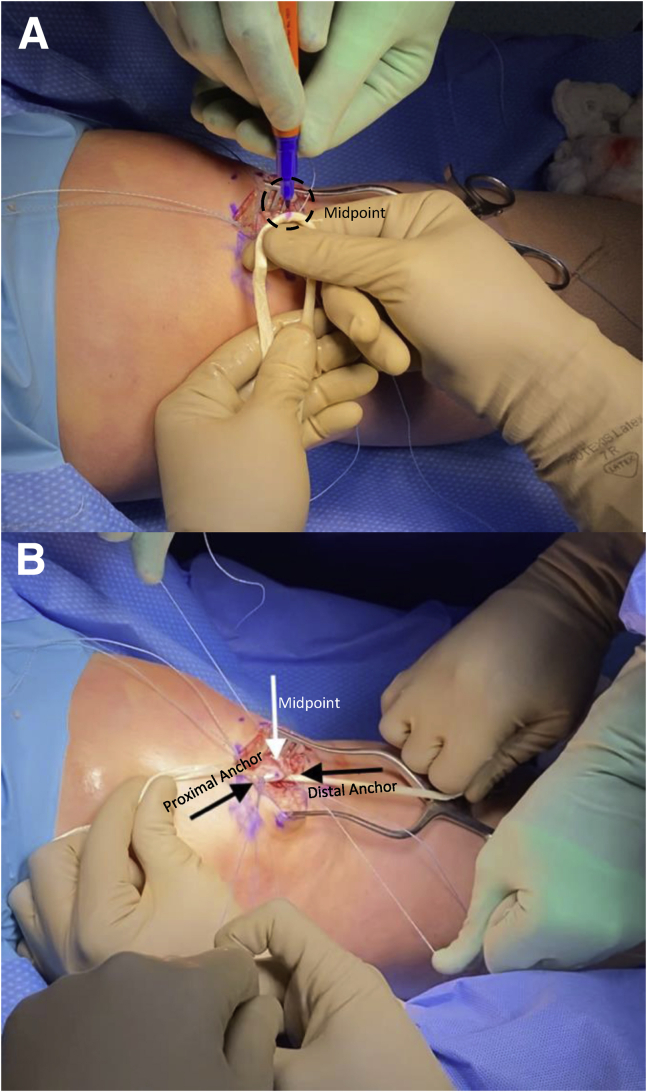
After visualization of the joint space arthroscopically, a 3- to 4-cm longitudinal incision is made over the superior border of the patella, and dissection is performed past layers 1 and 2. By use of a 2.4-mm drill bit, the proximal anchor is placed at the superior one-third of the proximal patella. The drill bit is used to create a blind tunnel, and a 3.0-mm suture anchor (Mitek Surgical Products, Westwood, MA) is then drilled into the blind tunnel until it is fully seated. Biplanar intraoperative fluoroscopy is used to confirm the anchor position with the bone and assess the height of the anchor. On the basis of the position of the first anchor, the second anchor can then be placed appropriately to re-create the anatomy. This process is repeated for placement of the distal anchor, which is about 0.75 cm distal to the proximal anchor. During placement of the proximal and distal suture anchors, counterpressure is placed on the lateral border of the patella for increased stability (Fig 3).
Fig 3.
A 3- to 4-cm longitudinal incision is made over the superior border of the patella (black dashed line) in a left knee, and dissection is performed past layers 1 and 2. By use of a 2.4-mm drill bit, the proximal anchor is placed at the superior one-third of the proximal patella. This process is repeated for placement of the distal anchor, which is about 0.75 cm distal to the proximal anchor. During placement of the proximal and distal suture anchors, counterpressure (white arrow) is placed on the lateral border of the patella for increased stability.
The semitendinosus allograft is folded in half, and the midpoint is marked (Fig 4). The 2 suture anchors are used to secure the ends of the graft and create a “parachute.” An inverted mattress suture is used to secure the graft to the medial edge of the patella, as shown in Video 1. Once patellar graft fixation is confirmed, the femoral insertion site is addressed.
Fig 4.
(A) The midpoint of the semitendinosus graft (black dashed line) is marked using a surgical pen. The mark is used as a reference when placing the graft into the border of the left knee's patella to ensure that the point is equidistant from the proximal and distal anchor sutures. (B) The proximal (left black arrow) and distal (right black arrow) suture anchors are tied down to the medial border of the patella. The marked midpoint (white arrow) is in the middle of the proximal and distal anchor sutures.
