Abstract
Developing continuing medical education (CME) training programs is a strategy for communicating emerging science to health practitioners. This research tests the feasibility of using CME modules for translating and disseminating research findings from the Breast Cancer and Environment Research Program. Recent findings have identified certain windows of susceptibility, like during puberty, in which exposure to endocrine-disrupting chemicals can increase breast cancer risk later in life. In order to reach pediatric patients and their caregivers, using a Diffusion of Innovations framework, pediatric health care providers were identified as opinion leaders. Two CME modules informed by theory and formative research were tested with a sample of pediatricians and pediatric nurse practitioners. Participants completed knowledge, attitude, intention, and behavior items immediately before and after exposure to a randomly assigned module, and then again three weeks later. Quantitative and qualitative results indicate knowledge gain and strong links between practitioners’ intentions to enact and implemented behavior learned from training recommendations with parents and caregivers in their practices. Results indicate that CMEs can be an effective strategy for translational activities targeted to health providers in order to change behavior within practice.
Since the inception of the Breast Cancer and the Environment Research Program (BCERP) in 2003 (see bcerp.org), a fundamental part of its mission has been translational research, which has the goal to move important medical and scientific findings to individuals who need the information the most (Sung et al. 2003). To meet the translational mission of the BCERP, communication scientists and community partners have translated and disseminated epidemiological and biological research findings that connect environmental factors with breast cancer risk via townhall meetings, videos, pamphlets (BCERP, 2016), and website resources (bcerp.org).
Reaching health care providers so they are knowledgeable about emerging scientific findings is difficult given that providers generally maintain busy practice schedules and already have limited time with their patients (Zabar et al., 2010). Perhaps because of this, few purposeful efforts have attempted to disseminate strategic and theory-driven information to health care providers (Dearing & Krueter, 2010). However, recent findings demonstrate the utility of using Continuing Medical Education (CME) to improve knowledge and overall care for providers (Rotthoff et al., 2011; Silk et al., 2019), and specifically for pediatricians (Boese-O’Reilly, 2007; Finnegan et al., 2020; Nelson, 2019). Relevant research has aimed to improve training methods for providers, in general, (Burns et al., 2016; Hildenbrand, 2020) and training methods for pediatricians (Gittelman et al., 2015; Hardy et al., 2019; Jones et al., 2009; Kainth et al. 2018; Kumar et al., 2012; Pak-Gorstein et al. 2018), indicating that translational efforts (Silk et al., 2019), or “implementation science” (Blair, 2014), can be successful in moving insights from research findings into practice. CME is a translational opportunity to reach health care providers with emerging findings about the environment and breast cancer so that providers may share breast cancer risk reduction information with their patients and caregivers.
The current study evaluated the feasibility of using CME to encourage pediatric health care providers (PHCPs) to move emerging science on the breast cancer and environment connection to patients and caregivers, incorporating persuasive, evidence-based content gleaned from the body of research produced by BCERP scientists. The goal was to not only educate PHCPs about breast cancer risk factors, but to equip them with communication strategies to share important findings with their patients and caregivers in ways that encourage preventive risk reduction behaviors. To assess the effectiveness of the BCERP CME summative evaluation assessed knowledge, attitude, behavioral intention, and self-reported behavior at baseline and at a 3-week post-test (Atkin & Rice, 2013; Valente & Kwan, 2013). First, an overview of the BCERP is provided, followed by an introduction to CME, and the theoretical foundations that informed the CME training program and evaluation.
The BCERP
Breast cancer risk remains high for women, as one in eight will develop the disease in her lifetime (American Cancer Society, 2019). Advancements in cancer research have made it clear that a substantial amount of breast cancer risk comes from one’s environment and lifestyle behavior, rather than genetic predispositions only (American Cancer Society, 2019; CDC, 2009; President’s Cancer Panel, 2010). The BCERP is an interdisciplinary research team that includes scientists from fields including epidemiology, biology, chemistry, public health, and communication who collaborate with each other and community partners. With long-term support from the National Institute of Environmental Health Sciences (NIEHS) and the National Cancer Institute (NCI), BCERP collaborators have focused on windows of susceptibility, or women’s exposure to environmental agents during sensitive developmental periods across their lifetime affecting their breast cancer risk (BCERP, 2016). The BCERP has worked to better understand exactly when breast cancer windows of susceptibility occur for women, what environmental lifestyle factors affect breast cancer risk independently and in conjunction with windows of susceptibility, and finally, how best to translate these findings into actionable messages for the public (see bcerp.org).
One of the most consequential of these windows is puberty (Biro & Deardorff, 2013; Silk et al., 2019), warranting a focus on parents (i.e., caregivers) to reduce exposures for their children. BCERP social scientists have reported that caregivers tend to feel efficacious about implementing risk reduction recommendations (Neuberger et al., 2011), but are unsure about the cancer-environment link (Silk et al., 2006; Volkman & Silk, 2008). To manage uncertainty around breast cancer information, caregivers report turning to PHCPs with questions about the role of the environment in their children’s health (Silk et al., 2014), suggesting that providers are an important information source for disseminating and translating BCERP findings into actionable information for patients and caregivers. However, getting information on the link between breast cancer and the environment to providers in a way that fosters understanding about subsequent sharing with patients is challenging.
Continuing Medical Education
Despite limited opportunities to formally learn new skills outside of practice, providers are required to maintain a certain number of CME hours to continue practicing. CME programs are intended to facilitate change in clinical settings by keeping providers up-to-date with emerging science and advancements to improve their competence and, ultimately, patient health. CME training provides an opportunity to share information and encourage dissemination of risk-reducing behavior among patient populations while respecting providers’ workloads (Fox & Bennett, 1998; Mansouri & Lockyer, 2007).
CME training is generally self-selected and provides content and formats that best fit with providers’ needs (Rotthoff et al., 2011). Previous research shows CME programs can be effective in changing provider behavior, specifically for improving provider communication skills (Levinson & Roter, 1993; Roter et al., 1998); and, they are most effective when interactive and based on needs assessment (Davis et al., 1999; Towle, 1998; Zabar et al., 2010). Given this potential, CME training offers a translational opportunity for BCERP to put information into the hands of health care providers who can then impact the behavior and beliefs of patients (Silk et al., 2019).
Theoretical Foundations for CME
Diffusion of Innovation (DoI) theory explains how ideas spread through social systems (Rogers, 2003). DoI identifies early adopters, or opinion leaders, as individuals who are highly-connected and assumed by others in their network to be knowledgeable and influential, giving them potential to impact others’ behavior and opinions (Boster et al., 2011). Health providers, information gatekeepers who are seen as reliable sources of accurate health information, have the ability to choose topics to discuss with patients and their caregivers within interactions like well-child visits (Hwang, 2020). In regard to breast cancer risk reduction strategies (the innovation of interest), PHCPs have been identified as opinion leaders given their inherent ability to influence caregivers and patients as well as other PCHPs (Ong et al., 1995; Silk et al., 2019; Smith et al., 2009). Thus, PHCPS were prioritized as the key audience for the BCERP CME training.
A wide range of theories are available to inform interventions and campaigns on how to motivate and influence health behavior, and these theories often incorporate constructs such as knowledge, attitudes, and intentions (see Ajzen (1991), Rosenstock (1974), and Fishbein (2000) for examples). Targeting relevant attitudes can influence behavioral intention (Boers et al., 2018), and by designing interventions to target intentions, behavior change may follow (Brandes et al., 2016). Some findings indicate behavior change does not occur without knowledge about the health behavior (Houston et al., 1992), highlighting the importance for increasing knowledge gain to change behavior.
