Background:
Sensation following anterolateral thigh (ALT) phalloplasty is traditionally viewed as inferior to sensation following radial forearm phalloplasty, potentially due to fewer nerve coaptations performed. Neural anatomy of the ALT is well described, with branches of the femoral nerve innervating the medial flap. The purpose of this article is to draw attention to these nerves as a potential source of additional coaptation in ALT phalloplasty allowing for dual flap innervation.
Methods:
A PRISMA literature review was conducted to assess nerve coaptations used in ALT phalloplasty. Anatomic location and territory of the nerves of the thigh in ALT phalloplasty cases are reviewed.
Results:
Seventeen articles discuss ALT phalloplasty innervation, and 16 mention the use of only one nerve coaptation with the lateral femoral cutaneous nerve. In our experience performing ALT phalloplasty, perforating branch(es) of the femoral nerve are the first nerve(s) encountered on the medial border of the ALT flap lying on the fascia over the sartorius. With a flap design where the urethra is based laterally, the femoral perforating nerves can innervate a significant portion of the phallic shaft (medial flap), where sensation is most desired.
Conclusions:
It is common practice to perform only one nerve coaptation in ALT phalloplasty with the lateral femoral cutaneous nerve. However, perforating branches of the femoral nerve consistently innervate medial skin of the ALT. The authors propose that the femoral perforating nerves, when present, can be used as additional nerves for coaptation in ALT phalloplasty to allow for dual innervation.
Takeaways
Question: Are multiple nerve coaptations possible in ALT phalloplasty?
Findings: There is a consistent yet minimally studied medial sensory nerve from the femoral system that innervates the ALT flap. Most reports of ALT phalloplasty perform one coaptation with the lateral femoral cutaneous nerve, potentially leaving the neo-phallus suboptimally innervated.
Meaning: Multiple nerve coaptations are routine in forearm phalloplasty; in contrast to current clinical practices of performing one coaptation in ALT phalloplasty, the availability of a second coaptation (medial femoral perforating nerves) may better meet patient goals and expectations regarding sensory outcomes.
INTRODUCTION
Optimal phallic sensation is a high priority for transmasculine individuals seeking phalloplasty.1,2 Anterolateral thigh (ALT) phalloplasty is a technique utilized in gender-affirming phalloplasty with innervation most commonly described utilizing the lateral femoral cutaneous nerve (LFCN) in a single coaptation.3 This differs from the more common radial forearm phalloplasty, where it is frequent for multiple nerve coaptations to be performed.4
Neural anatomy of the ALT flap has been previously described, with established presence of femoral perforating nerves, referred to as the superior and/or medial perforating nerves (SPN and MPN), innervating the medial flap.5,6 Use of these nerves in addition to the LFCN allows for multiple nerve coaptations in ALT phalloplasty. Despite this, dual innervation in ALT phalloplasty has been minimally described in the literature. This represents an opportunity to potentially improve sensory outcomes in ALT phalloplasty and better meet patient sensory needs and expectations. The purpose of this article is to review the anatomic distribution of innervation of the ALT flap as it relates to phalloplasty cases and highlight the possible role of the femoral perforating branches as an additional source of innervation.
METHODS
A PRISMA style literature review of the nerves used in ALT phalloplasty was done utilizing the PubMed database. (See figure, Supplemental Digital Content 1, which shows a flow diagram of a systematic review of the nerves used for coaptation in ALT phalloplasty, http://links.lww.com/PRSGO/C164.) Only articles discussing ALT phalloplasty and details of nerve coaptation were included. The number of nerve coaptations performed and the nerve used for innervation are reported (Table 1).
Table 1.
Results of a Systematic Review of the Nerves Used for Coaptation in ALT Phalloplasty
| LFCN | Femoral Perforating Nerves | |
|---|---|---|
| No. ALT articles | 17 | 1 |
RESULTS
Five hundred sixty-one articles mention phalloplasty, with 17 specifically discussing nerve coaptation in ALT phalloplasty. (See figure, Supplemental Digital Content 1, http://links.lww.com/PRSGO/C164.) The femoral perforating branches were not used or mentioned in 16 of these articles. In all 16 of these studies, only one nerve coaptation was performed using the LFCN. One article mentioned using the “medial femoral cutaneous nerve” in addition to the LFCN for coaptation in a single case report. “Medial femoral cutaneous” in this instance is likely a synonym for the femoral perforating branches, although these nerves innervate the anterior, not medial thigh skin.
