Abstract
The progressive decline of bone mass and the deterioration of bone microarchitecture are hallmarks of the bone aging. The resulting increase in bone fragility is the leading cause of bone fractures, a major cause of disability. As the frontline pharmacological treatments for osteoporosis suffer from low patients’ adherence and occasional side effects, the importance of diet regimens for the prevention of excessive bone fragility has been increasingly recognized. Indeed, certain diet components have been already associated to a reduced fracture risk. Organosulfur compounds are a broad class of molecules containing sulfur. Among them, several molecules of potential therapeutic interest are found in edible plants belonging to the Allium and Brassica botanical genera. Polysulfides derived from Alliaceae and isothiocyanates derived from Brassicaceae hold remarkable nutraceutical potential as anti-inflammatory, antioxidants, vasorelaxant and hypolipemic. Some of these effects are linked to the ability to release the gasotrasmitter hydrogen sulfide (H2S). Recent preclinical studies have investigated the effect of organosulfur compounds in bone wasting and metabolic bone diseases, revealing a strong potential to preserve skeletal health by exerting cytoprotection and stimulating the bone forming activity by osteoblasts and attenuating bone resorption by osteoclasts. This review is intended for revising evidence from preclinical and epidemiological studies on the skeletal effects of organosulfur molecules of dietary origin, with emphasis on the direct regulation of bone cells by plant-derived polysulfides, glucosinolates and isothiocyanates. Moreover, we highlight the potential molecular mechanisms underlying the biological role of these compounds and revise the importance of the so-called ‘H2S-system’ on the regulation of bone homeostasis.
Keywords: organosulfur compounds (OSCs), osteoporosis, hydrogen sulfide (H2S), Brassicaceae, Allium, glucosinolates, isothiocyanates, polysulfides
Highlights
A literature search was conducted using MEDLINE database. Relevant pre-clinical and clinical studies were selected using a combination of keywords including bone, diet and/or organosulfur compounds, Allium, Brassicaceae, alliin, allicin, garlic, ajoene, diallyl trisulfide, diallyl disulfide, S-allylcysteine, diallyl sulfide, glucosinolate, thiosulfinate, sulforaphane, broccoli, methyl sulfide, isothiocyanates. Additional studies were identified by an extensive manual search of bibliographic references in original papers and reviews. Abstracts and non-English papers were not included. This study selected a total of in vitro studies (10 Alliaceae, 9 Brassicaceae); in vivo studies (17 Alliaceae, 11 Brassicaceae) and population-based studies (4 Alliaceae, 1 Brassicaceae).
Introduction
Osteoporosis (OP) is a chronic metabolic bone disease characterized by the deterioration of bone microarchitecture and a reduction in bone mass, leading to decreased bone strength and increased risk of bone fracture (1). Approximately 6 % of men and 21 % of women aged 50–84 years are diagnosed with OP and the number of fragility fractures in Europe has increased from 3.1 to nearly 4.3 million in 20 years since year 2000 (2); due to the strong correlation with the ageing of the population, the prevalence of OP is projected to further increase over the next decades (3).
At the bone tissue level, OP is characterized by increased bone porosity which results from the loss of balance between bone formation and bone resorption as aging, disuse, inflammatory diseases, hormonal imbalance or the effect of glucocorticoids impair the ability of osteoblast to keep up with the pace of bone resorption by the osteoclasts (4). Importantly, aging is associated with a decreased number of osteoprogenitor cells, inhibited proliferation, decreased mineralizing capacity, and a shift of osteogenic differentiation toward adipogenesis in senescent mesenchymal stromal cells (MSCs) (5–7).
Pharmacotherapy helps patients to prevent the occurrence or recurrence of fragility fractures and to manage symptoms. However, drugs are mostly used in patients who already show severe bone loss, and the existence of side effects, although very limited in prevalence, often leads to low patient’s adherence to anti-OP drugs (8, 9). In this context, non-pharmacological strategies aimed at preventing excessive bone loss hold relevance given that OP remains in most cases a subclinical condition until fracture occurs.
One safe way to prevent bone loss and reduce the risk of bone fracture is to positively impact bone mass through healthy lifestyles and nutrition (10, 11). In particular, the importance of defining specific diet regimens for the prevention of excessive bone fragility has been increasingly recognized (12–15). Adherence to Mediterranean diet lowered hip fracture risk (16) and certain micronutrients contained in fruit and vegetables contributed to delay bone fragility in ageing and to decrease the incidence of bone fractures (17–20). Moreover, a dietary pattern consisting of a high consumption of fruits, vegetables and seafood, has been shown to be directly associated with increased bone mineral density (BMD), independent of dietary calcium intake (21, 22).
Phytochemicals are defined as the chemical bioactive components of nutrient plants that may provide desirable health benefits beyond basic nutrition to reduce the risk of major chronic diseases. They include several classes of compounds: terpenoids, polyphenols, alkaloids, organosulfur compounds (OSCs) and phytosterols (23). Concerning OSCs, much of the research on their health benefits has been in the areas of cardiovascular diseases, cancer and neurological disorders (24–26). However, a growing body of scientific evidence supports the idea that dietary OSCs may play an important role for skeletal health by favoring bone anabolism, inhibiting bone catabolism, and preventing pathological bone loss.
This manuscript intends to provide an up-to-date review of the current evidence from preclinical (both in vitro and in vivo) and clinical studies on the skeletal effects of OSCs of dietary origin, discussing the chemical nature, the mechanism of action and the potential role of hydrogen sulfide (H2S) in their biological action. A specific focus is given to the pair glucoraphanin (GRA)-sulforaphane (SFN) as a paradigm of OSCs-H2S system in bone tissue. Finally, implications and future challenges in the field will be discussed considering the potential translation of OSCs-containing dietary components to clinical studies.
Dietary sources and chemical nature of OSCs
Naturally derived OSCs are a broad class of molecules containing sulfur, predominantly found in edible plants belonging to the Allium and Brassica (also known as cruciferous vegetables) genera. These plants have been widely used throughout the centuries either as vegetables for culinary purposes as well as in folk and traditional medicine, given their renowned medicinal properties and therapeutic effects. Allium genus consists of more than 600 species which are among the oldest cultivated vegetables used as food and still represent one of the main components of the Mediterranean diet (27). Brassica genus consists of 37 species; among them, several species are known for their nutritional and therapeutic properties (28, 29). A partial list of edible plants belonging to the Allium and Brassica genera, and their main content in OSCs, is reported in Table 1 .
Table 1.
Most common OSCs found in edible Allium and Brassica vegetables.
| Edible plants | Genus | Main OSCs | REF | ||
|---|---|---|---|---|---|
| Garlic (Allium sativum L.) | Allium | • γ-glutamyl-S-allyl-l-cysteine • allicin • alliin • methiin • S-trans-1-propenylcysteine sulfoxide • S-2-carboxypro-pylglutathione • S-allylcysteine • ajoene • vinyldithiins • diallyl sulfide • diallyl disulfide • diallyl trisulfide |
• S-allylcysteine • S-allylmercaptocysteine • S-allylmercaptoglutathione • methyl allyl disulfide • methyl allyl trisulfide • S-allylmercaptocysteine • dipropyl disulfide • dipropyl trisulfide • 1-propenylpropyl disulfide • dimethyl disulfide • allyl mercaptan • propyl propane thiosulfonate |
(30–39) | |
| Onion (Allium cepa L.) | Allium | • isoalliin • methiin • propiin • diallyl disulfide • diallyl trisulfide • γ-l-glutamyl-trans-S-1-propenyl-l-cysteine sulfoxide |
• onionin A • cycloalliin • S-methyl cysteine sulfoxide • S-propenyl cysteine sulfoxide • S-alk(en)yl cysteine sulfoxides • dipropyl disulfide • cycloalliin |
(40–45) | |
| Welsh onion (Allium fistulosum L.) | Allium | • γ-glutamyl-S-allyl-l-cysteine • allicin |
• alliin • diallyl disulfide |
(46, 47) | |
| Hooker’s Onion (Allium hookeri) | Allium | • alliin • methiin |
• cycloalliin • S-propyl-l-cysteine sulfoxide |
(48–50) | |
| Long-stamen chive (Allium macrostemon) | Allium | • alliin • methyl alliin |
(51) | ||
| Leek (Allium ampeloprasum var. porrum) | Allium | • methiin • isoalliin |
(52) | ||
| Shallot (Allium ascalonicum) | Allium | • isoalliin • methiin |
• propiin • γ-glutamyl-S-alk(en)ylcysteines |
(53) | |
| Turnip (Brassica rapa L.) | Brassica | • glucoraphanin & sulforaphane • gluconapin & 3-butenyl isothiocyanate • glucobrassicanapin & 4-pentenyl isothiocyanate/gluconapoleiferin • gluconasturtiin & 2-phenethyl isothiocyanate • goitrin • berteroin |
• progoitrin • glucoalyssin • glucoerucin • glucobrassicin & 4-hydroxyglucobrassicin/4-methoxyglucobrassicin • glucoberteroin • neoglucobrassicin |
(54, 55) | |
| Broccoli (Brassica oleracea var. italica L.) | Brassica | • sulforaphane • glucoiberin • 3-hydroxy,4(α-L-rhamnopyranosyloxy) benzyl glucosinolate |
(56–58) | ||
| Water cress (Lepidum sativum L.) | Brassica | • glucotropaeolin | (59) | ||
| Cabbages (Brassica oleracea var. capitata L.) | Brassica | • glucoraphanin • progoitrin • sinigrin • gluconapin • glucoerucin |
• glucobrassicin & 4-hydroxyglucobrassicin/• 4-methoxyglucobrassicin • neoglucobrassicin • glucoiberin |
(60, 61) | |
| Rocket (Eruca sativa) | Brassica | • glucoraphanin • glucoraphenin • glucosativin • glucoerucin • 4-hydroxyglucobrassicin • glucotropaeolin |
• glucolepiidin • glucoiberverin • glucoalyssin • diglucothiobeinin • glucoibarin |
(62) | |
| Kohlrabi (Brassica oleracea var. gongylodes) | Brassica | • glucoraphanin & sulforaphane • glucoerucin & methylthiobutyl isothiocyanate • benzyl isothiocyanate • gluconasturtiin & phenylethyl isothiocyanate |
• sinigrin & allyl isothiocyanate • glucobrassicin & hydroxyglucobrassicin • neoglucobrassicin • methiin |
(63, 64) | |
| Radish (Raphanus sativus) | Brassica | • 3-butenyl isothiocyanate • glucobrassicin/4-methoxyglucobrassicin/4- hydroxyglucobrassicin/indole-3-carbinol |
• glucodehydroerucin • glucoraphasatin • glucoraphenin/sulforaphene • sulforaphane |
(65) | |
| Tuscan black kale (Brassica oleracea L.) | Brassica | • glucoerucin • glucobrassicin • glucoraphanin |
(66) | ||
| Rapes (Brassica napus L.) | Brassica | • glucoalyssin • glucobrassicin & hydroxyglucobrassicin • neoglucobrassicin |
• gluconasturtin • gluconapin • glucobrassicanapin • progoitrin |
(61, 67) | |
| Arugula (Eruca Sativa Mill.) | Brassica | • glucoraphanin & sulforaphane | • glucoerucin & erucin | (68) | |
In Allium, over half of the total sulfur content within the mature garlic bulb is found in the form of S-alk(en)yl cysteine sulfoxides (ASCOs) (69), non-protein sulfur amino acids which are converted to their respective thiosulfinates or propanethial-S-oxide upon tissue damage (70).
The synthesis of ASCOs in Allium species starts with the transformation of γ-glutamyl peptides (such as γ-l-glutamyl-S-methyl-L-cysteine) into sulfur-containing γ-glutamyl-S-alk(en)yl-cysteines such as γ-glutamyl-S-methyl-cysteines, γ-glutamyl-S-allyl-cysteine, γ-glutamyl-propenyl-l-cysteine sulfoxide (PeCSO). These are further deglutamylated and S-oxygenated to yield S-alk(en)yl-l-cysteine sulfoxides (71, 72). These reactions are catalyzed by γ-glutamyl transpeptidase, l-glutaminases, and oxidase in the cytoplasm of plant cells. The intact garlic bulbs contain alliin, γ-glutamyl-S-allyl-l-cysteine (GSAC), methiin, S-trans-1-propenyl-l-cysteine sulfoxide, S-2-carboxypropylglutathione, S-allylcysteine (SAC) (37).
When the bulbs are cut, crushed, chopped or chewed, the enzyme alliinase (a vacuolar lyase) is released from vacuoles and catalyzes the formation of sulfenic acids from l-cysteine sulfoxides: S-allyl-l-cysteine sulfoxide (alliin); S-methyl-l-cysteine sulfoxide (methiin); S-propyl-l-cysteine sulfoxide (propiin); S-trans-1-propenyl-l-cysteine sulfoxide (isoallin) (71, 72). Sulfenic acids spontaneously react with each other to form unstable compounds called thiosulfinates (69): eg. alliin is converted into allicin (alkenyl alkene thiosulfinate - diallyl thiosulfinate). Allicin immediately decomposes into allyl sulfide (AS), diallyl disulfide (DADS), diallyl trisulfide (DATS), diallyl tetrasulfide, dipropyl disulfide (DPDS), ajoenes, and vinyldithiins (72). The direct catabolism of γ-glutamylcysteine by γ-glutamyltranspeptidase leads to the formation of SAC and S-allylmercaptocysteine (SAMC). Allicin can react with glutathione and l-cysteine to produce S-allylmercaptoglutathione (SAMG) and SAMC, respectively (69, 72).
Among Allium, the most common ASCOs are alliin, methiin, propiin and isoalliin (70, 73, 74). However, they are differentially expressed in specific edible plants. The most abundant in garlic is alliin; in onion isoalliin, methiin, propiin are predominantly detected.
In Brassica vegetables two different kinds of OSCs are present: methiin, mainly known from Allium vegetables, and glucosinolates (S-β-thioglucoside N-hydroxhysulfates, GLS). Methiin is metabolized to (+)-S-alk(en)yl-l-cysteine sulfoxides which can degrade to volatile organosulfur compounds (VOSCs) such as S-methyl methane thiosulfinate, which is converted to dimethyl trisulfide and dimethyl disulfide.
GLS are sulfur-based compounds that consist of β-thioglycoside N-hydroxysulfates with various side chains and a sulfur-linked β-d-glycopyranose moiety. A very different profile of GLS may be found in different Brassica extracts (75). Natural isothiocyanates (ITCs) are bioactive OSCs derived from the hydrolysis of GLS by the enzyme myrosinase. In plant cells, GLS are physically separated from myrosinases and come in contact only upon tissue damage or crushing. Importantly, myrosinase is not expressed by mammalian cells; however, a small proportion is converted in the mouth by action of plant myrosinase released by chewing (76); moreover, the gut microbiota is entailed with myrosinase activity and constitutes the major site in humans where GLS are hydrolyzes to ITCs (77). While GLS are chemically stable and are characterized by a relatively long half-life, ITCs are highly reactive and short-lived in vivo (75, 78).
Effect of OSCs on bone tissue: Preclinical evidence
The effect of OSCs in bone tissue has been investigated in several preclinical models, revealing a strong potential to preserve skeletal health by stimulating the bone forming activity of osteoblasts and inhibiting the bone resorbing activity of osteoclasts, two of the key processes of bone remodeling (79).
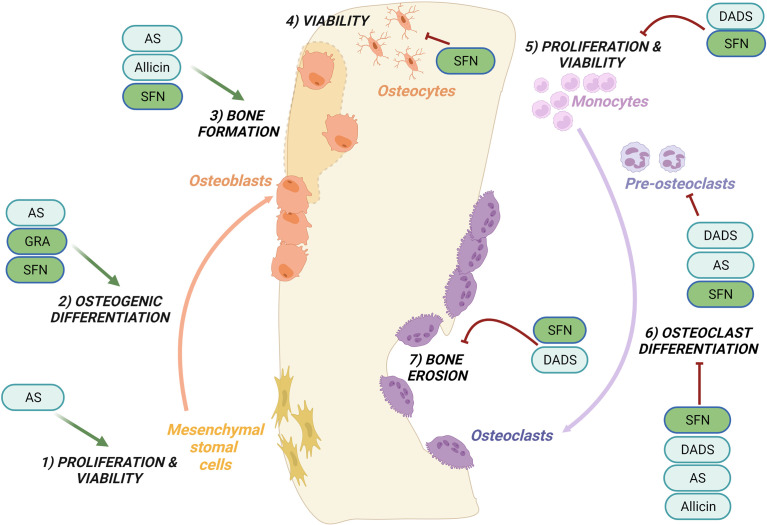
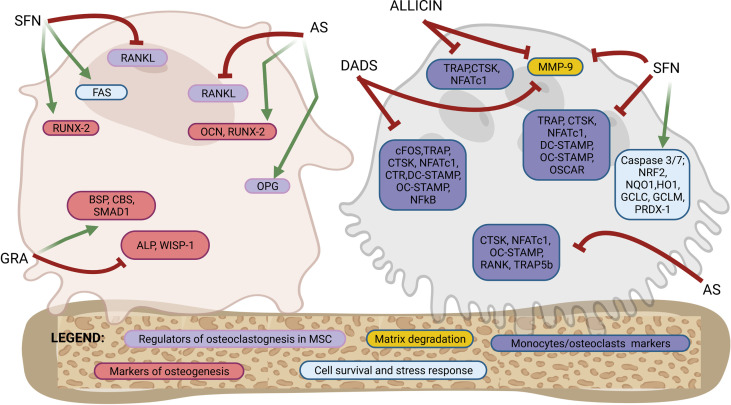
Figures 1 , 2 provide a graphical summary, respectively, of the main biological processes and molecular targets regulated by OSCs within MSCs/osteoblasts and monocytes/osteoclasts. A detailed description of these mechanisms is provided in the next paragraphs.
Figure 1.
Regulation of bone remodeling processes by purified OSCs molecules. Bone remodeling is governed by the balance between bone formation by the osteoblasts (left side) and bone erosion by the osteoclasts (right side). Ancillary processes are shown. OSCs specifically regulate the following processes: promote cells proliferation and viability of mesenchymal stromal cells (1) while inhibit the proliferation and viability of monocytes (5); promote the osteogenic differentiation (2) and bone formation (3); inhibit at different stages osteoclast differentiation (6) and reduce bone erosion (7); inhibit the viability of osteocytes (4). Among the OSCs which modulate bone processes are allicin, allyl sulfide (AS), sulforaphane (SFN), glucoraphanin (GRA), diallyl sulfide (DADS). See the text for details.
Figure 2.