Under fluoroscopic guidance, lateral radiographs are obtained to identify the Schöttle point and determine the optimal location for graft placement. The Schöttle point is identified as 1 mm anterior to the posterior cortex extension line, 2.5 mm distal to the posterior origin of the medial femoral condyle, and proximal to the posterior point of the Blumensaat line seen on a lateral radiograph.15 Under fluoroscopy, a Kelly clamp is used to hold a 1.6-mm Kirschner wire (K-wire) at the medial condyle where the insertion point will be placed (Fig 5). The K-wire is drilled once the insertion point has been confirmed. Once the location of the drilled K-wire is determined to be isometric, it is then over-reamed using a cannulated drill bit to create a blind-ended socket. Isometry is determined by wrapping the double-ended portion of the graft around the K-wire and marking a point on the graft that is on either end of the wire. The graft is then held tight around the K-wire while the knee is taken through a range of motion. If the previously made mark moves less than 2 mm across the double-ended graft as the graft is tightened around the K-wire, we consider the tunnel to be sufficiently isometric. The reamer size used by the cannulated drill is the same diameter as the interference screw that will be used.
Fig 5.
Schöttle point (white dashed line) on lateral view of left knee. Under fluoroscopy, a Kelly clamp is used to hold a 1.6-mm Kirschner wire (K-wire) at the medial condyle where the insertion point will be placed. The K-wire is drilled once the insertion point has been confirmed. Once the location of the drilled K-wire is determined to be isometric, it is then over-reamed using a cannulated drill bit to create a blind-ended socket. The Schöttle point is identified as 1 mm anterior to the posterior cortex extension line, 2.5 mm distal to the posterior origin of the medial femoral condyle, and proximal to the posterior point of the Blumensaat line seen on a lateral radiograph.
Attention then returns to the graft. A Kelly clamp is used to create a path to transfer the graft through the tissues between layers 2 and 3 of the medial knee (Fig 6). FiberLoop (Arthrex, Naples, FL) is then used to integrate the 2 free ends of the graft together. The FiberLoop ends are attached to the eyelet of a Beath pin, and the semitendinosus graft is placed inside the drill hole using a Beath pin to shuttle the graft into the tunnel and dock the graft within the blind-ended socket. An interference screw (Mitek Surgical Products) is then placed within the reamed tunnel while the knee is positioned at between 30° and 45° of flexion.
Fig 6.
Dissection through layers 2 and 3 of the left knee should be performed using tonsil forceps passed between both layers. Dissection of both layers should be performed from the patellar incision to the femoral incision to avoid disruption of the insertion site of the vastus medialis on the anterior portion of the medial patellofemoral ligament. A Kelly clamp is used to transfer the suture ends of the semitendinosus graft through layers 2 and 3 (black dashed line) of the medial knee in a lateral-to-medial direction.
After fixation and prior to skin closure, the knee is taken through its full range of motion to assess patellar tracking and stability. Arthroscopy is performed again to ensure that the graft is not intra-articular. Standard wound closure is performed. Of note, layers 1 and 2 are closed as 1 large flap to ensure that the graft has healthy coverage between itself and the subcutaneous layer.
Postoperative Care
Postoperatively, the patient is restricted to toe-touch weight bearing with 0% to 10% of body weight with a brace locked at 0° of extension for the first 2 weeks. Physical training begins after the first postoperative visit and continues until the patient shows more than 90% range of motion and more than 90% quadriceps and hamstring strength compared with the uninvolved side, which can take between 8 and 9 months. After 6 weeks, the patient advances to full weight bearing without assisted devices. After 7 weeks, the patient is weaned from using the range-of-motion knee brace when his or her gait returns to normal and 120° of knee flexion is achieved. The patient is then transitioned to use of a patella stabilizer brace. After 3 months, the patient may begin to run, and at around 8 to 9 months, the patient may return to full-contact sports.
