Abstract
Posterior shoulder instability is becoming increasingly recognized in young active patient populations. Diagnosing posterior instability can be challenging because patients commonly present with a complaint of pain without a history of a dislocation or subluxation event. Additionally, a posterior labral tear is not always clearly visualized on advanced imaging studies. As such, physical examination is critical to the diagnosis. We report a simple physical examination maneuver for the diagnosis of symptomatic posterior shoulder instability. The thumb test attempts to replicate a posterior bone block procedure, helping to re-establish stability and relieve pain. The examiner places his or her thumb over the posterior glenohumeral joint line while the patient actively forward elevates the affected arm overhead. Improvement in pain and stability with this maneuver is diagnostic for symptomatic posterior shoulder instability. This test augments current physical examination maneuvers to assist with correctly diagnosing posterior shoulder instability.
Technique Video
Thumb test in a patient with a symptomatic posterior labral tear in the right shoulder with posterior shoulder instability. The patient has pain and dynamic posterior humeral head translation with active forward elevation and then shows improvement in pain and stability with the thumb test.
Posterior shoulder instability is increasingly recognized as a common cause of instability in young athletic populations.1 Diagnosing symptomatic posterior shoulder instability is often challenging because patients commonly present with pain and no history of a dislocation or subluxation event. Posterior labral tears are not always readily apparent on either magnetic resonance imaging or magnetic resonance arthrogram.2 Furthermore, anterior shoulder pain and tenderness along the bicipital groove are commonly reported.3 Radiographic and advanced imaging parameters such as increased glenoid retroversion, glenoid dysplasia, increased posterior capsular area, and increased posterior acromial height and decreased posterior acromial slope are associated with posterior shoulder instability and can aid clinicians in the diagnosis.4, 5, 6, 7, 8, 9, 10, 11
Physical examination, however, remains the most critical step in the diagnosis of posterior shoulder instability. Prior tests for diagnosing posterior shoulder instability include the jerk test, Kim test, push-pull test, Porcellini test, and posterior load-and-shift test.12, 13, 14 These tests are variably effective in making a definitive diagnosis. This article describes an additional physical examination maneuver, the thumb test, which is simple and effective and can be used to augment current tests in making a diagnosis of posterior shoulder instability. Informed verbal consent was obtained from the patient shown in the figures and Video 1.
Physical Examination Technique
Patient Positioning
The thumb test is performed with the patient in a seated or standing position. The examiner stands behind the patient on the affected side.
Test Steps
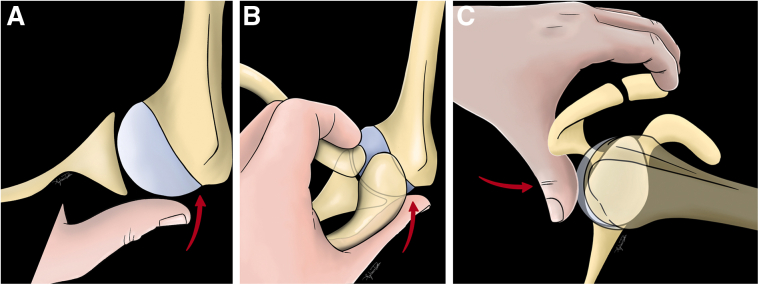