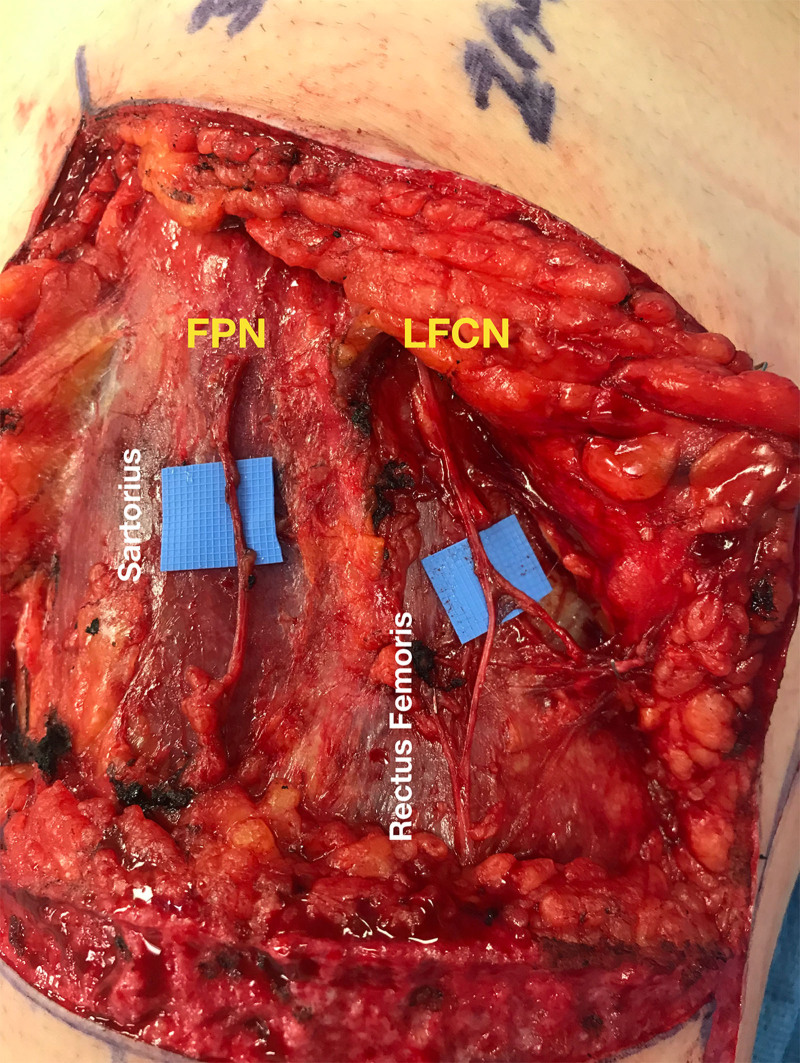
When performing ALT phalloplasty, we find that the femoral perforating branches are the first nerves visualized when dissecting from medial to lateral. They are found on the fascia overlying the sartorius (Figs. 1, 2). Proximally, they can be seen either penetrating through or traveling adjacent to the medial border of the sartorius (Fig. 3). The LFCN is seen more laterally on the fascia overlying the rectus femoris (Figs. 1, 2). The LFCN innervates the lateral and central aspects of the ALT, whereas the femoral perforating branches innervate the most medial aspects of the flap (Figs. 1, 2).
Fig. 1.
Innervation territory of the FPN and the LFCN in anterolateral thigh tube-in-tube phalloplasty. Note that in a design with the urethra based laterally, the phallic shaft is innervated largely by the more medial perforating branches from the femoral nerve. FPN indicates femoral perforating nerve.
Fig. 2.
The anterior and posterior branches of the LFCN are most commonly identified on the fascia overlying the rectus femoris and the septum between the vastus lateralis. The FPN branches are found medially overlying the sartorius muscle. FPN indicates femoral perforating nerve.
Fig. 3.
The femoral perforating branches will either penetrate the substance of the sartorius muscle or emerge just medial to its medial border.
DISCUSSION
The femoral perforating nerves are well described in cadaveric studies assessing innervation potential of the ALT flap and, in our experience, are frequently available in ALT phalloplasty cases as an additional source of flap innervation.5,6 Despite this clinical reality, on systematic review of the literature, only a single study reported using a medial femoral nerve for coaptation in phalloplasty. These nerves seem to be less known and less commonly used by surgeons in clinical practice. Unlike the LFCN, the femoral perforating nerves do not have described pain conditions (ie, meralgia paresthetica) associated with them and are less commonly seen in routine operations. The LFCN is commonly encountered in procedures, such as abdominoplasty and hernia repair, with known painful sequelae following iatrogenic injury, likely highlighting its clinical and educational importance.7
Two sensory branches of the femoral nerve primarily innervate the medial ALT flap: the SPN and the MPN. In a series of cadaveric ALT dissections, the LFCN was present in 29 of 29 (100%) cases, the SPN in 26 of 29 (89.7%) cases, and the MPN in 24 of 29 cases (82.8%).5,6 At least one femoral perforating nerve (SPN or MPN) was seen in 90% of dissections and is, therefore, available in many ALT phalloplasty cases. Local anesthetic injections in the study demonstrated the femoral perforating nerves innervating approximately 65% of flap territory.
