Abstract
Distance runners represent a unique patient population. The cyclic activity associated with distance running leads to a high incidence of injury. Gait patterns, the extrinsic and intrinsic muscles of the foot and ankle, foot strike pattern, shoe wear considerations, alignment, and orthotics are also all important considerations that must be considered by the treating provider. The purpose of this work is to review relevant functional anatomy, recent studies on gait patterns in running, orthotics, and theory on how the body moves through space during running in order to better equip the clinician to treat long distance runners.
Keywords: marathon, ultramarathon, running, long distance running, foot and ankle injuries
Introduction
Running has been reported to be the second most popular physical activity in the world. 45 As such, foot and ankle surgeons will frequently encounter distance runners who have symptoms and/or questions about shoes, orthotics, alignment, and injury prevention. Although distance running is not a contact sport, it is associated with substantial cyclic loading that may lead to overuse injuries. The patient assessment must therefore incorporate anatomical, biomechanical, and physiological evaluations.
Although there are many health benefits of running, there is a high incidence of running injuries, especially stress reaction and tendinitis. Distance runners, because of the high demands on the ankle and feet, may also have different expectations and specific concerns than nonrunners.
The purpose of this article is to examine the evolution, biomechanics, and functional anatomy of the foot as it applies to long-distance running. In addition, the use of orthotics as well as the incidence and treatment of stress injury will be reviewed.
Epidemiology
Although distance running lacks a clear definition, the marathon has traditionally been used to define a “long” distance. The marathon (26.2 miles/42 km) has been referred to as the “suburban Mt Everest” in popular culture. It is estimated that roughly 1.3 million people completed a marathon in 2018. 3 Ultramarathons are defined as distances greater than a marathon. The participation in ultramarathons has increased by 1676% in the last 23 years to roughly 611 098 yearly participants as of 2021. 86 The health benefits of running include a 30% reduced risk of all-cause mortality and a 45% reduced risk of cardiovascular mortality. 57
Nevertheless, it has been reported that up to 79% of runners sustain an injury of some sort during any given year, of which the vast majority involve the lower limb.60,63,101,104,105 These are evenly distributed across the foot and ankle, knee, and lower leg. These injuries are also important to clinicians who treat nonelite runners because the injury rate for novice runners is higher than for elite runners. Per 1000 hours of running, the injury rate has been reported to be 17.8% for novice runners, 7.7% for recreational runners, and 3.5% for elite or professional runners.10,106
VanderWorp and colleagues divided the risk factors for injuries in runners into 3 domains: (1) personal factors including sex, age, and body shape/alignment; (2) running/training factors (experience, training mileage, surface, shoe use, etc); and (3) health- and lifestyle-related factors (history of previous injury, orthotics etc). 103 In their extensive review on the topic, these authors found that a history of previous injury, training errors, and orthotic use had the strongest association with an increased risk for running-related injuries. 103 The female runner is thought to be at a particularly increased risk of injury because of a possible combination of factors described as the female athlete triad. This is characterized by menstrual dysfunction, low energy availability, and reduced bone mineral density. The prevalence of these factors in the general population is low. However, sports such as running, whose female athletes typically have lean body mass, have rates of amenorrhea as high as 69%, disordered eating as high as 49.2%, and an osteopenia prevalence ranging from 22% to 50%.49,51,75
The Evolution of Running: Historical Perspective
The modern foot is thought to have evolved from an ancestor similar to the African ape, where its function is in both ground-based movement as well as arboreal movement. 23 The evolutionary transition from trees to the ground came with changes in foot shape and function. Although bipedal gait is one function that differentiates human movement from modern chimpanzees, the human ancestor Australopithecus is thought to have walked bipedally for several million years without otherwise looking like a modern human. 13
Thus, although bipedal gait may not differentiate us from our ancestors, running may. The change in foot shape and function from Australopithecus to modern Homo sapiens suggests that modern humans have more demanding locomotion behaviors such as carrying heavy objects and running from predators. The modern human shape and features, especially in the musculoskeletal system, are reflective of elements necessary for distance running. Our feet are shaped and function differently than modern apes. 13 These differences include (1) a larger and adducted first ray, (2) mobile and shortened lateral rays, (3) tarsal bone alignment that can change conformation and allows for rigidity during the toe-off phase of gait, and (4) well-defined transverse and longitudinal arches supported by strong planar tissues that are resistant to tensile loads and capable of energy storage.39,99,107
When compared to walking, running requires strong ankle plantarflexion as well as a strong plantar aponeurosis and soft tissue resistance to support plantar tensile loads during late stance and the toe-off phase of gait. The underdevelopment of these structures in the human ancestor Australopithecus provides further support that Homo sapiens further evolved to run.1,66
Additionally, the intrinsic muscles of the foot are also important in running when compared to walking. Electromyographic (EMG) activity in the planar intrinsic muscles is greater in running than in walking and greater in higher load activities.7,81 Unlike most quadrupeds, humans have well-developed intrinsic foot muscles. In quadrupeds, these muscles are nearly or completely absent. 66 This is likely because human running requires careful balance on uneven surfaces as well as during single leg stance.
Intrinsic Muscles in Running
Although underappreciated, the intrinsic muscles are of particular importance in running. These structures have been likened to the abdominal and paraspinal muscles of the lumbopelvic-hip core. 66 The function of the intrinsic muscles as a group includes providing support to the arches of the foot,33,40,71 being responsive to applied loads,64,65 acting in synergy with the extrinsic muscles of the foot, and serving to regulate how forces are transmitted during gait, posture, and balance activities such as single leg stance.50,94
Weakness or atrophy of the intrinsic muscles have been associated with several pathologic conditions including pes cavus and Charcot-Marie-Tooth,20,36 hammer toe and claw toe deformities,27,74 plantar fasciitis,18,66 hallux valgus,28,52,97 and pes planus.48,67,97 In runners, intrinsic weakness may manifest as nonspecific arch pain and fatigue, as well as unexplained metatarsalgia.
Although these muscles are not large contributors to force generation in gait, they are thought to play an important role in proprioception by providing sensory input via the stretch response. Although other contributors to sensory input such as the capsular ligaments are static, the intrinsic muscles of the foot can be modulated through training to alter sensitivity to foot loads. 47
Additionally, either through contraction, resistance to stretch, or by neuromuscular feedback, the intrinsic musculature seems to be an important contributor to foot shape. Headlee et al 40 showed that after fatigue of the intrinsic muscles of the foot, measured by a change in navicular height, pronation significantly increased and was independent of the magnitude of pronation before the fatigue test. The authors concluded that while the change in muscle force led to the change in posture, the change in muscle force may be associated with a change in sensory feedback of the muscles. This concept of muscle fatigue from repetitive contractions leading to a decrease in joint position sense has been shown elsewhere in the lower extremity. 41
It has been shown that the shape of a runner’s foot changes with prolonged running.22,31,43 As measured by navicular drop, Cowley and Marsden 22 noted that there was an average of 5 mm drop in the navicular after the half marathon distance. Fukano et al 35 noted a similar navicular drop of 4.8 mm after a full marathon and noted that the drop persisted even 8 days after the race. It is thought that in addition to intrinsic fatigue, decreased stiffness of the plantar fascia may be contributory. Shiotani et al 90 performed a study measuring long-distance runners and noted a decrease in plantar fascia stiffness after a long-distance run.
Strengthening the intrinsic muscles has been a recent interest and should be considered as a conservative treatment for runners thought to have weak intrinsics. Given the function of the intrinsics, weakness in this muscle group can present as nonspecific foot pain with activities such as running that have a high dynamic demand without other identifiable cause.