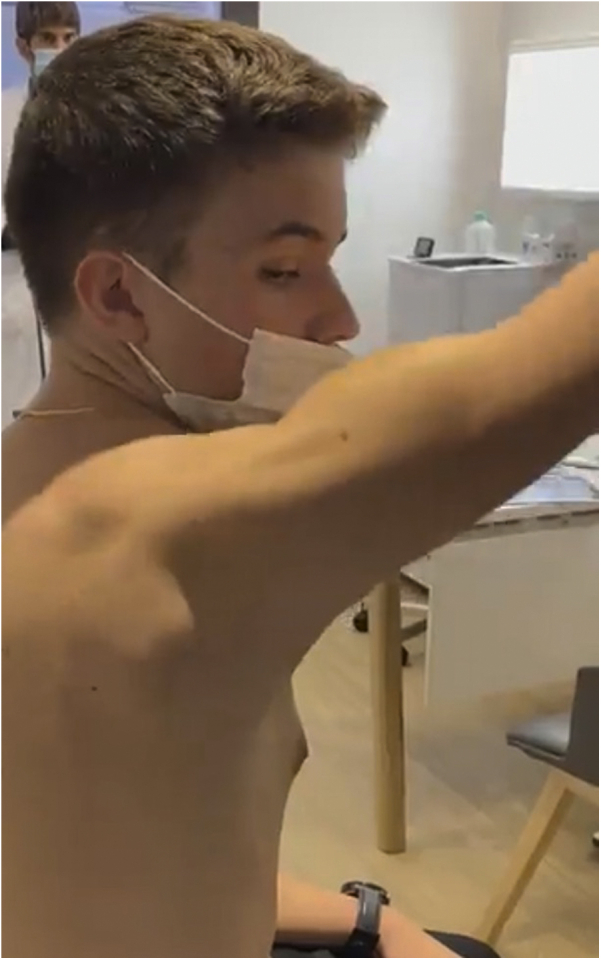
First, the patient is asked to forward elevate the affected arm overhead in neutral adduction (Fig 1). It is noted whether the patient experiences posterior shoulder pain and/or instability with this provocative maneuver. Figure 2 is a pictorial representation of dynamic posterior humeral head translation in the setting of a posterior labral tear that leads to shoulder pain in these patients. Next, standing behind the patient, the examiner uses his or her thumb to stabilize the scapula and places it directly over the posterior glenohumeral joint line. The examiner must place half of the thumb on the posterior glenoid rim and half on the posterior humeral head (Fig 3A). The examiner’s ipsilateral fingers can be used to anchor over the anterior clavicle as a counterforce (Fig 3 B and C). This allows the examiner to press his or her thumb firmly against the glenohumeral joint line, which is meant to act functionally like a posterior bone block. Furthermore, if the patient is very strong and muscular, the examiner can use his or her hands and 2 thumbs to resist the posterior forces. The patient is then asked to repeat the provocative maneuver performed in the first step (Fig 4).
Fig 1.
The examiner stands behind the patient and asks the patient to forward elevate the affected extremity overhead in neutral adduction. In patients with posterior labral tears and posterior instability, this maneuver commonly leads to pain and a sense of posterior shoulder instability or frank subluxation.
Fig 2.
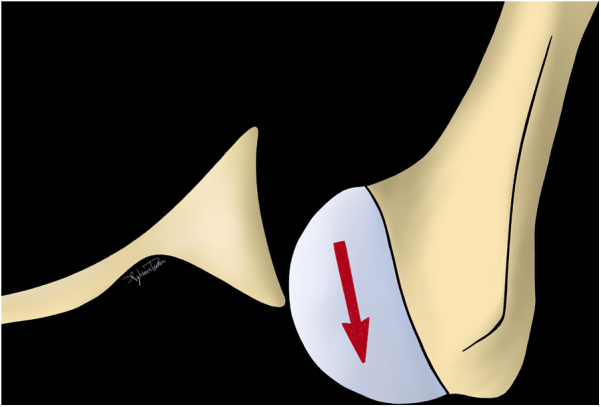
An axial drawing showing that with forward elevation in neutral adduction, dynamic posterior humeral head subluxation occurs that loads the torn posterior labrum and leads to pain and discomfort.
Fig 3.
(A) Axial drawing depicting the thumb test for a right shoulder with placement of the examiner’s thumb over the posterior glenohumeral joint line, which creates a functional posterior “bone block.” (B) Axial drawing depicting the thumb test for a right shoulder with placement of the thumb over the posterior glenohumeral joint line. The examiner uses the fingers from the same hand to anchor to the anterior clavicle as a counterforce. (C) Sagittal drawing depicting the thumb test with the fingers anchored on the anterior clavicle.
Fig 4.

Clinical photograph of the thumb test performed in a patient with posterior shoulder instability of the right shoulder. The patient has relief of pain and instability with this maneuver.
Test Interpretation
The result of the thumb test is considered positive if the patient has relief of posterior shoulder pain and improved stability with or without improvement in range of motion with the thumb in place. Clinically, in the senior author’s clinic, patients with a diagnosis of a posterior labral tear and/or instability with a positive thumb test result were all found to have correlating posterior labral pathology on shoulder arthroscopy requiring repair (Video 1). Pearls and pitfalls of the described technique are presented in Table 1.
Table 1.