Molecular targets of purified OSCs molecules in bone cells. Osteoblastogenesis and osteoclastogenesis are the two key processes of bone remodeling and are regulated by a tightly organized activation of specific molecular targets. This figure shows a schematic representation of a mesenchymal stromal cells/osteoblast and a monocyte/osteoclast to highlight the specific molecular targets regulated by OSCs at different stages of differentiation from precursors to fully differentiated cells. Among the OSCs which drives the modulation of specific molecular targets are allicin, allyl sulfide (AS), sulforaphane (SFN), glucoraphanin (GRA) and diallyl sulfide (DADS). The overall effects are an activation of osteogenic differentiation in mesenchymal stromal cells and both a direct and indirect inhibition of osteoclast differentiation. Follows a list of the molecular targets shown in the figure. Markers of osteoblastogenesis: osteocalcin (OCN), runt-related transcription factor 2 (RUNX-2), alkaline phosphatase (ALP), WNT1-inducible-signaling pathway protein 1 (WISP-1), bone sialoprotein (BSP), cystathionine-β-synthase (CBS), SMAD family member 1 (SMAD-1). Markers of regulators of osteoclastogenesis produced by mesenchymal stromal cells or osteoblasts: receptor activator of nuclear factor-κB ligand (RANKL), osteoprotegerin (OPG). Marker of cells survival and stress response: FAS, caspase 3/7, nuclear factor erythroid-derived 2-related factor 2 (NRF2), NAD(P)H: quinone oxidoreductase 1 (NQO1), heme oxygenase-1 (HO1), glutamate cysteine ligase catalytic subunit (GCLC), glutamate-cysteine ligase modifier subunit (GCLM), peroxiredoxin 1 (PRDX-1). Markers of osteoclasts: nuclear factor of activated T-cells cytoplasmic 1 (NFATc1), cathepsin K (CTSK), receptor activator of NF-KB (RANK), osteoclast stimulatory transmembrane protein (OC-STAMP), dendritic cell specific transmembrane protein (DC-STAMP), osteoclasts-specific activating receptor (OSCAR), tartrate-resistant acid phosphatase (TRAP), calcitonin receptor (CTR), c-fos, tartrate-resistant acid phosphatase 5b (TRAP-5b), matrix metallopeptidase 9 (MMP-9). See the text for details.
Tables 2 – 5 summarize data from preclinical studies showing an effect of extracts rich in OSCs or individual OSCs molecules derived from Allium ( Tables 2 , 3 ) and Brassica vegetables ( Tables 4 , 5 ).
Table 2.
Alliaceae-derived OSCs: effects on in vitro models of osteoclastogenesis and osteoblastogenesis.
| Molecule tested | Experimental in vitro model | Concentration | Main effect | Specific outcomes | Authors | Ref |
|---|---|---|---|---|---|---|
| Hot-water extract and ethanol extracts of Allium hookeri roots | MG-63 cells line | 0.1-0.5-1-5-10-25-50-100 μg/ml | Increased proliferation and osteogenesis | • ↑ viability/proliferation; no cytotoxicity (WST-8 assay) • ↑ ALP activity (pNPP detection) • ↑ collagen (Sirius red assay) • ↑ mineralization (Alizarin Red staining) |
Park et al. | (48) |
| Aqueous and ethanolic extracts of Allium fistulosum | MG-63 cell line | 1-4-8-10-16-32-50-63-125 μg/ml | Increased osteogenesis | • no cytotoxicity (MTT assay) • ↑ ALP activity (ALP assay kit) |
Ryuk et al. | (80) |
| Water solution of onion crude powder | MG-63 cell line | 300 μg/ml | No effect on proliferation or differentiation | • ALP activity similar to control cells (ALP assay kit) • Col I on cell lysate was similar to control cells (4- hydroxyproline quantification) • OCN, OPN in cells surnatants similar to control cells (ELISA) |
Tang et al. | (81) |
| Aqueous and ethanolic extracts of Allium fistulosum | MC3T3-E1 cell line | 1-4-8-10-16-32-50-63-125 μg/ml | Increased proliferation and osteogenesis | Ethanolic extracts: • ↑ viability/proliferation; no cytotoxicity (MTT assay) • ↑ALP activity (ALP assay kit) Water extracts: • no cytotoxicity (MTT assay) • ↑ALP activity (ALP assay kit) |
Ryuk et al. | (80) |
| Water Allium sativum L. extract | Human fetal osteoblast cells | 3D-printed calcium phosphate scaffolds releasing ginger and garlic extract | Increased osteoblast proliferation | • ↑ proliferation (MTT assay) | Bose et al. | (82) |
| Allyl sulfide (AS) * | BMMSCs isolated from Age-associated OP mice’s femurs |
Mice were fed by oral gavage with AS (200 mg/kg) for 3-months | • Rescue of proliferation and osteogenesis • Indirect inhibition of osteoclastogenesis |
• ↑ proliferation as compared to aged mice (MTT assay) • ↑ALP activity (ALP staining), ↑ mineralization (Alizarin red staining), • ↑ RUNX-2 and OCN in cells (western blot) • ↑ OPG and ↓ RANKL in surnatants (ELISA) |
Behera et al. | (83) |
| Allium cepa L. extracts | In vitro bioactivity assay (simulated body fluid) | Chitosan + Allium cepa L. (ChAC) and Chitosan + Allium cepa L. + PLGA (ChPAC) | Improved natural bioactivity of chitosan | • Increased apatite cristals in the surface • Improved Phosphorous/Calcium ratio |
Monárrez-Cordero et al. | (84) |
| Water Allium sativum L. extract | Human osteoclast cells from THP1 monocytes | 3D-printed calcium phosphate scaffolds releasing ginger and garlic extract | Inhibition of osteoclast activity | • ↓ resorption (pit assay) | Bose et al. | (82) |
|
Ethanolic extract of
onion |
RAW 264.7 cell line | 0.1-0.2-0.4 mg/ml | Inhibition of osteoclastogenesis | • no cytotoxicity (MTT assay) • ↓ osteoclasts (TRAP assay) |
Law et al. | (85) |
| Freeze dried onion juice | RAW 264.7 cell line | 0.1-0.2-0.4 mg/ml | Inhibition of osteoclastogenesis | • no cytotoxicity (MTT assay) • ↓ osteoclasts (TRAP assay) |
Law et al. | (85) |
| Water solution of onion crude powder | RAW 264.7 cell line | 15-50-150-300 μg/ml | Inhibition of osteoclastogenesis | • no cytotoxicity (MTT assay) • ↓ osteoclasts (TRAP assay) • ↓ CD51/61 (vitronectin receptor), MMP-9 and TRAP mRNA (RT-PCR) • ↓ ERK, p38 and NF-κB (western blot) |
Tang et al. | (81) |
| Diallyl disulfide (DADS) * | RAW 264.7 cell line | 1-10-100-1000 μg/ml 20-40-60-80-100 μg/ml |
Inhibition of osteoclastogenesis and bone resorption | • ↓ cytotoxicity at concentration higher to 100 μg/ml (CCK-8 assay) • ↓ osteoclast and resorption (TRAP assay PIT assay) • ↓ c-fos, NFATc1, TRAP, MMP9, CTR, CTSK, DC-STAMP, OC-STAMP mRNA • ↓ osteoclast fusion (FAK staining) • ↓ NF-ĸB, p-STAT3, NFATc1, c-FOS (western blot) |
Yang et al. | (86) |
| Alliin * | RAW 264.7 cell line | 0.1-0.5-1-5-10-100 μg/ml | Inhibition of osteoclastogenesis | • No cytotoxicity (CCK-8 assay) • ↓ osteoclasts and resorption (TRAP assay and pit assay) • ↓ c-fos, NFATc1, MMP9, DC-STAMP, OC-STAMP, RANK, TRAP (RT-PCR) • ↓ Nox-1, NFATc1, c-fos (western blot) • ↓ ROS (detection by fluorescent probe) |
Chen et al. | (87) |
| Water solution of onion crude powder | Osteoclast derived from bone marrow cells of femurs of 6-8-week-old Sprague–Dawley rats | 15-50-150-300 μg/ml | Inhibition of osteoclastogenesis | • no cytotoxicity (MTT assay) • ↓ osteoclasts (TRAP assay) |
Tang et al. | (81) |
| Water solution of onion crude powder | Osteoclast derived from long bones of 6-day-old rabbits | 15-50-150-300 μg/ml | Inhibition of bone resorption | • ↓ resorption (pit assay) | Tang et al. | (81) |
| Commercial onion powder (Chia Hui, Taipei, Taiwan) | Osteoclast derived from bone marrow cells of femurs of 6-8-week-old Sprague–Dawley rats | 300 μg/ml | Inhibition of osteoclastogenesis | • ↓ osteoclasts (TRAP assay) • Inhibition of ERK, p38, and NF-κB activation (western blot) |
Tang et al. | (81) |
|
GPCS isolated by bioassay-guided fractionation of
Allium cepa L. Bulbs * |
Osteoclasts derived from femora and tibiae of 2-days-old Wistar Hanlbm rats | 1-10-30 mg/ml 2-4-8 mM |
Inhibition of osteoclast differentiation and activity | • ↓ osteoclast differentiation and resorption by GPCS (TRAP staining and pit assays) | Wetli et al. | (41) |
| Diallyl disulfide (DADS) * | BMMs obtained from the femur and tibia bone marrow of 6-wk-old C57BL/6 mice | 20-40-60-80-100 μg/ml | Inhibition of osteoclastogenesis | • ↓ cytotoxicity at concentration higher to 100 μg/ml (CCK-8 assay) • ↓ osteoclast (TRAP assay) |
Yang et al. | (86) |
| Allyl sulfide (AS)* | BM cells | Cultured under 15% conditioned medium derived from BMMSCs culture of Age-associated OP mouse model (Fed by oral gavage with AS (200 mg/kg) for 3-months) | Inhibition of osteoclastogenesis via a paracrine mechanism | • ↓ osteoclasts (TRAP staining) • ↓ TRAP-5b expression in cells lysates (ELISA) • ↓ NFATc1, CTSK, RANK and OC-STAMP mRNA (RT-PCR) |
Behera et al. | (83) |
Most in vitro studies were conducted by using water or ethanol extracts from Allium edible plants (4 studies, 13 in vitro models; Allium hookeri roots, Allium fistulosum, Allium sativum L., Allium cepa L.); a few used purified OSCs (3 studies, 6 in vitro models; diallyl disulfide (DADS), allyl sulfide (AS), γ-glutamyl-trans-S-1-propenyl-L-cysteine sulfoxide – GPCS, alliin). Most studies showed an increased osteoblast proliferation and osteogenesis and an inhibited osteoclastogenesis. Notably, only the effects of purified OSCs (labeled with * in the table) can be attributable entirely to OSCs. The concentrations tested ranged from 0.1 to 300 μg/ml. Murine in vitro models of osteoclastogenesis: osteoclasts derived from bone marrow of femora and tibiae of rats, rabbits, mice; RAW 264.7 cells. Human in vitro models of osteoclastogenesis: osteoclast cells from human THP1 monocytes. Murine in vitro models of osteoblastogenesis used: MC3T3-E1 (mouse C57BL/6 calvaria cells line); murine bone marrow (BM) cells; bone marrow-derived mesenchymal stem cells (BMMSCs) isolated from age-associated (AG) osteoporosis (OP) mice’s femurs. Murine in vitro models for studying indirect inhibition of osteoclastogenesis: bone marrow-derived mesenchymal stem cells (BMMSCs), bone marrow macrophages (BMM) and murine bone marrow (BM). Human in vitro models of osteoblastogenesis: MG-63 cells line (human osteosarcoma cells line), human fetal osteoblast. Functional assays for osteoclastogenesis used: tartrate-resistant acid phosphatase positive (TRAP staining); pit assay. Functional assays for osteoblastogenesis: alizarin red staining (marker of mineralization), sirius red assay (marker of collagen I), p-nitrophenyl phosphate (pNPP) measurement. Proliferation/viability assays: 3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) assay, cell counting kit-8 (CCK-8) cell viability assay, water-soluble tetrazolium-8 (WST-8) assay. Markers of osteoclasts: nuclear factor of activated T-cells cytoplasmic 1 (NFATc1), cathepsin K (CTSK), receptor activator of NF-KB (RANK), osteoclast stimulatory transmembrane protein (OC-STAMP), tartrate-resistant acid phosphatase (TRAP), tartrate-resistant acid phosphatase 5b (TRAP-5b), receptor activator of nuclear factor-κB ligand (RANKL), dendritic cell specific transmembrane protein (DC-STAMP), reactive oxygen species (ROS), calcitonin receptor (CTR), p-signal transducer and activator of transcription 3 (p-STAT3), NADPH Oxidase 1 (Nox-1), c-fos, nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB), p38, extracellular signal-regulated kinase (ERK), matrix metallopeptidase 9 (MMP-9), CD51/61 (vitronectin receptor). Markers of osteoblastogenesis: collagen I (Col I), osteocalcin (OCN), osteopontin (OPN), runt-related transcription factor 2 (RUNX-2), osteoprotegerin (OPG), alkaline phosphatase (ALP). ↑ means up-regulation; ↓ means down-regulation.
Table 5.
Brassicaceae-derived OSCs: effects on in vivo models of bone loss.
| Molecule tested | Experimental in vivo model description | Mode of administration, dose and duration | Main effect | Specific features | Authors | Ref |
|---|---|---|---|---|---|---|
| Sulforaphane | C57BL/6 mice, Mouse calvarial models treated with LPS (10 mg/kg body weight injected in calvaria) | Intraperitoneal injection, 10 mg/kg body weight, the day before LPS treatment for 6 days | Protection against LPS-induced calvarial bone erosion by inhibition of osteoclastogenesis | • ↑ BV/TV, Tb.N, ↓Tb.Sp (microCT) • ↓ osteoclasts (TRAP staining in histological samples) • ↓ CTSK (immunohistochemical and immunofluorescence analysis) |
Luo et al. | (103) |
| Sulforaphane | Ex vivo culture of calvariae explants of 2–3-day-old and 7-week-old, C57BL/6 mice | 3 μM | Promotes osteogenesis inhibits osteoclastogenesis | • ↑ ECM mineralization (alizarin red staining on calvaria tissue) • ↓ RANKL (RT-PCR on calvariae lysates) |
Thaler et al. | (97) |
| Sulforaphane | Mice model of OP (Female, 8-week-old, C57BL/6 mice, ovariectomy) | Intraperitoneal injection, 7.5 mM DL-SFN, every other day for 5 weeks | Prevention of bone loss | • ↑ BV/TV, Tb.N ↓Tb.Sp, no effect on Tb.Th or Co.Th in tibiae (micro CT) | Thaler et al. | (97) |
| SFX- 01® (a stable form of Sulforaphane) | Osteoarthritis model (Male, 26-week-old, STR/Ortmice) | Oral administration, 100 mg/kg, daily for 3 months | Improvements in cortical bone mass | • ↑ TV, BV and BV/TV of tibial epiphyseal trabecular bone and metaphyseal trabecular bone (micro CT) • ↑serum P1NP (ELISA) • ↓serum CTX-I (ELISA) |
Javaheri et al. | (105) |
| Brassica rapa L. root ethanol extract | Female, 3-week-old, Sprague- Dawley rats | Oral administration, 500 mg/kg/day, single daily dose for 6 weeks | Increased bone formation | • ↑ BMD, BV, BV/TV, Tb.N, Tb.Th., ↓Tb.Sp. (microCT) • ↑ serum OCN (immunoassay) |
Jeong et al. | (54) |
| Lepidum sativum seed extract | Rat model of OP (Female Wistar rats, ovariectomy) | Oral gavage 50 and 100 mg/kg | Prevention of bone loss and bone strengthening activity | • ↑ femur weight (weights were calculated as wet femur weight/body weight) • ↑ femur compression strength (hardness tester (Erweka GmbH, Heusen-stamm, Germany) • ↑ ALP, OCN serum levels; ↓ TRAP, CTX-I serum levels (ELISA) • ↓ RANKL, ↑ OPG mRNA (RT-PCR) |
Abdallah et al. | (59) |
| Lepidum sativum seed | Glucocorticoid-induced OP (GIO) model (Female Wistar rat, subcutaneous injection of methylprednisolone 3.5 mg/kg per day for 4 weeks) | Oral gavage, 6 g of LS seeds in diet daily | Prevention of GIO-dependent bone loss | • ↑ percentage of trabecular bone vs GIO (histopathological examination and Image J quantification) • ↓ serum TRAP vs GIO (commercial kit) • ↑ serum b-ALP (immunoassay), phosforous and calcium (automated analyser) vs GIO |
Elshal et al. | (106) |
| Lepidum sativum seed | Fracture-induced healing model (New Zealand White rabbits, induced fractures in the midshaft of the left femur) | Oral gavage, 6 g of Lepidum sativum seeds in their food daily after surgery | Increased healing of fractures | Increased callus formation in fractures (x-rays and quantification) | Juma et al. | (83) |
| Methanolic and aqueous extract of Lepidium sativum seeds | Fracture healing model (Charles foster rats, hand held three-point bending technique) | Oral administration, methanolic extracts 400 mg/kg or aqueous extracts 550 mg/kg, from the day of fracture induction for 2 months | Increased healing of fractures | • Larger callus formation (x-rays and quantification) • ↑ calcium, phosphorus, and ALP serum levels (commercial kits) |
Dixit Jr Iii et al. | (28) |
| Lepidium sativum seeds | Glucocorticoid-induced OP (Adult male guinea pigs, methyl prednisolone 3.5 mg/kg per day for 4 weeks subcutaneously) | Oral administration trough a gastric tube, 300 mg/kg, for 4 weeks | Prevention of bone loss in femur | • Prevention of caspase-3 activation (caspase-3 immunostaining) • Prevention of decrease of OPN (immunohystochemistry) • Prevention of decrease in osteoblast and Co.th. in femur (histomorphometric analysis) • Prevention of increase of osteoclasts in femur (histomorphometric analysis) |
EL-Haroun et al. | (107) |
| Ethanol extracts of Maca root (Lepidium meyenii Walp.) | Rat model of OP (Female, 90-day-old, Sprague-Dawley rats, ovariectomy) | Oral gavage, 0.096 and 0.24 g/kg, for 28 weeks | Prevention of estrogen deficient bone loss | • ↑ calcium content of femur (Atomic Absorption Spectrophotometer) • ↑ BMD and trabecular bone of the lumbar vertebrae (DEXA) • ↑ serum OCN (radioimmunoassay commercial kit) |
Zhang et al. | (108) |
| Hot water extract of Brassica oleracea (Bo) | Mice model of OP (Female, 7-week-old, C57BL/6 mice, ovariectomy) | Oral administration, 500 mg/kg, daily for 10 weeks | Inhibits OVX-induced bone loss | • ↑ BMD when in combination with Panax ginseng (DEXA) • ↓ osteoclast number when in combination with Panax ginseng (immunohistochemistry, TRAP staining) |
Kang et al. | (99) |
Most in vivo studies were conducted by using water or ethanol extracts of Brassica edible plants (8 studies; Brassica rapa, Lepidum sativum, Lepidum meyenii Walp, Brassica oleracea). A minority of studies used Brassicaceae-purified OSCs (3 studies; 4 models; SFN, SFX-01). Most studies were performed in osteoporosis mice showing prevention of bone loss. Notably, only the effects of purified OSCs (labeled with * in the table) can be attributable entirely to OSCs. The route of administration was mainly by oral administration. Markers of bone formation in serum: procollagen 1 intact N-terminal propeptide (P1NP); osteocalcin (OCN). Markers of bone resorption in serum: serum type I collagen breakdown product (CTX-I), tartrate-resistant acid phosphatase (TRAP), osteoprotegerin (OPG), cortical thickness (Co.Th). Bone microstructural parameters analyzed by microCT analysis: BMD (bone mineral density), bone volume (BV), bone volume/total volume (BV/TV), trabecular thickness (Tb.Th), trabecular number (Tb.N), trabecular space (Tb.Sp.). Bone mineral density analyzed by Dual-energy X-ray absorptiometry (DEXA). Markers of bone formation in histological specimen: alkaline phosphatase (ALP), osteopontin (OPN). Markers of osteoclasts/bone resorption in histological specimen: tartrate-resistant acid phosphatase (TRAP), cathepsin K (CTSK). Measurements of bone strength: Erweka GmbH, Heusen-stamm Germany. Extracellular matrix (ECM). Markers of osteoclast in histological specimen: receptor activation of nuclear factor-kB ligand (RANKL). ↑ means up-regulation; ↓ means down-regulation. ↑ means up-regulation; ↓ means down-regulation.
Table 3.