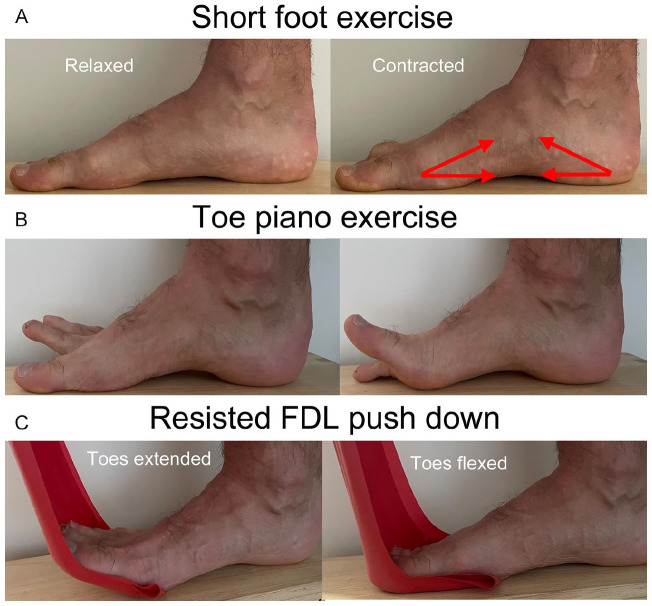
Although there is no gold standard for evaluating the intrinsic muscles, 94 intrinsic strength and control can be evaluated in the office setting. The first useful test is the paper pullout test. This is performed by having the patient grip a strip of paper against the ground with a lesser toe. The examiner then attempts to pull the paper out while the patient grips the paper against the ground. With intrinsic weakness, the examiner will generally be able to remove the paper without ripping it, a sign of poor toe flexion strength. Another test is the “short foot exercise” (SFE) (see Figure 1). If the patient is unable to easily perform the SFE while standing, this is likely due to intrinsic weakness.
Figure 1.
Three common intrinsic foot strengthening exercises: (A) The short foot exercise entails contraction of the intrinsic muscles of the foot. This causes the foot to shorten and an elevation of the medial column. This is performed by having the patient flex their toes and pull them proximally toward the heel. This should begin to lift the metatarsophalangeal joints and shorten the arch. (B) In the toe piano exercise, the goal is to build control of the lesser toes independent of the great toe by altering extension of the great toe with extension of the lesser toes in isolation from either other. (C) Resisted toe flexion exercises utilize a band to resist flexion of the toes from extension to neutral and in reverse. There are many progressions of each of these exercises.
Strengthening of the intrinsic foot muscles can be helpful to long-distance runners. In addition to being a diagnostic test, the SFE is also a commonly performed intrinsic strengthening exercise. The goal of the SFE is to recruit and strengthen the lumbricals and interossei of the foot. Such muscle recruitment and conditioning has been shown to be a mechanism to improve neuromuscular control, balance, and intrinsic foot strength.80,87 The SFE can initially be performed sitting. Thereafter, it is progressed to being performed standing on 2 legs and then 1 leg. There is increasing evidence that intrinsic strengthening improves foot function. For example, Sulowska et al 98 performed a 6-week prospective study on long-distance runners performing intrinsic strengthening exercises and noted improved functional movement patterns and foot alignment measured by the foot posture index. Mulligan and Cook 71 demonstrated a reduction in navicular drop, arch height index, and improved balance after 4 weeks of short foot exercises. Lynn et al 62 showed short foot exercise improved balance compared to traditional intrinsic strengthening exercise in another 4-week study of healthy patients.
It has also been proposed that barefoot running strengthens the intrinsic foot muscles and may decrease injury rates. To examine this concept, Bell et al 11 used ultrasonography to indirectly measure the strength of the intrinsic muscles in experienced barefoot and traditionally shod runners. They found no difference between runners, which implies that barefoot running alone does not necessarily increase intrinsic strength. 11
Two other intrinsic strengthening exercises include the toe piano exercise and resisted toe flexion exercises (Figure 1). These exercises are also thought to strengthen and provide neuromuscular recruitment of the intrinsic muscles to stabilize the metatarsophalangeal and proximal interphalangeal joints with toe motion as opposed to the SFE, which has more effect on arch stabilization.
In summary, the intrinsic muscles of the foot have an important function in gait, and specific strengthening exercise should be considered in activities such as long-distance running that may cause muscle fatigue.
Impact Forces and “Comfort”
Over the last decade, there has been substantial focus in the running literature on foot strike pattern, minimalist shoes, impact forces, and the relationship between the 3. The discussions on various shoe designs and running forms often begin with the concept of impact forces.
To start, most runners (89%) have a heel strike gait pattern with running. 55 In this pattern, the heel strikes the ground first followed by the rest of the foot and body mass. In forefoot running, the forefoot impacts the ground before the heel while the ankle is in a more plantarflexed position.
To understand the difference in tissue stress between forefoot and heel strike running, the difference between externally measured ground reaction forces and internal tissue forces and loading rates must be appreciated. Many studies use a force-time curve, as measured by ground reaction force, to represent the forces experienced during running (Figure 2). As runner speed increases, so does the peak ground reaction force. It has been reported that increased peak ground reaction forces and peak loading rates are important considerations and may be potentially harmful to the runner.25,44,70,91-93,112 The externally measured peak vertical ground reaction force with walking and running is approximately 1 to 1.5 times body weight for walking and 2 to 2.9 times body weight for running. 79 Meanwhile, the joint reaction force across the ankle joint with walking and running is up to 5 times body weight and 13 times body weight, respectively. 14 This conceptual model, however, is likely an oversimplification of the stress seen at the tissue level. Other factors such as neuromuscular control, skeletal position, as well as loading mechanism are likely important considerations as well. Forces seen at the tissue level are harder to directly measure but are likely more nuanced than what is seen at a force transducer on the running surface.
Figure 2.
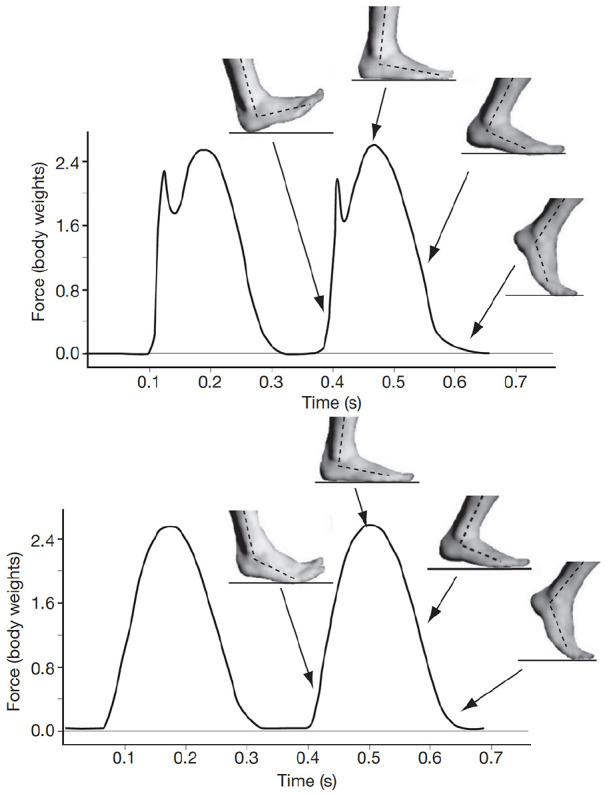
Vertical ground reaction forces and foot kinematics for 3 foot strikes at 3.5 m/s in the same runner. Top: rear foot striker during barefoot heel-toe running. Bottom: forefoot strike during barefoot running (reproduced with permission from Lieberman et al 58 ). Note the increased impact impulse (higher initial slope of the curve) in heel strike compared to forefoot strike.