Contextual Knowledge
Knowledge about behavior and the health context is a prerequisite in order to change health-related beliefs and behavior (Anderson, 2018; Bresnahan et al., 2017; Hungerford & Volk, 1990; Smith et al., 2013; Smith et al., 2017). Lack of knowledge is one factor related to patients’ failure to utilize recommended practices and behavior (McKenzie et al., 2019), and recent research has indicated a need for communication training in the medical field in order to increase knowledge and health literacy (Hildenbrand, 2020). Importantly, providers can increase parental knowledge in order to influence children’s attitudes, intentions, and health-related behavior (Lwin et al., 2017).
In the context of the current translation activity, knowledge is conceptualized as understanding various endocrine-disrupting chemicals suspected to influence breast cancer risk, effective strategies to mitigate risk factors, and communication approaches to best convey information to pediatric patients and caregivers. Although it can be expected that PHCPS have some baseline levels of knowledge related to environmental risk factors for breast cancer, formative research with PHCPs identified a knowledge gap: providers desired more information about environmental risk factors for breast cancer and strategies for integrating this information into well-child checks (Silk et al., 2019). Addressing such knowledge gaps, especially in the context of cancer prevention, can be effective in changing behavior (Coughlin et al., 2016). A primary goal of the CME training was to increase knowledge about the breast cancer and environment connection, a necessary antecedent to behavior change.
H1: PHCPs will exhibit knowledge gain after the CME training for a) environmental exposures and breast cancer, and b) communication strategies to convey breast cancer risk information to pediatric patients.
H2: PHCPs will retain net knowledge gain from the immediate post-test to follow-up (at three weeks).
Attitude toward discussing exposures
Targeting attitudes is an effective strategy for influencing behavioral intentions and behavior change (Avery et al., 2013; Boers et al., 2018). Attitudes generally refer to an individuals’ evaluative judgment of some object (O’Keefe, 2016). In health behavior frameworks, attitudes are conceptualized as having an indirect effect on behavior (the attitude object) by influencing motivation (i.e., Ajzen & Fishbein, 2005). In the current context, the attitude of interest is the evaluative judgment about discussing environmental breast cancer risks with pediatric patients and their caregivers. Past research has found that knowledge about breast cancer can influence health beliefs and attitudes (Akhigbe & Omeumu, 2009; Nguefack et al., 2018; Rick et al., 2019), and that the absence of adequate knowledge can result in more negative attitudes toward relevant health behaviors (Early et al., 2011). Further, providers exposed to information about practice behaviors often report more positive evaluations of those behaviors (Bekker et al., 1999; Lurie et al., 1997). Therefore, the current study aimed to present PHCPs with BCERP findings to improve attitudes about communicating that information.
H3: Knowledge will be positively related to attitude toward discussing environmental exposures following CME training.
Behavior and Intention
There has been extensive theorizing on the link between intentions and behavior such that individuals enact new behaviors or change their current behavior if they plan or intend to do so (Fishbein, 2000; Sniehotta et al., 2016). Previous findings have indicated that by targeting intentions, behavior change will result (Brinberg, 1979), and that intentions to perform a health behavior are related to higher likelihoods of performing those behaviors (Bresnahan et al., 2007; Kim & Park, 2012; Schwarzer, 2001, Sontag et al., 2020). In the practice context, providers’ attitudes about topics have been found to influence their care-related behavior (Arron, 2004; Ishibani et al., 2008) and are linked to the behavior of their patients (Meredith et al., 2005). Based on previous theory and findings, it is expected that positive evaluations (attitudes) of discussing environmental exposures should lead to PHCPs’ intention to share BCERP-related information in well-child checks.
H4: Attitudes toward discussing environmental exposures will be positively related to behavioral intention among PHCP participants who engaged in the CME training.
Previous research has shown that behavior is driven, at least in part, by behavioral intentions (Boster et al., 2014; Fishbein & Ajzen, 1975). When it comes to health care providers, findings indicate that behavioral intention plays a key role in influencing behavior, which can affect the provider-patient interaction and the health decision-making of their patients (Godin et al., 2008). However, many studies stop at intention or motivations and do not capture actual behavior (Sniehotta et al., 2005), in which case complete testing on the behavior change process is limited. The current evaluation sought to test the relationship between behavioral intention and behavior by measuring health care providers’ intent to change their behavior in well-child checks and measuring their self-reported behavior in a follow-up three weeks after training.
H5: Behavioral intention will be positively related to actual PHCP dissemination behavior at the three-week follow-up.
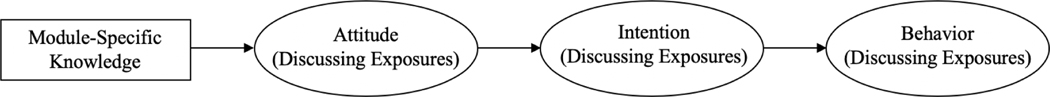
Overall, the CME aimed to influence provider behavior through increasing knowledge on the breast cancer and environment connection and communication strategies to motivate dissemination behavior. It is expected that PHCPs will learn information about BCERP-related environmental exposures, which will increase their attitudes and intentions to share risk reduction information with patients. Related studies have tested theoretical models incorporating the relationship between knowledge, attitudes, and intentions (Fishbein, 2000), along with other concepts like the influence of close others, perceptions of control (Ajzen, 1985), perceptions of severity and susceptibility (Witte, 1992), need for additional information (Kahlor, 2010), and other relevant variables. Given that the goal of the current study is to evaluate the feasibility of a CME training and given that evaluation of CME and their impact on behavior change is sparse and inconsistent, the current study aimed to investigate the behavior change process.
H6: Knowledge predicts dissemination behavior of PHCPs indirectly through attitudes and behavioral intention.
Method
The CME was developed based on formative research with caregivers and PHCPs, increasing the likelihood of effective training content (Mansouri & Lockyer, 2007). Reported elsewhere (Silk et al., 2019), formative research, via focus groups and interviews with caregivers of young patients and with PHCPs, identified knowledge and practice gaps. Despite reporting that they turn to PHCPs for information and answers to questions they have when it comes to healthcare behavior (supporting previous findings, see Silk et al., 2014), caregivers reported little to no knowledge about breast cancer risk factors. Interviews and focus groups with PHCPs indicated low levels of knowledge about breast cancer risk reduction behavior, which provided a basis for developing CME training that could bridge the knowledge and practice gaps. These findings were translated into CME content, developed using funds awarded through the R21 mechanism from NIEHS and NCI (see Silk et al., 2019), to fit identified needs and preferences.
Participants
PHCPs were recruited to participate in the CME training. Snowball sampling was used to recruit pediatricians (N = 50) and pediatric nurses or nurse practitioners (N = 50). Participants were recruited via advertisements from state chapters of the American Academy of Pediatrics and the National Association of Pediatric Nurse Practitioners, as well as a variety of children’s hospitals, children’s health centers, local pediatric offices, and pediatric departments of hospitals or medical schools (see Appendix A for details). Recruitment text explained the purpose of the study and that participants would receive two $75 Amazon gift cards for completing a one-hour training and a second survey, three weeks later.
