Abstract
Background
Prostate needle biopsy (PNB) remains the referent standard for diagnosing prostate cancer. Contemporary data highlight an increase in PNB-related infections particularly when performed transrectally. Non-infectious complications, however, may similarly contribute to biopsy-related morbidity. We review the incidence and predictors of non-infectious complications following transrectal PNB in a large statewide quality registry.
Methods
Transrectal ultrasound-guided prostate needle biopsies performed between 2015 and 2018 were retrospectively reviewed. The incidence and distribution of non-infectious complications were annotated. Clinical, demographic, and biopsy variables of interest were evaluated by logistic regression for potential association with specific types of non-infectious complications.
Results
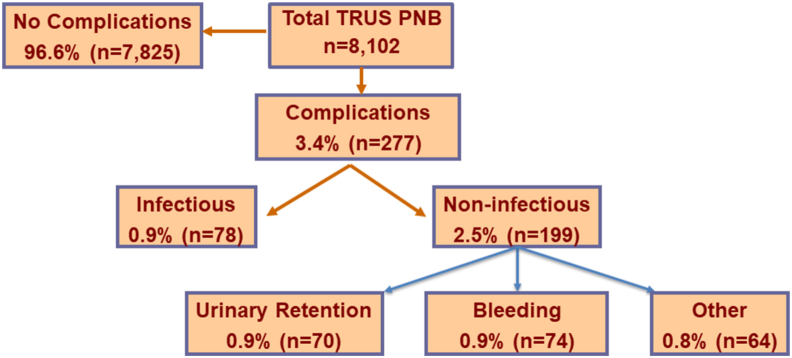
Of 8,102 biopsies, 277 (3.4%) biopsies had reported post-procedure complications including 199 (2.5%) non-infectious and 78 (0.9%) infectious. Among the non-infectious complications, the most common events included urinary or rectal bleeding (74; 0.9%), urinary retention (70, 0.9%), vasovagal syncope (13, 0.2%), and severe post-operative pain (10, 0.1%). Approximately 56% of these non-infectious complications required an Emergency Department visit (111/199) and 27% (54/199) hospital admission for monitoring. Increasing transrectal ultrasound prostate volume was associated with post-procedure urinary retention (Odds ratio (OR) 1.07, 1.02–1.11, p = 0.002). No specific variables noted association with post-biopsy bleeding.
Conclusion
Non-infectious complications occurred 2.5 times more often than infectious complications following transrectal ultrasound prostate needle biopsies. Larger prostate size was associated with a greater risk of post-procedure urinary retention. These data originating from experience from over 100 urologists across different health systems provide an important framework in counseling patients regarding expectations following transrectal prostate biopsy.
Keywords: Biopsy, Complications, Non-infectious, Prostate
1. Introduction
Prostate cancer is the most common cancer in men, with 1 in 9 being diagnosed in their lifetime and more than 3.6 million currently, or previously, carrying the diagnosis in the United States.1,2 Indications for prostate biopsy include the clinical suspicion of prostate cancer by digital rectal examination, elevation of prostate specific antigen level, and/or suspicious imaging.3,4 Transrectal ultrasound-guided prostate biopsy (TRUS PNB) is currently one approach for making a histological diagnosis of prostate cancer. This procedure is frequently performed in an outpatient setting with over 2 million cases annually in the United States and Europe.5
Infectious complications, including urinary tract infections, urosepsis, abscesses, and prostatitis, are one of the most common adverse sequelae of TRUS PNB.6 Contemporary data highlight an increase in PNB-related infections7 and accordingly algorithms with the goal of decreasing these inherent infectious risks have been proposed.8, 9, 10
Non-infectious complications, such as hematuria, bleeding, urinary retention, and erectile dysfunction, also contribute to biopsy-related morbidity, and add to the increasing average cost of care, which has been estimated at $5,800 per post-biopsy hospitalization.7,11 Most burdensome of the non-infectious complications include hematuria and urinary retention.11,12 Prior reports highlight the incidence of hematuria ranging from 5 to 90% with less than 1% of patients requiring hospitalization. Urinary retention has been reported to occur in 0.4–6% of procedures and requires intervention at a rate of 0.2–2.6%.7,11
Discussing such complications with patients optimizes counseling prior to TRUS PNB. Literature to date has largely focused on single or multi-institution series or administrative claims data. To better encompass a contemporary experience spanning a large and diverse patient cohort, we evaluated TRUS PNB outcomes within a large regional quality collaborative. We sought to both determine the rates of non-infectious complications, need for ancillary medical care, and associations with clinical, demographic, and biopsy-related variables.