Discussion
Patellar fixation is a critical component during MPFL reconstruction. There are various techniques that may be used to achieve patellar fixation, each with its advantages and disadvantages. Multiple techniques for patellar fixation during MPFL reconstruction have been described in the literature, including the use of suture anchors, interference screws, and transpatellar bone tunnels.1 The most common complications after MPFL reconstruction are patellar fracture and recurrent patellar instability, which have a greater association with transpatellar bone tunnels. Past studies have reported a high rate of patellar fractures in patients with transverse patellar tunnels.4 More recent studies have shown that suture anchors result in a greater degree of improvement in patient-reported outcomes compared with double–transpatellar tunnel fixation.16 However, suture anchors are associated with lower failure loads and stiffness compared with transpatellar bone tunnels and interference screws for patellar fixation.16
Our technique provides a means to avoid using transpatellar bone tunnels while providing adequate patellar stability. This technique re-creates the native stabilizing forces of the patella by anchoring the semitendinosus graft in a manner that fans out and more closely replicates the native insertion of the MPFL. This configuration for graft insertion increases the contact surface area and promotes the process of ligamentization. The increased contact surface area promotes the formation of Sharpey fibers and integration between graft and bone.10
The most important consideration for our proposed technique is the ability to achieve patellar stability without using transpatellar bone tunnels. With our technique, there is not extensive involvement within the cancellous tissue of the patella, which avoids compromising the microenvironment of the patella and avoids potential fractures in the future. The primary advantage of the described technique is the decreased risk of patellar bone fracture by avoiding the use of transpatellar bone tunnels. A relative disadvantage of not using transpatellar bone tunnels is a biomechanically weaker graft construct. However, suture anchors have been shown to have more favorable clinical outcomes, primarily with less reported knee pain, reduced rates of positive apprehension test findings, and reduced rates of revision surgery.17
Advantages and disadvantages of the described procedure are summarized in Table 1, and pearls and pitfalls are presented in Table 2.18 In conclusion, the use of a hybrid 2-point fixation technique during MPFL reconstruction for patellar instability decreases the chance of recurrent patellar instability and the chance of patellar fracture.
Table 1.
Advantages and Disadvantages of MPFL Reconstruction Using Hybrid 2-Point Suture Anchor Technique
| Advantages |
| The use of transpatellar bone tunnels is avoided. |
| The risk of fracture to the patella is decreased. |
| The graft-to-bone contact surface area is increased. |
| The native stabilizing forces on the patella are re-created. |
| Disadvantages |
| The graft construct is biomechanically weaker compared with the use of transpatellar bone tunnels. |
| The MQTFL is not re-created. |
MPFL, medial patellofemoral ligament; MQTFL, medial quadriceps tendon-femoral ligament.
Table 2.
Pearls and Pitfalls of MPFL Reconstruction Using Hybrid 2-Point Suture Anchor Technique
| Pearls |
| A true lateral view of the knee is required to determine the Schöttle point for femoral graft placement. |
| Counterpressure should be placed on the lateral border of the patella during suture anchor placement for increased stability and control. |
| When integrating the free ends of the graft together, one should use 5-7 passes of the FiberLoop. |
| The femoral interference screw should be fixed at 30° to 45° of knee flexion. |
| Pitfalls |
| Over-tensioning the graft can lead to increased medial contact pressure and patellar tilting.16 |
| Delayed advancement of weight-bearing activities can result in prolonged knee stiffness. |
MPFL, medial patellofemoral ligament.
Footnotes
The authors report no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Patellar graft fixation during medial patellofemoral ligament reconstruction of the left knee using hybrid 2-point fixation technique of senior author (B.M.G.). The step-by-step process for the open portion of the procedure is outlined. After visualization of the joint space arthroscopically, a 3- to 4-cm longitudinal incision is made over the superior border of the patella, and dissection is performed past layers 1 and 2. By use of a 2.4-mm drill bit, the proximal anchor is placed at the superior one-third of the proximal patella. The drill bit is used to create a blind tunnel, and a 3.0-mm suture is then drilled into the blind tunnel until it is fully seated. Biplanar intraoperative fluoroscopy is used to confirm the anchor position with the bone and assess the height of the anchor. On the basis of the position of the first anchor, the second anchor can then be placed appropriately to re-create the anatomy. This process is repeated for placement of the distal anchor, which is about 0.75 cm distal to the proximal anchor. During placement of the proximal and distal suture anchors, counterpressure is placed on the lateral border of the patella for increased stability. Once the suture anchors on the patella are placed, the semitendinosus allograft is sutured onto the medial border of the patella to create a “parachute.” The graft is then transferred between layers 2 and 3 of the medial knee toward the distal femoral insertion site. Under fluoroscopic guidance, the Schöttle point is determined for graft placement at the femoral attachment site. An interference screw is then placed within the reamed tunnel while the knee is positioned at between 30° and 45° of flexion.