Of the 100 participants, 92 completed the follow-up and were included in analyses. The mean participant age was 35.13 (SD = 11.27) years, with a majority of females (79.3%). PHCP participants identified mostly as Caucasian (69.5%), followed by Asian/Pacific Islander (12%), and African American (8.7%). A slight majority of the final respondents identified as nurse/nurse practitioner (51.1%). While participants were randomly and equally distributed into groups at the initial data collection, Module Two had slightly more participants (n = 49) at final data collection compared to Module Two (n = 43).
Procedure
All procedures received ethical approved by the Institutional Review Board (IRB) at XXX. After informed consent, participants completed a pre-test to assess baseline beliefs, knowledge about environmental exposures, and attitudes toward environmental and breast cancer risk. After they completed one of two randomly assigned modules that included a series of professionally produced videos, graphics, and powerpoint slides with voiceover (Module One – focus on endocrine disrupting chemicals and windows of susceptibility; Module Two – focus on communication strategies) of the CME training, participants responded to questions regarding their beliefs and knowledge about environmental exposures covered in the training, as well as attitudes and intentions related to sharing the information with patients during well-child checks. Approximately three weeks later, PHCPs (N = 92) reported knowledge, attitudes, and the extent that they integrated material from training into their practice and in conversations with other PHCPs.
Measures
Unless otherwise noted, all items used 5-point Likert-type scales (1 = strongly disagree, 5 = strongly agree). Knowledge items were module-specific, and they, along with attitude items, were consistent across time points. Behavioral intention was only measured after completing the training, whereas behavior was measured only at the three-week follow-up.
Knowledge
Both sets of knowledge items included true/false, yes/no, and multiple-choice questions. Knowledge assessments of this type have been applied successfully in previous BCERP research (Hitt et al., 2015; Smith et al., 2013). Knowledge about environmental exposures, covered in Module One, was measured using 16 items regarding the presence of endocrine disrupting chemicals such as BPA and PFOA in everyday products and the role of lifestyle choices in breast cancer risk. Knowledge about communication strategies, covered in Module Two, was measured using 14 items regarding patient-centered communication strategies applied to the breast cancer and environment context. Each item was re-coded for accuracy (1 = correct, 0 = incorrect) and then averaged to create a knowledge index. Items were adapted from previous research that measured knowledge about health behaviors (Smith et al., 2017) (e.g., “A window of susceptibility is a time of possible increased risk to the effects of endocrine disrupting chemicals, which could increase a girl’s risk of developing breast cancer later in life: 1 – true; 2 – false”).
Attitude
Attitude toward discussing environmental exposures with patients (α = 94) was evaluated with four items. Attitude items measured providers’ perceived importance of addressing environmental exposures with patients. These items were adapted from previous research measuring attitudes related to behavior change (Ajzen & Fishbein, 2005) (e.g., “early environmental exposures is an important topic for me to address as a health care provider.”).
Behavioral Intention
Provider intentions were assessed by measuring participants’ motivations to enact dissemination behavior and incorporate BCERP findings into their practice. Behavioral intention (α = .95) was measured with three items regarding providers’ plans to integrate information from the training into well-child checks and discussions with patients, caregivers, and with other providers. These items were adapted from previous research (Fishbein & Ajzen, 2005; Sniehotta et al., 2016) (e.g., “I intend to integrate breast cancer risk reduction strategies into interactions with my patients and caregivers.”).
Behavior
Self-reported behavior was measured at the three-week follow-up. Behavior (α = .95) was assessed with three items regarding providers’ actual integration of information from the training into well-child checks and discussions with patients, caregivers, and other providers in the three weeks since completing the CME. Items were adapted from previous research that measured actual behavior in the context of behavior change (Sniehotta et al., 2016) (e.g., “I have discussed the role of early environmental exposures as potential risk factors for breast cancer with my patients and caregivers.”).
Open-ended items
Three open-ended items were used to collect feedback about using CME for translational science in this context. Open-ended items asked about lessons learned, barriers to implementation of training, and general feedback about the training (e.g., format, content, issues).
Results
All reliability analyses, correlations, and descriptive statistics were computed using SPSS software (IBM, 2013). Confirmatory factor analysis and path modeling were computed using Mplus version 7 (Muthén & Muthén, 2012). Given that the proposed model was saturated and fit indices could not be reported, beta coefficients are reported to test the effect of knowledge, attitude, and intentions after the CME training on behavior reported at the three-week follow-up. Analyses were conducted using 1,000 percentile bootstrapping techniques to test the direct and indirect effects of each variable on behavior.
Confirmatory Factor Analysis
Confirmatory factor analysis assessed internal consistency and parallelism (Hunter, 1982) for the items used to measure each variable in the model. The measurement model with three factors (attitude, intention, and behavior) was statistically significant and fit the data well (χ2(32) = 68.86, p < .05, CFI = .96, RMSEA = .11 95% CI [.08, .15], SRMR = .045).
Hypothesis Testing
The first two hypotheses concern change in knowledge. Knowledge was assessed before, immediately after, and three weeks after completing the CME. For Module one, pre-test knowledge ranged from .38 to .88 (M = .7, SD = .11); knowledge immediately after training ranged from .5 to .88 (M = .74, SD = .08); and knowledge at the three-week follow-up ranged from .56 to .88 (M = .75, SD = .08). Participants in Module one scored higher in knowledge about environmental exposures and breast cancer in the immediate post-test and at the follow-up, indicating support for H1(a). For Module two, pre-test knowledge ranged from .0 to 1 (M = .78., SD = .4); knowledge immediately after training ranged from .0 to 1 (M = .87, SD = .44); and knowledge at the three-week follow-up ranged from .0 to 1 (M = .86, SD = .44). Participants in Module two scored higher in knowledge about communication strategies to convey breast cancer risk information to pediatric patients in the immediate post-test and at the follow-up, indicating support for H1(b). Additionally, PHCPs retained the knowledge gain from the immediate post-test (Module One: M =.74, SD = .08; Module Two: M = .87, SD = .44) to the three-week follow-up (Module One: M = .75, SD = .08; Module Two: M = .86, SD = .44), indicating support for H2.
H3 predicted that knowledge would be positively associated with attitudes toward discussing environmental exposures. To test the relationship between knowledge and attitude, Pearson Product-Moment correlations were computed. There was no relationship between knowledge and attitudes for PHCPs in Module One (r(47) = −.08, p = .58), however there was a positive, statistically significant, association between knowledge and attitudes for PHCPs in Module Two (r(48) = .44, p < .05), indicating partial support for H3.
H4 predicted that attitudes toward discussing environmental exposures would be positively related to behavioral intention among PHCP participants. Data show support for H4, in that there were positive, statistically significant relationships between attitudes and behavioral intention for PHCPs in Module One (r(39) = .38, p < .05) and in Module Two (r(48) = .43, p < .01).
H5 predicted that behavioral intention would be positively related to behavior. The data indicate support for H5 in that behavioral intention was positively related to behavior for PHCPs in Module One (r(46) = .7, p < .01) and in Module 2 (r(46) = .51, p < .01).