ALT flap width used in phalloplasty is frequently greater than that typically seen for use in other reconstructive procedures. For this reason, flap margins typically extend further medial beyond the innervation territory of the LFCN, and may include territories that are innervated by these more medial sensory branches of the femoral nerve. Excluding these branches may lead to flap areas that are suboptimally innervated. Additionally, due to the size of the ALT flap in phalloplasty, the SPN and MPN are often routinely transected. Therefore, we have not identified additional morbidity in harvesting these nerves.
Being aware of the femoral perforating nerves as additional recipient nerves overall allows greater flexibility in targeting specific territories of the flap for innervation. When performing ALT phalloplasty at our center, the urethra is based laterally and the shaft medially. In these cases, the secondary source of innervation from the femoral perforating branches may represent a significant contribution to phallic shaft innervation, where sensation is most desired. We have had cases of ALT shaft-only phalloplasty (where the template is more narrower than traditional ALT phalloplasty), where the flap was not shifted medially enough to include the femoral perforating nerves, and, therefore, were only able to perform a single nerve coaptation with the LFCN. Now in our practice, knowledge of nerve topography is used for planning variations, such as shaft-only phalloplasty, to increase the chances of including both sources of innervation. This assists in placing the flap in an ideal location to include both the LFCN and femoral perforating nerves as centered as possible on each hemiside of the flap while accounting for perforator location. If unfamiliar with this anatomy, the femoral perforating nerves can easily be missed, transected, or even confused for the anterior branch of the LFCN. Notably, accurate nomenclature is critical to correctly report nerves coapted in phalloplasty to standardize the literature and better assess sensory outcomes.
In our experience, some patients may choose radial forearm phalloplasty over ALT due to the desire for multiple nerve coaptations. The ability to perform dual innervation of an ALT phalloplasty may have a significant impact on individual decision-making regarding ideal donor site as it relates to sensation. Although dual innervation will be available in many cases, some will not have femoral perforating branches of sufficient size, or the flap template, if based too lateral, will miss the femoral perforating nerves. These cases will have an ALT flap with dominant innervation by the LFCN.
This article is notably limited to a description of a surgical technique and its associated anatomy. Its purpose is to introduce the concept of a second nerve coaptation in ALT phalloplasty and serve as a launching pad for further investigations. Future studies are needed for assessing sensory outcomes and clinical and histologic comparisons between different recipient nerves in phalloplasty surgery.
In conclusion, the femoral perforating nerves can innervate a significant portion of the medial flap in ALT phalloplasty, yet their use is minimally described. We introduce the femoral perforating nerves, when present, for consideration as additional nerves for coaptation, allowing for dual innervation in ALT phalloplasty.
Supplementary Material
Footnotes
Published online 28 September 2022.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
Related Digital Media are available in the full-text version of the article on www.PRSGlobalOpen.com.
REFERENCES
- 1.van de Grift TC, Pigot GLS, Kreukels BPC, et al. Transmen’s experienced sexuality and genital gender-affirming surgery: findings from a clinical follow-up study. J Sex Marital Ther. 2019;45:201–205. [DOI] [PubMed] [Google Scholar]
- 2.Hage JJ, De Graaf FH. Addressing the ideal requirements by free flap phalloplasty: some reflections on refinements of technique. Microsurgery. 1993;14:592–598. [DOI] [PubMed] [Google Scholar]
- 3.Terrell M, Roberts W, Price CW, et al. Anatomy of the pedicled anterolateral thigh flap for phalloplasty in transitioning-males. Clin Anat. 2018;31:160–168. [DOI] [PubMed] [Google Scholar]
- 4.Peters BR. Optimizing innervation in radial forearm phalloplasty: consider the posterior antebrachial cutaneous nerve (PABC). Oral presentation at: United States Professional Association of Transgender Health (USPATH) Meeting: November 4th, 2022. Virtual. [DOI] [PubMed] [Google Scholar]
- 5.Luenam S, Prugsawan K, Kosiyatrakul A, et al. Neural anatomy of the anterolateral thigh flap. J Hand Microsurg. 2015;7:49–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ribuffo D, Cigna E, Gargano F, et al. The innervated anterolateral thigh flap: anatomical study and clinical implications. Plast Reconstr Surg. 2005;115:464–470. [DOI] [PubMed] [Google Scholar]
- 7.Sürücü HS, Tanyeli E, Sargon MF, et al. An anatomic study of the lateral femoral cutaneous nerve. Surg Radiol Anat. 1997;19:307–310. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.