Alliaceae-derived OSCs: effects on in vivo models of bone loss.
| Molecule tested | Experimental in vivo model description | Mode of administration, dose and duration | Main effect | Specific outcomes | Authors | Ref |
|---|---|---|---|---|---|---|
| Ethanol extracts of Allium macrostemon bulbs | Female, 25-day-old, Sprague–Dawley rats (adolescent mice) |
Gavage, 100 and 300 mg/kg, twice daily for 10 days | Increase tibial longitudinal bone growth |
|
Kim et al. | (85) |
| Hot-water extracts of Allium hookeri roots | Female, 3-week-old, Sprague-Dawley rats | Oral treatment, 500 mg/kg, single daily dose, for 6 weeks | Improved bone formation |
|
Park et al. | (48) |
| Wheat bread added with Allium sativum L. | Male weaning Wistar rats | Oral administration, 3 g per 100 g wheat flour, for 60 days | Increase in BMD |
|
Weisstaub et al. | (88) |
| Ethanolic extracts of Allium cepa L. bulbs | Male, 9-week-old, Wistar Hanlbm rats | Orally given, one gram, daily treatment, for 10 days | Inhibition of bone resorption | ↓ bone resorption (urinary excretion of tritium) | Wetli et al. | (41) |
| Homogenized of Allium sativum L. | Hypercholesterolemic rat model (Pregnant albinorat Wistar fed with hypercholesterolemic diet, and their offspring) |
Intragastrical injection, 100 mg/kg, a week prior to onset of feeding with hypercholesterolemic diet | Improved endochondral ossification | ↑ ossification in mandibular, humerus, radio-ulna, femur, tibio-fibula, scapula and ilium (Alizarin red S for ossified skeletal bones in fixed offspring) |
El-Sayyad et al. | (89) |
| Water Allium sativum L. extract | In vivo implants in bicortical rat distal femur defects (Sprague–Dawley rats) | 3D-printed calcium phosphate scaffolds designed with a bimodal pore distribution releasing ginger and garlic extract, implanted for 4-10 weeks | Increase in osteoinductivity |
|
Bose et al. | (82) |
| Aqueous and ethanolic extracts of Allium fistulosum | CDD mice - Mice model of bone loss due to nutritional deficiency (Male, 4-week-old, C57BL/6 mice, fed with a calcium- and vitamin D-deficient diet for 5 weeks) |
Oral treatment, 150 and 450 mg/kg, ad libitum feeding for 4 weeks | Prevention nutritional deficiency-induced bone loss and retarded bone growth |
|
Ryuk et al. | (80) |
| Water extract of Allium fistulosum root | Rat model of OP and osteoarthritis (Female, 8-week-old, Sprague–Dawley rats, ovariectomy and MIA-induced OA) | Within rice porridge, 250 and 750 mg/kg, food supply was replaced every two days for 8 weeks |
Prevention of bone loss |
|
Yang et al. | (47) |
| Oil extract of Allium sativum L. from raw cloves | Rat model of OP (Female albinorats, ovariectomy) | Gavage, 100 mg/kg body wt/day, single evening dose for 30 days | Prevention of bone loss |
|
Mukherjee et al. | (90) (91) |
| ↑ calcium and phosphate content in femur, lumbar vertebra, thoracic vertebra, thoracic rib (method of Adeniyi et al. (1993) and Lowry and Lopez (1946)) |
Mukherjee et al. | (91) (92) | ||||
|
Mukherjee et al. | (92) | ||||
| Oil extract of Allium sativum L. from raw cloves | Rat model of OP (Female Wistar, ovariectomy) | Gavage, 100 mg/kg body wt/day, single evening dose for 30 days | Increase in bone strength and inhibition of bone resorption |
|
Mukherjee et al. | (93) |
| Allium cepa L. powder | Rat model of OP (Female, 14-week-old, Wistar rats) treated or not with 1 mg/kg/day alendronate | Dietary administration, diet containing 3%, 7% and 14% (wt/wt) Allium cepa L. powder, for 6 weeks | Prevention of Ovx-induced bone loss and deterioration of biomechanical properties (efficacy was slightly inferior to that of alendronate) |
|
Huang et al. | (94) |
| Diallyl disulfide (DADS) * | A mouse calvarial osteolysis model (Female, 6-wk-old, C57BL/6 mice, LPS treatment 5 mg/kg) | Subcutaneous injections, 20-40 mg/kg DADS, every alternate day for 14 days | Inhibition of LPS-induced osteolysis |
|
Yang et al. | (86) |
| Allyl sulfide (AS) * | Age-associated OP mouse model (Female, 20-months-old (aged), C57BL/6 J mice) | Oral gavage, 200 mg/kg, 3-months | Restored osteogenesis and bone density |
|
Behera et al. | (83) |
| Allicin * | Mice model of lead-induced bone loss (Male, 3-weeks-old, C57BL/6 J mice, 0.2% lead acetate in drinking water ad libitum for 12 weeks) |
Intraperitoneally injection, 10 mg/kg, in the last 4 weeks | Prevention lead-induced bone loss |
|
Li et al. | (95) |
| Allicin * | Mice model of aging rats (Male, 13 months-old, F344 rats) | Intragastric administration, 4-8-16 mg/kg, once daily for 8 months | Reverse aging-associated bone loss and frailty |
|
Liu et al. | (96) |
Most in vivo studies were conducted by using water or ethanol extracts of Allium edible plants (11 studies; Allium macrostemon, Allium hookeri, Allium fistulosum, Allium sativum L., Allium cepa L.). A few studies used Allium-derived OSCs (4 studies; diallyl sulfide, allyl sulfide, allicin). Most studies were performed in normal control mice showing improved bone formation and inhibited bone resorption; and in osteoporosis mice showing prevention of bone loss. Notably, only the effects of purified OSCs (labeled with * in the table) can be attributable entirely to OSCs. Markers of bone formation in serum: procollagen 1 intact N-terminal propeptide (P1NP); osteocalcin (OCN); collagen I (Col I), alkaline phosphatase (ALP), parathormone (PTH). Markers of bone resorption in serum: serum type I collagen breakdown product (CTX-I). Markers of bone resorption in urine: urinary excretion of tritium. Bone microstructural parameters analyzed by microCT analysis: BMD (bone mineral density), bone volume fraction (BVF), spine BMD (s-SMD), tibia BMD (t-BMD), BMC (bone mineral content), bone volume (BV), bone volume/total volume (BV/TV), bone surface/bone volume (BS/BV), trabecular thickness (Tb.Th), trabecular number (Tb.N), trabecular space (Tb.Sp), bone volume fraction (BVF). Bone mineral density analyzed by dual-energy X-ray absorptiometry (DEXA). Markers of bone formation in histological specimen: ALP, Col I. Osteoid tissue detection by masson-goldner trichrome assay. Markers of osteoclasts/bone resorption in histological specimen: tartrate-resistant acid phosphatase (TRAP), nuclear factor of activated T-cells cytoplasmic 1 (NFATc1), cathepsin K (CTSK). Markers of redox stress response: catalase (CAT), superoxide dismutase (SOD), reduced glutathione (GSH), malondialdehyde (MDA). Measurements of bone strength: method of Shapiro and Heaney (2003); three-Point Bending Test. Other abbreviations: insulin-like growth factor 1 (IGF-1), bone morphogenetic protein 2 (BMP-2), lipopolysaccharide (LPS), sirtuin (SIRT); forkhead box O (FOXO). ↑ means up-regulation; ↓ means down-regulation.
Table 4.
Brassicaceae-derived OSCs: effects on in vitro models of osteoclastogenesis and osteoblastogenesis.
| Molecule (organosulfur compouds) | Experimental in vitro model | Concentration | Main effect | Specific outcomes | Authors | Ref |
|---|---|---|---|---|---|---|
| Sulforaphane * | MLO-Y4, an osteocyte – cell line | 3-10-15-30-100 μM | Inhibits cells proliferation; induces apoptosis; and inhibits osteoclastogenesis | • ↓ viability and metabolic activity (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide-like assay (EZ4U) • ↑ in the activities of Caspase 3/7 and 8 (assay kit) • ↑ Fas mRNA expression (RT-PCR) • ↓ RANKL mRNA expression (RT-PCR) |
Thaler et al. | (97) |
| Glucoraphanin * | In vitro culture of human mesenchymal stromal cells from tibial plateau | 3.3-10-33-100 μM | Induction of osteogenesis | • ↑ mineralization (alizarin red staining) • ↑ BSP, CBS, SMAD-1 mRNA (RT-PCR) • ↓ ALP, WISP-1 mRNA (RT-PCR) |
Gambari et al. | (98) |
| Brassica rapa L. root ethanol extract | MG-63 cells line | 1-5-10-25-50 μg/ml | Increased osteogenesis | • ↑ viability (Wst-8 assay) • ↑ ALP activity (pNPP measurements) • ↑ collagen (Sirius Red) • ↑ mineralization (alizarin red staining) |
Jeong et al. | (54) |
| Sulforaphane * | MC3T3-E1 | 3-10-15-20-30-100 μM SFN | Promotion osteoblast differentiation and induction of apoptosis | • ↓ cells proliferation (3-(EZ4U) • ↑ in the activities of Caspase 3/7 and 8 (assay kit) • ↑ Fas mRNA expression (RT-PCR) • ↑ mineralization (alizarin red staining) • ↑ RUNX-2 mRNA expression (RT-PCR) |
Thaler et al. | (97) |
| Sulforaphane * | BMMSCs from long bones of 6-week-old C57BL/6 mice | 3 μM | Promotes osteoblast differentiation | • ↑ mineralization (alizarin red staining) • ↑ RUNX-2 mRNA expression (RT-PCR) |
Thaler et al. | (97) |
| Hot water extract of Brassica oleracea | RAW 264.7 cell line | 200 g/mL | Inhibition of osteoclast formation | ↓ osteoclasts in femur, when in combination with P. ginseng extract (TRAP staining) | Kang et al. | (99) |
| Sulforaphane * | RAW 264.7 cell line | 3-10-15-30-100 μM | Reduces proliferation and induces apoptosis | • ↓ viability and metabolic activity (EZ4U) • No alteration in Acp5, Clcr, and CTSK mRNA expression (RT-PCR) • ↑ Tet1 and Fas-Caspase 8-Caspase 3/7 pathway (western blot, assay kit) |
Thaler et al. | (97) |
| Sulforaphane * | RAW 264.7 cell line | 1-2-5-10 μM | Inhibition of osteoclastogenesis | • ↓osteoclasts (TRAP staining) • ↑ NRF2 protein accumulation (western blot); ↑ HO1, NQO1, GCLC and GCLM mRNA (RT-PCR) • ↓ ROS (2′,7′-Dichlorofluorescin diacetate) • ↓ NFATc1, C-FOS, TNFα, TRAP, CTSK, MMP-9, DC-STAMP mRNA (RT-PCR) |
Xue et al. | (100) |
| Sulforaphane * | RAW 264.7 cell line | 0.01-0.1-0.5-1 μM | 1. Inhibits osteoclastogenesis 2. Inhibits osteoclasts cells-fusion |
• induced cytotoxicity at > 5 μM (CCK-8 assay) • ↓ osteoclasts (TRAP assay) • ↓NFATc1, TRAP, CTSK mRNA (RT-PCR) • ↓ OSCAR, DC-STAMP, OC-STAMP mRNA (RT-PCR) • ↑ phosphorylation of STAT1 (Tyr701) (western blot) |
Takagi et al. | (101) |
| Sulforaphane * | RAW 264.7 cell line | 0.01-0.1-1-10 μM | Inhibition of osteoclastogenesis | • ↓ osteoclasts • ↓NF-kappaB activation |
Kim et al. | (102) |
| Sulforaphane * | RAW 264.7 cell line | 0.5, 1, 2.5, 5, 10, 20 μM | Decreased viability and osteoclastogenesis | • Marked cytotoxicity at concentration > 5 μM, low cytotoxicity 1-2.5 μM (CCK-8 assay) • ↓osteoclasts (TRAP staining) • ↓ CTSK, MMP-9 mRNA and protein (RT-PCR) • ↓ in autophagosomes and LC3-II, Beclin1, and Atg5–Atg12 mRNA and protein; ↓ of JNK phosphorylation (RT-PCR, western blot) • ↓size of F-actin rings |
Luo et al. | (103) |
| Sulforaphane * | Primary mouse osteoclasts from tibial and femoral bone marrow of 8-week-old C57BL/6 mice | 3 μM | Inhibition of osteoclasts resorption | ↓ resorption activity | Thaler et al. | (97) |
| Sulforaphane * | Primary osteoclast precursors isolated from BM of tibias and femurs of 8–12 weeks old male C57BL/6 mice | 1-5 μM | Inhibition of osteoclastogenesis | ↓ osteoclasts (TRAP staining) | Xue et al. | (100) |
| Sulforaphane * | BM cells obtained from the femur and tibia of 7–10-week-old ddY male mice | 0.01-0.1-0.5-1 μM | Inhibition of osteoclastogenesis | • induced cytotoxicity at > 5 μM (CCK-8 assay) • ↓ osteoclasts (TRAP staining) • ↓ NFATc1, TRAP, CTSK mRNA expression (RT-PCR) |
Takagi et al. | (101) |
| Sulforaphane * | BM cells isolated from femora and tibiae of 4- 6-week-old C57BL/6 mice | 0.01-0.1-1-10 μM | Inhibition of osteoclastogenesis | • ↓ osteoclasts • Early inhibition of osteoclastogenesis • No effects on osteoclasts resorption • No effects on RANK or c-fms mRNA |
Kim et al. | (102) |
| Sulforaphane * | BMMs from 5-week-old C57BL/6 female mice | 1, 2.5, 5 μM | Decreased viability and inhibition of osteoclastogenesis | • Moderate cytotoxicity at concentration >2.5 μM (CCK-8 assay) • ↓ osteoclasts (TRAP staining) |
Luo et al. | (103) |
| Sulforaphane * | Human monocytes isolated from peripheral blood of healthy volunteers | 0.2-1-5 μM | Inhibition of osteoclastogenesis | • ↓ osteoclasts (TRAP staining) • ↑NRF2 accumulation (immunocytochemistry) • ↑ NQO1 and PRDX1 mRNA expression (RT-PCR) |
Gambari et al. | (104) |
Most in vitro studies were conducted using purified OSCs (6 studies, 15 in vitro models; sulforaphane, glucoraphanin); while only a few used water or ethanol extracts from Brassicaceae edible plants (2 studies, 2 in vitro models; Brassica rapa, Brassica oleracea). Most studies showed increased osteogenesis and decreased osteoclastogenesis. Notably, only the effects of purified OSCs (labeled with * in the table) can be attributable to OSCs. The concentrations tested ranged from 0.01 to 100 μg/ml. Murine in vitro models of osteoclastogenesis: osteoclasts derived from bone marrow of femora and tibiae of mice, RAW 264.7 cell line. Human in vitro models of osteoclastogenesis: human monocytes isolated from peripheral blood of healthy volunteers. Murine in vitro models of osteoblastogenesis: MC3T3-E1 (Mouse C57BL/6 calvaria cells line); murine bone marrow (BM) cells; bone marrow-derived mesenchymal stem cells (BMMSCs), bone marrow macrophages (BMMs). Human in vitro models of osteoblastogenesis: MC3T3-E1, MSCs isolated from human tibial plateau. Osteocyte – cell line: MLO-Y4. Functional assays for osteoclastogenesis: tartrate-resistant acid phosphatase positive (TRAP staining); pit assay. Functional assays for osteoblastogenesis: Alizarin red staining (marker of mineralization), Sirius red assay (marker of collagen I), p-nitrophenyl phosphate (pNPP) quantification. Proliferation/viability assays: cell counting kit-8 (CCK-8) cell viability assay, water-soluble tetrazolium-8 (WST-8) assay, 3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide-like assay (EZ4U). Markers of osteoclasts: nuclear factor of activated T-cells cytoplasmic 1 (NFATc1), cathepsin K (CTSK), receptor activator of NF-KB (RANK), osteoclast stimulatory transmembrane protein (OC-STAMP), tartrate-resistant acid phosphatase (TRAP), receptor activator of nuclear factor-κB ligand (RANKL), dendritic cell specific transmembrane protein (DC-STAMP), reactive oxygen species (ROS), c-fos, nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB), matrix metallopeptidase 9 (MMP-9), osteoclasts-specific activating receptor (OSCAR), acid phosphatase 5, tartrate resistant (ACP5), calcitonin receptor-like receptor (Clcr), colony-stimulating factor-1 receptor (c-fsm), c-fos. Markers of osteoblastogenesis: cystathionine-β-synthase (CBS), bone sialoprotein (BSP), SMAD family member 1 (SMAD-1), alkaline phosphatase (ALP), WNT1-inducible-signaling pathway protein 1 (WISP-1), osteocalcin (OCN), runt-related transcription factor 2 (RUNX-2). Markers of cell viability – apoptosis: Fas, Caspase 3/7 and 8, nuclear factor erythroid-derived 2-related factor 2 (NRF2), heme oxygenase-1 (HO1), NAD(P)H: quinone oxidoreductase 1 (NQO1), peroxiredoxin-1 (PRDX-1), glutamate cysteine ligase catalytic subunit (GCLC), glutamate-cysteine ligase modifier subunit (GCLM), peroxiredoxin 1 (PRDX-1), microtubule-associated protein 1A/1B-light chain 3 (LC3-II), beclin1, autophagy related 5 (ATG5), Jun N-terminal kinases (JNK), autophagy related 12 (Atg12). ↑ means up-regulation; ↓ means down-regulation
Importantly, while data obtained from studies on purified molecules (labeled with * in the tables) clearly attest to the effectiveness of individual OSCs, the effect of OSCs-rich extracts may result from the combined action of other phytochemicals contained in the extracts. Indeed, Allium species contains polyphenols, flavonoids, flavanols, anthocyanins, tannins, ascorbic acid, saponins and fructans (109–111); Brassica species contains ascorbic acid, phenolics, carotenoids, terpenes, phytoalexins and alkaloids (29, 112).
Regulation of osteogenesis and bone formation
Osteoblasts, the bone forming cells, regulate bone homeostasis by synthesizing a wide variety of extracellular protein of bone matrix. They differentiate from MSCs through the osteogenic differentiation process which is regulated by an orchestrated activation of several pathways. The master regulator of osteogenic differentiation is runt-related transcription factor 2 (RUNX-2), which is expressed in the early stages of differentiation and is at the intersection of several signaling pathways among which growth hormone-janus Kinase 2 (GH-JAK2), bone morphogenetic protein-SMAD (BMP-SMAD), canonical Wingless/Integrated (Wnt) and Notch signaling (113, 114). Among the genes targeted by RUNX-2 are osteocalcin (OCN), collagen I (Col I), bone sialoprotein (BSP), osteopontin (OPN), alkaline phosphatase (ALP). BSP, OPN and ALP are correlated to matrix mineralization; Coll I and OCN are among the major components of bone matrix. Wnts-β-catenin signal activates osteogenic target genes such as distal-less homeobox 5 (Dlx5) and osterix (Osx) (115) and suppresses the transcription of adipogenic transcription factors such as peroxisome proliferator-activated receptor-γ (PPAR-γ) (116). SMAD family number 1 (SMAD-1) is a critical immediate downstream mediator of BMP receptor transduction (117). Among downstream targets of canonical Wnt and BMP signaling is WNT1-inducible signaling pathway protein 1 (WISP-1), which is involved in the positive regulation of osteogenesis and negative regulation of adipogenesis (118). Interestingly, the expression of H2S generating enzymes, cystathionine-β-synthase (CBS) and cystathionine-γ-lyase (CSE), was found to be transcriptionally up-regulated during osteogenesis and to correlate with the biosynthesis of mineral matrix (119), thus suggesting a role for endogenous H2S in osteogenic differentiation. Osteogenic differentiation is associated to increased ALP activity and mineralization in vitro and increased BMD in vivo. Osteoblast finally differentiate toward osteocytes, multifunctional bone cells that are embedded in mineralized bone matrix. Osteocytes act as orchestrators of bone remodeling, through regulation of both osteoclast and osteoblast activity; as regulators of phosphate metabolism and calcium availability, by functioning as an endocrine cell; as mechanosensory cells (120). Key factors produced by osteocytes are sclerostin (a negative regulator of bone mass), FGF-23 (a regulator of phosphate metabolism), and the key regulator of osteoclast differentiation receptor activator of nuclear factor κβ ligand (RANKL), also produced by osteoblasts and MSCs (120, 121).