Finally, H6 predicted that module-specific knowledge would determine dissemination behavior of PHCPs, indirectly through attitudes and behavioral intention. H6 was tested separately for each module using path analysis and data indicate limited support for the proposed model (see Table 3). In Module One, the path between intention and behavior was statistically significant (β = .54, SE = .13, p < .01) 95% CI [0.24, 0.76]), however the paths from knowledge to attitude (β = −.77, SE = 1.23, p = .53) [−3.29, 1.54]) and from attitude to intention (β = 0.32, SE = .26, p = .22) 95% CI [−.10, 0.87]) were not statistically significant. For Module Two, the path from attitude to intention (β = .45, SE = .21, p < .05) 95% CI [0.02, 0.86]) and the path from intention to behavior (β = .52, SE = .21, p < .05.) 95% CI[0.21, 0.91]) were statistically significant, but the path from knowledge to attitudes was not significant ((β = 3.51, SE = 2.33, p = .13) 95% CI [−1.35, 6.58]). No significant indirect effects were found in either module.
Qualitative Analysis
Open-ended items were analyzed qualitatively via thematic analysis procedures adapted from recent research (Merrill et al., 2020) to understand common concepts and themes about participants’ evaluations of the CME. Participants indicated they were likely to “discuss environmental exposures” (n = 42, 46%), and reported that the concept of “windows of susceptibility” (n = 16, 17%) was memorable. The most common barrier reported was “time” (n = 34, 37%). Participants also indicated that they “enjoyed” the training (n = 10, 10.9%), found it “helpful” (n =10, 10.9%) and “very informative” (n = 7, 7.6%) and thought it was “easy to follow” (n = 6, 6.5%).
Participants reported increased knowledge and expressed this in open-ended items. For example, one MD participant noted, “I learned about windows of susceptibility, how to effectively communicate with patients and caregivers, and how to incorporate this info into my care of patients.” Additionally, one nurse practitioner mentioned, “I learned the importance of education to patient about risk factors for developing breast cancer.” Participants also indicated positive attitudes though the open-ended items, such as one MD who noted, “I believe avoidance of exposures can have a major positive impact on the future quality of life for my patients.” These attitudes were linked to behavioral intentions, as demonstrated by one pediatric nurse practitioner who said, “I plan to discuss this topic and what I learned with other providers as well as discuss environmental exposures with my patients and their families.” Finally, PHCP participants indicated their intent to use specific patient-centered communication strategies from the CME; for example, one MD wrote, “I will use more open-ended questions with families,” and another MD who wrote, “ I will use this information more effectively with my younger patients and families to help prevent additional long term consequences from poor lifestyle choices.”
Discussion
The current paper evaluated the feasibility of using CME to disseminate emerging science on the breast cancer and environment connection. Formative evaluation with caregivers and PHCPs identified knowledge and practice gaps – caregivers and providers both reported little to no knowledge about environmental and lifestyle risk factors for breast cancer. The developed CME training program aimed to increase PHCP knowledge, attitudes, and behavioral intention in order to ultimately change behavior within well-child checks. The findings indicate that the CME was effective in changing PHCP behavior; in both modules, PHCPs reported adopting recommended communication strategies to share breast cancer risk information with their patients and caregivers during visits. Results highlight the relationship between behavioral intention and behavior, supporting previous literature on behavior change theory (Avery et al., 2013; Boers et al., 2018; Brandes et al., 2016; Fishbein, 2000; Sontag et al., 2020). These findings have implications for CME design and for the evaluation of training programs in changing behavior for healthcare providers.
Implications for CME design
With a theoretical background in DoI theory (Boster et al. 2011; Rogers, 2003), PCHPs were targeted as opinion leaders for caregivers of young patients. Formative evaluation (via focus groups and interviews with PHCPs and with caregivers) was used to inform the CME design, and effectiveness was evaluated with summative evaluation (Atkin & Rice, 2013; Valente & Kwan, 2013) by collecting data at baseline, immediately after completing the training, and at a three-week follow-up.
Changes from baseline to follow-up, three weeks after participation in the CME, demonstrated that the CME was effective in increasing the relevant provider knowledge, attitudes, and behavioral intention, and that providers implemented the behavior in their well-child checks in between the CME and the follow-up. Quantitative and qualitative analyses offer evidence for the utility of using CME for translational science – to move scientific findings from the academic community to medical communities so that it can be communicated to the lay public. Participants across two modules of training content demonstrated knowledge gain from pre-test to immediate post-test, and the knowledge was retained, as the average knowledge scores at the three-week follow-up were higher than baseline scores. In addition to quantitative evidence of effectiveness, qualitative data also indicated that participants enjoyed the format, were likely to discuss environmental exposures in well-child checks, and recalled the key concept of interest, windows of susceptibility.
Implications for CME and Behavior Change
Another goal of the current CME evaluation was to investigate the relationship between knowledge, attitudes, behavioral intention, and behavior in the context of changing strategies PHCPs use to share risk reduction information. Knowledge, attitude, and behavioral intention have been studied extensively in the context of changing health behaviors (see Fishbein, 2000; Houston et al., 1992; Sniehotta et al. 2016), but few studies follow-up by measuring implemented behavior, identified by researchers as the “intention-behavior gap” (Sniehotta et al., 2005). In previous behavior change research, effects in knowledge show only small effects on attitudes, even smaller changes in behavioral intention, and the least change seen in actual behavior (Ajzen, 2015). By assessing knowledge, attitudes, and behavioral intention before and immediately after the CME, and comparing these variables with actual reported behavior from participants three weeks after training, the current study analyzed the relationship through the entire decision-making process as is suggested for summative evaluation (Atkin & Rice, 2013; Valente & Kwan, 2013). Findings indicated a strong, significant, and positive relationship between behavioral intention and behavior across both modules. This finding is important for behavior change research, as it supports previous findings about the importance of targeting intentions to change behavior (Brandes et al., 2016; Fishbein, 2000; Sniehotta et al., 2016), which might be the strongest predictor of behavior (Avery et al., 2013; Brandes et al., 2016).
Knowledge gain was achieved in both modules and it was retained three weeks later, which is evidence for CME in addressing knowledge gaps in the context of changing health behavior (Coughlin et al., 2016). As one of the goals of the BCERP was to disseminate novel information to different audiences, this evaluation shows that the CME modules helped BCERP to reach that goal with PHCPs. Knowledge was associated with attitudes for participants in the CME module specific to communication strategies, but there was not a significant relationship between knowledge and attitude for the module specific to environmental exposures. Attitudes were related to intention to engage in conversations about BCERP material across both modules, supporting previous literature demonstrating that targeting attitudes is an effective strategy for influencing behavioral intentions and behavior change (Avery et al. 2013; Boers et al., 2018).
The findings of the current study have implications for using CME to enhance health care provider education and care, especially for pediatricians. Previous research has attempted to identify best strategies for training pediatric health care providers to incorporate emerging research findings into current practices (Burns et al., 2016; Gittelman et al., 2015; Hardy et al., 2019; Jones et al., 2009; Kainth et al., 2018). Results of the current study demonstrate the effectiveness of using CME to increase topic-specific knowledge, attitudes, behavioral intentions, and practice behavior, which highlight the utility of CME training for providers (Rotthoff et al., 2011; Silk et al., 2019) and specifically for pediatricians (Boese-O’Reilly, 2007; Finnegan et al., 2020; Nelson, 2019). By conducting a targeted needs-assessment with relevant samples (Blair, 2014; Nelson, 2019), in this case, with caregivers of pediatric patients and with pediatric health care providers, an interactive, online CME program was effective in achieving knowledge, attitude, and behavioral change. This model of using CME for translational science (see Silk et al., 2019) can be applied to other topics in provider and pediatric education and training to create needs-based programs to address gaps in provider practices (Finnegan et al., 2020; Fox & Bennett, 1998; Mansouri & Lockyer, 2007; Nelson, 2019).