2. Patients and methods
The Pennsylvania Urologic Regional Collective is a physician led partnership of eleven health care organizations based in Pennsylvania and New Jersey with the Health Care Improvement Foundation. The aim of this consortium is to collect regional prostate biopsy and cancer data to reduce variation in access and care, track clinical outcomes for prostate cancer, and improve therapies offered to patients. Patient data is inputted into to a shared, de-identified database, and covers many aspects of the treatment course, including laboratory parameters, biopsy information, and subsequent therapy.
After receiving institutional review board and individual site approval, we accrued and retrospectively analyzed data on 8,102 transrectal prostate needle biopsies performed from 2015 to 2018. Our query first isolated reported complications within the dataset. We then filtered these patients by type of complication (infectious and non-infectious) including those that had a combination of such complications. The frequency and need for additional medical care for specific non-infectious complication types was then evaluated.
Among our data set, eight clinical and biopsy-related variables of interest were reviewed for association with non-infectious complications. These variables were selected based on prior publications and included number of prior biopsies (0 or ≥ 1), presence of cancer on biopsy, number of cores obtained, ultrasound (US) guided prostate volume (cc), body mass index (BMI), history of prostatitis, peripheral vascular disease, and coronary vascular disease. Routine practice within the Pennsylvania Urologic Regional Collective includes stopping therapeutic anticoagulants and platelet modifying medications 3–7 days prior to procedures based on specific agent. The doses of anticoagulation or anti-platelet medications (i.e., 81 mg aspirin) that did not impact coagulation cascade or bleeding time were not recorded within our dataset. Therefore, due to low numbers, these were not queried variables.
Logistical regression was determined if significant associations existed between variables of interest and the most common non-infectious complications. The significance level was finalized at 5%. All data analyses were performed using SPSS Statistics, Version 27.0.
3. Results
8,102 men with a median age of 68 years (range, 45–86) underwent a transrectal ultrasound-guided biopsy. Median BMI of patients was 28, 18% of patient had a history of diabetes, 20% had a recorded history of prostatitis, and 2% had either peripheral or cardiovascular disease. For 84% of patients, this marked their first biopsy, 11% of patients had one prior biopsy, and 5% had multiple prior biopsies. At biopsy, median cores obtained was 12 (range, 3–48) and median prostate volume was 43 cc (range, 5–666). 62% of patients had evidence of cancer on biopsy.
277 of 8,102 (3.4%) had a documented post-biopsy complication of which 78 (0.9%) were infectious and 199 (2.5%) were non-infectious (Fig. 1). Among those 78 with infectious complications, the distribution included 32 (41%) with urinary tract infections, 29 (37%) with fevers, and 17 (22%) with sepsis. Forty-nine of these 78 patients (63%) required an Emergency Department (ED) visit while 44 (56%) patients were admitted to the hospital for treatment.
Fig. 1.
Distribution of complications in 8102 patients undergoing TRUS PNB. TRUS PNB, transrectal ultrasound-guided prostate needle biopsies.