The effect that foot strike pattern and shoewear has on injury rates is important to consider as well but the overall evidence is limited. In a shoewear study, Altman et al 2 performed a prospective cohort study of traditionally shod runners and barefoot runners and noted similar overall injury rates. Daoud et al 25 performed a study of 52 collegiate cross-country team runners and correlated injuries to foot strike pattern. They noted that 74% of runners experienced a moderate or severe injury each year and that those who habitually rearfoot strike had approximately twice the risk of injury compared to those who habitually forefoot strike. 25
Comfort while running is poorly defined and understood, but it seems to be important in selection of running shoewear. Although not definitively proven, running comfortably may be a sign of low tissue stress and subsequent decreased injury risk. Different people experience comfort differently and shoes that may be comfortable for some may be uncomfortable for others. 69 Wearing the most comfortable shoes may reduce injury. Mundermann et al 72 performed a study of military personnel and offered them 6 different shoe orthotic types that varied in arch and heel cup shape, hardness, and elasticity. The recruits then wore the insert they found most comfortable and were monitored for injury during military training exercise and compared these recruits to a control group. The authors found that the orthotic group sustained less overall stress fractures and foot pain than the control group (8.8% vs 22.2%). This study supports that if orthotics are considered, then subjective comfort should be taken into consideration.
Meanwhile, Basford and Smith 6 performed a study on women who stand at work and showed that subjectively comfortable noncustom orthotics improved comfort while reducing back, leg, and foot pain when standing at work. They noted that 40% to 50% of participants preferred the insoles to standard shoewear whereas the others had no preference or felt the orthotics made their pain worse.
Finally, shoes that are more comfortable have been associated with decreased oxygen consumption while running. 61 In this study, Luo et al 61 asked a group of proficient runners to try 5 different pairs of shoes and select the most comfortable and the least comfortable. They then measured the runners’ mean oxygen consumption with Vo2 data collection equipment while running on a treadmill and found a 0.7% improvement in running economy when the runners used the most comfortable compared with the least comfortable shoes.
Foot Alignment, Shoes, and Custom Orthotics
Foot alignment is a common concern among runners. Foot pronation has been described as a risk factor for running injuries, and running shoe design has been a suggested intervention to prevent injuries, despite a lack of evidence. 83 In fact, mild pronation may be protective against injury. Neilsen et al 76 performed a study of 730 runners (all wearing the same neutral shoes) to correlate foot posture to running-related injury in shoes in order to determine if foot posture increased the risk of injury. Interestingly, they found that, overall, pronated feet were the least likely to be injured (0.63 relative incidence rate per 1000 km compared with neutral feet). However, highly pronated feet were the more likely to be injured (3.25 relative incidence rate per 1000 km compared to neutral feet). Supinated and highly supinated feet did not reach a statistically significant increase in injury rate (1.03 and 1.24 relative incidence rate per 1000 km compared with neutral feet, P value .83 and .49, respectively). These results support the notion that mild pronation may actually be protective against injury, likely secondary to hindfoot suppleness at heel strike.
The mechanism of action of orthotics, the indications for orthotics, the appropriate orthotic design, and the effectiveness of orthotics are complex issues. Orthotics have several potential mechanisms of action. First, there may be a placebo effect. Second, orthotics may change kinematics. For example, they may alter hindfoot alignment. Third, orthotics may work kinetically by altering muscle demands. With an orthotic in the shoe, the muscle(s) firing may be different than without an orthotic. This may increase or decrease muscle activity and the stress placed on particular tissues. Fourth, orthotics may change neuromuscular control by altering proprioceptive feedback.
Although orthotics may be beneficial for some runners, the evidence is unclear regarding who may benefit and in which way. The published studies on orthotics in runners are generally difficult to generalize because most lack a control group and have a small sample size. 37 In addition, orthotic fitting is highly practitioner dependent. 19
Runners themselves believe that orthotics and shoe design matter. Enke et al 30 performed a study and found that 73% of runners believe that the shape of their foot should be the most important factor when choosing a running shoe. Up to 80% of runners report positive outcomes from orthotics despite no standardization of indication, orthotic shape, material, type, or orthotist.38,46 To the authors’ knowledge, however, there are no high-level controlled trials investigating orthotics in runners. Several controlled studies on nonrunners including patients with Achilles tendinitis, rheumatoid arthritis, and other causes of foot pain have not shown a compelling benefit of orthotics over sham or placebo.21,54,73
D’Ambrosia retrospectively reported on 200 runners with injuries treated with orthotics, mostly for pronation with forefoot varus, and noted that 73% of patients improved from posterior tibial tendonitis, 86% from metatarsalgia, 82% from plantar fasciitis, and 66% from iliotibial band syndrome. 24 There was a poor response in patients who had a cavus foot deformity. Banwell et al 5 performed a systematic review of foot orthotics for flexible pes planus and found no high-level evidence supporting the use of foot orthoses in flexible pes planus. They found good to moderate evidence that foot orthoses improve medial to lateral sway during standing and energy cost during walking and low evidence that foot orthoses improve pain or alter loading and impact forces. Zammit et al 111 in 2007 performed a study on hindfoot motion with and without orthotics and found a small but statistically significant effect on hindfoot motion but no significant correlation with pain and function scores.
The change in neuromuscular control from an orthotic has been shown to be difficult to quantify. 32 The effect of orthotics on the kinematics is also difficult to quantify, with several studies measuring hindfoot motion in orthotics demonstrating inconsistent results. Some authors have found a difference in hindfoot motion with orthotic intervention,100,110 whereas others have not.8,29,78,85 These studies generally use skin markers, which are known to overestimate the true effect on the motion of the underlying bone.17,82 To clarify this effect, Stacoff et al 96 performed a study using pins placed in the tibia, calcaneus, and shoes of subjects who then ran with and without orthotics. The authors noted that orthotics did not significantly change the movement of the tibia or calcaneus during the stance phase of running. Using similar techniques, Stacoff et al 95 performed a study comparing barefoot running to running with shoes with and without an orthotic. They showed the difference between barefoot running and running with shoes to be not clinically significant. These studies both support the notion that changing the shoe type or introducing orthotics does not change the movement path of the skeleton during running. 77
The extension of this concept to barefoot running is also demonstrated in the literature. In 2010, Lieberman et al 58 published a study demonstrating that heel strike in barefoot running results in increased vertical loading rates compared to a forefoot strike pattern. This drove a rise in popularity of barefoot running as most barefoot runners tend to adapt a forefoot strike pattern.
More recently, however, Udofa et al 102 performed a study to look more closely at the relationship between shoewear and ground reaction forces when ground reaction forces are modeled in a more complex way (Figure 3). Specifically, the authors modeled the ground reaction force during running as 2 masses rather than a single mass, and showed that a runner’s gait changes with a change in shoewear. They noted that with barefoot running, the runner more commonly has a more plantarflexed ankle and therefore a forefoot strike pattern. When there is a large heel cushion, the runner more commonly has a less plantarflexed ankle and therefore a heel strike pattern. 102 This is consistent with the conceptual model that gait patterns change with shoewear. Without a heel cushion, the gait will adapt a plantarflexed foot (forefoot strike) to minimize impact force. In the presence of a heel cushion, the gait pattern will trend toward a heel strike pattern. These data support the notion that runners will adapt their running style to avoid high heel impacts. 68
Figure 3.