Most studies investigating OSCs extracts focused on a commonly used human osteoblastic model, the human osteosarcoma cell line (MG-63 cells). They showed increased cell proliferation and increased osteogenesis/mineralization by Allium Hookeri roots treatments (48); increased osteogenesis by Allium fistulosum (80) and Brassica Rapa L. (Jeong); while no effect on proliferation and differentiation was shown by treatment with water solution of onion crude powder (81). However, MG-63 cells are osteoblasts derived from osteosarcoma, a malignant bone tumors, thus are not fully representative of physiological osteoblasts (122). Increased cells proliferation by Allium genus was also shown by ginger and garlic extracts released by 3D-printed calcium phosphate scaffolds on human fetal osteoblast cells (82); increased osteogenesis by Allium fistulosum was also shown in the mouse C57BL/6 osteoblastic calvaria cell line (MC3T3-E1) (80). Up to date no studies on primary cultures of human MSCs have been performed with extracts derived from Alliaceae or Brassicaceae.
Treatment with Alliaceae extracts improved bone formation in normal control rats (41, 48, 88) and mitigated the bone loss due to several pathological conditions among which osteoporosis (47, 80, 94). Similarly, extracts from Brassicaceae induced bone formation in control rats (54) and prevented bone loss in several models of osteoporosis (59, 99, 106–108). Interestingly, treatment with Lepidium sativum resulted in improved fracture healing (28, 123).
Notably, several studies focused on purified OSCs molecules, revealing a specific effect of OSCs on proliferation, osteogenic differentiation, and bone formation. Behera et al. showed increased proliferation, ALP activity and mineralization in murine MSCs derived from femur bone marrow (BMMSCs) upon allyl sulfide stimulation, with a mechanism implicating increased RUNX-2 and OCN expression (83). Thaler et al. demonstrated increased mineralization in mouse MSCs and in an ex vivo culture of calvariae explants treated with SFN (97); at the molecular level, SFN induced up-regulation of RUNX-2 in mouse MSCs (97). Gambari et al. showed increased mineralization and BSP, CBS and SMAD-1 mRNA up-regulation by GRA administration in primary human MSCs (98). Finally, with regards to osteocyte regulation, Thaler et al. showed that SFN inhibited proliferation in murine osteocyte-like cell line (MLO-Y4) (97).
Purified OSCs have also been tested in in vivo models of bone loss or osteolysis, showing beneficial effects on preserving bone mass. Oral administration of allyl sulfide in an age-associated osteoporosis mouse model resulted in increased bone density at X-ray analysis and increased serum levels of procollagen 1 intact N-terminal propeptide (P1NP; a marker of bone formation) (83). Similarly, intragastric administration of allicin increased BMD, as detected by dual energy X-ray absorptiometry, and bone strength, as measured by three-point bending assay, in a model of aging osteoporotic rats (96). Intraperitoneal administration of allicin prevented the bone loss in a mice model of lead-induced bone loss (osteoporosis induced by a toxic heavy metal), as measured by increased BMD, trabecular number (Tb.N), trabecular thickness (Tb.Th) and decreased trabecular space (Tb.Sp), quantified using micro-CT analysis (95). Finally, SFN showed to be protective against bone loss in different in vivo models. Intraperitoneal injection of SFN in lipopolysaccharide (LPS)-induced erosion of the mice calvaria bone induced increased trabecular bone volume (BV/TV), increased Tb.N and decreased Tb.Sp, as measured by micro-CT analysis (103); moreover, intraperitoneal injection of SFN in a mice model of ovariectomy-induced bone loss stimulated trabecular bone formation, increased Tb.N and decreased Tb.Sp (97); finally, the oral administration of SFN-01 (a stabilized form of SFN) in a mice model of osteoarthritis, resulted in increased trabecular bone volume and serum P1NP (105).
Regulation of osteoclastogenesis and bone resorption
Osteoclasts are bone-resorbing cells which arise from immature monocytes and mature tissue macrophages (124). Osteoclasts differentiation stems from the signaling triggered by two critical cytokines produced by MSCs, osteoblasts and osteocytes: macrophage colony-stimulating factor (M-CSF) and RANKL binding, respectively, to the receptors colony-stimulating factor-1 receptor (c-fms) and receptor activator of nuclear factor κ B (RANK) (125, 126). RANKL signaling activation induces various intracellular signal transduction cascades such as tumor necrosis factor receptor-associated factor 6 (TRAF-6), NADPH oxidase 1 (NOX-1), RAC family small GTPase 1 (RAC1), nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB), and nuclear factor-activated T cells c1 (NFATc1), c-fos (127–129). Other receptors involved in osteoclastogenesis are calcitonin receptor (CTR), ITAM bearing Fc receptor standard g chain (FcRγ), osteoclasts-specific activating receptor (OSCAR) (126, 130); key signaling is mediated by mitogen-activated protein kinases (MAPK), and includes extracellular signal-regulated kinase (ERK), c-Jun N-terminal kinase (JNK), and p38 activation. Moreover, critical to osteoclast differentiation and function are: intracellular reactive oxygen species (ROS) generation, which act as key signaling molecules (82, 88, 94); osteoclast fusion mediated among other factors, by the fusogenic molecules osteoclasts-stimulatory transmembrane protein (OC-STAMP) and dendritic cell-specific transmembrane protein (DC-STAMP) (126, 131, 132); and expression of specific enzymes such as tartrate-resistant acid phosphatase (TRAP), cathepsin K (CTSK) (126, 130), tartrate-resistant acid phosphatase 5b (TRAP5b) (83) and matrix metallopeptidase 9 (MMP-9).
Extracts from both Allium and Brassica species were shown to attenuate osteoclast differentiation in vitro in the murine macrophage cell line, RAW 264.7. In particular, extracts of onion (85), freeze dried onion juice (85), solution of onion crude powder (81) inhibited osteoclastogenesis, as measured by TRAP staining in vitro. A similar effect was achieved by an extract of Brassica oleracea but only in combination with extract from Panax ginseng (99). Using human THP1 monocytes, Bose et al. showed that ginger and garlic extracts reduce the frequency and the size of resorption pits carved by osteoclasts (82); inhibition of osteoclast number was found also by onion and commercial onion extracts in rat and rabbit osteoclasts (81). Notably, Wetli et al. demonstrated that onion extract reduced rat osteoclast differentiation and were able to isolate a specific sulfoxide component of onion powder, γ-glutamyl-trans-S-1-propenyl-l-cysteine sulfoxide (GPCS), which the authors found to be the key responsible of this biological activity (41).
In vivo administration of extracts rich in OSCs decreased osteoclastogenesis and bone erosion in rodent model of osteoporosis; Huang et al. showed that ovariectomized rats fed with different concentrations of onion extracts (up to 14% wt/wt in the diet powder) were partly protected against loss of bone mass and bone material properties (94); moreover, histomorphometry revealed that treatment with onion extracts was associated with a lower number of osteoclasts in vivo (94). Similar findings were reported by Kang et al. using ovariectomized mice fed with a combination of extracts obtained from Panax ginseng and Brassica oleracea (99). Furthermore, Abdallah HM et al. reported that ovariectomized rats treated with extracts of Lepidium sativum were partly protected against osteoporosis and showed a sharply decreased RANKL/osteoprotegerin (OPG) ratio in femur bones (59).
Studies that used purified OSCs molecules further supported efficacy and specificity. Yang et al. demonstrated a dose-dependent inhibition of osteoclast differentiation and a decreased bone resorption by mature osteoclasts upon treatment with DADS (86). Monocytes proliferation and viability was inhibited by SFN (97).
Luo et al. (103) and Xue et al. (100) showed that SFN inhibits osteoclast differentiation in RAW 264.7 murine macrophagic cell line; Takagi et al. (101) and Kim et al. (102) showed similar findings in murine BM cells and so did Gambari et al. (104) in a model of osteoclast derived from human monocytes. Moreover, Chen et al. reported the inhibition of osteoclast differentiation by alliin in RAW 264.7 via scavenging of ROS signaling (87).
Mechanisms of regulation of osteoclastic differentiation by OSCs involved different molecular targets. Li et al. reported that the anti-osteoclastogenic activity of allicin in mice is associated to the activation of the SIRT1/FOXO1 pathway and ROS scavenging (95). Similarly, one key mechanism of action of SFN is the activation of the master regulator of the antioxidant defense system, nuclear factor erythroid-derived 2-related factor 2 (NRF2), and its downstream target antioxidant and detoxifying enzymes (133), which is known to actively inhibit mouse osteoclasts differentiation in vitro (104, 134). SFN modifies sulfhydryl groups in kelch-like erythroid-cell-derived protein with CNC homology (ECH)-associated protein (KEAP-1), causing KEAP-1 dislocation, NRF2 stabilization and nuclear translocation (135); moreover, SFN regulates NRF2 expression via epigenetic mechanisms (136). Coherently, SFN was shown to increase NRF2 protein accumulation in RAW 264.7 murine cell line, to increase the expression of some NRF2-mediated antioxidant genes (heme oxygenase-1, HO1; NAD(P)H: quinone oxidoreductase 1, NQO1; glutamate cysteine ligase catalytic subunit, GCLC; ligase modifier subunit, GCLM) and decrease intracellular ROS production, and the overall number of osteoclasts as shown by Xue et al. (100). Similarly, SFN was shown to inhibit the osteoclast differentiation of human monocytes while increasing NRF2 nuclear translocation and protein expression of NRF2-mediated antioxidant genes (NQO1; Peroxiredoxin 1, PRDX-1), as published by Gambari et al. (104). Finally, SFN induces Caspase 8 and 3/7, thus inducing apoptosis in a RAW 264.7 murine cell line as shown by Thaler et al. (97).
Moreover, downregulation of the key transcription factor NFATc1 is implicated in several studies showing inhibition of osteoclast development: Yang et al. reported a dose-dependent down-regulation of NFATc1 in a RAW 264.7 murine cell line after DADS treatment (86); Xue et al. (100) and Takagi et al. (101), respectively, reported similar findings in RAW 264.7 murine cell line and in murine BM cells after SFN treatment; Behera et al. in murine BM cells after allyl sulfide treatment (83). The inhibition of other key transcription factor c-Fos and Nf-kB was shown by Yang et al. in a RAW 264.7 murine cell line after DADS treatment (86).
Several other proteins implicated in the adhesion an (83, 95, 100, 137), in RAW264.7 cells and murine BM and are detailed in Tables 2 , 4 .
OSCs can modulate the expression of osteoclasts-specific activating receptors, necessary for the co-stimulatory signaling with immunoreceptors and prevented osteoclast fusion by inhibiting fusogenic molecules. Takagi et al. showed in RAW 264.7 murine cell line that OSCAR is inhibited by SFN (101). DC-STAMP was found inhibited in RAW 264.7 murine cell line after SFN treatment as shown by Takagi et al. (101) and by Xue et al. (100) and after DADS treatment as shown by Yang et al. (86). OC-STAMP was found inhibited in RAW 264.7 murine cell line after SFN treatment as shown by Takagi et al. (101).
Finally, OSCs compounds were shown to inhibit osteoclast differentiation via a paracrine mechanism, acting on osteoclasts-supporting cells. Thaler et al. showed that RANKL was inhibited by SFN in a murine osteocytes cell line (MLO-Y4) (97). Behera et al. showed that RANKL was inhibited while OPG was increased in supernatants of murine MSCs cells culture treated with allyl sulfide (83); and that treatment with this conditioned medium inhibited the expression of RANK and osteoclast differentiation of murine bone marrow (BM) cells (83).
Only a few in vivo studies used purified OSCs to investigate bone metabolism. In a mice model of lead-induced bone loss, intraperitoneal injection of allicin alleviates bone loss by preventing oxidative stress and osteoclastogenesis by modulating SIRT1/FOXO1 pathway (95). SFN treatment in a mouse calvaria model treated with LPS decreased the number of osteoclasts (103). Treatment of Lepidium sativum in a rat model of ovariectomy-induced osteoporosis improved mechanical properties of femurs while decreasing TRAP, serum type I collagen breakdown product (CTX-I), RANKL (59) and the number of osteoclasts (107).
H2S release from OSCs as a potential mechanism of bioactivity in bone
H2S is a pleiotropic molecule which provides numerous health benefits by improving hypertension and cardiometabolic disorders (138) (139), relieving pain (140, 141), and increasing insulin sensitivity (142); protecting against neurological diseases including Alzheimer disease (143). Moreover, H2S is critically involved in the extension of lifespan provided by caloric restriction (144, 145). Supraphysiological levels of H2S may be generated in certain pathological conditions and lead to toxicity, inducing inflammation or tissue damage (146).
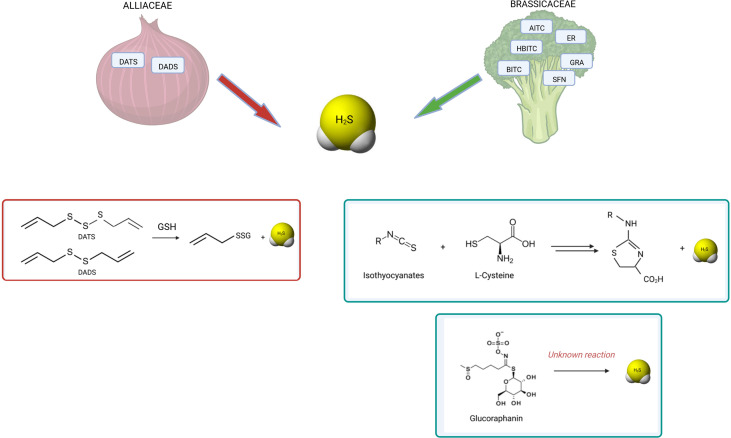
The intriguing overlap between biological effects attributed to some Allium and Brassica species and those exhibited by the gasotransmitter H2S prompted several researchers to verify the H2S releasing capacity of those molecules. Recently, the ability of releasing H2S was found as a distinctive feature of several OSCs, and a plausible mechanism for their biological effects across different organs and tissues was described. The biological relevance of H2S release by OSCs was first demonstrated by Benavides et al. in the context of a study on the vasoactivity of garlic. The authors showed that garlic polysulfides DATS and DADS, the downstream metabolites of alliin, released H2S in red blood cells; importantly, pre-treating the cells with the thiol-blocking reagent iodoacetamide inhibited the release of H2S, thereby demonstrating that the mechanism by which polysulfides release H2S is dependent on intracellular thiols, such as glutathione (GSH) (147). Chemically, this reaction involves a nucleophilic substitution from thiol at the α carbon of the H2S-donor moiety and a subsequent release of H2S (148). This mechanism is biologically relevant as the relaxation induced by both garlic extract and DADS on isolated rat aortic rings strongly correlated to the amount of H2S released. In the wake of this work, Citi et al. first revealed that a similar mechanism accounts for the ability of several Brassicaceae-derived ITCs to release pharmacologically relevant concentrations of H2S in an l-cysteine dependent manner (149): allyl isothiocyanate (AITC), 4-hydroxybenzyl isothiocyanate (HBITC), benzyl isothiocyanate (BITC), erucin (ER), SFN (149, 150). The same group reported that H2S-release is associated with the in vivo anti-hypertensive, hypoglycemic, pain-relieving, and anti-inflammatory effects of OSCs derived from the Brassicacea Eruca Sativa (138, 151–153). Interestingly, Lucarini et al. first demonstrated that GRA, a GLS, can release H2S in aqueous solution independent of myrosinase, but the chemical mechanism underlying this phenomenon is still unclear (150). Whether other Alliaceae or Brassicaceae-derived OSCs releases H2S is still unknown.
Figure 3 summarizes the known reactions leading to H2S release from polysulfides, GLS or ITCs.
Figure 3.
H2S release by OSCs derived from Alliaceae and Brassicaceae. The known reactions occurring for H2S release by polysulfides and isothiocyanates are shown. Among garlic-derived polysulfides, diallyl disulfide (DADS) and diallyl trisulfide (DATS) have been shown to release H2S by reaction with glutathione (GSH) by polarographic H2S sensor (154) (147) (148). Among glucosinolates, GRA has been found to release H2S by amperometric approach (149). Similarly, several isothiocyanates showed H2S-releasing activity: allyl isothiocyanate (AITC), 4-hydroxybenzyl isothiocyanate (HBITC), benzyl isothiocyanate (BITC), erucin (ER), sulforaphane (SFN) (149) (150). While the mechanism of release is unknown for glucosinolates, the mechanism of release by isothiocyanates is dependent on L-cysteine reaction (155). Moreover, different OSCs have different kinetics of H2S release.
This mechanism holds important implications for bone. Recent findings by our group and others demonstrated that H2S plays an important role in the regulation of bone cell differentiation and function. In vitro, H2S-donors promote osteogenic differentiation and stimulate mineralization by increasing calcium intake (156) and the expression of genes directly involved in the biosynthesis of hydroxyapatite, such BSP (157). Furthermore, the expression of the enzymes CBS and CSE, which are responsible for endogenous H2S production, steadily increased during osteogenic differentiation and correlated to mineral apposition (119). Moreover, H2S-donors inhibit osteoclast maturation and resorption by activating the antioxidant response elicited by the NRF2 transcription factor (104, 158). Further attesting to the relevance of H2S in bone homeostasis, evidence from several in vivo preclinical models showed that the depletion of H2S levels is associated with loss of bone mass; similar findings were reported in ovariectomized mice (157), in H2S-deficient CBS+/− mice (156), in glucocorticoids-induced osteoporosis (159). Interestingly, when animals were treated with pharmacological H2S-donors to normalize the plasma level of H2S, bone loss was prevented or reversed (156, 157). The ability of H2S to stimulate bone formation appears to be maintained across various conditions, even unrelated to systemic or genetic disfunctions: for example, the exogenous administration of H2S by means of the pharmacological donor GYY4137 was effective to attenuate the bone loss induced by modelled microgravity (160) and to promote osteogenesis in a model of distraction osteogenesis (161).
Overall, these data demonstrate that H2S regulates osteogenesis and bone formation in both healthy and pathological conditions.
Therefore, H2S release by OSCs could account, at least in part, for their biological properties. However, up to date no clinical or preclinical in vivo studies have investigated the effect of OSCs by correlating their bioactivity to the H2S levels.