Of the total 199 non-infectious complications, the most common etiologies included urinary or rectal bleeding (74; 37%), urinary retention (70, 35%), vasovagal syncope (13, 7%), and severe post-operative pain (10, 5%). 111 (56%) of the 199 non-infectious complication resulted in an ED visit, while 54 (27%) non-infectious complications required hospitalization. The management of non-infectious complications was almost exclusively conservative, including observation with analgesia, intravenous fluid hydration, urinary catheter placement ± bladder irrigation, and rectal packing for bleeding. Recalcitrant bleeding events requiring procedural intervention included urinary tract hemorrhage requiring cystoscopy and fulguration and rectal vault bleeding necessitating endoscopic clipping. Among the patients who presented with a non-infectious complication, 17 (9%) non-infectious complications subsequently developed an infection within the urinary tract.
When specifically considering associations with non-infectious complications, we focused on the two most common events: urinary retention and bleeding. With respect to urinary retention, larger gland size was the only variable significantly associated with an increased risk of this event (OR 1.07 per 5 cc increase, 95% CI 1.02–1.11, P = 0.002) (Table 1). For urinary or rectal bleeding complications, no specific clinical or pathological variables were identified (Table 2).
Table 1.
Association of Variables of Interest with post-TRUS PNB Urinary Retention
| Variable | Odds ratio (95% CI) | P |
|---|---|---|
| 0 prior biopsies | 0.62 (0.23–1.70) | 0.36 |
| ≥1 prior biopsies | 0.68 (0.19–2.38) | 0.54 |
| Cancer present on current biopsy | 0.76 (0.43–1.35) | 0.35 |
| Number of cores obtained | 1.22 (0.41–3.65) | 0.72 |
| US Prostate volume (cc) | 1.07 (1.02–1.11) | 0.002 |
| BMI | 0.92 (0.65–1.29) | 0.63 |
| Prostatitis history | 1.39 (0.43–4.49) | 0.58 |
| Vascular disease history | 1.81 (0.36–9.20) | 0.47 |
Table 2.
Association of Variables of Interest with post-TRUS PNB and Bleeding Complications
| Variable | Odds Ratio (95% CI) | P |
|---|---|---|
| 0 prior biopsies | 1.07 (0.34–3.32) | 0.91 |
| ≥1 prior biopsies | 0.85 (0.19–3.71) | 0.83 |
| Cancer present on current biopsy | 1.04 (0.53–2.06) | 0.90 |
| Number of cores obtained | 1.15 (0.93–1.42) | 0.19 |
| US Prostate volume (cc) | 0.98 (0.94–1.02) | 0.33 |
| BMI | 0.89 (0.63–1.25) | 0.51 |
| Prostatitis | 0.83 (0.16–4.21) | 0.83 |
| Vascular disease history | 2.40 (0.33–17.56) | 0.39 |
4. Discussion
Following the Unites States Preventative Task Force recommendation in 2012, a reduction in the number of prostate biopsies was observed.13 However, TRUS PNB still remains as an integral component of prostate cancer diagnosis and surveillance for patients. TRUS PNB is generally a well-tolerated procedure performed in the outpatient setting. Complications following TRUS PNB are classified as either infectious or non-infectious. The prevention, management, and impact of infectious complications on our healthcare system are well studied. Non-infectious complications, along with their management, have similarly been documented.14
Both infectious and non-infectious complications, following TRUS PNB, have been previously reported to result in hospitalization at a rate as high as 6.9%.12,15,16 Non-infectious complications have been reported to occur in upward of 90% of patients.12,17 Though most are mild and transient, some such as urinary retention, require medical intervention upward of 2.6% of cases.6,11 Identifying at-risk patients for non-infectious complications appropriately sets patient expectations and may potentially obviate or mitigate such complications from occurring. For example, Hara et al., in 2008, showed that the administration of an alpha-blocker the day prior to, and seven days following, biopsy, experienced less acute urinary retention.18
We present a large multi-hospital experience of TRUS PNB focusing both on the incidence of non-infectious complications as well as factors associated with their occurrence. We noted an overall complication rate of 3.4%, with non-infectious complications occurring 2.5 times more often than infectious complications. Our infection-related complication rate was 0.9%, which was slightly lower than previously reported rates of 1.2–4.1%.12,19
The most common non-infectious complications observed within our study was bleeding and urinary retention. The incidence of bleeding has been reported to vary with patient factors such as prostate size, anticoagulant medications, medical comorbidities, anxiety, and procedural factors such as the number of biopsy cores taken.15,20 We, however, did not identify any significant correlation between our clinical and pathological variables of interest and bleeding. Notably, within our cohort, patients rarely undergo biopsy under therapeutic anticoagulant or anti-platelet therapy and thus the association of such medications with bleeding complications was not assessed.