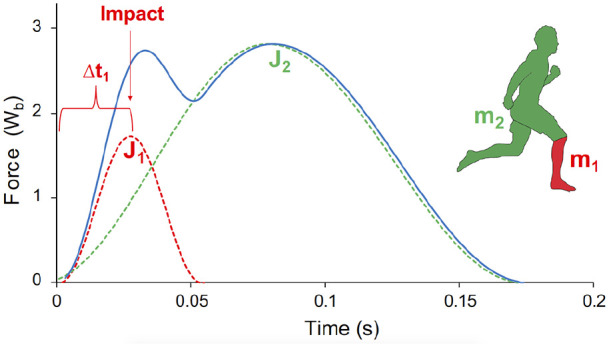
Two-mass model of the ground reaction force during running. In this model, the ground reaction force modeled as the sum of mass 1 and mass 2. Changing the timing of when mass 1 contacts the surface (later in heel strike), explains the increase in impact impulse in heel strike runners compared with forefoot strikers (used with permission). 102
Stress Injuries in Runners
The 1-year incidence of bone stress injuries in runners has been reported to be as high 21%. 12 There are several risk factors for injury (Table 1). Low serum vitamin D has been frequently cited in the foot and ankle. In athletes in general, it has been found that those with a lower serum vitamin D level have a higher risk of stress fractures.15,26,89 Horas et al 42 performed a study in a group of patients with MRI findings of bone marrow edema (BME) of the foot and ankle. They found that 84% of the patients had low vitamin D levels; 61% were vitamin D deficient, and 23% were vitamin insufficient.
Table 1.
Risk Factors for Bone Stress Injuries.
| Biological factors |
| Female sex |
| Genetics |
| Smoking |
| Medications (anticonvulsants, steroids, antidepressants, antacids) |
| Female athlete triad (interrelationship between energy availability, menstrual function, and bone mass) |
| Diet and nutrition |
| Calcium and Vitamin D deficiency |
| Biomechanical |
| Running experience, distance, frequency |
| Training pattern |
| Bone characteristics (bone density) |
| Gait characteristics |
| Anatomic characteristics |
Conversely, it has also been shown that an increased serum vitamin D level is associated with a reduced risk of stress fracture. 4 Serum vitamin D levels lower than 30 ng/mL may lead to defects in bone mineralization as well as impaired muscle function, whereas levels greater than 40 ng/mL may have a protective effect on the development of stress fractures. 16 Williams et al 109 recently performed a study demonstrating that almost half of the tested NCAA Division 1 athletes (including cross country runners) were either vitamin D insufficient or deficient. They also showed that vitamin D3 supplementation of deficient athletes reduced the stress fracture rate by a statistically significant amount from a historical rate of 7.51% to 1.65% in the study group. 109 In a study of female Navy recruits, Burgi et al 15 demonstrated that recruits with a serum vitamin D level below 20 ng/mL had twice the risk of stress fracture compared with those above 40 ng/mL, and thus recommend this as a target level.
The diagnosis of a bone stress injury should be clinically differentiated from a finding of bone marrow edema itself on MRI, which can sometimes be a confusing image finding. Bone marrow edema (BME) has been shown to be a sign of bone turnover, which may be either adaptive or a sign of overuse injury. Kornaat et al 53 performed a study in which 16 asymptomatic professional runners were followed for a 7-month running season after getting preseason MRI studies. Fourteen of the 16 runners had BME lesions before the season started. Sixty-nine percent of the lesions were located in the foot and ankle. Lesions came and went throughout the season with 20% developing new lesions and 22% of the lesions resolving, without clinical correlation. The authors concluded that incidental BME lesions in professional runners should not necessarily alter clinical care or running behavior. 53
Lazzarini et al 56 found that 16 of 20 (80%) collegiate cross-country runners had BME in the foot and ankle. This was higher than the 4 of 12 nonrunners. They noted that an average of 3.4 bones had edema in the runner group and 0.7 in the nonrunner group. Ridge et al 84 performed a study on BME before and after a 10-week transition to minimalist running shoes in experienced recreational runners. Thirty-six runners participated (17 in a control group, 19 in the transition group). Although they reported no difference in bone signal pretraining, they noted that 10 of 19 demonstrated an increase in BME in the minimalist transition group whereas only 1 of 16 showed lesions in the control group. 84
Lohman et al 59 performed an MRI study in 19 marathon runners and 19 matched controls. In the marathon group, who each had completed a mean of 60 previous full-length marathons, subjects underwent an MRI within 3 hours of running a marathon. Four of 19 runners demonstrated BME (1 severe and 3 slight). This was similar to the control group, in which 3 of 19 subjects demonstrated slight BME lesions. The reduced incidence of BME in these athletes may be attributed to the fact that the MRIs were obtained within 3 hours of the race as it is ultimately unknown how long BME takes to become visible on MRI. It also could be the case that because these runners had completed a mean of 60 previous marathons, that this length of run was not a significant tissue stress for these runners.
Importantly, Freund et al 34 studied a group of 22 ultramarathon runners participating in a 4487-km (2789-mile) multistage ultramarathon. The average mileage in these participants was 1.7 marathons per day for 64 consecutive days. They underwent foot and ankle MRIs at the beginning of the race and then roughly every 1000 km throughout the run. The authors noted that the peak intraosseous signal intensity as well as the number of BME lesions increased from baseline to 1000 km into the race, but thereafter the maximal intraosseous signal intensity actually decreased compared with the final MRI for a mean of 3667 km into the race from 411.7 to 399.9. They also noted that the number of bone lesions stayed relatively constant from 3.2 to 3.6 from 1000 km to 3669 km. None of these lesions coincided with stress fractures or were correlated with dropping out of the race. These data support the notion that BME is a result of stress response and evidence of adaption, given that it seems to have increased to the 1000-km mark, but it was not found to be progressive or pathologic.
The treatment of bone stress injuries depends on several factors and should be individualized. When injured, the athlete should initially reduce activity to a pain-free level of function. Immobilization in a boot or hard-soled shoe should be continued for a short period of time. The treating physician must identify and address associated risk factors for stress injury while also creating a program to maintain physical conditioning and, when appropriate, a return to running program. 108 In the author’s experience, once symptoms allow, deep-water running and antigravity treadmill work under the direction of an experienced physical therapist are the most specific activities that may help to reproduce the running mechanics while offloading the tissues (Figure 4).
Figure 4.
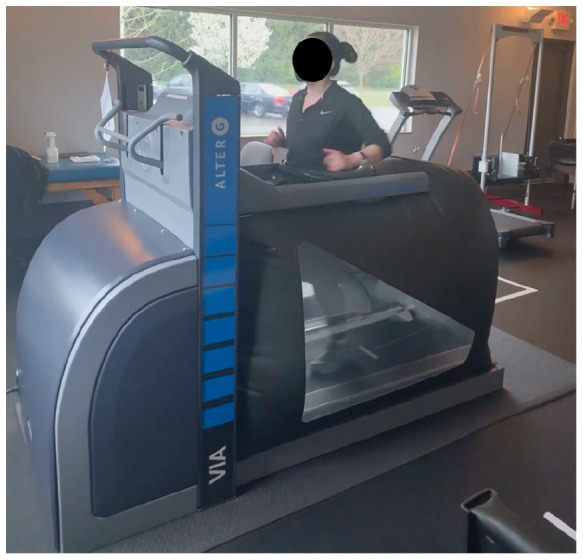
Commercially available offloading rehabilitation treadmill that allows preservation of running mechanics while offloading tissues (AlterG).
Accelerating tissue healing is often a goal of runners, and there is growing interest in both electrical and ultrasonic bone stimulation. Although the risk profile is low for noninvasive treatments, the effectiveness in the published literature is lacking. Rue et al 88 performed a randomized controlled trial of 26 patients treated with low-intensity ultrasound and showed no decrease in healing time of tibial stress fractures. Similarly, Beck et al 9 performed a randomized controlled trial of 44 patients using electrical stimulation on tibial stress fractures and demonstrated no benefit. Given these findings, although bone stimulators are generally well tolerated by patients, there is a lack of high-level evidence to support their use.
Summary
The current work provides a background and summary of the foot and ankle in distance runners. Runners are a unique patient population and involvement of an experienced athletic trainer and physical therapist can be useful.
Several important considerations include the following:
• Distance running is increasingly common, and evidence supports that humans have evolved to be runners.