The GRA/SFN system: A case-model for OSCs bioactivity based on H2S release
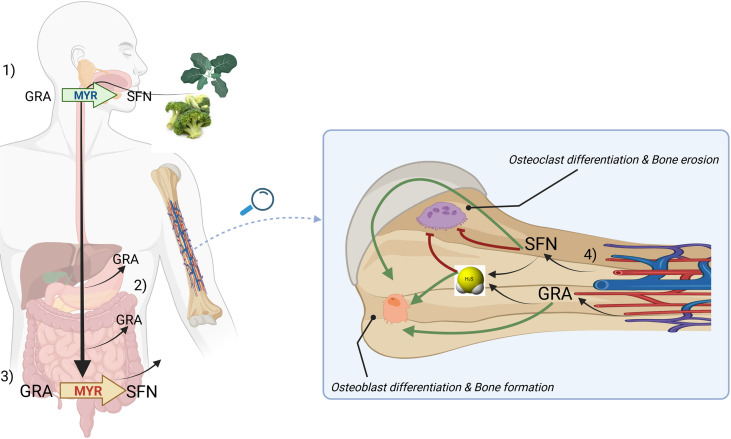
GRA is a glucosinolate abundant in aerial portions, developing florets (flower buds), sprouts, seeds and mature plants of cabbage, broccoli, cauliflower, kale and Brussels sprouts (77). GRA conversion to SFN, an ITC, requires the enzyme myrosinase, an intracellular thioglucosidase, which catalyzes its hydrolysis to an unstable aglucone that spontaneously rearranges to give rise to a range of products, including SFN. SFN is the progenitor of a family of compounds widely studied in the literature mostly due to their antioxidant and anticancer properties. In mammalians, GRA conversion to SFN is primarily mediated by bacterial microflora of the gastrointestinal tract; while a small proportion is generated in the mouth by plant myrosinase when released by plants after chewing. Our current knowledge on the bioavailability and the rate of conversion of GSL into ITCs are largely based on studies on the GRA/SFN system.
Although most of GRA introduced with diet undergoes hydrolysis in the gut by microbial thioglucosidases, a fraction of GRA (around 10-15%) is absorbed directly in the stomach and in the small intestine, before the catabolic breakdown to SFN is triggered by gut microbiota (77, 162).
Gastric acidity appears to attenuate GSL bioavailability (163). However, GRA is not destroyed by digestive enzymes during passage through the digestive tract and is able to reach the rat cecum intact, when is hydrolyzed to SFN which is able to cross the cecal enterocyte for systemic absorption and enterohepatic circulation (164, 165). Conversion of GRA to bioactive SFN by the rat cecal microbiota requires four or more days after broccoli consumption and is reversible (166); however, recent randomized clinical trials have ascertained that upon ingestion of GRA-enriched soups, increased SFN levels were detectable as early as 30’ in plasma and 1h in the urine of patients (162). Attesting the tissue systemic absorption of SFN and ITCs in general, they have been detected in both plasma and synovial fluid of osteoarthritis patients undergoing consumption of GLS-rich diets for 2 weeks (167). On the other hand, the direct delivery of SFN from foods is possible and was demonstrated in recent clinical studies (168, 169) where SFN was shown to be readily bioavailable (170); however, SFN is unstable, requires storage at freezing temperature, and SFN-enriched extracts are difficult to prepare and very expensive (163).
Although most of the research on the biological effects of SFN is focused on cancer because of its effect on cell cycle and apoptosis (171–173), it also regulates bone cells: in vitro, SFN inhibits monocyte cell proliferation and osteoclast differentiation in multiple ways, detailed above (100–104), while increases mineralization in mouse MSCs and in an ex vivo culture of calvariae explants (97). Notably, in one in vivo study the administration of SFN for 5 weeks to normal and ovariectomized mice lead to an approximate 20% increase in bone mass (97), shifting the balance of bone homeostasis and favoring bone acquisition and/or mitigation of bone resorption.
Of note, our group recently demonstrated that GRA obtained from Tuscan black kale promotes osteogenesis in human MSCs, independent of SFN, and this effect is associated to the release of H2S and an increased H2S uptake inside the cells (98). This is relatively unexpected as GLS have been considered for many years a relatively inert precursor of reactive derivatives ITCs. Although the chemistry underlying this phenomenon is still unclear and will require further investigation, this finding suggests that GLS may exert inherent biological activity based on their capacity to release H2S.
As the hydrolytic product of GRA, SFN, had been already shown to inhibit the activity of osteoclast in bone, it can be suggested that the ‘GRA-SFN system’ exerts a beneficial effect on bone both at level of GLS and of its cognate ITC. The routes of absorption of GRA and SFN as well as the proposed mode of action on bone cells is summarized in Figure 4 .
Figure 4.
A general model describing the routes of absorption of GRA and SFN and a proposed mechanism of action on bone cells based on H2S-release. Briefly, upon chewing of plants belonging to Brassica genus, myrosinase (MYR, green) is released and can convert glucoraphanin (GRA) to sulforaphane (SFN) (1). GRA can be adsorbed in the stomach or in the small intestine (2). Microbacterial thioglucosidases (MYR, red) converts GRA to SFN which is further adsorbed in large quantities (3). SFN and GRA are released by circulation in bone tissue where can release H2S and exert anabolic and anticatabolic properties on bone cells (4). The mechanism by which H2S can be directly released from GRA has not been clarified yet.
Clinical studies
OSCs and chronic diseases
Despite this review focuses primarily on the skeletal effects of OSCs, much of the clinical research on the health benefits of OSCs is aimed at metabolic or cardiovascular disease and cancer.
Vegetables or extracts rich in OSCs improved dyslipidemia, insulin resistance, hypertension and cardiovascular risk linked to atherosclerotic plaques in human studies.
Among interventional, randomized clinical trials, Jeon et al. evidenced that ethanol extracts from Brassica rapa, administrated as a part of the diet of overweight human for 10 weeks, induce a significant increase in the HLDL-cholesterol concentration and a significant reduction in the total cholesterol/HDL-cholesterol ratio, free fatty acid, and adipsin levels (174). A randomized double-blind trial, performed by Bahadoran et. al., investigated the effects of broccoli sprouts powder containing high concentration of SFN for four weeks in type 2 diabetic patients and showed that broccoli sprouts improve insulin resistance by decreasing serum insulin concentration and ‘homeostatic model assessment for insulin resistance’ (HOMA-IR) score (175).
In a prospective cohort study on Australian women aged 70 years and older, without clinical atherosclerotic vascular disease (ASVD) or diabetes mellitus at baseline, Blekkenhorst et al. investigated the occurrence of ASVD‐related deaths during 15 years of follow‐up and correlated it with several dietary intake, through a multivariable‐adjusted model. Among the nutrients tested, intakes of cruciferous and Allium vegetables were inversely associated with ASVD mortality supporting the evidence that the effect of increased intake of cruciferous and Allium vegetables lowered cardiovascular disease risk (176).
In cancer, treatment with OSCs-rich food showed promising results as chemopreventive.
A placebo double-blind randomized controlled trial on men scheduled for prostate biopsy and treated with broccoli sprout extract (BSE) supplementation (providing SFN and myrosinase) for 4.4 wk, performed by Zhang et. al., showed that BSE supplementation correlated with changes in gene expression but not with other prostate cancer immunohistochemistry biomarkers (173). In a double-blind placebo randomized clinical trial in patients with colorectal adenomas-precancerous lesions of the large bowel treated with aged garlic extract (AGE), Tanaka et al. demonstrated that AGE significantly reduced the size and number of colon adenomas in patients after 12 month (25). Several epidemiological studies showed that SFN consumption has been reported to be associated with a lower risk of cancer development (breast, lung, stomach, esophagus, mammary glands, gastric, colorectal, prostate, skin, head and neck, and liver) (172). In a large cohort study Millen et al. correlated the presence of adenoma with food intake of several fruit and vegetables, as assessed by a food-frequency questionnaire, and showed that onions and garlic were significantly related to lower risk of adenoma (177). Notably, a randomized double-blinded intervention study, performed by Traka et. al., showed that consuming GRA-rich broccoli for 12 months reduced the risk of prostate cancer progression (178). In particular, patients administrated with a weekly portion of soup made from a standard broccoli or 2 experimental broccoli genotypes with enhanced concentrations of GRA, showed dose-dependent attenuated activation of gene expression associated to oncogenic pathways in transperineal biopsies; and an inverse association between consumption of cruciferous vegetables and cancer progression was observed (178).
Overall, these studies highlighted the significant role of diet administration of OSCs in several chronic diseases and substantiate the relevance of creating specific dietary regimen for their prevention.
OSCs in the prevention of bone loss and skeletal frailty
A few clinical trials or population-based studies have revealed positive relationships between the consumption of vegetables, bone density, muscle strength and fractures in women/men, as summarized in Table 6 .
Table 6.
Clinical studies on musculoskeletal effects of OSCs-rich food and extracts.
| Molecule tested | Patients data | Mode of administration, concentration, treatments | Main effect | Specific features | Authors | Ref |
|---|---|---|---|---|---|---|
| Onion | Perimenopausal and postmenopausal non-Hispanic white women, 50 years and older | Onion consumption ≥ once a day; 3-5 a week; 2 a month to 2 a week, 1 a month or less | Prevention of bone loss | ↑ BMD by increased consumption | Matheson et al. | (179) |
| Onion juice | Healthy subjects, male and female, 40-80 years | 100 mL of onion juice or placebo for 8 weeks | Decreased bone anabolic markers |
|
Law et al. | (85) |
| Onion juice | Postmenopausal women | 100 mL of onion juice or placebo for 8 weeks | Mild changes in BMD |
|
Law et al. | (85) |
| Allium vegetables (onion, leek, and garlic) | Women, ≥70 years | Habitual intakes of Allium intake | Inversely associated with all fractures | Inversely associated with all fractures | Blekkenhorst et al. | (18) |
|
Cruciferous
(cabbage, brussel sprouts, cauliflower, and broccoli) |
Women aged >70 years |
Cruciferous vegetables intake | Inversely associated with all fractures | Inversely associated with all fractures | Blekkenhorst et al. | (18) |
| Raw garlic consumption | 28958 patients (males and females) | Habitual intakes of raw garlic | Positive correlation with handgrip strength | Gu et al. | (139) |
Analysis of bone mineral density (BMD) by Dual-energy X-ray absorptiometry (DEXA). Measurement of alkaline phosphatase (ALP). ↑ means up-regulation; ↓ means down-regulation.
Matheson et al. used a food frequency questionnaire added to the Nutritional Health and Nutrition Examination Survey (2003–2004) to examine the correlation between habitual consumption of onion over the past 12 months to BMD (N unweighted =507; N weighed =35.7 million). They found that higher consumption of onion increased the BMD by 5% (179). Law et al. administrated onion juice to healthy men and women and post-menopausal women for 8 weeks and investigated the association with bone BMD; the results found that the BMD of 3 postmenopausal women was mildly improved at the end of the treatment (85).
In an intriguing study, Blekkenhorst et al. used a food frequency questionnaire to examine the associations of vegetable and fruit intakes, separately, and specific types of vegetables and fruits with fracture-related hospitalizations in a prospective cohort of elderly women (mean age ≥ 70; n=1468); the authors found that the consumption of vegetable, but not fruit, is associated to a lower incidence of fracture; of note, the habitual consumption of cruciferous vegetables and Allium vegetables was significantly inversely associated with all fractures (18); importantly, these results were adjusted for energy intake and physical activity.
In musculoskeletal ageing, sarcopenia and declining physical activity are often associated with osteoporosis as the clinical hallmarks of frailty (180).
Interestingly, a prospective cohort study performed on elderly women (mean age ≥ 70; n=1429) investigated the correlation between vegetable consumption and incident falls-related hospitalization over a time-period of 14 years. The authors found that hospitalizations were lower in participants consuming more vegetables, but the consumption of cruciferous vegetables was most strongly associated with lower falls-related hospitalization (181) and was associated with increased muscle strength.
Finally, cross-sectional study, by Gu et. al., demonstrated a positive correlation between raw garlic consumption, assessed using a food frequency questionnaire, and handgrip strength in both males and females (182). The results were adjusted for age, body mass index, smoking status, alcohol-consumption status, education levels, employment status, household income, family history of diseases (cardiovascular disease, hypertension, hyperlipidemia, and diabetes), metabolic syndromes, physical activity, total energy intake, dietary pattern, onion intake. Although this study did not directly assess indexes of bone quantity, it supports an overall protective effect of OSCs-rich vegetables on the musculoskeletal system (181).
Perspectives and challenges
The present literature revision stems from the increasing appreciation of the link between dietary habits, and particularly the use of phytochemicals, and bone health. We show that a growing body of evidence supports a beneficial effect of dietary OSCs on skeletal health. Of note, although a few population-based studies offer interesting clues on the clinical relevance of OSCs-rich vegetables for the prevention of bone fragility (18, 85, 179, 183), no clinical studies have been performed yet to specifically address the potential protective role of OSCs against osteoporosis or bone fractures; this goal would require a study design including a controlled intake of OSCs-rich nutrients for long time-periods and/or the evaluation of purified OSCs molecules.
The ability of OSCs to work a as dietary source of the bioactive molecule H2S provide interesting future perspectives. OSCs-rich vegetables appear as the ideal candidate for clinical investigations on whether nutrients rich in sulfur can affect the pool of circulating reactive sulfur species (RSS), which include H2S; this may have a broad implication for the prevention of those pathologies, sometimes referred to as ‘H2S-poor diseases’, where the onset of the disease was associated to a lower systemic concentration of RSS compared to healthy controls. Increasing systemic RSS levels may also have important implication for bone-wasting diseases such as osteoporosis: indeed, animal studies have established that the bone loss associated to estrogen deficiency or to corticosteroid therapy is associated to a low systemic level of H2S (157, 159). However, these preclinical data still await confirmation in observational clinical studies in humans. To obtain reliable data on this topic, it will be critical to include in the study design a robust analytical methodology to quantitatively measure the different sulfur species in human serum or plasma since they may hold different importance in different pathologies (184, 185) and the high reactivity of these gaseous molecules implies a complex chemistry (186).
Further investigations may be addressed to the evaluation of the effect of these compounds on the gut-bone axis. OSCs show a considerable ability to modulate the gut microbiome and its secondary metabolites (187–190) and to mitigate the gut-based inflammatory response; given the paramount importance of metabolites and cytokines originated from the gut on the regulation on bone metabolism (191), it is conceivable that dietary OSCs may modulate the bone-bioactive components of the microbiota.
In the end, it is apparent that members of the OSCs family of phytochemicals affect bone homeostasis in several ways and may provide new insights into the potential bone health benefits of plant-derived food and leading to a more effective prevention of osteoporosis by non-pharmacological tools. This review may be useful to fuel clinical trials that may use a robust set of outcome measurements, aiming at assessing both bone quantity and bone quality before and after specific nutrition protocols; correlation between nutrients intake, H2S blood levels and bone status would help to define preventive/clinical dietary protocols for patients with an increased risk of bone fragility.