Our results confirmed prior studies noting that urinary retention is indeed one of the more common non-infectious complications following TRUS PNB. The risk of urinary retention after TRUS PNB ranges from 0.2 to 1.7%11 and is usually transient without requiring surgical intervention. Not surprising, we did find that increasing prostate gland size was significantly associated with an increasing risk of urinary retention. Other studies have previously confirmed this observation.21,22 We did not, however, note that the number of biopsy cores was associated with an increased risk of urinary retention as others previously have observed.23 Raaijmakers et al. reported that ratio of transition zone volume to total prostate volume and a higher IPSS are also associated with an increased risk of urinary retention after prostate biopsy in addition to prostate volume.21 Our data did not have the granularity to specifically evaluate baseline IPSS score or transition zone volume.
Patients’ expectations play an important role on physical and mental outcomes-procedure.24 Providing information as highlighted in this manuscript during pre-biopsy counseling appropriately sets patient expectations following TRUS PNB. Although infectious complications are the leading cause for hospital admission following TRUS PNB, we found that over 50% of non-infectious complications also yielded a hospital admission.
We acknowledge several limitations. This study originates from a large multi-center data set with annotated data entry by persons not involved in patient care. Therefore, the review is retrospective and the complication rates are attributable to recall bias. We further acknowledge that due to recall bias, our complication rates are likely lower than the reported literature and also enriched in more significant sequelae warranting documentation in the respective electronic medical records. Additionally, the study was limited by the inconsistency of documentation of anticoagulation and anti-platelet use in the data extraction particularly when considering lower dose regimens. Nonetheless, we believe this series from over 8000 biopsies performed by over 100 urologists provides robust and meaningful outcomes data that aid in patient counseling prior to TRUS PNB.
5. Conclusions
Non-infectious complications occurred in 2.5% of patients undergoing TRUS PNB with the most common events including urinary or rectal bleeding (0.9%) and urinary retention (0.9%). Over 50% of these complications required an ED visit and over 25% hospital admission for monitoring. Larger prostate size was associated with a higher risk of urinary retention following TRUS PNB.
Funding
The Keith and Lynda Harring Fund for Urology Research at Penn State Health.
Conflicts of interest
The authors have no conflict of interest pertaining to the material published in this manuscript.
References
- 1.Torre L.A., Siegel R.L., Ward E.M., Jemal A. Global Cancer Incidence and Mortality Rates and Trends--An Update. Cancer Epidemiol Biomarkers Prev. 2016 Jan;25(1):16–27. doi: 10.1158/1055-9965.EPI-15-0578. 10.1158/1055-9965.EPI-15-0578 Epub 2015 Dec 14. PMID: 26667886. [DOI] [PubMed] [Google Scholar]
- 2.American Cancer Society . 2022. Key Statistics for Prostate Cancer.https://www.cancer.org/cancer/prostate-cancer/about/key-statistics.html [Google Scholar]