Limitations and Future Directions
There are some limitations of the current study. The major limitation is the small sample size, which resulted in the study being underpowered for the statistical test of the overall path model. Limited resources to compensate respondents, as well as the hard-to-reach nature of the PHCP participants contributed to a low sample size, however it is important to note that despite the small sample, significant results were detected. Additionally, only two of three BCERP modules were evaluated due to lack of resources. Future research should strive to assess all content and to follow-up beyond three weeks to determine long-term adoption of training recommendations. Understanding that effects in behavior change typically diminish over time (Eyberg et al., 2006), booster information should be included in subsequent follow-up material shared with PHCPs so that the content remains salient and accessible. With these limitations taken into account, future research can solidify the link between knowledge and attitude, attitude and behavioral intention, and between behavior implemented into practice.
Conclusions
This feasibility study evaluated a CME training program to change PHCP behavior during well-child visits with patients. Specifically, based in DoI theory and the concepts of knowledge, attitudes, and behavioral intention, the CME training targeted PHCP behaviors related to discussing breast cancer risk information with patients and caregivers. The current CME training program effectively changed module-specific and general breast cancer risk knowledge, attitudes relevant to discussing breast cancer preventive recommendations with patients and caregivers, intentions to change behavior to implement recommended communication strategies, and self-reported behavior relevant to sharing breast cancer risk information after participating in the CME.
Figure 1.
Proposed model for participants in both CME modules.
Table 1.
Correlations and means (with standard deviation) between attitude toward discussing environmental exposures and intention to discuss risk reduction with patients (both post-test measures recorded immediately after training) and self-reported behavior for both Module One and Two combined (reported in follow-up three weeks after training).
| M (SD) | 1. | 2. | 3. | |
|---|---|---|---|---|
| 1. Attitude (Discuss Exposures) | 4.44 (.78) | |||
| 2. Intention | 4.27 (.64) | .41* | ||
| 3. Behavior | 3.66 (.72) | .28* | .39* |
Table 2A.
Correlations and means (with standard deviation) between knowledge of exposures (immediate post-test), attitude toward discussing environmental exposures (immediate post-test), intention to discuss risk reduction with patients (immediate post-test), and self-reported behavior (three-week follow-up) for Module One participants.
| M (SD) | 1. | 2. | 3. | 4. | |
|---|---|---|---|---|---|
| 1. Knowledge (Exposures) | .74(.09) | ||||
| 2. Attitude (Discuss Exposures) | 4.40 (.84) | −.08 | |||
| 3. Intention | 4.10 (.70) | .10 | .38* | ||
| 4. Behavior | 4.42 (.59) | .01 | .42* | .70* |
Table 2B.
Correlations and means (with standard deviation) between knowledge of communication skills (immediate post-test), attitude toward discussing environmental exposures (immediate post-test), intention to discuss risk reduction with patients (immediate post-test), and self-reported behavior (three-week follow-up) for Module Two participants.
| M (SD) | 1. | 2. | 3. | 4. | |
|---|---|---|---|---|---|
| 1. Knowledge (Communication Skills) | .87 (.09) | ||||
| 2. Attitude (Discuss Exposures) | 4.48 (.73) | .44* | |||
| 3. Intention | 4.42 (.55) | −.11 | .43* | ||
| 4. Behavior | 3.66 (.72) | −.17 | .29* | .51* |
Appendix A
Recruitment Strategy
Participants were recruited by requesting participants and/or study advertisements from National Association of Pediatric Nurse Practitioners (NAPNAP) and American Academy of Pediatrics (AAP) chapters in Michigan, Ohio, and Illinois were contacted, as well as the Minnesota NAPNAP chapter. Additional recruitment was requested from the Children’s Hospitals of Alabama, Chicago (Lurie), Wisconsin, Minnesota, Michigan (Detroit Medical Center), University of Michigan C.S. Mott (Ann Arbor), and the University of Illinois, and the Department of Pediatrics at the University of Alabama (Birmingham), the University of Illinois, the University of Minnesota, the University of Wisconsin, the Medical College of Wisconsin, Wayne State University, and Michigan State University. Local contact was also made with the Michigan Medical Society (a partner in the development of this study’s CME), the Michigan State University Health Team, and a number of local pediatric offices and medical centers. Lastly, recruitment messages were also sent out in newsletters to members of the Michigan Chapter of NAPNAP, the Michigan Chapter of the AAP, and the Michigan State Medical Society with links to the survey.
Footnotes
Declaration of Interest: None
References
- Aarons GA (2004). Mental health provider attitudes toward adoption of evidence-based practice: The Evidence-Based Practice Attitude Scale (EBPAS). Mental Health Services Research, 6, 61–74. 10.1023/b:mhsr.0000024351.12294.65 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ajzen I. (1985). From intentions to actions: A theory of planned behavior. In Action control (pp. 11–39). Springer, Berlin, Heidelberg. 10.1007/978-3-642-69746-3_2 [DOI] [Google Scholar]
- Ajzen I. (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50, 179–211. 10.1016/0749-5978(91)90020-t [DOI] [Google Scholar]
- Ajzen I. (2015). The theory of planned behavior is alive and well, and not ready to retire: A commentary on Sniehotta, Presseau, and Araujo-Soares. Health Psychology Review, 9, 131–137. 10.1080/17437199.2014.883474 [DOI] [PubMed] [Google Scholar]
- Ajzen I, & Fishbein M. (2005). The influence of attitudes on behavior. In Albaracín D, Johnson BT, & Zanna MP (Eds.), The handbook of attitudes (pp. 173–221). Erlbaum. [Google Scholar]
- Albarracín D, Johnson BT, Zanna MP, & Kumkale GT (2005). Attitudes: Introduction and scope. In Albarracín D, Johnson BT, & Zanna MP (Eds.), The handbook of attitudes (pp. 3–19). Erlbaum. [Google Scholar]
- Akhigbe AO & Omuemu VO (2009). Knowledge, attitudes and practice of breast cancer screening among female health workers in a Nigerian urban city. BMC Cancer, 9, 10.1186/1471-2407-9-203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Cancer Society (2019). How Common Is Breast Cancer? https://www.cancer.org/cancer/breast-cancer/about/how-common-is-breast-cancer.html