Author contributions
FG and LG contributed to the conception and design of the review. FG ad LG wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Glossary
| ACP5 | Acid phosphatase 5, tartrate resistant |
| AG | Age-associated |
| AGE | Aged garlic extract |
| AITC | Allyl isothiocyanate |
| ALP | Alkaline phosphatase |
| ASCOs | S-alk(en)yl cysteine sulfoxides |
| AS | Allyl sulfide |
| ASVD | Atherosclerotic vascular disease |
| Atg5 | Autophagy related 5 |
| Atg12 | Autophagy related 12 |
| BITC | Benzyl isothiocyanate |
| BM | Bone marrow |
| BMD | Bone mineral density |
| BMM | Bone marrow macrophages |
| BMMSCs | Bone marrow-derived mesenchymal stem cells |
| BMP | Bone morphogenetic protein |
| BS/BV | Bone surface/bone volume |
| BSE | Broccoli sprout extract |
| BSP | Bone sialoprotein |
| BV | Bone volume |
| BVF | Bone volume fraction |
| BV/TV | Bone volume / trabecular volume |
| CAT | Catalase |
| CBS | Cystathionine beta synthase |
| Clcr | Calcitonin receptor-like receptor |
| CCK-8 | Cell counting kit-8 |
| c-fms | Colony-stimulating factor-1 receptor |
| Col I | Collagen I |
| CSE | Cystathionine-γ-lyase |
| CTR | Calcitonin receptor |
| CTX-I | Serum type I collagen breakdown product |
| CTSK | Cathepsin K |
| DADS | Diallyl disulfide |
| DATS | Diallyl trisulfide |
| DC-STAMP | Dendritic cell-specific transmembrane protein |
| DEXA | Dual-energy X-ray absorptiometry |
| Dlx5 | Distal-Less Homeobox 5 |
| DPDS | Dipropyl disulfide |
| ECM | Extracellular matrix |
| ER | Erucin |
| ERK | Extracellular signal-regulated kinase |
| EZ4U | 3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide-like assay |
| FcRγ | Fc receptor standard g chain |
| FOXO | Forkhead box O |
| GCLC | Glutamate cysteine ligase catalytic subunit |
| GCLM | Glutamate-cysteine ligase modifier subunit |
| GH | Growth hormone |
| GLS | S-β-thioglucoside N-hydroxhysulfates; glucosinolates |
| GPCS | γ-glutamyl-trans-S-1-propenyl-L-cysteine sulfoxide |
| GRA | Glucoraphanin |
| GSAC | γ-glutamyl-S-allyl-L-cysteine |
| GSH | Glutathione |
| HBITC | 4-hydroxybenzyl isothiocyanate |
| HO1 | Heme oxygenase-1 |
| HOMA-IR | Homeostatic Model Assessment for Insulin Resistance |
| H2S | Hydrogen sulfide |
| IGF-1 | Insulin-like growth factor 1 |
| ITCs | Isothiocyanates |
| JAK2 | Janus Kinase 2 |
| JNK | Jun N-terminal kinases |
| KEAP-1 | Kelch-like erythroid-cell-derived protein with CNC homology (ECH)-associated protein |
| LC3-II | Microtubule-associated protein 1A/1B-light chain 3 |
| LPS | Lipopolysaccharide |
| MAPK | Mitogen-activated protein kinase |
| M-CSF | Macrophage colony-stimulating factor |
| MMP-9 | Matrix metallopeptidase 9 |
| MDA | Malondialdehyde |
| MSC | Mesenchymal stromal cells |
| MTT | 3-(4,5-Dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide |
| NFATc1 | Nuclear factor-activated T cells c1 |
| NF-κB | Nuclear factor kappa-light-chain-enhancer of activated B cells |
| NQO1 | NAD(P)H: quinone oxidoreductase 1 |
| NOX-1 | NADPH oxidase 1 |
| NRF2 | Nuclear factor erythroid-derived 2-related factor 2 |
| OCN | Osteocalcin |
| OC-STAMP | Osteoclast-stimulatory transmembrane protein |
| OP | Osteoporosis |
| OPG | Osteoprotegerin |
| OPN | Osteopontin |
| OSCAR | Osteoclasts-specific activating receptor |
| OSCs | Organosulfur compounds |
| OSX | Osterix |
| P1NP | Procollagen 1 intact N-terminal propeptide |
| PeCSO | γ-glutamyl-propenyl-L-cysteine sulfoxide |
| pNPP | p-nitrophenyl phosphate |
| PPAR-γ | Proliferator-activated receptor-γ |
| PRDX-1 | Peroxiredoxin 1 |
| PTH | Parathormone |
| RAC1 | RAC family small GTPase 1 |
| RANK | Receptor activator of nuclear factor κ B |
| RANKL | Receptor activator for nuclear factor κ B ligand |
| RUNX-2 | Runt-related transcription factor 2 |
| ROS | Reactive oxygen species |
| RSS | Reactive sulfur species |
| SAC | S-allylcysteine |
| SAMC | S-allylmercaptocysteine |
| SAMG | S-allylmercaptoglutathione |
| SFN | Sulforaphane |
| SIRT | Sirtuin |
| SMAD-1 | SMAD family member 1 |
| STAT3 | Signal transducer and activator of transcription 3 |
| Tb.N | Trabecular number |
| Tb.Th | Trabecular thickness |
| Tb.Sp | Trabecular space |
| TRAF-6 | Tumor necrosis factor receptor-associated factor 6 |
| TRAP | Tartrate-resistant acid phosphatase |
| TRAP5b | Tartrate-resistant acid phosphatase 5b |
| VOSCs | Volatile organosulfur compounds |
| WISP-1 | WNT1-inducible-signaling pathway protein 1 |
| Wnt | Wingless/Integrated |
| WST-8 | Water-soluble tetrazolium-8 |
References
- 1. Clynes MA, Harvey NC, Curtis EM, Fuggle NR, Dennison EM, Cooper C. The epidemiology of osteoporosis. Br Med Bull (2020) 133(1):105–17. doi: 10.1093/bmb/ldaa005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hernlund E, Svedbom A, Ivergard M, Compston J, Cooper C, Stenmark J, et al. Osteoporosis in the European union: medical management, epidemiology and economic burden. a report prepared in collaboration with the international osteoporosis foundation (IOF) and the European federation of pharmaceutical industry associations (EFPIA). Arch Osteoporos. (2013) 8:136. doi: 10.1007/s11657-013-0136-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Kanis JA, Norton N, Harvey NC, Jacobson T, Johansson H, Lorentzon M, et al. SCOPE 2021: a new scorecard for osteoporosis in Europe. Arch Osteoporos. (2021) 16(1):82. doi: 10.1007/s11657-020-00871-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Zaidi M. Skeletal remodeling in health and disease. Nat Med (2007) 13(7):791–801. doi: 10.1038/nm1593 [DOI] [PubMed] [Google Scholar]
- 5. Meunier P, Aaron J, Edouard C, Vignon G. Osteoporosis and the replacement of cell populations of the marrow by adipose tissue. a quantitative study of 84 iliac bone biopsies. Clin Orthop Relat Res (1971) 80:147–54. doi: 10.1097/00003086-197110000-00021 [DOI] [PubMed] [Google Scholar]
- 6. Verma S, Rajaratnam JH, Denton J, Hoyland JA, Byers RJ. Adipocytic proportion of bone marrow is inversely related to bone formation in osteoporosis. J Clin Pathol (2002) 55(9):693–8. doi: 10.1136/jcp.55.9.693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Infante A, Rodriguez CI. Osteogenesis and aging: lessons from mesenchymal stem cells. Stem Cell Res Ther (2018) 9(1):244. doi: 10.1186/s13287-018-0995-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Papaioannou A, Kennedy CC, Dolovich L, Lau E, Adachi JD. Patient adherence to osteoporosis medications: problems, consequences and management strategies. Drugs Aging. (2007) 24(1):37–55. doi: 10.2165/00002512-200724010-00003 [DOI] [PubMed] [Google Scholar]
- 9. Siris ES, Harris ST, Rosen CJ, Barr CE, Arvesen JN, Abbott TA, et al. Adherence to bisphosphonate therapy and fracture rates in osteoporotic women: relationship to vertebral and nonvertebral fractures from 2 US claims databases. Mayo Clin Proc (2006) 81(8):1013–22. doi: 10.4065/81.8.1013 [DOI] [PubMed] [Google Scholar]
- 10. Willems HME, van den Heuvel E, Schoemaker RJW, Klein-Nulend J, Bakker AD. Diet and exercise: a match made in bone. Curr Osteoporos Rep (2017) 15(6):555–63. doi: 10.1007/s11914-017-0406-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Karpouzos A, Diamantis E, Farmaki P, Savvanis S, Troupis T. Nutritional aspects of bone health and fracture healing. J Osteoporos. (2017) 2017:4218472. doi: 10.1155/2017/4218472 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Munoz-Garach A, Garcia-Fontana B, Munoz-Torres M. Nutrients and dietary patterns related to osteoporosis. Nutrients (2020) 12(7):1986 . doi: 10.3390/nu12071986 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rizzoli R. Dairy products and bone health. Aging Clin Exp Res (2022) 34(1):9–24. doi: 10.1007/s40520-021-01970-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Rizzoli R, Biver E, Brennan-Speranza TC. Nutritional intake and bone health. Lancet Diabetes Endocrinol (2021) 9(9):606–21. doi: 10.1016/S2213-8587(21)00119-4 [DOI] [PubMed] [Google Scholar]
- 15. Warensjo Lemming E, Byberg L. Is a healthy diet also suitable for the prevention of fragility fractures? Nutrients (2020) 12(9):2642. doi: 10.3390/nu12092642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Benetou V, Orfanos P, Feskanich D, Michaelsson K, Pettersson-Kymmer U, Byberg L, et al. Mediterranean Diet and hip fracture incidence among older adults: the CHANCES project. Osteoporos Int (2018) 29(7):1591–9. doi: 10.1007/s00198-018-4517-6 [DOI] [PubMed] [Google Scholar]
- 17. Benetou V, Orfanos P, Pettersson-Kymmer U, Bergstrom U, Svensson O, Johansson I, et al. Mediterranean Diet and incidence of hip fractures in a European cohort. Osteoporos Int (2013) 24(5):1587–98. doi: 10.1007/s00198-012-2187-3 [DOI] [PubMed] [Google Scholar]
- 18. Blekkenhorst LC, Hodgson JM, Lewis JR, Devine A, Woodman RJ, Lim WH, et al. Vegetable and Fruit Intake and Fracture-Related Hospitalisations: A Prospective Study of Older Women. (2017) 9(5):11. doi: 10.3390/nu9050511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Byberg L, Bellavia A, Orsini N, Wolk A, Michaelsson K. Fruit and vegetable intake and risk of hip fracture: a cohort study of Swedish men and women. J Bone Miner Res (2015) 30(6):976–84. doi: 10.1002/jbmr.2384 [DOI] [PubMed] [Google Scholar]
- 20. Tucker KL, Chen H, Hannan MT, Cupples LA, Wilson PW, Felson D, et al. Bone mineral density and dietary patterns in older adults: the framingham osteoporosis study. Am J Clin Nutr (2002) 76(1):245–52. doi: 10.1093/ajcn/76.1.245 [DOI] [PubMed] [Google Scholar]
- 21. de Haas SCM, de Jonge EAL, Voortman T, Graaff JS, Franco OH, Ikram MA, et al. Dietary patterns and changes in frailty status: the Rotterdam study. Eur J Nutr (2018) 57(7):2365–75. doi: 10.1007/s00394-017-1509-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. de Jonge EAL, Rivadeneira F, Erler NS, Hofman A, Uitterlinden AG, Franco OH, et al. Dietary patterns in an elderly population and their relation with bone mineral density: the Rotterdam study. Eur J Nutr (2018) 57(1):61–73. doi: 10.1007/s00394-016-1297-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Somani SJ, Modi KP, Majumdar AS, Sadarani BN. Phytochemicals and their potential usefulness in inflammatory bowel disease. Phytother Res (2015) 29(3):339–50. doi: 10.1002/ptr.5271 [DOI] [PubMed] [Google Scholar]
- 24. Mathew BC, Prasad NV, Prabodh R. Cholesterol-lowering effect of organosulphur compounds from garlic: a possible mechanism of action. (KUMJ) (2004) 2(2):100–2. [PubMed] [Google Scholar]
- 25. Tanaka S, Haruma K, Yoshihara M, Kajiyama G, Kira K, Amagase H, et al. Aged garlic extract has potential suppressive effect on colorectal adenomas in humans. J Nutr (2006) 136(3 Suppl):821S–6S. doi: 10.1093/jn/136.3.821S [DOI] [PubMed] [Google Scholar]
- 26. Panjwani AA, Liu H, Fahey JW. Crucifers and related vegetables and supplements for neurologic disorders: what is the evidence? Curr Opin Clin Nutr Metab Care (2018) 21(6):451–7. doi: 10.1097/MCO.0000000000000511 [DOI] [PubMed] [Google Scholar]
- 27. Del Chierico F, Vernocchi P, Dallapiccola B, Putignani L. Mediterranean Diet and health: food effects on gut microbiota and disease control. Int J Mol Sci (2014) 15(7):11678–99. doi: 10.3390/ijms150711678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Dixit V, Jr Iii, Kumar I, Palandurkar K, Giri R, Giri K. Lepidium sativum: Bone healer in traditional medicine, an experimental validation study in rats. J Family Med Prim Care (2020) 9(2):812–8. doi: 10.4103/jfmpc.jfmpc_761_19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Ramirez D, Abellan-Victorio A, Beretta V, Camargo A, Moreno DA. Functional ingredients from brassicaceae species: Overview and perspectives. Int J Mol Sci (2020) 21(6):1998. doi: 10.3390/ijms21061998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Iberl B, Winkler G, Muller B, Knobloch K. Quantitative determination of allicin and alliin from garlic by HPLC*. Planta Med (1990) 56(3):320–6. doi: 10.1055/s-2006-960969 [DOI] [PubMed] [Google Scholar]
- 31. Bose S, Laha B, Banerjee S. Quantification of allicin by high performance liquid chromatography-ultraviolet analysis with effect of post-ultrasonic sound and microwave radiation on fresh garlic cloves. Pharmacogn Mag. (2014) 10(Suppl 2):S288–93. doi: 10.4103/0973-1296.133279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Iberl B, Winkler G, Knobloch K. Products of allicin transformation: Ajoenes and dithiins, characterization and their determination by HPLC*. Planta Med (1990) 56(2):202–11. doi: 10.1055/s-2006-960926 [DOI] [PubMed] [Google Scholar]
- 33. Egen-Schwind C, Eckard R, Jekat FW, Winterhoff H. Pharmacokinetics of vinyldithiins, transformation products of allicin. Planta Med (1992) 58(1):8–13. doi: 10.1055/s-2006-961379 [DOI] [PubMed] [Google Scholar]
- 34. Lawson LD, Wang ZJ, Hughes BG. Identification and HPLC quantitation of the sulfides and dialk(en)yl thiosulfinates in commercial garlic products. Planta Med (1991) 57(4):363–70. doi: 10.1055/s-2006-960119 [DOI] [PubMed] [Google Scholar]
- 35. Rabinkov A, Miron T, Mirelman D, Wilchek M, Glozman S, Yavin E, et al. S-allylmercaptoglutathione: the reaction product of allicin with glutathione possesses SH-modifying and antioxidant properties. Biochim Biophys Acta (2000) 1499(1-2):144–53. doi: 10.1016/S0167-4889(00)00119-1 [DOI] [PubMed] [Google Scholar]
- 36. Bastaki SMA, Ojha S, Kalasz H, Adeghate E. Chemical constituents and medicinal properties of allium species. Mol Cell Biochem (2021) 476(12):4301–21. doi: 10.1007/s11010-021-04213-2 [DOI] [PubMed] [Google Scholar]
- 37. Iciek M, Kwiecien I, Wlodek L. Biological properties of garlic and garlic-derived organosulfur compounds. Environ Mol Mutagen (2009) 50(3):247–65. doi: 10.1002/em.20474 [DOI] [PubMed] [Google Scholar]
- 38. Rauf A, Abu-Izneid T, Thiruvengadam M, Imran M, Olatunde A, Shariati MA, et al. Garlic (Allium sativum l.): Its chemistry, nutritional composition, toxicity and anticancer properties. Curr Top Med Chem (2021) 22(11):957–72. doi: 10.2174/1568026621666211105094939 [DOI] [PubMed] [Google Scholar]
- 39. Cascajosa-Lira A, Prieto Ortega AI, Guzman-Guillen R, Catunescu GM, de la Torre JM, Guillamon E, et al. Simultaneous determination of allium compounds (Propyl propane thiosulfonate and thiosulfinate) in animal feed using UPLC-MS/MS. Food Chem Toxicol (2021) 157:112619. doi: 10.1016/j.fct.2021.112619 [DOI] [PubMed] [Google Scholar]
- 40. Kim S, Lee S, Shin D, Yoo M. Change in organosulfur compounds in onion (Allium cepa l.) during heat treatment. Food Sci Biotechnol (2016) 25(1):115–9. doi: 10.1007/s10068-016-0017-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wetli HA, Brenneisen R, Tschudi I, Langos M, Bigler P, Sprang T, et al. A gamma-glutamyl peptide isolated from onion (Allium cepa l.) by bioassay-guided fractionation inhibits resorption activity of osteoclasts. J Agric Food Chem (2005) 53(9):3408–14. doi: 10.1021/jf040457i [DOI] [PubMed] [Google Scholar]
- 42. Nohara T, Fujiwara Y, Kudo R, Yamaguchi K, Ikeda T, Murakami K, et al. Isolation and characterization of new onionins A2 and A3 from allium cepa, and of onionins A1, A2, and A3 from allium fistulosum. Chem Pharm Bull (Tokyo). (2014) 62(11):1141–5. doi: 10.1248/cpb.c14-00461 [DOI] [PubMed] [Google Scholar]
- 43. Ueda Y, Tsubuku T, Miyajima R. Composition of sulfur-containing components in onion and their flavor characters. Biosci Biotechnol Biochem (1994) 58(1):108–10. doi: 10.1271/bbb.58.108 [DOI] [PubMed] [Google Scholar]
- 44. Wang H, Li J, Wang Z, Zhang X, Ni Y. Modified method for rapid quantitation of s-alk(en)yl-L-cysteine sulfoxide in yellow onions (Allium cepa l.). J Agric Food Chem (2007) 55(14):5429–35. doi: 10.1021/jf070298d [DOI] [PubMed] [Google Scholar]
- 45. Fernandes S, Gois A, Mendes F, Perestrelo R, Medina S, Camara JS. Typicality assessment of onions (Allium cepa) from different geographical regions based on the volatile signature and chemometric tools. Foods (2020) 9(3):375. doi: 10.3390/foods9030375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Tigu AB, Moldovan CS, Toma VA, Farcas AD, Mot AC, Jurj A, et al. Phytochemical analysis and In vitro effects of allium fistulosum l. and allium sativum l. extracts on human normal and tumor cell lines: A comparative study. Molecules (2021) 26(3):574. doi: 10.3390/molecules26030574 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Yang HJ, Kim MJ, Qiu JY, Zhang T, Wu X, Jang DJ, et al. Rice porridge containing welsh onion root water extract alleviates osteoarthritis-related pain behaviors, glucose levels, and bone metabolism in osteoarthritis-induced ovariectomized rats. Nutrients (2019) 11(7):1503. doi: 10.3390/nu11071503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Park H, Jeong J, Hyun H, Kim J, Kim H, Oh HI, et al. Effects of a hot-water extract of allium hookeri roots on bone formation in human osteoblast-like MG-63 cells In vitro and in rats in vivo. Planta Med (2016) 82(16):1410–5. doi: 10.1055/s-0042-108733 [DOI] [PubMed] [Google Scholar]
- 49. Kim S, Kim DB, Lee S, Park J, Shin D, Yoo M. Profiling of organosulphur compounds using HPLC-PDA and GC/MS system and antioxidant activities in hooker chive (Allium hookeri). Nat Prod Res (2016) 30(24):2798–804. doi: 10.1080/14786419.2016.1164700 [DOI] [PubMed] [Google Scholar]
- 50. Jang JY, Lee MJ, You BR, Jin JS, Lee SH, Yun YR, et al. Allium hookeri root extract exerts anti-inflammatory effects by nuclear factor-kappaB down-regulation in lipopolysaccharide-induced RAW264.7 cells. BMC Complement Altern Med (2017) 17(1):126. doi: 10.1186/s12906-017-1633-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Kim HJ, Lee SH, Lee SH, Lee J, Kim H, Chang GT, et al. Longitudinal bone growth stimulating effect of allium macrostemon in adolescent female rats. Molecules (2020) 25(22):5449. doi: 10.3390/molecules25225449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Bernaert N, Goetghebeur L, De Clercq H, De Loose M, Daeseleire E, Van Pamel E, et al. Influence of cultivar and harvest time on the amounts of isoalliin and methiin in leek (Allium ampeloprasum var. porrum). J Agric Food Chem (2012) 60(44):10910–9. doi: 10.1021/jf302132a [DOI] [PubMed] [Google Scholar]
- 53. Kubec R, Dadakova E. Chromatographic methods for determination of s-substituted cysteine derivatives–a comparative study. J Chromatogr A. (2009) 1216(41):6957–63. doi: 10.1016/j.chroma.2009.08.032 [DOI] [PubMed] [Google Scholar]
- 54. Jeong J, Park H, Hyun H, Kim J, Kim H, Oh HI, et al. Effects of glucosinolates from turnip (Brassica rapa l.) root on bone formation by human osteoblast-like MG-63 cells and in normal young rats. Phytother Res (2015) 29(6):902–9. doi: 10.1002/ptr.5331 [DOI] [PubMed] [Google Scholar]
- 55. Barbieri GPR, Maggio A, De Pascale S, Fogliano V. Glucosinolates profile of brassica rapa l. subsp. sylvestris l. janch. var. esculenta hort. Food Chem (2008) 107(4):1687–91. doi: 10.1016/j.foodchem.2007.09.054 [DOI] [Google Scholar]