- 3.Ross A.E., Loeb S., Landis P., Partin A.W., Epstein J.I., Kettermann A., et al. Prostate-specific antigen kinetics during follow-up are an unreliable trigger for intervention in a prostate cancer surveillance program. J Clin Oncol. 2010 Jun 10;28(17):2810–2816. doi: 10.1200/JCO.2009.25.7311. 10.1200/JCO.2009.25.7311 Epub 2010 May 3. PMID: 20439642. [DOI] [PubMed] [Google Scholar]
- 4.Roobol M.J., Kranse R., Bangma C.H., ERSPC Rotterdam Study Group Screening for prostate cancer: results of the Rotterdam section of the European randomized study of screening for prostate cancer. Eur Urol. 2013 Oct;64(4):530–539. doi: 10.1016/j.eururo.2013.05.030. 10.1016/j.eururo.2013.05.030 Epub 2013 May 25. PMID: 23759326. [DOI] [PubMed] [Google Scholar]
- 5.Zembower T.R., Maxwell K.M., Nadler R.B., Cashy J., Scheetz M.H., Qi C., et al. Evaluation of targeted antimicrobial prophylaxis for transrectal ultrasound guided prostate biopsy: a prospective cohort trial. BMC Infect Dis. 2017 Jun 7;17(1):401. doi: 10.1186/s12879-017-2470-1. 10.1186/s12879-017-2470-1 PMID: 28592230; PMCID: PMC5463462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Borghesi M., Ahmed H., Nam R., Schaeffer E., Schiavina R., Taneja S., et al. Complications after systematic, random, and image-guided prostate biopsy. Eur Urol. 2017 Mar;71(3):353–365. doi: 10.1016/j.eururo.2016.08.004. 10.1016/j.eururo.2016.08.004 Epub 2016 Aug 17. PMID: 27543165. [DOI] [PubMed] [Google Scholar]
- 7.Roberts M.J., Bennett H.Y., Harris P.N., Holmes M., Grummet J., Naber K., et al. Prostate biopsy-related infection: a systematic review of risk factors, prevention strategies, and management approaches. Urology. 2017 Jun;104:11–21. doi: 10.1016/j.urology.2016.12.011. 10.1016/j.urology.2016.12.011 Epub 2016 Dec 19. PMID: 28007492. [DOI] [PubMed] [Google Scholar]
- 8.Fahmy A., Rhashad H., Mohi M., Elabbadie A., Kotb A. Optimizing prophylactic antibiotic regimen in patients admitted for transrectal ultrasound-guided prostate biopsies: a prospective randomized study. Prostate Int. 2016 Sep;4(3):113–117. doi: 10.1016/j.prnil.2016.06.001. 10.1016/j.prnil.2016.06.001 Epub 2016 Jul 1. PMID: 27689069; PMCID: PMC5031895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lim D.G., Jung S.I., Kim M.S., Chung H.S., Hwang E.C., Kwon D.D. Comparison of a combined regimen of fosfomycin and ciprofloxacin with ciprofloxacin alone as antimicrobial prophylaxis for transrectal prostate biopsy in the era of high fluoroquinolone-resistant rectal flora. Prostate Int. 2021 Sep;9(3):163–168. doi: 10.1016/j.prnil.2021.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ramedani S., Clark J.Y., Knoedler J.J., MacDonald S., Kaag M.G., Merrill S.B., et al. Topical antiseptic at time of transrectal ultrasound prostate biopsy is associated with fewer severe clinical infections and improves antibiotic stewardship. Prostate Int. 2021 Dec;9(4):185–189. doi: 10.1016/j.prnil.2021.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loeb S., Vellekoop A., Ahmed H.U., Catto J., Emberton M., Nam R., et al. Systematic review of complications of prostate biopsy. Eur Urol. 2013 Dec;64(6):876–892. doi: 10.1016/j.eururo.2013.05.049. [DOI] [PubMed] [Google Scholar]
- 12.Pinkhasov G.I., Lin Y.K., Palmerola R., Smith P., Mahon F., Kaag M.G., et al. Complications following prostate needle biopsy requiring hospital admission or emergency department visits – experience from 1000 consecutive cases. BJU Int. 2012 Aug;110(3):369–374. doi: 10.1111/j.1464-410X.2011.10926.x. [DOI] [PubMed] [Google Scholar]