References
- 1.Godin J.A., Karas V., Visgauss J.D., Garrett W.E. Medial patellofemoral ligament reconstruction using a femoral loop button fixation technique. Arthrosc Tech. 2015;4:e601–e607. doi: 10.1016/j.eats.2015.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.McNeilan R.J., Everhart J.S., Mescher P.K., Abouljoud M., Magnussen R.A., Flanigan D.C. Graft choice in isolated medial patellofemoral ligament reconstruction: A systematic review with meta-analysis of rates of recurrent instability and patient-reported outcomes for autograft, allograft, and synthetic options. Arthroscopy. 2018;34:1340–1354. doi: 10.1016/j.arthro.2017.11.027. [DOI] [PubMed] [Google Scholar]
- 3.Shah J.N., Howard J.S., Flanigan D.C., Brophy R.H., Carey J.L., Lattermann C. A systematic review of complications and failures associated with medial patellofemoral ligament reconstruction for recurrent patellar dislocation. Am J Sports Med. 2012;40:1916–1923. doi: 10.1177/0363546512442330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schiphouwer L., Rood A., Tigchelaar S., Koëter S. Complications of medial patellofemoral ligament reconstruction using two transverse patellar tunnels. Knee Surg Sports Traumatol Arthrosc. 2017;25:245–250. doi: 10.1007/s00167-016-4245-4. [DOI] [PubMed] [Google Scholar]
- 5.Parikh S.N., Nathan S.T., Wall E.J., Eismann E.A. Complications of medial patellofemoral ligament reconstruction in young patients. Am J Sports Med. 2013;41:1030–1038. doi: 10.1177/0363546513482085. [DOI] [PubMed] [Google Scholar]
- 6.Beck P., Brown N.A., Greis P.E., Burks R.T. Patellofemoral contact pressures and lateral patellar translation after medial patellofemoral ligament reconstruction. Am J Sports Med. 2007;35:1557–1563. doi: 10.1177/0363546507300872. [DOI] [PubMed] [Google Scholar]
- 7.DeVries Watson N.A., Duchman K.R., Bollier M.J., Grosland N.M. A finite element analysis of medial patellofemoral ligament reconstruction. Iowa Orthop J. 2015;35:13–19. [PMC free article] [PubMed] [Google Scholar]
- 8.Elias J.J., Cosgarea A.J. Technical errors during medial patellofemoral ligament reconstruction could overload medial patellofemoral cartilage: A computational analysis. Am J Sports Med. 2006;34:1478–1485. doi: 10.1177/0363546506287486. [DOI] [PubMed] [Google Scholar]
- 9.Aframian A., Smith T.O., Tennent T.D., Cobb J.P., Hing C.B. Origin and insertion of the medial patellofemoral ligament: A systematic review of anatomy. Knee Surg Sports Traumatol Arthrosc. 2017;25:3755–3772. doi: 10.1007/s00167-016-4272-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nebelung W., Becker R., Urbach D., Röpke M., Roessner A. Histological findings of tendon-bone healing following anterior cruciate ligament reconstruction with hamstring grafts. Arch Orthop Trauma Surg. 2003;123:158–163. doi: 10.1007/s00402-002-0463-y. [DOI] [PubMed] [Google Scholar]
- 11.Atkin D.M., Fithian D.C., Marangi K.S., Stone M.L., Dobson B.E., Mendelsohn C. Characteristics of patients with primary acute lateral patellar dislocation and their recovery within the first 6 months of injury. Am J Sports Med. 2000;28:472–479. doi: 10.1177/03635465000280040601. [DOI] [PubMed] [Google Scholar]
- 12.Fithian D.C., Paxton E.W., Stone M.L., et al. Epidemiology and natural history of acute patellar dislocation. Am J Sports Med. 2004;32:1114–1121. doi: 10.1177/0363546503260788. [DOI] [PubMed] [Google Scholar]
- 13.Ward B.D., Lubowitz J.H. Basic knee arthroscopy part 3: Diagnostic arthroscopy. Arthrosc Tech. 2013;2:e503–e505. doi: 10.1016/j.eats.2013.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moran T.E., Burke J.F., Diduch D.R. Small (3.2-mm), short, oblique patellar tunnels for patellar fixation in MPFL reconstruction. Arthrosc Tech. 2020;9:e1613–e1617. doi: 10.1016/j.eats.2020.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Schöttle P.B., Hensler D., Imhoff A.B. Anatomical double-bundle MPFL reconstruction with an aperture fixation. Knee Surg Sports Traumatol Arthrosc. 2010;18:147–151. doi: 10.1007/s00167-009-0868-z. [DOI] [PubMed] [Google Scholar]
- 16.Heo J.W., Ro K.H., Lee D.H. Patellar redislocation rates and clinical outcomes after medial patellofemoral ligament reconstruction: Suture anchor versus double transpatellar tunnel fixation. Am J Sports Med. 2019;47:1254–1262. doi: 10.1177/0363546518765458. [DOI] [PubMed] [Google Scholar]