• The intrinsic muscles of the foot play an important role in running. Despite a runner’s shoewear or gait pattern, strengthening the intrinsic muscles may be an important component of preventing or treating running injuries.
• Runners will adapt their running style to minimize internal impact forces despite the type of shoewear.
• Ground reaction forces may oversimplify the understanding of internal forces and the way the skeleton moves during running.
• There is a high treatment effect of placebo/sham orthotics. There is little evidence to support the routine use of orthotics in runners.
• Running with shoes and a gait pattern that optimizes “comfort” may prevent injury and be most efficient.
• Bone marrow edema on MRI may be adaptive. In the setting of symptoms, however, treatment includes rest, activity modification, and vitamin D supplementation as needed. Thereafter, return to running is based on symptoms.
• There is no high-level evidence to support the routine use of bone stimulators for stress-related injury.
Footnotes
Ethical Approval: Ethical approval was not sought for the present study because it is a contemporary review article.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ICMJE forms for all authors are available online.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: James R. Jastifer, MD,  https://orcid.org/0000-0002-9559-2736
https://orcid.org/0000-0002-9559-2736
References
- 1. Alexander RM. Energy-saving mechanisms in walking and running. J Exp Biol. 1991;160:55-69. [DOI] [PubMed] [Google Scholar]
- 2. Altman AR, Davis IS. Prospective comparison of running injuries between shod and barefoot runners. Br J Sports Med. 2016;50(8):476. doi: 10.1136/bjsports-2014-094482. [DOI] [PubMed] [Google Scholar]
- 3. Anderson J. Marathon Statistics 2019 Worldwide (Research). 2019; https://runrepeat.com/research-marathon-performance-across-nations. Accessed Sep 26 2021. [Google Scholar]
- 4. Armstrong RA, Davey T, Allsopp AJ, et al. Low serum 25-hydroxyvitamin D status in the pathogenesis of stress fractures in military personnel: An evidenced link to support injury risk management. PloS One. 2020;15(3):e0229638. doi: 10.1371/journal.pone.0229638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Banwell HA, Mackintosh S, Thewlis D. Foot orthoses for adults with flexible pes planus: a systematic review. J Foot Ankle Res. 2014;7(1):23. doi: 10.1186/1757-1146-7-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Basford JR, Smith MA. Shoe insoles in the workplace. Orthopedics. 1988;11(2):285-288. [DOI] [PubMed] [Google Scholar]
- 7. Basmajian JV, Stecko G. The Role of Muscles in Arch Support of the Foot. J Bone Joint Surg Am. 1963;45:1184-1190. [PubMed] [Google Scholar]
- 8. Bates BT, Osternig LR, Mason BR, James SL. Functional variability of the lower extremity during the support phase of running. Med Sci Sports. 1979;11(4):328-331. [PubMed] [Google Scholar]
- 9. Beck BR, Matheson GO, Bergman G, et al. Do capacitively coupled electric fields accelerate tibial stress fracture healing? A randomized controlled trial. Am J Sports Med. 2008;36(3):545-553. doi: 10.1177/0363546507310076. [DOI] [PubMed] [Google Scholar]
- 10. Begizew DM, Grace JM, van Heerden HJ. Lower-extremity running-related injuries among 10,000-meter long distance runners in Ethiopia. J Human Sport Exerc. 2019;14. doi: 10.14198/jhse.2019.142.09 [DOI] [Google Scholar]
- 11. Bell EA, Hibbert JE, Domire ZJ. Measurement of intrinsic foot stiffness in minimally and traditionally shod runners using ultrasound elastography: a pilot study. J Sports Sci. 2020;38(13):1516-1523. doi: 10.1080/02640414.2020.1746595 [DOI] [PubMed] [Google Scholar]
- 12. Bennell KL, Malcolm SA, Thomas SA, Wark JD, Brukner PD. The incidence and distribution of stress fractures in competitive track and field athletes. A twelve-month prospective study. Am J Sports Med. 1996;24(2):211-217. doi: 10.1177/036354659602400217 [DOI] [PubMed] [Google Scholar]
- 13. Bramble DM, Lieberman DE. Endurance running and the evolution of Homo. Nature. 2004;432(7015):345-352. doi: 10.1038/nature03052 [DOI] [PubMed] [Google Scholar]
- 14. Burdett RG. Forces predicted at the ankle during running. Med Sci Sports Exerc. 1982;14(4):308-316. doi: 10.1249/00005768-198204000-00010 [DOI] [PubMed] [Google Scholar]
- 15. Burgi AA, Gorham ED, Garland CF, et al. High serum 25-hydroxyvitamin D is associated with a low incidence of stress fractures. J Bone Miner Res. 2011;26(10):2371-2377. doi: 10.1002/jbmr.451 [DOI] [PubMed] [Google Scholar]
- 16. Butscheidt S, Rolvien T, Ueblacker P, Amling M, Barvencik F. [Impact of Vitamin D in Sports: Does Vitamin D Insufficiency Compromise Athletic Performance?]. Article in German. Sportverletzung Sportschaden. 2017;31(1):37-44. doi: 10.1055/s-0042-121748 [DOI] [PubMed] [Google Scholar]
- 17. Cappozzo A, Catani F, Leardini A, Benedetti MG, Croce UD. Position and orientation in space of bones during movement: experimental artefacts. Clin Biomech (Bristol, Avon). 1996;11(2):90-100. doi: 10.1016/0268-0033(95)00046-1 [DOI] [PubMed] [Google Scholar]
- 18. Chang R, Kent-Braun JA, Hamill J. Use of MRI for volume estimation of tibialis posterior and plantar intrinsic foot muscles in healthy and chronic plantar fasciitis limbs. Clin Biomech (Bristol, Avon). 2012;27(5):500-505. doi: 10.1016/j.clinbiomech.2011.11.007 [DOI] [PubMed] [Google Scholar]
- 19. Chevalier TL, Chockalingam N. Effects of foot orthoses: How important is the practitioner? Gait Posture. 2012;35(3):383-388. doi: 10.1016/j.gaitpost.2011.10.356 [DOI] [PubMed] [Google Scholar]
- 20. Chung KW, Suh BC, Shy ME, et al. Different clinical and magnetic resonance imaging features between Charcot-Marie-Tooth disease type 1A and 2A. Neuromuscul Disord. 2008;18(8):610-618. doi: 10.1016/j.nmd.2008.05.012 [DOI] [PubMed] [Google Scholar]
- 21. Conrad KJ, Budiman-Mak E, Roach KE, et al. Impacts of foot orthoses on pain and disability in rheumatoid arthritics. J Clin Epidemiol. 1996;49(1):1-7. doi: 10.1016/0895-4356(96)00534-3 [DOI] [PubMed] [Google Scholar]
- 22. Cowley E, Marsden J. The effects of prolonged running on foot posture: a repeated measures study of half marathon runners using the Foot Posture Index and navicular height. J Foot Ankle Res. 2013;6:20. doi: 10.1186/1757-1146-6-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Crompton RH, Vereecke EE, Thorpe SK. Locomotion and posture from the common hominoid ancestor to fully modern hominins, with special reference to the last common panin/hominin ancestor. J Anat. 2008;212(4):501-543. doi: 10.1111/j.1469-7580.2008.00870.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. D'Ambrosia RD. Orthotic devices in running injuries. Clin Sports Med. 1985;4(4):611-618. [PubMed] [Google Scholar]
- 25. Daoud AI, Geissler GJ, Wang F, et al. Foot strike and injury rates in endurance runners: a retrospective study. Med Sci Sports Exerc. 2012;44(7):1325-1334. doi: 10.1249/MSS.0b013e3182465115 [DOI] [PubMed] [Google Scholar]