- 13.Blair B.M., Robyak H., Clark J.Y., Kaag M.G., Lehman E.B., Raman J.D. Impact of United States preventive services task force recommendations on prostate biopsy characteristics and disease presentation at a tertiary-care medical center. Prostate Int. 2018 Sep;6(3):110–114. doi: 10.1016/j.prnil.2018.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Liss M.A., Ehdaie B., Loeb S., Meng M.V., Raman J.D., Spears V., et al. An update of the American urological association white paper on the prevention and treatment of the more common complications related to prostate biopsy. J Urol. 2017 Aug;198(2):329–334. doi: 10.1016/j.juro.2017.01.103. [DOI] [PubMed] [Google Scholar]
- 15.Loeb S., Carter H.B., Berndt S.I., Ricker W., Schaeffer E.M. Complications after prostate biopsy: data from SEER-Medicare. J Urol. 2011 Nov;186(5):1830–1834. doi: 10.1016/j.juro.2011.06.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ganeswaran D., Sweeney C., Yousif F., Lang S., Goodman C., Nabi G. Population-based linkage of health records to detect urological complications and hospitalisation following transrectal ultrasound-guided biopsies in men suspected of prostate cancer. World J Urol. 2014 Apr;32(2):309–315. doi: 10.1007/s00345-012-0893-2. [DOI] [PubMed] [Google Scholar]
- 17.Shen P.F., Zhu Y.C., Wei W.R., Li Y.Z., Yang J., Li Y.T., et al. The results of transperineal versus transrectal prostate biopsy: a systematic review and meta-analysis. Asian J Androl. 2012 Mar;14(2):310–315. doi: 10.1038/aja.2011.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hara R., Jo Y., Fujii T., Kondo N., Yokoyoma T., Miyaji Y., et al. Optimal approach for prostate cancer detection as initial biopsy: prospective randomized study comparing transperineal versus transrectal systematic 12-core biopsy. Urology. 2008 Feb;71(2):191–195. doi: 10.1016/j.urology.2007.09.029. [DOI] [PubMed] [Google Scholar]
- 19.Nam R.K., Saskin R., Lee Y., Liu Y., Law C., Klotz L.H., et al. Increasing hospital admission rates for urological complications after transrectal ultrasound guided prostate biopsy. J Urol. 2010 Mar;183(3):963–968. doi: 10.1016/j.juro.2009.11.043. [DOI] [PubMed] [Google Scholar]
- 20.Borghesi M., Ahmed H., Nam R., Schaeffer E., Schiavina R., Taneja S., et al. Complications after systematic, random, and image-guided prostate biopsy. Eur Urol. 2017 Mar;71(3):353–365. doi: 10.1016/j.eururo.2016.08.004. [DOI] [PubMed] [Google Scholar]
- 21.Raaijmakers R., Kirkels W.J., Roobol M.J., Wildhagen M.F., Schrder F.H. Complication rates and risk factors of 5802 transrectal ultrasound-guided sextant biopsies of the prostate within a population-based screening program. Urology. 2002 Nov;60(5):826–830. doi: 10.1016/s0090-4295(02)01958-1. [DOI] [PubMed] [Google Scholar]
- 22.Zaytoun O.M., Anil T., Moussa A.S., Jianbo L., Fareed K., Jones J.S., et al. Morbidity of prostate biopsy after simplified versus complex preparation protocols: assessment of risk factors. Urology. 2011 Apr;77(4):910–914. doi: 10.1016/j.urology.2010.12.033. [DOI] [PubMed] [Google Scholar]
- 23.Berger A.P., Gozzi C., Steiner H., Frauscher F., Varkarakis J., Rogatsch H., et al. Complication rate of transrectal ultrasound guided prostate biopsy: a comparison among 3 protocols with 6, 10 and 15 cores. J Urol. 2004 Apr;171(4):1478–1480. doi: 10.1097/01.ju.0000116449.01186.f7. [DOI] [PubMed] [Google Scholar]
- 24.Laferton J.A., Kube T., Salzmann S., Auer C.J., Shedden-Mora M.C. Patients’ expectations regarding medical treatment: a critical review of concepts and their assessment. Front Psychol. 2017 Feb 21;8:233. doi: 10.3389/fpsyg.2017.00233. [DOI] [PMC free article] [PubMed] [Google Scholar]