Abstract
Heterotaxy syndrome is a rare congenital heart disease with a disarrangement of the heart and abdominal organs. We present a young African female with features of heart failure, diffuse irregular cardiac murmurs, and palpable, tender epigastric mass. A chest and abdominal computed tomography (CT) identified heterotaxy syndrome with left isomerism and fused adrenal glands. This case highlights the feature of fused adrenal glands in a patient with polysplenia.
Keywords: Congenital heart disease, diabetes mellitus, fused adrenal glands, polysplenia, pulmonary arterial hypertension, imaging
Introduction
Heterotaxy syndrome is an abnormal arrangement of internal organs in the chest and abdominal cavity across the left-right body axis. Heterotaxy syndrome excludes patients with normal arrangement (situs solitus) or mirror-image arrangement (situs inversus) of internal organs along the left-right axis. However, it may include components of both situs solitus and situs inversus being neither normal nor mirror-image arrangements (situs ambiguous) in the same person. Isomerism is where paired organs are symmetrical mirror-images on opposite sides of the left-right axis. 1 We present a 26-year-old female who came with heart failure and was diagnosed with heterotaxy syndrome, polysplenia, and fused adrenal glands by computed tomography (CT) imaging.
Case Report
A 26-year-old female presented with symptoms of awareness of heartbeat, easy fatigue, and exertional dyspnea since childhood, with worsening of symptoms for the past 6 months. She was diagnosed with type 1 diabetes mellitus 1 year before presentation. Her gynecological history revealed she had one successful vaginal delivery and 3 spontaneous abortions.
On examination, she was tachypneic with oxygen saturation of 77% on room air, an irregular pulse rate of 85 beats per minute, and a normal blood pressure of 113/77 mmHg. She had distended neck veins with positive hepatojugular reflux. There were multiple pulsations visible over the third intercostal space right of the sternal border and the sixth intercostal space left of the sternal border with parasternal heave. Systolic and diastolic murmurs were heard all over the chest. She had epigastric distension with palpable, tender mass of around 8 cm extending below the left subcostal margin.
On her electrocardiogram, she had atrial fibrillation (Figure 1). A transthoracic echocardiogram showed a common atrium with a large atrial septal defect (Figure 2). She had severe mitral and tricuspid regurgitation with moderate aortic regurgitation, and an elevated right ventricular systolic pressure of 168 mmHg.
Figure 1.
Electrocardiogram shows atrial fibrillation.
Figure 2.
Echocardiogram shows (A) common atrium with a large atrioseptal defect. (B) Severe mitral regurgitation. (C) Severe tricuspid regurgitation.
The chest computed tomography (CT) showed the cardiac apex directed toward the left, with both cardiac atria having the morphology of the left atrium. There is a large atrial septal defect resulting in a common atrium (Figures 3 and 4). The left and right ventricles are in a normal position with a possible atrioventricular canal defect. The left superior vena cava drains via the coronary sinus, and the inferior vena cava, residing near the midline, drains into the common cardiac atrium. The common ostium of the left pulmonary vein drains into the posterior cardiac atrium (Figure 5), while the right superior and inferior pulmonary veins drain into the anterior cardiac atrium. The aortic arch is toward the right (Figure 6). The origin of the left main coronary artery is visible and arises from the left coronary cusp. The right coronary artery is not visible. There are 2 vessel arches; the first vessel is a dominant right common carotid and the second is a right subclavian artery that produces a dominant right vertebral artery (Figure 7). The left common carotid and left subclavian arteries do not arise from the arch and are supplied via a small tortuous vessel arising from the proximal descending aorta at the level of T4–T5, which courses superiorly across the midline. As a result, the left common carotid, subclavian, and vertebral arteries are diminutive. The trachea is midline, and both the lungs are bilobed with a hyperarterial location of the airways relative to the pulmonary arteries.
Figure 3.
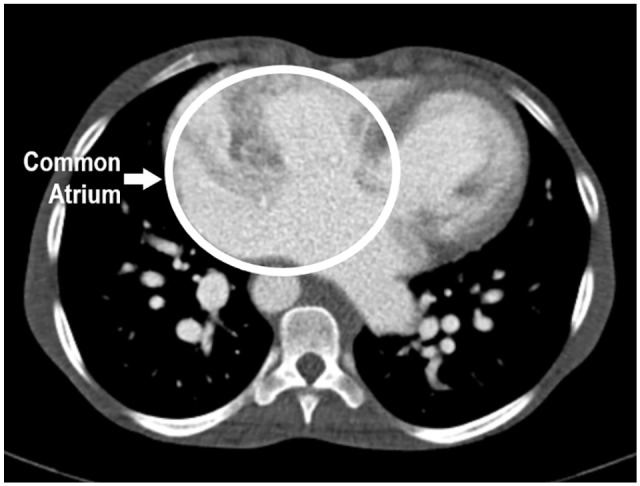
Axial CT shows the common atrium with a large atrioseptal defect.
Figure 4.