- 26. Davey T, Lanham-New SA, Shaw AM, et al. Low serum 25-hydroxyvitamin D is associated with increased risk of stress fracture during Royal Marine recruit training. Osteoporos Int. 2016;27(1):171-179. doi: 10.1007/s00198-015-3228-5 [DOI] [PubMed] [Google Scholar]
- 27. Dodd A, Le I. Foot compartment syndrome: diagnosis and management. J Am Acad Orthop Surg. 2013;21(11):657-664. doi: 10.5435/JAAOS-21-11-657 [DOI] [PubMed] [Google Scholar]
- 28. Donatelli RA. Abnormal biomechanics of the foot and ankle. J Orthop Sports Phys Ther. 1987;9(1):11-16. doi: 10.2519/jospt.1987.9.1.11 [DOI] [PubMed] [Google Scholar]
- 29. Eng JJ, Pierrynowski MR. The effect of soft foot orthotics on three-dimensional lower-limb kinematics during walking and running. Phys Ther. 1994;74(9):836-844. doi: 10.1093/ptj/74.9.836. [DOI] [PubMed] [Google Scholar]
- 30. Enke RC, Laskowski ER, Thomsen KM. Running shoe selection criteria among adolescent cross-country runners. PM & R. 2009;1(9):816-819. doi: 10.1016/j.pmrj.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 31. Escamilla-Martinez E, Martinez-Nova A, Gomez-Martin B, Sanchez-Rodriguez R, Fernandez-Seguin LM. The effect of moderate running on foot posture index and plantar pressure distribution in male recreational runners. J Am Podiatr Med Assoc. 2013;103(2):121-125. doi: 10.7547/1030121. [DOI] [PubMed] [Google Scholar]
- 32. Feuerbach JW, Grabiner MD, Koh TJ, Weiker GG. Effect of an ankle orthosis and ankle ligament anesthesia on ankle joint proprioception. Am J Sports Med. 1994;22(2):223-229. doi: 10.1177/036354659402200212 [DOI] [PubMed] [Google Scholar]
- 33. Fiolkowski P, Brunt D, Bishop M, Woo R, Horodyski M. Intrinsic pedal musculature support of the medial longitudinal arch: an electromyography study. J Foot Ankle Surg. 2003;42(6):327-333. doi: 10.1053/j.jfas.2003.10.003 [DOI] [PubMed] [Google Scholar]
- 34. Freund W, Weber F, Billich C, Schuetz UH. The foot in multistage ultra-marathon runners: experience in a cohort study of 22 participants of the Trans Europe Footrace Project with mobile MRI. BMJ Open. 2012;2(3). doi: 10.1136/bmjopen-2012-001118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Fukano M, Inami T, Nakagawa K, Narita T, Iso S. Foot posture alteration and recovery following a full marathon run. Eur J Sport Sci. 2018;18(10):1338-1345. doi: 10.1080/17461391.2018.1499134 [DOI] [PubMed] [Google Scholar]
- 36. Gallardo E, Garcia A, Combarros O, Berciano J. Charcot-Marie-Tooth disease type 1A duplication: spectrum of clinical and magnetic resonance imaging features in leg and foot muscles. Brain. 2006;129(Pt 2):426-437. doi: 10.1093/brain/awh693 [DOI] [PubMed] [Google Scholar]
- 37. Griffiths IB, Spooner SK. Foot orthoses research: identifying limitations to improve translation to clinical knowledge and practice. Br J Sports Med. 2018;52(6):350. doi: 10.1136/bjsports-2016-096269 [DOI] [PubMed] [Google Scholar]
- 38. Gross ML, Davlin LB, Evanski PM. Effectiveness of orthotic shoe inserts in the long-distance runner. Am J Sports Med. 1991;19(4):409-412. doi: 10.1177/036354659101900416 [DOI] [PubMed] [Google Scholar]
- 39. Harcourt-Smith WE, Aiello LC. Fossils, feet and the evolution of human bipedal locomotion. J Anat. 2004;204(5):403-416. doi: 10.1111/j.0021-8782.2004.00296.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Headlee DL, Leonard JL, Hart JM, Ingersoll CD, Hertel J. Fatigue of the plantar intrinsic foot muscles increases navicular drop. J Electromyogr Kinesiol. 2008;18(3):420-425. doi: 10.1016/j.jelekin.2006.11.004 [DOI] [PubMed] [Google Scholar]
- 41. Hiemstra LA, Lo IK, Fowler PJ. Effect of fatigue on knee proprioception: implications for dynamic stabilization. J Orthop Sports Phys Ther. 2001;31(10):598-605. doi: 10.2519/jospt.2001.31.10.598 [DOI] [PubMed] [Google Scholar]
- 42. Horas K, Fraissler L, Maier G, et al. High prevalence of vitamin D deficiency in patients with bone marrow edema syndrome of the foot and ankle. Foot Ankle Int. 2017;38(7):760-766. doi: 10.1177/1071100717697427 [DOI] [PubMed] [Google Scholar]
- 43. Hreljac A. Impact and overuse injuries in runners. Med Sci Sports Exerc. 2004;36(5):845-849. doi: 10.1249/01.mss.0000126803.66636.dd [DOI] [PubMed] [Google Scholar]
- 44. Hreljac A, Marshall RN, Hume PA. Evaluation of lower extremity overuse injury potential in runners. Med Sci Sports Exerc. 2000;32(9):1635-1641. doi: 10.1097/00005768-200009000-00018 [DOI] [PubMed] [Google Scholar]
- 45. Hulteen RM, Smith JJ, Morgan PJ, et al. Global participation in sport and leisure-time physical activities: a systematic review and meta-analysis. Prev Med. 2017;95:14-25. doi: 10.1016/j.ypmed.2016.11.027 [DOI] [PubMed] [Google Scholar]
- 46. James S, Jones D. Biomechanical aspects of distance running injuries. Human Kinetics Books; 1990. [Google Scholar]
- 47. Janda V, Vavrova M, Hervenova A, et al. Sensory Motor Stimulation. Lippincott Williams & Wilkins; 2006. [Google Scholar]
- 48. Jung DY, Koh EK, Kwon OY. Effect of foot orthoses and short-foot exercise on the cross-sectional area of the abductor hallucis muscle in subjects with pes planus: a randomized controlled trial. J Back Musculoskelet Rehabil. 2011;24(4):225-231. doi: 10.3233/BMR-2011-0299 [DOI] [PubMed] [Google Scholar]
- 49. Kato K, Jevas S, Culpepper D. Body image disturbances in NCAA Division I and III female athletes. Sport J. 2011;14(1):1-2. [Google Scholar]
- 50. Kelly LA, Kuitunen S, Racinais S, Cresswell AG. Recruitment of the plantar intrinsic foot muscles with increasing postural demand. Clin Biomech (Bristol, Avon). 2012;27(1):46-51. doi: 10.1016/j.clinbiomech.2011.07.013 [DOI] [PubMed] [Google Scholar]
- 51. Khan KM, Liu-Ambrose T, Sran MM, et al. New criteria for female athlete triad syndrome? As osteoporosis is rare, should osteopenia be among the criteria for defining the female athlete triad syndrome? Br J Sports Med. 2002;36(1):10-13. doi: 10.1136/bjsm.36.1.10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Kim MH, Kwon OY, Kim SH, Jung DY. Comparison of muscle activities of abductor hallucis and adductor hallucis between the short foot and toe-spread-out exercises in subjects with mild hallux valgus. J Back Musculoskelet Rehabil. 2013;26(2):163-168. doi: 10.3233/BMR-2012-00363 [DOI] [PubMed] [Google Scholar]
- 53. Kornaat PR, Van de Velde SK. Bone marrow edema lesions in the professional runner. Am J Sports Med. 2014;42(5):1242-1246. doi: 10.1177/0363546514521990 [DOI] [PubMed] [Google Scholar]
- 54. Landorf KB, Keenan AM, Herbert RD. Effectiveness of foot orthoses to treat plantar fasciitis: a randomized trial. Arch Intern Med. 2006;166(12):1305-1310. doi: 10.1001/archinte.166.12.1305 [DOI] [PubMed] [Google Scholar]