- Anderson A. (2018). Online health information and public knowledge, attitudes, and behaviours regarding antibiotics in the UK: Multiple regression analysis of Wellcome Monitor and Eurobarometer Data. PLoS ONE, 13, e0204878. 10.1371/journal.pone.0204878 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkin CK, & Rice RE (2013). Theory and principles of public communication campaigns. In Rice RE & Atkin C. (Eds.), Public communication campaigns (4th ed., pp. 3–19). SAGE Publications. 10.4135/9781544308449.n1 [DOI] [Google Scholar]
- Avery KNL, Donovan JL, Horwood J, & Lane JA (2013). Behavior theory for dietary interventions for cancer prevention: A systematic review of utilization and effectiveness in creating behavior change. Cancer Causes Control, 24. 409–420. 10.1007/s10552-012-9995-9 [DOI] [PubMed] [Google Scholar]
- Bekker H, Morrison L, & Marteau TM (1999). Breast screening: GPs’ beliefs, attitudes and practices. Family Practice, 16, 60–65. 10.1093/fampra/16.1.60 [DOI] [PubMed] [Google Scholar]
- Biro FM, & Deardorff J. (2013). Identifying opportunities for cancer prevention during preadolescence and adolescence: Puberty as a window of susceptibility. Journal of Adolescent Health, 52, S15–S20. 10.1016/j.adohealth.2012.09.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blair M. (2014). Getting evidence into practice – implementation science for pediatricians. Archives of Disease in Childhood, 99, 307–309. 10.1136/archdischild-2012-303464 [DOI] [PubMed] [Google Scholar]
- Boers E, Zebregs S, Hendriks H, & Van Den Putte B, (2018). Is it more feeling or thinking? The influence of affective and cognitive attitude on adolescents’ intention to engage in binge drinking. Journal of Health Communication, 5, 430–434. 10.1080/10810730.2018/1461960 [DOI] [PubMed] [Google Scholar]
- Boese-O’Reilly S. (2007). Continuous medical education (CME): Do we need CME for pediatric environmental medicine in Europe? International Journal of Hygiene and Environmental Health, 531–534. 10.1016/j.ijheh.2007.07.009 [DOI] [PubMed]
- Boster FJ, Kotowski MR, Andrews KR, & Serota K. (2011). Identifying influence: Development and validation of the connectivity, persuasiveness, and maven scales. Journal of Communication, 61, 178–196. 10.1111/jcom.2011.61.issue-1 [DOI] [Google Scholar]
- Boster FJ, Shaw AZ, Carpenter CJ, & Massi Lindsey LL (2014). Simulation of a dynamic theory of reasoned action. Simulation & Gaming, 45, 699–731. 10.1177/1046878114562930 [DOI] [Google Scholar]
- Brandes K, Linn AJ, Smit EG, & van Weert JCM (2016). Unraveling the determinants of cancer patients’ intention to express concerns. Journal of Health Communication, 21, 327–336. 10.1080/10810730.2015.1080325 [DOI] [PubMed] [Google Scholar]
- <au>Breast Cancer and the Environment Research Program (2016). Background information for health professionals [Pamphlet]. https://bcerp.org/wp-content/uploads/2016/11/1_BCERP_Bkgrnd_HealthProfessionals_508-FNLv2.pdf
- Bresnahan M, Lee SY, Smith SW, Shearman S, Nebashi R, Park CY, & Yoo J. (2007). A theory of planned behavior study of college students’ intentions to register as organ donors in Japan, Korea, and the United States. Health Communication, 21, 201–211. 10.1080/10410230701307436 [DOI] [PubMed] [Google Scholar]
- Brinberg D. (1979). An examination of the determinants of intention an behavior: A comparison of two models Journal of Applied Social Psychology, 9, 560–575. 10.1111/j.1559-1816.1979.tb00816.x [DOI] [Google Scholar]
- Burns AM, Kushner JA, Ward MA, Turner TL, Kline MW, & Orange JS (2016). Developing a comprehensive approach to training pediatrician-scientists at Texas Children’s Hospital and Baylor College of Medicine: The pediatrician-scientist training and development program. Academic Pediatrics, 16, e38–e39. 10.1016/j.acap.2016.05.094 [DOI] [PubMed] [Google Scholar]
- Burak L, & Boone B. (2008). College women and breast cancer: knowledge, behavior, and beliefs regarding risk reduction. American Journal of Health Education, 39, 206–212. 10.1080/19325037.2008.10599040 [DOI] [Google Scholar]
- Centers for Disease Control and Prevention [CDC] (2009). Polybrominated Diphenyl Ethers and 2,2’,4,4’,5,5’-Hexabromobiphenyl (BB-153). Fourth National Report on Human Exposure to Environmental Chemicals (pp. 311–320). Atlanta, GA: Centers for Disease Control and Prevention; National Center for Environmental Health. [Google Scholar]
- Coughlin CC, Perez M, Kumar MG, Jeffe DB, Bayliss SJ, & Sternhell-Blackwell K. (2016). Skin cancer risk education in pediatric solid organ transplant patients: An evaluation of knowledge, behavior, and perceptions over time. Pediatric Transplantation, 21, e12817. 10.1111/petr.12817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis D, O’Brien MA, Freemantle N, Wolf FM, Mazmanian P, & Taylor-Vaisey A. (1999). Impact of formal continuing medical education: Do conferences, workshops, rounds, and other traditional continuing education activities change physician behavior or health care outcomes? JAMA, 282, 867–874. 10.1001/jama.282.9.867 [DOI] [PubMed] [Google Scholar]
- Dearing JW, & Kreuter MW (2010). Designing for diffusion: How can we increase uptake of cancer communication innovations? Patient Education and Counseling, 815, S100–S110. 10.1016/j.pec.2010.10.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Desteno D, Petty RE, Rucker DD, Wegener DT, & Braverman J. (2004). Discrete emotions and persuasion: The role of emotion-induced expectancies. Journal of Personality and Social Psychology, 86, 43–56. 10.1037/0022-3514.86.1.43 [DOI] [PubMed] [Google Scholar]
- Eagly AH, & Chaiken S. (1993). The psychology of attitudes. Harcourt Brace Jovanovich College Publishers. 10.1002/mar.4220120509 [DOI]
- Early J, Armstrong SN, Burke S, & Thompson DL (2011). US female college students’ breast health knowledge, attitudes, and determinants of screening practices: new implications for health education. Journal of American College Health, 59, 640–647. 10.1080/07448481.2010.528098 [DOI] [PubMed] [Google Scholar]
- Eyberg SM, Edwards D, Boggs SR, & Foote R. (2006). Maintaining the treatment effects of parent training: The role of booster sessions and other maintenance strategies. Clinical Psychology Science and Practice, 5, 544–554. 10.1111/j.1468-2850.1998.tb00173.x [DOI] [Google Scholar]
- Finnegan T, Murray CF, Hughes S, & Maski K. (2020). Online CME-certified case challenges improve competence for the diagnosis and management of pediatric narcolepsy among pediatricians. Sleep, 43, A445. 10.1093/sleep/zsaa056.1159 [DOI] [Google Scholar]
- Fishbein M. (2000). The role of theory in HIV prevention. AIDS Care, 12, 273–278. 10.1080/09540120050042918 [DOI] [PubMed] [Google Scholar]
- Fishbein M, & Ajzen I. (1975). Belief, attitude, intention, and behavior. Addison-Wesley.