- 56. Cramer JM, Teran-Garcia M, Jeffery EH. Enhancing sulforaphane absorption and excretion in healthy men through the combined consumption of fresh broccoli sprouts and a glucoraphanin-rich powder. Br J Nutr (2012) 107(9):1333–8. doi: 10.1017/S0007114511004429 [DOI] [PubMed] [Google Scholar]
- 57. Liang H, Li C, Yuan Q, Vriesekoop F. Separation and purification of sulforaphane from broccoli seeds by solid phase extraction and preparative high-performance liquid chromatography. J Agric Food Chem (2007) 55(20):8047–53. doi: 10.1021/jf0706833 [DOI] [PubMed] [Google Scholar]
- 58. Hashem FA, Motawea H, El-Shabrawy AE, Shaker K, El-Sherbini S. Myrosinase hydrolysates of brassica oleraceae l. var. italica reduce the risk of colon cancer. Phytother Res (2012) 26(5):743–7. doi: 10.1002/ptr.3591 [DOI] [PubMed] [Google Scholar]
- 59. Abdallah HM, Farag MA, Algandaby MM, Nasrullah MZ, Abdel-Naim AB, Eid BG, et al. Osteoprotective activity and metabolite fingerprint via UPLC/MS and GC/MS of lepidium sativum in ovariectomized rats. Nutrients (2020) 12(7):2075. doi: 10.3390/nu12072075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Robin AH, Yi GE, Laila R, Yang K, Park JI, Kim HR, et al. Expression profiling of glucosinolate biosynthetic genes in brassica oleracea l. var. capitata inbred lines reveals their association with glucosinolate content. Molecules (2016) 21(6):787. doi: 10.3390/molecules21060787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Soengas P, Velasco P, Fernandez JC, Cartea ME. New vegetable brassica foods: A promising source of bioactive compounds. Foods (2021) 10(12):2911. doi: 10.3390/foods10122911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Bell L, Oruna-Concha MJ, Wagstaff C. Identification and quantification of glucosinolate and flavonol compounds in rocket salad (Eruca sativa, eruca vesicaria and diplotaxis tenuifolia) by LC-MS: highlighting the potential for improving nutritional value of rocket crops. Food Chem (2015) 172:852–61. doi: 10.1016/j.foodchem.2014.09.116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Gerendas J, Breuning S, Stahl T, Mersch-Sundermann V, Muhling KH. Isothiocyanate concentration in kohlrabi (Brassica oleracea l. var. gongylodes) plants as influenced by sulfur and nitrogen supply. J Agric Food Chem (2008) 56(18):8334–42. doi: 10.1021/jf800399x [DOI] [PubMed] [Google Scholar]
- 64. Marcinkowska M, Frank S, Steinhaus M, Jelen HH. Key odorants of raw and cooked green kohlrabi (Brassica oleracea var. gongylodes l.). J Agric Food Chem (2021) 69(41):12270–7. doi: 10.1021/acs.jafc.1c04339 [DOI] [PubMed] [Google Scholar]
- 65. Manivannan A, Kim JH, Kim DS, Lee ES, Lee HE. Deciphering the nutraceutical potential of raphanus sativus-a comprehensive overview. Nutrients (2019) 11(2):402. doi: 10.3390/nu11020402 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Giorgetti L, Giorgi G, Cherubini E, Gervasi PG, Della Croce CM, Longo V, et al. Screening and identification of major phytochemical compounds in seeds, sprouts and leaves of Tuscan black kale brassica oleracea (L.) ssp acephala (DC) var. sabellica l. Nat Prod Res (2018) 32(14):1617–26. doi: 10.1080/14786419.2017.1392953 [DOI] [PubMed] [Google Scholar]
- 67. Liu Z, Hirani AH, McVetty PB, Daayf F, Quiros CF, Li G. Reducing progoitrin and enriching glucoraphanin in brassica napus seeds through silencing of the GSL-ALK gene family. Plant Mol Biol (2012) 79(1-2):179–89. doi: 10.1007/s11103-012-9905-2 [DOI] [PubMed] [Google Scholar]
- 68. Ku KM, Kim MJ, Jeffery EH, Kang YH, Juvik JA. Profiles of glucosinolates, their hydrolysis products, and quinone reductase inducing activity from 39 arugula (Eruca sativa mill.) accessions. J Agric Food Chem (2016) 64(34):6524–32. doi: 10.1021/acs.jafc.6b02750 [DOI] [PubMed] [Google Scholar]
- 69. Rektorisova M, Hrbek V, Jiru M, Ovesna J, Hajslova J. Variability in s-Alk(en)yl-L-Cysteine sulfoxides in garlic within a seven-month period determined by a liquid chromatography - tandem mass spectrometry method. Plant Foods Hum Nutr (2020) 75(3):376–82. doi: 10.1007/s11130-020-00817-z [DOI] [PubMed] [Google Scholar]
- 70. Rose P, Whiteman M, Moore PK, Zhu YZ. Bioactive s-alk(en)yl cysteine sulfoxide metabolites in the genus allium: the chemistry of potential therapeutic agents. Nat Prod Rep (2005) 22(3):351–68. doi: 10.1039/b417639c [DOI] [PubMed] [Google Scholar]
- 71. Kodera Y, Kurita M, Nakamoto M, Matsutomo T. Chemistry of aged garlic: Diversity of constituents in aged garlic extract and their production mechanisms via the combination of chemical and enzymatic reactions. Exp Ther Med (2020) 19(2):1574–84. doi: 10.3892/etm.2019.8393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Yoshimoto N, Saito K. S-alk(en)ylcysteine sulfoxides in the genus allium: proposed biosynthesis, chemical conversion, and bioactivities. J Exp Bot (2019) 70(16):4123–37. doi: 10.1093/jxb/erz243 [DOI] [PubMed] [Google Scholar]
- 73. Block E. Recent results in the organosulfur and organoselenium chemistry of genus allium and brassica plants. relevance for cancer prevention. Adv Exp Med Biol (1996) 401:155–69. doi: 10.1007/978-1-4613-0399-2_13 [DOI] [PubMed] [Google Scholar]
- 74. Calvey EM, White KD, Matusik JE, Sha D, Block E. Allium chemistry: identification of organosulfur compounds in ramp (Allium tricoccum) homogenates. Phytochemistry (1998) 49(2):359–64. doi: 10.1016/S0031-9422(98)00191-5 [DOI] [PubMed] [Google Scholar]
- 75. Prieto MA, Lopez CJ, Simal-Gandara J. Glucosinolates: Molecular structure, breakdown, genetic, bioavailability, properties and healthy and adverse effects. Adv Food Nutr Res (2019) 90:305–50. doi: 10.1016/bs.afnr.2019.02.008 [DOI] [PubMed] [Google Scholar]
- 76. Shekarri Q, Dekker M. A physiological-based model for simulating the bioavailability and kinetics of sulforaphane from broccoli products. Foods (2021) 10(11):2761. doi: 10.3390/foods10112761 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77. Angelino DJ E. Glucosinolate hydrolysis and bioavailability of resulting isothiocyanates: Focus on glucoraphanin. J Funct Foods (2014) 7:67–76. doi: 10.1016/j.jff.2013.09.029 [DOI] [Google Scholar]
- 78. Shapiro TA, Fahey JW, Wade KL, Stephenson KK, Talalay P. Human metabolism and excretion of cancer chemoprotective glucosinolates and isothiocyanates of cruciferous vegetables. Cancer Epidemiol Biomarkers Prev (1998) 7(12):1091–100. [PubMed] [Google Scholar]
- 79. Datta HK, Ng WF, Walker JA, Tuck SP, Varanasi SS. The cell biology of bone metabolism. J Clin Pathol (2008) 61(5):577–87. doi: 10.1136/jcp.2007.048868 [DOI] [PubMed] [Google Scholar]
- 80. Ryuk JA. Effect of allium fistulosum extracts on the stimulation of longitudinal bone growth in animal modeling diet-induced calcium and vitamin d deficiencies. Appl Sci (2021) 11(17):7786. doi: 10.3390/app11177786 [DOI] [Google Scholar]
- 81. Tang CH, Huang TH, Chang CS, Fu WM, Yang RS. Water solution of onion crude powder inhibits RANKL-induced osteoclastogenesis through ERK, p38 and NF-kappaB pathways. Osteoporos Int (2009) 20(1):93–103. doi: 10.1007/s00198-008-0630-2 [DOI] [PubMed] [Google Scholar]
- 82. Bose S, Banerjee D, Vu AA. Ginger and garlic extracts enhance osteogenesis in 3D printed calcium phosphate bone scaffolds with bimodal pore distribution. ACS Appl Mater Interfaces (2022) 4(11):12964–75. doi: 10.1021/acsami.1c19617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Behera J, Ison J, Rai H, Tyagi N. Allyl sulfide promotes osteoblast differentiation and bone density via reducing mitochondrial DNA release mediated Kdm6b/H3K27me3 epigenetic mechanism. Biochem Biophys Res Commun (2021) 543:87–94. doi: 10.1016/j.bbrc.2021.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Monarrez-Cordero BE, Rodriguez-Gonzalez CA, Valencia-Gomez LE, Hernandez-Paz JF, Martel-Estrada SA, Camacho-Montes H, et al. The effect of allium cepa extract on the chitosan/PLGA scaffolds bioactivity. J Appl Biomater Funct Mater (2021) 19:2280800021989701. doi: 10.1177/2280800021989701 [DOI] [PubMed] [Google Scholar]
- 85. Law YY, Chiu HF, Lee HH, Shen YC, Venkatakrishnan K, Wang CK. Consumption of onion juice modulates oxidative stress and attenuates the risk of bone disorders in middle-aged and post-menopausal healthy subjects. Food Funct (2016) 7(2):902–12. doi: 10.1039/C5FO01251A [DOI] [PubMed] [Google Scholar]
- 86. Yang J, Tang R, Yi J, Chen Y, Li X, Yu T, et al. Diallyl disulfide alleviates inflammatory osteolysis by suppressing osteoclastogenesis via NF-kappaB-NFATc1 signal pathway. FASEB J (2019) 33(6):7261–73. doi: 10.1096/fj.201802172R [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Chen Y, Sun J, Dou C, Li N, Kang F, Wang Y, et al. Alliin attenuated RANKL-induced osteoclastogenesis by scavenging reactive oxygen species through inhibiting Nox1. Int J Mol Sci (2016) 17(9):1516. doi: 10.3390/ijms17091516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Weisstaub AR, Salinas MV, Correa MJ, Barchuk M, Berg G, Zuleta A. Effects of the intake of white wheat bread added with garlic and resistant starch: action on calcium bioavailability and metabolic parameters of growing wistar rats. Food Funct (2018) 9(11):5707–14. doi: 10.1039/C8FO01407H [DOI] [PubMed] [Google Scholar]
- 89. El-Sayyad HI, Abou-El-Naga AM, Gadallah AA, Bakr IH. Protective effects of allium sativum against defects of hypercholesterolemia on pregnant rats and their offspring. Int J Clin Exp Med (2010) 3(2):152–63. [PMC free article] [PubMed] [Google Scholar]
- 90. Mukherjee M, Das AS, Mitra S, Mitra C. Prevention of bone loss by oil extract of garlic (Allium sativum linn.) in an ovariectomized rat model of osteoporosis. Phytother Res (2004) 18(5):389–94. doi: 10.1002/ptr.1448 [DOI] [PubMed] [Google Scholar]
- 91. Mukherjee M, Das AS, Das D, Mukherjee S, Mitra S, Mitra C. Effects of garlic oil on postmenopausal osteoporosis using ovariectomized rats: comparison with the effects of lovastatin and 17beta-estradiol. Phytother Res (2006) 20(1):21–7. doi: 10.1002/ptr.1795 [DOI] [PubMed] [Google Scholar]
- 92. Mukherjee M, Das AS, Das D, Mukherjee S, Mitra S, Mitra C. Role of oil extract of garlic (Allium sativum linn.) on intestinal transference of calcium and its possible correlation with preservation of skeletal health in an ovariectomized rat model of osteoporosis. Phytother Res (2006) 20(5):408–15. doi: 10.1002/ptr.1888 [DOI] [PubMed] [Google Scholar]
- 93. Mukherjee M, Das AS, Das D, Mukherjee S, Mitra S, Mitra C. Role of peritoneal macrophages and lymphocytes in the development of hypogonadal osteoporosis in an ovariectomized rat model: possible phytoestrogenic efficacy of oil extract of garlic to preserve skeletal health. Phytother Res (2007) 21(11):1045–54. doi: 10.1002/ptr.2209 [DOI] [PubMed] [Google Scholar]
- 94. Huang TH, Muhlbauer RC, Tang CH, Chen HI, Chang GL, Huang YW, et al. Onion decreases the ovariectomy-induced osteopenia in young adult rats. Bone (2008) 42(6):1154–63. doi: 10.1016/j.bone.2008.01.032 [DOI] [PubMed] [Google Scholar]
- 95. Li D, Liang H, Li Y, Zhang J, Qiao L, Luo H. Allicin alleviates lead-induced bone loss by preventing oxidative stress and osteoclastogenesis Via SIRT1/FOXO1 pathway in mice. Biol Trace Elem Res (2021) 199(1):237–43. doi: 10.1007/s12011-020-02136-5 [DOI] [PubMed] [Google Scholar]
- 96. Liu Y, You M, Shen J, Xu Y, Li L, Wang D, et al. Allicin reversed the process of frailty in aging Male Fischer 344 rats with osteoporosis. J Gerontol A Biol Sci Med Sci (2020) 75(5):821–5. doi: 10.1093/gerona/glz205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Thaler R, Maurizi A, Roschger P, Sturmlechner I, Khani F, Spitzer S, et al. Anabolic and antiresorptive modulation of bone homeostasis by the epigenetic modulator sulforaphane, a naturally occurring isothiocyanate. J Biol Chem (2016) 291(13):6754–71. doi: 10.1074/jbc.M115.678235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98. Gambari L, Barone M, Amore E, Grigolo B, Filardo G, Iori R, et al. Glucoraphanin increases intracellular hydrogen sulfide (H2S) levels and stimulates osteogenic differentiation in human mesenchymal stromal cell. Nutrients (2022) 14(3):435. doi: 10.3390/nu14030435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Kang IS, Agidigbi TS, Kwon YM, Kim DG, Kim RI, In G, et al. Effect of Co-administration of panax ginseng and brassica oleracea on postmenopausal osteoporosis in ovariectomized mice. Nutrients (2020) 12(8):2415. doi: 10.3390/nu12082415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Xue P, Hu X, Powers J, Nay N, Chang E, Kwon J, et al. CDDO-me, sulforaphane and tBHQ attenuate the RANKL-induced osteoclast differentiation via activating the NRF2-mediated antioxidant response. Biochem Biophys Res Commun (2019) 511(3):637–43. doi: 10.1016/j.bbrc.2019.02.095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101. Takagi T, Inoue H, Takahashi N, Katsumata-Tsuboi R, Uehara M. Sulforaphane inhibits osteoclast differentiation by suppressing the cell-cell fusion molecules DC-STAMP and OC-STAMP. Biochem Biophys Res Commun (2017) 483(1):718–24. doi: 10.1016/j.bbrc.2016.12.075 [DOI] [PubMed] [Google Scholar]
- 102. Kim SJ, Kang SY, Shin HH, Choi HS. Sulforaphane inhibits osteoclastogenesis by inhibiting nuclear factor-kappaB. Mol Cells (2005) 20(3):364–70. [PubMed] [Google Scholar]
- 103. Luo T, Fu X, Liu Y, Ji Y, Shang Z. Sulforaphane inhibits osteoclastogenesis via suppression of the autophagic pathway. Molecules (2021) 26(2):34. doi: 10.3390/molecules26020347 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104. Gambari L, Lisignoli G, Cattini L, Manferdini C, Facchini A, Grassi F. Sodium hydrosulfide inhibits the differentiation of osteoclast progenitor cells via NRF2-dependent mechanism. Pharmacol Res (2014) 87:99–112. doi: 10.1016/j.phrs.2014.06.014 [DOI] [PubMed] [Google Scholar]
- 105. Javaheri B, Poulet B, Aljazzar A, de Souza R, Piles M, Hopkinson M, et al. Stable sulforaphane protects against gait anomalies and modifies bone microarchitecture in the spontaneous STR/Ort model of osteoarthritis. Bone (2017) 103:308–17. doi: 10.1016/j.bone.2017.07.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106. Elshal MF, Almalki AL, Hussein HK, Khan JA. Synergistic antiosteoporotic effect of lepidium sativum and alendronate in glucocorticoid-induced osteoporosis in wistar rats. Afr J Tradit Complement Altern Med (2013) 10(5):267–73. doi: 10.4314/ajtcam.v10i5.8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107. El-Haroun H. Comparative study on the possible protective effect of lepidium sativum versus teriparatide in induced osteoporosis in adult Male Guinea pigs. Egiptian J Hystol (2020) 43(3):931–47. doi: 10.21608/ejh.2020.18855.1193 [DOI] [Google Scholar]
- 108. Zhang Y, Yu L, Ao M, Jin W. Effect of ethanol extract of lepidium meyenii walp. on osteoporosis in ovariectomized rat. J Ethnopharmacol (2006) 105(1-2):274–9. doi: 10.1016/j.jep.2005.12.013 [DOI] [PubMed] [Google Scholar]
- 109. Gorinstein S, Leontowicz H, Leontowicz M, Namiesnik J, Najman K, Drzewiecki J, et al. Comparison of the main bioactive compounds and antioxidant activities in garlic and white and red onions after treatment protocols. J Agric Food Chem (2008) 56(12):4418–26. doi: 10.1021/jf800038h [DOI] [PubMed] [Google Scholar]
- 110. Kothari D, Lee WD, Niu KM, Kim SK. The genus allium as poultry feed additive: A review. Anim (Basel). (2019) 9(12):1032. doi: 10.3390/ani9121032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Sobolewska D, Michalska K, Podolak I, Grabowska K. Steroidal saponins from the genus allium. Phytochem Rev (2016) 15:1–35. doi: 10.1007/s11101-014-9381-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. Raiola A, Errico A, Petruk G, Monti DM, Barone A, Rigano MM. Bioactive compounds in brassicaceae vegetables with a role in the prevention of chronic diseases. Molecules (2017) 23(1):15. doi: 10.3390/molecules23010015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113. Darvin P, Joung YH, Yang YM. JAK2-STAT5B pathway and osteoblast differentiation. JAKSTAT (2013) 2(4):e24931. doi: 10.4161/jkst.24931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Lin GL, Hankenson KD. Integration of BMP, wnt, and notch signaling pathways in osteoblast differentiation. J Cell Biochem (2011) 112(12):3491–501. doi: 10.1002/jcb.23287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115. Kang S, Bennett CN, Gerin I, Rapp LA, Hankenson KD, Macdougald OA. Wnt signaling stimulates osteoblastogenesis of mesenchymal precursors by suppressing CCAAT/enhancer-binding protein alpha and peroxisome proliferator-activated receptor gamma. J Biol Chem (2007) 282(19):14515–24. doi: 10.1074/jbc.M700030200 [DOI] [PubMed] [Google Scholar]
- 116. Jeon MJ, Kim JA, Kwon SH, Kim SW, Park KS, Park SW, et al. Activation of peroxisome proliferator-activated receptor-gamma inhibits the Runx2-mediated transcription of osteocalcin in osteoblasts. J Biol Chem (2003) 278(26):23270–7. doi: 10.1074/jbc.M211610200 [DOI] [PubMed] [Google Scholar]
- 117. Wang M, Jin H, Tang D, Huang S, Zuscik MJ, Chen D. Smad1 plays an essential role in bone development and postnatal bone formation. Osteoarthr Cartil (2011) 19(6):751–62. doi: 10.1016/j.joca.2011.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118. Meyers CA, Xu J, Asatrian G, Ding C, Shen J, Broderick K, et al. WISP-1 drives bone formation at the expense of fat formation in human perivascular stem cells. Sci Rep (2018) 8(1):15618. doi: 10.1038/s41598-018-34143-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Gambari L, Lisignoli G, Gabusi E, Manferdini C, Paolella F, Piacentini A, et al. Distinctive expression pattern of cystathionine-beta-synthase and cystathionine-gamma-lyase identifies mesenchymal stromal cells transition to mineralizing osteoblasts. J Cell Physiol (2017) 232(12):3574–85. doi: 10.1002/jcp.25825 [DOI] [PubMed] [Google Scholar]
- 120. Robling AG, Bonewald LF. The osteocyte: New insights. Annu Rev Physiol (2020) 82:485–506. doi: 10.1146/annurev-physiol-021119-034332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121. Kitaura H, Marahleh A, Ohori F, Noguchi T, Shen WR, Qi J, et al. Osteocyte-related cytokines regulate osteoclast formation and bone resorption. Int J Mol Sci (2020) 21(14):5169. doi: 10.3390/ijms21145169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122. Pautke C, Schieker M, Tischer T, Kolk A, Neth P, Mutschler W, et al. Characterization of osteosarcoma cell lines MG-63, saos-2 and U-2 OS in comparison to human osteoblasts. Anticancer Res (2004) 24(6):3743–8. [PubMed] [Google Scholar]