Pearls and Pitfalls
| The thumb test is easily performed and less technically challenging given that it is an active maneuver and is less susceptible to patient guarding and apprehension. |
| The examiner must ensure that the thumb is placed directly over the glenohumeral joint line, with half of the thumb contacting the posterior glenoid rim and half of it contacting the medial aspect of the posterior humeral head. |
| This article serves only as a description of this examination technique, and further study is needed to determine sensitivity and specificity. |
Discussion
Historically, posterior shoulder instability was believed to account for only 2% to 10% of all glenohumeral instability.15 However, with increased awareness, it is apparent that posterior shoulder instability may be far more frequent and could comprise as much as 20% of operatively treated instability cases in active young adults.1 Additionally, pathologic activation patterns of muscles can lead to posterior positional functional shoulder instability.16 The accuracy of magnetic resonance imaging for diagnosing posterior labral injuries is lower than for anterior inferior labral pathology.17,18 This highlights the role of the physical examination to assist with diagnosis, but commonly used maneuvers have varying sensitivities and specificities and can be challenging to perform in patients guarding with pain. For instance, the Kim test was found to have 80% sensitivity and 94% specificity and the authors recommended its use in conjunction with the Jerk test to better detect posteroinferior instability.18 In contrast, the jerk test was shown to have a sensitivity of only 73% and specificity of 98%.19
The thumb test is a simple examination maneuver for diagnosing posterior shoulder instability and labral tears as confirmed by arthroscopic findings at the time of surgery by the senior author. The examiner’s thumb functions as a posterior glenoid “bone block,” helping to re-establish stability and relieve pain. Additionally, the thumb test is helpful in confirming the direction of instability, which is not always obvious clinically and on imaging studies in the absence of labral or capsular tears. Overall, this examination is easy to perform and is less limited by patient guarding and apprehension because it is an active examination and not passively performed by the examiner. Limitations currently are a lack of statistical validation with calculated sensitivities and specificities, along with interobserver and intraobserver reliability. Diagnosing posterior labral tears and instability can be challenging, and no test performed alone has shown excellent sensitivity and specificity.20 As such, an examiner must frequently use multiple provocative tests to make the diagnosis. This is the first description of the thumb test, which adds to currently established physical examination maneuvers and aids in the diagnosis of posterior labral tears and symptomatic unidirectional posterior shoulder instability.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: P.B. is a paid consultant for Tornier Stryker and receives royalties from Tornier Stryker, outside the submitted work. G.G. is a paid consultant for Tigon Medical, outside the submitted work. J.W.G. is a paid consultant for FH Ortho, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Thumb test in a patient with a symptomatic posterior labral tear in the right shoulder with posterior shoulder instability. The patient has pain and dynamic posterior humeral head translation with active forward elevation and then shows improvement in pain and stability with the thumb test.
References
- 1.Song D.J., Cook J.B., Krul K.P., et al. High frequency of posterior and combined shoulder instability in young active patients. J Shoulder Elbow Surg. 2015;24:186–190. doi: 10.1016/j.jse.2014.06.053. [DOI] [PubMed] [Google Scholar]
- 2.Teske L.G., Arvesen J., Kissenberth M.J., et al. Athletes diagnosed with anterior and posterior shoulder instability display different chief complaints and disability. J Shoulder Elbow Surg. 2021;30:S21–S26 (suppl). doi: 10.1016/j.jse.2021.04.007. [DOI] [PubMed] [Google Scholar]
- 3.Galvin J.W., Yu H., Slevin J., et al. High incidence of anterior shoulder pain in young athletes undergoing arthroscopic posterior labral repair for posterior shoulder instability. Arthrosc Sports Med Rehabil. 2021;3:e1441–e1447. doi: 10.1016/j.asmr.2021.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Meyer D.C., Ernstbrunner L., Boyce G., Imam M.A., El Nashar R., Gerber C. Posterior acromial morphology is significantly associated with posterior shoulder instability. J Bone Joint Surg Am. 2019;101:1253–1260. doi: 10.2106/JBJS.18.00541. [DOI] [PubMed] [Google Scholar]