- 55. Larson P, Higgins E, Kaminski J, et al. Foot strike patterns of recreational and sub-elite runners in a long-distance road race. J Sports Sci. 2011;29(15):1665-1673. doi: 10.1080/02640414.2011.610347 [DOI] [PubMed] [Google Scholar]
- 56. Lazzarini KM, Troiano RN, Smith RC. Can running cause the appearance of marrow edema on MR images of the foot and ankle? Radiology. 1997;202(2):540-542. doi: 10.1148/radiology.202.2.9015087 [DOI] [PubMed] [Google Scholar]
- 57. Lee DC, Pate RR, Lavie CJ, et al. Leisure-time running reduces all-cause and cardiovascular mortality risk. J Am Coll Cardiol. 2014;64(5):472-481. doi: 10.1016/j.jacc.2014.04.058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Lieberman DE, Venkadesan M, Werbel WA, et al. Foot strike patterns and collision forces in habitually barefoot versus shod runners. Nature. 2010;463(7280):531-535. doi: 10.1038/nature08723 [DOI] [PubMed] [Google Scholar]
- 59. Lohman M, Kivisaari A, Vehmas T, et al. MRI abnormalities of foot and ankle in asymptomatic, physically active individuals. Skeletal Radiol. 2001;30(2):61-66. doi: 10.1007/s002560000316 [DOI] [PubMed] [Google Scholar]
- 60. Lun V, Meeuwisse WH, Stergiou P, Stefanyshyn D. Relation between running injury and static lower limb alignment in recreational runners. Br J Sports Med. 2004;38(5):576-580. doi: 10.1136/bjsm.2003.005488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Luo G, Stergiou P, Worobets J, Nigg B, Stefanyshyn D. Improved footwear comfort reduces oxygen consumption during running. Footwear Sci. 2009;1(1):25-29. doi: 10.1080/19424280902993001 [DOI] [Google Scholar]
- 62. Lynn SK, Padilla RA, Tsang KK. Differences in static- and dynamic-balance task performance after 4 weeks of intrinsic-foot-muscle training: the short-foot exercise versus the towel-curl exercise. J Sport Rehabil. 2012;21(4):327-333. doi: 10.1123/jsr.21.4.327 [DOI] [PubMed] [Google Scholar]
- 63. Malisoux L, Nielsen RO, Urhausen A, Theisen D. A step towards understanding the mechanisms of running-related injuries. J Sci Med Sport. 2015;18(5):523-528. doi: 10.1016/j.jsams.2014.07.014 [DOI] [PubMed] [Google Scholar]
- 64. Mann R, Inman VT. Phasic activity of intrinsic muscles of the foot. J Bone Joint Surg Am. 1964;46:469-481. [PubMed] [Google Scholar]
- 65. Mann RA, Hagy JL. The function of the toes in walking, jogging and running. Clin Orthop Relat Res. 1979(142):24-29. [PubMed] [Google Scholar]
- 66. McKeon PO, Hertel J, Bramble D, Davis I. The foot core system: a new paradigm for understanding intrinsic foot muscle function. Br J Sports Med. 2015;49(5):290. doi: 10.1136/bjsports-2013-092690 [DOI] [PubMed] [Google Scholar]
- 67. Michelson JD, Durant DM, McFarland E. The injury risk associated with pes planus in athletes. Foot Ankle Int. 2002;23(7):629-633. doi: 10.1177/107110070202300708 [DOI] [PubMed] [Google Scholar]
- 68. Milani TL, Hennig EM, Lafortune MA. Perceptual and biomechanical variables for running in identical shoe constructions with varying midsole hardness. Clin Biomech (Bristol, Avon). 1997;12(5):294-300. doi: 10.1016/s0268-0033(97)00008-9 [DOI] [PubMed] [Google Scholar]
- 69. Miller JE, Nigg BM, Liu W, Stefanyshyn DJ, Nurse MA. Influence of foot, leg and shoe characteristics on subjective comfort. Foot Ankle Int. 2000;21(9):759-767. doi: 10.1177/107110070002100908 [DOI] [PubMed] [Google Scholar]
- 70. Milner CE, Ferber R, Pollard CD, Hamill J, Davis IS. Biomechanical factors associated with tibial stress fracture in female runners. Med Sci Sports Exerc. 2006;38(2):323-328. doi: 10.1249/01.mss.0000183477.75808.92 [DOI] [PubMed] [Google Scholar]
- 71. Mulligan EP, Cook PG. Effect of plantar intrinsic muscle training on medial longitudinal arch morphology and dynamic function. Man Ther. 2013;18(5):425-430. doi: 10.1016/j.math.2013.02.007 [DOI] [PubMed] [Google Scholar]
- 72. Mundermann A, Stefanyshyn DJ, Nigg BM. Relationship between footwear comfort of shoe inserts and anthropometric and sensory factors. Med Sci Sports Exerc. 2001;33(11):1939-1945. doi: 10.1097/00005768-200111000-00021 [DOI] [PubMed] [Google Scholar]
- 73. Munteanu SE, Scott LA, Bonanno DR, et al. Effectiveness of customised foot orthoses for Achilles tendinopathy: a randomised controlled trial. Br J Sports Med. 2015;49(15):989-994. doi: 10.1136/bjsports-2014-093845 [DOI] [PubMed] [Google Scholar]
- 74. Myerson MS, Shereff MJ. The pathological anatomy of claw and hammer toes. J Bone Joint Surg Am. 1989;71(1):45-49. [PubMed] [Google Scholar]
- 75. Nazem TG, Ackerman KE. The female athlete triad. Sports Health. 2012;4(4):302-311. doi: 10.1177/1941738112439685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76. Nielsen RO, Buist I, Parner ET, et al. Foot pronation is not associated with increased injury risk in novice runners wearing a neutral shoe: a 1-year prospective cohort study. Br J Sports Med. 2014;48(6):440-447. doi: 10.1136/bjsports-2013-092202 [DOI] [PubMed] [Google Scholar]
- 77. Nigg BM, Baltich J, Hoerzer S, Enders H. Running shoes and running injuries: mythbusting and a proposal for two new paradigms: 'preferred movement path' and 'comfort filter.' Br J Sports Med. 2015;49(20):1290-1294. doi: 10.1136/bjsports-2015-095054 [DOI] [PubMed] [Google Scholar]
- 78. Nigg BM, Khan A, Fisher V, Stefanyshyn D. Effect of shoe insert construction on foot and leg movement. Med Sci Sports Exerc. 1998;30(4):550-555. doi: 10.1097/00005768-199804000-00013 [DOI] [PubMed] [Google Scholar]
- 79. Nilsson J, Thorstensson A. Ground reaction forces at different speeds of human walking and running. Acta Physiol Scand. 1989;136(2):217-227. doi: 10.1111/j.1748-1716.1989.tb08655.x [DOI] [PubMed] [Google Scholar]
- 80. Prentice WE. Rehabilitation Techniques in Sports Medicine. New York: McGraw Hill Higher Education; 2009. [Google Scholar]
- 81. Reeser LA, Susman RL, Stern JT., Jr. Electromyographic studies of the human foot: experimental approaches to hominid evolution. Foot Ankle. 1983;3(6):391-407. doi: 10.1177/107110078300300607 [DOI] [PubMed] [Google Scholar]
- 82. Reinschmidt C, van Den Bogert AJ, Murphy N, Lundberg A, Nigg BM. Tibiocalcaneal motion during running, measured with external and bone markers. Clin Biomech (Bristol, Avon). 1997;12(1):8-16. doi: 10.1016/s0268-0033(96)00046-0 [DOI] [PubMed] [Google Scholar]
- 83. Richards CE, Magin PJ, Callister R. Is your prescription of distance running shoes evidence-based? Br J Sports Med. 2009;43(3):159-162. doi: 10.1136/bjsm.2008.046680 [DOI] [PubMed] [Google Scholar]
- 84. Ridge ST, Johnson AW, Mitchell UH, et al. Foot bone marrow edema after a 10-wk transition to minimalist running shoes. Med Sci Sports Exerc. 2013;45(7):1363-1368. doi: 10.1249/MSS.0b013e3182874769 [DOI] [PubMed] [Google Scholar]
- 85. Rodgers MM, Leveau BF. Effectiveness of foot orthotic devices used to modify pronation in runners*. J Orthop Sports Phys Ther. 1982;4(2):86-90. [DOI] [PubMed] [Google Scholar]
- 86. Ronto P. The state of Ultra Running 2020. 2021; https://runrepeat.com/state-of-ultra-running.