- Fishbein M, & Ajzen I. (2010). Predicting and changing behavior: The reasoned action approach. Psychology Press, Taylor & Francis Group. [Google Scholar]
- Forman MR, Winn DM, Collman GW, Rizzo J, & Birnbaum LS (2015). Environmental exposures, breast development and cancer risk: through the looking glass of breast cancer prevention. Reproductive Toxicology, 54, 6–10. 10.1016/j.reprotox.2014.10.019 [DOI] [PubMed] [Google Scholar]
- Fox RD, & Bennett NL (1998). Continuing medical education: learning and change: implications for continuing medical education. BMJ, 316, 466. 10.1136/bmj.316.7129.466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghaffari M, Mohammadi S, Rakhshanderou S. (2018). Effect of an intervention on the breast cancer screening behavior in women: Application of integrated behavioral model. International Journal of Preventive Medicine, 9, 99. 10.4103/ijpvm.IJPVM_147_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gittelman MA, Denny S, Anzeljc S, FitzGerald M, & Arnold MW (2015). A pilot quality improvement program to increase pediatrician injury anticipatory guidance. Journal of Trauma and Acute Care Surgery, 79, S9–S14. 10.1097/TA.0000000000000672 [DOI] [PubMed] [Google Scholar]
- Godin G, Belanger-Gravel A, Eccles M, & Grimshaw J. (2008). Healthcare professionals’ intentions and behaviours: A systematic review of studies based on social cognitive theories. Implementation Science, 3. 10.1186/1748-5908-3-36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Godin G,. Gagne C, Maziade J, Moreault L, Beaulieu D, & Morel S. (2001). Breast cancer: The intention to have a mammography and a clinical breast examination – application of the theory of planned behavior. Psychology and Health, 16, 423–441. 10.1080/08870440108405517 [DOI] [Google Scholar]
- Hardy A, Fuller DG, Forrester M, Anderson KP, Cooper C, Jenner B, Marshall I, Sanderson C, Standish J, Worth J, Vuillermin P, & McCloskey K (2019). Survey of procedural and resuscitation requirements for pediatricians working in a non-tertiary center: Implications for training. Journal of Paediatrics and Child Health, 55, 441–445. 10.1111/jpc.14224 [DOI] [PubMed] [Google Scholar]
- Hildenbrand GM, Perrault EK, Keller PE (2020). Evaluating a health literacy communication training for medical students: Using plain language. Journal of Health Communication. 10.1080/10810730.2020.1827098 [DOI] [PubMed]
- Hitt R, Perrault E, Smith S, Keating D, Nazione S, Silk K, & Russell J. (2015). Scientific message translation and the Heuristic Systematic Model: Insights for designing educational messages about progesterone and breast cancer risks. Journal of Cancer Education. 10.1007/s13187-015-0835-y [DOI] [PMC free article] [PubMed]
- Houston TP, Fischer PM & Richards JW (1992). The public, the press, and tobacco research. Tobacco Control, 1, 118–122. 10.1136/tc.1.2.118 [DOI] [Google Scholar]
- Hungerford HR, & Volk TL (1990). Changing learner behavior through environmental education. The Journal of Environmental Education, 21, 8–21. 10.1080/00958964.1990.10753743 [DOI] [Google Scholar]
- Hwang J. (2020). Health information sources and the influence vaccination: The mediating role of perceived vaccine efficacy and safety. Journal of Health Communication. 10.1080/10810730.2020.1840675 [DOI] [PubMed]
- IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. IBM Corp. [Google Scholar]
- Ishibashi KL, Koopmans J, Curlin FA, Alexander KA, & Ross LF (2008). Paediatricians’ attitudes and practices towards HPV vaccination. Acta Paediatrica, 97, 1550–1556. 10.1111/j.1651-2227.2008.00958.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones MD, McGuinness GA, First LR, & Leslie LK (2009). Linking process to outcome: Are we training pediatricians to meet evolving health care needs? Pediatrics, 123, S1–S7. 10.1542/peds.2008-1578C [DOI] [PubMed] [Google Scholar]
- Kahlor L. (2010). PRISM: A planned risk information seeking model. Health Communication, 25, 345–356. 10.1080/10410231003775172 [DOI] [PubMed] [Google Scholar]
- Kainth R, Soo AKS, Dhaliwal J, Smith B, & Klaber RE (2018). Understanding and improving the experience of pediatricians in training. Archives of Disease in Childhood, 103, 521–522. 10.1136/archdischild-2017-313180 [DOI] [PubMed] [Google Scholar]
- Kim J, & Park HA (2012). Development of a health information technology acceptance model using consumers’ health behavior intention. Journal of Medical Internet Research, 14, e133. 10.2196/jmir.2143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kratzke C, Vilchis H, & Amatya A. (2013). Breast cancer prevention knowledge, attitudes, and behaviors among college women and mother–daughter communication. Journal of Community Health, 38, 560–568. 10.1007/s10900-013-9651-7 [DOI] [PubMed] [Google Scholar]
- Kumar G, Ni A, Lawrence S, & Doja A. (2012). Incorporating CanMEDS and subspecialty training into pediatric residency programs: Why are we still deficient? Pediatrics & Child Health, 17, e7–e11. 10.1093/pch/17.1.e7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinson W, & Roter D. (1993). The effects of two continuing medical education programs on communication skills of practicing primary care physicians. Journal of General Internal Medicine, 8, 318–324. 10.1007/bf02600146 [DOI] [PubMed] [Google Scholar]
- Lurie N, Margolis KL, McGovern PG, Mink PJ, & Slater JS (1997). Why do patients of female physicians have higher rates of breast and cervical cancer screening? Journal of General Internal Medicine, 12, 34–43. 10.1046/j.1525-1497.1997.12102.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lwin MO, Shin W, Yee AZH, & Ward RJ (2017). A parental health education model of children’s food consumption: Influence on children’s attitudes, intention, and consumption of healthy and unhealthy foods. Journal of Health Communication, 22, 403–412. 10.1080/10810730.2017.1302523 [DOI] [PubMed] [Google Scholar]
- Madden TJ, Ellen PS, & Ajzen I. (1992). A comparison of the theory of planned behavior and the theory of reasoned action. Personality and Psychology Bulletin, 18, 3–9. 10.1177/0146167292181001 [DOI] [Google Scholar]
- Mansouri M, & Lockyer J. (2007). A meta-analysis of continuing medical education effectiveness. The Journal of Continuing Education in the Health Professions, 27, 6–15. 10.1002/chp.88 [DOI] [PubMed] [Google Scholar]
- McKenzie LB, Roberts KJ, Collins CL, Clark RM, Clegg Smith K, & Manganello J. (2019). Maternal knowledge, attitudes, and behavioral intention after exposure to injury prevention recommendation news media. Journal of Health Communication, 24, 625–632. 10.1080/10810730.2019.1646357 [DOI] [PubMed] [Google Scholar]
- Meredith LS, Yano EM, Hickey SC, & Sherman SE (2005). Primary care provider attitudes are associated with smoking cessation counseling and referral. Medical Care, 43, 929–934. 10.1097/01.mlr.0000173566.01877.ac [DOI] [PubMed] [Google Scholar]
- Merrill JE, Ward RM, & Riordan BC (2020). Posting post-blackout: A qualitative examination of the positive and negative valence of tweets posted after “blackout” drinking. Journal of Health Communication, 25, 150–158. 10.1080/10810730.2020.1719242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, & Muthén BO (2012). Mplus User’s Guide (7th ed.). Muthén & Muthén. [Google Scholar]