- 5.Galvin J.W., Morte D.R., Grassbaugh J.A., Parada S.A., Burns S.H., Eichinger J.K. Arthroscopic treatment of posterior shoulder instability in patients with and without glenoid dysplasia: A comparative outcomes analysis. J Shoulder Elbow Surg. 2017;26:2103–2109. doi: 10.1016/j.jse.2017.05.033. [DOI] [PubMed] [Google Scholar]
- 6.Gottschalk M.B., Ghasem A., Todd D., Daruwalla J., Xerogeanes J., Karas S. Posterior shoulder instability: Does glenoid retroversion predict recurrence and contralateral instability? Arthroscopy. 2015;31:488–493. doi: 10.1016/j.arthro.2014.10.009. [DOI] [PubMed] [Google Scholar]
- 7.Eichinger J.K., Galvin J.W., Grassbaugh J.A., Parada S.A., Li X. Glenoid dysplasia: Pathophysiology, diagnosis, and management. J Bone Joint Surg Am. 2016;98:958–968. doi: 10.2106/JBJS.15.00916. [DOI] [PubMed] [Google Scholar]
- 8.Galvin J.W., Parada S.A., Li X., Eichinger J.K. Critical findings on magnetic resonance arthrograms in posterior shoulder instability compared with an age-matched controlled cohort. Am J Sports Med. 2016;44:3222–3229. doi: 10.1177/0363546516660076. [DOI] [PubMed] [Google Scholar]
- 9.Dewing C.B., McCormick F., Bell S.J., et al. An analysis of capsular area in patients with anterior, posterior, and multidirectional shoulder instability. Am J Sports Med. 2008;36:515–522. doi: 10.1177/0363546507311603. [DOI] [PubMed] [Google Scholar]
- 10.Sheean A.J., Kibler W.B., Conway J., Bradley J.P. Posterior labral injury and glenohumeral instability in overhead athletes: Current concepts for diagnosis and management. J Am Acad Orthop Surg. 2020;28:628–637. doi: 10.5435/JAAOS-D-19-00535. [DOI] [PubMed] [Google Scholar]
- 11.Antosh I.J., Tokish J.M., Owens B.D. Posterior shoulder instability. Sports Health. 2016;8:520–526. doi: 10.1177/1941738116672446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Harryman D.T., II, Sidles J.A., Harris S.L., Matsen F.A., III Laxity of the normal glenohumeral joint: A quantitative in vivo assessment. J Shoulder Elbow Surg. 1992;1:66–76. doi: 10.1016/S1058-2746(09)80123-7. [DOI] [PubMed] [Google Scholar]
- 13.Kim S.H., Park J.C., Park J.S., Oh I. Painful jerk test: A predictor of success in nonoperative treatment of posteroinferior instability of the shoulder. Am J Sports Med. 2004;32:1849–1855. doi: 10.1177/0363546504265263. [DOI] [PubMed] [Google Scholar]
- 14.Morey V.M., Singh H., Paladini P., Merolla G., Phadke V., Porcellini G. The Porcellini test: A novel test for accurate diagnosis of posterior labral tears of the shoulder: Comparative analysis with the established tests. Musculoskelet Surg. 2016;100:199–205. doi: 10.1007/s12306-016-0422-3. [DOI] [PubMed] [Google Scholar]
- 15.Provencher M.T., LeClere L.E., King S., et al. Posterior instability of the shoulder: Diagnosis and management. Am J Sports Med. 2011;39:874–886. doi: 10.1177/0363546510384232. [DOI] [PubMed] [Google Scholar]
- 16.Moroder P., Danzinger V., Maziak N., et al. Characteristics of functional shoulder instability. J Shoulder Elbow Surg. 2020;29:68–78. doi: 10.1016/j.jse.2019.05.025. [DOI] [PubMed] [Google Scholar]
- 17.Chandnani V.P., Yeager T.D., DeBerardino T., et al. Glenoid labral tears: Prospective evaluation with MRI imaging, MR arthrography, and CT arthrography. AJR Am J Roentgenol. 1993;161:1229–1235. doi: 10.2214/ajr.161.6.8249731. [DOI] [PubMed] [Google Scholar]
- 18.Legan J.M., Burkhard T.K., Goff W.B., II, et al. Tears of the glenoid labrum: MR imaging of 88 arthroscopically confirmed cases. Radiology. 1991;179:241–246. doi: 10.1148/radiology.179.1.2006284. [DOI] [PubMed] [Google Scholar]
- 19.Kim S.H., Park J.S., Jeong W.K., Shin S.K. The Kim test: A novel test for posteroinferior labral lesion of the shoulder—A comparison to the jerk test. Am J Sports Med. 2005;33:1188–1192. doi: 10.1177/0363546504272687. [DOI] [PubMed] [Google Scholar]
- 20.Sheean A.J., Arner J.W., Bradley J.P. Posterior glenohumeral instability: Diagnosis and management. Arthroscopy. 2020;36:2580–2582. doi: 10.1016/j.arthro.2020.05.018. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Thumb test in a patient with a symptomatic posterior labral tear in the right shoulder with posterior shoulder instability. The patient has pain and dynamic posterior humeral head translation with active forward elevation and then shows improvement in pain and stability with the thumb test.
Thumb test in a patient with a symptomatic posterior labral tear in the right shoulder with posterior shoulder instability. The patient has pain and dynamic posterior humeral head translation with active forward elevation and then shows improvement in pain and stability with the thumb test.