- 123. Juma A. The effects of lepidium sativum seeds on fracture-induced healing in rabbits. MedGenMed (2007) 9(2):23. doi: 10.1016/j.jep.2005.12.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Boyce BF. Advances in the regulation of osteoclasts and osteoclast functions. J Dent Res (2013) 92(10):860–7. doi: 10.1177/0022034513500306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125. Kim JM, Lin C, Stavre Z, Greenblatt MB, Shim JH. Osteoblast-osteoclast communication and bone homeostasis. Cells (2020) 9(9). doi: 10.3390/cells9092073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126. Gambari L, Grassi F, Roseti L, Grigolo B, Desando G. Learning from monocyte-macrophage fusion and multinucleation: Potential therapeutic targets for osteoporosis and rheumatoid arthritis. Int J Mol Sci (2020) 21(17):6001. doi: 10.3390/ijms21176001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. Kim JH, Kim N. Regulation of NFATc1 in osteoclast differentiation. J Bone Metab (2014) 21(4):233–41. doi: 10.11005/jbm.2014.21.4.233 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128. Lee NK, Choi YG, Baik JY, Han SY, Jeong DW, Bae YS, et al. A crucial role for reactive oxygen species in RANKL-induced osteoclast differentiation. Blood (2005) 106(3):852–9. doi: 10.1182/blood-2004-09-3662 [DOI] [PubMed] [Google Scholar]
- 129. Youn MY, Takada I, Imai Y, Yasuda H, Kato S. Transcriptionally active nuclei are selective in mature multinucleated osteoclasts. Genes Cells (2010) 15(10):1025–35. doi: 10.1111/j.1365-2443.2010.01441.x [DOI] [PubMed] [Google Scholar]
- 130. Costa AG, Cusano NE, Silva BC, Cremers S, Bilezikian JP. Cathepsin K: its skeletal actions and role as a therapeutic target in osteoporosis. Nat Rev Rheumatol (2011) 7(8):447–56. doi: 10.1038/nrrheum.2011.77 [DOI] [PubMed] [Google Scholar]
- 131. Miyamoto K, Ninomiya K, Sonoda KH, Miyauchi Y, Hoshi H, Iwasaki R, et al. MCP-1 expressed by osteoclasts stimulates osteoclastogenesis in an autocrine/paracrine manner. Biochem Biophys Res Commun (2009) 383(3):373–7. doi: 10.1016/j.bbrc.2009.04.020 [DOI] [PubMed] [Google Scholar]
- 132. Witwicka H, Hwang SY, Reyes-Gutierrez P, Jia H, Odgren PE, Donahue LR, et al. Studies of OC-STAMP in osteoclast fusion: A new knockout mouse model, rescue of cell fusion, and transmembrane topology. PloS One (2015) 10(6):e0128275. doi: 10.1371/journal.pone.0128275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133. Kensler TW, Wakabayashi N, Biswal S. Cell survival responses to environmental stresses via the Keap1-Nrf2-ARE pathway. Annu Rev Pharmacol Toxicol (2007) 47:89–116. doi: 10.1146/annurev.pharmtox.46.120604.141046 [DOI] [PubMed] [Google Scholar]
- 134. Kanzaki H, Shinohara F, Kajiya M, Kodama T. The Keap1/Nrf2 protein axis plays a role in osteoclast differentiation by regulating intracellular reactive oxygen species signaling. J Biol Chem (2013) 288(32):23009–20. doi: 10.1074/jbc.M113.478545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135. Dinkova-Kostova AT, Holtzclaw WD, Cole RN, Itoh K, Wakabayashi N, Katoh Y, et al. Direct evidence that sulfhydryl groups of Keap1 are the sensors regulating induction of phase 2 enzymes that protect against carcinogens and oxidants. Proc Natl Acad Sci U S A. (2002) 99(18):11908–13. doi: 10.1073/pnas.172398899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Bhattacharjee S, Dashwood RH. Epigenetic regulation of NRF2/KEAP1 by phytochemicals. Antioxid (Basel). (2020) 9(9):865. doi: 10.3390/antiox9090865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137. Yang H, Qin J, Wang X, Ei-Shora HM, Yu B. Production of plant-derived anticancer precursor glucoraphanin in chromosomally engineered escherichia coli. Microbiol Res (2020) 238:126484. doi: 10.1016/j.micres.2020.126484 [DOI] [PubMed] [Google Scholar]
- 138. Martelli A, Piragine E, Citi V, Testai L, Pagnotta E, Ugolini L, et al. Erucin exhibits vasorelaxing effects and antihypertensive activity by H2 s-releasing properties. Br J Pharmacol (2020) 177(4):824–35. doi: 10.1111/bph.14645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139. Yang G, Wu L, Jiang B, Yang W, Qi J, Cao K, et al. H2S as a physiologic vasorelaxant: hypertension in mice with deletion of cystathionine gamma-lyase. Science (2008) 322(5901):587–90. doi: 10.1126/science.1162667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Di Cesare Mannelli L, Lucarini E, Micheli L, Mosca I, Ambrosino P, Soldovieri MV, et al. Effects of natural and synthetic isothiocyanate-based H2S-releasers against chemotherapy-induced neuropathic pain: Role of Kv7 potassium channels. Neuropharmacology (2017) 121:49–59. doi: 10.1016/j.neuropharm.2017.04.029 [DOI] [PubMed] [Google Scholar]
- 141. Kida K, Marutani E, Nguyen RK, Ichinose F. Inhaled hydrogen sulfide prevents neuropathic pain after peripheral nerve injury in mice. Nitric Oxide (2015) 46:87–92. doi: 10.1016/j.niox.2014.11.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Xue R, Hao DD, Sun JP, Li WW, Zhao MM, Li XH, et al. Hydrogen sulfide treatment promotes glucose uptake by increasing insulin receptor sensitivity and ameliorates kidney lesions in type 2 diabetes. Antioxid Redox Signal (2013) 19(1):5–23. doi: 10.1089/ars.2012.5024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Giovinazzo D, Bursac B, Sbodio JI, Nalluru S, Vignane T, Snowman AM, et al. Hydrogen sulfide is neuroprotective in alzheimer's disease by sulfhydrating GSK3beta and inhibiting tau hyperphosphorylation. Proc Natl Acad Sci U.S.A. (2021) 118(4):e2017225118. doi: 10.1073/pnas.2017225118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Hine C, Harputlugil E, Zhang Y, Ruckenstuhl C, Lee BC, Brace L, et al. Endogenous hydrogen sulfide production is essential for dietary restriction benefits. Cell (2015) 160(1-2):132–44. doi: 10.1016/j.cell.2014.11.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Hine C, Mitchell JR. Calorie restriction and methionine restriction in control of endogenous hydrogen sulfide production by the transsulfuration pathway. Exp Gerontol. (2015) 68:26–32. doi: 10.1016/j.exger.2014.12.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Whiteman M, Winyard PG. Hydrogen sulfide and inflammation: the good, the bad, the ugly and the promising. Expert Rev Clin Pharmacol (2011) 4(1):13–32. doi: 10.1586/ecp.10.134 [DOI] [PubMed] [Google Scholar]
- 147. Benavides GA, Squadrito GL, Mills RW, Patel HD, Isbell TS, Patel RP, et al. Hydrogen sulfide mediates the vasoactivity of garlic. Proc Natl Acad Sci U S A. (2007) 104(46):17977–82. doi: 10.1073/pnas.0705710104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148. Liang D, Wu H, Wong MW, Huang D. Diallyl trisulfide is a fast H2S donor, but diallyl disulfide is a slow one: The reaction pathways and intermediates of glutathione with polysulfides. Org Lett (2015) 17(17):4196–9. doi: 10.1021/acs.orglett.5b01962 [DOI] [PubMed] [Google Scholar]
- 149. Citi V, Martelli A, Testai L, Marino A, Breschi MC, Calderone V. Hydrogen sulfide releasing capacity of natural isothiocyanates: is it a reliable explanation for the multiple biological effects of brassicaceae? Planta Med (2014) 80(8-9):610–3. doi: 10.1055/s-0034-1368591 [DOI] [PubMed] [Google Scholar]
- 150. Lucarini E, Micheli L, Trallori E, Citi V, Martelli A, Testai L, et al. Effect of glucoraphanin and sulforaphane against chemotherapy-induced neuropathic pain: Kv7 potassium channels modulation by H2 s release in vivo. Phytother Res (2018) 32(11):2226–34. doi: 10.1002/ptr.6159 [DOI] [PubMed] [Google Scholar]
- 151. Lucarini E, Pagnotta E, Micheli L, Parisio C, Testai L, Martelli A, et al. Eruca sativa meal against diabetic neuropathic pain: An H2S-mediated effect of glucoerucin. Molecules (2019) 24(16):3006. doi: 10.3390/molecules24163006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152. Martelli A, Piragine E, Gorica E, Citi V, Testai L, Pagnotta E, et al. The H2S-donor erucin exhibits protective effects against vascular inflammation in human endothelial and smooth muscle cells. Antioxid (Basel) (2021) 10(6):961. doi: 10.3390/antiox10060961 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Piragine E, Flori L, Di Cesare Mannelli L, Ghelardini C, Pagnotta E, Matteo R, et al. Eruca sativa mill. seed extract promotes anti-obesity and hypoglycemic effects in mice fed with a high-fat diet. Phytother Res (2021) 35(4):1983–90. doi: 10.1002/ptr.6941 [DOI] [PubMed] [Google Scholar]
- 154. Cai YR, Hu CH. Computational study of H2S release in reactions of diallyl polysulfides with thiols. J Phys Chem B (2017) 121(26):6359–66. doi: 10.1021/acs.jpcb.7b03683 [DOI] [PubMed] [Google Scholar]
- 155. Lin Y, Yang X, Lu Y, Liang D, Huang D. Isothiocyanates as H2S donors triggered by cysteine: Reaction mechanism and structure and activity relationship. Org Lett (2019) 21(15):5977–80. doi: 10.1021/acs.orglett.9b02117 [DOI] [PubMed] [Google Scholar]
- 156. Liu Y, Yang R, Liu X, Zhou Y, Qu C, Kikuiri T, et al. Hydrogen sulfide maintains mesenchymal stem cell function and bone homeostasis via regulation of Ca(2+) channel sulfhydration. Cell Stem Cell (2014) 15(1):66–78. doi: 10.1016/j.stem.2014.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Grassi F, Tyagi AM, Calvert JW, Gambari L, Walker LD, Yu M, et al. Hydrogen sulfide is a novel regulator of bone formation implicated in the bone loss induced by estrogen deficiency. J Bone Miner Res (2016) 31(5):949–63. doi: 10.1002/jbmr.2757 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Lee SK, Chung JH, Choi SC, Auh QS, Lee YM, Lee SI, et al. Sodium hydrogen sulfide inhibits nicotine and lipopolysaccharide-induced osteoclastic differentiation and reversed osteoblastic differentiation in human periodontal ligament cells. J Cell Biochem (2013) 114(5):1183–93. doi: 10.1002/jcb.24461 [DOI] [PubMed] [Google Scholar]
- 159. Ma J, Shi C, Liu Z, Han B, Guo L, Zhu L, et al. Hydrogen sulfide is a novel regulator implicated in glucocorticoids-inhibited bone formation. Aging (Albany NY). (2019) 11(18):7537–52. doi: 10.18632/aging.102269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160. Zheng W, Li X, Zhang T, Wang J. Biological mechanisms and clinical efficacy of sulforaphane for mental disorders. Gen Psychiatr (2022) 35(2):e100700. doi: 10.1136/gpsych-2021-100700 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161. Jiang X, Chen Y, Lu K, Zhang H, Fan X. GYY4137 promotes bone formation in a rabbit distraction osteogenesis model: a preliminary report. J Oral Maxillofac Surg (2015) 73(4):732.e1–6. doi: 10.1016/j.joms.2014.11.012 [DOI] [PubMed] [Google Scholar]
- 162. Sivapalan T, Melchini A, Saha S, Needs PW, Traka MH, Tapp H, et al. Bioavailability of glucoraphanin and sulforaphane from high-glucoraphanin broccoli. Mol Nutr Food Res (2018) 62(18):e1700911. doi: 10.1002/mnfr.201700911 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163. Fahey JW, Wade KL, Stephenson KK, Panjwani AA, Liu H, Cornblatt G, et al. Bioavailability of sulforaphane following ingestion of glucoraphanin-rich broccoli sprout and seed extracts with active myrosinase: A pilot study of the effects of proton pump inhibitor administration. Nutrients (2019) 11(7):1489. doi: 10.3390/nu11071489 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164. Lai RH, Miller MJ, Jeffery E. Glucoraphanin hydrolysis by microbiota in the rat cecum results in sulforaphane absorption. Food Funct (2010) 1(2):161–6. doi: 10.1039/c0fo00110d [DOI] [PubMed] [Google Scholar]
- 165. Bheemreddy RM, Jeffery EH. The metabolic fate of purified glucoraphanin in F344 rats. J Agric Food Chem (2007) 55(8):2861–6. doi: 10.1021/jf0633544 [DOI] [PubMed] [Google Scholar]
- 166. Liu X, Wang Y, Hoeflinger JL, Neme BP, Jeffery EH, Miller MJ. Dietary broccoli alters rat cecal microbiota to improve glucoraphanin hydrolysis to bioactive isothiocyanates. Nutrients (2017) 9(3):262. doi: 10.3390/nu9030262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167. Davidson R, Gardner S, Jupp O, Bullough A, Butters S, Watts L, et al. Isothiocyanates are detected in human synovial fluid following broccoli consumption and can affect the tissues of the knee joint. Sci Rep (2017) 7(1):3398. doi: 10.1038/s41598-017-03629-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Oliviero T, Lamers S, Capuano E, Dekker M, Verkerk R. Bioavailability of isothiocyanates from broccoli sprouts in protein, lipid, and fiber gels. Mol Nutr Food Res (2018) 62(18):e1700837. doi: 10.1002/mnfr.201700837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169. Dinkova-Kostova AT, Fahey JW, Kostov RV, Kensler TW. KEAP1 and done? targeting the NRF2 pathway with sulforaphane. Trends Food Sci Technol (2017) 69(Pt B):257–69. doi: 10.1016/j.tifs.2017.02.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170. Fahey JW, Wade KL, Wehage SL, Holtzclaw WD, Liu H, Talalay P, et al. Stabilized sulforaphane for clinical use: Phytochemical delivery efficiency. Mol Nutr Food Res (2017) 61(4). doi: 10.1002/mnfr.201600766 [DOI] [PubMed] [Google Scholar]
- 171. Gasparello J, Gambari L, Papi C, Rozzi A, Manicardi A, Corradini R, et al. High levels of apoptosis are induced in the human colon cancer HT-29 cell line by Co-administration of sulforaphane and a peptide nucleic acid targeting miR-15b-5p. Nucleic Acid Ther (2020) 30(3):164–74. doi: 10.1089/nat.2019.0825 [DOI] [PubMed] [Google Scholar]
- 172. Ullah MF. Sulforaphane (SFN): An isothiocyanate in a cancer chemoprevention paradigm. Medicines (Basel). (2015) 2(3):141–56. doi: 10.3390/medicines2030141 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173. Zhang Z, Garzotto M, Davis EW, 2nd, Mori M, Stoller WA, Farris PE, et al. Sulforaphane bioavailability and chemopreventive activity in men presenting for biopsy of the prostate gland: A randomized controlled trial. Nutr Cancer. (2020) 72(1):74–87. doi: 10.1080/01635581.2019.1619783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174. Jeon SM, Kim JE, Shin SK, Kwon EY, Jung UJ, Baek NI, et al. Randomized double-blind placebo-controlled trial of powdered brassica rapa ethanol extract on alteration of body composition and plasma lipid and adipocytokine profiles in overweight subjects. J Med Food (2013) 16(2):133–8. doi: 10.1089/jmf.2012.2249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175. Bahadoran Z, Tohidi M, Nazeri P, Mehran M, Azizi F, Mirmiran P. Effect of broccoli sprouts on insulin resistance in type 2 diabetic patients: a randomized double-blind clinical trial. Int J Food Sci Nutr (2012) 63(7):767–71. doi: 10.3109/09637486.2012.665043 [DOI] [PubMed] [Google Scholar]
- 176. Blekkenhorst LC, Bondonno CP, Lewis JR, Devine A, Zhu K, Lim WH, et al. Cruciferous and allium vegetable intakes are inversely associated with 15-year atherosclerotic vascular disease deaths in older adult women. J Am Heart Assoc (2017) 6(10):e006558. doi: 10.1161/JAHA.117.006558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Millen AE, Subar AF, Graubard BI, Peters U, Hayes RB, Weissfeld JL, et al. Fruit and vegetable intake and prevalence of colorectal adenoma in a cancer screening trial. Am J Clin Nutr (2007) 86(6):1754–64. doi: 10.1093/ajcn/86.5.1754 [DOI] [PubMed] [Google Scholar]
- 178. Traka MH, Melchini A, Coode-Bate J, Al Kadhi O, Saha S, Defernez M, et al. Transcriptional changes in prostate of men on active surveillance after a 12-mo glucoraphanin-rich broccoli intervention-results from the effect of sulforaphane on prostate CAncer PrEvention (ESCAPE) randomized controlled trial. Am J Clin Nutr (2019) 109(4):1133–44. doi: 10.1093/ajcn/nqz012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179. Matheson EM, Mainous AG, 3rd, Carnemolla MA. The association between onion consumption and bone density in perimenopausal and postmenopausal non-Hispanic white women 50 years and older. Menopause (2009) 16(4):756–9. doi: 10.1097/gme.0b013e31819581a5 [DOI] [PubMed] [Google Scholar]
- 180. Greco EA, Pietschmann P, Migliaccio S. Osteoporosis and sarcopenia increase frailty syndrome in the elderly. Front Endocrinol (Lausanne). (2019) 10:255. doi: 10.3389/fendo.2019.00255 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181. Sim M, Blekkenhorst LC, Lewis JR, Bondonno CP, Devine A, Zhu K, et al. Vegetable and fruit intake and injurious falls risk in older women: a prospective cohort study. Br J Nutr (2018) 120(8):925–34. doi: 10.1017/S0007114518002155 [DOI] [PubMed] [Google Scholar]
- 182. Gu Y, Zhang S, Wang J, Chi VTQ, Zhang Q, Liu L, et al. Relationship between consumption of raw garlic and handgrip strength in a large-scale adult population. Clin Nutr (2020) 39(4):1234–41. doi: 10.1016/j.clnu.2019.05.015 [DOI] [PubMed] [Google Scholar]
- 183. Sim M, Blekkenhorst LC, Lewis JR, Bondonno CP, Devine A, Zhu K, et al. Vegetable diversity, injurious falls, and fracture risk in older women: A prospective cohort study. Nutrients (2018) 10(8):1081. doi: 10.3390/nu10081081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184. Zuhra K, Tome CS, Forte E, Vicente JB, Giuffre A. The multifaceted roles of sulfane sulfur species in cancer-associated processes. Biochim Biophys Acta Bioenerg. (2021) 1862(2):148338. doi: 10.1016/j.bbabio.2020.148338 [DOI] [PubMed] [Google Scholar]
- 185. Kolluru GK, Shen X, Kevil CG. Reactive sulfur species: A new redox player in cardiovascular pathophysiology. Arterioscler Thromb Vasc Biol (2020) 40(4):874–84. doi: 10.1161/ATVBAHA.120.314084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186. Roda B, Zhang N, Gambari L, Grigolo B, Eller-Vainicher C, Gennari L, et al. Optimization of a monobromobimane (MBB) derivatization and RP-HPLC-FLD detection method for sulfur species measurement in human serum after sulfur inhalation treatment. Antioxid (Basel) (2022) 11(5):939. doi: 10.3390/antiox11050939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187. Chen K, Nakasone Y, Xie K, Sakao K, Hou DX. Modulation of allicin-free garlic on gut microbiome. Molecules (2020) 25(3):682. doi: 10.3390/molecules25030682 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188. Chen K, Xie K, Liu Z, Nakasone Y, Sakao K, Hossain A, et al. Preventive effects and mechanisms of garlic on dyslipidemia and gut microbiome dysbiosis. Nutrients (2019) 11(6):1225. doi: 10.3390/nu11061225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189. Keirns BH, Lucas EA, Smith BJ. Phytochemicals affect T helper 17 and T regulatory cells and gut integrity: implications on the gut-bone axis. Nutr Res (2020) 83:30–48. doi: 10.1016/j.nutres.2020.08.006 [DOI] [PubMed] [Google Scholar]
- 190. Lee SH, Bang S, Jang HH, Lee EB, Kim BS, Kim SH, et al. Effects of allium hookeri on gut microbiome related to growth performance in young broiler chickens. PloS One (2020) 15(1):e0226833. doi: 10.1371/journal.pone.0226833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191. Pacifici R. Bone remodeling and the microbiome. Cold Spring Harb Perspect Med (2018) 8(4):a031203. doi: 10.1101/cshperspect.a031203 [DOI] [PMC free article] [PubMed] [Google Scholar]