- 17.Migliorini F., Driessen A., Quack V., Schenker H., Tingart M., Eschweiler J. Patellar fixation graft via suture anchors versus tunnel techniques during isolated MPFL reconstruction for recurrent patellofemoral instability: A systematic review of the literature. Arch Orthop Trauma Surg. 2020;140:1201–1210. doi: 10.1007/s00402-020-03420-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stephen J.M., Kaider D., Lumpaopong P., Deehan D.J., Amis A.A. The effect of femoral tunnel position and graft tension on patellar contact mechanics and kinematics after medial patellofemoral ligament reconstruction. Am J Sports Med. 2014;42:364–372. doi: 10.1177/0363546513509230. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Patellar graft fixation during medial patellofemoral ligament reconstruction using hybrid 2-point fixation technique of senior author. The step-by-step process for the open portion of the procedure is outlined. After visualization of the joint space arthroscopically, a 3- to 4-cm longitudinal incision is made over the superior border of the patella, and dissection is performed past layers 1 and 2. By use of a 2.4-mm drill bit, the proximal anchor is placed at the superior one-third of the proximal patella. The drill bit is used to create a blind tunnel, and a 3.0-mm suture is then drilled into the blind tunnel until it is fully seated. Biplanar intraoperative fluoroscopy is used to confirm the anchor position with the bone and assess the height of the anchor. On the basis of the position of the first anchor, the second anchor can then be placed appropriately to re-create the anatomy. This process is repeated for placement of the distal anchor, which is about 0.75 cm distal to the proximal anchor. During placement of the proximal and distal suture anchors, counterpressure is placed on the lateral border of the patella for increased stability. Once the suture anchors on the patella are placed, the semitendinosus allograft is sutured onto the medial border of the patella to create a “parachute.” The graft is then transferred between layers 2 and 3 of the medial knee toward the distal femoral insertion site. Under fluoroscopic guidance, the Schöttle point is determined for graft placement at the femoral attachment site. An interference screw is then placed within the reamed tunnel while the knee is positioned at between 30° and 45° of flexion.
Patellar graft fixation during medial patellofemoral ligament reconstruction of the left knee using hybrid 2-point fixation technique of senior author (B.M.G.). The step-by-step process for the open portion of the procedure is outlined. After visualization of the joint space arthroscopically, a 3- to 4-cm longitudinal incision is made over the superior border of the patella, and dissection is performed past layers 1 and 2. By use of a 2.4-mm drill bit, the proximal anchor is placed at the superior one-third of the proximal patella. The drill bit is used to create a blind tunnel, and a 3.0-mm suture is then drilled into the blind tunnel until it is fully seated. Biplanar intraoperative fluoroscopy is used to confirm the anchor position with the bone and assess the height of the anchor. On the basis of the position of the first anchor, the second anchor can then be placed appropriately to re-create the anatomy. This process is repeated for placement of the distal anchor, which is about 0.75 cm distal to the proximal anchor. During placement of the proximal and distal suture anchors, counterpressure is placed on the lateral border of the patella for increased stability. Once the suture anchors on the patella are placed, the semitendinosus allograft is sutured onto the medial border of the patella to create a “parachute.” The graft is then transferred between layers 2 and 3 of the medial knee toward the distal femoral insertion site. Under fluoroscopic guidance, the Schöttle point is determined for graft placement at the femoral attachment site. An interference screw is then placed within the reamed tunnel while the knee is positioned at between 30° and 45° of flexion.