Three-dimensional virtual reconstruction shows a right-sided aortic arch, a large common atrium, and a left-sided superior vena cava.
Figure 5.

Three-dimensional virtual reconstruction shows a right descending aorta and left pulmonary vein draining into the posterior cardiac atrium.
Figure 6.
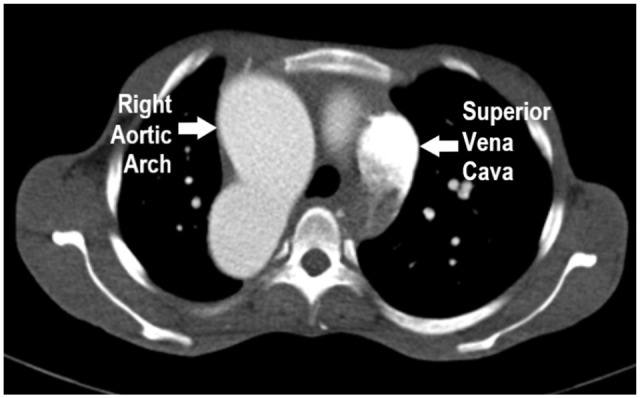
Axial CT shows a right aortic arch and left superior vena cava.
Figure 7.

Three-dimensional virtual reconstruction shows a dominant right common carotid and a right subclavian artery arising from the aortic arch.
The abdominal CT showed the liver is midline (Figure 8), and there are clustered foci of splenic tissue in the right upper quadrant consistent with polysplenia (Figure 9). The stomach resides underneath the right hemidiaphragm. All of the small bowel loops reside in the left abdomen and colon on the right, consistent with bowel malrotation. Highly vascular adrenal glands are observed to the right and left of the abdominal aorta, which appears fused (Figure 8). Duplicated inferior vena cava with hemiazygos continuation.
Figure 8.

Coronal CT shows a midline liver, a left-sided inferior vena cava, and fused adrenal glands seen on either side of the descending aorta.
Figure 9.