- Nguefack CT, N’djeudjui C, Engbang JPN, Nana TN, Ekane GH, & Tebeu PM (2018). Knowledge, attitude, and practice on breast cancer among health professionals in Douala references hospitals, Cameroon. Journal of Cancer Education, 33, 457–462. 10.1007/s13187-016-1158-3 [DOI] [PubMed] [Google Scholar]
- Nelson BA (2019) Creating effective and efficient pediatric-specific CME content: More than just checking a box. Journal of Continuing Education in the Health Professions, 39, 64–68. 10.1097/CEH.0000000000000237 [DOI] [PubMed] [Google Scholar]
- Neuberger L, Silk KJ, Yun D, Bowman ND, & Anderson J. (2011). Concern as motivation for protection: Identifying mothers’ concerns about their daughters’ breast cancer risk. Journal of Health Communication, 16, 1055–1071. 10.1080/10810730.2011.571339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Keefe D, (2016). Persuasion: Theory And Research (3rd ed.). Sage. [Google Scholar]
- Ong LML, de Haes JCJM, Hoos AM, & Lammes FB (1995). Doctor-patient communication: A review of the literature. Social Science & Medicine, 40, 903–918. 10.1016/0277-9536(94)00155-M [DOI] [PubMed] [Google Scholar]
- Pak-Gorstein S, Batra M, Johnston B, Grow HM, Grant A, Shugerman R, Lago S, Stapleton FB, & McPhillips H. (2018). Training pediatricians to address health disparities: An innovative residency track combining global health with community pediatrics and advocacy. Academic Medicine, 93, 1315–1320. 10.1097/ACM.0000000000002304 [DOI] [PubMed] [Google Scholar]
- President’s Cancer Panel (2010). Reducing environmental risk: What we can do now – 2008–2009 annual report of the President’s Cancer Panel. Retrieved from http://pcp.cancer.gov
- Rick TJ, Deming CM, Helland JR, & Hartwig KA (2019). Cancer training for frontline healthcare providers in Tanzania. Journal of Cancer Education, 34, 111–115. 10.1007/s13187-017-1274-8 [DOI] [PubMed] [Google Scholar]
- Rogers EM (2003). Diffusion of innovations (5th ed.). Free Press. [Google Scholar]
- Rosenstock IM (1974). Historical origins of the health belief model. Health Education & Behavior, 2, 328–335. 10.1177/109019817400200403 [DOI] [Google Scholar]
- Roter D, Rosenbaum J, de Negri B, Renaud D, DiPrete-Brown L, & Hernandez O. (1998). The effects of a continuing medical education programme in interpersonal communication skills on doctor practice and patient satisfaction in Trinidad and Tobago. Medical Education, 32, 181–189. 10.1046/j.1365-2923.1998.00196.x [DOI] [PubMed] [Google Scholar]
- Rotthoff T, Baehring T, David DM, Bartnick C, Linde F, Willers R, ... Scherbaum WA (2011). The value of training in communication skills for continuing medical education. Patient Education and Counseling, 84, 170–175. 10.1016/j.pec.2010.07.034 [DOI] [PubMed] [Google Scholar]
- Sadler GR, Ko CM, Cohn JA, White M, Weldon RN, & Wu P. (2007). Breast cancer knowledge, attitudes, and screening behaviors among African American women: the Black cosmetologists promoting health program. BMC Public Health, 7, 57. 10.1186/1471-2458-7-57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwarzer R. (2001). Social-cognitive factors in changing health-related behaviors. Current Directions in Psychological Science, 10, 47–51. 10.1111/1467-8721.00112 [DOI] [Google Scholar]
- Silk KJ, Bigsby E, Volkman J, Kingsley C, Atkin CK, Ferrara M, & Goins LA (2006). Formative research on adolescent and adult risk perceptions for breast cancer. Social Science and Medicine, 63, 3124–3136. 10.1016/j.socscimed.2006.08.010 [DOI] [PubMed] [Google Scholar]
- Silk KJ, Perrault EK, Neuberger L, Rogers A, Atkin C, Barlow J, & Duncan DM (2014). Translating and testing breast cancer risk reduction messages for mothers of adolescent girls. Journal of Health Communication, 19, 226–243. 10.1080/10810730.2013.811322 [DOI] [PubMed] [Google Scholar]
- Silk KJ, Walling B, Totzkay D, Mulroy M, Smith S, Quaderer T, Boumis J, & Thomas B. (2019). Continuing Medical Education as a Translational Science Opportunity for Health Communication Researchers: The BCERP Model. Health Communication, 35, 1266–1273. 10.1080/10410236.2019.1625003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith SW, Clark-Hitt R, Nazione S, Russell J, Silk K, & Atkin CK (2013). The effects of motivation, ability, and heuristic cues on systematic processing of information about breast cancer environmental factors. Journal of Health Communication, 18, 845–865. 10.1080/10810730.2013.768722 [DOI] [PubMed] [Google Scholar]
- Smith SW, Hitt R, Russell J, Nazione S, Silk K, Atkin CK, & Keating D. (2017). Risk belief and attitude formation from translated scientific messages about PFOA, an environmental risk associated with breast cancer. Health Communication, 32, 279–287. 10.1080/10410236.2016.1138350 [DOI] [PubMed] [Google Scholar]
- Smith SW, Munday S, LaPlante C, Kotowski MR, Atkin CK, Skubisz C, & Stohl C. (2009). Topics and sources of memorable breast cancer messages: Their impact on prevention and detection behaviors. Journal of Health Communication, 14, 293–307. 10.1080/10810730902805903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sniehotta FF, Presseau J, Allan J, & Araujo-Soares V. (2016). “You can’t always get what you want”: A novel research paradigm to explore the relationships between multiple intentions and behaviors. Applied Psychology: Health and Well-Being, 8, 258–275. 10.1111/aphw.12071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sniehotta FF, Scholz U, & Schwarzer R. (2005). Bridging the intention-behaviour gap: Planning, self-efficscy, and action control in the adoption and maintenance of physical exercise. Psychology & Health, 20, 143–160. 10.1080/08870440512331317670 [DOI] [Google Scholar]
- Sontag JM, Delnevo CD, Hegy T, Ostfeld. B. M., & Wackowski, O. A. (2020). Secondhand smoke risk communication: Effects on parent smokers’ perceptions and intentions. Journal of Health Communication, 7, 554–565. 10.1080/10810730.2020.1797947 [DOI] [PubMed] [Google Scholar]
- Towle A. (1998). Continuing medical education: Changes in health care and continuing medical education for the 21st century. BMI, 316, 301–304. 10.1136/bmj.316.7127.301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Valente TW, & Kwan PP (2013). Evaluating communication campaigns. In Rice RE & Atkin C. (Eds.), Public communication campaigns (4th ed., pp. 83–97). SAGE Publications. 10.4135/9781544308449 [DOI] [Google Scholar]
- Volkman J, & Silk KJ (2008). Adolescent females and their mothers: Examining perceptions of the environment and breast cancer. Journal of Health Psychology, 13, 1180–1189. 10.1177/1359105308095972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witte K. (1992). Putting the fear back into fear appeals: The extended parallel process model. Communication Monographs, 59, 329–349. 10.1080/03637759209376276 [DOI] [Google Scholar]
- Yun D, Silk K, Bowman N, Neuberger L, Atkin C. (2009). Mothers’ intentions to teach adolescent daughters about breast cancer risk reduction activities: The influence of self- efficacy, response efficacy, & personal responsibility. Communication Research Reports, 26(2), 134–145. 10.1080/08824090902861606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zabar S, Hanley K, Stevens DL, Ciotoli C, Hsieh A, Griesser C, ... Kalet A. (2010). Can interactive skills-based seminars with standardized patients enhance clinicians’ prevention skills? Measuring the impact of a CME program. Patient Education and Counseling, 80, 248–252. 10.1016/j.pec.2009.11.015 [DOI] [PubMed] [Google Scholar]