- 87. Rothermel S, Hale S, Hertel J, Denegar C. Effect of active foot positioning on the outcome of a balance training program. Phys Ther Sport. 2004;5(2). [Google Scholar]
- 88. Rue JP, Armstrong DW, Frassica FJ, Deafenbaugh M, Wilckens JH. The effect of pulsed ultrasound in the treatment of tibial stress fractures. Orthopedics. 2004;27(11):1192-1195. doi: 10.3928/0147-7447-20041101-18 [DOI] [PubMed] [Google Scholar]
- 89. Shimasaki Y, Nagao M, Miyamori T, et al. Evaluating the risk of a fifth metatarsal stress fracture by measuring the serum 25-hydroxyvitamin D levels. Foot Ankle Int. 2016;37(3):307-311. doi: 10.1177/1071100715617042 [DOI] [PubMed] [Google Scholar]
- 90. Shiotani H, Mizokuchi T, Yamashita R, Naito M, Kawakami Y. Acute effects of long-distance running on mechanical and morphological properties of the human plantar fascia. Scand J Med Sci Sports. 2020;30(8):1360-1368. doi: 10.1111/sms.13690 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Shorten MR. The energetics of running and running shoes. J Biomech. 1993;26(suppl 1):41-51. doi: 10.1016/0021-9290(93)90078-s [DOI] [PubMed] [Google Scholar]
- 92. Shorten MR. Running Shoe Design: Protection and Performance. Royal Society of Medicine Press Limited; 2000. [Google Scholar]
- 93. Shorten MR, Winslow DS. Spectral analysis of impact shock during running. Int J Sport Biomech. 1992;8(4):288-304. [Google Scholar]
- 94. Soysa A, Hiller C, Refshauge K, Burns J. Importance and challenges of measuring intrinsic foot muscle strength. J Foot Ankle Res. 2012;5(1):29. doi: 10.1186/1757-1146-5-29 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95. Stacoff A, Nigg BM, Reinschmidt C, van den Bogert AJ, Lundberg A. Tibiocalcaneal kinematics of barefoot versus shod running. J Biomech. 2000;33(11):1387-1395. [DOI] [PubMed] [Google Scholar]
- 96. Stacoff A, Reinschmidt C, Nigg BM, et al. Effects of foot orthoses on skeletal motion during running. Clin Biomech (Bristol, Avon). 2000;15(1):54-64. doi: 10.1016/s0268-0033(99)00028-5 [DOI] [PubMed] [Google Scholar]
- 97. Stewart S, Ellis R, Heath M, Rome K. Ultrasonic evaluation of the abductor hallucis muscle in hallux valgus: a cross-sectional observational study. BMC Musculoskelet Disord. 2013;14:45. doi: 10.1186/1471-2474-14-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Sulowska I, Oleksy L, Mika A, Bylina D, Soltan J. The influence of plantar short foot muscle exercises on foot posture and fundamental movement patterns in long-distance runners, a non-randomized, non-blinded clinical trial. PloS One. 2016;11(6):e0157917. doi: 10.1371/journal.pone.0157917 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Susman RL, Stern JT, Jungers WL. Arboreality and bipedality in the Hadar hominids. Folia Primatol (Basel). 1984;43(2-3):113-156. doi: 10.1159/000156176 [DOI] [PubMed] [Google Scholar]
- 100. Taunton JE, Clement DB, Smart GW, Wiley JP, McNicol KL. A triplanar electrogoniometer investigation of running mechanics in runners with compensatory overpronation. Can J Appl Sport Sci. 1985;10(3):104-115. [PubMed] [Google Scholar]
- 101. Taunton JE, Ryan MB, Clement DB, et al. A retrospective case-control analysis of 2002 running injuries. Br J Sports Med. 2002;36(2):95-101. doi: 10.1136/bjsm.36.2.95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Udofa AB, Clark KP, Ryan LJ, Weyand PG. Running ground reaction forces across footwear conditions are predicted from the motion of two body mass components. J Appl Physiol. 2019;126(5):1315-1325. doi: 10.1152/japplphysiol.00925.2018. [DOI] [PubMed] [Google Scholar]
- 103. van der Worp MP, ten Haaf DS, van Cingel R, et al. Injuries in runners; a systematic review on risk factors and sex differences. PloS One. 2015;10(2):e0114937. doi: 10.1371/journal.pone.0114937 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. van Gent RN, Siem D, van Middelkoop M, et al. Incidence and determinants of lower extremity running injuries in long distance runners: a systematic review. Br J Sports Med. 2007;41(8):469-480; discussion 480. doi: 10.1136/bjsm.2006.033548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105. Van Middelkoop M, Kolkman J, Van Ochten J, Bierma-Zeinstra SM, Koes BW. Risk factors for lower extremity injuries among male marathon runners. Scand J Med Sci Sports. 2008;18(6):691-697. doi: 10.1111/j.1600-0838.2007.00768.x [DOI] [PubMed] [Google Scholar]
- 106. Videbaek S, Bueno AM, Nielsen RO, Rasmussen S. Incidence of running-related injuries per 1000 h of running in different types of runners: a systematic review and meta-analysis. Sports Med. 2015;45(7):1017-1026. doi: 10.1007/s40279-015-0333-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. Ward CV, Kimbel WH, Johanson DC. Complete fourth metatarsal and arches in the foot of Australopithecus afarensis. Science. 2011;331(6018):750-753. doi: 10.1126/science.1201463 [DOI] [PubMed] [Google Scholar]
- 108. Warden SJ, Davis IS, Fredericson M. Management and prevention of bone stress injuries in long-distance runners. J Orthop Sports Phys Ther. 2014;44(10):749-765. doi: 10.2519/jospt.2014.5334 [DOI] [PubMed] [Google Scholar]
- 109. Williams K, Askew C, Mazoue C, et al. Vitamin D3 supplementation and stress fractures in high-risk collegiate athletes - a pilot study. Orthop Res Rev. 2020;12:9-17. doi: 10.2147/ORR.S233387 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Woensel WV, Cavanagh P. A perturbation study of lower extremity motion during running. Int J Sport Biomech. 1992;8:30-47. [Google Scholar]
- 111. Zammit GV, Payne CB. Relationship between positive clinical outcomes of foot orthotic treatment and changes in rearfoot kinematics. J Am Podiatr Med Assoc. 2007;97(3):207-212. doi: 10.7547/0970207 [DOI] [PubMed] [Google Scholar]
- 112. Zifchock RA, Davis I, Hamill J. Kinetic asymmetry in female runners with and without retrospective tibial stress fractures. J Biomech. 2006;39(15):2792-2797. doi: 10.1016/j.jbiomech.2005.10.003 [DOI] [PubMed] [Google Scholar]