Coronal CT shows right-sided polysplenia (white circle under right hemidiaphragm).
As a result, a diagnosis of heterotaxy syndrome with left isomerism was made. She was kept on sildenafil 25 mg once daily, spironolactone 25 mg once daily, digoxin 0.25 mg once daily, furosemide 40 mg once daily, and basal insulin. Additionally, bisoprolol 5 mg once daily was added later on follow-up, and continuous counseling was done over her medication use, lifestyle changes, and regular follow-up. The option of surgery was brought up, but due to the risk of complications, the patient opted out of the surgery.
Discussion
The syndrome is mainly classified according to the arrangement of the atrial appendages, being right or left isomerism. Further classification is done on the basis of the splenic status, bronchopulmonary situs, and level of breaching. 2 In right isomerism, patients have a double right atrium, bilateral trilobed lungs, eparterial bronchi, a centrally located liver, and no spleen. In left isomerism, patients have isomeric left atrial appendages, bilateral bilobed lungs, and multiple spleens. 3
Patients with right isomerism have right-to-left shunting due to obstruction of the pulmonary outflow, which is typically not seen in left isomerism. Therefore, there is inadequate pulmonary blood flow with survival highly dependent on a patent ductus arteriosus to ensure circulating pulmonary blood flow. 4 It may have been thought that fused adrenal glands were exclusively seen in patients with asplenia, with around 10% of cases. 5 This case presents fused adrenal glands with another anomaly of right-sided polysplenia.
A high incidence of pancreatic variations has been reported, either short or truncated, involving the pancreatic head or a small portion of the pancreatic body, in polysplenia patients. 6 Dorsal pancreas agenesis may occur from an abnormal arrangement of organs across the left-to-right axis, which is also one of the accompanying anomalies of heterotaxy syndrome. Although pancreatic abnormalities have been reported in heterotaxy syndrome, the incidence of pancreatic abnormalities has not been thoroughly studied. Pancreatic abnormalities in heterotaxy syndrome can lead to an increased incidence of pancreatitis, obstructive jaundice, and diabetes mellitus. 7 However, the patient appeared to have a normal pancreas and still developed diabetes, either relating to the heterotaxy syndrome or to a separate indication.
The prognosis of patients with heterotaxy syndrome is poor. On follow-up, her clinical status has improved with these medications, even though there is a 35% survival rate by the age of 25 years. 4 Five-year survival for patients with right isomerism and left isomerism was 76% and 94%, respectively, while the 10-year survival was 64% and 83%, respectively. The 1-year mortality for asplenia patients is >85%, and >50% for polysplenia patients. 8
In conclusion, this case demonstrates the presentation and imaging findings of heterotaxy syndrome. This syndrome is a complex compilation of a broad spectrum of cardiac and extra-cardiac abnormalities. Heterotaxy syndrome is difficult to manage and mainly depends on the anatomy of both cardiac and non-cardiac lesions.
Acknowledgments
We thank the patient and her family for their patience and co-operation
Footnotes
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Informed Consent Statement: Written informed consent was obtained from the patient for publication of this case report and any accompanying images
ORCID iD: Abid M. Sadiq  https://orcid.org/0000-0002-7812-8042
https://orcid.org/0000-0002-7812-8042
References
- 1. Jacobs JP, Anderson RH, Weinberg PM, et al. The nomenclature, definition and classification of cardiac structures in the setting of heterotaxy. Cardiol Young. 2007;17 Suppl 2:1-28. [DOI] [PubMed] [Google Scholar]
- 2. Yim D, Nagata H, Lam CZ, et al. Disharmonious patterns of heterotaxy and isomerism: how often are the classic patterns breached? Circ Cardiovasc Imaging. 2018;11:e006917-e006919. [DOI] [PubMed] [Google Scholar]
- 3. Kim S-J. Heterotaxy syndrome. Korean Circ J. 2011;41:227-232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Loomba RS, Nijhawan K, Anderson R. Impact of era, type of isomerism, and ventricular morphology on survival in heterotaxy. World J Pediatr Congenit Heart Surg. 2016;7:54-62. [DOI] [PubMed] [Google Scholar]
- 5. Ticho BS, Goldstein AM, Van Praagh R. Extracardiac anomalies in the heterotaxy syndromes with focus on anomalies of midline-associated structures. Am J Cardiol. 2000;85:729-734. [DOI] [PubMed] [Google Scholar]
- 6. El Mortaji H, Elatiqi K, El Hammaoui H, Alj S. Polysplenia syndrome with situs ambiguous, common mesentery, and IVC interruption discovered incidentally in an adult. Radiol Case Rep. 2019;14:1072-1075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Jung JE, Hur JH, Jung MK, et al. Diabetes mellitus due to agenesis of the dorsal pancreas in a patient with heterotaxy syndrome. Ann Pediatric Endocrinol Metab. 2017;22:125-128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bartz PJ, Driscoll DJ, Dearani JA, et al. Early and late results of the modified Fontan operation for heterotaxy syndrome 30 years of experience in 142 patients. J Am Coll Cardiol. 2006;48:2301-2305. [DOI] [PubMed] [Google Scholar]




